Advanced Cytokine Sensing and Dynamic Monitoring: Technologies Shaping Drug Development and Clinical Research
This article provides a comprehensive overview of the rapidly evolving landscape of cytokine sensing and dynamic monitoring technologies, tailored for researchers, scientists, and drug development professionals.
Advanced Cytokine Sensing and Dynamic Monitoring: Technologies Shaping Drug Development and Clinical Research
Abstract
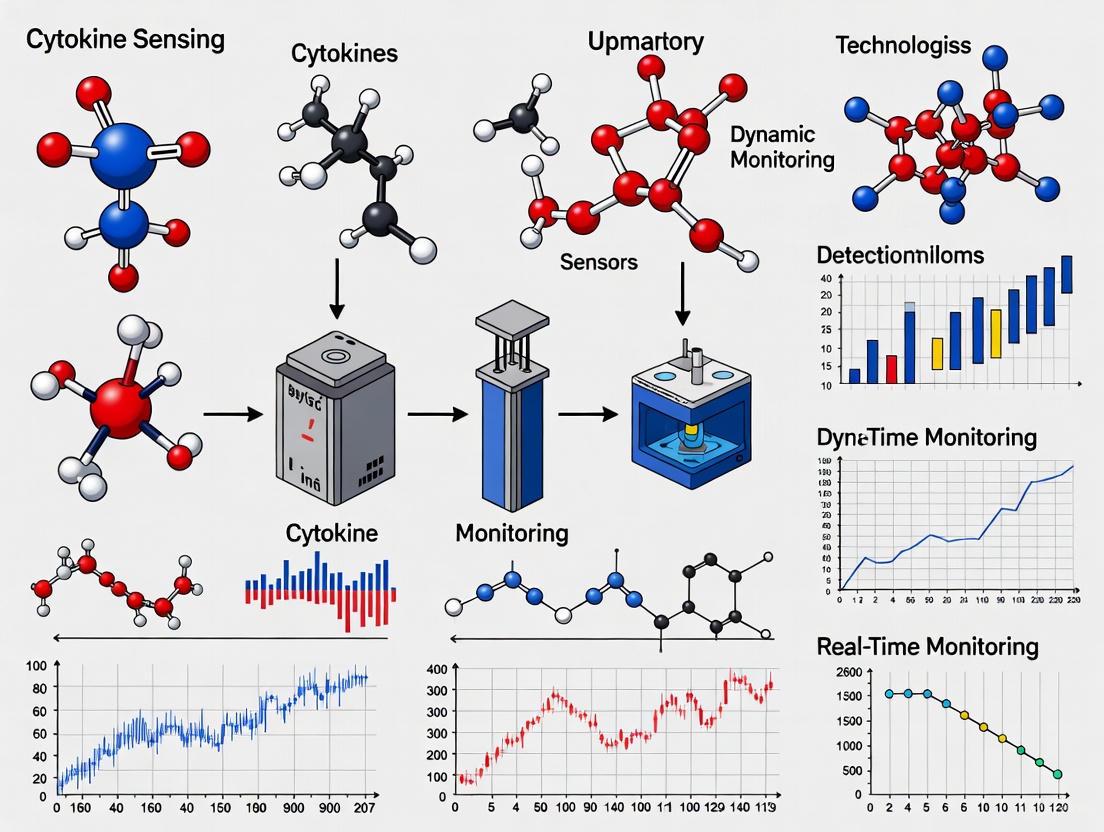
This article provides a comprehensive overview of the rapidly evolving landscape of cytokine sensing and dynamic monitoring technologies, tailored for researchers, scientists, and drug development professionals. It explores the foundational role of cytokines as critical biomarkers in immunology, cancer, and inflammatory diseases. The scope spans from established methodological platforms and their specific applications in therapeutics like T-cell engagers (TCEs) to troubleshooting common analytical challenges. A comparative analysis of current and emerging technologies—including MSD, Luminex, ELISA, and novel biosensors—equips readers to select and validate optimal assays for their specific R&D and clinical needs, ultimately accelerating the development of safer and more effective immunotherapies.
The Critical Role of Cytokine Dynamics in Disease and Therapy
Cytokines are low molecular weight, soluble proteins or glycoproteins that function as pivotal intercellular signaling molecules within the immune system. These molecules regulate nearly every aspect of immunity and inflammation, balancing pathogen defense against potential tissue damage from excessive inflammatory responses [1]. Their activity is characterized by two fundamental properties: pleiotropy, where a single cytokine can exert different effects depending on cellular context and receptor usage, and redundancy, where multiple cytokines can mediate overlapping functions [2]. In physiological conditions, cytokines maintain immune homeostasis through complex, tightly regulated networks. However, dysregulated cytokine production can trigger a cytokine storm (CS), also known as cytokine release syndrome (CRS)—a life-threatening systemic inflammatory syndrome characterized by immune cell hyperactivation and dramatically elevated circulating cytokine levels [1] [3].
The clinical significance of cytokine monitoring has expanded dramatically with the recognition that CS drives pathology across diverse conditions including sepsis, COVID-19, chimeric antigen receptor T-cell (CAR-T) therapy complications, autoimmune disorders, and hematologic conditions like hemophagocytic lymphohistiocytosis (HLH) [4] [1]. In sepsis, for instance, CS is a central pathogenic mechanism contributing to systemic inflammatory response syndrome (SIRS) and multiple organ dysfunction syndrome (MODS), with septic shock carrying mortality rates up to 70% [4]. The ability to quantitatively measure cytokine profiles has therefore transitioned from basic research to critical clinical application, providing biomarkers for early diagnosis, risk stratification, prognostic assessment, and therapeutic monitoring [4] [5] [6].
Cytokine Monitoring Technologies and Performance Specifications
Advanced cytokine detection platforms have evolved significantly from traditional single-plex enzyme-linked immunosorbent assays (ELISA) to sophisticated multiplex systems that enable comprehensive immune monitoring. The following table summarizes the key technical characteristics of major cytokine detection methodologies:
Table 1: Performance Comparison of Cytokine Detection Technologies
| Technology Platform | Multiplexing Capacity | Sample Volume | Time to Results | Limit of Detection Range | Key Advantages |
|---|---|---|---|---|---|
| Conventional ELISA | Single-plex | 50-100 µL | 4-6 hours | Varies by analyte | Gold standard, widely available, high sensitivity |
| Flow Cytometry (FCM)-based Multiplex | 12-plex+ | 50-100 µL | 1.5-2 hours | Similar to ELISA | High throughput, widespread instrument availability |
| Luminex/xMAP Technology | 50-plex+ | 50 µL | 3-4 hours | 0.01-100 pg/mL | High multiplexing, good dynamic range |
| AI-Enabled Point-of-Care Biosensing | 5-10 plex | 1-50 µL | 5-30 minutes | 0.01-100 pg/mL | Rapid results, portable, minimal sample requirement |
| Implantable Protein Sensors | 2-plex (currently) | Continuous in vivo | Real-time monitoring | Not specified | Continuous monitoring, in vivo application |
Technological innovations are progressively addressing the limitations of conventional laboratory-based methods. Flow cytometry-based multiplex assays now enable simultaneous quantification of 12 or more cytokines from minimal sample volumes (50-100 μL) with significantly reduced processing times [7]. Recent developments have further simplified these assays through lyophilized reagent systems and one-step detection protocols, eliminating cold chain requirements and reducing operator hands-on time while maintaining analytical performance comparable to conventional methods [7].
The emerging frontier in cytokine monitoring involves continuous in vivo sensing, analogous to continuous glucose monitors (CGMs) for diabetes management. Recently developed implantable protein sensors utilizing an "active-reset" mechanism with high-frequency vibration can dynamically track cytokine level changes in real-time within living organisms [8]. These electrochemical sensors specifically target cytokines like IL-6 and TNF-α, forming the basis for future clinical monitoring platforms that could enable early intervention in inflammatory cascades [8].
Artificial intelligence (AI) integration is simultaneously enhancing the analytical capabilities of cytokine diagnostics. AI-enabled multiplex point-of-care platforms now achieve limits of detection as low as 0.01-100 pg/mL, with dynamic ranges spanning 3-4 orders of magnitude, using just 1-50 µL of sample and delivering results within 5-30 minutes [6]. Machine learning algorithms provide calibrated predictive outputs, uncertainty estimates, and drift monitoring, significantly strengthening performance and clinical utility [6].
Experimental Protocols for Cytokine Analysis
One-Step Flow Cytometry-Based Multiplex Cytokine Assay
This protocol describes a simplified workflow for simultaneous quantification of 12 cytokines from serum samples, integrating lyophilized reagents to eliminate cold storage requirements and reduce processing steps [7].
Table 2: Research Reagent Solutions for Flow Cytometry-Based Multiplex Cytokine Assay
| Reagent/Material | Specifications | Function/Purpose |
|---|---|---|
| Carboxylated Fluorescently Encoded Microspheres | 100,000 particles/mL, Spherotech | Capture antibody immobilization, analyte detection |
| Cytokine Capture Antibodies | BioLegend, BD, or Thermo Fisher Scientific | Specific cytokine binding |
| Phycoerythrin (PE)-Labeled Detection Antibodies | 2 μg/mL concentration | Detection and quantification |
| Lyophilization Buffer | PBS with 0.1% BSA, 5% mannitol, 3% trehalose | Reagent preservation and stabilization |
| 96-Well Plates | U-bottom, non-sterile | Assay platform |
| Wash Buffer | 0.15 M PBS, 0.05% Tween-20, pH 7.4 | Removal of unbound components |
| Reading Buffer | 0.15 M PBS, pH 7.4 | Sample resuspension for analysis |
| Flow Cytometer | Beckman Coulter DxFlex or equivalent | Signal detection and quantification |
Procedure:
Lyophilized Bead Reconstitution: Add 100 μL of serum sample or standard directly to wells containing lyophilized reagent beads in a 96-well plate. The lyophilized spheres contain pre-mixed capture-antibody-modified microspheres and PE-labeled detection antibodies.
Incubation: Seal the plate and incubate with continuous shaking at room temperature for 1.5 hours. Ensure thorough mixing to dissolve lyophilized components completely.
Washing: After incubation, wash twice with 200 μL wash buffer using a plate washer or manual pipetting. Centrifuge at 300 × g for 5 minutes between washes and carefully decant supernatant to remove unbound detection antibodies.
Resuspension: Add 100-150 μL of reading buffer to each well and vortex thoroughly to resuspend the beads.
Flow Cytometric Analysis: Acquire samples immediately using a flow cytometer equipped with appropriate lasers and detectors for bead identification and PE fluorescence quantification. Analyze at least 100 events per bead set to ensure statistical reliability.
Data Analysis: Generate standard curves for each cytokine using recombinant protein standards included in the assay. Calculate cytokine concentrations in unknown samples through interpolation from respective standard curves.
Technical Notes:
- Lyophilized reagents remain stable for at least 6 months when stored desiccated at 4°C.
- For low-abundance cytokines, sample volume can be increased to 150 μL with proportional increases in reagent volumes.
- Performance validation against conventional ELISA is recommended when establishing the assay for new sample types.
- The one-step method reduces total hands-on time by approximately 60% compared to conventional multi-step FCM assays while maintaining equivalent sensitivity and dynamic range [7].
Dynamic Cytokine Monitoring for Prognostic Assessment
This protocol applies to serial cytokine measurements for risk stratification in inflammatory conditions, with specific application in elderly community-acquired pneumonia (CAP) patients [5].
Procedure:
Baseline Sample Collection: Draw blood samples at patient admission (Timepoint 0). Process within 2 hours of collection by centrifugation at 1000 × g for 10 minutes. Aliquot serum and store at -80°C until analysis.
Follow-up Sample Collection: Obtain a second blood sample within 48 hours of admission (Timepoint 48h). Process identically to baseline samples.
Cytokine Quantification: Analyze samples using multiplex cytokine panels (e.g., Bio-Plex Pro Human Cytokine 27-plex Assay) according to manufacturer instructions. Include IL-6, IL-8, IL-10, TNF-α, and other cytokines relevant to the specific pathology.
Dynamic Change Calculation: Calculate relative cytokine changes using the formula:
Dynamic Change Ratio = (Follow-up Value - Baseline Value) / Baseline Value
A positive ratio indicates increasing levels, while a negative ratio indicates decreasing levels.
Clinical Correlation: Integrate cytokine dynamics with established severity scores (e.g., PSI, CURB-65 for CAP) using multivariate analysis or machine learning approaches.
Technical Notes:
- In elderly CAP patients, an 88% increase in IL-6 within 48 hours predicts mortality with significantly higher accuracy than static measurements alone [5].
- The combination of IL-6 dynamics with traditional severity scores (PSI + IL-6 dynamics) achieves AUC values of 0.7676 for mortality prediction, substantially outperforming individual metrics [5].
- For CAR-T therapy patients, monitoring should occur on days 4, 7, and 10 post-infusion to capture CRS development kinetics [9].
Diagram Title: Dynamic Cytokine Monitoring Workflow
Key Signaling Pathways in Cytokine Storm Pathogenesis
Understanding the molecular pathways driving cytokine storms is essential for developing targeted interventions and interpreting cytokine profile data. The following diagram and description outline the primary signaling cascades involved in CS pathogenesis:
Diagram Title: Cytokine Storm Signaling Pathways
The JAK/STAT pathway represents a central signaling cascade in CS pathogenesis, activated by numerous cytokines including IL-6, IFNs, and others [1]. Upon cytokine binding to their cognate receptors, receptor-associated Janus kinases (JAKs) phosphorylate signal transducers and activators of transcription (STATs), which then dimerize and translocate to the nucleus to drive expression of pro-inflammatory genes [1]. Notably, IL-6 can signal through classical cis-signaling (via membrane-bound IL-6R), trans-signaling (via soluble IL-6R), and trans-presentation mechanisms, amplifying its pleiotropic effects in CS [1]. The significance of this pathway is demonstrated by the therapeutic efficacy of JAK inhibitors in conditions like CAR-T associated CRS and COVID-19-related CS [1].
Toll-like receptor (TLR) signaling initiates CS in response to pathogen-associated molecular patterns (PAMPs) and damage-associated molecular patterns (DAMPs) [4] [1]. TLR activation on innate immune cells triggers downstream NF-κB and inflammasome pathways, leading to production of pro-inflammatory cytokines including IL-1β, IL-6, and TNF-α [1]. Inflammasomes, particularly NLRP3, activate caspase-1, which processes pro-IL-1β and pro-IL-18 into their active forms while simultaneously inducing pyroptotic cell death [4].
Inflammatory cell death pathways including pyroptosis, necroptosis, and their integration in "panoptosis" create self-amplifying loops in CS [4]. These lytic cell death modalities release additional DAMPs that further activate PRRs, establishing a vicious cycle of inflammation and cell death that drives organ damage in severe sepsis and other CS-associated conditions [4].
Advanced Sensing Platforms and Computational Approaches
Implantable Cytokine Sensors for Real-Time Monitoring
Breakthrough technology in continuous cytokine monitoring has been achieved through implantable protein sensors that function similarly to continuous glucose monitors [8]. These devices employ an "active-reset" mechanism where high-frequency vibration dissociates the cytokine-sensor complex, enabling continuous monitoring of cytokine level fluctuations in real-time [8].
Technical Specifications:
- Detection Method: Electrochemical sensing using cytokine-specific receptors
- Target Analytes: IL-6 and TNF-α (expandable to other cytokines)
- Form Factor: Microneedle-shaped housing for subcutaneous implantation
- Key Innovation: Active-reset mechanism through voltage-induced oscillation
- Validation: Demonstrated accurate tracking of LPS-induced inflammation in rodent models with agreement to ELISA results [8]
This technology platform represents a transformative approach to inflammation monitoring, potentially enabling pre-symptomatic detection of CS and personalized management of chronic inflammatory conditions [8].
Computational Prediction of Cytokine Dynamics
Advanced computational methods have been developed to address the challenge of limited temporal cytokine profiling data. The TSCytoPred framework utilizes deep learning to infer cytokine expression trajectories from time-series gene expression data [2]. This model employs a biologically informed gene selection pipeline that integrates transcription factor-cytokine relationships, protein-protein interactions, and correlation filtering to identify predictive features [2].
Model Architecture and Performance:
- Input: Time-series gene expression data
- Core Components: Feature selection module, multilayer perceptron (MLP) block, interpolation mechanism
- Output: Inferred cytokine expression trajectories
- Performance: Significantly outperforms baseline regression methods (highest R², lowest MAE) on COVID-19 dataset
- Application: Enhanced COVID-19 patient severity risk prediction using inferred cytokine data [2]
Machine learning approaches have also been successfully applied to predict clinical outcomes such as high-grade CRS in CAR-T therapy recipients. The XGBoost algorithm demonstrated superior performance in predicting high-grade CRS using clinical parameters including SpO₂, D-dimer, diastolic blood pressure, and INR [9]. Feature importance analysis validated these parameters as key predictors, enabling development of a validated risk assessment algorithm with impressive predictive performance in an independent CAR-T cohort (n=45) [9].
Table 3: Machine Learning Applications in Cytokine Research
| Application Area | Algorithm/Method | Key Features | Performance |
|---|---|---|---|
| Cytokine Trajectory Inference | TSCytoPred (Deep Learning) | Gene expression integration, interpolation for missing time points | Superior to regression methods (R²=highest, MAE=lowest) |
| High-Grade CRS Prediction | XGBoost | SpO₂, D-dimer, diastolic BP, INR | High predictive accuracy in CAR-T cohort (n=45) |
| COVID-19 Severity Prediction | SHAP-based Explainable AI | VEGF-A, MIP-1β, IL-17 as severe case indicators | Robust severity classification |
| HBV Viral Load Prediction | Logistic Regression, Random Forest, SVM | 12-cytokine panel with ALT/AST | Accurate viral load stratification |
The integration of advanced sensing technologies with computational approaches represents the future of cytokine monitoring in both research and clinical settings. As these technologies mature, they promise to transform the management of cytokine storms from reactive treatment to proactive prevention and personalized intervention. The protocols and methodologies detailed in this application note provide researchers with robust frameworks for implementing these cutting-edge approaches in their investigative workflows, ultimately contributing to improved patient outcomes across diverse inflammatory conditions.
The clinical management of cancer patients undergoing immunotherapy has traditionally relied on static, endpoint-based biomarkers. These include conventional measures such as tumor size reduction, overall survival, and static measurements of a limited set of immune markers like PD-L1 expression or circulating cytokine levels [10]. While these metrics have guided initial clinical decisions, they often fail to capture the complex, heterogeneous, and dynamically evolving nature of anti-tumor immune responses. The immune landscape is not static; responses can evolve rapidly over time and vary widely between different tumor regions [10]. This fundamental mismatch between static measurement tools and dynamic biological processes creates a critical clinical imperative: the development and integration of dynamic monitoring technologies that can capture the spatiotemporal dynamics of immune responses to guide more precise and effective immunotherapy.
The limitations of static snapshots are particularly evident in the context of immuno-oncology, where therapeutic effects can be delayed, indirect, or spatially restricted. Immune cells may transiently infiltrate tumors, reorganize spatially, or engage in local interactions that are critical for therapeutic outcomes but remain undetectable using conventional assays [10]. Furthermore, the tumor microenvironment (TME) is rich with soluble mediators, including cytokines, that shape the quality and magnitude of immune responses. A static measurement of these factors provides limited insight compared to understanding their flux and dynamics over the course of therapy. This white paper outlines the clinical need for dynamic monitoring, summarizes emerging technologies addressing this need, and provides detailed application notes and protocols for researchers developing and implementing these solutions within the broader context of cytokine sensing and dynamic monitoring technologies research.
The Evolving Biomarker Landscape: From Single Cytokines to Multiplexed Spatial Analysis
The Diagnostic and Prognostic Value of Cytokines
Inflammatory cytokines have gained significant attention for their dual role as both diagnostic indicators and biological mediators of tumorigenesis. In gastric carcinoma (GC), for instance, serum levels of interleukin (IL)-1β, IL-6, IL-8, and interferon-gamma (IFN-γ) are consistently elevated in patients compared to healthy controls [11]. These molecules are not merely bystanders but active participants in modulating tumor-promoting inflammation, angiogenesis, and immune evasion. The diagnostic performance of individual cytokines has been demonstrated in multiple studies, with several cytokines achieving receiver operating characteristic (ROC) curves and area under the curve (AUC) values exceeding 0.70, suggesting reasonable diagnostic utility [11].
Table 1: Diagnostic Performance of Key Cytokines in Gastric Carcinoma
| Cytokine | Change in GC vs Control | Reported Diagnostic Performance (AUC) | Therapeutic/Prognostic Notes |
|---|---|---|---|
| IL-1β | Increased | AUC = 0.70–0.71 [11] | Central in Helicobacter pylori-driven inflammation; associated with tumor invasiveness and poor prognosis [11]. |
| IL-6 | Increased | AUC = 0.72; Meta-analysis: AUC = 0.90 [11] | Potent growth factor via JAK/STAT3; high IL-6 predicts worse survival and chemoresistance [11]. |
| IL-8 | Increased | AUC = 0.78 [11] | Promotes angiogenesis/metastasis; rising IL-8 after treatment predicts chemoresistance [11]. |
| IFN-γ | Increased | AUC = 0.65 [11] | Reflects T-cell immune activation; has a context-dependent dual role in tumor biology [11]. |
However, single-cytokine tests often lack sufficient sensitivity and specificity for robust clinical application. For example, IL-6 has shown high specificity (97%) but low sensitivity (39%) in some studies, while showing the opposite pattern (85.7% sensitivity, 50.1% specificity) in others [11]. This variability underscores the biological complexity and technical challenges in cytokine monitoring. Critically, combining markers into multiplex panels significantly improves diagnostic performance. A three-cytokine panel (IL-1β + IL-6 + IFN-γ) demonstrated an AUC of 0.888, far surpassing the performance of any single analyte [11]. This evidence strongly supports the transition from single-analyte measurements to multiplexed panels that better reflect the complex immunobiology of tumor progression.
The Critical Role of Spatial Context in the Tumor Microenvironment
Conventional bulk assays, such as ELISA or flow cytometry, fail to capture the spatial organization of the TME, which is increasingly recognized as a critical determinant of immunotherapy response. The presence of tertiary lymphoid structures, spatial clustering of CD8+ T cells near tumor nests, or the exclusion of effector T cells from tumor cores are spatial features correlated with response or resistance to immune checkpoint inhibitors [10].
Multiplexed spatial imaging technologies have emerged as powerful tools to overcome these limitations. Techniques such as Imaging Mass Cytometry (IMC), Multiplexed Ion Beam Imaging (MIBI), and Cyclic Immunofluorescence (CycIF) allow simultaneous visualization of 30 to over 60 proteins within intact tissue sections, preserving spatial architecture [10]. These technologies enable researchers to quantify how immunotherapies reshape the TME, revealing shifts in cell phenotypes, activation states, and the emergence of suppressive cell types that would be masked in bulk analyses.
Diagram Title: Multiplexed Spatial Imaging Workflow
Advanced Methodologies for Dynamic Immune Monitoring
High-Throughput Cytokine Screening Platforms
For profiling soluble immune mediators, high-throughput screening platforms are essential for capturing dynamic changes. Homogeneous time-resolved fluorescence (HTRF) assays represent a robust methodology for quantifying cytokine secretion in a high-throughput format. This platform has been successfully implemented in a 1536-well plate format for screening environmental chemicals, demonstrating significant increases in IL-6 and TNF-α secretion upon stimulation [12]. The assay window for IL-6 secretion increased 3.71-fold over the vehicle control group, with an EC50 of approximately 50 ng/mL upon lipopolysaccharide (LPS) treatment [12].
Table 2: Key Research Reagent Solutions for Dynamic Immune Monitoring
| Category/Reagent | Specific Example | Function/Application | Research Context |
|---|---|---|---|
| Multiplex Cytokine Assay | Luminex xMAP Technology | Simultaneous quantification of multiple cytokines (e.g., IL-1β, IL-6, IL-8, IFN-γ) from small sample volumes [11]. | Validation of cytokine panels for gastric cancer diagnosis [11]. |
| High-Throughput Screening | HTRF Assay (1536-well format) | High-throughput quantification of cytokine secretion (e.g., IL-6, TNF-α) in response to various stimuli [12]. | Screening neuroinflammatory potential of environmental toxicants in microglial models [12]. |
| Spatial Imaging Panel | NanoString PanCancer IO360 Panel (+ nCounter) | Targeted gene expression profiling of 770 immune-related genes from FFPE tissue; enables immune signature scoring [13]. | Immune profiling in melanoma patients pre-anti-PD-1 therapy [13]. |
| Synthetic Biosensor | NatE MESA Receptors | Engineered T cells with synthetic receptors to sense immunosuppressive cues (e.g., VEGF, IL-10) and respond with customized transcriptional output [14]. | Engineering T cells to resist immunosuppressive tumor microenvironment [14]. |
Protocol: HTRF-Based Cytokine Secretion Assay in a 1536-Well Format
Principle: This protocol enables high-throughput screening of compounds or conditions that modulate cytokine secretion (e.g., IL-6, TNF-α) from immune cells using Homogeneous Time-Resolved Fluorescence.
Materials:
- Human induced pluripotent stem cell-derived microglia (hiMG) or other relevant immune cell type [12]
- 1536-well tissue culture plates
- HTRF compatibility-compatible microplate reader
- HTRF cytokine detection kits (e.g., Cisbio IL-6 or TNF-α HTRF kit)
- Lipopolysaccharides (LPS) for positive control stimulation
- Test compounds or environmental agents
Procedure:
- Cell Seeding: Seed hiMG cells in 1536-well plates at a density of 1,000-2,000 cells per well in appropriate growth medium. Incubate for 24 hours.
- Stimulation: Treat cells with test compounds or control stimuli (e.g., LPS at ~50 ng/mL for IL-6 induction). Include vehicle controls. Incubate for predetermined time (e.g., 6-24 hours).
- HTRF Detection:
- Transfer a small aliquot of cell culture supernatant to a new 1536-well assay plate.
- Add HTRF detection antibodies according to manufacturer's instructions.
- Incubate plates in the dark for 3-5 hours at room temperature.
- Reading and Analysis:
- Read plates on an HTRF-compatible microplate reader.
- Calculate HTRF ratio (Signal 665 nm / Signal 620 nm) × 10,000.
- Normalize data to vehicle controls and positive stimulation controls.
- Generate dose-response curves and calculate EC50/IC50 values.
Validation: A robust assay should yield a signal-to-background ratio of ≥2.5 and a Z-factor of ≥0.5. For hiMG cells stimulated with LPS, expect an assay window of 3.71-fold and 2.62-fold over vehicle control for IL-6 and TNF-α, respectively [12].
Cross-Platform Immune Signature Analysis for Biomarker Validation
As novel biomarkers emerge, validating them across technology platforms is essential for clinical translation. The single-sample rank-based scoring method (singscore) represents a robust computational approach for generating comparable immune signature scores from different transcriptomic platforms, such as NanoString and whole transcriptome sequencing (WTS) [13].
Protocol: Immune Signature Scoring Using Singscore
Principle: The singscore method evaluates the absolute average deviation of a gene from the median rank in a predefined gene set, providing a stable, rank-based signature score that is comparable across platforms.
Materials:
- Normalized gene expression data (e.g., from NanoString nCounter PanCancer IO360 Panel or RNA-Seq)
- R statistical environment (version 4.2.0 or higher)
- singscore R package (version 1.16.0)
- Curated immune signature gene sets (e.g., Tumour Inflammation Signature - TIS)
Procedure:
- Data Preprocessing: Import normalized gene expression counts. For NanoString data, perform quality control and background correction using nSolver software.
- Gene Ranking: Use the
rankGenes()function in singscore to generate per-sample gene ranks. For cross-platform compatibility, utilize a set of stable genes (e.g., 20 housekeeping genes) to calibrate ranks across different transcriptomic datasets. - Signature Scoring: Apply the
singscore()function to calculate signature scores for your gene sets of interest using the undirected mode. - Cross-Platform Validation:
- Calculate signature scores on both NanoString and WTS data from the same samples.
- Assess correlation using Spearman correlation and linear regression.
- High-quality cross-platform performance should yield Spearman correlation interquartile range [0.88, 0.92] and r² IQR [0.77, 0.81] [13].
Application: This approach has successfully identified informative signatures for predicting immunotherapy response, such as TIS and Personalised Immunotherapy Platform (PIP) PD-1, achieving an AUC of 86.3% for predicting response in advanced melanoma patients treated with anti-PD-1-based therapies [13].
Emerging Frontiers: Synthetic Biology and In Vivo Imaging for Real-Time Monitoring
Engineering Synthetic Cytokine Receptors for Cell-Based Biosensing
A revolutionary approach to dynamic monitoring involves engineering the therapeutic cells themselves as biosensors. Recent work has demonstrated the conversion of natural cytokine receptors into orthogonal synthetic biosensors through modular extracellular sensor architecture (MESA) [14]. This technology co-opts natural cytokine receptor ectodomains (NatE) and pairs them with synthetic intracellular signaling mechanisms to create receptors that sense soluble cues in the TME and trigger customized transcriptional responses.
Diagram Title: Synthetic Cytokine Receptor Engineering
This technology enables T cells to logically evaluate multiple cues associated with the TME, sensing immunosuppressive factors such as VEGF and responding with enhanced chimeric antigen receptor (CAR) T cell activity [14]. The ability to engineer cells that simultaneously sense their environment and adapt their therapeutic function represents a paradigm shift in dynamic monitoring and therapeutic intervention.
In Vivo Imaging Technologies for Real-Time Immune Monitoring
Beyond blood-based and tissue-based assays, advanced imaging modalities now enable non-invasive, real-time monitoring of immune responses in living subjects.
Table 3: In Vivo Imaging Modalities for Dynamic Immune Monitoring
| Imaging Modality | Spatial Resolution | Temporal Resolution | Primary Applications in Immunotherapy | Key Advantages | Limitations |
|---|---|---|---|---|---|
| Intravital Microscopy | High (subcellular) | Minutes to hours | Real-time visualization of T-cell infiltration, tumor cell killing, immune cell interactions [10]. | Unprecedented resolution of dynamic cellular behaviors in live animals [10]. | Limited penetration depth; requires window chambers or superficial tumors. |
| Positron Emission Tomography (PET) | Moderate (1-2 mm) | Hours to days | Whole-body assessment of immune cell distribution, PD-L1 expression, therapeutic antibody biodistribution [10]. | Highly sensitive, quantitative, clinically translatable. | Requires radioactive tracers; lower resolution than MRI. |
| Magnetic Resonance Imaging (MRI) | High (50-100 μm) | Minutes to hours | Anatomical tumor response, immune cell infiltration using contrast agents [10]. | Excellent soft tissue contrast; no ionizing radiation. | Lower sensitivity for molecular targets compared to PET. |
These imaging technologies provide critical insights into the dynamics of immune cell trafficking, engagement with tumor cells, and the spatial heterogeneity of response that cannot be captured through blood or tissue sampling alone. For instance, intravital microscopy has revealed that stable, long-lasting interactions between cytotoxic T lymphocytes and tumor cells correlate with enhanced tumor cell apoptosis, while transient interactions may indicate ineffective immune responses [10].
The clinical imperative for dynamic monitoring in immunotherapy is clear. Static biomarkers provide limited insight into the evolving battle between the immune system and cancer. The technologies and methodologies outlined herein—from multiplexed cytokine panels and spatial transcriptomics to engineered cellular biosensors and in vivo imaging—provide a roadmap for capturing the dynamic, spatial, and functional complexity of immune responses. As these tools mature and become more accessible, their integration into clinical trials and ultimately routine practice will be essential for realizing the full potential of precision immuno-oncology. The future of immunotherapy management lies not in single timepoint assessments, but in continuous, multidimensional monitoring that can guide therapeutic adaptations in real time, ensuring that each patient receives the right immunotherapeutic intervention at the right time throughout their treatment journey.
The global cytokine market is experiencing significant growth, driven by their expanding role in therapeutics and their critical value as diagnostic biomarkers. Cytokines are low molecular weight proteins (approximately 6–70 kDa) that act as key mediators of immune responses, facilitating communication between cells and coordinating defense mechanisms [15] [16]. The market for cytokine-based interventions was valued at approximately USD 95.11 billion to USD 98.84 billion in 2025 and is projected to exhibit a robust compound annual growth rate (CAGR) of 7.1% to 8.8%, reaching an estimated USD 178.50 billion to USD 188.85 billion by 2032-2035 [17] [18]. This expansion is fueled by the increasing prevalence of chronic diseases, advancements in diagnostic technologies, and growing recognition of cytokines' therapeutic potential. The dual application of cytokines—as therapeutic agents themselves and as biomarkers for disease monitoring—creates a synergistic driver for both market and research advancements, positioning this field at the forefront of personalized medicine and immunology.
Market Analysis and Growth Projections
Global Market Size and Forecast
The cytokine market demonstrates strong global growth potential, with projections indicating sustained expansion through 2035. The following table summarizes the key market size metrics and growth trends:
Table 1: Global Cytokine Market Size and Growth Projections
| Metric | 2025 Baseline | 2035 Projection | CAGR (2025-2035) |
|---|---|---|---|
| Market Size | USD 95.11 - 98.84 Billion [17] [18] | USD 178.50 - 188.85 Billion [17] [18] | 7.1% - 8.8% [17] [18] |
| Dominant Segment (Type) | Tumor Necrosis Factor (TNF) - 45.4% share [17] | Tumor Necrosis Factor (TNF) - 40% share [18] | - |
| Dominant Segment (Application) | Cancer Therapeutics - 39.9% share [17] | Cancer Therapeutics - 50% share [18] | - |
| Leading Region | North America - 38.4% share [17] | North America - 35% share [18] | - |
| Fastest-Growing Region | Asia Pacific [17] | Asia Pacific [17] [18] | - |
Key Market Drivers and Challenges
Several interconnected factors are propelling the cytokine market forward, while certain challenges require addressing for full market potential realization.
Table 2: Key Market Drivers and Restraining Factors
| Growth Drivers | Market Restraints |
|---|---|
| Rising Chronic Disease Burden: Increasing global incidence of cancer, autoimmune disorders, and chronic inflammatory diseases [17] [18]. | High Cost Structures: Significant costs associated with cytokine-based treatments and sophisticated detection assays limit accessibility [17] [18]. |
| Expanding Therapeutic Applications: Growing use in immunotherapy regimens, stem cell therapies, and regenerative medicine [17] [18]. | Technical Complexity: Challenges in storage, transportation, and ensuring stability of cytokine therapeutics and reagents [17]. |
| Biomarker Adoption: Growing clinical acceptance of cytokine profiling for disease diagnosis, prognosis, and treatment monitoring [18]. | Regulatory Hurdles: Stringent regulatory pathways for biomarker assay validation and therapeutic approval [18]. |
| Technology Advancements: Development of multiplexed assays, point-of-care devices, and advanced analytics enabling precise cytokine measurement [19]. | Limited Reimbursement: Inadequate insurance coverage for cytokine testing procedures in some healthcare systems [17]. |
Analytical Techniques for Cytokine Detection
Accurate cytokine measurement is fundamental to both clinical diagnostics and research. The technological landscape has evolved from single-analyte approaches to sophisticated multiplex platforms.
Established Detection Methodologies
Enzyme-Linked Immunosorbent Assay (ELISA) ELISA remains the gold standard for quantitative cytokine detection due to its high specificity and sensitivity [20] [21]. The typical sandwich ELISA protocol involves:
- Coating: Immobilizing a capture antibody specific to the target cytokine onto a microplate [20].
- Blocking: Adding a protein-based blocking buffer to prevent non-specific binding [20].
- Sample Incubation: Applying standards and samples, allowing the target cytokine to bind to the capture antibody [20].
- Detection Antibody: Adding a biotin-conjugated detection antibody that binds to the captured cytokine [20].
- Signal Amplification: Incubating with streptavidin-conjugated horseradish peroxidase (HRP) [20].
- Signal Development: Adding a chromogenic substrate (e.g., TMB) and measuring the color intensity spectrophotometrically [20].
Despite its reliability, ELISA is limited to single-analyte measurement, requires relatively large sample volumes, and has a narrow dynamic range [21].
Multiplex Array Technologies Multiplex platforms address ELISA limitations by enabling simultaneous quantification of multiple cytokines from a single small-volume sample [21]. Flow cytometry-based multiplex assays (e.g., Luminex xMAP technology) use antibody-coated bead sets distinguishable by their fluorescent signatures [22] [21]. Recent innovations have simplified these assays through lyophilized reagent beads and one-step incubation protocols, reducing total assay time from over 3 hours to approximately 1.5 hours while maintaining performance comparable to conventional methods [22] [7]. This advancement simplifies reagent storage and transportation by eliminating the need for continuous cold storage [22].
Table 3: Comparison of Major Cytokine Detection Platforms
| Parameter | Traditional ELISA | Multiplex Bead Arrays | Novel CRISPR-based Sensors |
|---|---|---|---|
| Analytes per Sample | Single [21] | Up to 25+ [21] | Potentially multiplexable [16] |
| Sample Volume | High (e.g., 100μL) [21] | Low (e.g., 50μL) [21] | Very Low (potential) [16] |
| Assay Time | 4-6 hours [20] | 1.5 - 3 hours [22] | Potentially <1 hour [16] |
| Dynamic Range | Narrow [21] | Broad [21] | Not fully established |
| Throughput | Moderate | High | To be determined |
| Best Application | Targeted, single-analyte quantification | Comprehensive cytokine profiling research | Potential for point-of-care diagnostics |
Emerging Sensing Technologies
CRISPR-Assisted Cytokine Sensing CRISPR-Cas technology is emerging as a transformative tool for cytokine detection by converting protein signals into nucleic acid signals that can be amplified and detected [16]. This approach leverages the collateral cleavage activity of Cas enzymes (e.g., Cas12, Cas13), which, upon activation by a target-specific nucleic acid, indiscriminately cleave reporter molecules to generate amplified signals [16]. The key advantage lies in high sensitivity and programmability—by modifying guide RNA sequences, biosensors can be reprogrammed to detect different cytokines. This technology shows particular promise for developing cost-effective, point-of-care diagnostic devices for real-time cytokine monitoring [16].
Integrated Machine Learning Approaches Advanced data analytics are enhancing the prognostic value of cytokine measurements. Studies in COVID-19 and HBV patients have demonstrated that supervised machine learning models (logistic regression, random forest, support vector machine) can effectively predict disease severity or viral load using multi-cytokine profiling data [22]. Furthermore, unsupervised learning (t-SNE analysis) can identify distinct patient clusters based on cytokine expression patterns, providing deeper insights into disease heterogeneity [22].
Application Notes: Clinical and Research Implementation
Cytokine Monitoring in Sepsis and Critical Care
Sepsis management represents a critical application where cytokine monitoring provides significant diagnostic and prognostic value. The interleukin network is central to sepsis pathogenesis, with specific cytokines serving distinct roles in the dysregulated immune response [15]:
- Pro-inflammatory Mediators: IL-1β and IL-6 drive hyperinflammation, amplifying vascular permeability, coagulation activation, and shock. IL-6 has been validated as a robust prognostic biomarker [15].
- Anti-inflammatory Mediators: IL-10 limits tissue injury but may foster immunosuppression and secondary infections [15].
- Therapeutic Targets: IL-1 receptor antagonist (anakinra) and IL-6 receptor blockade (tocilizumab) have shown promise in selected patient subgroups, highlighting the translational potential of cytokine monitoring [15].
The following diagram illustrates the central role of interleukins in the sepsis cytokine network:
Dynamic Monitoring in Respiratory Infections
Dynamic cytokine profiling enhances the predictive accuracy of traditional severity scores in respiratory infections like community-acquired pneumonia (CAP), particularly in elderly patients. A prospective study demonstrated that:
- IL-6 Dynamics: Patients who died from CAP showed an 88% increase in IL-6 levels within 48 hours, whereas survivors showed a 49% decrease [5].
- Enhanced Prognostication: Integrating IL-6 dynamics with traditional PSI and CURB-65 scores significantly improved mortality prediction (PSI + IL-6 dynamics: AUC = 0.7676; CURB-65 + IL-6 dynamics: AUC = 0.7564) compared to scores alone [5].
This integrated approach provides a more precise risk stratification tool, enabling personalized clinical decision-making in vulnerable populations [5].
The Scientist's Toolkit: Essential Research Reagents
Successful cytokine analysis requires specialized reagents and materials. The following table details key components for establishing cytokine detection protocols:
Table 4: Essential Research Reagent Solutions for Cytokine Analysis
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Capture Antibodies (purified anti-cytokine) | Immobilizes target cytokine onto solid phase [20] | Coated at 1-4 μg/mL in binding solution (pH 9.0 or 6.0); specificity is critical [20]. |
| Detection Antibodies (biotin-conjugated) | Binds captured cytokine for detection [20] | Used at 0.5-2 μg/mL; different epitope than capture antibody required [20]. |
| Streptavidin-HRP Conjugate | Signal generation through enzyme-substrate reaction [20] | Provides amplification; requires careful titration to optimize signal-to-noise [20]. |
| Lyophilized Multiplex Beads | Multiplexed capture matrix for flow cytometry [22] | Enable one-step assays; eliminate cold chain requirements; contain pre-mixed detection antibodies [22]. |
| Chromogenic Substrates (TMB, ABTS) | Enzyme substrate for colorimetric detection [20] | TMB offers high sensitivity; stop solution required for reaction termination [20]. |
| Blocking Buffer (BSA or serum) | Prevents non-specific antibody binding [20] | 1% BSA or 10% serum in PBS; filtering removes particulates that cause background [20]. |
Experimental Protocols
Detailed Protocol: Sandwich ELISA for Cytokine Quantification
This protocol provides standardized methodology for quantitative cytokine detection using sandwich ELISA, adaptable to various cytokine targets [20].
Day 1: Coating Phase
- Dilute capture antibody to 1-4 μg/mL in binding solution (0.1 M Na₂HPO₄, pH 9.0; use pH 6.0 for mouse IL-10, MCP-1, TNF) [20].
- Add 100 μL diluted antibody to each well of an enhanced protein-binding ELISA plate.
- Seal plate to prevent evaporation and incubate overnight at 4°C.
Day 2: Assay Procedure
- Bring plate to room temperature. Remove coating solution and block with 200 μL/well blocking buffer (1% BSA or 10% serum in PBS) for 1-2 hours at room temperature [20].
- Wash plate ≥3 times with PBS/Tween-20 (0.05% Tween-20) [20].
- Add 100 μL/well of standards (serial dilutions) and samples diluted in blocking buffer with 0.05% Tween-20. Incubate 2-4 hours at room temperature or overnight at 4°C [20].
- Wash plate ≥4 times with PBS/Tween-20.
- Add 100 μL/well of biotinylated detection antibody (0.5-2 μg/mL in blocking buffer/Tween-20). Incubate 1 hour at room temperature [20].
- Wash plate ≥4 times with PBS/Tween-20.
- Add 100 μL/well of streptavidin-HRP diluted in blocking buffer/Tween-20. Incubate 30 minutes at room temperature [20].
- Wash plate ≥5 times with PBS/Tween-20.
- Add 100 μL/well of TMB substrate solution. Incubate for color development (5-30 minutes) [20].
- Stop reaction if necessary (with acid for TMB) and read optical density at appropriate wavelength (e.g., 450nm for TMB) [20].
The following workflow diagram outlines the key steps in the sandwich ELISA protocol:
Advanced Protocol: One-Step Flow Cytometry-Based Multiplex Assay
This streamlined protocol enables simultaneous quantification of 12 cytokines in a single assay with reduced hands-on time [22].
Reagent Preparation
- Utilize lyophilized reagent beads containing pre-mixed capture-antibody-modified microspheres and phycoerythrin-labeled detection antibodies [22].
- Reconstitute lyophilized beads according to manufacturer specifications.
Assay Procedure
- Add 100 μL of standard or sample to each well of a 96-well plate containing lyophilized reagent beads [22].
- Seal plate and incubate with shaking at room temperature for 1.5 hours [22].
- Wash to remove unbound components using appropriate buffer.
- Add reading buffer and analyze immediately using a flow cytometer equipped with appropriate lasers and detectors (e.g., Beckman Coulter DxFlex) [22].
- Analyze data using instrument-specific software and generate standard curves for each cytokine.
Key Advantages
- Time Efficiency: Total assay time reduced from >3 hours to 1.5 hours [22].
- Simplified Storage: Lyophilized reagents eliminate requirement for continuous cold chain [22].
- Multiplexing Capacity: Simultaneous measurement of 12 cytokines from single 100μL sample [22].
The cytokine field continues to evolve rapidly, driven by technological innovations and expanding clinical applications. Several key trends are shaping future research directions:
Integration of Advanced Analytics Machine learning algorithms applied to multiplex cytokine data are enhancing disease stratification and outcome prediction. The combination of cytokine profiling with other omics data will further advance personalized medicine approaches [22].
Point-of-Care Diagnostic Development Novel sensing technologies, particularly CRISPR-based platforms, show significant promise for developing rapid, cost-effective cytokine detection devices for clinical settings [16]. These technologies could transform critical care monitoring and therapeutic decision-making.
Therapeutic Targeting Advancements Research continues to elucidate the complex roles of specific cytokines in disease pathogenesis, enabling development of more targeted immunomodulatory therapies. Clinical trials targeting IL-10 receptor agonists for inflammatory diseases represent one such emerging approach [17].
The continued growth of cytokine-based therapeutics and diagnostics will depend on overcoming current challenges related to cost, standardization, and regulatory approval. However, the field's trajectory suggests cytokines will remain central to advancing immunology research and developing novel precision medicine interventions for complex diseases.
Platforms in Practice: From Established Immunoassays to Emerging Biosensors
In biomedical research, particularly in immunology and drug development, the precise quantification of cytokines is indispensable for understanding immune responses, disease pathogenesis, and therapeutic efficacy. Cytokines are not static biomarkers; their concentrations fluctuate dynamically in response to physiological and pathological stimuli. Traditional single-plex methods often fail to capture the complex, interconnected nature of cytokine networks. This application note details three cornerstone technologies—ELISA, Flow Cytometry, and Multiplexed Bead-Based Assays—framed within the critical context of dynamic cytokine monitoring. As demonstrated in a 2025 clinical study, integrating dynamic cytokine changes (e.g., a 49% decrease in IL-6 in survivors versus an 88% increase in non-survivors of community-acquired pneumonia) with traditional clinical scores significantly enhanced mortality prediction accuracy (AUC increased from 0.66 to 0.77) [5]. This underscores the value of precise, multi-analyte profiling for advanced risk stratification and personalized medicine.
ELISA: Quantitative Gold Standard for Cytokine Analysis
The Enzyme-Linked Immunosorbent Assay (ELISA) remains a fundamental tool for robust, quantitative protein measurement, valued for its high sensitivity and specificity [23].
Core Principles and Protocol Selection
ELISA is a plate-based assay technique for detecting and quantifying peptides, proteins, antibodies, and hormones. Its foundation is the specific binding of an antibody to an antigen, with an enzyme-linked conjugate producing a measurable signal upon substrate addition [23]. The choice of ELISA format depends on the experimental goal and sample type.
- Direct ELISA: The simplest format, where a labeled primary antibody detects immobilized antigen. It is fast but offers minimal signal amplification [23].
- Indirect ELISA: An unlabeled primary antibody is detected by a labeled secondary antibody. This offers high sensitivity and a wide range of available labeled secondary antibodies [23].
- Sandwich ELISA: Two antibodies specific to different, non-overlapping epitopes of the antigen are used. This format provides high specificity and is ideal for complex samples, as it requires no prior purification of the target antigen [24] [23].
- Competitive ELISA: Used for detecting small antigens. The signal is inversely proportional to the amount of antigen in the sample, providing high sensitivity for compositional analysis of complex mixtures [23].
Detailed Protocol: Sandwich ELISA for Cytokine Quantification
The following protocol is a general guide for a colorimetric sandwich ELISA, which is the most common format for cytokine detection [24] [23]. Optimization is required for each specific assay.
- Coating: Dilute the capture antibody in a suitable coating buffer (e.g., carbonate-bicarbonate buffer, pH 9.6). Add the solution to a 96-well polystyrene microplate and incubate overnight at 4°C.
- Washing and Blocking: Wash the plate 3 times with a wash buffer (e.g., PBS with 0.05% Tween 20). Add a blocking agent (e.g., 1% BSA, 5% non-fat dry milk in PBS) to all wells to cover any unsaturated binding sites. Incubate for 1-2 hours at room temperature.
- Sample and Standard Incubation: Wash the plate 3 times. Add prepared standards of known concentration and samples to the wells. Incubate for 2 hours at room temperature on a shaker.
- Detection Antibody Incubation: Wash the plate 3 times to remove unbound antigen. Add the enzyme-conjugated detection antibody diluted in blocking buffer. Incubate for 1-2 hours at room temperature on a shaker.
- Substrate Incubation and Signal Detection: Wash the plate 3 times. Add an enzyme-specific substrate (e.g., TMB for HRP, ABTS for HRP). Incubate for 15-30 minutes in the dark. Stop the reaction with a stop solution (e.g., 1M H2SO4 for TMB). Read the optical density immediately using a microplate reader.
Workflow and Data Interpretation
The following diagram illustrates the key steps and decision points in a sandwich ELISA workflow.
Data Analysis: ELISA data is graphed as optical density versus the log of the concentration, producing a sigmoidal curve. The concentration of unknown samples is determined by comparing their signal to the linear portion of the standard curve generated from known standards [23].
Essential Reagents for ELISA
Table 1: Key Reagent Solutions for ELISA Protocols.
| Reagent / Solution | Function / Explanation |
|---|---|
| Coated Microplate | 96-well polystyrene plates that passively bind antibodies and proteins [23]. |
| Coating Buffer | Typically carbonate-bicarbonate buffer; facilitates adsorption of the capture antibody to the plate [23]. |
| Blocking Buffer | Contains agents like BSA or casein to block non-specific binding sites, reducing background noise [24] [23]. |
| Wash Buffer | PBS with a detergent; removes unbound material, critical for reducing background [23]. |
| Coated Capture Antibody | The first layer; specifically binds the target cytokine and immobilizes it on the plate [23]. |
| Detection Antibody | Enzyme-conjugated antibody that binds a different epitope on the captured cytokine [23]. |
| Enzyme Substrate | Produces a measurable colorimetric, chemiluminescent, or fluorescent signal when acted upon by the enzyme [24]. |
Flow Cytometry: Multiparameter Single-Cell Analysis
Flow cytometry is a powerful technology that enables rapid, multi-parametric analysis of the physical and chemical characteristics of single cells or particles in suspension [25].
As cells flow past single or multiple lasers, they scatter light and may emit fluorescence from dyes or conjugated antibodies. Forward Scatter (FSC) correlates with cell size, while Side Scatter (SSC) indicates internal complexity or granularity [25]. Modern flow cytometers can measure over 30 parameters simultaneously, using an array of lasers and sensitive detectors like photomultiplier tubes (PMTs) [25]. Specialized cytometers include:
- Cell Sorters: Physically purify cell populations based on their fluorescence characteristics [25].
- Imaging Cytometers: Combine flow cytometry with fluorescence microscopy for morphological analysis [25].
- Mass Cytometers (CyTOF): Use metal-tagged antibodies and time-of-flight mass spectrometry, eliminating spectral overlap and allowing for >40 parameter analysis [25].
Protocol for Intracellular Cytokine Staining
This protocol is used to detect cytokines produced and stored within immune cells, such as T cells.
- Cell Stimulation and Culture: Isolate peripheral blood mononuclear cells (PBMCs) or other relevant cells. Stimulate cells with a mitogen (e.g., PHA), an antigen, or a cell activation cocktail (e.g., PMA/lonomycin) in the presence of a protein transport inhibitor (e.g., Brefeldin A) for 4-18 hours.
- Cell Surface Staining: Harvest cells and resuspend in FACS buffer. Add fluorescently conjugated antibodies against surface markers (e.g., CD3, CD4, CD8). Incubate for 20-30 minutes at 4°C in the dark. Wash cells to remove unbound antibody.
- Fixation and Permeabilization: Fix cells using a formaldehyde-based fixative to preserve cell structure. Permeabilize cells using a detergent-based buffer (e.g., saponin) to allow antibodies to access the intracellular space.
- Intracellular Staining: Add fluorescently conjugated antibodies against the intracellular cytokine of interest (e.g., IFN-γ, IL-2, TNF-α). Incubate for 30-60 minutes at 4°C in the dark. Wash cells thoroughly.
- Data Acquisition and Analysis: Resuspend cells in FACS buffer and acquire data on a flow cytometer. Use sequential gating strategies to identify the cell population of interest and then analyze cytokine expression within that population.
Gating Strategy for Cytokine-Producing T Cells
A logical gating strategy is essential for accurately identifying rare cytokine-producing cell subsets.
Essential Reagents for Flow Cytometry
Table 2: Key Reagent Solutions for Flow Cytometry.
| Reagent / Solution | Function / Explanation |
|---|---|
| Fluorescently Conjugated Antibodies | Antibodies against surface or intracellular targets linked to fluorochromes; enable detection of specific proteins [25]. |
| Viability Dye | Distinguishes live from dead cells; critical for excluding false-positive signals from compromised cells [26]. |
| Fixation Reagent | Stabilizes cells and inactivates pathogens; typically a formaldehyde-based solution [26]. |
| Permeabilization Buffer | A detergent-containing buffer that pokes holes in the cell membrane, allowing access to intracellular targets [26]. |
| FACS Buffer | PBS with protein and often azide; used to wash and resuspend cells during staining to maintain viability and reduce nonspecific binding. |
| Compensation Beads | Uniform particles used to capture antibodies and calculate spectral overlap (compensation) between fluorochromes in a panel [26]. |
Multiplexed Bead-Based Assays: High-Density Profiling
Multiplexed bead-based assays, such as those employing Luminex xMAP technology, revolutionize cytokine profiling by allowing the simultaneous quantification of dozens of analytes from a single small-volume sample [27].
Principle and Advantages
The core technology uses superparamagnetic beads that are color-coded with varying ratios of fluorescent dyes, creating a unique spectral signature for each bead set. Each bead set is pre-coated with a capture antibody specific to a different cytokine. This allows all bead sets to be mixed and incubated with a single sample, where each analyte binds to its specific bead [27]. Detection is achieved using a cocktail of biotinylated detection antibodies and streptavidin conjugated to phycoerythrin (PE) [27]. The instrument then identifies each bead by its color code and quantifies the amount of bound analyte by the PE fluorescence intensity.
Detailed Protocol: Luminex Assay Procedure
This protocol follows the general steps for an R&D Systems Luminex Assay [27].
- Preparation: Reconstitute and dilute all standards, the microparticle cocktail, biotinylated antibody cocktail, and streptavidin-PE according to the manufacturer's instructions.
- Sample and Bead Incubation: Add 50 µL of standard or sample to each well of a 96-well plate. Add 50 µL of the diluted microparticle cocktail to each well. Seal the plate and incubate for 2 hours at room temperature on a plate shaker (~800 rpm).
- Wash: Wash the plate 3 times using a magnetic plate washer. For each wash, remove liquid, add 100 µL of Wash Buffer, and remove again.
- Detection Antibody Incubation: Add 50 µL of the diluted biotin-antibody cocktail to each well. Cover and incubate for 1 hour at room temperature on the shaker.
- Streptavidin-PE Incubation: Wash the plate 3 times. Add 50 µL of diluted Streptavidin-PE to each well. Incubate for 30 minutes at room temperature on the shaker, protected from light.
- Readiness and Reading: Wash the plate 3 times. Add 100 µL of Wash Buffer to each well and resuspend the beads on the shaker for 2 minutes. Read the plate on a Luminex or Bio-Rad analyzer within 90 minutes.
Multiplexed Assay Workflow
The streamlined workflow of a multiplexed bead-based assay demonstrates its efficiency for high-content screening.
Comparative Analysis and Application in Dynamic Monitoring
Technology Comparison for Cytokine Sensing
The choice of technology depends on the specific research question, required throughput, number of targets, and sample volume.
Table 3: Comparative Analysis of Cytokine Sensing Technologies.
| Feature | ELISA | Flow Cytometry | Multiplex Bead-Based Assays (e.g., Luminex) |
|---|---|---|---|
| Multiplexing Capacity | Single-plex (typically) | High (10-40+ parameters) [25] | Medium-High (Up to 50 analytes) [27] |
| Sample Throughput | High (full 96-well plate) | Medium | High (96-well plate format) [27] |
| Sample Volume Required | Low-Medium (50-100 µL) | Medium (100-200 µL) | Very Low (as little as 25-50 µL) [27] |
| Primary Output | Quantitative concentration | Relative fluorescence per cell | Quantitative concentration for multiple analytes |
| Key Advantage | High sensitivity, wide dynamic range, gold standard for quantification | Single-cell resolution, functional analysis (e.g., intracellular staining) | Maximum data per sample volume, profiling of analyte networks |
| Best Suited For | Validating specific biomarker concentrations; high-throughput screening of single targets. | Deep immunophenotyping, identifying rare cell populations, analyzing cell function and signaling. | Comprehensive biomarker discovery, pathway analysis, and studies with limited sample volume. |
Application in Dynamic Cytokine Monitoring: A Case Study
The clinical relevance of dynamic cytokine monitoring is powerfully illustrated by a 2025 prospective pilot study on elderly patients with community-acquired pneumonia (CAP) [5]. The study measured multiple cytokines at admission and within 48 hours, calculating a dynamic change ratio. The key finding was that IL-6 dynamics significantly improved the prognostic accuracy of traditional severity scores (PSI and CURB-65). The mortality group showed an 88% increase in IL-6 levels over 48 hours, contrasting with a 49% decrease in survivors [5]. Integrating IL-6 dynamics with PSI improved the predictive AUC from 0.66 to 0.77 [5]. This case demonstrates how these "workhorse" technologies, when applied to serial monitoring, can yield critical insights for patient stratification and prognostication, moving beyond static snapshots to capture the biologically relevant dynamics of the immune system.
The accurate, real-time detection of cytokines is paramount for advancing research in immunology, drug development, and personalized medicine. Cytokines are central regulators of immune responses and have emerged as key biomarkers in diverse pathological conditions, including infections, autoimmune disorders, and cancer [6]. Conventional laboratory methods for cytokine detection, while accurate, often lack the speed, portability, and multiplexing capacity required for timely clinical decision-making. This application note details emerging optical biosensing modalities—Surface Plasmon Resonance (SPR), photonic crystals, and nanomaterial-enhanced biosensors—that are reshaping the landscape of cytokine sensing. These technologies enable rapid, decentralized, and sensitive detection of cytokine panels in complex biological samples, facilitating dynamic monitoring that was previously unattainable [6]. We focus on practical protocols, key performance parameters, and integration with artificial intelligence (AI) to provide researchers and drug development professionals with the tools to implement these cutting-edge technologies.
Core Sensing Technologies
Surface Plasmon Resonance (SPR) Biosensors, particularly those based on photonic crystal fiber (PCF), have become essential tools for real-time, label-free biomolecular detection [28] [29]. Their operation hinges on the excitation of surface plasmons—coherent electron oscillations at a metal-dielectric interface—which are extremely sensitive to changes in the local refractive index (RI) caused by analyte binding [28]. The integration of PCF with SPR allows for exceptional control over light guidance, dispersion management, and light confinement, making these sensors highly suitable for refractive index sensing and biomedical imaging [28].
Photonic Crystal (PhC) Biosensors are periodic dielectric or metallic-dielectric structures that can control the propagation of light [30]. They feature photonic bandgaps (PBGs)—ranges of wavelength where light propagation is forbidden. By introducing defects into the periodic lattice, light can be localized in specific regions, creating highly sensitive resonant cavities for biosensing applications [30]. Two-dimensional PhC structures, often composed of silicon rods in air or air holes in silicon, can be engineered into devices like multiplexers that also function as biosensors [30].
Nanomaterial-Enhanced Biosensors leverage the unique properties of materials like graphene, transition metal dichalcogenides (TMDCs) such as molybdenum disulfide (MoS₂), and MXenes to significantly boost the performance of traditional optical biosensors [31] [29]. Graphene, with its exceptional electrical conductivity, biocompatibility, and enormous surface-to-volume ratio, enhances SPR sensitivity and resolution to unprecedented levels [31]. Hybrid nanostructures, such as MoS₂-graphene heterostructures and graphene quantum dot-enhanced SPR, are pushing the boundaries of detection limits, enabling real-time biomolecular interaction studies at femtomolar or even attomolar concentrations [31].
Quantitative Performance Comparison
The table below summarizes the performance metrics of various advanced optical biosensors relevant to cytokine and biomarker detection.
Table 1: Performance Metrics of Emerging Optical Biosensors
| Sensor Technology | Target Analyte | Sensitivity (nm/RIU) | Figure of Merit (RIU⁻¹) | Detection Limit | Reference |
|---|---|---|---|---|---|
| D-shaped PCF-SPR (Au/TiO₂) | Cancer Cells (Multi-type) | 42,000 | 1393.1 | Not Specified | [32] |
| PCF-SPR (Au/MXene) | General Bio-sensing | 64,600 | Not Specified | Not Specified | [32] |
| AI-enabled Multiplex POC | Cytokines | 0.01-100 pg/mL (Concentration) | Not Specified | Not Specified | [6] |
| 2:1 PhC Multiplexer | Cholesterol | 2,673.4 | 80.9-82.1 | 0.00125-0.00143 RIU | [30] |
| 2:1 PhC Multiplexer | Creatinine | 3,582.7 | 199.0-201.3 | 4.98e-4 - 5.26e-4 RIU | [30] |
| D-shaped PCF (Pentagonal) | General Bio-sensing | 27,800 | Not Specified | Not Specified | [33] |
Table 2: Key Sensing Parameters for PCF-SPR Biosensors
| Parameter | Symbol | Description | Importance |
|---|---|---|---|
| Wavelength Sensitivity | WS | Shift in resonance wavelength per refractive index unit (nm/RIU) | Determines the sensor's ability to detect small RI changes. |
| Amplitude Sensitivity | AS | Change in resonance amplitude per RIU (RIU⁻¹) | An alternative interrogation method. |
| Figure of Merit | FOM | Ratio of sensitivity to resonance peak width (RIU⁻¹) | Measures overall sensor performance and resolution. |
| Confinement Loss | CL | Attenuation of light due to leakage (dB/cm) | Affects signal clarity and detection accuracy. |
| Quality Factor | Q | Ratio of resonant wavelength to peak width (λ₀/Δλ) | Indicates the sharpness and quality of the resonance. |
Experimental Protocols
Protocol: D-Shaped PCF-SPR Sensor for Biomarker Detection
This protocol outlines the methodology for utilizing a D-shaped photonic crystal fiber Surface Plasmon Resonance (PCF-SPR) sensor, optimized for the detection of biomarkers such as cancer cells [32] or cytokines [6].
1. Sensor Preparation and Functionalization
- Sensor Chip: Obtain a D-shaped PCF sensor coated with a plasmonic layer (e.g., Gold, 40-50 nm) and a sensitivity-enhancing layer (e.g., TiO₂, 10-15 nm) [32].
- Surface Cleaning: Mount the sensor in the flow cell and rinse the surface with ethanol (70%) and deionized water for 5 minutes each at a flow rate of 20 µL/min.
- Functionalization: For cytokine detection, immobilize a specific capture element (e.g., an antibody or aptamer) onto the gold surface. This can be achieved by first creating a self-assembled monolayer (SAM) of carboxylated alkanethiols (e.g., 11-MUA) via immersion for 12 hours, followed by activation with a mixture of EDC and NHS for 30 minutes. Finally, inject the solution of the capture antibody (10-50 µg/mL in 10 mM acetate buffer, pH 5.0) over the surface for 1 hour [6] [29].
2. Instrument Setup and Calibration
- Optical System: Assemble the setup comprising a tunable laser source (visible to near-infrared range), a polarizer to ensure transverse-magnetic (TM) polarized light, an SMF-28 optical fiber for light transmission, a microfluidic flow cell housing the sensor, and an optical spectrum analyzer (OSA) [32].
- Fluidics System: Connect a programmable syringe pump to the flow cell via tubing to control the introduction and removal of the analyte solution at a stable pressure [32].
- Baseline Establishment: Flow a continuous stream of running buffer (e.g., PBS, pH 7.4) over the sensor until a stable baseline signal is observed on the OSA, indicating a stable refractive index.
3. Sample Introduction and Data Acquisition
- Sample Injection: Replace the running buffer with the sample solution (e.g., serum, cell lysate, or purified analyte) without introducing air bubbles. The analyte binds to the capture element, causing a local change in the refractive index.
- Real-time Monitoring: Monitor the output spectrum from the OSA in real-time. The binding event will cause a shift in the resonance wavelength (dip in the transmission spectrum).
- Regeneration: After the binding signal saturates, flush the surface with a regeneration solution (e.g., 10 mM Glycine-HCl, pH 2.0) to dissociate the bound analyte and regenerate the sensor surface for the next cycle. Re-equilibrate with the running buffer.
4. Data Analysis
- Sensitivity Calculation: Calculate the wavelength sensitivity (WS) using the formula: ( WS = \frac{\Delta \lambda}{\Delta n} ) nm/RIU, where ( \Delta \lambda ) is the resonance wavelength shift and ( \Delta n ) is the change in refractive index [30].
- Binding Kinetics: If performing a concentration series, the rate of resonance shift can be analyzed to determine association ((k{on})) and dissociation ((k{off})) rate constants, and the equilibrium dissociation constant ((K_D)).
Diagram 1: SPR Sensor Experimental Workflow. This flowchart outlines the key steps for operating a D-shaped PCF-SPR biosensor, from preparation to data analysis.
Protocol: Cytokine Detection using AI-Enhanced Multiplexed Biosensing
This protocol describes a framework for leveraging artificial intelligence to enhance the performance of multiplexed optical biosensors for cytokine detection at the point-of-care [6].
1. Biosensor Platform Configuration
- Platform Selection: Employ a multiplexed optical biosensing platform (e.g., based on SPR, fluorescence, or colorimetric detection) capable of simultaneously detecting a panel of cytokines (e.g., IL-6, IL-10, TNF-α) from a single small-volume sample (1-50 µL) [6].
- Chip Functionalization: Pattern the sensor chip with an array of distinct capture probes (antibodies, aptamers) specific to the target cytokines. Each spot corresponds to a specific cytokine.
2. Data Acquisition and Pre-processing
- Sample Running: Apply the clinical sample (e.g., blood, plasma) to the sensor and allow the assay to run, typically resulting in results within 5-30 minutes [6].
- Signal Collection: The biosensor output, which may be spectral data (wavelength shifts), image data (colorimetric changes), or intensity data (fluorescence), is collected by the built-in optical reader.
- Data Cleaning: The raw data is automatically pre-processed to reduce noise, correct for baseline drift, and normalize signals.
3. AI/ML-Powered Analysis
- Model Application: Process the cleaned data using a pre-trained machine learning model. Common models used include Convolutional Neural Networks (CNNs) for image-based data or decision-tree models for feature-based data [6].
- Prediction and Quantification: The AI model outputs the calibrated concentration for each cytokine in the panel, along with uncertainty estimates. These systems can achieve limits of detection as low as 0.01-100 pg/mL, with dynamic ranges spanning 3-4 orders of magnitude [6].
4. Clinical Interpretation and Action
- Decision Support: The quantified results are presented to the clinician via a user-friendly interface, often with interpretive comments or flags based on established reference ranges.
- Model Retraining (Ongoing): As more clinical data is accumulated, the AI models can be periodically retrained to improve their accuracy, generalizability, and predictive power.
Diagram 2: AI-Enhanced Cytokine Sensing Dataflow. This diagram illustrates the integration of hardware and AI analytics for multiplexed cytokine detection.
The Scientist's Toolkit: Research Reagent Solutions
The following table lists essential materials and their applications in the development and operation of advanced optical biosensors for cytokine and biomarker research.
Table 3: Essential Research Reagents and Materials for Advanced Optical Biosensing
| Item/Category | Specific Examples | Function/Application | Context/Note |
|---|---|---|---|
| Plasmonic Materials | Gold (Au), Silver (Ag) | Forms the active layer for SPR excitation. Au offers high stability; Ag offers sharper resonance [28] [32]. | The foundational material for SPR sensors. |
| 2D Materials & Nanocoatings | Graphene, MoS₂, MXene (Ti₃C₂Tₓ), TiO₂ | Enhances sensitivity, protects the metal layer, and provides a high surface area for biomolecule immobilization [31] [29] [32]. | Used to create hybrid, high-performance sensor designs. |
| Photonic Crystal Substrates | Silicon Rods (in air), PCF with hexagonal/elliptical air holes | Provides the structured medium for light confinement and manipulation, enabling precise control over optical properties [28] [30]. | The backbone of PhC and PCF-SPR sensors. |
| Capture Molecules | Cytokine-specific Antibodies, Aptamers | Serves as the biorecognition element that specifically binds to the target cytokine, providing selectivity [6] [29]. | Critical for the specificity of the biosensor. |
| Immobilization Chemistry | Carboxylated Alkanethiols (e.g., 11-MUA), EDC/NHS crosslinkers | Creates a stable, functional layer on the sensor surface for covalent attachment of capture molecules [29]. | Ensures robust and oriented probe immobilization. |
| Buffer Systems | Phosphate Buffered Saline (PBS), Acetate Buffer | Provides a stable ionic and pH environment for biomolecular interactions during sensing and surface functionalization [32]. | Essential for maintaining bioactivity. |
| Regeneration Solutions | Low pH Glycine-HCl, High pH NaOH | Dissociates bound analyte from the capture probe without damaging it, allowing for sensor reuse [29]. | Enables multiple analysis cycles with the same sensor chip. |
The convergence of SPR, photonic crystal technology, and nanomaterials is creating a new generation of biosensors with transformative potential for cytokine sensing and dynamic monitoring. These platforms offer the high sensitivity, specificity, and multiplexing capacity required to decipher complex immune signaling in real-time. The integration of artificial intelligence further augments their analytical performance, enabling intelligent signal processing and automated decision-making at the point of care [6] [34]. While challenges in fabrication cost, sensor reproducibility, and clinical validation remain, the protocols and technologies outlined in this document provide a robust foundation for researchers and drug developers to advance the field of precision medicine and immune monitoring.
T-cell engagers (TCEs) are an emerging class of immunotherapeutic agents designed to redirect the host's immune system against tumor cells by bridging T lymphocytes with cancer cells, generating an immunologic synapse that leads to potent immune-mediated tumor destruction [35]. Despite their remarkable clinical efficacy, particularly in hematologic malignancies, TCE therapies are commonly accompanied by excessive cytokine production and the risk of Cytokine Release Syndrome (CRS), a systemic inflammatory response that can range from mild symptoms to life-threatening multi-organ dysfunction [36] [37]. The first dose of CD3-engaging bispecific antibody therapy presents the highest risk for CRS, termed the "first-dose effect," with mechanisms rooted in distinct T-cell biology between initial and subsequent exposures [36]. The timely detection and prediction of severe CRS are therefore crucial for managing patient safety and enabling the full therapeutic potential of TCEs.
Pathophysiology and Key Biomarkers of CRS
CRS arises as a direct consequence of immune system overactivation following TCE administration. When TCEs bridge T-cells and tumor cells, they trigger T-cell activation, proliferation, and the release of inflammatory cytokines, culminating in a potentially dangerous positive feedback loop [38]. This process involves not only effector T-cells but also bystander immune cells, particularly monocytes and macrophages, which amplify the inflammatory cascade [36] [38].
The cytokine profiles involved in TCE-mediated CRS encompass a broad spectrum of pro-inflammatory and immunomodulatory factors. Research has identified several key cytokines that serve as critical biomarkers for CRS severity and progression:
- IL-6: Regarded as a principal cytokine driving CRS, instigating a proinflammatory signaling cascade that underpins several severe CRS symptoms [39].
- IFN-γ: A key effector cytokine released by activated T-cells that contributes to the inflammatory cascade [39] [40].
- IL-2: Notably rises at an earlier stage of severe CRS and has potential as the most effective cytokine for promptly detecting condition onset [39].
- IL-10: An immunomodulatory cytokine that increases significantly during CRS and serves as a predictive biomarker [39] [40].
- IL-1, TNF-α, GM-CSF: Additional inflammatory cytokines that contribute to the CRS pathophysiology [38].
In addition to cytokine biomarkers, conventional clinical biomarkers are also elevated in CRS and provide valuable monitoring parameters:
- C-reactive Protein (CRP): Consistently elevated in patients experiencing CRS [40] [38].
- Ferritin: Significantly increased, with peak levels highly associated with severe CRS [40].
- Lactate Dehydrogenase (LDH): Reflects tissue injury and tumor lysis, with elevated levels correlated with higher-grade CRS [40].
Table 1: Key Biomarkers for CRS Detection and Monitoring
| Biomarker Category | Specific Biomarkers | Clinical Significance | Timing Characteristics |
|---|---|---|---|
| Core Cytokines | IL-6, IFN-γ, IL-2, IL-10 | Prediction of CRS severity and early detection | IL-2 rises early; others peak with severe CRS |
| Inflammatory Mediators | CRP, Ferritin | Monitoring CRS progression and severity | Elevations correspond with clinical symptoms |
| Tissue Damage Indicators | LDH, AST, ALT, Creatinine | Assessment of organ dysfunction | Later elevations indicate established toxicity |
| Hematological Factors | Lymphocyte count, Neutrophil count | Enhancement of predictive models | Fluctuations correspond with T-cell activation |
Predictive Models and Analytical Approaches
Decision Tree Predictive Models
Recent advances in CRS biomarker research have enabled the development of predictive models that can stratify patients according to their risk of developing severe CRS. A 2024 study developed a decision tree model incorporating lymphocyte counts, IL-2, and IL-6 levels that achieved an accuracy of 85.11% (95% CI = 0.763–0.916) for early prediction of severe CRS, with validation in an independent cohort showing 74.47% accuracy (95% CI = 0.597–0.861) [39]. This model demonstrates the power of combining multiple biomarker classes for enhanced predictive performance.
Another study analyzing 202 patients who received CAR-T cell therapy developed decision tree models to predict the timing of severe CRS using same-day, day-ahead, and initial value predictions [40]. These models identified that peak levels of 25 clinical factors, including IFN-γ, IL-6, IL-10, ferritin, and D-dimer, were highly associated with severe CRS after T-cell engaging therapies [40].
Single-Cell Insights into CRS Mechanisms
Cutting-edge single-cell multi-omics approaches have revealed fundamental biological mechanisms underlying the "first-dose effect" in TCE therapies. Research comparing initial versus subsequent CD3/CD20 bispecific antibody treatment demonstrated:
- In initial treatment: T effector memory (Tem) cells are the primary responders, producing moderate levels of cytolytic molecules and high levels of cytokines [36].
- In subsequent treatment: A new population of high TCF7 expressing central memory CD8+ cells (CD8-Tcm-TCF7) emerges as the primary responding population, producing a shifted balance with high cytolytic gene transcription (GZMB) and low cytokine gene transcription (TNF-α and IFN-γ) [36].
This fundamental shift in responding T-cell populations explains why CRS risk is primarily limited to the initial dose of TCE therapy and suggests that tumor killing capacity and cytokine production can be uncoupled in different T-cell populations [36].
Diagram 1: Differential T-cell Response to Initial vs. Subsequent TCE Treatment
Experimental Protocols for CRS Biomarker Detection
Comprehensive Cytokine Monitoring Protocol
Objective: To quantitatively measure cytokine levels in patient serum for early detection and monitoring of CRS severity.
Materials and Reagents:
- Cytometric Bead Array (CBA) Human Th1/Th2/Th17 Cytokine Kit (BD Biosciences) for simultaneous detection of IL-2, IL-4, IL-6, IL-10, IL-17A, TNF-α, and IFN-γ [39]
- Flow cytometry instrument (e.g., BD FACS Canto II)
- Serum collection tubes
- Standard curve calibrators
- Assay buffer and wash buffer
Procedure:
- Sample Collection: Collect peripheral blood serum before TCE infusion, then daily for a minimum of two weeks post-treatment [39].
- Sample Preparation: Centrifuge blood samples at 1000-2000 × g for 10 minutes. Aliquot serum and store at -80°C if not testing immediately.
- Assay Setup: Prepare capture bead mixtures according to manufacturer instructions. Add 50μL of mixed capture beads to each assay tube.
- Standard Curve Preparation: Serially dilute cytokine standards to generate a 7-point standard curve.
- Incubation: Add 50μL of serum sample or standard to each tube, followed by 50μL of PE detection reagent. Incubate for 3 hours at room temperature protected from light.
- Washing and Acquisition: Wash beads with wash buffer, resuspend in assay buffer, and acquire on flow cytometer.
- Data Analysis: Use flow cytometry analysis software to determine cytokine concentrations from standard curves.
Timeline Considerations: For predictive modeling, analyze samples at three critical timepoints: (1) pre-infusion baseline, (2) fever onset, and (3) peak CRS symptoms [39].
Integrated CRS Risk Assessment Protocol
Objective: To combine cytokine data with clinical parameters for comprehensive CRS risk stratification.
Materials and Reagents:
- Automated hematology analyzer for complete blood count with differential
- Clinical chemistry analyzer for CRP, LDH, ferritin
- Cytokine detection system (as above)
- Electronic data capture system for clinical symptoms
Procedure:
- Clinical Parameter Monitoring:
- Record vital signs (temperature, blood pressure, respiratory rate, oxygen saturation) every 4-8 hours during initial treatment phase
- Document CRS symptoms according to ASTCT consensus criteria [39]
- Laboratory Assessment:
- Perform daily complete blood count with emphasis on lymphocyte and neutrophil counts [39]
- Measure CRP, ferritin, LDH daily during the first week, then as clinically indicated
- Data Integration:
- Input cytokine levels (IL-2, IL-6, IFN-γ, IL-10) and lymphocyte counts into decision tree algorithm [39]
- Calculate CRS risk score using validated model parameters
- Risk Stratification:
- High-risk patients: Implement intensive monitoring and consider preemptive interventions
- Moderate-risk patients: Continue standard monitoring frequency
- Low-risk patients: Maintain routine surveillance
Table 2: CRS Biomarker Monitoring Schedule
| Time Point | Cytokine Panel | Clinical Biomarkers | Hematological Parameters | Clinical Assessment |
|---|---|---|---|---|
| Baseline (Pre-treatment) | X | X | X | X |
| Daily (Days 1-7) | X | X | X | X |
| Fever Onset | X (STAT) | X (STAT) | X | X (q4h vitals) |
| Clinical Deterioration | X (STAT) | X (STAT) | X (STAT) | X (continuous monitoring) |
| Weekly (After Day 7) | X | X | X | X |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for CRS Detection Studies
| Reagent/Category | Specific Examples | Application in CRS Research |
|---|---|---|
| Cytokine Detection Kits | CBA Human Th1/Th2/Th17 Cytokine Kit (BD) | Multiplex cytokine measurement for CRS biomarker identification [39] |
| Flow Cytometry Instruments | BD FACS Canto II | Analysis of immune cell populations and cytokine bead arrays [39] |
| T-cell Engaging Reagents | CD3/CD20 Bispecific Antibody | In vitro modeling of TCE therapy and CRS mechanisms [36] |
| Single-Cell Analysis Platforms | 10x Genomics Single Cell Multi-omics | Deep profiling of T-cell responses to initial vs. subsequent TCE exposure [36] |
| Tyrosine Kinase Inhibitors | Dasatinib | Modulation of T-cell activation to uncouple cytotoxicity from cytokine release [36] |
| Clinical Chemistry Analyzers | CRP, LDH, Ferritin assays | Monitoring conventional inflammatory biomarkers in CRS [40] |
Technological Integration and Future Directions
The evolving landscape of CRS detection is increasingly incorporating advanced computational approaches and novel sensing technologies. Artificial intelligence (AI) is accelerating TCE discovery by identifying favourable epitope interactions, reducing immunogenicity risks, and enhancing overall design efficiency [37]. Future developments in CRS monitoring will likely include:
- Real-time cytokine sensors for continuous monitoring of key biomarkers
- Point-of-care testing platforms enabling rapid bedside assessment of CRS risk
- Multi-omics integration combining transcriptomic, proteomic, and clinical data for personalized risk prediction
- Advanced predictive algorithms incorporating temporal biomarker patterns for earlier intervention
The integration of these technologies with the biomarker panels and experimental protocols described herein will ultimately enhance the safety profile of TCE therapies, enabling their full therapeutic potential while minimizing the risks associated with cytokine release syndrome.
Application Notes
The development of orthogonal synthetic biosensors represents a paradigm shift in cellular engineering, enabling therapeutic cells to detect disease-specific cues and execute customized responses independent of native signaling pathways. Unlike conventional chimeric antigen receptors (CARs) that rely on endogenous signaling, orthogonal biosensors operate through self-contained mechanisms, minimizing crosstalk and enabling sophisticated computation of disease signals within complex biological environments [14] [41]. This technology is particularly valuable for cancer immunotherapy, where precision targeting remains a significant challenge.
The Modular Extracellular Sensor Architecture (MESA) platform provides a foundational framework for constructing these biosensors. By integrating naturally evolved receptor-ligand interactions with synthetic signaling components, researchers have created a new class of Natural Ectodomain (NatE) MESA receptors that combine the sophisticated sensing capabilities of natural systems with the programmability of synthetic biology [14] [42]. This approach allows bioengineers to co-opt natural cytokine receptor ectodomains—the portions that first contact external signals—and rewire them to control user-defined therapeutic outputs [41].
Key Applications in Therapeutic Cell Engineering
Tumor Microenvironment Sensing: NatE MESA receptors can be engineered to detect immunosuppressive cytokines such as interleukin-10 (IL-10) that are upregulated in the tumor microenvironment (TME). This enables T cells to sense and respond to these cues with customized transcriptional outputs that enhance CAR-T cell activity [14]. For example, engineered T cells can be programmed to activate protective pathways only when they encounter both a tumor antigen and specific TME signals, thereby increasing specificity and reducing off-target effects.
Multi-Cue Integration and Logic Gating: A particularly powerful application involves multiplexing NatE MESA receptors to implement Boolean logic operations. Cells can be programmed to activate therapeutic responses only when specific combinations of signals are present (AND logic) or when certain signals are absent (NOT logic) [14] [41]. This allows engineered therapies to distinguish more precisely between diseased and healthy tissue based on complex molecular fingerprints rather than single markers.
Dynamic Response Programming: Beyond simple sensing, these biosensors enable dynamic control of therapeutic functions. Engineered cells can be designed to release immunomodulatory molecules, activate proliferation pathways, or induce suicide switches in response to specific cytokine concentrations, creating "smart" therapies that adapt to their environment [41].
Table 1: Natural Cytokine Receptors Converted into NatE MESA Biosensors
| Natural Receptor | Ligand Sensed | Receptor Class | Signaling Mechanism | Therapeutic Context |
|---|---|---|---|---|
| VEGFR1/VEGFR2 | VEGF-A165/VEGF-A121 | Receptor tyrosine kinase | Homo/heterodimerization | Tumor angiogenesis, TME sensing |
| IL-10Rα/IL-10Rβ | IL-10 | Type II cytokine receptor | Heterodimerization | Immunosuppressive cue detection |
| TNFR1/TNFR2 | TNF-α | TNF receptor superfamily | Trimerization | Inflammation sensing |
| TGFβR1/TGFβR2 | TGF-β | Serine/threonine kinase receptor | Heterotetramerization | Tumor microenvironment |
Experimental Protocols
Protocol: Engineering and Testing VEGF NatE MESA Receptors
Receptor Design and Assembly
Principle: Convert natural VEGF receptors into orthogonal biosensors by fusing their ectodomains with MESA intracellular signaling components while systematically evaluating domain swapping strategies [14].
Materials:
- DNA Constructs: Expression vectors encoding receptor chains (NTEVp and CTEVp) with modular domains
- Cell Line: HEK293 cells or primary human T cells for functional testing
- Ligands: Recombinant VEGFA165 and VEGFA121 isoforms
- Detection Reagents: Flow cytometry antibodies for surface expression validation, Western blot reagents
Procedure:
- Domain Organization: Design receptor chains with the following architecture:
- NTEVp Chain: Native signal sequence → VEGFR2 ectodomain → Native TMD and JMD or CD28 TMD → N-terminal split TEV protease (75S;190K mutant)
- CTEVp Chain: Native signal sequence → VEGFR1 ectodomain → Native TMD and JMD or CD28 TMD → C-terminal split TEV protease → Synthetic transcription factor (ZF domain)
Surface Expression Validation:
- Transfect HEK293 cells with receptor chain plasmids
- After 48 hours, detach cells and stain with anti-VEGFR1 or anti-VEGFR2 antibodies conjugated to fluorophores
- Analyze surface expression using flow cytometry
- Confirm full-length receptor expression by Western blot under reducing conditions [14]
Ligand-Inducible Signaling Assessment:
- Cotransfect cells with both receptor chains and a ligand-encoding plasmid (autocrine stimulation)
- Include a reporter construct with the synTF-responsive promoter driving fluorescent protein expression
- Measure fluorescence output after 72 hours using flow cytometry or plate cytometry
- Compare to negative controls (receptor chains without ligand)
Dose-Response Characterization:
- Transfer receptor-expressing cells to plates with titrated doses of recombinant VEGF (0.1-100 ng/mL)
- Measure signaling output after 24-48 hours of ligand exposure
- Calculate fold induction relative to no-ligand controls [14]
Troubleshooting:
- High Background Signaling: If ligand-independent activation is observed, consider replacing CD28 TMD with native TMD or introducing point mutations to reduce aggregation propensity [14]
- Low Surface Expression: Optimize signal sequences (test CD8α or IgG VH-derived sequences) and verify proper protein folding
- Poor Induction: Tune split protease reconstitution propensity by testing different TEVp mutants or adjusting linker lengths between domains
Protocol: Implementing Logic Gates with Multiplexed NatE MESA
Two-Input AND Gate Configuration
Principle: Engineer T cells to activate therapeutic outputs only when two distinct tumor microenvironment cues are simultaneously detected [14] [41].
Materials:
- Primary Human T Cells: Isolated from donor blood
- NatE MESA Pairs: Two orthogonal receptor systems sensing different ligands (e.g., VEGF and IL-10)
- Gene Delivery System: Lentiviral or retroviral vectors for stable expression
- Output Reporter: Therapeutic gene (e.g., IL-12, CD40L) under control of a synTF-responsive promoter
Procedure:
- Receptor Design for Orthogonality:
- Select two NatE MESA receptors with different cytokine specificities (e.g., VEGFR-based and IL-10R-based)
- Ensure split protease systems are orthogonal—each TEVp pair should only reconstitute with its cognate partner
- Design synTFs with distinct DNA-binding specificities (e.g., different ZF domains)
Logic Gate Assembly:
- Engineer an output promoter that requires both synTFs for activation (composite promoter with adjacent distinct binding sites)
- Clone both complete receptor systems and the output construct into a single viral vector using T2A or P2A self-cleaving peptides
Functional Validation:
- Transduce primary T cells with the logic gate construct
- Stimulate with: (1) Ligand A alone, (2) Ligand B alone, (3) Both ligands, (4) No ligand
- Measure output gene expression (mRNA by qPCR or protein by ELISA/flow cytometry) after 24-48 hours
- Calculate fold induction for each condition
Therapeutic Efficacy Testing:
- Co-culture engineered T cells with target tumor cells in the presence of different ligand combinations
- Measure tumor cell killing (e.g., via luciferase reporter or flow cytometry-based cytotoxicity assays)
- Assess selective activation by comparing cytotoxicity in conditions with complete vs. incomplete signal combinations
Signaling Pathway and Mechanism Visualization
NatE MESA Receptor Signaling Mechanism
Multi-Cue Logic Gating with NatE MESA
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Reagents for NatE MESA Engineering
| Reagent/Category | Specific Examples | Function & Application | Key Characteristics |
|---|---|---|---|
| Natural Ectodomains | VEGFR1, VEGFR2, IL-10Rα/β, TNFR1/2, TGFβR1/2 | Ligand recognition domain providing specificity | Define sensing capability; influence surface expression and ligand affinity |
| Split Protease Systems | TEVp mutant 75S;190K | Intracellular signaling module; reconstitutes upon ligand binding | Orthogonal to native pathways; tunable cleavage kinetics |
| Synthetic TFs | Zinc finger (ZF) domains fused to VP64/p65AD | Transcriptional activation of output genes | Customizable DNA-binding specificity; modular transactivation domains |
| Transmembrane Domains | Native TMD/JMD, truncated CD28 TMD | Membrane anchoring and influence on receptor association | Impact background signaling and surface expression |
| Signal Sequences | Native, CD8α, IgG VH | Guide receptor trafficking and surface expression | Critical for proper folding and membrane localization |
| Output Reporters | Fluorescent proteins (GFP, mCherry), luciferase | Quantitative assessment of receptor activation | Enable high-throughput screening and dose-response characterization |
| Therapeutic Payloads | Cytokines (IL-12), costimulatory molecules, CARs | Customized functional outputs for cell therapies | Determines therapeutic mechanism of action |
Performance Characterization Data
Table 3: Quantitative Performance of Representative NatE MESA Receptors
| Receptor Configuration | Ligand | Background Signal | Max Induction | Fold Induction | EC₅₀ | Key Design Features |
|---|---|---|---|---|---|---|
| VEGFR2(N)-VEGFR1(C) | VEGFA165 | Low | ~45% activation | 8.5 | ~5 nM | Native TMD, heterodimeric |
| VEGFR1(N)-VEGFR1(C) | VEGFA165 | Medium | ~35% activation | 4.2 | ~12 nM | Homodimeric, CD28 TMD |
| VEGFR2(N)-VEGFR2(C) | VEGFA121 | Low | ~52% activation | 10.3 | ~3 nM | Isoform-specific response |
| IL-10Rα(N)-IL-10Rβ(C) | IL-10 | Low | ~38% activation | 7.8 | ~8 nM | Heterodimeric, immunosuppressive cue |
| AND Gate (VEGF + IL-10) | Both cues | Minimal | ~48% activation | 25.6 | N/A | Logic operation, high specificity |
The data demonstrate that careful optimization of receptor configuration, transmembrane domains, and protease components enables the development of NatE MESA receptors with varying performance characteristics suitable for different therapeutic applications. The logic gate implementation shows dramatically improved fold induction through signal integration, highlighting the potential for enhanced specificity in complex disease environments [14].
Navigating Analytical Challenges: Sensitivity, Multiplexing, and Throughput
Overcoming Sensitivity Limits and Narrow Dynamic Ranges
The accurate measurement of cytokines is fundamental to understanding immune responses in contexts ranging from infectious diseases and autoimmune disorders to cancer [6]. However, conventional cytokine detection methods, particularly enzyme-linked immunosorbent assays (ELISAs), are constrained by significant limitations in sensitivity and dynamic range. These constraints can obscure the true dynamics of cytokine secretion, which is transient, cell-subset-dependent, and often occurs at low, yet biologically critical, concentrations [20]. Overcoming these analytical hurdles is paramount for advancing research, drug development, and clinical diagnostics. This application note details the limitations of traditional workflows and presents advanced protocols and technologies designed to push the boundaries of what is measurable in cytokine sensing.
Quantitative Comparison of Cytokine Sensing Technologies
The evolution of cytokine sensing platforms has led to dramatic improvements in performance. The table below summarizes key metrics for traditional and advanced technologies.
Table 1: Performance Metrics of Cytokine Detection Platforms
| Technology | Typical Limit of Detection (LOD) | Dynamic Range | Sample Volume | Time to Result | Multiplexing Capacity |
|---|---|---|---|---|---|
| Traditional Sandwich ELISA [43] [20] | ~5-10 pg/mL [20] | ~2 orders of magnitude | 50-100 µL [43] | 6-8 hours to overnight [20] | Single-plex |
| Sequential ELISA [43] | Similar to standard ELISA | Similar to standard ELISA | Re-used sample (limited volume) | Significantly longer than single-plex | Low-plex (Limited by sample volume) |
| AI-Enabled Multiplex POC Biosensors [6] | 0.01-100 pg/mL | 3-4 orders of magnitude | 1-50 µL | 5-30 minutes | High-plex (e.g., 17+ analytes) |
| Implantable 'Active-Reset' Sensors [8] | Demonstrated for IL-6, TNF-α in vivo | Enabled continuous, real-time monitoring | Minimal (interstitial fluid) | Continuous, real-time | Low-plex (proof-of-concept) |
Advanced Experimental Protocols
Protocol: Checkerboard Titration for ELISA Optimization
A critical step in developing a sensitive and robust sandwich ELISA is optimizing the concentrations of the capture and detection antibodies. This protocol ensures maximum signal-to-noise ratio [43].
Key Research Reagent Solutions:
- Matched Antibody Pairs: Monoclonal capture antibody and biotinylated detection antibody.
- Recombinant Cytokine Standard: Purified protein of known concentration for generating a standard curve.
- Blocking Buffers: Solutions like Blotto, Casein, or BSA in PBS to prevent non-specific binding.
- Streptavidin-HRP Conjugate: Enzyme conjugate for signal amplification.
- Chromogenic Substrate: TMB or ABTS, which produces a measurable color change upon reaction with HRP.
Methodology:
- Day 1: Coating. Prepare four dilutions of the capture antibody in phosphate-buffered saline (PBS). Coat a 96-well high-binding microplate with 50 µL/well of each dilution, typically in a checkerboard pattern. Incubate overnight at 4°C.
- Day 2: Blocking and Assay. Wash the plate with PBS/Tween-20. Block non-specific binding by adding 150 µL/well of blocking buffer and incubating for 1 hour at ambient temperature.
- Standard and Sample Incubation. Prepare a dilution series of the cytokine standard (e.g., high, medium, low, zero). Wash the plate, add 50 µL/well of each standard, and incubate for 2 hours.
- Detection. Prepare three dilutions of the biotinylated detection antibody. Wash the plate and add 50 µL/well of the detection antibody, incubating for 2 hours.
- Signal Amplification and Development. Wash the plate and add streptavidin-HRP conjugate for 30 minutes. After a final wash, add TMB substrate and incubate in the dark for 20-30 minutes. Stop the reaction with sulfuric acid and read the optical density (OD) at 450 nm.
- Analysis. The optimal antibody combination is identified as the pair of concentrations that produces the highest OD for the low standard while maintaining a low background for the zero standard.
Diagram 1: Checkerboard titration workflow for ELISA optimization.
Protocol: Multiplexed Cytokine Detection via Printed Array ELISA
For analyzing multiple cytokines from a single, small-volume sample, a multiplex ELISA using an antibody array is a superior alternative to sequential ELISAs [43].
Key Workflow Modifications from Standard ELISA:
- Array Printing: A non-contact spotter (e.g., a piezoelectric printer) is used to "print" distinct capture antibodies onto the bottom of each well of a microplate, creating an array of spots within each well.
- Assay Execution: The general steps of a sandwich ELISA (blocking, sample incubation, detection) are performed on the entire plate well, simultaneously capturing all target cytokines on their specific antibody spots.
- Detection and Imaging: Instead of colorimetric detection with HRP, a streptavidin-conjugated infrared (IR) dye is used with the biotinylated detection antibody. A high-resolution IR scanner (e.g., Li-Cor) then detects and quantifies the signal from each individual spot.
- Critical Consideration: An automatic plate washer is essential to avoid physical disruption of the printed spots during washes.
Diagram 2: Multiplex ELISA using a printed antibody array.
Next-Generation Technologies for Dynamic Monitoring
AI-Enhanced Point-of-Care Biosensing
The convergence of multiplexed biosensing with artificial intelligence represents a paradigm shift. Modern AI-enabled point-of-care (POC) platforms now achieve limits of detection as low as 0.01 pg/mL with a dynamic range spanning 3-4 orders of magnitude using just 1-50 µL of sample [6]. Machine learning algorithms, including convolutional neural networks (CNNs) and decision-tree models, are integrated to perform autonomous signal processing, provide calibrated predictive outputs, monitor sensor drift, and estimate uncertainty. This AI integration enhances analytical performance and interpretability, moving beyond the capabilities of traditional centralized testing [6].
Implantable 'Active-Reset' Sensors for Real-TimeIn VivoMonitoring
A groundbreaking advancement for overcoming temporal resolution limits is the development of implantable, reagent-less protein sensors. This technology, inspired by continuous glucose monitors, uses microneedle-shaped electrodes implanted under the skin to monitor cytokine levels in interstitial fluid [8].
Core Innovation: The "Active-Reset" Mechanism The major challenge for continuous protein monitoring is the slow dissociation of affinity receptors, which prevents the sensor from tracking decreasing analyte levels. This was solved by applying high-frequency voltage oscillations to the electrode, which physically "shakes" the bound cytokine proteins off the sensor [8]. This resets the sensor, allowing it to take subsequent measurements and track dynamic changes in cytokine levels (e.g., IL-6 and TNF-α) in real-time, as demonstrated in proof-of-concept studies in diabetic mice [8].
Diagram 3: Implantable sensor cycle with active-reset mechanism.
Strategies for Effective Multiplexing in Complex Biological Samples
The comprehensive analysis of biomarkers in complex biological samples is fundamental to advancing research in immunology, drug development, and personalized medicine. Multiplexing technologies enable the simultaneous quantification of multiple analytes from a single, often limited, sample volume [21]. This capability is crucial for capturing the dynamic and interconnected nature of biological systems, particularly in cytokine sensing, where signaling cascades involve complex networks of proteins [44]. These application notes provide detailed protocols and strategic guidance for implementing effective multiplexing strategies within challenging matrices such as serum, plasma, and extracellular vesicle (EV) isolates, supporting robust data generation for dynamic monitoring technologies research [45] [46].
Multiplexing Platform Comparison
Selecting the appropriate platform is the first critical step in experimental design. The table below summarizes the key characteristics of widely used multiplexing technologies.
Table 1: Comparison of Multiplex Immunoassay Platforms
| Platform | Core Technology | Multiplexing Capacity | Approximate Sample Volume | Key Advantages | Reported Limits of Detection |
|---|---|---|---|---|---|
| Bead-Based (e.g., Luminex xMAP) [21] [44] | Flow cytometry with color-coded beads | Up to 500 analytes [45] | 10-50 µL [21] | High plex, good dynamic range, well-established | Varies by analyte; similar to ELISA [21] |
| Electrochemiluminescence (e.g., MSD) [21] [44] | Electrochemiluminescence on spotted arrays | Typically up to 10-40 analytes [21] [44] | 10-50 µL [21] | Broad dynamic range, sensitive, low background | Varies by analyte; can be more sensitive than ELISA [21] |
| Microfluidic LSPR [46] | Label-free nanoplasmonic sensing on gold nanorods | Demonstrated for 6 analytes | 1 µL | Extremely low sample volume, rapid results (~40 min) | 5-20 pg/mL in serum [46] |
| Traditional ELISA [21] | Colorimetric or chemiluminescent detection in wells | Single analyte | 50-100 µL per analyte | Gold standard, highly quantitative | Varies by analyte kit |
Detailed Experimental Protocols
Protocol 1: Bead-Based Multiplex Immunoassay for Serum Cytokines
This protocol outlines the steps for performing a multiplex cytokine assay using bead-based technology (e.g., Luminex xMAP), which is widely used for profiling inflammatory mediators in serum [21] [44] [45].
Principle: Distinct populations of color-coded magnetic beads are each conjugated with a capture antibody specific to a different cytokine. The beads are mixed with the sample, allowing target cytokines to bind. A biotinylated detection antibody is then added, followed by a streptavidin-phycoerythrin (SA-PE) conjugate. The beads are read on a analyzer that identifies each bead by its color and quantifies the bound cytokine based on the PE fluorescence intensity [44] [45].
Diagram 1: Bead-based assay workflow.
Materials:
- Research Reagent Solutions:
- Premixed Multiplex Bead Kit: Contains antibody-coupled magnetic beads for each target cytokine [44] [45].
- Assay Buffer: A protein-based buffer (e.g., PBS with BSA) used to dilute samples and reagents and to block non-specific binding.
- Biotinylated Detection Antibodies: A cocktail of antibodies specific to the target cytokines.
- Streptavidin-Phycoerythrin (SA-PE): Fluorescent reporter molecule that binds to biotin.
- Wash Buffer: Typically a buffered solution with a surfactant.
- Calibration Standards: Recombinant cytokines of known concentration for generating the standard curve.
Procedure:
- Preparation: Thaw and centrifuge all samples and reagents. Prepare serial dilutions of calibration standards in the same matrix as the samples (e.g., pooled serum) to minimize matrix effects.
- Bead Incubation: Add the mixed bead suspension to each well of a microtiter plate. Use a magnetic plate washer to separate beads and remove supernatant.
- Sample/Antigen Incubation: Resuspend beads in assay buffer, sample, or standard. Incubate for 2 hours with shaking at room temperature. Wash beads twice.
- Detection Antibody Incubation: Resuspend beads in the biotinylated detection antibody cocktail. Incubate for 1 hour with shaking. Wash beads twice.
- Reporter Incubation: Resuspend beads in SA-PE solution. Incubate for 30 minutes with shaking, protected from light. Wash beads twice.
- Reading: Resuspend beads in reading buffer. Analyze on the multiplex analyzer according to the manufacturer's instructions. Use the standard curve to calculate cytokine concentrations in the samples.
Protocol 2: Nanoplasmonic LSPR Microarray for Low-Volume Serum Analysis
This protocol describes a novel, label-free approach using a localized surface plasmon resonance (LSPR) microarray for rapid, high-sensitivity cytokine profiling from minute sample volumes, ideal for longitudinal monitoring where sample is limited [46].
Principle: A microfluidic chip is patterned with discrete stripes of gold nanorods (AuNRs), each functionalized with a different anti-cytokine antibody. When a serum sample flows over the chip, target cytokines bind to their specific antibodies on the AuNRs, causing a local change in the refractive index. This change induces a redshift in the resonant Rayleigh scattering spectrum of the AuNRs, which is detected as a measurable intensity change using dark-field imaging microscopy [46].
Diagram 2: LSPR microarray assay workflow.
Materials:
- Research Reagent Solutions:
- LSPR Microarray Chip: Fabricated with 480 sensing spots across 8 microfluidic channels, each stripe conjugated to a unique capture antibody [46].
- Gold Nanorods (AuNRs): Engineered to ~40 nm width with an aspect ratio of 2 for optimal sensitivity [46].
- Running Buffer: A biocompatible buffer for sample dilution and washing.
- Dark-Field Microscope: Equipped with a high-speed imaging camera for scanning the scattering light intensity across the sensor arrays.
Procedure:
- Chip Preparation: Prime the microfluidic channels of the LSPR chip with running buffer.
- Sample Loading: Dilute serum samples 1:1 in running buffer. Load approximately 1 µL of the prepared sample into each microfluidic channel inlet. The sample will be drawn through the channel by capillary action or gentle pressure.
- Incubation: Allow the sample to incubate on the chip for a brief period (typically 10-20 minutes) to enable cytokine binding.
- Washing: Flush each channel with running buffer to remove unbound proteins and matrix components.
- Detection & Analysis: Immediately place the chip under the dark-field microscope. Scan the scattering light intensity across all AuNR ensemble stripes. The intensity change relative to a baseline measurement is proportional to the concentration of bound cytokine, quantified against a pre-established standard curve.
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of multiplex assays relies on a set of core reagents. The following table details these essential components and their functions.
Table 2: Key Research Reagent Solutions for Multiplex Immunoassays
| Reagent / Material | Function | Key Considerations |
|---|---|---|
| Capture Beads / Substrate (e.g., color-coded beads [44] [45] or AuNR arrays [46]) | Solid-phase support for immobilizing specific capture antibodies. | Bead spectral uniqueness or nanorod optical properties are critical for multiplexing. |
| Matched Antibody Pairs (Capture & Biotinylated Detection) [44] | Provide specificity for the target analyte. | Must be validated as a pair with minimal cross-reactivity in the multiplex format. |
| Signal Reporter (e.g., Streptavidin-PE [44] [45]) | Generates a measurable signal proportional to the amount of bound analyte. | High quantum yield and stability are essential for sensitivity. |
| Assay / Running Buffer [46] | Diluent for samples and reagents; blocks non-specific binding. | Must be optimized for the sample matrix (e.g., serum, EV lysate) to minimize background. |
| Calibration Standards (Recombinant Proteins) | Used to generate a standard curve for quantitative analysis. | Purity and accurate concentration are paramount. Ideally should be in a matched matrix. |
Strategic Considerations for Complex Samples
The complexity of biological samples presents significant challenges that require strategic mitigation.
- Sample Type and Preparation: The choice between serum and plasma can significantly impact results. Plasma preparation removes fibrinogen and other clotting factors, potentially also removing cytokines that bind to these proteins, thereby altering measurable levels compared to serum [21]. For EV analysis, ultracentrifugation or affinity chromatography are common isolation methods, and the resulting EV lysates must be compatible with the multiplex platform [45].
- Managing Dynamic Range and Matrix Effects: Analytes within a single sample can exist at concentrations spanning several orders of magnitude. Utilize platforms with a broad dynamic range, such as MSD or bead-based systems [21]. To address matrix effects—where abundant proteins interfere with the assay—dilution of samples is often necessary. However, this can also dilute the analyte and any potential circulating inhibitors, potentially skewing results [21]. The LSPR platform is noted for its performance in complex serum matrices with minimal sample preparation [46].
- Cross-Reactivity and Validation: In a multiplex format, the risk of non-specific interactions and cross-reactivity between different antibody-analyte pairs increases [21]. It is critical to validate that each analyte measurement within a multiplex panel is specific and accurate. This often involves spiking experiments and comparison with a validated single-plex method like ELISA [21].
Effective multiplexing in complex biological samples is a powerful strategy for deconvoluting intricate biological pathways. The choice between established bead-based methods and emerging label-free technologies like LSPR should be guided by the specific research requirements, including sample volume availability, required throughput, and the need for speed. Adherence to robust protocols and careful consideration of sample-specific challenges are paramount for generating reliable, clinically relevant data in cytokine sensing and dynamic monitoring research. As these technologies continue to converge with artificial intelligence, they hold transformative potential for real-time immune monitoring and precision medicine [6].
Optimizing Assay Robustness, Cost, and Workflow for High-Throughput Screening
High-Throughput Screening (HTS) serves as a foundational technology in modern drug discovery and biomarker research, enabling the rapid evaluation of thousands to millions of chemical, biochemical, or genetic perturbations. Within cytokine sensing and dynamic monitoring research, HTS platforms facilitate the discovery of novel cytokine modulators, the identification of cytokine signatures associated with disease states, and the characterization of immune response dynamics. The global HTS market, valued at $25.26 billion in 2025 and projected to grow at a compound annual growth rate (CAGR) of 8.7% to $35.29 billion by 2029, reflects the increasing adoption of these technologies across pharmaceutical, biotechnology, and academic research institutions [47]. This growth is particularly driven by the rising prevalence of chronic diseases and the expanding focus on personalized medicine, which demands robust, cost-effective, and workflow-efficient screening methodologies.
Optimizing HTS assays for cytokine research requires a meticulous balance between analytical performance and practical implementation constraints. Key optimization parameters include the Z′-factor (>0.4 indicates a robust assay), signal-to-noise ratio, dynamic range, cost per well, and throughput capacity. Cell-based assays, which constitute 33.4-39.4% of the HTS technology segment, are particularly valuable in cytokine research as they provide physiologically relevant data on cytokine signaling pathways, receptor interactions, and immunomodulatory compound effects within a living cellular context [48] [49]. The integration of artificial intelligence and machine learning with HTS platforms is further enhancing screening efficiency by enabling predictive analytics, advanced pattern recognition, and automated data interpretation, thereby reducing false positive rates and accelerating hit identification [48].
Fundamental Principles of HTS Assay Development
Critical Performance Metrics and Validation Parameters
Assay robustness in HTS is quantitatively measured using specific statistical parameters that ensure reliability and reproducibility across large-scale screening campaigns. The Z′-factor is a definitive metric for assessing assay quality, incorporating both the dynamic range of the signal and the data variation associated with the sample and control measurements. A Z′-factor > 0.5 is considered excellent, while values between 0.4 and 0.5 indicate a marginal but acceptable assay. The signal-to-background ratio (S/B) and coefficient of variation (CV) provide additional validation of assay performance, with optimal values being >2 and <10%, respectively [50] [51].
The dynamic range of an assay represents the span between the minimum detectable concentration and the saturation point of detection, which for cytokine sensing typically ranges from 3-4 orders of magnitude, with limits of detection as low as 0.01-100 pg/mL for AI-enabled platforms [6]. For cell-based cytokine assays, careful optimization of cell seeding density, incubation times, and reagent concentrations is essential to maintain cellular health while ensuring sufficient signal intensity for detection. Additional considerations include plate uniformity, edge effects, and stability of reagents and samples throughout the screening process.
Table 1: Key Statistical Parameters for HTS Assay Validation
| Parameter | Calculation Formula | Optimal Value | Interpretation |
|---|---|---|---|
| Z′-factor | 1 - (3σₚ + 3σₙ)/|μₚ - μₙ| | > 0.5 | Excellent assay window with minimal variance |
| Signal-to-Background Ratio | μₚ/μₙ | > 2 | Sufficient distinction between positive and negative controls |
| Coefficient of Variation (CV) | (σ/μ) × 100 | < 10% | Low well-to-well variability |
| Signal Window | (μₚ - μₙ)/(σₚ² + σₙ²)⁰·⁵ | > 2 | Robust distinction between signals |
Technological Platforms for Cytokine HTS
Multiple detection technologies are available for cytokine HTS applications, each with distinct advantages and limitations. Time-Resolved Fluorescence Resonance Energy Transfer (TR-FRET) assays offer homogeneous, no-wash protocols with high sensitivity and reduced interference from autofluorescence, making them suitable for studying cytokine-receptor interactions such as the SLIT2/ROBO1 signaling axis [52]. Flow cytometry-based multiplexed assays enable simultaneous quantification of up to 12 cytokines from minimal sample volumes (1-50 μL), with recent advancements simplifying procedures through lyophilized reagents and one-step incubation protocols [22]. Luminex xMAP technology utilizes color-coded magnetic beads to measure multiple cytokines in a single well, providing high-throughput capability with reduced sample consumption compared to traditional ELISA methods.
Cell-based viability and functional assays represent another critical technology platform, with ATP-based luminescent assays (e.g., CellTiter-Glo) providing high sensitivity for monitoring cell health during cytokine stimulation or inhibition studies. Reporter gene assays engineered with luciferase or fluorescent protein readouts under the control of cytokine-responsive promoters enable specific monitoring of pathway activation in response to library compounds. High-content screening platforms combine automated microscopy with multiplexed fluorescent staining to capture complex cytokine-mediated phenotypic changes, including cell morphology, protein localization, and organelle structure [50].
HTS Technology Applications: This diagram illustrates the relationship between different HTS technology platforms and their primary applications in cytokine research.
Experimental Protocols for Cytokine HTS
TR-FRET-Based Protein-Protein Interaction Assay
The following protocol describes the development of a TR-FRET assay for screening inhibitors of the SLIT2/ROBO1 interaction, a cytokine signaling axis involved in immune regulation and tumor progression [52]. This assay format is particularly valuable for studying extracellular protein-protein interactions and can be adapted for other cytokine-receptor pairs.
Materials and Reagents:
- Recombinant SLIT2 and ROBO1 proteins with appropriate tags (e.g., His-tag, GST-tag)
- TR-FRET-compatible anti-tag antibodies (e.g., anti-His-Tb cryptate donor, anti-GST-XL665 acceptor)
- Low-volume 384-well or 1536-well white assay plates
- Assay buffer: 25 mM HEPES, 100 mM NaCl, 0.1% BSA, pH 7.4
- Test compounds in DMSO (final DMSO concentration ≤1%)
- Positive control inhibitor (e.g., SMIFH2 for SLIT2/ROBO1)
Procedure:
- Plate Preparation: Dispense 2 µL of compound solutions or controls into assay plates using acoustic dispensing or pintool transfer.
- Protein Mixture Preparation: Prepare a master mix containing:
- 5 nM recombinant ROBO1-His
- 5 nM recombinant SLIT2-GST
- 1 nM anti-His-Tb cryptate donor antibody
- 5 nM anti-GST-XL665 acceptor antibody in assay buffer.
- Reaction Assembly: Add 18 µL of protein mixture to each well using a non-contact dispenser.
- Incubation: Centrifuge plates briefly (500 rpm, 30 seconds) and incubate for 2 hours at room temperature protected from light.
- Detection: Measure TR-FRET signal using a compatible plate reader (e.g., PerkinElmer EnVision) with excitation at 337 nm and dual emission detection at 620 nm (donor) and 665 nm (acceptor).
- Data Analysis: Calculate TR-FRET ratio as (acceptor emission / donor emission) × 10,000. Normalize data to positive (100% inhibition) and negative (0% inhibition) controls.
Optimization Notes:
- Titrate protein concentrations to achieve optimal signal-to-background ratio while minimizing material usage.
- Include DMSO tolerance tests to ensure compatibility with compound libraries.
- Implement liquid handling automation to enhance reproducibility and throughput.
Multiplexed Cytokine Profiling Assay Using Flow Cytometry
This protocol describes a simplified one-step flow cytometry-based assay for simultaneous quantification of 12 cytokines from serum samples, incorporating lyophilized reagents to enhance workflow efficiency and eliminate cold chain requirements [22]. The method has been successfully applied to cytokine profiling in COVID-19 and HBV patients, with machine learning approaches used for disease severity prediction.
Materials and Reagents:
- Carboxylated fluorescently encoded microspheres (e.g., Spherotech)
- Capture antibodies for target cytokines (e.g., BioLegend, BD, Thermo Fisher Scientific)
- Phycoerythrin (PE)-conjugated detection antibodies
- Lyophilization buffer: 0.15 M PBS (pH 7.4) with 0.1% BSA, 5% mannitol, and 3% trehalose
- 96-well filter plates (1.2 µm pore size)
- Flow cytometer with 488 nm laser and PE detection capability (e.g., Beckman Coulter DxFlex)
Procedure:
- Bead Conjugation:
- Activate carboxylated microspheres with EDC and sulfo-NHS in activation buffer.
- Incubate with capture antibodies (0.1-0.5 mg/mL) for 2 hours at room temperature.
- Block remaining active sites with 1% BSA for 30 minutes.
- Wash and resuspend beads in storage buffer at 10,000 beads/µL.
Lyophilized Reagent Preparation:
- Prepare detection antibody mixture (2 µg/mL each antibody in lyophilization buffer).
- Combine encoded capture beads (100,000 particles/mL) with detection antibodies.
- Dispense 250 µL aliquots into liquid nitrogen for rapid freezing.
- Transfer to pre-cooled vacuum freeze-dryer for 12 hours to obtain lyophilized reagent spheres.
Sample Analysis:
- Reconstitute lyophilized reagents with 100 µL of serum sample or standard.
- Incubate with shaking at room temperature for 1.5 hours.
- Wash twice with washing buffer (0.15 M PBS, 0.05% Tween-20, pH 7.4).
- Resuspend in reading buffer and analyze using flow cytometer.
Data Processing:
- Collect minimum of 100 events per bead population.
- Calculate median PE fluorescence intensity for each cytokine.
- Generate standard curves using recombinant cytokines (0-10,000 pg/mL).
- Apply machine learning algorithms (logistic regression, random forest, SVM) for pattern recognition and severity prediction.
Optimization Notes:
- Validate lyophilized reagent stability under various storage conditions.
- Perform cross-reactivity testing to ensure assay specificity.
- Implement automated liquid handling for consistent washing steps.
Table 2: Comparison of HTS Assay Platforms for Cytokine Research
| Parameter | TR-FRET Assay | Flow Cytometry Multiplex | Cell-Based Reporter Assay |
|---|---|---|---|
| Throughput | Ultra-high (1536-well) | Medium-high (96-384 well) | Medium-high (384-well) |
| Sample Volume | 5-20 µL | 50-100 µL | 20-50 µL |
| Multiplexing Capacity | Low (1-2 targets) | High (up to 12+ targets) | Medium (2-4 reporters) |
| Assay Time | 2-4 hours | 1.5-3 hours | 24-72 hours |
| Cost per Well | $$ | $$$ | $$ |
| Primary Application | Protein-protein interactions | Cytokine profiling | Pathway activation |
| Key Equipment | TR-FRET plate reader | Flow cytometer | Luminescence/Fluorescence plate reader |
Workflow Integration and Automation Strategies
Efficient integration of HTS assays into automated workflows is essential for maximizing throughput, minimizing variability, and reducing operational costs. A typical automated HTS workflow for cytokine research encompasses multiple interconnected modules: compound management, liquid handling, incubation, detection, and data analysis. The instruments segment, comprising liquid handling systems, detectors, and readers, accounts for 49.3% of the HTS product and services market, reflecting the critical importance of automation in screening operations [48].
Liquid handling systems form the core of HTS automation, with advanced platforms capable of dispensing volumes from milliliters to picoliters with high precision. For cytokine HTS applications, non-contact dispensers utilizing piezoelectric or acoustic technologies are preferred for adding detection reagents to cell-based assays, as they minimize cross-contamination and preserve delicate cell layers. Integration of robotic plate handlers enables continuous operation of multiple instruments, significantly increasing daily throughput. Modern systems, such as the Beckman Coulter Cydem VT Automated Clone Screening System, can reduce manual steps in cell line development by up to 90%, dramatically accelerating screening timelines [48].
Data analysis workflow integration represents another critical optimization area. The implementation of AI and machine learning algorithms enables real-time quality control, hit selection, and pattern recognition in large cytokine datasets. For dynamic cytokine monitoring studies, such as those investigating community-acquired pneumonia in elderly patients, the integration of cytokine dynamics (e.g., IL-6 changes over 48 hours) with traditional clinical severity scores significantly improves prognostic accuracy (AUC increases from 0.66 to 0.77) [5]. Establishing automated data pipelines that connect plate readers with analysis software and laboratory information management systems (LIMS) ensures traceability and facilitates rapid decision-making.
HTS Workflow Optimization: This diagram illustrates the integrated automated workflow for HTS and key parameters for optimization at each stage.
Cost Optimization and Scalability Considerations
Strategic management of screening costs is essential for maintaining sustainable HTS operations while ensuring data quality. The reagents and kits segment constitutes 36.5% of the HTS products and services market, highlighting the significant financial impact of consumables on screening budgets [49]. Several approaches can substantially reduce per-well costs without compromising assay robustness.
Assay miniaturization represents the most effective strategy for cost reduction, transitioning from 96-well to 384-well or 1536-well formats to decrease reagent consumption by 4-fold or 16-fold, respectively. For cytokine TR-FRET assays, miniaturization to 1536-well format can reduce recombinant protein requirements from microgram to nanogram per well while maintaining Z′-factors >0.6 [52]. Implementation of non-contact dispensing technologies enables precise low-volume liquid handling, with modern acoustic dispensers capable of transferring 2.5 nL droplets with CVs <5%, significantly reducing reagent usage compared to traditional pipetting systems.
Bulk reagent procurement and lyophilization provide additional cost-saving opportunities. The development of lyophilized reagent spheres for multiplexed cytokine detection eliminates cold chain requirements and reduces shipping costs while maintaining stability for over 12 months [22]. For cell-based cytokine assays, implementing centralized cell banking and standardized culture protocols ensures consistent cellular material across screening campaigns, reducing batch-to-batch variability and associated validation costs. Strategic partnerships with reagent manufacturers for bulk purchases or custom formulations can further decrease material expenses by 20-30%.
Table 3: Cost-Benefit Analysis of HTS Optimization Strategies
| Optimization Strategy | Implementation Cost | Long-term Savings | Impact on Data Quality | Time to Implement |
|---|---|---|---|---|
| Assay Miniaturization | High (equipment investment) | 40-60% reagent reduction | Maintains or improves Z′-factor | 2-4 months |
| Liquid Handling Automation | High (system purchase) | 30% labor reduction | Improves reproducibility | 3-6 months |
| Lyophilized Reagents | Medium (development cost) | 25% reagent cost, eliminates cold chain | Comparable to fresh reagents | 6-12 months |
| Centralized Cell Banking | Low-medium | 15% cell culture costs | Reduces biological variability | 1-2 months |
| AI-Enabled Hit Selection | Medium (software/licensing) | 50% follow-up costs | Reduces false positive rate | 1-3 months |
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful implementation of optimized HTS assays for cytokine research requires access to specialized reagents and materials with defined performance characteristics. The following toolkit outlines essential solutions that form the foundation of robust, cost-effective screening workflows.
Table 4: Essential Research Reagent Solutions for Cytokine HTS
| Reagent Category | Specific Examples | Function in HTS Workflow | Key Selection Criteria |
|---|---|---|---|
| Detection Technologies | TR-FRET compatible antibodies (anti-His-Tb, anti-GST-XL665) | Enable homogeneous, no-wash detection of protein-protein interactions | Low background signal, high energy transfer efficiency |
| Multiplex Bead Arrays | Carboxylated fluorescently encoded microspheres (Spherotech) | Simultaneous quantification of multiple cytokines in limited sample volumes | Minimal spectral overlap, uniform coupling efficiency |
| Cell Viability Assays | ATP-based luminescent assays (CellTiter-Glo) | Measure cell health and compound cytotoxicity in functional assays | Linear dynamic range, compatibility with automation |
| Lyophilization Stabilizers | Trehalose-mannitol formulations | Enable room temperature storage of critical reagents | Maintain >90% activity post-reconstitution |
| Reporter Gene Systems | Luciferase under cytokine-responsive promoters | Monitor pathway activation in cell-based screening | Low background, high induction ratio |
| Cytokine Standards | Recombinant human cytokines (BioLegend) | Quantification and assay standardization | >95% purity, biological activity verification |
The continuous optimization of assay robustness, cost-efficiency, and workflow integration remains paramount for advancing cytokine sensing and dynamic monitoring research through high-throughput screening. The integration of artificial intelligence and machine learning with HTS platforms represents a transformative development, enabling predictive assay design, real-time quality control, and enhanced hit identification from complex cytokine datasets [48] [6]. These technologies are particularly valuable for analyzing dynamic cytokine patterns, as demonstrated in studies of COVID-19 and HBV patients, where machine learning models successfully predicted disease severity and viral load based on multiplexed cytokine profiles [22].
Future directions in cytokine HTS optimization will likely focus on further miniaturization through nanoliter-scale dispensing technologies, increased multiplexing capacity to capture immune response complexity, and the development of more physiologically relevant 3D cell culture models for cytokine signaling studies. The growing emphasis on drug repurposing, facilitated by HTS of FDA-approved compound libraries against cytokine targets, presents additional opportunities for accelerated therapeutic development [51]. As these technological advances converge with increasingly sophisticated data analytics platforms, HTS will continue to evolve as an indispensable tool for deciphering cytokine biology and developing novel immunomodulatory therapies.
Benchmarking Cytokine Detection Technologies: A Data-Driven Comparison
Accurate cytokine quantification is fundamental to understanding immune system function in health and disease. Cytokines are critical messengers regulating immunity, inflammation, and cell communication, making their accurate measurement essential for characterizing immune status, discovering biomarkers, and developing new therapies [53]. The choice of detection technology significantly influences the reliability, depth, and interpretation of results in both basic research and drug development contexts. This assessment provides a comprehensive comparative analysis of five prominent cytokine detection platforms: Meso Scale Discovery (MSD), Luminex, Enzyme-Linked Immunosorbent Assay (ELISA), Time-Resolved Förster Resonance Energy Transfer (TR-FRET), and Amplified Luminescent Proximity Homogeneous Assay (AlphaLISA). Each technology offers distinct advantages and limitations in sensitivity, multiplexing capability, throughput, and operational requirements, making platform selection a critical strategic decision for researchers and drug development professionals. Understanding these technological characteristics ensures alignment between methodological capabilities and specific research objectives, whether for broad discovery screening, targeted validation studies, or high-throughput drug screening applications.
Fundamental Assay Principles
- MSD (Meso Scale Discovery): This platform utilizes electrochemiluminescence detection. Capture antibodies are immobilized on carbon electrode-coated microplates. Upon voltage application, sulfo-tag labels on detection antibodies emit light, providing a highly sensitive signal with minimal background [54].
- Luminex xMAP Technology: This bead-based multiplexing system uses color-coded magnetic microspheres impregnated with varying ratios of two fluorescent dyes, creating up to 100 distinct spectral addresses. Each bead class is coated with a specific capture antibody, enabling simultaneous detection of multiple analytes in a single sample well through flow cytometry-based laser detection [55] [53].
- ELISA (Enzyme-Linked Immunosorbent Assay): The traditional workhorse of immunoassays, ELISA employs enzyme-mediated colorimetric or chemiluminescent detection on antibody-coated polystyrene plates. It typically follows a sandwich immunoassay format with washing steps between reagent additions to remove unbound material [55] [53].
- TR-FRET (Time-Resolved Förster Resonance Energy Transfer): This homogeneous technology uses a sandwich immunoassay format with lanthanide chelate donors (e.g., Europium) and far-red acceptor fluorophores. Energy transfer occurs only when antibodies bring donor and acceptor into close proximity, with time-resolved detection minimizing background fluorescence [56] [57].
- AlphaLISA: A homogeneous, no-wash bead-based technology utilizing photosensitizer-containing donor beads and biotin-conjugated acceptor beads. Laser excitation at 680nm generates singlet oxygen molecules that travel to nearby acceptor beads, triggering a chemiluminescent emission at 615nm [58].
Comprehensive Performance Comparison
Table 1: Technical Specifications and Performance Metrics Across Platforms
| Parameter | MSD | Luminex | ELISA | TR-FRET | AlphaLISA |
|---|---|---|---|---|---|
| Detection Mechanism | Electrochemiluminescence | Fluorescence-based bead array | Colorimetric/Chemiluminescent | Time-Resolved FRET | Singlet Oxygen Chemiluminescence |
| Multiplexing Capacity | Moderate (∼10-plex) | High (30-500 analytes) | Single-plex | Low to Moderate | Low to Moderate |
| Sensitivity (Typical LOD) | Very High (sub-pg/mL) | High (Low pg/mL) | Moderate (Low pg/mL) | High (e.g., IL-1β: 1 pg/mL) | Very High (e.g., IL-6: 0.3 pg/mL) |
| Dynamic Range | 3-5 logs | 3-5 logs | 2-3 logs | >3 logs (e.g., TNFα: 41 LLOQ) | >4 logs (e.g., IL-6: 0.1-30,000 pg/mL) |
| Sample Volume Required | 20-40 μL/panel | 25-50 μL/panel | 100-200 μL/analyte | 20 μL/reaction | 5-10 μL/reaction |
| Throughput | High | High | Moderate | High | High |
| Assay Time | ∼3-5 hours | ∼3-5 hours | ∼4-8 hours | ∼1-2 hours | ∼1.5 hours |
| Homogeneous (No-wash) | No | No | No | Yes | Yes |
| Best Applications | Sensitive quantification of low-abundance targets, clinical studies | Comprehensive immune profiling, biomarker discovery | Targeted analysis, validation studies | High-throughput screening, kinetic studies | High-throughput sensitive detection, limited sample availability |
Table 2: Operational Considerations and Cost Analysis
| Consideration | MSD | Luminex | ELISA | TR-FRET | AlphaLISA |
|---|---|---|---|---|---|
| Equipment Costs | High | High | Low | Moderate-High | Moderate-High |
| Reagent Costs | High | Moderate-High | Low-Moderate | Moderate | Moderate |
| Technical Expertise Required | Moderate | Moderate | Low | Low-Moderate | Low-Moderate |
| Assay Development Time | Short (pre-optimized) | Short (pre-optimized) | Short (kits available) | Short (pre-optimized) | Short (pre-optimized) |
| Data Complexity | Moderate | High (requires specialized software) | Low | Moderate | Moderate |
| Sample Matrix Tolerance | High | Moderate | High | Moderate (buffer optimization needed) | Moderate (buffer optimization needed) |
Detailed Experimental Protocols
MSD Multiplex Cytokine Assay Protocol
The MSD platform provides sensitive, multiplex cytokine quantification with broad dynamic range, suitable for detecting low-abundance analytes in complex matrices like serum and plasma [53] [54].
Materials:
- MSD MULTI-ARRAY or U-PLEX Plate (pre-coated with capture antibodies)
- MSD Diluent
- Calibrator standards (recombinant cytokines)
- Detection Antibody Solution (sulfo-tag labeled)
- MSD Read Buffer T (with surfactant)
- MSD MESO QuickPlex SQ 120 or SECTOR Imager
Procedure:
- Plate Preparation: Equilibrate MSD plate to room temperature for 10-15 minutes.
- Standard and Sample Addition:
- Prepare standard curve by serial dilution in appropriate matrix-matched diluent.
- Add 25-50 μL of standards, controls, and samples to appropriate wells.
- Cover plate and incubate with shaking (300-600 rpm) for 2 hours at room temperature.
- Washing: Wash plate 3× with PBS-T (PBS with 0.05% Tween-20) using an automated plate washer (150-300 μL per wash).
- Detection Antibody Incubation:
- Add 25-50 μL of detection antibody solution to each well.
- Cover plate and incubate with shaking for 2 hours at room temperature.
- Final Wash: Wash plate 3× with PBS-T as before.
- Read Buffer Addition: Add 150 μL of MSD Read Buffer T to each well.
- Signal Detection: Immediately read plate on MSD instrument equipped with electrochemiluminescence detection.
Data Analysis:
- Generate 4-parameter logistic (4PL) standard curves for each analyte.
- Calculate sample concentrations using instrument software, applying appropriate dilution factors.
- Quality control: CV <20% for replicates, standard curve R² >0.98.
TR-FRET Cytokine Assay Protocol (THUNDER Technology)
THUNDER assays provide homogeneous, no-wash cytokine quantification with excellent sensitivity and rapid turnaround, ideal for high-throughput screening applications [56] [57].
Materials:
- THUNDER Human Cytokine Assay Kit (including Eu-Ab1, FR-Ab2, Assay Buffer)
- Low-volume 384-well white plates
- PHERAstar FSX or other TR-FRET compatible microplate reader
- Recombinant cytokine standards
Procedure:
- Standard Preparation: Prepare cytokine standard dilutions in assay buffer to create a standard curve (typically 8 points plus blank).
- Reaction Setup:
- Add 15 μL of standards or samples to assay plates.
- Add 5 μL of Antibody Mix to each well.
- Centrifuge plates briefly (∼1000 × g, 1 minute) to collect contents.
- Incubation: Incubate plate at room temperature for 60-120 minutes protected from light.
- Signal Detection: Read plate on TR-FRET compatible reader using settings below.
TR-FRET Instrument Settings (PHERAstar FSX):
- Optics: Time-resolved fluorescence, plate mode endpoint
- Excitation: 320-340 nm
- Emission: 620 nm (donor) and 665 nm (acceptor)
- Delay time: 40 μsec
- Integration time: 400 μsec
- Number of flashes: 40
- Settling time: 0.1 sec
Data Analysis:
- Calculate TR-FRET ratio = (665 nm emission / 620 nm emission) × 1000
- Fit standard curve using 4PL model with 1/Y² weighting
- Determine sample concentrations from standard curve
AlphaLISA IL-6 Detection Protocol
AlphaLISA technology enables highly sensitive, homogeneous cytokine detection without wash steps, significantly reducing hands-on time while maintaining excellent performance characteristics [58].
Materials:
- AlphaLISA HP Human IL-6 Kit (Acceptor beads, Biotinylated detection antibody, Streptavidin-coated Donor beads)
- White opaque 384-well AlphaPlate
- Recombinant human IL-6 standard
- Assay Buffer
- Acoustic liquid handler (optional)
Procedure:
- Standard and Sample Preparation:
- Prepare IL-6 standard curve in assay buffer (typically 0.1-30,000 pg/mL range).
- Dilute samples as needed in assay buffer.
- Assay Assembly:
- Add 5 μL of standards or samples to assay plate.
- Add 10 μL of biotinylated detector antibody/Acceptor bead mixture (pre-incubated 30 minutes).
- Incubate for 60 minutes at room temperature protected from light.
- Donor Bead Addition:
- Add 10 μL of Streptavidin-coated Donor beads (under subdued light).
- Incubate for 30 minutes at room temperature protected from light.
- Signal Detection: Read plate on AlphaLISA-compatible reader (EnVision, PHERAstar FSX) with Alpha screen settings.
Data Analysis:
- Generate 4PL standard curve using Alpha signal (615 nm)
- Calculate sample concentrations from standard curve
- Validate assay performance: LLOQ ≤0.8 pg/mL, intra-assay CV <15%
Technology Workflow Visualization
Research Reagent Solutions and Essential Materials
Table 3: Essential Research Reagents and Materials for Cytokine Detection
| Category | Specific Items | Function & Importance | Technology Application |
|---|---|---|---|
| Core Reagents | Matched Antibody Pairs (Capture/Detection) | Specific target recognition; critical for assay specificity and sensitivity | All platforms |
| Recombinant Cytokine Standards | Standard curve generation for absolute quantification | All platforms | |
| Assay Buffers & Blocking Solutions | Minimize non-specific binding; optimize assay conditions | All platforms | |
| Detection Components | Streptavidin-Conjugated Donor Beads | Generate singlet oxygen upon laser excitation | AlphaLISA |
| Acceptor Beads with Fluorophores | Emit light at 615nm upon singlet oxygen transfer | AlphaLISA | |
| Europium Chelate Donor Antibodies | Long-lifetime fluorescence donor for TR-FRET | TR-FRET | |
| Far-Red Acceptor Fluorophore Antibodies | FRET acceptor for signal generation | TR-FRET | |
| Electrochemiluminescent SULFO-Tags | Generate light signal upon electrochemical stimulation | MSD | |
| Fluorescently-Labeled Detection Antibodies | Provide detection signal in bead-based assays | Luminex | |
| Enzyme-Conjugated Detection Antibodies | Catalyze colorimetric/chemiluminescent reaction | ELISA | |
| Specialized Consumables | Carbon Electrode-Coated Microplates | Platform for electrochemical stimulation | MSD |
| Spectrally-Distinct Magnetic Microspheres | Multiplexing platform with unique spectral addresses | Luminex | |
| White Opaque Low-Volume Microplates | Optimize signal detection for fluorescence/luminescence | TR-FRET, AlphaLISA | |
| High-Binding Polystyrene Microplates | Antibody immobilization for traditional ELISA | ELISA | |
| Sample Preparation | Protein Stabilizer Cocktails | Preserve cytokine integrity during processing | All platforms |
| Protease Inhibitor Mixtures | Prevent cytokine degradation | All platforms | |
| Matrix-Matched Diluents | Minimize matrix effects in biological samples | All platforms |
Platform selection should be driven by specific research requirements rather than seeking a universally superior technology. For comprehensive immune profiling requiring simultaneous measurement of 30+ cytokines, Luminex provides the highest multiplexing capacity [53]. When investigating low-abundance cytokines or requiring exceptional sensitivity for early disease biomarkers, MSD and AlphaLISA offer superior performance with detection limits in the sub-pg/mL range [58] [54]. For high-throughput screening applications where rapid turnaround and minimal hands-on time are prioritized, TR-FRET and AlphaLISA homogeneous platforms eliminate wash steps and reduce assay time to under 2 hours [56] [58] [57]. For targeted analysis of a limited number of analytes or validation studies, traditional ELISA remains cost-effective and widely accessible [53]. Ultimately, matching technology capabilities to specific research objectives, sample availability, and operational constraints ensures optimal data quality and research efficiency in cytokine sensing and dynamic monitoring applications.
{{ const reagentSolutions = [ { reagent: 'Simoa HD-X Analyzer', application: 'Ultra-sensitive digital immunoassay system for running single-plex and multiplex cytokine panels. [59]' }, { reagent: 'Cytokine Advantage PLUS Kits', application: 'Pre-optimized single-plex and multiplex assay kits for specific cytokine panels, include standardized controls and reagents. [59]' }, { reagent: 'Conductive Fracturing Fluids', application: 'Electrolyte-containing fluids used with AC excitation to create a "conductor antenna effect" for electromagnetic fracture monitoring. [60]' }, { reagent: 'Molecular Sensors (MOMS)', application: 'Aptamer-based sensors anchored to yeast cell membranes for high-throughput metabolic secretion analysis. [61]' }, { reagent: 'AI-Enabled POC Biosensors', application: 'Integrated platforms using machine learning for signal processing and drift monitoring in decentralized cytokine testing. [6] [62]' }, { reagent: 'Particulate Diverters', application: 'Materials used in reservoir stimulation, shown via monitoring to achieve 93.1% diversion efficiency. [60]' } ]; }}
Comparative Metrics: Sensitivity, Dynamic Range, Precision, and Recovery Rates
Cytokine sensing and dynamic monitoring technologies are pivotal for advancing biomarker-driven research and clinical applications in immunology, oncology, and inflammatory diseases. The accurate quantification of these low-abundance signaling proteins requires analytical platforms with exceptional sensitivity, precision, and robustness. This application note provides a systematic comparison of current cytokine detection technologies, focusing on ultra-sensitive immunoassays, emerging biosensors, and computational activity estimation methods. We present structured quantitative data, detailed experimental protocols, and pathway visualizations to support researchers in selecting appropriate methodologies for their specific applications. The convergence of high-sensitivity detection with artificial intelligence and multiplexing capabilities is reshaping the landscape of immune monitoring, enabling unprecedented insights into real-time cytokine dynamics in both clinical and research settings [59] [6].
Technology Performance Comparison
The evaluation of cytokine detection platforms requires careful assessment of multiple analytical parameters. The following table provides a comparative analysis of key performance metrics across major technology categories, highlighting significant advancements in sensitivity and operational efficiency.
| Parameter | Ultra-Sensitive Simoa | AI-Enabled POC Biosensors | Traditional ELISA |
|---|---|---|---|
| Limit of Detection (LOD) | {{performanceData[0].simoa}} [59] | {{performanceData[0].aiPocBiosensors}} [6] | {{performanceData[0].traditionalElisa}} [59] |
| Dynamic Range | {{performanceData[1].simoa}} [59] | {{performanceData[1].aiPocBiosensors}} [6] | {{performanceData[1].traditionalElisa}} [59] |
| Precision (Intra-assay CV) | {{performanceData[2].simoa}} [59] | {{performanceData[2].aiPocBiosensors}} [6] | {{performanceData[2].traditionalElisa}} [59] |
| Sample Volume | {{performanceData[3].simoa}} [59] | {{performanceData[3].aiPocBiosensors}} [6] | {{performanceData[3].traditionalElisa}} [63] |
| Assay Time | {{performanceData[4].simoa}} [59] | {{performanceData[4].aiPocBiosensors}} [6] | {{performanceData[4].traditionalElisa}} [63] |
| Multiplexing Capability | {{performanceData[5].simoa}} [59] | {{performanceData[5].aiPocBiosensors}} [6] | {{performanceData[5].traditionalElisa}} [63] |
Analysis of Comparative Data
The Simoa platform demonstrates superior sensitivity with detection limits in the single-digit femtogram per milliliter range, representing an improvement of approximately three orders of magnitude over traditional ELISA. This exceptional sensitivity enables detection of previously unquantifiable low-abundance cytokines in complex biological matrices like serum and plasma [59]. The AI-enabled point-of-care biosensors offer a balanced profile with good sensitivity (0.01-100 pg/mL) combined with rapid turnaround times (5-30 minutes) and minimal sample volume requirements (1-50 µL), making them particularly suitable for clinical settings where rapid results are critical for therapeutic decision-making [6]. Both advanced platforms maintain high precision, with Simoa achieving intra- and inter-assay coefficients of variation under 10% through rigorous validation protocols [59].
Experimental Protocols
Protocol 1: Simoa Ultra-Sensitive Cytokine Assay Validation
This protocol outlines the procedure for validating ultrasensitive cytokine detection assays using the Simoa HD-X platform, based on the validation work conducted by Frontage Laboratories [59].
Materials and Equipment
- Simoa HD-X Analyzer
- Cytokine Advantage PLUS kit (single-plex or multiplex)
- Recombinant cytokine standards
- Serum or plasma samples
- Simoa sample diluent
- Microplate shaker
- Pipettes and tips
Procedure
- Instrument Preparation: Initialize the Simoa HD-X Analyzer and perform quality control checks as per manufacturer instructions.
- Reagent Preparation: Reconstitute standards and prepare calibrators according to the kit protocol. Allow all reagents to reach room temperature.
- Sample Preparation: Dilute serum/plasma samples 1:2 with sample diluent. For spike-and-recovery tests, add a known concentration of recombinant cytokine to the sample.
- Assay Setup: Pipette 50 µL of standards, controls, and samples into the designated wells of the assay plate.
- Automated Processing: Load the plate onto the HD-X instrument where automated processing occurs, including:
- Immunocomplex formation with paramagnetic beads
- Enzyme conjugate labeling
- Washing and transfer to sealed disc arrays
- Substrate addition and fluorescence imaging
- Data Analysis: Use the Simoa software to generate a standard curve and calculate cytokine concentrations in samples based on the average enzymes per bead (AEB) values.
Validation Parameters
- Limit of Detection (LOD): Determine through 10 replicates of the zero standard; calculate as mean + 2SD of the measured concentration.
- Precision: Assess intra-assay precision with 16 replicates each of low, medium, and high controls in a single run. Determine inter-assay precision across 3 separate runs.
- Recovery: Perform spike-and-recovery by adding known cytokine concentrations to serum matrix; calculate percentage recovery of measured vs. expected values.
- Linearity: Evaluate dilutional linearity by serially diluting high-concentration samples and assessing linear regression of measured concentrations.
Protocol 2: AI-Enhanced Point-of-Care Cytokine Biosensing
This protocol describes the operation of emerging AI-enhanced biosensors for rapid, multiplexed cytokine detection at the point of care, based on recently reviewed technologies [6].
Materials and Equipment
- AI-enabled multiplex POC biosensor platform
- Disposable sensor cartridges
- Blood collection devices (for fingerstick samples)
- Buffer solutions
- Data processing unit with integrated machine learning algorithms
Procedure
- Sample Collection: Collect 1-50 µL of sample (whole blood, serum, or plasma) via venipuncture or fingerstick.
- Cartridge Loading: Apply sample directly to the sample chamber of the disposable sensor cartridge.
- Automated Analysis: Insert the cartridge into the biosensor reader, which automatically:
- Processes the sample through microfluidic channels
- Enables simultaneous binding to multiple cytokine-specific capture areas
- Converts binding events to electrical or optical signals
- Applies AI algorithms (CNNs or decision-tree models) for signal processing and drift correction
- Result Interpretation: Review results on the display within 5-30 minutes, including raw concentration data and AI-interpreted predictive outputs with uncertainty estimates.
Performance Verification
- Calibration Verification: Run quality control materials with known cytokine concentrations to verify calibration.
- Multiplexing Accuracy: Confirm specificity of each cytokine detection channel through cross-reactivity testing.
- AI Performance: Validate machine learning algorithm outputs against reference methods for critical result interpretation.
Signaling Pathways and Workflow Visualization
Cytokine Signaling and Detection Pathway
The following diagram illustrates the core signaling pathway of cytokines and the fundamental principle of immunoassay-based detection, which forms the basis for both conventional and novel sensing technologies.
Experimental Workflow Comparison
This diagram compares the key steps and technological approaches of three major cytokine detection methodologies, highlighting differences in complexity, time requirements, and operational characteristics.
Research Reagent Solutions
The following table details essential reagents and technologies used in advanced cytokine sensing and dynamic monitoring applications, providing researchers with key solutions for implementing these methodologies.
| Research Reagent Solution | Application and Function |
|---|---|
| {{reagentSolutions[0].reagent}} | {{reagentSolutions[0].application}} |
| {{reagentSolutions[1].reagent}} | {{reagentSolutions[1].application}} |
| {{reagentSolutions[2].reagent}} | {{reagentSolutions[2].application}} |
| {{reagentSolutions[3].reagent}} | {{reagentSolutions[3].application}} |
| {{reagentSolutions[4].reagent}} | {{reagentSolutions[4].application}} |
| {{reagentSolutions[5].reagent}} | {{reagentSolutions[5].application}} |
This comprehensive analysis of cytokine sensing technologies demonstrates significant advancements in detection capabilities, with ultra-sensitive platforms like Simoa achieving single-digit femtogram per milliliter sensitivity and AI-enhanced POC biosensors enabling rapid, decentralized testing with minimal sample volumes. The integration of artificial intelligence for signal processing and drift correction further enhances the reliability and clinical utility of these emerging platforms. These technological innovations are transforming cytokine biomarker quantification, enabling more precise monitoring of immune responses in therapeutic development, clinical diagnostics, and personalized medicine applications. Researchers should select technologies based on their specific requirements for sensitivity, throughput, speed, and operational complexity, considering that the continued convergence of nanotechnology, AI, and multiplexing capabilities will likely drive further improvements in dynamic monitoring of cytokine networks.
In the rapidly advancing field of biomedical research, particularly in cytokine sensing and dynamic monitoring technologies, selecting the appropriate tools for preclinical versus clinical applications represents a critical decision point that directly impacts the success of drug development and translational research. The distinction between these phases extends far beyond simple semantics; it encompasses fundamental differences in biological models, validation requirements, regulatory frameworks, and ultimate application goals. Within the specific context of cytokine research, where dynamic monitoring of immune signaling molecules provides crucial insights into disease mechanisms and therapeutic efficacy, this tool selection process becomes particularly significant [5] [64].
Cytokines, as key regulators of the immune system, play a pivotal role in the progression and prognosis of numerous conditions, from infectious diseases like community-acquired pneumonia to cancer immunotherapy outcomes [5] [65]. The ability to accurately measure and monitor these dynamic biomarkers throughout the drug development pipeline enables researchers to predict efficacy, monitor disease progression, and tailor treatments to specific patient populations. However, the tools and methodologies required for initial discovery phases differ substantially from those needed for clinical application, with each phase demanding specialized approaches to address distinct scientific questions and regulatory requirements [64].
This application note provides a comprehensive framework for selecting appropriate cytokine sensing and monitoring technologies across the preclinical-to-clinical continuum. By synthesizing current methodologies, validation standards, and emerging technologies, we aim to equip researchers with the practical knowledge needed to navigate the complex transition from laboratory discoveries to clinical applications, ultimately enhancing the efficiency and success of therapeutic development.
Fundamental Distinctions: Preclinical vs. Clinical Biomarker Applications
Core Definitions and Strategic Objectives
The journey from preclinical discovery to clinical application requires a clear understanding of the distinct purposes and validation requirements at each stage. Preclinical biomarkers serve as essential tools during early-stage drug development, where they provide crucial insights into a compound's pharmacokinetics, pharmacodynamics, and potential toxicity before advancing to human trials [64]. These biomarkers help researchers understand how a drug candidate will behave in human systems, guiding candidate selection and optimization while significantly de-risking clinical development. In contrast, clinical biomarkers are quantifiable biological indicators used during human clinical trials to assess drug efficacy, monitor safety, and personalize patient treatment strategies [64]. These biomarkers play an indispensable role in regulatory approval processes by demonstrating that a drug is both safe and effective for its intended use, while also enabling precision medicine approaches through patient stratification.
The strategic objectives for these biomarker classes differ substantially. Preclinical biomarker development focuses primarily on predictive accuracy for human responses, mechanistic understanding of drug-target interactions, and early toxicity identification. Conversely, clinical biomarker application emphasizes patient stratification, treatment monitoring, safety assessment, and providing surrogate endpoints for accelerated regulatory approval [64]. This fundamental divergence in purpose directly influences the selection of appropriate sensing technologies, validation approaches, and implementation strategies at each development stage.
Comparative Analysis: Key Distinctions
Table 1: Core Differences Between Preclinical and Clinical Biomarker Applications
| Feature | Preclinical Biomarkers | Clinical Biomarkers |
|---|---|---|
| Primary Purpose | Predict drug efficacy and safety in early research | Assess efficacy, safety, and patient response in human trials |
| Common Models Used | In vitro organoids, patient-derived xenografts (PDX), genetically engineered mouse models [64] | Human patient samples, blood tests, imaging biomarkers [64] |
| Validation Process | Primarily experimental and computational validation [64] | Requires extensive clinical trial data and regulatory review [64] |
| Regulatory Role | Supports Investigational New Drug applications [64] | Integral for FDA/EMA drug approvals [64] |
| Patient Impact | Identifies promising drug candidates for clinical trials [64] | Enables personalized treatment and therapeutic monitoring [64] |
| Common Technologies | Single-cell RNA sequencing, CRISPR-based functional genomics, high-throughput screening [64] | Liquid biopsy, digital biomarkers, wearable sensors, advanced imaging [64] |
Preclinical Applications: Tools and Models for Discovery
Advanced Model Systems for Cytokine Research
Preclinical cytokine sensing relies on increasingly sophisticated model systems that better recapitulate human physiology. The emergence of bioengineered immunocompetent platforms represents a significant advancement, enabling more accurate assessment of cytokine dynamics within human-relevant contexts. For instance, organotypic chips that recapitulate microarchitectural and pathophysiological characteristics of human tissues provide unprecedented opportunities for real-time spatiotemporal monitoring of immune responses [66]. These systems permit researchers to observe cytokine-mediated interactions, including immune cell extravasation, target recognition, immune activation, and cytotoxicity, within a controlled yet physiologically relevant environment [66].
Patient-derived organoids have revolutionized preclinical cytokine research by replicating human tissue biology more accurately than traditional two-dimensional cell lines [64]. These three-dimensional culture systems allow for biomarker discovery in controlled laboratory settings while maintaining patient-specific characteristics. Similarly, patient-derived xenografts provide clinically relevant insights into drug responses and are particularly crucial for validating cancer biomarkers and assessing resistance mechanisms [64]. For immunotherapy research, humanized mouse models engineered to carry components of the human immune system have become indispensable for cytokine biomarker discovery, providing critical insights into drug interactions with human immune cells [64].
Preclinical Cytokine Sensing Methodologies
Table 2: Preclinical Cytokine Sensing and Monitoring Technologies
| Technology | Key Applications | Advantages | Limitations |
|---|---|---|---|
| Single-Cell RNA Sequencing | Heterogeneity within cell populations, biomarker signatures [64] | Unprecedented resolution of cellular responses | Loss of spatial context, technical complexity |
| CRISPR-Based Functional Genomics | Identify genetic biomarkers influencing drug response [64] | Systematic functional screening | Off-target effects, translation challenges |
| Microfluidic Organ-on-a-Chip | Dynamic biomarker discovery, drug screening [64] | Human physiological relevance, real-time monitoring | Limited throughput, specialized expertise required |
| Multiscale Quantitative Systems Pharmacology Modeling | Characterize biodistribution and tumor killing kinetics [67] | Integrates multiscale knowledge, informs dosing strategies | Computational complexity, model validation required |
| Multiplex Cytokine Assays | Comprehensive cytokine profiling, pathway analysis [5] | High-parameter data from limited samples | Cost, data analysis complexity |
Experimental Protocol: Dynamic Cytokine Monitoring in Preclinical Models
Objective: To evaluate dynamic changes in cytokine levels as prognostic indicators in disease models.
Materials:
- Animal model of disease (e.g., elderly mouse model for CAP studies)
- Bio-Plex Pro Human Cytokine 27-plex Assay or similar multiplex platform
- Centrifuge and sample storage equipment (-80°C freezer)
- Flow cytometer or compatible analyzer
- Statistical analysis software (IBM SPSS, GraphPad Prism)
Procedure:
- Baseline Sample Collection: Collect blood samples at admission/time of intervention via approved venipuncture methods [5].
- Follow-up Sampling: Obtain subsequent samples within 48 hours using consistent collection protocols [5].
- Sample Processing: Centrifuge blood samples at appropriate g-force, aliquot serum, and store at -80°C until analysis [5].
- Cytokine Measurement: Perform multiplex cytokine analysis according to manufacturer protocols, measuring key cytokines including IL-1β, IL-2, IL-6, IL-8, IL-10, TNF-α, and others relevant to the research context [5].
- Dynamic Change Calculation: Calculate relative changes from baseline using the formula:
Dynamic Change Ratio = (Follow-up Value - Baseline Value) / Baseline Value[5]. - Statistical Analysis: Compare dynamic changes between experimental groups using appropriate statistical tests (e.g., Mann-Whitney U test for non-normally distributed variables) with significance defined as p < 0.05 [5].
Interpretation: In elderly CAP models, an 88% increase in IL-6 within 48 hours distinguished non-survivors from survivors who showed a 49% decrease, demonstrating the prognostic value of dynamic cytokine monitoring [5].
Diagram 1: Preclinical cytokine monitoring workflow.
Clinical Applications: Tools for Human Trials and Diagnostics
Clinical Cytokine Sensing Technologies
Clinical applications of cytokine sensing demand technologies that are not only accurate and reliable but also practical for implementation in healthcare settings and acceptable to patients. Non-invasive wearable biosensors have emerged as a transformative technology for continuous inflammation monitoring, offering significant advantages in convenience, comfort, and the ability to provide real-time data [68]. These devices include microneedle patches, flexible electronic skins, and textile-based sensors that can detect inflammatory biomarkers in biofluids such as sweat and interstitial fluid [68]. For cytokine monitoring specifically, these platforms aim to detect key inflammatory markers including IL-1β, IL-6, IL-8, TNF-α, IFN-γ, and CRP, with temporal kinetics that mimic their expression in serum [68].
Liquid biopsy approaches have gained substantial traction for clinical cytokine monitoring, enabling non-invasive detection of inflammatory markers through circulating tumor DNA (ctDNA) and other blood-based biomarkers [64]. This technology is particularly valuable for tracking minimal residual disease and predicting relapse in oncology patients, where cytokine profiles often provide early indicators of treatment response or disease progression. Advanced imaging biomarkers utilizing PET, MRI, and CT scans have evolved to track molecular-level responses to treatments, refining disease monitoring and assessment capabilities in clinical practice [64]. The integration of AI and machine learning with these clinical data streams has further enhanced the ability to identify novel biomarker signatures and predict treatment responses, moving beyond static measurements to dynamic profiling [64].
Analytical Validation for Clinical Implementation
The transition of cytokine sensing technologies from research tools to clinically validated diagnostics requires rigorous analytical validation to meet regulatory standards. This process encompasses both analytical validation, which ensures the test accurately measures the intended biological parameter, and clinical validation, which demonstrates that the biomarker correlates with meaningful clinical outcomes or treatment responses [64]. Regulatory agencies including the FDA and EMA require extensive clinical trial data to ensure the safety, efficacy, and reliability of biomarkers in drug development, with submissions forming part of the Investigational New Drug or New Drug Application processes [64].
For cytokine sensing technologies specifically, key validation parameters include:
- Accuracy and precision across the measurable range of cytokine concentrations
- Reproducibility across multiple sites and operators
- Stability under various storage conditions
- Specificity in complex biological matrices
- Clinical performance characteristics including sensitivity, specificity, and predictive values
The increasing emphasis on dynamic monitoring rather than single-time-point measurements represents a paradigm shift in clinical cytokine assessment, as research demonstrates that cytokine dynamics may better predict outcomes than absolute concentrations [5].
Experimental Protocol: Integrating Cytokine Dynamics with Clinical Severity Scores
Objective: To enhance the prognostic accuracy of clinical severity scores through integration with dynamic cytokine monitoring.
Materials:
- Patient population meeting inclusion criteria (e.g., elderly CAP patients)
- Standard severity scoring tools (PSI, CURB-65)
- Blood collection supplies
- Multiplex cytokine analysis platform
- Statistical software capable of ROC curve analysis
Procedure:
- Patient Enrollment: Recruit eligible patients according to established criteria (e.g., age ≥65 years with radiographically confirmed CAP) [5].
- Baseline Assessment: Calculate traditional severity scores (PSI and CURB-65) at admission [5].
- Serial Blood Collection: Obtain blood samples at admission and within 48 hours using consistent phlebotomy procedures [5].
- Cytokine Measurement: Process samples and analyze cytokine levels using validated multiplex assays, with particular attention to IL-6 based on its established prognostic value [5].
- Dynamic Change Calculation: Compute relative changes in cytokine levels using the standard formula:
Dynamic Change Ratio = (48h Value - Baseline Value) / Baseline Value[5]. - Integrated Model Development: Combine traditional severity scores with cytokine dynamic changes using multivariate analysis.
- Predictive Performance Assessment: Evaluate models using Receiver Operating Characteristic curve analysis, comparing area under the curve values for individual parameters versus combined approaches [5].
Interpretation: In elderly CAP patients, while PSI alone showed an AUC of 0.6631 and CURB-65 an AUC of 0.6231, integration with IL-6 dynamics significantly improved predictive accuracy (PSI + IL-6: AUC = 0.7676; CURB-65 + IL-6: AUC = 0.7564) [5].
Diagram 2: Clinical integration of cytokine dynamics with severity scores.
The Scientist's Toolkit: Essential Research Reagent Solutions
Core Reagents and Platforms
Table 3: Essential Research Reagents for Cytokine Sensing Applications
| Reagent/Platform | Function | Preclinical Application | Clinical Application |
|---|---|---|---|
| Bio-Plex Pro Human Cytokine Assays | Multiplex cytokine quantification | Comprehensive cytokine profiling in disease models [5] | Validation of biomarker signatures in patient cohorts [5] |
| Patient-Derived Organoids | 3D culture systems replicating human tissue biology | Study patient-specific drug responses and disease mechanisms [64] | Bridge to clinical responses; ex vivo therapeutic testing [64] |
| Orthogonal Cytokine-Receptor Platform | Selective activation of specific cytokine pathways | Probe specific JAK-STAT signaling outputs [65] | Engineer therapeutic T cells with enhanced functionality [65] |
| Microfluidic Organ-on-Chip Systems | Mimic human physiological conditions | Dynamic biomarker discovery in human-relevant context [66] | Personalized therapy screening platform [66] |
| Wearable Biosensors | Continuous biomarker monitoring in biofluids | Limited application in preclinical models | Clinical monitoring of inflammatory biomarkers in sweat/ISF [68] |
| scRNA-seq Platforms | Single-cell resolution of transcriptional responses | Identify heterogeneous cellular responses to therapy [64] | Define patient-specific immune responses in clinical trials [64] |
Emerging Technologies and Future Directions
The field of cytokine sensing is rapidly evolving with several emerging technologies poised to bridge the gap between preclinical discovery and clinical application. Non-invasive wearable biosensors represent a particularly promising direction, with advancements in microneedle patches, flexible electronic skins, and textile-based sensors enabling continuous monitoring of inflammatory biomarkers in clinically relevant biofluids [68]. These technologies address the critical need for convenient, comfortable monitoring platforms that can provide real-time data for chronic disease management, though challenges remain in achieving reliable detection of key inflammatory biomarkers with sufficient sensitivity and specificity [68].
Engineered cytokine receptor systems offer innovative approaches to manipulate cellular responses for therapeutic purposes. Recent research demonstrates that expanding the cytokine receptor alphabet through orthogonal receptor platforms can reprogram T cells into diverse functional states with enhanced therapeutic properties [65]. For instance, T cells engineered with orthogonal IL-22R (o22R) exhibit stem-like and exhaustion-resistant transcriptional and chromatin landscapes, while orthogonal GCSFR (oGCSFR) induces a myeloid-like state with phagocytic capacity [65]. These approaches enable diversification of T cell states beyond those induced by natural cytokines, potentially addressing current limitations in cell therapies.
Integrated microphysiological systems continue to advance in physiological relevance, with recent developments including bioengineered immunocompetent chips that recapitulate microarchitectural and pathophysiological characteristics of human leukemia bone marrow stromal and immune niches [66]. These systems enable real-time spatiotemporal monitoring of therapeutic cell functionality, including extravasation, target recognition, immune activation, and cytotoxicity, providing unprecedented insights into dynamic cytokine-mediated interactions within human-relevant contexts [66]. As these technologies mature, they offer the potential to significantly improve the predictive accuracy of preclinical testing, enhancing translation to clinical success.
The convergence of these technological advances with artificial intelligence and machine learning approaches is creating new opportunities for predictive biomarker discovery and validation. The integration of multi-omics data streams—including genomics, transcriptomics, proteomics, and metabolomics—provides a comprehensive view of disease mechanisms and biomarker interactions, potentially overcoming current challenges in biomarker translation and validation [64]. As these integrated approaches continue to evolve, they promise to enhance the precision and efficiency of therapeutic development across the preclinical-clinical continuum.
Conclusion
The field of cytokine sensing is undergoing a transformative shift, moving from single-analyte measurements toward dynamic, multiplexed, and highly sensitive monitoring. This evolution is critically supported by a clear understanding of the relative strengths of established platforms like MSD and CBA for sensitivity and throughput, alongside the promising potential of nanomaterial-enhanced biosensors and synthetic biology approaches for future point-of-care applications. For researchers and drug developers, the key takeaway is that strategic technology selection, guided by robust comparative data, is paramount for de-risking drug development—particularly in high-stakes areas like TCE therapy and oncology. The future will be shaped by continued innovation in orthogonal sensing, AI-driven data analysis, and the development of integrated platforms that provide real-time, actionable cytokine profiles to guide personalized immunotherapy and improve patient outcomes.
References
- 1. Deep insight into cytokine storm: from pathogenesis to ... [https://www.nature.com/articles/s41392-025-02178-y]
- 2. TSCytoPred: a deep learning framework for inferring cytokine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12614104/]
- 3. The Impact of Cytokine Storms on Severe Infectious ... [https://jpmsonline.com/article/the-impact-of-cytokine-storms-on-severe-infectious-diseases-progression-a-narrative-review-720/]
- 4. Roles of cytokine storm in sepsis progression [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1696366/full]
- 5. Dynamic cytokine monitoring enhances CAP severity ... [https://link.springer.com/article/10.1007/s11739-025-03975-7]
- 6. AI, multiplexing, and point-of-care biosensing technologies [https://pubmed.ncbi.nlm.nih.gov/41175281/]
- 7. Simplified flow cytometry-based assay for rapid multi-cytokine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12245854/]
- 8. Cytokine TV: Implantable Protein Sensors Monitor Live ... [https://www.insideprecisionmedicine.com/topics/molecular-dx/cytokine-tv-implantable-protein-sensors-monitor-live-inflammation/]
- 9. Machine learning-based predictive model for high [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1692892/full]
- 10. rethinking drug efficacy evaluation in cancer immunotherapy [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1609606/full]
- 11. Rethinking the biomarker landscape in gastric cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12476615/]
- 12. High-Throughput Cytokine Detection Platform for ... [https://www.sciencedirect.com/science/article/pii/S2472630325001050]
- 13. Cross-platform comparison of immune signatures in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10103529/]
- 14. Conversion of natural cytokine receptors into orthogonal ... [https://www.nature.com/articles/s41589-025-01986-1]
- 15. The Interleukin Network in Sepsis: From Cytokine Storm to ... [https://www.mdpi.com/2075-4418/15/22/2927]
- 16. CRISPR-assisted bioanalytical sensing of cytokines [https://www.sciencedirect.com/science/article/abs/pii/S0165993625001864]
- 17. Size, Share and Opportunities, Cytokine -2032 Market 2025 [https://www.coherentmarketinsights.com/market-insight/cytokine-market-5238]
- 18. Size, Share & Cytokine Outlook 2035 Market Growth [https://www.researchnester.com/reports/cytokine-market/5867]
- 19. Exploring Cytokine Detection Service Trends 2025-2033 [https://www.marketreportanalytics.com/reports/cytokine-detection-service-52457]
- 20. Cytokine ELISA Protocol [https://www.bdbiosciences.com/en-us/resources/protocols/cytokine-elisa]
- 21. ELISA AND MULTIPLEX TECHNOLOGIES FOR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2562869/]
- 22. Simplified flow cytometry-based assay for rapid multi- ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1594141/full]
- 23. Application Guides / ELISA Protocol [https://www.2bscientific.com/resources/application-guides/elisa-guide/elisa-protocol]
- 24. General ELISA Protocols | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/references/protocols/cell-and-tissue-analysis/elisa-protocol/general-elisa-protocol.html]
- 25. Flow Cytometry: An Overview - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5939936/]
- 26. Flow Cytometry Application Notes [https://www.thermofisher.com/us/en/home/life-science/cell-analysis/flow-cytometry/flow-cytometry-learning-center/flow-cytometry-resource-library/flow-cytometry-application-notes.html]
- 27. How to Run an R&D Systems Luminex® Assay [https://www.rndsystems.com/resources/protocols/how-run-rd-systems-luminex-assay]
- 28. Recent Advances in Photonic Crystal Fiber-Based SPR ... [https://www.mdpi.com/2072-666X/16/7/747]
- 29. Advances in PCF-SPR sensors: a comprehensive review of ... [https://www.sciencedirect.com/science/article/abs/pii/S0263224125025850]
- 30. Bio-sensing applications of a 2:1 photonic crystal multiplexer [https://www.nature.com/articles/s41598-025-01238-1]
- 31. Graphene-Enhanced SPR Sensors in 2025 [https://www.linkedin.com/pulse/graphene-enhanced-spr-sensors-2025-smarter-biosensing-j1zoc]
- 32. Advanced SPR biosensor with optimized gold-TiO2 D ... [https://www.nature.com/articles/s41598-025-24697-y]
- 33. Highly Sensitive D-Shaped Photonic Crystal Fiber SPR ... [https://link.springer.com/article/10.1007/s11468-025-03310-y]
- 34. Emerging trends in AI-integrated optical biosensors for point ... [https://pubs.rsc.org/en/content/articlehtml/2025/cc/d5cc04899k]
- 35. Current landscape of T-cell engagers in early-phase ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1665838/full]
- 36. Single cell multi-omics reveals re-dosing with CD3 ... [https://www.sciencedirect.com/science/article/pii/S0753332225001672]
- 37. T cell engagers: expanding horizons in oncology and beyond [https://www.nature.com/articles/s41416-025-03125-y]
- 38. Biomarkers of cytokine release syndrome and neurotoxicity ... [https://biomarkerres.biomedcentral.com/articles/10.1186/s40364-018-0116-0]
- 39. Identification of early predictive biomarkers for severe ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11424402/]
- 40. Prediction of severe CRS and determination of biomarkers ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2023.1273507/full]
- 41. Building “Smart” Cell Sensors for Safer, More Precise Cancer ... [https://www.mccormick.northwestern.edu/news/articles/2025/08/building-smart-cell-sensors-for-safer-more-precise-cancer-therapies/]
- 42. New paper: Conversion of natural cytokine receptors into ... [https://www.leonard.northwestern.edu/2025/08/22/new-preprint-conversion-of-natural-cytokine-receptors-into-orthogonal-synthetic-biosensors/]
- 43. Detection and Quantification of Cytokines and Other ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5659280/]
- 44. Multiplexed Cytokine Analysis in Drug Development [https://www.bioagilytix.com/blog/multiplexed-cytokine-analysis-in-drug-development/]
- 45. Advancing disease biomarker research with EV multiplex ... [https://www.drugtargetreview.com/article/190607/advancing-disease-biomarker-research-with-ev-multiplex-profiling/]
- 46. Multiplex Serum Cytokine Immunoassay Using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4447431/]
- 47. High Throughput Screening Market Size, Share Report [https://www.thebusinessresearchcompany.com/report/high-throughput-screening-hts-global-market-report]
- 48. High Throughput Screening Market Forecast, 2025-2032 [https://www.coherentmarketinsights.com/industry-reports/high-throughput-screening-market]
- 49. High Throughput Screening Market [https://www.futuremarketinsights.com/reports/high-throughput-screening-market]
- 50. Developing Robust In Vitro Cell-Based Assays for High ... [https://www.marinbio.com/developing-robust-in-vitro-cell-based-assays-for-high-throughput-screening-hts/]
- 51. A robust bacterial high-throughput screening assay to ... [https://www.sciencedirect.com/science/article/abs/pii/S0014299925008027]
- 52. Optimization and development of a high-throughput TR-FRET ... [https://pubmed.ncbi.nlm.nih.gov/40393541/]
- 53. How to Choose the Right Cytokine Detection Method for ... [https://cytokine.creative-proteomics.com/choosing-right-cytokine-detection-method-research-success.htm]
- 54. Olink Cytokine Panel vs Other Cytokine Detection Methods [https://olinkpanel.creative-proteomics.com/knowledge/olink-cytokine-panel-vs-other-methods.html]
- 55. Validation and comparison of luminex multiplex cytokine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5738327/]
- 56. Cell-based THUNDER™ cytokine assay [https://www.bmglabtech.com/en/application-notes/excellent-assay-performance-of-thunder-tr-fret-cell-based-cytokine-assays-performed-on-the-pherastar-fsx/]
- 57. 3 Reasons Why the THUNDER™ Human Cytokine Assay ... [https://bioauxilium.com/2023/01/23/3-reasons-why-the-thunder-human-cytokine-assay-kits-are-the-best-tr-fret-kits-on-the-market/]
- 58. AlphaLISA High Performance Human IL-6 Detection Kit [https://www.revvity.com/product/alphalisa-hp-human-il-6-kit-100-pts-al3202hv]
- 59. Unlocking Ultra-Sensitive Cytokine Detection: Insights from ... [https://www.quanterix.com/blog-unlocking-ultra-sensitive-cytokine-detection-insights-from-the-frontage-amp-quanterix-webinar/]
- 60. Research and Application of Dynamic Monitoring ... [https://www.mdpi.com/2227-9717/13/9/3025]
- 61. Sensitive, high-throughput, metabolic analysis by ... [https://www.nature.com/articles/s41467-025-63964-4]
- 62. Transforming cytokine diagnostics: AI, multiplexing, and ... [https://read.qxmd.com/read/41175281/transforming-cytokine-diagnostics-ai-multiplexing-and-point-of-care-biosensing-technologies]
- 63. Nanobiosensors for Key Inflammatory Mediators: Cytokines ... [https://www.sciencedirect.com/science/article/abs/pii/S0009898125006060]
- 64. Preclinical vs. Clinical Biomarkers: Understanding Their ... [https://blog.crownbio.com/preclinical-vs-clinical-biomarkers-understanding-their-distinct-roles-in-drug-development]
- 65. Expanding the cytokine receptor alphabet reprograms T ... [https://www.nature.com/articles/s41586-025-09393-1]
- 66. Bioengineered immunocompetent preclinical trial-on-chip ... [https://www.nature.com/articles/s41551-025-01428-2]
- 67. Mechanistic data-informed multiscale quantitative systems ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12516987/]
- 68. Non-Invasive Wearables in Inflammation Monitoring [https://pmc.ncbi.nlm.nih.gov/articles/PMC12190971/]