AISI vs. CRP: A Novel Paradigm for Predicting Abscess Severity and Clinical Outcomes
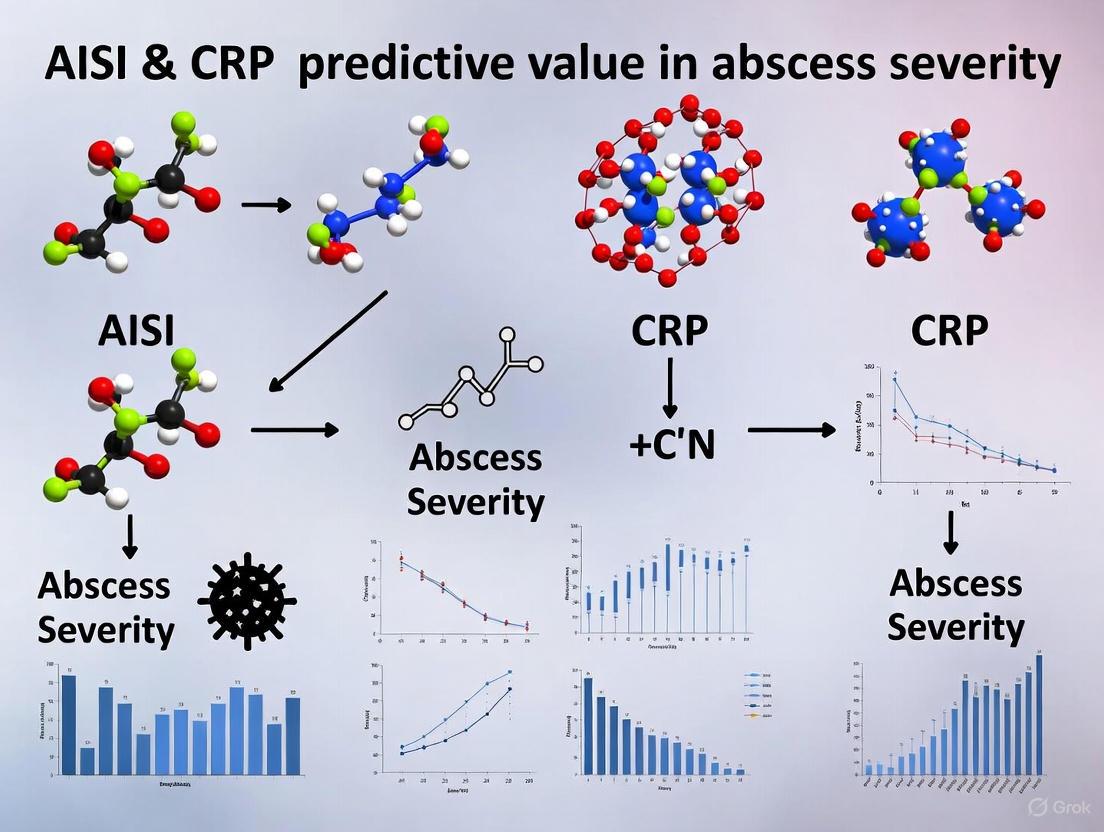
This article provides a comprehensive analysis of the predictive value of the Aggregate Index of Systemic Inflammation (AISI) compared to the established biomarker C-reactive protein (CRP) in assessing abscess severity.
AISI vs. CRP: A Novel Paradigm for Predicting Abscess Severity and Clinical Outcomes
Abstract
This article provides a comprehensive analysis of the predictive value of the Aggregate Index of Systemic Inflammation (AISI) compared to the established biomarker C-reactive protein (CRP) in assessing abscess severity. Targeting researchers and drug development professionals, it synthesizes recent evidence demonstrating AISI's superior sensitivity and specificity in forecasting complications like systemic inflammatory response syndrome (SIRS), prolonged hospitalization, and mortality across various abscess types, including odontogenic and intra-abdominal. The content explores the methodological application of these biomarkers, troubleshoots limitations of conventional markers, and validates AISI's efficacy through comparative statistical performance and machine learning integration. The findings advocate for the integration of AISI into clinical prognostication and as a potential endpoint in therapeutic development for severe inflammatory infections.
Understanding the Inflammatory Landscape: From CRP to Novel Systemic Indices
The Established Role of CRP in Infection and Inflammation
C-reactive protein (CRP) has long been the cornerstone biomarker for detecting and monitoring inflammatory states in clinical practice. As an acute-phase reactant produced by the liver in response to pro-inflammatory cytokines, primarily interleukin-6 (IL-6), CRP serves as a sensitive indicator of systemic inflammation across diverse pathological conditions including infections, autoimmune disorders, and tissue injury [1] [2]. Despite its widespread use and diagnostic utility, emerging research reveals limitations in CRP's predictive value for certain clinical scenarios, prompting investigation of novel inflammatory indices such as the Aggregate Index of Systemic Inflammation (AISI) that integrate multiple hematological parameters [3] [4] [5]. This review examines the established role of CRP in infection and inflammation within the context of recent comparative studies evaluating AISI versus CRP for predicting abscess severity.
CRP Biochemistry and Physiological Functions
C-reactive protein is a pentraxin family protein characterized by its pentameric structure, composed of five identical 23-kDa subunits arranged in a cyclic disc-shaped formation [1]. Each subunit contains a conserved calcium-binding site essential for its ligand-binding capability, particularly for phosphocholine (PCh) moieties exposed on damaged cell membranes and bacterial surfaces [1]. The protein exists in two primary conformational states: the native pentameric form (pCRP) and the monomeric form (mCRP), which exhibits distinct pro-inflammatory properties [1].
The binding face (B-face) of pCRP recognizes PCh and phosphoethanolamine headgroups on activated or apoptotic cell membranes, while the effector face (A-face) mediates complement activation through interaction with C1q and Fcγ receptors [1]. Upon binding to damaged membranes in inflammatory environments, pCRP undergoes a conformational transition to an activated state (pCRP*) and may dissociate into mCRP subunits, both of which exhibit enhanced pro-inflammatory activities including complement activation, leukocyte recruitment, and platelet stimulation [1].
CRP Activation Pathway: This diagram illustrates the inflammatory signaling cascade leading from tissue injury to CRP-mediated immune responses.
Established Clinical Applications of CRP
Diagnostic and Monitoring Utility
CRP measurement remains a fundamental tool in clinical practice for several key applications. It serves as a sensitive marker for detecting bacterial infections, differentiating inflammatory from non-inflammatory conditions, monitoring disease activity in autoimmune disorders such as rheumatoid arthritis and lupus, and assessing treatment response [2] [6]. The high-sensitivity CRP (hs-CRP) assay enables detection of low-grade inflammation relevant for cardiovascular risk stratification, with concentrations <1.0 mg/L indicating low risk, 1.0-3.0 mg/L indicating average risk, and >3.0 mg/L indicating high risk for cardiovascular events [2] [7].
In acute inflammatory states, CRP levels rise rapidly and markedly—often increasing before significant elevation in erythrocyte sedimentation rate (ESR)—and can reach concentrations up to 1000-fold above baseline within 24-48 hours of inflammatory stimulus [2]. During recovery, CRP normalizes more quickly than ESR, making it particularly valuable for monitoring treatment response [2]. The test is widely available, relatively inexpensive, and provides objective data to guide clinical decision-making across numerous medical specialties.
Reference Ranges and Interpretation
Standard CRP reference values are generally <1.0 mg/dL or <10.0 mg/L, while hs-CRP assays used for cardiovascular risk assessment have lower detection limits [2]. CRP levels demonstrate intraindividual variability and can be influenced by factors including body mass index, smoking, hormonal therapy, and demographic factors such as sex and race, with African Americans and females typically having higher baseline levels [2]. Proper interpretation requires two measurements taken at least two weeks apart when used for cardiovascular risk assessment, with the average value determining risk classification [6] [7].
Comparative Analysis: AISI vs. CRP in Odontogenic Abscess Severity
Study Design and Methodology
A recent retrospective comparative study conducted at Dubrava University Hospital evaluated the prognostic value of multiple systemic inflammatory indices for predicting severity of odontogenic abscesses [3] [4] [5]. The investigation included 221 patients hospitalized for odontogenic abscesses between January 2019 and December 2023, with comprehensive clinical and laboratory data collected at admission.
Experimental Protocol:
- Patient Population: Adults (>18 years) with clinical diagnosis of odontogenic abscess requiring surgical intervention
- Exclusion Criteria: Non-odontogenic infections, immune disorders, therapies affecting inflammatory parameters (corticosteroids, immunosuppressants, NSAIDs, antibiotics), incomplete medical data
- Severity Assessment: Symptom Severity (SS) Score based on SIRS criteria, trismus, dysphagia, affected anatomical spaces, dehydration signs, and comorbidities [4] [5]
- Laboratory Analysis: Complete blood count with differential and CRP measurements performed at hospital admission
- Index Calculation:
- AISI = (Neutrophils × Monocytes × Platelets) / Lymphocytes
- SII = (Neutrophils × Platelets) / Lymphocytes
- NLR = Neutrophils / Lymphocytes
- PLR = Platelets / Lymphocytes
- LMR = Lymphocytes / Monocytes
- Statistical Analysis: ROC curve analysis to assess predictive accuracy for abscess severity
Experimental Workflow: This diagram outlines the methodological approach for comparing inflammatory indices in abscess severity prediction.
Quantitative Performance Comparison
The study demonstrated superior predictive performance of AISI compared to traditional inflammatory markers including CRP. The following table summarizes the key comparative findings:
Table 1: Predictive Performance of Inflammatory Indices for Odontogenic Abscess Severity
| Biomarker | AUC | Sensitivity (%) | Specificity (%) | Performance Characteristics |
|---|---|---|---|---|
| AISI | 0.90 | 82.93 | 81.63 | Superior predictor of severity, significant correlation with hospital stay and SIRS |
| CRP | 0.74 | - | - | Moderate predictive value for severe abscesses |
| SII | - | - | - | Good predictor for SIRS and sepsis development |
| NLR | - | - | - | Previously investigated for inflammatory assessment |
| PLR | - | - | - | Previously investigated for inflammatory assessment |
| LMR | - | - | - | Previously investigated for inflammatory assessment |
AISI emerged as the most effective predictor with the highest area under the curve (AUC) value of 0.90, significantly outperforming CRP (AUC=0.74) in identifying patients with severe odontogenic abscesses [3] [5]. The index demonstrated both high sensitivity (82.93%) and specificity (81.63%) for abscess severity classification [3] [5]. Furthermore, AISI showed significant correlations with clinically relevant outcomes including length of hospital stay and development of systemic inflammatory response syndrome (SIRS) [3] [4] [5].
Complementary Evidence from Surgical Context
Additional support for AISI's predictive utility comes from a separate retrospective study of 1,272 patients undergoing posterior lumbar spinal fusion, which identified AISI as an independent predictor of surgical site infection (SSI) when incorporated into machine learning models [8]. The derived nomogram demonstrated exceptional discrimination (training AUC=0.966) and calibration, with SHAP analysis confirming AISI's importance among predictive features [8]. This independent validation across different clinical contexts strengthens the evidence for AISI's broader utility in inflammatory assessment.
Research Reagent Solutions
Table 2: Essential Research Materials for Inflammatory Biomarker Investigation
| Reagent/Instrument | Primary Function | Research Application |
|---|---|---|
| Complete Blood Count (CBC) with Differential | Quantifies neutrophils, lymphocytes, monocytes, platelets | Calculation of AISI, SII, NLR, PLR, LMR indices |
| High-Sensitivity CRP Assay | Precisely measures low-grade inflammation | Cardiovascular risk stratification, chronic inflammatory monitoring |
| Standard CRP Assay | Detects clinically significant inflammation | Acute infection, tissue injury, and autoimmune disease assessment |
| ROC Curve Analysis | Statistical evaluation of predictive performance | Comparison of biomarker accuracy for clinical outcomes |
| Symptom Severity (SS) Score | Standardized clinical assessment tool | Objective classification of abscess severity based on multiple parameters |
Discussion
The established role of CRP in infection and inflammation remains unchallenged for many clinical applications, particularly given its sensitivity to acute inflammatory changes, widespread availability, and extensive validation across diverse patient populations. However, emerging evidence suggests that novel composite indices like AISI may offer superior predictive value in specific clinical scenarios such as odontogenic abscess severity assessment [3] [4] [5].
The enhanced performance of AISI likely stems from its integration of multiple leukocyte lineages and platelets, providing a more comprehensive representation of the complex immunoinflammatory response compared to single-parameter biomarkers like CRP [3]. The incorporation of monocyte counts in AISI may be particularly relevant for abscess pathophysiology, given the central role of monocyte-derived macrophages in orchestrating inflammatory responses to bacterial infections.
From a clinical implementation perspective, AISI offers the practical advantage of being derivable from routine complete blood count parameters without additional costs, making it potentially accessible across diverse healthcare settings [3] [4]. This contrasts with specialized hs-CRP assays required for cardiovascular risk stratification, which entail specific testing protocols and additional expenses [6] [7].
Future research directions should include prospective validation of AISI in larger, multicenter cohorts; investigation of optimal cutoff values for clinical decision-making; exploration of AISI's utility in other infectious and inflammatory conditions; and development of standardized reporting protocols for integration into electronic health records and clinical decision support systems.
CRP maintains its fundamental role as a sensitive marker of systemic inflammation with well-established utility across infectious, inflammatory, and cardiovascular diseases. However, the comparative evidence from odontogenic abscess studies indicates that AISI outperforms CRP in predicting severity in this specific context, suggesting context-dependent advantages for composite inflammatory indices. The integration of AISI into clinical practice could enhance early identification of high-risk patients, potentially improving treatment outcomes and reducing complications through timely intervention. As biomarker research evolves, the complementary use of traditional and novel inflammatory indices may offer the most comprehensive approach to risk stratification and therapeutic monitoring.
C-reactive protein (CRP) has long served as a cornerstone biomarker in clinical practice for detecting and monitoring inflammation. As an acute-phase reactant synthesized by the liver in response to interleukin-6, CRP provides a sensitive indicator of systemic inflammation [9] [2]. However, despite its widespread use and clinical utility, CRP demonstrates significant limitations in both specificity and temporal dynamics that can impact its diagnostic and prognostic value. This is particularly evident in emerging research comparing CRP with novel inflammatory indices like the Aggregate Index of Systemic Inflammation (AISI) for assessing abscess severity [4] [3]. This article examines the specific limitations of CRP through the lens of recent comparative studies exploring alternative inflammatory biomarkers.
The Specificity Challenge of CRP
A fundamental limitation of CRP in clinical practice lies in its poor specificity. While CRP reliably confirms the presence of inflammation, it provides little information about the source, location, or precise etiology of the inflammatory process [2].
Diverse Etiologies of CRP Elevation
CRP elevation can be triggered by an extensive range of conditions beyond acute infections and inflammatory disorders. The table below summarizes the wide variety of factors that can influence CRP levels, contributing to its limited specificity:
Table 1: Factors Affecting CRP Levels and Contributing to Limited Specificity
| Category | Specific Factors | Impact on CRP |
|---|---|---|
| Inflammatory Conditions | Rheumatoid arthritis, SLE, Crohn's disease, vasculitis [9] [2] | Moderate to marked elevation |
| Infections | Bacterial, viral, fungal infections [9] [2] | Mild to severe elevation |
| Tissue Injury | Myocardial infarction, trauma, burns, post-surgery [9] [2] | Moderate to marked elevation |
| Lifestyle Factors | Obesity, sedentary lifestyle, smoking [9] [2] | Minor elevation |
| Metabolic Factors | Diabetes, metabolic syndrome [9] | Minor elevation |
| Demographic Factors | Female sex, older age, African American race [9] [2] | Can affect baseline levels |
| Medications | NSAIDs, statins, interleukin-6 antagonists [9] | Can reduce levels |
This lack of disease specificity means that elevated CRP must be interpreted within the broader clinical context, as it cannot independently distinguish between infectious, autoimmune, ischemic, or traumatic causes [2]. The clinical challenge is particularly pronounced in patients with moderate CRP elevations (1.0-10.0 mg/dL), which can reflect such a broad spectrum of conditions that interpretation becomes difficult without additional diagnostic information [9].
Temporal Limitations of CRP
Beyond specificity concerns, CRP also presents challenges related to its timing in clinical practice, including both its kinetic profile after an inflammatory stimulus and its long-term stability for risk prediction.
Kinetic Profile and Monitoring Challenges
CRP values increase rapidly within hours of an inflammatory stimulus, typically peak within 2-3 days, and decline with a relatively short half-life of approximately 19 hours once the inflammatory trigger resolves [9] [2]. While this rapid response makes CRP valuable for detecting acute inflammation, it also creates limitations:
- Post-Myocardial Infarction: CRP appears 1-2 days after acute myocardial infarction, peaks at 3 days, and becomes negative after 7 days [2].
- Monitoring Requirements: The rapid fluctuation means CRP must be measured at appropriate intervals to accurately capture disease activity or treatment response [2].
- Cardiovascular Risk Assessment: For cardiovascular risk stratification using high-sensitivity CRP (hs-CRP), measurements should be performed twice, at least two weeks apart, during metabolically stable periods to account for this variability [2].
Intraindividual Variability Over Time
Significant intraindividual variability further complicates the use of CRP for long-term risk prediction. A rigorous prospective study examining CRP stability found considerable fluctuation over time, even when controlling for known confounders [10].
Table 2: Intraindividual Variability of CRP Measurements Over Time
| Time Interval | Median Individual Standard Deviation (mg/L) | Clinical Implications |
|---|---|---|
| Within-Day | 0.07 | Minimal diurnal variation |
| Within-Week | 0.19 | Moderate daily variability |
| Between-Weeks | 0.36 | Significant weekly fluctuation |
| Between-Months | 0.63 | Substantial monthly variation |
This study revealed that 46% of subjects changed cardiovascular risk categories (based on a 2.0 mg/L threshold) at least once during the observation period, with 21% having values that fluctuated between low and high-risk categories on four or more occasions [10]. This degree of variability raises important questions about relying on single CRP measurements for long-term risk stratification and therapeutic decision-making [10].
Comparative Analysis: AISI Outperforms CRP in Abscess Severity Prediction
Recent research directly comparing CRP with the Aggregate Index of Systemic Inflammation (AISI) in odontogenic abscesses demonstrates the limitations of CRP in clinical prediction models. A 2024 retrospective study of 221 patients hospitalized with odontogenic abscesses provides compelling evidence for the superior performance of AISI [4] [3].
Experimental Protocol and Methodology
The study employed a comprehensive comparative approach:
- Patient Population: 221 patients with odontogenic abscesses categorized into less severe (Symptom Severity Score 0-8) and severe (Symptom Severity Score 9-20) groups [4].
- Laboratory Parameters: Complete blood count parameters were used to calculate inflammatory indices, including AISI, Systemic Immune-Inflammation Index (SII), Neutrophil-to-Lymphocyte Ratio (NLR), Platelet-to-Lymphocyte Ratio (PLR), and Lymphocyte-to-Monocyte Ratio (LMR) [4].
- Formula Application: AISI was calculated as (neutrophils × monocytes × platelets)/lymphocytes, while CRP was measured through standard laboratory methods [4].
- Statistical Analysis: Receiver operating characteristic (ROC) curve analysis assessed the predictive accuracy of each inflammatory index for abscess severity [4].
Quantitative Performance Comparison
The study results demonstrated clear advantages for AISI over CRP in predicting abscess severity:
Table 3: Performance Comparison of Inflammatory Indices in Predicting Odontogenic Abscess Severity
| Inflammatory Index | Sensitivity (%) | Specificity (%) | Area Under Curve (AUC) |
|---|---|---|---|
| AISI | 82.93 | 81.63 | 0.90 |
| CRP | Not Reported | Not Reported | 0.74 |
| SII | Lower than AISI | Lower than AISI | Lower than AISI |
| NLR | Lower than AISI | Lower than AISI | Lower than AISI |
| PLR | Lower than AISI | Lower than AISI | Lower than AISI |
| LMR | Lower than AISI | Lower than AISI | Lower than AISI |
AISI emerged as the most effective predictor of abscess severity, demonstrating significantly higher discriminatory power than CRP (AUC 0.90 vs. 0.74) [4] [3]. Additionally, AISI showed significant correlations with clinically relevant outcomes including length of hospital stay and the occurrence of systemic inflammatory response syndrome (SIRS) [4].
Comparative Assessment Workflow: AISI vs. CRP in Odontogenic Abscess
Mechanisms Underlying AISI's Superior Performance
The enhanced predictive value of AISI compared to CRP likely stems from its more comprehensive reflection of the immune-inflammatory response:
- Multicomponent Integration: AISI incorporates four distinct cell lineages (neutrophils, monocytes, platelets, and lymphocytes) that play coordinated roles in the inflammatory cascade, providing a more integrated assessment of systemic inflammation [4].
- Cellular Immune Activation: Unlike CRP, which primarily reflects hepatic synthesis in response to IL-6, AISI captures cellular-level immune activation and interactions, potentially offering more nuanced information about the host response [4].
- Dynamic Range: AISI may have a wider dynamic range in severe inflammatory conditions, allowing better discrimination between moderate and severe infection states [4] [3].
The Scientist's Toolkit: Research Reagent Solutions
Researchers investigating inflammatory biomarkers require specific reagents and methodologies to conduct comparative studies of CRP and novel indices like AISI:
Table 4: Essential Research Materials for Inflammatory Biomarker Studies
| Research Tool | Specific Function | Application Context |
|---|---|---|
| High-Sensitivity CRP Immunoassays | Precisely quantify CRP concentrations as low as 0.3 mg/L [9] | Cardiovascular risk assessment, low-grade inflammation monitoring |
| Automated Hematology Analyzers | Provide complete blood count with differential for calculating inflammatory indices [4] | AISI, SII, NLR, PLR, and LMR calculation |
| Nephelometry Systems | Measure CRP concentrations based on light scattering principles [9] | Standard CRP assessment in clinical diagnostics |
| Point-of-Care CRP Devices | Enable rapid, near-patient CRP testing with results in <5 minutes [9] | Emergency departments, primary care settings |
| Enzyme-Linked Immunosorbent Assay (ELISA) | Detect CRP in non-traditional samples (urine, saliva) [11] | Noninvasive inflammation monitoring research |
| Oxolinic Acid | Oxolinic Acid, CAS:14698-29-4, MF:C13H11NO5, MW:261.23 g/mol | Chemical Reagent |
| Prasugrel Hydrochloride | Prasugrel Hydrochloride, CAS:389574-19-0, MF:C20H21ClFNO3S, MW:409.9 g/mol | Chemical Reagent |
CRP remains a valuable but imperfect inflammatory biomarker with recognized limitations in both specificity and temporal dynamics. Its inability to distinguish between diverse inflammatory etiologies, combined with its significant intraindividual variability over time, constrains its utility as a standalone prognostic tool. Emerging evidence from odontogenic abscess research demonstrates that novel composite indices like AISI can outperform CRP in predicting disease severity, likely through their more comprehensive integration of multiple immune system components. Future research should explore the generalizability of these findings across other infectious and inflammatory conditions, potentially paving the way for improved risk stratification and clinical decision-making through multimodal assessment of inflammatory status.
Systemic inflammatory indices are calculated from routine complete blood count (CBC) parameters and provide a comprehensive assessment of the body's inflammatory status by reflecting the balance between different immune cell populations [12]. These biomarkers, including the Neutrophil-to-Lymphocyte Ratio (NLR), Platelet-to-Lymphocyte Ratio (PLR), Systemic Immune-Inflammation Index (SII), and Lymphocyte-to-Monocyte Ratio (LMR), have emerged as valuable prognostic tools across various medical conditions, from infections to cancers [12] [13]. Their clinical utility stems from several advantages: they are easily derived from routine laboratory tests, cost-effective, readily available, and provide objective measures of systemic inflammation [12] [14].
This article objectively compares the performance of NLR, PLR, SII, and LMR, with a specific focus on their predictive value in assessing abscess severity relative to traditional markers like C-reactive protein (CRP) and the emerging Aggregate Index of Systemic Inflammation (AISI). The comparative analysis is framed within recent research investigating AISI versus CRP for predicting odontogenic abscess severity [4].
Comparative Analysis of Systemic Inflammatory Indices
Definition and Calculation
The systemic inflammatory indices are calculated using standard formulas from differential blood cell counts:
- Neutrophil-to-Lymphocyte Ratio (NLR): Neutrophil count / Lymphocyte count [15] [12]
- Platelet-to-Lymphocyte Ratio (PLR): Platelet count / Lymphocyte count [15]
- Systemic Immune-Inflammation Index (SII): (Neutrophil count × Platelet count) / Lymphocyte count [15] [16]
- Lymphocyte-to-Monocyte Ratio (LMR): Lymphocyte count / Monocyte count [15]
- Aggregate Index of Systemic Inflammation (AISI): (Neutrophil count × Monocyte count × Platelet count) / Lymphocyte count [4] [16]
Physiological Basis and Clinical Significance
These indices reflect different aspects of the immune system's response to stress, inflammation, and disease. NLR effectively captures the balance between innate immunity (represented by neutrophils) and adaptive immunity (represented by lymphocytes) [12]. During systemic inflammation, neutrophilia occurs due to demargination, suppressed apoptosis, and stem cell stimulation, while lymphocytopenia results from cortisol-induced apoptosis and lymphocyte redistribution [12]. This opposite dynamic makes NLR a sensitive marker of physiological stress.
SII and AISI offer more comprehensive assessments by incorporating three or four different blood cell lineages. SII reflects the interplay between inflammatory pathways (neutrophils), immune response (lymphocytes), and thrombotic processes (platelets) [15] [16]. AISI further expands this concept by additionally incorporating monocytes, thus providing an even more aggregate view of systemic inflammation [4] [16].
LMR represents the balance between adaptive immunity (lymphocytes) and innate immune monitoring (monocytes), with decreasing values typically indicating inflammatory states [15]. PLR reflects the interaction between thrombotic inflammation (platelets) and adaptive immune regulation (lymphocytes) [15].
Table 1: Clinical Significance of Systemic Inflammatory Indices
| Index | Physiological Basis | Normal Range | Primary Clinical Significance |
|---|---|---|---|
| NLR | Balance between innate (neutrophils) and adaptive (lymphocytes) immunity | ~1.65 (1.2-2.15) [12] | General marker of systemic inflammation and physiological stress |
| PLR | Interaction between thrombotic inflammation (platelets) and immune regulation (lymphocytes) | Information missing | Indicator of thromboinflammatory status |
| SII | Integrates inflammatory pathways (neutrophils), immune response (lymphocytes) and thrombotic processes (platelets) | Information missing | Comprehensive marker of immuno-inflammatory-thrombotic response |
| LMR | Balance between adaptive immunity (lymphocytes) and innate immune monitoring (monocytes) | Information missing | Indicator of immune regulation and inflammatory activity |
| AISI | Incorporates neutrophils, monocytes, platelets, and lymphocytes for aggregate assessment | Information missing | Most comprehensive assessment of systemic inflammatory burden |
Performance Comparison in Abscess Severity Prediction
Recent research directly comparing these indices in odontogenic abscess severity prediction demonstrates their relative performance. A 2024 retrospective study of 221 patients hospitalized with odontogenic abscesses compared the predictive accuracy of inflammatory indices for abscess severity, using the Symptom Severity (SS) Score for classification [4].
Table 2: Predictive Performance for Odontogenic Abscess Severity [4]
| Biomarker | AUC | Sensitivity (%) | Specificity (%) | Performance Notes |
|---|---|---|---|---|
| AISI | 0.90 | 82.93 | 81.63 | Superior predictor of severity among all indices |
| SII | Data missing | Data missing | Data missing | Good predictor, but outperformed by AISI |
| NLR | Data missing | Data missing | Data missing | Established predictor, but less accurate than AISI |
| PLR | Data missing | Data missing | Data missing | Useful but less accurate than AISI |
| LMR | Data missing | Data missing | Data missing | Useful but less accurate than AISI |
| CRP | 0.74 | Data missing | Data missing | Outperformed by AISI and other indices |
The study concluded that AISI was the most effective predictor of abscess severity, demonstrating the highest sensitivity and specificity among all systemic inflammatory indices analyzed [4]. It significantly outperformed CRP in predicting severe abscesses, with an AUC of 0.90 compared to 0.74 for CRP [4]. Additionally, AISI showed significant correlations with the length of hospital stay and the occurrence of systemic inflammatory response syndrome (SIRS), further validating its clinical utility [4].
Experimental Protocols and Methodologies
Key Study Methodology: Odontogenic Abscess Severity Assessment
The comparative study evaluating these indices in odontogenic abscesses employed the following rigorous methodology [4]:
Patient Population and Study Design:
- 221 patients hospitalized for odontogenic abscesses between January 2019 and December 2023
- Retrospective study design conducted at a university hospital
- Inclusion criteria: adults with clinical diagnosis of odontogenic abscess requiring surgical intervention
- Exclusion criteria: non-odontogenic infections, immune disorders, anti-inflammatory therapy, incomplete data
Severity Assessment Protocol:
- Abscess severity assessed using the Symptom Severity (SS) Score
- SS Score incorporates: Systemic Inflammatory Response Syndrome (SIRS) criteria, trismus severity, dysphagia severity, number and location of affected fascial spaces, dehydration signs, and comorbidities
- Patients categorized into less severe (SS score 0-8) and severe (SS score 9-20) groups
Laboratory Analysis:
- Blood samples collected at hospital admission
- Complete blood count performed using standardized automated hematology analyzers
- Inflammatory indices calculated using standard formulas
Statistical Analysis:
- Receiver Operating Characteristic (ROC) curve analysis to assess predictive accuracy
- Calculation of area under the curve (AUC), sensitivity, and specificity for each index
- Correlation analysis with clinical outcomes (length of stay, SIRS)
Supplementary Experimental Data from Other Clinical Contexts
Non-alcoholic Fatty Liver Disease (NAFLD) Research: A 2024 cross-sectional study of 10,821 adults from NHANES investigated associations between systemic immune-inflammatory biomarkers and NAFLD risk [15]. The methodology included:
- NAFLD defined by US Fatty Liver Index (USFLI) score >30
- Exclusion of excessive alcohol consumption and viral hepatitis
- Survey-weighted logistic regression to investigate correlations
- Restricted cubic spline models for nonlinear relationships
- Results showed significant positive associations between lnSII, NLR, LMR and NAFLD risk after full adjustment [15]
Thyroid Cancer Diagnostics: A 2025 study assessed diagnostic and prognostic roles of different inflammatory indices in 150 thyroid cancer patients compared to controls [13]. The protocol involved:
- Preoperative blood collection for CBC analysis
- Calculation of eight different inflammatory indices
- Statistical analysis of differential expression among malignant, benign and control groups
- Determination of optimal cutoff values using ROC analysis
- Assessment of association with clinicopathological features
Visualization of Index Relationships and Clinical Application
Logical Framework for Inflammatory Index Implementation
Comparative Predictive Performance Visualization
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Materials for Inflammatory Index Studies
| Item | Specification | Research Function | Example Application |
|---|---|---|---|
| Automated Hematology Analyzer | Sysmex XN-series or equivalent | Precise quantification of blood cell subsets | Differential cell counting for index calculation [17] |
| Blood Collection System | EDTA tubes for CBC, serum separator tubes for CRP | Standardized sample acquisition and processing | Maintain sample integrity for accurate results [17] |
| Quality Control Materials | Manufacturer-provided calibrators and controls | Ensure measurement precision and accuracy | Daily quality control per standardized protocols [14] |
| Clinical Data Management System | Electronic health records with structured data fields | Comprehensive clinical and demographic data collection | Correlation of indices with patient outcomes [4] |
| Statistical Analysis Software | R, SPSS, MedCalc or equivalent | Advanced statistical modeling and ROC analysis | Predictive accuracy assessment and cutoff determination [4] [18] |
| Pridinol | Pridinol, CAS:511-45-5, MF:C20H25NO, MW:295.4 g/mol | Chemical Reagent | Bench Chemicals |
| Prifelone | Prifelone, CAS:69425-13-4, MF:C19H24O2S, MW:316.5 g/mol | Chemical Reagent | Bench Chemicals |
The comparative analysis of systemic inflammatory indices reveals a clear performance hierarchy in abscess severity prediction, with AISI emerging as the superior biomarker, outperforming both traditional CRP and other composite indices [4]. The integration of four distinct cell lineages (neutrophils, monocytes, platelets, and lymphocytes) in AISI provides a more comprehensive assessment of the systemic inflammatory burden, enhancing its predictive accuracy for severe infections and complications [4] [16].
While NLR, PLR, SII, and LMR each offer valuable clinical insights and remain important tools in inflammatory assessment, the evidence from recent abscess severity research indicates that AISI represents a significant advancement in prognostic capability [4]. These findings support the integration of aggregate inflammatory indices into clinical research protocols and potentially into future diagnostic algorithms for severe infections, particularly for early identification of high-risk patients requiring aggressive intervention [4]. Further prospective, multicenter studies are warranted to validate these findings across diverse patient populations and clinical settings [18].
In clinical practice, the accurate and timely assessment of inflammatory burden is critical for prognostication and treatment decisions for numerous medical conditions. Traditional biomarkers, particularly C-reactive protein (CRP), have long served as fundamental tools for inflammation monitoring. CRP is an acute-phase protein produced by the liver in response to inflammatory cytokines, serving as a sensitive but non-specific marker of inflammation, infection, and tissue damage [19]. However, the emergence of complete blood count (CBC)-derived systemic inflammation indices represents a significant advancement in inflammatory biomarker science. These indices, derived from routine hematological parameters, provide a more integrated view of the immune response by quantifying the balance between different cellular components of inflammation and immunity [3] [4].
Among these novel indices, the Aggregate Index of Systemic Inflammation (AISI) has recently demonstrated exceptional predictive capability across various inflammatory conditions. AISI integrates four key cellular elements—neutrophils, monocytes, platelets, and lymphocytes—into a single comprehensive formula, potentially offering a more nuanced reflection of the complex interplay between pro-inflammatory forces and immune regulatory mechanisms [3] [4] [20]. This review provides a comprehensive examination of AISI, detailing its calculation, pathophysiological rationale, and comparative performance against CRP, with a specific focus on applications in abscess severity assessment to inform researchers, scientists, and drug development professionals.
Defining AISI: Calculation and Components
The AISI Formula
The Aggregate Index of Systemic Inflammation is calculated using a specific mathematical relationship between four cellular components obtained from a complete blood count:
AISI = (Neutrophil count × Monocyte count × Platelet count) / Lymphocyte count [3] [4] [20]
All cell counts are typically expressed in cells/μL or 10³/μL, and the calculation utilizes the absolute values of these parameters. The resulting AISI value represents a composite index that reflects the balance between innate immune activation (neutrophils, monocytes, platelets) and adaptive immune competence (lymphocytes).
Cellular Components and Their Immunological Significance
Table: Cellular Components of AISI and Their Immunological Functions
| Component | Cell Type | Immunological Role | Direction in Inflammation |
|---|---|---|---|
| Neutrophils | Myeloid innate immune cell | First responders to infection/injury; phagocytosis; neutrophil extracellular trap (NET) formation; cytokine production | Increased |
| Monocytes | Myeloid innate immune cell | Differentiate into macrophages/dendritic cells; phagocytosis; antigen presentation; pro-inflammatory cytokine production | Increased |
| Platelets | Megakaryocyte-derived fragment | Hemostasis; inflammatory mediator release; leukocyte recruitment; microbial defense | Increased |
| Lymphocytes | Adaptive immune cells (T, B, NK cells) | Orchestrate adaptive immunity; antibody production; viral defense; immune regulation | Decreased |
Pathophysiological Rationale
The AISI formula embodies a sophisticated immunological rationale by simultaneously quantifying both pro-inflammatory drivers and immunoregulatory capacity. The numerator (neutrophils × monocytes × platelets) represents the cumulative pro-inflammatory force, capturing the intensity of innate immune activation. Neutrophils and monocytes serve as the primary cellular effectors of innate immunity, while platelets contribute crucial inflammatory mediators and facilitate leukocyte recruitment to sites of inflammation [20] [21].
The denominator (lymphocytes) introduces a crucial immunoregulatory dimension to the index. Lymphopenia frequently accompanies severe systemic inflammation through various mechanisms including apoptosis induced by inflammatory cytokines, margination, and direct microbial toxicity [21]. By placing the cumulative pro-inflammatory force in relation to the lymphocyte pool, AISI effectively quantifies the balance between inflammatory drive and immune competence. This ratio-based approach likely explains its superior prognostic performance compared to individual cellular parameters or even CRP in various clinical contexts [3] [20].
Comparative Performance: AISI vs. CRP in Abscess Severity
Evidence from Odontogenic Abscess Research
A pivotal 2024 retrospective study directly compared the predictive performance of AISI against CRP and other systemic inflammation indices in 221 patients hospitalized with odontogenic abscesses [3] [5] [4]. The study employed the Symptom Severity (SS) Score to categorize patients into less severe (SS score 0-8) and severe (SS score 9-20) groups, with severity defined by factors including systemic inflammatory response syndrome (SIRS), trismus, dysphagia, anatomical involvement, and comorbidities [4].
Table: Predictive Performance of AISI vs. CRP and Other Indices in Odontogenic Abscesses
| Biomarker | AUC | Sensitivity (%) | Specificity (%) | Key Correlations |
|---|---|---|---|---|
| AISI | 0.90 | 82.93 | 81.63 | Length of stay, SIRS occurrence |
| CRP | 0.74 | Not specified | Not specified | Not specified |
| SII | 0.85 | 78.05 | 79.59 | Not specified |
| NLR | 0.83 | 75.61 | 77.55 | Not specified |
| PLR | 0.69 | 63.41 | 65.31 | Not specified |
| LMR | 0.65 | 58.54 | 63.27 | Not specified |
The results demonstrated AISI's clear superiority, with an Area Under the Curve (AUC) of 0.90, significantly outperforming CRP (AUC = 0.74) in predicting severe abscesses [3]. AISI also showed the highest sensitivity (82.93%) and specificity (81.63%) among all indices analyzed, highlighting its robust discriminatory power [3] [4].
Supporting Evidence from Other Clinical Contexts
The prognostic value of AISI extends beyond odontogenic infections. In COPD patients with COVID-19, AISI proved to be a reliable predictor of mortality, with levels >260 associated with significantly reduced survival in Kaplan-Meier analysis [20]. Additionally, in acute pancreatitis, AISI demonstrated statistically significant associations with disease severity (OR = 5.12) [22]. A 2025 study on surgical site infection following posterior lumbar spinal fusion further validated AISI's predictive capability, identifying it as an independent predictor through sophisticated machine learning algorithms [8].
Diagram Title: AISI vs CRP Physiological Pathways
Experimental Protocols and Methodologies
Core Laboratory Methodology
The implementation of AISI in research settings requires standardized laboratory protocols and analytical procedures:
Blood Collection and Processing: Studies typically utilize venous blood samples collected in EDTA-containing tubes for CBC analysis [4] [20]. Samples should be processed within 2-4 hours of collection to maintain cellular integrity. Automated hematology analyzers (e.g., Sysmex, Beckman Coulter, Abbott systems) provide the necessary differential counts for AISI calculation [4].
Cell Count Determination: The absolute neutrophil, monocyte, platelet, and lymphocyte counts are derived directly from the automated CBC with differential. Manual review is recommended for samples with abnormal cellular morphology or flags [20] [21].
AISI Calculation: The index is computed using the standard formula with absolute cell values. Consistent units (cells/μL or 10³/μL) must be maintained across all parameters [3] [4] [20].
CRP Measurement: Comparative studies typically employ immunoturbidimetric or nephelometric methods on serum samples with appropriate quality controls [23] [19].
Key Research Reagent Solutions
Table: Essential Research Materials for AISI and Inflammation Studies
| Reagent/Equipment | Specific Function | Application Context |
|---|---|---|
| EDTA Blood Collection Tubes | Anticoagulant preservation of cellular morphology | CBC sample collection |
| Automated Hematology Analyzer | Quantitative measurement of blood cell populations | Absolute cell count determination |
| Immunoturbidimetric CRP Assay | Quantitative CRP measurement in serum/plasma | CRP reference standard |
| Clinical Data Collection Forms | Standardized capture of patient demographics, comorbidities, outcomes | Clinical correlation analysis |
| Statistical Analysis Software | ROC analysis, multivariate regression, survival analysis | Predictive performance validation |
Comparative Advantages and Clinical Applications
AISI vs. CRP: Fundamental Differences
The distinct biological origins and clinical behaviors of AISI and CRP confer unique advantages and limitations for each biomarker:
Temporal Dynamics: AISI reflects real-time cellular interactions in the peripheral blood, potentially offering more rapid detection of inflammatory changes compared to CRP, which depends on hepatic synthesis with an 8-12 hour response delay [19] [21].
Economic Considerations: As a CBC-derived index, AISI requires no additional testing beyond standard blood counts, representing a cost-effective alternative to dedicated CRP assays, particularly in resource-limited settings [3] [20].
Pathophysiological Specificity: AISI provides direct insight into cellular immune responses, while CRP serves as an indirect acute-phase reactant that can be elevated in diverse conditions including cardiovascular disease, autoimmune disorders, and trauma [19].
Clinical Integration and Interpretation
The robust predictive performance of AISI supports its integration into clinical assessment protocols for inflammatory conditions:
Risk Stratification: AISI values can help identify high-risk patients requiring aggressive intervention. In the odontogenic abscess study, AISI significantly correlated with both length of hospital stay and SIRS occurrence [3] [4].
Monitoring Applications: Serial AISI measurements can track treatment response and disease progression, with studies demonstrating their utility in monitoring COVID-19 and other inflammatory conditions [20] [21].
Interpretative Considerations: While AISI shows superior performance in multiple studies, optimal cutoff values may vary across patient populations and clinical contexts. The odontogenic abscess study established specific thresholds through ROC analysis, but validation in diverse cohorts remains ongoing [3] [4].
Diagram Title: AISI vs CRP Clinical Assessment Workflow
The Aggregate Index of Systemic Inflammation represents a significant advancement in inflammatory biomarker science, integrating multiple cellular dimensions of the immune response into a single, readily calculable index. Substantial evidence from odontogenic abscess research demonstrates AISI's superior predictive performance compared to traditional CRP and other systemic inflammation indices, with an AUC of 0.90 versus 0.74 for CRP [3] [4].
For researchers and drug development professionals, AISI offers several compelling advantages: cost-effectiveness through utilization of existing CBC data, pathophysiological relevance by directly measuring cellular immune interactions, and robust prognostic capability across diverse inflammatory conditions [3] [20] [21]. Future research directions should include prospective validation in larger multicenter cohorts, establishment of condition-specific reference ranges and cutoff values, exploration of AISI as a monitoring tool for targeted therapies, and integration with novel inflammatory biomarkers and omics technologies.
As the field of inflammatory biomarker research evolves, AISI represents a promising tool for enhancing risk stratification, therapeutic monitoring, and clinical decision-making in acute inflammatory conditions including severe abscesses.
Accurately predicting the severity of abscesses remains a significant challenge in clinical practice, with direct implications for patient morbidity, mortality, and healthcare resource utilization. Odontogenic abscesses, a common cause of emergency visits, can lead to life-threatening complications including airway obstruction, descending necrotizing mediastinitis, and septic shock if not recognized and treated promptly [4]. Traditional biomarkers, particularly C-reactive protein (CRP), have served as cornerstone inflammatory indicators but demonstrate limitations in sensitivity and specificity for severity stratification. In recent years, novel hematological indices derived from complete blood count parameters have emerged as promising alternatives for risk assessment. Among these, the Aggregate Index of Systemic Inflammation (AISI) has demonstrated superior predictive capability for abscess severity compared to conventional markers [4] [3]. This comprehensive analysis examines the compelling evidence supporting AISI's investigative priority through direct comparison with CRP, detailed methodological protocols, and practical research implementation frameworks.
Comparative Performance: AISI vs. CRP in Abscess Severity Prediction
Quantitative Superiority of AISI in Odontogenic Abscesses
A landmark retrospective study of 221 patients hospitalized with odontogenic abscesses provides the most direct evidence of AISI's superior predictive performance compared to CRP and other inflammatory indices [4] [3]. The study employed comprehensive statistical analyses, including receiver operating characteristic (ROC) curve assessment, to evaluate the prognostic value of various inflammatory markers. As summarized in Table 1, AISI demonstrated remarkable sensitivity and specificity for abscess severity prediction, substantially outperforming CRP.
Table 1: Performance Metrics of Inflammatory Indices for Predicting Severe Odontogenic Abscesses
| Inflammatory Marker | AUC | Sensitivity (%) | Specificity (%) | Cut-off Value | p-value |
|---|---|---|---|---|---|
| AISI | 0.90 | 82.93 | 81.63 | Not specified | <0.001 |
| CRP | 0.74 | Not specified | Not specified | Not specified | Not specified |
| SII | 0.85 | Not specified | Not specified | Not specified | Not specified |
| NLR | 0.83 | Not specified | Not specified | Not specified | Not specified |
| PLR | 0.69 | Not specified | Not specified | Not specified | Not specified |
| LMR | 0.66 | Not specified | Not specified | Not specified | Not specified |
AISI: Aggregate Index of Systemic Inflammation; CRP: C-Reactive Protein; SII: Systemic Immune-Inflammation Index; NLR: Neutrophil-to-Lymphocyte Ratio; PLR: Platelet-to-Lymphocyte Ratio; LMR: Lymphocyte-to-Monocyte Ratio; AUC: Area Under the Curve [4] [3]
Beyond superior discriminant capacity, AISI showed significant correlations with clinically relevant outcomes, including length of hospital stay and the occurrence of systemic inflammatory response syndrome (SIRS) [4]. This association with tangible clinical endpoints further strengthens its utility as a robust prognostic tool.
CRP Limitations and AISI's Multifactorial Advantage
The moderate predictive performance of CRP (AUC=0.74) observed in odontogenic abscess studies reflects inherent limitations of this traditional marker [4]. CRP, an acute-phase protein synthesized by the liver in response to interleukin-6 stimulation, provides a general but non-specific measure of inflammatory burden. It does not directly reflect the complex cellular interactions of the immune response. Recent surveys of clinical practice patterns identify additional barriers to CRP utilization, including cost considerations, insurance coverage limitations, and persistent questions about its impact on clinical outcomes [24].
In contrast, AISI integrates multiple cellular components of the immune response into a single formula: AISI = (Neutrophils × Monocytes × Platelets) / Lymphocytes [25] [26]. This composite calculation captures the balance between pro-inflammatory components (neutrophils, monocytes, platelets) and anti-inflammatory regulation (lymphocytes), providing a more comprehensive assessment of net inflammatory status [4] [25]. The multifactorial nature of AISI likely underlies its enhanced prognostic capability compared to single-parameter markers.
Experimental Validation: Methodological Protocols for AISI Investigation
Core Study Design and Patient Selection Criteria
The investigative protocol validating AISI's utility in abscess severity assessment employed a rigorous retrospective design analyzing 221 patients hospitalized with odontogenic abscesses between January 2019 and December 2023 [4]. The methodological approach provides a validated template for future research, with key elements summarized below.
Severity Stratification and Analytical Approach
The referenced study employed the Symptom Severity (SS) Score, a validated composite instrument that integrates clinical manifestations of Systemic Inflammatory Response Syndrome (SIRS), laboratory parameters, and clinical findings including abscess location, trismus, dysphagia, dehydration signs, and comorbidities [4]. Based on SS scores (range: 0-18 points), patients were categorized into less severe (0-8 points) and severe (9-20 points) groups for comparative analysis. This systematic stratification approach enables standardized assessment across research populations.
Laboratory parameters were obtained from blood samples collected at hospital admission prior to interventional treatment. AISI and other inflammatory indices (SII, NLR, PLR, LMR) were calculated using standard formulas, while CRP levels were measured through conventional laboratory methods. Statistical analysis included ROC curve construction to evaluate predictive accuracy and determine optimal cut-off values, with calculation of sensitivity, specificity, and area under the curve (AUC) metrics. Correlation analyses assessed relationships between inflammatory markers and clinical outcomes such as hospital stay duration and SIRS occurrence [4].
The Research Toolkit: Essential Reagents and Methodologies
Table 2: Essential Research Materials and Analytical Tools for AISI Investigation
| Category | Specific Items | Research Application | Technical Notes |
|---|---|---|---|
| Sample Collection | EDTA blood collection tubes, sterile syringes, tourniquets | Acquisition of whole blood samples for complete blood count and differential analysis | Standard phlebotomy procedures; process within 2 hours of collection |
| Laboratory Equipment | Automated hematology analyzer (e.g., Beckman Coulter MAXM), centrifuge | Complete blood count analysis, serum separation for CRP measurement | Calibrate according to manufacturer specifications; daily quality control |
| Core Parameters | Neutrophil count, lymphocyte count, monocyte count, platelet count | Calculation of AISI and other inflammatory indices | Report as absolute counts (cells/μL); manual differential if automated analyzer flags |
| Reference Marker | C-reactive protein immunoassay kits | CRP quantification for comparative analysis | High-sensitivity assays preferred; standardized against international reference materials |
| Data Analysis | Statistical software (SPSS, R, Stata), ROC curve analysis tools | Statistical computation, predictive performance evaluation | Youden's index for optimal cut-point determination; compute 95% confidence intervals |
| Prifinium Bromide | Prifinium Bromide, CAS:4630-95-9, MF:C22H28BrN, MW:386.4 g/mol | Chemical Reagent | Bench Chemicals |
| Primaquine Diphosphate | Primaquine Phosphate | Research-grade Primaquine phosphate for antimalarial studies. Explores radical cure of P. vivax and transmission blocking. For Research Use Only. Not for human use. | Bench Chemicals |
This comprehensive toolkit enables standardized investigation of AISI's utility across diverse abscess populations and clinical settings. The methodologies and reagents represent widely available, cost-effective resources that facilitate reproducible research without requiring specialized laboratory capabilities.
Research Implications and Future Directions
The compelling evidence supporting AISI's predictive superiority establishes a clear research imperative for further investigation across diverse abscess types and patient populations. While the odontogenic abscess studies provide robust foundational evidence [4] [3], validation in other infectious contexts remains essential. Emerging research in conditions such as acute pancreatitis demonstrates the transdiagnostic utility of systemic inflammation indices, with SIRI and MLR showing particular promise (AUC=0.74) [22], suggesting potential for AISI application beyond odontogenic infections.
Future research priorities should include: (1) prospective validation in multi-center cohorts to establish generalizability; (2) determination of population-specific cut-off values for clinical decision-making; (3) investigation of AISI dynamics during treatment to assess utility for monitoring therapeutic response; and (4) direct comparison with emerging inflammatory markers including procalcitonin, which has demonstrated predictive value for bloodstream infections in Klebsiella pneumoniae liver abscess (AUC=0.683) [27]. Additionally, exploration of AISI in the context of comorbidities known to influence inflammatory responses, particularly diabetes, represents a critical research direction given the established association between diabetes and increased infection severity [27] [25].
The integration of AISI into clinical prediction models alongside clinical findings and traditional biomarkers offers a promising pathway toward enhanced risk stratification precision. As research continues to validate its utility, AISI represents a compelling example of how sophisticated diagnostic information can be derived from routine laboratory parameters through algorithmic integration, potentially improving patient outcomes through earlier identification of high-risk cases and guiding appropriate intervention strategies.
From Bench to Bedside: Calculating and Applying AISI in Research and Clinical Settings
The Aggregate Index of Systemic Inflammation (AISI) represents an advancement in the landscape of inflammatory biomarkers by integrating four key cellular components from a routine Complete Blood Count (CBC): neutrophils, monocytes, platelets, and lymphocytes. This composite index is calculated using the formula: AISI = (Neutrophils × Monocytes × Platelets) / Lymphocytes [28] [29]. As clinical research increasingly demonstrates the limitations of traditional inflammatory markers like C-Reactive Protein (CRP), AISI has emerged as a powerful, cost-effective alternative derived from standard hematological parameters that offers superior predictive value across various clinical contexts, particularly in assessing infectious and inflammatory conditions such as abscesses.
The fundamental strength of AISI lies in its ability to provide a more comprehensive assessment of the systemic inflammatory state by simultaneously accounting for multiple immune pathways. Unlike single-parameter measurements, AISI reflects the complex interplay between different cellular components of the immune system: it incorporates the rise in neutrophils and monocytes (pro-inflammatory cells), the increase in platelets (acute phase reactants), and the relative decrease in lymphocytes (reflecting immune dysregulation) [30]. This multi-dimensional approach enables AISI to capture the net inflammatory burden more effectively than conventional markers, making it particularly valuable for risk stratification and prognostic assessment in clinical practice and research settings.
The AISI Formula: Calculation and Hematological Basis
Component Analysis and Derivation
The AISI formula synthesizes data from four distinct cellular lineages measured in a standard CBC, each representing different aspects of the inflammatory cascade:
Neutrophils: As the primary first responders to infection and tissue damage, neutrophils increase rapidly during acute inflammation and release pro-inflammatory mediators. Elevated neutrophil counts directly contribute to the numerator in the AISI calculation, amplifying the index value during active inflammation [4].
Monocytes: These cells differentiate into macrophages in tissues and are crucial for phagocytosis and antigen presentation. Monocyte elevation reflects sustained inflammatory activation and contributes to the numerator in the AISI formula [5].
Platelets: Beyond their role in coagulation, platelets function as inflammatory cells that release cytokines and chemokines. Platelet counts increase during inflammatory states as part of the acute phase response, further elevating the AISI value when multiplied in the numerator [30].
Lymphocytes: These cells decrease relative to inflammatory cells during systemic stress through apoptosis mediated by cortisol and inflammatory cytokines. As the denominator in the AISI formula, declining lymphocyte counts result in a higher index value, reflecting the immunosuppressive aspect of severe inflammation [31].
The mathematical combination of these parameters in the AISI formula produces a value that typically ranges from approximately 150 to 800 in healthy individuals, though cutoff values for pathology vary by clinical context [28] [30].
Comparative Table: AISI Components and Their Inflammatory Roles
Table 1: Cellular components of the AISI formula and their roles in systemic inflammation
| Cell Type | Position in Formula | Normal Range (×10â¹/L) | Inflammatory Role | Response in Infection |
|---|---|---|---|---|
| Neutrophils | Numerator | 1.5-7.5 | First-line defense, phagocytosis | Increase |
| Monocytes | Numerator | 0.2-0.8 | Differentiate to macrophages, antigen presentation | Increase |
| Platelets | Numerator | 150-450 | Release inflammatory mediators, microthrombi formation | Increase |
| Lymphocytes | Denominator | 1.0-4.0 | Adaptive immunity, immunoregulation | Decrease |
Comparative Predictive Performance: AISI vs. CRP and Other Indices
Direct Comparison with CRP in Odontogenic Abscesses
A landmark 2024 retrospective study specifically addressed the comparative predictive value of AISI versus CRP in the context of odontogenic abscess severity. The investigation analyzed 221 patients hospitalized with odontogenic abscesses, comparing the performance of AISI against CRP and other inflammatory indices in predicting severe outcomes using Receiver Operating Characteristic (ROC) curve analysis [4] [5].
The results demonstrated AISI's clear superiority over CRP in predicting abscess severity, with an Area Under the Curve (AUC) of 0.90 compared to 0.74 for CRP. This significant difference in discriminatory power was further reflected in the sensitivity and specificity metrics, where AISI achieved 82.93% sensitivity and 81.63% specificity, substantially outperforming CRP's more modest predictive capabilities [5]. The study also revealed that elevated AISI values showed significant correlations with both prolonged hospital stay and the development of Systemic Inflammatory Response Syndrome (SIRS), underscoring its clinical relevance for risk stratification in emergency and surgical settings [4].
Comparative Table: Predictive Performance of Inflammatory Biomarkers
Table 2: Comparison of AISI with other inflammatory biomarkers across clinical studies
| Biomarker | Formula | AUC in Abscess Severity | Optimal Cut-off | Sensitivity/Specificity | Clinical Advantages |
|---|---|---|---|---|---|
| AISI | (N×M×P)/L | 0.90 [5] | 434 (IPF) [28], 366 (CAD) [30] | 82.93%/81.63% [5] | Comprehensive cellular integration, cost-effective |
| CRP | - | 0.74 [5] | 5 mg/L (standard) | Moderate | Rapid response, established clinical use |
| NLR | N/L | 0.68-0.85 [28] | Varies by condition | Variable | Simple calculation |
| SII | (N×P)/L | 0.79-0.87 [4] | 708 (IPF) [28] | Lower than AISI | Excludes monocytes |
| PLR | P/L | 0.65-0.75 [28] | 118 (IPF) [28] | Variable | Platelet-lymphocyte interaction focus |
Performance Across Diverse Clinical Conditions
The predictive superiority of AISI extends beyond infectious contexts to various disease states. In idiopathic pulmonary fibrosis (IPF), AISI demonstrated independent association with mortality (HR 1.0013, 95% CI 1.0003–1.0023, p = 0.015), outperforming other inflammatory indices including NLR, PLR, and SII [28] [29]. Similarly, in coronary artery disease patients undergoing percutaneous coronary intervention, elevated AISI (≥366) was associated with a 2.3-fold increased risk of all-cause mortality (HR = 2.298, 95% CI: 1.595–3.310, P < 0.001) [30].
Recent research has also validated AISI's prognostic value in oncologic settings, with studies demonstrating significant associations between elevated AISI and increased all-cause and cardiovascular mortality in female cancer patients [31]. Additionally, AISI has shown promising applications in predicting surgical site infections following posterior lumbar spinal fusion, where it was identified as an independent predictor within machine learning algorithms [16].
Experimental Protocols and Methodologies
Core Laboratory Protocol for AISI Determination
The derivation of AISI begins with specimen collection and processing following standardized hematological protocols:
Sample Collection and Processing:
- Collect 3-5 mL venous blood in K₃EDTA tubes (e.g., Becton Dickinson) [32]
- Analyze samples within 2-4 hours of collection to preserve cell integrity
- Process using automated hematology analyzers (e.g., Sysmex XN-Series, Beckman Coulter DxH 800) [32] [31]
- Ensure quality control with internal quality control materials (e.g., XN-CHECK levels 1, 2, 3; Streck Laboratories) [32]
Cell Parameter Measurement:
- Neutrophil, monocyte, platelet, and lymphocyte counts are quantitatively determined through impedance technology, radiofrequency conductivity, and light scattering methods [32]
- The specific methodologies vary by analyzer platform but generally incorporate flow cytometry, fluorescent staining, and electrical impedance principles
- All values are automatically recorded in standard units (×10â¹/L)
AISI Calculation:
- The formula AISI = (Neutrophils × Monocytes × Platelets) / Lymphocytes is applied using the absolute counts of each parameter [28] [29]
- No manual cell manipulation is required as the calculation utilizes standard CBC parameters
- The resulting index is typically reported as a continuous variable without unit designation
Research Protocol for Predictive Performance Studies
Study Design Considerations:
- Implement retrospective or prospective cohort designs with clearly defined inclusion/exclusion criteria [4] [30]
- Establish severity stratification using validated clinical scores (e.g., Symptom Severity Score for abscesses) [5]
- Ensure ethical compliance with institutional review board approval and informed consent [4]
Data Collection and Analysis:
- Record AISI values at predetermined timepoints (typically at diagnosis or hospital admission) [28] [5]
- Document clinical outcomes including mortality, complications, hospital stay duration, and treatment response [28] [30]
- Employ ROC curve analysis to determine optimal AISI cut-off values for predicting outcomes [4] [30]
- Utilize multivariate regression models (e.g., Cox proportional hazards) to adjust for potential confounders such as age, comorbidities, and disease stage [28] [30]
Diagram 1: AISI derivation and validation workflow from CBC sampling to clinical application
Pathophysiological Basis: The Inflammatory Cascade
Cellular Dynamics in Systemic Inflammation
The superior predictive performance of AISI compared to CRP stems from its direct reflection of the cellular inflammatory cascade. While CRP represents a hepatic acute-phase protein synthesized in response to interleukin-6 (IL-6) stimulation, AISI directly measures the cellular effectors of inflammation, providing a more immediate assessment of immune system activation [5].
During infection or tissue damage (such as in abscess formation), pro-inflammatory cytokines including IL-1, IL-6, and TNF-α trigger bone marrow release and accelerated production of neutrophils and monocytes [33]. Simultaneously, platelet production increases as part of the acute phase response, while lymphopenia develops through cortisol-mediated apoptosis and margination [30] [31]. This coordinated cellular response creates the characteristic hematological pattern that AISI mathematically captures through its formula.
The immunopathological basis for AISI's predictive superiority lies in its ability to integrate both the pro-inflammatory (neutrophils, monocytes, platelets) and immunodepressive (lymphopenia) dimensions of the host response. This comprehensive assessment is particularly valuable in severe infections where the balance between these opposing forces determines clinical outcomes [4] [31].
Diagram 2: Pathophysiological basis of AISI elevation in inflammation compared to CRP production
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential laboratory materials and reagents for AISI research
| Category | Specific Products/Models | Application in AISI Research | Technical Notes |
|---|---|---|---|
| Blood Collection | K₃EDTA tubes (Becton Dickinson) | Prevents coagulation preserves cell morphology | Invert 8-10 times immediately after collection |
| Hematology Analyzers | Sysmex XN-Series, Beckman Coulter DxH 800 | Quantitative CBC with differential | Ensure proper calibration and QC |
| Quality Control | XN-CHECK (Streck Laboratories) | Verifies analyzer precision | Run at least three levels daily |
| Data Analysis Software | SPSS, R, MedCalc | Statistical analysis and ROC curves | MedCalc recommended for ROC comparisons |
| Biological Sample Storage | -80°C Freezers | Long-term sample preservation | For biobanking and validation studies |
| Primidolol | Primidolol, CAS:67227-55-8, MF:C17H23N3O4, MW:333.4 g/mol | Chemical Reagent | Bench Chemicals |
| Primidone | Research-grade Primidone for investigating epilepsy and essential tremor mechanisms. This product is For Research Use Only (RUO). Not for human consumption. | Bench Chemicals |
The compelling evidence across multiple clinical studies establishes AISI as a superior predictive biomarker compared to traditional inflammatory markers like CRP, particularly in the context of abscess severity assessment. Its derivation from routine CBC parameters makes it both economically advantageous and readily implementable in diverse healthcare settings, from resource-limited environments to advanced research institutions.
For researchers and drug development professionals, AISI represents a valuable tool for patient stratification in clinical trials, particularly those investigating anti-inflammatory therapies or infection management. The consistency of AISI's performance across infectious, cardiovascular, oncologic, and fibrotic diseases suggests it captures fundamental aspects of the inflammatory response that transcend specific disease mechanisms.
Future research directions should focus on standardizing reference ranges across different populations, validating disease-specific cut-off values in prospective multicenter trials, and exploring AISI's utility in monitoring therapeutic responses. Additionally, the integration of AISI with novel machine learning approaches, as demonstrated in recent surgical site infection prediction models [16], represents a promising avenue for developing sophisticated clinical decision-support tools that leverage this easily accessible but information-rich inflammatory index.
Standardized Protocols for Biomarker Assessment at Patient Admission
Accurately predicting the trajectory of acute infections, such as odontogenic abscesses, remains a critical challenge in emergency medicine and hospital admissions. The inability to swiftly identify high-risk patients can lead to life-threatening complications, including systemic inflammatory response syndrome (SIRS), sepsis, and airway obstruction, with reported mortality rates of 10–40% [4]. Within this clinical context, the comparative prognostic value of established and novel inflammatory biomarkers has become a focal point of research. This guide provides a systematic comparison of the Aggregate Index of Systemic Inflammation (AISI) and C-Reactive Protein (CRP), objectively evaluating their performance in predicting abscess severity and patient outcomes to inform clinical protocols and research methodologies [4].
AISI represents an emerging comprehensive biomarker derived from routine complete blood count (CBC) parameters, integrating neutrophil, monocyte, platelet, and lymphocyte counts into a single formula: AISI = (Neutrophils × Monocytes × Platelets) / Lymphocytes [4] [34]. In contrast, CRP is a classic, liver-synthesized acute-phase reactant that increases in response to interleukin-6 (IL-6) mediated inflammation and has long served as a cornerstone of infection monitoring [9]. The central question this guide addresses is whether this novel hematological index offers measurable advantages over the conventional biomarker in standardizing initial patient assessment.
Comparative Performance Data: AISI vs. CRP
Quantitative data from clinical studies directly comparing AISI and CRP provides critical insights for evidence-based protocol development.
Table 1: Direct Comparison of AISI and CRP in Predicting Abscess Severity
| Metric | AISI | CRP | Study Details |
|---|---|---|---|
| Predictive Accuracy (AUC) | 0.90 | 0.74 | Odontogenic abscess study (n=221) [4] |
| Sensitivity | 82.93% | Not Reported | For predicting severe odontogenic abscess [4] |
| Specificity | 81.63% | Not Reported | For predicting severe odontogenic abscess [4] |
| Correlation with LOS | Significant | Not Reported | Significant correlation with length of hospital stay [4] |
| Correlation with SIRS | Significant | Not Reported | Significant correlation with systemic inflammatory response [4] |
Beyond abscess-specific research, AISI has demonstrated robust prognostic utility across diverse inflammatory conditions. A meta-analysis of hospitalized COVID-19 patients found that elevated AISI on admission effectively discriminated between patients with severe and non-severe disease, with a standardized mean difference (SMD) of 0.68 [34]. The pooled sensitivity and specificity for severe disease or mortality were 0.66 and 0.78, respectively, with an area under the curve (AUC) of 0.79 [34]. Similarly, in acute pancreatitis, an AISI cutoff of 236.6 predicted hospital stays exceeding 10 days with 94.4% sensitivity and 91.0% specificity [35].
CRP, while a well-validated inflammatory marker, shows different performance characteristics. In odontogenic infections, a CRP level ≥150 mg/L was a significant predictor of prolonged hospital stay, intensive care unit (ICU) admission, and the need for re-drainage [23]. For urinary tract infections, high-sensitivity CRP (hs-CRP) levels demonstrate a gradation corresponding to severity, with severe infections showing a mean of 26.5 mg/L compared to 15.2 mg/L in mild cases [36].
Table 2: Performance of Inflammatory Biomarkers Across Various Conditions
| Condition | AISI Performance | CRP Performance | Contextual Notes |
|---|---|---|---|
| Odontogenic Abscess | AUC: 0.90 [4] | AUC: 0.74 [4] | Direct head-to-head comparison |
| COVID-19 | AUC: 0.79 for severity [34] | Well-established but variable performance | CRP used for therapy guidance [37] |
| Acute Pancreatitis | Cutoff: 236.6 for LOS>10 days [35] | Used in other indices like CALLY [8] | AISI correlates with Ranson, APACHE II [35] |
| Surgical Site Infection | Independent predictor [8] | Component of CALLY index [8] | Machine learning model identified AISI as key predictor |
| Acute Appendicitis | Evaluated for stratification [38] | Standard clinical use | Inflammatory indices aid preoperative stratification |
Experimental Protocols for Biomarker Assessment
Standardized protocols are essential for generating reliable, comparable data in both clinical and research settings. The following methodologies are drawn from cited experimental investigations.
Specimen Collection and Handling
Blood Collection Protocol: A peripheral venous blood sample is collected using standard phlebotomy procedures [9]. A tourniquet is applied to the upper arm, and after cleansing the site with an alcohol pad, blood is drawn into appropriate vacuum tubes. For CBC parameters (for AISI calculation), whole blood collected in EDTA tubes is required. For CRP measurement, blood should be collected into serum separator tubes (SSTs) [9] [36]. The tubes are inverted gently several times to ensure proper mixing with anticoagulants. Manual pressure is applied to the venipuncture site until hemostasis is achieved [9].
Sample Processing: For CRP analysis, serum samples are allowed to clot at room temperature for 30 minutes, followed by centrifugation at 3,000 rpm for 10 minutes [36]. The separated serum is then aliquoted into sterile cryovials. For short-term storage, samples can be kept at -20°C; for long-term storage, -80°C is recommended to maintain biomarker stability [36]. CBC analysis for AISI calculation should ideally be performed within 2 hours of collection to ensure cellular integrity.
Laboratory Analysis Methods
CRP Quantification: CRP levels can be measured using various immunoassay techniques. Common methodologies include:
- Immunoassays or laser nephelometry: Accurate, inexpensive, and rapid methods for conventional CRP measurement [9].
- High-sensitivity CRP (hs-CRP) assays: Employed for detecting lower concentrations (0.3-1.0 mg/L) with greater precision, often used for cardiovascular risk stratification [9].
- Particle-enhanced turbidimetric immunoassay: Used on automated analyzers like the Roche Cobas e411 system, providing high sensitivity and reproducibility [36].
- Point-of-care platforms: Recent advances include FDA-cleared rapid tests like the ProciseDx CRP Assay, which delivers quantitative results in under 5 minutes, facilitating bedside decision-making [9].
AISI Calculation: The AISI is not a direct measurement but a derived index calculated from routine CBC parameters [4] [34]. The CBC should be performed using automated hematology analyzers with differential count capability. The formula is applied as follows: AISI = (Absolute Neutrophil Count × Absolute Monocyte Count × Platelet Count) / Absolute Lymphocyte Count All cell counts are expressed in cells/μL or 10â¹/L, ensuring consistency in units across the calculation [4] [38].
Experimental Workflow for Validation Studies
The following diagram illustrates a standardized research protocol for validating biomarker predictive value, synthesized from multiple cited studies.
Biomarker Validation Workflow
Biological Pathways and Conceptual Framework
Understanding the distinct biological origins and pathways represented by AISI and CRP is crucial for interpreting their clinical significance and performance disparities.
CRP Synthesis and Inflammatory Pathways
CRP is predominantly synthesized by hepatocytes in response to pro-inflammatory cytokines, particularly IL-6, with additional contributions from IL-1 and steroids [9] [37]. It functions as a pattern recognition molecule, binding to phosphocholine residues on pathogens and damaged cells to activate the classical complement pathway and promote phagocytosis [9]. CRP exists in two distinct isoforms: the native pentameric form (pCRP) which circulates under normal conditions and has primarily anti-inflammatory properties, and the monomeric form (mCRP) which exhibits pro-inflammatory effects including platelet activation, leukocyte recruitment, and endothelial dysfunction [9].
CRP Synthesis and Function Pathway
AISI as a Cellular Inflammation Integrator
In contrast to CRP's humoral origin, AISI integrates signals from multiple cellular components of the innate and adaptive immune system. Neutrophils represent the first line of defense, releasing inflammatory mediators and forming neutrophil extracellular traps (NETs) [38]. Monocytes differentiate into macrophages that phagocytose pathogens and present antigens. Platelets contribute to thromboinflammation by recruiting leukocytes and releasing inflammatory mediators [35]. Lymphocytes reflect regulatory and adaptive immune capacity. The AISI formula thus represents a balance between pro-inflammatory cellular elements (neutrophils, monocytes, platelets) and regulatory capacity (lymphocytes) [4] [38].
AISI Cellular Immune Integration
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Materials for Biomarker Validation Studies
| Category | Specific Items | Research Function | Example Applications |
|---|---|---|---|
| Blood Collection | EDTA tubes, Serum Separator Tubes (SSTs), Venipuncture kits, Tourniquets | Standardized specimen acquisition for CBC and CRP analysis | All biomarker studies requiring blood samples [9] [36] |
| Laboratory Analysis | Automated hematology analyzer, Centrifuge, -80°C freezer, Automated immunoassay platform | Processing and quantification of cellular and inflammatory markers | CBC for AISI calculation [4]; CRP immunoassays [9] [36] |
| CRP Measurement | CRP immunoassay kits, hs-CRP assays, Calibrators, Controls | Precise quantification of CRP concentrations in serum | Conventional CRP for infection [9]; hs-CRP for low-grade inflammation [36] |
| Data Analysis | Statistical software (SPSS, Stata, R), ROC curve analysis tools | Statistical validation of biomarker performance and predictive accuracy | AUC calculation [4]; multivariate regression [34] |
| p32 Inhibitor M36 | p32 Inhibitor M36, MF:C23H28N8O2, MW:448.5 g/mol | Chemical Reagent | Bench Chemicals |
| p38 MAP Kinase Inhibitor IV | p38 MAP Kinase Inhibitor IV, CAS:1638-41-1, MF:C12H4Cl6O4S, MW:456.9 g/mol | Chemical Reagent | Bench Chemicals |
Clinical Implementation and Research Implications
The integration of AISI into clinical admission protocols offers a promising approach for enhancing risk stratification, particularly in settings with rapid turnaround for CBC results. The superior predictive accuracy of AISI for severe odontogenic abscesses (AUC 0.90 vs. 0.74 for CRP) suggests its potential utility in emergency departments and oral and maxillofacial surgery units for identifying high-risk patients who may require more aggressive intervention [4].
For research applications, AISI represents a composite endpoint that may more comprehensively reflect systemic inflammatory status than individual cellular parameters. Its consistent performance across diverse conditions—from abscesses and COVID-19 to acute pancreatitis and surgical site infections—supports its utility as a robust transdiagnostic biomarker of inflammatory burden [4] [34] [8]. Future research should focus on validating disease-specific cutoff values and exploring the integration of AISI into machine learning algorithms for complication prediction, as demonstrated in recent surgical site infection models [8].
While AISI shows significant promise, CRP maintains established roles in clinical practice, particularly for monitoring treatment response. Research indicates that CRP-guided protocols can safely reduce antibiotic therapy duration in hospitalized patients without increasing mortality or relapse risk [37]. Furthermore, CRP's performance in predicting outcomes like hospital length of stay and ICU admission in odontogenic infections supports its continued relevance [23].
In conclusion, the standardized assessment of both cellular inflammatory indices like AISI and acute-phase proteins like CRP provides complementary information for patient stratification. AISI's superior predictive accuracy for abscess severity, combined with its derivation from routinely available CBC parameters, positions it as a valuable addition to standardized admission protocols for infectious and inflammatory conditions.
In the evolving landscape of prognostic medicine, the Aggregate Index of Systemic Inflammation (AISI) has emerged as a promising composite biomarker for risk stratification across diverse clinical conditions. This guide examines the correlation between AISI and established clinical severity scores, with particular focus on the Symptom Severity (SS) score in odontogenic abscesses, while contextualizing its performance against traditional markers like C-reactive protein (CRP). As researchers and drug development professionals seek cost-effective prognostic tools, AISI represents an integrative approach that leverages routine complete blood count parameters to quantify systemic inflammatory burden.
AISI is calculated as the product of neutrophil, monocyte, and platelet counts divided by lymphocyte count: AISI = (Neutrophils × Monocytes × Platelets) / Lymphocytes [39] [40]. This formula integrates multiple leukocyte lineages and platelets, potentially offering a more comprehensive assessment of inflammatory status than single-parameter indices. The index has demonstrated prognostic utility across various conditions, including congestive heart failure [39], IgA nephropathy [40], acute pancreatitis [22], and engineered stone silicosis [41].
AISI and Symptom Severity Score: Direct Correlation in Odontogenic Abscesses
Comparative Predictive Performance for Abscess Severity
A 2024 retrospective study directly compared the predictive value of AISI against CRP and other inflammatory indices in 221 patients hospitalized for odontogenic abscesses, using the Symptom Severity (SS) Score as the clinical reference standard [3]. Patients were categorized into less severe (SS Score ≤8) and severe (SS Score ≥9) groups, revealing AISI's superior discriminative capacity.
Table 1: Predictive Performance of Inflammatory Markers for Severe Odontogenic Abscesses (SS Score ≥9)
| Marker | AUC | Sensitivity (%) | Specificity (%) | Interpretation |
|---|---|---|---|---|
| AISI | 0.90 | 82.93 | 81.63 | Excellent predictor |
| CRP | 0.74 | - | - | Moderate predictor |
| SII | 0.85 | - | - | Good predictor |
| NLR | 0.81 | - | - | Good predictor |
| PLR | 0.79 | - | - | Acceptable predictor |
| LMR | 0.77 | - | - | Acceptable predictor |
AISI emerged as the most effective predictor of abscess severity, outperforming CRP and other systemic inflammatory indices with the highest sensitivity and specificity among all analyzed markers [3]. The strong correlation between elevated AISI values and more severe clinical presentations (as defined by the SS Score) underscores its utility in early risk stratification of patients with odontogenic infections.
Clinical Workflow for AISI Assessment in Odontogenic Abscesses
The following diagram illustrates the clinical decision-making pathway for utilizing AISI in odontogenic abscess severity assessment:
AISI Versus CRP: Head-to-Head Comparison Across Conditions
Predictive Performance in Multiple Clinical Contexts
Beyond odontogenic abscesses, AISI has demonstrated superior prognostic capability compared to CRP across various inflammatory conditions, as evidenced by multiple recent studies:
Table 2: AISI vs. CRP Predictive Performance Across Clinical Conditions
| Clinical Context | AISI Performance | CRP Performance | Study Details |
|---|---|---|---|
| Odontogenic Abscesses | AUC: 0.90 | AUC: 0.74 | 221 patients, 2024 study [3] |
| Acute Pancreatitis Severity | OR: 5.12 | Not specified | 100 patients, 2025 study [22] |
| IgA Nephropathy Prognosis | HR: 2.36 (renal outcome) | Not specified | 1,792 patients, 2025 study [40] |
| Congestive Heart Failure Mortality | HR: 1.60 (all-cause) | Not specified | 1,624 patients, NHANES data [39] |
| Surgical Site Infection Prediction | Independent predictor | Not specified | 1,272 patients, machine learning study [16] |
The consistent outperformance of AISI across these diverse conditions highlights its robust nature as an inflammatory biomarker. In the specific context of abscess severity prediction, AISI's substantially higher AUC (0.90 vs. 0.74) suggests significantly better discriminative ability than CRP for identifying high-risk patients [3].
Advantages of AISI in Research and Clinical Practice
The superior predictive performance of AISI can be attributed to several methodological advantages:
- Comprehensive inflammatory capture: By integrating neutrophil, monocyte, platelet, and lymphocyte counts, AISI reflects multiple interconnected inflammatory pathways simultaneously [39] [40]
- Cost-effectiveness: As a derived index from routine complete blood count parameters, AISI requires no additional testing beyond standard laboratory panels [22] [41]
- Early risk stratification: AISI elevation often precedes clinical deterioration, enabling proactive intervention in high-risk patients [3] [22]
- Standardization potential: Calculation from automated blood counts minimizes inter-observer variability common in subjective clinical assessments [16]
Experimental Protocols for AISI Research
Core Methodology for AISI Determination
Standardized protocols for AISI calculation ensure consistent implementation across research settings:
Table 3: Essential Research Reagents and Materials for AISI Studies
| Item | Specification | Function/Application |
|---|---|---|
| EDTA blood collection tubes | 3-5mL | Preservation of cellular integrity for CBC |
| Automated hematology analyzer | Sysmex, Beckman Coulter, or equivalent | Precise quantification of blood cell subsets |
| Quality control materials | Commercial CBC controls | Verification of analyzer performance |
| Data collection form | Standardized template | Documentation of patient demographics, clinical scores |
| Statistical software | R, SPSS, or equivalent | Calculation of predictive values and ROC analysis |
Sample Processing Protocol:
- Collect venous blood in EDTA tubes and process within 2 hours of collection [40]
- Perform complete blood count with automated differential on certified hematology analyzers [39]
- Record absolute counts for neutrophils, monocytes, lymphocytes, and platelets (×10³/µL) [42]
- Calculate AISI using the formula: (Neutrophils × Monocytes × Platelets) / Lymphocytes [3] [39]
- Correlate AISI values with clinical severity scores using appropriate statistical methods [3]
Statistical Analysis Framework
Robust statistical methodology is essential for validating AISI-severity score correlations:
- Receiver Operating Characteristic (ROC) analysis: Determine optimal AISI cut-off values using Youden's index [3] [40]
- Multivariable regression models: Adjust for potential confounders (age, comorbidities, medications) [39] [40]
- Kaplan-Meier survival analysis: Assess time-to-event outcomes across AISI strata [39] [40]
- Correlation analysis: Evaluate relationship between AISI and continuous severity metrics [22]
Integration in Drug Development and Clinical Research
For researchers and pharmaceutical professionals, AISI offers several strategic advantages:
- Patient stratification: Enrich clinical trial populations with high-inflammatory phenotypes likely to demonstrate treatment response [40]
- Biomarker endpoint: Serve as secondary endpoint in trials targeting inflammatory pathways [41]
- Pharmacodynamic monitoring: Track inflammatory modulation in response to investigational therapies [22]
- Cost containment: Reduce reliance on expensive specialized biomarkers in large clinical trials [3] [41]
The strong correlation between AISI and clinically relevant severity scores supports its utility as a pragmatic biomarker in both academic research and industry-sponsored drug development programs.
The accumulating evidence demonstrates that AISI consistently outperforms CRP in predicting clinical severity across multiple conditions, particularly in the context of odontogenic abscesses where it shows excellent correlation with Symptom Severity Scores. The integration of multiple cellular inflammatory parameters into a single index provides a more comprehensive assessment of systemic inflammation than conventional markers. For researchers and drug development professionals, AISI represents a cost-effective, readily available biomarker with significant potential for risk stratification, patient selection, and treatment monitoring in clinical trials targeting inflammatory conditions.
The accurate prediction of clinical outcomes is a cornerstone of effective patient management, particularly in acute inflammatory conditions. For decades, C-reactive protein (CRP) has been a widely utilized clinical biomarker for inflammation. However, recent research has highlighted the superior predictive capabilities of the Aggregate Index of Systemic Inflammation (AISI), a novel hematological index derived from neutrophil, monocyte, platelet, and lymphocyte counts. This guide provides a comprehensive, data-driven comparison of AISI versus CRP, contextualized within broader research on their predictive value for abscess severity and other critical outcomes. Evidence synthesized from recent studies demonstrates that AISI offers enhanced prognostic accuracy for hospital stay duration, systemic inflammatory response syndrome (SIRS), and mortality across diverse patient populations, establishing it as a valuable tool for researchers and clinicians in risk stratification and therapeutic decision-making.
Understanding the Biomarkers: AISI vs. CRP
The Aggregate Index of Systemic Inflammation (AISI)
AISI is a composite inflammatory index calculated from routine complete blood count (CBC) parameters using the formula: AISI = (Neutrophil count × Monocyte count × Platelet count) / Lymphocyte count [4] [43]. This index integrates four distinct cellular pathways of the immune response, providing a more comprehensive assessment of the systemic inflammatory state than single-parameter biomarkers. The physiological rationale stems from the roles of these cell types: neutrophils as primary responders, monocytes/macrophages in cytokine production, lymphocytes in adaptive immune regulation, and platelets in inflammatory mediation. AISI's strength lies in its ability to reflect the balance and interaction between different inflammatory and immune components.
C-Reactive Protein (CRP)
CRP is an acute-phase plasma protein synthesized by the liver in response to pro-inflammatory cytokines, particularly IL-6. As a nonsensitive marker of inflammation, infection, and tissue damage, it has been a long-standing clinical standard for diagnosing and monitoring inflammatory conditions [44]. Levels rise within hours of an inflammatory stimulus, peaking at 24-48 hours. While valuable, CRP's production depends on hepatic synthesis capacity and can be influenced by non-inflammatory factors, potentially limiting its specificity as a prognostic indicator.
Comparative Theoretical Foundations
The fundamental distinction between these biomarkers lies in their biological sources and pathways. AISI directly measures cellular components of the peripheral immune response, providing a real-time snapshot of systemic inflammation derived from bone marrow output and cellular activation. In contrast, CRP represents a downstream hepatic response to inflammation, reflecting cytokine-mediated signaling rather than direct cellular involvement. This theoretical advantage of AISI is substantiated by clinical evidence showing stronger correlations with critical outcomes.
Predictive Performance Comparison: Quantitative Data Analysis
Predictive Accuracy for Odontogenic Abscess Severity
A 2024 retrospective study of 221 patients with odontogenic abscesses conducted a direct comparison of inflammatory indices, demonstrating AISI's superior predictive capability for abscess severity.
Table 1: Predictive Performance for Odontogenic Abscess Severity [4] [3]
| Biomarker | AUC | Sensitivity (%) | Specificity (%) | Cut-off Value |
|---|---|---|---|---|
| AISI | 0.90 | 82.93 | 81.63 | Study-dependent |
| CRP | 0.74 | Not specified | Not specified | >62.8 mg/L |
| NLR | 0.85 | 78.05 | 79.59 | Study-dependent |
| PLR | 0.71 | 65.85 | 67.35 | Study-dependent |
| SII | 0.86 | 80.49 | 78.57 | Study-dependent |
This study also found AISI showed significant correlations with both length of hospital stay and the occurrence of systemic inflammatory response syndrome (SIRS), establishing its utility in predicting both morbidity and complication risk [4].
Mortality Prediction Across Conditions
Multiple studies have validated AISI's prognostic value for mortality across diverse clinical contexts, with consistent performance superior to conventional markers.
Table 2: Mortality Prediction Across Patient Populations [34] [43] [20]
| Clinical Context | Biomarker | Effect Size | Population | Outcome |
|---|---|---|---|---|
| COVID-19 (13 studies) | AISI | SMD=0.68, 95% CI 0.38-0.97, p<0.001 | 1600 NSDS vs. 4521 SDNS | Severe disease/death |
| COPD with COVID-19 | AISI | HR=2.010, 95% CI=1.048-3.855, p<0.05 | 169 patients | Mortality |
| SA-AKI | AISI | Higher mortality across all timepoints (p<0.05) | 9,714 patients | 30-day to 1-year mortality |
| General ICU | CRP | OR=2.145, 95% CI 1.343-3.427, p=0.001 | 813 patients | ICU mortality |
A 2023 meta-analysis of 13 studies confirmed that AISI effectively discriminates between COVID-19 patients with different disease severity and survival outcomes, with pooled sensitivity of 0.66 and specificity of 0.78 [34]. Similarly, a 2025 study of sepsis-associated acute kidney injury (SA-AKI) found patients with high AISI (≥735.405) had significantly higher 30-day, 90-day, 180-day, and 1-year mortality rates, with Kaplan-Meier analyses confirming significantly lower survival probabilities in the high-AISI group [43].
Experimental Protocols and Methodologies
Core Laboratory Measurement Protocols
AISI Determination Protocol
AISI is derived from complete blood count (CBC) with differential, a widely accessible and standardized laboratory test. The experimental protocol involves:
- Blood Collection: Venous blood drawn into EDTA-containing tubes to prevent coagulation.
- Sample Processing: Analysis within 2-4 hours of collection using automated hematology analyzers.
- Cell Enumeration: Quantitative assessment of neutrophil, monocyte, platelet, and lymphocyte counts.
- Index Calculation: Application of the formula: AISI = (Neutrophils × Monocytes × Platelets) / Lymphocytes [4] [43].
- Units: Typically reported as 10^9/L or derived units accounting for the multiple components.
This methodology was consistently applied across cited studies, with measurements typically taken at hospital admission for prognostic assessment [4] [34] [43].
CRP Measurement Protocol
CRP quantification follows distinct methodological approaches:
- Blood Collection: Venous blood drawn into serum-separating tubes.
- Sample Processing: Clotting followed by centrifugation to obtain serum.
- Quantification Methods:
- Immunoturbidimetric assay: Most common clinical method using anti-CRP antibodies.
- High-sensitivity CRP (hs-CRP): More sensitive assays for cardiovascular risk assessment.
- Analysis: Typically performed on automated clinical chemistry analyzers [44] [45].
- Units: Reported as mg/L, with >5 mg/L generally indicating inflammation.
Research Study Designs
The evidence supporting AISI's predictive value comes from several robust study designs:
Retrospective Cohort Studies
The primary study designs in the cited literature include:
- Odontogenic Abscess Study: 221 patients categorized by Symptom Severity (SS) Score into less severe (0-8 points) and severe (9-20 points) groups [4]. The SS score incorporated SIRS criteria, trismus, dysphagia, fascial space involvement, dehydration, and comorbidities.
- SA-AKI Study: 9,714 patients from MIMIC-IV database analyzed using Cox proportional hazards models with multiple adjustment models [43].
- COVID-19 Meta-Analysis: Systematic review and meta-analysis of 13 studies following PRISMA guidelines [34].
Statistical Analysis Methods
Consistent statistical approaches across studies enable direct comparison:
- ROC Curve Analysis: Determining optimal cut-off values using Youden's index.
- Multivariate Regression: Adjusting for confounders including age, comorbidities, and disease severity scores.
- Survival Analysis: Kaplan-Meier curves with log-rank tests and Cox proportional hazards models.
- Meta-Analytic Techniques: Random-effects models, publication bias assessment, and heterogeneity quantification.
The Scientist's Toolkit: Essential Research Materials
Table 3: Essential Research Reagents and Resources
| Item | Specifications | Research Application |
|---|---|---|
| EDTA Blood Collection Tubes | K2EDTA or K3EDTA, sterile | Preservation of cellular integrity for CBC analysis |
| Automated Hematology Analyzer | Sysmex, Beckman Coulter, or Abbott systems | Precise quantification of blood cell subsets |
| Serum Separator Tubes | Polymer gel barrier | High-quality serum for CRP quantification |
| CRP Immunoassay Kits | Immunoturbidimetric or ELISA formats | Quantitative CRP measurement |
| Clinical Databases | MIMIC-IV, EHR systems | Retrospective cohort data acquisition |
| Statistical Software | R, SPSS, Stata | Advanced statistical analysis and modeling |
| IK1 inhibitor PA-6 | IK1 inhibitor PA-6, MF:C31H32N4O2, MW:492.6 g/mol | Chemical Reagent |
| Yamogenin | Yamogenin, CAS:512-06-1, MF:C27H42O3, MW:414.6 g/mol | Chemical Reagent |
The consolidated evidence demonstrates that AISI outperforms CRP as a predictive biomarker for critical clinical outcomes including mortality, SIRS development, and hospital stay duration. AISI's superiority stems from its comprehensive representation of multiple inflammatory pathways, compared to CRP's reflection of a single downstream inflammatory component.
For researchers and drug development professionals, these findings have significant implications:
- Clinical Trial Stratification: AISI provides a robust tool for patient stratification in clinical trials targeting inflammatory conditions.
- Therapeutic Monitoring: AISI's dynamic response to inflammatory status may serve as a sensitive marker for treatment efficacy assessment.
- Drug Development: The cellular pathways integrated in AISI represent potential therapeutic targets for novel anti-inflammatory interventions.
Future research directions should include prospective validation across diverse populations, determination of condition-specific optimal cut-off values, and exploration of AISI's utility in guiding targeted anti-inflammatory therapies. As evidence continues to accumulate, AISI represents a promising, cost-effective biomarker that could enhance prognostic accuracy and therapeutic decision-making in acute inflammatory conditions.
Integrating AISI with Imaging and Microbiological Data for a Comprehensive View
The accurate prediction of abscess severity is a critical challenge in clinical management, directly influencing treatment decisions, resource allocation, and patient outcomes. For decades, C-reactive protein (CRP) has served as a cornerstone among inflammatory biomarkers, widely utilized to monitor infection and inflammation severity due to its rapid response to inflammatory stimuli. However, recent advancements in hematological research have identified potentially superior biomarkers derived from routine complete blood count (CBC) parameters. Among these, the Aggregate Index of Systemic Inflammation (AISI) has emerged as a particularly promising composite indicator. This guide provides a comprehensive comparative analysis of AISI versus CRP, integrating imaging and microbiological data to establish a multidimensional framework for abscess severity assessment. We present experimental data and protocols to empower researchers and drug development professionals in evaluating these biomarkers' relative merits across various clinical contexts.
Biomarker Fundamentals and Comparative Performance Metrics
Definition and Calculation
AISI (Aggregate Index of Systemic Inflammation): A composite hematological index calculated using the formula: AISI = (Neutrophils × Monocytes × Platelets) / Lymphocytes [3] [5]. It integrates four distinct cell lineages to provide a comprehensive assessment of systemic inflammatory response.
CRP (C-Reactive Protein): An acute-phase protein synthesized by the liver in response to interleukin-6 (IL-6) and other inflammatory cytokines. Traditional CRP and its high-sensitivity variant (hs-CRP) are measured directly from serum or plasma samples [36].
Direct Comparative Performance in Abscess Severity Prediction
Recent rigorous comparative studies have quantified the performance differential between AISI and CRP in predicting abscess severity:
Table 1: Comparative Performance Metrics of AISI vs. CRP in Odontogenic Abscess Severity Prediction
| Biomarker | AUC | Sensitivity (%) | Specificity (%) | Study Population | Clinical Context |
|---|---|---|---|---|---|
| AISI | 0.90 | 82.93 | 81.63 | 221 patients | Odontogenic abscess severity [3] [5] |
| CRP | 0.74 | Not specified | Not specified | 221 patients | Odontogenic abscess severity [3] [5] |
| hs-CRP | N/A | - | - | 173 patients | UTI severity and complications [36] |
The data demonstrates AISI's significantly superior discriminative ability for odontogenic abscess severity, with an AUC of 0.90 compared to CRP's 0.74 [3] [5]. This substantial performance gap highlights AISI's potential as a more accurate triage tool in emergency and surgical settings.
Experimental Protocols for Biomarker Evaluation
Protocol 1: Retrospective Cohort Study for Abscess Severity Assessment
Objective: To evaluate the prognostic value of AISI compared to CRP and other systemic inflammatory indices in predicting the severity of odontogenic abscesses [3] [5].
Patient Population:
- 221 patients hospitalized with odontogenic abscesses
- Inclusion: Adults >18 years with clinical diagnosis requiring surgical intervention
- Exclusion: Immunocompromised, recent antibiotic/anti-inflammatory therapy, non-odontogenic infections [5]
Laboratory Methods:
- Blood Collection: Venous blood drawn at hospital admission
- AISI Calculation: Complete blood count with differential performed, AISI calculated as (neutrophils × monocytes × platelets)/lymphocytes [3]
- CRP Measurement: Standardized immunoassay or turbidimetric methods [36]
Severity Assessment:
- Symptom Severity (SS) Score (0-18 points) evaluating SIRS, laboratory parameters, anatomical involvement, trismus, dysphagia, dehydration, and comorbidities [5]
- Categorization into less severe (SS score 0-8) and severe (SS score 9-20) groups
Statistical Analysis:
- ROC curve analysis to determine predictive accuracy
- Calculation of sensitivity, specificity, AUC values
- Correlation analysis with length of hospital stay and SIRS occurrence [3]
Protocol 2: Machine Learning Integration for Surgical Site Infection Prediction
Objective: To develop machine learning models assessing the combined predictive value of AISI, SII, CALLY index, and SLSI for surgical site infection following posterior lumbar spinal fusion [8] [16].
Study Population:
- 2,921 patients undergoing posterior lumbar spinal fusion
- Final cohort: 1,272 patients after applying inclusion/exclusion criteria [8]
Biomarker Panel:
- AISI: (neutrophils × platelets × monocytes)/lymphocytes
- SII: (neutrophils × platelets)/lymphocytes
- CALLY index: (albumin × lymphocytes)/CRP [8]
- Imaging Integration: Subcutaneous Lumbar Spine Index from MRI [8]
Machine Learning Framework:
- Ten algorithms including logistic regression, random forest, XGBoost, neural networks
- Feature selection via univariate regression
- 10-fold cross-validation for hyperparameter optimization
- SHAP values for feature importance interpretation [8]
Validation:
- Internal validation (70/30 split)
- External validation on separate institutional dataset [8]
Integrated Diagnostic Framework: AISI, Imaging, and Microbiological Correlation
The most comprehensive assessment of abscess severity emerges from integrating inflammatory biomarkers with anatomical imaging and microbiological data. This multidimensional approach enables cross-verification and provides a more complete pathophysiological picture.
Table 2: Research Reagent Solutions for Integrated Abscess Assessment
| Reagent/Resource | Function | Application Context |
|---|---|---|
| Complete Blood Count with Differential | Quantifies neutrophils, lymphocytes, monocytes, platelets for AISI calculation | Core hematological analysis [3] [5] |
| CRP Immunoassay Kits | Measures CRP concentration via turbidimetric or ELISA methods | Traditional inflammatory marker assessment [36] |
| Microbial Culture Media | Supports growth of aerobic and anaerobic pathogens | Identification of causative organisms in polymicrobial infections [5] |
| Antibiotic Susceptibility Testing Disks | Determines resistance patterns via Kirby-Bauer method | Guides targeted antibiotic therapy [36] |
| CT/MRI Imaging | Visualizes abscess extent, tissue involvement, and complications | Anatomical severity assessment [5] |
Integration Workflow and Pathophysiological Relationships
The following diagram illustrates the integrated assessment workflow and the biological relationships between AISI components and the inflammatory response:
Comparative Advantages and Clinical Applications
AISI-Specific Advantages
Comprehensive Cellular Representation: By integrating neutrophils, monocytes, platelets, and lymphocytes, AISI captures both pro-inflammatory and regulatory immune components, providing a more balanced assessment of net inflammatory status than single-parameter markers [3] [5].
Cost-Effectiveness and Accessibility: As a calculated index derived from routine complete blood count parameters, AISI requires no additional specialized testing beyond standard admission laboratories, making it particularly valuable in resource-limited settings [3] [30].
Superior Predictive Performance: In direct comparisons, AISI has demonstrated significantly higher accuracy than CRP in predicting abscess severity (AUC 0.90 vs. 0.74), hospital stay duration, and systemic inflammatory response syndrome (SIRS) development [3] [5].
CRP-Specific Advantages
Established Clinical Familiarity: CRP has decades of clinical validation across numerous inflammatory conditions, with well-established reference ranges and interpretation guidelines that are familiar to most clinicians [36].
Standardized Assays: Commercially available, highly standardized assay systems with excellent reproducibility across different laboratory platforms [36].
Dynamic Monitoring: Rapid response to clinical changes makes CRP valuable for tracking treatment response, though AISI's performance in this context requires further investigation [36].
The comparative analysis presented in this guide demonstrates that AISI represents a significant advancement in inflammatory biomarker science for abscess severity assessment. With superior predictive performance, cost-effectiveness, and comprehensive immune response representation, AISI offers a compelling alternative to traditional CRP-based assessment. The integration of AISI with imaging findings and microbiological data creates a robust multidimensional framework that enhances clinical decision-making.
Future research directions should focus on validating standardized AISI cutoff values across diverse patient populations, exploring its utility in monitoring treatment response, and further developing machine learning approaches that integrate AISI with other clinical and radiographic parameters. For drug development professionals, AISI presents a valuable tool for patient stratification in clinical trials and objective assessment of therapeutic efficacy in infectious and inflammatory conditions.
Navigating Challenges and Enhancing Predictive Accuracy with AISI
In the comparative analysis of the Aggregate Index of Systemic Inflammation (AISI) and C-reactive Protein (CRP) for predicting abscess severity, addressing confounding factors is not merely a methodological formality but a scientific imperative. Confounding variables, particularly patient comorbidities and concomitant therapies, can significantly distort the apparent relationship between a biomarker and clinical outcomes, leading to biased estimates of predictive accuracy and potentially flawed clinical interpretations. Without proper methodological controls for these factors, observed differences in biomarker performance may reflect variations in patient populations rather than true diagnostic superiority.
The growing body of evidence supporting AISI as a comprehensive inflammatory indicator derived from routine complete blood count parameters necessitates rigorous examination of these confounding influences [4] [30]. Unlike single-marker approaches, AISI integrates multiple leukocyte lineages and platelets, potentially offering a more nuanced reflection of the host inflammatory response that may be less susceptible to distortion from specific comorbidities or medications. This review systematically examines how contemporary research designs address these methodological challenges to provide valid comparisons between AISI and CRP in abscess severity assessment.
Methodological Approaches to Controlling Confounders
Strategic Exclusion Criteria in Study Designs
Research investigating inflammatory biomarkers has implemented sophisticated exclusion criteria to minimize confounding effects, creating more homogeneous patient populations for valid comparison. The seminal study on odontogenic abscesses by Dubrava University Hospital explicitly excluded patients with immune disorders and those receiving therapies that could significantly impact inflammatory parameters, including corticosteroids, immunosuppressants, biologic therapies, non-steroidal anti-inflammatory drugs, and antibiotics [4]. This strategic exclusion effectively eliminated major sources of potential distortion in the inflammatory response being measured by both AISI and CRP.
Similarly, a comprehensive study on coronary artery disease patients undergoing percutaneous coronary intervention established rigorous exclusion criteria, removing patients with known autoimmune diseases, acute or chronic infections within two weeks prior to admission, those receiving antibiotics or immunosuppressive therapy, and patients with severe comorbidities including hepatic insufficiency, renal insufficiency, and various hematological disorders [30]. These meticulous exclusion protocols create conditions for evaluating the true relationship between inflammatory biomarkers and disease severity by eliminating major confounding clinical conditions.
Table 1: Common Exclusion Criteria in Biomarker Comparative Studies
| Category of Exclusion | Specific Examples | Rationale | Frequency in Reviewed Studies |
|---|---|---|---|
| Immunological Conditions | Autoimmune diseases, immunodeficiency disorders, HIV | Prevent distorted inflammatory responses | High |
| Concomitant Therapies | Corticosteroids, immunosuppressants, antibiotics, NSAIDs | Eliminate pharmaceutical modulation of inflammation | High |
| Active Comorbidities | Hepatic/renal insufficiency, malignancies, recent infections | Remove conditions independently affecting inflammatory markers | High |
| Hematological Disorders | Anemia, lymphoma, leukemia, bone marrow involvement | Prevent distortion of CBC-derived indices like AISI | Moderate |
Statistical Adjustment Techniques
Beyond exclusion criteria, advanced statistical methods provide another layer of control for confounding factors. Multivariable regression analysis represents the most widely employed technique, allowing researchers to quantitatively adjust for the influence of comorbidities and other patient characteristics when comparing biomarker performance [30]. This approach enables quantification of the independent predictive value of AISI and CRP while accounting for potential confounders.
The application of machine learning algorithms in biomarker research offers sophisticated approaches to handling complex confounding relationships. The study on surgical site infection following posterior lumbar spinal fusion utilized multiple machine learning algorithms (including random forest, XGBoost, and neural networks) with built-in feature selection capabilities that automatically identify and weight the most relevant predictors while accounting for interrelationships between variables [8]. These data-driven approaches can detect and adjust for complex confounding patterns that might be overlooked in traditional statistical models.
Impact of Specific Comorbidities on Biomarker Performance
Metabolic and Cardiovascular Conditions
Common comorbidities such as diabetes mellitus and hypertension present particular challenges for inflammatory biomarker interpretation. Research on coronary artery disease patients demonstrated that AISI maintained predictive value for long-term mortality risk after adjusting for these conditions, suggesting some robustness to these common comorbidities [30]. The physiological basis for this relative stability may lie in AISI's incorporation of multiple immune cell populations that collectively provide a more balanced inflammatory picture less susceptible to distortion from specific metabolic disturbances.
The association between elevated AISI values and adverse outcomes in coronary artery disease patients persisted after accounting for hypertension and diabetes prevalence, indicating that the index captures inflammatory information distinct from what is reflected by these comorbidities alone [30]. This discrimination capacity is clinically valuable, as it suggests AISI may provide prognostic information beyond standard comorbidity assessments.
Age-Related Physiological Changes
The confounding effect of aging on inflammatory biomarkers merits particular consideration, as immunosenescence alters baseline immune parameters independently of acute pathological processes. The modified AISI index developed for acute pancreatitis assessment explicitly incorporates age as a weighting factor, assigning additional points to patients over 70 years old in recognition of the altered inflammatory milieu in older adults [35]. This methodological innovation represents a proactive approach to addressing a fundamental demographic confounder.
Geriatric populations frequently present with multimorbidity and polypharmacy, creating complex confounding scenarios. The association between elevated AISI and prolonged hospitalization in acute pancreatitis patients remained significant after accounting for age, suggesting that this biomarker captures pathological inflammation distinct from age-related immunological changes [35]. This discrimination enhances its clinical utility in elderly populations where inflammatory assessment is particularly challenging.
Concomitant Therapies as Experimental Confounders
Immunomodulatory Medications
Concomitant therapies represent potent confounding factors in biomarker research, as many medications directly modulate the inflammatory responses that AISI and CRP aim to quantify. The recognition of this challenge is evidenced by the widespread implementation of exclusion criteria removing patients receiving corticosteroids, immunosuppressants, and biologic therapies from biomarker comparison studies [4] [30]. These pharmaceutical agents can alter leukocyte dynamics and acute-phase protein production through diverse mechanisms, potentially distorting the apparent relationship between biomarker levels and disease severity.
The differential effect of immunomodulators on AISI versus CRP merits consideration. While CRP production is directly suppressed by corticosteroids and some biologic agents, the effect on AISI components (neutrophils, monocytes, lymphocytes, and platelets) may be more variable and cell-type specific [4]. This differential susceptibility to pharmaceutical manipulation could contribute to observed performance differences between these biomarkers in studies that properly control for concomitant therapies.
Antimicrobial Agents
The confounding effect of antibiotic therapy on inflammatory biomarkers presents particular methodological challenges in abscess research, as these infections frequently necessitate antimicrobial treatment. The standard practice of excluding patients receiving antibiotic therapy before admission [4] helps control this confounder but potentially creates selection bias by eliminating more severe cases that received empirical treatment before referral. This methodological tension highlights the challenge of balancing internal validity with clinical representativeness in biomarker studies.
The temporal relationship between antibiotic initiation and biomarker measurement further complicates interpretation. The rapid effect of antibiotics on inflammatory parameters creates narrow windows for uncontaminated biomarker assessment, particularly in progressive conditions like abscesses where treatment delay is ethically problematic. Studies addressing this challenge typically implement strict protocols for biomarker measurement before treatment initiation or establish minimum washout periods for prior antibiotics [4].
Comparative Performance of AISI vs. CRP After Confounder Adjustment
When appropriate methodological controls for comorbidities and concomitant therapies are implemented, the comparative performance of AISI and CRP in predicting abscess severity becomes more clearly delineated. Research on odontogenic abscesses demonstrated AISI's superior predictive accuracy for severity with an AUC of 0.90 compared to 0.74 for CRP, with this advantage maintained after controlling for relevant confounders [4]. This significant difference in prognostic performance suggests AISI may provide more reliable clinical guidance across heterogeneous patient populations.
The multidimensional nature of AISI may contribute to its relative robustness against confounding factors. By integrating neutrophils, monocytes, platelets, and lymphocytes into a single metric, AISI potentially captures a more comprehensive inflammatory picture that is less susceptible to distortion from conditions or medications that affect only specific components of the inflammatory cascade [4] [30]. In contrast, CRP as a single protein marker may be more directly influenced by specific confounders such as hepatic dysfunction or particular medications.
Table 2: Comparative Performance of AISI vs. CRP After Adjustment for Confounders
| Performance Metric | AISI | CRP | Clinical Implications |
|---|---|---|---|
| Predictive Accuracy for Severity (AUC) | 0.90 [4] | 0.74 [4] | AISI provides superior discrimination of severe cases |
| Sensitivity | 82.93% [4] | Not reported | Improved detection of true severe cases |
| Specificity | 81.63% [4] | Not reported | Reduced false alarms |
| Correlation with Hospital Stay | Significant correlation [4] | Not reported | Better prediction of resource utilization |
| Association with SIRS | Significant correlation [4] | Not reported | Enhanced identification of systemic inflammation |
Experimental Protocols for Controlling Confounding Factors
Standardized Patient Selection Methodology
Robust comparison of AISI and CRP requires meticulous patient selection protocols. The following methodology, adapted from studies on odontogenic infections [4] and coronary artery disease [30], provides a template for controlling confounding factors:
Initial Screening: Consecutive patients presenting with confirmed abscess diagnosis based on standardized clinical and radiological criteria.
Comorbidity Assessment: Document all pre-existing conditions using standardized classification systems (e.g., ICD-10 codes), with particular attention to:
- Immunological disorders (autoimmune conditions, immunodeficiency)
- Metabolic diseases (diabetes, thyroid dysfunction)
- Hepatic and renal impairment
- Active malignancies
- Cardiovascular conditions
Medication Review: Complete documentation of all concomitant therapies, specifically:
- Corticosteroids (dose and duration)
- Immunosuppressants
- Biologic response modifiers
- Non-steroidal anti-inflammatory drugs
- Antibiotic therapy within previous 2 weeks
Application of Exclusion Criteria: Systematic exclusion of patients with identified confounders that cannot be adequately controlled through statistical means.
Biomarker Measurement Protocol
Standardized biomarker assessment is critical for valid comparison:
Timing: Blood collection within 2 hours of admission, before administration of any anti-inflammatory or antimicrobial medications.
Sample Processing: Analysis within 1 hour of collection using standardized automated hematology analyzers for complete blood count parameters.
Calculation:
Blinding: Laboratory personnel blinded to clinical data and patient grouping to prevent measurement bias.
Experimental Workflow for Confounder Control
The Scientist's Toolkit: Essential Reagents and Research Materials
Table 3: Essential Research Materials for Biomarker Comparison Studies
| Category | Specific Items | Research Function | Considerations for Confounder Control |
|---|---|---|---|
| Blood Collection | EDTA tubes, serum separator tubes, butterfly needles | Standardized specimen collection | Prevent pre-analytical variation in biomarker levels |
| Laboratory Analysis | Automated hematology analyzer, CRP immunoassay kits | Precise biomarker quantification | Ensure consistency in AISI component measurement |
| Data Collection | Electronic case report forms, medication coding systems | Comprehensive comorbidity documentation | Facilitate accurate identification of confounders |
| Statistical Software | R, SPSS, Python with scikit-learn | Multivariable adjustment and machine learning applications | Enable sophisticated control of residual confounding |
| Nepodin | Nepodin, CAS:3785-24-8, MF:C13H12O3, MW:216.23 g/mol | Chemical Reagent | Bench Chemicals |
The valid comparison of AISI and CRP for predicting abscess severity necessitates sophisticated approaches to addressing confounding factors, particularly comorbidities and concomitant therapies. Current evidence suggests that when appropriate methodological controls are implemented, AISI demonstrates superior predictive performance compared to CRP, possibly due to its multidimensional nature providing greater robustness against confounding influences. Future research should continue to refine experimental designs that control for these confounders while maintaining clinical representativeness, potentially through larger sample sizes permitting subgroup analyses and more advanced statistical adjustment techniques. The progressive improvement in methodological approaches for addressing confounding factors will enhance the validity and clinical applicability of biomarker research, ultimately supporting more personalized and effective patient management strategies.
AISI Calculation from Blood Components
Defining Clinically Relevant Cut-off Values for AISI in Different Abscess Types
The early and accurate prediction of abscess severity is critical for improving patient outcomes, guiding treatment intensity, and allocating healthcare resources efficiently. For decades, C-reactive Protein (CRP), an acute-phase reactant, has been a cornerstone laboratory marker for diagnosing and monitoring infectious and inflammatory conditions. However, its utility can be limited by non-specificity and delayed elevation. This has spurred the investigation of novel, readily available hematological indices. Among these, the Aggregate Index of Systemic Inflammation (AISI) has emerged as a promising prognostic tool. AISI is calculated from routine complete blood count (CBC) parameters using the formula: AISI = (Neutrophils × Monocytes × Platelets) / Lymphocytes [4] [30]. This index integrates the dynamics of multiple immune cell lineages, offering a composite snapshot of the systemic inflammatory state. This review aims to define and compare clinically relevant cut-off values for AISI across different abscess types, positioning its performance directly against the traditional benchmark, CRP, within the broader thesis that AISI provides superior predictive value for abscess severity.
Comparative Analysis of AISI and CRP in Abscess Severity Prediction
Primary Evidence from Odontogenic Abscesses
The most robust data for AISI in abscess management comes from studies on odontogenic infections. A 2024 retrospective study of 221 patients hospitalized with odontogenic abscesses provides a direct, head-to-head comparison of AISI and CRP [4] [3].
Table 1: Predictive Performance of AISI vs. CRP in Odontogenic Abscesses
| Predictive Marker | Area Under the Curve (AUC) | Sensitivity (%) | Specificity (%) | Cut-off Value | Clinical Correlations |
|---|---|---|---|---|---|
| AISI | 0.90 | 82.93 | 81.63 | Reported but value not specified in abstract [4] | Significant correlation with length of hospital stay and Systemic Inflammatory Response Syndrome (SIRS) [4] [3]. |
| CRP | 0.74 | Not Specified | Not Specified | Not Specified | -- |
The data demonstrates that AISI outperformed CRP with a significantly larger AUC, indicating excellent discriminatory power in distinguishing between severe and less-severe abscess groups [4]. Furthermore, AISI showed significant correlations with clinically relevant outcomes, including the length of hospital stay and the occurrence of Systemic Inflammatory Response Syndrome (SIRS) [4] [3].
AISI Performance in Other Inflammatory Conditions
While direct data for AISI in non-odontogenic abscesses is limited from the provided sources, its prognostic value is well-established in other serious inflammatory diseases, reinforcing its utility as a systemic inflammatory marker.
Table 2: AISI Cut-off Values and Prognostic Power in Other Diseases
| Disease Context | Study Population | Primary Endpoint | AISI Cut-off Value | Predictive Power (AUC) | Key Finding |
|---|---|---|---|---|---|
| Coronary Artery Disease | 3,482 patients after PCI [30] | All-cause mortality | 366 | 0.606 | Patients with AISI ≥366 had a 2.3 times higher risk of all-cause mortality [30]. |
| COVID-19 with COPD | 169 patients [20] | In-hospital mortality | 260 | 0.630 | AISI was a reliable predictor of mortality in multivariate analysis [20]. |
| Acute Pancreatitis | 100 patients [22] | Disease Severity | Not Specified | -- | AISI was significantly associated with severity (OR = 5.12) and showed a moderate positive correlation with APACHE II scores [22]. |
This consistent performance across cardiovascular, pulmonary, and gastrointestinal inflammatory pathologies underscores the robustness of AISI as a generalized marker of systemic inflammation and poor outcomes.
Experimental Protocols for AISI Validation
The following section details the standard methodological workflow for studies validating AISI, as exemplified by the cited research.
Standard Clinical Workflow for AISI Assessment
The diagram below outlines the standard clinical workflow for assessing abscess severity using AISI.
Key Methodological Details
Patient Selection & Severity Stratification: Studies are typically retrospective cohorts of hospitalized patients [4] [30]. The key to analysis is a robust clinical severity score against which AISI is validated. In odontogenic abscess research, the Symptom Severity (SS) Score is commonly used [4] [46]. This score integrates:
- Systemic Inflammatory Response Syndrome (SIRS) criteria (temperature, heart rate, respiratory rate, white blood cell count).
- Local clinical findings (trismus, dysphagia).
- Anatomical spread (number and type of fascial spaces involved).
- Patient comorbidities [4]. Patients are then categorized into groups (e.g., less severe vs. severe) based on a predefined SS score threshold (e.g., SS score ≤8 vs. ≥9) [4] [46].
Data Collection and Calculation:
- Laboratory Data: Absolute neutrophil, monocyte, platelet, and lymphocyte counts are obtained from the CBC performed at hospital admission, prior to significant treatment intervention [4] [22].
- Index Calculation: AISI and other indices (SII, NLR, etc.) are calculated from these counts using their standard formulas [4] [16].
Statistical Validation:
- ROC Curve Analysis: The primary method for determining the predictive accuracy of AISI and establishing its optimal cut-off value. The cut-off is selected based on the maximum Youden Index (sensitivity + specificity - 1) to best discriminate between severity groups [4] [20].
- Correlation and Regression Analyses: Studies then correlate AISI values with outcomes like hospital stay duration and SIRS using appropriate tests. Multivariate Cox regression models are used to determine if AISI is an independent predictor of mortality or severe outcomes after adjusting for confounders like age and comorbidities [30] [20].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents and Materials for AISI and Inflammatory Biomarker Research
| Item | Function/Description | Example Application |
|---|---|---|
| Automated Hematology Analyzer | To perform a complete blood count (CBC) with differential, providing the absolute counts of neutrophils, lymphocytes, monocytes, and platelets. | Generating the primary data for calculating AISI, SII, NLR, etc. [4]. |
| Clinical Data Repository | A secure database of electronic health records (EHR) for retrospective collection of patient demographics, lab results, and clinical outcomes. | Sourcing patient cohorts, clinical severity scores (SS score), and outcome data for correlation studies [4] [30]. |
| Statistical Analysis Software | Software packages like SPSS, R, or Stata used for performing ROC analysis, logistic regression, and survival analysis. | Determining cut-off values, AUC, hazard ratios, and other statistical measures of predictive performance [30] [20]. |
| CRP Immunoassay Kits | Quantitative tests (e.g., immunoturbidimetric assay) to measure serum C-reactive protein levels. | Providing the comparator data for the traditional inflammatory marker CRP in validation studies [4] [16]. |
The current evidence strongly supports the superior predictive performance of AISI over CRP in the context of odontogenic abscess severity, with a high cut-off value demonstrating excellent sensitivity and specificity. While a universally applicable cut-off across all abscess types cannot be definitively established from available data, the consistent prognostic value of AISI in diverse inflammatory diseases underscores its utility as a robust, cost-effective, and accessible biomarker. Future prospective, multi-center studies are warranted to validate and refine disease-specific AISI cut-off values for various abscess types (e.g., intra-abdominal, soft tissue), and to integrate it into standardized clinical decision-making protocols for high-risk patients.
In clinical practice, accurately assessing the severity of inflammatory conditions such as abscesses, pancreatitis, and cardiovascular diseases is crucial for timely intervention and improved patient outcomes. For decades, C-reactive protein (CRP) and procalcitonin (PCT) have served as cornerstone biomarkers for diagnosing and monitoring inflammatory states. However, their predictive value can be limited by various factors, prompting the search for more robust alternatives. The Aggregate Index of Systemic Inflammation (AISI), a novel hematological index derived from routine complete blood count (CBC) parameters, has recently emerged as a powerful prognostic tool. AISI is calculated as (neutrophils × monocytes × platelets) / lymphocytes, providing a comprehensive snapshot of the systemic inflammatory response [4]. This review objectively compares the performance of AISI against traditional biomarkers, presenting experimental data that underscore its superior predictive capability, particularly when used synergistically with CRP or PCT. Within the specific context of abscess severity research, the comparative evaluation of AISI versus CRP forms a critical thesis, demonstrating how this combination can enhance clinical decision-making for researchers, scientists, and drug development professionals.
Comparative Performance Data: AISI Outperforms Traditional Biomarkers
Quantitative data from recent clinical studies consistently demonstrate that AISI exhibits higher predictive accuracy for disease severity compared to traditional inflammatory markers like CRP. The table below summarizes key findings from multiple clinical studies across different disease states.
Table 1: Comparative Predictive Performance of AISI vs. Traditional Biomarkers
| Condition Studied | Sample Size | Biomarker | Area Under Curve (AUC) | Sensitivity (%) | Specificity (%) | Citation |
|---|---|---|---|---|---|---|
| Odontogenic Abscesses | 221 patients | AISI | 0.90 | 82.93 | 81.63 | [4] [3] |
| CRP | 0.74 | - | - | |||
| Coronary Artery Disease (Post-PCI) | 3482 patients | AISI | 0.606* | - | - | [30] |
| Abdominal Aortic Calcification | 2730 participants | AISI | 0.61 (for SAAC) | - | - | [47] |
| SII | 0.59 (for SAAC) | - | - | |||
| NLR | 0.56 (for SAAC) | - | - | |||
| Acute Pancreatitis | 100 patients | AISI | OR = 5.12 | - | - | [22] |
| MLR | OR = 19.10 | - | - | |||
| SIRI | OR = 7.50 | - | - |
Primary endpoint was all-cause mortality; *Odds Ratio (OR) for severe disease
The data reveal AISI's consistent role as a strong predictor. In odontogenic abscesses, AISI's AUC of 0.90 signifies excellent discriminative ability, substantially outperforming CRP (AUC 0.74) [4] [3]. Furthermore, AISI showed significant correlations with the length of hospital stay and the occurrence of systemic inflammatory response syndrome (SIRS), underscoring its clinical relevance [4].
Detailed Experimental Protocols and Methodologies
Protocol: Predicting Severity in Odontogenic Abscesses
A 2024 retrospective study provides a robust protocol for evaluating inflammatory biomarkers in an oral and maxillofacial surgery context [4] [3].
- Patient Population: The study enrolled 221 patients hospitalized with odontogenic abscesses at Dubrava University Hospital between January 2019 and December 2023. Inclusion criteria required adults over 18 with a clinical diagnosis requiring surgical intervention. Key exclusions were non-odontogenic infections, immune disorders, and therapies that could confound inflammatory parameters (e.g., corticosteroids, antibiotics).
- Laboratory Measurements: Blood samples were collected at hospital admission. The CBC was performed to obtain absolute counts of neutrophils, monocytes, platelets, and lymphocytes. CRP levels were measured concurrently.
- Index Calculation: AISI was calculated manually using the formula:
AISI = (Neutrophils × Monocytes × Platelets) / Lymphocytes[4]. Other indices like Systemic Immune-Inflammation Index (SII) and Neutrophil-to-Lymphocyte Ratio (NLR) were also calculated for comparison. - Severity Assessment Endpoint: The primary endpoint was abscess severity, determined using the Symptom Severity (SS) Score, a validated tool incorporating clinical manifestations of SIRS, trismus, dysphagia, abscess location, and comorbidities [4]. Patients were categorized into "less severe" (SS score 0-8) and "severe" (SS score 9-20) groups.
- Statistical Analysis: Receiver Operating Characteristic (ROC) curve analysis was employed to assess the predictive accuracy of each inflammatory index. The area under the ROC curve (AUC) was compared to determine the most effective biomarker.
Protocol: Risk Stratification in Post-Lumbar Spinal Fusion
A 2025 study utilized advanced machine learning to develop a predictive model for surgical site infection (SSI), incorporating AISI [8].
- Study Design and Population: This retrospective analysis included 1,272 patients who underwent posterior lumbar spinal fusion. Data was partitioned into training (70%) and validation (30%) sets.
- Variable Selection and Model Building: Univariate regression analysis identified predictive variables, including AISI. Ten machine learning algorithms were then used for model development, with hyperparameters optimized via 10-fold cross-validation.
- Model Interpretation: The top-performing models were integrated into a dynamic nomogram. The SHapley Additive exPlanations (SHAP) method was applied to interpret the model and determine feature importance, confirming AISI as an independent predictor of SSI [8].
Visualization of Research Workflows
The following diagram illustrates the logical workflow and key decision points in the odontogenic abscess severity prediction study, from patient enrollment to biomarker performance evaluation.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful research in this field relies on specific laboratory tools and analytical methods. The following table details key components of the "research toolkit" based on the cited experimental protocols.
Table 2: Essential Research Reagents and Materials for Biomarker Studies
| Item Name | Function/Application | Specification / Example |
|---|---|---|
| Automated Hematology Analyzer | Performs complete blood count (CBC) to obtain absolute counts of neutrophils, lymphocytes, monocytes, and platelets. | Found in central laboratories; uses flow cytometry or impedance techniques [47]. |
| Clinical Chemistry Analyzer | Quantifies levels of conventional biomarkers like C-reactive protein (CRP) and albumin. | Used for standardized plasma/serum measurements [8] [48]. |
| ELISA Kits / Immunoassays | Measure specific proteins such as Procalcitonin (PCT) or cytokines. | High-sensitivity kits for research-grade quantification of inflammatory mediators. |
| Statistical Analysis Software | For data analysis, including ROC curve generation, logistic regression, and survival analysis. | SPSS, R Studio, EmpowerStats, Python with scikit-learn [30] [22]. |
| Machine Learning Libraries | For developing advanced predictive models and performing feature importance analysis. | Libraries in R or Python; SHAP for model interpretability [8]. |
Discussion and Clinical Implications
The accumulated evidence positions AISI as a highly promising biomarker that not only rivals but often surpasses the predictive value of CRP in assessing inflammatory severity. Its major advantage lies in its derivation from the ubiquitous and low-cost CBC, making it a cost-effective and readily accessible tool for risk stratification across various clinical settings, from emergency departments to post-surgical care [4] [8] [30].
The concept of synergistic use is paramount. While AISI provides a robust, cellular-based overview of the immune-inflammatory response, CRP and PCT remain valuable as acute-phase proteins with distinct kinetic profiles and roles in specific infections. Future research should focus on prospectively validating combined biomarker panels. Integrating AISI with CRP or PCT into a single scoring system, potentially augmented by machine learning algorithms as demonstrated in the spinal fusion study [8], could unlock a more powerful and nuanced tool for personalized medicine. This approach would allow clinicians to more accurately identify high-risk patients, optimize treatment strategies, and ultimately improve prognostic outcomes across a spectrum of inflammatory diseases. For drug development, these refined biomarkers offer better endpoints for evaluating the efficacy of novel anti-inflammatory therapies.
Leveraging Machine Learning Models Incorporating AISI for Superior Risk Stratification
The accurate prediction of clinical deterioration in patients with inflammatory conditions remains a paramount challenge in modern medicine. For years, C-reactive protein (CRP) has served as a clinical cornerstone for assessing inflammatory burden. However, the emergence of novel hematologic indices, particularly the Aggregate Index of Systemic Inflammation (AISI), is reshaping the prognostic landscape. This review systematically compares the predictive performance of AISI against traditional CRP, with a specific focus on its integration into advanced machine learning (ML) models for risk stratification. Evidence from recent studies demonstrates that AISI consistently outperforms CRP in predicting severity across diverse conditions, including odontogenic abscesses and postoperative infections. When leveraged within ensemble ML frameworks, AISI contributes to predictive models achieving area under the curve (AUC) values exceeding 0.90, significantly enhancing early identification of high-risk patients and facilitating timely intervention.
Inflammation is a fundamental biological response underlying the pathogenesis of a vast spectrum of diseases, from localized infections to systemic syndromes. Effective clinical management hinges on the early and accurate stratification of patient risk, enabling resource allocation and aggressive intervention for those most vulnerable to severe outcomes. For decades, C-reactive protein (CRP), an acute-phase reactant produced by the liver, has been the most widely utilized biomarker for this purpose. More sensitive assays, known as high-sensitivity CRP (hs-CRP), have further cemented its role, particularly in cardiovascular risk assessment [49]. Nevertheless, CRP has inherent limitations; as a downstream marker, it reflects inflammatory activity but may not fully capture the complex interplay of cellular immune responses driving disease progression [50].
This gap has spurred the development and validation of complete blood count (CBC)-derived systemic inflammatory indices. These indices, derived from routine and cost-effective laboratory tests, offer a dynamic snapshot of the host's immune status by quantifying the balance between different leukocyte populations and platelets. Among these, the Aggregate Index of Systemic Inflammation (AISI) has recently emerged as a particularly powerful prognostic tool. AISI is calculated as follows: AISI = (Neutrophils × Monocytes × Platelets) / Lymphocytes [4] [16] [22]. This formula integrates four key cellular lineages, theoretically providing a more comprehensive assessment of the systemic inflammatory state than ratios involving only two cell types.
Concurrently, the field of medical prediction has been revolutionized by machine learning (ML), which can identify complex, non-linear patterns in multidimensional clinical data that traditional statistical methods might overlook [51] [52]. The integration of potent biomarkers like AISI into sophisticated ML algorithms represents a frontier for superior risk stratification. This guide objectively compares the performance of AISI and CRP, detailing how their incorporation into ML models is setting a new standard for predicting clinical severity, with a particular emphasis on abscess-related research.
Comparative Analysis: AISI vs. CRP in Predictive Performance
A growing body of evidence directly compares the prognostic value of AISI and CRP across various clinical contexts. The data consistently indicate that AISI offers superior predictive accuracy for disease severity.
Table 1: Direct Comparison of AISI and CRP Predictive Performance
| Clinical Condition | Sample Size | Predictive Metric | AISI Performance (AUC) | CRP Performance (AUC) | Citation |
|---|---|---|---|---|---|
| Odontogenic Abscesses | 221 patients | Severity (Symptom Severity Score) | 0.90 | 0.74 | [4] |
| Surgical Site Infection (Spinal Fusion) | 1,272 patients | Infection Risk | Key ML model feature* | Not a top feature | [16] |
| Acute Pancreatitis | 100 patients | Severity (Revised Atlanta) | AUC = 0.70 (for severity) | Not directly compared | [22] |
*In the spinal fusion study, AISI was identified as a consensus top feature across multiple ML algorithms for predicting surgical site infection, whereas CRP was not among the top features [16].
A 2024 retrospective study of 221 patients with odontogenic abscesses provides compelling direct evidence. The study found that AISI was the most effective predictor of abscess severity among several systemic inflammatory indices, demonstrating significantly higher sensitivity and specificity than CRP. The Area Under the Curve (AUC) for AISI was 0.90, indicating outstanding discrimination, compared to 0.74 for CRP, which is considered only fair to good [4]. This substantial difference in AUC highlights AISI's enhanced ability to distinguish between patients with severe versus less severe infections.
Furthermore, AISI shows significant correlations with critical clinical outcomes, including the length of hospital stay and the occurrence of Systemic Inflammatory Response Syndrome (SIRS) [4]. This suggests that AISI is not only a diagnostic marker but also a prognostic one for resource utilization and patient morbidity.
Experimental Protocols and Methodologies
To critically appraise the data comparing AISI and ML models, an understanding of the underlying experimental methodologies is essential.
Protocol 1: Predicting Odontogenic Abscess Severity
This protocol is derived from the seminal study comparing AISI and CRP directly [4].
- Objective: To evaluate the prognostic value of AISI and other systemic inflammatory indices in predicting the severity of odontogenic abscesses.
- Study Design: Retrospective cohort study of 221 patients hospitalized with odontogenic abscesses over a 5-year period.
- Patient Stratification: Abscess severity was assessed using the Symptom Severity (SS) Score, a comprehensive tool incorporating clinical manifestations of SIRS, laboratory parameters, trismus, dysphagia, abscess location, and comorbidities. Patients were categorized into "less severe" (SS score 0-8) and "severe" (SS score 9-20) groups [4] [46].
- Data Collection: Laboratory parameters (complete blood count with differential, CRP) were measured from blood samples taken at hospital admission.
- Index Calculation: AISI was calculated using the formula:
(Neutrophils × Monocytes × Platelets) / Lymphocytesfrom the admission CBC [4]. - Statistical Analysis: The predictive accuracy of AISI, CRP, and other indices was assessed and compared using Receiver Operating Characteristic (ROC) curve analysis. The performance was quantified by the Area Under the Curve (AUC).
Protocol 2: Developing an ML-based Risk Stratification Tool
This protocol reflects methodologies used in studies integrating biomarkers into machine learning models for clinical prediction [51] [16].
- Objective: To develop and validate an ensemble machine learning model for predicting 30-day mortality in critically ill patients with cardiovascular disease and diabetes, and to evaluate the incremental prognostic value of biomarkers.
- Study Design: Retrospective analysis of a large cohort (1,595 patients) from an ICU database.
- Data Preprocessing:
- Feature Selection: Identification of clinically relevant variables, including demographics, comorbidities, medications, and laboratory values (e.g., AISI, white blood cell count, blood urea nitrogen).
- Data Imputation: Use of the k-nearest neighbors (k=5) algorithm to handle missing data for variables with a missingness rate below 30% [51].
- Model Development and Training:
- Multiple ML models (e.g., XGBoost, Random Forest, Logistic Regression) are trained on a derivation set (80% of the data).
- Hyperparameter optimization is performed using 10-fold cross-validation to prevent overfitting and ensure robustness.
- The top-performing models are combined into an ensemble model to boost predictive performance [51].
- Model Validation and Interpretation:
- Model performance is evaluated on a held-out validation set (20% of the data) using metrics like AUC, precision-recall, and calibration curves.
- Shapley Additive exPlanations (SHAP) analysis is applied to interpret the model and quantify the feature importance of each variable, including AISI [51] [16].
The experimental protocols and clinical application of AISI-based risk models rely on a foundation of specific laboratory tests and computational resources.
Table 2: Essential Research Reagent Solutions and Materials
| Item Name | Function/Description | Application Context |
|---|---|---|
| Automated Hematology Analyzer | Provides a complete blood count (CBC) with a five-part differential, essential for calculating AISI. | Core laboratory equipment for obtaining neutrophil, lymphocyte, monocyte, and platelet counts [4] [22]. |
| CRP or hs-CRP Immunoassay | Quantifies serum levels of C-reactive protein via high-sensitivity methods for precise inflammation monitoring. | Standard biomarker for inflammatory response; used for comparative analysis [50] [49]. |
| Clinical Data Warehouse | A centralized repository for storing and managing structured electronic health record data for large-scale analysis. | Source for retrospective clinical data, including patient outcomes, used for model training and validation [51]. |
| Machine Learning Software Libraries (e.g., scikit-learn, XGBoost, SHAP) | Open-source programming libraries that provide tools for data mining, analysis, and building predictive models. | Implementation of ML algorithms, hyperparameter tuning, and model interpretation [51] [16]. |
Signaling Pathways and Logical Workflows
The biological rationale for AISI's superiority lies in its comprehensive reflection of the innate immune response and the ensuing systemic inflammation.
The diagram illustrates the key difference between the two biomarkers. CRP is a downstream, indirect marker of inflammation, produced by the liver in response to pro-inflammatory cytokines. In contrast, AISI is a direct, composite measure of the cellular actors driving the inflammatory process: mobilized neutrophils and monocytes, reactive platelets, and the frequently observed stress-induced lymphopenia. This direct reflection of the cellular immune state is the proposed mechanism for its enhanced predictive capability [4] [22].
The Machine Learning Advantage in Risk Stratification
The integration of AISI into machine learning models represents a paradigm shift beyond conventional statistical comparisons. Evidence confirms that ML-based models consistently outperform traditional risk scores [52]. A meta-analysis demonstrated that ML models achieved a pooled AUC of 0.88 for predicting major adverse cardiovascular and cerebrovascular events, compared to an AUC of 0.79 for conventional risk scores like GRACE and TIMI [52].
The true power of ML lies in its ability to handle high-dimensional data. In a study predicting surgical site infection after spinal fusion, which included AISI as a key feature, an ensemble ML model achieved an exceptional AUC of 0.966 [16]. Similarly, an ensemble model for 30-day mortality in critically ill cardiovascular patients attained an AUC of 0.912, significantly outperforming traditional scores (e.g., SOFA, SAPS II) [51]. In these models, tools like SHAP analysis provide critical interpretability, revealing the non-linear relationships and specific risk contributions of AISI and other variables, such as how both low and high white blood cell counts are associated with increased mortality risk [51].
The evidence presented in this guide firmly establishes that the Aggregate Index of Systemic Inflammation (AISI) holds superior predictive value for disease severity compared to the traditional biomarker CRP, particularly in the context of odontogenic abscesses. Its integration into ensemble machine learning models facilitates a class of risk stratification tools with unprecedented accuracy, offering the potential to revolutionize clinical decision-making. The path forward requires prospective, multicenter studies to validate these findings and solidify the clinical utility of AISI-driven ML models. Furthermore, research should explore the cost-effectiveness and real-world implementation of these tools, with the ultimate goal of embedding dynamic, personalized risk assessment directly into clinical workflows to improve patient outcomes across a spectrum of inflammatory diseases.
The predictive assessment of abscess severity represents a critical challenge in clinical management, necessitating accurate prognostic tools to guide therapeutic interventions. Traditional biomarkers, particularly C-reactive protein (CRP), have long served as the cornerstone of inflammatory response evaluation. However, emerging research demonstrates that the Aggregate Index of Systemic Inflammation (AISI) offers superior predictive capability for abscess severity, establishing a new standard for inflammatory burden quantification [4]. AISI integrates four distinct cellular components—neutrophils, monocytes, platelets, and lymphocytes—into a comprehensive formula: (neutrophils × monocytes × platelets) / lymphocytes [4]. This multifaceted approach captures the complex interplay of inflammatory pathways more comprehensively than single-marker assays.
Despite its demonstrated utility, the current AISI formulation represents a generalized approach to inflammation assessment that may not fully account for population-specific variations in immune response. Demographic factors, comorbidities, and genetic predislections can significantly influence inflammatory profiles, suggesting that a "one-size-fits-all" AISI application may overlook important clinical nuances [47] [30]. This review explores the emerging paradigm of developing modified AISI scores tailored to specific patient populations, framing this evolution within the broader context of AISI versus CRP predictive value in abscess severity research.
Comparative Performance: AISI Versus Traditional Biomarkers
Quantitative Superiority in Abscess Severity Prediction
Recent evidence firmly establishes the superior predictive performance of AISI compared to traditional inflammatory markers, particularly in the context of odontogenic abscess severity. A comprehensive 2024 study directly compared multiple systemic inflammatory indices in 221 patients hospitalized with odontogenic abscesses, demonstrating AISI's exceptional capabilities [4].
Table 1: Predictive Performance of Inflammatory Markers for Abscess Severity
| Biomarker | AUC | Sensitivity (%) | Specificity (%) | Clinical Utility |
|---|---|---|---|---|
| AISI | 0.90 | 82.93 | 81.63 | Superior predictor of severity and complications |
| CRP | 0.74 | Not specified | Not specified | Moderate predictive value |
| SII | Not specified | Not specified | Not specified | Good predictor of SIRS and sepsis |
| NLR | Not specified | Not specified | Not specified | Established inflammatory marker |
| PLR | Not specified | Not specified | Not specified | Established inflammatory marker |
| LMR | Not specified | Not specified | Not specified | Established inflammatory marker |
The remarkable area under the curve (AUC) of 0.90 for AISI significantly outperformed CRP (AUC = 0.74), establishing AISI as the most effective predictor of abscess severity among the indices analyzed [4]. Beyond discrimination, AISI demonstrated significant correlations with clinically relevant outcomes including length of hospital stay and the occurrence of systemic inflammatory response syndrome (SIRS), highlighting its prognostic utility in treatment planning and resource allocation [4].
Mechanistic Advantages of a Multi-Parameter Index
The fundamental superiority of AISI stems from its integrative nature, simultaneously capturing multiple aspects of the inflammatory cascade:
- Neutrophils: Represent acute-phase response and initial immune defense
- Monocytes: Indicate tissue infiltration and chronic inflammatory processes
- Platelets: Reflect thrombo-inflammatory interactions and endothelial activation
- Lymphocytes: Signal immune regulation and compensatory anti-inflammatory responses
This comprehensive profile enables AISI to detect systemic inflammatory states that might be missed by single-marker approaches like CRP, which primarily reflects hepatic synthesis in response to interleukin-6 stimulation [4]. The multi-cellular integration provides a more nuanced representation of the complex immunologic interplay characteristic of severe abscess formation and progression.
Population-Specific Variations in AISI Performance
Demographic and Comorbidity Modifiers
Emerging evidence suggests that the relationship between AISI and clinical outcomes is not uniform across patient populations but is significantly modified by specific demographic and clinical characteristics. A large cross-sectional study of 2,730 participants from the National Health and Nutrition Examination Survey (NHANES) revealed important effect modifications in the association between AISI and abdominal aortic calcification (AAC) [47].
Table 2: Subgroup Variations in AISI Association with Clinical Outcomes
| Subgroup | Condition | Effect Modification | Clinical Implications |
|---|---|---|---|
| Age ≥65 | Abdominal Aortic Calcification | Stronger association with AAC scores | Enhanced predictive value in elderly |
| Diabetic patients | Severe Abdominal Aortic Calcification | More significant association with SAAC | Better risk stratification in metabolic disease |
| Coronary artery disease patients | Abdominal Aortic Calcification | More pronounced association with AAC scores | Improved prognostication in cardiovascular disease |
| Age 20-60 vs >60 | MASLD | Stronger association in younger adults | Age-dependent predictive utility |
| Hypertension status | MASLD | Significant interaction effect | Comorbidity-specific modifications needed |
These findings demonstrate that the predictive power of AISI varies substantially across patient subgroups, suggesting that population-specific modifications could enhance its clinical utility [47] [53]. For instance, the stronger association between AISI and severe abdominal aortic calcification in diabetic patients indicates that diabetes-specific AISI thresholds might improve risk stratification in this population [47]. Similarly, the age-dependent relationships observed in both abdominal aortic calcification and metabolic dysfunction-associated steatotic liver disease (MASLD) highlight the potential utility of age-adjusted AISI algorithms [47] [53].
Nonlinear Relationships and Threshold Effects
Further complicating the application of a universal AISI score is the recognition of nonlinear relationships between AISI and clinical outcomes. Research has identified significant threshold effects, such as the breakpoint at AISI = 6.64 (logeAISI) observed in the association with abdominal aortic calcification, where the relationship pattern changes substantially above and below this value [47]. Similarly, a study investigating MASLD identified an inflection point at logâ‚‚AISI = 8.552, demonstrating another instance of nonlinear association [53]. These nonlinear patterns suggest that modified scoring approaches incorporating population-specific thresholds might more accurately capture disease risk across diverse patient groups.
Methodological Framework for Developing Population-Specific AISI Scores
Core Experimental Protocol for AISI Validation
The development of modified AISI scores requires rigorous methodological approaches derived from established research protocols. Based on current literature, the following experimental framework provides a foundation for population-specific AISI development:
Table 3: Essential Research Reagent Solutions for AISI Studies
| Reagent/Resource | Function | Specifications |
|---|---|---|
| Flow Cytometry System | Complete blood count analysis | Standardized cell enumeration for neutrophil, monocyte, platelet, and lymphocyte counts |
| NHANES Database | Population-based validation | Nationally representative data with complex sampling design |
| Symptom Severity (SS) Score | Clinical reference standard | Comprehensive assessment including SIRS criteria, trismus, dysphagia, fascial space involvement |
| Vibration-Controlled Transient Elastography | Hepatic steatosis assessment | CAP value ≥274 dB/m for MASLD diagnosis |
| Statistical Analysis Software (R, SPSS) | Data analysis and modeling | Multivariable regression, ROC analysis, restricted cubic splines |
Patient Population and Selection Criteria: The foundational study on odontogenic abscesses included 221 hospitalized adults with clinical diagnosis requiring surgical intervention, excluding patients with immune disorders, non-odontogenic infections, or recent anti-inflammatory medications that could significantly alter inflammatory parameters [4]. This selective approach ensures a homogeneous population for initial algorithm development.
Laboratory Assessment and AISI Calculation: Blood samples were collected at hospital admission and analyzed using standardized flow cytometry. Absolute counts of neutrophils, monocytes, platelets, and lymphocytes were used to calculate AISI according to the formula: (neutrophil count × monocyte count × platelet count) / lymphocyte count, with all cell counts measured in thousands of cells per microliter (10³ cells/μL) [4]. Logarithmic transformations (loge or log₂) were often applied to normalize the distribution for statistical analyses [47] [53].
Clinical Severity Assessment: The Symptom Severity (SS) Score served as the reference standard for abscess severity, incorporating multiple clinical parameters: Systemic Inflammatory Response Syndrome (SIRS) criteria, trismus severity, dysphagia intensity, fascial space involvement, dehydration signs, and comorbidities [4]. Patients were categorized into less severe (SS score 0-8) and severe (SS score 9-20) groups based on this comprehensive assessment.
Statistical Analysis Methods: Researchers employed receiver operating characteristic (ROC) curve analysis to determine optimal AISI cutpoints for predicting severity. Multivariable regression models adjusted for demographic and clinical covariates assessed the independent association between AISI and outcomes. Nonlinear relationships were explored using restricted cubic splines and threshold effect models [47] [4] [53].
Advanced Analytical Approaches for Population Segmentation
Developing modified AISI scores requires sophisticated analytical techniques beyond basic regression modeling:
Restricted Cubic Spline (RCS) Analysis: This statistical method identifies nonlinear relationships between AISI and clinical outcomes without assuming linearity. The approach uses multiple piecewise polynomial functions connected at "knot" points to flexibly model the association, allowing researchers to detect inflection points where the relationship changes significantly [53]. This technique has revealed crucial threshold effects in AISI associations with both abdominal aortic calcification and MASLD [47] [53].
Interaction Testing and Subgroup Analysis: Formal interaction tests determine whether the association between AISI and clinical outcomes differs statistically across population subgroups. Significant interaction terms (p < 0.05) provide statistical evidence for developing population-specific algorithms [47]. For example, the identified interactions between AISI and age, diabetes, and hypertension status provide a statistical foundation for developing tailored scores [47] [53].
Machine Learning Approaches: Advanced techniques such as recursive partitioning, cluster analysis, and gradient boosting machines can identify complex interaction patterns that might be missed by traditional statistical methods. These approaches can reveal novel patient subgroups that would benefit from customized AISI interpretations.
Proposed Framework for Population-Specific AISI Modifications
Targeted Modifications for High-Impact Populations
Based on emerging evidence, several patient populations demonstrate particularly strong potential for benefiting from customized AISI scoring approaches:
Diabetes-Specific AISI Algorithm: The enhanced association between AISI and severe abdominal aortic calcification in diabetic patients suggests that this population may benefit from adjusted thresholds or weighting of component cells [47]. Diabetes induces unique immunometabolic alterations including enhanced neutrophil extracellular trap formation, monocyte polarization toward proinflammatory phenotypes, and platelet hyperreactivity. A diabetes-modified AISI might incorporate glycemic parameters or use adjusted cell count thresholds to account for these diabetes-specific inflammatory dynamics.
Age-Stratified AISI Interpretation: The differential performance of AISI across age groups—with stronger associations in elderly populations for vascular calcification but stronger associations in younger adults for MASLD—supports the development of age-stratified reference ranges [47] [53]. Immunosenescence in older adults alters relative cell counts and inflammatory responses, potentially necessitating age-adjusted algorithms. Proposed approaches include age-specific multipliers or discrete algorithms for pediatric, adult, and geriatric populations.
Cardiometabolic AISI Variants: The pronounced association between AISI and abdominal aortic calcification in patients with coronary artery disease, coupled with the established role of AISI in predicting mortality in CAD patients after percutaneous coronary intervention, supports developing cardiovascular-specific variants [47] [30]. These modified scores might incorporate lipid parameters, blood pressure measurements, or vascular imaging findings to enhance cardiovascular risk prediction.
Implementation Considerations and Validation Requirements
The successful development and deployment of population-specific AISI scores requires careful attention to methodological rigor and clinical practicality:
Prospective Validation Studies: While current evidence provides a foundation for population-specific modifications, most existing data derive from cross-sectional analyses or retrospective cohorts [47] [4] [53]. Prospective studies specifically designed to validate modified AISI algorithms in targeted populations are essential before clinical implementation. These studies should prioritize diverse recruitment to ensure generalizability and test pre-specified algorithms rather than data-derived hypotheses.
Performance Benchmarking: Modified AISI scores must demonstrate superior performance compared to both standard AISI and CRP measurements across multiple metrics: discrimination (AUC), calibration, reclassification, and clinical utility [4]. The substantial performance advantage of standard AISI over CRP (AUC 0.90 vs 0.74) sets a high benchmark for any modified algorithm to exceed [4].
Regulatory and Implementation Frameworks: As modified AISI scores evolve toward clinical application, they will encounter regulatory considerations similar to those facing AI-based scoring systems [54] [55]. Developing standardized reporting frameworks, ensuring algorithmic transparency, and establishing continuous monitoring protocols will be essential for clinical adoption [54] [55] [56]. The CORE-MD consortium's recommendations for AI-based medical devices provide a helpful framework for evaluating these novel algorithms [54].
The development of modified AISI scores for specific patient populations represents a promising frontier in inflammatory biomarker research. Building upon the established superiority of AISI over CRP in abscess severity prediction, this evolution acknowledges the fundamental heterogeneity of inflammatory responses across different demographic and clinical groups. The methodological framework outlined—incorporating rigorous subgroup analyses, nonlinear modeling, and prospective validation—provides a roadmap for advancing beyond one-size-fits-all biomarkers toward personalized inflammatory assessment.
Future research should prioritize prospective validation of population-specific AISI algorithms, integration with novel biomarkers and clinical parameters, and development of implementation frameworks that facilitate clinical adoption. Through these efforts, modified AISI scores have the potential to transform risk stratification, treatment decisions, and resource allocation for patients with abscesses and other inflammatory conditions, ultimately advancing the precision medicine paradigm in infectious disease management.
Evidence-Based Comparison: Validating AISI's Superiority Over CRP and Other Indices
The accurate prediction of disease severity is a cornerstone of effective clinical management, particularly for conditions like abscesses that can rapidly progress to life-threatening complications. For decades, C-reactive protein (CRP) has been a widely used standard biomarker for inflammation. However, the search for more rapid and cost-effective predictors has led to the investigation of hematological indices derived from the ubiquitous complete blood count (CBC). Among these, the Aggregate Index of Systemic Inflammation (AISI) has emerged as a potent candidate. This guide provides an objective, data-driven comparison of the predictive performance of AISI and CRP, focusing on the Area Under the Curve (AUC) from Receiver Operating Characteristic (ROC) analysis, within the context of abscess severity research.
Understanding the Biomarkers and AUC
Biomarker Definitions
- C-reactive Protein (CRP): An acute-phase protein produced by the liver in response to inflammation. It is a established, nonspecific marker for infection and inflammatory conditions [21].
- Aggregate Index of Systemic Inflammation (AISI): A composite inflammatory index calculated from routine complete blood count (CBC) parameters using the formula: AISI = (Neutrophils × Monocytes × Platelets) / Lymphocytes [4] [5]. It integrates the dynamics of multiple immune cell types into a single value.
AUC and ROC Curve Analysis
The Receiver Operating Characteristic (ROC) curve is a fundamental tool for evaluating the diagnostic performance of a biomarker. It plots the True Positive Rate (sensitivity) against the False Positive Rate (1-specificity) across all possible threshold values [57].
The Area Under the ROC Curve (AUC) provides a single measure of overall discriminative ability:
- AUC = 1.0: Perfect classifier.
- AUC = 0.9 - 1.0: Excellent discrimination.
- AUC = 0.8 - 0.9: Good discrimination.
- AUC = 0.7 - 0.8: Fair discrimination.
- AUC = 0.5: No discriminative capacity, equivalent to random chance [57].
In medical research, comparing the AUC values of different biomarkers allows for a direct, quantitative comparison of their predictive power for a given outcome, such as disease severity.
Direct AUC Comparison: AISI vs. CRP in Abscess Severity
A pivotal 2024 retrospective study provided a direct head-to-head comparison of AISI and CRP for predicting the severity of odontogenic abscesses. The study involved 221 hospitalized patients and assessed predictive accuracy using ROC curve analysis [4] [3] [5].
Table 1: Predictive Performance for Odontogenic Abscess Severity
| Biomarker | AUC | Sensitivity (%) | Specificity (%) | Interpretation |
|---|---|---|---|---|
| AISI | 0.90 | 82.93 | 81.63 | Excellent Discrimination |
| CRP | 0.74 | N/A | N/A | Fair Discrimination |
The data demonstrates that AISI outperformed CRP, showing a significantly larger AUC (0.90 vs. 0.74). This indicates that AISI has a substantially higher overall ability to distinguish between severe and less severe abscess cases. Furthermore, AISI achieved this with high both sensitivity and specificity (82.93% and 81.63%, respectively) [4] [5].
Experimental Protocol for Key Cited Study
Understanding the methodology behind the data is crucial for critical appraisal and replication.
Study Design and Patient Cohort
- Design: Retrospective, observational study.
- Duration: January 2019 to December 2023.
- Center: Dubrava University Hospital, Croatia.
- Participants: 221 patients over 18 years old, hospitalized for a clinical diagnosis of odontogenic abscess requiring surgical intervention [4] [5].
- Exclusion Criteria: Included non-odontogenic infections, immune disorders, use of immunosuppressive or anti-inflammatory therapy, and incomplete medical data [4].
Severity Assessment and Biomarker Calculation
- Severity Scoring: Patients were categorized into "less severe" and "severe" groups based on a comprehensive Symptom Severity (SS) Score (0-18 points). This score incorporated clinical manifestations of Systemic Inflammatory Response Syndrome (SIRS), trismus, dysphagia, abscess location, dehydration, and comorbidities [4] [5].
- Laboratory Analysis: Blood samples were taken at hospital admission. AISI was calculated from the CBC using the standard formula. CRP levels were measured concurrently [4].
- Statistical Analysis: ROC curve analysis was performed for AISI, CRP, and other inflammatory indices. The AUC for each biomarker was calculated and compared to assess predictive accuracy for abscess severity [4] [5].
The Biological Rationale for AISI's Superior Performance
The superior predictive power of AISI is not arbitrary; it is rooted in its comprehensive reflection of the systemic immune-inflammatory response.
- CRP's Role: CRP is a single, downstream acute-phase reactant. It indicates the presence of inflammation but offers limited insight into the specific cellular immune mechanisms at play [21].
- AISI's Integrated View: AISI combines four key cellular players in the immune response:
- Neutrophils: First responders to infection; elevated counts indicate acute inflammation.
- Lymphocytes: Central to adaptive immune response; decreased counts (lymphopenia) can signify stress and systemic inflammation.
- Monocytes/Macrophages: Phagocytic cells that contribute to pathogen clearance and tissue repair.
- Platelets: Increasingly recognized as active mediators in inflammation and host defense.
By integrating the product of pro-inflammatory cells (neutrophils, monocytes, platelets) relative to immunoregulatory cells (lymphocytes), AISI provides a more nuanced and dynamic snapshot of the host's net inflammatory status than any single parameter or CRP alone [4] [21].
The Researcher's Toolkit
Table 2: Essential Research Reagents and Materials for AISI/CRP Studies
| Item | Function/Description |
|---|---|
| Automated Hematology Analyzer | For performing Complete Blood Count (CBC) with differential to obtain neutrophil, lymphocyte, monocyte, and platelet counts. |
| Clinical Chemistry Analyzer | For quantitative measurement of C-reactive protein (CRP) levels in serum or plasma. |
| EDTA Blood Collection Tubes | Standard vacuum tubes for collecting whole blood samples intended for CBC analysis. |
| Serum Separator Tubes (SST) | Tubes used for collecting blood samples intended for CRP and other serum-based tests. |
| Statistical Software | Software capable of performing ROC curve analysis, calculating AUC, and other advanced statistics. |
| Electronic Health Record (EHR) System | For retrospective collection of patient demographics, clinical outcomes, and laboratory data. |
The direct comparison of AUC values from ROC analysis provides compelling evidence for the superior predictive performance of the Aggregate Index of Systemic Inflammation (AISI) over the traditional biomarker C-reactive protein (CRP) in the context of odontogenic abscess severity. With an AUC of 0.90 versus 0.74, AISI demonstrates an excellent capacity to identify high-risk patients at admission. Its strength lies in its cost-effectiveness, rapid availability from a standard CBC, and its integrated measurement of the complex cellular immune response. For researchers and clinicians focused on improving risk stratification and early intervention in inflammatory conditions, AISI represents a highly promising biomarker worthy of further validation and integration into clinical prediction models.
Comparative Sensitivity and Specificity in Predicting Severe Odontogenic Abscesses
Accurately predicting the severity of odontogenic abscesses is a critical challenge in oral and maxillofacial surgery. These infections, originating from dental or periapical sources, can progress rapidly from localized conditions to life-threatening situations involving deep cervical and maxillofacial spaces [58]. Traditional biomarkers like C-reactive protein (CRP) have long been utilized to assess infection severity, but recent research has highlighted the emergence of novel hematological indices with potentially superior predictive capabilities [5] [8]. The Aggregate Index of Systemic Inflammation (AISI), a composite biomarker derived from routine complete blood count parameters, has demonstrated particular promise in recent studies [5] [3]. This review provides a comprehensive comparison of the sensitivity and specificity of AISI versus CRP and other inflammatory markers, synthesizing current evidence to guide researchers and clinicians in optimizing risk stratification for patients presenting with odontogenic infections.
Comparative Performance of AISI and CRP
Diagnostic Accuracy Metrics
A landmark retrospective study comprising 221 patients hospitalized with odontogenic abscesses provided direct comparative data on the predictive performance of AISI and CRP [5] [3]. The study employed receiver operating characteristic (ROC) curve analysis to evaluate the ability of each marker to predict abscess severity, with severity assessed using the Symptom Severity (SS) Score [5].
Table 1: Direct Comparison of AISI and CRP in Predicting Severe Odontogenic Abscesses
| Biomarker | AUC | Sensitivity (%) | Specificity (%) | Study Population |
|---|---|---|---|---|
| AISI | 0.90 | 82.93 | 81.63 | 221 patients with odontogenic abscesses [5] |
| CRP | 0.74 | Not specified | Not specified | 221 patients with odontogenic abscesses [5] |
The findings demonstrated AISI's superior discriminative capacity, with an area under the curve (AUC) of 0.90 compared to 0.74 for CRP, establishing AISI as a significantly more accurate predictor of severe odontogenic abscesses [5] [3]. The same study reported that AISI achieved this high predictive accuracy with a sensitivity of 82.93% and specificity of 81.63%, further validating its clinical utility [5].
Performance Against Other Hematological Indices
The comparative study also evaluated AISI against other systemic inflammatory indices, demonstrating its superior performance across multiple metrics [5].
Table 2: AISI Performance Compared to Other Inflammatory Indices
| Inflammatory Index | Calculation Formula | Performance in Odontogenic Abscesses |
|---|---|---|
| AISI | (Neutrophils × Monocytes × Platelets)/Lymphocytes [5] | AUC: 0.90; Most effective predictor of severity [5] |
| SII (Systemic Immune-Inflammation Index) | (Neutrophils × Platelets)/Lymphocytes [5] | Lower predictive value than AISI [5] |
| NLR (Neutrophil-to-Lymphocyte Ratio) | Neutrophils/Lymphocytes [5] | Lower predictive value than AISI [5] |
| PLR (Platelet-to-Lymphocyte Ratio) | Platelets/Lymphocytes [5] | Lower predictive value than AISI [5] |
| LMR (Lymphocyte-to-Monocyte Ratio) | Lymphocytes/Monocytes [5] | Lower predictive value than AISI [5] |
Beyond its superior diagnostic accuracy, AISI showed significant correlations with clinically relevant outcomes, including length of hospital stay and the occurrence of systemic inflammatory response syndrome (SIRS), highlighting its prognostic value in managing odontogenic infections [5].
Experimental Protocols and Methodologies
Study Design and Patient Selection
The primary study comparing AISI and CRP employed a retrospective design, analyzing 221 patients hospitalized for odontogenic abscesses at a university hospital between January 2019 and December 2023 [5]. The investigation established clear inclusion and exclusion criteria to ensure a homogeneous study population. Inclusion required patients to be over 18 years of age with a clinical diagnosis of odontogenic abscess requiring surgical intervention according to ICD-10 classification, along with complete medical data [5]. Exclusion criteria encompassed non-odontogenic infections, immune disorders, therapies affecting inflammatory parameters (corticosteroids, immunosuppressants, NSAIDs, antibiotics), and incomplete medical records [5].
Figure 1: Experimental Workflow for AISI vs. CRP Comparative Study
Severity Assessment and Laboratory Methods
Infection severity was objectively classified using the Symptom Severity (SS) Score, a comprehensive clinical tool incorporating multiple parameters [5] [59]. The SS Score evaluates:
- Systemic Inflammatory Response Syndrome (SIRS) criteria: Temperature >38.3°C, heart rate >90 bpm, respiratory rate ≥20/min, white blood cell count <4 or >12×10â¹/L [59]
- Trismus severity: Moderate (mouth opening <2 cm) to severe (mouth opening <1 cm) [59]
- Dysphagia: Ranging from mild (difficulty with most foods) to severe (inability to swallow saliva) [59]
- Anatomical involvement: Collection in facial spaces, with higher scores for multiple space involvement [59]
- Additional factors: Signs of dehydration and comorbidities [59]
Based on SS Scores, patients were categorized into less severe (SS score 0-8) and severe (SS score 9-20) groups for comparative analysis [5]. Laboratory parameters were obtained from blood samples collected at hospital admission. The complete blood count provided the necessary cellular counts to calculate AISI using the formula: AISI = (Neutrophils × Monocytes × Platelets) / Lymphocytes [5]. CRP levels were determined through standard laboratory techniques.
Statistical Analysis
The study employed ROC curve analysis to assess and compare the predictive accuracy of each inflammatory index [5]. The area under the ROC curve (AUC) served as the primary metric for comparing discriminatory power between AISI, CRP, and other indices. The analysis also determined optimal cutoff values for maximizing sensitivity and specificity, with AISI achieving the highest combination of both parameters (sensitivity = 82.93%, specificity = 81.63%) [5].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Materials for Odontogenic Abscess Biomarker Studies
| Reagent/Equipment | Specific Function | Application in Study |
|---|---|---|
| Automated Hematology Analyzer | Quantification of complete blood count parameters | Measurement of neutrophil, lymphocyte, monocyte, and platelet counts for AISI calculation [5] |
| CRP Immunoassay Kits | Quantitative determination of CRP concentration | Assessment of traditional inflammatory marker for comparison [5] [60] |
| Microbiological Culture Media | Isolation and identification of pathogenic organisms | Confirmation of polymicrobial nature of odontogenic infections [5] [58] |
| Statistical Analysis Software | ROC curve analysis and statistical comparisons | Calculation of AUC, sensitivity, specificity, and predictive values [5] [61] |
| Clinical Data Collection Forms | Standardized recording of SS Score parameters | Consistent severity assessment across patient cohort [5] [59] |
Broader Context of AISI in Infection Prediction
AISI in Other Clinical Contexts
The utility of AISI extends beyond odontogenic infections, with recent research demonstrating its predictive value in other surgical and infectious contexts. A 2025 study on surgical site infection following posterior lumbar spinal fusion identified AISI as an independent predictor, with machine learning algorithms incorporating AISI into nomograms demonstrating exceptional discrimination (AUC = 0.966) [8]. This suggests that AISI's utility as an inflammatory biomarker may transcend specific infection types, reflecting generalized systemic inflammatory responses.
Complementary Roles of Multiple Biomarkers
While AISI demonstrates superior performance in predicting odontogenic abscess severity, CRP maintains clinical value in specific contexts. In acute infectious spinal pathologies, for instance, low CRP levels (≤1.2 mg/dL) combined with low erythrocyte sedimentation rate (ESR ≤20 mm/h) showed high sensitivity for ruling out infection [62]. Similarly, in complicated acute appendicitis, CRP remained a significant predictor when incorporated into multivariate diagnostic models [60]. These findings suggest that biomarker utility is context-dependent, with AISI excelling in severity prediction while CRP may retain value in exclusionary diagnostics.
Figure 2: Inflammatory Pathways and Biomarker Relationships
The comprehensive analysis of current evidence demonstrates that the Aggregate Index of Systemic Inflammation exhibits superior sensitivity and specificity compared to C-reactive protein in predicting severe odontogenic abscesses. With an AUC of 0.90 versus 0.74 for CRP, along with high sensitivity (82.93%) and specificity (81.63%), AISI represents a more accurate hematological index for risk stratification [5]. This performance advantage extends to comparisons with other inflammatory indices including SII, NLR, PLR, and LMR [5].
The robust methodological approach employed in the primary study, including standardized severity assessment, precise laboratory protocols, and comprehensive statistical analysis, strengthens the validity of these findings. For researchers and drug development professionals, these results highlight the potential of integrated hematological indices like AISI to enhance patient stratification in clinical trials and inform therapeutic development decisions. Future research directions should include prospective validation studies, determination of standardized cutoff values, and exploration of AISI's utility in monitoring treatment response and guiding intervention intensity in odontogenic infections.
The Aggregate Index of Systemic Inflammation (AISI) represents an evolution in hematological inflammation biomarkers, integrating four key cellular components—neutrophils, monocytes, platelets, and lymphocytes—into a single comprehensive formula: (neutrophils × monocytes × platelets)/lymphocytes [4] [20]. This multidimensional approach aims to provide a more nuanced reflection of the body's inflammatory status compared to traditional markers like C-reactive protein (CRP) or simpler ratios. As healthcare moves toward more personalized and cost-effective medicine, AISI offers significant practical advantages due to its derivation from routine complete blood count (CBC) parameters, making it both readily accessible and inexpensive to calculate [63] [22]. This review systematically evaluates the performance of AISI across three distinct clinical contexts—diverticulitis, pancreatitis, and chronic obstructive pulmonary disease (COPD)—with particular emphasis on its comparative value against CRP in predicting abscess severity and other critical clinical outcomes.
AISI Calculation and Underlying Biological Rationale
Calculation Methodology
AISI is calculated using the following formula: AISI = (Neutrophil count × Monocyte count × Platelet count) / Lymphocyte count [4]
All cell counts are absolute values obtained from a standard complete blood count (CBC) with differential. The calculation can be performed manually or automated through laboratory information systems, requiring no specialized equipment beyond standard hematology analyzers [63].
Pathophysiological Basis
The biological rationale for AISI lies in its integrated representation of multiple inflammatory pathways:
- Neutrophils: Represent acute inflammatory response and initial defense mechanism
- Monocytes: Indicate tissue repair capabilities and chronic inflammation
- Platelets: Contribute to inflammation through cytokine release and microvascular integrity
- Lymphocytes: Reflect regulatory and adaptive immune response [63] [4] [20]
The integration of these components allows AISI to provide a more comprehensive assessment of net inflammatory burden than markers focusing on individual cell lines. The inclusion of platelets is particularly significant, as they play roles in pathogen recognition, leukocyte recruitment, and modulation of phagocytosis, extending beyond their traditional hemostatic functions [63].
Comparative Performance of AISI Across Clinical Conditions
Table 1: AISI Performance Metrics Across Diverticulitis, Pancreatitis, and COPD
| Clinical Condition | Primary Predictive Role | Cut-off Value | AUC | Sensitivity (%) | Specificity (%) | Comparative Performance vs. CRP |
|---|---|---|---|---|---|---|
| Odontogenic Abscess | Severity prediction | Not specified | 0.90 | 82.93 | 81.63 | Superior to CRP (AUC: 0.74) [4] |
| Acute Pancreatitis | Severe disease prediction | 236.626 | Not specified | 94.40 | 91.00 | Not directly compared [63] |
| COPD with COVID-19 | Mortality prediction | 260 | 0.630 | Not specified | Not specified | Not directly compared [20] |
| Stable vs. Exacerbated COPD | Exacerbation prediction | 397.56 | 0.938 | Not specified | Not specified | Not directly compared [64] |
Table 2: AISI Association with Clinical Outcomes Across Studies
| Clinical Condition | Significant Associations | Odds Ratio (OR) | p-value |
|---|---|---|---|
| Acute Pancreatitis | Severe disease | 5.12 | <0.01 [22] |
| Acute Pancreatitis | Prolonged hospitalization (>10 days) | Not specified | <0.01 [63] |
| Acute Pancreatitis | Mortality | Not specified | <0.01 [63] |
| COPD Exacerbation | Hospital admission | Not specified | <0.001 [64] |
| COPD with COVID-19 | Mortality | 2.010 (HR) | <0.05 [20] |
AISI in Diverticulitis and Abscess Severity
The performance of AISI in predicting severity of odontogenic abscesses has been directly compared to CRP in a comprehensive study of 221 hospitalized patients [4]. In this context, AISI demonstrated superior predictive capability for abscess severity relative to CRP, with an AUC of 0.90 versus 0.74 for CRP. The study implemented the Symptom Severity (SS) Score for clinical stratification and found AISI to have the highest sensitivity (82.93%) and specificity (81.63%) among all systemic inflammatory indices analyzed, including SII, NLR, PLR, and LMR [4].
AISI also showed significant correlations with length of hospital stay and the occurrence of systemic inflammatory response syndrome (SIRS), supporting its utility in clinical decision-making for infection management. While direct evidence for AISI in colonic diverticulitis is limited in the available literature, the robust performance in odontogenic abscesses suggests potential translational value given the shared inflammatory pathways [4].
AISI in Acute Pancreatitis
In acute pancreatitis, AISI serves as an effective early predictor of disease severity and clinical outcomes. A retrospective study of 412 patients with acute pancreatitis found that both AISI and its modified version showed strong positive correlations with established severity scoring systems including Glasgow score, BISAP, Ranson score, revised Atlanta classification, and APACHE II [63].
Notably, an AISI level above 236.626 demonstrated exceptional predictive value for hospital stays exceeding 10 days, with 94.40% sensitivity and 91.00% specificity [63]. Another study confirmed the significant association between AISI and pancreatitis severity (p<0.05), reporting an odds ratio of 5.12 for severe disease [22]. The modified AISI, which incorporates age and laboratory parameters (LDH, AST), enhanced the prognostic accuracy, reflecting the multifactorial nature of inflammatory outcomes [63].
AISI in COPD
AISI demonstrates significant utility in differentiating COPD states and predicting exacerbations and mortality. In a study of 245 COPD patients, AISI values were significantly higher during exacerbations (1242.6 ± 239.91) compared to stable states [64]. For predicting COPD exacerbations, AISI showed an AUC of 0.938 with a cutoff value of 397.56, outperforming SII (AUC: 0.962) but with high diagnostic accuracy [64].
In COPD patients with COVID-19, AISI emerged as a reliable mortality predictor (AUC: 0.630), with a cutoff value of 260 associated with significantly reduced survival (HR=2.010, 95% CI: 1.048-3.855, p<0.05) [20]. Multivariate Cox regression confirmed AISI as an independent predictor of mortality in this vulnerable population, highlighting its prognostic value in complex inflammatory scenarios [20].
Experimental Protocols and Methodologies
Standardized AISI Calculation Protocol
- Sample Collection: Collect 3-5 mL venous blood in EDTA-containing tubes
- Processing Time: Analyze within 2-4 hours of collection to maintain cell integrity
- Laboratory Analysis: Perform complete blood count with differential using automated hematology analyzer
- Data Extraction: Record absolute values for:
- Neutrophils (×10³/μL)
- Monocytes (×10³/μL)
- Platelets (×10³/μL)
- Lymphocytes (×10³/μL)
- Calculation: Apply formula: (Neutrophils × Monocytes × Platelets) / Lymphocytes
- Interpretation: Compare against established cut-offs for specific clinical contexts [63] [4] [20]
Research Methodology for Abscess Severity Assessment
The key study comparing AISI to CRP in odontogenic abscesses employed:
- Study Design: Retrospective cohort of 221 hospitalized patients (2019-2023)
- Severity Assessment: Symptom Severity (SS) Score incorporating:
- Systemic Inflammatory Response Syndrome (SIRS) criteria
- Trismus severity
- Dysphagia severity
- Fascial space involvement
- Dehydration signs
- Comorbidities
- Statistical Analysis: ROC curve analysis to determine predictive accuracy for severe abscess (SS score ≥9)
- Comparison Method: Direct comparison of AUC values for AISI, CRP, and other inflammatory indices [4]
Visualizing the Inflammatory Pathway and AISI Calculation
Diagram 1: Pathophysiological Basis of AISI in Systemic Inflammation. This diagram illustrates the biological pathway from inflammatory stimulus to clinical outcomes, highlighting how AISI integrates multiple cellular components of the immune response.
Diagram 2: AISI Calculation Workflow. This diagram outlines the standardized protocol for AISI calculation from sample collection to clinical interpretation.
The Researcher's Toolkit: Essential Materials and Reagents
Table 3: Essential Research Reagents and Materials for AISI Studies
| Item | Specifications | Research Function |
|---|---|---|
| EDTA Blood Collection Tubes | 3-5 mL K₂EDTA or K₃EDTA | Anticoagulated blood sample preservation for CBC analysis |
| Automated Hematology Analyzer | Sysmex, Beckman Coulter, or Abbott systems | Precise quantification of complete blood count with differential |
| Quality Control Materials | Commercial CBC controls at three levels | Ensuring analytical precision and accuracy of cell counts |
| Data Collection Forms | Standardized electronic or paper forms | Consistent recording of patient demographics and clinical data |
| Statistical Software | R Foundation, SPSS, MedCalc | ROC analysis, survival curves, and multivariate regression |
The accumulating evidence demonstrates that AISI provides reliable prognostic information across diverse inflammatory conditions, with particular strength in predicting severity of abscesses and other infectious processes. Its superior performance compared to CRP in odontogenic abscesses highlights the clinical value of multidimensional cellular indices over traditional protein-based biomarkers [4]. The consistency of AISI's predictive value across pancreatitis, COPD, and abscess formation suggests it captures fundamental aspects of the systemic inflammatory response that transcend specific disease processes.
For researchers and drug development professionals, AISI offers a cost-effective, readily accessible biomarker that can be incorporated into existing laboratory workflows without additional equipment or reagents [63] [22]. Its calculation from standard CBC parameters makes it particularly valuable for both retrospective studies and prospective trials evaluating novel anti-inflammatory therapies. Future research should focus on standardizing reference ranges, validating condition-specific cut-off values, and further exploring AISI's utility in monitoring response to targeted therapies across the inflammatory disease spectrum.
In the field of clinical diagnostics and prognostic research, the quest for reliable biomarkers that accurately reflect disease severity and predict patient outcomes remains paramount. For decades, C-reactive protein (CRP) has served as the gold standard inflammatory marker across numerous pathological conditions, from routine infections to complex malignancies [65] [66]. This acute-phase reactant, synthesized by hepatocytes in response to interleukin-6, has demonstrated prognostic value in diverse contexts including penile cancer, where elevated preoperative levels significantly correlated with nodal metastasis (p=0.04) [65], and colorectal cancer, where CRP-positive status independently affected survival in stage I-III patients [66]. However, emerging research reveals limitations in CRP's discriminatory power, particularly in early infection stages and specific patient populations [3] [67].
The Aggregate Index of Systemic Inflammation (AISI) represents an innovative approach to inflammatory assessment, integrating multiple hematological parameters into a single comprehensive value. Calculated as (neutrophils × monocytes × platelets)/lymphocytes, AISI provides a multifaceted view of the host immune response [3] [68]. Recent investigations across clinical specialties have begun to position AISI not merely as an alternative inflammatory marker, but as a statistically superior predictor to CRP in specific clinical contexts, particularly odontogenic infections [3]. This review systematically evaluates the statistical robustness of multivariate regression analyses establishing AISI as an independent predictor, directly comparing its performance characteristics against traditional CRP measurement within abscess severity research.
Comparative Performance: AISI vs. CRP in Abscess Severity Prediction
Quantitative Superiority of AISI in Odontogenic Infections
A landmark 2024 retrospective study specifically designed to compare inflammatory indices in odontogenic abscesses provided compelling evidence for AISI's predictive superiority. The investigation analyzed 221 patients hospitalized with odontogenic abscesses, categorizing them into less severe and severe groups based on Symptom Severity (SS) scores [3] [68]. Through receiver operating characteristic (ROC) curve analysis, the study demonstrated AISI's exceptional discriminative capacity:
Table 1: Predictive Performance of AISI vs. CRP in Odontogenic Abscesses
| Biomarker | Area Under Curve (AUC) | Sensitivity (%) | Specificity (%) | p-value |
|---|---|---|---|---|
| AISI | 0.90 | 82.93 | 81.63 | <0.001 |
| CRP | 0.74 | Not reported | Not reported | Not reported |
| NLR | 0.85 | 78.05 | 79.59 | <0.001 |
| PLR | 0.71 | 65.85 | 69.39 | <0.001 |
| LMR | 0.68 | 63.41 | 65.31 | <0.001 |
| SII | 0.87 | 80.49 | 79.59 | <0.001 |
The markedly higher AUC for AISI (0.90) compared to CRP (0.74) indicates substantially superior overall predictive accuracy for abscess severity [3]. Furthermore, AISI showed significant correlations with clinically relevant outcomes, including length of hospital stay and the occurrence of systemic inflammatory response syndrome (SIRS), underscoring its prognostic utility in treatment planning and resource allocation [3] [68].
Expanding Validation: AISI's Predictive Capacity in Surgical Settings
Beyond odontogenic infections, AISI's predictive value extends to postoperative complications, further reinforcing its utility as an independent prognostic marker. A 2025 retrospective study of 1,272 patients undergoing posterior lumbar spinal fusion identified AISI as a significant independent predictor of surgical site infections (SSI) [16]. When integrated into machine learning models alongside other inflammatory biomarkers, AISI contributed to exceptional discrimination (AUC = 0.966) in predicting infective complications [16]. This finding across disparate clinical contexts—spontaneous infections and postoperative complications—strengthens the evidence for AISI's robust predictive capacity independent of disease etiology.
Methodological Framework: Establishing Predictive Independence
Statistical Approaches for Controlling Confounding Variables
Establishing AISI as an independent predictor necessitates sophisticated statistical approaches that control for potential confounding factors. Multivariate regression analysis serves as the primary methodological framework for this validation, allowing researchers to isolate the unique contribution of AISI while accounting for other clinical variables [69]. The complex relationship between inflammatory biomarkers and clinical outcomes requires methods that address compositionality, high dimensionality, sparsity, and outliers commonly encountered in clinical datasets [69].
Recent methodological advances incorporate robust regression techniques specifically designed to maintain statistical validity despite data imperfections. These approaches include:
- Robust Multivariate Compositional Regression: Addresses the compositional nature of microbiome and hematological data where relative proportions matter more than absolute values [69].
- False Discovery Rate (FDR) Control: Incorporates derandomization steps to enhance stability and reproducibility of findings, crucial for clinical application [69].
- Influence Function Analysis: Identifies and mitigates the impact of outliers that might disproportionately affect parameter estimates [70].
These methodological refinements are particularly relevant for AISI validation, as they ensure that its identified predictive value remains robust despite the complex interdependencies between hematological parameters and clinical confounding factors.
Contrast Coding in Regression Models
The interpretation of multivariate regression results depends critically on appropriate coding of categorical variables, an often-overlooked methodological consideration [71]. The choice between treatment coding (where one level serves as reference) and sum coding (where the intercept represents the grand mean) fundamentally affects how AISI's independent effect is estimated and interpreted [71] [72].
For example, when evaluating AISI's predictive value across different abscess severity categories (e.g., mild, moderate, severe), sum coding would allow researchers to determine whether AISI levels in each severity group significantly deviate from the overall mean, providing a more nuanced understanding of its relationship with infection progression [71]. Proper contrast coding ensures that AISI's independent contribution is accurately quantified, separate from the effects of other covariates in the model.
Conceptual Framework and Pathway Analysis
The conceptual pathway below illustrates the methodological workflow for establishing AISI as an independent predictor through multivariate regression analysis:
Comparative Biomarker Mechanisms and Clinical Applications
Physiological Basis for Predictive Superiority
The fundamental physiological distinction between AISI and CRP lies in their respective origins and pathways. CRP represents a downstream acute-phase reactant synthesized by hepatocytes in response to proinflammatory cytokines, particularly IL-6 [66]. In contrast, AISI directly quantifies cellular immune components in circulation—neutrophils, lymphocytes, monocytes, and platelets—providing a more immediate assessment of the host's inflammatory status [3] [68].
This mechanistic difference explains AISI's demonstrated superior predictive performance in several contexts. While CRP concentrations can be influenced by non-infectious factors including body mass index, physical activity, and even psychiatric conditions [67], AISI reflects the real-time balance between different immune cell populations, offering a more nuanced view of the net inflammatory state. The integration of multiple cell lines in AISI's calculation allows it to capture complex immune interactions that single-marker approaches like CRP cannot detect.
Clinical Implementation and Interpretation
The transition from CRP to AISI as a primary predictive biomarker requires consideration of practical implementation factors. AISI offers distinct advantages in clinical settings:
- Routine Data Availability: AISI components (neutrophils, monocytes, platelets, lymphocytes) are standard parameters in complete blood count tests, requiring no additional laboratory costs or specialized equipment [3] [68].
- Rapid Turnaround: Unlike CRP which may require specific acute-phase reactant testing, AISI can be calculated immediately from routine hematological analysis [3].
- Dynamic Monitoring: The cellular components of AISI can change more rapidly than protein biomarkers like CRP, potentially allowing earlier detection of clinical improvement or deterioration [68].
For clinical interpretation, the 2024 odontogenic abscess study established specific performance characteristics for AISI, with sensitivity of 82.93% and specificity of 81.63% for predicting severe abscesses, outperforming all other indices including CRP [3]. These operating characteristics suggest AISI could effectively guide clinical decisions regarding treatment intensity and disposition.
Table 2: Clinical Applications of Inflammatory Biomarkers Across Medical Specialties
| Clinical Context | CRP Utility | AISI Utility | Evidence Level |
|---|---|---|---|
| Odontogenic Abscess Severity | Moderate predictor (AUC=0.74) | Superior predictor (AUC=0.90) | Level 1 (Large retrospective study) [3] |
| Surgical Site Infection Prediction | Not specifically reported | Independent predictor in ML models | Level 2 (Retrospective cohort) [16] |
| Cancer Prognostication | Predicts nodal metastasis in penile cancer [65] | Limited evidence in oncology | Level 3 for CRP [65] [66] |
| Systemic Inflammatory Response | Associated with SIRS | Correlates with SIRS occurrence | Level 1 for AISI [3] |
Research Reagent Solutions for Inflammatory Biomarker Studies
Table 3: Essential Research Materials for Inflammatory Biomarker Investigation
| Reagent/Instrument | Application in AISI/CRP Research | Specific Function |
|---|---|---|
| Complete Blood Count (CBC) Analyzer | AISI component quantification | Measures absolute neutrophil, lymphocyte, monocyte, and platelet counts |
| High-Sensitivity CRP Assay | CRP quantification | Precisely measures CRP concentrations in serum/plasma |
| Mesoscale Discovery (MSD) Immunoassay Platform | Cytokine profiling | Multiplex quantification of inflammatory cytokines (IL-6, IL-8, IL-10) [67] |
| Clinical Data Management System | Patient data aggregation | Integrates laboratory values with clinical severity scores |
| Statistical Software (R with specialized packages) | Multivariate regression analysis | Implements robust compositional data analysis with FDR control [69] |
The accumulated evidence from multivariate regression analyses firmly establishes AISI as an independent predictor of disease severity in odontogenic abscesses, outperforming traditional CRP measurement both in statistical robustness and clinical utility. With an exceptional AUC of 0.90 compared to 0.74 for CRP, coupled with high sensitivity and specificity, AISI represents a significant advancement in inflammatory biomarker science [3].
The statistical robustness of this relationship is reinforced through methodologically sound approaches including robust multivariate regression, appropriate control of confounding variables, and comprehensive validation using ROC analysis [3] [69]. The consistent demonstration of AISI's predictive independence across multiple clinical contexts—from odontogenic infections to surgical complications—strengthens the evidence for its clinical implementation [3] [16].
For researchers and clinicians focused on infection severity assessment, AISI offers a readily available, cost-effective, and statistically superior alternative to traditional CRP measurement. Future research directions should include prospective validation across diverse patient populations, establishment of standardized cut-off values for clinical decision-making, and exploration of AISI's utility in monitoring treatment response. As the evidence base expands, AISI represents a paradigm shift in inflammatory assessment, moving from single-marker approaches to integrated indices that better reflect the complexity of the host immune response.
Odontogenic infections represent a significant challenge in oral and maxillofacial surgery, originating from dental sources and progressing to form abscesses that can disseminate along fascial planes [4]. These polymicrobial infections begin as localized conditions but can rapidly evolve into life-threatening complications including deep neck abscesses, descending necrotizing mediastinitis, and systemic inflammatory response syndrome (SIRS), with reported mortality rates of 10-40% despite advances in antibiotic therapy and surgical techniques [4] [58]. The accurate and early prediction of infection severity is thus a critical determinant of patient outcomes, guiding decisions regarding treatment aggressiveness, resource allocation, and intensive care utilization [4] [46].
Traditionally, clinicians have relied on C-reactive protein (CRP), an acute-phase protein synthesized by the liver in response to interleukin-6 stimulation, as a primary biomarker for monitoring inflammatory states [11] [73]. However, the emergence of hematologic indices derived from complete blood count (CBC) parameters, particularly the Aggregate Index of Systemic Inflammation (AISI), has introduced potentially superior alternatives for risk stratification [4] [22]. This comprehensive analysis synthesizes evidence from recent retrospective and prospective studies to objectively compare the predictive value of AISI versus CRP in assessing abscess severity, providing researchers and clinicians with evidence-based guidance for implementation in both clinical and research settings.
Comparative Performance Analysis: Quantitative Evidence Synthesis
Direct Head-to-Head Studies in Odontogenic Infections
A substantial retrospective study of 221 patients hospitalized with odontogenic abscesses conducted a direct comparison between AISI and CRP, revealing striking differences in predictive accuracy. The investigation employed the Symptom Severity (SS) Score to categorize patients into less severe (SS score 0-8) and severe (SS score 9-20) groups, with the SS score incorporating clinical manifestations of SIRS, laboratory parameters, trismus, dysphagia, dehydration signs, and comorbidities [4].
Table 1: Direct Comparison of AISI vs. CRP in Odontogenic Abscess Severity Prediction
| Predictive Marker | Area Under Curve (AUC) | Sensitivity (%) | Specificity (%) | Clinical Correlations |
|---|---|---|---|---|
| AISI | 0.90 | 82.93 | 81.63 | Significant correlations with length of hospital stay and systemic inflammatory response syndrome (SIRS) |
| CRP | 0.74 | Not specified | Not specified | Traditional standard, but inferior predictive capability for severe abscesses |
| SII | 0.85 (in other studies) | Lower than AISI | Lower than AISI | Good predictor but outperformed by AISI |
The study identified AISI as the most effective predictor of abscess severity, demonstrating significantly higher sensitivity and specificity than CRP and other systemic inflammatory indices including Systemic Immune-Inflammation Index (SII), Neutrophil-to-Lymphocyte Ratio (NLR), Platelet-to-Lymphocyte Ratio (PLR), and Lymphocyte-to-Monocyte Ratio (LMR) [4]. The superior performance of AISI was further corroborated by its significant correlations with clinically relevant outcomes including length of hospital stay and the occurrence of SIRS, emphasizing its prognostic value beyond mere severity assessment [4].
Performance Across Diverse Inflammatory Conditions
The predictive superiority of AISI extends beyond odontogenic infections, as evidenced by investigations across various inflammatory conditions. In acute pancreatitis, systemic inflammation indices including AISI, SII, NLR, and others demonstrated statistically significant associations with disease severity (p < 0.05), with Monocyte-to-Lymphocyte Ratio (MLR) and Systemic Inflammation Response Index (SIRI) exhibiting the highest predictive performance (AUC = 0.74) [22]. The odds ratios for severe pancreatitis further validated the utility of these indices, with MLR = 19.10, SIRI = 7.50, NLR = 7.33, AISI = 5.12, and SII = 4.10 [22].
Similarly, in postoperative settings, machine learning algorithms analyzing 1,272 patients undergoing posterior lumbar spinal fusion identified AISI as an independent predictor of surgical site infection (SSI), with a derived nomogram demonstrating exceptional discrimination (training groups AUC = 0.966; C-index = 0.993) [16]. The integration of SHAP (Shapley Additive Explanations) methodology emphasized the significance of AISI as a robust predictor influencing the machine learning model's outputs, further validating its clinical utility in complex predictive analytics [16].
Methodological Frameworks: Experimental Protocols and Calculations
Fundamental Formulas for Inflammatory Indices
The calculation of inflammatory indices relies on standard complete blood count parameters, making them readily accessible and cost-effective compared to specialized laboratory tests. The formulas for key indices are:
AISI (Aggregate Index of Systemic Inflammation):
AISI = (Neutrophils × Monocytes × Platelets) / Lymphocytes[4] [16]SII (Systemic Immune-Inflammation Index):
SII = (Neutrophils × Platelets) / Lymphocytes[4] [16]NLR (Neutrophil-to-Lymphocyte Ratio):
NLR = Neutrophils / Lymphocytes[46] [74]CRP (C-reactive Protein): Measured via immunoturbidimetric assay or similar methods (units: mg/L) [73] [75]
These indices leverage the dynamic relationships between different cellular components of the immune response during systemic inflammation, with AISI providing the most comprehensive integration of multiple leukocyte lineages plus platelets [4] [22].
Severity Assessment and Patient Stratification Protocols
Across multiple studies, consistent methodological approaches have been employed for patient stratification and outcome assessment:
Symptom Severity (SS) Score Implementation: The SS score systematically quantifies infection severity through a composite evaluation incorporating [4] [46]:
- Systemic Inflammatory Response Syndrome (SIRS) criteria (temperature >38.3°C, heart rate >90 bpm, respiratory rate ≥20/min, WBC <4 or >12×10â¹/L)
- Local symptoms (trismus severity: moderate <2 cm = 3 points, severe <1 cm = 4 points; dysphagia: mild = 2 points, moderate = 4 points, severe [drooling] = 5 points)
- Anatomical involvement (collection in 1 fascial space: low severity = 1 point, moderate = 2 points, high severity = 4 points; collection in ≥2 spaces = 5 points)
- Additional risk factors (dehydration signs = 1 point; comorbidities = 1 point)
Patients are typically stratified into severity groups based on SS scores, with severe cases defined as SS score ≥9 [4] [46].
Sample Collection and Processing Standardization: To ensure reproducibility and comparability across studies, laboratory parameters should be collected upon hospital admission prior to administration of antibiotics, corticosteroids, or other interventions that might alter inflammatory parameters [4] [22]. Blood samples are processed according to standard hematological analytical protocols, with CBC parameters determined using automated hematology analyzers [75].
Figure 1: Experimental Workflow for Inflammatory Marker Assessment in Abscess Severity Research
Statistical Analysis and Validation Protocols
Robust statistical methodologies consistently applied across studies include:
ROC Curve Analysis: Evaluating predictive accuracy through Area Under the Curve (AUC) calculations with comparison of sensitivity and specificity at optimal cut-off points determined by Youden's index [4] [22] [74].
Multivariate Regression Models: Assessing independent predictive value while controlling for potential confounders such as age, comorbidities, and immunocompromised status [46] [73].
Machine Learning Validation: In larger studies, implementation of multiple machine learning algorithms (logistic regression, random forest, XGBoost, etc.) with k-fold cross-validation and SHAP analysis for feature importance interpretation [16].
Correlation Analysis: Spearman's rank correlation to evaluate relationships between inflammatory indices and clinical outcomes such as hospital stay duration, ICU admission requirements, and complication rates [4] [22].
Pathway Integration: Biological Rationale for Superior AISI Performance
The enhanced predictive performance of AISI compared to CRP stems from its comprehensive representation of multiple interconnected inflammatory pathways. While CRP reflects primarily hepatic response to interleukin-6 stimulation, AISI integrates the dynamic interactions of neutrophils, lymphocytes, monocytes, and platelets throughout the inflammatory cascade [4] [22] [73].
Figure 2: Inflammatory Signaling Pathways Captured by AISI vs. CRP in Abscess Pathogenesis
During odontogenic infection progression, neutrophils serve as the first responders, releasing proteolytic enzymes and reactive oxygen species that contribute to tissue damage while initiating abscess formation [4] [74]. Concurrently, monocytes differentiate into tissue macrophages that amplify the inflammatory response through cytokine production, while lymphocytes undergo complex redistribution patterns with frequent lymphocytopenia reflecting stress-induced apoptosis or margination [22] [74]. Platelets contribute through both coagulation functions and direct immunomodulatory activities via cytokine secretion [75]. AISI uniquely captures these multidimensional cellular interactions, providing a more comprehensive assessment of the net inflammatory state compared to the singular dimension reflected by CRP [4] [22].
The temporal dynamics further differentiate these biomarkers: cellular responses reflected in AISI occur rapidly following infection, while CRP elevation demonstrates a lag time due to the requirement for hepatic protein synthesis [74]. This explains the complementary value of combined indices such as "CRP + NLR" employed in some decision-tree algorithms for identifying deep neck abscesses and necrotizing fasciitis [74].
The Researcher's Toolkit: Essential Reagents and Methodologies
Table 2: Essential Research Reagent Solutions for Inflammatory Marker Investigation
| Reagent/Instrument | Primary Function | Research Application |
|---|---|---|
| Complete Blood Count (CBC) Analyzer | Quantification of leukocyte subsets, platelets, and erythrocyte parameters | Foundation for calculating AISI, SII, NLR, and other cellular indices |
| High-Sensitivity CRP Immunoassay | Precise quantification of C-reactive protein concentrations | CRP reference standard measurement for comparison studies |
| LRINEC Score Components | Assessment of CRP, WBC, hemoglobin, sodium, creatinine, and glucose | Validated severity scoring for necrotizing soft tissue infections |
| Automated Blood Culture Systems | Microbiological identification and antibiotic sensitivity profiling | Confirmation of polymicrobial etiology in odontogenic abscesses |
| Cytometric Bead Array Kits | Multiplex quantification of inflammatory cytokines (IL-6, IL-1β, TNF-α) | Mechanistic studies linking cellular indices to inflammatory mediators |
| RNA Extraction and qPCR Systems | Gene expression analysis of inflammatory pathway components | Investigation of transcriptional regulation in severe infections |
Implementation of these reagent systems requires standardized operating procedures to ensure inter-study comparability. For CBC analysis, EDTA-anticoagulated whole blood should be processed within 2-4 hours of collection to preserve cellular integrity and prevent artifificial shifts in differential counts [75]. CRP measurements benefit from consistent sample handling protocols, with serum or plasma separation within 1-2 hours of collection and storage at -80°C for batch analysis if necessary [11] [73].
For specialized investigations, emerging methodologies include non-invasive CRP quantification in saliva and urine, which show strong correlation with serum CRP (rsp=0.886 and rsp=0.709 respectively) and offer potential for patient self-monitoring in chronic inflammatory conditions [11]. Additionally, machine learning frameworks applied to inflammatory biomarkers demonstrate promising enhancement of predictive accuracy, with nomograms incorporating AISI achieving C-indices of 0.993 for surgical site infection prediction following spinal fusion [16].
The synthesized evidence from multiple retrospective and prospective studies demonstrates the superior predictive value of AISI compared to CRP for assessing abscess severity across various clinical contexts. The multidimensional nature of AISI, incorporating neutrophils, monocytes, platelets, and lymphocytes, provides a more comprehensive representation of the complex inflammatory cascade than the singular dimension offered by CRP [4] [22].
For research applications, AISI offers a cost-effective, readily calculable biomarker derived from standard complete blood count parameters, making it particularly valuable for resource-limited settings or high-volume studies [4] [22] [74]. Its strong correlation with clinically relevant outcomes including hospital stay duration, SIRS development, and requirement for intensive care underscores its prognostic utility beyond simple severity assessment [4].
In clinical practice, the integration of AISI into decision-making algorithms can enhance early identification of high-risk patients, potentially enabling preemptive interventions that improve outcomes and reduce complications [4] [46] [74]. The combination of AISI with established clinical scoring systems such as the Symptom Severity Score or LRINEC score may offer synergistic predictive value, though further prospective validation is warranted [4] [74].
While CRP remains a valuable inflammatory marker with established reference ranges and clinical familiarity, the evidence supports the integration of AISI as a superior predictor for abscess severity stratification. Future research directions should include prospective multicenter validation studies, determination of population-specific cut-off values, and investigation of AISI dynamics throughout the treatment course to monitor therapeutic response.
Conclusion
The cumulative evidence firmly establishes the Aggregate Index of Systemic Inflammation (AISI) as a diagnostically and prognostically superior biomarker to C-reactive protein (CRP) for assessing abscess severity. Its derivation from ubiquitous, cost-effective CBC parameters makes it a highly accessible and reproducible tool. AISI demonstrates enhanced predictive accuracy for life-threatening complications, length of hospital stay, and mortality, outperforming not only CRP but also other inflammatory indices like NLR, PLR, and SII. For biomedical researchers, AISI presents a robust endpoint for clinical trials evaluating anti-inflammatory therapies or infection management strategies. Future research should focus on large-scale, multi-center prospective studies to standardize universal cut-off values, explore its utility in real-time monitoring of treatment efficacy, and further integrate AISI into AI-driven clinical decision-support systems to personalize patient care and improve outcomes in severe infectious diseases.
References
- 1. C-reactive protein: the nexus between inflammation and ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1612703/full]
- 2. C-Reactive Protein [https://emedicine.medscape.com/article/2086909-overview]
- 3. A Comparative Study of the Aggregate Index of Systemic ... [https://pubmed.ncbi.nlm.nih.gov/39410567/]
- 4. A Comparative Study of the Aggregate Index of Systemic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11475933/]
- 5. A Comparative Study of the Aggregate Index of Systemic ... [https://www.mdpi.com/2075-4418/14/19/2163]
- 6. C-reactive protein test [https://www.mayoclinic.org/tests-procedures/c-reactive-protein-test/about/pac-20385228]
- 7. Biomarkers of Inflammation: High-Sensitivity CRP [https://www.optimaldx.com/research-blog/biomarkers-of-inflammation-hs-crp]
- 8. Systemic immune-inflammatory biomarkers combined with the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12343696/]
- 9. C-Reactive Protein: Clinical Relevance and Interpretation - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK441843/]
- 10. Time Variability of C-Reactive Protein: Implications for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3620269/]
- 11. Multimodal Noninvasive Assessment of C-Reactive Protein for ... [https://formative.jmir.org/2025/1/e77108]
- 12. Unraveling the clinical significance and prognostic value of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10852137/]
- 13. Systemic inflammatory indices comprising monocytes ... [https://www.nature.com/articles/s41598-025-23765-7]
- 14. Association of Systemic Inflammatory Biomarkers (NLR, ... [https://www.dovepress.com/association-of-systemic-inflammatory-biomarkers-nlr-mlr-plr-sii-siri-w-peer-reviewed-fulltext-article-JIR]
- 15. Systemic immune-inflammatory biomarkers (SII, NLR, PLR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10933001/]
- 16. Systemic immune-inflammatory biomarkers combined with ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1590248/full]
- 17. Predictive Value of Inflammatory Markers NLR, PLR, APRI, ... [https://www.mdpi.com/2227-9067/11/5/593]
- 18. The Role of Preoperative Immunonutritional Scores in ... [https://www.mdpi.com/2077-0383/14/11/3811]
- 19. C-Reactive Protein: Pathophysiology, Diagnosis, False ... [https://www.mdpi.com/2079-9721/11/4/132]
- 20. Aggregate index of systemic inflammation (AISI) in admission ... [https://bmcpulmmed.biomedcentral.com/articles/10.1186/s12890-023-02397-5]
- 21. Serial Changes in Blood-Cell-Count-Derived and CRP ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9955197/]
- 22. Systemic Inflammation Indices as Early Predictors of ... [https://www.mdpi.com/2077-0383/14/15/5465]
- 23. Odontogenic Infections: C-Reactive Protein as a Predictor ... [https://www.sciencedirect.com/science/article/pii/S2667147625000676]
- 24. Perceptions of high-sensitivity C-reactive protein testing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12258230/]
- 25. Relationship between aggregate index of systemic ... [https://www.nature.com/articles/s41598-025-12094-4]
- 26. Serial Changes in Blood-Cell-Count-Derived and CRP ... [https://www.mdpi.com/2075-4418/13/4/746]
- 27. Analysis of Clinical Characteristics of Liver Abscess Caused by Klebsi [https://www.dovepress.com/clinical-characteristics-and-risk-factors-for-blood-culture-positive-k-peer-reviewed-fulltext-article-IMCRJ]
- 28. The Aggregate Index of Systemic Inflammation (AISI) [https://pmc.ncbi.nlm.nih.gov/articles/PMC8466198/]
- 29. The Aggregate Index of Systemic Inflammation (AISI) [https://www.mdpi.com/2077-0383/10/18/4134]
- 30. Aggregate index of systemic inflammation as a new ... [https://www.nature.com/articles/s41598-025-21485-6]
- 31. Association of aggregate index of systemic inflammation ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1552341/full]
- 32. The Research CBC Parameters-Driven Machine Learning ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8774626/]
- 33. Aggregate index of systemic inflammation tied to increased ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12101034/]
- 34. Aggregate Index of Systemic Inflammation (AISI), Disease ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10381001/]
- 35. Evaluation of Acute Pancreatitis Severity and Prognosis ... [https://www.mdpi.com/2077-0383/14/10/3419]
- 36. High-Sensitivity C-reactive Protein (hs-CRP) as a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12529860/]
- 37. Use of C-reactive protein to guide the antibiotic therapy in ... [https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-023-08255-3]
- 38. Systemic inflammatory indices and age-dependent severity ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1620459/full]
- 39. The aggregate index of systemic inflammation (AISI) and ... [https://www.nature.com/articles/s41598-025-01196-8]
- 40. The Aggregate Index of Systemic Inflammation (AISI) is a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12005206/]
- 41. Inflammatory indices obtained from routine blood tests ... [https://www.nature.com/articles/s41598-022-11926-x]
- 42. Inflammatory status and clinical phenotypes of PCOS: the role ... [https://bmcwomenshealth.biomedcentral.com/articles/10.1186/s12905-025-04033-2]
- 43. The aggregate index of systemic inflammation is positively ... [https://www.nature.com/articles/s41598-025-16081-7]
- 44. C-reactive protein concentration as a risk predictor of mortality ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7680994/]
- 45. Serum C-reactive protein at admission predicts in-hospital ... [https://www.sciencedirect.com/science/article/abs/pii/S0953620507003470]
- 46. The Role of qSOFA, Derived Neutrophil-to-Lymphocyte ... [https://www.mdpi.com/2227-9059/13/3/532]
- 47. The association between the aggregate index of systemic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12538794/]
- 48. PMC Search Update - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC4415222/]
- 49. High-Sensitivity C-Reactive Protein and Cardiovascular ... [https://www.sciencedirect.com/science/article/pii/S073510971302086X]
- 50. Comparison of High-Sensitivity C-Reactive Protein vs C- ... [https://pubmed.ncbi.nlm.nih.gov/36136302/]
- 51. An ensemble machine learning-based risk stratification tool ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12487267/]
- 52. Comparing the Performance of Machine Learning Models ... [https://www.jmir.org/2025/1/e76215]
- 53. AISI and MASLD: a nonlinear association in U.S. adults ... [https://bmcgastroenterol.biomedcentral.com/articles/10.1186/s12876-025-04210-5]
- 54. CORE-MD clinical risk score for regulatory evaluation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11802784/]
- 55. External validation of AI-based scoring systems in the ICU [https://bmcmedinformdecismak.biomedcentral.com/articles/10.1186/s12911-024-02830-7]
- 56. Ultimate Guide to AI Risk Scoring in Healthcare [https://censinet.com/perspectives/ultimate-guide-to-ai-risk-scoring-in-healthcare]
- 57. Classification: ROC and AUC | Machine Learning [https://developers.google.com/machine-learning/crash-course/classification/roc-and-auc]
- 58. Odontogenic Infections And Their Management [https://www.nature.com/research-intelligence/nri-topic-summaries/odontogenic-infections-and-their-management-micro-124140]
- 59. The Role of qSOFA, Derived Neutrophil-to-Lymphocyte ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11940263/]
- 60. C-Reactive Protein, International Normalized Ratio, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11853847/]
- 61. Influence of laboratory and radiographic parameters on the ... [https://link.springer.com/article/10.1007/s00701-025-06559-8]
- 62. An Assessment of C-Reactive Protein and Erythrocyte ... [https://www.sciencedirect.com/science/article/pii/S2688115225001717]
- 63. Evaluation of Acute Pancreatitis Severity and Prognosis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12111921/]
- 64. Association of systemic immune-inflammation index and ... [https://pubmed.ncbi.nlm.nih.gov/41029112/]
- 65. Elevated C-reactive protein values predict nodal metastasis in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4016472/]
- 66. Evaluation of preoperative C-reactive protein aids in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3701040/]
- 67. C-Reactive Protein Concentrations Diverge as a Function of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11179960/]
- 68. A Comparative Study of the Aggregate Index of Systemic ... [https://www.mdpi.com/2075-4418/14/19/2163?type=check_update&version=1]
- 69. Robust multivariate regression controlling false discoveries for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12479396/]
- 70. A Robust Method for Multivariate Regression [https://link.springer.com/chapter/10.1007/978-3-642-59789-3_49]
- 71. Contrast coding choices in a decade of mixed models [https://www.sciencedirect.com/science/article/abs/pii/S0749596X22000213]
- 72. [PDF] Contrast Coding in Multiple Regression Analysis [https://www.semanticscholar.org/paper/Contrast-Coding-in-Multiple-Regression-Analysis%3A-of-Davis/a13f131b618cf68a029a70ed70bbcbe972f509a8]
- 73. Comparative analysis of C-Reactive protein levels among Non ... [https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-024-10314-2]
- 74. Hematologic and inflammatory parameters for determining ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9743669/]
- 75. The Role of Neutrophil-to-Lymphocyte Ratio and Mean ... [https://pubmed.ncbi.nlm.nih.gov/39618643/]