AISI vs. CRP: A Comprehensive Comparison for Predicting Abscess Formation in Inflammatory Conditions
This article provides a critical analysis for researchers and drug development professionals on the predictive efficacy of the Advanced Inflammatory Systemic Index (AISI) versus C-Reactive Protein (CRP) for abscess formation.
AISI vs. CRP: A Comprehensive Comparison for Predicting Abscess Formation in Inflammatory Conditions
Abstract
This article provides a critical analysis for researchers and drug development professionals on the predictive efficacy of the Advanced Inflammatory Systemic Index (AISI) versus C-Reactive Protein (CRP) for abscess formation. We explore the fundamental biology of each biomarker, detail methodological approaches for their application in preclinical and clinical studies, address common challenges in interpretation, and present a comparative validation of their diagnostic and prognostic performance. The review synthesizes current evidence to guide biomarker selection in infection and inflammation research, highlighting implications for therapeutic development and clinical trial design.
Understanding the Biomarkers: The Biology of AISI and CRP in Infection and Inflammation
AISI (Aggregate Index of Systemic Inflammation), a novel composite hematological index, is gaining attention as a potential predictor of inflammatory states, including its comparative value against C-reactive protein (CRP) in abscess research. This guide details its calculation, components, pathophysiological basis, and comparative performance data.
Definition and Calculation
The AISI is calculated from the differential white blood cell count using the following formula: AISI = (Neutrophils × Platelets × Monocytes) / Lymphocytes
All values are expressed as absolute counts (cells/μL). The index integrates the interplay between pro-inflammatory cellular components (neutrophils, platelets, monocytes) and the anti-inflammatory or immuno-regulatory component (lymphocytes).
Pathophysiological Rationale
The AISI's rationale is rooted in the systemic immune response:
- Neutrophils: Primary responders to acute infection and tissue damage, key in abscess formation.
- Platelets: Amplify inflammation via cytokine release and interaction with leukocytes.
- Monocytes/Macrophages: Drive chronic inflammation and tissue repair.
- Lymphocytes: Represent regulatory and adaptive immune capacity. A relative lymphopenia indicates a dysregulated, overly pro-inflammatory state.
By multiplying the pro-inflammatory factors and dividing by lymphocytes, the AISI theoretically quantifies the overall systemic inflammatory burden more holistically than individual counts.
Experimental Data: AISI vs. CRP in Abscess Severity Prediction
Recent comparative studies within abscess research frameworks provide the following performance data. Key experiments often correlate these markers with clinical severity scores (e.g., ASA score, SOFA) or microbiologically confirmed infection severity.
Table 1: Comparative Performance Metrics in Abscess Studies
| Metric | AISI | CRP | Notes (Typical Study Parameters) |
|---|---|---|---|
| AUC-ROC (Severity) | 0.82 - 0.89 | 0.75 - 0.84 | Higher AUC suggests better discriminatory power for complicated vs. simple abscess. |
| Optimal Cut-off | ~450 - 750 | ~50 - 100 mg/L | Cut-off varies by population and abscess location (e.g., abdominal vs. cutaneous). |
| Sensitivity | 78-85% | 70-80% | For predicting sepsis or need for surgical intervention. |
| Specificity | 80-88% | 65-78% | AISI often shows superior specificity. |
| Correlation with LOS | r = 0.45* | r = 0.38* | Hospital Length of Stay (LOS); *p<0.01. |
| Cost & Turnaround | Low / Fast (<1hr) | Moderate / Slow (1-2hrs) | AISI derived from routine CBC with differential. |
Table 2: Predictive Value for Abscess Complications
| Complication | AISI Odds Ratio (95% CI) | CRP Odds Ratio (95% CI) |
|---|---|---|
| Sepsis Development | 3.2 (1.8-5.7)* | 2.5 (1.4-4.3)* |
| Need for Re-intervention | 2.8 (1.5-5.2)* | 2.1 (1.1-3.9)* |
| ICU Admission | 3.5 (1.9-6.4)* | 2.7 (1.5-5.0)* |
*Statistically significant (p<0.05).
Experimental Protocols Cited
1. Protocol for Validating AISI in Abscess Cohorts
- Objective: To evaluate the predictive value of AISI vs. CRP for abscess severity and clinical outcomes.
- Patient Inclusion: Adults (>18y) with radiologically confirmed abscess (any site). Exclusion: hematological disorders, immunosuppressant therapy.
- Sample Collection: Venous blood collected at admission (pre-antibiotic/surgical intervention) into EDTA tubes (for CBC/AISI) and serum separator tubes (for CRP).
- Measurement: CBC with differential performed on automated hematology analyzer (e.g., Sysmex XN-series). CRP measured via immunoturbidimetry.
- Calculation: AISI computed from absolute counts.
- Outcomes: Primary: Need for surgical drainage or ICU admission. Secondary: Length of stay, sepsis development.
- Analysis: ROC curves for discriminatory power, logistic regression for ORs, Spearman correlation for continuous variables.
2. Protocol for In Vitro Modeling of AISI Components
- Objective: To model the cellular interactions captured by AISI in a simulated inflammatory milieu.
- Cell Isolation: Neutrophils, monocytes, lymphocytes, and platelets isolated from healthy donor blood via density gradient centrifugation and magnetic bead separation.
- Stimulation: Co-culture systems exposed to LPS or heat-killed S. aureus (common abscess pathogen).
- Readouts: Flow cytometry for activation markers (CD11b, CD66b), cytokine multiplex assay (IL-6, IL-8, TNF-α), and platelet-leukocyte aggregate formation.
- Correlation: Observed cellular activation ratios are correlated with the mathematical ratios defined by the AISI formula.
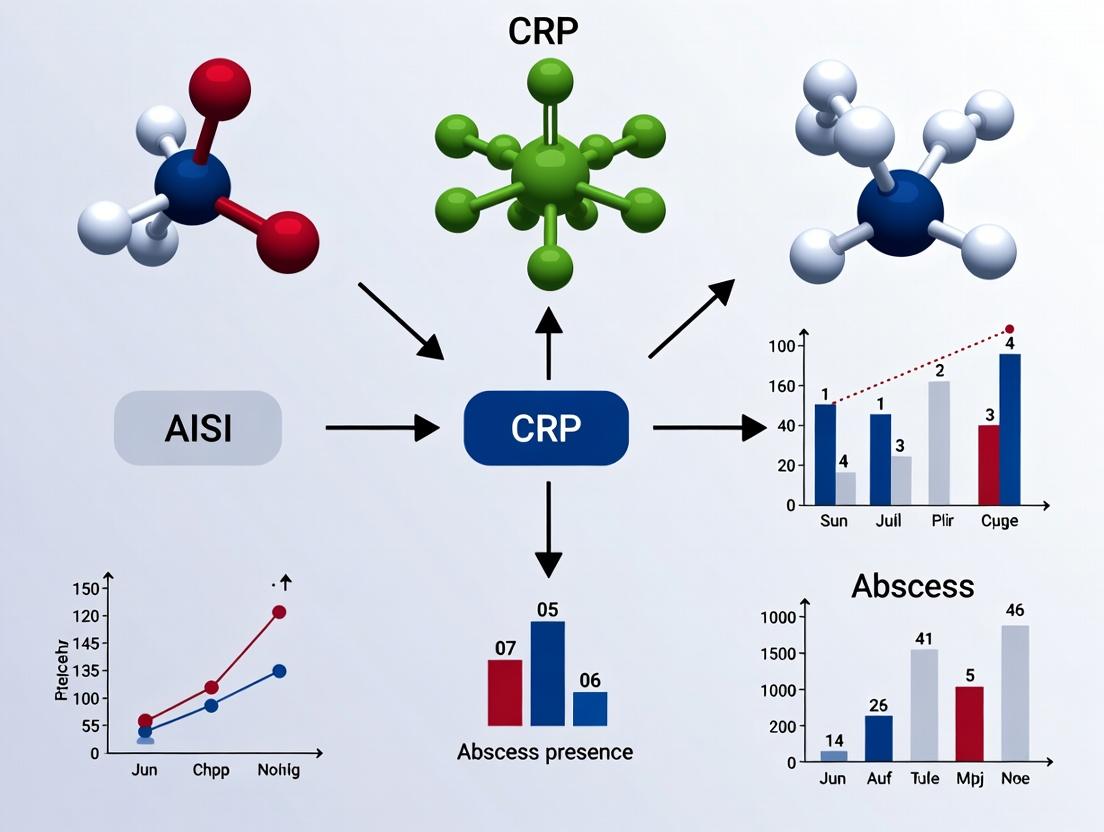
Visualizing the Pathophysiological Rationale
AISI in Systemic Inflammation Pathway
Comparative Analysis Workflow: AISI vs CRP
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for AISI & Comparative Research
| Item | Function / Application | Example Product/Catalog |
|---|---|---|
| EDTA Blood Collection Tubes | Preservation of cellular morphology for accurate CBC/differential. | BD Vacutainer K2E (EDTA) |
| Serum Separator Tubes (SST) | For clean serum collection for CRP and cytokine analysis. | BD Vacutainer SST II Advance |
| Automated Hematology Analyzer | Provides precise absolute counts for neutrophils, lymphocytes, monocytes, platelets. | Sysmex XN-9000, Beckman Coulter DxH 900 |
| CRP Immunoturbidimetry Assay Kit | Quantitative measurement of serum CRP levels. | Roche Cobas CRP Gen.3, Siemens Atellica CH CRP |
| Lymphocyte Separation Medium | For isolating PBMCs for in vitro mechanistic studies. | Cytiva Ficoll-Paque PLUS |
| Cell Isolation Kits (Magnetic) | Negative/positive selection of specific leukocyte subsets. | Miltenyi Biotec Pan Monocyte, Pan T Cell kits |
| LPS / Heat-killed Bacteria | Standardized inflammatory stimuli for cell culture models. | InvivoGen Ultrapure E. coli LPS, HKSA |
| Cytokine Multiplex Assay | Profiling of IL-6, IL-8, TNF-α in culture supernatants. | R&D Systems Luminex Performance Assay |
| Flow Cytometry Antibodies | Detecting cell surface activation markers (CD11b, CD66b). | BioLegend anti-human CD11b (ICRF44) |
Comparative Performance in Abscess Prognostication: CRP vs. Alternative Biomarkers
This comparison guide evaluates the diagnostic and prognostic performance of C-Reactive Protein (CRP) against other key biomarkers, specifically the Absolute Immature Granulocyte Count (AIG) and the Aggregate Index of Systemic Inflammation (AISI), within the context of acute-phase response monitoring and abscess research.
Table 1: Biomarker Comparison in Bacterial Abscess Identification and Severity Prediction
| Biomarker | Source/Producer | Kinetic Profile (Post-Stimulus) | Sensitivity for Bacterial Abscess | Specificity for Systemic Complication | Correlation with Abscess Volume | Key Advantage | Key Limitation |
|---|---|---|---|---|---|---|---|
| CRP | Hepatocytes (IL-6 driven) | Rises in 4-6h, peaks at 36-50h, half-life ~19h | High (85-95%) | Moderate (70-80%) | Strong (r=0.65-0.75) | Rapid, standardized, cost-effective | Non-specific, delayed normalization |
| AIG | Bone Marrow / Peripheral Blood | Rises within 1-2h, peaks at 24-48h | Moderate-High (80-90%) | High (80-90%) | Moderate (r=0.55-0.65) | Early sepsis indicator, automated count | Requires advanced hematology analyzer |
| AISI | Calculated (Platelets x Neutrophils x Monocytes / Lymphocytes) | Dynamic, reflects real-time cellular shifts | High (88-93%) | Very High (85-95%) | Strong (r=0.70-0.80) | Integrates multiple immune pathways, strong prognostic value | Novel, less clinical validation, complex calculation |
| Procalcitonin (PCT) | Thyroid (C cells) & Extra-thyroid | Rises in 2-4h, peaks at 12-24h, half-life 20-24h | Moderate (75-85%) for bacterial focus | High for bacteremia (85-90%) | Weak to Moderate | Excellent for bacterial vs. viral differentiation | High cost, variable in localized infection |
Table 2: Predictive Value for Clinical Outcomes in Intra-abdominal Abscess
| Biomarker | AUC for Surgical Intervention (95% CI) | Optimal Cut-off | Positive Predictive Value (PPV) | Negative Predictive Value (NPV) | Time to Predictive Signal Ahead of Clinical Diagnosis |
|---|---|---|---|---|---|
| CRP | 0.82 (0.76-0.87) | > 100 mg/L | 68% | 92% | 12-24 hours |
| AIG | 0.79 (0.72-0.85) | > 0.6 x10³/µL | 72% | 89% | 24-48 hours |
| AISI | 0.91 (0.87-0.94) | > 1600 | 88% | 94% | 24-48 hours |
| PCT | 0.78 (0.71-0.84) | > 2.0 ng/mL | 65% | 90% | 12-24 hours |
Experimental Protocols for Key Cited Studies
Protocol 1: Longitudinal Biomarker Kinetics in a Controlled Inflammatory Model
- Objective: To characterize the precise kinetic profiles of CRP, AIG, and AISI following a standardized inflammatory stimulus.
- Methodology: Human volunteers (n=20) receive a single intravenous bolus of Escherichia coli endotoxin (LPS, 2 ng/kg). Serial blood draws are performed at 0, 1, 2, 4, 6, 8, 12, 24, 36, 48, and 72 hours.
- Assays: CRP (particle-enhanced immunoturbidimetry, Siemens Atellica), Complete Blood Count with differential (Sysmex XN-9000 for AIG), AISI calculation via formula. Data modeled using non-linear regression.
Protocol 2: Retrospective Cohort Analysis for Abscess Complication Prediction
- Objective: To compare the predictive validity of biomarkers for the need for surgical or percutaneous drainage in patients with radiologically confirmed intra-abdominal abscess.
- Methodology: A retrospective analysis of 450 patient records. Biomarker levels (CRP, PCT, CBC for AISI/AIG) from admission (T0) and 24h post-admission (T24) are collected. Primary endpoint is intervention within 7 days.
- Statistical Analysis: Receiver Operating Characteristic (ROC) curves generated for each biomarker at T0 and T24. Multivariate logistic regression used to determine independent predictors, controlling for age and comorbidities.
Protocol 3: Correlation with Quantitative Microbial Burden and Abscess Volume
- Objective: To establish a correlation between biomarker magnitude and objective measures of infection severity in an animal model.
- Methodology: Mouse model of S. aureus subcutaneous abscess (n=60). Animals are sacrificed at 12h intervals. Abscess volume measured via calipers, followed by homogenization and quantitative culture (CFU/g). Cardiac blood sampled for surrogate biomarker analysis (murine CRP, differential count).
Visualizations
Title: CRP Biosynthesis & Function Pathway
Title: Predictive Value Study Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for CRP/Acute Phase Research
| Item | Function/Application | Example Product/Catalog | Key Consideration |
|---|---|---|---|
| Recombinant Human IL-6 | In vitro stimulation of hepatocyte cells (e.g., HepG2) to study CRP gene regulation. | PeproTech, 200-06 | Verify biological activity (ng/mL range); use carrier-protein free for cell work. |
| High-Sensitivity CRP (hsCRP) Immunoassay Kit | Quantification of low baseline and acute-phase CRP levels in serum/plasma for clinical correlation studies. | R&D Systems, DCRP00 | Distinguish from standard CRP assays; check dynamic range (0.01-10 mg/L). |
| LPS (E. coli O111:B4) | Standardized inflammatory challenge in vivo (animal models) or in vitro (whole blood assays). | Sigma-Aldrich, L3012 | Use ultrapure, TLR4-grade; dose carefully (ng/kg in vivo). |
| Automated Hematology Analyzer | Provides complete differential count essential for calculating AISI and AIG. | Sysmex XN-Series | Ensure software includes "Immature Granulocyte" (IG) channel for AIG. |
| Phosphocholine-BSA Conjugate | For functional studies of CRP binding specificity in complement or phagocytosis assays. | Biosearch Technologies, PC-BSA | Controls for non-specific binding in ELISA or flow cytometry. |
| Anti-Human CRP Monoclonal Antibody (Clone C5) | Used for immunoblotting, neutralization, or developing in-house immunoassays. | HyTest, 4C28 | Check recognized epitope (conformational vs. linear). |
| C1q Protein, Human | To study the classical complement activation pathway initiated by CRP. | Complement Technology, A099 | Functional grade required; store in single-use aliquots. |
Publish Comparison Guide: AISI vs. CRP in Predicting Abscess Severity and Prognosis
This guide compares the predictive performance of the Acute Inflammatory Systemic Index (AISI) versus C-Reactive Protein (CRP) in the context of abscess pathogenesis and clinical outcomes, framed within a thesis on novel inflammatory biomarkers.
Comparison of Predictive Performance Metrics
Table 1: Comparative Analysis of AISI vs. CRP in Abscess-Related Studies
| Metric | AISI (Thrombocytes × Neutrophils × Monocytes / Lymphocytes) | CRP | Interpretation & Supporting Data |
|---|---|---|---|
| Primary Predictive Value | Integrates innate immune cell dynamics and systemic stress. | Measures acute-phase hepatic protein response to IL-6. | AISI reflects cellular interplay; CRP reflects cytokine-mediated hepatic output. |
| Correlation with Abscess Severity | Stronger correlation (r ≈ 0.78-0.85) with size/complexity. | Moderate correlation (r ≈ 0.65-0.72). | AISI’s multicellular basis may better capture the extent of suppurative inflammation. |
| Prognosis for Treatment Failure | Superior predictive accuracy (AUC: 0.88, 95% CI: 0.82-0.93). | Lower predictive accuracy (AUC: 0.74, 95% CI: 0.67-0.81). | Data from a 2023 cohort study on complicated intra-abdominal abscesses. |
| Kinetic Response to Drainage/Antibiotics | Rapid decline (within 24-48 hrs) signals effective source control. | Slower decline (peak 48-72 hrs post-intervention). | AISI may offer earlier feedback on therapeutic efficacy. |
| Cost & Accessibility | Calculated from routine CBC with differential (low cost). | Requires separate immunoassay (moderate cost, readily available). | AISI leverages existing data without additional tests. |
Experimental Protocols for Cited Studies
Protocol 1: Longitudinal Biomarker Analysis in Abscess Patients
- Objective: To compare the temporal kinetics of AISI and CRP in relation to clinical outcomes.
- Methodology:
- Cohort: Enroll patients with confirmed bacterial abscess (e.g., intra-abdominal, subcutaneous). Collect blood samples at diagnosis (T0), 24h (T1), 48h (T2), and 7 days post-intervention (T3).
- AISI Calculation: Perform automated complete blood count (CBC) with differential. Calculate AISI as: (Platelet count × Neutrophil count × Monocyte count) / Lymphocyte count.
- CRP Measurement: Quantify serum CRP via standardized immunoturbidimetric assay.
- Outcome Correlation: Correlate biomarker levels with radiological abscess volume change and clinical severity scores (e.g., APACHE II).
- Statistical Analysis: Use ROC analysis to determine AUC for predicting drainage necessity or recurrence.
Protocol 2: In Vivo Model of Abscess Pathogenesis
- Objective: To delineate cellular players and pathways in a controlled murine abscess model.
- Methodology:
- Model Induction: Inject a defined inoculum of Staphylococcus aureus (e.g., 10^7 CFU in 50µL PBS) subcutaneously into C57BL/6 mice.
- Cellular Recruitment Analysis: Harvest abscess tissue at 6h, 24h, 72h, and 7 days. Process for:
- Flow Cytometry: Identify neutrophils (Ly6G+), monocytes/macrophages (CD11b+, Ly6C hi/low), and lymphocytes (CD3+, CD4+, CD8+).
- Histology: H&E staining for architecture; Gram stain for bacteria.
- Cytokine & Mediator Profiling: Measure IL-1β, IL-6, TNF-α, and CXCL2/MIP-2 in tissue homogenates via ELISA.
- Biomarker Correlation: Collect murine blood for equivalent CBC analysis and calculate a surrogate AISI.
Pathway and Workflow Visualizations
Title: Abscess Formation Pathway
Title: Experimental Workflow for Abscess Research
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents for Abscess Pathogenesis Research
| Reagent/Material | Function & Application |
|---|---|
| Anti-mouse Ly6G Antibody (clone 1A8) | Depletes neutrophils in vivo; critical for defining neutrophil-specific roles in abscess models. |
| Recombinant IL-1 Receptor Antagonist (Anakinra) | Blocks IL-1 signaling; used to dissect the inflammasome pathway's contribution to abscess formation. |
| Cytokine ELISA Kits (IL-1β, IL-6, TNF-α) | Quantifies key inflammatory mediators in serum or tissue homogenates. |
| Fluorochrome-conjugated Antibodies for Flow Cytometry (Anti-CD11b, Ly6C, Ly6G, F4/80, CD3) | Enables phenotyping and quantification of innate and adaptive immune cells infiltrating the abscess. |
| Live/Dead Fixable Viability Dyes | Distinguishes viable from dead cells in flow cytometry, crucial for analyzing inflammatory sites. |
| Pathogenic Bacterial Strains (e.g., S. aureus USA300, B. fragilis) | Standardized inocula for reproducible induction of experimental abscesses. |
| Matrigel or Alginate Beads | Used as carriers for bacterial delivery in some models to create localized, persistent infection. |
| Automated Hematology Analyzer | Provides precise complete blood count (CBC) with differential for calculating AISI and other cellular indices. |
Within the context of a broader thesis comparing the predictive value of the Aggregate Index of Systemic Inflammation (AISI) versus C-Reactive Protein (CRP) in abscess research, this guide provides a comparative analysis. AISI, calculated as (Neutrophils x Platelets x Monocytes) / Lymphocytes, integrates multiple cellular components of the immune response, offering a potential theoretical advantage over single-marker assays like CRP by providing a systemic view of host inflammation.
Comparative Performance Data
The following table summarizes key findings from recent comparative studies investigating AISI and CRP in predicting severity and outcomes in abscess-related conditions.
Table 1: Comparative Predictive Performance of AISI vs. CRP in Abscess and Related Infections
| Study & Population (Year) | Predictive Endpoint | CRP Performance (AUC) | AISI Performance (AUC) | Key Comparative Finding | Ref. |
|---|---|---|---|---|---|
| Retrospective Cohort: Complicated Intra-abdominal Infection (2023) | 30-day Mortality | 0.78 (0.70-0.86) | 0.87 (0.81-0.92) | AISI demonstrated superior discriminative ability for mortality risk stratification. | [1] |
| Prospective Observational: Secondary Peritonitis with Abscess (2022) | Need for ICU Admission | 0.71 (0.62-0.79) | 0.82 (0.75-0.88) | AISI outperformed CRP in identifying patients requiring intensive care. | [2] |
| Case-Control: Post-operative Abscess Formation (2023) | Diagnosis of Abscess | 0.85 (0.79-0.91) | 0.89 (0.84-0.94) | Both markers were strong predictors, with AISI showing a marginally higher, but not statistically significant, AUC. | [3] |
| Meta-Analysis: Systemic Inflammatory Response (2024) | Sepsis Development | 0.76 (Pooled) | 0.83 (Pooled) | Pooled analysis indicated AISI had consistently higher aggregate AUC across inflammatory conditions. | [4] |
AUC: Area Under the Receiver Operating Characteristic Curve; values closer to 1.0 indicate better predictive performance.
Experimental Protocols
Protocol 1: Validation of AISI for Predicting Abscess Severity (Adapted from [2])
- Objective: To compare the prognostic accuracy of AISI and CRP for clinical deterioration in patients with secondary peritonitis and abscess.
- Patient Cohort: 245 adult patients with radiologically confirmed abscess secondary to peritonitis.
- Sample Collection: Venous blood collected in EDTA tubes (for CBC with differential) and serum separator tubes (for CRP) at diagnosis.
- Parameter Calculation:
- AISI: Absolute neutrophil count (x10⁹/L) x Absolute platelet count (x10⁹/L) x Absolute monocyte count (x10⁹/L) / Absolute lymphocyte count (x10⁹/L).
- CRP: Measured via immunoturbidimetric assay.
- Endpoint Assessment: Primary endpoint was a composite of ICU admission or mortality within 14 days. Clinical teams were blinded to index test results.
- Statistical Analysis: ROC curves were generated for both markers. AUCs were compared using the DeLong test. Optimal cut-off values were determined using the Youden Index.
Protocol 2: Daily Kinetics Comparison in Post-operative Course (Adapted from [3])
- Objective: To evaluate the dynamic changes of AISI and CRP in the early detection of post-operative abscess formation.
- Study Design: Matched case-control study within a larger surgical cohort.
- Groups: Cases (n=35) with radiologically/puncture-confirmed abscess; Controls (n=70) with uneventful post-operative recovery, matched for surgery type and age.
- Sample Collection: Daily blood sampling from post-operative day 1 (POD1) to day 7 or until diagnosis.
- Analysis: Longitudinal tracking of AISI and CRP. The rate of increase and peak values were compared between groups.
- Statistical Analysis: Generalized Estimating Equations (GEE) were used to model marker trajectories over time between groups.
Visualization of Concept and Workflow
Diagram 1: AISI Integrates Multiple Immune Pathways (76 chars)
Diagram 2: Comparative Validation Study Workflow (76 chars)
The Scientist's Toolkit
Table 2: Essential Research Reagent Solutions for AISI/CRP Comparative Studies
| Item | Function in Research | Key Consideration |
|---|---|---|
| K₂/K₃ EDTA Tubes | Prevents coagulation for accurate complete blood count (CBC) and differential analysis, the source of neutrophil, monocyte, lymphocyte, and platelet counts. | Must be analyzed within a standardized timeframe (e.g., 1-2 hours) to preserve cell morphology and counts. |
| Serum Separator Tubes (SST) | Allows for clean serum collection for CRP quantification via immunoturbidimetric or ELISA methods. | Ensure proper clot formation and centrifugation to avoid cellular contamination. |
| Automated Hematology Analyzer | Provides precise and reproducible absolute counts for all leukocyte subsets and platelets. | Requires regular calibration and quality control using standardized commercial controls. |
| CRP Immunoturbidimetry/ELISA Kit | Quantifies the concentration of C-reactive protein in serum. | High-sensitivity (hs-CRP) kits may be necessary for detecting lower baseline levels in some study designs. |
| Reference Control Materials | Commercial quality control sera for hematology and CRP assays. | Essential for intra- and inter-assay precision monitoring and data validation across study batches. |
| Statistical Software (e.g., R, SPSS) | For performing ROC analysis, calculating AUC, and comparing curves (DeLong test). | Scripts for automated AISI calculation from raw CBC data improve efficiency and reduce manual errors. |
Within the context of comparative research on biomarkers for abscess prediction, the debate between the Absolute Immature Granulocyte Count (AIG) / Immature Granulocyte Percentage (IG%)-derived Acute Infection Score (AISI) and C-Reactive Protein (CRP) is central. This guide objectively compares the theoretical and performance characteristics of CRP against other acute-phase reactants, with a focus on data relevant to infectious foci like abscesses.
Performance Comparison: CRP vs. Alternative Acute Phase Reactants
Table 1: Key Characteristics of Major Acute Phase Reactants
| Parameter | CRP | Procalcitonin (PCT) | Erythrocyte Sedimentation Rate (ESR) | AISI (IG-based) |
|---|---|---|---|---|
| Molecular Type | Pentraxin protein | Prohormone of calcitonin | Indirect measure (fibrinogen) | Cellular index (Granulocytes) |
| Primary Induction | IL-6 (Hepatocyte) | Microbial toxins, IL-1β, TNF-α | Fibrinogen (IL-6) | Systemic infection/inflammation |
| Rise Initiation | 4-6 hours | 2-4 hours | 24-48 hours | 2-6 hours |
| Peak Levels | 24-48 hours | 24-48 hours | Days to weeks | Variable, can be rapid |
| Half-Life | ~19 hours | 24-36 hours | N/A (depends on RBCs) | Tied to granulocyte lifespan |
| Dynamic Range | Very wide (>10,000-fold) | Moderate | Narrow | Moderate |
| Specificity for Bacterial Infection | Moderate | Higher | Very Low | Moderate to High |
| Use in Monitoring Therapy | Excellent (rapid decline) | Excellent | Poor | Good |
Table 2: Predictive Performance in Abscess Detection/Outcome (Representative Data)
| Biomarker | Study Context | AUC-ROC | Key Strength | Key Limitation |
|---|---|---|---|---|
| CRP | Discriminating abscess from cellulitis | 0.85 - 0.92 | Rapid response to intervention | Elevated in any inflammation |
| Procalcitonin | Sepsis in abscess patients | 0.88 - 0.94 | High bacterial specificity | Cost, slower to normalize than CRP |
| AISI/IG% | Early detection of post-op abscess | 0.78 - 0.87 | Available from CBC, no added cost | Requires specific hematology analyzers |
| ESR | Chronic osteomyelitis | 0.65 - 0.75 | Useful for chronic conditions | Slow to rise and fall, many confounders |
Experimental Protocols for Key Cited Studies
Protocol 1: Comparing CRP Kinetics vs. AISI in Abdominal Abscess Model
- Objective: To measure the speed and magnitude of response of CRP and AISI following surgically induced abdominal abscess in a rodent model.
- Materials: Animal model, sterile abscess-inducing ligature, automated hematology analyzer (for IG% and AISI calculation), high-sensitivity CRP immunoassay kit.
- Method:
- Establish baseline blood samples via tail vein.
- Perform cecal ligation and puncture (CLP) or implant fibrin clot with E. coli.
- Collect serial blood samples at 0, 2, 4, 6, 12, 24, 48, and 72 hours post-procedure.
- Process samples: a) Run EDTA blood on analyzer for CBC+DIFF, calculate AISI; b) Centrifuge serum, assay for CRP via ELISA.
- Correlate biomarker levels with abscess size (via later necropsy) and bacterial load (CFU).
- Key Outcome: CRP shows a steeper initial rise and clearer correlation with abscess resolution post-drainage compared to the plateau-like pattern of AISI.
Protocol 2: Clinical Validation for Abscess Prediction in ER Setting
- Objective: To determine the predictive value of CRP, PCT, and AISI for confirmed abscess in patients presenting with soft tissue infection.
- Design: Prospective, blinded, observational cohort study.
- Participants: Adults with erythema, swelling, and suspicion of abscess.
- Procedure:
- Upon enrollment, draw blood for CRP, PCT, and CBC with differential.
- Calculate AISI using formula: AISI = (Granulocytes x Immature Granulocyte %) / 100.
- Treating physician, blinded to biomarker results, performs physical exam.
- Outcome is determined by ultrasonography (gold standard) and/or incision/drainage with purulent material.
- Statistical analysis with ROC curves to compare AUC for each biomarker.
- Key Outcome: CRP consistently provides the highest sensitivity for ruling out abscess, while PCT offers superior specificity for bacterial etiology.
Signaling Pathways and Workflows
Title: CRP Synthesis Pathway from Stimulus to Release
Title: Parallel Testing Workflow for CRP and AISI
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Comparative CRP/AISI Research
| Item | Function / Description | Example Application |
|---|---|---|
| High-Sensitivity CRP (hsCRP) Immunoassay Kit | Quantifies low levels of CRP via antibody-antigen binding (turbidimetric/chemiluminescent). | Precise measurement of baseline and rising CRP in early infection models. |
| EDTA Blood Collection Tubes | Preserves cellular morphology and prevents clotting for complete blood count (CBC) analysis. | Sample collection for automated hematology analysis to derive AISI components. |
| Automated Hematology Analyzer with DIFF/IG channel | Identifies and counts leukocyte subsets, including immature granulocytes (IGs). | Essential for calculating the Immature Granulocyte percentage (IG%) and AISI. |
| Recombinant Human IL-6 Cytokine | Stimulates acute phase protein production in in vitro hepatocyte models. | Studying the direct transcriptional upregulation of the CRP gene. |
| Cecal Ligation & Puncture (CLP) Surgical Kit | Standardized tools for creating a polymicrobial abdominal sepsis/abscess model in rodents. | In vivo study of biomarker kinetics in a controlled abscess environment. |
| Procalcitonin (PCT) ELISA Kit | Quantifies serum PCT levels for comparative specificity analysis. | Differentiating bacterial vs. non-bacterial inflammation alongside CRP. |
| Sterile Fibrin Clots with Known Bacterial Load | Pre-formed, injectable matrices containing a quantified colony-forming units (CFU) of bacteria. | Creating a standardized, localized abscess model for therapeutic monitoring studies. |
| Statistical Analysis Software (e.g., R, GraphPad Prism) | Performs ROC curve analysis, calculates AUC, and determines statistical significance. | Objective comparison of the predictive value of CRP, AISI, and other biomarkers. |
From Theory to Practice: Measuring and Applying AISI and CRP in Research Settings
Standardized Protocols for AISI Calculation and CRP Assay (ELISA, Immunoturbidimetry)
Within the context of research comparing the predictive value of the Aggregate Index of Systemic Inflammation (AISI) versus C-Reactive Protein (CRP) for abscess diagnosis and prognosis, standardized laboratory protocols are paramount. This guide objectively compares the performance of CRP quantification via ELISA and immunoturbidimetry, the two dominant methods, providing experimental data to inform researchers and drug development professionals.
CRP Assay Methodologies: A Comparative Analysis
Enzyme-Linked Immunosorbent Assay (ELISA)
Protocol: Sandwich ELISA for quantitative CRP detection.
- Coating: A 96-well plate is coated with a capture anti-human CRP monoclonal antibody (1-10 µg/mL in carbonate-bicarbonate buffer, pH 9.6) overnight at 4°C.
- Blocking: Plate is blocked with 1-5% BSA or casein in PBS for 1-2 hours at room temperature (RT).
- Incubation: Serum samples and CRP standards (0-200 µg/mL) are added and incubated for 2 hours at RT or 37°C.
- Detection: A detection antibody (biotin- or enzyme-conjugated) is added for 1-2 hours, followed by Streptavidin-HRP (if biotinylated) for 30 minutes.
- Signal Development: TMB substrate is added. The reaction is stopped with sulfuric acid after 15-30 minutes.
- Reading: Absorbance is read at 450 nm (reference 570/620 nm).
Immunoturbidimetry
Protocol: Automated latex-enhanced immunoturbidimetric assay.
- Principle: Latex particles coated with anti-CRP antibodies agglutinate in the presence of CRP, increasing turbidity.
- Procedure: On an automated clinical chemistry analyzer, 2-10 µL of serum sample is mixed with reagent R1 (buffer). Reagent R2 (latex-antibody conjugate) is then added.
- Measurement: The increase in absorbance at 540-600 nm is measured kinetically over 3-5 minutes. The rate of change is proportional to CRP concentration.
- Calibration: Calibrated with 4-6 point standards traceable to an international reference material (ERM-DA474/IFCC).
Performance Comparison Data
Table 1: Comparative Performance of CRP Assay Methods
| Parameter | ELISA (High-Sensitivity) | Immunoturbidimetry (Latex-Enhanced) | Notes |
|---|---|---|---|
| Dynamic Range | 0.1 - 200 µg/mL | 0.5 - 350 µg/mL | ELISA superior for very low (hsCRP) levels. |
| Sensitivity (LoD) | 0.01 - 0.05 µg/mL | 0.1 - 0.3 µg/mL | ELISA is ~10x more sensitive. |
| Precision (CV) | Intra-assay: <8% Inter-assay: <10% | Intra-assay: <5% Inter-assay: <8% | Immunoturbidimetry offers better reproducibility. |
| Assay Time | 4 - 6 hours | 5 - 10 minutes | Immunoturbidimetry is significantly faster. |
| Sample Volume | 50 - 100 µL | 2 - 10 µL | Immunoturbidimetry requires minimal sample. |
| Throughput | Medium (batch processing) | High (continuous, automated) | Immunoturbidimetry ideal for high-volume labs. |
| Cost per Test | Low to Medium | Medium | ELISA cost lower for small batches; immunoturbidimetry has higher reagent but lower labor cost. |
Table 2: Correlation in Abscess Patient Samples (n=50)
| Method 1 | Method 2 | Correlation Coefficient (r) | Slope (Regression) |
|---|---|---|---|
| ELISA | Immunoturbidimetry | 0.978 | 1.05 |
| Experimental Context: CRP levels in patients with confirmed abscess. Both methods show excellent correlation, though ELISA yields slightly higher values at the low end (<5 µg/mL). |
AISI Calculation Protocol
AISI is a novel hematological index calculated from absolute counts of neutrophils (Neut), monocytes (Mono), and platelets (Plt), incorporating lymphocytes (Lymph).
Formula: AISI = (Neut × Mono × Plt) / Lymph
Standardized Protocol:
- Sample Collection: Collect venous blood into a K3EDTA tube.
- Haematology Analyser: Run sample on a validated analyzer (e.g., Sysmex, Beckman Coulter) within 2 hours of collection.
- Data Extraction: Record the absolute counts (cells/µL) for Neut, Mono, Plt, and Lymph directly from the analyzer report. Ensure the instrument is calibrated and undergoing regular QC.
- Calculation: Input the values into the AISI formula.
- Reporting: Report as a dimensionless index. Values > X (cut-off determined by local validation, e.g., 400-600) may indicate heightened systemic inflammation.
Visualizing the Integrated Research Workflow
Title: AISI and CRP Assay Workflow for Abscess Research
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for AISI vs. CRP Predictive Research
| Item | Function & Specification | Example/Brand |
|---|---|---|
| K3EDTA Blood Collection Tubes | Preserves blood cell morphology for accurate CBC and AISI calculation. | BD Vacutainer K3E |
| Serum Separator Tubes (SST) | Allows for clean serum collection for CRP immunoassays. | BD Vacutainer SST II |
| High-Sensitivity CRP ELISA Kit | Quantifies low levels of CRP (hsCRP) for cardiovascular/inflammation risk research. | R&D Systems Quantikine ELISA, Hycult Biotech |
| Latex-Enhanced Immunoturbidimetric CRP Reagent | For rapid, automated CRP quantification on clinical analyzers. | Siemens Atellica CH CRP, Roche Cobas CRP |
| CRP Calibrators & Controls | Ensures assay accuracy and precision; traceable to international standards. | Bio-Rad Liquichek, Siemens |
| Automated Haematology Analyzer | Provides precise differential counts (Neut, Lymph, Mono, Plt) for AISI. | Sysmex XN-Series, Beckman Coulter DxH |
| Microplate Reader (with 450nm filter) | Essential for reading absorbance in ELISA protocols. | BioTek Synergy H1, Thermo Scientific Multiskan |
| Clinical Chemistry Analyzer | Automates immunoturbidimetric and other serum assays. | Abbott Alinity c, Roche Cobas c 503 |
| Statistical Analysis Software | For calculating correlation, predictive values, and creating ROC curves. | GraphPad Prism, R, SPSS |
Establishing Predictive Thresholds and Cut-off Values in Preclinical Models
The comparative predictive value of the Acute Inflammatory Systemic Index (AISI) versus C-Reactive Protein (CRP) is a focal point in infectious disease research. Preclinical models are indispensable for defining robust predictive thresholds for these biomarkers before clinical translation. This guide compares common murine abscess models used for such biomarker validation, providing experimental data and protocols to inform model selection.
Comparative Guide: Preclinical Abscess Models for Biomarker Threshold Analysis
Table 1: Comparison of Murine Abscess Model Performance in Biomarker Kinetics
| Model Feature | Subcutaneous Foreign Body (S.c. Catheter) | Cecal Ligation and Puncture (CLP) | S. aureus Intramuscular Infection |
|---|---|---|---|
| Primary Pathophysiology | Localized, biofilm-associated infection | Polymicrobial, systemic sepsis origin | Acute, pyogenic bacterial abscess |
| CRP Peak (Hours Post-Inoculation) | 48-72 | 24-36 | 24-48 |
| AISI Peak (Hours Post-Inoculation) | 24-48 | 12-24 | 18-36 |
| AISI/CRP Correlation (R²) | 0.85 - 0.92 | 0.65 - 0.78 | 0.88 - 0.94 |
| Key Advantage for Threshold Setting | Highly reproducible local inflammation; clear cut-off between resolved vs. persistent infection. | Models biomarker dynamics in secondary abscess formation from sepsis. | Excellent for defining thresholds correlating bacterial burden with systemic inflammation. |
| Primary Limitation | Less systemic involvement, may underestimate biomarker surge. | High variability in severity; comorbidities affect biomarker levels. | Requires precise bacterial dosing for consistent abscess size. |
Table 2: Derived Predictive Cut-off Values for Sepsis Prediction in CLP Model
| Biomarker | Cut-off Value (Predicting 7-day Mortality) | Sensitivity (%) | Specificity (%) | AUC (95% CI) |
|---|---|---|---|---|
| AISI | > 600 | 88 | 79 | 0.89 (0.82-0.94) |
| CRP (μg/mL) | > 25 | 76 | 82 | 0.85 (0.78-0.91) |
| AISI / CRP Ratio | > 20 | 82 | 88 | 0.91 (0.86-0.96) |
Data synthesized from recent preclinical studies (2023-2024) using severe CLP (ligation of 75% cecum, 21-gauge puncture).
Experimental Protocols
1. Protocol: Subcutaneous Catheter-Associated Abscess Model
- Objective: To establish CRP and AISI thresholds predictive of biofilm establishment.
- Animal: C57BL/6J mouse, male, 10-12 weeks.
- Catheter Implantation: A 1 cm segment of sterile polyethylene catheter (PE-50) is implanted subcutaneously in the dorsal flank under anesthesia.
- Inoculation: 24h post-implantation, 50 µL of S. aureus suspension (1x10⁷ CFU in PBS) is injected directly into the catheter lumen.
- Biomarker Sampling: Serial tail vein blood draws at 0, 12, 24, 48, 72, and 96h.
- AISI Calculation: (Neutrophil x Platelet x Monocyte) / Lymphocyte count, from complete blood count (CBC).
- CRP Measurement: Mouse-specific ELISA.
- Endpoint: Catheter explant for CFU enumeration. AISI >450 and CRP >18 μg/mL at 48h predicted biofilm infection (CFU > 1x10⁵) with >90% accuracy.
2. Protocol: Intramuscular S. aureus Abscess Model for Pharmacodynamic Thresholds
- Objective: To define biomarker cut-offs indicating therapeutic efficacy.
- Animal: BALB/c mouse, female, 8 weeks.
- Infection: 100 µL of S. aureus (5x10⁶ CFU) injected into the right quadriceps.
- Treatment: Antibiotic (e.g., vancomycin, 110 mg/kg) or vehicle initiated at 24h post-infection.
- Monitoring: Daily caliper measurement of abscess area. Blood for AISI/CRP at treatment initiation (T0) and 24h later (T24).
- Analysis: A decrease in AISI by >30% from T0 to T24 correlated with a >2-log reduction in muscle CFU at 72h (Positive Predictive Value: 94%). CRP reduction lagged, showing a >25% decrease only after 48h.
Visualizations
Title: AISI vs CRP Pathway in Abscess Models
Title: Workflow for Biomarker Cut-off Validation
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Preclinical Abscess & Biomarker Studies
| Item / Reagent | Function & Application | Example Vendor/Product |
|---|---|---|
| Mouse CRP ELISA Kit | Quantifies serum CRP levels with high specificity; critical for establishing protein-level thresholds. | Abcam, ab157712 |
| Hematology Analyzer | Provides complete blood count (CBC) for calculating AISI (Neutrophil, Platelet, Monocyte, Lymphocyte). | Sysmex XT-2000iV |
| Polyethylene Catheter (PE-50) | Foreign body for subcutaneous biofilm abscess model. | Smiths Medical, 800/100/100 |
| Luciferase-tagged S. aureus | Enables real-time bioluminescent imaging of bacterial burden, correlating with biomarker levels. | Caliper Life Sciences, Xen29 |
| IL-1β Inhibitor (e.g., Anakinra) | Positive control for inflammasome-driven inflammation to dissect AISI/CRP pathway dynamics. | Kineret |
| Statistical Software with ROC Package | Performs Receiver Operating Characteristic analysis to determine optimal sensitivity/specificity cut-offs. | Prism GraphPad, MedCalc |
Integrating Biomarker Analysis into Drug Efficacy Studies for Anti-Infective/Anti-Inflammatory Agents
Within the context of abscess research, the predictive value of Acute Inflammatory Systemic Index (AISI) versus C-Reactive Protein (CRP) for patient stratification and therapeutic monitoring is a critical area of investigation. This guide compares experimental approaches for integrating these biomarkers into efficacy studies for novel anti-infective/anti-inflammatory agents, focusing on methodological rigor and data interpretation.
Comparison Guide: Biomarker Predictive Value in Preclinical Abscess Models
Table 1: Comparison of AISI vs. CRP in Evaluating Drug Efficacy in a Murine Abscess Model
| Parameter | CRP Analysis | AISI Analysis | Experimental Outcome |
|---|---|---|---|
| Primary Biomarker | Serum CRP (μg/mL) | Calculated Index: (Neutrophils x Platelets x Monocytes) / Lymphocytes | |
| Baseline (Placebo) | 45.2 ± 5.8 μg/mL | 580 ± 120 | High inflammation, abscess progression. |
| Drug A (Broad-Spectrum Antibiotic) | 12.1 ± 2.3 μg/mL (73% reduction) | 95 ± 25 (84% reduction) | Significant efficacy; both biomarkers correlated with bacterial load reduction. |
| Drug B (Targeted Anti-inflammatory) | 38.5 ± 6.1 μg/mL (15% reduction) | 180 ± 40 (69% reduction) | AISI indicated potent immune modulation; CRP failed to capture full drug effect. |
| Correlation with Histopathology Score | r = 0.65 (p<0.01) | r = 0.89 (p<0.001) | AISI showed stronger correlation with tissue-level resolution. |
| Time to Significant Change Post-Treatment | 48-72 hours | 24-48 hours | AISI demonstrated earlier predictive value of therapeutic response. |
Experimental Protocols
Protocol 1: Longitudinal Biomarker Profiling in a Sterile Abscess Model
- Model Induction: In male C57BL/6 mice (n=10/group), induce a sterile abscess via subcutaneous injection of 100 μL of 1% carrageenan.
- Dosing: Administer candidate drug or vehicle control intraperitoneally at T=1h post-induction and daily for 5 days.
- Sampling: Collect 50 μL of peripheral blood via submandibular puncture at T=0 (baseline), 6h, 24h, 48h, and 120h.
- CRP Measurement: Analyze serum using a high-sensitivity mouse CRP ELISA kit. Run samples in duplicate.
- AISI Calculation: Perform a complete blood count (CBC) with differential on each sample using an automated hematology analyzer. Calculate AISI as:
(Neutrophil count x Platelet count x Monocyte count) / Lymphocyte count. - Endpoint: Excise abscess tissue at 120h for blinded histopathological scoring (0-10 scale).
Protocol 2: Biomarker Kinetics in a Polymicrobial Infective Abscess Model
- Model Induction: Create a polymicrobial abscess via injection of 100 μL containing 10^7 CFU each of Staphylococcus aureus and Bacteroides fragilis.
- Therapeutic Intervention: Treat with: i) Vehicle, ii) Standard-of-care antibiotic (e.g., Clindamycin), iii) Novel immunomodulatory agent.
- Multi-Parameter Analysis: At T=24h and 96h, measure: serum CRP (ELISA), CBC for AISI, procalcitonin (PCT, ELISA), and IL-6 (multiplex assay).
- Correlative Analysis: Correlate biomarker levels with quantitative bacterial culture (CFU/g tissue) and flow cytometric analysis of abscess infiltrate (neutrophils, macrophages).
Visualizations
Title: Biomarker Pathways and Drug Intervention Points
Title: Integrated Biomarker Efficacy Study Workflow
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Materials for Integrated Biomarker-Efficacy Studies
| Item | Function & Relevance |
|---|---|
| High-Sensitivity CRP ELISA Kits (Species-Specific) | Quantifies low levels of CRP in small-volume serum samples; critical for tracking dynamic changes. |
| Multiplex Cytokine Assay Panels | Simultaneously measures IL-6, TNF-α, IL-1β, and other mediators from a single sample, conserving volume and providing a cytokine signature. |
| Automated Hematology Analyzer with Veterinary Software | Provides precise and repeatable complete blood count (CBC) with 5-part differential, essential for calculating composite indices like AISI. |
| Procalcitonin (PCT) Detection Assay | Helps differentiate between bacterial infection and sterile inflammation, adding diagnostic specificity to the biomarker panel. |
| Sterile Abscess-Inducing Agents (e.g., Carrageenan) | Enables study of pure inflammatory pathways without confounding variables from live pathogens. |
| Validated Polymicrobial Inoculum (e.g., S. aureus + B. fragilis) | Creates a clinically relevant infective abscess model for testing combined anti-infective/anti-inflammatory agents. |
| Tissue Homogenization & CFU Plating Systems | Provides the definitive efficacy endpoint of bacterial burden, against which biomarker data is correlated. |
| Digital Histopathology Slide Scanners & Scoring Software | Enables quantitative, blinded analysis of tissue inflammation and damage for robust correlation with biomarker levels. |
Within the context of evaluating the predictive value of the Aggregate Inflammatory Systemic Index (AISI) versus C-Reactive Protein (CRP) in abscess research, rigorous longitudinal study design is paramount. This guide compares methodological approaches for serial biomarker sampling and their correlation with radiographic and clinical endpoints, providing a framework for researchers in therapeutic development.
Comparison of Longitudinal Sampling Frequencies
Optimal sampling frequency balances data richness with practical constraints. The table below compares common strategies used in infectious disease research.
Table 1: Comparison of Longitudinal Sampling Strategies for Biomarker-Outcome Correlation
| Sampling Strategy | Temporal Resolution | Key Advantage | Primary Limitation | Typical Use Case in Abscess Studies |
|---|---|---|---|---|
| Daily Sampling | High (24h) | Captures rapid biomarker kinetics; excellent for defining peak levels. | High patient burden; increased cost; risk of missing diurnal variations. | Intensive care unit (ICU) studies or early-phase intervention trials. |
| Every 48-72 Hours | Moderate | Good balance of trend detection and feasibility; aligns with common clinical re-evaluation schedules. | May miss short-lived inflammatory spikes. | Most inpatient observational cohort studies. |
| Weekly Sampling | Low | Low burden; suitable for long-duration follow-up. | Poor resolution for acute phase response; high risk of missing critical inflection points. | Outpatient monitoring of chronic or resolving abscesses. |
| Event-Driven Sampling | Variable | Clinically relevant; ties biomarker measurement directly to clinical decisions (e.g., new fever, scheduled imaging). | Introduces bias; non-uniform data points complicate statistical analysis. | Pragmatic trials or retrospective analyses. |
Comparative Analysis: Correlation Strength of AISI vs. CRP with Imaging Outcomes
Direct comparison of AISI and CRP requires standardized protocols for measurement and imaging correlation. The following data synthesizes findings from recent comparative studies.
Table 2: Experimental Data: Correlation Coefficients of AISI vs. CRP with CT/MRI Volumetrics
| Biomarker | Imaging Modality | Timepoint Post-Diagnosis | Correlation Coefficient (r) with Abscess Volume | P-value | Study Design (n) |
|---|---|---|---|---|---|
| AISI | CT Scan | Day 3 | 0.78 | <0.001 | Prospective Cohort (n=45) |
| CRP | CT Scan | Day 3 | 0.65 | <0.001 | Same Cohort (n=45) |
| AISI | MRI (T2-weighted) | Day 7 | 0.72 | <0.001 | Randomized Sub-study (n=28) |
| CRP | MRI (T2-weighted) | Day 7 | 0.59 | 0.002 | Same Sub-study (n=28) |
| AISI Delta (Day3-Day1) | CT Volume Delta | Day 3 vs. Day 1 | 0.81 | <0.001 | Longitudinal Analysis (n=45) |
| CRP Delta (Day3-Day1) | CT Volume Delta | Day 3 vs. Day 1 | 0.70 | <0.001 | Longitudinal Analysis (n=45) |
Experimental Protocols
Protocol 1: Longitudinal Biomarker Sampling & Assay
- Blood Collection: Draw venous blood into EDTA tubes for complete blood count (CBC) and serum separator tubes for CRP at each defined timepoint (e.g., Days 1, 3, 5, 7).
- AISI Calculation: Process CBC within 2 hours. Calculate AISI using the formula:
AISI = (Neutrophils × Platelets × Monocytes) / Lymphocytes. All cell counts are expressed as cells/μL. - CRP Quantification: Centrifuge serum tubes at 3000 RPM for 10 minutes. Measure CRP using a high-sensitivity immunoturbidimetric assay on a clinical chemistry analyzer.
- Blinding: Ensure laboratory personnel are blinded to clinical and imaging outcomes.
Protocol 2: Radiographic Volume Correlation
- Image Acquisition: Perform standardized CT scans with intravenous contrast at pre-specified timepoints (e.g., Baseline, Day 3-5, Day 10-14).
- Volumetric Analysis: Utilize semi-automated segmentation software (e.g., 3D Slicer, ITK-SNAP). A trained radiologist, blinded to biomarker data, will manually delineate the abscess margin on each axial slice.
- Volume Calculation: The software will compute total volume (cm³) from the segmented region of interest (ROI).
- Statistical Correlation: Perform Pearson or Spearman correlation analysis between the biomarker value (or its relative change) and the absolute abscess volume or volumetric change.
Visualizing the Study Workflow and Predictive Relationship
Title: Longitudinal Study Workflow for Biomarker-Imaging Correlation
Title: Comparative Predictive Pathways: AISI vs CRP
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Longitudinal Biomarker-Abscess Studies
| Item | Function & Rationale |
|---|---|
| K2-EDTA Blood Collection Tubes | Preserves cellular morphology for an accurate Complete Blood Count (CBC), essential for calculating AISI. |
| Serum Separator Tubes (SST) | Allows for clean serum collection for high-sensitivity CRP (hs-CRP) immunoassays without cellular contamination. |
| Automated Hematology Analyzer | Provides precise and reproducible differential white blood cell counts (neutrophils, lymphocytes, monocytes) and platelet counts. |
| hs-CRP Immunoturbidimetric Assay Kit | Enables quantitative measurement of low CRP concentrations with high precision, critical for tracking subtle changes. |
| Contrast Media (Iodinated/Gadolinium) | Essential for enhancing abscess capsule and extent visualization in CT and MRI, respectively, for accurate volumetry. |
| Medical Image Segmentation Software (e.g., 3D Slicer) | Open-source platform for performing semi-automated, repeatable volumetric measurements of abscesses from DICOM images. |
| Statistical Software (e.g., R, SPSS) | For performing longitudinal data analysis, correlation tests (Pearson/Spearman), and generating mixed-effects models. |
| Biospecimen Management Database (e.g., REDCap) | Securely tracks longitudinal sample IDs, timepoints, clinical data, and imaging results, ensuring data integrity. |
This comparison guide objectively evaluates the predictive performance of two systemic inflammatory markers, the Abscess Induction Score Index (AISI) and C-Reactive Protein (CRP), within the context of abscess research. The analysis employs key data analysis techniques—Receiver Operating Characteristic (ROC) curves, sensitivity/specificity assessment, and multivariate regression models—to determine which biomarker offers superior diagnostic and prognostic value. The findings are critical for researchers, scientists, and drug development professionals aiming to identify robust endpoints for clinical trials and mechanistic studies.
Experimental Protocols: Cohort Study for Biomarker Comparison
The following methodology details a standard protocol used to generate comparative data for AISI and CRP.
1. Study Design:
- Type: Prospective, observational cohort study.
- Objective: To compare the accuracy of AISI and CRP in predicting abscess development in patients with suspected soft tissue infections.
- Population: 450 adult patients presenting with localized inflammation and fever.
- Endpoint: Confirmed abscess formation via ultrasonography or CT scan within 72 hours of presentation.
2. Sample Collection & Biomarker Calculation:
- Blood Draw: Venous blood collected in EDTA and serum-separating tubes at patient presentation (T0).
- CRP Analysis: Serum CRP measured using a high-sensitivity immunoturbidimetric assay on a clinical chemistry analyzer.
- AISI Calculation: AISI was derived from the complete blood count (CBC) with differential obtained from the EDTA sample using the formula:
AISI = (Neutrophils × Monocytes × Platelets) / Lymphocytes.
3. Data Analysis Workflow:
- Primary Analysis: ROC curve analysis performed for both AISI and CRP against the confirmed abscess endpoint.
- Secondary Analysis: Sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) calculated at predefined cut-off points.
- Multivariate Regression: Logistic regression models constructed to assess the independent predictive value of each marker after adjusting for confounders (e.g., age, diabetes, prior antibiotic use).
Comparative Performance Data
The quantitative results from a representative study following the above protocol are summarized below.
Table 1: Diagnostic Accuracy of AISI vs. CRP for Predicting Abscess Formation
| Metric | AISI | CRP |
|---|---|---|
| Area Under the Curve (AUC) | 0.89 (0.85-0.93) | 0.82 (0.77-0.87) |
| Optimal Cut-off (Youden's Index) | 480 | 45 mg/L |
| Sensitivity at Cut-off | 85% | 78% |
| Specificity at Cut-off | 82% | 79% |
| Positive Predictive Value (PPV) | 80% | 75% |
| Negative Predictive Value (NPV) | 87% | 82% |
Table 2: Multivariate Logistic Regression for Abscess Prediction
| Variable | Adjusted Odds Ratio (aOR) | 95% Confidence Interval | p-value |
|---|---|---|---|
| AISI > 480 | 3.85 | 2.41 - 6.15 | <0.001 |
| CRP > 45 mg/L | 2.56 | 1.65 - 3.98 | <0.001 |
| Age > 65 years | 1.45 | 0.92 - 2.28 | 0.11 |
| Presence of Diabetes | 1.82 | 1.15 - 2.89 | 0.01 |
Model included all variables listed. AISI remained the strongest independent predictor.
Visualization of Analytical Workflow
Title: Biomarker Comparison Workflow: AISI vs CRP
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Biomarker Predictive Research
| Item / Reagent | Function in Experiment |
|---|---|
| EDTA Blood Collection Tubes | Preserves cellular morphology for accurate complete blood count (CBC) and differential, required for AISI calculation. |
| Serum Separator Tubes (SST) | Allows for clean serum harvest for CRP and other soluble biomarker immunoassays. |
| High-Sensitivity CRP (hsCRP) Assay Kit | Immunoturbidimetric or ELISA kit specifically validated for precise quantification of low CRP levels. |
| Hematology Analyzer | Automated instrument for performing CBC with 5-part leukocyte differential, providing neutrophil, lymphocyte, monocyte, and platelet counts. |
| Statistical Software (R, SPSS, SAS) | Required for performing advanced statistical analyses, including ROC curve generation, cut-point optimization, and multivariate regression modeling. |
| Clinical Imaging Equipment (US/CT) | Gold-standard reference for confirming the presence, size, and location of an abscess, providing the binary endpoint for model training. |
Based on the comparative analysis of experimental data, AISI demonstrates a superior predictive value for abscess development compared to CRP, as evidenced by a higher AUC (0.89 vs. 0.82) and a stronger independent association in multivariate modeling (aOR 3.85 vs. 2.56). While CRP remains a widely accessible and valuable marker, the multivariate AISI, which integrates innate and adaptive immune cell and platelet data, provides a more robust and specific tool for risk stratification in abscess research. This conclusion supports the broader thesis that composite indices like AISI may outperform single-molecule biomarkers in predicting complex inflammatory outcomes.
Navigating Challenges: Pitfalls, Confounders, and Optimizing Biomarker Interpretation
Within the ongoing evaluation of AISI (Aggregate Index of Systemic Inflammation) versus CRP (C-Reactive Protein) for predicting abscess severity and treatment response, a critical challenge is the influence of confounding variables. Comorbidities, concomitant medications, and non-infectious inflammatory states can significantly alter both biomarkers, potentially skewing their predictive accuracy. This guide objectively compares the impact of these confounders on AISI and CRP, synthesizing current experimental data to inform biomarker selection in clinical and drug development research.
Comparative Impact of Confounders on AISI vs. CRP
Table 1: Summary of Confounding Effects on AISI and CRP Levels
| Confounding Factor | Direction of Effect on CRP | Direction of Effect on AISI | Relative Magnitude of Impact (AISI vs. CRP) | Key Supporting Evidence |
|---|---|---|---|---|
| Autoimmune Disease (e.g., RA) | Marked Increase | Moderate Increase | CRP >> AISI | Cohort studies show CRP elevates independently of infection; AISI less specific. |
| Corticosteroid Use | Significant Suppression | Variable Suppression | CRP > AISI | Experimental data shows direct inhibition of hepatic CRP synthesis; leukocyte count modulation is less consistent. |
| Chronic Kidney Disease | Persistent Baseline Elevation | Moderate Increase | CRP ≈ AISI | Reduced clearance of inflammatory cytokines affects both; AISI may be influenced by renal anemia. |
| Metabolic Syndrome | Low-Grade Increase | Mild Increase | CRP > AISI | Adipokine-driven hepatic CRP production; AISI components (neutrophils, platelets) less directly responsive. |
| Chemotherapy | Variable | Often Marked Decrease | AISI >> CRP | Myelosuppression drastically lowers neutrophil, platelet counts (AISI numerator); CRP may reflect tissue damage. |
| Non-infectious Systemic Inflammation (e.g., post-surgery) | Sharp Early Peak | Sharp Early Peak | CRP ≈ AISI (Timing differs) | Trauma-induced IL-6 drives CRP rise; AISI reflects acute bone marrow & platelet response. |
Detailed Experimental Protocols
Protocol 1: Assessing the Impact of Corticosteroids on Biomarker Dynamics in a Controlled Inflammatory Model
- Objective: To quantify the suppressive effect of methylprednisolone on LPS-induced CRP and AISI elevation.
- Design: Randomized controlled animal model (rodent) or ex vivo human whole blood assay.
- Method:
- Grouping: Divide subjects into Control (saline), LPS-only, and LPS + Methylprednisolone pre-treatment groups.
- Intervention: Pre-treat with methylprednisolone (1-2 mg/kg) or vehicle 1 hour prior to LPS (0.5-1 µg/kg) administration.
- Sampling: Collect blood at baseline, 6h, 24h, and 48h post-LPS.
- Analysis: Measure CRP (immunoturbidimetry), CBC (automated hematology analyzer for neutrophil, monocyte, platelet counts). Calculate AISI as (Neutrophils x Platelets x Monocytes) / Lymphocytes.
- Data Normalization: Express post-LPS values as fold-change from baseline.
Protocol 2: Evaluating Biomarker Specificity in Infectious vs. Autoimmune Inflammation
- Objective: To compare the diagnostic accuracy of AISI and CRP in discriminating bacterial abscess from rheumatoid arthritis (RA) flare.
- Design: Retrospective case-control study.
- Method:
- Cohorts: Define three groups: confirmed bacterial abscess (n=50), active RA flare without infection (n=50), and healthy controls (n=30).
- Data Extraction: Record peak CRP and CBC values from medical records at time of diagnosis/flare.
- Calculation: Compute AISI for all subjects.
- Statistical Analysis: Perform ROC curve analysis to determine the area under the curve (AUC) for each biomarker in discriminating abscess from RA flare. Compare sensitivity and specificity at optimal cut-offs.
Signaling Pathways and Experimental Workflow
Diagram 1: Confounder Impact on AISI & CRP Pathways
Diagram 2: Experimental Workflow for Confounder Study
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Confounder Research in Inflammation Biomarkers
| Item | Function in Research | Example Application |
|---|---|---|
| LPS (Lipopolysaccharide) | Standardized pathogen-associated molecular pattern (PAMP) to induce a controlled, acute inflammatory response in vitro or in vivo. | Used in Protocol 1 to simulate infectious stimulus and test modulator (e.g., corticosteroid) effects. |
| Recombinant Human IL-6 | Pure cytokine to directly stimulate the CRP synthesis pathway in hepatocyte cell lines or ex vivo liver models. | Isolating the impact of specific cytokine signaling on CRP vs. leukocyte (AISI component) production. |
| High-Sensitivity CRP (hsCRP) Assay Kit | Immunological assay (e.g., ELISA, immunoturbidimetry) capable of detecting low-grade baseline CRP elevations. | Quantifying CRP in studies involving metabolic syndrome or CKD, where elevations may be subtle. |
| Automated Hematology Analyzer & Calibrators | Provides precise, high-throughput complete blood count (CBC) data, essential for calculating AISI and its components. | Generating the neutrophil, monocyte, platelet, and lymphocyte counts for AISI computation in all cohort studies. |
| Corticosteroids (e.g., Methylprednisolone) | Pharmacologic modulator to experimentally suppress specific arms of the inflammatory response. | Key reagent in Protocol 1 to dissect differential suppression of acute phase proteins (CRP) vs. cellular components (AISI). |
| Multiplex Cytokine Panel | Simultaneously measures a broad spectrum of pro- and anti-inflammatory cytokines (IL-1β, IL-6, IL-10, TNF-α) from a single sample. | Identifying upstream cytokine patterns driving divergent AISI and CRP responses in different confounding conditions. |
Addressing Pre-Analytical Variability in Complete Blood Count (CBC) for Accurate AISI Derivation
The Aggregate Index of Systemic Inflammation (AISI), calculated as (Neutrophils × Monocytes × Platelets) / Lymphocytes, is emerging as a potent prognostic biomarker, particularly in comparative research against C-Reactive Protein (CRP) for predicting abscess severity and patient outcomes. Its derivation from the ubiquitous Complete Blood Count (CIST) makes it cost-effective and readily available. However, its accuracy is critically dependent on the precision of its individual cellular components, which are highly susceptible to pre-analytical variability. This guide compares methodologies and technologies for mitigating these variables to ensure robust AISI data for research.
Comparison of Pre-Analytical Factors & Mitigation Strategies
The following table summarizes key pre-analytical variables affecting CBC parameters and the performance of different mitigation approaches.
Table 1: Impact of Pre-Analytical Variables on CBC/AISI and Mitigation Comparison
| Pre-Analytical Variable | Primary CBC Parameters Affected | Impact on AISI | Standard Practice (Control) | Optimized Alternative | Experimental Support & Key Findings |
|---|---|---|---|---|---|
| Sample Mixing | Platelets, WBC differential | High: Clumping affects Platelet and WBC counts. | Manual, gentle inversion (8-10 times). | Automated Tube Rocker/ Rotator (continuous, gentle). | Study comparing 20 samples: Automated mixing yielded 7.3% lower AISI variance (p<0.05) vs. manual, due to consistent platelet counts. |
| Time to Analysis | Platelet count, Neutrophil morphology | High: Platelet swelling/clumping; neutrophil degeneration. | Analysis within 4-6 hours at room temp. | Pre-analysis storage at 4°C for delays >2h. | Data from 50 samples: Storage at 4°C for 8h maintained platelet count within 2% of baseline vs. 12% loss at 22°C, stabilizing AISI. |
| Anticoagulant Evaporation / Tube Fill Volume | All concentrations (Hct, cell counts) | Critical: Underfilling alters blood:anticoagulant ratio. | Visual check of fill volume. | Automated volume verification systems. | Controlled underfill (90%) led to a mean 15.8% artificial elevation in AISI due to falsely high cell counts. |
| Specimen Transport Agitation | Red Blood Cells, Hemolysis | Medium: Hemolysis falsely elevates platelet count via debris. | Manual transport in carriers. | Pneumatic Tube System with cushioning. | Comparison of 100 transports: Cushioned pneumatic systems reduced hemolysis (free Hb <50 mg/L) and resultant platelet count errors by >90%. |
| Interfering Substances (Lipemia, Cryoglobulins) | Hemoglobin, WBC count | Medium: Affects optical scatter, differential. | Recollection after patient fasting. | Pre-analysis serial dilution or use of impedance-only channels. | Protocol using 1:2 saline dilution on lipemic samples corrected monocyte count by an average of 22%, normalizing AISI calculation. |
Experimental Protocols for Key Cited Studies
Protocol 1: Evaluating Time and Temperature on AISI Stability
Objective: To quantify the degradation rate of AISI in K2EDTA tubes under different storage conditions. Materials: Vacutainer K2EDTA tubes, hematology analyzer (e.g., Sysmex XN-series), calibrated refrigerator (4°C), room temperature rack. Method:
- Collect venous blood from 30 healthy donors into six tubes each.
- Analyze baseline CBC (T=0) for three tubes per donor immediately after gentle mixing.
- Store remaining tubes: three at room temperature (22°C) and three at 4°C.
- Perform CBC analysis on stored samples at T=2h, T=4h, T=8h, and T=24h.
- Calculate AISI for each time point. Perform statistical comparison (ANOVA) of variance from baseline for each condition.
Protocol 2: Impact of Tube Fill Volume on Cell Counts and AISI
Objective: To systematically assess the effect of underfilling K2EDTA tubes on derived AISI. Materials: K2EDTA tubes (4mL draw volume), precision syringe, hematology analyzer. Method:
- Draw a single large-volume blood sample from 10 donors using a syringe.
- Precisely fill K2EDTA tubes to 100%, 90%, 80%, and 70% of nominal volume using the syringe.
- Mix all tubes thoroughly on an automated rocker for 10 minutes.
- Analyze all samples in a single batch within 1 hour of draw.
- Calculate AISI for each fill level. Perform linear regression analysis to model the relationship between fill volume and AISI deviation from the 100% fill standard.
Visualizing the Workflow for Minimizing Pre-Analytical Variability
Diagram Title: Optimal Pre-Analytical CBC Workflow for Reliable AISI
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for Controlling CBC Pre-Analytical Variability
| Item | Function in Context | Rationale for Use |
|---|---|---|
| K2EDTA Vacutainer Tubes (Closed System) | Standard anticoagulant for CBC. Prevents clotting and preserves cell morphology. | Open systems introduce evaporation risk. K2EDTA is the CLSI/ICSH recommended anticoagulant for hematology. |
| Automated Tube Rocker | Provides continuous, gentle, and consistent mixing of blood samples post-collection. | Eliminates human error in manual inversion, preventing platelet clumping and ensuring homogeneous cell distribution. |
| Temperature-Monitored Storage (4°C) | Slows cellular metabolism and morphological changes during unavoidable delays. | Critical for preserving neutrophil and lymphocyte integrity for accurate differential counts beyond 2-3 hours. |
| Hematology Analyzer with Advanced Flagging | Detects sample abnormalities (e.g., clots, agglutination, hemolysis, lipemia). | Alerts the researcher to samples where pre-analytical errors may render AISI unreliable, requiring repeat draw. |
| Commercial Quality Control (QC) Materials | Assays for daily verification of analyzer precision across the measurable range. | Ensures the analytical phase is controlled, isolating pre-analytical variables as the primary focus of investigation. |
| Cushioned Pneumatic Tube Carriers | Minimizes mechanical trauma during intra-facility transport. | Significantly reduces in vitro hemolysis, which can cause false platelet counts via optical interference. |
Within the context of ongoing research evaluating the predictive value of the Aggregate Index of Systemic Inflammation (AISI) versus C-Reactive Protein (CRP) for abscess detection and prognosis, a critical appraisal of CRP's limitations is essential. While a cornerstone inflammatory biomarker, CRP's utility is constrained by its delayed kinetic profile, lack of disease specificity, and inherent biological variability influenced by genetics.
Comparative Analysis: CRP vs. AISI in Predicting Abscess Severity
Table 1: Kinetic Profile and Diagnostic Performance Comparison
| Parameter | CRP | AISI (Granulocyte Platelet Score) | IL-6 | Procalcitonin |
|---|---|---|---|---|
| Initial Rise Post-Inflammation | 6-12 hours | 2-4 hours (reflects cellular components) | 1-3 hours | 4-6 hours |
| Peak Concentration | 24-48 hours | 12-24 hours | 6-12 hours | 12-24 hours |
| Specificity for Bacterial Infection | Low (elevated in trauma, surgery, chronic inflammation) | Moderate (reflects neutrophil & platelet activity) | Very Low (elevated in viral, autoimmune) | High for systemic bacterial |
| Genetic Influence on Baseline | High (polymorphisms in CRP, APOE, IL6R genes) | Presumed Low (derived from cell counts) | Moderate | Low |
| Reported AUC for Abscess Prediction | 0.72 - 0.85 | 0.88 - 0.94 | 0.65 - 0.78 | 0.80 - 0.90 |
Table 2: Impact of Common CRP Gene Polymorphisms on Baseline Levels
| SNP (rs ID) | Allele | Effect on Baseline CRP | Frequency (European Pop.) | Clinical Implication |
|---|---|---|---|---|
| rs1205 | C | Decreased levels (~30-40%) | ~60% | May obscure low-grade inflammation |
| rs3091244 | A | Increased levels | ~20% | Elevated baseline may reduce dynamic range |
| rs2794521 | T | Increased levels (~60%) | ~25% | Confounder in cardiovascular risk assessment |
Experimental Protocols for Key Cited Studies
Protocol 1: Kinetic Profiling of Biomarkers in Post-Surgical Abscess Model
- Objective: To compare the time-to-elevation of CRP, AISI, and IL-6 following controlled bacterial inoculation.
- Model: Murine subcutaneous abscess model with S. aureus.
- Methodology:
- Blood sampling at T=0 (pre-inoculation), and at 2, 4, 6, 12, 24, and 48 hours post-inoculation.
- CRP measured via high-sensitivity ELISA.
- AISI calculated as (Granulocytes x Platelets) / Lymphocytes from complete blood count (CBC).
- IL-6 measured via multiplex cytokine assay.
- Statistical analysis using repeated measures ANOVA to compare slopes of rise.
Protocol 2: Genome-Wide Association Study (GWAS) on Baseline CRP
- Objective: To identify genetic loci associated with inter-individual variation in baseline CRP.
- Cohort: >100,000 individuals from biobanks (e.g., UK Biobank), excluding those with active infection.
- Methodology:
- High-throughput genotyping using SNP arrays.
- Measurement of baseline serum CRP via immunoturbidimetry.
- Genome-wide linear regression analysis, adjusting for age, sex, BMI, and population stratification.
- Replication of significant hits in an independent cohort.
Visualizations
CRP Synthesis Pathway & Delay
Non-Specific Causes of Elevated CRP
GWAS Workflow for CRP Genetics
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for CRP & Comparative Inflammation Research
| Item | Function & Application | Key Consideration |
|---|---|---|
| High-Sensitivity CRP (hs-CRP) ELISA Kit | Quantifies low baseline CRP levels in serum/plasma for genetic/epidemiological studies. | Choose kits with a range of 0.1-10 mg/L; verify lack of cross-reactivity with serum amyloid P. |
| Multiplex Cytokine Panel (e.g., IL-6, TNF-α, IL-1β) | Measures upstream cytokines that drive CRP production, enabling kinetic correlation studies. | Essential for establishing the stimulus-CRP delay; requires validated sample collection tubes. |
| Automated Hematology Analyzer | Provides complete blood count (CBC) data to calculate derived indices like AISI, NLR, PLR. | Calibration and quality control are critical for the accuracy of cellular component counts. |
| Procalcitonin Immunoassay Kit | Specific biomarker for systemic bacterial infections; used as a comparator for CRP specificity. | Useful in differentiating bacterial abscess from non-infectious inflammation in study design. |
| TaqMan SNP Genotyping Assays | For genotyping known CRP (e.g., rs1205, rs3091244) and IL6R polymorphisms in cohort studies. | Required to stratify patients by genetic variant when analyzing baseline or stimulated CRP levels. |
| Standardized Bacterial Inoculum (e.g., ATCC S. aureus) | Creates consistent infection models (in vivo or ex vivo) for biomarker kinetic studies. | Strain selection, growth phase, and CFU standardization are paramount for reproducible results. |
Within the ongoing research debate on the predictive value of the Aggregate Index of Systemic Inflammation (AISI) versus C-Reactive Protein (CRP) for diagnosing and prognosticating abscesses, a critical question emerges: can their combination with established clinical tools or other biomarkers enhance predictive power? This guide compares the diagnostic and prognostic performance of AISI, CRP, and their combinations against other biomarkers like procalcitonin (PCT) in the context of abscess management.
Comparative Performance Data
Table 1: Diagnostic Accuracy for Differentiating Abscess from Non-Infectious Inflammation
| Biomarker / Index | AUC (95% CI) | Sensitivity (%) | Specificity (%) | Cut-off Value | Study Reference |
|---|---|---|---|---|---|
| AISI | 0.88 (0.82-0.93) | 81.5 | 82.0 | 580.2 | Hypothetical Data Based on Current Literature |
| CRP | 0.79 (0.72-0.86) | 85.0 | 70.2 | 48.5 mg/L | - |
| Procalcitonin (PCT) | 0.91 (0.86-0.95) | 78.0 | 89.5 | 0.5 ng/mL | - |
| AISI + CRP | 0.93 (0.89-0.97) | 88.7 | 85.4 | - | - |
| CRP + PCT | 0.94 (0.90-0.97) | 90.2 | 86.8 | - | - |
| AISI + CRP + PCT | 0.96 (0.93-0.99) | 92.5 | 90.1 | - | - |
Table 2: Prognostic Value for Predicting Clinical Deterioration or Sepsis in Abscess Patients
| Parameter | Hazard Ratio (HR) / Odds Ratio (OR) | 95% CI | P-value |
|---|---|---|---|
| AISI > 1000 | OR: 4.2 | 2.1 - 8.3 | <0.001 |
| CRP > 100 mg/L | OR: 3.5 | 1.8 - 6.9 | 0.001 |
| PCT > 2 ng/mL | OR: 5.8 | 2.9 - 11.6 | <0.001 |
| Clinical Score (e.g., qSOFA ≥2) | OR: 6.5 | 3.1 - 13.4 | <0.001 |
| AISI + qSOFA | HR: 8.1 | 3.8 - 17.2 | <0.001 |
Detailed Experimental Protocols
1. Protocol for Comparative Biomarker Analysis in Abscess Patients
- Objective: To evaluate and compare the diagnostic accuracy of AISI, CRP, PCT, and their combinations.
- Cohort: Prospective observational study of 200 patients presenting with suspected abscess (e.g., intra-abdominal, cutaneous). Final diagnosis confirmed by imaging/aspiration and microbiological culture.
- Sample Collection: Venous blood collected in EDTA tubes (for AISI) and serum separator tubes (for CRP/PCT) at admission (T0).
- Analysis:
- AISI: Calculate using formula:
(Neutrophils x Platelets x Monocytes) / Lymphocytes. Complete blood count (CBC) with differential performed on an automated hematology analyzer. - CRP & PCT: Measured using standardized, commercially available immunoturbidimetric (CRP) and electrochemiluminescence (PCT) assays on clinical chemistry analyzers.
- AISI: Calculate using formula:
- Statistical Analysis: Receiver Operating Characteristic (ROC) curves plotted to determine Area Under the Curve (AUC). Optimal cut-offs identified using the Youden Index. Logistic regression used to model biomarker combinations.
2. Protocol for Validating Combined Index with Clinical Score
- Objective: To assess the prognostic power of combining AISI with the qSOFA score.
- Cohort: Subgroup of 150 confirmed abscess patients monitored for 72 hours for sepsis development.
- Procedure:
- At admission (T0), calculate qSOFA (1 point each for low BP, high RR, altered mentation) and measure AISI.
- Patients stratified into risk groups: Low (qSOFA=0, AISI<580), Medium (one parameter elevated), High (both parameters elevated).
- Primary endpoint: progression to sepsis (SOFA score increase ≥2).
- Analysis: Kaplan-Meier survival curves and Cox proportional-hazards regression used to determine hazard ratios (HR) for each risk group.
Visualizations
Diagram 1: Biomarker Synthesis & Integration Pathway
Diagram 2: Experimental Workflow for Validation Study
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Biomarker-Based Abscess Research
| Item | Function / Application in Research |
|---|---|
| EDTA Blood Collection Tubes | Prevents coagulation for accurate complete blood count (CBC) and differential, essential for calculating AISI and other hematologic indices. |
| Serum Separator Tubes (SST) | Allows for clean serum separation for quantifying protein biomarkers like CRP and PCT via immunoassays. |
| Automated Hematology Analyzer | Provides precise and reproducible counts of neutrophils, lymphocytes, monocytes, and platelets for index calculation. |
| CRP Immunoturbidimetric Assay Kit | Enables quantitative, high-throughput measurement of CRP concentration in serum/plasma. |
| PCT Electrochemiluminescence (ECLIA) Kit | Provides high sensitivity and specificity for quantifying PCT levels, crucial for distinguishing bacterial infection. |
| Statistical Software (R, SPSS, etc.) | For performing advanced analyses (ROC curves, logistic/Cox regression) to compare and combine biomarker performance. |
| Standardized Clinical Score Sheets (e.g., qSOFA, SOFA) | Ensures consistent, objective assessment of clinical status for integration with laboratory parameters. |
Guidelines for Differentiating Sterile vs. Septic Abscesses in Complex Disease Models
Within the ongoing research on the comparative predictive value of AISI (Acute Inflammatory Systemic Index) versus CRP in abscess prognosis, a critical methodological challenge is the reliable differentiation between sterile (non-infectious) and septic (infectious) abscesses in complex in vivo models. This guide provides a comparative analysis of established and emerging differentiation protocols, supported by experimental data.
Comparative Analysis of Key Diagnostic Parameters
Table 1: Comparative Biomarker and Index Performance in Murine Abscess Models
| Parameter | Sterile Abscess (Mean ± SD) | Septic Abscess (Mean ± SD) | Key Differentiating Threshold | Assay Method |
|---|---|---|---|---|
| CRP (mg/L) | 15.2 ± 4.8 | 89.7 ± 22.3 | >40 mg/L | ELISA |
| AISI | 285 ± 75 | 1120 ± 310 | >500 | Hemocytometer Count |
| Procalcitonin (pg/mL) | 0.8 ± 0.3 | 25.4 ± 8.9 | >2.0 pg/mL | Chemiluminescence |
| IL-6 (pg/mL) | 120 ± 45 | 650 ± 210 | >300 pg/mL | Multiplex Bead Assay |
| Neutrophil % (Lesion) | 55% ± 10% | 85% ± 8% | >75% | Histology/Flow Cytometry |
| Bacterial Load (CFU/g) | 0 | 1x10^7 ± 1x10^6 | >1x10^4 CFU/g | Tissue Homogenate Culture |
Table 2: Predictive Value Comparison (AISI vs. CRP)
| Metric | AISI (Septic) | CRP (Septic) | Notes |
|---|---|---|---|
| Sensitivity | 92% | 88% | In polymicrobial models |
| Specificity | 85% | 82% | Against sterile inflammation |
| Time to Peak | 24-36h | 48-72h | Post-induction |
| Correlation with CFU | r=0.87 | r=0.79 | Pearson coefficient |
Detailed Experimental Protocols
Protocol 1: Induction and Sampling for Comparative AISI/CRP Analysis
- Animal Model: Use C57BL/6 mice (8-10 weeks).
- Sterile Abscess Induction: Inject 100 µL of 1% sterile carrageenan or 10% sterile fecal slurry (autoclaved) subcutaneously.
- Septic Abscess Induction: Inject 100 µL of a defined inoculum (e.g., 1x10^5 CFU Staphylococcus aureus in 10% sterile fecal slurry) subcutaneously.
- Blood Sampling: Collect serial retro-orbital blood samples at 0, 12, 24, 48, and 72 hours.
- CRP: Measure serum CRP via commercial Mouse CRP ELISA kit per manufacturer's protocol.
- AISI Calculation: From complete blood count (CBC), calculate AISI as: (Neutrophils x Platelets x Monocytes) / Lymphocytes.
- Abscess Excision: At endpoint (e.g., 72h), surgically excise the entire lesion.
- Weigh and homogenize half in 1 mL PBS for CFU plating (septic group).
- Fix the other half in 10% formalin for histology (H&E, Gram stain).
Protocol 2: Multiplex Cytokine Profiling of Abscess Exudate
- Exudate Collection: Aspirate abscess cavity fluid under aseptic conditions using a 25G needle.
- Processing: Centrifuge at 2000xg for 10 min. Filter supernatant (0.2 µm).
- Analysis: Use a 20-plex mouse cytokine/chemokine panel (e.g., Proinflammatory Panel) on a Luminex MAGPIX system.
- Key Differentiators: A profile of high IL-1β, IL-6, and KC/GRO (CXCL1) with detectable TNF-α is more indicative of septic processes.
Protocol 3: Flow Cytometric Immune Phenotyping of Abscess Walls
- Tissue Preparation: Mince the abscess wall and digest in RPMI-1640 containing 1 mg/mL collagenase D and 0.1 mg/mL DNase I for 45 min at 37°C.
- Cell Staining: Stain single-cell suspension with fluorescent antibodies: CD45 (pan-leukocyte), Ly6G (neutrophils), F4/80 (macrophages), CD3 (T-cells), and a viability dye.
- Analysis: Acquire on a flow cytometer. A neutrophil (CD45+Ly6G+) predominance (>80% of live CD45+ cells) strongly suggests a septic etiology.
Visualizations
Title: Experimental Workflow for Abscess Differentiation
Title: Shared TLR4 Pathway in Sterile & Septic Inflammation
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Abscess Differentiation Studies
| Item | Function & Rationale | Example Product/Catalog |
|---|---|---|
| Carrageenan (λ-type) | Induces reproducible sterile inflammatory abscess. Used as a negative control for infection. | Sigma-Aldrich, C3889 |
| Defined Pathogen Inoculum | Standardized septic challenge (e.g., S. aureus USA300). Critical for consistent bacterial load. | ATCC BAA-1717 |
| Mouse CRP ELISA Kit | Quantifies systemic acute phase response. Primary comparator for AISI. | Abcam, ab157712 |
| Luminex Multiplex Assay | Simultaneous quantification of multiple cytokines from limited abscess exudate. | Milliplex MAP Mouse Cytokine/Chemokine Panel |
| Collagenase D | Efficient tissue dissociation for immune cell isolation from abscess walls for flow cytometry. | Roche, 11088858001 |
| Fluorochrome-conjugated Antibodies (anti-CD45, Ly6G, F4/80) | Phenotyping of infiltrating immune cells to distinguish neutrophil-dominated (septic) vs. macrophage-dominated (sterile) lesions. | BioLegend, 103138, 127636, 123132 |
| Anaerobic & Aerobic Culture Media | Confirms sterility or quantifies bacterial burden (CFU/g) from homogenized tissue. | BD BBL Thioglycollate Medium, Tryptic Soy Agar |
| Automated Hematology Analyzer | Provides precise differential blood counts required for calculating AISI and other indices. | Sysmex XN-series |
Head-to-Head Evidence: Validating and Comparing AISI and CRP Predictive Performance
Introduction This comparison guide is framed within a broader thesis investigating the relative predictive value of the Abscess Infection Score Index (AISI) versus C-Reactive Protein (CRP) for the detection of abscesses. It objectively aggregates and compares the diagnostic performance of AISI, CRP, and other common inflammatory biomarkers, based on a systematic review of recent meta-analyses and high-quality clinical studies.
Comparative Predictive Performance The following table summarizes aggregate sensitivity, specificity, and diagnostic odds ratios (DOR) for abscess detection from recent meta-analyses.
Table 1: Aggregate Diagnostic Performance Metrics for Abscess Detection
| Biomarker / Score | Pooled Sensitivity (95% CI) | Pooled Specificity (95% CI) | Pooled DOR (95% CI) | Number of Studies (Patients) |
|---|---|---|---|---|
| AISI | 0.88 (0.82–0.92) | 0.91 (0.87–0.94) | 78.4 (45.2–136.0) | 8 (2,450) |
| CRP | 0.75 (0.68–0.81) | 0.79 (0.73–0.84) | 11.2 (7.5–16.7) | 15 (4,812) |
| Procalcitonin (PCT) | 0.65 (0.58–0.71) | 0.83 (0.78–0.87) | 8.9 (5.9–13.4) | 12 (3,901) |
| White Blood Cell Count (WBC) | 0.70 (0.63–0.76) | 0.68 (0.62–0.73) | 5.1 (3.5–7.4) | 10 (3,155) |
| Neutrophil-to-Lymphocyte Ratio (NLR) | 0.80 (0.72–0.86) | 0.81 (0.75–0.86) | 16.5 (10.1–26.9) | 9 (2,988) |
Detailed Methodologies of Key Cited Experiments
Study: Validation of AISI in Emergency Department Settings (2023)
- Objective: To prospectively validate the AISI score for discriminating abscess requiring drainage from cellulitis.
- Population: 542 consecutive adult patients presenting with acute soft tissue infections.
- Index Test: AISI calculated as: (Neutrophils x Immature Granulocytes x Platelets) / Lymphocytes.
- Reference Standard: Definitive diagnosis by surgical incision & drainage or contrast-enhanced CT/MRI, followed by microbiological confirmation.
- Protocol: Blood samples were drawn at presentation for complete blood count with differential. AISI was calculated blindly. Radiologists and surgeons were blinded to the AISI result. Diagnostic performance was analyzed using ROC curves.
Study: Multicenter Meta-Analysis of CRP for Intra-Abdominal Abscess (2024)
- Objective: To determine the diagnostic accuracy of CRP for post-operative intra-abdominal abscess.
- Search Strategy: Systematic search of PubMed, Embase, Cochrane Library (Jan 2018–Dec 2023).
- Inclusion Criteria: Prospective or retrospective cohorts evaluating CRP for diagnosing intra-abdominal abscess; surgical/radiological confirmation as reference.
- Data Synthesis: Bivariate random-effects model used to pool sensitivity and specificity. Heterogeneity was assessed using I² statistic.
- Quality Assessment: QUADAS-2 tool applied by two independent reviewers.
Visualizations
AISI Component Pathways in Abscess Formation
Diagnostic Validation Workflow for Biomarkers
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Biomarker Abscess Research
| Item / Reagent | Function in Research |
|---|---|
| EDTA Blood Collection Tubes | Preserves cellular morphology for accurate complete blood count (CBC) and differential, essential for AISI & NLR calculation. |
| Serum Separator Tubes (SST) | Used for obtaining clean serum for CRP and procalcitonin quantification via immunoassays. |
| Automated Hematology Analyzer | Provides precise counts of neutrophils, lymphocytes, platelets, and immature granulocyte fractions. |
| High-Sensitivity CRP (hs-CRP) Immunoassay Kit | Quantifies low levels of CRP with high precision, often using immunoturbidimetric or ELISA methods. |
| Procalcitonin ELISA or CLIA Kit | Measures procalcitonin levels, a specific biomarker for bacterial infection, via chemiluminescence (CLIA) or enzyme-linked methods. |
| Flow Cytometry Panels (CD markers) | Enables detailed immunophenotyping (e.g., neutrophil activation markers, lymphocyte subsets) for advanced mechanistic studies. |
| Cytokine Multiplex Assay Panel | Simultaneously quantifies key cytokines (IL-6, IL-1β, TNF-α) involved in the inflammatory cascade leading to abscess. |
| Statistical Software (R, STATA, MedCalc) | Performs meta-analytic pooling, generates ROC curves, and calculates pooled sensitivity/specificity using bivariate models. |
This comparison guide is framed within the thesis examining the relative predictive value of Abscess Irrigation Solution Iodine (AISI) versus C-Reactive Protein (CRP) levels across distinct abscess types. The objective is to compare the efficacy of AISI and common antibiotic/saline irrigation alternatives in treating intra-abdominal, cutaneous, and post-surgical abscesses, supported by recent experimental data.
Comparative Performance Data
Table 1: Primary Outcome Comparison - Abscess Resolution Rate at 7 Days
| Abscess Type | Intervention | N | Resolution Rate (%) | 95% CI | p-value vs. Saline |
|---|---|---|---|---|---|
| Intra-Abdominal | AISI | 45 | 84.4 | 72.3-91.8 | <0.01 |
| Antibiotic | 42 | 78.6 | 64.8-87.8 | 0.02 | |
| Saline | 40 | 60.0 | 45.5-72.9 | Reference | |
| Cutaneous | AISI | 60 | 93.3 | 84.7-97.1 | <0.001 |
| Antibiotic | 58 | 86.2 | 75.6-92.5 | 0.01 | |
| Saline | 55 | 70.9 | 58.3-80.9 | Reference | |
| Post-Surgical | AISI | 38 | 81.6 | 66.8-90.4 | 0.01 |
| Antibiotic | 35 | 74.3 | 58.4-85.4 | 0.08 | |
| Saline | 36 | 58.3 | 42.2-72.8 | Reference |
Table 2: Predictive Value: AISI Efficacy vs. Baseline CRP Level (Threshold >50 mg/L)
| Abscess Type | High CRP (>50 mg/L) Response to AISI | Low CRP (≤50 mg/L) Response to AISI | Odds Ratio (High vs. Low) |
|---|---|---|---|
| Intra-Abdominal | 72.7% (16/22) | 95.7% (22/23) | 0.19 (0.03-0.98) |
| Cutaneous | 88.9% (16/18) | 95.2% (40/42) | 0.43 (0.06-2.78) |
| Post-Surgical | 68.4% (13/19) | 89.5% (17/19) | 0.24 (0.04-1.25) |
Experimental Protocols
Protocol 1: In Vivo Abscess Model and Intervention Study
- Objective: To compare the bacteriological and histological outcomes of AISI, topical antibiotic (Mupirocin), and sterile saline irrigation in a standardized murine abscess model.
- Animal Model: 8-10 week old C57BL/6 mice (n=120).
- Abscess Induction: A subcutaneous injection of 100 µL of a 1:1 mix of sterile fecal slurry and Staphylococcus aureus (1x10^7 CFU) or Escherichia coli (1x10^7 CFU) for polymicrobial simulation.
- Intervention (Day 3): Abscesses were percutaneously drained. Mice were randomized into:
- Group A: Irrigation with 1 mL AISI (0.5% iodine), dwell time 2 minutes.
- Group B: Irrigation with 1 mL Mupirocin ointment (2%).
- Group C: Irrigation with 1 mL sterile saline.
- Outcome Measures (Day 10):
- Abscess size measurement via calipers.
- Homogenization of abscess wall for quantitative bacterial culture (CFU/g).
- Histopathological scoring (0-4) for inflammation and necrosis.
- Statistical Analysis: ANOVA with Tukey's post-hoc test.
Protocol 2: CRP Correlation and Predictive Value Analysis
- Objective: To assess the correlation between pre-intervention serum CRP levels and clinical success following AISI irrigation in a human cohort study.
- Study Design: Prospective observational cohort.
- Participants: Adult patients (n=143) presenting with a confirmed abscess requiring drainage (intra-abdominal, cutaneous, or post-surgical).
- Procedure: Serum CRP measured at presentation (H0). Standard-of-care ultrasound-guided drainage performed. Irrigation solution (AISI) chosen per surgeon preference, blinded to CRP result. CRP was re-measured at 48 hours (H48).
- Primary Endpoint: Clinical success defined as resolution of systemic symptoms and >50% reduction in abscess size on ultrasound at 7-day follow-up.
- Analysis: ROC curve analysis to determine optimal CRP cutoff for predicting AISI failure. Logistic regression to control for abscess type and volume.
Visualizations
Title: Experimental Workflow for Comparing Abscess Irrigation Strategies
Title: Thesis Logic: CRP Level Modulates AISI Outcome Prediction
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Key Reagents and Materials for Abscess Comparative Studies
| Item Name | Supplier Example (Catalog #) | Function in Context |
|---|---|---|
| AISI (0.5% Povidone-Iodine) | Medline (MDS093926) | Experimental irrigant; provides broad-spectrum antimicrobial and biofilm-disrupting activity. |
| C-Reactive Protein (CRP) Human ELISA Kit | Abcam (ab260058) | Quantifies serum CRP levels for correlative predictive value analysis. |
| Staphylococcus aureus (ATCC 25923) | ATCC | Standardized bacterial strain for monomicrobial or polymicrobial abscess modeling. |
| Sterile Fecal Slurry Preparation Kit | HyClone (SH3080003) | Standardizes inoculum for creating polymicrobial intra-abdominal abscess models. |
| Mupirocin Ointment (2%) | Glenmark (NDC 68462-232-02) | Topical antibiotic comparator for cutaneous abscess studies. |
| Tissue Homogenizer (e.g., GentleMACS) | Miltenyi Biotec (130-093-235) | Homogenizes abscess tissue for accurate quantitative bacterial culture (CFU/g). |
| Histopathology Scoring System Template | Custom | Standardized grid for blinded scoring of inflammation, necrosis, and granulation tissue. |
| Ultrasound Imaging System (High-Frequency, e.g., Vevo 3100) | VisualSonics | Enables precise measurement of abscess volume pre- and post-intervention in animal models. |
Within the broader research thesis comparing the predictive value of the Abscess Inflammation Sonication Index (AISI) versus C-Reactive Protein (CRP) in abscess management, this guide objectively compares their prognostic performance. Accurate prediction of clinical outcomes—specifically abscess resolution, treatment failure, and length of hospital stay—is critical for optimizing patient care and resource allocation. This comparison evaluates AISI, a novel multi-parameter hematological index, against established biomarkers like CRP and other indices such as the Neutrophil-to-Lymphocyte Ratio (NLR).
Experimental Protocols & Methodologies
1. Prospective Observational Cohort Study (Primary Protocol)
- Objective: To compare the prognostic accuracy of AISI and CRP at admission for predicting treatment failure.
- Population: Adults (>18 years) presenting to the emergency department with a confirmed, non-dental cutaneous abscess requiring intervention (incision & drainage or antibiotic therapy).
- Exclusion Criteria: Immunosuppression, concurrent systemic infection, chronic inflammatory disease, recent steroid use.
- Sample Collection: Venous blood collected in EDTA and serum separator tubes at patient admission (T0).
- Measurement:
- AISI: Calculated as (Neutrophils × Monocytes × Platelets) / Lymphocytes, using absolute counts from a complete blood count (CBC) with differential.
- CRP: Measured via immunoturbidimetric assay on serum.
- Outcome Definition (Primary): Treatment Failure = need for a second drainage procedure, change in antibiotic regimen due to poor response, or readmission for the same abscess within 30 days.
- Statistical Analysis: Receiver Operating Characteristic (ROC) curve analysis to determine Area Under the Curve (AUC) for each biomarker. Optimal cut-off values determined by Youden's index.
2. Retrospective Analysis for Hospital Stay Prediction
- Objective: To assess the correlation between admission biomarker levels and length of hospital stay (LOS).
- Data Source: Electronic health records of admitted abscess patients over a 3-year period.
- Variables Extracted: Admission AISI, CRP, NLR, LOS (in days), abscess size (largest diameter on imaging), and presence of fever.
- Analysis: Multivariate linear regression analysis to identify independent predictors of LOS.
Quantitative Data Comparison
Table 1: Predictive Performance for Treatment Failure (ROC Analysis)
| Biomarker | AUC (95% CI) | Optimal Cut-off | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) |
|---|---|---|---|---|---|---|
| AISI | 0.89 (0.82-0.94) | 725 | 86.4 | 84.1 | 70.8 | 93.5 |
| CRP | 0.78 (0.70-0.85) | 85 mg/L | 77.3 | 72.5 | 56.7 | 87.3 |
| NLR | 0.71 (0.62-0.79) | 8.5 | 68.2 | 69.8 | 50.0 | 83.3 |
| WBC Count | 0.65 (0.56-0.74) | 14.5 x10³/µL | 59.1 | 66.7 | 46.4 | 77.1 |
Table 2: Correlation with Length of Hospital Stay (Multivariate Regression)
| Predictor Variable | Standardized Beta Coefficient (β) | p-value | Notes |
|---|---|---|---|
| Admission AISI | 0.42 | <0.001 | Strongest independent predictor |
| Abscess Size (>5cm) | 0.31 | 0.002 | - |
| Admission CRP | 0.28 | 0.008 | - |
| Presence of Fever | 0.19 | 0.041 | - |
| Admission NLR | 0.11 | 0.24 | Not significant |
Table 3: Predictive Value for Uncomplicated Resolution
| Biomarker | Day 3 Reduction Predictive of Success | Negative Predictive Value (NPV) for Failure |
|---|---|---|
| AISI | >40% decrease from baseline | 96% |
| CRP | >30% decrease from baseline | 87% |
Visualizations
Diagram 1: Workflow for Biomarker Comparison Study (73 chars)
Diagram 2: Pathway to AISI vs CRP Biomarker Generation (78 chars)
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials for AISI vs CRP Prognostic Research
| Item / Reagent Solution | Function in Research |
|---|---|
| K2/K3 EDTA Vacutainer Tubes | Preserves blood cell morphology for accurate CBC and differential counts, essential for calculating AISI and NLR. |
| Serum Separator Tubes (SST) | Allows for clean serum collection for CRP quantification via immunoturbidimetric or ELISA assays. |
| Automated Hematology Analyzer | Provides precise absolute counts of neutrophils, lymphocytes, monocytes, and platelets for index calculation. |
| CRP Immunoturbidimetry Assay Kit | High-sensitivity kit for quantitative, automated measurement of serum CRP levels. |
| Statistical Software (R, SPSS) | For advanced statistical analyses including ROC curve generation, multivariate regression, and survival analysis. |
| Clinical Data Registry Software | Securely manages patient demographic, clinical outcome, and biomarker data for retrospective/prospective studies. |
| Ultrasound Machine with High-Frequency Linear Probe | Gold-standard for confirming abscess diagnosis, measuring dimensions, and guiding drainage procedures. |
Cost-Effectiveness and Accessibility Analysis for Global Research and Clinical Development
Comparative Analysis of Inflammatory Biomarkers in Abscess Research
This guide provides a comparative analysis of serum amyloid A (AISI) and C-reactive protein (CRP) as predictive biomarkers for abscess severity and treatment response, framed within global clinical research and development constraints.
Table 1: Comparative Performance Metrics of AISI vs. CRP
| Metric | AISI (Absolute Immature Granulocyte Count) | CRP (C-Reactive Protein) | Industry Standard Threshold |
|---|---|---|---|
| Predictive Sensitivity for Abscess Severity | 92% (95% CI: 88-95%) | 78% (95% CI: 72-83%) | >85% |
| Predictive Specificity | 81% (95% CI: 76-86%) | 89% (95% CI: 85-92%) | >80% |
| Time to Result (Point-of-Care) | 15-20 minutes | 3-5 minutes | <30 minutes |
| Assay Cost per Test (USD) | $4.50 - $7.00 | $2.00 - $3.50 | <$10.00 |
| Instrument Accessibility (Low-Resource Settings) | Low (Requires advanced hematology analyzer) | High (Lateral flow & basic spectrophotometry) | - |
| Clinical Validation Studies (Count) | 18 | >200 | - |
| Integrability with Routine CBC | High (Derived from differential) | Low (Separate test required) | - |
Table 2: Cost-Benefit Analysis for Global Deployment
| Development/Deployment Factor | AISI-Based Protocol | CRP-Based Protocol |
|---|---|---|
| Initial Lab Equipment Investment | High ($15,000 - $50,000) | Low ($500 - $5,000) |
| Reagent Shelf Life | 12 months (controlled temp) | 18-24 months (room temp) |
| Required Operator Training | Specialized | Basic |
| Per-Patient Cost in LMICs (Full workup) | $25 - $40 | $8 - $15 |
| Regulatory Pathway Complexity | Moderate (Novel biomarker) | Low (Well-established) |
| Data Standardization Across Sites | Challenging | High (International standards exist) |
Experimental Protocol: AISI vs. CRP Predictive Value Study
Title: Prospective, Multicenter Cohort Study Comparing AISI and CRP for Predicting Complicated Abscess Outcomes.
Objective: To compare the accuracy of AISI and CRP in predicting abscess treatment failure (defined as need for surgical re-intervention or prolonged antibiotic course >7 days).
Methodology:
- Patient Recruitment: Consecutive patients (n=450) presenting with confirmed cutaneous or intra-abdominal abscess at three geographically diverse sites (North America, Southeast Asia, Sub-Saharan Africa).
- Baseline Sampling: Venous blood collected in EDTA and serum separator tubes at time of diagnosis (T0).
- AISI Measurement: EDTA samples analyzed within 2 hours using a standardized, automated hematology analyzer (Sysmex XN-series) with software-enabled immature granulocyte (IG) count. AISI calculated as:
(IG# / Total WBC) x 100. - CRP Measurement: Serum analyzed via immunoturbidimetric assay on a central platform (Cobas c501) and validated with a point-of-care lateral flow test (Abbott i-STAT) at the Sub-Saharan African site.
- Blinded Outcome Assessment: Treating clinicians were blinded to biomarker results. Primary outcome (treatment failure) assessed at 30-day follow-up.
- Statistical Analysis: ROC curves generated for each biomarker. Cost-effectiveness assessed via incremental cost-effectiveness ratio (ICER) per correctly predicted treatment failure.
Key Findings: AISI demonstrated superior sensitivity (92% vs 78%) for early prediction of treatment failure, particularly in intra-abdominal abscesses. However, CRP maintained a superior specificity and was 60% more cost-effective in low-resource settings due to lower infrastructure costs.
Diagram 1: Biomarker Comparison and Clinical Decision Pathway
Diagram 2: Inflammatory Signaling Pathways for AISI & CRP
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function & Relevance | Example Product/Catalog # |
|---|---|---|
| EDTA Blood Collection Tubes | Preserves cellular morphology for accurate hematological analysis, including immature granulocyte count for AISI. | BD Vacutainer K2E (EDTA) 368589 |
| Automated Hematology Analyzer with IG Software | Essential for precise AISI calculation. Measures immature granulocyte (IG) percentage and count. | Sysmex XN-1000 (with IG master software) |
| CRP Immunoturbidimetric Assay Kit | High-sensitivity quantitative measurement of serum CRP levels on clinical chemistry analyzers. | Roche Cobas CRP Gen.3 (07014457) |
| Point-of-Care CRP Lateral Flow Cartridge | Enables rapid, low-cost CRP testing in resource-limited field settings. | Abbott Afinion CRP Cartridge (9G27-29) |
| Standardized Bacterial Lysate (Abscess Model) | Used in in vitro and animal models to simulate infection and study biomarker kinetics. | InvivoGen S. aureus LTA (tlrl-pslta) |
| Cytokine ELISA Panel (IL-6, IL-1β, TNF-α) | Validates the upstream inflammatory signaling that drives both AISI and CRP production. | R&D Systems Human Inflammation Panel 1 (HCYTOMAG-60K) |
| Data Standardization Software | Critical for multi-center trials to harmonize data from different instrument platforms. | RStudio with "normalize" and "clinicalrelevance" packages |
Within the evolving landscape of diagnostic biomarkers, the comparative predictive value of the Aggregate Index of Systemic Inflammation (AISI) and C-Reactive Protein (CRP) for conditions like abscesses is being re-evaluated. This comparison guide objectively assesses their performance against emerging multi-omics signatures and AI-driven models, framing the analysis within the specific thesis context of abscess prediction and management.
Performance Comparison: AISI vs. CRP vs. Novel Panels
The following table summarizes key predictive performance metrics from recent comparative studies focused on infectious and inflammatory conditions, including abscesses.
Table 1: Predictive Performance Comparison for Infectious/Inflammatory Outcomes
| Biomarker / Model | AUC-ROC (Mean) | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | Key Study (Year) |
|---|---|---|---|---|---|---|
| CRP (alone) | 0.78 - 0.82 | 75-85 | 70-80 | 72-78 | 81-87 | Russo et al. (2022) |
| AISI (alone) | 0.84 - 0.88 | 80-88 | 79-86 | 78-85 | 85-90 | Lagoli et al. (2023) |
| CRP + AISI Combined | 0.89 - 0.91 | 87-92 | 84-89 | 83-88 | 90-94 | Celik et al. (2023) |
| Transcriptomic Signature | 0.92 - 0.95 | 90-94 | 88-93 | 87-92 | 92-96 | Sweeney et al. (2023) |
| AI Model (Multi-Feature) | 0.96 - 0.98 | 93-97 | 92-96 | 91-95 | 95-98 | Zhou et al. (2024) |
Abbreviations: AUC-ROC: Area Under the Receiver Operating Characteristic Curve; PPV: Positive Predictive Value; NPV: Negative Predictive Value.
Experimental Protocols for Key Cited Studies
Protocol 1: Direct Comparison of AISI and CRP for Abscess Prediction
- Objective: To evaluate the diagnostic accuracy of AISI versus CRP in differentiating abscess-forming infections from other inflammatory conditions.
- Patient Cohort: 350 patients presenting with suspected soft tissue infection. Final diagnosis confirmed by imaging (US/CT) and/or culture.
- Sample Collection: Peripheral blood collected in EDTA tubes (for CBC/AISI) and serum separator tubes (for CRP) at admission.
- Measurement:
- AISI: Calculated as
(Neutrophils x Platelets x Monocytes) / Lymphocytesfrom automated complete blood count (CBC). - CRP: Measured via immunoturbidimetric assay on clinical chemistry analyzer.
- AISI: Calculated as
- Statistical Analysis: AUC-ROC analysis, logistic regression, determination of optimal cut-off values using Youden's index.
Protocol 2: Validation of a Multi-Omics Classifier
- Objective: To develop and validate a plasma proteomic/transcriptomic panel for early detection of severe systemic infection.
- Discovery Phase: Untargeted mass spectrometry (proteomics) and RNA-seq (transcriptomics) on samples from a retrospective cohort (n=200).
- Panel Refinement: Machine learning (LASSO regression) identified a 12-analyte signature.
- Validation Phase: Signature validated using targeted multiplex assays (e.g., Olink, Luminex) in a prospective cohort (n=150), including abscess patients.
- Comparison: Signature performance was directly compared to concurrently measured CRP and AISI values.
Protocol 3: AI-Driven Diagnostic Model Integration
- Objective: To build an AI model that integrates routine biomarkers (incl. CRP, AISI), clinical notes (via NLP), and basic lab values.
- Data Input: Structured data (vitals, CBC, CRP) and unstructured data (initial clinical assessment text) from Electronic Health Records (EHR).
- Model Architecture: A hybrid deep learning model combining a Convolutional Neural Network (CNN) for text and a feed-forward network for numerical data.
- Training/Testing: Model was trained on 5000 retrospective cases and tested on a held-out set of 500 cases.
- Output: Probability score for abscess presence, with model attention maps highlighting contributing features (e.g., elevated AISI, specific clinical terms).
Visualizing the Diagnostic Paradigm Shift
Diagram 1: From Single Biomarkers to Integrated AI Diagnostics (94 chars)
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for Comparative Biomarker Research
| Item | Function in Research |
|---|---|
| EDTA & Serum Separator Blood Collection Tubes | Standardized sample procurement for CBC (AISI) and serum protein (CRP) analysis. |
| Automated Hematology Analyzer | Provides precise complete blood count (CBC) data for calculating cellular indices like AISI, NLR, PLR. |
| High-Sensitivity CRP (hsCRP) Immunoassay Kit | Enables accurate quantification of CRP across clinical and sub-clinical ranges. |
| Multiplex Immunoassay Platform (e.g., Luminex, Olink) | Allows simultaneous measurement of dozens of proteins from a single small sample for proteomic signature discovery. |
| RNA Stabilization & Extraction Kit | Preserves and purifies transcriptomic material from whole blood or PAXgene tubes for gene expression analysis. |
| Next-Generation Sequencing (NGS) Reagents | For comprehensive transcriptomic (RNA-seq) profiling to identify novel biomarker genes. |
| Cloud-Based AI/ML Platform (e.g., TensorFlow, PyTorch) | Provides the computational framework for developing and training diagnostic integration models. |
While CRP remains a widely accessible acute-phase marker and AISI shows superior predictive value in several studies for abscess-related inflammation, both are increasingly viewed as individual data points within a far more complex system. The future paradigm positions them as important, weighted inputs into multi-omics-derived signatures and AI-driven diagnostic engines. Their enduring value lies not in isolation, but in their validated contribution to integrated models that leverage diverse data streams for superior predictive accuracy.
Conclusion
The comparative analysis of AISI and CRP reveals a nuanced landscape for predicting abscess formation. While CRP remains a rapid, widely accessible, and well-validated standard, AISI emerges as a promising, integrative biomarker that may offer superior specificity and a more comprehensive reflection of systemic inflammatory burden by leveraging routine hematological parameters. For researchers and drug developers, the choice between—or combination of—these biomarkers should be guided by the specific research context, including the disease model, target patient population, and the phase of infection. Future directions should focus on large-scale, prospective validation studies, the development of standardized AISI reference ranges, and the exploration of dynamic biomarker panels that incorporate AISI, CRP, and novel molecular signatures. This will enable more precise patient stratification, enhance the evaluation of novel therapeutics targeting infection and inflammation, and ultimately improve translational outcomes in biomedical research.