Pathogen-Associated Molecular Patterns (PAMPs): From Innate Immune Sensing to Therapeutic Targeting in Inflammatory Diseases
This article provides a comprehensive overview of Pathogen-Associated Molecular Patterns (PAMPs) and their critical role in initiating inflammatory responses.
Pathogen-Associated Molecular Patterns (PAMPs): From Innate Immune Sensing to Therapeutic Targeting in Inflammatory Diseases
Abstract
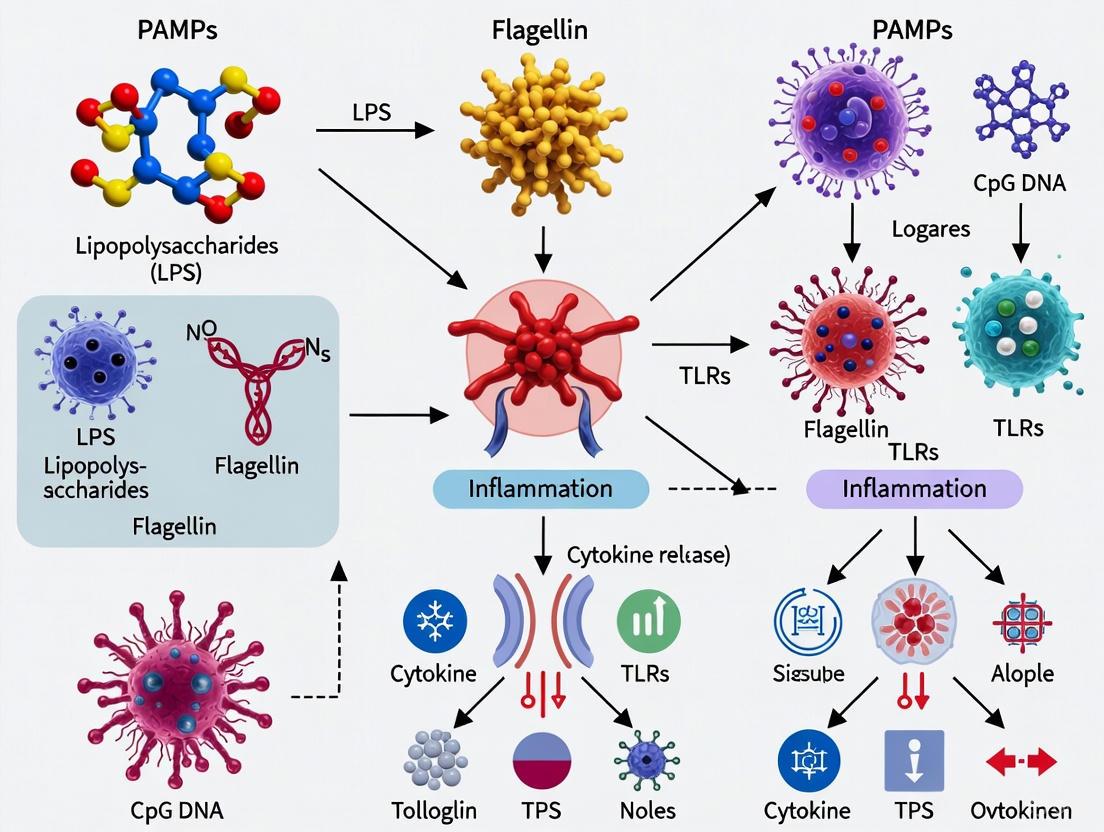
This article provides a comprehensive overview of Pathogen-Associated Molecular Patterns (PAMPs) and their critical role in initiating inflammatory responses. Tailored for researchers, scientists, and drug development professionals, we explore the foundational biology of PAMPs and their recognition by Pattern Recognition Receptors (PRRs), detailing the subsequent signaling cascades that activate innate immunity. The content extends to methodological approaches for studying PAMP-PRR interactions, addresses challenges in discriminating pathogenic signals from non-threatening microbial noise, and compares immune responses across diverse pathogens. By synthesizing current research and emerging concepts like lifestyle-associated molecular patterns (LAMPs), this review aims to bridge fundamental immunology with translational applications for diagnosing and treating infectious, chronic inflammatory, and autoimmune diseases.
The First Line of Defense: Understanding PAMPs, PRRs, and the Innate Immune Alarm System
Pathogen-Associated Molecular Patterns (PAMPs) represent a cornerstone concept in immunology, providing the foundational mechanism by which innate immune systems detect invading microorganisms. These evolutionarily conserved molecular motifs are exclusively expressed by microbial pathogens and absent in the host, enabling precise discrimination between "self" and "non-self" [1] [2]. PAMPs are recognized by specialized pattern recognition receptors (PRRs), triggering immediate antimicrobial and inflammatory responses while bridging innate and adaptive immunity [3] [4]. This technical review comprehensively examines PAMP classification, recognition mechanisms, signaling pathways, and experimental methodologies, with particular emphasis on recent advances including viability-associated PAMPs (vita-PAMPs) and biofilm-associated molecular patterns (BAMPs) [5] [6]. The elucidation of PAMP-PRR interactions continues to revolutionize our understanding of immune initiation and offers promising therapeutic avenues for inflammatory diseases, infections, and vaccine development.
The innate immune system constitutes the first line of defense against pathogenic microorganisms, employing a limited set of germline-encoded pattern recognition receptors (PRRs) to detect invariant molecular structures shared by broad classes of microbes [4]. These structures, termed Pathogen-Associated Molecular Patterns (PAMPs), represent essential components for microbial survival that remain evolutionarily conserved across pathogens but are distinct from host molecules [1] [2]. Charles Janeway first proposed the conceptual framework of PAMP recognition in 1989, hypothesizing that innate immune receptors must recognize conserved microbial products to trigger protective immunity [3] [2]. This revolutionary insight established the biological basis for how multicellular organisms distinguish infectious non-self from self.
PAMPs exhibit characteristic features that make them ideal recognition targets: (1) they are produced only by microorganisms, not by the host; (2) they recognize entire classes of pathogens rather than specific species; (3) they target molecular structures essential for microbial survival that cannot be easily discarded or mutated through evolution [2] [4]. The recognition of PAMPs by PRRs occurs in various cellular compartments, including plasma membranes, endosomal membranes, and the cytoplasm, enabling comprehensive immune surveillance against diverse pathogenic threats [3]. This initial recognition event triggers intracellular signaling cascades that culminate in the expression of proinflammatory molecules, initiating the early host response to infection and establishing a crucial bridge to adaptive immunity [4].
Major Classes of PAMPs and Their Recognition
PAMPs encompass diverse molecular structures including lipids, proteins, carbohydrates, and nucleic acids derived from bacteria, viruses, fungi, and protozoa. The table below summarizes the major PAMP classes, their microbial origins, and their corresponding recognition receptors.
Table 1: Major Classes of Pathogen-Associated Molecular Patterns
| PAMP Class | Specific Examples | Microbial Origin | Recognition Receptors |
|---|---|---|---|
| Bacterial Lipids | Lipopolysaccharide (LPS), Lipoteichoic acid (LTA) | Gram-negative bacteria, Gram-positive bacteria | TLR4/MD-2 (LPS), TLR2/TLR1 or TLR2/TLR6 (LTA) |
| Bacterial Proteins | Flagellin, Bacterial lipoproteins | Flagellated bacteria, Various pathogens | TLR5 (Flagellin), TLR2 heterodimers (Lipoproteins) |
| Bacterial Peptidoglycans | Peptidoglycan, Muramyl dipeptide | Gram-positive and Gram-negative bacteria | TLR2, NOD1, NOD2 |
| Viral Nucleic Acids | dsRNA, ssRNA, CpG DNA | RNA and DNA viruses | TLR3 (dsRNA), TLR7/8 (ssRNA), TLR9 (CpG DNA) |
| Fungal Carbohydrates | Zymosan, β-Glucan | Fungi | TLR2/TLR6, Dectin-1 |
| Bacterial Nucleic Acids | CpG DNA, rRNA | Bacteria | TLR9 (CpG DNA), TLR13 (bacterial rRNA in mice) |
The cellular localization of PRRs determines their specific PAMP recognition capabilities. Membrane-bound Toll-like receptors (TLRs) situated on cell surfaces or within endosomes typically recognize extracellular PAMPs. For instance, TLR4 complexed with MD-2 recognizes lipopolysaccharide (LPS) from Gram-negative bacteria, while TLR5 detects bacterial flagellin [1] [3]. Intracellular sensors including RIG-I-like receptors (RLRs) and NOD-like receptors (NLRs) detect microbial components that access the cytosol during infection. RIG-I and MDA5 sense viral RNA species, while NOD1 and NOD2 detect bacterial peptidoglycan fragments [1] [4]. This multi-compartmental surveillance system ensures comprehensive pathogen detection regardless of invasion route or replication strategy.
Recent conceptual expansions have refined the traditional PAMP paradigm. Viability-associated PAMPs (vita-PAMPs) represent a special class of microbial molecules that indicate metabolically active, replicating pathogens. Bacterial RNA exemplifies a vita-PAMP, as its synthesis ceases immediately upon microbial death, providing the immune system with a "warning sign" of active infection [5]. Similarly, biofilm-associated molecular patterns (BAMPs) constitute immunostimulatory molecules expressed specifically by biofilm-embedded bacteria, such as the simultaneous overexpression of alginate and Psl exopolysaccharides in Pseudomonas aeruginosa biofilms [6]. These specialized PAMP categories highlight the sophistication of immune recognition in distinguishing not merely microbial presence, but also metabolic state and lifestyle.
Pattern Recognition Receptors: Structure and Function
Pattern recognition receptors (PRRs) constitute a diverse protein family that specifically recognizes PAMPs and initiates downstream immune signaling. Based on protein domain homology and function, PRRs are classified into five major families: Toll-like receptors (TLRs), NOD-like receptors (NLRs), RIG-I-like receptors (RLRs), C-type lectin receptors (CLRs), and AIM2-like receptors (ALRs) [3]. These receptors share common structural organization featuring ligand recognition domains, intermediate domains, and effector domains that facilitate signal transduction upon PAMP engagement [3].
Toll-like receptors (TLRs) represent the most extensively characterized PRR family. These type I transmembrane glycoproteins contain extracellular leucine-rich repeat (LRR) domains responsible for PAMP recognition and intracellular Toll/IL-1 receptor (TIR) domains that mediate downstream signaling [3]. Humans encode 10 functional TLRs (TLR1-TLR10), while mice express 12 (TLR1-TLR9, TLR11-TLR13) [3]. TLRs localize to distinct cellular compartments: certain TLRs (TLR1, TLR2, TLR4, TLR5, TLR6, TLR10) reside on plasma membranes where they recognize microbial membrane components like lipids, lipoproteins, and proteins, while others (TLR3, TLR7, TLR8, TLR9) localize to endosomal membranes where they primarily detect microbial nucleic acids [3]. This strategic compartmentalization enables recognition of diverse PAMP classes while minimizing inappropriate activation by host molecules.
Cytosolic PRRs provide critical surveillance against intracellular pathogens. RIG-I-like receptors (RLRs), including RIG-I and MDA5, detect viral RNA in the cytoplasm. RIG-I recognizes short double-stranded RNA and RNA with 5'-triphosphates, while MDA5 senses long double-stranded RNA structures [1]. NOD-like receptors (NLRs) form large multi-protein complexes called inflammasomes that activate caspase-1 and process pro-inflammatory cytokines IL-1β and IL-18 [3]. The AIM2-like receptor (ALR) family detects cytosolic DNA, initiating inflammasome assembly and type I interferon responses [3]. This diverse PRR arsenal ensures comprehensive pathogen detection across all cellular compartments.
Table 2: Major Pattern Recognition Receptor Families and Their Characteristics
| PRR Family | Representative Members | Localization | Structural Features | PAMP Ligands |
|---|---|---|---|---|
| Toll-like Receptors (TLRs) | TLR4, TLR3, TLR9 | Plasma membrane, Endosomes | LRR extracellular/endosomal domain, TIR intracellular domain | LPS (TLR4), dsRNA (TLR3), CpG DNA (TLR9) |
| RIG-I-like Receptors (RLRs) | RIG-I, MDA5 | Cytoplasm | Caspase activation and recruitment domains (CARDs), DExD/H-box RNA helicase domain | Short dsRNA/5'-triphosphate RNA (RIG-I), long dsRNA (MDA5) |
| NOD-like Receptors (NLRs) | NOD1, NOD2, NLRP3 | Cytoplasm | CARD, PYD, or BIR domains; NACHT domain; LRR domain | Peptidoglycan fragments (NOD1/NOD2), various PAMPs/DAMPs (NLRP3) |
| C-type Lectin Receptors (CLRs) | Dectin-1, MR-CTLD4-7 | Plasma membrane | Carbohydrate recognition domain (CRD) | β-glucans (Dectin-1), Psl/Pel EPS (MR-CTLD4-7) |
| AIM2-like Receptors (ALRs) | AIM2 | Cytoplasm | HIN-200 domain, PYD domain | Cytosolic DNA |
PAMP-Triggered Signaling Pathways and Immune Activation
PAMP recognition by PRRs initiates sophisticated intracellular signaling cascades that orchestrate antimicrobial and inflammatory responses. These pathways demonstrate remarkable specificity, with different PRR families engaging distinct adaptor molecules and activation kinetics to generate tailored immune responses against diverse pathogens.
TLR Signaling Pathways
TLR signaling bifurcates into MyD88-dependent and TRIF-dependent pathways based on adaptor molecule utilization. Most TLRs (except TLR3) signal through the adaptor protein MyD88, ultimately activating NF-κB and MAPK pathways to induce proinflammatory cytokine production [3]. TLR3 exclusively utilizes the TRIF adaptor, while TLR4 employs both MyD88 and TRIF pathways [3]. TRIF-dependent signaling leads to IRF3 activation and type I interferon production, crucial for antiviral defense [3]. The specific signaling pathway engaged depends on both the TLR activated and the cell type involved, enabling customized immune responses against different pathogen classes.
Cytosolic PRR Signaling
Cytosolic RNA sensors including RIG-I and MDA5 signal through the mitochondrial antiviral signaling protein (MAVS), activating IRF3/7 and NF-κB to induce type I interferons and proinflammatory cytokines [1] [5]. NLR family members detect various intracellular PAMPs and DAMPs: NOD1 and NOD2 engage RIP2 kinase to activate NF-κB and MAPK pathways, while NLRP3 forms inflammasome complexes that process IL-1β and IL-18 through caspase-1 activation [3]. DNA sensors like AIM2 form inflammasomes, while cGAS produces the second messenger cGAMP that activates STING and subsequent type I interferon responses [5].
The following diagram illustrates the major signaling pathways triggered by PAMP recognition:
The integration of these signaling pathways coordinates a multifaceted immune response characterized by: (1) production of proinflammatory cytokines (TNF-α, IL-1β, IL-6) that activate immune cells and induce antimicrobial states; (2) secretion of type I interferons that establish antiviral defenses in neighboring cells; (3) increased expression of costimulatory molecules on antigen-presenting cells that facilitate adaptive immunity; and (4) induction of specialized cell death pathways (pyroptosis) that eliminate intracellular replication niches while promoting further inflammation [3] [4]. This coordinated response effectively contains infections while shaping subsequent adaptive immune mechanisms.
Experimental Protocols for PAMP Research
NETosis Induction and Quantification
Neutrophil extracellular trap (NET) formation represents an important antimicrobial mechanism triggered by PAMP recognition. The following protocol details NETosis induction and quantification:
Isolation of Human Neutrophils:
- Collect peripheral blood from healthy donors using heparin or EDTA anticoagulant.
- Separate neutrophils using density gradient centrifugation (e.g., Ficoll-Paque PLUS).
- Perform erythrocyte lysis using ammonium-chloride-potassium (ACK) buffer.
- Resuspend neutrophils in RPMI-1640 medium without serum at 1-5×10^6 cells/mL.
- Assess viability using trypan blue exclusion (>95% viability required).
NETosis Induction with PAMPs:
- Plate neutrophils on poly-L-lysine-coated coverslips or tissue culture plates.
- Stimulate with purified PAMPs: LPS (100 ng/mL), Pam3CSK4 (1 μg/mL), or bacterial RNA (1-5 μg/mL).
- Include positive controls: PMA (100 nM) or ionomycin (1 μM).
- Incubate at 37°C, 5% CO₂ for 2-4 hours.
- For inhibition studies, pre-treat with NADPH oxidase inhibitor (DPI, 10 μM) or PAD4 inhibitor (GSK484, 5 μM) for 1 hour before PAMP stimulation.
NET Quantification Methods:
- Immunofluorescence microscopy: Fix cells with 4% PFA, permeabilize with 0.1% Triton X-100, stain with anti-histone H3 (citrulline R2+R8+R17) antibody and anti-neutrophil elastase antibody, counterstain with DAPI. Quantify NET-forming cells as those exhibiting decondensed DNA colocalized with granular enzymes.
- SYTOX Green assay: Add cell-impermeable DNA dye SYTOX Green (5 μM) to culture supernatants. Measure fluorescence (excitation 504 nm, emission 523 nm) as indicator of extracellular DNA release.
- MPO-DNA complex ELISA: Capture NETs in supernatant using anti-MPO antibody, detect with anti-DNA peroxidase antibody and TMB substrate.
- Neutrophil elastase activity: Measure elastase activity in supernatants using N-methoxysuccinyl-AAPV-p-nitroanilide substrate (absorbance at 405 nm) [7].
Bacterial RNA Isolation and Transfection
Bacterial RNA serves as a prototypical vita-PAMP. The following protocol details its isolation and application in immune activation studies:
RNA Isolation from Bacteria:
- Culture bacteria to mid-logarithmic phase (OD₆₀₀ = 0.5-0.7).
- Stabilize RNA using RNA-protect Bacterial Reagent.
- Lyse bacteria using lysozyme (5 mg/mL) and proteinase K treatment.
- Isolve total RNA using commercial kits (e.g., RNeasy Mini Kit) with DNase I treatment.
- Assess RNA quality (RNA Integrity Number >8.0) and quantity using spectrophotometry.
- Confirm absence of genomic DNA contamination by PCR amplification of 16S rRNA gene.
Immune Cell Transfection and Stimulation:
- Culture immortalized macrophages (e.g., RAW264.7, THP-1) or primary bone marrow-derived macrophages in antibiotic-free medium.
- For TLR activation studies: Stimulate cells with extracellular bacterial RNA (1-5 μg/mL) in the presence or absence of chloroquine (20 μM) to inhibit endosomal acidification.
- For cytosolic RLR activation: Transfect cells with bacterial RNA using lipofectamine 2000 (1-2 μg RNA per 10⁶ cells).
- Collect supernatants at 6 hours (cytokine measurement) and 18 hours (type I IFN measurement).
- Analyze cytokine production via ELISA (IL-6, TNF-α, IL-1β, IFN-β) and gene expression via RT-qPCR for interferon-stimulated genes (ISGs) [5].
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Research Reagents for PAMP Studies
| Reagent Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| TLR Agonists | Ultrapure LPS (TLR4), Pam3CSK4 (TLR2/1), Poly(I:C) (TLR3), Imiquimod (TLR7) | PRR signaling studies, Immune cell activation | Verify purity (e.g., LAL testing for LPS), Use specific inhibitors to confirm receptor involvement |
| Cytosolic PRR Agonists | 3pRNA (RIG-I), Poly(I:C) HMW (MDA5), CDN (STING), dsDNA (AIM2/cGAS) | Intracellular pathogen recognition, Inflammasome activation | Optimize transfection method (lipofection, electroporation), Monitor cytotoxicity |
| PRR Inhibitors | TAK-242 (TLR4), Chloroquine (endosomal TLRs), BX795 (TBK1/IKKε), MCC950 (NLRP3) | Pathway validation, Therapeutic targeting | Assess specificity using multiple PRR agonists, Confirm inhibition of downstream signaling |
| Detection Antibodies | Phospho-specific IRF3, NF-κB p65, STAT1; Cytokine ELISA kits; Citrullinated histone H3 | Signaling pathway analysis, NETosis quantification | Validate species reactivity, Optimize staining conditions for phospho-epitopes |
| Cell Culture Models | Primary neutrophils/macrophages, THP-1, RAW264.7, HEK-Blue TLR reporter cells | Immune response characterization, Signaling studies | Differentiate THP-1 with PMA, Use primary cells for physiological relevance |
| Animal Models | TLR knockout mice, MYD88/TRIF knockout mice, Germ-free mice | In vivo validation, Host-pathogen interactions | Consider microbiota effects, Use appropriate infection models |
Research Implications and Therapeutic Applications
The elucidation of PAMP-PRR interactions has profound implications for understanding immune homeostasis, inflammatory diseases, and therapeutic development. Dysregulated PAMP recognition contributes to numerous pathologies: excessive TLR signaling drives septic shock, while inappropriate nucleic acid sensing underlies autoimmune disorders like lupus erythematosus [3] [7]. Conversely, defective PAMP recognition creates immunodeficiency states with increased infection susceptibility [4]. These insights have catalyzed novel therapeutic approaches targeting PAMP-PRR axes.
Vaccine adjuvants represent the most successful clinical application of PAMP research. TLR agonists including monophosphoryl lipid A (MPL, TLR4 agonist) and CpG oligonucleotides (TLR9 agonist) enhance vaccine efficacy by promoting dendritic cell maturation and robust adaptive immunity [1] [8]. Similarly, anticancer immunotherapies utilize PRR agonists to overcome immunosuppressive microenvironments: intratumoral injection of TLR9 agonists promotes antitumor immunity in lymphoma, while STING agonists demonstrate efficacy against solid tumors [1]. Anti-inflammatory therapies targeting PRR signaling include TLR4 antagonists for sepsis and NLRP3 inhibitors for gout and inflammatory bowel disease [3] [7]. The evolving understanding of vita-PAMPs and BAMPs offers further therapeutic opportunities for combating chronic infections and biofilm-associated diseases [5] [6].
Future research directions include: (1) elucidating the crosstalk between different PRR families in integrated immune responses; (2) characterizing novel PAMP classes from emerging pathogens; (3) developing tissue-specific PRR modulators to minimize systemic toxicity; and (4) exploring personalized immunotherapies based on PRR polymorphism profiles [3]. The continued dissection of PAMP recognition mechanisms will undoubtedly yield novel therapeutic strategies against infection, cancer, and inflammatory disorders.
Pathogen-Associated Molecular Patterns represent the fundamental language through which the immune system detects microbial invasion. These conserved molecular motifs enable rapid, nonspecific defense mechanisms while simultaneously instructing pathogen-specific adaptive immunity. The sophisticated PRR network that recognizes PAMPs demonstrates remarkable specificity despite its limited receptor repertoire, employing strategic localization, combinatorial signaling, and cross-regulatory mechanisms to generate appropriate inflammatory responses. Ongoing research continues to expand the PAMP paradigm through concepts like vita-PAMPs and BAMPs, refining our understanding of immune discrimination between viable and dead microorganisms, planktonic and biofilm growth states. The therapeutic translation of these insights is already yielding novel vaccine adjuvants, immunotherapies, and anti-inflammatory agents, highlighting the profound clinical implications of fundamental research into these universal danger signals. As our understanding of PAMP-PRR interactions deepens, so too will our ability to manipulate these pathways for therapeutic benefit across diverse disease contexts.
Pattern Recognition Receptors (PRRs) represent the cornerstone of the innate immune system, serving as germline-encoded host sensors that provide the crucial first line of defense against pathogenic invasion [9] [10]. These receptors function as specialized cellular sentinels, continuously monitoring for conserved molecular structures known as Pathogen-Associated Molecular Patterns (PAMPs) that are characteristic of diverse microbes but absent in the host [3] [9]. Additionally, PRRs detect Damage-Associated Molecular Patterns (DAMPs) released from injured host cells during cellular stress, damage, or death [11] [9]. This dual recognition capability enables the immune system to respond effectively to both infectious threats and sterile injury, bridging innate detection with the initiation of adaptive immunity [3] [10].
The conceptual foundation for PRRs was established by Charles Janeway in 1989, who hypothesized that the innate immune system possesses a specific capacity to detect microbial infections through receptors that recognize molecular patterns unique to pathogens [9]. This paradigm was later expanded by Polly Matzinger's "danger model," which proposed that immune activation occurs in response to danger signals emanating from both pathogens and host-derived damage molecules [9]. The discovery of Toll-like receptors in Drosophila by Hoffmann and colleagues in 1996, followed by the identification of human TLR4 by Janeway and Medzhitov, provided molecular validation for these theoretical frameworks and launched extensive research into diverse PRR families [3] [9].
PRRs are strategically expressed on various immune cells—including macrophages, dendritic cells, monocytes, and neutrophils—as well as non-immune epithelial and endothelial cells [11] [10]. Through their recognition capabilities, PRRs initiate intracellular signaling cascades that trigger the production of proinflammatory cytokines, interferons, chemokines, and other mediators that collectively coordinate anti-pathogen responses, activate inflammatory pathways, and shape subsequent adaptive immunity [3] [11]. The strategic positioning of different PRR families throughout cellular compartments ensures comprehensive surveillance of extracellular, endosomal, and cytoplasmic spaces, creating a multi-layered defense network against invading pathogens and endogenous threats [9] [10].
PRR Classification and Structural Features
PRRs are categorized into distinct families based on their protein domain homology, subcellular localization, and ligand specificity. The major families include Toll-like receptors (TLRs), NOD-like receptors (NLRs), RIG-I-like receptors (RLRs), C-type lectin receptors (CLRs), and DNA sensors such as AIM2-like receptors (ALRs) and cGAS [3] [9] [10]. While these families differ in structure and function, they share a common architectural principle: most contain ligand recognition domains, intermediate domains, and effector domains that facilitate pathogen detection and signal transduction [3] [9].
Table 1: Major Pattern Recognition Receptor Families
| PRR Family | Localization | Representative Members | Structural Domains | Key Features |
|---|---|---|---|---|
| Toll-like Receptors (TLRs) | Cell surface & endosomal membranes | TLR1-TLR10 (humans) | Extracellular LRR, transmembrane, intracellular TIR | First discovered PRR family; form homo/heterodimers |
| NOD-like Receptors (NLRs) | Cytoplasm | NOD1, NOD2, NLRP3 | CARD, NOD/NACHT, LRR | Form inflammasomes; regulate caspase-1 activation |
| RIG-I-like Receptors (RLRs) | Cytoplasm | RIG-I, MDA5, LGP2 | RNA helicase, CARD domains | Detect viral RNA; induce type I interferon production |
| C-type Lectin Receptors (CLRs) | Cell surface | Dectin-1, DC-SIGN, Mannose Receptor | Carbohydrate recognition domain (CRD) | Recognize carbohydrate patterns; important for antifungal immunity |
| DNA Sensors | Cytoplasm & nucleus | cGAS, AIM2 | - | Detect mislocalized DNA; initiate STING pathway |
Membrane-bound PRRs include TLRs and CLRs, which surveil extracellular and endosomal compartments, while cytoplasmic PRRs encompass NLRs, RLRs, and various DNA sensors that monitor the intracellular environment for signs of invasion or damage [9] [10]. TLRs are type I transmembrane glycoproteins characterized by an extracellular leucine-rich repeat (LRR) domain responsible for ligand binding, and an intracellular Toll/IL-1 receptor (TIR) domain that initiates signaling cascades [3] [11]. Different TLRs localize to distinct cellular compartments: TLR1, 2, 4, 5, 6, and 10 reside on the plasma membrane, while TLR3, 7, 8, and 9 are embedded in endosomal membranes where they encounter nucleic acids from internalized pathogens [3] [11].
NLRs and RLRs represent major cytoplasmic receptor families. NLRs typically contain a C-terminal leucine-rich repeat (LRR) domain for ligand sensing, a central nucleotide-binding oligomerization domain (NOD/NACHT), and N-terminal caspase activation and recruitment domains (CARD) or pyrin domains (PYD) that mediate downstream signaling [9] [10]. RLRs—including RIG-I, MDA5, and LGP2—feature DExD/H-box RNA helicase domains that enable recognition of viral RNA patterns, with RIG-I and MDA5 additionally containing CARD domains for signal transduction [9]. CLRs possess C-type lectin domains (CTLDs) that often recognize carbohydrate structures in a calcium-dependent manner, making them particularly important for detecting fungal pathogens [10].
PRR Ligand Recognition Mechanisms
Pathogen-Associated Molecular Patterns (PAMPs)
PAMPs represent conserved molecular structures essential for microbial survival and pathogenicity, making them reliable indicators of infection [3] [12]. These invariant motifs differ fundamentally from host components, enabling the immune system to distinguish "self" from "non-self" with remarkable precision [3]. PAMPs encompass diverse molecular classes including bacterial cell wall components (LPS, peptidoglycan, lipopeptides), microbial nucleic acids (bacterial DNA, viral RNA), flagellar proteins, and fungal carbohydrates [12] [10]. Their conservation across pathogen classes allows for a limited repertoire of PRRs to detect a vast array of microorganisms [12].
Different PRR families exhibit specialized recognition capabilities for distinct PAMP categories. Surface TLRs (TLR1, 2, 4, 5, 6) primarily detect membrane components of pathogens, with TLR4 recognizing lipopolysaccharide (LPS) from Gram-negative bacteria in complex with MD-2 protein [3] [11]. TLR2 forms heterodimers with TLR1 or TLR6 to recognize a broad spectrum of bacterial lipopeptides and lipoproteins [11]. Endosomal TLRs (TLR3, 7, 8, 9) specialize in nucleic acid detection, with TLR3 binding double-stranded RNA (dsRNA) from viruses, while TLR7/8 recognize single-stranded RNA (ssRNA), and TLR9 identifies unmethylated CpG DNA motifs prevalent in bacterial genomes [3] [11].
Cytoplasmic PRRs survey the intracellular environment for signs of invasion. RLRs (RIG-I and MDA5) detect distinct viral RNA patterns: RIG-I recognizes short double-stranded RNA with 5'-triphosphate groups, while MDA5 senses longer dsRNA structures [9]. NLRs mainly recognize bacterial peptidoglycan derivatives, with NOD1 detecting meso-diaminopimelic acid (meso-DAP) from Gram-negative bacteria, and NOD2 responding to muramyl dipeptide (MDP) present in both Gram-positive and Gram-negative bacteria [10]. CLRs such as Dectin-1 recognize β-glucans in fungal cell walls, while other CLRs bind mannose, fucose, or glucan patterns characteristic of various pathogens [10].
Damage-Associated Molecular Patterns (DAMPs)
Beyond pathogen detection, PRRs recognize endogenous danger signals known as DAMPs, which are released during cellular stress, damage, or necrotic death [11] [9]. DAMPs include * intracellular molecules that normally reside within cells but assume immunostimulatory properties when exposed to the extracellular environment* following tissue injury [9]. Common DAMPs include high mobility group box 1 (HMGB1), histones, uric acid, extracellular ATP, hyaluronic acid fragments, heat shock proteins, and genomic DNA released from damaged nuclei or mitochondria [11] [9].
The recognition of DAMPs by PRRs initiates "sterile inflammation"—inflammatory responses in the absence of infection—that serves to eliminate damaged cells and initiate tissue repair processes [11]. However, excessive or persistent DAMP signaling can contribute to chronic inflammatory conditions, autoimmune diseases, and cancer progression [9]. This dual nature of DAMP recognition highlights the sophisticated balance PRRs maintain in distinguishing protective from pathological inflammation, with context-dependent outcomes determined by the magnitude, duration, and combination of signals received [9].
Table 2: Representative PAMPs, DAMPs, and Their PRRs
| Ligand Category | Specific Ligands | Recognizing PRRs | Cellular Source |
|---|---|---|---|
| Bacterial PAMPs | Lipopolysaccharide (LPS) | TLR4/MD-2 | Gram-negative bacteria |
| Lipoteichoic acid | TLR2 | Gram-positive bacteria | |
| Flagellin | TLR5 | Flagellated bacteria | |
| Peptidoglycan fragments | NOD1, NOD2 | Bacterial cell walls | |
| Unmethylated CpG DNA | TLR9 | Bacterial DNA | |
| Viral PAMPs | Double-stranded RNA | TLR3, RIG-I, MDA5 | Viral replication intermediates |
| Single-stranded RNA | TLR7, TLR8 | RNA viruses | |
| 5'-triphosphate RNA | RIG-I | Negative-sense RNA viruses | |
| Fungal PAMPs | Zymosan | TLR2/Dectin-1 | Fungal cell walls |
| β-glucans | Dectin-1 | Fungal cell walls | |
| Mannans | MR, DC-SIGN | Fungal surfaces | |
| DAMPs | HMGB1 | TLR4, RAGE | Necrotic cells |
| Extracellular ATP | P2X7 receptor | Damaged cells | |
| Mitochondrial DNA | cGAS | Cellular damage | |
| Hyaluronic acid fragments | TLR4 | Extracellular matrix degradation |
Signaling Pathways and Immune Activation
TLR Signaling Pathways
TLR activation initiates signaling cascades that diverge into two principal pathways: the MyD88-dependent pathway utilized by all TLRs except TLR3, and the TRIF-dependent pathway employed by TLR3 and TLR4 [3] [10]. Upon ligand binding and receptor dimerization, TLRs recruit adaptor proteins through homophilic interactions between their TIR domains and those of the adaptors [3]. The MyD88-dependent pathway begins with the recruitment of the master adaptor MyD88, which subsequently recruits interleukin-1 receptor-associated kinases (IRAK4, IRAK1, IRAK2) to form a signaling complex [10]. This complex interacts with TRAF6, leading to activation of TAK1 and subsequent induction of two key signaling branches: the NF-κB pathway and the MAP kinase pathway [10]. These pathways ultimately activate transcription factors that translocate to the nucleus and induce expression of proinflammatory cytokines (TNF-α, IL-1, IL-6) and chemokines [3].
The TRIF-dependent pathway (also called the MyD88-independent pathway) is initiated by TLR3 and TLR4, resulting in the recruitment of the adaptor TRIF [10]. TRIF activates TBK1 and IKKε kinases, which phosphorylate IRF3, leading to IRF3 dimerization, nuclear translocation, and induction of type I interferon genes (IFN-α/β) [3]. Simultaneously, TRIF activates the same NF-κB and MAPK pathways as the MyD88-dependent route through RIP1 and TRAF6, providing complementary inflammatory signaling [10]. The specific adaptor usage and resulting gene expression profiles are tailored to the cellular context and pathogen threat, enabling customized immune responses.
Diagram 1: TLR Signaling Pathways - The MyD88-dependent and TRIF-dependent pathways
NLR and RLR Signaling Pathways
NLR signaling typically converges on NF-κB and MAPK activation through the serine-threonine kinase RIP2, leading to inflammatory gene expression [10]. Certain NLRs (such as NLRP3, NLRC4, and AIM2) form multiprotein complexes called inflammasomes that serve as activation platforms for caspase-1 [9]. Active caspase-1 processes pro-IL-1β and pro-IL-18 into their mature, bioactive forms and cleaves gasdermin D to induce pyroptosis—an inflammatory form of cell death that eliminates infected cells [9].
RLR signaling is initiated when RIG-I or MDA5 detects viral RNA in the cytoplasm, triggering their interaction with the mitochondrial adaptor protein MAVS (also called IPS-1, VISA, or Cardif) [9]. MAVS activation nucleates the formation of large prion-like polymers that serve as signaling hubs, recruiting TRAF family members and activating IKK-related kinases TBK1 and IKKε, which phosphorylate IRF3 and IRF7 [9]. These phosphorylated IRFs dimerize and translocate to the nucleus to induce type I interferon gene expression, establishing an antiviral state in the cell and surrounding tissues [9]. Simultaneously, MAVS activates the IKK complex leading to NF-κB activation and proinflammatory cytokine production [9].
Diagram 2: RLR and NLR Signaling Pathways - Antiviral and antibacterial immune responses
Research Methodologies and Experimental Approaches
PRR Expression Analysis
Investigating PRR expression patterns across different cell types and conditions provides fundamental insights into their roles in immunity and disease. The most common methodologies include:
Quantitative Real-Time PCR (qRT-PCR): Enables precise quantification of PRR mRNA expression levels in cells or tissues following pathogen challenge, cytokine stimulation, or under pathological conditions [13]. This approach allows researchers to correlate PRR expression changes with specific immune challenges. Experimental protocol: Extract total RNA using TRIzol or column-based methods, synthesize cDNA with reverse transcriptase, perform qPCR using gene-specific primers for target PRRs (e.g., TLRs, RLRs, NLRs), and normalize data using housekeeping genes (GAPDH, β-actin). Include no-template controls and standard curves for quantification.
Western Blotting: Detects and quantifies PRR protein expression, post-translational modifications, and cleavage events that regulate PRR activity [13]. This technique is essential for confirming that mRNA expression correlates with protein production and for assessing PRR activation states. Experimental protocol: Prepare cell lysates in RIPA buffer with protease and phosphatase inhibitors, separate proteins by SDS-PAGE, transfer to PVDF membranes, block with 5% BSA, incubate with primary antibodies against specific PRRs (e.g., anti-TLR4, anti-NOD2), followed by HRP-conjugated secondary antibodies, and detect using chemiluminescence substrates.
Flow Cytometry: Facilitates analysis of PRR surface expression on specific immune cell populations and permits correlation with activation markers or intracellular signaling molecules [13]. This approach is particularly valuable for heterogeneous cell samples. Experimental protocol: Harvest cells, block Fc receptors to prevent non-specific binding, stain with fluorochrome-conjugated antibodies against surface PRRs (e.g., anti-TLR2, anti-TLR4), fix cells if performing intracellular staining, acquire data on a flow cytometer, and analyze using software such as FlowJo to determine expression levels across cell populations.
Immunohistochemistry/Immunofluorescence: Allows spatial localization of PRRs within tissues and correlation with pathological features in clinical specimens or disease models [13]. This technique preserves architectural context that is lost in dissociated cell analyses. Experimental protocol: Prepare tissue sections (4-6μm), perform antigen retrieval if required, block endogenous peroxidases and non-specific binding, incubate with primary antibodies against PRRs, followed by enzyme-conjugated or fluorescent secondary antibodies, develop with chromogenic substrates (DAB for IHC) or mounting media with DAPI (for IF), and visualize by light or fluorescence microscopy.
PRR Functional Assays
Determining the functional consequences of PRR activation requires specialized assays that measure downstream signaling events and biological responses:
Luciferase Reporter Assays: Quantify activation of specific transcription factors (NF-κB, IRF3, AP-1) following PRR stimulation [13]. These assays provide sensitive, quantitative readouts of pathway-specific PRR signaling. Experimental protocol: Plate cells in 24-well or 48-well plates, co-transfect with PRR expression plasmids and reporter constructs (e.g., NF-κB-luc, IFN-β-luc), stimulate with specific PRR ligands (e.g., LPS for TLR4, poly(I:C) for TLR3), lyse cells after 6-24 hours, measure luciferase activity using a luminometer, and normalize data to co-transfected control reporters (e.g., Renilla luciferase).
Cytokine/Chemokine Measurement: Evaluate functional outputs of PRR activation by quantifying secretion of inflammatory mediators using ELISA, multiplex bead arrays, or MSD assays [13]. These measurements correlate PRR signaling with biologically relevant immune responses. Experimental protocol: Stimulate PRR-expressing cells with specific ligands (PAMPs or DAMPs), collect culture supernatants at various time points (typically 6-48 hours), quantify cytokine levels (e.g., TNF-α, IL-6, IL-1β, IFN-α/β) using commercial ELISA kits or multiplex arrays according to manufacturer protocols, and generate standard curves for absolute quantification.
Knockdown/Knockout Approaches: Determine PRR-specific functions using genetic disruption techniques including siRNA, shRNA, CRISPR/Cas9, or genetic deletion in animal models [13]. These loss-of-function experiments establish necessity for specific PRRs in immune responses. Experimental protocol: Design and synthesize targeting sequences for specific PRRs, deliver using appropriate transfection/transduction methods (lipofection, electroporation, viral vectors), confirm knockdown/knockout efficiency by qRT-PCR or Western blot, stimulate cells with relevant ligands, and measure downstream responses compared to control cells.
Table 3: Key Research Reagents for PRR Investigation
| Reagent Category | Specific Examples | Research Application | Mechanism of Action |
|---|---|---|---|
| TLR Agonists | Pam3CSK4 (TLR1/2) | Bacterial lipopeptide simulation | Activates TLR1/2 heterodimers |
| Poly(I:C) (TLR3) | Viral dsRNA mimic | Binds and activates TLR3 | |
| LPS (TLR4) | Gram-negative bacterial infection models | Activates TLR4/MD-2 complex | |
| Imiquimod (TLR7) | Antiviral response studies | Activates endosomal TLR7 | |
| CpG ODN (TLR9) | Bacterial DNA recognition | Binds and activates TLR9 | |
| NLR Agonists | MDP (NOD2) | Bacterial peptidoglycan response | Activates NOD2 signaling |
| iE-DAP (NOD1) | Gram-negative bacterial sensing | Specific NOD1 ligand | |
| Nigericin (NLRP3) | Inflammasome activation | Potassium ionophore activating NLRP3 | |
| RLR Agonists | 5'ppp-RNA (RIG-I) | Viral RNA recognition studies | Specific RIG-I ligand |
| Poly(I:C) (MDA5) | Long dsRNA viral infection mimic | Activates MDA5 signaling | |
| Inhibitors | TAK-242 (TLR4) | TLR4 signaling blockade | Inhibits TLR4-TIR domain interactions |
| BX795 (TBK1/IKKε) | IRF3 pathway inhibition | Blocks TBK1/IKKε kinase activity | |
| MCC950 (NLRP3) | Inflammasome inhibition | Specific NLRP3 inflammasome inhibitor | |
| Antibodies | Anti-TLR4 | Receptor expression/blocking | Detects or blocks TLR4 |
| Anti-phospho-IRF3 | Signaling activation readout | Detects activated IRF3 | |
| Anti-NLRP3 | Inflammasome formation studies | Detects NLRP3 expression |
Pathogen Evasion Strategies and PRR Regulation
Microbial Evasion of PRR Recognition
Successful pathogens have evolved sophisticated mechanisms to evade or subvert PRR-mediated detection, representing a dynamic evolutionary arms race between host immunity and microbial survival strategies [13]. These evasion tactics include:
Structural Modification of PAMPs: Many pathogens alter their molecular patterns to avoid PRR recognition. For example, some bacteria modify their lipid A moiety of LPS to reduce TLR4 activation, while certain viruses cap their RNA or mask 5'-triphosphates to avoid RIG-I detection [13].
Sequestration of PAMPs: Pathogens may physically hide their immunostimulatory molecules from PRR surveillance. Some intracellular bacteria and viruses assemble within membrane-bound compartments that limit exposure to cytoplasmic PRRs, while others export PAMPs to cellular locations devoid of appropriate sensors [13].
Expression of PRR Inhibitors: Numerous pathogens encode proteins that directly interfere with PRR signaling cascades. Viral proteins may target key signaling adaptors (MAVS, MyD88, TRIF) for degradation, while bacterial effectors can inhibit critical kinases (TBK1, IKK) or cleave signaling components to disrupt communication pathways [13].
Modulation of Host Epigenetic Regulation: Certain pathogens manipulate host epigenetic machinery to suppress PRR expression or function. This includes inducing repressive histone modifications at PRR gene promoters or driving DNA methylation that silences critical components of immune signaling pathways [13].
SARS-CoV-2 exemplifies sophisticated PRR evasion through multiple mechanisms, including masking its RNA to avoid RIG-I/MDA5 detection, encoding proteins that degrade PRR signaling components, and disrupting IFN signaling pathways [13]. These evasion strategies contribute to the delayed interferon response observed in severe COVID-19 cases, allowing rapid viral replication before immune containment [13].
Endogenous Regulation of PRR Activity
To prevent excessive or inappropriate inflammation, PRR signaling is subject to multiple layers of endogenous regulation that fine-tune immune responses:
Transcriptional and Post-transcriptional Control: PRR expression and function are regulated through transcription factor networks, microRNAs, and RNA-binding proteins that adjust receptor levels in response to cellular conditions [9]. Negative feedback mechanisms induced by PRR signaling itself help terminate responses once threats are eliminated.
Post-translational Modifications: Phosphorylation, ubiquitination, and proteolytic cleavage dynamically regulate PRR activity, subcellular localization, and interactions with signaling partners [9]. Both activating and inhibitory modifications create molecular switches that control signal initiation and duration.
Compartmentalization and Trafficking: Strategic localization within specific cellular compartments (plasma membrane, endosomes, mitochondria) controls PRR access to ligands and signaling components [9]. Regulated trafficking between compartments provides an additional control layer for PRR activity.
Inhibitory PRRs (iPRRs): A specialized class of receptors including CD300a/f, Siglecs, CEACAM1, LILRB1, and LAIR-1 recognizes endogenous or microbial patterns associated with homeostasis or modified self, delivering inhibitory signals that counterbalance activating PRRs [9]. These iPRRs provide contextual information to prevent excessive inflammation against non-threatening stimuli.
Metabolic and Microbial Regulation: Cellular metabolic states and the commensal microbiome significantly influence PRR responses through metabolite production, cross-talk with other signaling pathways, and tonic stimulation that sets activation thresholds [9].
This sophisticated regulatory network ensures that PRR-mediated immunity remains appropriately scaled to threats, minimizing collateral tissue damage while maintaining effective pathogen defense. Dysregulation of these control mechanisms contributes to inflammatory diseases, autoimmunity, and cancer pathogenesis [9].
Clinical Applications and Therapeutic Targeting
PRRs in Disease Pathogenesis
PRRs play pivotal roles in the pathogenesis of diverse human diseases, making them attractive therapeutic targets:
Infectious Diseases: PRR function directly impacts susceptibility to and outcomes of infectious diseases. Genetic polymorphisms in PRRs (TLR3, TLR7, RIG-I) are associated with increased severity of COVID-19, while deficiencies in NLRs or TLRs predispose to specific bacterial and fungal infections [13]. The magnitude and timing of PRR activation critically determine whether protective immunity or pathological inflammation develops during infections.
Autoimmune and Autoinflammatory Disorders: Excessive or inappropriate PRR activation contributes to autoimmune pathology. In systemic lupus erythematosus, defective clearance of cellular debris leads to persistent DAMP exposure and TLR7/TLR9 activation, driving anti-nuclear antibody production [9]. NLRP3 inflammasome overactivation underlies several autoinflammatory syndromes like cryopyrin-associated periodic syndromes (CAPS) [9].
Cancer: PRRs demonstrate dual roles in oncogenesis and cancer control. Chronic inflammation driven by PRR signaling can promote tumor development, while PRR activation in tumor cells or immune cells can stimulate antitumor immunity [11] [9]. "Viral mimicry"—the transcriptional reactivation of endogenous retroelements—in cancer cells can trigger RLR and MDA5 sensing, inducing interferon responses that enhance antitumor immunity [14] [15].
Long COVID: Altered PRR expression and signaling persistence may contribute to long COVID pathogenesis. Changes in TLRs, cGAS, and STING expression have been detected in long COVID patients, suggesting sustained innate immune activation drives persistent symptoms [13].
Therapeutic Targeting of PRRs
The strategic position of PRRs at the immunity interface makes them promising targets for therapeutic intervention:
PRR Agonists as Vaccine Adjuvants: PRR ligands effectively enhance vaccine immunogenicity by activating innate immunity and promoting adaptive responses [16]. Multiple TLR agonists are incorporated into licensed vaccines: MPLA (TLR4 agonist) in AS04-adjuvanted vaccines (Hepatitis B, HPV), CpG 1018 (TLR9 agonist) in Heplisav-B, and AS01 (containing MPL and saponin) in Shingrix [16]. Combination of multiple PRR agonists may provide synergistic benefits through complementary pathway activation [16].
PRR Agonists in Cancer Immunotherapy: PRR activation can overcome immunosuppression in the tumor microenvironment and stimulate antitumor immunity [11]. Intratumoral injection of PRR agonists (TLR agonists, STING agonists) is being explored to convert "cold" tumors into "hot," T-cell-inflamed tumors responsive to checkpoint inhibitors [11] [9].
PRR Antagonists in Inflammatory Diseases: Inhibiting excessive PRR signaling may benefit autoimmune and inflammatory conditions. TLR7/TLR9 antagonists are investigated for lupus, while NLRP3 inhibitors (MCC950) show promise in inflammatory diseases [9]. STING antagonists are being developed to ameliorate type I interferonopathies [9].
Personalized Approaches: Understanding how PRR polymorphisms affect disease susceptibility and treatment responses will enable personalized immunotherapeutic strategies tailored to individual genetic backgrounds and disease characteristics [13] [9].
The continuing elucidation of PRR biology, ligand recognition mechanisms, signaling networks, and regulatory principles promises to unlock new therapeutic opportunities for infectious diseases, cancer, inflammatory disorders, and immune-mediated conditions. As the central sentinels of cellular immunity, PRRs remain compelling targets for manipulating immune responses in human health and disease.
Pathogen-associated molecular patterns (PAMPs) are conserved molecular structures essential for microbial survival that are recognized by the host innate immune system through pattern recognition receptors (PRRs). This recognition initiates inflammatory signaling pathways that constitute the first line of defense against invading pathogens [17] [3]. The conceptual framework of PAMPs and PRRs, first proposed by Charles Janeway in 1989, has fundamentally shaped our understanding of innate immunity and its role in activating adaptive immune responses [17] [9] [3]. This whitepaper provides an in-depth technical analysis of four major PAMP classes: lipopolysaccharide (LPS), flagellin, peptidoglycan, and microbial nucleic acids, with particular focus on their structures, recognition mechanisms, and associated signaling pathways relevant to inflammation initiation research and therapeutic development.
Lipopolysaccharide (LPS)
Structure and Function
Lipopolysaccharide (LPS), also known as endotoxin, is an amphipathic glycolipid that constitutes the major component of the outer leaflet of the outer membrane in Gram-negative bacteria [17] [18]. LPS maintains membrane integrity, provides a permeability barrier against environmental toxins and antimicrobial compounds, and is essential for bacterial fitness in most Gram-negative species [17]. Structurally, LPS consists of three domains: the hydrophobic lipid A region embedded in the outer membrane, a core oligosaccharide, and a distal O-antigen polysaccharide chain [18]. The lipid A moiety, which contains phosphorylated glucosamine disaccharides with multiple acyl chains, is the conserved PAMP responsible for the immunostimulatory activity of LPS [17] [19].
Recognition Mechanisms and Signaling Pathways
Mammalian systems have evolved a sophisticated multi-protein complex for detecting LPS with exceptional sensitivity, capable of responding to picomolar concentrations [19]. The extracellular recognition process involves a sequential protein cascade:
- LPS-binding protein (LBP), a serum glycoprotein, initially binds to LPS aggregates and facilitates the extraction of LPS monomers [17] [18] [19].
- Monomeric LPS is transferred to cluster of differentiation 14 (CD14), which exists in both membrane-bound (GPI-anchored) and soluble forms [17] [18].
- CD14 presents LPS to the MD-2/TLR4 complex. MD-2, which is stably associated with Toll-like receptor 4 (TLR4), is the essential coreceptor that directly binds the lipid A moiety of LPS [18] [19].
- LPS binding induces dimerization of the TLR4-MD-2 complex, forming a symmetric `m'-shaped heterotetramer (2:2:2 complex of LPS:MD-2:TLR4) that initiates intracellular signaling [18] [19].
This receptor assembly triggers two distinct intracellular signaling cascades:
- MyD88-Dependent Pathway: Initiated at the plasma membrane, this pathway recruits the adaptor protein MyD88, leading to the activation of IRAK and TRAF6, ultimately activating NF-κB and AP-1 transcription factors. This results in the rapid production of pro-inflammatory cytokines such as TNF-α, IL-1β, and IL-6 [18].
- TRIF-Dependent Pathway (MyD88-Independent): Initiated after endocytosis of the TLR4 complex, this pathway utilizes the adaptor TRIF to activate TBK1 and IKKε, leading to phosphorylation and nuclear translocation of IRF3. This induces the production of Type I interferons (IFN-α and IFN-β) [18].
In addition to the cell surface TLR4 pathway, cytosolic LPS can be detected by inflammatory caspases (caspase-4/5 in humans, caspase-11 in mice). This intracellular sensing triggers pyroptosis, an inflammatory form of cell death, and activates the NLRP3 inflammasome to process and release mature IL-1β [17].
Table 1: Key Proteins in LPS Recognition and Signaling
| Protein | Structure | Function in LPS Response |
|---|---|---|
| LBP | 58-60 kDa glycoprotein, N-terminal cationic residue cluster for LPS binding [18]. | Binds LPS aggregates, facilitates monomer extraction and transfer to CD14 [18] [19]. |
| CD14 | Leucine-rich repeat (LRR) glycoprotein, GPI-anchored or soluble [18]. | Recognizes LBP-delivered LPS, presents it to the TLR4-MD-2 complex [18]. |
| MD-2 | ~18 kDa protein, member of ML lipid-binding family [18] [19]. | Coreceptor for TLR4; directly binds lipid A; essential for TLR4 response to LPS [18] [19]. |
| TLR4 | Type I transmembrane protein with LRR extracellular domain and TIR intracellular domain [18]. | Pattern recognition receptor; forms complex with MD-2 and LPS; initiates intracellular signaling [17] [18]. |
| MyD88 | Adaptor protein with TIR and Death domains [18] [3]. | Primary TIR-domain adaptor for most TLRs; activates NF-κB and MAPK for pro-inflammatory cytokine production [18] [3]. |
Figure 1: LPS Recognition and Signaling Pathways. LPS is sequentially transferred by LBP and CD14 to the TLR4/MD-2 complex, triggering both MyD88-dependent pro-inflammatory cytokine production and TRIF-dependent type I interferon production.
Experimental Protocols for LPS Research
Protocol 1: Assessing TLR4 Activation via NF-κB Reporter Assay
- Cell Model: HEK293 cells stably expressing TLR4, MD-2, and CD14, transfected with an NF-κB-luciferase reporter plasmid.
- Stimulation: Treat cells with purified LPS (e.g., from E. coli O111:B4) across a concentration range (0.1-100 ng/mL) for 6-24 hours.
- Control: Include cells treated with lipid IVa (TLR4 antagonist) or LPS from Rhodobacter sphaeroides to confirm specificity [19].
- Readout: Measure luciferase activity. Validate cytokine secretion (e.g., IL-8) via ELISA [18].
Protocol 2: Detecting Cytosolic LPS-Induced Pyroptosis
- Cell Model: Primary murine bone-marrow-derived macrophages (BMDMs) or human monocytic cell lines (THP-1).
- Transfection: Transfect cells with ultrapure LPS (1 µg/mL) using a transfection reagent (e.g., Lipofectamine 2000) to deliver LPS into the cytosol.
- Inhibition: Pre-treat with caspase-4/11 inhibitor (e.g., Z-VAD-FMK) [17].
- Readout: Measure cell viability (MTT assay) and lactate dehydrogenase (LDH) release to quantify pyroptosis. Analyze IL-1β in supernatant via ELISA [17].
Flagellin
Structure and Function
Flagellin is the primary structural protein subunit of the bacterial flagellum, a whip-like appendage that enables bacterial motility [20]. As a PAMP, flagellin is recognized by the immune system at sub-nanomolar concentrations [20]. The protein is characterized by a highly conserved D1 domain at the N- and C-termini, which is essential for its recognition by PRRs, and a central hypervariable D3 domain that is dispensable for immune activation [20].
Recognition Mechanisms and Signaling Pathways
Flagellin is detected by immune cells via two primary mechanisms:
Extracellular Sensing by TLR5: Toll-like receptor 5 (TLR5) is a membrane-bound PRR that recognizes the conserved D1 domain of extracellular flagellin [20]. Upon binding, TLR5 dimerizes and recruits the adaptor protein MyD88, leading to the activation of NF-κB and MAPK pathways. This results in the production of pro-inflammatory cytokines and chemokines [20]. In intestinal epithelial cells, TLR5 is exclusively expressed on the basolateral surface, providing a molecular basis for the polarity of the innate immune response. Pathogenic bacteria like Salmonella can translocate flagellin across the epithelium to the basolateral side, thereby triggering inflammation, whereas commensal bacteria primarily present flagellin at the apical surface, which does not initiate a response [21].
Cytosolic Sensing by the NLRC4 Inflammasome: When flagellin is delivered into the host cell cytoplasm by bacterial type III secretion systems (T3SS), it is recognized by members of the NLR family apoptosis inhibitory proteins (NAIPs). In mice, NAIP5 and NAIP6 bind directly to flagellin [20]. This flagellin-NAIP complex then recruits and activates NLRC4, leading to the assembly of a multi-protein complex called the inflammasome. The inflammasome activates caspase-1, which cleaves pro-IL-1β and pro-IL-18 into their active forms and triggers pyroptosis [20].
Table 2: Flagellin Receptors and Their Functions
| Receptor | Location | Ligand Specificity | Key Functions |
|---|---|---|---|
| TLR5 | Plasma Membrane (Basolateral in gut epithelium) | Conserved D1 domain of flagellin [20] [21] | MyD88-dependent activation of NF-κB/MAPK; induces proinflammatory gene expression [20]. |
| NAIP/ NLRC4 | Cytosol | C-terminal 35 amino acids of flagellin (in mice, via NAIP5/6) [20] | Forms inflammasome complex; activates caspase-1; processes and releases IL-1β and IL-18; induces pyroptosis [20]. |
Figure 2: Flagellin Sensing Pathways. Extracellular flagellin is sensed by TLR5, triggering a MyD88-dependent cytokine response. Cytosolic flagellin, often injected via a Type 3 Secretion System (T3SS), is detected by NAIPs, which activate the NLRC4 inflammasome, leading to caspase-1 activation and pyroptosis.
Experimental Protocols for Flagellin Research
Protocol 1: Evaluating TLR5-Specific Signaling
- Cell Model: HEK293 cells transiently transfected with human TLR5 and an NF-κB-luciferase reporter.
- Stimulation: Treat with purified flagellin (e.g., from Salmonella typhimurium, 10-100 ng/mL) for 6-18 hours.
- Control: Use a recombinant flagellin protein lacking the hypervariable D3 domain (contains only D1/D2 domains) to confirm that immune stimulation is retained [20].
- Readout: Measure luciferase activity and quantify IL-8 secretion via ELISA.
Protocol 2: Assessing NAIP/NLRC4 Inflammasome Activation
- Cell Model: Primary BMDMs from C57BL/6 mice (which express functional NAIP5) or human macrophage models.
- Infection/Transfection: Infect with flagellated, T3SS-competent Salmonella (e.g., S. Typhimurium SL1344) at an MOI of 10:1, OR transfect with purified flagellin (0.5-1 µg/mL) using a transfection reagent.
- Inhibition: Pre-treat with caspase-1 inhibitor (YVAD) or NLRC4-specific siRNA [20].
- Readout: Measure LDH release for pyroptosis. Analyze culture supernatants for mature IL-1β by western blot and ELISA.
Peptidoglycan
Structure and Function
Peptidoglycan (also known as murein) is a vast, mesh-like macromolecule that forms a protective layer (sacculus) surrounding the cytoplasmic membrane of most bacteria [22] [23]. Its primary function is to provide structural strength and counteract the intracellular osmotic pressure, thereby preventing cell lysis [22]. The peptidoglycan polymer consists of glycan chains of alternating N-acetylglucosamine (NAG) and N-acetylmuramic acid (NAM) residues, connected by β-(1,4)-glycosidic bonds [22] [23]. A short peptide stem (usually 4-5 amino acids) is attached to each NAM residue. Adjacent peptide stems are cross-linked, often by D-glutamic acid and D-alanine residues, creating a robust, 3-dimensional network that defines cell shape [22] [23]. The peptidoglycan layer is substantially thicker in Gram-positive bacteria (20-80 nm) than in Gram-negative bacteria (7-8 nm) [23].
Recognition Mechanisms and Signaling Pathways
The innate immune system recognizes peptidoglycan through both extracellular and cytosolic PRRs:
Extracellular Recognition: Peptidoglycan fragments can be recognized by several transmembrane receptors, including Toll-like receptor 2 (TLR2), often in heterodimeric complexes with TLR1 or TLR6, and certain C-type lectin receptors (CLRs) [3]. TLR2 recognition leads to the activation of NF-κB and the production of inflammatory cytokines.
Cytosolic Recognition: The primary cytosolic sensors for peptidoglycan are NOD-like receptors (NLRs), specifically NOD1 and NOD2 [3]. NOD1 recognizes meso-diaminopimelic acid (meso-DAP)-containing peptides derived primarily from Gram-negative bacteria, while NOD2 senses muramyl dipeptide (MDP), a motif found in peptidoglycan from both Gram-positive and Gram-negative bacteria [3]. Upon ligand binding in the cytosol, NOD1 and NOD2 oligomerize and recruit the adaptor protein RIPK2 (also known as RICK), which leads to the activation of NF-κB and MAPK signaling pathways, promoting inflammatory gene expression [3].
Table 3: Peptidoglycan Structure and Recognition
| Feature | Description | Immunological Significance |
|---|---|---|
| Sugar Backbone | Alternating N-acetylglucosamine (NAG) and N-acetylmuramic acid (NAM) with β-(1,4) linkages [22] [23]. | Target for lysozyme, a host enzyme that cleaves these bonds and acts as an antimicrobial agent [23]. |
| Peptide Stem | 4-5 amino acid chain attached to NAM; composition varies by species (e.g., contains D-amino acids) [22] [23]. | Source of unique molecular patterns (e.g., D-amino acids) not found in host proteins, enabling self/non-self discrimination. |
| Cross-links | Connect peptide stems from adjacent glycans; mediated by enzymes like DD-transpeptidases (penicillin-binding proteins) [22] [23]. | Targeted by beta-lactam antibiotics (e.g., penicillin), which inhibit the cross-linking enzymes [22]. |
| Primary Sensors | TLR2 (extracellular), NOD1/NOD2 (cytosolic) [3]. | Initiate pro-inflammatory signaling; NOD2 mutations are linked to Crohn's disease, highlighting its role in gut immunity [3]. |
Microbial Nucleic Acids
Microbial nucleic acids (DNA and RNA) constitute a major class of PAMPs distinguished from host nucleic acids by their structure, modification status, and subcellular localization during infection [24]. The innate immune system has evolved numerous PRRs to detect these molecules in various compartments, including endosomes and the cytosol.
- Bacterial DNA: Characterized by unmethylated CpG dinucleotides within specific sequence contexts (CpG motifs), which are underrepresented and methylated in vertebrate DNA [24] [3].
- Viral RNA: Features include 5'-triphosphate groups on single-stranded RNA (ssRNA), long double-stranded RNA (dsRNA) generated during replication, and specific secondary structures [24].
- Viral/Bacterial DNA: Can be sensed in the cytosol, particularly when in a double-stranded (dsDNA) form [24].
Recognition Mechanisms and Signaling Pathways
Endosomal Recognition
- TLR9 is the primary sensor for unmethylated CpG DNA within endosomes. It signals through MyD88 to activate NF-κB and IRF7, inducing pro-inflammatory cytokines and type I interferons [24] [3].
- TLR3 binds to viral or synthetic dsRNA in endosomes. It signals via the adaptor TRIF (MyD88-independent pathway), leading to the activation of IRF3 and NF-κB, and the production of type I interferons and cytokines [24] [3].
- TLR7 (in humans) and TLR8 recognize viral ssRNA in endosomes, signaling through MyD88 to activate NF-κB and IRF7 [24].
Cytosolic Recognition
- RIG-I-like Receptors (RLRs): This family includes RIG-I and MDA5. RIG-I recognizes short dsRNA with a 5'-triphosphate, while MDA5 senses long dsRNA. Both signal through the mitochondrial adaptor MAVS (mitochondrial antiviral-signaling protein), leading to the activation of IRF3, IRF7, and NF-κB, and the potent induction of type I interferons [24] [3].
- cGAS (Cyclic GMP-AMP Synthase): This is the primary sensor for cytosolic dsDNA. Upon binding DNA, cGAS synthesizes the second messenger 2'3'-cGAMP. cGAMP then binds to the adaptor protein STING on the endoplasmic reticulum, which activates TBK1 and IRF3, resulting in a robust type I interferon response [24] [3].
- AIM2-like Receptors (ALRs): AIM2 forms an inflammasome in response to cytosolic dsDNA by recruiting ASC and caspase-1, leading to the maturation of IL-1β/IL-18 and pyroptosis [9] [3].
- NOD2: In addition to sensing peptidoglycan, NOD2 can also function as a cytosolic sensor of viral ssRNA, activating NF-κB and IRF3 to induce type I interferons [24].
Table 4: Nucleic Acid Sensing PRRs and Their Ligands
| Receptor | Location | Ligand | Key Adaptor | Primary Output |
|---|---|---|---|---|
| TLR9 | Endosome | Unmethylated CpG DNA [24] [3] | MyD88 | Type I IFN, Pro-inflammatory Cytokines [24] [3] |
| TLR3 | Endosome | Double-stranded RNA (dsRNA) [24] [3] | TRIF | Type I IFN [24] [3] |
| TLR7/8 | Endosome | Single-stranded RNA (ssRNA) [24] [3] | MyD88 | Type I IFN, Pro-inflammatory Cytokines [24] [3] |
| RIG-I | Cytosol | Short dsRNA with 5' triphosphate [24] | MAVS | Type I IFN [24] |
| MDA5 | Cytosol | Long dsRNA [24] | MAVS | Type I IFN [24] |
| cGAS | Cytosol | Double-stranded DNA (dsDNA) [24] [3] | STING | Type I IFN [24] [3] |
| AIM2 | Cytosol | Double-stranded DNA (dsDNA) [24] [3] | ASC (Inflammasome) | Caspase-1 activation, IL-1β, Pyroptosis [24] [3] |
Figure 3: Nucleic Acid Sensing Pathways. Endosomal TLRs (3, 7/8, 9) detect nucleic acids after pathogen internalization. Cytosolic RNA is sensed by RIG-I-like Receptors (RLRs) via MAVS, while cytosolic DNA is detected by cGAS-STING and AIM2 inflammasome pathways.
Experimental Protocols for Nucleic Acid Sensing
Protocol 1: Measuring cGAS-STING Pathway Activation
- Cell Model: Human monocytic THP-1 cells or primary human macrophages.
- Stimulation/Transfection: Transfert with synthetic dsDNA (e.g., ISD, 45BP DNA, 1 µg/mL) or interferon-stimulatory DNA (ISD) using a transfection reagent. Alternatively, infect with DNA viruses (e.g., HSV-1).
- Inhibition: Use cGAS- or STING-specific inhibitors (e.g., H-151, RU.521) or siRNA knockdown [24].
- Readout: Measure IFN-β mRNA by qRT-PCR and protein by ELISA. Analyze phosphorylation of IRF3 by western blot.
Protocol 2: Assessing RIG-I Activation
- Cell Model: A549 lung epithelial cells or primary fibroblasts.
- Stimulation/Transfection: Infect with Sendai virus or transfect with synthetic 5'-triphosphate RNA (3p-hpRNA, 1 µg/mL).
- Inhibition: Use RIG-I-specific inhibitor (e.g., RIG-I-N) or MAVS-deficient cells [24].
- Readout: Measure IFN-β and ISG (e.g., MX1) mRNA levels by qRT-PCR. Assess IRF3 phosphorylation by western blot.
The Scientist's Toolkit: Research Reagent Solutions
Table 5: Essential Research Tools for PAMP Signaling Studies
| Reagent / Tool | Function/Description | Example Application |
|---|---|---|
| Ultrapure LPS | Highly purified LPS with low protein/contaminant content, specific to bacterial serotypes. | Defining specific TLR4-MD-2 activation without confounding PRR engagement [18]. |
| Recombinant Flagellin (D1/D2 domains) | Purified flagellin protein containing the conserved TLR5-binding domains. | Studying TLR5-specific signaling in vitro and in vivo; used as a vaccine adjuvant [20]. |
| Muramyl Dipeptide (MDP) | Minimal bioactive peptidoglycan fragment recognized by NOD2. | Activating the NOD2 signaling pathway in cellular assays [3]. |
| CL-097 | Synthetic imidazoquinoline compound that acts as a TLR7 agonist. | Studying endosomal TLR7 signaling and type I interferon responses [3]. |
| Poly(I:C) | Synthetic analog of double-stranded RNA (dsRNA). | A TLR3 and MDA5 agonist for mimicking viral infection and inducing interferon responses [24] [3]. |
| 2'3'-cGAMP | Native second messenger produced by cGAS upon DNA sensing. | Directly activating the STING pathway downstream of cGAS [24]. |
| CRISPR/Cas9 Knockout Cells | Isogenic cell lines with specific PRR or adaptor gene (e.g., MYD88, TRIF, MAVS) knocked out. | Defining the specific roles of signaling molecules in PAMP-induced pathways [17] [24]. |
| NF-κB/IRF Luciferase Reporter Cells | Stable cell lines with inducible promoters driving luciferase expression. | Quantifying activation of key transcription factors in response to PAMP stimulation [20] [18]. |
The detailed molecular understanding of PAMP recognition by their corresponding PRRs has profoundly advanced the field of immunology and provides a robust framework for therapeutic innovation. The structural insights into receptor-ligand interactions, such as the LPS-TLR4/MD-2 complex or the flagellin-TLR5 interface, reveal precise targets for drug discovery. The distinct signaling pathways activated—leading to cytokine production, interferon responses, or inflammasome activation—offer multiple avenues for intervention. Agents that modulate these pathways, either as antagonists to curb deleterious inflammation (e.g., in sepsis or autoimmune diseases) or as agonists to boost immune responses (e.g., in vaccines or cancer immunotherapy), represent a promising frontier in biomedical research. Continued investigation into the intricate regulation of PAMP-PRR interactions and their downstream signaling cascades is essential for developing the next generation of immunomodulatory therapies.
This technical guide delineates the fundamental signaling pathways activated by pathogen-associated molecular patterns (PAMPs) and damage-associated molecular patterns (DAMPs), with a focused analysis of NF-κB signaling and inflammasome activation. These pathways represent the cornerstone of the innate immune response, orchestrating initial inflammatory responses to infection and injury. For researchers and drug development professionals, understanding the precise mechanisms—from receptor engagement to transcriptional regulation and protease activation—is paramount for developing targeted therapies for inflammatory diseases, autoimmune disorders, and cancer. This whitepaper integrates current mechanistic insights, experimental methodologies, and key reagent solutions to support advanced research in immunology and translational medicine.
The innate immune system serves as the first line of defense, employing a limited set of germline-encoded pattern recognition receptors (PRRs) to detect conserved molecular signatures. PAMPs, derived from microorganisms, and DAMPs, released from damaged or stressed host cells, are the primary ligands for these receptors [25] [7]. The engagement of PRRs triggers highly conserved signal transduction cascades that lead to the production of inflammatory mediators, the recruitment of immune cells, and the activation of adaptive immunity. Two of the most critical downstream signaling events are the activation of the transcription factor NF-κB and the assembly of inflammasome complexes, which are central to the pathogenesis of numerous chronic inflammatory and autoimmune conditions. The interplay between PAMPs and DAMPs can fine-tune these responses, with their combined presence often leading to synergistic amplification of inflammation, a key consideration for therapeutic intervention [26] [7].
NF-κB Signal Transduction Pathway
NF-κB is a family of transcription factors that regulates a vast array of genes involved in inflammation, immunity, cell survival, and proliferation. It is a pivotal mediator of the response to both PAMPs and DAMPs [27] [28] [29].
Pathway Architecture and Key Components
The NF-κB family comprises five members: RelA (p65), RelB, c-Rel, NF-κB1 (p50/p105), and NF-κB2 (p52/p100). These proteins share a conserved Rel homology domain (RHD) responsible for DNA binding and dimerization. NF-κB dimers are sequestered in the cytoplasm by inhibitory proteins, primarily the IκB family (e.g., IκBα), which mask their nuclear localization signals [30] [28] [29]. Activation occurs via two principal pathways:
- The Canonical NF-κB Pathway: This pathway is rapidly activated by a broad range of stimuli, including PAMPs (via TLRs, IL-1R), DAMPs, and cytokines like TNF-α. It primarily leads to the activation of p50:RelA and p50:c-Rel dimers [28] [29].
- The Non-Canonical NF-κB Pathway: This pathway is selectively activated by a subset of TNF receptor superfamily members (e.g., CD40, BAFFR, RANK). It involves the processing of p100 to p52, resulting in the nuclear translocation of p52:RelB dimers [29].
Table 1: Core Components of the NF-κB Signaling Pathways
| Component | Gene | Primary Function | Key Characteristics |
|---|---|---|---|
| RelA (p65) | RELA | Transcriptional activator | Contains transactivation domain; part of canonical pathway |
| p105/p50 | NFKB1 | DNA binding subunit | Processed from p105; lacks transactivation domain |
| p100/p52 | NFKB2 | DNA binding subunit | Processed from p100 in non-canonical pathway |
| RelB | RELB | Transcriptional activator | Primarily functions in non-canonical pathway |
| IκBα | NFKBIA | Inhibitory protein | Sequesters NF-κB in cytoplasm; primary target in canonical pathway |
| IKKα | CHUK | Kinase subunit | Critical for non-canonical pathway; also involved in canonical |
| IKKβ | IKBKB | Kinase subunit | Main catalytic driver of canonical pathway |
| NEMO (IKKγ) | IKBKG | Regulatory subunit | Essential scaffold for canonical IKK complex activation |
| NIK | MAP3K14 | Kinase | Central regulator of non-canonical pathway |
Mechanism of Canonical NF-κB Activation
The canonical pathway is a model of inducible, ubiquitin-dependent signal transduction. The process can be broken down into key steps, as illustrated in the diagram below:
Diagram 1: Canonical NF-κB Activation Pathway.
- Receptor Proximal Signaling: Ligation of receptors like TLR4 by LPS leads to the recruitment of adapter proteins (e.g., MyD88, TRIF), initiating a kinase cascade involving IRAKs and TRAF6. TRAF6 acts as an E3 ubiquitin ligase, generating K63-linked ubiquitin chains that activate the kinase TAK1 [28] [29].
- IKK Complex Activation: TAK1 phosphorylates and activates the IKK complex (IKKα, IKKβ, NEMO). IKKβ is the critical kinase for the canonical pathway [29].
- IκBα Phosphorylation and Degradation: The activated IKK complex phosphorylates IκBα on two critical N-terminal serine residues. This phosphorylation tags IκBα for K48-linked ubiquitination and subsequent degradation by the 26S proteasome [30] [28].
- NF-κB Translocation and Transcription: With IκBα degraded, the canonical NF-κB dimer (typically p50:RelA) is freed, exposes its nuclear localization signal, and translocates to the nucleus. There, it binds to κB enhancer elements and drives the expression of target genes, including those encoding pro-inflammatory cytokines (TNFα, IL-6, IL-1β), chemokines, adhesion molecules, and its own inhibitor, IκBα, which creates an auto-regulatory negative feedback loop [27] [28].
Mechanism of Non-Canonical NF-κB Activation
The non-canonical pathway is characterized by its reliance on the kinase NIK (NF-κB Inducing Kinase) and the processing of NF-κB2 p100 to p52.
Diagram 2: Non-Canonical NF-κB Activation Pathway.
- NIK Stabilization: In unstimulated cells, NIK is continuously bound and targeted for degradation by a complex containing TRAF3 and cIAP1/2. Engagement of receptors like CD40 or BAFFR leads to the degradation of TRAF3, allowing NIK to accumulate [29].
- p100 Phosphorylation and Processing: NIK, in concert with IKKα, phosphorylates the C-terminal region of p100. This phosphorylation event triggers the polyubiquitination and partial proteasomal degradation of p100, removing its IκB-like inhibitory domain and generating the mature p52 subunit [29].
- Nuclear Translocation: The processed p52:RelB dimer translocates to the nucleus to regulate genes involved in lymphoid organ development, B-cell maturation, and adaptive immunity [29].
Inflammasome Activation Pathway
Inflammasomes are multi-protein cytoplasmic complexes that serve as activation platforms for inflammatory caspases, primarily caspase-1. Their activation is a key mechanism for the maturation and secretion of the potent pro-inflammatory cytokines IL-1β and IL-18, and for the induction of a pro-inflammatory form of cell death called pyroptosis [27].
Inflammasome Assembly and Function
Inflammasomes are typically composed of a sensor protein (a PRR), the adapter protein ASC, and pro-caspase-1. Sensor proteins can be NLRs (e.g., NLRP3), ALRs (e.g., AIM2), or others.
Diagram 3: Canonical Inflammasome Activation (Two-Signal Model).
- Priming (Signal 1): This initial step is often provided by PAMPs (e.g., LPS via TLR4) or cytokines that activate NF-κB. This leads to the transcriptional upregulation of inflammasome components, including the sensor protein (e.g., NLRP3) and the inactive precursor cytokines pro-IL-1β and pro-IL-18 [27].
- Activation (Signal 2): A second, distinct signal triggers the assembly of the inflammasome complex. This signal can be provided by a wide range of DAMPs and PAMPs, including extracellular ATP (via P2X7 receptor inducing K+ efflux), crystalline structures (e.g., uric acid crystals, cholesterol crystals), reactive oxygen species (ROS), and microbial toxins [7].
- Caspase-1 Activation and Effector Functions: Upon sensing the activation signal, the sensor protein oligomerizes and recruits ASC, which then aggregates into a large filamentous structure ("speck") that recruits and activates pro-caspase-1 through proximity-induced autoproteolysis. Active caspase-1 then:
- Cleaves pro-IL-1β and pro-IL-18 into their biologically active forms.
- Cleaves gasdermin D (GSDMD); the N-terminal fragment of GSDMD forms pores in the plasma membrane, leading to pyroptosis—a lytic cell death that releases inflammatory contents, including mature cytokines [7].
Experimental Protocols for Key Pathway Analysis
Protocol: Assessing Canonical NF-κB Activation by Immunoblotting
This protocol is a cornerstone for evaluating pathway activity in response to PAMPs like LPS.
Method:
- Cell Stimulation: Seed immortalized macrophages (e.g., RAW 264.7, THP-1 derived) in 6-well plates. Stimulate with a canonical NF-κB inducer (e.g., 100 ng/mL E. coli LPS) for time points ranging from 0 to 120 minutes.
- Protein Extraction: Lyse cells in RIPA buffer supplemented with protease and phosphatase inhibitors. Centrifuge at 14,000 x g for 15 minutes at 4°C to collect the supernatant (whole cell lysate). For nuclear-cytoplasmic fractionation, use a commercial kit to separate fractions.
- Immunoblotting: Resolve 20-30 μg of protein by SDS-PAGE and transfer to a PVDF membrane. Probe with the following primary antibodies:
- Phospho-IκBα (Ser32/36)
- Total IκBα
- Phospho-IKKβ (Ser177)
- NF-κB p65
- Lamin B1 (nuclear fraction control)
- β-Actin (loading control)
- Detection and Analysis: Use HRP-conjugated secondary antibodies and chemiluminescent substrate for detection. Key indicators of activation are the rapid degradation of total IκBα and the appearance of phospho-IκBα, followed by the accumulation of p65 in the nuclear fraction.
Protocol: Measuring NLRP3 Inflammasome Activation
This protocol utilizes a two-signal model to trigger and assess inflammasome function.
Method:
- Cell Priming: Differentiate THP-1 monocytes into macrophages using 100 nM PMA for 48 hours. Prime the cells with 1 μg/mL LPS for 3 hours to induce pro-IL-1β and NLRP3 expression (Signal 1).
- Inflammasome Activation: Aspirate the medium and provide Signal 2 for 1-2 hours. Common activators include:
- 5 mM ATP (transfected or added to medium for 30 minutes)
- 20 μM nigericin (45 minutes)
- 250 μg/mL monosodium urate (MSU) crystals (4-6 hours)
- Sample Collection: Collect the cell culture supernatant. Lyse the remaining cells with RIPA buffer to obtain the cell lysate.
- Analysis:
- ELISA: Quantify mature IL-1β in the supernatant and cell lysate using a specific ELISA kit. Successful activation is indicated by high levels of IL-1β in the supernatant.
- Immunoblotting: Analyze supernatant (concentrated via TCA precipitation) and lysate for caspase-1 cleavage (detection of p20 subunit) and IL-1β processing (mature p17 form).
- Cell Death Assay: Measure lactate dehydrogenase (LDH) release into the supernatant as an indicator of pyroptosis.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Studying NF-κB and Inflammasome Pathways
| Reagent / Assay | Function / Target | Example Use |
|---|---|---|
| Ultrapure LPS | TLR4 agonist; priming signal | Canonical NF-κB activation; Inflammasome priming [28] |
| Recombinant TNF-α | TNFR agonist | Canonical NF-κB activation and study of feedback kinetics [29] |
| BAFF / CD40L | TNFR superfamily ligands | Specific activation of the non-canonical NF-κB pathway [29] |
| IKK Inhibitors (e.g., BMS-345541) | Selective IKKβ inhibitor | Inhibition of canonical NF-κB signaling; mechanism studies [29] |
| NLRP3 Activators (ATP, Nigericin, MSU Crystals) | Induce K+ efflux / lysosomal damage | Provide signal 2 for NLRP3 inflammasome assembly [7] |
| MCC950 | Selective NLRP3 inhibitor | Pharmacological inhibition of NLRP3 inflammasome [7] |
| VX-765 | Caspase-1 inhibitor | Inhibition of inflammasome-mediated cytokine processing and pyroptosis [7] |
| Phospho-specific Antibodies (IκBα Ser32/36, IKK S177/181) | Detect active pathway states | Immunoblot analysis of pathway activation kinetics [28] [29] |
| ELISA Kits (IL-1β, IL-6, TNF-α) | Quantify cytokine secretion | Functional readout of NF-κB and inflammasome activity |
| LDH Cytotoxicity Assay Kit | Measure plasma membrane integrity | Quantification of pyroptosis following inflammasome activation [7] |
Data Presentation: Quantitative Pathway Kinetics
Table 3: Representative Kinetic and Dosage Data for Pathway Inducers and Inhibitors
| Stimulus / Inhibitor | Typical Working Concentration | Time to Peak Activity | Primary Readout |
|---|---|---|---|
| LPS (TLR4 agonist) | 10-100 ng/mL | IκBα degradation: 15-30 min; Cytokine mRNA: 1-4 h | Phospho-IκBα, Nuclear p65, TNF-α secretion [28] |
| TNF-α | 10-50 ng/mL | IκBα degradation: 5-15 min | Phospho-IκBα, Nuclear p65 [29] |
| ATP (NLRP3 activator) | 1-5 mM | IL-1β secretion: 30-60 min | Caspase-1 p20, Mature IL-1β in supernatant [7] |
| Nigericin (NLRP3 activator) | 10-20 μM | IL-1β secretion: 45-90 min | Caspase-1 p20, Mature IL-1β, LDH release [7] |
| BMS-345541 (IKKβ inhibitor) | 1-10 μM | Pre-incubation 1 h; blocks IκBα phosphorylation | Suppression of LPS-induced cytokine production [29] |
| MCC950 (NLRP3 inhibitor) | 0.1-1 μM | Pre-incubation 30-60 min; blocks ASC oligomerization | Inhibition of ATP/nigericin-induced IL-1β release [7] |
A cytokine and chemokine storm represents a life-threatening, dysregulated immune response characterized by the uncontrolled and excessive release of pro-inflammatory mediators. This systemic inflammatory cascade, while intended as a defense mechanism, can inflict severe tissue damage and precipitate organ failure, posing significant clinical challenges in conditions such as severe infections, sepsis, and autoimmune disorders [31] [32]. The pathogenesis of this storm is intrinsically linked to the innate immune system's initial recognition of invading pathogens via specialized Pattern Recognition Receptors (PRRs) that detect conserved Pathogen-Associated Molecular Patterns (PAMPs) [33] [32]. The ensuing signal transduction and transcriptional activation initiate a powerful inflammatory cascade, which, if unchecked, can escalate into the systemic turmoil of a cytokine storm. This technical guide delves into the molecular mechanisms orchestrating this early inflammatory response, providing a detailed framework for researchers and drug development professionals engaged in immunology and therapeutic intervention.
Molecular Initiation: PAMP Recognition and PRR Signaling
The cytokine storm is initiated at the molecular level by the engagement of PRRs with PAMPs. PRRs are germline-encoded host sensors that can be broadly categorized into transmembrane receptors, such as Toll-like Receptors (TLRs) and C-type Lectin Receptors (CLRs), and cytosolic receptors, including NOD-like Receptors (NLRs), AIM2-like Receptors (ALRs), and RIG-I-like Receptors (RLRs) [33]. A distinct group of inhibitory PRRs (iPRRs) has also been identified, which help prevent immune overactivation and maintain homeostasis by providing contextual balance to the danger signals [33].
Toll-like Receptors (TLRs) serve as prototypical initiators. For instance, TLR4 recognizes lipopolysaccharide (LPS) from Gram-negative bacteria [33]. Upon ligand binding, TLRs dimerize and undergo a conformational change that facilitates the recruitment of adaptor proteins via homotypic interactions between their Toll/Interleukin-1 Receptor (TIR) domains [33]. This assembly nucleates a complex signaling cascade.
The diagram below illustrates the core signaling pathways triggered by PRR engagement, culminating in the transcriptional activation of pro-inflammatory cytokines and type I interferons.
Figure 1: PRR Signaling Pathways. PAMP binding to PRRs (e.g., TLRs) activates two major adaptor proteins, MyD88 and TRIF. The MyD88-dependent pathway leads to IKK complex activation, degradation of IκBα, and nuclear translocation of NF-κB. The TRIF-dependent pathway activates TBK1, which phosphorylates IRF3. These transcription factors drive the expression of pro-inflammatory cytokines and type I interferons, respectively [33] [32].
The Inflammasome Nexus: Amplification via IL-1 Family Cytokines
A critical amplification step in the cytokine storm involves the activation of multi-protein complexes known as inflammasomes. Cytosolic PRRs, such as NLRP3, NLRP1, NLRC4, and AIM2, can nucleate inflammasome assembly in response to PAMPs or host-derived Damage-Associated Molecular Patterns (DAMPs), such as extracellular ATP or uric acid crystals [34].
The core inflammasome structure consists of a sensor protein (e.g., NLRP3), the adaptor protein ASC (Apoptosis-associated Speck-like protein containing a CARD), and the effector protease caspase-1 [34]. Assembly leads to caspase-1 activation, which performs two key functions:
- Proteolytic maturation of the potent pro-inflammatory cytokines IL-1β and IL-18.
- Cleavage of Gasdermin D (GSDMD), whose N-terminal fragment forms pores in the plasma membrane, facilitating the release of the mature cytokines and initiating an inflammatory form of cell death known as pyroptosis [34]. The membrane rupture in pyroptosis is further mediated by the membrane protein NINJ1 [34].
The following diagram details the sequential process of canonical inflammasome activation and its functional consequences.
Figure 2: Inflammasome Activation. A two-step process is required for canonical inflammasome activation. The priming signal (e.g., via TLR-NF-κB) upregulates components like NLRP3 and pro-IL-1β. A second activation signal (PAMP/DAMP) triggers inflammasome assembly, activating caspase-1, which processes IL-1β, IL-18, and GSDMD to drive inflammation and pyroptosis [34] [32].
Quantitative Profiling of the Storm: Key Cytokines and Chemokines
The synergistic action of PRR signaling and inflammasome activation results in the massive release of cytokines and chemokines. The table below summarizes the key mediators, their primary cellular sources, and main functions in orchestrating the inflammatory response. Notably, IL-6 is a dominant marker due to its significant role in the inflammatory response associated with severe cytokine storms [35].
Table 1: Key Mediators in Cytokine and Chemokine Storms
| Mediator | Primary Cell Source | Main Functions in the Storm |
|---|---|---|
| IL-6 | Macrophages, Dendritic Cells, T cells | Fever, acute phase protein production, T & B cell activation, a dominant marker in severe storms [36] [35]. |
| TNF-α | Macrophages, Neutrophils, NK cells | Systemic inflammation, endothelial activation, vascular permeability, pyroptosis initiation [31] [32]. |
| IL-1β | Macrophages, Monocytes | Potent pyrogen, endothelial activation, neutrophil recruitment, requires inflammasome processing [34] [32]. |
| IL-18 | Macrophages, Kupffer cells | Induces IFN-γ production, enhances NK and T cell cytotoxicity [34]. |
| IFN-γ | NK cells, T cells, Macrophages | Activates macrophages, enhances antigen presentation, contributes to tissue damage [36] [31]. |
| GM-CSF | T cells, Macrophages, Endothelial cells | Drives myeloid cell differentiation and activation; aberrant expression drives excessive inflammation [36]. |
| IL-8 (CXCL8) | Macrophages, Endothelial cells | Potent neutrophil chemoattractant and activator [37]. |
| MCP-1 (CCL2) | Macrophages, Endothelial cells | Recruits monocytes and macrophages to sites of inflammation [35]. |
Quantitative assessment is critical for risk stratification. Dose-response relationships have been established for key cytokines. For instance, the effective dose (ED₅₀) for CXCL8 release is exceptionally low at 0.01 μg mL⁻¹, followed by IL-6 (0.39 μg mL⁻¹), IL-1β (0.46 μg mL⁻¹), and TNF-α (0.56 μg mL⁻¹), indicating a particularly high potency for CXCL8 induction in response to persistent antigenic stimuli like the SARS-CoV-2 spike protein [37].
Experimental Models and Methodologies
Studying the cytokine storm requires robust in vitro and ex vivo models that recapitulate the hyperinflammatory response. A common methodology involves stimulating immune cells with specific PAMPs or viral proteins and quantifying the resulting cytokine output.
Detailed Protocol: Spike Protein-Induced Cytokine Release in Human Macrophages
Objective: To characterize the dose-response relationship between SARS-CoV-2 spike protein concentration and the release of proinflammatory mediators from human macrophages [37].
Materials and Reagents:
- Primary Cells: Human Lung Macrophages (HLMs) or human monocyte-derived macrophages.
- Stimulant: Recombinant SARS-CoV-2 spike protein (S1 subunit or full-length).
- Culture Media: RPMI-1640 or DMEM supplemented with 10% FBS and 1% Penicillin/Streptomycin.
- Positive Control: Lipopolysaccharide (LPS) at 1 μg mL⁻¹.
- Assay Kits: ELISA or multiplex bead-based arrays for IL-6, IL-1β, TNF-α, and CXCL8.
Procedure:
- Cell Seeding: Seed HLMs in 96-well plates at a density of 1x10⁵ cells per well in complete media. Incubate overnight at 37°C, 5% CO₂ to allow cell adherence.
- Stimulation: Prepare serial dilutions of the spike protein in culture media. Replace the media in the wells with the spike protein solutions, covering a concentration range (e.g., 0.001 to 10 μg mL⁻¹). Include negative control (media only) and positive control (LPS) wells.
- Incubation: Incubate the plate for 18-24 hours under standard culture conditions.
- Supernatant Collection: Carefully centrifuge the plate and collect the cell-free supernatants for cytokine analysis.
- Cytokine Quantification: Determine the concentrations of IL-6, IL-1β, TNF-α, and CXCL8 in the supernatants using validated ELISA kits according to the manufacturer's instructions.
- Data Analysis: Fit the dose-response data to a three-parameter Hill model:
E(D) = Emax / (1 + ED50 / Dⁿ), whereE(D)is the effect (cytokine concentration or fraction of LPS response),Emaxis the maximum effect,ED50is the half-maximal effective dose,Dis the spike protein dose, andnis the Hill coefficient [37].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for Cytokine Storm Research
| Research Reagent | Function/Application | Example Use Case |
|---|---|---|
| Recombinant PAMPs (e.g., LPS, Poly(I:C)) | Ligands for specific PRRs (TLR4, TLR3) used to trigger defined inflammatory pathways in vitro and in vivo [33]. | Studying TLR4-mediated NF-κB signaling and cytokine production in macrophages. |
| SARS-CoV-2 Spike Protein | A key viral PAMP/antigen that can trigger prolonged immune activation and cytokine release, relevant for studying COVID-19-related storms [37]. | Modeling post-COVID sequelae (Long COVID) and dose-response relationships in immune cells. |
| Cytokine ELISA/Multiplex Assays | Quantitative measurement of specific cytokine and chemokine levels in cell culture supernatants, serum, or plasma. | Profiling the cytokine storm in patient samples or experimental models for biomarker discovery. |
| NLRP3 Inhibitors (e.g., MCC950) | Selective small-molecule inhibitors of the NLRP3 inflammasome. | Investigating the contribution of inflammasome-derived IL-1β and pyroptosis to the overall cytokine storm pathology [34]. |
| Neutralizing Antibodies (e.g., anti-IL-6R, anti-TNF-α) | Block the activity of specific cytokines or their receptors. | Mechanistic studies to delineate the role of a specific cytokine and pre-clinical evaluation of therapeutic candidates. |
The cytokine and chemokine storm represents a critical juncture in the host response to infection, where the protective mechanisms of innate immunity, initiated by PAMP recognition, spiral into a self-destructive and often lethal systemic inflammation. A deep understanding of the molecular choreography—from PRR signaling and inflammasome activation to the quantitative dynamics of cytokine release—is paramount for the scientific community. The experimental frameworks and quantitative data summarized here provide a foundation for advancing this understanding. Future research must continue to dissect the complex regulatory networks and temporal shifts in immune phenotypes to develop targeted, effective immunomodulatory strategies that can calm the storm without compromising host defense.
Distinguishing PAMPs from DAMPs and the Emerging Role of LAMPs
The immune system's ability to discriminate between harmful invaders and self-tissues represents a cornerstone of protective immunity. For decades, this paradigm was understood through the lens of "self versus non-self" recognition, a framework established by Charles Janeway in 1989 [33] [2]. This model introduced the concept of Pathogen-Associated Molecular Patterns (PAMPs)—conserved microbial motifs recognized by germline-encoded Pattern Recognition Receptors (PRRs) [33] [2]. This discovery provided the molecular basis for understanding infectious inflammation. A pivotal expansion of this theory emerged in 1994 with Polly Matzinger's "Danger Model," which proposed that immune activation responds not solely to foreignness but to endogenous danger signals emanating from damaged, stressed, or dying cells [38] [39] [33]. This conceptual shift led to the identification of Damage-Associated Molecular Patterns (DAMPs) as critical initiators of sterile inflammation. More recently, a third category of immune stimuli has been defined: Lifestyle-Associated Molecular Patterns (LAMPs). These molecules, derived from lifestyle-related factors and chronic conditions, are increasingly recognized as key drivers of maladaptive immune responses in non-communicable diseases [26]. This whitepaper provides a technical distinction between these three classes of immune activators, detailing their recognition, signaling pathways, and roles in disease pathogenesis, with a specific focus on their relevance to inflammation initiation research.
Defining the Molecular Patterns: PAMPs, DAMPs, and LAMPs
Pathogen-Associated Molecular Patterns (PAMPs)
PAMPs are highly conserved, essential molecular structures unique to microorganisms but absent in the host, enabling the immune system to reliably detect infection [2]. They are recognized by a diverse array of PRRs, including Toll-like receptors (TLRs), C-type lectin receptors (CLRs), NOD-like receptors (NLRs), and RIG-I-like receptors (RLRs) [33] [2]. The recognition of PAMPs by PRRs on innate immune cells triggers signaling cascades that lead to the production of inflammatory cytokines and type I interferons, initiating host defense and bridging innate and adaptive immunity [33] [2].
Table 1: Characteristics of Major PAMP Classes
| Pathogen Class | Exemplary PAMPs | Sensing PRRs | Key Structural Motifs |
|---|---|---|---|
| Gram-negative Bacteria | Lipopolysaccharide (LPS), Peptidoglycan | TLR4 (TLR4-MD2 complex), TLR2 | Lipid A (in LPS), conserved glycan chains |
| Gram-positive Bacteria | Lipoteichoic Acid (LTA), Bacterial Lipoproteins | TLR2/TLR1 or TLR6 heterodimers | Lipopeptide motifs, glycerol phosphate polymers |
| Viruses | dsRNA, ssRNA, CpG DNA, Viral Glycoproteins | TLR3, TLR7/8, TLR9, RLRs (RIG-I, MDA5) | Double-stranded RNA, unmethylated CpG islands |
| Fungi | Zymosan, Mannans, β-Glucans | TLR2, Dectin-1 | Branched carbohydrate polymers (e.g., chitin, glucans) |
| Mycobacteria | Lipomannan, Lipoarabinomannan, Mycobacterial DNA | TLR2/TLR1, TLR9 | Complex cell wall lipoglycans, hypomethylated DNA |
Damage-Associated Molecular Patterns (DAMPs)
DAMPs are endogenous host molecules that are normally sequestered intracellularly or occupy specific extracellular compartments but are released, exposed, or modified following cellular stress, damage, or non-programmed cell death [38] [39] [40]. Their translocation to the extracellular milieu or alteration in concentration or physicochemical properties transforms them into potent "danger signals" that activate PRRs, often the same receptors that sense PAMPs [38] [39]. DAMPs serve as critical mediators of sterile inflammation, a pathogenic process underlying numerous autoimmune, degenerative, and metabolic diseases [38] [40].
Table 2: Classification and Features of Key DAMPs
| DAMP Class | Exemplary DAMPs | Cellular Origin | Sensing PRRs | Primary Release Mechanism |
|---|---|---|---|---|
| Nuclear Proteins | HMGB1, HMGN1, Histones, IL-1α, IL-33 | Nucleus | TLR2/4/9, RAGE, IL-1R, ST2 | Necrosis, pyroptosis, NETosis, active secretion |
| Cytosolic Proteins | S100A8/A9, HSP70, HSP90, Cyclophilin A | Cytosol | TLR2/4, RAGE, CD91, CD147 | Necrosis, passive leakage |
| Metabolites & Ions | Extracellular ATP, Uric Acid Crystals, K+ Efflux | Cytosol, Metabolic Pathways | P2X7, NLRP3 | Plasma membrane rupture, channel activation |
| Nucleic Acids | Cell-free DNA, mtDNA, RNA | Nucleus, Mitochondria | TLR9, TLR3/7/8, cGAS, AIM2 | Membrane disruption, NETosis, mitochondrial damage |
| ECM Components | LMW Hyaluronan, Biglycan, Tenascin-C, Fibronectin-EDA | Extracellular Matrix | TLR2/4, CD44, NLRP3 | Enzymatic degradation (e.g., hyaluronidase) |
Lifestyle-Associated Molecular Patterns (LAMPs)
LAMPs represent a recently defined category of immunostimulatory molecules originating from lifestyle-related factors and chronic metabolic conditions [26]. Unlike PAMPs, they are not derived from pathogens, and unlike many DAMPs, they are not primarily products of acute cellular injury. Instead, LAMPs arise from persistent metabolic dysregulation and are often inefficiently cleared, leading to chronic sterile inflammation that drives the pathogenesis of non-communicable diseases [26]. Key examples include oxidized low-density lipoprotein (oxLDL), cholesterol crystals, monosodium urate, and components of the Western diet [26]. A critical aspect of LAMP biology is their ability to induce "trained immunity," a long-term functional reprogramming of innate immune cells mediated by epigenetic and metabolic changes, which results in enhanced responses to subsequent inflammatory challenges [26]. This maladaptive trained immunity perpetuates chronic inflammation in conditions like atherosclerosis, metabolic syndrome, and chronic kidney disease [26].
Comparative Analysis: Molecular Origins, Recognition, and Functional Outcomes
The fundamental distinctions between PAMPs, DAMPs, and LAMPs lie in their origin, context of release, and the physiological purpose of the immune response they trigger. The following diagram illustrates the core conceptual relationships and immune outcomes for each class of molecular patterns.
Core Distinctions and Pathophysiological Roles
- Origin and Context: PAMPs are exclusively derived from microorganisms, signaling infection [2]. DAMPs are host-derived, signaling tissue damage, stress, or non-physiological cell death (e.g., necrosis) [38] [39]. LAMPs, while also host-derived, originate from dietary components or metabolic waste products that accumulate due to specific lifestyle factors or chronic disease states [26].
- Primary Immune Objective: The inflammatory response to PAMPs aims to eliminate an invading pathogen [38]. DAMP-induced inflammation primarily functions to promote repair of damaged tissue and restore homeostasis [38]. LAMP-induced immune activation lacks a clear protective or reparative objective and often drives chronic, pathological inflammation that underlies diseases like atherosclerosis [26].
- Nature of Immune Memory: PAMPs and some DAMPs can induce classical adaptive immune memory (T and B cell responses). A key differentiator for LAMPs is their prominent role in inducing innate immune memory or "trained immunity" [26]. This involves epigenetic reprogramming (e.g., H3K4me3, H3K27ac) and metabolic shifts (e.g., upregulation of glycolysis, mevalonate pathway) in innate immune cells and their bone marrow progenitors, leading to a hyperresponsive state upon secondary challenge [26].
Table 3: Functional and Experimental Distinctions Between PAMPs, DAMPs, and LAMPs
| Feature | PAMPs | DAMPs | LAMPs |
|---|---|---|---|
| Primary Source | Microbes (non-self) | Stressed/Damaged Host Cells (self) | Metabolic Byproducts, Diet (self) |
| Biological Role | Eradicate Infection | Initiate Tissue Repair | Induce Maladaptive Chronic Inflammation |
| Key Signaling Hubs | MyD88, TRIF, NF-κB, IRF3 | NF-κB, MAPK, Inflammasomes | mTOR-HIF1α, Mevalonate Pathway |
| Disease Association | Sepsis, Infectious Diseases | RA, SLE, I/R Injury, Trauma | Atherosclerosis, CKD, Metabolic Syndrome |
| Hallmark Assays | LAL for LPS, Bacterial Culture | LDH Release, HMGB1 ELISA, cfDNA Quantification | oxLDL ELISA, Cholesterol Crystal Imaging, Trained Immunity Re-challenge |
| Therapeutic Targeting | Antibiotics, Antivirals, TLR Antagonists | Neutralizing mAbs (e.g., anti-HMGB1), Cell Death Inhibitors | Metabolic Inhibitors, Epigenetic Modulators, Diet Modification |
Methodologies for Experimental Differentiation and Analysis
Experimental Workflow for Pattern Identification
A systematic approach is required to distinguish between PAMP-, DAMP-, and LAMP-driven immune activation in experimental models, particularly when studying complex disease etiologies. The following diagram outlines a generalized experimental workflow.
Key Methodologies and Protocols
Establishing the Origin of the Inflammatory Trigger
- PAMP Detection: Utilize sterility tests (e.g., microbial culture), limulus amebocyte lysate (LAL) assay for Gram-negative endotoxin, and PCR-based pathogen detection (e.g., 16S rRNA sequencing for bacteria) to confirm or rule out microbial contamination [41].
- DAMP Quantification: Employ enzyme-linked immunosorbent assays (ELISAs) for specific DAMPs like HMGB1, S100 proteins, or histones in serum or cell culture supernatants [40]. Measure cell-free DNA (cfDNA) using fluorescent dyes like PicoGreen or quantitative PCR [39]. Lactate dehydrogenase (LDH) release assays provide a standard measure of general cellular cytotoxicity and necrosis [39].
- LAMP and Metabolic Profiling: Quantify oxidized LDL via specific ELISA. Visualize cholesterol crystals in tissues using polarized light microscopy. Analyze urate levels in serum. For comprehensive analysis, metabolomic profiling (via LC-MS) can identify broader shifts in metabolic pathways associated with LAMP exposure [26].
Dissecting the Immune Response and Memory
- PRR Signaling Pathway Analysis: To delineate specific PRR involvement, use phospho-specific flow cytometry or western blotting to detect key signaling nodes like phospho-NF-κB, phospho-p38 MAPK, and TBK1 [33]. Utilize PRR-specific inhibitors (e.g., TAK-242 for TLR4) or gene knockdown/knockout models.
- Inflammasome Activation Assay: Measure caspase-1 activation using fluorescent substrates (e.g., FLICA) or western blotting for cleaved caspase-1. Quantify the mature forms of IL-1β and IL-18 in supernatants by ELISA, as their secretion is a hallmark of inflammasome activity [39] [40].
- Trained Immunity Protocols: To confirm LAMP-induced trained immunity, adopt a standard two-hit model [26].
- Priming Phase: Prime human monocytes or macrophages with a LAMP (e.g., oxLDL, β-glucan) for 24 hours.
- Resting Phase: Culture cells in stimulus-free medium for 5-7 days to allow a return to baseline.
- Re-challenge Phase: Re-stimulate cells with a low dose of a heterologous stimulus (e.g., LPS).
- Readout: Measure enhanced cytokine production (TNF-α, IL-6) compared to unprimed controls. Analyze associated epigenetic marks (H3K4me3, H3K27ac) via ChIP-qPCR at promoter regions of trained immunity genes and assess metabolic rewiring (e.g., increased glycolysis) via Seahorse Analyzer [26].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagent Solutions for Pattern Recognition Studies
| Reagent / Tool Category | Specific Examples | Primary Function in Research |
|---|---|---|
| PRR Agonists & Antagonists | Ultrapure LPS (TLR4), Pam3CSK4 (TLR2/1), TAK-242 (TLR4 inhibitor), MCC950 (NLRP3 inhibitor) | To specifically activate or inhibit PRR pathways and establish causal links in signaling. |
| Recombinant DAMPs/PAMPs | Recombinant HMGB1, HSP70, S100A8/A9, Flagellin, Poly(I:C) | To provide defined, pure stimuli for in vitro and in vivo models of sterile or infectious inflammation. |
| Neutralizing Antibodies | Anti-HMGB1 mAb, Anti-TLR2 mAb, Anti-RAGE mAb | To block the function of specific DAMPs or their receptors, validating their role in experimental models. |
| Cytokine Detection Assays | ELISA/Multiplex Kits for TNF-α, IL-6, IL-1β, IL-18, IFN-β | To quantify the inflammatory output of immune cells upon pattern recognition. |
| Cell Death/Permeability Assays | LDH Release Assay, Propidium Iodide, Annexin V | To distinguish between DAMP release mechanisms (e.g., necrosis vs. apoptosis). |
| Epigenetic Analysis Kits | ChIP Kits (H3K4me3, H3K27ac), DNA Methylation Kits | To investigate the epigenetic basis of LAMP-induced trained immunity. |
| Metabolic Probes & Assays | 2-NBDG (Glucose Uptake), MitoSOX (mtROS), Seahorse Assay Kits | To profile metabolic reprogramming associated with trained immunity and inflammatory activation. |
The precise distinction between PAMPs, DAMPs, and the emerging category of LAMPs is fundamental to advancing our understanding of immune activation in health and disease. While PAMPs and DAMPs initiate protective responses against infection and injury, respectively, LAMPs represent a pathophysiological driver of chronic sterile inflammation through the induction of maladaptive trained immunity. The experimental frameworks and methodologies detailed herein provide a roadmap for researchers to dissect the specific contributions of these molecular patterns in complex disease models. Targeting the specific receptors, signaling pathways, and epigenetic mechanisms underpinning LAMP recognition and response holds significant therapeutic promise for a wide spectrum of chronic inflammatory diseases, paving the way for novel treatment strategies in precision medicine.
From Bench to Bedside: Research Tools, Models, and Therapeutic Applications of PAMP Signaling
Pathogen-associated molecular patterns (PAMPs) are conserved molecular structures essential for microbial survival that are recognized by the innate immune system as "non-self" through pattern recognition receptors (PRRs) [42]. This recognition represents the initial "Signal 0" that triggers immune activation, a concept pioneered by Charles Janeway that distinguishes immune responses to pathogens from responses to innocuous antigens [42]. Lipopolysaccharide (LPS), a major component of the outer membrane of Gram-negative bacteria, serves as one of the most potent and well-characterized PAMPs in innate immunity research [43] [18]. The host defense response to LPS includes expression of various pro-inflammatory cytokines, such as tumour necrosis factor-α (TNF-α) and interferon-β (IFN-β), along with other pro-inflammatory proteins including inducible NO synthase (iNOS) [43]. Understanding LPS signal transduction provides a molecular basis for the lethal effect of LPS during septic shock and points the way to novel therapies [43]. In vitro stimulation of peripheral blood mononuclear cells (PBMCs) with LPS and other PAMPs enables researchers to model innate immune responses, investigate signaling pathways, and identify potential therapeutic targets for inflammatory diseases [44].
Molecular Recognition of PAMPs
The LPS Recognition Complex
The recognition of LPS by immune cells involves a sophisticated cascade of extracellular "pattern recognition receptors" that chaperone LPS from the bacterial membrane to the transmembrane receptor Toll-like Receptor 4 (TLR4) [45]. This process begins with LPS-binding protein (LBP), an acute-phase protein produced in the liver that circulates in the bloodstream [43] [18]. LBP recognizes and forms a high-affinity complex with the lipid A moiety of LPS, whether as free molecules, fragments, or still bound to the outer membrane of intact bacteria [43]. The primary sequence of LBP shows identity with bactericidal/permeability-increasing protein (BPI) and cholesterol ester transport protein [43]. The role of LBP is to aid LPS docking at the receptor complex by initially binding LPS and then forming a ternary complex with CD14 [43].
CD14 exists in two forms: soluble CD14 (sCD14) found in plasma, which helps convey LPS signaling in cells lacking membrane-bound CD14 (e.g., endothelial and epithelial cells), and membrane-bound CD14 (mCD14) attached to the surface of myeloid cells via a glycosylphosphatidylinositol tail [43]. CD14 was initially thought to be the receptor for LPS, but as it lacks a transmembrane domain, it was unlikely to convey signals independently [43]. Subsequent research revealed that the actual signaling receptor for LPS is TLR4, with CD14 serving to bind LPS and present it to MD-2 and TLR4 [43]. Regions of CD14 essential for LPS binding and transfer to MD-2/TLR4 have been mapped to amino acids 35–44, 144–153, 235–243, and 270–275, though none likely participate in direct association with TLR4 [43].
The secreted glycoprotein MD-2 acts as an extracellular adapter protein in TLR4 activation and is essential for LPS signaling [43]. A mutant form (C95Y) completely abolishes LPS responses, while wild-type MD-2 restores LPS responsiveness in TLR4-expressing cells lacking MD-2 [43]. MD-2 directly binds LPS, which in turn associates with TLR4 via extracellular leucine-rich repeats, inducing TLR4 aggregation and signal transduction [43]. Knockout studies in mice demonstrate that MD-2 is indispensable for LPS responses [43]. The MD-2/TLR4 complex binds lipid A with a Kd ≈ 3 nM on the surface of cells expressing CD14 [43].
Table 1: Core Components of the LPS Recognition Complex
| Component | Structure | Function | Cellular Location |
|---|---|---|---|
| LBP | 53 kDa glycoprotein, 481 amino acids, two structural domains with antiparallel β-strands surrounded by α-helix [18] | Binds LPS and facilitates transfer to CD14; disrupts LPS aggregates [45] | Serum glycoprotein, synthesized in liver, lungs, GI tract [18] |
| CD14 | 375 amino acids, curved spiral structure with thirteen β-chains, 11 overlapping LRR region [18] | Pattern recognition receptor; binds LBP-delivered LPS and presents to TLR4/MD-2 [18] | GPI-anchored membrane glycoprotein or soluble serum protein [43] |
| MD-2 | 18 kDa protein, 160 amino acids, seven conserved cysteine residues, glycosylation sites [18] | Binds LPS monomer; senses acylation pattern of lipid A; essential for TLR4 activation [45] | Secreted glycoprotein, associates with TLR4 extracellular domain [43] |
| TLR4 | 95 kDa transmembrane protein, 839 amino acids, LRR extracellular domain, cytoplasmic TIR domain [18] | Pattern recognition receptor; forms complex with MD-2; initiates intracellular signaling [18] | Type I transmembrane receptor on immune cells [43] |
Other PAMPs and Their Receptors
Beyond LPS, numerous other PAMPs activate innate immune responses through specific PRRs. Major PAMPs include microbial nucleic acids (e.g., unmethylated CpG DNA motifs, double-stranded RNA, single-stranded RNA, 5'-triphosphate RNA), lipoproteins, surface glycoproteins, and membrane components such as peptidoglycan, lipoteichoic acid, and glycosylphosphatidylinositol [42]. These are recognized by various PRRs including Toll-like receptors (TLRs), retinoid acid-inducible gene I (RIG-I)-like receptors (RLRs), AIM2-like receptors (ALRs), and nucleotide-binding oligomerization domain (NOD)-like receptors (NLRs) [42]. Most TLRs function as homodimers, though heterodimers exist for TLR1:TLR2 and TLR2:TLR6 [42]. The responsiveness to different PAMPs enables researchers to model various types of infections in vitro.
LPS-Induced Intracellular Signaling Pathways
MyD88-Dependent Pathway
The MyD88-dependent pathway represents the primary signaling cascade activated by LPS, leading to rapid pro-inflammatory gene expression. Upon LPS binding, TLR4 dimerizes and undergoes conformational changes that facilitate the recruitment of intracellular adapter proteins through homotypic interactions between TIR domains [43]. MyD88 (myeloid differentiation primary response protein 88) serves as the central adapter, recruiting interleukin-1 receptor-associated kinase (IRAK) family members through death domain interactions [18]. This complex then activates TNF receptor-associated factor 6 (TRAF6), leading to the activation of transforming growth factor-β-activated kinase 1 (TAK1) [18]. TAK1 subsequently activates both the nuclear factor-κB (NF-κB) and mitogen-activated protein kinase (MAPK) pathways [18].
NF-κB activation occurs through the phosphorylation and degradation of IκB inhibitors, allowing NF-κB dimers (typically p50/p65) to translocate to the nucleus and induce the expression of pro-inflammatory mediators including cytokines (TNF-α, IL-1β, IL-6), chemokines, and adhesion molecules [18]. Simultaneously, MAPK activation (JNK, p38) leads to the phosphorylation and activation of transcription factors such as activator protein 1 (AP-1) [18]. This pathway drives macrophage M1 polarization and the release of pro-inflammatory cytokines central to the initial immune response against Gram-negative bacteria [18].
MyD88-Independent Pathway
The MyD88-independent pathway, also known as the TRIF-dependent pathway, mediates later responses to LPS and is critical for type I interferon production [43]. This pathway employs different sets of adapters, primarily TIR-domain-containing adapter-inducing interferon-β (TRIF) and TRIF-related adapter molecule (TRAM) [43]. TRAM functions as a sorting adapter that recruits TRIF to the activated TLR4 complex [43]. TRIF then activates TRAF3 and TRAF6, leading to the activation of interferon regulatory factors (IRFs) and NF-κB, respectively [18].
The late activation of NF-κB and IRF3 through this pathway induces the production of type I interferons (IFN-α and IFN-β), cytokines, chemokines, and other transcription factors [43]. This response is particularly important for antiviral immunity and provides a delayed wave of gene expression that complements the immediate MyD88-dependent response [43]. The ability to mount both rapid and sustained responses to LPS enables the immune system to effectively combat Gram-negative bacterial infections while maintaining appropriate inflammatory tone.
Metabolic Reprogramming in LPS-Activated Immune Cells
Activation of macrophages and dendritic cells by LPS and other pro-inflammatory stimuli triggers a metabolic switch from oxidative phosphorylation (OXPHOS) to glycolysis, even in the presence of oxygen - a phenomenon analogous to the Warburg effect in tumors [46]. This metabolic reprogramming provides rapid ATP generation and biosynthetic precursors necessary for immune effector functions. Several interconnected mechanisms drive this metabolic shift:
Nitric Oxide and Mitochondrial Changes
Stimulation of macrophages and dendritic cells with LPS increases expression of inducible nitric oxide synthase (iNOS), which generates nitric oxide (NO) [46]. NO inhibits mitochondrial respiration by nitrosylating iron-sulfur proteins in electron transport chain complexes, particularly Complex I and cytochrome c oxidase [46]. This NO-mediated inhibition of mitochondrial metabolism is a key driver of the glycolytic switch, as inhibition of iNOS restores normal mitochondrial respiration while blunting the LPS-induced increase in glycolysis [46]. The amino acid arginine serves as the substrate for iNOS, and citrulline recycling via argininosuccinate synthase (Ass1) and argininosuccinate lyase (Asl) sustains optimal NO production during prolonged activation [46].
HIF-1α and Glycolytic Regulation
Hypoxia-inducible factor-1α (HIF-1α) plays a central role in promoting glycolysis under both hypoxic and normoxic conditions in LPS-activated cells [46]. HIF-1α facilitates the metabolic switch by binding to hypoxia response elements in target genes including glucose transporter GLUT1 and glycolytic enzymes [46]. It induces expression of lactate dehydrogenase (LDH), which catalyzes lactate production from pyruvate, thereby limiting acetyl-CoA production for the TCA cycle [46]. HIF-1α also increases expression of pyruvate dehydrogenase kinase, which inhibits pyruvate dehydrogenase - the enzyme that catalyzes acetyl-CoA formation from pyruvate [46]. The essential nature of this metabolic reprogramming is demonstrated by the finding that inhibition of glycolysis with 2-deoxyglucose decreases the inflammatory response to LPS, while mitochondrial respiration inhibitors have no such effect [46].
Table 2: Metabolic Changes in LPS-Activated Immune Cells
| Metabolic Parameter | Resting State | LPS-Activated State | Functional Significance |
|---|---|---|---|
| Primary Metabolic Pathway | Oxidative Phosphorylation | Aerobic Glycolysis (Warburg Effect) | Rapid ATP generation despite mitochondrial inhibition [46] |
| Glucose Consumption | Low | High | Increased glycolytic flux for energy and biosynthesis [46] |
| Lactate Production | Low | High | Regeneration of NAD+ for continued glycolysis; endpoint of anaerobic metabolism [46] |
| TCA Cycle Activity | Normal | Decreased with citrate withdrawal | Citrate used for lipid biosynthesis; succinate accumulation stabilizes HIF-1α [46] |
| Pentose Phosphate Pathway | Basal activity | Increased | Generates NADPH for ROS production and nucleotides for biosynthesis [46] |
| Mitochondrial Function | ATP production | ROS production, inhibited respiration | Shift from energy production to bactericidal function [46] |
Experimental Models: PBMC Stimulation with PAMPs
Establishing PBMC Stimulation Protocols
Peripheral blood mononuclear cells (PBMCs) serve as a valuable ex vivo model for investigating innate immune responses to PAMPs. A 2024 study employed comprehensive multi-omic profiling of pathogen-stimulated PBMCs from healthy donors to discover new transcript and protein isoforms expressed during immune responses [44]. In this experimental setup, PBMCs were stimulated for 24 hours with various microbial stimuli mimicking bacterial (E. coli LPS, S. aureus), viral (poly(I:C)), and fungal (C. albicans) infections, with RPMI incubation as a negative control [44]. This approach enables researchers to compare immune responses across different pathogen types while controlling for inter-individual variability.
The selection of appropriate PAMP concentrations and stimulation durations depends on the specific research objectives. For acute inflammatory responses, LPS concentrations typically range from 10-100 ng/mL over 6-24 hours, while longer exposures or chronic models may utilize lower concentrations (0.1-10 ng/mL) over several days [44] [47]. The timing of analysis is critical, as early signaling events (NF-κB activation, MAPK phosphorylation) may peak within minutes to hours, while cytokine production typically peaks between 6-24 hours, and phenotypic changes may require several days [44].
Multi-Omic Analysis of Immune Responses
Advanced sequencing technologies have revolutionized our understanding of PBMC responses to PAMP stimulation. Long-read transcriptome profiling reveals novel sequences and isoform switching induced upon pathogen stimulation, including transcripts that are difficult to detect using traditional short-read sequencing [44]. A 2024 study identified a total of 37,312 unique transcript sequences from 11,872 genes across all samples, with 47.4% of detected transcripts being novel [44]. Widespread loss of intron retention occurs as a common result of all pathogen stimulations, representing a previously underappreciated layer of immune regulation [44].
Integrated transcriptomic and proteomic analysis enables comprehensive characterization of the immune response. Such studies typically identify hundreds to thousands of differentially expressed genes (DEGs) and proteins depending on the stimulus [44] [48]. For instance, pairwise comparisons in PBMC stimulation experiments identified 9,776 DEGs for S. aureus versus PBS control, 10,230 for P. mirabilis versus control, and 1,309 for S. aureus versus P. mirabilis [48]. Similarly, proteomic analyses revealed 175 differentially expressed proteins (DEPs) for S. aureus versus control, 277 for P. mirabilis versus control, and 223 for S. aureus versus P. mirabilis [48]. Pathway analysis typically shows enrichment in immune system pathways, apoptosis, Toll and IMD signaling pathways, MAPK signaling, and NF-κB signaling [48].
Research Applications and Implications
Modeling Neuroinflammatory Responses
LPS stimulation models have proven valuable for investigating neuroinflammatory processes relevant to neurological and psychiatric disorders. Chronic LPS exposure induces a depressive-like phenotype in rodents that extends beyond acute sickness behavior, providing insights into the molecular mechanisms linking neuroinflammation to depression [47]. Studies in Sprague Dawley rats demonstrate that both single and multiple LPS doses induce systemic inflammation and subsequent neuroinflammation, evidenced by increased circulating concentrations and regional brain expression of pro-inflammatory cytokines (Tnf-α and Il1β) [47]. These effects exhibit time- and region-specific patterns, with single LPS administration reducing open field exploration after one week, while repeated LPS exposure reduces sucrose consumption - an indicator of anhedonia [47].
LPS administration also shows time- and region-specific effects on neurotrophin expression, with increased mRNA expression of Ngf and Nt-3 in both short-term and long-term LPS groups, while Bdnf and Il6 expression increases only in long-term LPS groups, and Creb expression increases only in short-term LPS groups [47]. These findings suggest that in LPS-induced systemic inflammation, Tnf-α and Il1β drive region-specific neurodegeneration via apoptotic processes, while Il6 and its regulatory interaction with neurotrophins may serve as a protective mechanism in neuroinflammation [47].
Trained Immunity and Immunomodulation
The concept of trained immunity has recently gained relevance in understanding how innate immune responses are regulated in various diseases. Trained immunity refers to the adaptation of innate immune cells based on previous insults, resulting in enhanced responses upon re-exposure [49]. Hematopoietic progenitors in bone marrow and peripheral innate immune cells can undergo epigenetic and metabolic reprogramming that establishes this innate immune memory [49]. LPS challenge can induce trained immunity that provides heterologous protection against subsequent infections, as demonstrated by studies showing that intranasal LPS challenge confers protection against S. pneumoniae infection [49].
Trained immunity is induced by immunological signaling and metabolic reprogramming mediated by HIF-1α downstream of mTOR, directing a shift towards aerobic glycolysis and allowing accumulation of metabolites that fuel histone modifying enzymes [49]. Epigenetic reprogramming in trained immunity is mediated through deposition of H3K4me1, H3K4me3, H3K18la, and H3K27ac histone marks in promoter or enhancer regions of inflammatory response genes, leading to permissive chromatin and facilitated expression [49]. This phenomenon represents an important consideration when interpreting repeated stimulation experiments and has therapeutic implications for enhancing immune responses in immunosuppressed individuals.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for PAMP Stimulation Studies
| Reagent Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| PAMP Stimuli | E. coli LPS, S. aureus, Poly(I:C), C. albicans [44] | Mimic bacterial, viral, and fungal infections; activate specific PRR pathways | Purity critical for specificity; concentration and timing determine response profile [44] |
| Cell Isolation Kits | Ficoll-Paque PLUS, PBMC isolation kits | Isolation of peripheral blood mononuclear cells from whole blood | Preserve cell viability and functionality; minimize activation during isolation [44] |
| Culture Media | RPMI-1640, DMEM with standardized supplements | Maintain cell viability and support immune responses | Serum lot consistency important; antibiotic use may affect responses [44] |
| TLR4 Pathway Inhibitors | TAK-242, CLI-095, E5531 [43] [18] | Specific inhibition of TLR4 signaling; mechanistic studies | E5531 directly inhibits MD-2/TLR4 complex independent of CD14 [43] |
| Cytokine Detection | ELISA kits, Multiplex bead arrays, ELISpot | Quantify inflammatory mediators (TNF-α, IL-1β, IL-6, IFNs) | Dynamic range should match expected concentrations; consider secretion versus intracellular [50] |
| Transcriptomics Tools | RNA extraction kits, long-read sequencing, qPCR reagents | Gene expression analysis, novel isoform detection | Long-read sequencing reveals full-length transcripts and splicing variants [44] |
| Proteomics Solutions | TMT reagents, mass spectrometry, antibody arrays | Protein expression quantification, secretome analysis | Correlation with mRNA data often incomplete; provides functional validation [44] |
In vitro models using LPS and other PAMPs to stimulate immune cells represent a cornerstone of innate immunity research, providing insights into signaling pathways, gene regulation, and metabolic reprogramming underlying inflammatory responses. The LPS-TLR4 signaling pathway exemplifies the complexity of these responses, involving precisely coordinated extracellular recognition and intracellular signal transduction that determines immunological outcomes. Advanced multi-omic approaches now enable comprehensive characterization of these responses at unprecedented resolution, revealing novel transcripts, proteoforms, and regulatory mechanisms. These models continue to provide fundamental insights with translational relevance for infectious diseases, neurodegenerative disorders, cancer, and therapeutic development. As research progresses, particularly in understanding trained immunity and heterologous protection, these in vitro systems will remain essential tools for deciphering the complexities of innate immune recognition and response.
The study of inflammation in vivo is fundamental to understanding host defense mechanisms, disease pathogenesis, and developing novel therapeutic interventions. Inflammation is a complex biological response to harmful stimuli, characterized by two primary phases: acute inflammation, which serves as the primary line of host defense, and chronic inflammation, which can develop when the inducing agent persists, often with detrimental consequences [51]. Central to the initiation of inflammatory responses are pathogen-associated molecular patterns (PAMPs), which are conserved microbial structures recognized by the innate immune system, and damage-associated molecular patterns (DAMPs), which are endogenous molecules released during cellular damage or stress [52] [53].
Animal challenge models provide indispensable platforms for investigating the mechanisms of inflammation in a controlled, physiological context where complex interactions between immune cells, mediators, and tissues can be studied in their entirety. These models allow researchers to dissect the molecular pathways triggered by PAMPs and DAMPs, from initial recognition by pattern recognition receptors (PRRs) to the downstream activation of transcription factors such as nuclear factor kappa B (NF-κB) and the production of inflammatory cytokines [51] [54]. The use of these models has been essential for inflammation research, offering insights into biological processes that are often unfeasible to study in humans due to ethical and financial constraints [51]. This guide provides a comprehensive technical resource for researchers utilizing animal challenge models to study systemic and localized inflammation within the broader context of PAMP-driven immune activation.
Animal Models for Inflammation Research
Model Selection Criteria
Selecting an appropriate animal model is crucial and depends heavily on the research question and hypothesis. Key considerations include:
- Genetic and physiological similarity to humans in the relevant inflammatory pathways.
- The specific phase of inflammation (acute vs. chronic) under investigation.
- The organ system or tissue of interest (e.g., gut, brain, systemic circulation).
- The feasibility of genetic manipulation for mechanistic studies.
- Practical aspects such as reproductive cycle, lifespan, and handling requirements [51].
Comparative Analysis of Common Animal Models
The following table summarizes the primary animal models used in inflammation research, highlighting their key features and applications related to PAMP and DAMP sensing.
Table 1: Comparison of Animal Models for Inflammation Research
| Animal Model | Genetic/Physiological Relevance to Humans | Strengths and Applications | Limitations |
|---|---|---|---|
| Mice (Mus musculus) | ~85% genome similarity; conserved NF-κB activation, neutrophil chemotaxis, and TLR signaling [51]. | - Genetic manipulability (transgenic, knockout strains) [51] [55].- Short gestation (~21 days) and rapid sexual maturity (5-8 weeks) [51].- Well-characterized models for IBD, sepsis, and autoinflammation [55] [56]. | - Genetically identical inbred strains lack human population heterogeneity [51].- Some models require genetic modification for human pathogen susceptibility (e.g., SARS-CoV-2) [57]. |
| Rats (Rattus norvegicus) | ~85% genome similarity; preferred in genetics and genomics research [51]. | - Larger size facilitates surgical procedures and repeated sampling.- Robust models for chemical-induced colitis and complex disease studies [55]. | - Fewer genetic tools available compared to mice. |
| Zebrafish (Danio rerio) | High conservation of innate and adaptive immune system components [51]. | - Optical transparency allows real-time, in vivo imaging of inflammatory processes.- Useful for large-scale genetic and therapeutic screens [51] [55]. | - Limited adaptive immunity in early stages of development.- Physiological differences from mammals. |
| Caenorhabditis elegans | Conserved innate immune defense mechanisms [51]. | - Powerful model for host-pathogen interactions and innate immunity signaling [51] [55].- Short life cycle and ease of cultivation enable high-throughput studies. | - Lacks an adaptive immune system and many mammalian cell types. |
| Non-Human Primates | Close physiological and immunological similarity to humans [55]. | - Ideal for translating basic research findings to clinical applications.- Spontaneous models of colitis exist [55]. | - High cost, ethical constraints, and specialized housing requirements. |
| Guinea Pigs | Unique neurological and immunological interplay [55]. | - Valuable for studying the gut-brain axis and neuro-immune interactions in inflammation [55]. | - Less common, with fewer species-specific reagents available. |
Modeling Systemic Inflammation
Systemic inflammation involves a widespread, often dysregulated, immune response that can lead to multi-organ dysfunction. Animal models of systemic inflammation are critical for understanding conditions like sepsis and for evaluating anti-inflammatory therapeutics.
Lipopolysaccharide (LPS)-Induced Systemic Inflammation
Experimental Protocol:
- Animal Preparation: Typically use mice (e.g., C57BL/6) or rats (e.g., Sprague-Dawley), 8-12 weeks old.
- LPS Administration: LPS from Escherichia coli is the most common PAMP inducer. It is administered via intraperitoneal (IP) or intravenous (IV) injection. The dose ranges from 1 to 20 mg/kg, depending on the desired severity [58].
- Monitoring: Animals are monitored for sickness behavior (lethargy, piloerection), weight loss, and hypothermia. Blood and tissue samples are collected at predetermined timepoints for analysis.
- Endpoint Analysis: Includes plasma cytokine profiling (TNF-α, IL-1β, IL-6), histopathological examination of organs (lung, liver, kidney), and immune cell phenotyping via flow cytometry [58].
Mechanistic Insights: LPS is a prototypical PAMP from Gram-negative bacteria. It binds to the TLR4/MD2/CD14 complex on immune cells (e.g., macrophages), initiating a downstream signaling cascade. This cascade activates NF-κB and MAPK pathways, leading to a storm of pro-inflammatory cytokines [58] [54]. The following diagram illustrates the core LPS/TLR4 signaling pathway.
Diagram Title: LPS-Induced TLR4 Signaling and NF-κB Activation
Inflammasome Activation in Sepsis Models
Sepsis is a life-threatening syndrome characterized by a dysregulated host response to infection. Inflammasomes, cytosolic multiprotein complexes (e.g., NLRP3, NLRC4, AIM2), are critical platforms that sense PAMPs and DAMPs in sepsis. Their activation leads to the maturation of IL-1β and IL-18 and induction of pyroptosis, a pro-inflammatory cell death [53].
Experimental Protocol for NLRC4-Associated Autoinflammation:
- Animal Model: Use genetically engineered knock-in mice expressing a gain-of-function mutation in the Nlrc4 gene (e.g., V341A) [56].
- Phenotypic Monitoring: Monitor for systemic inflammation, including growth retardation, diarrhea, and mortality. Assess cytopenia (reduction in blood cells) and hemophagocytosis (engulfment of blood cells by macrophages) [56].
- Molecular Analysis: Measure caspase-1 and gasdermin D (GSDMD) cleavage in intestinal epithelial cells and bone marrow-derived macrophages via immunoblotting. Quantify serum levels of IL-1β and IL-18 by ELISA [56].
- Therapeutic Testing: Evaluate interventions like IL-18 blockade, TNF inhibition, or metabolic support (e.g., glucose supplementation) [56].
The diagram below illustrates the canonical inflammasome activation pathway triggered by various sensors.
Diagram Title: Canonical Inflammasome Activation Pathway
Modeling Localized Inflammation
Localized inflammatory diseases, such as inflammatory bowel disease (IBD), involve specific tissues and require specialized models to accurately replicate the pathophysiology.
Inflammatory Bowel Disease (IBD) Models
Experimental Protocol for Chemical-Induced Colitis:
- Induction Agent: Dextran Sodium Sulfate (DSS) is commonly added to drinking water (e.g., 2-5% w/v) for 5-7 days. Alternatively, 2,4,6-Trinitrobenzenesulfonic acid (TNBS) can be administered intrarectally via enema [55].
- Animal Monitoring: Monitor daily for weight loss, diarrhea, and rectal bleeding. Calculate a Disease Activity Index (DAI) that scores these parameters [55].
- Endpoint Analysis:
- Macroscopic: Measure colon length (shortening indicates severity) and score mucosal damage.
- Histopathological: Assess epithelial damage, crypt loss, goblet cell depletion, and immune cell infiltration.
- Molecular: Analyze inflammatory markers (MPO, TNF-α, IL-1β, IL-6) in colon tissue and evaluate intestinal barrier integrity (mucin secretion, tight junction proteins) [55].
Mechanistic Insights: These chemicals disrupt the colonic epithelial barrier, allowing commensal bacteria (a source of PAMPs) to penetrate the lamina propria. This triggers an innate immune response via PRRs (e.g., TLRs) on macrophages and dendritic cells, leading to the production of pro-inflammatory cytokines and recruitment of neutrophils and T cells, perpetuating chronic inflammation [55].
Table 2: Key Experimental Parameters for Assessing Localized Inflammation in IBD Models
| Category | Specific Evaluation Index | Measurement Technique |
|---|---|---|
| Clinical Observation | Weight loss, diarrhea, bloody stool, posture, fur quality | Daily clinical scoring, DAI calculation [55]. |
| Pathological Observation | Colon length, spleen weight, mucosal damage, crypt architecture | Macroscopic examination, histopathology (H&E staining) [55]. |
| Intestinal Epithelial Barrier & Fibrosis | Mucin secretion, intestinal permeability, tight junction proteins (e.g., occludin), collagen deposition | Immunofluorescence, ELISA for serum D-lactate/diamine oxidase, Masson's trichrome staining [55]. |
| Inflammatory Markers | Myeloperoxidase (MPO) activity, pro-inflammatory cytokines (TNF-α, IL-1β, IL-6, IL-17A) | ELISA, multiplex immunoassays, RT-qPCR [55]. |
| Intestinal Microbiome | Microbial diversity, abundance of beneficial bacteria (e.g., Lactobacillus), short-chain fatty acids | 16S rRNA sequencing, metabolomics [55]. |
The Scientist's Toolkit: Essential Research Reagents
Successful execution of inflammation studies relies on a suite of well-characterized reagents and tools. The following table details key solutions used in the field.
Table 3: Key Research Reagent Solutions for Inflammation Models
| Research Reagent | Function and Application | Example Use in Protocols |
|---|---|---|
| Lipopolysaccharide (LPS) | A prototypical PAMP from Gram-negative bacteria; induces systemic inflammation via TLR4 activation [58] [54]. | Administered via IP or IV injection (1-20 mg/kg) to model endotoxemia and sepsis [58]. |
| Dextran Sulfate Sodium (DSS) | A chemical that disrupts the colonic epithelium, inducing innate immune activation and colitis [55]. | Added to drinking water (2-5% w/v) for 5-7 days to model ulcerative colitis in mice [55]. |
| Recombinant Cytokines (e.g., IL-2) | Used to modulate immune cell functions in vivo. Low-dose IL-2 expands regulatory T cells (Tregs) to suppress inflammation [59]. | Subcutaneous administration in therapeutic models, such as combination therapy for neuroinflammation [59]. |
| TNF-α & IL-1β/IL-18 Blockers | Neutralizing antibodies or receptor antagonists that inhibit specific pro-inflammatory cytokine pathways [56]. | Used to validate the role of specific cytokines or as a therapeutic intervention in autoinflammatory models [56]. |
| Mesenchymal Stem Cells (MSCs) | Cellular therapeutics with immunomodulatory, anti-inflammatory, and tissue-repair properties [58]. | Administered intravenously after LPS challenge or in colitis models to study mitigation of inflammation and organ damage [58]. |
Advanced Concepts and Future Directions
Trained Immunity in Chronic Inflammation
Emerging research highlights the role of "trained immunity"—a long-term functional reprogramming of innate immune cells—in chronic inflammatory diseases. This phenomenon can be induced not only by PAMPs but also by DAMPs and lifestyle-associated molecular patterns (LAMPs), leading to enhanced responses to subsequent challenges through epigenetic and metabolic changes [26]. This maladaptive trained immunity may contribute to the persistence and exacerbation of conditions like atherosclerosis, CKD, and autoimmune disorders, offering novel therapeutic targets for immunomodulation [26].
Integration of Imaging and Longitudinal Monitoring
Advanced in vivo imaging techniques are crucial for non-invasively monitoring the spatiotemporal dynamics of inflammation in animal models. These modalities allow for longitudinal tracking of immune cell recruitment, vascular permeability, and tissue damage in the same animal over time, reducing inter-subject variability and providing a more comprehensive understanding of disease progression and treatment efficacy, particularly in complex conditions like PASC (Post-Acute Sequelae of COVID-19) [57].
Animal challenge models remain a cornerstone of immunological research, providing unparalleled insights into the mechanisms of systemic and localized inflammation initiated by PAMPs and DAMPs. From the well-established LPS and DSS models to sophisticated genetic models of inflammasomopathies, these systems enable the dissection of complex signaling pathways and the evaluation of novel therapeutic strategies. As the field advances, the integration of concepts like trained immunity, along with cutting-edge imaging and omics technologies, will further refine these models and deepen our understanding of inflammatory diseases, accelerating the translation of basic research findings into clinical applications.
The initiation of an immune response is fundamentally regulated by the recognition of specific molecular patterns. Pathogen-associated molecular patterns (PAMPs) are conserved molecules from microbes, while damage-associated molecular patterns (DAMPs) are endogenous molecules released by damaged, stressed, or dead cells [60] [39]. Both PAMPs and DAMPs are recognized by pattern recognition receptors (PRRs) found on immune cells and various non-immune cell types, including fibroblasts and epithelial cells [60] [61]. This recognition triggers intracellular signaling cascades—most notably the NF-κB and MAPK pathways—that drive the expression of pro-inflammatory cytokines and chemokines, initiating and amplifying the immune response [60] [39] [48].
Table 1: Common PAMPs, DAMPs, and Their Recognized Receptors
| Category | Examples | Recognizing PRRs |
|---|---|---|
| PAMPs | Lipopolysaccharide (LPS), Microbial nucleic acids, Peptidoglycan | Toll-like receptors (TLRs), NOD-like receptors (NLRs) [60] |
| DAMPs | HMGB1, Heat shock proteins, Extracellular ATP, Mitochondrial DNA, Uric acid | TLRs, NLRs, RAGE, CLEC [60] [39] |
Understanding this initial molecular dialogue is crucial for deconstructing the immune response. Contemporary research employs a multi-faceted analytical approach, integrating technologies that profile cytokine secretion, transcriptomic changes, and proteomic landscapes to build a comprehensive picture of immune activation. This guide details these core methodologies and their application in PAMP/DAMP research.
Core Analytical Technologies
Multiplex Cytokine Profiling
Moving beyond single-analyte assays, multiplex cytokine profiling allows for the simultaneous measurement of dozens of cytokines, chemokines, and growth factors from a single small-volume sample, providing a powerful snapshot of the immune state.
2.1.1 Flow Cytometry-Based Multiplex Bead Array (FCMBA) This technology uses multiple sets of microscopic beads, each with a unique spectral signature and coated with a capture antibody for a specific cytokine. When incubated with a sample, cytokines bind to their respective beads, and a PE-conjugated detection antibody completes the "sandwich" assay, allowing quantification via flow cytometry [62] [63]. The FCMBA platform demonstrates advantages over conventional ELISA, including higher throughput, reduced sample volume requirements, and broader dynamic range [62].
Table 2: Key Characteristics of Cytokine Detection Platforms
| Platform | Multiplexing Capacity | Sample Volume | Assay Time | Key Features |
|---|---|---|---|---|
| Conventional FCMBA | High (up to 65-plex) [60] | 50 μL [63] | ~3 hours [63] | High-throughput, requires cold chain for reagents |
| One-Step FCMBA | High (e.g., 12-plex) [63] | 100 μL [63] | ~1.5 hours [63] | Simplified protocol, lyophilized reagents for stability |
| AI-Enhanced POC Biosensors | Moderate | 1-50 μL [64] | 5-30 minutes [64] | Extreme sensitivity (LOD: 0.01-100 pg/mL), portability |
2.1.2 Advanced Protocols and Applications A simplified "one-step" FCMBA protocol has been developed, where all reagents are pre-mixed and lyophilized. This innovation reduces the total assay time to approximately 90 minutes, eliminates cold storage requirements, and minimizes operator-induced variability [63]. This method has been successfully applied to profile immune responses in clinical settings, such as stratifying COVID-19 and HBV patients based on disease severity by analyzing a 12-plex cytokine panel (e.g., IL-6, IL-8, IL-10, TNF-α) [63]. Furthermore, the integration of machine learning models (e.g., Random Forest, Support Vector Machine) with multiplex cytokine data has enhanced the ability to predict clinical outcomes like HBV viral load and disease severity [63].
Transcriptomic and Proteomic Analysis
Omics technologies provide a systems-level view of the genetic and protein-level changes underlying the immune response.
2.2.1 Transcriptomic Workflow (RNA-seq) Transcriptome sequencing (RNA-seq) is a powerful tool for identifying differentially expressed genes (DEGs) in response to immune challenges like PAMPs. A standard workflow involves:
- Sample Preparation & RNA Extraction: Tissues or cells of interest (e.g., cephalopod white body, tick immune tissues) are collected post-stimulation (e.g., with LPS). Total RNA is extracted using methods like the Trizol protocol, and its quality is assessed [65] [48].
- Library Construction & Sequencing: mRNA is purified, fragmented, and reverse-transcribed into a cDNA library. The library is sequenced on platforms like Illumina NovaSeq 6000 to generate raw reads [65].
- Data Analysis: Quality-controlled clean reads are assembled, and DEGs are identified using software like DESeq2. Subsequent bioinformatic analyses, such as Gene Ontology (GO) and Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway enrichment, reveal biological processes and signaling pathways (e.g., Toll, IMD, NF-κB, MAPK) activated by the immune challenge [65] [48].
2.2.2 Integrated Multi-Omics and Protein-Protein Interaction (PPI) Networks To gain deeper mechanistic insights, transcriptomic data can be integrated with proteomics. In a study on Amphioctopus fangsiao challenged with LPS, researchers combined RNA-seq with bioinformatics to construct a PPI network from the DEGs. This analysis identified 20 hub genes (e.g., AKT3, MAPK14, PIK3CA) central to the immune response, which were validated using qRT-PCR [65]. This integrated approach moves beyond single-gene studies to elucidate the complex regulatory networks that govern immunity.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful execution of these assays relies on a suite of specialized reagents and tools.
Table 3: Key Research Reagent Solutions for Immune Response Assays
| Reagent / Material | Function / Application | Example Use Case |
|---|---|---|
| LPS (Lipopolysaccharide) | A potent PAMP from Gram-negative bacteria used to model immune activation and inflammatory pathways in vitro and in vivo [60]. | Inducing cytokine production in PBMCs; creating challenge models in animals [60]. |
| ProCartaPlex Multiplex Assay Kits | Ready-to-use panels for multiplex cytokine detection via bead-based immunoassays. | Simultaneous quantification of 65+ human cytokines from cell culture supernatant [60]. |
| TRIzol Reagent | A monophasic solution of phenol and guanidine isothiocyanate for the effective isolation of high-quality total RNA. | RNA extraction for subsequent transcriptome sequencing (RNA-seq) [65] [48]. |
| NEBNext Ultra II RNA Library Prep Kit | A complete kit for preparing high-quality cDNA libraries for next-generation sequencing. | Construction of sequencing-ready libraries from purified mRNA for transcriptomic studies [65]. |
| Fluorophore-Conjugated Antibodies | Antibodies tagged with fluorescent dyes for detection in flow cytometry. | Detection and quantification of captured cytokines in FCMBA or specific cell surface markers [63]. |
| Lyophilization Buffers | Stabilizing formulations (e.g., with trehalose) for preserving reagent activity without cold storage. | Enabling the production of stable, one-step FCMBA reagent beads [63]. |
Integrated Workflow and Signaling Pathways
A typical integrated study of the immune response involves a coordinated series of experimental and analytical steps, as outlined below. This workflow begins with immune stimulation and proceeds through sample processing, multi-modal data collection, and integrative bioinformatic analysis to yield a systems-level understanding.
The core of the immune response to PAMPs and DAMPs is mediated by specific intracellular signaling pathways. The following diagram illustrates the key pathway activations, from receptor-ligand binding to final immunological outputs, integrating concepts from multiple research studies [60] [39] [48].
The modern assay of the immune response requires a synergistic application of technologies. Multiplex cytokine profiling delivers a high-resolution, kinetic view of secreted immune mediators; transcriptomics uncovers the comprehensive genetic blueprint of the response; and integrated proteomics validates functional protein expression and interactions. When these datasets are combined through sophisticated bioinformatic analysis, they empower researchers to move from observing phenomena to understanding the complex, interconnected networks that define the immune response to PAMPs, DAMPs, and disease. This integrated approach is pivotal for advancing both basic immunology research and the development of novel immunotherapies.
High-Throughput Screening for PRR Agonists and Antagonists in Drug Discovery
Pattern Recognition Receptors (PRRs) constitute the foundational element of the innate immune system, providing the first line of defense against pathogenic invasion. These receptors, expressed on and in innate immune cells, are tasked with recognizing conserved molecular signatures known as Pathogen-Associated Molecular Patterns (PAMPs) derived from microbes, and Damage-Associated Molecular Patterns (DAMPs) released from host cells during stress, damage, or death [3]. The activation of PRR signaling pathways initiates inflammatory responses crucial for pathogen clearance and tissue repair. However, dysregulated PRR activation is a hallmark of numerous diseases, including autoimmune disorders, chronic inflammation, and cancer [40] [3]. Consequently, the discovery of pharmacological agents that can precisely modulate PRR activity—either stimulating (agonists) or inhibiting (antagonists) their function—has emerged as a pivotal frontier in immunology and drug discovery. This whitepaper details the application of high-throughput screening (HTS) methodologies to identify and characterize novel PRR agonists and antagonists, framing this pursuit within the critical context of PAMP-driven inflammation initiation research.
PRR Families, Their Ligands, and Inflammatory Roles
A comprehensive understanding of PRR biology is a prerequisite for rational drug screening. PRRs are categorized into several families based on protein domain homology and subcellular location [3].
- Toll-like Receptors (TLRs): Membrane-bound receptors (cell surface or endosomal) that recognize a diverse array of PAMPs and DAMPs. For instance, TLR4 recognizes bacterial lipopolysaccharide (LPS), while intracellular TLRs like TLR9 recognize microbial DNA [3].
- NOD-like Receptors (NLRs): Cytosolic receptors that often form large complexes called inflammasomes in response to danger signals, leading to the maturation of potent pro-inflammatory cytokines like IL-1β [40].
- RIG-I-like Receptors (RLRs): Cytosolic sensors that detect viral RNA and initiate anti-viral interferon responses [3].
- C-type Lectin Receptors (CLRs): Primarily recognize carbohydrate structures on fungi and other pathogens [3].
The interplay between PAMPs and DAMPs is particularly relevant in chronic inflammatory diseases. PAMPs initiate inflammation, while subsequently released DAMPs can perpetuate and amplify the inflammatory response, even in the absence of the original pathogen [25] [7]. For example, in autoimmune diseases like rheumatoid arthritis, PAMPs from microbial infections can trigger initial NETosis (a form of neutrophil cell death that releases neutrophil extracellular traps), leading to tissue damage and DAMP release (e.g., HMGB1, histones), which further exacerbates NETosis and chronic inflammation in a vicious cycle [7]. This synergistic interplay underscores the therapeutic potential of targeting the PRRs that sense these molecules.
Table 1: Major PRR Families and Their Characteristics
| PRR Family | Key Members | Example Ligands (PAMPs/DAMPs) | Localization | Primary Signaling Adapters |
|---|---|---|---|---|
| Toll-like Receptors (TLRs) | TLR4, TLR9, TLR7/8 | LPS (PAMP), HMGB1 (DAMP), DNA (PAMP) | Plasma Membrane, Endosomes | MyD88, TRIF |
| NOD-like Receptors (NLRs) | NOD2, NLRP3 | Muramyl dipeptide (PAMP), ATP (DAMP), Uric Acid (DAMP) | Cytosol | RIP2, ASC (for inflammasomes) |
| RIG-I-like Receptors (RLRs) | RIG-I, MDA5 | Viral dsRNA (PAMP) | Cytosol | MAVS/IPS-1 |
| C-type Lectin Receptors (CLRs) | Dectin-1, Mincle | β-glucans (PAMP), SAP130 (DAMP) | Plasma Membrane | SYK |
Signaling Pathways in PAMP-Driven Inflammation
The following diagram outlines the core signaling pathways triggered when PRRs recognize PAMPs, leading to the activation of key transcription factors and the initiation of a pro-inflammatory gene program.
Figure 1: Core PRR Signaling Pathway upon PAMP Recognition
High-Throughput Screening Platforms for PRR Modulators
High-Throughput Screening (HTS) leverages automation, miniaturization, and parallel processing to rapidly test thousands to millions of compounds for a desired biological activity [66]. In the context of PRR drug discovery, the primary aim is to identify compounds that either activate (agonists) or suppress (antagonists) PRR signaling in a specific and potent manner.
Cell-Based Reporter Gene Assays
This is one of the most established and widely used HTS platforms for PRR modulator discovery. The core technology involves engineering a cell line that stably expresses the PRR of interest and a reporter gene (e.g., Secreted Alkaline Phosphatase (SEAP), luciferase) under the control of a PRR-responsive promoter, such as one containing NF-κB or IRF binding sites [67].
Detailed Experimental Protocol:
- Cell Line Engineering: A suitable cell line (e.g., HEK-293, NIH/3T3) with low endogenous PRR expression is selected. The gene for the target human PRR is stably transfected into the cells. Subsequently, a reporter construct (e.g., a plasmid with an NF-κB promoter driving SEAP expression) is stably integrated [67].
- Assay Miniaturization: The engineered cells are seeded into 384- or 1536-well microtiter plates using automated liquid handlers.
- Compound Library Addition: Libraries of small molecules, natural product extracts, or other chemical entities are transferred to the assay plates, each well containing a unique compound.
- Stimulation (for Antagonist Mode): For antagonist screening, a known, potent agonist (e.g., LPS for TLR4, CpG-ODN for TLR9) is added to all wells to stimulate the PRR pathway. An agonist that inhibits the pathway is identified by a reduction in reporter signal compared to agonist-only controls [67].
- Incubation: Plates are incubated for a predetermined period (e.g., 6-24 hours) to allow for signal transduction and reporter gene expression/production.
- Signal Detection: The activity of the secreted or intracellular reporter is quantified. For SEAP, this involves adding a chemiluminescent substrate and measuring light emission with a plate reader.
- Data Analysis: Raw luminescence data is normalized to positive (agonist control) and negative (vehicle control) controls. IC₅₀ (half-maximal inhibitory concentration) values are calculated for antagonists, and EC₅₀ (half-maximal effective concentration) values for agonists [67].
Pharmacotranscriptomics-Based Screening (PTDS)
This is an emerging, powerful HTS paradigm that moves beyond single-reporter readouts. PTDS involves treating cells with a compound and using high-throughput transcriptomic technologies (e.g., RNA-seq) to profile the global changes in gene expression [68] [69]. The resulting "gene signature" can be compared to databases of known drug signatures or analyzed to see if it mimics (for agonists) or suppresses (for antagonists) the transcriptional response induced by a known PAMP.
Detailed Experimental Protocol:
- Cell Treatment: Wild-type or engineered immune cells (e.g., primary monocytes, macrophage cell lines) are treated with compounds from a library in a multi-well plate format.
- RNA Extraction: After incubation, total RNA is isolated from all wells in a highly parallel, automated manner.
- Library Preparation and Sequencing: RNA-seq libraries are prepared and sequenced. Recent advancements allow for this process to be miniaturized and cost-effective for HTS.
- Bioinformatic Analysis: Supervised and unsupervised machine learning algorithms are applied to the transcriptomic data [69]. The effect of a compound is analyzed by examining its impact on gene sets, signaling pathways, and complex disease signatures perturbed by PAMPs. A pathway-based drug screening strategy can then be employed to identify compounds that reverse a PAMP-induced inflammatory signature [68].
Table 2: Comparison of Primary HTS Platforms for PRR Modulator Discovery
| Platform | Key Readout | Throughput | Key Advantages | Key Limitations |
|---|---|---|---|---|
| Reporter Gene Assay | Activity of a single PRR-responsive reporter (e.g., SEAP) | Very High | Simple, quantitative, low cost per well, easily automated. | Limited to a single, predefined pathway; risk of false positives/negatives. |
| Pharmacotranscriptomics (PTDS) | Genome-wide gene expression changes | High (increasing with tech.) | Provides rich, mechanistic data; can detect polypharmacology; suitable for complex systems like Traditional Chinese Medicine [68]. | Higher cost and computational burden; complex data analysis. |
| Cytokine Profiling | Secretion of multiple inflammatory cytokines (e.g., IL-6, TNF-α) | Medium to High | Measures a direct, functional downstream output; physiologically relevant. | Can be more variable and expensive than reporter assays. |
The Scientist's Toolkit: Essential Research Reagents and Solutions
Successful HTS for PRR modulators relies on a suite of specialized reagents and tools.
Table 3: Key Research Reagent Solutions for PRR HTS
| Research Tool | Function in HTS | Specific Examples |
|---|---|---|
| Engineered Reporter Cell Lines | Provides the biological sensor for PRR activation; the core of the assay. | NIH/3T3 cells stably expressing human TLR4 and an NF-κB-SEAP reporter [67]. |
| Defined PAMP Agonists | Used as positive controls and for stimulating pathways in antagonist screens. | Ultrapure LPS (TLR4 agonist), CpG ODN (TLR9 agonist), Pam3CSK4 (TLR2/1 agonist). |
| Validated PRR Antagonists | Used as positive controls in antagonist screening campaigns. | TAK-242 (TLR4 antagonist), ODN TTAGGG (TLR9 antagonist). |
| High-Throughput Transcriptomic Kits | Enable miniaturized, parallel RNA extraction and library prep for PTDS. | Plate-based RNA extraction kits, low-input RNA-seq library prep kits. |
Computational and Technological Advancements
The scale and complexity of HTS demand robust computational and technological infrastructure.
- AI and Machine Learning: AI algorithms are used to analyze massive HTS datasets, detect patterns, and predict the activity of untested compounds, thereby prioritizing the most promising hits [66]. In PTDS, supervised learning algorithms are crucial for classifying drug mechanisms based on transcriptomic profiles [69].
- Molecular Simulations for Virtual Screening: In silico methods can vastly reduce the time and cost of initial screening. Using 3D binding models of PRRs, software can screen virtual compound libraries for molecules that are predicted to bind to the agonist or antagonist site, creating a focused, high-probability library for empirical testing [67].
- GPU-Accelerated Computing: The molecular simulations and AI-driven data analysis involved in modern HTS are computationally intensive. Graphics Processing Units (GPUs) dramatically accelerate these processes through parallel processing, reducing analysis times from days to minutes [66].
- Automation and Robotics: Automated robotic systems handle physical tasks like sample preparation, liquid handling, and plate management, enabling thousands of daily experiments with minimal human intervention and ensuring consistency and reproducibility [66].
Integrated HTS and Hit Validation Workflow
The journey from a compound library to a validated hit involves a multi-stage process, integrating both computational and empirical biological steps, as illustrated below.
Figure 2: Integrated Workflow for PRR Modulator Discovery
High-throughput screening represents a powerful and evolving engine for discovering novel pharmacological modulators of Pattern Recognition Receptors. By leveraging sophisticated cell-based assays, expansive pharmacotranscriptomic approaches, and cutting-edge computational and AI tools, researchers can efficiently sift through vast chemical spaces to identify promising drug candidates. Framing this search within the intricate biology of PAMP-driven inflammation and its crosstalk with DAMP pathways ensures that discovered agents are not only potent but also biologically relevant. As these technologies continue to mature, they hold the promise of delivering a new generation of immunomodulatory therapeutics to better manage a wide spectrum of inflammatory diseases.
Pattern recognition receptors (PRRs) are cornerstone components of the innate immune system, responsible for detecting pathogen-associated molecular patterns (PAMPs) from invading microbes and damage-associated molecular patterns (DAMPs) released during cellular stress. The strategic targeting of PAMP-PRR pathways represents a transformative approach in modern immunology, enabling the development of novel anti-inflammatory therapeutics and advanced vaccine adjuvants. This whitepaper provides a comprehensive technical analysis of PRR signaling mechanisms, current therapeutic development strategies, and detailed experimental methodologies for researchers and drug development professionals. By elucidating the complex interplay between PRR activation, immune modulation, and inflammatory pathogenesis, this guide establishes a foundational framework for advancing therapeutic innovation in infectious, inflammatory, and autoimmune diseases, with significant implications for precision medicine and vaccine development.
Pattern recognition receptors (PRRs) are germline-encoded host sensors that serve as essential sentinels of the innate immune system, providing the first line of defense against pathogenic invasion [33] [54]. These receptors detect conserved molecular structures known as pathogen-associated molecular patterns (PAMPs) derived from microorganisms, as well as damage-associated molecular patterns (DAMPs) released during cellular stress or tissue injury [33] [70]. The strategic positioning of PRRs at the interface of innate and adaptive immunity enables them to initiate immediate protective responses while simultaneously shaping antigen-specific immunity, making them prime targets for therapeutic intervention [33] [16].
The conceptual foundation of pattern recognition emerged from Charles Janeway's seminal hypothesis proposing that the innate immune system detects microbial infections through specific receptors recognizing molecular patterns absent in the host [33]. This was subsequently expanded by Polly Matzinger's "danger model," which introduced the concept that immune responses are triggered not only by foreign pathogens but also by endogenous danger signals indicating tissue damage [33] [25]. Over the past three decades, these theoretical frameworks have catalyzed the identification and characterization of numerous PRR families, their ligands, and downstream signaling pathways, revolutionizing our understanding of immune activation and homeostasis [33].
PRRs are broadly categorized by their structural characteristics, ligand specificity, and subcellular localization. The major PRR families include Toll-like receptors (TLRs), C-type lectin receptors (CLRs), nucleotide-binding oligomerization domain (NOD)-like receptors (NLRs), retinoic acid-inducible gene I (RIG-I)-like receptors (RLRs), absent in melanoma 2 (AIM2)-like receptors (ALRs), and cytosolic DNA sensors such as cyclic GMP-AMP synthase (cGAS) [33] [54] [71]. These receptors are expressed on various immune cells, including dendritic cells, macrophages, and neutrophils, as well as non-immune cells such as epithelial and endothelial cells, enabling comprehensive surveillance throughout the body [16] [70].
Table 1: Major PRR Families and Their Characteristics
| PRR Family | Subcellular Localization | Representative Members | Primary Ligands (PAMPs/DAMPs) |
|---|---|---|---|
| Toll-like Receptors (TLRs) | Plasma membrane, endosomal membranes | TLR1-TLR10 (human), TLR1-TLR9, TLR11-TLR13 (mouse) | LPS (TLR4), dsRNA (TLR3), ssRNA (TLR7/8), CpG DNA (TLR9) |
| RIG-I-like Receptors (RLRs) | Cytosol | RIG-I, MDA5, LGP2 | Viral dsRNA, short dsRNA fragments |
| NOD-like Receptors (NLRs) | Cytosol | NOD1, NOD2, NLRP3 | Bacterial peptidoglycan, viral RNA, crystals, ATP |
| C-type Lectin Receptors (CLRs) | Plasma membrane | Dectin-1, Dectin-2, MINCLE | Fungal β-glucans, mycobacterial glycolipids |
| AIM2-like Receptors (ALRs) | Cytosol | AIM2, IFI16 | Viral and bacterial dsDNA |
| DNA Sensors (cGAS) | Cytosol | cGAS | Cytosolic dsDNA, self-DNA |
Upon ligand engagement, PRRs initiate intracellular signaling cascades that culminate in the activation of transcription factors such as nuclear factor-κB (NF-κB), interferon regulatory factors (IRFs), and activator protein 1 (AP-1) [33] [54]. This leads to the production of proinflammatory cytokines, type I interferons, chemokines, and antimicrobial peptides, which collectively establish an anti-pathogen state and recruit additional immune cells to sites of infection or injury [71]. Additionally, PRR activation enhances antigen presentation and provides co-stimulatory signals that are essential for the activation and differentiation of T and B lymphocytes, thereby bridging innate and adaptive immunity [72] [16].
The critical role of PRRs in immune surveillance makes them attractive targets for therapeutic development. However, their activation must be precisely regulated, as excessive or prolonged PRR signaling can lead to chronic inflammation, autoimmunity, and tissue damage [33] [70]. Understanding the molecular mechanisms governing PRR activation, signal transduction, and resolution is therefore paramount for developing targeted therapies that modulate these pathways effectively while minimizing adverse effects.
PRR Signaling Pathways and Mechanisms
Toll-like Receptor Signaling Networks
Toll-like receptors (TLRs) represent the most extensively characterized PRR family, consisting of 10 functional members in humans and 12 in mice [33] [54]. These type I transmembrane proteins feature extracellular leucine-rich repeat (LRR) domains responsible for ligand recognition and intracellular Toll/IL-1 receptor (TIR) domains that mediate downstream signaling [33]. TLRs are strategically localized to either the plasma membrane (TLR1, TLR2, TLR4, TLR5, TLR6) or intracellular endosomal compartments (TLR3, TLR7, TLR8, TLR9), enabling detection of a diverse array of PAMPs and DAMPs [54] [71].
TLR signaling proceeds primarily through two adapter protein-dependent pathways: the myeloid differentiation primary response 88 (MyD88)-dependent pathway and the TIR-domain-containing adapter-inducing interferon-β (TRIF)-dependent pathway [54]. All TLRs except TLR3 signal via MyD88, which recruits interleukin-1 receptor-associated kinases (IRAKs) and tumor necrosis factor receptor-associated factor 6 (TRAF6), leading to activation of transforming growth factor-β-activated kinase 1 (TAK1) [54]. TAK1 subsequently activates both the NF-κB and mitogen-activated protein kinase (MAPK) pathways, driving the expression of proinflammatory cytokines such as TNF-α, IL-1β, and IL-6 [54]. The TRIF-dependent pathway, utilized by TLR3 and TLR4, activates TRAF3 and TRAF6, resulting in the phosphorylation of interferon regulatory factor 3 (IRF3) and production of type I interferons [54] [71].
Diagram 1: TLR Signaling Pathways - This diagram illustrates the major Toll-like receptor signaling pathways, showing the bifurcation into MyD88-dependent and TRIF-dependent cascades that ultimately lead to production of proinflammatory cytokines and type I interferons.
Cytosolic PRR Signaling Mechanisms
Cytosolic PRRs, including RLRs, NLRs, and DNA sensors, provide critical intracellular surveillance against invading pathogens that breach cell membranes or replicate within the cytoplasm [54] [71]. The RLR family, comprising RIG-I, MDA5, and LGP2, detects viral RNA in the cytosol and signals through the mitochondrial adapter protein MAVS (mitochondrial antiviral-signaling protein) [71]. MAVS activation leads to the recruitment of TRAF3 and TRAF6, ultimately activating TBK1 (TANK-binding kinase 1) and IKKε, which phosphorylate IRF3 and IRF7 to induce type I interferon production [71].
The cGAS-STING pathway represents a major cytosolic DNA sensing mechanism. Upon binding double-stranded DNA, cGAS synthesizes the second messenger 2'3'-cyclic GMP-AMP (cGAMP), which activates the endoplasmic reticulum-resident protein STING (stimulator of interferon genes) [71]. Activated STING then traffics to the Golgi apparatus, recruiting TBK1 and phosphorylating IRF3, leading to interferon production [71]. Recent studies have identified that STING activation is terminated through ESCRT-dependent lysosomal degradation, providing a crucial regulatory mechanism to prevent excessive inflammation [71].
NOD-like receptors (NLRs) represent a large family of cytosolic sensors that detect bacterial peptidoglycan fragments, viral RNA, and various DAMPs [54]. Some NLRs, including NOD1 and NOD2, activate NF-κB and MAPK signaling pathways through receptor-interacting serine/threonine-protein kinase 2 (RIPK2) [54]. Other NLRs, such as NLRP3, NLRC4, and AIM2, form multiprotein complexes called inflammasomes that activate caspase-1, leading to the proteolytic maturation and secretion of proinflammatory cytokines IL-1β and IL-18, and induction of pyroptotic cell death [54].
Table 2: Cytosolic PRR Signaling Pathways and Effector Functions
| PRR Family | Signaling Adaptors | Key Effector Pathways | Biological Outcomes |
|---|---|---|---|
| RLRs (RIG-I, MDA5) | MAVS, TRAF3, TRAF6 | TBK1/IKKε → IRF3/7 phosphorylation | Type I IFN production, antiviral state |
| cGAS-STING | cGAMP, STING, TBK1 | IRF3 phosphorylation, NF-κB activation | Type I IFN production, proinflammatory cytokines |
| NLRs (NOD1/2) | RIPK2, TRAF6 | TAK1 → NF-κB/MAPK activation | Proinflammatory cytokine production |
| Inflammasome-forming NLRs (NLRP3) | ASC, caspase-1 | IL-1β/IL-18 maturation, gasdermin D cleavage | Pyroptosis, inflammatory cytokine release |
Regulatory Mechanisms and Inhibitory PRRs
To prevent excessive immune activation and maintain homeostasis, PRR signaling is subject to multiple layers of regulation [33]. These include transcriptional and post-transcriptional regulation of PRR expression, protein degradation through ubiquitination, subcellular localization, and the action of inhibitory PRRs (iPRRs) [33]. iPRRs recognize both endogenous and microbial patterns associated with homeostasis, providing contextual information that helps establish appropriate activation thresholds and prevents immune overactivation [33]. Additionally, crosstalk between different PRR families enables the formation of supramolecular signaling complexes, such as PANoptosomes, which integrate signals from multiple PRRs to coordinate appropriate inflammatory responses and cell death pathways during infection [54].
The sophisticated regulation of PRR signaling reflects the evolutionary necessity to balance effective pathogen clearance with prevention of collateral tissue damage. Understanding these regulatory mechanisms provides critical insights for developing targeted therapeutic strategies that either enhance PRR-mediated immunity in the context of vaccines or suppress pathological PRR signaling in inflammatory diseases.
Therapeutic Targeting Strategies
PRR Agonists as Vaccine Adjuvants
The immunostimulatory properties of PRR agonists make them ideal candidates for vaccine adjuvants, as they can enhance antigen presentation, promote dendritic cell maturation, and shape adaptive immune responses [16]. Traditional vaccine formulations often suffer from reduced immunogenicity, particularly for subunit vaccines that contain purified antigens but lack the contextual signals of whole pathogens [16]. PRR agonists address this limitation by activating innate immune sensors that mimic natural infection, thereby enhancing the magnitude, quality, and durability of adaptive immunity [72] [16].
Multiple PRR agonists have been developed as commercial adjuvants or are in advanced clinical development. Monophosphoryl lipid A (MPLA), a TLR4 agonist derived from Salmonella Minnesota lipopolysaccharide, is utilized in the AS04 adjuvant system found in Cervarix (HPV vaccine) and Fendrix (hepatitis B vaccine) [16]. Similarly, CpG 1018, a synthetic oligodeoxynucleotide that activates TLR9, is employed in Heplisav-B, a hepatitis B vaccine that induces more rapid and robust antibody responses compared to conventional formulations [16]. The incorporation of PRR agonists into vaccine platforms is particularly valuable for populations with compromised immune function and for pathogens that have historically evaded effective vaccine development.
Table 3: PRR Agonists in Vaccine Adjuvants
| PRR Target | Agonist | Vaccine Application | Mechanism of Action |
|---|---|---|---|
| TLR4 | MPLA (AS04) | Cervarix (HPV), Fendrix (Hep B) | Enhances antibody titers and T cell responses via NF-κB activation |
| TLR9 | CpG 1018 | Heplisav-B (Hep B) | Promotes plasma cell differentiation and antibody production |
| TLR3 | poly(I:C) | Experimental vaccines | Induces type I interferons and cross-presentation for CD8+ T cells |
| TLR7/8 | Imidazoquinolines | Experimental vaccines | Enhances Th1 responses and cytotoxic T lymphocyte activation |
| STING | cGAMP derivatives | Cancer immunotherapy, experimental vaccines | Potent induction of type I interferons and CD8+ T cell responses |
The remarkable success of mRNA vaccines against COVID-19 exemplifies how PRR activation can be harnessed for protective immunity [72] [71]. The mRNA component of these vaccines is recognized by multiple endosomal and cytosolic PRRs, including TLR3, TLR7, TLR8, and RIG-I, triggering innate immune activation that enhances antigen presentation and T and B cell responses [72] [71]. Strategic nucleoside modifications, such as incorporation of N1-methylpseudouridine, have been employed to modulate PRR activation, balancing sufficient immunostimulation for adjuvant effects with excessive inflammation that could increase reactogenicity [72].
Anti-inflammatory Therapeutics Targeting PAMP-PRR Pathways
In contrast to the adjuvant approach that enhances PRR signaling, anti-inflammatory strategies aim to suppress pathological PRR activation in conditions characterized by excessive inflammation. Chronic inflammatory diseases, autoimmune disorders, and sepsis are associated with dysregulated PRR signaling that drives tissue damage and disease progression [33] [70]. Therapeutic approaches to mitigate harmful PRR activation include monoclonal antibodies that neutralize DAMPs, small molecule inhibitors that block PRR signaling, and decoy receptors that sequester inflammatory ligands [70].
DAMPs have emerged as particularly attractive targets for anti-inflammatory therapy, as they perpetuate inflammatory cascades in sterile inflammation and sepsis [70]. Major DAMPs of therapeutic interest include high mobility group box 1 (HMGB1), extracellular cold-inducible RNA-binding protein (eCIRP), histones, and extracellular ATP [70]. These molecules are released during cellular injury and activate PRRs such as TLR4, TLR9, and RAGE, creating feed-forward loops of inflammation that contribute to organ dysfunction in conditions like sepsis, trauma, and ischemia-reperfusion injury [70].
Several innovative therapeutic platforms are being developed to target DAMPs and their receptors. Monoclonal antibodies against eCIRP have shown efficacy in preclinical models of sepsis and acute lung injury by reducing inflammatory cytokine production and neutrophil extracellular trap formation [70]. Similarly, HMGB1-specific antibodies and antagonists have demonstrated protective effects in models of rheumatoid arthritis, sepsis, and myocardial infarction [70]. Scavenger receptors and decoy receptors represent an alternative approach; for example, the soluble form of RAGE (sRAGE) acts as a decoy receptor that neutralizes HMGB1 and other RAGE ligands, attenuating inflammation in diabetic complications and vascular diseases [70].
Small molecule inhibitors targeting intracellular signaling components of PRR pathways offer another strategic approach. Compounds that inhibit TBK1, IRAK4, and RIPK2 have shown promise in preclinical models of autoimmune and autoinflammatory diseases [33]. Additionally, the discovery of inhibitory PRRs (iPRRs) has revealed endogenous mechanisms that could be therapeutically enhanced to suppress excessive inflammation [33]. These regulatory receptors recognize homeostatic molecular patterns and establish activation thresholds that prevent inappropriate immune responses [33].
Experimental Methods and Research Applications
Methodologies for Studying PRR Activation and Signaling
The investigation of PAMP-PRR pathways requires a multifaceted experimental approach encompassing ligand-receptor interactions, intracellular signaling cascades, and functional immune responses. Surface plasmon resonance (SPR) and isothermal titration calorimetry (ITC) provide quantitative data on binding affinity and kinetics between PRRs and their ligands [33]. Crystallographic studies of PRR-ligand complexes, such as those conducted for TLRs and their agonists, have revealed the structural basis of pattern recognition and facilitated structure-based drug design [33].
For functional analysis of PRR signaling, reporter cell lines stably expressing PRRs of interest coupled with luciferase or GFP reporters under the control of NF-κB or interferon-sensitive response elements enable high-throughput screening of agonists and antagonists [16]. Primary immune cells, particularly dendritic cells and macrophages, serve as biologically relevant systems for evaluating PRR-mediated cytokine production, maturation markers, and antigen-presenting capacity using techniques such as ELISA, flow cytometry, and multiplex bead arrays [72] [16].
Genetic approaches, including RNA interference and CRISPR-Cas9-mediated gene knockout, allow for functional validation of specific PRRs and signaling components in cellular models [33]. For in vivo studies, genetically modified mice lacking specific PRRs or signaling adaptors have been instrumental in delineating the non-redundant functions of different recognition pathways in host defense and inflammation [33] [54].
Assessing Immunological Outcomes
The evaluation of PRR-targeted therapies requires comprehensive assessment of immunological outcomes at cellular and systemic levels. For vaccine adjuvants, key parameters include antigen-specific antibody titers, neutralizing capacity, avidity, and isotype distribution, which inform about the quality of humoral immunity [16]. T cell responses should be characterized through intracellular cytokine staining, proliferation assays, and tetramer staining to assess the generation of CD4+ T helper subsets (Th1, Th2, Th17) and CD8+ cytotoxic T lymphocytes [72] [16].
Antigen-presenting cell activation is a critical endpoint for PRR agonist activity, typically measured through surface expression of major histocompatibility complex (MHC) molecules, co-stimulatory markers (CD80, CD86, CD40), and cytokine secretion profiles [72]. Dendritic cell maturation is particularly important as it directly influences T cell priming and differentiation [72].
For anti-inflammatory therapeutics targeting PAMP-PRR pathways, assessment of inflammatory mediators in serum or tissue homogenates provides insight into pharmacodynamic effects [70]. Histopathological evaluation of target organs, along with analysis of immune cell infiltration using immunohistochemistry or flow cytometry, helps determine the impact on tissue inflammation and damage [70]. In models of sterile inflammation and sepsis, functional outcomes such as organ function (e.g., serum creatinine for kidney function, transaminases for liver damage) and survival serve as clinically relevant endpoints [70].
Diagram 2: PRR Research Methodologies - This diagram outlines the major experimental approaches for studying pattern recognition receptor function, spanning from molecular binding assays to in vivo disease models.
The Scientist's Toolkit: Key Research Reagents
Table 4: Essential Research Reagents for PAMP-PRR Pathway Investigation
| Reagent Category | Specific Examples | Research Applications | Technical Considerations |
|---|---|---|---|
| PRR Agonists | Pam3CSK4 (TLR1/2), poly(I:C) (TLR3), LPS (TLR4), Flagellin (TLR5), R848 (TLR7/8), CpG ODN (TLR9) | Immune cell stimulation, adjuvant development, signaling studies | Verify purity and absence of contaminants; use appropriate concentrations to avoid overstimulation |
| PRR Inhibitors | TAK-242 (TLR4), IRS954 (TLR7/9), BX795 (TBK1), wedelolactone (IKK) | Pathway validation, therapeutic screening | Assess specificity through counter-screens; monitor cell viability |
| Antibodies for Detection | Anti-phospho-IRF3, anti-phospho-NF-κB p65, anti-TLR4, anti-MyD88, anti-RIG-I | Western blot, immunofluorescence, flow cytometry | Validate antibodies in knockout cells; optimize fixation for phospho-epitopes |
| Reporter Systems | NF-κB-luciferase, ISRE-GFP, IFN-β-promoter constructs | High-throughput screening, signaling kinetics | Use minimal passage cells; include multiple controls for specificity |
| Genetically Modified Cells | THP-1-XBlue, HEK-Blue hTLR, PRR-knockout macrophages | Pathway-specific assays, receptor specificity studies | Maintain selection pressure; regularly verify genotype and phenotype |
Future Directions and Concluding Perspectives
The therapeutic targeting of PAMP-PRR pathways represents a rapidly advancing frontier in immunology and drug development. Several emerging areas hold particular promise for future research and clinical translation. The concept of "trained immunity," wherein innate immune cells develop memory-like characteristics through epigenetic and metabolic reprogramming, reveals novel aspects of PRR biology that could be harnessed for improved vaccines and immunotherapies [26]. Sterile inflammatory triggers, including DAMPs and lifestyle-associated molecular patterns (LAMPs), can induce trained immunity that contributes to chronic inflammatory diseases, suggesting new therapeutic targets for conditions like atherosclerosis, diabetes, and autoimmunity [26].
The development of synergistic PRR agonist combinations represents another promising direction. Evidence suggests that simultaneous activation of multiple PRR pathways can produce additive or synergistic effects that enhance immunogenicity while potentially allowing for dose reduction of individual components [16]. This approach may be particularly valuable for next-generation vaccines against challenging pathogens such as HIV, tuberculosis, and malaria, which have eluded conventional vaccine strategies.
Advancements in delivery systems, particularly lipid nanoparticles (LNPs), have created new opportunities for precision targeting of PRR agonists to specific tissues or cell types [72]. LNPs not only protect nucleic acid-based therapeutics but also serve as adjuvants through activation of innate immune sensors, as demonstrated by their role in mRNA COVID-19 vaccines [72]. Further engineering of delivery systems to target specific PRRs in particular cell populations could enhance vaccine efficacy while minimizing systemic inflammatory responses.
From a therapeutic perspective, the discovery of novel regulatory mechanisms controlling PRR signaling, including inhibitory PRRs (iPRRs), microRNA networks, and metabolic checkpoints, provides new targets for modulating pathological inflammation [33]. The development of small molecule inhibitors targeting key signaling nodes, such as TBK1, IRAK4, and STING, is progressing rapidly, with several candidates entering clinical trials for autoimmune and autoinflammatory conditions [33] [71].
In conclusion, the strategic targeting of PAMP-PRR pathways offers unprecedented opportunities for developing novel anti-inflammatory therapeutics and advanced vaccine platforms. The continued elucidation of PRR biology, coupled with innovative therapeutic approaches and delivery technologies, promises to transform the management of infectious diseases, inflammatory disorders, and cancer. As our understanding of the complex interplay between different PRR signaling networks deepens, so too will our ability to precisely modulate these pathways for therapeutic benefit, ushering in a new era of immunology-based medicine.
The liver faces a unique immunological challenge: it must continuously filter a massive load of commensal-derived microbial molecules from the gut portal blood while remaining vigilant against genuine pathogenic threats. This whitepaper explores the liver's sophisticated mechanisms for differentiating pathogenic from commensal pathogen-associated molecular patterns (PAMPs), a discrimination essential for maintaining hepatic homeostasis while mounting effective immune responses. We examine the anatomical, cellular, and molecular basis of liver immunity, highlighting how compartmentalized blood flow, specialized cell populations, and contextual signal integration enable this critical differentiation. The insights presented herein have significant implications for understanding liver pathophysiology and developing novel therapeutic interventions for infectious, inflammatory, and metabolic liver diseases.
The liver exists in a constant state of immunological tension. As the primary filter for blood draining the gastrointestinal tract, it receives a continuous influx of microbial products from the intestinal microbiota, including lipopolysaccharide (LPS), bacterial DNA, peptidoglycan, and other conserved molecular motifs classified as PAMPs [73]. Under normal conditions, these commensal-derived PAMPs are present in portal blood at substantial concentrations—LPS levels ranging from 0.01 to 0.5 EU/mL in healthy humans—yet they do not trigger destructive inflammatory responses [73]. This state of "physiological inflammation" requires the liver to maintain immunological tolerance to commensal products while retaining the capacity to mount robust immune responses against true pathogens [12] [73].
This discriminatory capacity represents a fundamental dilemma in innate immunity. The innate immune system traditionally relies on pattern recognition receptors (PRRs) that detect conserved microbial structures [12] [2]. However, since both pathogens and commensals express these conserved motifs, the mere presence of PAMPs provides insufficient information for threat assessment. The liver has therefore evolved sophisticated mechanisms to interpret the context of PAMP exposure rather than simply detecting their presence [74] [73]. This contextual interpretation occurs at multiple levels, including the anatomical organization of blood flow, cellular composition of hepatic tissues, integration of co-stimulatory signals, and temporal dynamics of PAMP presentation.
Table 1: Key PAMPs Relevant to Liver Immunology
| PAMP Class | Specific Examples | Source Microbes | PRR Recognized |
|---|---|---|---|
| Lipids/Lipoproteins | Lipopolysaccharide (LPS) | Gram-negative bacteria | TLR4/MD-2 |
| Lipoteichoic acid | Gram-positive bacteria | TLR2/TLR6 | |
| Bacterial lipoproteins | Various bacteria | TLR2/TLR1 | |
| Nucleic Acids | Unmethylated CpG DNA | Bacteria | TLR9 |
| Double-stranded RNA | Viruses | TLR3 | |
| Single-stranded RNA | Viruses | TLR7/8 | |
| Proteins | Flagellin | Flagellated bacteria | TLR5, Naip5/Ipaf |
| Glycans | Peptidoglycan | Bacteria | TLR2, NOD1/2 |
| Zymosan | Fungi | TLR2/TLR6 |
Anatomical and Cellular Basis of Hepatic PAMP Discrimination
Dual Blood Supply and Sinusoidal Compartmentalization
The liver's unique vascular architecture forms the foundation for its discriminatory capabilities. Unlike other organs, the liver receives blood from two sources: the hepatic portal vein (approximately 80% of inflow) and the hepatic artery (approximately 20%) [73]. This dual supply creates distinct microenvironments within the hepatic lobule:
- Portal Sinusoids: Continuously exposed to blood enriched with intestinal-derived PAMPs at variable concentrations. These sinuosoids are characterized by low oxygen tension and high PAMP load, creating an environment evolutionarily shaped for tolerance induction [73].
- Arterial Sinusoids: Primarily receive systemic blood with significantly lower concentrations of commensal PAMPs. These segments are hypothesized to serve as conventional immune surveillance sites capable of initiating robust inflammatory responses to true pathogens [73].
This anatomical segregation enables the liver to impose spatial regulation on immune responses, with arterial sinusoidal segments potentially serving as sites for initiating immune responses against non-intestinal pathogens (viruses, systemic bacteria) and tumors, while portal segments specialize in tolerance to commensal antigens [73].
Specialized Hepatic Cell Populations and Their Roles
The liver contains a diverse array of specialized cell types that collectively maintain immunological homeostasis:
Liver Sinusoidal Endothelial Cells (LSECs): These fenestrated endothelial cells form the structural lining of sinusoids and constitute approximately 20% of total liver cells [73]. LSECs constitutively express immunoregulatory molecules including PD-L1, Fas-L, IL-10, and TGF-β, creating a tolerogenic microenvironment [73]. Their strategic position enables direct contact with blood contents, allowing efficient PAMP clearance through scavenger receptors while simultaneously suppressing potentially harmful immune activation.
Kupffer Cells (KCs): As tissue-resident macrophages, KCs are critical for phagocytosing particulate matter and pathogens from the blood. Under steady-state conditions, KCs exposed to portal blood contribute to tolerance through production of anti-inflammatory mediators [73]. However, when appropriately activated, they can produce proinflammatory cytokines including TNF-α, IL-1β, and IL-6 [73].
Hepatocytes: Parenchymal cells that perform most of the liver's metabolic functions. Under steady-state conditions, hepatocytes express low levels of MHC molecules and may contribute to tolerance by interacting with regulatory immune cells [73].
Table 2: Hepatic Cell Types and Their Immunological Functions
| Cell Type | Key Immunological Features | Role in PAMP Response |
|---|---|---|
| LSECs | Fenestrated endothelium; Express PD-L1, IL-10, TGF-β; Scavenger receptor activity | PAMP clearance; Treg induction; Tolerance maintenance |
| Kupffer Cells | Tissue-resident macrophages; Phagocytic capability; TLR expression | Pathogen phagocytosis; Context-dependent cytokine production |
| Hepatocytes | Metabolic processing; Low MHC expression under homeostasis; Acute phase protein production | PAMP metabolism; Limited antigen presentation; Regulation of inflammation |
| Hepatic Stellate Cells | Pericytes in space of Disse; Vitamin A storage; Extracellular matrix production | Immunomodulation; Tissue repair responses |
Molecular Mechanisms of Differential PAMP Recognition
Pattern Recognition Receptor Signaling in Hepatic Cells
The liver employs the same classes of pattern recognition receptors (PRRs) as other tissues, but their expression and regulation are adapted to the liver's unique environment. Key PRR families include Toll-like receptors (TLRs), NOD-like receptors (NLRs), RIG-I-like receptors (RLRs), and cytosolic DNA sensors [75] [76].
Toll-like Receptors represent the best-characterized PRR family in liver immunity. Cell surface TLRs (TLR1, 2, 4, 5, 6) primarily recognize microbial membrane components, while intracellular TLRs (TLR3, 7, 8, 9) detect nucleic acids [75]. TLR4 recognizes bacterial LPS through a complex process requiring MD-2 and CD14 co-factors, leading to downstream signaling through either the MyD88-dependent or TRIF-dependent pathways [75]. The intracellular localization of nucleic acid-sensing TLRs prevents inappropriate activation by self-nucleic acids while enabling detection of viral and bacterial genomes within endosomal compartments [75].
Inflammasome Formation represents a critical mechanism for converting PAMP detection into inflammatory responses. Inflammasomes are cytoplasmic multiprotein complexes comprising a sensor protein (often an NLR or PYHIN family member), the adapter ASC, and the effector procaspase-1 [77] [76]. Activation leads to caspase-1-mediated cleavage of pro-IL-1β and pro-IL-18 into their active forms, plus induction of pyroptosis, an inflammatory cell death [77] [76].
Diagram 1: Differential Signaling Outcomes Based on PAMP Context
Contextual Signal Integration and Co-stimulatory Requirements
The liver's ability to discriminate between commensal and pathogenic PAMPs depends on integrating multiple simultaneous signals rather than relying on single PAMP-PRR interactions. This contextual interpretation occurs through several mechanisms:
PAMP Dose and Timing: Continuous low-level PAMP exposure, characteristic of commensal influx, promotes tolerance, while sudden high-concentration exposure may indicate breach of barrier integrity or pathogenic invasion [73].
Co-stimulatory Danger Signals: True pathogens typically trigger additional danger signals through their virulence activities, including membrane pore formation, toxin release, or cellular damage. These activities release damage-associated molecular patterns (DAMPs) such as ATP, uric acid, and HMGB1 that provide contextual co-stimulation [74] [76].
Cellular Location of PRR Engagement: The subcellular compartment where PAMP recognition occurs significantly influences the outcome. For example, flagellin detected at the cell surface by TLR5 may induce tolerance, while the same molecule detected in the cytosol by Naip5/Ipaf triggers inflammasome activation [74].
Cellular Metabolic State: The metabolic programming of hepatic immune cells influences their response to PAMPs. For example, LPS exposure under metabolically stressed conditions (as in NAFLD/NASH) promotes inflammation rather than tolerance [78].
Experimental Approaches for Studying Hepatic PAMP Discrimination
In Vitro and Ex Vivo Models
Research into hepatic PAMP discrimination employs multiple complementary experimental systems:
Primary Cell Isolation and Culture: Hepatic cell populations (hepatocytes, LSECs, KCs) can be isolated via collagenase perfusion and density gradient centrifugation. These primary cultures enable cell-type-specific response profiling to defined PAMP stimuli [73].
Precision-cut Liver Slices (PCLS): This ex vivo technique maintains tissue architecture and cellular interactions, allowing investigation of PAMP responses in a more physiological context than dissociated cell cultures.
Flow Cytometry and Cytometric Bead Arrays: Enable quantification of cell surface marker expression, intracellular signaling events, and cytokine production at single-cell resolution across mixed hepatic cell populations.
In Vivo Models
Animal models, particularly mice, remain essential for studying hepatic PAMP discrimination in physiological context:
Portal Vein Infusion Models: Direct cannulation and infusion of defined PAMP preparations into the portal vein allows controlled investigation of hepatic responses to blood-borne microbial products [73].
Genetic Manipulation Models: Cell-type-specific knockout mice (e.g., LysM-Cre for myeloid cells, Alb-Cre for hepatocytes) enable dissection of cell-specific contributions to PAMP discrimination.
Disease Context Models: Investigating PAMP responses in models of metabolic liver disease (e.g., methionine-choline deficient diet for NASH, high-fat diet for NAFLD) reveals how disease states alter hepatic discrimination capacity [78].
Table 3: Key Research Reagent Solutions for Hepatic PAMP Studies
| Reagent Category | Specific Examples | Research Application | Key Functions |
|---|---|---|---|
| PRR Agonists/Antagonists | Ultrapure LPS (TLR4 agonist); Pam3CSK4 (TLR2/1 agonist); ODN CpG (TLR9 agonist); Flagellin (TLR5 agonist) | Selective PRR activation; Pathway dissection | Define receptor-specific responses; Identify signaling requirements |
| Cytokine Detection | ELISA kits; Luminex multiplex arrays; ELISpot kits; Intracellular cytokine staining | Quantify inflammatory mediators; Profile immune responses | Measure outcome of PAMP recognition; Distinguish tolerance vs. activation |
| Cell Isolation Kits | Collagenase perfusion systems; Magnetic bead separation kits (e.g., for KCs, LSECs); Density gradient media | Isolation of specific hepatic cell populations | Enable cell-type-specific analysis; Study cellular crosstalk |
| Signaling Inhibitors | TAK-242 (TLR4 inhibitor); VX-765 (caspase-1 inhibitor); BAY 11-7082 (NF-κB inhibitor) | Pathway blockade; Mechanistic studies | Establish necessity of specific pathways; Therapeutic target validation |
| Gene Expression Analysis | RT-qPCR reagents; RNA-seq kits; CRISPR-Cas9 gene editing systems | Molecular mechanism elucidation; Functional genomics | Identify transcriptional responses; Validate gene function |
Diagram 2: Experimental Workflow for Hepatic PAMP Studies
Pathophysiological Implications and Therapeutic Opportunities
Disease Contexts of Dysregulated PAMP Discrimination
Failure of the liver's PAMP discrimination mechanisms contributes to numerous disease states:
Metabolic Liver Disease: In nonalcoholic fatty liver disease (NAFLD) and steatohepatitis (NASH), increased gut permeability and dysbiosis elevate portal PAMP levels while hepatosteatosis alters hepatic cell responses, creating a proinflammatory state [78]. TLR4 and TLR9 signaling activation by increased PAMP exposure contributes to inflammation, insulin resistance, and fibrogenesis [78].
Alcoholic Liver Disease: Alcohol-induced gut barrier dysfunction increases portal PAMP load while alcohol metabolism impairs hepatic PAMP clearance, creating a perfect storm of inflammation and hepatocyte damage.
Liver Fibrosis and Cirrhosis: Chronic PAMP exposure, particularly when combined with parenchymal injury, activates profibrogenic pathways in hepatic stellate cells, driving extracellular matrix deposition and architectural distortion [78].
Sepsis and Systemic Inflammation: When the liver's capacity for PAMP clearance is overwhelmed, either by excessive portal influx or via systemic circulation, it can contribute to the systemic inflammatory response syndrome characteristic of sepsis [73].
Emerging Therapeutic Strategies
Understanding the molecular basis of hepatic PAMP discrimination reveals multiple therapeutic opportunities:
Gut-Liver Axis Modulation: Prebiotics, probiotics, and gut barrier enhancers aim to reduce pathological PAMP influx while maintaining beneficial commensal signaling [78].
PRR-Targeted Therapeutics: Selective TLR antagonists, particularly for TLR4 and TLR9, show promise for reducing PAMP-driven inflammation while preserving beneficial signaling [78].
Inflammasome Regulation: Compounds that modulate inflammasome assembly or activity offer potential for controlling excessive inflammation in response to pathogenic PAMPs [76].
Metabolic Pathway Modulation: Since cellular metabolic state influences PAMP responses, metabolic interventions (e.g., AMPK activators, FXR agonists) may restore appropriate discrimination in disease states [78].
The liver's dilemma—discriminating pathogenic from commensal PAMPs in a sea of continuous microbial exposure—represents a paradigm of sophisticated immune contextual sensing. Through specialized anatomy, cellular composition, and molecular signaling networks, the liver maintains a delicate balance between tolerance and immunity. Understanding these mechanisms provides not only fundamental insights into liver physiology but also reveals novel therapeutic approaches for numerous inflammatory, metabolic, and infectious liver diseases. Future research should focus on elucidating the precise molecular switches that determine tolerance versus activation outcomes, with particular attention to how these switches are manipulated in disease states.
Navigating Experimental and Biological Complexity in PAMP-Mediated Inflammation
Pathogen-associated molecular patterns (PAMPs) are conserved molecular motifs from microbes that are recognized by the host innate immune system through pattern recognition receptors (PRRs) [2]. Among these, bacterial endotoxin—specifically lipopolysaccharide (LPS) from Gram-negative bacteria—serves as the prototypical PAMP for studying inflammatory pathways [2] [8]. Endotoxin contamination in experimental systems represents a significant confounding variable, while the specificity of models used to study endotoxin responses presents considerable methodological challenges. LPS is recognized primarily by Toll-like receptor 4 (TLR4), initiating signaling cascades that trigger NF-κB activation and pro-inflammatory cytokine production [2] [33]. This pathway represents a fundamental mechanism of innate immune activation, making endotoxin a critical focus for both basic research and drug development. Understanding and controlling for endotoxin contamination is thus essential for ensuring data integrity across immunology, neuroscience, and therapeutic development [79] [80].
Endotoxin as a PAMP: Recognition and Signaling Pathways
Molecular Recognition of Endotoxin
Endotoxin (LPS) consists of three structural domains: a conserved hydrophobic lipid A moiety responsible for toxicity, a core oligosaccharide, and a variable O-antigen polysaccharide [80]. As a PAMP, endotoxin is recognized by the innate immune system through specific PRRs. TLR4, in complex with accessory proteins MD-2 and CD14, serves as the primary receptor for LPS [2] [33]. The lipid A component is particularly crucial for recognition by the TLR4-MD-2 complex [2]. This recognition event initiates intracellular signaling cascades that lead to inflammatory gene expression.
Downstream Signaling and Inflammasome Activation
TLR4 engagement by endotoxin triggers two primary signaling pathways: the MyD88-dependent pathway, which leads to early-phase NF-κB activation and pro-inflammatory cytokine production, and the TRIF-dependent pathway, which results in IRF3 activation and type I interferon production [33]. Additionally, intracellular LPS can activate non-canonical inflammasomes through caspase-4, caspase-5 (in humans), and caspase-11 (in mice), leading to gasdermin D-mediated pyroptosis [81]. These signaling events culminate in the production of key inflammatory mediators including TNF-α, IL-1β, IL-6, and IL-18 [40] [81].
Figure 1: Endotoxin (LPS) activates inflammatory signaling through multiple pathways including TLR4 and inflammasomes.
Detection and Quantification of Endotoxin Contamination
Established Detection Methodologies
Multiple assay formats have been developed for endotoxin detection, each with distinct advantages and limitations. The Limulus Amebocyte Lysate (LAL) assay, derived from horseshoe crab blood, remains the gold standard for endotoxin detection [80]. The LAL assay exists in three primary formats, while recombinant alternatives are gaining traction:
Table 1: Endotoxin Detection Methods and Characteristics
| Method | Principle | Detection Limit | Throughput | Regulatory Status |
|---|---|---|---|---|
| Gel Clot LAL | Visual clot formation | ~0.03 EU/mL | Low | USP, EP, JP compendial |
| Chromogenic LAL | Colorimetric substrate cleavage | 0.01-0.05 EU/mL | Medium | USP, EP, JP compendial |
| Turbidimetric LAL | Turbidity measurement | 0.01-0.05 EU/mL | Medium | USP, EP, JP compendial |
| Recombinant Factor C (rFC) | Fluorescent enzyme activity | 0.01-0.05 EU/mL | High | Included in EP, draft USP |
| Cartridge-Based Systems | Automated rFC technology | 0.001-0.05 EU/mL | High | Increasing acceptance |
Emerging Technologies and Market Trends
The global bacterial endotoxin testing market is projected to grow from USD 1.26 billion in 2024 to approximately USD 3.02 billion by 2034, reflecting increasing regulatory stringency and technological advancement [82]. Recombinant Factor C (rFC) assays represent the fastest-growing segment due to their animal-free nature, superior specificity, and avoidance of horseshoe crab blood supply limitations [82]. Artificial intelligence is increasingly being integrated into testing platforms to enhance accuracy, speed, and data analysis capabilities while minimizing human error [82]. These technological advances are particularly relevant for cell and gene therapies, which require extremely sensitive detection limits due to their heightened sensitivity to endotoxin contamination [82].
Experimental Models for Endotoxin Research
Human Experimental Endotoxemia
Administration of purified endotoxin to human volunteers (experimental endotoxemia) serves as a highly standardized translational model for systemic inflammation [83] [79]. This approach provides a controlled system for investigating inflammatory mechanisms and testing novel therapeutics in humans. The model induces a well-characterized cascade of inflammatory changes, including increased blood concentrations of IL-6, TNF-α, and CRP, along with affective and behavioral symptoms that resemble core features of inflammation-associated depression [79]. These symptoms include increased sadness, anhedonia, anxiety, and social disconnection, typically emerging within 2 hours post-administration and lasting 4-5 hours [79]. Neuroimaging studies in endotoxin-challenged individuals have revealed increased neural responses in the amygdala, anterior cingulate cortex, and prefrontal regions during emotional processing, along with reduced ventral striatal activity to reward cues—neural signatures also observed in major depression [79].
Table 2: Human Experimental Endotoxemia Model Parameters
| Parameter | Low Dose | Medium Dose | High Dose | Key Measurements |
|---|---|---|---|---|
| LPS Dose Range | 0.1-0.5 ng/kg | 0.5-1.0 ng/kg | 1.0-2.0 ng/kg | Plasma cytokine levels |
| Cytokine Peak | 2-4 hours | 2-4 hours | 2-4 hours | TNF-α, IL-6, IL-1RA |
| Symptom Onset | 1-2 hours | 1-2 hours | 1-2 hours | Mood scales, sickness scores |
| Resolution | 4-6 hours | 6-8 hours | 8-24 hours | Vital signs, symptom monitoring |
| Safety Monitoring | Continuous vitals | Continuous vitals | Continuous vitals | ECG, temperature, BP |
In Vitro Models and Their Limitations
Cellular models for endotoxin research range from primary immune cells to immortalized cell lines and specialized co-culture systems. Macrophages and dendritic cells represent the most relevant cellular models as they express the complete TLR4 signaling machinery and respond robustly to LPS challenge [2]. However, significant inter-species differences in TLR4 signaling components and downstream responses necessitate careful model selection [33]. The use of primary human cells provides the most translational relevance but introduces donor variability, while immortalized cell lines offer reproducibility but may have altered signaling pathways. Endotoxin contamination in cell culture systems represents a particular concern, as even low-level contamination (0.01-0.1 EU/mL) can alter cellular responses and confound experimental outcomes [80].
Mitigation Strategies for Endotoxin Contamination
Prevention and Removal Techniques
Effective endotoxin control requires a multi-faceted approach spanning from reagent selection to experimental design. Key strategies include:
- Source Control: Selecting ultra-low endotoxin reagents (<0.01 EU/μg for sensitive applications) and verifying endotoxin levels upon receipt [80]
- Process Controls: Using endotoxin-free labware, maintaining separate work areas for "clean" and "dirty" procedures, and employing sterile technique
- Removal Methods: Applying specialized purification techniques including affinity chromatography (Polymyxin B resin), phase separation, and ultrafiltration
- Validation Testing: Implementing routine endotoxin screening of buffers, media, and critical reagents using appropriate detection methods
For recombinant proteins produced in bacterial systems, endotoxin removal represents a particular challenge due to the association of LPS with the protein product. Multiple purification strategies may be required, including detergent washes, ion-exchange chromatography, and endotoxin-specific affinity resins [80].
Experimental Design Considerations
Appropriate experimental controls are essential for distinguishing specific effects from endotoxin-mediated artifacts. Control conditions should include:
- Vehicle controls matching the buffer composition of test substances
- Endotoxin controls using purified LPS at levels matching potential contamination
- Inhibition controls using specific TLR4 antagonists (e.g., TAK-242, LPS-RS) to confirm pathway specificity
- Heat inactivation of test substances to denature proteins while preserving endotoxin activity
For highly sensitive applications such as animal immunization studies, T-cell assays, or preclinical testing of therapeutic candidates, endotoxin levels should be maintained below established thresholds (typically <0.01 EU/μg for proteins and <0.1 EU/mL for buffers) [80].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Endotoxin and PAMP Research
| Reagent Category | Specific Examples | Research Application | Considerations |
|---|---|---|---|
| TLR4 Agonists | Ultrapure LPS (E. coli, S. minnesota) | Positive control for TLR4 activation | Source, purity, and formulation affect activity |
| TLR4 Antagonists | TAK-242, LPS-RS, Polymyxin B | Confirming TLR4-specific effects | Specificity, potency, and cellular permeability |
| Detection Reagents | LAL reagents, rFC assay kits | Endotoxin quantification | Match method sensitivity to application needs |
| Cytokine Assays | ELISA, Luminex, ELISA kits | Measuring inflammatory responses | Dynamic range, multiplex capability |
| Signaling Inhibitors | BAY11-7082 (NF-κB), SB203580 (p38) | Pathway mechanism studies | Specificity and potential off-target effects |
| Ultra-Low Endotoxin Reagents | Certified proteins, antibodies | Sensitive cellular assays | Require validation for specific applications |
The study of endotoxin as a prototypical PAMP continues to provide fundamental insights into innate immunity and inflammatory processes. Addressing the dual challenges of inadvertent contamination and model specificity requires rigorous detection methodologies, appropriate model selection, and strategic experimental design. The growing adoption of human experimental endotoxemia models bridges mechanistic discoveries from in vitro studies to human physiology, while advances in detection technologies such as rFC assays offer more sustainable and specific alternatives to traditional methods. As research increasingly focuses on complex inflammatory conditions and novel biologic therapeutics, maintaining awareness of endotoxin-related artifacts and implementing robust control strategies remains essential for generating reproducible, physiologically relevant data.
The innate immune system faces the formidable challenge of rapidly identifying genuine microbial threats amidst a vast array of molecular patterns. This discriminative capacity is mediated by an elaborate system of pattern recognition receptors (PRRs) that detect conserved pathogen-associated molecular patterns (PAMPs) while maintaining tolerance to self-structures. Recent advances have illuminated the sophisticated strategies employed at the level of receptor localization, combinatorial signaling, and cellular context to achieve precise threat assessment. This whitepaper examines the molecular mechanisms governing immune signal specificity and their implications for therapeutic development in inflammatory and autoimmune diseases.
The traditional view of innate immunity as a nonspecific first-line defense has been fundamentally revised. The discovery that germline-encoded receptors recognize conserved microbial structures has established that innate immunity possesses remarkable specificity [4] [84]. Charles Janeway's pioneering concept of PAMPs as "Signal 0s" laid the foundation for understanding how the immune system distinguishes infectious nonself from noninfectious self [2] [42] [85].
PAMPs represent conserved molecular motifs essential for microbial survival, including bacterial lipopolysaccharide (LPS), flagellin, peptidoglycan, and microbial nucleic acids [2] [4]. These structures differ fundamentally from host molecules in their biochemical composition, subcellular localization, and abundance. The immune system leverages these differences through multiple families of PRRs that collectively generate a specific and appropriate inflammatory response [3].
Molecular Basis of Pattern Recognition
Structural Complementarity in PAMP-PRR Interactions
Specific immune recognition begins at the structural level, where PRRs exhibit precise complementarity for their cognate PAMPs. Toll-like receptors (TLRs) exemplify this principle through their leucine-rich repeat (LRR) domains, which form curved structures that directly bind specific microbial components [3]. The molecular basis for this specificity has been elucidated through X-ray crystallography studies of TLR-ligand complexes [3].
Table 1: Major PRR Families and Their Cognate PAMPs
| PRR Family | Prototype Members | Localization | Representative PAMPs | Pathogen Source |
|---|---|---|---|---|
| Toll-like Receptors (TLRs) | TLR4, TLR3, TLR9 | Plasma membrane, endosomes | LPS (TLR4), dsRNA (TLR3), CpG DNA (TLR9) | Gram-negative bacteria, viruses, bacteria/protozoa |
| RIG-I-like Receptors (RLRs) | RIG-I, MDA5 | Cytoplasm | Short dsRNA, 5'-triphosphate RNA (RIG-I); long dsRNA (MDA5) | RNA viruses |
| NOD-like Receptors (NLRs) | NOD1, NOD2 | Cytoplasm | Diaminopimelic acid (NOD1), MDP (NOD2) | Gram-negative bacteria, Gram-positive/negative bacteria |
| C-type Lectin Receptors (CLRs) | Dectin-1, MBL | Plasma membrane | β-glucans, mannose structures | Fungi, various pathogens |
| AIM2-like Receptors (ALRs) | AIM2 | Cytoplasm | Cytosolic DNA | DNA viruses, intracellular bacteria |
Compartmentalization as a Specificity Strategy
The strategic localization of PRRs constitutes a fundamental mechanism for achieving signal specificity. Membrane-bound TLRs (TLR1, 2, 4, 5, 6) primarily survey the extracellular environment for microbial surface components, while endosomal TLRs (TLR3, 7, 8, 9) detect microbial nucleic acids within intracellular compartments [3]. This compartmentalization prevents inappropriate activation by self-nucleic acids under normal conditions and ensures that nucleic acid sensing occurs primarily in the context of infectious agents that have invaded cellular compartments [4].
Cytosolic PRRs, including RIG-I-like receptors (RLRs) and AIM2-like receptors (ALRs), provide a complementary surveillance system for intracellular pathogens that have breached membrane barriers [4] [3]. This multi-compartment recognition strategy enables the immune system to attribute specific meaning to PAMP detection based on subcellular context.
Figure 1: Compartmentalization of PRR Surveillance Systems. Membrane-bound TLRs detect extracellular PAMPs, endosomal TLRs detect internalized nucleic acids, and cytoplasmic receptors detect intracellular pathogens, providing layered specificity.
Mechanisms of Signal Discrimination and Integration
Combinatorial Recognition and Heterodimerization
Many PRRs achieve enhanced specificity through combinatorial assembly. TLR2 forms heterodimers with either TLR1 or TLR6, enabling discrimination between triacyl and diacyl lipopeptides respectively [2] [4]. This subtle differentiation demonstrates how receptor combinations expand the coding capacity of the limited PRR repertoire. The specificity is further refined through accessory molecules; TLR4 requires MD-2 and CD14 for optimal LPS recognition, creating a multi-component recognition complex that precisely identifies this critical Gram-negative bacterial signature [4].
Cooperative Signaling and Cross-Talk Between PRR Pathways
Individual PAMPs often activate multiple PRR systems simultaneously, generating a composite signal that provides context for appropriate response scaling. For instance, viral infection typically engages both nucleic acid-sensing TLRs and RLRs, while bacterial infection may simultaneously activate surface TLRs and intracellular NLRs [4]. This cooperative signaling enables the immune system to discriminate between pathogen classes based on the unique combination of PRRs engaged.
Table 2: Quantitative Signaling Outputs Based on PAMP Context
| PAMP Combination | PRRs Engaged | NF-κB Activation | IRF Activation | Cytokine Profile | Inferred Pathogen Context |
|---|---|---|---|---|---|
| LPS | TLR4 | ++++ | ++ | High TNF-α, IL-6, moderate IFN-β | Gram-negative bacteria |
| dsRNA | TLR3, RIG-I/MDA5 | +++ | ++++ | Moderate IL-6, high IFN-α/β | RNA viruses |
| CpG DNA | TLR9 | ++ | + | High IL-12, moderate IFN-α | DNA viruses, intracellular bacteria |
| LPS + Bacterial RNA | TLR4, TLR8 | +++++ | +++ | High TNF-α, IL-6, IFN-γ | Viable Gram-negative bacteria |
Discrimination Through Signaling Kinetics and Amplitude
The immune system extracts critical information from the temporal dynamics of PRR signaling. Transient PAMP exposure may induce a self-limited inflammatory response, while persistent signaling indicates ongoing infection and triggers enhanced adaptive immunity [2] [4]. Similarly, signaling amplitude correlates with pathogen burden, enabling proportional response scaling. Negative feedback regulators such as IRAK-M, SOCS, and A20 help terminate responses once the threat is eliminated, preventing excessive inflammation [4].
Experimental Approaches for Studying PAMP Recognition
PRR Signaling Pathway Analysis
Methodology: To investigate TLR4 signaling specificity, researchers typically stimulate primary macrophages or specialized cell lines (HEK293-TLR4/MD2) with ultrapure LPS (100 ng/mL) for time courses ranging from 15 minutes to 24 hours [4] [3]. Signaling intermediates are analyzed via Western blotting for phosphorylation of IRAK1, IRAK4, IκBα, and MAPKs, while NF-κB and IRF3 nuclear translocation is assessed by immunofluorescence and EMSA. Cytokine output is quantified by ELISA (TNF-α, IL-6) and multiplex assays.
Specificity Controls: Critical controls include using TLR4-specific inhibitors (TAK-242), MD-2 antagonists, and genetic approaches (siRNA knockdown) to confirm pathway specificity [3]. Comparison with other TLR agonists (Pam3CSK4 for TLR2, poly(I:C) for TLR3) establishes signaling pathway uniqueness.
Gene Expression Profiling in Pattern Recognition
Methodology: Transcriptional specificity is assessed through RNA sequencing or Nanostring analysis of PRR-stimulated cells. Cells are treated with specific PAMPs for 4-8 hours, followed by RNA extraction and analysis. Bioinformatic approaches identify unique gene signatures for different PRR pathways.
Application: This approach has revealed that different TLR agonists induce both shared inflammatory genes and unique transcriptional programs. For example, TLR4 activation induces a distinct interferon-stimulated gene profile compared to TLR3 activation, despite both activating IRF3 [4] [3].
Figure 2: Experimental Framework for Analyzing PRR Signaling Specificity. Comprehensive approach combining specific stimulation, multiple analytical techniques, and data integration to elucidate discrimination mechanisms.
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for PAMP-PRR Research
| Reagent Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| Ultrapure PAMPs | LPS from E. coli (TLR4 ligand), Pam3CSK4 (TLR2/1 ligand), High-MW poly(I:C) (TLR3 ligand) | Specific PRR activation without contaminating agonists | Verify purity and absence of contaminants (e.g., protein in LPS preps) |
| PRR-Specific Inhibitors | TAK-242 (TLR4 inhibitor), Chloroquine (endosomal TLR inhibitor), ODN TTAGGG (TLR9 antagonist) | Pathway validation and functional studies | Confirm specificity through multiple PRR testing |
| Genetic Manipulation Tools | PRR knockout cells/mice, siRNA/shRNA, CRISPR-Cas9 gene editing | Establish necessity and sufficiency of specific PRRs | Consider compensatory mechanisms in knockout models |
| Signaling Antibodies | Phospho-specific antibodies (p-IRAK, p-IκB, p-IRF3), Total protein antibodies | Western blot, immunofluorescence for pathway activation | Optimize time courses for phosphorylation events |
| Cytokine Detection | ELISA kits (TNF-α, IL-6, IFN-β), Multiplex cytokine arrays, ELISpot kits | Quantify functional output of PRR activation | Establish standard curves and dynamic range |
Therapeutic Implications and Future Directions
Understanding the molecular basis of immune specificity opens transformative therapeutic opportunities. Targeting specific PRRs or their downstream signaling components offers potential for precision immunomodulation in infectious, inflammatory, and autoimmune diseases [4] [3]. TLR agonists are being developed as vaccine adjuvants and anticancer agents, while TLR antagonists show promise for treating sepsis and autoimmune conditions [4].
Emerging research on trained immunity reveals that innate immune cells can develop memory-like properties following PAMP exposure, mediated by epigenetic and metabolic reprogramming [26]. This phenomenon blurs the traditional distinction between innate and adaptive immunity and offers new therapeutic avenues for enhancing immune responses in immunocompromised individuals.
The convergence of PAMP and damage-associated molecular pattern (DAMP) signaling presents both challenges and opportunities [42] [86] [26]. In chronic inflammatory diseases, DAMPs may synergize with low levels of PAMPs to perpetuate inflammation, suggesting that combination therapies targeting both pathways may be more effective than single-target approaches.
The immune system achieves remarkable specificity in discriminating genuine threats through a multi-layered strategy involving structural complementarity, subcellular compartmentalization, combinatorial receptor usage, and context-dependent signal integration. Rather than relying on a single mechanism, the system employs concurrent strategies that collectively enable precise threat assessment. Continued elucidation of these discrimination mechanisms will inform next-generation therapeutics that selectively modulate inappropriate inflammation while preserving protective immunity.
Mechanisms of Immune Regulation and Tolerance to Prevent Excessive Inflammation
Within the context of pathogen-associated molecular patterns (PAMPs) and inflammation initiation research, a critical question emerges: how does the immune system prevent its powerful defensive reactions from causing excessive collateral damage to host tissues? The investigation of PAMPs has traditionally focused on how the innate immune system recognizes conserved microbial structures to initiate inflammatory responses. However, this paradigm alone cannot explain how the immune system maintains equilibrium in the face of persistent challenges. The discovery of damage-associated molecular patterns (DAMPs)—endogenous molecules released from stressed or damaged host cells—has revealed that sterile inflammation shares recognition and signaling pathways with pathogen-driven responses [7] [39]. This convergence places tremendous importance on the regulatory mechanisms that must operate to prevent pathological inflammation, whether triggered by PAMPs, DAMPs, or their interplay.
This whitepaper examines the sophisticated biological systems that maintain immune homeostasis, with particular emphasis on mechanisms that counterbalance PAMP and DAMP-driven inflammation. We explore the cellular players, molecular pathways, and experimental approaches that define the current understanding of immune regulation, providing researchers and drug development professionals with a technical framework for investigating and therapeutically targeting these processes.
Cellular Mechanisms of Peripheral Tolerance
Regulatory T Cells (Tregs): Masters of Immune Equilibrium
The immune system maintains balance through active suppression mechanisms, primarily mediated by regulatory T cells (Tregs). The 2025 Nobel Prize in Physiology or Medicine recognized foundational discoveries in this field, honoring the work of Brunkow, Ramsdell, and Sakaguchi, who identified Tregs and their master regulator, Foxp3 [87]. These cells constitute a specialized subset of CD4+ T cells dedicated to suppressing excessive immune activation and maintaining self-tolerance.
Classification and Heterogeneity: Tregs demonstrate remarkable heterogeneity and can be categorized based on their origin and functional specialization:
- Origin-based subsets: Include thymus-derived Tregs (tTregs), peripherally derived Tregs (pTregs), and in vitro-induced Tregs (iTregs). tTregs exhibit a stable regulatory phenotype with full demethylation of the Treg-specific demethylated region (TSDR), while pTregs and iTregs show less stable epigenetic configurations [88].
- Tissue-resident Tregs: Specialized subsets adapt to local microenvironments. Adipose tissue Tregs express PPARγ and ST2 (the IL-33 receptor); intestinal Tregs frequently co-express RORγt; and tumor-infiltrating Tregs typically express high levels of ICOS, PD-1, and CCR8 [88].
Suppressive Mechanisms: Tregs employ multiple contact-dependent and independent mechanisms to suppress effector immune cells:
- Cytokine secretion: Production of anti-inflammatory cytokines IL-10, IL-35, and TGF-β.
- Metabolic disruption: Consumption of IL-2 via high-affinity CD25 receptors, creating local cytokine deprivation.
- Cytolytic activity: Direct killing of effector cells via granzyme and perforin pathways.
- Inhibition of dendritic cell function: Via CTLA-4-mediated downregulation of CD80/CD86 co-stimulatory molecules [88].
Table 1: Key Subsets of Regulatory T Cells and Their Characteristics
| Subset Classification | Defining Markers/Features | Primary Functional Role | Stability/Plasticity |
|---|---|---|---|
| Thymic Treg (tTreg) | Foxp3⁺, CD25⁺, GPA33⁺ (human), fully demethylated TSDR | Establishment of self-tolerance | Highly stable |
| Peripheral Treg (pTreg) | Foxp3⁺, generated from naive Tconv cells in periphery | Tolerance to commensals, environmental antigens | Moderate stability |
| Activated Treg (aTreg) | CD45RO⁺ (human), CD44hiCD62L⁻ (mouse), high ICOS/CTLA-4 | Potent suppression at inflammatory sites | Stable during activation |
| Tissue-Resident Tregs | Tissue-specific markers (PPARγ in fat, RORγt in gut) | Local tissue homeostasis and repair | Adapted to niche signals |
The critical importance of Tregs is starkly evident in their dysregulation. Insufficient Treg activity or numbers can lead to multi-organ autoimmune disease, while excessive Treg activity may result in immunodeficiency, chronic infections, and cancer progression [87] [88]. This delicate balance makes Tregs a prime therapeutic target across multiple disease contexts.
Trained Immunity: Innate Immune Memory and Its Regulation
The traditional dichotomy between innate and adaptive immunity has been redefined by the discovery of "trained immunity"—a de facto memory response in innate immune cells. This phenomenon involves long-term functional reprogramming of innate immune cells following exposure to exogenous or endogenous stimuli, mediated by epigenetic and metabolic changes [26].
Inducers and Mechanisms: While microbial stimuli (PAMPs) were the first recognized inducers, sterile inflammatory factors such as DAMPs and lifestyle-associated molecular patterns (LAMPs) can similarly establish trained immunity. Key mechanisms include:
- Epigenetic reprogramming: Accumulation of activating histone marks (H3K4me3, H3K27ac) at promoters and enhancers of genes related to inflammation and metabolism.
- Metabolic reconfiguration: A shift from oxidative phosphorylation to aerobic glycolysis, increased glutaminolysis, and cholesterol synthesis, mediated by the mTOR-HIF-1α pathway [26].
- Central trained immunity: Long-term reprogramming of hematopoietic stem and progenitor cells (HSPCs) in the bone marrow, leading to myeloid lineage bias [26].
The maladaptive consequences of DAMP-induced trained immunity are particularly relevant to chronic inflammatory diseases. For example, oxidized LDL (oxLDL) and uremic toxins can induce trained immunity in monocytes and macrophages, contributing to the persistence of inflammation in atherosclerosis, chronic kidney disease, and other sterile inflammatory conditions [26]. This creates a self-perpetuating cycle of inflammation that represents a significant challenge for therapeutic intervention.
Molecular Pathways in Immune Regulation
Pattern Recognition Receptors: Gatekeepers of Inflammation
The innate immune system utilizes pattern recognition receptors (PRRs) to detect both PAMPs and DAMPs, initiating signaling cascades that can trigger inflammatory responses. The same receptor families often recognize both exogenous and endogenous danger signals, creating a potential for self-reinforcing inflammatory loops that require stringent regulation [7] [39] [89].
Table 2: Major PRR Families and Their Ligands in Inflammation and Tolerance
| Receptor Family | Example Receptors | PAMP Ligands | DAMP Ligands | Key Signaling Pathways |
|---|---|---|---|---|
| Toll-like Receptors (TLRs) | TLR4, TLR9 | LPS (TLR4), viral RNA (TLR7/8) | HMGB1, histones, mtDNA (TLR4, TLR9) | MyD88/TRIF → NF-κB, MAPK |
| NOD-like Receptors (NLRs) | NLRP3 | Microbial toxins | ATP, uric acid crystals, ROS | Inflammasome → Caspase-1 → IL-1β/IL-18 |
| RIG-I-like Receptors (RLRs) | RIG-I, MDA5 | Viral dsRNA | - | MAVS → IRF3/7 → Type I IFNs |
| DNA Sensors | cGAS | Microbial DNA | Self-DNA (mtDNA, nuclear) | STING → IRF3 → Type I IFNs |
| Other | RAGE | - | HMGB1, S100 proteins | Multiple (NF-κB, MAPK) |
The NLRP3 inflammasome exemplifies the convergence of PAMP and DAMP signaling. Its activation requires two steps: a priming signal (often through TLR recognition of PAMPs/DAMPs) that upregulates NLRP3 and pro-IL-1β expression, followed by an activation signal triggered by diverse PAMPs and DAMPs including ATP, ROS, and crystalline structures [89]. This two-step mechanism provides multiple regulatory checkpoints to prevent inappropriate inflammasome activation.
The Foxp3 Regulatory Network in Treg Development and Function
The transcription factor Foxp3 serves as the master regulator of Treg development and function. The discovery that mutations in the Foxp3 gene cause the fatal autoimmune disorder IPEX in humans and the scurfy phenotype in mice provided definitive evidence of its non-redundant role in immune tolerance [87] [90] [88].
Foxp3 governs Treg differentiation and function through several key mechanisms:
- Transcriptional regulation: Foxp3 modulates the expression of specific genes, either activating or repressing targets that define the Treg transcriptional signature.
- Stable lineage commitment: Stable Foxp3 expression is maintained by epigenetic modifications, particularly demethylation of the TSDR, ensuring long-term suppressive capacity.
- Metabolic programming: Foxp3 influences Treg metabolic pathways to support their suppressive functions and survival in inflammatory environments [88].
The critical importance of Foxp3⁺ Tregs extends beyond autoimmune protection to diverse physiological and pathological contexts, including tissue repair, cancer, metabolic homeostasis, and transplantation tolerance [88].
Therapeutic Applications and Experimental Approaches
Targeting Regulatory Pathways for Disease Intervention
Understanding immune regulatory mechanisms has opened promising avenues for therapeutic intervention across multiple disease areas. Strategies to modulate Treg function represent a particularly active area of investigation:
- Autoimmunity and Transplantation: Approaches to expand or stabilize Treg function include low-dose IL-2 therapy, adoptive transfer of ex vivo expanded Tregs, and small molecules that enhance Treg stability and function. Clinical trials using Treg transfer have shown promise in type 1 diabetes, graft-versus-host disease, and organ transplantation [88].
- Cancer Immunotherapy: Strategies to deplete or inhibit Tregs in the tumor microenvironment include monoclonal antibodies targeting Treg surface markers (e.g., anti-CTLA-4), small-molecule inhibitors disrupting Treg metabolic adaptation, and bispecific antibodies that selectively target tumor-infiltrating Tregs while sparing systemic Tregs [88].
- Inflammatory Diseases: Targeting maladaptive trained immunity represents an emerging therapeutic frontier. Potential approaches include metabolic inhibitors that disrupt the epigenetic reprogramming underlying trained immunity, and compounds that reverse persistent histone modifications in innate immune cells [26].
The Scientist's Toolkit: Key Research Reagents and Methodologies
Investigating immune regulation requires specialized experimental approaches and reagents. The following table summarizes essential tools for studying immune tolerance mechanisms:
Table 3: Essential Research Reagents for Investigating Immune Tolerance Mechanisms
| Reagent/Category | Specific Examples | Research Application | Technical Function |
|---|---|---|---|
| Treg Isolation & Detection | Anti-Foxp3 antibodies, anti-CD25 antibodies, anti-CD4 antibodies, TSDR methylation analysis | Identification, purification, and characterization of Treg subsets | Flow cytometry, immunohistochemistry, intracellular staining, epigenetic analysis |
| In vivo Treg Modulation | Anti-CTLA-4 antibodies, Anti-CD25 antibodies (PC61), IL-2/anti-IL-2 complexes, DEREG mice | Functional studies of Treg depletion or expansion in disease models | Targeted depletion or activation of Tregs in vivo |
| Treg Suppression Assays | CFSE-labeled Tconv cells, antigen-presenting cells, anti-CD3/anti-CD28 beads | In vitro assessment of Treg suppressive function | Measure proliferation inhibition of effector T cells |
| Cytokine & Signaling Analysis | Recombinant IL-2, TGF-β, IL-10; inhibitors for mTOR, STAT; phospho-flow antibodies | Studying Treg stability, plasticity, and signaling pathways | Cell culture stimulation, signaling pathway inhibition, phosphoprotein detection |
| Genetic Models | Foxp3-GFP reporter mice, Foxp3-Cre mice, conditional Foxp3 knockout mice | Fate-mapping, lineage tracing, and conditional gene deletion in Tregs | Visualization, ablation, or genetic manipulation of Tregs |
Advanced model systems are increasingly important for studying immune regulation. Immune-competent 3D in vitro models that incorporate macrophage co-cultures and cytokine feedback loops help capture the regulatory dynamics that determine real-world biological responses, providing more physiologically relevant platforms for investigating immune tolerance [90].
Signaling Pathways and Experimental Visualization
Integrated Signaling in PAMP/DAMP Recognition and Control
The following diagram illustrates the key signaling pathways involved in PAMP and DAMP recognition, inflammasome activation, and the counter-regulatory mechanisms that prevent excessive inflammation:
Diagram 1: Integrated Signaling in PAMP/DAMP Recognition and Control. This diagram illustrates the convergence of PAMP and DAMP signaling through pattern recognition receptors (PRRs), leading to inflammasome activation and cytokine production. Counter-regulatory mechanisms include Treg-mediated suppression and the potential maladaptive pathway of trained immunity, which can enhance subsequent inflammatory responses through epigenetic and metabolic reprogramming.
Experimental Workflow for Treg Suppression Assay
The following diagram outlines a standard experimental protocol for assessing Treg suppressive function in vitro, a fundamental methodology in immune tolerance research:
Diagram 2: Experimental Workflow for Treg Suppression Assay. This methodology assesses the functional capacity of Tregs to suppress the proliferation of conventional T cells (Tconv) in response to stimulation, typically measured by flow cytometric analysis of CFSE dye dilution.
The mechanisms governing immune regulation and tolerance represent sophisticated biological systems that continuously counterbalance the inflammatory potential of both PAMP and DAMP recognition pathways. From the Foxp3-directed specialization of regulatory T cells to the epigenetic reprogramming of innate immune memory, these regulatory layers ensure that immune responses remain proportionate to the threat while minimizing collateral damage to host tissues. The convergence of PAMP and DAMP signaling through shared pattern recognition receptors highlights the evolutionary logic of regulating both infectious and sterile inflammation through integrated mechanisms. For researchers and drug development professionals, understanding these regulatory networks provides not only fundamental biological insight but also promising therapeutic avenues for restoring immune equilibrium in autoimmunity, chronic inflammation, cancer, and transplantation medicine.
The innate immune system serves as the host's first line of defense, relying on pattern recognition receptors (PRRs) to detect conserved pathogen-associated molecular patterns (PAMPs) and initiate protective immune responses [91] [4]. This recognition system triggers signaling cascades that activate transcription factors such as NF-κB and IRF3/7, leading to the production of type I interferons (IFN-α and IFN-β), proinflammatory cytokines, and interferon-stimulated genes (ISGs) that collectively establish an antiviral state [91] [92]. However, successful pathogens have evolved sophisticated countermeasures to subvert these host defense mechanisms. The molecular interplay between PAMP-PRR signaling and pathogen evasion strategies represents a critical frontier in host-pathogen interactions, with significant implications for understanding infectious disease pathogenesis and developing novel therapeutic interventions [13] [93].
This review comprehensively examines the molecular mechanisms by which diverse pathogens, particularly viruses, evade or subvert PRR-mediated innate immune recognition and signaling. We focus on the strategic targeting of key nodes in PRR signaling pathways, the consequent impact on host immunity, and the experimental approaches used to investigate these evasion strategies. The insights gained from studying these host-pathogen interactions not only advance our fundamental understanding of immunology but also reveal potential targets for therapeutic manipulation in infectious diseases, inflammatory disorders, and cancer.
PRR Signaling Pathways: Prime Targets for Pathogen Subversion
Major PRR Families and Their Signaling Mechanisms
PRRs are strategically localized throughout the cell to detect pathogens at various entry points and stages of the infectious cycle. These receptors can be broadly categorized into transmembrane receptors (e.g., Toll-like receptors or TLRs) and cytosolic sensors (e.g., RIG-I-like receptors or RLRs, and DNA sensors like cGAS) [33] [3]. Each PRR family recognizes distinct PAMPs and activates specific signaling pathways that converge on the induction of antiviral and inflammatory genes.
Toll-like receptors (TLRs) are type I transmembrane proteins characterized by extracellular leucine-rich repeat (LRR) domains for ligand recognition and intracellular Toll/IL-1 receptor (TIR) domains for signal transduction [33] [3]. Among the TLRs, TLR3, TLR7, TLR8, and TLR9 are localized to endosomal compartments where they recognize viral nucleic acids, while TLR2, TLR4, TLR5, and TLR6 are primarily expressed on the cell surface where they detect microbial membrane components such as lipids and proteins [3] [4]. TLR signaling occurs primarily through two adapter pathways: the MyD88-dependent pathway utilized by all TLRs except TLR3, and the TRIF-dependent pathway employed by TLR3 and TLR4 [91].
RIG-I-like receptors (RLRs), including RIG-I and MDA5, function as cytosolic sensors for viral RNA [91] [4]. These receptors contain DExD/H-box RNA helicase domains that recognize distinct RNA species and caspase activation and recruitment domains (CARDs) that initiate downstream signaling through the mitochondrial adapter protein MAVS (also known as IPS-1, VISA, or Cardif) [91]. RLR signaling activates the kinases TBK1 and IKKε, which phosphorylate the transcription factors IRF3 and IRF7, leading to type I interferon production [91].
The cGAS-STING pathway represents a major cytosolic DNA sensing mechanism. cGAS (cyclic GMP-AMP synthase) detects double-stranded DNA and synthesizes the second messenger 2'3'-cGAMP, which binds to and activates STING (stimulator of interferon genes) on the endoplasmic reticulum membrane [91]. Activated STING then traffics to the Golgi apparatus, where it recruits TBK1 to phosphorylate IRF3, inducing interferon gene expression [91].
Table 1: Major PRR Families and Their Characteristics
| PRR Family | Localization | Representative Members | Key PAMP Ligands | Adapter Proteins | Key Transcription Factors |
|---|---|---|---|---|---|
| Toll-like Receptors (TLRs) | Cell Surface, Endosomes | TLR3, TLR4, TLR7, TLR8, TLR9 | dsRNA, LPS, ssRNA, CpG DNA | MyD88, TRIF, MAL, TRAM | NF-κB, IRF3, IRF7, AP-1 |
| RIG-I-like Receptors (RLRs) | Cytosol | RIG-I, MDA5 | Short dsRNA, 5'-triphosphate RNA, Long dsRNA | MAVS | IRF3, IRF7, NF-κB |
| DNA Sensors | Cytosol | cGAS, AIM2 | Cytosolic DNA | STING, ASC | IRF3, NF-κB |
| NOD-like Receptors (NLRs) | Cytosol | NOD1, NOD2, NLRP3 | Peptidoglycan fragments, DAMPs | RIP2, ASC, Caspase-1 | NF-κB, Inflammasome |
Downstream Antiviral Effector Mechanisms
PRR signaling culminates in the activation of transcription factors that translocate to the nucleus and induce the expression of hundreds of genes involved in antiviral defense [91]. Type I interferons (IFN-α and IFN-β) are secreted and act in autocrine and paracrine manners by binding to the interferon-α/β receptor (IFNAR), which activates the JAK-STAT pathway [91] [92]. This leads to the formation of the ISGF3 complex (STAT1, STAT2, and IRF9) that drives the expression of interferon-stimulated genes (ISGs) [91]. Among these ISGs, ISG15 plays a crucial role in the ISGylation process, a ubiquitin-like modification that tags both viral and host proteins to regulate immune responses and inhibit viral replication [91] [92]. The coordinated action of these effector molecules establishes a cellular antiviral state that limits pathogen replication and spread.
Molecular Mechanisms of Pathogen Evasion
Viral Evasion of PRR Signaling
Viruses have evolved numerous strategies to evade or subvert PRR-mediated innate immune recognition at multiple levels of the signaling cascade. These evasion mechanisms can be categorized based on their specific molecular targets within the host defense system.
Interference with PRR ligand recognition represents a primary evasion strategy. Some viruses mask their PAMPs to avoid detection, as observed with certain coronaviruses that conceal their viral RNA through membrane-bound replication compartments [13]. Other viruses, like influenza A virus, generate decoy RNAs or cap snatching to avoid RIG-I recognition [93]. SARS-CoV-2 employs a complex strategy involving the formation of double-membrane vesicles that sequester viral RNA from cytosolic sensors, effectively hiding its replication intermediates from PRR surveillance [13].
Direct targeting of PRR signaling components provides another efficient evasion mechanism. The Kaposi's sarcoma-associated herpesvirus (KSHV) encodes multiple proteins that systematically dismantle PRR signaling pathways [93]. For instance, KSHV vIRF1 protein directly interacts with and inhibits TBK1, preventing IRF3 phosphorylation and subsequent interferon production [93]. Similarly, SARS-CoV-2 has been shown to encode proteins that disrupt key nodes in PRR signaling, with several of its accessory proteins (e.g., ORF3a, ORF6, and ORF9b) interfering with both RLR and TLR pathways at the level of MAVS and TBK1 [13].
Manipulation of the interferon response represents a common viral strategy to circumvent the effector phase of innate immunity. Many viruses encode proteins that directly inhibit JAK-STAT signaling or promote the degradation of STAT proteins [93]. Furthermore, viruses have developed specific countermeasures against individual ISGs; for example, several viruses including influenza A virus and SARS-CoV-2 have evolved mechanisms to evade the antiviral effects of ISG15 and ISGylation, either by encoding viral deISGylating enzymes or by preventing the ISGylation of specific viral proteins [91] [92].
Table 2: Viral Evasion Strategies Targeting PRR Signaling Pathways
| Target Pathway | Viral Pathogen | Evasion Mechanism | Molecular Consequence |
|---|---|---|---|
| TLR Signaling | SARS-CoV-2 | Downregulation of TLR expression; Proteolytic cleavage of TLR adapters | Reduced IFN production; Impaired NF-κB activation |
| RLR Signaling | Influenza A Virus, KSHV | Sequestration of viral RNA; Direct inhibition of RIG-I, MAVS, or TBK1 | Blocked IRF3 activation; Suppressed IFN-β production |
| cGAS-STING Pathway | HIV, HSV | Degradation of cGAS or STING; Prevention of STING trafficking | Impaired response to cytosolic DNA; Reduced IRF3 activation |
| JAK-STAT Signaling | Multiple Viruses | Inhibition of JAK kinases; Degradation of STAT proteins | Blunted response to IFNs; Reduced ISG expression |
| ISG Effector Functions | SARS-CoV-2, Influenza A Virus | Counteraction of ISG15-mediated ISGylation | Enhanced viral replication; Immune evasion |
Bacterial and Fungal Evasion Strategies
While viral evasion mechanisms have been extensively characterized, bacterial and fungal pathogens have also evolved sophisticated strategies to subvert PRR-mediated immunity. These include modification of PAMPs to avoid recognition, secretion of effector proteins that inhibit signaling components, and manipulation of host cell death pathways to limit inflammatory responses [4] [94].
In Drosophila, the Persephone protease defines a parallel proteolytic cascade activated by danger signals such as abnormal proteolytic activities during fungal and Gram-positive bacterial infections [94]. Some bacterial pathogens modify their surface components, such as lipid A of LPS in Gram-negative bacteria, to reduce TLR4 activation [4]. Additionally, various bacterial secretion systems deliver effector proteins directly into host cells that can inhibit key signaling molecules in PRR pathways, including IKK complexes and MAP kinases [4].
Experimental Approaches for Studying Evasion Mechanisms
Methodologies for Investigating PRR-Pathogen Interactions
The elucidation of pathogen evasion strategies relies on a multidisciplinary experimental approach combining molecular biology, biochemistry, and immunology techniques. Key methodologies include:
Gene expression profiling to assess pathogen-induced changes in PRR and ISG expression. For SARS-CoV-2 infection, studies have utilized quantitative PCR and RNA sequencing to demonstrate altered expression of TLRs (particularly TLRs 2, 3, 4, 7, 8 and 9), RLRs, and DNA sensors in patient-derived samples and cell culture models [13]. These approaches have revealed that SARS-CoV-2 infection modulates the expression of multiple PRRs, contributing to the dysregulated interferon response observed in severe COVID-19.
Protein-protein interaction studies to identify direct targeting of signaling components. Co-immunoprecipitation assays coupled with mass spectrometry have been instrumental in discovering viral proteins that physically interact with key signaling molecules such as MAVS, TBK1, and IRF3 [13] [93]. For instance, these approaches demonstrated that KSHV proteins form complexes with multiple nodes in the RLR signaling pathway, effectively shutting down interferon production [93].
Luciferase reporter assays to measure pathway-specific activation or inhibition. These assays employ engineered reporter constructs containing interferon-stimulated response elements (ISRE) or NF-κB binding sites upstream of a luciferase gene [13]. This methodology has been crucial for mapping the specific steps in PRR signaling targeted by viral proteins, such as the identification of SARS-CoV-2 ORF6 as a potent inhibitor of IRF3 nuclear translocation [13].
Functional genomics approaches including CRISPR/Cas9 screens to identify host factors essential for pathogen evasion. Genome-wide knockout screens have revealed host dependencies for viral replication and identified restriction factors that pathogens must counter for successful infection [13]. These studies have highlighted the complex interplay between viral evasion mechanisms and host defense systems.
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Research Reagents for Studying PRR Evasion Mechanisms
| Reagent Category | Specific Examples | Research Application | Key Functions |
|---|---|---|---|
| PRR-Specific Agonists | Poly(I:C) (TLR3), R848 (TLR7/8), CpG ODN (TLR9), 3p-RNA (RIG-I) | Pathway activation controls | Selective PRR stimulation; Positive controls for signaling assays |
| Reporter Cell Lines | ISRE-Luc, NF-κB-Luc, IFN-β-Luc | Pathway activity measurement | Quantification of PRR pathway activation/inhibition; High-throughput screening |
| Pathway Inhibitors | BX795 (TBK1/IKKε inhibitor), MRT67307 (IKKε inhibitor) | Signal transduction dissection | Validation of specific pathway components; Mechanism of action studies |
| Genetic Manipulation Tools | PRR knockout cells, siRNA/shRNA libraries, CRISPR/Cas9 systems | Functional gene analysis | Identification of essential pathway components; Validation of pathogen targets |
| Cytokine Detection Assays | ELISA, ELISpot, Multiplex bead arrays | Immune response quantification | Measurement of IFN and cytokine production; Correlation with PRR activation |
| Protein Interaction Tools | Co-IP kits, Proximity ligation assays, Yeast two-hybrid systems | Molecular mechanism elucidation | Identification of direct pathogen-host protein interactions; Complex formation analysis |
Signaling Pathway Diagrams
PAMP-PRR Signaling and Major Viral Evasion Points
Experimental Workflow for Elucidating Evasion Mechanisms
Concluding Perspectives and Therapeutic Implications
The continuous molecular arms race between host PRR signaling and pathogen evasion strategies represents a fundamental aspect of host-pathogen coevolution. The sophisticated mechanisms employed by viruses, bacteria, and fungi to subvert innate immune recognition highlight the selective pressure exerted by the host defense system and underscore the critical importance of PAMP-PRR interactions in determining infection outcomes [91] [93] [4].
Understanding these evasion mechanisms at molecular resolution provides valuable insights for therapeutic development. Several strategies are currently being explored to counteract pathogen evasion, including the use of PRR agonists to boost innate immune responses before or during early infection [13]. For SARS-CoV-2, therapeutic modulation of PRR pathways represents a promising approach, with TLR7/8 agonists such as imiquimod showing potential in enhancing antiviral immunity [13]. Similarly, STING agonists are being investigated for their ability to restore interferon responses in chronic viral infections [33].
Future research directions should focus on elucidating the structural basis of pathogen-host protein interactions to enable rational drug design, exploring combinatorial therapeutic approaches that target multiple evasion mechanisms simultaneously, and investigating how different pathogen species converge on similar evasion strategies despite evolutionary divergence. Additionally, the role of PRR evasion in the pathogenesis of long COVID deserves particular attention, as emerging evidence suggests that altered PRR expression and signaling may contribute to the persistence of symptoms [13].
As our understanding of pathogen evasion strategies continues to deepen, so too will our ability to develop targeted interventions that restore effective immune recognition and response, ultimately shifting the balance in favor of host defense in the eternal battle against infectious diseases.
Research on pathogen-associated molecular patterns (PAMPs) and the initiation of inflammation represents a frontier area in immunology and drug development. The fundamental understanding of how innate immune receptors such as Toll-like receptors (TLRs) recognize conserved microbial components has largely been established through reductionist in vitro models [95] [96]. However, a significant translational gap persists between these controlled experimental findings and the complex pathophysiology observed in living organisms. This whitepaper examines the core challenges in extrapolating in vitro PAMP research to in vivo systems, with particular emphasis on the confounding variables of cellular context, metabolic influence, and systemic integration that complicate prediction of biological outcomes. The dilemma is particularly acute in organs such as the liver, which faces a constant flood of non-pathogenic PAMPs from the intestinal microbiota and must distinguish these from true danger signals—what has been termed the problem of finding "a signal in a sea of noise" [97]. Through structured analysis of experimental data, signaling pathways, and methodological considerations, this review provides a framework for enhancing translational validity in inflammation research.
Quantitative Disparities Between In Vitro and In Vivo Systems
Comparative Analysis of Inflammatory Responses
Table 1: Differential Responses to LPS Stimulation Across Experimental Systems
| Experimental System | Concentration/Dose | Key Inflammatory Markers | Magnitude of Response | Temporal Dynamics |
|---|---|---|---|---|
| RAW 264.7 Macrophages [96] | 100 ng/mL LPS | NO, PGE₂, TNF-α, IL-1β, IL-6 | High NO production (54.2% inhibition with DSHT) | Acute peak (6-24 hours) |
| Mouse Systemic Inflammation [98] | 10 mg/kg LPS (i.p.) | Plasma ALT, AST, BUN, Creatinine | Significant plasma biomarker elevation | Sustained (4-24 hours) |
| Zebrafish Tail Fin Injury [99] | Endogenous TNF-α | tnfa:egfp reporter, macrophage recruitment | Directed macrophage migration | Rapid (2 hpa), spatially restricted |
| Human Trained Immunity [26] | β-glucan, oxLDL | H3K4me3, H3K27ac, cytokine production | Epigenetic reprogramming | Long-term (months to years) |
The quantitative disparities evident in Table 1 highlight the fundamental challenge of dose selection when translating between systems. The lipopolysaccharide (LPS) concentrations required to elicit robust inflammatory responses in isolated macrophages (typically 100 ng/mL) [96] far exceed the physiological relevance of circulating PAMPs in vivo, where the liver must process constant low-level exposure from intestinal microbiota [97]. Furthermore, the magnitude and persistence of inflammatory responses differ substantially, with in vitro systems exhibiting acute, self-limiting responses while in vivo systems demonstrate complex temporal dynamics including the emerging concept of "trained immunity"—a long-term functional reprogramming of innate immune cells mediated by epigenetic and metabolic changes [26].
Methodological Considerations in Experimental Models
Table 2: Technical Approaches for Validating PAMP Responses
| Methodology | Application | Key Parameters | Technical Limitations |
|---|---|---|---|
| Macrophage Polarization Assays [100] | M1/M2 phenotype quantification | IRF-5, STAT-1, cytokine profiles | In vitro polarization may not reflect in vivo spectrum |
| Cytokine Profiling (Luminex/ELISA) [101] | Multiplex cytokine measurement | IL-6, TNF-α, IL-1β, IL-8, MCP-1 | Plasma levels may not reflect tissue microenvironment |
| Gene Expression (RT-qPCR) [101] | Targeted inflammatory gene analysis | STAT1, STAT3, CXCL10, SOCS3 | mRNA levels may not correlate with protein expression |
| Flow Cytometry Immune Profiling [98] | Immune cell population analysis | M1/M2 macrophages, neutrophil maturation | Tissue dissociation artifacts |
| Epigenetic Modification Analysis [26] | Trained immunity assessment | H3K4me3, H3K27ac histone marks | Cell heterogeneity in complex tissues |
The methodological approaches summarized in Table 2 represent core techniques for investigating PAMP-induced inflammation across experimental systems. Recent advances in epigenetic mapping and single-cell technologies have revealed previously unappreciated dimensions of immune reprogramming, particularly the role of damage-associated molecular patterns (DAMPs) and lifestyle-associated molecular patterns (LAMPs) in inducing trained immunity through metabolic and epigenetic rewiring [26]. This expanded understanding complicates the interpretation of traditional in vitro models that examine PAMP responses in isolation, without the contextual signals from tissue damage or metabolic factors present in vivo.
Experimental Protocols for Enhanced Translational Validity
Standardized Macrophage Activation Protocol
The following protocol, synthesized from multiple methodologies [98] [100] [96], provides a standardized approach for evaluating PAMP responses in macrophages with enhanced translational relevance:
Cell Culture Conditions:
- Use primary bone marrow-derived macrophages (BMDMs) or human monocyte-derived macrophages alongside immortalized cell lines (e.g., RAW 264.7) to enable comparison.
- Culture in serum-free conditions for 24 hours prior to stimulation to minimize confounding effects of serum components.
Stimulation Protocol:
- Apply LPS (100 ng/mL) or other PAMPs (β-glucan, 10 μg/mL) for 6-24 hours.
- Include co-stimulation with DAMPs (HMGB1, 50 ng/mL; mtDNA, 100 ng/mL) to model sterile inflammation contexts [7].
- Pre-treat with potential inhibitors (e.g., DSHT 100-400 μg/mL [96], PDZ peptide 7.5 mg/kg [98]) 2-4 hours prior to PAMP exposure.
Response Assessment:
- Quantify inflammatory mediators (NO, PGE₂) via Griess assay and ELISA.
- Analyze cytokine expression (TNF-α, IL-1β, IL-6) at protein (ELISA/Luminex) and transcriptional (RT-qPCR) levels.
- Evaluate protein expression (iNOS, COX-2, TLR4, MyD88) via Western blotting.
- Assess NF-κB and MAPK signaling pathways through phosphoprotein analysis and nuclear translocation assays.
In Vivo Validation Protocol
To bridge the in vitro-in vivo gap, the following validation protocol is recommended:
Animal Model Selection:
- Utilize zebrafish tail fin injury model for real-time visualization of immune cell behavior [99].
- Employ murine systemic inflammation models (LPS 10 mg/kg, i.p.) for physiological relevance [98].
- Consider chronic inflammatory models (e.g., atherosclerosis, CKD) to assess trained immunity contributions [26].
Endpoint Analysis:
- Monitor tissue injury markers (ALT, AST, BUN, Creatinine) in plasma.
- Perform histopathological examination of target tissues (liver, kidney, lung).
- Conduct immune cell profiling via flow cytometry (M1/M2 macrophages, neutrophil subsets).
- Assess functional outcomes (tissue regeneration, survival rate).
Signaling Pathway Complexity and Cross-System Discrepancies
TLR4/NF-κB Signaling Network
Diagram 1: PAMP Signaling in Isolated vs. Integrated Contexts. The core TLR4/NF-κB pathway (yellow) demonstrates how in vitro studies reveal linear signaling, while in vivo contexts (green) introduce complex feedback loops and integrated signaling with DAMPs/LAMPs (red) that drive long-term epigenetic and metabolic reprogramming.
The signaling network depicted in Diagram 1 illustrates the fundamental complexity of PAMP-induced inflammation. While in vitro models reveal a relatively linear TLR4/MyD88/NF-κB pathway leading to pro-inflammatory gene expression [96], in vivo systems demonstrate nonlinear feedback regulation and cross-talk with parallel signaling systems. For instance, in zebrafish models of tissue regeneration, an NF-κB/TNF-α feedback loop precisely coordinates macrophage recruitment and inflammatory responses to injury [99]. This regulatory complexity creates significant interpretation challenges, as pharmacological inhibition of specific pathway components (e.g., IKK2 inhibition with BMS-345541) may produce diametrically opposed outcomes in different cellular contexts.
Experimental Workflow for Pathway Validation
Diagram 2: Iterative Workflow for Translational Validation. This workflow outlines an iterative approach for bridging in vitro and in vivo findings, emphasizing the critical importance of discrepancy identification and contextual analysis in refining experimental models.
The experimental workflow in Diagram 2 provides a systematic approach for addressing translational challenges. This iterative process emphasizes the importance of contextual factor analysis when discrepancies emerge between experimental systems. For example, the discovery that TNF-α promotes macrophage survival in the presence of methotrexate in vitro [102] required validation in complex in vivo systems to establish its relevance to rheumatoid arthritis treatment. Similarly, observations of PEGylated PDZ peptide efficacy in suppressing LPS-induced systemic inflammation in mice [98] must be reconciled with in vitro macrophage activation studies to establish mechanism of action.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for PAMP-Inflammation Studies
| Reagent/Category | Specific Examples | Research Application | Technical Considerations |
|---|---|---|---|
| PAMP Agonists | LPS, β-glucan, Flagellin | TLR4, Dectin-1, TLR5 activation | Purity critical (ultrapure LPS vs. contaminated preparations) |
| DAMP Agonists [26] [7] | HMGB1, mtDNA, Histones, ATP | Sterile inflammation models | Concentration-dependent effects (chemoattractant vs. pro-inflammatory) |
| Signaling Inhibitors [99] [96] | BMS-345541 (IKK2i), JSH-23 (NF-κB i), DSHT | Pathway dissection, therapeutic candidates | Specificity validation essential (off-target effects) |
| Cytokine Analysis [101] | ELISA/Luminex panels: TNF-α, IL-1β, IL-6, IL-10 | Inflammatory response quantification | Temporal expression patterns critical for interpretation |
| Epigenetic Modifiers [26] | Set7 methyltransferase inhibitors, KDM5 demethylase inhibitors | Trained immunity investigation | Cell type-specific effects; metabolic connections |
| Animal Models [98] [99] | Zebrafish tail fin injury, Murine LPS challenge, Chronic disease models | Physiological validation | Species-specific differences in TLR4 signaling |
The research reagents summarized in Table 3 represent essential tools for investigating PAMP-mediated inflammation across experimental systems. Recent additions to this toolkit reflect the growing appreciation of trained immunity as a mechanism whereby innate immune cells develop memory-like characteristics through epigenetic reprogramming [26]. This paradigm shift necessitates reagents that target not only traditional signaling pathways but also the metabolic and epigenetic regulators (e.g., mTOR-HIF-1α, mevalonate, KDM5 demethylases) that underlie long-term functional reprogramming of immune cells.
The interpretation challenges in linking in vitro findings to in vivo pathophysiology in PAMP research stem from fundamental biological complexities that cannot be fully reduced to isolated systems. The cellular microenvironment, metabolic cross-talk, neural and endocrine influences, and tissue-specific structural organization collectively create emergent properties that cannot be predicted from reductionist models alone. Addressing this translational gap requires methodological sophistication including (1) iterative validation across experimental systems, (2) incorporation of relevant contextual signals (DAMPs, LAMPs), (3) temporal analysis extending beyond acute responses to capture trained immunity phenomena, and (4) application of computational modeling to integrate multifactorial signaling data. By embracing these approaches, researchers can enhance the predictive validity of in vitro systems and accelerate the development of therapeutics targeting PAMP-driven inflammatory diseases.
Defining the Role of Ion Channels (e.g., TRP Channels) in Inflammasome Activation by PAMPs/DAMPs
The innate immune system responds to pathogen invasion and tissue damage through pattern recognition receptors (PRRs) that detect pathogen-associated molecular patterns (PAMPs) and damage-associated molecular patterns (DAMPs). Emerging research reveals that ion channels, particularly transient receptor potential (TRP) channels, serve as critical intermediaries in the activation of inflammasomes—multiprotein complexes that drive inflammatory responses. This technical review examines the molecular mechanisms by which ion channels, in response to PAMPs/DAMPs, facilitate NLRP3 inflammasome assembly through calcium signaling, potassium efflux, and membrane potential modulation. We synthesize current experimental evidence, detail methodological approaches for investigating these pathways, and discuss the therapeutic potential of targeting ion channels in inflammatory diseases. The integration of ion channel biology with inflammasome research provides a novel framework for understanding sterile inflammation and developing precision immunotherapies.
Innate immunity constitutes the first line of defense against infectious agents and tissue damage, relying on germline-encoded pattern recognition receptors (PRRs) to detect conserved molecular signatures known as PAMPs and DAMPs [33]. While PRR signaling pathways have been extensively characterized, recent evidence identifies ion channels as essential components in the resulting inflammatory cascade, particularly in the activation of the NLRP3 inflammasome [103].
The NLRP3 inflammasome, a multiprotein complex comprising NLRP3, ASC, and caspase-1, processes pro-IL-1β and pro-IL-18 into their active forms and induces pyroptosis [104]. Its activation requires two signals: priming (transcriptional upregulation of components) and activation (complex assembly) [104]. Ion channels have emerged as crucial mediators of the activation phase, translating PAMP/DAMP recognition into ionic fluxes that trigger inflammasome assembly [103].
This review focuses on the role of TRP channels and other ion channels in bridging PAMP/DAMP sensing to NLRP3 inflammasome activation, with emphasis on underlying mechanisms, experimental methodologies, and therapeutic implications for inflammatory diseases.
Molecular Mechanisms of Ion Channel-Mediated Inflammasome Activation
TRP Channels: Calcium Gatekeepers in Inflammation
Transient receptor potential (TRP) channels constitute a large family of non-selective cation-permeable channels that function as polymodal cellular sensors. These channels are classified into six subfamilies based on sequence homology: TRPC (canonical), TRPV (vanilloid), TRPM (melastatin), TRPP (polycystin), TRPML (mucolipin), and TRPA (ankyrin) [103]. These channels share a common topology with six transmembrane segments and a cation-permeable pore region between the fifth and sixth segments [103].
In immune cells, TRP channels, particularly TRPV1, TRPV2, TRPV4, TRPM2, TRPM7, and TRPA1, are activated by various PAMPs/DAMPs and mediate calcium influx that serves as a critical second messenger for NLRP3 inflammasome activation [103]. The resulting increased intracellular calcium ([Ca²⁺]i) promotes several pro-inflammatory processes:
- Mitochondrial dysfunction: Calcium overload induces mitochondrial permeability transition pore (mPTP) opening and reactive oxygen species (ROS) production, a potent NLRP3 activator [103].
- Phospholipase C activation: Calcium activates PLC, generating inositol trisphosphate (IP3) that further releases calcium from endoplasmic reticulum stores [103].
- Calmodulin signaling: Calcium-bound calmodulin activates downstream kinases and phosphatases that regulate NLRP3 phosphorylation status [103].
Table 1: TRP Channels in Inflammasome Activation
| TRP Channel | Activators | Immune Role | Linked Diseases |
|---|---|---|---|
| TRPV1 | Capsaicin, heat, endocannabinoids, inflammatory mediators | Pain, neurogenic inflammation | Chronic pain, inflammatory disorders |
| TRPV2 | Osmolarity changes, cannabinoids | Macrophage activation, cytokine production | Cardiovascular inflammation |
| TRPV4 | Osmolarity, arachidonic acid metabolites | Endothelial inflammation, barrier disruption | Pulmonary edema, arthritis |
| TRPM2 | ROS, ADP-ribose | Oxidative stress response, cytokine release | Neurodegeneration, diabetes |
| TRPM7 | ROS, nucleotides | Magnesium homeostasis, dendritic cell activation | Allergic contact dermatitis |
| TRPA1 | Reactive chemicals, cold temperature | Chronic visceral inflammation, pain | Asthma, inflammatory bowel disease |
Potassium Efflux: A Conserved Activation Mechanism
Potassium efflux represents a common mechanism for NLRP3 inflammasome activation across multiple PAMP/DAMP signaling pathways. Several ion channels contribute to this process:
- Two-pore domain potassium channels: These background channels regulate resting membrane potential and can be modulated by PAMPs/DAMPs [103].
- Voltage-gated potassium channels: Changes in membrane potential during immune cell activation affect these channels [103].
- Calcium-activated potassium channels: TRP channel-mediated calcium influx activates these channels, creating coordinated ion flux [103].
The mechanism by which potassium efflux activates NLRP3 involves cellular depletion of potassium ions below a threshold concentration (approximately 90 mM), which induces a conformational change in NLRP3 that facilitates its interaction with NEK7 and subsequent oligomerization [104]. This potassium efflux can occur through specific potassium channels or through membrane damage induced by pore-forming toxins or crystals [39].
Membrane Potential and Chloride Flux
Beyond calcium and potassium fluxes, changes in membrane potential and chloride ion movement also contribute to inflammasome regulation:
- Membrane depolarization: TRP channel-mediated cation influx depolarizes membranes, potentially affecting voltage-sensitive signaling molecules [103].
- Chloride efflux: NLRP3 activators like ATP and crystals induce chloride efflux through CLIC proteins, which works synergistically with potassium efflux [39].
- Sodium fluxes: While less studied, sodium influx through non-selective cation channels may contribute to osmotic imbalances that affect inflammasome activation [103].
Experimental Approaches for Studying Ion Channel-Inflammasome Axis
Electrophysiological Recordings
Electrophysiological techniques directly measure ion channel activity in immune cells:
Patch-clamp Recordings:
- Whole-cell configuration: Measures total current across the entire cell membrane while controlling intracellular environment
- Perforated-patch configuration: Maintains natural intracellular signaling components while accessing electrical properties
- Single-channel recording: Resolves individual channel opening/closing events for pharmacological characterization
Loose-patch clamp technique: As employed by Bertagna et al. to study hippocampal neurons, this method can be adapted for immune cells to link intracellular Ca²⁺ release to modulation of voltage-gated currents with minimal disruption to intracellular signaling [105].
Calcium Imaging and Flux Measurements
Intracellular calcium dynamics represent a key signaling node between ion channels and inflammasomes:
Fluorescent calcium indicators:
- Ratiometric dyes (Fura-2, Indo-1): Provide quantitative [Ca²⁺]i measurements through emission/excitation ratioing
- Single-wavelength dyes (Fluo-4, Cal-520): Offer higher signal-to-noise ratio for detecting rapid calcium transients
- Genetically encoded indicators (GCaMP): Enable cell-specific targeting and long-term monitoring in primary cells
Experimental workflow:
- Load immune cells with calcium-sensitive fluorescent dye
- Stimulate with PAMPs/DAMPs (LPS, ATP, crystals) in presence/absence of channel inhibitors
- Monitor fluorescence changes in real-time using confocal microscopy or plate readers
- Correlate calcium signatures with inflammasome activation (caspase-1 cleavage, IL-1β secretion)
Genetic and Pharmacological Manipulation
Genetic approaches:
- CRISPR/Cas9-mediated knockout: Generate immune cells lacking specific ion channels or inflammasome components
- siRNA/shRNA knockdown: Transient reduction of target channel expression in primary immune cells
- Transgenic expression: Introduce wild-type or mutant channels into channel-deficient cells
Pharmacological tools:
- Channel agonists/antagonists: Selective modulators to establish causal relationships
- Toxins: Natural products with high specificity for certain channel classes
- Small molecule inhibitors: Developed through targeted drug discovery efforts
Table 2: Key Research Reagents for Ion Channel-Inflammasome Studies
| Reagent Category | Specific Examples | Function/Application |
|---|---|---|
| TRP Channel Modulators | Capsazepine (TRPV1 antagonist), HC-030031 (TRPA1 antagonist), Ruthenium Red (broad TRP blocker) | Inhibit specific TRP channels to establish their contribution to inflammasome activation |
| Potassium Channel Modulators | Glibenclamide (KATP blocker), TRAM-34 (KCa3.1 blocker), Charybdotoxin (KCa blocker) | Evaluate role of potassium efflux pathways in NLRP3 activation |
| Calcium Indicators | Fura-2 AM, Fluo-4 AM, Rhod-2 AM (mitochondrial Ca²⁺) | Measure spatial and temporal dynamics of intracellular calcium signals |
| NLRP3 Activators | ATP, nigericin, monosodium urate crystals, imiquimod | Induce canonical and non-canonical NLRP3 activation pathways |
| NLRP3 Inhibitors | MCC950, CY-09, OLT1177 (dapansutrile) | Specifically block NLRP3 oligomerization or activity |
| Gene Editing Tools | CRISPR/Cas9 systems, siRNA pools, lentiviral shRNAs | Knock out or knock down specific ion channel or inflammasome genes |
| Antibodies for Detection | Anti-caspase-1 p20, anti-IL-1β p17, anti-NLRP3, anti-ASC | Assess inflammasome activation through immunoblotting, immunofluorescence |
Structural Biology Approaches
Advanced structural techniques provide atomic-level insights into ion channel function and regulation:
Cryo-electron microscopy (cryo-EM): As demonstrated in the structural analysis of BK channels [106], cryo-EM enables visualization of channel conformations in different functional states, revealing mechanisms like the "ball-and-chain" inactivation process.
X-ray crystallography: Has provided structural information for TLR extracellular domains in complex with ligands, revealing conserved recognition mechanisms [33].
Molecular dynamics simulations: As employed by Cui et al. to study lipid regulation of GIRK2 channels [105], MD simulations can model interactions between ion channels, membranes, and signaling lipids at atomic resolution.
Integrated Signaling Pathways
The following diagram illustrates the core signaling pathway connecting PAMP/DAMP recognition to ion channel activation and subsequent NLRP3 inflammasome assembly:
Diagram 1: Integrated pathway of ion channel-mediated inflammasome activation. PAMPs/DAMPs binding to PRRs activates ion channels, leading to ionic fluxes that generate secondary signals which trigger NLRP3 oligomerization and inflammasome assembly, resulting in inflammatory responses.
Methodological Workflow
The following diagram outlines a comprehensive experimental approach for investigating ion channel involvement in inflammasome activation:
Diagram 2: Experimental workflow for studying ion channel-inflammasome connections. The approach combines cell models with PAMP/DAMP stimulation and channel modulation to assess multiple functional readouts.
Therapeutic Implications and Future Directions
Targeting ion channels involved in inflammasome activation presents unique therapeutic opportunities for inflammatory diseases. Several approaches show promise:
Channel-Targeted Therapeutics
TRP channel modulators: Compounds targeting TRPV1, TRPV4, and TRPA1 are in development for pain and inflammation, with potential application in sterile inflammatory conditions [103].
Potassium channel blockers: Specific inhibitors of potassium efflux pathways could provide more targeted alternatives to general potassium depletion for NLRP3 inhibition.
BK channel activators: As precise structural understanding of BK channel regulation advances, including the "ball-and-chain" inactivation mechanism [106], targeted modulators could be developed to fine-tune immune cell excitability.
Integrated Therapeutic Strategies
Combination approaches that target both ion channels and downstream inflammasome components may offer synergistic benefits:
- DAMP neutralization: Monoclonal antibodies against specific DAMPs like HMGB1 and eCIRP can reduce initial trigger for channel activation [70].
- Channel inhibition: Selective channel blockers can prevent ionic fluxes necessary for inflammasome assembly [103].
- Inflammasome inhibition: Direct NLRP3 inhibitors (MCC950) can block final common pathway [104].
Technological Advances
Future research will be accelerated by emerging technologies:
- Advanced delivery systems: Nanoparticles for targeted delivery of channel modulators to specific immune cell populations [39].
- Optogenetics: Light-sensitive channels for precise temporal control of ion fluxes in immune cells.
- Single-cell multi-omics: Simultaneous analysis of ion channel expression, calcium signaling, and inflammatory mediator production in individual cells.
- AI-driven drug discovery: Machine learning approaches to identify novel channel modulators with optimal specificity and safety profiles [39].
Ion channels, particularly TRP channels, serve as critical integration nodes that translate PAMP/DAMP recognition into functional inflammasome responses through coordinated regulation of ionic fluxes. The mechanistic understanding of calcium signaling, potassium efflux, and membrane potential changes in NLRP3 activation provides a refined framework for understanding sterile inflammation. Methodological advances in electrophysiology, live-cell imaging, and structural biology continue to reveal novel aspects of this connection. Therapeutic targeting of specific ion channels involved in inflammasome activation represents a promising approach for numerous inflammatory conditions, with several strategies currently in preclinical development. Future research should focus on cell-type-specific roles of channel-inflammasome connections and temporal regulation of these interactions throughout disease progression.
Comparative Immunology and Translational Validation of PAMP-Induced Pathways
Comparative Analysis of PAMP Recognition Across Pathogen Classes (Viral, Bacterial, Fungal)
The innate immune system serves as the host's first line of defense, employing a sophisticated array of pattern recognition receptors (PRRs) to detect conserved microbial structures known as pathogen-associated molecular patterns (PAMPs) [9] [3]. This recognition initiates critical signaling cascades that trigger inflammatory responses, bridge innate and adaptive immunity, and determine the outcome of host-pathogen interactions [33] [54]. The fundamental importance of PAMP recognition is underscored by its conservation across evolutionary lineages, with PRRs functioning as essential sensors in vertebrates, invertebrates, and plants [107] [49]. The conceptual framework for this recognition system was established by Charles Janeway, who proposed that PRRs detect PAMPs absent in host cells, enabling precise discrimination between self and non-self [9] [33].
This review provides a comprehensive comparative analysis of PAMP recognition mechanisms across three major pathogen classes: viral, bacterial, and fungal. We examine the specialized PRR families involved, their specific PAMP ligands, subcellular localization, and downstream signaling pathways. Additionally, we detail experimental methodologies for studying these interactions and discuss emerging therapeutic implications, providing researchers with both theoretical knowledge and practical tools for advancing this critical field of immunology.
PRR Families and Their General Classification
Pattern recognition receptors are germline-encoded host proteins strategically localized at cell membranes or within cytoplasmic compartments to survey for invading pathogens [9] [54]. They are classified into several major families based on protein domain homology and subcellular localization:
Transmembrane PRRs include Toll-like receptors (TLRs) and C-type lectin receptors (CLRs). TLRs feature leucine-rich repeat (LRR) ectodomains for ligand recognition and intracellular Toll/interleukin-1 receptor (TIR) domains for signal transduction [3] [33]. CLRs possess carbohydrate-recognition domains (CRDs) that primarily bind fungal and mycobacterial carbohydrate components [9] [108].
Cytosolic PRRs encompass NOD-like receptors (NLRs), RIG-I-like receptors (RLRs), AIM2-like receptors (ALRs), and additional sensors such as cyclic GMP-AMP synthase (cGAS) [9] [54]. NLRs characteristically contain nucleotide-binding oligomerization domains (NOD) and LRRs, while RLRs feature DExD/H-box RNA helicase domains for viral RNA detection [3] [54].
A distinct group of inhibitory PRRs (iPRRs), including CD300a and Siglecs, has been identified to prevent immune overactivation by recognizing both endogenous and microbial patterns, ensuring a balanced response to danger signals [9] [33]. This sophisticated receptor network enables the host to mount appropriately tailored immune responses against diverse pathogenic threats.
Viral PAMP Recognition
Key Viral PAMPs and Their Recognition Receptors
Viral infections present distinct molecular signatures primarily comprising nucleic acids that differ from host molecules in structure, modification, or subcellular location [3] [54]. These viral PAMPs are detected by both endosomal and cytoplasmic PRRs, triggering antiviral immune responses characterized by type I interferon production.
Table 1: Principal Viral PAMPs and Their Cognate PRRs
| Viral PAMP | PRR Receptor | PRR Family | Localization | Signaling Adaptor |
|---|---|---|---|---|
| dsRNA | TLR3 | TLR | Endosomal | TRIF |
| ssRNA | TLR7/8 | TLR | Endosomal | MyD88 |
| CpG DNA | TLR9 | TLR | Endosomal | MyD88 |
| dsRNA (short) | RIG-I | RLR | Cytosolic | MAVS |
| dsRNA (long) | MDA5 | RLR | Cytosolic | MAVS |
| dsDNA | cGAS | Cytosolic DNA Sensor | Cytosolic | STING |
| dsDNA | AIM2 | ALR | Cytosolic | ASC |
Viral double-stranded RNA (dsRNA), a replication intermediate for many viruses, is recognized by multiple PRRs. TLR3 localizes to endosomes and detects dsRNA, signaling through the TIR-domain-containing adapter-inducing interferon-β (TRIF) pathway [3] [54]. Cytosolic RIG-I recognizes short dsRNA with 5'-triphosphates, while MDA5 senses longer dsRNA structures [3] [54]. Both RLRs signal through mitochondrial antiviral-signaling protein (MAVS) to induce interferon-stimulated genes.
Viral single-stranded RNA (ssRNA) from viruses like influenza is detected by TLR7 and TLR8 in endosomal compartments, which signal via myeloid differentiation primary response 88 (MyD88) to produce proinflammatory cytokines and type I interferons [3] [7]. Viral DNA is sensed by multiple receptors: TLR9 detects unmethylated CpG DNA in endosomes, while cytosolic DNA is recognized by cGAS, which produces the second messenger cyclic GMP-AMP (cGAMP) to activate STING signaling [9] [54]. AIM2 forms inflammasomes in response to cytosolic DNA, leading to IL-1β maturation and pyroptosis [9] [54].
Signaling Pathways in Antiviral Immunity
Viral PAMP recognition triggers specialized signaling pathways that establish an antiviral state in infected and neighboring cells. The diagram below illustrates key antiviral signaling pathways initiated by viral nucleic acid detection:
Figure 1: Antiviral signaling pathways triggered by viral PAMP recognition. Viral nucleic acids are detected by endosomal TLRs and cytosolic sensors, activating transcription factors that induce interferon and inflammatory cytokine production.
The cGAS-STING pathway represents a crucial cytoplasmic DNA sensing mechanism. Upon binding double-stranded DNA, cGAS synthesizes (2',3')-cGAMP, which binds to STING on the endoplasmic reticulum [9] [54]. Activated STING traffics to the Golgi apparatus, recruiting TANK-binding kinase 1 (TBK1) that phosphorylates interferon regulatory factor 3 (IRF3). Phosphorylated IRF3 dimerizes and translocates to the nucleus to induce type I interferon gene expression [54].
RLR signaling demonstrates remarkable specificity in antiviral responses. RIG-I preferentially recognizes short dsRNA with (5')-triphosphate groups, characteristic of many negative-strand RNA viruses, while MDA5 detects long dsRNA structures produced during picornavirus replication [3] [54]. Both receptors activate MAVS on mitochondrial membranes, leading to NF-κB and IRF3 activation and subsequent production of proinflammatory cytokines and type I interferons [54].
Bacterial PAMP Recognition
Key Bacterial PAMPs and Their Recognition Receptors
Bacteria present diverse PAMPs derived from their cell wall components, membrane structures, and nucleic acids. These conserved microbial signatures are recognized by multiple PRR families, initiating immune responses tailored to control bacterial infections.
Table 2: Principal Bacterial PAMPs and Their Cognate PRRs
| Bacterial PAMP | PRR Receptor | PRR Family | Localization | Pathogen Examples |
|---|---|---|---|---|
| Lipopolysaccharide (LPS) | TLR4 | TLR | Cell Surface | Gram-negative bacteria |
| Lipoteichoic Acid (LTA) | TLR2 | TLR | Cell Surface | Gram-positive bacteria |
| Peptidoglycan | NOD1/NOD2 | NLR | Cytosolic | Most bacteria |
| Flagellin | TLR5 | TLR | Cell Surface | Flagellated bacteria |
| Lipopeptides | TLR2/1, TLR2/6 | TLR | Cell Surface | Various bacteria |
| CpG DNA | TLR9 | TLR | Endosomal | Various bacteria |
| Unmethylated DNA | cGAS | Cytosolic DNA Sensor | Cytosolic | Intracellular bacteria |
Lipopolysaccharide (LPS), a major component of Gram-negative bacterial outer membranes, is recognized by the TLR4-MD2 complex on the cell surface [3] [54]. CD14 facilitates LPS shuttling to the TLR4-MD2 complex, where ligand engagement induces receptor dimerization and downstream signaling [54]. Lipoteichoic acid (LTA) from Gram-positive bacteria is detected by TLR2, which forms heterodimers with TLR1 or TLR6 to recognize diverse lipid structures [3] [54].
Peptidoglycan, a essential component of most bacterial cell walls, is sensed intracellularly by NOD1 and NOD2 [108] [54]. NOD1 recognizes meso-diaminopimelic acid-containing peptides from primarily Gram-negative bacteria, while NOD2 detects muramyl dipeptide present in both Gram-positive and Gram-negative species [54]. Flagellin, the subunit protein of bacterial flagella, is recognized by TLR5 on cell surfaces [3] [54]. Bacterial CpG DNA is detected by TLR9 in endosomal compartments, while cytosolic bacterial DNA activates the cGAS-STING pathway [9] [54].
Signaling Pathways in Antibacterial Immunity
Bacterial PAMP recognition initiates signaling cascades that coordinate inflammatory responses critical for bacterial clearance. The primary pathways include MyD88-dependent signaling for most TLRs and NOD-mediated NF-κB activation.
TLR4 signaling demonstrates remarkable complexity, engaging both MyD88-dependent and TRIF-dependent pathways [3] [54]. LPS binding induces TLR4 dimerization and TIR domain conformational changes, recruiting TIRAP and MyD88 to the plasma membrane. MyD88 then recruits IL-1 receptor-associated kinases (IRAK1/4), leading to TRAF6 activation and subsequent TAK1 activation. TAK1 phosphorylates IκB kinase (IKK) complex and MAPK pathways, resulting in NF-κB and AP-1 translocation to the nucleus and proinflammatory gene expression [54]. Following endocytosis, TLR4 engages TRAM and TRIF adaptors, activating TBK1 and IRF3 to induce type I interferon production [54].
NOD1/2 signaling represents a key cytosolic bacterial sensing mechanism. Upon peptidoglycan recognition, NOD proteins oligomerize and recruit receptor-interacting protein kinase 2 (RIPK2) through CARD-CARD interactions [54]. RIPK2 undergoes ubiquitination, activating TAK1 and IKK complexes, ultimately leading to NF-κB activation and inflammatory cytokine production [54]. Additionally, NOD signaling can activate MAPK pathways, further amplifying inflammatory responses.
Certain intracellular bacteria can activate inflammasome complexes. For example, bacterial flagellin that accesses the cytosol can activate NLRC4 inflammasomes, while pore-forming toxins can activate NLRP3 inflammasomes, leading to caspase-1 activation, IL-1β/IL-18 maturation, and pyroptotic cell death to eliminate the replication niche [54].
Fungal PAMP Recognition
Key Fungal PAMPs and Their Recognition Receptors
Fungal pathogens present unique carbohydrate-rich cell wall components that serve as PAMPs, recognized primarily by TLRs and CLRs to initiate protective immune responses.
Table 3: Principal Fungal PAMPs and Their Cognate PRRs
| Fungal PAMP | PRR Receptor | PRR Family | Localization | Ligand Specificity |
|---|---|---|---|---|
| Zymosan | TLR2/6 | TLR | Cell Surface | β-glucans, mannans |
| β-glucans | Dectin-1 | CLR | Cell Surface | β-1,3/β-1,6-glucans |
| Mannans | Dectin-2 | CLR | Cell Surface | α-mannans, hyphae |
| Chitin | TLR2 | TLR | Cell Surface | Chitin fragments |
| Chitin | NOD2 | NLR | Cytosolic | Chitin fragments |
| Unknown | MINCLE | CLR | Cell Surface | Malassezia, C. albicans |
Zymosan, a component from fungal cell walls, contains β-glucans and mannans recognized by TLR2/TLR6 heterodimers [108] [3]. β-glucans, major structural components of fungal cell walls, are specifically recognized by Dectin-1, a CLR that signals through an immunoreceptor tyrosine-based activation motif (ITAM)-like domain [108] [3]. Dectin-1 collaborates with TLR2 to enhance proinflammatory responses to fungi.
Mannans and hyphal forms of fungi are detected by Dectin-2, which associates with the FcRγ chain for signaling [108]. Chitin, a polymer of N-acetylglucosamine in fungal cell walls, is recognized by TLR2 on the cell surface and potentially by NOD2 in the cytosol [108]. The CLR MINCLE recognizes Malassezia species and Candida albicans, though its specific fungal ligand remains incompletely characterized [9].
Signaling Pathways in Antifungal Immunity
Fungal PAMP recognition engages specialized signaling networks that coordinate immune responses critical for fungal clearance, particularly important for phagocytosis and Th17 responses.
Dectin-1 signaling represents a paradigm for CLR-mediated antifungal immunity. Upon β-glucan binding, Dectin-1 phosphorylates its hemITAM motif, recruiting spleen tyrosine kinase (SYK) [108]. SYK then activates CARD9-BCL10-MALT1 complex, leading to NF-κB activation and expression of proinflammatory cytokines including IL-1β, IL-6, and IL-23 [108]. Additionally, Dectin-1 signaling can activate NLRP3 inflammasomes through SYK and reactive oxygen species production, leading to IL-1β maturation [108].
Collaborative signaling between CLRs and TLRs enhances antifungal immunity. Dectin-1 synergizes with TLR2 to amplify NF-κB activation and cytokine production [108]. This cooperation is essential for mounting effective Th17 responses, which recruit neutrophils and promote barrier immunity at mucosal surfaces. Fungal chitin recognition involves multiple PRRs; smaller chitin fragments activate TLR2 on macrophages, while larger fragments potentially access the cytosol for NOD2 recognition [108].
The following diagram illustrates the integrated signaling network in antifungal immunity:
Figure 2: Integrated signaling network in antifungal immunity. Fungal PAMPs are recognized by CLRs and TLRs that coordinate phagocytosis, inflammasome activation, and Th17 differentiation through collaborative signaling.
Experimental Methodologies for PAMP-PRR Research
Key Experimental Approaches
Investigating PAMP-PRR interactions requires multidisciplinary approaches spanning molecular biology, immunology, and biochemistry. Well-established methodologies enable researchers to characterize these critical immune recognition events.
Ligand Binding Assays utilizing surface plasmon resonance (SPR) and isothermal titration calorimetry (ITC) provide quantitative data on binding affinity and kinetics [3]. SPR measures real-time interactions between purified PRR ectodomains and PAMP ligands immobilized on sensor chips, determining association ((k{on})) and dissociation ((k{off})) rate constants and calculating equilibrium dissociation constants ((K_D)) [3]. ITC directly measures heat changes during binding interactions, providing thermodynamic parameters including enthalpy (ΔH), entropy (ΔS), and binding stoichiometry.
Cellular Activation Assays employ PRR-specific agonists and knockout models to elucidate receptor function. Commonly used PAMPs include ultrapure LPS (TLR4 agonist), Pam3CSK4 (TLR1/2 agonist), poly(I:C) (TLR3 agonist), R848 (TLR7/8 agonist), CpG ODN (TLR9 agonist), MDP (NOD2 agonist), and curdlan (Dectin-1 agonist) [108] [3]. Immortalized macrophage cell lines with specific PRR deficiencies (e.g., HEK293T cells lacking endogenous TLRs) or primary cells from knockout mice enable specific pathway analysis.
Signal Transduction Analysis investigates downstream signaling events through western blotting for phosphorylation of key signaling molecules (IKKα/β, p65, p38, JNK, ERK, TBK1, IRF3), electrophoretic mobility shift assays (EMSA) for NF-κB DNA binding, and luciferase reporter assays for NF-κB, AP-1, and IRF activation [3] [54]. Immunofluorescence and confocal microscopy track subcellular translocation of transcription factors and adaptor proteins.
Advanced Methodologies
Structural Biology approaches including X-ray crystallography and cryo-electron microscopy have revealed atomic-level details of PRR-PAMP complexes [3] [33]. Crystal structures of TLR ectodomains with their ligands show characteristic M-shaped architectures with ligand binding at the convex surface [3] [33]. The horseshoe-shaped LRR domains facilitate PAMP recognition through conserved "LxxLxLxxN" motifs [3] [33].
Genetic and Genomic Techniques include CRISPR-Cas9 mediated gene editing for precise PRR manipulation, single-cell RNA sequencing to identify cell-type-specific PRR expression patterns, and chromatin immunoprecipitation sequencing (ChIP-seq) to map transcription factor binding and epigenetic modifications in trained immunity [109] [49].
Table 4: Research Reagent Solutions for PAMP-PRR Studies
| Research Reagent | Specific Target/Function | Experimental Application | Key References |
|---|---|---|---|
| Ultrapure LPS | TLR4 signaling | Gram-negative bacterial recognition | [3] [54] |
| Pam3CSK4 | TLR1/TLR2 heterodimer | Bacterial lipopeptide recognition | [3] |
| Poly(I:C) | TLR3 and RIG-I/MDA5 | Viral dsRNA recognition | [3] [7] |
| R848 | TLR7/TLR8 | Viral ssRNA recognition | [3] [7] |
| Curdlan | Dectin-1 | Fungal β-glucan recognition | [108] |
| MDP | NOD2 | Bacterial peptidoglycan recognition | [54] |
| cGAMP | STING | Cytosolic DNA sensing pathway | [9] [54] |
| MCC950 | NLRP3 inhibitor | Inflammasome regulation | [7] |
Therapeutic Implications and Future Perspectives
The therapeutic targeting of PAMP-PRR interactions represents a promising frontier in immunology, with applications in infectious diseases, cancer, and autoimmune disorders [33] [49]. Several strategies are currently under investigation:
PRR Agonists as Vaccine Adjuvants leverage the ability of PRR ligands to enhance adaptive immunity. Monophosphoryl lipid A (MPL), a detoxified TLR4 agonist derived from Salmonella LPS, is incorporated in FDA-approved vaccines including Cervarix and Fendrix [33]. Similarly, CpG ODN (TLR9 agonist) is used in hepatitis B vaccines and cancer immunotherapies to promote Th1 responses [33].
PRR Antagonists for Inflammatory Diseases aim to dampen excessive inflammation driven by aberrant PRR signaling. TAK-242 (resatorvid) inhibits TLR4 signaling by binding to its TIR domain and has shown promise in clinical trials for sepsis and rheumatoid arthritis [33]. NLRP3 inflammasome inhibitors including MCC950 and CY-09 are in development for gout, Alzheimer's disease, and other sterile inflammatory conditions [7].
Trained Immunity Modulation represents a novel therapeutic concept wherein innate immune memory is harnessed for protection or suppressed in chronic inflammation [109] [49]. BCG vaccination induces trained immunity that provides heterologous protection against unrelated pathogens, while β-glucan training enhances antifungal and antitumor responses [109] [49]. Conversely, reversing maladaptive trained immunity may benefit autoimmune and inflammatory diseases including atherosclerosis, systemic lupus erythematosus, and Alzheimer's disease [109] [49].
Future research directions should focus on understanding PRR collaboration in complex infections, wherein multiple PAMPs activate distinct PRRs that interact to shape integrated immune responses [54]. The emerging concept of PANoptosis, a coordinated inflammatory cell death pathway initiated by ZBP1 and other sensors during influenza infection, exemplifies this complexity [54]. Additionally, tissue-specific PRR regulation and the impact of host microbiota on tonic PRR signaling represent critical areas for further investigation [33] [49].
This comparative analysis elucidates the sophisticated specialization of PAMP recognition systems across viral, bacterial, and fungal pathogen classes. While all PRRs ultimately activate common inflammatory signaling modules including NF-κB and IRF transcription factors, their specific ligands, subcellular localization, and adaptor usage enable tailored immune responses appropriate to each pathogen type. Viral recognition focuses predominantly on nucleic acid sensors, bacterial detection emphasizes membrane component recognition, and antifungal immunity relies heavily on carbohydrate-sensing CLRs.
The experimental methodologies outlined provide researchers with robust tools for further investigating these critical immune interactions, while the therapeutic perspectives highlight the translational potential of modulating PAMP-PRR pathways. As our understanding of these systems continues to evolve, particularly regarding PRR cross-talk, tissue-specific regulation, and innate immune memory, new opportunities will emerge for precisely manipulating these pathways to combat infectious diseases, fine-tune inflammatory responses, and develop novel immunotherapeutic strategies.
This technical guide provides a comprehensive framework for drug target validation, with a specific focus on targets within pathogen-associated molecular pattern (PAMP) signaling pathways and inflammation initiation. We present a systematic approach spanning from initial genetic evidence to clinical confirmation, emphasizing the critical decision points that determine therapeutic success. The methodologies and strategies outlined herein are designed to assist researchers and drug development professionals in building robust validation workflows that can withstand the high attrition rates characteristic of contemporary drug development. Special emphasis is placed on integrating human genetic evidence with functional validation in advanced model systems to de-risk the translation from preclinical findings to clinical applications, particularly in the context of innate immune signaling and inflammatory diseases.
The validation of drug targets in the context of PAMP-driven inflammation presents unique challenges and opportunities for therapeutic development. Pathogen-associated molecular patterns (PAMPs) are conserved molecular signatures derived from microorganisms that are recognized by pattern recognition receptors (PRRs) of the innate immune system, initiating signaling cascades that trigger inflammatory responses [7]. While essential for host defense, dysregulated PAMP signaling contributes to the pathogenesis of numerous autoimmune, chronic inflammatory, and infectious diseases. The recent emergence of trained immunity concepts—where innate immune cells develop memory-like properties through epigenetic and metabolic reprogramming following PAMP exposure—further complicates the therapeutic landscape [26]. This phenomenon demonstrates that innate immune cells can exhibit enhanced responsiveness to subsequent challenges, which may be beneficial for host defense but detrimental in chronic inflammatory conditions.
Target validation in this space requires specialized approaches that account for the complex interplay between PAMPs, damage-associated molecular patterns (DAMPs), and the resulting inflammatory cascades. The convergence of PAMP and DAMP signaling creates a particularly challenging environment for therapeutic intervention, as these pathways often synergize to drive pathology [25] [7]. Furthermore, the liver presents a unique case study in PAMP recognition, as it must distinguish between potentially dangerous signals and the constant stream of non-pathogenic microbial products from the intestine, representing a significant challenge in distinguishing signal from noise [97]. This guide systematically addresses these challenges through a structured validation approach that leverages genetic insights, advanced model systems, and strategic clinical translation.
Genetic Validation Approaches
Human Genetic Evidence and Direction of Effect
Human genetic evidence has emerged as a cornerstone of effective target validation, with genetically supported targets demonstrating a 2.6-fold increase in drug development success rates [110]. The integration of genetic data across the allele frequency spectrum—from common to rare variants—enables the construction of allelic series that model dose-response relationships critical for determining the correct direction of therapeutic effect. For PAMP signaling pathways, this is particularly important, as both excessive and deficient inflammatory responses can be pathological.
Key considerations for genetic validation include:
- Variant Interpretation: Loss-of-function (LOF) variants in PAMP sensors or signaling components typically confer increased susceptibility to infections but may protect against autoimmune pathology, while gain-of-function (GOF) variants often drive autoinflammatory diseases.
- Direction of Effect (DOE) Prediction: Advanced frameworks now predict DOE-specific druggability using gene and protein embeddings combined with genetic associations, achieving macro-averaged AUROCs of 0.95 for activator and inhibitor mechanisms [110].
- Pleiotropy Assessment: Genes in PAMP pathways frequently exhibit pleiotropic effects, necessitating careful evaluation of potential on-target toxicities before therapeutic development.
Table 1: Genetic Evidence Types for Target Validation
| Evidence Type | Application to PAMP Pathways | Strengths | Limitations |
|---|---|---|---|
| Common Variant Associations (GWAS) | Identifies regulators of inflammatory response intensity | High statistical power; natural randomization | Small effect sizes; polygenic architecture |
| Rare Loss-of-Function Variants | Establishes non-redundant pathway components | Large effect sizes; clear mechanistic interpretation | Limited carrier numbers; possible embryonic lethality |
| Gain-of-Function Mutations | Validates targets for inhibitory therapeutics | Strong support for inhibitor development; often monogenic | May represent extreme phenotypes not generalizable |
| Copy Number Variations | Informs on gene dosage sensitivity | Models gene amplification/deletion effects | Technical challenges in detection and interpretation |
Genetic Knockout Models: From Murine to Humanized Systems
Genetic knockout models remain fundamental for establishing causal relationships between target modulation and phenotypic outcomes. For PAMP pathway validation, specialized models must account for species-specific differences in innate immune recognition.
Experimental Protocol: Generation and Validation of PRR Knockout Models
- Model Selection: Choose appropriate model organisms based on pathway conservation. Murine models are preferred for initial validation due to tractability, but critical pathway differences must be considered.
- Genetic Engineering: Utilize CRISPR-Cas9 for precise gene editing of pattern recognition receptors (TLRs, NLRs, RLRs) and downstream signaling components.
- Phenotypic Characterization: Challenge knockout models with specific PAMPs (LPS, flagellin, viral RNA) and pathogens to establish:
- Inflammatory cytokine production (ELISA, multiplex arrays)
- Immune cell recruitment (flow cytometry)
- Pathogen clearance (colony forming unit assays, viral load)
- End-organ damage (histopathology, serum biomarkers)
- Humanized Model Validation: Reconstitute immunodeficient mice with human hematopoietic cells or transgenic human PRRs to confirm relevance to human biology [111].
Interpretation Guidelines:
- Complete protection from PAMP-driven pathology suggests strong target validation but may indicate unacceptable infection risk.
- Partial reduction in inflammation with preserved host defense represents an ideal therapeutic profile.
- Tissue-specific effects should be carefully evaluated, as PAMP signaling has organ-specific consequences (e.g., liver vs. lung) [97].
Preclinical Functional Validation
Advanced In Vitro Model Systems
Traditional two-dimensional cell cultures poorly recapitulate the complexity of PAMP-driven inflammatory responses. Advanced in vitro systems now enable more physiologically relevant target validation.
Table 2: Advanced Model Systems for PAMP Pathway Validation
| Model System | Key Applications | Relevance to PAMP Research | Technical Considerations |
|---|---|---|---|
| Organ-on-a-Chip | Gut-liver axis for oral PAMP exposure; blood-brain barrier for neuroinflammation | Models tissue barriers and multicellular crosstalk | Requires specialized microfluidic equipment; parameter optimization complex |
| 3D Organoid Cultures | Intestinal, pulmonary, and hepatic organoids for tissue-specific responses | Maintains tissue-specific cell types and architecture | Variable maturity; immune component often lacking |
| Primary Immune Cell Cocultures | Myeloid-lymphoid interactions in trained immunity | Captures human-specific responses without species differences | Donor-to-donor variability; limited lifespan |
| Induced Pluripotent Stem Cell (iPSC)-Derived Models | Patient-specific genetic backgrounds; disease modeling | Enables incorporation of human genetic variants | Differentiation efficiency; fetal-like phenotype |
Experimental Protocol: Gut-Liver Axis-on-a-Chip for PAMP Exposure
- System Fabrication: Utilize microfluidic devices with separate but interconnected chambers for gut epithelium (Caco-2 cells or primary enteroids) and hepatic tissue (HepG2/HepaRG cells or primary hepatocytes).
- Condition Optimization: Establish physiological flow rates, shear stress, and media composition that maintain both tissue types.
- PAMP Exposure: Introduce purified PAMPs (LPS, peptidoglycan) or bacterial metabolites to the gut compartment.
- Response Monitoring: Measure:
- Transepithelial electrical resistance (gut barrier integrity)
- Inflammatory mediators (multiplex cytokine analysis)
- Metabolic competence (hepatic albumin/urea production)
- Transcriptomic/epigenetic changes (RNA-seq, ATAC-seq)
- Therapeutic Testing: Assess target modulation using specific inhibitors/activators with monitoring of both efficacy and potential toxicity [111].
Assessing Target Engagement and Pathway Modulation
Confirming that a therapeutic candidate engages its intended target and produces the desired downstream pharmacological effect is critical for validation.
Experimental Protocol: Target Engagement Assessment in PAMP Signaling
- Cellular System Selection: Use primary human macrophages or dendritic cells, as these are central to PAMP recognition and response.
- Stimulus Optimization: Establish PAMP exposure conditions that yield submaximal pathway activation (typically 10-100 ng/mL LPS for TLR4 signaling).
- Engagement Measurement:
- Biophysical Methods: SPR, ITC for binding affinity determination
- Cellular Binding: NanoBRET, FRET-based assays in live cells
- Pharmacodynamic Readouts: Phospho-specific flow cytometry, Western blot for signaling intermediates (IKKα/β, IRAK, p38 MAPK)
- Functional Consequences:
- NF-κB and IRF nuclear translocation (imaging flow cytometry)
- Inflammasome assembly (ASC speck formation)
- Pro-inflammatory cytokine secretion (IL-1β, IL-6, TNF-α)
- Trained immunity markers (H3K4me3, H3K27ac) [26]
Validation Criteria:
- Concentration-dependent target engagement should correlate with functional effects
- Engagement should be specific versus related targets (e.g., selective TLR4 inhibition versus other TLRs)
- Engagement should block downstream signaling nodes within the pathway
The Experimental Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for PAMP Pathway Target Validation
| Reagent Category | Specific Examples | Research Applications | Technical Notes |
|---|---|---|---|
| Recombinant PAMPs | Ultrapure LPS (TLR4 ligand), Pam3CSK4 (TLR1/2), Poly(I:C) (TLR3) | Pathway-specific stimulation; positive controls | Verify purity and absence of contaminants |
| PRR-Specific Agonists | CL097 (TLR7/8), Flagellin (TLR5), ODN2006 (TLR9) | Selective pathway activation; mechanism of action studies | Concentration optimization critical |
| PRR Inhibitors | TAK-242 (TLR4), CU-CPT9a (TLR8), ODN TTAGGG (TLR9 antagonist) | Target validation; pathway dissection | Assess selectivity across PRR family |
| Pathway Reporter Systems | NF-κB, IRF, AP-1 luciferase reporters; TRE-Luc systems | High-throughput screening; mechanism confirmation | Combine with endogenous readouts |
| Cytokine Detection Assays | Multiplex Luminex, ELISA, ELISpot | Inflammatory response quantification | Measure both pro- and anti-inflammatory mediators |
| Epigenetic Tools | H3K4me3, H3K27ac ChIP-grade antibodies; BET bromodomain inhibitors | Trained immunity assessment [26] | Consider temporal dynamics of modifications |
| Neutralizing Antibodies | Anti-TLR4, Anti-MyD88, Anti-TRIF | Pathway blockade; target validation | Species cross-reactivity verification |
Bridging to Clinical Validation
Preclinical to Clinical Translation Framework
The transition from preclinical target validation to clinical confirmation requires strategic planning and assessment of translatable biomarkers. The GOT-IT framework provides systematic recommendations for this transition, emphasizing timely focus on target-related safety issues, druggability, and potential for therapeutic differentiation [112].
Key Translational Considerations for PAMP-Targeted Therapeutics:
- Biomarker Strategy: Develop pharmacodynamic biomarkers that directly measure target engagement and pathway modulation in accessible human tissues (e.g., whole blood cytokine release, PBMC phospho-signaling, transcriptomic signatures).
- Safety Assessment: PAMP pathway modulation carries inherent infection risks, requiring specialized safety pharmacology assessing:
- Controlled infection models (e.g., Listeria challenge)
- Vaccine response evaluation
- Microbiome impact assessment
- Clinical Trial Design: Incorporate:
- Human endotoxin challenge models for early proof-of-concept
- Patient selection based on genetic or biomarker evidence of pathway hyperactivation
- Adaptive designs for dose optimization
Clinical Validation Milestones
Clinical validation progresses through sequential evidence generation, with each phase addressing distinct validation questions:
Phase 1:
- Establish target engagement in humans using biomarkers developed in preclinical models
- Define pharmacokinetic/pharmacodynamic relationships
- Identify preliminary safety signals related to pathway modulation
Phase 2:
- Demonstrate pathway-specific modulation in disease-relevant tissues
- Establish clinical proof-of-concept in selected patient populations
- Validate biomarker-stratified enrichment strategies
Phase 3:
- Confirm efficacy in broader populations
- Establish definitive benefit-risk profile
- Identify potential biomarkers for companion diagnostics
Recent clinical trials in related inflammatory pathways illustrate these principles. For example, BTK inhibitors like fenebrutinib represent a newer generation of drugs designed to reach the brain and target autoimmune diseases such as multiple sclerosis, with Phase 3 trials (FENhance 1/2, FENtrepid) currently evaluating their efficacy [113]. Similarly, amlitelimab, an OX40L-blocking antibody, is in advanced trials for multiple inflammatory conditions, with efficacy readouts expected to provide important validation for this approach [113].
Signaling Pathways and Experimental Workflows
PAMP Recognition and Signaling Cascade
The following diagram illustrates key signaling pathways in PAMP recognition and their connections to inflammatory responses, highlighting potential therapeutic intervention points:
Integrated Target Validation Workflow
The validation of drug targets in PAMP pathways requires a systematic, multi-stage approach as depicted in the following workflow:
The validation of drug targets in PAMP-driven inflammatory pathways requires increasingly sophisticated approaches that integrate human genetic evidence with advanced model systems and strategic clinical trial design. The framework presented in this guide emphasizes the critical importance of establishing direction of effect early, utilizing physiologically relevant model systems, and developing translatable biomarkers that can bridge the preclinical-clinical divide. As our understanding of innate immune memory and trained immunity evolves [26], new therapeutic opportunities and challenges will emerge, particularly in distinguishing beneficial from maladaptive inflammatory responses. The successful translation of PAMP pathway therapeutics will depend on rigorous application of these validation principles, with careful attention to the balance between anti-inflammatory efficacy and preservation of host defense mechanisms. Future directions will likely include increased use of humanized models, multi-omics integration for patient stratification, and adaptive clinical trial designs that can efficiently test therapeutic hypotheses in appropriately selected populations.
Pattern recognition receptors (PRRs) form the cornerstone of the innate immune system, providing a rapid, first line of defense against pathogenic invasion. This whitepaper synthesizes current research on the remarkable evolutionary conservation of PRR pathways from invertebrates to mammals. It details the structural and functional homology of major PRR families, including Toll-like receptors (TLRs) and C-type lectin receptors (CLRs), and their shared signaling cascades. Within the context of pathogen-associated molecular patterns (PAMPs) and inflammation initiation, we discuss how cross-kingdom analyses of organisms—from Drosophila and zebrafish to humans—reveal both conserved and diverged mechanistic strategies for pathogen sensing. The document provides a comprehensive technical guide, including summarized quantitative data, experimental protocols for key cross-species assays, and essential research reagents. Finally, we explore the implications of these conserved pathways for therapeutic intervention in inflammatory and immune-related diseases.
The innate immune system represents an ancient and evolutionarily conserved defense network found in all multicellular organisms. Its strategic importance lies in its role as the initial sensor of infection and tissue damage, critically shaping subsequent inflammatory responses. Central to this system are pattern recognition receptors (PRRs), germline-encoded host proteins that detect invariant molecular signatures known as pathogen-associated molecular patterns (PAMPs) and damage-associated molecular patterns (DAMPs) [9] [3]. The foundational hypothesis of PRR function, proposed by Charles Janeway, posited that these receptors provide the essential "second signal" required to activate adaptive immunity in vertebrates, thereby bridging innate and adaptive immune responses [9] [3].
Research over the past three decades has confirmed that PRRs and their core signaling pathways are extensively conserved across a wide evolutionary spectrum, from plants and invertebrates to mammals [114] [115]. This conservation underscores the fundamental efficacy of this immune strategy. For instance, cell surface PRRs include TLRs and CLRs, while cytosolic PRRs encompass NOD-like receptors (NLRs), RIG-I-like receptors (RLRs), AIM2-like receptors (ALRs), and sensors like cGAS [9] [3]. The deep homology of these systems provides a powerful framework for using model organisms to dissect the intricacies of human immune responses and inflammation initiation. This review delves into the molecular architecture, functional conservation, and experimental analysis of these critical pathways, providing a resource for researchers and drug development professionals working at the intersection of immunology and inflammation.
Evolutionary Conservation of Major PRR Families
The conservation of PRR families is not merely structural but also functional, with homologous receptors often recognizing similar PAMPs and activating analogous inflammatory pathways in diverse species.
Toll-like Receptors (TLRs)
TLRs are one of the most extensively studied and evolutionarily conserved PRR families. They are type I transmembrane glycoproteins characterized by an extracellular leucine-rich repeat (LRR) domain for ligand recognition and an intracellular Toll/IL-1 receptor (TIR) domain for signal transduction [3]. The discovery of Toll in Drosophila and its role in antifungal defense provided the first evidence of the conservation of this pathway [3]. Humans possess 10 functional TLRs (TLR1-TLR10), while mice have 12 (TLR1-TLR9, TLR11-TLR13) [3]. Their cellular localization dictates ligand specificity; surface TLRs (e.g., TLR1, 2, 4, 5, 6) primarily recognize microbial membrane components like lipids and proteins, whereas endosomal TLRs (e.g., TLR3, 7, 8, 9) detect nucleic acids [3]. The TIR domain recruits adaptor proteins such as MyD88, initiating signaling cascades that lead to the activation of NF-κB and the production of pro-inflammatory cytokines, a process conserved from flies to humans [114] [3].
C-type Lectin Receptors (CLRs)
CLRs are a large family of receptors that recognize carbohydrate-based PAMPs, particularly those found in fungal cell walls, such as β-glucan and mannans [115]. A prime example of functional conservation is Dectin-1, a key CLR for β-glucan recognition. In mammals, Dectin-1 signals through the Syk/Card9 pathway to activate NF-κB and drive pro-inflammatory gene expression, which is crucial for antifungal immunity [115]. Although zebrafish lack a direct sequence ortholog of Dectin-1, they possess putative CLRs (Sclra and Clec4c) in a genomic region with partial synteny to the human and mouse Dectin-1 locus. Functional studies confirm that these receptors, along with Tlr2, are involved in the response to zymosan (a fungal particle rich in β-glucan), demonstrating that the innate immune function of fungal PAMP sensing is conserved, even if the specific receptor genes have diverged [115].
Cytosolic PRRs: NLRs, RLRs, and Beyond
Cytosolic PRRs surveil the intracellular environment for signs of infection. The NLR family, which includes nucleotide-binding oligomerization domain (NOD) receptors, is conserved between plants and animals. In plants, NLRs (often called NBS-LRRs) confer strain-specific resistance to pathogens [114]. In mammals, NLRs like NOD1 and NOD2 sense bacterial peptidoglycan fragments and signal through RIP2 kinase to activate NF-κB, a pathway that also involves the IRAK family kinase IRAK1 [114]. Similarly, RLRs (RIG-I, MDA5) are conserved cytosolic sensors of viral RNA that activate antiviral interferon responses across vertebrate species [3].
Table 1: Conservation of Major PRR Families Across Species
| PRR Family | Key Ligands (PAMPs) | Representative Receptors | Conservation Highlights |
|---|---|---|---|
| Toll-like Receptors (TLRs) | LPS (TLR4), Lipoproteins (TLR1/2/6), Viral RNA (TLR3/7/8), Bacterial DNA (TLR9) | TLR1-TLR10 (Human), TLR1-TLR9, TLR11-TLR13 (Mouse), Toll (Drosophila) | TIR domain signaling conserved; Drosophila Toll functions in antifungal defense. |
| C-type Lectin Receptors (CLRs) | β-glucan, Mannans, Chitin | Dectin-1 (Human/Mouse), Sclra, Clec4c (Zebrafish) | Functional conservation of β-glucan sensing and Syk/Card9 signaling. |
| NOD-like Receptors (NLRs) | Bacterial peptidoglycan, Danger signals | NOD1, NOD2 (Mammals), NBS-LRRs (Plants) | Plant NLRs indirectly detect pathogen effectors; mammalian NLRs like NOD1/2 signal via RIP2. |
| RIG-I-like Receptors (RLRs) | Viral dsRNA | RIG-I, MDA5 (Mammals and other vertebrates) | Conserved role in antiviral interferon response. |
Molecular Mechanisms of PRR Signaling
The activation of PRRs triggers a limited number of highly conserved intracellular signaling cascades that culminate in the initiation of inflammation.
The Central Role of Non-RD Kinases in PRR Signaling
A striking feature of PRR-associated kinases is their enrichment in the non-RD kinase class. Kinases are classified as RD or non-RD based on the presence or absence of a conserved arginine (R) immediately preceding the catalytic aspartate (D) in subdomain VI. RD kinases are typically regulated by activation loop phosphorylation, whereas many non-RD kinases are constitutively active or regulated by alternative mechanisms [114]. A genomic survey of human, fly, worm, Arabidopsis, and rice kinomes revealed that while non-RD kinases make up only 9-29% of all kinases, 12 out of 15 kinases known or predicted to function in PRR signaling are non-RD [114]. This includes human IRAKs, Drosophila Pelle, and the plant receptor kinases XA21 and FLS2. This suggests that non-RD kinases may have evolved unique regulatory properties suited to the demands of front-line pathogen defense, such as resilience against pathogen-encoded inhibitors [114].
Conserved Downstream Signaling Pathways
Despite the diversity of PRRs, their signaling converges on a few key effector pathways. The transcription factor NF-κB is a master regulator of inflammation and is activated by multiple PRR families. In the canonical TLR pathway, ligand binding recruits adaptors like MyD88, leading to the formation of a complex with IRAK family kinases and ultimately activating NF-κB and MAPK to induce pro-inflammatory cytokines like TNF and IL-6 [3]. This pathway is functionally conserved in zebrafish, where macrophages and neutrophils respond to zymosan by activating NF-κB and inducing the homolog of the key chemokine CXCL8 [115]. The CLR pathway, exemplified by Dectin-1, signals through the kinase Syk and the adaptor Card9 to also activate NF-κB. The Card9 pathway is similarly conserved, as demonstrated by the impaired neutrophil recruitment in card9 mutant zebrafish [115].
The diagram below illustrates the core conserved signaling pathways triggered by TLRs and CLRs, leading to NF-κB activation and inflammatory responses.
Cross-Species Experimental Approaches and Protocols
Leveraging cross-species comparisons requires robust experimental models and methodologies. The following section outlines key protocols and tools for investigating conserved PRR pathways.
Key Experimental Model Organisms
- Zebrafish (Danio rerio): Larval zebrafish are a powerful model because their adaptive immune system does not mature until about 4 weeks post-fertilization. This allows for the isolated study of innate immunity in an intact vertebrate [115]. They are transparent, enabling live imaging of immune cell behaviors, and are amenable to genetic manipulation.
- Drosophila (Drosophila melanogaster): The discovery of the role of Toll in antifungal defense in Drosophila established it as a foundational model for innate immunity [3]. Its powerful genetic tools continue to provide insights into conserved immune pathways.
- Comparative Genomics and Single-Cell RNA-Seq: Cross-species single-cell transcriptome sequencing (scRNA-seq) of peripheral blood mononuclear cells (PBMCs) from 12 vertebrate species (from fish to mammals) has identified universally conserved genes characterizing immune cells and revealed that monocytes maintain a conserved transcriptional program [116]. This approach overcomes the limitations of antibody-based cell identification across species.
Detailed Methodology: Zebrafish Larval Hindbrain Injection and Immune Response Assay
This protocol, adapted from [115], is used to assess the innate immune response to fungal PAMPs in larval zebrafish.
1. Preparation:
- Zebrafish Larvae: Use 2 days post-fertilization (dpf) wild-type or transgenic larvae. Useful transgenic lines include those with fluorescently labeled macrophages (e.g., mpeg1::mCherry-H2B) and neutrophils (e.g., lyz::BFP).
- Microinjection Setup: Prepare a microinjection rig with pulled glass capillaries.
- PAMP Solution: Prepare 10-20 nL of a suspension of zymosan particles (5-10 mg/mL) in PBS. Zymosan is a fungal derivative rich in β-glucans.
2. Injection Procedure:
- Anesthetize larvae in tricaine.
- Position the larva laterally under a dissecting microscope. Using the glass needle, inject the zymosan suspension directly into the hindbrain ventricle.
- Allow injected larvae to recover in fresh embryo medium.
3. Imaging and Quantification:
- At defined time points post-injection (e.g., 4-6 hours), anesthetize larvae and mount them for live confocal microscopy.
- Quantifiable Readouts:
- Immune Cell Recruitment: Count the number of fluorescently labeled neutrophils and macrophages at the injection site over time.
- Phagocytosis: Assess the internalization of zymosan particles by macrophages and neutrophils based on fluorescence co-localization.
- NF-κB Activation: Use transgenic NF-κB reporter zebrafish lines (e.g., with GFP under an NF-κB-responsive promoter) to measure fluorescence intensity as a proxy for pathway activation.
4. Genetic/Pharmacological Perturbation:
- To test the role of specific receptors or pathways, repeat the assay using mutant larvae (e.g., card9 mutants [115]) or larvae treated with pharmacological inhibitors (e.g., Syk inhibitors).
Table 2: Research Reagent Solutions for PRR Pathway Analysis
| Reagent / Tool | Function / Application | Example in Research |
|---|---|---|
| Zymosan A (S. cerevisiae) | A particulate preparation of fungal cell walls rich in β-glucans and mannans. Used to stimulate CLR (e.g., Dectin-1) and TLR pathways. | Injected into zebrafish hindbrain to study neutrophil/macrophage recruitment and NF-κB activation [115]. |
| Transgenic Reporter Lines | Genetically modified organisms with fluorescent proteins under the control of immune-responsive promoters (e.g., NF-κB). | Zebrafish NF-κB::GFP reporter line used to visualize and quantify innate immune pathway activation in real-time [115]. |
| Morpholino Oligonucleotides / CRISPR-Cas9 | Technologies for targeted gene knockdown (morpholino) or knockout (CRISPR-Cas9) to determine gene function. | Used in zebrafish to generate card9 mutants, which showed impaired neutrophil recruitment in response to zymosan [115]. |
| Cross-Species Proteomics/Analytics | Computational pipelines to distinguish host and donor proteins in cross-species transplant or infection models. | A cross-species proteomic strategy was developed to distinguish donor vs. host extracellular matrix in explanted biomaterials, a method applicable to xenotransplantation studies [117]. |
| Single-Cell RNA-Seq | High-resolution profiling of gene expression in individual cells across species, allowing for identification of conserved cell types and states. | Used to profile PBMCs from 12 vertebrate species, identifying conserved monocyte gene expression programs and universal immune cell markers [116]. |
Implications for Inflammation and Therapeutic Intervention
Understanding the deep conservation of PRR pathways not only illuminates immune evolution but also provides critical insights into human inflammatory diseases and novel therapeutic avenues.
PRRs in Chronic Inflammatory Diseases
Dysregulated PRR signaling is a hallmark of many chronic inflammatory and autoimmune diseases. Excessive or persistent activation by PAMPs or DAMPs can lead to pathological inflammation. For example, in psoriasis, the CLR Dectin-1 is highly upregulated in the epidermis and is thought to contribute to the disease pathology, potentially in response to local cytokines rather than direct fungal ligands [118]. Furthermore, the concept of "trained immunity"—a long-term functional reprogramming of innate immune cells driven by epigenetic and metabolic changes—has emerged as a key mechanism whereby initial PRR activation can lead to enhanced responses to subsequent challenges. While beneficial for host defense, this process can also maladaptively contribute to chronic inflammatory diseases like atherosclerosis, where sterile triggers such as oxidized LDL can induce trained immunity in monocytes and macrophages [26].
Therapeutic Targeting of Conserved Pathways
The conservation of PRR pathways validates them as targets for therapeutic intervention across a range of conditions.
- Inhibitory PRRs (iPRRs): The immune system has evolved intrinsic regulatory mechanisms, including a distinct class of inhibitory PRRs (iPRRs) such as CD300a, Siglecs, and LAIR-1. These receptors recognize endogenous or microbial ligands and set a context-sensitive threshold for immune activation, preventing excessive inflammation. Targeting iPRRs to dampen aberrant immune responses represents a promising therapeutic strategy [9].
- Targeting Signaling Hubs: Given the convergence of PRR signaling on hubs like NF-κB and the NLRP3 inflammasome, developing inhibitors against these nodes has broad potential. The conservation of these pathways from model organisms to humans strengthens the predictive value of pre-clinical studies in these models.
- Metabolic and Epigenetic Regulators: As trained immunity is maintained by metabolic rewiring and epigenetic marks like H3K4me3 and H3K27ac, targeting the underlying enzymes (e.g., mTOR, histone methyltransferases) offers a novel approach to treat PRR-driven chronic inflammatory diseases [26].
The study of pattern recognition receptors across the evolutionary spectrum reveals a powerful narrative of conservation and adaptation. From the Toll pathway in Drosophila to the complex network of TLRs, CLRs, and cytosolic sensors in mammals, the core machinery for sensing PAMPs and initiating inflammation has been remarkably preserved. This conservation is evident not only in receptor structure and ligand specificity but also in the central signaling pathways and kinase families, such as the non-RD kinases, that they engage. Cross-species experimental approaches, leveraging organisms like zebrafish and employing modern techniques like scRNA-seq, continue to be indispensable for unraveling the intricacies of these pathways and their role in both protective immunity and pathological inflammation. For drug development professionals, this evolutionary perspective highlights the fundamental importance of PRR pathways and validates them as high-value targets. Future therapeutic success will likely depend on strategies that either enhance the protective functions of these conserved pathways or, conversely, inhibit their maladaptive roles in chronic inflammatory disease.
The innate immune system employs a sophisticated surveillance mechanism to detect both external threats and internal damage, primarily through the recognition of Pathogen-Associated Molecular Patterns (PAMPs) and Damage-Associated Molecular Patterns (DAMPs). These molecular patterns are sensed by Pattern Recognition Receptors (PRRs) expressed on various immune and non-immune cells, triggering inflammatory signaling pathways that represent the body's first line of defense [33] [54]. PAMPs are conserved, essential microbial structures—such as lipopolysaccharide (LPS) from Gram-negative bacteria—that signal infection [33]. In contrast, DAMPs are endogenous molecules, including HMGB1 and extracellular DNA, which are released from stressed or damaged cells during sterile injury, such as trauma, chemical toxicity, or ischemia [52] [119]. Although the inflammatory responses they initiate share common features, such as the recruitment of leukocytes and production of pro-inflammatory cytokines, the underlying mechanisms and long-term consequences of PAMP- versus DAMP-driven inflammation exhibit critical differences [120] [121]. Understanding these distinctions is paramount for developing targeted therapeutic strategies for infectious diseases, sterile inflammatory conditions (e.g., atherosclerosis, autoimmune disorders), and cancer [33] [26].
Fundamental Concepts and Molecular Triggers
Pattern Recognition Receptors (PRRs)
PRRs are germline-encoded host proteins that act as sensors for both PAMPs and DAMPs. They can be broadly categorized into membrane-bound receptors (e.g., Toll-like receptors or TLRs, and C-type lectin receptors or CLRs) and cytosolic receptors (e.g., NOD-like receptors or NLRs, RIG-I-like receptors or RLRs, and AIM2-like receptors or ALRs) [33] [54]. A key concept is the sharing of receptors; for instance, TLR4 can be activated by the exogenous PAMP LPS and by endogenous DAMPs like HMGB1 and heparan sulfate [122] [33]. This shared recognition system can lead to similar inflammatory outcomes from distinct initial insults.
Key Triggers: PAMPs vs. DAMPs
The table below summarizes the primary characteristics and examples of PAMPs and DAMPs.
Table 1: Key Characteristics of PAMPs and DAMPs
| Feature | PAMPs (Pathogen-Associated Molecular Patterns) | DAMPs (Damage-Associated Molecular Patterns) |
|---|---|---|
| Origin | Exogenous (microbial) [33] | Endogenous (host) [52] |
| Nature | Conserved microbial structures [33] | Molecules released during cellular stress or damage [52] [119] |
| Examples | Lipopolysaccharide (LPS), Lipoteichoic acid, Flagellin, Microbial nucleic acids [33] [54] | HMGB1, ATP, Uric acid crystals, Extracellular DNA, Heat shock proteins [121] [52] [123] |
| Primary Context | Infectious inflammation [120] | Sterile inflammation (e.g., trauma, ischemia, toxicity) [120] [123] |
Mechanisms of Inflammatory Pathway Activation
Shared Signaling Cascades
Despite their different origins, both PAMPs and DAMPs converge on major pro-inflammatory signaling pathways. The primary pathways activated upon PRR engagement are the NF-κB (Nuclear Factor kappa-light-chain-enhancer of activated B cells) pathway, the MAPK (Mitogen-Activated Protein Kinase) pathway, and the JAK-STAT pathway [122]. For example, TLR4 activation by either LPS or DAMPs like HMGB1 leads to the recruitment of the adaptor protein MyD88, initiating a signaling cascade that activates IKK complex. IKK then phosphorylates the inhibitory protein IκB, targeting it for degradation and allowing NF-κB to translocate to the nucleus to induce the transcription of cytokines such as TNF-α, IL-1β, and IL-6 [122] [33] [54].
Key Mechanistic Differences
Although they share signaling components, PAMP and DAMP responses are not identical. Research has revealed fundamental differences in the intensity and nature of the immune activation they provoke.
Table 2: Mechanistic Differences Between PAMP- and DAMP-Induced Inflammation
| Mechanistic Aspect | PAMP-Driven (Infectious) Inflammation | DAMP-Driven (Sterile) Inflammation |
|---|---|---|
| Innate Immune Activation | Robust, leads to strong cytokine production (e.g., high TNF-α, IL-10) [121] | Weaker innate immune activation compared to PAMPs [121] |
| TLR Tolerance | Induces strong TLR tolerance (desensitization to subsequent stimulation) [121] | Induces only partial TLR tolerance [121] |
| Induction of Cell Death | Significant innate immune cell death and G0/G1 cell cycle arrest [121] | Minimal impact on innate immune cell viability or cell cycle [121] |
| Coagulation Effects | Lesser coagulopathic effects in localized models [121] | Potent procoagulant effects, can cause significant thrombosis [121] |
| Key Signaling Mediators | NF-κB activation; can be independent of oxidative stress [120] | p38 MAPK-induced cellular senescence; linked to oxidative stress [120] |
These mechanistic differences explain distinct clinical outcomes. The potent cell death and immune paralysis induced by PAMPs can lead to immunoparalysis in sepsis, increasing susceptibility to secondary infections [121]. Conversely, the partial tolerance and survival of immune cells upon DAMP stimulation, coupled with strong procoagulant effects, may contribute to thrombotic complications and chronic inflammation in conditions like severe trauma [121].
Figure 1: Simplified Signaling and Outcome Differences between PAMP and DAMP Pathways. Both triggers activate PRRs and downstream pathways like NF-κB, but their effector outcomes diverge significantly, with PAMPs driving strong cytokine production and immune tolerance, while DAMPs promote senescence and coagulation [120] [121].
Experimental Approaches and Research Toolkit
Key Experimental Models and Methodologies
Investigating the nuances of sterile versus infectious inflammation requires well-defined experimental models. Key methodologies include:
- In Vitro Cell Stimulation: Isolated innate immune cells (e.g., mouse macrophages) are stimulated with purified PAMPs (e.g., LPS for TLR4) or DAMPs (e.g., HMGB1, heparan sulfate). This allows for the controlled assessment of cytokine production (via ELISA or bead arrays), cell viability (via assays like MTT), cell cycle analysis (via flow cytometry), and downstream signaling (e.g., NF-κB activation via reporter assays) [121].
- Necrotic Cell Supernatant Model: To recapitulate sterile injury, cells (e.g., fibroblasts) are subjected to sonication-induced traumatic cell death. The supernatant, rich in diverse DAMPs (HMGB1, exDNA), is used to stimulate immune cells, providing a more physiologically relevant mixture of danger signals than single DAMP molecules [121].
- In Vivo Murine Models:
- Local Inflammation: Intraperitoneal injection of PAMPs (e.g., LPS, sonicated bacteria supernatant) or DAMPs (e.g., sonicated fibroblast supernatant) to study local and systemic inflammatory responses, organ damage (via plasma ALT, creatinine), and survival [121].
- Systemic Inflammation: Intravenous injection is used to model systemic effects. A critical finding is that while local DAMP administration is less lethal, systemic injection can cause acute mortality primarily due to inferior vena cava thrombosis, an effect preventable by anticoagulants like heparin [121].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Studying PAMP/DAMP Pathways
| Reagent / Assay | Function/Application | Experimental Context |
|---|---|---|
| Ultrapure LPS | Canonical PAMP; selective TLR4 agonist [121] [33] | Used as a positive control for infectious inflammation in vitro and in vivo. |
| Recombinant HMGB1 | Canonical DAMP; activates TLR4 and other receptors [121] [52] | Used to model sterile inflammation induced by proteinaceous DAMPs. |
| Heparan Sulfate | Endogenous DAMP; TLR4 agonist [121] | Used to study sterile inflammation, particularly in contexts of extracellular matrix breakdown. |
| Sonicated Cell Supernatants | Complex mixture of DAMPs (HMGB1, exDNA) [121] | Provides a physiologically relevant sterile inflammatory stimulus. |
| Cytokine Bead Array (CBA) / ELISA | Multiplex or single-plex quantification of cytokines (TNF-α, IL-6, IL-1β, IL-10) [121] [124] | Essential for profiling the inflammatory response. |
| TLR Reporter Cell Lines | Cells (e.g., HEK293) engineered to express a specific TLR and a reporter gene (e.g., luciferase) under an NF-κB promoter [121] | Used to specifically quantify TLR pathway activation. |
| Anticoagulants (Heparin) | Inhibits coagulation cascade [121] | Used in vivo to confirm the role of coagulation in DAMP-driven pathology. |
Functional and Clinical Consequences of Differential Inflammation
Unique Inflammatory Mediator Profiles
Clinical studies in complex patient populations provide evidence for distinct inflammatory signatures. Research on febrile neutropenic hematology patients—who experience inflammation from both infections and sterile tissue damage from chemotherapy—revealed that specific patterns of inflammatory mediators can distinguish these etiologies. Using pattern recognition methods like O-PLS (orthogonal projection to latent structures), it was found that combinations of clinical, physiological, and laboratory parameters (including cytokines, markers of metabolism, and organ function) could segregate patients with microbiologically defined infections from those with sterile inflammation [124]. This suggests that while the classical inflammatory cytokines may be elevated in both scenarios, the broader physiological response creates a unique fingerprint for each trigger.
Role in Chronic Inflammation and Trained Immunity
A paradigm-shifting discovery in immunology is the concept of "trained immunity," a de facto memory in innate immune cells. Initially described for PAMPs (e.g., after BCG vaccination), it is now clear that DAMPs and Lifestyle-Associated Molecular Patterns (LAMPs), such as oxidized LDL (oxLDL), cholesterol crystals, and uremic toxins, can also induce long-term functional reprogramming of innate immune cells and their bone marrow progenitors [26]. This reprogramming involves epigenetic changes (e.g., histone modifications H3K4me3 and H3K27ac) and metabolic shifts (e.g., upregulation of aerobic glycolysis) [26]. While beneficial for host defense, maladaptive trained immunity driven by chronic sterile stimuli is implicated in the pathogenesis of chronic diseases like atherosclerosis, autoimmune disorders, and chronic kidney disease [26]. This provides a mechanistic link between sterile insults and the perpetuation of chronic inflammation.
Inflammasome Activation
The inflammasome, a multi-protein complex (e.g., featuring an NLR sensor, ASC adaptor, and caspase-1), is a critical component of innate immunity that processes and activates the potent pro-inflammatory cytokines IL-1β and IL-18 [123]. Both PAMPs and DAMPs can activate inflammasomes. The NLRP3 inflammasome, in particular, is a key sensor for a wide array of sterile danger signals, including ATP, uric acid crystals, cholesterol crystals, and silica [119] [123]. This makes it a central player in sterile inflammatory diseases like gout, atherosclerosis, and asbestosis. Furthermore, complexes like the PANoptosome demonstrate how multiple PRRs can cooperate to drive robust inflammatory cell death in response to combined PAMP and DAMP stimulation [54].
The delineation of PAMP- versus DAMP-driven inflammation has moved beyond a simple dichotomy of trigger origin to reveal profound differences in immune activation strength, induction of tolerance, cell fate, coagulopathy, and long-term immune reprogramming. These differences have direct clinical implications, from the high mortality of septic immunoparalysis to the thrombotic complications and chronicity of sterile inflammatory diseases.
Future research and therapeutic development will be guided by several key principles. First, the discovery of distinct inflammatory "fingerprints" in patients [124] opens the door for improved diagnostic tools using pattern recognition of multiple biomarkers. Second, the shared use of receptors like TLR4 by PAMPs and DAMPs presents a challenge, as blocking them could compromise host defense against pathogens. Therefore, targeting more downstream, divergent pathways—such as specific components of the senescence pathway for sterile inflammation or specific tolerance mechanisms for sepsis—may yield more precise and safer therapeutics. Finally, the emerging role of DAMP-induced trained immunity [26] unveils novel therapeutic targets. Modulating the epigenetic and metabolic engines of maladaptive innate immune memory holds promise for preventing and treating the growing burden of chronic inflammatory diseases.
Pathogen-associated molecular patterns (PAMPs) are highly conserved, essential molecular structures unique to microbes but not present in the host organism [2]. These patterns serve as fundamental "danger signals" that are directly recognized by the innate immune system through pattern recognition receptors (PRRs) expressed on various immune cells, including dendritic cells, macrophages, and neutrophils [3] [2]. This recognition event represents the critical initial step in mounting an immune defense against invading pathogens, triggering a cascade of inflammatory responses that not only combat immediate threats but also orchestrate subsequent adaptive immunity [2]. The prototypical example of a PAMP is bacterial lipopolysaccharide (LPS), a component of gram-negative bacterial membranes recognized predominantly by Toll-like receptor 4 (TLR4) [2]. Other well-characterized PAMPs include flagellin (recognized by TLR5), peptidoglycan (recognized by TLR2), double-stranded RNA (recognized by TLR3), and unmethylated CpG DNA motifs (recognized by TLR9) [2].
The interaction between PAMPs and PRRs initiates intracellular signaling pathways that lead to the production and release of pro-inflammatory cytokines and chemokines, creating an inflammatory environment conducive to pathogen clearance [2]. This process also promotes the maturation of antigen-presenting cells, which subsequently travel to lymph nodes to activate T-cells and initiate antigen-specific antibody production by B-cells, thereby bridging innate and adaptive immunity [2]. When dysregulated, however, PAMP-induced immune activation can contribute to pathological inflammation, making the quantitative measurement of PAMP exposure and subsequent immune activation crucial for understanding disease pathogenesis, identifying prognostic biomarkers, and developing targeted therapeutic interventions [49] [125].
Pattern Recognition Receptors and Signaling Pathways
Classification of PRRs and Their DAMP Ligands
PRRs constitute a diverse array of immune receptors that detect both PAMPs and damage-associated molecular patterns (DAMPs), which are endogenous molecules released during cellular stress or tissue injury [40] [3]. Based on protein domain homology and function, PRRs in vertebrates are primarily classified into five major families, each with distinct ligand recognition profiles and subcellular locations [3].
Table 1: Major Families of Pattern Recognition Receptors (PRRs) and Their DAMP Ligands
| PRR Family | Major Members | DAMP Ligands | Cellular Localization |
|---|---|---|---|
| Toll-like Receptors (TLRs) | TLR1-9 (humans) | HMGB1, HSPs, S100 proteins, histones, RNA, DNA, mtDNA, biglycan, hyaluronan, fibrinogen [40] | Cell surface (TLR1,2,4,5,6) and endosomal membranes (TLR3,7,8,9) [3] |
| NOD-like Receptors (NLRs) | NOD1, NOD2, NLRP family | Uric acid, Aβ, mitochondrial ROS, biglycan, hyaluronan [40] | Cytoplasm [3] |
| RIG-I-like Receptors (RLRs) | RIG-I, MDA5, LGP2 | RNA (self) [40] | Cytoplasm [3] |
| C-type Lectin Receptors (CLRs) | Dectin-1, Dectin-2, Mincle | SAP130, F-actin [40] | Cell surface [3] |
| AIM2-like Receptors (ALRs) | AIM2, IFI16 | DNA (self) [3] | Cytoplasm [3] |
PAMP/PRR Signaling Pathways
Upon ligand binding, PRRs activate conserved downstream signaling pathways that lead to the expression of inflammatory mediators. TLR signaling, for instance, diverges into two principal pathways: the MyD88-dependent pathway and the TRIF-dependent pathway [3]. The MyD88-dependent pathway is utilized by all TLRs except TLR3 and leads to the activation of NF-κB and MAPK pathways, resulting in the production of pro-inflammatory cytokines like TNF-α, IL-1, and IL-6 [3]. The TRIF-dependent pathway, utilized by TLR3 and TLR4, induces type I interferons (IFNs) critical for antiviral responses [3]. Cytosolic PRRs, such as RLRs and ALRs, typically sense viral nucleic acids and activate signaling cascades that also converge on IFN production, while NLRs can form inflammasome complexes that process and activate pro-inflammatory cytokines like IL-1β and IL-18 [3].
Diagram: PAMP Recognition and Downstream Signaling Pathways
Quantitative Approaches for Measuring PAMP Exposure and Immune Activation
Accurately quantifying PAMP exposure and the ensuing immune response is fundamental for evaluating disease severity, progression, and therapeutic efficacy. Advanced proteomic and molecular techniques now enable researchers to profile complex biomarker signatures associated with PAMP-driven pathologies.
Proteomic Profiling of Immune Responses
Sequential Window Acquisition of all Theoretical Mass Spectra (SWATH-MS) is a high-resolution, data-independent acquisition mass spectrometry method ideal for large-scale quantitative proteomic studies. This approach has been successfully applied to characterize serum protein profiles across the spectrum of COVID-19 disease severity, from asymptomatic individuals to severe cases in intensive care units [126]. The experimental workflow typically involves:
- Sample Preparation: Serum samples are collected, heat-inactivated, and clustered into biological pools. Proteins are then digested into peptides using trypsin (e.g., with the FASP Protein Digestion Kit) [126].
- Chromatographic Separation: The resulting tryptic peptides are separated by reverse-phase liquid chromatography [126].
- Mass Spectrometric Analysis: Peptides are analyzed by mass spectrometry using an Information-Dependent Acquisition (IDA) method to build a spectral library, followed by SWATH-MS for quantitative data acquisition across predefined mass-to-charge windows [126].
- Data Analysis: Dysregulated proteins are identified through statistical comparison of expression levels across patient cohorts. Bioinformatics tools like Metascape are used to interpret the biological processes and pathways associated with the altered proteins [126].
This methodology identified several immune-related prognostic biomarkers, including Selenoprotein P (SELENOP) and Serum paraoxonase/arylesterase 1 (PON1) for disease recovery, Carboxypeptidase B2 (CBP2) for severity, and Pregnancy zone protein (PZP) for general symptomatology [126].
Molecular Biomarkers of Immune Activation
Quantifying specific cytokines and microRNAs (miRNAs) provides a targeted approach to assessing immune activation. Enzyme-Linked Immunosorbent Assay (ELISA) is a standard technique for measuring serum cytokine levels. For instance, the pro-inflammatory cytokine IL-6 and the anti-inflammatory cytokine IL-10 can be quantified using commercial ELISA kits with sensitivities typically around 1.03 pg/mL and 2.59 pg/mL, respectively [125]. The IL-6/IL-10 ratio has emerged as a potent indicator of inflammatory imbalance and disease severity in conditions like COVID-19 [125].
Simultaneously, the expression of immunoregulatory miRNAs can be assessed using quantitative real-time PCR (qRT-PCR). A validated protocol involves:
- miRNA Extraction: Total miRNA is extracted from plasma (preferred over serum to avoid platelet-derived miRNA contamination) using a specialized kit like the miRNeasy serum/plasma Kit [125].
- Reverse Transcription (RT): Extracted miRNA is reverse transcribed into cDNA using specific stem-loop RT primers and a MicroRNA Reverse Transcription Kit [125].
- qPCR Amplification: The cDNA is amplified using TaqMan probes (e.g., for miR-155 and the reference gene U6 snRNA) on a real-time PCR system. Relative expression levels are calculated using the 2−ΔΔCT method [125].
Research has shown that miR-155 expression is significantly elevated in severe COVID-19 patients, correlates with ICU admission and mortality, and serves as an independent predictor of disease severity [125]. The following table summarizes key biomarkers identified in recent clinical studies.
Table 2: Immune-Related Biomarkers in Human Disease: The Case of COVID-19
| Biomarker | Biomarker Type | Association with Disease | Measurement Technique |
|---|---|---|---|
| IL-6 | Pro-inflammatory cytokine | Positively correlated with disease severity and inflammation [125] | ELISA |
| IL-6/IL-10 Ratio | Cytokine Ratio | Indicator of inflammatory imbalance; higher in severe disease [125] | Derived from ELISA data |
| miR-155 | MicroRNA | Independent risk factor for severity, ICU admission, and mortality [125] | qRT-PCR |
| SELENOP & PON1 | Serum Proteins | Predictive of disease recovery [126] | SWATH-MS Proteomics, ELISA |
| CBP2 | Serum Protein | Predictive of disease severity [126] | SWATH-MS Proteomics, ELISA |
Experimental Protocols for Assessing Immune Competence
In Vivo Challenge Models with PAMPs
Controlled in vivo challenges with purified PAMPs provide a direct method for evaluating an organism's immune competence. A representative protocol, adapted from nanoplastic exposure studies in arthropods, involves challenging the subject with well-characterized PAMPs and measuring cellular immune responses [127].
Protocol: Total Hemocyte Count (THC) and Encapsulation Response Post-PAMP Challenge
- PAMP Preparation: Prepare solutions of Lipopolysaccharide (LPS) and β-1,3-glucan in phosphate-buffered saline (PBS). LPS is a major component of gram-negative bacterial walls, while β-1,3-glucan is a fungal cell wall component [127].
- Challenge Injection: Inject the experimental subject (e.g., the tarantula Chilobrachys guangxiensis) with a defined volume of LPS, β-1,3-glucan, or PBS as a control [127].
- Hemolymph Collection: Collect hemolymph at multiple time points post-injection (e.g., 0, 6, 12, and 24 hours) [127].
- Total Hemocyte Count (THC): Immediately fix the collected hemolymph and load it onto a hemocytometer to count the total number of hemocytes (immune cells) under a microscope. THC serves as a primary indicator of immune system mobilization [127].
- Encapsulation Rate Assay: The encapsulation response, a cellular defense mechanism where hemocytes form layers around a foreign body, can be quantified by implanting a small, inert substrate (e.g., a nylon filament) and measuring the degree of melanization and cell adhesion after a set period [127].
This protocol can reveal how prior exposures (e.g., to environmental stressors like nanoplastics) weaken immunocompetence, as evidenced by a significantly reduced THC following PAMP challenge in exposed subjects compared to controls [127].
Transcriptomic Analysis of Immune Pathways
Following the phenotypic immune assays, transcriptomic analysis of immune tissues (e.g., hemolymph) provides a comprehensive view of the molecular mechanisms underlying the observed immune responses.
Protocol: Hemolymph Transcriptomic Analysis
- RNA Sequencing: Extract total RNA from hemolymph samples of control and experimental groups. Prepare cDNA libraries and perform high-throughput RNA sequencing (RNA-Seq) [127].
- Differential Expression Analysis: Map sequencing reads to a reference genome and identify genes that are significantly differentially expressed between the PAMP-challenged experimental and control groups.
- Pathway Enrichment Analysis: Input the list of differentially expressed genes into bioinformatics databases (e.g., KEGG, GO) to identify enriched immune signaling pathways, such as the Toll, IMD, and JAK/STAT pathways in arthropods (functional analogs of TLR, TNF, and JAK/STAT pathways in mammals) [127]. This analysis can reveal which specific arms of the immune system are activated or suppressed by PAMP exposure and prior stressors.
Diagram: Experimental Workflow for PAMP Challenge and Immune Analysis
The Scientist's Toolkit: Key Research Reagent Solutions
Successful investigation into PAMP exposure and immune activation relies on a suite of well-characterized reagents and methodologies. The following table outlines essential tools for researchers in this field.
Table 3: Research Reagent Solutions for PAMP and Immune Response Studies
| Reagent / Assay | Function / Target | Example Application |
|---|---|---|
| Ultrapure LPS | TLR4 agonist; models gram-negative bacterial infection [2] | In vivo immune challenge to induce acute inflammatory response [127] |
| β-1,3-glucan | Dectin-1 agonist; models fungal infection [127] | In vivo challenge to probe antifungal immune mechanisms [127] |
| ELISA Kits (IL-6, IL-10) | Quantify specific cytokine protein levels in serum/plasma [125] | Assessment of pro-inflammatory and anti-inflammatory cytokine balance [125] |
| TaqMan MicroRNA Assays | Detect and quantify specific miRNA expression (e.g., miR-155) [125] | Evaluation of immunoregulatory miRNA levels linked to disease severity [125] |
| SWATH-MS Proteomics | Large-scale identification and quantification of serum proteins [126] | Discovery of novel protein biomarkers associated with disease symptomatology and outcomes [126] |
| RNA-Seq | Genome-wide analysis of transcriptional changes | Unbiased profiling of immune pathway activation (e.g., Toll, IMD) following PAMP challenge [127] |
Research Applications and Therapeutic Implications
The measurement of PAMP exposure and immune activation extends beyond basic research into practical applications in clinical prognosis, understanding disease mechanisms, and therapeutic development. In COVID-19, the quantification of miR-155 and the IL-6/IL-10 ratio provides clinicians with valuable prognostic tools to identify patients at high risk of severe disease, ICU admission, and mortality, enabling earlier and more aggressive interventions [125]. Furthermore, the persistence of epigenetic trained immunity signatures in monocytes and hematopoietic progenitors of severe COVID-19 patients for up to one year post-infection illustrates the long-term impact of PAMP-driven immune activation and may explain chronic symptoms and comorbidities [49].
In oncology, local tumor treatments like thermal ablation (e.g., radiofrequency, microwave, and cryoablation) induce immunogenic cell death, releasing cancer antigens and DAMPs that function as in situ vaccines [128]. Measuring the resulting immune responses, such as changes in T-cell populations and cytokine profiles, helps predict treatment efficacy and can guide combination strategies with immune checkpoint inhibitors to enhance systemic anti-tumor immunity [128]. The field is also moving towards therapeutic interventions that directly target PRR signaling pathways. Clinical trials are exploring monoclonal antibodies to neutralize DAMPs, small-molecule inhibitors to block key signaling nodes like MyD88 or NF-κB, and enzymatic degradation of accumulated DAMPs (e.g., uricase for gout) [39]. While challenges remain in achieving specificity and avoiding immunosuppression, these approaches hold significant promise for modulating PAMP- and DAMP-driven pathologies across a spectrum of inflammatory diseases [39].
The therapeutic modulation of Pathogen-Associated Molecular Pattern (PAMP) signaling represents a frontier in treating infectious diseases, cancer, and inflammatory disorders. Targeting Pattern Recognition Receptors (PRRs) can potentiate immune responses but risks triggering detrimental immunosuppression or cytokine storms. This whitepaper analyzes the delicate balance between efficacy and toxicity in PAMP-directed therapies. We evaluate quantitative parameters defining therapeutic windows, detail experimental protocols for their determination, and visualize critical signaling pathways. Emerging strategies—including nano-immunomodulators and combination therapies—show promise for widening therapeutic indices. For researchers and drug development professionals, this review provides a technical framework for developing precise immunomodulatory interventions that maximize protective immunity while minimizing pathological consequences.
The immune system detects microbial invasions through Pattern Recognition Receptors (PRRs) that identify conserved Pathogen-Associated Molecular Patterns (PAMPs) [33]. This recognition initiates innate immune responses that form the first line of defense and orchestrate subsequent adaptive immunity. While PAMP signaling is crucial for host defense, its dysregulation can lead to either excessive inflammation or inadequate immune activation, presenting a fundamental challenge for therapeutic intervention.
PAMPs are recognized by several PRR families, including Toll-like receptors (TLRs), C-type lectin receptors (CLRs), NOD-like receptors (NLRs), RIG-I-like receptors (RLRs), and cytosolic DNA sensors such as cGAS [33]. Upon activation, these receptors trigger signaling cascades—most commonly involving NF-κB, MAPK, and IRF3 pathways—that result in proinflammatory cytokine production, interferon responses, and immune cell activation. Therapeutically, PRR agonists are being investigated as vaccine adjuvants, standalone immunotherapies for cancer, and antiviral agents [129]. Conversely, PRR antagonists may treat autoimmune and chronic inflammatory diseases.
The central challenge in modulating PAMP signaling lies in defining and exploiting the therapeutic window—the dose range where treatment provides efficacy without unacceptable toxicity. An insufficient immune stimulus fails to provide therapeutic benefit, while excessive activation can cause systemic inflammatory response syndrome (SIRS), organ damage, or paradoxical immunosuppression through compensatory mechanisms [49] [130]. This review examines the quantitative parameters of this balance, explores experimental approaches for its evaluation, and discusses emerging strategies to maximize therapeutic potential while mitigating risks.
The Dual Faces of PAMP Signaling: Protective Immunity vs. Immunopathology
Beneficial Immune Activation
Appropriate PAMP signaling provides heterologous protection against infections and tumors. The phenomenon of trained immunity, where innate immune cells develop enhanced nonspecific responsiveness after exposure to certain PAMPs, exemplifies this beneficial aspect [26] [49]. For instance, BCG vaccination reprograms hematopoietic stem cells and myeloid progenitors, leading to enhanced cytokine production and improved defense against unrelated pathogens [49]. This protection is mediated through epigenetic reprogramming and metabolic shifts in innate immune cells, particularly toward aerobic glycolysis [26].
In oncology, PAMP signaling can overcome the immunosuppressive tumor microenvironment (TME). TLR agonists promote dendritic cell (DC) maturation, enhance antigen presentation to T cells, and stimulate production of inflammatory cytokines such as type I interferons and IL-12 [129]. This activation reverses T cell exhaustion and enables robust anti-tumor responses, particularly when combined with other immunotherapies like immune checkpoint inhibitors (ICIs) [131] [129].
Pathological Consequences and Immunosuppression Risks
Excessive or persistent PAMP signaling drives severe pathologies. In sepsis, uncontrolled activation of PRRs by both PAMPs and Damage-Associated Molecular Patterns (DAMPs) leads to cytokine storms, characterized by dramatically elevated levels of TNF-α, IL-6, and IL-1β [70] [130]. This hyperinflammatory state causes widespread tissue damage, organ failure, and high mortality.
Paradoxically, following initial hyperinflammation, PAMP signaling can induce a state of immunosuppression—a key feature of Persistent Inflammation, Immunosuppression, and Catabolism Syndrome (PICS) [130]. Mechanisms include:
- Lymphocyte apoptosis: Particularly of B and CD4+ T cells, depleting the adaptive immune compartment.
- Expansion of immunosuppressive cells: Including myeloid-derived suppressor cells (MDSCs) and regulatory T cells (Tregs).
- T cell exhaustion: Upregulation of inhibitory receptors such as PD-1 and TIM-3.
- Metabolic reprogramming: Immune cells shift toward oxidative phosphorylation and impaired glucose utilization, reducing their effector functions [132] [130].
Table 1: Pathological Consequences of Dysregulated PAMP Signaling
| Pathological State | Key Mechanisms | Clinical Manifestations |
|---|---|---|
| Cytokine Release Syndrome | Excessive NF-κB signaling, Elevated TNF-α, IL-6, IL-1β | Hypotension, capillary leak, multi-organ failure |
| Compensatory Immunosuppression | Lymphocyte apoptosis, T cell exhaustion, MDSC expansion | Secondary infections, viral reactivation, sepsis mortality |
| Trained Immunity in Chronic Inflammation | DAMP/PAMP-induced epigenetic reprogramming | Atherosclerosis, autoimmunity, neurodegenerative diseases |
Quantitative Parameters Defining the Therapeutic Window
Determining the therapeutic window for PAMP modulation requires evaluating quantitative parameters across cellular, tissue, and organismal levels. The following table summarizes key metrics and their implications for efficacy and toxicity.
Table 2: Quantitative Parameters for Evaluating PAMP Therapeutic Window
| Parameter | Efficacy Range | Toxicity Threshold | Measurement Techniques |
|---|---|---|---|
| Cytokine Induction | Moderate IFN-γ, IL-12 | TNF-α > 500 pg/mL, IL-6 > 1000 pg/mL (in vitro) | Multiplex ELISA, intracellular staining |
| Immune Cell Activation | 30-60% CD86+ DCs, 20-40% CD69+ T cells | >80% MHC-II+ monocytes with simultaneous PD-L1 upregulation | Flow cytometry, mass cytometry |
| PRR Expression | 2-5 fold increase post-stimulation | Sustained >10-fold increase correlating with tolerance | qPCR, Western blot, receptor binding assays |
| Metabolic Activity | 1.5-3 fold increase in ECAR (glycolysis) | Simultaneous decrease in OCR (oxidative phosphorylation) | Seahorse Analyzer, glucose uptake assays |
| Pathogen Clearance | 2-4 log reduction in bacterial load | >50% tissue damage in infection models | CFU counts, bioluminescent imaging, histology |
Critical considerations for interpreting these parameters include:
- Timing: Early cytokine production (6-24 hours) typically correlates with protection, while prolonged elevation (>48 hours) often predicts pathology.
- Cell-type specificity: Responses differ substantially between immune cell subsets; monocyte activation may benefit host defense while endothelial cell activation promotes vascular leakage.
- Synergistic effects: Combinations of PAMPs can trigger non-linear responses where subthreshold concentrations become toxic when combined.
Experimental Protocols for Assessing Therapeutic Windows
In Vitro Dose-Response and Temporal Profiling
Purpose: To establish preliminary efficacy and toxicity thresholds using human immune cells.
Primary Protocol:
- Isolate human peripheral blood mononuclear cells (PBMCs) from healthy donors using density gradient centrifugation.
- Stimulate with titrated doses of TLR agonists (e.g., Pam3CSK4 for TLR2, poly(I:C) for TLR3, LPS for TLR4, R848 for TLR7/8) across a 6-log concentration range.
- Collect supernatants at multiple time points (6, 24, 48, 72 hours) for cytokine profiling via multiplex ELISA.
- Analyze cell surface markers (CD80, CD86, HLA-DR, PD-L1) by flow cytometry at 24 and 48 hours.
- Assess metabolic reprogramming via Seahorse Analyzer to measure extracellular acidification rate (ECAR) and oxygen consumption rate (OCR).
- Evaluate induction of tolerance by re-stimulating cells with a standard LPS dose after initial priming.
Key Outputs:
- Half-maximal effective concentration (EC50) for desired responses (e.g., IL-12 production)
- Half-maximal toxic concentration (TC50) for adverse outcomes (e.g., excessive TNF-α production)
- Therapeutic index calculated as TC50/EC50
In Vivo Efficacy and Toxicity Models
Purpose: To validate therapeutic windows in physiologically relevant contexts.
Primary Protocol:
- Utilize murine models of infection (e.g., Listeria monocytogenes, influenza) or cancer (e.g., MC38, CT26).
- Administer PRR agonists via appropriate routes (intravenous, intraperitoneal, intratumoral) in escalating doses.
- Monitor clinical signs (weight loss, temperature, activity) twice daily.
- Quantify bacterial/viral loads in organs (spleen, liver, lungs) at predetermined endpoints.
- Analyze immune parameters including:
- Serum cytokine levels
- Immune cell infiltration in tissues by flow cytometry
- Histopathological examination of major organs
- Assess long-term immunological consequences including:
- Development of trained immunity
- Presence of immunosuppressive markers
- Response to secondary challenges
Key Outputs:
- Maximum tolerated dose (MTD)
- Optimal biological dose (OBD) providing protection without pathology
- Comprehensive immunological profiling correlating specific parameters with outcomes
Diagram 1: Experimental workflow for determining the therapeutic window of PAMP-targeting therapies, integrating in vitro and in vivo approaches.
Signaling Pathways and Molecular Checkpoints
Understanding the intricate signaling networks downstream of PRRs is essential for targeted therapeutic interventions. The diagram below illustrates key pathways and potential intervention points.
Diagram 2: PAMP signaling pathways and regulatory checkpoints, highlighting the balance between protective immunity and pathological consequences.
The diagram illustrates how PAMP engagement of PRRs activates multiple signaling pathways that culminate in diverse immune outputs. Critical regulatory checkpoints include:
- SOCS proteins: Negative feedback regulators that dampen JAK-STAT signaling
- A20/TNFAIP3: Limits NF-κB activation by deubiquitinating signaling intermediates
- ATF3: Transcription factor that suppresses TLR4-induced gene expression
- Regulatory microRNAs: Fine-tune immune responses by targeting key signaling molecules
Therapeutic interventions can target these checkpoints to widen the therapeutic window, either by enhancing negative regulators to prevent excessive inflammation or inhibiting them to overcome immunosuppression.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for PAMP Signaling Studies
| Reagent Category | Specific Examples | Research Applications | Key Considerations |
|---|---|---|---|
| PRR Agonists | LPS (TLR4), Pam3CSK4 (TLR1/2), Poly(I:C) (TLR3), R848 (TLR7/8), CpG ODN (TLR9) | In vitro and in vivo immune activation, dose-response studies | Purity critical (e.g., ultrapure LPS vs. standard preparations); vehicle compatibility |
| PRR Antagonists | TAK-242 (TLR4), CLI-095 (TLR4), ODN TTAGGG (TLR9 antagonist) | Control for specificity, modeling immunosuppression | Off-target effects at high concentrations; species-specific efficacy |
| Cytokine Measurement | Multiplex ELISA panels, LEGENDplex, ELISA kits for TNF-α, IL-6, IL-1β, IFN-α/β/γ | Quantifying immune responses, determining therapeutic windows | Dynamic range considerations; species cross-reactivity |
| Pathway Inhibitors | BAY 11-7082 (NF-κB), SP600125 (JNK), SB203580 (p38), Ruxolitinib (JAK) | Mechanistic studies, identifying key signaling nodes | Specificity varies; compensatory pathway activation possible |
| Flow Cytometry Panels | Surface: CD14, CD80, CD86, HLA-DR, PD-L1; Intracellular: phospho-proteins, cytokines | Immune cell phenotyping, activation status, signaling analysis | Panel design optimization; fixation/permeabilization conditions |
| Metabolic Assays | Seahorse XF Glycolysis Stress Test, 2-NBDG glucose uptake, MitoTracker dyes | Evaluating metabolic reprogramming in trained immunity | Culture conditions significantly impact results |
| Epigenetic Tools | H3K4me3, H3K27ac antibodies (ChIP), BET inhibitors, HDAC inhibitors | Studying trained immunity mechanisms | Cell number requirements for ChIP; inhibitor specificity |
Emerging Strategies to Widen the Therapeutic Window
Nano-Immunomodulators for Targeted Delivery
Recent advances in nanotechnology offer promising approaches to enhance the specificity of PAMP-directed therapies. TLR agonist nanoformulations improve pharmacokinetics and biodistribution through:
- Size-controlled accumulation in lymphoid tissues via the reticuloendothelial system
- Surface functionalization with targeting ligands (antibodies, peptides) for specific immune cell subsets
- Stimuli-responsive release mechanisms (pH-, enzyme-, or redox-sensitive) that activate drugs in desired microenvironments
- Co-delivery systems combining PRR agonists with antigens, checkpoint inhibitors, or other immunomodulators [129]
These strategies collectively enhance therapeutic indices by increasing local drug concentrations at target sites while minimizing systemic exposure. For example, nanoparticles sized 20-100 nm preferentially drain to lymph nodes, while those 100-200 nm accumulate in tumor tissues via the enhanced permeability and retention effect.
Combination Therapies and Sequential Scheduling
Rational combination approaches can uncouple beneficial from detrimental effects of PAMP signaling:
- PRR agonists with immune checkpoint blockade: TLR stimulation creates an inflammatory TME while ICIs reverse T cell exhaustion [131] [129]
- Sequential scheduling: Initial PAMP activation followed by later immunosuppression blockade (or vice versa) aligned with disease pathophysiology
- Metabolic modulators: Compounds that enhance or inhibit specific metabolic pathways to shape the quality of immune responses
- Epigenetic regulators: BET inhibitors and HDAC inhibitors that modulate trained immunity induction [26] [49]
Biomarker-Guided Patient Stratification
Identifying predictive biomarkers can optimize patient selection for PAMP-targeted therapies:
- Baseline PRR expression levels on immune cells
- Polymorphisms in PRR signaling pathways
- Metabolic profiling of circulating immune cells
- Transcriptomic signatures of pre-treatment tumor or immune cells
These biomarkers help identify patients most likely to respond favorably while avoiding those at high risk for adverse events, effectively widening the therapeutic window at the population level.
The therapeutic modulation of PAMP signaling requires careful navigation between efficacy and toxicity. Key parameters including cytokine levels, immune cell activation status, metabolic reprogramming, and epigenetic changes define the therapeutic window for these interventions. Experimental approaches must evaluate both immediate effects and long-term consequences, including the induction of trained immunity or immunosuppressive states.
Emerging technologies—particularly nano-immunomodulators, rational combination therapies, and biomarker-guided patient selection—show significant promise for widening therapeutic indices. Future research should focus on:
- Spatiotemporal control of PRR agonist delivery and activity
- Personalized approaches based on individual immune and metabolic profiles
- Advanced modeling of signaling networks to predict therapeutic windows
- Standardized reporting of efficacy and toxicity parameters across studies
As our understanding of PAMP signaling complexity deepens, so too does our ability to precisely manipulate these pathways for therapeutic benefit while minimizing the risks of immunosuppression and immunopathology.
Conclusion
The study of PAMPs and their recognition by the innate immune system has fundamentally reshaped our understanding of host-pathogen interactions and inflammation. This synthesis of knowledge reveals a highly sophisticated alarm system capable of discriminating between diverse microbial threats, yet one that is vulnerable to dysregulation leading to chronic disease. Future research must focus on unraveling the complex crosstalk between different PRR pathways, understanding the context-dependent outcomes of PAMP exposure in different tissues like the liver, and translating these insights into next-generation therapeutics. The emerging concepts of LAMPs and the nuanced role of ion channels in inflammation open new frontiers. For drug development, the challenge and opportunity lie in selectively modulating these pathways—enhancing protective immunity while preventing pathological inflammation—to treat a broad spectrum of diseases from sepsis to autoimmune disorders and cancer.
References
- 1. Pathogen Associated Molecular Pattern - an overview [https://www.sciencedirect.com/topics/pharmacology-toxicology-and-pharmaceutical-science/pathogen-associated-molecular-pattern]
- 2. Pathogen-associated molecular pattern [https://en.wikipedia.org/wiki/Pathogen-associated_molecular_pattern]
- 3. Pattern recognition receptors in health and diseases [https://www.nature.com/articles/s41392-021-00687-0]
- 4. Pathogen Recognition and Inflammatory Signaling in Innate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2668232/]
- 5. Microbial RNA, the New PAMP of Many Faces [https://www.frontiersin.org/journals/tropical-diseases/articles/10.3389/fitd.2022.924719/full]
- 6. Biofilm-associated molecular patterns: BAMPs - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12519799/]
- 7. Mechanistic insights into PAMP and DAMP driven ... [https://www.sciencedirect.com/science/article/abs/pii/S1567576925011397]
- 8. Pathogen-Associated Molecular Pattern - an overview [https://www.sciencedirect.com/topics/immunology-and-microbiology/pathogen-associated-molecular-pattern]
- 9. Pattern recognition receptors: function, regulation and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12246121/]
- 10. Pattern recognition receptor [https://en.wikipedia.org/wiki/Pattern_recognition_receptor]
- 11. Toll-Like Receptors (TLRs), NOD-Like Receptors (NLRs), and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8704656/]
- 12. Pathogen Associated Molecular Pattern - an overview [https://www.sciencedirect.com/topics/medicine-and-dentistry/pathogen-associated-molecular-pattern]
- 13. Pattern Recognition Receptors (PRRs) Expression and ... [https://www.mdpi.com/2076-2607/13/9/2176]
- 14. Repeats mimic pathogen-associated patterns across a vast ... [https://www.sciencedirect.com/science/article/pii/S2666979X25002678]
- 15. Innate Immune Surveillance and Recognition of Epigenetic ... [https://pubmed.ncbi.nlm.nih.gov/40981069/]
- 16. Exploring the Role of Pattern Recognition Receptors as ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12093340/]
- 17. Lipopolysaccharide detection by the innate immune system ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9533005/]
- 18. An examination of the LPS-TLR4 immune response through ... [https://biosignaling.biomedcentral.com/articles/10.1186/s12964-025-02149-4]
- 19. Structural biology of the LPS recognition [https://www.sciencedirect.com/science/article/abs/pii/S1438422107000689]
- 20. Bacterial flagellin—a potent immunomodulatory agent [https://www.nature.com/articles/emm2017172]
- 21. bacterial flagellin activates basolaterally expressed TLR5 to ... [https://pubmed.ncbi.nlm.nih.gov/11489966/]
- 22. 2.3: The Peptidoglycan Cell Wall [https://bio.libretexts.org/Bookshelves/Microbiology/Microbiology_(Kaiser)/Unit_1%3A_Introduction_to_Microbiology_and_Prokaryotic_Cell_Anatomy/2%3A_The_Prokaryotic_Cell_-_Bacteria/2.3%3A_The_Peptidoglycan_Cell_Wall]
- 23. Peptidoglycan [https://en.wikipedia.org/wiki/Peptidoglycan]
- 24. Innate Sensing of Viral Nucleic Acids and Their Use in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11860339/]
- 25. Innate Immunity and Inflammation: Conuersim Between ... [https://pubmed.ncbi.nlm.nih.gov/41177771/]
- 26. Trained immunity induced by DAMPs and LAMPs in ... [https://www.nature.com/articles/s12276-025-01542-w]
- 27. NF-κB signaling in inflammation - PubMed [https://pubmed.ncbi.nlm.nih.gov/29158945/]
- 28. NF-κB signaling in inflammation | Signal Transduction and Targeted Therapy [https://www.nature.com/articles/sigtrans201723]
- 29. Targeting NF-κB pathway for the therapy of diseases: mechanism and clinical study | Signal Transduction and Targeted Therapy [https://www.nature.com/articles/s41392-020-00312-6]
- 30. NF-κB [https://en.wikipedia.org/wiki/NF-%CE%BAB]
- 31. The Impact of Cytokine Storms on Severe Infectious ... [https://jpmsonline.com/article/the-impact-of-cytokine-storms-on-severe-infectious-diseases-progression-a-narrative-review-720/]
- 32. Cytokines in sepsis: a critical review of the literature on ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1682306/full]
- 33. Pattern recognition receptors: function, regulation and ... [https://www.nature.com/articles/s41392-025-02264-1]
- 34. Molecular mechanisms and regulation of inflammasome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12575685/]
- 35. Global Cytokine Storm market size is USD XX million in 2024. [https://www.cognitivemarketresearch.com/cytokine-storm-market-report]
- 36. Immune Dysregulation in Sepsis. A Narrative Review for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12561552/]
- 37. Biomarker-Based Risk Assessment Strategy for Long COVID [https://pmc.ncbi.nlm.nih.gov/articles/PMC12474022/]
- 38. The Role of Damage-Associated Molecular Patterns in Human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4318613/]
- 39. Damage-associated molecular patterns (DAMPs) in diseases [https://pmc.ncbi.nlm.nih.gov/articles/PMC12394712/]
- 40. Damage-Associated Molecular Patterns in Inflammatory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6117512/]
- 41. Damage- and pathogen-associated molecular patterns ... [https://insight.jci.org/articles/view/127925]
- 42. PAMPs and DAMPs: signal 0s that spur autophagy and immunity [https://pmc.ncbi.nlm.nih.gov/articles/PMC3662247/]
- 43. Signal transduction by the lipopolysaccharide receptor, Toll ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1782563/]
- 44. Multi-omic profiling of pathogen-stimulated primary immune cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC11293528/]
- 45. Structural biology of the LPS recognition [https://pubmed.ncbi.nlm.nih.gov/17481951/]
- 46. Metabolic reprogramming in macrophages and dendritic ... [https://www.nature.com/articles/cr201568]
- 47. Regional Molecular Changes in Chronic ... [https://www.sciencedirect.com/science/article/pii/S2667174325000692]
- 48. Integrated transcriptomic and proteomic analysis of the ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1576721/full]
- 49. Trained immunity: induction of an inflammatory memory in ... [https://www.nature.com/articles/s41422-025-01171-y]
- 50. Progranulin modulates inflammatory responses to immune ... [https://pubmed.ncbi.nlm.nih.gov/40799615/]
- 51. Experimental Models and Their Applicability in Inflammation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12250041/]
- 52. DAMPs and DAMP-sensing receptors in inflammation and ... [https://www.sciencedirect.com/science/article/pii/S1074761324000980]
- 53. Inflammasomes and Signaling Pathways: Key Mechanisms in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12191029/]
- 54. Pattern recognition receptors and inflammasome [https://pmc.ncbi.nlm.nih.gov/articles/PMC12270683/]
- 55. Animal models of inflammatory bowel disease - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC11021814/]
- 56. An animal model of NLRC4-associated autoinflammation ... [https://www.nature.com/articles/s41423-025-01355-x]
- 57. Post Pandemic Problem, is there an animal model suitable ... [https://www.nature.com/articles/s44303-025-00101-2]
- 58. Harnessing stem cell therapeutics in LPS-induced animal ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04290-w]
- 59. News Details [https://ir.coyatherapeutics.com/news/news-details/2025/Coya-Therapeutics-COYA-303-Shows-Promising-Central-Nervous-System-CNS-Anti-inflammatory-Effects-and-Systemic-Regulatory-T-Cell-Treg-Enhancing-Effects-in-a-Preclinical-Animal-Inflammation-Model/default.aspx]
- 60. Overview | Thermo Fisher Scientific - DE Inflammation [https://www.thermofisher.com/de/de/home/life-science/cell-analysis/cell-analysis-learning-center/immunology-at-work/inflammation-overview.html]
- 61. and DAMPs stimulate the expression of pro- PAMPs ... inflammatory [https://orbit.dtu.dk/en/publications/pamps-and-damps-stimulate-the-expression-of-pro-inflammatory-cyto]
- 62. Flow Cytometry Multiplex Bead Array Technology and Its ... [https://pubmed.ncbi.nlm.nih.gov/41200584/]
- 63. Simplified flow cytometry-based assay for rapid multi- ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1594141/full]
- 64. Transforming cytokine diagnostics: AI, multiplexing , and point-of-care... [https://pubmed.ncbi.nlm.nih.gov/41175281/]
- 65. Transcriptome-based protein-protein interaction analysis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11228953/]
- 66. How GPUs Can Accelerate High Throughput Screening ... [https://www.exxactcorp.com/blog/molecular-dynamics/how-gpus-can-accelerate-high-throughput-screening-research]
- 67. PRR antagonists and agonists - Fraunhofer IGB [https://www.igb.fraunhofer.de/en/research/cell-and-tissue-technologies/immunoreceptors-and-drug-screening/toll-like-rezeptoren.html]
- 68. Advances in high-throughput drug screening based on ... [https://www.sciencedirect.com/science/article/pii/S2090123225006897]
- 69. Advances in high-throughput drug screening based on ... [https://pubmed.ncbi.nlm.nih.gov/40945847/]
- 70. Anti-DAMP therapies for acute inflammation [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1579954/full]
- 71. Innate Sensing of Viral Nucleic Acids and Their Use in ... [https://www.mdpi.com/2076-393X/13/2/193]
- 72. Decrypting the Immune Symphony for RNA Vaccines - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12390541/]
- 73. The liver's dilemma: sensing real danger in a sea of PAMPs [https://pmc.ncbi.nlm.nih.gov/articles/PMC11808282/]
- 74. Patterns of pathogenesis: discrimination of pathogenic and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2777727/]
- 75. Toll-Like Receptor Signaling Pathways - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4174766/]
- 76. Inflammasome activation and regulation: toward a better ... [https://www.nature.com/articles/s41421-020-0167-x]
- 77. Inflammasome activation and assembly at a glance - PubMed [https://pubmed.ncbi.nlm.nih.gov/29196474/]
- 78. Drug discovery and treatment paradigms in nonalcoholic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7576222/]
- 79. Sick for science: experimental endotoxemia as a ... [https://www.nature.com/articles/s41380-020-00869-2]
- 80. The Silent Saboteur: Endotoxin Contamination [https://kactusbio.com/blogs/news/the-silent-saboteur-endotoxin-contamination?srsltid=AfmBOorpKFD1JxukcLkIvN78xr-CIXVlEMJo2OnF49BwTXz0wwUIfWAm]
- 81. Molecular mechanisms and regulation of inflammasome ... [https://www.nature.com/articles/s41423-025-01354-y]
- 82. Bacterial Endotoxin Testing Market Size 2025 to 2034 [https://www.precedenceresearch.com/bacterial-endotoxin-testing-market]
- 83. Human endotoxin administration as an experimental model in ... [https://pubmed.ncbi.nlm.nih.gov/25236665/]
- 84. Pathogen Recognition and Innate Immunity [https://www.sciencedirect.com/science/article/pii/S0092867406001905]
- 85. PAMPs and DAMPs: signal 0s that spur autophagy and immunity - PubMed [https://pubmed.ncbi.nlm.nih.gov/22889221/]
- 86. PAMPs and DAMPs: How do these molecules differ? [https://www.novusbio.com/antibody-news/pamps-and-damps-what-is-the-same-and-what-is-different-about-these-molecules?srsltid=AfmBOoqM9NpiW0MMQeHTXX60lH0JIVo2IUJeyQmd1tbPVUL6q9-whwyH]
- 87. Press release: The Nobel Prize in Physiology or Medicine ... [https://www.nobelprize.org/prizes/medicine/2025/press-release/]
- 88. Regulatory T cells in homeostasis and disease [https://www.nature.com/articles/s41392-025-02326-4]
- 89. Mechanisms of NLRP3 inflammasome in pathogenesis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12374694/]
- 90. Nobel 2025: Immune Tolerance and 3D In Vitro Models [https://insphero.com/nobel2025-celebrating-discoveries-in-immune-tolerance/]
- 91. Chasing Virus Replication and Infection: PAMP-PRR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12031425/]
- 92. PAMP-PRR Interaction Drives Type I Interferon Production ... [https://pubmed.ncbi.nlm.nih.gov/40284971/]
- 93. Viral Inhibition of PRR-Mediated Innate Immune Response [https://www.sciencedirect.com/science/article/pii/S1016847823051014]
- 94. Danger signal and PAMP sensing define binary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2768518/]
- 95. Tumor Necrosis Factor-α Signaling in Macrophages - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3066460/]
- 96. Daeshiho-tang attenuates inflammatory response and ... [https://www.nature.com/articles/s41598-023-46033-y]
- 97. Editorial: The liver's dilemma: sensing real danger in a sea ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1591911/full]
- 98. LPS-induced systemic inflammation is suppressed by the PDZ ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11460976/]
- 99. An NF-kB/TNF-alpha signalling feedback loop acts to ... [https://www.nature.com/articles/s41536-025-00414-1]
- 100. L-arabinose Attenuates LPS-Induced Intestinal ... [https://www.sciencedirect.com/science/article/pii/S0022316623726072]
- 101. Translational Insights into Interferon Alpha's Effects on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12293709/]
- 102. Tumor necrosis factor-alpha promotes survival in methotrexate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3241368/]
- 103. New insights into TRP channels - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC4048338/]
- 104. The NLRP3 inflammasome in urogenital cancers [https://pmc.ncbi.nlm.nih.gov/articles/PMC12289484/]
- 105. Editorial: Molecular mechanisms of ion channel activation ... [https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2025.1695777/full]
- 106. Study Establishes “Ball and Chain” Mechanism Inactivates ... [https://physiology.med.cornell.edu/study-establishes-ball-and-chain-mechanism-inactivates-key-mammalian-ion-channel/]
- 107. Effectors of plants pathogenic fungi and fungal like microbes [https://www.frontiersin.org/journals/plant-science/articles/10.3389/fpls.2025.1626960/full]
- 108. An Overview of Pathogen Recognition Receptors for Innate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4630409/]
- 109. Trained immunity induced by DAMPs and LAMPs in chronic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12586657/]
- 110. Genetic evidence informs the direction of therapeutic ... [https://www.nature.com/articles/s44386-025-00027-0]
- 111. Advanced In Vitro Models for Preclinical Drug Safety [https://www.mdpi.com/1467-3045/47/1/7]
- 112. Improving target assessment in biomedical research [https://www.nature.com/articles/s41573-020-0087-3]
- 113. 10 clinical trials to watch the rest of 2025 [https://www.biopharmadive.com/news/biotech-pharma-clinical-trials-watch-2025/736120/]
- 114. Plant and Animal Pathogen Recognition Receptors Signal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1331981/]
- 115. Zebrafish use conserved CLR and TLR signaling pathways ... [https://www.sciencedirect.com/science/article/abs/pii/S0145305X24001587]
- 116. Cross-species single-cell analysis reveals divergence and ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-024-11030-6]
- 117. Cross-species proteomics quantification pipeline ... [https://pubmed.ncbi.nlm.nih.gov/40667106/]
- 118. A Comprehensive Analysis of Pattern Recognition ... [https://www.sciencedirect.com/science/article/pii/S0022202X15345929]
- 119. Danger Signals and Inflammasomes: Stress-Evoked Sterile ... [https://www.nature.com/articles/npp2016125]
- 120. Mechanistic Differences Leading to Infectious and Sterile ... [https://pubmed.ncbi.nlm.nih.gov/26840942/]
- 121. Damage- and pathogen-associated molecular patterns play ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6777836/]
- 122. Inflammatory responses and inflammation-associated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5805548/]
- 123. IL-1 family cytokines trigger sterile inflammatory disease [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2012.00315/full]
- 124. Distinct Inflammatory Mediator Patterns Characterize ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0092319]
- 125. Role of immune-inflammatory biomarkers and their derived ... [https://www.nature.com/articles/s41598-025-24173-7]
- 126. Characterization by Quantitative Serum Proteomics of ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2021.730710/full]
- 127. Nanoplastic exposure weakens immunocompetence in the ... [https://www.sciencedirect.com/science/article/abs/pii/S0013935125005833]
- 128. Potential biomarkers for predicting immune response and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10646301/]
- 129. Breaking the barriers in effective and safe Toll-like receptor ... [https://www.sciencedirect.com/science/article/abs/pii/S0168365925002871]
- 130. Cell death signaling and immune regulation [https://cmbl.biomedcentral.com/articles/10.1186/s11658-025-00784-w]
- 131. From intracellular drivers to immune modulators: emerging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12542028/]
- 132. Innate immunity in tumors: roles and therapeutic targets [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1689714/full]