Autocrine and Paracrine Signaling of Inflammatory Cytokines: Mechanisms, Research Methods, and Therapeutic Targeting
This article provides a comprehensive analysis of autocrine and paracrine signaling mechanisms governing inflammatory cytokine networks, essential knowledge for researchers, scientists, and drug development professionals.
Autocrine and Paracrine Signaling of Inflammatory Cytokines: Mechanisms, Research Methods, and Therapeutic Targeting
Abstract
This article provides a comprehensive analysis of autocrine and paracrine signaling mechanisms governing inflammatory cytokine networks, essential knowledge for researchers, scientists, and drug development professionals. We explore fundamental biological principles, including distinct signaling pathways and their roles in physiological and pathological processes from immune regulation to cancer. The content covers advanced methodological approaches for studying these complex signaling loops, addresses common research challenges and optimization strategies, and provides frameworks for validating findings and comparing therapeutic interventions. By synthesizing current research and emerging technologies, this review aims to equip professionals with the insights needed to advance both fundamental understanding and clinical translation in this critical field.
Core Principles and Biological Significance of Inflammatory Cytokine Signaling
Defining Autocrine and Paracrine Signaling Mechanisms
Cell-to-cell communication is a cornerstone of multicellular life, enabling the coordination of complex physiological processes. Within this framework, autocrine and paracrine signaling represent two fundamental mechanisms for local cellular communication. Autocrine signaling occurs when a cell secretes a signaling molecule that binds to receptors on its own surface, thereby influencing its own behavior. In contrast, paracrine signaling involves a cell secreting molecules that act on nearby, distinct cells [1]. These signaling modes are particularly crucial for the function of inflammatory cytokines, which coordinate immune responses through complex local signaling networks [2] [3]. Understanding the precise mechanisms distinguishing these signaling types is essential for researchers and drug development professionals seeking to target specific pathways in diseases ranging from autoimmune disorders to cancer.
Core Definitions and Functional Distinctions
Fundamental Signaling Concepts
The classification of chemical signaling in multicellular organisms is primarily based on the distance the signal travels and the relationship between the signaling and target cells:
Autocrine Signaling: A cell produces and secretes a signaling molecule that then binds to receptors on its own membrane. This self-stimulation creates a feedback loop that can amplify responses, maintain cell states, or coordinate group behavior when multiple identical cells respond similarly [1]. Examples include pain regulation, inflammatory responses, and early developmental processes [1].
Paracrine Signaling: A cell releases signaling molecules into the extracellular fluid that act on nearby, distinct cells. These signals typically elicit rapid responses that are spatially and temporally localized, as the ligands are quickly degraded or removed from the extracellular space [1]. A classic example is synaptic transmission between nerve cells [1].
Endocrine Signaling: For comparative context, endocrine signaling involves hormones released into the bloodstream by specialized glands, affecting distant target cells throughout the body [1].
Comparative Analysis of Signaling Modes
Table 1: Characteristic comparison of autocrine and paracrine signaling mechanisms
| Characteristic | Autocrine Signaling | Paracrine Signaling |
|---|---|---|
| Spatial Range | Same cell or cells of identical type | Neighboring cells (short distances) |
| Temporal Dynamics | Can sustain prolonged cellular states | Typically rapid, transient responses |
| Signal Degradation | May be internalized or degraded after binding | Quickly degraded by enzymes or removed by neighboring cells |
| Primary Functions | Cellular self-maintenance, fate stabilization, population coordination | Local tissue coordination, rapid defensive responses |
| Example Contexts | Inflammatory pain regulation, viral response, development [1] | Synaptic transmission, immune cell recruitment [1] |
Quantitative Analysis of Signaling Parameters
Concentration and Temporal Dynamics
The functional differences between autocrine and paracrine signaling are reflected in their quantitative parameters:
Table 2: Quantitative parameters in cytokine signaling
| Parameter | Autocrine Signaling | Paracrine Signaling | Experimental Evidence |
|---|---|---|---|
| Effective Concentration | Can achieve high local concentration at producing cell membrane | Graded concentration decreasing with distance from source | Computational models show steep concentration gradients [4] |
| Response Time | Immediate initiation following production | Diffusion-dependent delay to target cells | Microcavity platforms demonstrate temporal delays [4] |
| Signaling Duration | Can be self-sustaining through positive feedback | Typically transient due to rapid degradation | TNF production shows sustained vs. transient patterns [3] |
| Cellular ECâ‚…â‚€ | Often lower due to preferential access to self-receptors | Higher concentrations needed for distant cell activation | Isolated VPC studies show differential dose responses [5] |
The concentration dynamics fundamentally differ between these signaling modes. In autocrine signaling, the producing cell experiences the highest effective concentration, potentially creating robust self-stimulation. In paracrine signaling, concentrations form spatial gradients, creating positional information across a field of cells [4]. These quantitative differences have profound implications for network behaviors, as demonstrated in studies of tumor necrosis factor (TNF) production where the same cytokine can function through autocrine loops in some contexts (CpG DNA stimulation) while acting primarily through paracrine mechanisms in others (LPS stimulation) [3].
Experimental Methodologies for Pathway Discrimination
Microcavity Platform for Signal Isolation
Objective: To distinguish autocrine from paracrine signals in hematopoietic stem cell (HSC) culture by physically constraining cell distributions.
Methodology Details:
- Microcavity Fabrication: Create arrayed microwells using poly(dimethyl siloxane) silicone (PDMS) or poly(ethylene oxide) (sPEG) hydrogels with precisely controlled diameters (15μm for single-cell confinement, 40μm for multi-cell clusters) [4].
- Surface Functionalization: Covalently link extracellular matrix components (fibronectin) or signaling molecules (heparin for cytokine presentation) to cavity surfaces [4].
- Cell Seeding and Culture: Seed CD34+ hematopoietic stem/progenitor cells at low density to achieve either single cells per microcavity (autocrine-dominated) or small cell clusters (paracrine-enabled) [4].
- Factor Analysis: Collect conditioned media and perform multiplex immunoassays for candidate factors, followed by partial least squares (PLS) analysis to correlate spatial configuration with secreted factors and cell fate outcomes [4].
Key Applications: This platform successfully identified autocrine VEGF and TGF-β loops in HSC self-renewal and demonstrated that autocrine signals predominantly maintain quiescence in single-cell niches, while paracrine signals drive proliferation in multi-cell environments [4].
Computational Modeling of Network Dynamics
Objective: To determine how autocrine loops contribute to cell fate patterning in C. elegans vulva development.
Methodology Details:
- Network Modeling: Construct ordinary differential equation-based models incorporating known interactions between EGF-Ras-MAPK and Delta-Notch pathways, including potential autocrine loops through secreted Delta ligands [5].
- Parameter Variation: Perform Monte Carlo sampling across parameter space (affinity constants, Hill coefficients, production/degradation rates) to identify parameter sets that reproduce wild-type cell fate patterns [5].
- Experimental Validation: Test model predictions using isolated vulva precursor cells (VPCs) exposed to varying EGF concentrations, assessing fate specification in the absence of neighboring cells (eliminating paracrine signals) [5].
Key Findings: The model revealed that 1.9% of wild-type parameter solutions could stabilize 2° cell fate in isolated VPCs through a DSL-Notch autocrine loop, characterized by high secreted Delta expression and specific network dynamics [5]. This demonstrated how quantitative variation in the same network can produce qualitatively distinct patterning modes.
Signaling Visualization
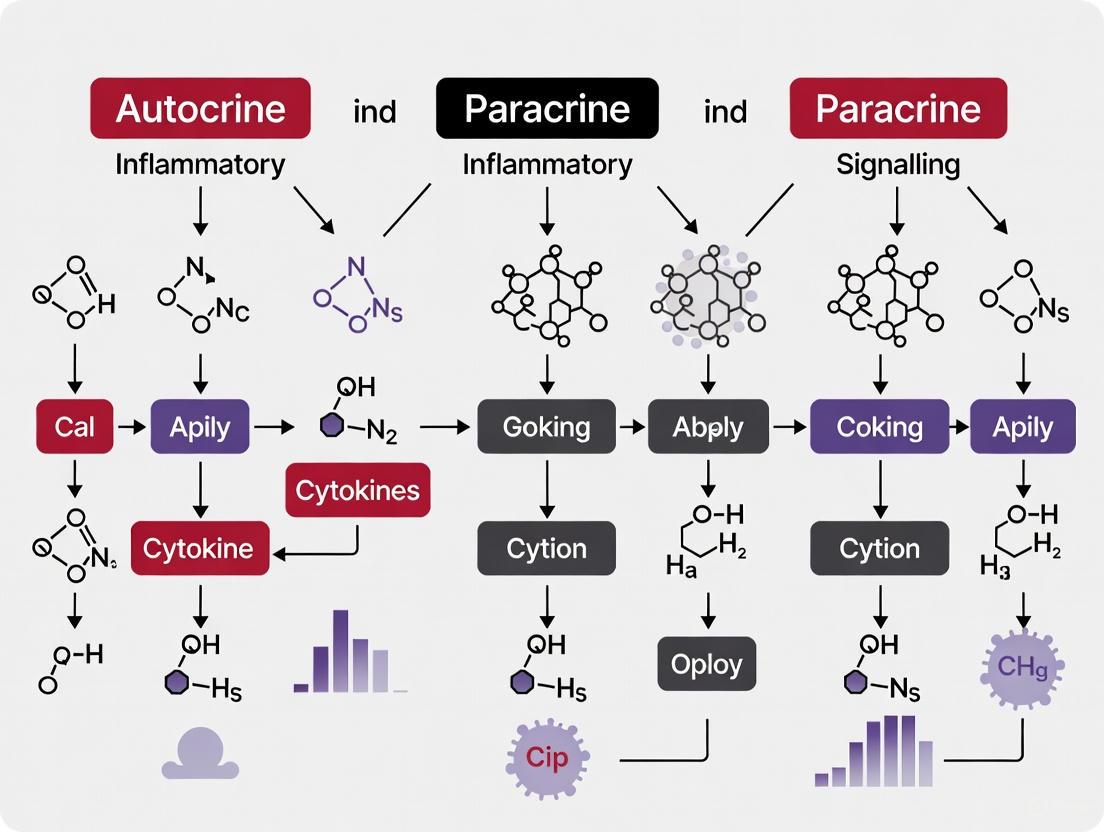
Cytokine Signaling Pathways Diagram
Research Reagent Solutions for Signaling Studies
Table 3: Essential research reagents for autocrine/paracrine signaling studies
| Reagent/Category | Specific Examples | Research Application | Functional Role |
|---|---|---|---|
| Microfabrication Materials | PDMS, sPEG-hydrogels, Heparin-functionalized matrices | Spatial constraint of cell signaling [4] | Creates defined microenvironments to physically separate autocrine vs. paracrine contexts |
| Pathway Inhibitors | TGF-β receptor kinase inhibitors (Galunisertib), JAK/STAT inhibitors (Tofacitinib) | Blocking specific paracrine pathways [6] | Inhibits receptor activation to dissect pathway contributions to observed phenotypes |
| Cytokine Neutralizing Antibodies | Anti-IL-6, Anti-TGF-β, Anti-TNF-α | Selective blockade of extracellular signaling molecules [3] [6] | Distinguishes functions of specific cytokines in complex mixtures; confirms paracrine actions |
| Recombinant Ligands | EGF, SCF, TPO, FLT3L, purified cytokines | Controlled stimulation studies [4] [5] | Provides defined signals at specific concentrations to measure cellular responses |
| Detection Systems | Multiplex immunoassays, Phospho-specific flow cytometry, GFP-reporters | Quantifying pathway activation and secretion [3] [4] | Measures dynamic changes in signaling activity and secreted factors with high sensitivity |
Implications for Inflammatory Cytokine Research
The distinction between autocrine and paracrine signaling mechanisms has profound implications for understanding inflammatory processes and developing targeted therapies. In cancer biology, cancer-associated fibroblasts (CAFs) extensively utilize paracrine signaling to establish immunosuppressive tumor microenvironments. Specific CAF subtypes secrete distinct paracrine factors: myCAFs produce TGF-β to suppress T-cell activation and promote regulatory T-cell differentiation, while iCAFs secrete IL-6 and CXCL12 to recruit additional immunosuppressive cells [6]. These paracrine networks create physical and biochemical barriers that limit effective immune responses and contribute to therapy resistance.
The dynamic allostery mechanism recently identified in TGF-β signaling exemplifies the sophisticated regulation of autocrine/paracrine decisions. The conformational entropy redistribution (CER) in the L-TGF-β1-GARP-avβ8 complex enables context-dependent signaling - either promoting autocrine signaling while TGF-β remains latent or allowing release for paracrine actions [7]. This structural insight reveals how the same cytokine can mediate distinct biological outcomes through different signaling modes, potentially explaining the paradoxical roles of TGF-β in both inhibiting and promoting cancer progression.
From a therapeutic perspective, targeting autocrine versus paracrine signaling requires distinct strategic approaches. Autocrine loops may be interrupted by receptor antagonists or intracellular pathway inhibitors, while paracrine signaling might be blocked by neutralizing antibodies or trap receptors. The emerging understanding that the same network can be quantitatively tuned to utilize different signaling modes [5] suggests that therapeutic strategies may need to account for potential plasticity in signaling mechanisms across physiological contexts and disease states.
Key Inflammatory Cytokines and Their Receptor Systems
Inflammatory cytokines are signaling proteins that play a pivotal role in coordinating the immune system's response to infection, injury, and other threats [8] [2]. These molecules are predominantly secreted by immune cells such as helper T cells (Th) and macrophages, and promote inflammation, a fundamental component of the host defence mechanism [8]. The precise interplay between pro-inflammatory and anti-inflammatory cytokines determines the net inflammatory outcome, and dysregulation of this balance is implicated in a wide array of diseases, including atherosclerosis, cancer, and autoimmune disorders [8] [9]. Understanding the specific receptor systems these cytokines engage is crucial for deciphering their biological functions and for developing targeted therapeutic strategies. This guide frames the complex landscape of key inflammatory cytokines within the context of autocrine and paracrine signaling, providing researchers and drug development professionals with a detailed technical resource.
Key Pro-inflammatory Cytokines and Their Functions
Pro-inflammatory cytokines are instrumental in initiating and amplifying the inflammatory response. The following table summarizes the core set of these cytokines, their primary cellular sources, and their major functions.
Table 1: Key Pro-Inflammatory Cytokines and Functions
| Cytokine | Main Cellular Sources | Major Functions |
|---|---|---|
| IL-1β [10] [9] | Macrophages, Monocytes, Fibroblasts, Endothelial Cells [10] [9] | Acts as an endogenous pyrogen; stimulates CD4+ T cell differentiation into Th17 cells; induces hyperalgesia; upregulates endothelial adhesion molecules [10] [9]. |
| TNF-α [10] [9] | Macrophages, T Cells [10] | Key mediator in inflammatory and neuropathic hyperalgesia; triggers expression of vascular endothelial adhesion molecules; promotes immune cell infiltration; can induce shock and tissue destruction [8] [10] [9]. |
| IL-6 [10] | Monocytes, Fibroblasts, Endothelial Cells, T & B Cells, Macrophages [10] | Pleiotropic cytokine; induces B-cell differentiation into plasma cells; stimulates acute-phase protein production in the liver; involved in neuronal reaction to injury [10] [9]. |
| IL-12 [8] | Macrophages, Dendritic Cells, Monocytes [10] | Activates NK cells and phagocytes; induces IFN-γ production; involved in tumor cytotoxicity and endotoxic shock [10]. |
| IL-17 [10] | Th17 Cells [10] | Recruits monocytes and neutrophils to infection sites; activates production of other cytokines (e.g., IL-1, IL-6, TNF-α) [10]. |
| IL-18 [10] | Macrophages, Dendritic Cells, Epithelial Cells [10] | Recruits monocytes and T lymphocytes; synergizes with IL-12 to induce IFN-γ production; inhibits angiogenesis [10]. |
| IFN-γ [8] [10] | T Cells, NK Cells [10] | Anti-viral effects; macrophage activation; increases neutrophil and monocyte function; upregulates MHC class I and II expression [10]. |
| GM-CSF [8] | T Cells, Macrophages, Fibroblasts [10] | Stimulates growth and differentiation of monocytes, eosinophils, and granulocytes from stem cells [10]. |
Receptor Systems and Signaling Mechanisms
Inflammatory cytokines exert their effects by binding to specific cell-surface or intracellular receptors, initiating complex intracellular signaling cascades. The major receptor families involved include those coupled to Janus kinases (JAKs), the IL-1 receptor family, and the TNF receptor superfamily.
JAK-STAT Coupled Receptor Systems
Cytokines such as IL-6 signal through receptors that are associated with the JAK-STAT pathway. The binding of IL-6 to its membrane-bound IL-6R (CD126) triggers the recruitment of a signal-transducing subunit, gp130 (CD130). This assembly activates the receptor-associated JAK kinases, which phosphorylate and activate STAT transcription factors. The phosphorylated STATs dimerize and translocate to the nucleus to drive the expression of target genes, including acute-phase proteins [10]. This pathway is a classic example of paracrine and endocrine signaling, influencing both immune and non-immune cells.
Figure 1: IL-6 JAK-STAT signaling pathway. IL-6 binding induces receptor dimerization, JAK kinase activation, STAT protein phosphorylation and dimerization, and nuclear translocation to regulate gene expression.
IL-1 Receptor/Toll-like Receptor (TLR) Family
The IL-1 system exemplifies a tightly regulated inflammatory pathway. IL-1β binds to the IL-1 Receptor type 1 (IL-1R1), initiating a signaling cascade that culminates in the activation of NF-κB, a master regulator of pro-inflammatory gene expression. A critical natural regulator of this system is the IL-1 Receptor Antagonist (IL-1ra), which binds to IL-1R1 without initiating signaling, thus acting as a competitive inhibitor. Additionally, the decoy receptor IL-1R2 (which exists in both membrane-bound and soluble forms) can bind IL-1 ligands but lacks signaling capability, further fine-tuning the IL-1 response [9]. This autocrine and paracrine regulatory mechanism is vital for preventing excessive inflammation.
Table 2: Key Receptor Systems and Signaling Pathways
| Cytokine | Receptor System | Signaling Pathway | Key Regulatory Components |
|---|---|---|---|
| IL-1β [9] | IL-1R1 (Signaling), IL-1R2 (Decoy), IL-1ra (Inhibitor) [9] | NF-κB Activation, MAPK [9] | IL-1ra competitively inhibits IL-1β; Soluble IL-1R2 acts as a molecular sink [9]. |
| TNF-α [9] | TNFR1 (Ubiquitous), TNFR2 (Immune cells) [9] | NF-κB, Apoptosis (via Caspases), SAPK [9] | Soluble TNFR (sTNFRp55/p75) binds circulating TNF, inhibiting receptor interaction [9]. |
| IL-6 [10] | IL-6R (CD126) & gp130 (CD130) [10] | JAK-STAT [10] | Soluble IL-6R (sIL-6R) can mediate trans-signaling [10]. |
| IFN-γ [10] | CDw119 (IFNGR1) [10] | JAK-STAT [10] | - |
| IL-12 [10] | CD212 [10] | JAK-STAT [10] | - |
TNF Receptor Superfamily
TNF-α signaling is mediated through two distinct cell surface receptors, TNFR1 and TNFR2. TNFR1 is ubiquitously expressed and its engagement can lead to either NF-κB-mediated cell survival and inflammation or caspase-activated apoptosis, depending on cellular context. TNFR2 expression is more restricted to immune cells and primarily promotes cell survival and proliferation. The activity of TNF-α is regulated by soluble forms of its receptors (sTNFRp55 and sTNFRp75), which sequester the cytokine in the circulation, preventing it from interacting with membrane-bound receptors [9].
Figure 2: TNF-α signaling and regulation. TNF-α binding to TNFR1 or TNFR2 triggers divergent downstream effects. Soluble TNF receptors act as endogenous inhibitors.
Experimental Methodologies for Cytokine Research
Quantifying Cytokine Expression and Secretion
A foundational methodology in cytokine research is the accurate measurement of cytokine levels. The Cytokine Panel is a blood test that uses immunoassay techniques (e.g., ELISA or multiplex bead-based assays) to simultaneously quantify the concentrations of multiple cytokines in serum, plasma, or cell culture supernatant [2]. This is critical for diagnosing inflammatory conditions and monitoring therapeutic responses. For gene expression analysis, Quantitative Reverse Transcription Polymerase Chain Reaction (qRT-PCR) is used to measure the relative abundance of cytokine mRNA transcripts from isolated cell populations or tissues, providing insights into transcriptional regulation [9].
Protocol: Cell Stimulation and Cytokine Measurement via ELISA
- Cell Preparation: Isolate primary immune cells (e.g., human peripheral blood mononuclear cells - PBMCs) or use a relevant immortalized cell line. Culture cells in an appropriate medium.
- Stimulation: Stimulate cells with an appropriate agonist. For pro-inflammatory cytokine induction, use E. coli Lipopolysaccharide (LPS) at a concentration of 100 ng/mL for 24 hours [9].
- Sample Collection: Post-incubation, centrifuge the cell culture plate or tube at 300 x g for 10 minutes. Carefully aspirate the supernatant for cytokine analysis.
- ELISA Execution:
- Coat a 96-well plate with a capture antibody specific to the cytokine of interest (e.g., anti-human IL-1β).
- Block the plate to prevent non-specific binding.
- Add samples and standards (recombinant cytokine of known concentration) to the plate and incubate.
- After washing, add a biotinylated detection antibody specific to the same cytokine.
- Add an enzyme-conjugated streptavidin solution.
- Add the enzyme's substrate solution to develop a colorimetric signal.
- Stop the reaction and measure the absorbance using a microplate reader.
- Data Analysis: Generate a standard curve from the known standards and calculate the cytokine concentration in the unknown samples.
Mapping Cell-Cell Communication Networks
Advanced single-cell technologies now allow for the deconvolution of complex cytokine-mediated communication between different cell types in a tissue. Single-Cell RNA Sequencing (scRNA-Seq) enables the profiling of gene expression in individual cells [11]. From this data, the co-expression of ligands (e.g., cytokines) in one cell type and their cognate receptors in another can be computationally inferred to map potential autocrine and paracrine signaling networks within the tissue microenvironment [11].
Protocol: Inferring CCC from scRNA-Seq Data
- Single-Cell Suspension & Sequencing: Create a single-cell suspension from the tissue of interest (e.g., synovial tissue from an arthritis model). Process the cells using a platform like 10x Genomics to generate barcoded scRNA-Seq libraries, which are then sequenced.
- Bioinformatic Processing: Use computational pipelines (e.g., Cell Ranger) to align sequencing reads to a reference genome, quantify gene expression, and perform quality control to obtain a gene expression matrix.
- Cell Clustering & Annotation: Cluster cells based on their gene expression profiles using tools like Seurat or Scanpy. Annotate cell types using known marker genes (e.g., CD68 for macrophages, CD3E for T cells).
- Ligand-Receptor Interaction Analysis: Input the annotated expression data into specialized CCC analysis tools such as CellPhoneDB, NicheNet, or CellChat. These tools use curated databases of ligand-receptor pairs to identify statistically significant interactions between user-defined cell types.
- Visualization & Validation: Visualize the inferred communication networks as circle plots, heatmaps, or hierarchy plots. Key interactions (e.g., macrophage-derived IL1B -> IL1R1 on fibroblasts) should be validated using orthogonal methods like immunohistochemistry or functional assays.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Cytokine Studies
| Reagent / Resource | Function / Application | Key Examples / Databases |
|---|---|---|
| Recombinant Cytokines [10] [9] | Used as stimulants in cell-based assays to study cytokine function, signaling, and downstream effects. | Recombinant human IL-1β, TNF-α, IL-6. |
| Neutralizing Antibodies [10] [9] | Block the activity of specific cytokines or their receptors; used for functional validation and as therapeutic prototypes. | Anti-human TNF-α, Anti-human IL-6R. |
| Pathway Databases [12] | Provide curated, computer-readable pathway models for analysis and hypothesis generation. | WikiPathways [12], Reactome [12], KEGG [12]. |
| Interaction Databases [12] | Source of known protein-protein and ligand-receptor interactions for network analysis. | BioGRID, IntAct [12], STRING [12]. |
| Cytokine ELISA Kits [2] | Gold-standard for quantitative measurement of specific cytokine protein levels in biological samples. | IL-1β ELISA Kit, TNF-α ELISA Kit. |
| JAK/STAT Inhibitors [10] | Small molecule inhibitors used to dissect specific signaling pathways in functional studies. | JAK inhibitor I (broad-spectrum), Tofacitinib (JAK1/3 selective). |
| Men 10208 | Men 10208, CAS:129781-07-3, MF:C61H75N15O12, MW:1210.3 g/mol | Chemical Reagent |
| Mepenzolate Bromide | Mepenzolate Bromide, CAS:76-90-4, MF:C21H26BrNO3, MW:420.3 g/mol | Chemical Reagent |
Figure 3: Typical workflow for cytokine signaling research, from hypothesis to validation.
Cytokine Signaling Cascades and Intracellular Transduction Pathways
1. Introduction
Within the inflammatory response, cytokines function as critical signaling molecules, primarily through autocrine (acting on the same cell) and paracrine (acting on nearby cells) mechanisms. Understanding the intricate intracellular transduction pathways they activate is fundamental to dissecting disease pathogenesis and developing targeted therapeutics. This whitepaper provides a technical guide to the core signaling cascades initiated by inflammatory cytokines, focusing on the JAK-STAT, NF-κB, and MAPK pathways.
2. Core Inflammatory Cytokine Signaling Pathways
2.1 The JAK-STAT Pathway Cytokines such as IL-6, IFNs, and IL-2 bind to type I/II cytokine receptors, which are associated with Janus Kinases (JAKs). Receptor dimerization brings JAKs into proximity, leading to their trans-phosphorylation and activation. The JAKs then phosphorylate tyrosine residues on the receptor cytoplasmic tails, creating docking sites for STAT (Signal Transducer and Activator of Transcription) proteins. Upon recruitment, STATs are phosphorylated by JAKs, dimerize, and translocate to the nucleus to drive the transcription of target genes.
2.2 The NF-κB Pathway The pro-inflammatory cytokines TNF-α and IL-1 are potent activators of the NF-κB pathway. TNF-α binding to its receptor (TNFR1) leads to the recruitment of adaptor proteins (TRADD, TRAF2) and the formation of a signaling complex that activates the IKK complex. IKK phosphorylates the inhibitory protein IκBα, targeting it for ubiquitination and proteasomal degradation. This releases the NF-κB dimer (typically p50/p65), allowing its nuclear translocation and the initiation of gene expression for numerous inflammatory mediators.
2.3 The MAPK Pathway Multiple cytokine families, including TNF and IL-1, activate the Mitogen-Activated Protein Kinase (MAPK) pathways. This involves a three-tiered kinase cascade: a MAPK Kinase Kinase (MAP3K) is activated, which then phosphorylates and activates a MAPK Kinase (MAP2K), which in turn phosphorylates and activates a MAPK (e.g., ERK, JNK, p38). Activated MAPKs phosphorylate a wide range of cytosolic and nuclear targets, including transcription factors like AP-1, to regulate cell proliferation, differentiation, and inflammatory responses.
3. Quantitative Data Summary
Table 1: Key Inflammatory Cytokines and Their Primary Signaling Pathways
| Cytokine | Receptor Family | Primary Intracellular Pathway | Key Transcription Factor(s) Activated |
|---|---|---|---|
| TNF-α | TNFR | NF-κB, MAPK (JNK/p38) | NF-κB (p65/p50), AP-1 |
| IL-1β | IL-1R | NF-κB, MAPK (p38) | NF-κB (p65/p50), AP-1 |
| IL-6 | GP130 (Type I Cytokine) | JAK-STAT | STAT3, STAT1 |
| Interferon-gamma (IFN-γ) | Type II Cytokine | JAK-STAT | STAT1 |
| IL-2 | Common Gamma Chain (Type I) | JAK-STAT | STAT5 |
Table 2: Common Research Assays for Pathway Analysis
| Assay Type | Target/Readout | Application in Cytokine Signaling |
|---|---|---|
| Phospho-Specific Flow Cytometry | Phosphorylation status of proteins (e.g., p-STAT, p-p38) | Single-cell analysis of pathway activation in mixed cell populations. |
| Western Blot | Protein expression and phosphorylation | Semi-quantitative validation of pathway component activation. |
| ELISA (Enzyme-Linked Immunosorbent Assay) | Cytokine concentration (e.g., IL-6, TNF-α) | Quantifying cytokine secretion in autocrine/paracrine contexts. |
| Electrophoretic Mobility Shift Assay (EMSA) | Transcription factor DNA-binding activity | Detecting NF-κB or STAT binding to DNA sequences. |
| Reporter Gene Assay | Transcriptional activity (e.g., Luciferase under NF-κB promoter) | Functional assessment of pathway activation downstream of kinase events. |
4. Experimental Protocol: Assessing JAK-STAT Activation
Title: Protocol for JAK-STAT Pathway Activation and Detection via Western Blot
Objective: To stimulate cells with a cytokine (e.g., IL-6) and detect the phosphorylation and nuclear translocation of STAT3.
Materials:
- Cell line of interest (e.g., HepG2)
- Recombinant human IL-6
- Cell culture media and serum
- Phosphatase and protease inhibitors
- Lysis Buffer (RIPA buffer)
- Nuclear Extraction Kit
- Antibodies: anti-p-STAT3 (Tyr705), anti-STAT3 (total), anti-Lamin B1 (nuclear marker), anti-β-Actin (cytosolic marker)
- SDS-PAGE and Western Blotting equipment
Methodology:
- Cell Culture and Starvation: Culture cells to 80% confluence. Serum-starve cells for 4-6 hours to reduce basal signaling activity.
- Cytokine Stimulation: Stimulate cells with IL-6 (e.g., 50 ng/mL) for a time-course (e.g., 0, 5, 15, 30, 60 minutes).
- Cell Lysis:
- Whole Cell Lysate: Aspirate media, wash with cold PBS, and lyse cells in ice-cold RIPA buffer containing inhibitors.
- Nuclear/Cytosolic Fractionation: Use a commercial kit to separate nuclear and cytosolic fractions post-stimulation.
- Protein Quantification: Determine protein concentration using a BCA or Bradford assay.
- Western Blotting: Resolve 20-30 μg of protein per lane by SDS-PAGE. Transfer to a PVDF membrane. Block with 5% BSA.
- Immunoblotting: Incubate membranes with primary antibodies (anti-p-STAT3, anti-STAT3) overnight at 4°C. Use appropriate HRP-conjugated secondary antibodies. Develop using enhanced chemiluminescence (ECL).
- Membrane Stripping and Reprobing: Strip the membrane and re-probe for loading controls (β-Actin for whole cell/cytosolic, Lamin B1 for nuclear).
Data Interpretation: Phospho-STAT3 levels should increase in whole cell lysates post-stimulation, followed by an increase in the nuclear fraction, indicating successful activation and translocation.
5. Pathway Visualizations
Title: JAK-STAT Signaling Pathway
Title: NF-κB Activation Pathway
Title: STAT Phosphorylation Assay Workflow
6. The Scientist's Toolkit
Table 3: Essential Research Reagents for Cytokine Signaling Studies
| Reagent | Function/Application | Example |
|---|---|---|
| Recombinant Cytokines | To stimulate specific pathways in cell culture models. | Human recombinant IL-6, TNF-α. |
| Phospho-Specific Antibodies | Detect activated (phosphorylated) forms of signaling proteins via Western Blot or Flow Cytometry. | Anti-phospho-STAT3 (Tyr705). |
| Pathway Inhibitors | Chemically inhibit specific kinases to establish causal relationships in signaling. | JAK Inhibitor (Ruxolitinib), IKK Inhibitor (IKK-16). |
| Proteasome Inhibitors | Block degradation of IκB, preventing NF-κB activation, used for mechanistic studies. | MG-132. |
| Nuclear Extraction Kits | Isolate nuclear and cytosolic fractions to study transcription factor translocation. | NE-PER Nuclear and Cytoplasmic Extraction Reagents. |
| siRNA/shRNA | Knock down expression of specific pathway components (e.g., JAK1, STAT3) to assess function. | Silencer Select Pre-designed siRNAs. |
| Reporter Assay Systems | Measure transcriptional activity downstream of a pathway (e.g., NF-κB Luciferase Reporter). | Cignal Lenti Reporter Assays. |
Physiological Roles in Immune Homeostasis and Tissue Repair
The immune system's role extends far beyond pathogen defense to encompass critical physiological functions in maintaining tissue homeostasis and facilitating repair. Central to these processes are intricate networks of autocrine and paracrine signaling mediated by cytokines, which coordinate cellular responses across different tissues and pathological conditions [13] [14]. This regulatory framework ensures a precise balance between pro-inflammatory responses necessary for initiating repair and anti-inflammatory mechanisms required for resolving inflammation and restoring tissue function. Dysregulation of these signaling pathways contributes significantly to chronic inflammatory states and impaired healing, particularly evident in conditions such as diabetic foot ulcers, pressure ulcers, and venous leg ulcers [13]. Recent advances in single-cell transcriptomics and spatial biology have revealed unprecedented complexity in cytokine responses, demonstrating highly cell-type-specific effects that underlie both physiological homeostasis and pathological states [15] [16]. This whitepaper synthesizes current understanding of how immune cells, particularly through cytokine signaling networks, maintain tissue integrity and drive repair processes, with implications for therapeutic development across a spectrum of inflammatory and degenerative diseases.
Cytokine Networks in Tissue Repair
Orchestrating the Repair Cascade
Tissue repair represents a finely orchestrated sequence of events involving numerous immune cell types and their signaling molecules. The process initiates with platelet activation and coagulation, which forms a provisional matrix and releases key growth factors including platelet-derived growth factor (PDGF), transforming growth factor-beta (TGF-β), and vascular endothelial growth factor (VEGF) [13]. These early signals establish a chemotactic gradient that recruits innate immune cells to the injury site. Neutrophils arrive first, clearing pathogens and cellular debris through phagocytosis and releasing proteolytic enzymes and reactive oxygen species [13]. Subsequently, monocytes enter the tissue and differentiate into macrophages, which undergo a dynamic phenotypic transition from pro-inflammatory (M1) to anti-inflammatory (M2) states—a critical switch that determines the progression from inflammation to resolution and regeneration [13].
The macrophage transition from M1 to M2 phenotype represents a pivotal checkpoint in tissue repair. M1 macrophages secrete pro-inflammatory cytokines such as TNF-α and IL-1β that maintain an inflammatory environment, while M2 macrophages produce anti-inflammatory factors including IL-10 and TGF-β that promote tissue repair [13]. This transition is regulated by a complex interplay of signals from the tissue microenvironment, with TGF-β playing a particularly crucial role. Recent research has elucidated that TGF-β1 can signal through autocrine mechanisms without dissociation from its latent complex when bound to integrin αvβ8, revealing a previously unrecognized layer of regulation in inflammatory resolution [17].
Regulatory T Cells as Orchestrators of Tissue Regeneration
Beyond innate immune mechanisms, adaptive immune cells—particularly regulatory T cells (Tregs)—play indispensable roles in tissue repair and regeneration. Originally characterized for their immunosuppressive functions, Tregs are now recognized as active contributors to tissue repair across multiple organs including skeletal muscle, heart, liver, kidneys, and skin [14]. Tissue-resident Tregs exhibit organ-specific functional specialization and contribute to repair through multiple mechanisms: suppression of excessive inflammation, direct secretion of growth factors, and support of stem cell function.
In skeletal muscle repair, Tregs accumulate following injury and facilitate the regeneration process by creating a permissive environment for muscle stem cells (MuSCs) to proliferate and differentiate [14]. Similarly, in cardiac tissue, Tregs have been shown to modulate the inflammatory response following myocardial infarction, reducing adverse remodeling and promoting functional recovery [14]. These diverse functions are enabled by the remarkable plasticity of Tregs, which can adopt distinct phenotypic states tailored to specific tissue environments. The therapeutic potential of harnessing Tregs for regenerative medicine is underscored by studies demonstrating that selective depletion of Tregs significantly impairs tissue repair across multiple organ systems [14].
Table 1: Key Immune Cell Types and Their Roles in Tissue Repair
| Cell Type | Primary Functions | Key Signaling Molecules | Tissue Specificity |
|---|---|---|---|
| M1 Macrophages | Pathogen clearance, debris phagocytosis, inflammation initiation | TNF-α, IL-1β, ROS | Ubiquitous; all injured tissues |
| M2 Macrophages | Inflammation resolution, matrix deposition, angiogenesis | IL-10, TGF-β, VEGF | Ubiquitous; all injured tissues |
| Tissue Tregs | Immune suppression, stem cell support, tissue remodeling | Amphiregulin, TGF-β, IL-10 | Tissue-specific adaptations |
| Neutrophils | Early responder, antimicrobial defense, matrix modification | MMPs, ROS, chemokines | Ubiquitous; early phase only |
| Platelets | Hemostasis, initial growth factor release | PDGF, TGF-β, VEGF | Ubiquitous; initial injury response |
Maintaining Immune Homeostasis
Cytokine Signaling Networks
Immune homeostasis depends on precisely balanced cytokine networks that maintain functional equilibrium across tissues. The Immune Dictionary project has systematically cataloged transcriptomic responses of over 17 immune cell types to 86 cytokines, revealing extraordinary specificity in cytokine-cell interactions [15]. This comprehensive analysis demonstrates that most cytokines induce highly cell-type-specific responses, with distinct gene expression programs activated in different cell types by the same cytokine. For example, the inflammatory cytokine IL-1β induces different gene programs in nearly every immune cell type, enabling a coordinated multicellular response despite using a common signaling molecule [15].
The CytoSig database further elucidates these complex signaling networks by modeling cytokine signaling activities from transcriptomic profiles [16]. This computational framework integrates 20,591 transcriptome profiles of human cytokine, chemokine, and growth factor responses, enabling prediction of signaling activities in diverse physiological and pathological contexts. Such approaches reveal that cytokine pleiotropy—where a single cytokine can have multiple different effects—largely results from cell-type-specific interpretation of shared signals rather than from inherent biochemical redundancy [16]. This understanding fundamentally shifts how we conceptualize cytokine networks in homeostasis and disease, emphasizing the importance of cellular context in determining functional outcomes.
Chromatin Regulation of Immune Responsiveness
Epigenetic mechanisms represent another critical layer of regulation in immune homeostasis. Naïve CD8+ T lymphocytes exposed to inflammatory cytokines such as IL-15 and IL-21 undergo chromatin remodeling that enhances their antigen responsiveness without full activation [18]. This "cytokine priming" creates a poised state characterized by increased chromatin accessibility at genes involved in T cell signaling, activation, effector differentiation, and negative regulation [18]. The primed cells demonstrate heightened sensitivity to subsequent antigen encounter, illustrating how cytokine signals can tune the functional potential of immune cells through epigenetic mechanisms.
Notably, cytokine priming and antigen stimulation induce partially overlapping but distinct chromatin accessibility profiles, suggesting complementary but non-identical mechanisms of immune cell preparation [18]. This priming phenomenon represents a homeostatic mechanism that allows the immune system to maintain a heightened state of readiness without initiating inappropriate activation, thereby balancing responsiveness with control. Dysregulation of such priming mechanisms may contribute to both autoimmune pathology and inadequate anti-tumor immunity.
Table 2: Experimental Platforms for Analyzing Immune Signaling Networks
| Platform/Technology | Primary Application | Key Capabilities | Limitations |
|---|---|---|---|
| CytoSig [16] | Cytokine activity prediction from transcriptomic data | Database of 20,591 cytokine response profiles; predictive modeling of signaling activities | Based primarily on in vitro data; requires validation in physiological contexts |
| Immune Dictionary [15] | Comprehensive cytokine response catalog | Single-cell transcriptomic responses to 86 cytokines across >17 immune cell types | Mouse model; human relevance requires confirmation |
| CellNEST [19] | Cell-cell communication mapping from spatial transcriptomics | Identifies relay networks (ligand-receptor-ligand-receptor chains); single-cell resolution | Computational inference; requires experimental validation |
| ATAC-seq [18] | Chromatin accessibility analysis | Genome-wide mapping of open chromatin regions; reveals regulatory landscape | Does not directly measure gene expression or protein binding |
Experimental Approaches and Methodologies
Mapping Cell-Cell Communication Networks
Understanding the spatial organization of immune signaling requires sophisticated analytical approaches. CellNEST represents a significant methodological advance by leveraging graph neural networks to decipher cell-cell communication patterns from spatial transcriptomics data [19]. This computational framework introduces relay-network communication detection, identifying multi-step signaling cascades (ligand-receptor-ligand-receptor) that form communication networks across multiple cells. Unlike methods limited to single ligand-receptor pairs, CellNEST reconstructs extended communication pathways that more accurately reflect the complexity of immune signaling in tissues.
The methodology involves several key steps: First, spatial transcriptomic data is processed to identify individual cells or spots and their gene expression profiles. Next, a graph attention network (GAT) encoder models the spatial relationships between cells, incorporating both expression data and physical proximity [19]. Finally, contrastive learning through Deep Graph Infomax (DGI) enables unsupervised identification of significant communication events without requiring predefined ground truth. This approach has been validated across multiple biological contexts, including T cell homing in lymph nodes and cancer microenvironment communication, demonstrating its utility for uncovering novel signaling networks in tissue homeostasis and repair [19].
Systematic Cytokine Response Profiling
The Immune Dictionary project established a comprehensive experimental framework for characterizing cytokine responses at single-cell resolution [15]. The methodology involves injecting individual cytokines subcutaneously in mice, followed by collection of skin-draining lymph nodes 4 hours post-injection—a timepoint capturing early transcriptomic responses. Single-cell RNA sequencing of over 386,000 cells enabled mapping of responses across more than 1,400 cytokine-cell type combinations [15].
Critical to this approach was rigorous quality control, including verification of batch-to-batch consistency and accurate cell type identification. The resulting dataset revealed an average of 51 differentially expressed genes per cytokine-cell type combination, with 72% being upregulated rather than downregulated [15]. This systematic profiling identified previously uncharacterized immune cell polarization states, such as IL-18-induced polyfunctional natural killer cells, expanding our understanding of the functional potential within immune cell populations. The accompanying analytical tool, Immune Response Enrichment Analysis (IREA), enables researchers to extract cytokine activities and immune cell states from their own transcriptomic data, facilitating translation of these findings to diverse experimental contexts [15].
The Scientist's Toolkit
Table 3: Essential Research Reagents and Resources
| Reagent/Resource | Function/Application | Key Features | Representative Examples/References |
|---|---|---|---|
| Ligand-Receptor Databases | Curated collections of known interactions for communication analysis | Foundation for computational prediction of cell-cell signaling | Databases integrated in CellNEST, NicheNet, CellChat [19] |
| Cytokine Response Signatures | Reference profiles for inferring cytokine activities from transcriptomic data | Enable deconvolution of active signaling pathways from bulk or single-cell data | CytoSig database (1,307 high-quality signatures) [16] |
| Spatial Transcriptomics Platforms | Mapping gene expression in tissue context with spatial resolution | Preservation of architectural relationships between cells | Visium, Visium HD, MERFISH [19] |
| Graph Neural Network Algorithms | Pattern recognition in spatially-resolved expression data | Identification of complex communication networks beyond pairwise interactions | CellNEST GAT encoder with DGI contrastive learning [19] |
| Chromatin Accessibility Tools | Mapping regulatory element activity and transcription factor occupancy | Reveals epigenetic basis of cellular responsiveness | ATAC-seq [18] |
| Mazethramycin | Mazethramycin, CAS:68373-96-6, MF:C17H19N3O4, MW:329.35 g/mol | Chemical Reagent | Bench Chemicals |
| MCHr1 antagonist 2 | MCHr1 antagonist 2, MF:C23H21FN2O5, MW:424.4 g/mol | Chemical Reagent | Bench Chemicals |
Signaling Pathway Visualizations
TGF-β Activation and Signaling Pathway
Cytokine Response Profiling Workflow
Chronic Wound Immune Dysregulation
The intricate interplay between immune homeostasis and tissue repair represents a frontier in understanding organismal physiology and developing novel therapeutic strategies. The emerging paradigm recognizes immune cells not merely as defenders against pathogens, but as essential architects of tissue integrity and restoration. Key advances include the recognition of highly cell-type-specific cytokine responses that enable precise coordination of repair processes [15], the discovery of non-canonical signaling mechanisms such as release-independent TGF-β activation [17], and the development of computational tools that can decode complex cell-cell communication networks from spatial transcriptomic data [19].
Future research directions will need to address several critical challenges: First, translating insights from murine models to human physiology, particularly given the species-specific differences in immune responses. Second, integrating multi-omics approaches to connect transcriptional regulation, protein signaling, and metabolic reprogramming in immune cells during tissue repair. Third, developing therapeutic strategies that can selectively modulate specific aspects of immune signaling without disrupting the delicate balance required for homeostasis. The rapidly advancing toolkit for analyzing and manipulating immune responses—including the resources described in this whitepaper—provides an exciting foundation for these future developments, with profound implications for treating degenerative, inflammatory, and neoplastic diseases.
Pathological Implications in Autoimmunity and Chronic Inflammation
Autoimmune diseases represent a complex group of disorders characterized by immune dysregulation, chronic inflammation, and multiorgan involvement, affecting approximately one in ten individuals with rising incidence, particularly in Western countries [20]. A hallmark of these conditions is the breakdown of self-tolerance, leading to the immune system mistakenly attacking healthy tissues [21]. Within this pathological framework, the autocrine and paracrine signaling of inflammatory cytokines has emerged as a critical mechanism driving disease pathogenesis. Cytokines, small signaling proteins produced by a broad range of cells including immune cells, endothelial cells, and fibroblasts, typically function through specific receptors on target cells and can signal in autocrine (acting on the same cell), paracrine (acting on nearby cells), or endocrine (systemic) manners [22].
The network dynamics of cytokine production and response govern stimulus-specific autocrine and paracrine functions that significantly impact disease progression [3]. In autoimmune conditions such as rheumatoid arthritis (RA), systemic lupus erythematosus (SLE), psoriatic arthritis (PsA), and multiple sclerosis (MS), dysregulated cytokine signaling creates self-perpetuating inflammatory loops that sustain chronic inflammation and mediate tissue damage [20] [21]. This whitepaper examines the pathological implications of these signaling mechanisms in autoimmunity, with particular focus on their role in immune cell senescence, therapeutic targeting challenges, and emerging research methodologies.
Cytokine Signaling Mechanisms in Autoimmunity
Autocrine and Paracrine Signaling Paradigms
Cytokines function as crucial immunomodulating agents through three primary signaling modalities: autocrine, paracrine, and endocrine. Autocrine signaling occurs when a cell secretes cytokines that bind to receptors on its own surface, thereby amplifying its own response. Paracrine signaling involves cytokines acting on immediately adjacent cells, while endocrine signaling refers to cytokines circulating systemically to affect distant tissues [22]. In autoimmune pathogenesis, autocrine and paracrine signaling mechanisms predominate in creating localized inflammatory milieus that drive disease processes.
The functional consequences of these signaling patterns are context-dependent and determined by underlying network dynamics. Research on tumor necrosis factor (TNF) production in macrophages has demonstrated that the same cytokine can serve distinct functions depending on the stimulus. In response to lipopolysaccharide (LPS), TNF primarily functions in a paracrine manner to activate neighboring cells, whereas in response to CpG DNA, it operates through autocrine signaling to extend the duration of NF-κB activity and shape gene expression programs [3].
Key Cytokine Families in Autoimmune Pathogenesis
Several cytokine families play particularly significant roles in autoimmune pathogenesis through their autocrine and paracrine actions:
TNF Superfamily: TNF-α is a pivotal inflammatory cytokine that coordinates innate and adaptive immune responses. It is produced by macrophages, T cells, and other immune cells upon activation and contributes to the pathogenesis of numerous autoimmune diseases including RA, Crohn's disease, and psoriasis [3]. TNF-α promotes inflammation through both autocrine and paracrine mechanisms, enhancing leukocyte migration, increasing vascular permeability, and inducing the production of other pro-inflammatory cytokines.
Interleukin Family: Multiple interleukins contribute to autoimmune pathology through complex signaling networks. IL-6, produced by macrophages, B cells, and other immune cells, promotes Th17 cell differentiation while inhibiting Treg function, creating an imbalance that drives autoimmunity [21]. IL-17, primarily secreted by Th17 cells, acts in a paracrine manner on stromal and epithelial cells to induce chemokine production and neutrophil recruitment, particularly in diseases like psoriasis and ankylosing spondylitis [20].
Interferons: Type I interferons (IFN-α and IFN-β) and type II interferon (IFN-γ) play crucial roles in autoimmune pathogenesis. In SLE, a characteristic "interferon signature" reflects the pervasive effects of IFN-α on immune cell function, while IFN-γ contributes to macrophage activation and pathogenesis in RA and multiple sclerosis [21].
Chemokines: This specialized subset of cytokines functions primarily in a paracrine manner to direct leukocyte migration and positioning. In autoimmune diseases, chemokines such as CXCL13 (B-cell attraction) and CCL2 (monocyte recruitment) create organizational networks within inflamed tissues that sustain chronic inflammation [21].
Table 1: Major Cytokine Classes and Their Roles in Autoimmunity
| Cytokine Family | Key Members | Primary Cellular Sources | Autoimmune Disease Associations |
|---|---|---|---|
| TNF Superfamily | TNF-α | Macrophages, T cells | RA, Crohn's disease, Psoriasis [3] |
| Interleukins | IL-6, IL-17, IL-10, IL-1 | Macrophages, T cells, Dendritic cells | SLE, RA, Psoriasis, Ankylosing Spondylitis [20] [21] |
| Interferons | IFN-α, IFN-β, IFN-γ | Plasmacytoid DCs, T cells, Macrophages | SLE, Multiple Sclerosis [21] |
| Chemokines | CXCL13, CCL2, CX3CL1 | Stromal cells, Macrophages, Endothelial cells | RA, Multiple Sclerosis, Lupus [21] |
Mechanistic Insights: From Signaling Dysregulation to Pathology
Immune Cell Senescence and SASP
A key mechanism linking autocrine/paracrine signaling to chronic inflammation in autoimmunity is the induction of immune cell senescence and the development of the senescence-associated secretory phenotype (SASP). Senescent immune cells become irreversibly arrested in the cell cycle, exhibit antimetabolic characteristics, and secrete pro-inflammatory mediators including TNF-α, IL-6, and IFN-γ, which disrupt immune homeostasis [21].
In T lymphocytes, senescence leads to distinctive phenotypic changes including loss of costimulatory receptors (CD27/CD28) and gain of NK-like markers (KLRG1, CD57). These senescent T cells demonstrate metabolic dysregulation, with impaired glucose transporter Glut1 and fatty acid transporters FATP2/3, along with mitochondrial dysfunction that further compromises T cell fitness [21]. The sustained exposure to cytokines and DNA damage in the autoimmune environment leads to persistent activation of ERK and P38 MAPK cascades, which activate cell cycle regulators (P53, P21, P16) that enforce cell cycle arrest and telomerase suppression—hallmarks of senescence [21].
In rheumatoid arthritis, the inflammatory milieu polarizes CD4+ T cells toward the pro-inflammatory Th17 phenotype with increased secretion of IL-17 and IL-22. Simultaneously, Tregs decrease in number and function, limiting their TGF-β and IL-10-mediated control of immune responses. This Th17/Treg imbalance is further enhanced by IL-6, which induces generation of T follicular helper (Tfh) cells that strongly stimulate autoreactive B lymphocytes to enhance autoantibody production and tissue destruction [21].
Network Dynamics and Feedback Loops
The pathological persistence of autoimmune inflammation is maintained by complex feedback loops within cytokine networks. Cytokines themselves trigger the release of other cytokines and lead to increased oxidative stress, making them central players in chronic inflammation [22]. This positive feedback amplification creates self-sustaining inflammatory circuits that are resistant to normal resolution mechanisms.
For instance, in the TNF signaling network, the same cytokine can have dramatically different functions depending on the cellular context and signaling dynamics. Research has revealed that network dynamics of MyD88 and TRIF signaling determine the stimulus-specific autocrine and paracrine functions of TNF [3]. This explains why in response to LPS, TNF does not have an autocrine function in amplifying the NF-κB response, while in response to CpG DNA, autocrine TNF extends the duration of NF-κB activity and shapes gene expression programs [3].
Table 2: Experimentally Validated Autocrine and Paracrine Functions of TNF
| TLR Agonist | Adaptor Proteins | TNF Signaling Mode | Functional Outcome | Experimental Validation |
|---|---|---|---|---|
| Lipopolysaccharide (LPS) | MyD88 and TRIF | Paracrine (not autocrine) | Potent activation of neighboring cells | Systems biology modeling with experimental confirmation in BMDMs [3] |
| CpG DNA | MyD88 | Autocrine | Extended duration of NF-κB activity, shaped gene expression | Prediction and validation in wild-type vs. knockout models [3] |
Mathematical modeling approaches have provided valuable insights into these complex network behaviors. Of the mechanistic mathematical models developed for autoimmune diseases, approximately 70% are constructed as nonlinear systems of ordinary differential equations, while others utilize partial differential equations, integro-differential equations, Boolean networks, or probabilistic models [23]. These models consistently describe core components of the immune system, particularly T-cell response, cytokine influence, and macrophage involvement in autoimmune processes [23].
Quantitative Data Analysis in Autoimmune Research
The complexity of cytokine networks in autoimmunity necessitates sophisticated quantitative approaches to elucidate pathological mechanisms. Bibliometric analysis reveals a steadily growing research output in autoimmune disease-associated pathologies, with the United States and China as the leading contributors, collectively publishing over 2,400 papers in this domain [24]. Research trends show increasing focus on immunotherapy and immune checkpoint inhibitors as potential treatment strategies [24].
Analysis of immune cell populations in autoimmune conditions provides quantitative insights into disease mechanisms. In difficult-to-treat rheumatoid arthritis, immunological profiling reveals a marked reduction in regulatory T cells accompanied by an increased Th17/Treg ratio, reflecting disrupted immune balance that correlates with heightened disease activity [20]. Similarly, complement activation products measured on B lymphocytes, erythrocytes, and platelets serve as sensitive indicators of disease activity in antiphospholipid syndrome (APS) [20].
Proteome-wide analyses have identified specific plasma proteins causally associated with autoimmune disease risk. Mendelian randomization studies have revealed seven proteins associated with psoriatic arthritis susceptibility, notably interleukin-10 (IL-10), which is inversely linked with disease risk, and apolipoprotein F (APOF), which shows a positive association [20]. In ankylosing spondylitis, eight plasma proteins including AIF1, TNF, FKBPL, AGER, ALDH5A1, and ACOT13 demonstrate causal relationships with disease risk [20].
Table 3: Quantitative Methodologies in Autoimmune Disease Research
| Methodology | Key Applications | Representative Findings | References |
|---|---|---|---|
| Systems Biology Modeling | Understanding TNF regulatory modules | TLR-specific autocrine/paracrine TNF functions | [3] |
| Bibliometric Analysis | Research trend identification | Immunotherapy and immune checkpoint inhibitors as emerging hotspots | [24] |
| Mendelian Randomization | Causal inference in disease pathogenesis | IL-10 and APOF as risk proteins in PsA; multiple proteins in AS | [20] |
| Senescent Cell Profiling | Immune aging characterization | CD28- T cells in RA, T1D, MS with CX3CR1 expression | [21] |
| Mathematical Modeling | Pathophysiology quantification | 38 models identified for 13 autoimmune conditions | [23] |
Experimental Approaches and Methodologies
Model Systems and Validation
The iterative systems biology approach has proven particularly powerful for elucidating cytokine functions in autoimmunity. This methodology involves developing quantitative understandings of regulatory modules controlling cytokine production at multiple levels—mRNA synthesis and processing, mRNA half-life, translation, and protein processing and secretion [3]. By linking models of cytokine production to models of signaling modules (e.g., TLR, TNFR, and NF-κB pathways), researchers can systematically investigate cytokine functions during inflammatory responses to diverse stimuli.
For TNF research, this approach has involved several key methodological steps: (1) quantitative measurement of TNF secretion in wild-type versus adaptor protein-deficient (trif-/- and myd88-/-) bone marrow-derived macrophages (BMDMs) stimulated with TLR agonists; (2) assessment of TNF production at mature mRNA level by RT-PCR; (3) measurement of nascent, intron-containing transcripts to distinguish transcriptional from post-transcriptional control; and (4) computational modeling integrated with experimental validation to test predictions about autocrine versus paracrine functions [3].
Synovial joint-on-a-chip models represent another innovative experimental platform that accurately mimics the joint microenvironment by integrating fluid dynamics, mechanical stimulation, and intercellular communication [20]. This technology facilitates preclinical modeling of rheumatoid arthritis, enabling precise evaluation of inflammation, drug efficacy, and personalized therapeutic strategies.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagent Solutions for Cytokine Signaling Studies
| Research Reagent | Function/Application | Experimental Context |
|---|---|---|
| Bone Marrow-Derived Macrophages (BMDMs) | Primary cell model for innate immune signaling | Investigation of TLR-responsive pathways and TNF production [3] |
| TLR Agonists (LPS, CpG DNA) | Specific activation of pattern recognition receptors | Dissection of MyD88 vs. TRIF-dependent signaling pathways [3] |
| Cytokine ELISA Kits | Quantitative protein measurement | Assessment of TNF, IL-6, and other cytokine secretion [3] |
| Senescence-Associated Biomarkers (CD57, KLRG1) | Identification of senescent immune cells | Flow cytometric analysis of T-cell senescence in autoimmunity [21] |
| Phospho-Specific Antibodies | Detection of signaling pathway activation | Analysis of MAPK (ERK, P38) and NF-κB pathway activity [21] |
| Recombinant Cytokines and Receptor Fc Fusion Proteins | Pathway activation and inhibition studies | Functional dissection of autocrine/paracrine signaling [3] |
| Mcl1-IN-1 | Mcl1-IN-1|Mcl-1 Inhibitor For Cancer Research | Mcl1-IN-1 is a potent Mcl-1 protein inhibitor. It is for Research Use Only and is not intended for diagnostic or therapeutic applications. |
| Mepronil | Mepronil, CAS:55814-41-0, MF:C17H19NO2, MW:269.34 g/mol | Chemical Reagent |
Visualization of Signaling Pathways
Autocrine and Paracrine Signaling in Autoimmunity
Cellular Signaling Modalities in Autoimmune Inflammation
TNF Signaling Dynamics in TLR Activation
Stimulus-Specific TNF Signaling Pathways
The pathological implications of autocrine and paracrine signaling in autoimmunity and chronic inflammation represent a complex yet crucial domain of immunological research. The context-specific functions of cytokines like TNF, determined by network dynamics of production and response, highlight the sophisticated regulatory mechanisms that can become dysregulated in autoimmune conditions. The emerging understanding of immune cell senescence and the SASP provides a mechanistic link between chronic cytokine exposure and persistent inflammation that characterizes progressive autoimmune diseases.
Future research directions should focus on leveraging quantitative systems pharmacology approaches and mathematical modeling to better predict therapeutic outcomes in heterogeneous patient populations. The integration of multi-omics data, advanced experimental model systems, and targeted therapeutic interventions holds promise for disrupting the pathological autocrine and paracrine signaling loops that drive autoimmunity. As our understanding of these mechanisms deepens, so too will our ability to develop precisely targeted therapies that restore immune homeostasis without compromising essential protective functions.
The tumor microenvironment (TME) is a complex ecosystem where cytokine networks act as master regulators of cancer initiation, progression, and metastasis. Operating through autocrine and paracrine signaling mechanisms, these small signaling proteins create a dynamic communication network between cancer cells and stromal components. This whitepaper examines the dualistic nature of cytokines in tumor biology, detailing their context-dependent roles as both tumor suppressors and promoters. We provide a technical analysis of key signaling pathways, experimental methodologies for cytokine research, and emerging therapeutic strategies targeting these networks for cancer treatment. The intricate balance of pro- and anti-tumor cytokines represents a critical frontier for developing next-generation immunotherapies and overcoming treatment resistance.
Cytokines are small proteins or polypeptides (5-140 kDa) that function as key signaling molecules in the TME, mediating intercellular communication through autocrine, paracrine, and endocrine mechanisms [25] [26]. These molecules are secreted by various cell types including immune cells, tumor cells, and stromal cells, creating a complex network that profoundly influences tumor behavior [25] [27]. The cytokine network exhibits significant functional plasticity, with many cytokines demonstrating a "double-edged sword" effect depending on context, concentration, and cellular environment [25].
Within the framework of autocrine and paracrine signaling research, cytokines establish self-sustaining loops that drive tumor progression. Autocrine signaling occurs when cancer cells secrete cytokines that bind to their own receptors, promoting self-proliferation and survival. Paracrine signaling involves cytokine-mediated communication between different cell types within the TME, facilitating cellular crosstalk that shapes the immunosuppressive landscape [28]. This bidirectional communication between malignant and stromal components represents a fundamental mechanism by which tumors evade immune destruction and promote their own growth [26] [27].
The dynamic regulation of cytokine networks is influenced by multiple factors including cytokine concentration, spatial distribution within the TME, temporal aspects of tumor development, and the evolving co-evolutionary relationship between tumors and the host immune system [25]. Understanding these complex interactions requires sophisticated experimental approaches that can capture the spatial and temporal dynamics of cytokine signaling in the TME.
The Dual Nature of Cytokines in Tumor Progression
Tumor-Suppressive Cytokines
Several cytokines demonstrate potent anti-tumor effects by activating immune effector cells, enhancing antigen presentation, and directly inhibiting tumor cell proliferation [25]. The table below summarizes key anti-tumor cytokines and their mechanisms of action.
Table 1: Key Cytokines with Demonstrated Tumor-Suppressive Effects
| Cytokine | Primary Cellular Sources | Main Anti-Tumor Mechanisms |
|---|---|---|
| IFN-γ | T cells, NK cells | Inhibits tumor cell growth, promotes apoptosis, upregulates MHC-I expression on tumor cells, activates M1 macrophages and NK cells [25] |
| IL-2 | T cells | Drives clonal expansion of CD4+ and CD8+ T cells, enhances cytotoxic activity of CTLs and NK cells, induces LAK cell activation [25] |
| IL-12 | Dendritic cells, macrophages | Directs naïve T cell differentiation toward Th1 phenotype, promotes IFN-γ secretion from Th1 and NK cells, enhances tumor-lytic activity of CTLs and NK cells, suppresses angiogenesis [25] |
| TGF-β (early stage) | Neutrophils, macrophages | Reduces cell proliferation, triggers apoptosis in early tumor development [25] |
| IL-36 | Epithelial cells, immune cells | Activates host immune system, synergizes with IL-2 and IL-12 to activate T cells and induce IFN-γ production [25] |
Tumor-Promoting Cytokines
In contrast to their protective functions, many cytokines acquire tumor-promoting capabilities during cancer progression, facilitating immune evasion, metastasis, and treatment resistance [25] [26]. These cytokines create a chronic inflammatory environment that supports multiple hallmarks of cancer.
Table 2: Key Cytokines with Demonstrated Tumor-Promoting Effects
| Cytokine | Primary Cellular Sources | Main Pro-Tumor Mechanisms |
|---|---|---|
| IL-6 | Macrophages, fibroblasts, tumor cells | Activates JAK-STAT3 signaling pathway, promotes tumor cell growth and prevents apoptosis, induces EMT, supports angiogenesis [25] [29] |
| TGF-β (late stage) | Macrophages, T cells | Enhances migratory and invasive abilities of tumor cells by inducing EMT, creates immunosuppressive microenvironment by reducing effector T cell function and promoting Treg development [25] [26] |
| TNF-α | Macrophages, mast cells | Induces PD-L1 overexpression in tumors, creates immunosuppressive TME, promotes resistance to targeted therapy [25] [29] |
| IL-10 | T cells, macrophages | Inhibits antigen presentation by DCs and macrophages, suppresses Th1-type immune responses, promotes Treg differentiation and longevity [25] |
| VEGF | Endothelial cells, platelets, tumor cells | Promotes angiogenesis, provides nutrients and oxygen to growing tumors [26] [27] |
| CSF-1 | Stromal cells, tumor cells | Recruits and polarizes monocytes into pro-tumor M2 macrophages [30] |
The functional duality of cytokines is particularly evident in factors like TGF-β, which exhibits stage-dependent effects—acting as a tumor suppressor in early carcinogenesis but transitioning to a potent tumor promoter in established cancers [25] [26]. This contextual duality represents a significant challenge for therapeutic targeting and underscores the importance of understanding the temporal dynamics of cytokine networks in cancer progression.
Autocrine and Paracrine Signaling Mechanisms
Fundamental Signaling Paradigms
The cytokine network operates through two primary signaling modalities that enable complex cellular crosstalk within the TME:
Autocrine Signaling: Cancer cells secrete cytokines that bind to receptors on their own surface, creating self-stimulating loops that drive uncontrolled proliferation and survival. For example, many tumors autonomously produce growth factors like EGF and FGF that sustain their expansion through autocrine mechanisms [28].
Paracrine Signaling: Stromal and immune cells within the TME secrete cytokines that influence the behavior of neighboring cancer cells, and vice versa. This bidirectional communication shapes the functional properties of the TME. A key example is the secretion of CSF-1 by tumor cells, which recruits monocytes and promotes their differentiation into pro-tumor M2 macrophages through paracrine signaling [30].
Cytokine-Mediated Cellular Crosstalk
The diagram below illustrates the complex autocrine and paracrine signaling networks between major cellular components in the tumor microenvironment.
Figure 1: Autocrine and Paracrine Cytokine Networks in TME
These signaling mechanisms establish feed-forward loops that maintain the immunosuppressive TME. For instance, tumor-derived TGF-β stimulates cancer-associated fibroblasts (CAFs) to produce additional TGF-β and IL-6, which further enhances tumor growth and immune suppression through paracrine action on both cancer cells and infiltrating lymphocytes [26] [27]. Similarly, the IL-6-STAT-3 signaling axis creates a positive feedback loop that sustains chronic inflammation and promotes tumor progression [29].
Key Signaling Pathways in Cytokine-Mediated Tumor Progression
JAK-STAT Signaling Pathway
The JAK-STAT pathway serves as a critical signaling node for multiple cytokines, including IL-6, and is frequently activated in cancer [25] [29]. The diagram below illustrates the key components and activation mechanism of this pathway.
Figure 2: JAK-STAT Signaling Pathway Activation
Chronic activation of the JAK-STAT pathway, particularly STAT-3, promotes tumorigenesis through multiple mechanisms: enhancing cancer cell proliferation and survival via upregulation of cyclins and anti-apoptotic proteins; driving angiogenesis through VEGF induction; and facilitating metastasis by activating EMT programs and matrix metalloproteinases [29]. Inflammatory cytokines like IL-6 activate this pathway through binding to their cognate receptors, initiating phosphorylation cascades that ultimately lead to transcriptional activation of pro-tumorigenic genes.
NF-κB Signaling Pathway
The NF-κB pathway serves as a central regulator of inflammation-associated cancer, connecting chronic inflammation to tumor development [29] [31]. This pathway can be activated by various stimuli including TNF-α, IL-1β, and pattern recognition receptors (PRRs) recognizing damage-associated molecular patterns (DAMPs) [31].
Table 3: Key Pro-tumorigenic Transcription Factors Activated by Cytokines
| Transcription Factor | Primary Activators | Key Target Genes | Pro-tumorigenic Functions |
|---|---|---|---|
| STAT-3 | IL-6, EGF, VEGF | Cyclin-D1, Bcl-2, Bcl-xL, VEGF, MMP-2, MMP-9 | Cell proliferation, survival, angiogenesis, metastasis [29] |
| NF-κB | TNF-α, IL-1β, LPS | IL-6, IL-8, TNF-α, Bcl-2, Bcl-xL, MMP-9 | Inflammation, cell survival, angiogenesis, invasion [29] [31] |
| SMAD | TGF-β | PAI-1, SMAD7, p15, p21 | EMT, immune suppression, extracellular matrix remodeling [26] |
These signaling pathways do not operate in isolation but exhibit significant crosstalk and redundancy. For example, NF-κB can induce the expression of IL-6, which subsequently activates STAT-3, creating a positive feedback loop that amplifies inflammatory signaling and promotes tumor progression [29]. Similarly, TGF-β signaling can synergize with NF-κB pathway to enhance EMT and metastasis [26].
Methodologies for Studying Cytokine Networks
Experimental Approaches for Cytokine Profiling
Comprehensive analysis of cytokine networks requires integration of multiple experimental techniques that capture both the spatial distribution and functional roles of these signaling molecules.
Table 4: Key Methodologies for Cytokine Network Analysis
| Methodology | Key Applications | Technical Considerations |
|---|---|---|
| Multiplex Immunoassays (Luminex, MSD) | High-throughput quantification of multiple cytokines in biological samples | Enables simultaneous measurement of 30+ analytes with small sample volumes; requires appropriate controls for matrix effects [32] |
| Single-Cell RNA Sequencing | Characterization of cytokine expression patterns at single-cell resolution | Identifies cellular sources and heterogeneity in cytokine production; requires specialized bioinformatics analysis [30] |
| Spatial Transcriptomics | Mapping cytokine expression within tissue architecture | Preserves spatial context of cytokine signaling; lower resolution than single-cell approaches but maintains tissue organization [32] |
| Cytokine Signaling Reporter Assays | Monitoring activation of specific signaling pathways in live cells | Uses engineered reporter constructs (GFP, luciferase) under control of cytokine-responsive elements; provides dynamic rather than endpoint data [33] |
| Phospho-Flow Cytometry | Quantifying phosphorylation of signaling intermediates in single cells | Enables analysis of signaling network activation in heterogeneous cell populations; requires careful antibody validation and fixation protocols [33] |
The Scientist's Toolkit: Essential Research Reagents
The table below compiles key research reagents and their applications for investigating cytokine networks in the tumor microenvironment.
Table 5: Essential Research Reagents for Cytokine Network Studies
| Reagent Category | Specific Examples | Research Applications |
|---|---|---|
| Recombinant Cytokines | Human IL-2, IL-6, TNF-α, TGF-β, IFN-γ | In vitro stimulation assays, functional validation studies, dose-response experiments [25] |
| Neutralizing Antibodies | Anti-IL-6, Anti-TGF-β, Anti-VEGF | Functional blockade of specific cytokine pathways, validation of cytokine dependencies [25] [30] |
| Signal Transduction Inhibitors | JAK inhibitors (Ruxolitinib), STAT-3 inhibitors, NF-κB inhibitors | Pathway perturbation studies, identification of critical signaling nodes [25] [29] |
| Cytokine ELISA Kits | Quantikine ELISA kits (R&D Systems) | Absolute quantification of specific cytokine concentrations in biological samples [33] |
| Multiplex Bead Arrays | Luminex xMAP technology, MSD U-PLEX | High-throughput screening of cytokine profiles in conditioned media, serum, or tissue lysates [32] |
| CRISPR-Cas9 Systems | Guide RNAs targeting cytokine receptors or signaling components | Genetic validation of cytokine pathway components, generation of knockout cell lines [30] |
| Mequitamium Iodide | Mequitamium Iodide, CAS:101396-42-3, MF:C21H25IN2S, MW:464.4 g/mol | Chemical Reagent |
| Meralein sodium | Meralein sodium, CAS:4386-35-0, MF:C19H9HgI2NaO7S, MW:858.7 g/mol | Chemical Reagent |
Experimental Workflow for Cytokine Signaling Analysis
The diagram below outlines a comprehensive experimental workflow for characterizing cytokine networks and their functional roles in the TME.
Figure 3: Cytokine Network Analysis Workflow
This integrated approach enables researchers to move from descriptive cytokine profiling to functional validation, ultimately generating mechanistic insights into how specific cytokine networks influence tumor behavior. The workflow emphasizes the importance of combining multiple complementary techniques to overcome the limitations of individual methodologies and provide a comprehensive understanding of cytokine signaling dynamics.
Therapeutic Targeting of Cytokine Networks
Current Clinical Strategies
Targeting cytokine networks has emerged as a promising approach for cancer therapy, with several strategies showing clinical promise:
Cytokine Neutralization: Monoclonal antibodies targeting pro-tumor cytokines or their receptors can disrupt pathogenic signaling networks. For example, IL-6 blockade with siltuximab has shown efficacy in certain lymphoproliferative disorders, while TGF-β inhibitors are being investigated in multiple solid tumors [25] [26].
Receptor Antagonists: Small molecule inhibitors targeting cytokine receptors or downstream signaling components can abrogate pro-tumor signaling. JAK inhibitors have demonstrated clinical activity in myeloproliferative neoplasms driven by dysregulated cytokine signaling [25] [29].
Combination with Immune Checkpoint Blockade: Cytokine modulation can synergize with PD-1/PD-L1 inhibitors to overcome resistance mechanisms. The combination of TGF-β blockade with PD-L1 inhibition has shown promising results in advanced tumors by mitigating the immunosuppressive TME [25] [30].
Emerging Therapeutic Approaches
Several innovative approaches are currently under investigation for targeting cytokine networks in cancer:
Bispecific Cytokine Engagers: Engineered molecules that simultaneously target tumor antigens and cytokine receptors can locally deliver immune-stimulatory cytokines while minimizing systemic toxicity [25] [33].
TAM Reprogramming: Strategies to redirect tumor-associated macrophages from pro-tumor (M2) to anti-tumor (M1) phenotypes through CSF-1R inhibition or CD47 blockade can alter the cytokine milieu of the TME [30].
Nanoparticle-Mediated Delivery: Encapsulation of cytokine modulators in nanoparticles enables targeted delivery to the TME, enhancing efficacy while reducing off-target effects [30] [26].
The therapeutic targeting of cytokine networks faces several challenges, including functional redundancy in cytokine signaling, context-dependent effects of specific cytokines, and the development of compensatory mechanisms that limit long-term efficacy. Future strategies will likely require sophisticated combination approaches that simultaneously target multiple nodes within these complex networks.
Cytokine networks represent a critical regulatory layer in the tumor microenvironment, orchestrating complex interactions between cancer cells and stromal components through autocrine and paracrine signaling mechanisms. The functional duality of many cytokines—capable of both suppressing and promoting tumor progression—highlights the contextual complexity of these signaling networks. A comprehensive understanding of cytokine biology requires sophisticated experimental approaches that capture the spatial, temporal, and functional dynamics of these systems within the TME. Emerging therapeutic strategies that target specific cytokine networks, particularly in combination with other modalities, hold significant promise for overcoming treatment resistance and improving outcomes for cancer patients. Future research should focus on deciphering the contextual rules governing cytokine function, developing more sophisticated models of network behavior, and translating these insights into targeted therapeutic interventions that modulate the immune landscape of tumors.
Positive and Negative Feedback Loops in Inflammatory Pathways
Inflammatory signaling pathways are fundamentally regulated by an intricate network of positive and negative feedback loops that determine the magnitude, duration, and spatial distribution of immune responses. These regulatory mechanisms operate through autocrine (self-signaling) and paracrine (neighboring cell signaling) communication of cytokines, particularly tumor necrosis factor-alpha (TNFα) and interleukins, to maintain immunological balance [3] [22]. Dysregulation of these feedback mechanisms contributes to pathological conditions including autoimmune diseases, cytokine storm syndromes, and impaired tissue regeneration [34] [35]. This technical review examines the molecular architecture of these feedback loops, their functional consequences in health and disease, and emerging therapeutic strategies for their modulation. Understanding these regulatory circuits provides critical insights for developing targeted interventions in inflammatory disorders and optimizing immune responses.
The inflammatory response represents a carefully orchestrated sequence of molecular events designed to eliminate pathogens and repair tissue damage. Central to this process are feedback mechanisms that amplify or attenuate signaling to achieve an appropriate response level. Positive feedback loops enhance signal transduction and promote robust immune activation, while negative feedback loops terminate signaling to prevent excessive inflammation and collateral tissue damage [36].
These feedback mechanisms operate through sophisticated cytokine networks that function in autocrine, paracrine, and endocrine fashions. Autocrine signaling occurs when a cell responds to cytokines it itself produces, enabling self-amplification or self-regulation of inflammatory responses. Paracrine signaling involves cytokine communication between neighboring cells, allowing for localized amplification or containment of inflammation within tissue microenvironments [3] [37]. The dynamic interplay between these signaling modes and feedback loops enables precise spatiotemporal control of inflammation, though dysregulation can lead to either uncontrolled inflammation or immunodeficiency.
Molecular Mechanisms of Key Inflammatory Feedback Loops
The NF-κB/TNFα Autocrine Feedback Loop
The NF-κB/TNFα axis represents a paradigmatic example of inflammatory feedback regulation with distinct autocrine and paracrine functions. Research using zebrafish models has revealed that NF-κB activity differentially regulates TNFα through TNF receptors 1a and 1b to control macrophage responses to injury [34].
Mechanism Details:
- Upon tissue injury, macrophages recruited to the site show rapid NF-κB activation and tnfa expression initiation from 2 hours post-amputation [34]
- NF-κB acts as a brake to uncontrolled TNFα signaling in an autocrine manner within macrophages
- Inhibition of NF-κB through IKK2 inhibitors (BMS-345541) or p65 nuclear translocation inhibitors (JSH-23) results in elevated TNFα expression and more directional macrophage migration
- This feedback disruption leads to prolonged inflammatory environments at wound blastemas and impaired regeneration [34]
Table 1: Quantitative Effects of NF-κB Pathway Manipulation on Cytokine Expression
| Experimental Condition | Pro-inflammatory Cytokines | Anti-inflammatory Cytokines | Macrophage Behavior |
|---|---|---|---|
| NF-κB silencing (iDREADD) | Increase up to 300% (IL-1β: 200→800 pg/ml) | Profound reduction (IL-10: 750→250 pg/ml) | More directional migration |
| NF-κB activation (hM3Dq) | Reduction ~70% | Increase nearly 10-fold | Not specified |
| IKK2 inhibition (BMS-345541) | Early reduction (3h); later elevation (6h) of tnfa | Increased il10 expression | Not specified |
MST1-Mediated NLRP3 Inflammasome Feedback
The Hippo pathway kinase MST1 mediates a recently characterized negative feedback loop that maintains NLRP3 inflammasome homeostasis [38].
Mechanism Details:
- NLRP3 inflammasome activation induces caspase-1-dependent cleavage of MST1 at its inhibitory linker region
- MST1 cleavage enhances its kinase activity, leading to phosphorylation of the inflammasome adaptor protein ASC at serine 58
- ASC phosphorylation disrupts ASC oligomerization, thereby attenuating inflammasome assembly
- Chemical induction of MST1 cleavage with staurosporine mitigates inflammation and tissue damage in LPS-induced sepsis models [38]
This feedback mechanism represents a promising therapeutic target for controlling inflammation, as it enables precise regulation of inflammasome activity without completely abolishing this critical defense mechanism.
Body-Brain Neural Regulation of Inflammation
Recent research has identified a body-brain circuit that regulates inflammatory responses through neural signaling [35]. This circuit represents a systemic negative feedback mechanism that operates across physiological systems.
Mechanism Details:
- Pro-inflammatory and anti-inflammatory cytokines communicate with distinct populations of vagal neurons
- These neurons signal to a genetically defined population of neurons in the brainstem (caudal nucleus of the solitary tract, cNST)
- cNST neurons tightly modulate the course of peripheral immune responses
- Genetic silencing of this circuit produces unregulated, exaggerated inflammatory responses, while activation suppresses pro-inflammatory responses and enhances anti-inflammatory states [35]
Table 2: Body-Brain Circuit Manipulation Effects on Inflammation
| Intervention | Neural Target | Pro-inflammatory Effect | Anti-inflammatory Effect |
|---|---|---|---|
| Circuit silencing | cNST neurons (iDREADD) | IL-1β increased to 300% of control | IL-10 reduced to 33% of control |
| Circuit activation | cNST neurons (hM3Dq) | Reduction to ~30% of control levels | Increase to ~1000% of control |
| Excitatory neuron activation | Vglut2-cre cNST neurons | Effective suppression | Enhanced response |
| Inhibitory neuron activation | Vgat-cre cNST neurons | No significant effect | No significant effect |
Experimental Analysis of Feedback Loops
Methodologies for Feedback Loop Characterization
Systems Biology Approaches: Iterative systems biology approaches combining experimental studies with computational models have proven particularly fruitful for developing predictive understanding of TNF production and feedback regulation [3]. This methodology involves:
- Regulatory Module Identification: Considering each regulatory mechanism as a module with defined inputs and outputs
- Mathematical Modeling: Constructing and parameterizing simple mathematical models to represent these modules
- Model Integration: Linking production models with signaling pathway models (TLR, TNFR, NF-κB)
- Experimental Validation: Testing model predictions through genetic and pharmacological interventions
Genetic Targeting Strategies:
- TRAP System: Targeted recombination in active populations enables genetic access to neurons activated by immune challenges [35]
- DREADD Technology: Chemogenetic silencing or activation of specific neuronal populations permits causal analysis of circuit function in immune regulation
- Cell-type-specific Cre drivers: Vglut2-cre and Vgat-cre mice allow selective manipulation of excitatory versus inhibitory neuronal populations in inflammatory control
Functional Imaging and Monitoring:
- Immediate early gene mapping: Fos induction identifies neurons activated by immune stimuli
- Fiber photometry: GCaMP6s expression enables real-time monitoring of neuronal population activity in awake, behaving animals during immune responses
- Single-cell RNA sequencing: Identifies molecularly defined cell populations involved in inflammatory feedback regulation [35]
Research Reagent Solutions
Table 3: Essential Research Reagents for Inflammatory Feedback Analysis
| Reagent/Category | Specific Examples | Research Application | Key Functions |
|---|---|---|---|
| Cytokine Measurement | ELISA for IL-6, IL-10, TNFα | Quantifying inflammatory responses | Protein-level cytokine quantification |
| Gene Expression Analysis | qRT-PCR for il1b, il6, tnfa, ikbaa | Transcriptional response assessment | mRNA-level cytokine and pathway analysis |
| Pathway Inhibitors | BMS-345541 (IKK2 inhibitor), JSH-23 (p65 translocation inhibitor) | Pathway manipulation studies | Specific inhibition of NF-κB signaling nodes |
| Genetic Silencing/Activation | DREADDs (iDREADD, hM3Dq), Cre-lox system | Circuit manipulation | Chemogenetic control of specific cell populations |
| Activity Reporters | Fos mapping, GCaMP6s, NFKB:EGFP, tnfa:egfp reporters | Neural and immune cell activity monitoring | Real-time activity reporting in specific cell types |
| Single-cell Analysis | scRNA-seq protocols | Cell population identification | Molecular profiling of heterogeneous cell types |
Signaling Pathway Diagrams
Diagram 1: NF-κB/TNFα Feedback Architecture. This diagram illustrates the core NF-κB/TNFα feedback loop showing both positive (green) and negative (red) regulatory components. The pathway begins with LPS binding to TLR4 receptors, initiating signaling through MyD88 and IKK that activates NF-κB. Nuclear-translocated NF-κB induces TNFα gene expression, leading to TNFα protein production. TNFα signals through TNF receptors in autocrine and paracrine fashion, reinforcing IKK activation (positive feedback). Simultaneously, NF-κB induces negative feedback mechanisms that inhibit IKK activity, creating a balanced regulatory system [3] [34].
Diagram 2: MST1/NLRP3 Negative Feedback Mechanism. This diagram details the MST1-mediated negative feedback loop that controls NLRP3 inflammasome activity. Inflammasome activation triggers caspase-1-mediated cleavage of MST1, enhancing its kinase activity. Activated MST1 phosphorylates the adaptor protein ASC at serine 58, which disrupts ASC oligomerization and subsequent inflammasome assembly. This negative feedback mechanism prevents excessive inflammasome activation while maintaining baseline surveillance capacity, representing a key homeostatic control point in inflammatory responses [38].
Discussion and Research Implications
The sophisticated feedback mechanisms governing inflammatory pathways represent promising targets for therapeutic intervention across a spectrum of diseases. The discovery that NF-κB acts as a brake on TNFα signaling in macrophages reveals potential strategies for enhancing tissue regeneration by fine-tuning this feedback relationship [34]. Similarly, the MST1/NLRP3 feedback loop offers opportunities for developing specific modulators that could temper excessive inflammasome activation in autoinflammatory diseases without completely abolishing this critical defense mechanism [38].
The emerging understanding of neural regulation of inflammation through the body-brain axis opens entirely new avenues for therapeutic development. The demonstration that activating specific brainstem circuits can suppress peripheral inflammation by nearly 70% while boosting anti-inflammatory responses tenfold suggests novel neuromodulatory approaches for treating cytokine storm syndromes and autoimmune conditions [35]. This neuroimmune axis represents a master regulator that could potentially be harnessed to rebalance immune function in diverse pathological states.
Future research should focus on developing more precise tools for manipulating specific feedback components in spatially and temporally controlled manners, as well as computational models that can predict the system-level consequences of therapeutic interventions targeting these regulatory circuits. The integration of single-cell technologies with functional imaging will further illuminate the cellular heterogeneity within these regulatory networks, potentially revealing cell-type-specific feedback mechanisms that could be targeted with greater precision and fewer off-target effects.
Cross-talk Between Autocrine, Paracrine, and Endocrine Systems
The intricate cross-talk between autocrine, paracrine, and endocrine signaling systems forms a complex regulatory network essential for maintaining physiological homeostasis. These communication paradigms, distinguished by the spatial scale over which signaling molecules operate, exhibit profound interdependencies particularly evident in inflammatory processes. Within the context of inflammatory cytokine research, this interplay enables precise localization, amplification, and resolution of immune responses. Dysregulation of these communicative networks underpins numerous pathological states, including autoimmune diseases, cancer, and metabolic disorders. This whitepaper provides a comprehensive technical examination of the mechanisms governing cross-talk between these signaling systems, with emphasis on experimental methodologies, computational frameworks, and therapeutic implications relevant to research scientists and drug development professionals.
Cell-cell communication (CCC) represents a fundamental characteristic of multicellular organisms, enabling the coordination of cellular activities essential for development, homeostasis, and immune responses [11]. Communication occurs through several distinct paradigms classified primarily by the distance over which signaling molecules travel: autocrine (self-signaling), paracrine (local signaling to adjacent cells), and endocrine (systemic signaling via circulation) [1] [39]. Inflammatory cytokines exemplify molecules that operate across all three modalities, allowing for finely-tuned regulation of immune processes [2] [22].
The conceptual distinction between these systems lies not only in spatial range but also in temporal dynamics, concentration gradients, and functional consequences. Paracrine signals typically elicit rapid, transient responses within localized tissue environments, while endocrine signals produce slower-onset, sustained effects throughout the organism [1] [39]. Autocrine signaling often serves amplification or self-regulatory functions, particularly during developmental processes and immune cell activation [1]. Understanding the integrated operation of these systems is paramount for deciphering complex physiological and pathological processes, especially in inflammation research where cytokine networks demonstrate remarkable plasticity and redundancy [2] [22].
Defining the Signaling Paradigms
Autocrine Signaling
Autocrine signaling occurs when cells respond to signaling molecules that they themselves produce and secrete [1] [39]. This self-referential communication mechanism enables individual cells or homogeneous cell populations to reinforce developmental decisions, synchronize responses, and regulate their own activation states. In immunological contexts, autocrine signaling provides critical positive feedback loops that amplify immune responses. For instance, macrophages utilizing autocrine TNF signaling can dramatically enhance their inflammatory output upon pathogen recognition [3]. The autocrine loop represents a fundamental regulatory module wherein a cell secretes a ligand that binds to receptors on its own surface, initiating intracellular signaling cascades that modulate gene expression and cellular behavior [40].
From a technical perspective, demonstrating bona fide autocrine signaling requires stringent experimental validation, as distinguishing true autocrine actions from paracrine signaling within homogeneous cell populations presents methodological challenges. Genetic approaches employing cell-type-specific receptor deletion or pharmacological inhibition of ligand secretion provide compelling evidence for autocrine mechanisms.
Paracrine Signaling
Paracrine signaling involves the secretion of signaling molecules that act locally on adjacent or nearby cells of different types [1] [41]. This short-range communication modality allows for precise spatial control of cellular responses within tissue microenvironments. Paracrine factors typically exhibit limited diffusion ranges due to rapid degradation, extracellular matrix binding, or uptake by neighboring cells, thereby restricting their action to the immediate cellular environment [39]. Classic examples include neurotransmitter signaling across synaptic clefts, cytokine-mediated communication between immune cells, and growth factor signaling during tissue development and repair [1] [41].
In inflammatory contexts, paracrine cytokine signaling enables coordinated responses between diverse cell types—immune cells, endothelial cells, fibroblasts—within inflamed tissues [3] [2]. For instance, TNF can function in a potent paracrine manner between neighboring cells, allowing localized amplification of inflammatory signals without triggering systemic consequences [3]. The spatial restriction of paracrine signaling makes it particularly amenable to therapeutic targeting with localized drug delivery approaches.
Endocrine Signaling
Endocrine signaling involves the secretion of hormones into the systemic circulation, enabling communication with distant target cells throughout the organism [1] [39]. This long-range signaling system coordinates whole-body physiological processes such as metabolism, growth, and stress responses. Endocrine signals typically exhibit slower onset but longer duration compared to paracrine signals, owing to the time required for circulation and the stability of many hormones in the bloodstream [1]. Classic endocrine organs include the pituitary, thyroid, and adrenal glands, though numerous tissues possess endocrine functions [40].
Several cytokines can also operate in an endocrine fashion when produced in sufficient quantities, particularly during systemic inflammation or sepsis [2] [22]. For example, IL-6 can function as both a paracrine inflammatory mediator within tissues and an endocrine hormone when reaching circulation, where it induces acute-phase protein production in the liver [22]. This endocrine dimension of cytokine biology represents a crucial interface between the immune system and overall physiological status.
Table 1: Comparative Characteristics of Signaling Paradigms
| Feature | Autocrine | Paracrine | Endocrine |
|---|---|---|---|
| Spatial Range | Same cell or same cell type | Local microenvironment (<100 μm) | Whole organism (via circulation) |
| Signaling Molecules | Cytokines, growth factors | Neurotransmitters, cytokines, eicosanoids | Hormones, some cytokines |
| Temporal Dynamics | Rapid (milliseconds-minutes) | Rapid (seconds-minutes) | Slower (minutes-hours) |
| Concentration at Target | Can be very high | High locally, steep gradient | Low (picomolar-nanomolar) |
| Example in Inflammation | TNF amplification in macrophages [3] | Neutrophil recruitment by chemokines | Systemic IL-6 in sepsis [22] |
| Therapeutic Targeting | Cell-intrinsic inhibitors | Localized drug delivery | Systemic administration |
Quantitative Comparison of Signaling Systems
The differentiation between autocrine, paracrine, and endocrine signaling extends beyond qualitative descriptions to quantifiable parameters including concentration gradients, diffusion coefficients, receptor affinity, and temporal dynamics. Endocrine signals circulate at picomolar to nanomolar concentrations and may exhibit concentration variations of several orders of magnitude during physiological challenges, while paracrine signals can achieve micromolar concentrations in localized environments such as synaptic clefts or immune synapses [1] [22]. The effective concentration of autocrine signals at the cell surface remains challenging to quantify but may approach the high local concentrations seen in paracrine signaling.
The following diagram illustrates the fundamental differences in spatial scale and mechanism between the three signaling systems:
Table 2: Quantitative Parameters of Inflammatory Cytokine Signaling
| Parameter | Autocrine TNF | Paracrine Chemokine | Endocrine IL-6 |
|---|---|---|---|
| Effective Concentration | ~10-100 nM (local) | ~1-10 nM (synapse) | ~0.1-1 nM (serum) |
| Diffusion Coefficient | Limited by self-binding | 10-100 μm²/s (tissue) | Systemic circulation |
| Response Time | Seconds-minutes | Seconds-minutes | Minutes-hours |
| Signal Duration | Short (min) unless reinforced | Short (min) | Longer (hours-days) |
| Receptor Kd | 0.1-1 nM | 1-10 nM | 0.1-1 nM |
| Pathway Specificity | High (cell-autonomous) | Context-dependent | Systemic effects |
Experimental Methodologies for Studying Cross-talk
Computational Inference of Cell-Cell Communication
Advanced computational methods have revolutionized our ability to decipher complex cell-cell communication networks from high-throughput data. The LIANA framework provides an open-source interface to multiple resources and methods for ligand-receptor analysis, enabling systematic inference of CCC from single-cell RNA sequencing data [42]. This approach leverages prior knowledge from 16 dedicated CCC resources containing ligand-receptor interactions, which can be combined with 7 distinct inference methods to predict autocrine, paracrine, and endocrine interactions [42].
The experimental workflow typically involves: (1) single-cell RNA sequencing to characterize cellular heterogeneity and identify cell clusters; (2) assignment of cell type identities based on known gene markers; (3) application of CCC inference tools to predict potential communication events between cell clusters; and (4) integration with spatial transcriptomics or protein data for validation [42]. Critical considerations include the choice of prior knowledge resource, as different databases show limited overlap and uneven coverage of specific pathways, and method selection, as each employs different scoring systems to prioritize interactions [42].
The following diagram outlines a representative computational workflow for inferring cell-cell communication from single-cell data:
Experimental Validation of TNF Autocrine and Paracrine Functions
Caldwell et al. provided a seminal example of how to dissect autocrine versus paracrine functions through an iterative systems biology approach combining mathematical modeling with experimental validation [3]. Their methodology for investigating TNF signaling in macrophages included:
Computational Modeling Components:
- Development of quantitative models for TNF mRNA synthesis, processing, half-life, translation, and protein processing/secretion
- Linking TNF production models to established TLR, TNFR, and NFκB signaling modules
- Model parameterization using wild-type, trif−/−, and myd88−/− bone marrow-derived macrophages (BMDMs)
- Simulation predictions of autocrine versus paracrine functions under different TLR agonist conditions
Experimental Validation Protocols:
- Cell Culture: Primary murine BMDMs stimulated with LPS (TLR4 agonist engaging both MyD88 and TRIF) or CpG DNA (TLR9 agonist engaging only MyD88)
- TNF Measurement: ELISA of secreted TNF in supernatant at multiple time points (1-4 hours)
- mRNA Analysis: RT-PCR of mature TNF transcripts and nascent intron-containing transcripts
- Pathway Inhibition: Antibody-mediated neutralization of secreted TNF to disrupt paracrine signaling
- Genetic Approaches: Comparison of wild-type versus receptor-deficient cells
This integrated approach revealed that TNF exhibits stimulus-specific functions: while LPS-induced TNF primarily operates through paracrine mechanisms with minimal autocrine contribution, CpG DNA-induced TNF significantly amplifies NFκB responses through autocrine signaling [3]. This methodology provides a template for rigorously distinguishing autocrine from paracrine actions in inflammatory contexts.
Spatial Mapping of Signaling Activities
GRASP (GFP reconstitution across synaptic partners) represents a powerful technique for visualizing sites of cell-cell contact and communication [11]. This method employs two nonfluorescent split GFP fragments fused to interacting partners on opposing cells; when cells make contact, the fragments associate and reconstitute functional GFP, enabling precise spatial mapping of interactions [11]. Advanced implementations now include multiple split fluorescent proteins (YFP, CFP) for simultaneous imaging of several interaction factors.
Additional approaches for spatial mapping include:
- Optical super-resolution microscopy (photoactivated localization microscopy) for nanometer-resolution imaging of fluorescent proteins within cells [11]
- Single-cell RNA sequencing coupled with spatial transcriptomics to correlate gene expression patterns with tissue architecture
- Proximity-based chemical labeling to identify proteins in immediate cellular environments
- Mechanical force analysis to quantify physical interactions between cells
The Inflammatory Cytokine Network: A Case Study in Cross-talk
Cytokines represent a particularly illustrative example of molecules operating across autocrine, paracrine, and endocrine contexts [2] [22]. These small signaling proteins (~5-25 kDa) include chemokines, interferons, interleukins, lymphokines, and tumor necrosis factors, and are produced by a broad range of cells including immune cells, endothelial cells, fibroblasts, and various connective tissue cells [2] [22].
The functional classification of cytokines into pro-inflammatory (e.g., TNFα, IFN-γ, IL-1, IL-6) and anti-inflammatory (e.g., TGF-β, IL-4, IL-10, IL-13) categories reflects their roles in regulating immune responses, with cytokines in one subset often inhibiting the effects of those in the other [22]. This regulatory balance becomes particularly important in cytokine storms, where excessive pro-inflammatory cytokine production leads to life-threatening systemic inflammation [2].
The following diagram illustrates how inflammatory cytokines operate across signaling modalities to coordinate immune responses:
Research Reagent Solutions for Cross-talk Studies
Table 3: Essential Research Tools for Studying Signaling Cross-talk
| Reagent Category | Specific Examples | Research Application | Technical Considerations |
|---|---|---|---|
| CCC Inference Resources | OmniPath, CellPhoneDB, CellChatDB, LIANA [42] | Prior knowledge for ligand-receptor interaction prediction | Resource selection strongly influences predictions; consider pathway coverage biases |
| Single-Cell Technologies | 10X Genomics, Drop-Seq, inDrop [11] | Cellular heterogeneity mapping and CCC inference | Enables identification of rare cell populations and their communication patterns |
| Spatial Biology Tools | GRASP, optical super-resolution microscopy, spatial transcriptomics [11] | Mapping interaction sites and validating predicted CCC | GRASP enables visualization of specific cell-cell contacts in living systems |
| Cytokine Measurement | ELISA, Luminex, cytokine panels [3] [2] | Quantifying cytokine levels in different compartments | Multiplex approaches enable comprehensive cytokine profiling |
| Pathway Reporter Systems | NFκB-GFP, STAT-luciferase, AP-1 assays [3] | Monitoring downstream signaling activities | Critical for validating functional consequences of signaling events |
| Genetic Manipulation Tools | CRISPR/Cas9, siRNA, conditional knockout systems [3] | Dissecting specific pathway components | Enables causal testing of specific ligands, receptors, or pathway elements |
Clinical Implications and Therapeutic Targeting
Dysregulation of autocrine, paracrine, and endocrine cross-talk contributes significantly to disease pathogenesis across multiple organ systems. In autoimmune conditions such as rheumatoid arthritis, dysregulated cytokine signaling creates self-amplifying inflammatory loops that perpetuate tissue damage [2] [22]. In cancer, tumor cells co-opt normal communication mechanisms to establish supportive microenvironments, promote angiogenesis, and evade immune surveillance [41] [11]. Metabolic disorders including type 2 diabetes involve disrupted cross-talk between pancreatic endocrine and exocrine functions, as well as communication between metabolic and immune tissues [43].
Therapeutic strategies targeting communicative networks include:
- Cytokine inhibitors such as TNFα antagonists (e.g., infliximab, adalimumab) that intercept paracrine and endocrine inflammatory signaling
- Receptor blockers including IL-6 receptor antibodies (tocilizumab) and chemokine receptor antagonists
- JAK-STAT pathway inhibitors that target intracellular signaling downstream of multiple cytokine receptors
- Stem cell therapies that leverage paracrine factors for tissue repair and regeneration [41]
Understanding signaling cross-talk is particularly relevant for managing cytokine release syndrome (CRS), a potentially life-threatening condition that can occur with certain immunotherapies [2]. In CRS, excessive activation of immune cells leads to massive cytokine production that operates through all three signaling modalities: autocrine amplification, paracrine recruitment, and endocrine systemic effects [2]. Therapeutic interventions typically target key cytokines (especially IL-6) that drive this pathological communication network.
The cross-talk between autocrine, paracrine, and endocrine systems represents a fundamental organizing principle in physiology and pathology. Inflammatory cytokines exemplify how signaling molecules operate across these spatial scales to coordinate immune responses, with autocrine signaling enabling amplification, paracrine signaling facilitating local coordination, and endocrine signaling mediating systemic effects. The integrated function of these systems allows for precisely regulated inflammatory responses that can be rapidly activated yet appropriately contained.
Future research directions include developing more sophisticated computational models that incorporate spatial constraints, dynamic receptor expression, and multi-ligand interactions; advancing single-cell technologies that simultaneously measure ligand production, receptor occupancy, and downstream signaling in complex tissues; and creating therapeutic strategies that specifically target pathological communication patterns while preserving physiological signaling. As our understanding of these communicative networks deepens, we anticipate more precise therapeutic interventions that can selectively modulate autocrine, paracrine, or endocrine dimensions of disease processes while preserving beneficial communicative functions.
Advanced Research Techniques and Experimental Approaches
Microfluidic Platforms for Parsing Autocrine and Paracrine Signals
The study of cell-to-cell communication via soluble factors is fundamental to understanding physiological and pathological processes, including inflammation and cancer progression. Autocrine signaling, where a cell responds to its own secreted signals, and paracrine signaling, where a cell influences its neighbors, are particularly crucial in the context of inflammatory cytokine networks. Traditional in vitro models often lack the spatiotemporal control necessary to deconvolute these complex signaling dynamics. This whitepaper provides an in-depth technical guide to advanced microfluidic platforms that enable researchers to overcome these limitations. By offering precise control over microenvironmental conditions, spatial arrangement of different cell types, and temporal sequencing of interactions, microfluidic technologies are revolutionizing the study of inflammatory cytokine signaling, with significant implications for drug discovery and development.
Inflammatory processes are orchestrated by a complex cascade of cytokine-mediated communication between immune cells (such as macrophages and T-cells), stromal cells, and tissue-specific cells. Parsing autocrine from paracrine signaling is technically challenging but biologically critical, as these distinct signaling modes can elicit different cellular responses and contribute differentially to disease progression. For instance, in the tumor microenvironment, cancer cells can manipulate macrophage polarization through paracrine signaling, which in turn influences angiogenesis and tumor progression through additional paracrine effects [44]. Similarly, understanding B-cell dynamics in autoimmune diseases requires disentangling autocrine survival signals from paracrine differentiation cues [45].
Microfluidic platforms address key limitations of conventional culture systems by:
- Providing precise spatial compartmentalization for different cell types while permitting controlled molecular exchange
- Enabling sequential introduction and removal of specific cell populations or stimuli
- Minimizing reagent volumes while maximizing experimental information content
- Supporting high-resolution, real-time monitoring of cellular responses
These capabilities make microfluidics particularly suited for investigating the spatiotemporal dynamics of inflammatory cytokine networks, where timing, sequence, and cellular context are critical determinants of functional outcomes.
Microfluidic Platform Architectures and Operating Principles
Reconfigurable Open Microfluidics (Stacks System)
The Stacks system represents a significant advancement in microfluidic design for studying sequential paracrine signaling events. This platform utilizes open and suspended microfluidic principles, where fluids are constrained in microchannels that lack a ceiling or floor, enabling direct access and reconfigurability [44].
Operating Principle: The system comprises stackable layers, each containing an array of open-microfluidic wells and channels accessible by pipette. Each layer can be independently configured to support different microenvironment conditions (2D culture, 3D matrices, or specific cell types). When stacked, these layers form interconnected microenvironments that allow diffusion-based communication without requiring tubing, pumps, or permanent bonding [44].
Key Innovation: The T-shaped pinning feature at layer connections uses surface tension to maintain fluidic integrity without leakage between layers, enabling stable multi-layered cultures while permitting dynamic reconfiguration during experiments [44]. This architecture specifically facilitates the modeling of complex sequential signaling events, such as tumor-cell-mediated macrophage differentiation followed by macrophage-facilitated angiogenesis.
Diffusion-Based Paracrine Signaling Platforms
Another microfluidic architecture employs parallel channels separated by arrays of posts that allow diffusion of paracrine molecules between adjacent cell populations. Computational modeling of these systems reveals that channel spacing significantly affects both spatial and temporal distribution of signaling molecules, while initial concentration primarily influences concentration gradients established by secreted factors [46].
Validation Model: This platform has been validated using a three-component system where lipopolysaccharide (LPS) diffuses to activate macrophages, which then secrete TNF-α that subsequently activates reporter cells in an adjacent channel. Quantitative response measurements demonstrated the platform's capability to capture dose-dependent paracrine signaling dynamics [46].
Droplet-Digital Microfluidic Integration
For single-cell secretion analysis, integrated droplet-digital (D2) platforms combine high-throughput droplet generation with the precise manipulation capabilities of digital microfluidics. This approach enables encapsulation of individual cells into picoliter droplets, fluorescence-activated sorting based on secreted factor detection, and efficient recovery of specific cells for downstream analysis [47].
Performance Advantage: This platform achieves an 18-fold increase in recovery rate of individual cells from droplets compared to conventional methods, addressing a critical bottleneck in linking functional secretion profiles to cellular characteristics [47]. This is particularly valuable for studying rare autocrine-signaling cells within heterogeneous populations.
Active Microfluidic Manipulation Systems
Emerging active microfluidic devices employ external fields (electrical, optical, magnetic, or acoustic) to manipulate individual cells with high precision. These systems eliminate the need for complex fluidic networks and valves while enabling addressable single-cell control [48].
Application Scope: These platforms are particularly suited for studying autocrine signaling at the single-cell level, as they can isolate individual cells, control their microenvironment, and monitor dynamic secretion profiles over time, all while minimizing cross-contamination between experimental conditions [48].
Quantitative Performance Comparison of Microfluidic Platforms
Table 1: Performance Characteristics of Microfluidic Platforms for Signaling Studies
| Platform Type | Spatial Control | Temporal Control | Throughput | Key Advantages | Signaling Focus |
|---|---|---|---|---|---|
| Reconfigurable Stacks | High (modular layers) | High (dynamic reconfiguration) | Medium (multiple conditions) | Enables sequential signaling studies; Independent conditioning | Paracrine (sequential) |
| Diffusion-Based Channels | Medium (fixed architecture) | Low (static setup) | Low to medium | Simplicity; Computational modeling support | Soluble factor-cell & Cell-cell paracrine |
| Droplet-Digital | High (single cells) | Medium (on-demand control) | High (thousands of droplets) | Links phenotype to function; High recovery efficiency | Autocrine & Single-cell paracrine |
| Active Microfluidics | Very high (single-cell manipulation) | High (real-time control) | Variable | Contact-free manipulation; Multi-modal integration | Autocrine & Micro-environment control |
Table 2: Technical Specifications for Signaling Studies
| Parameter | Reconfigurable Stacks | Diffusion-Based Platforms | Droplet-Digital Platforms |
|---|---|---|---|
| Culture Duration | 24 hours to weeks | Typically hours to days | Minutes to hours (analysis) |
| Volume Scale | Microliter-range wells | Nanoliter to microliter channels | Picoliter droplets |
| Cell Types Supported | Adherent and suspension cells; 2D and 3D culture | Primarily adherent cells | Suspension cells and adherent cells after dissociation |
| Molecular Exchange | Diffusion between stacked layers | Diffusion across post arrays | Encapsulated secretion analysis |
| Compatible Readouts | Imaging, PCR, immunocytochemistry | Fluorescence imaging, reporter assays | Single-cell sequencing, functional assays |
Experimental Methodologies for Inflammatory Signaling
Protocol: Studying Tumor-Macrophage-Endothelial Cell Sequential Signaling Using Stacks
This protocol exemplifies how microfluidic platforms can model complex multi-step paracrine signaling relevant to inflammatory processes in the tumor microenvironment [44].
Step 1: Layer Preparation and Independent Conditioning
- Prepare separate Stacks layers for different cell types:
- Cancer cell layer: Culture prostate cancer cells in a 2D culture layer with appropriate medium.
- Macrophage differentiation layer: Seed THP-1 monocytic cells in a 2D culture layer and differentiate using 24-hour PMA treatment, followed by culture with IL-4 and IL-13 for polarization, then a 2-day resting period.
- Angiogenesis layer: Co-culture HUVEC and normal human dermal fibroblasts (1:4 ratio) in a fibronectin-coated well with communication pores for 3 days to form microvasculature.
Step 2: Sequential Stacking and Paracrine Exposure
- Stack the cancer cell layer and macrophage differentiation layer for 24-48 hours to allow cancer-derived factors to polarize macrophages.
- Separate these layers and stack the conditioned macrophage layer with the angiogenesis layer to study macrophage-derived pro-angiogenic signaling.
Step 3: Endpoint Analysis
- Disassemble stacks and analyze each layer independently:
- Macrophage polarization: Analyze gene expression profiles of pro-inflammatory (M1) and anti-inflammatory (M2) cytokines using qPCR.
- Angiogenic response: Quantify vascular morphology parameters (branching length, junction density) via fluorescence imaging.
Protocol: Single-Cell Autocrine Signaling Analysis Using Droplet-Digital Microfluidics
This protocol enables high-resolution analysis of autocrine signaling at the single-cell level, particularly valuable for detecting rare cytokine-secreting cells [47].
Step 1: Droplet Generation and Cell Encapsulation
- Generate water-in-oin emulsions using a flow-focusing droplet generator.
- Co-encapsulate single cells with fluorescently-labeled detection antibodies specific to target cytokines (e.g., TNF-α, IL-6).
Step 2: Incubation and Secretion Detection
- Incubate droplets at 37°C for 2-4 hours to allow cytokine secretion and accumulation.
- Monitor fluorescence intensity increase within droplets due to antibody-cytokine binding.
Step 3: Fluorescence-Activated Droplet Sorting
- Sort droplets based on fluorescence intensity thresholds using dielectrophoresis.
- Direct high-secreting, low-secreting, and non-secreting populations to different outlets.
Step 4: Cell Recovery and Downstream Analysis
- Merge sorted droplets with recovery buffer containing surfactant to break emulsions.
- Transfer individual cells to 96- or 384-well plates for clonal expansion or single-cell RNA sequencing.
- Achieve >90% cell viability and 18-fold higher recovery rates compared to standard methods.
Protocol: Multi-Population Paracrine Signaling in Diffusion-Based Platforms
This established methodology enables controlled study of paracrine signaling between adjacent cell populations [46].
Step 1: Device Design and Computational Modeling
- Design microfluidic channels (typically 100-500 µm wide) separated by post arrays with gaps of 5-15 µm to allow molecular diffusion while containing cells.
- Use COMSOL Multiphysics modeling to predict spatial and temporal distribution of signaling molecules based on channel geometry and diffusion coefficients.
Step 2: Sequential Cell Loading
- Introduce different cell populations into separate channels using precision pipetting or syringe pumps.
- Allow cells to adhere and stabilize (typically 4-24 hours) before establishing communication.
Step 3: Paracrine Signaling Activation
- Introduce specific stimuli to source population (e.g., LPS for macrophage activation).
- Monitor signal propagation to responding cell populations in adjacent channels via:
- Fluorescent reporter expression (e.g., GFP under cytokine-responsive promoter)
- Real-time imaging of calcium fluxes
- FRET-based cytokine sensors
Step 4: Quantitative Analysis
- Measure response kinetics and amplitude as a function of:
- Inter-channel distance
- Initial stimulus concentration
- Cell density in source and responder channels
Signaling Pathways and Experimental Workflows
Diagram 1: Inflammatory Paracrine Signaling Cascade in Tumor Microenvironment. This multi-step paracrine signaling cascade can be effectively modeled using reconfigurable microfluidic platforms like the Stacks system, enabling sequential analysis of each signaling step [44].
Diagram 2: Microfluidic Experimental Workflow for Signaling Studies. This generalized workflow highlights the key advantage of microfluidic platforms: the ability to independently condition cell populations before establishing controlled communication, which is essential for parsing autocrine versus paracrine effects [44] [46] [48].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for Microfluidic Signaling Studies
| Reagent/Material | Function | Example Applications | Technical Considerations |
|---|---|---|---|
| PDMS (Polydimethylsiloxane) | Device fabrication; Gas-permeable cell culture | Stacks system; Diffusion devices | Optical clarity; Biocompatibility; Small molecule absorption |
| PMMA (Poly-methyl methacrylate) | Thermoplastic for injection-molded devices | Commercial scale production | Chemical resistance; Mass production compatibility |
| ECM Hydrogels (Collagen, Matrigel) | 3D cell culture microenvironment | Angiogenesis assays; Stromal co-cultures | Matrix stiffness; Composition; Polymerization conditions |
| Fluorescent Reporters (GFP, RFP) | Real-time signaling monitoring | Reporter cell lines; Activity sensors | Photostability; Expression level; Spectral overlap |
| Cytokine Detection Antibodies | Secreted factor quantification | Bead-based immunoassays; On-chip detection | Cross-reactivity; Affinity; Detection limits |
| Surface Treatment Reagents (PLL, PEG) | Surface modification for cell adhesion or repellency | Patterned co-cultures; Selective adhesion | Stability; Biocompatibility; Coating uniformity |
| Fluorocarbon Oils & Surfactants | Droplet generation and stabilization | Single-cell encapsulation; Digital assays | Biocompatibility; Droplet stability; Permeability |
| Cell Line-Specific Culture Media | Maintain cell viability and function | Multi-population culture; Conditioned media | Formulation compatibility; Additive stability |
| Merbarone | Merbarone, CAS:97534-21-9, MF:C11H9N3O3S, MW:263.27 g/mol | Chemical Reagent | Bench Chemicals |
| 5-Aminosalicylic Acid | 5-Aminosalicylic Acid, CAS:89-57-6, MF:C7H7NO3, MW:153.14 g/mol | Chemical Reagent | Bench Chemicals |
Microfluidic platforms represent a transformative technological advancement for studying autocrine and paracrine signaling in inflammatory contexts. The architectures described in this whitepaper—including reconfigurable Stacks, diffusion-based platforms, droplet-digital systems, and active manipulation devices—provide researchers with unprecedented control over the spatial and temporal dimensions of cell signaling studies. These systems enable the deconvolution of complex sequential signaling events, single-cell autocrine profiling, and precise manipulation of microenvironmental conditions that dictate inflammatory responses. As these technologies continue to evolve through integration with advanced biosensors, multi-omic readouts, and AI-driven analysis, they promise to accelerate both fundamental understanding of inflammatory cytokine networks and the development of targeted therapeutic interventions for immune-related diseases.
Biofunctional Microcavity Arrays for Single-Cell Analysis
Biofunctional microcavity arrays represent a transformative technological platform for investigating cellular heterogeneity, particularly in the context of inflammatory signaling. These systems enable the precise spatial segregation and analysis of individual cells, providing unprecedented resolution for studying the complex dynamics of autocrine and paracrine signaling. Within the inflammatory cascade, cells communicate through cytokines that act either on themselves (autocrine) or on nearby cells (paracrine), processes that are often dysregulated in disease states [49]. The ability to monitor these signaling patterns at single-cell resolution is crucial for understanding fundamental immunological processes and developing targeted therapeutic interventions.
Traditional bulk analysis methods obscure cell-to-cell variations that are critical in immune responses, where small subpopulations can drive pathological outcomes. Microcavity arrays overcome this limitation by combining microscale confinement with integrated biosensing capabilities, allowing researchers to simultaneously track cytokine secretion profiles and cellular responses across hundreds to thousands of individual cells. This technical guide examines the implementation of biofunctional microcavity arrays specifically configured for investigating autocrine and paracrine signaling of inflammatory cytokines, with detailed methodologies and performance characteristics for researchers and drug development professionals.
Technical Foundations and Working Principles
Biofunctional microcavity arrays operate on the principle of physically isolating individual cells within microfabricated cavities while incorporating sensing modalities to detect secreted analytes. The fundamental architecture consists of a structured substrate containing an array of microwells or microchambers, each capable of confining single cells along with integrated detection elements.
Cellular Isolation and Signaling Analysis: The confinement of individual cells within microcavities creates defined microenvironments where secreted signaling molecules can accumulate to detectable concentrations. For autocrine signaling studies, this allows the measurement of self-stimulation pathways where cytokines bind receptors on the same cell that produced them. In paracrine signaling investigations, controlled cell patterning enables the analysis of communication between adjacent but physically separated cells of different types [49]. Advanced systems incorporate selective surface functionalization to capture specific cytokines proximal to secreting cells, providing spatial mapping of secretion patterns.
Detection Modalities: Multiple detection strategies have been implemented in microcavity platforms, including optical, electrical, and electrochemical sensing. Silicon photonic microring resonators represent a particularly sensitive label-free approach, detecting binding events through changes in refractive index near the sensor surface [50]. These resonant optical microcavities can be functionalized with antibodies specific to inflammatory cytokines such as IL-6, IL-8, IL-10, and TNF-α, enabling multiplexed monitoring of secretory profiles from individual cells [50]. The detection mechanism relies on the shift in resonance wavelength that occurs when target analytes bind to capture agents immobilized on the sensor surface, providing quantitative data on cytokine concentrations with picomolar sensitivity.
Electrical Manipulation Techniques: Microcavity arrays often incorporate dielectrophoresis (DEP) for precise single-cell manipulation. The DEP force exerted on cells in a non-uniform electric field depends on the cell's polarizability relative to the surrounding medium, described by the Clausius-Mossoti factor [51]. This enables controlled positioning of specific cell types within the array for investigating directed paracrine signaling events. Positive DEP (pDEP) moves cells toward regions of high electric field gradient, while negative DEP (nDEP) repels cells from these regions, allowing sophisticated spatial patterning of different cell populations [51].
Quantitative Performance Characteristics
Biofunctional microcavity arrays demonstrate robust performance metrics for single-cell analysis applications, particularly in the context of inflammatory cytokine detection. The following table summarizes key quantitative parameters for representative platforms:
Table 1: Performance Metrics of Biofunctional Microcavity Arrays for Cytokine Detection
| Parameter | Silicon Photonic Microring Resonators [50] | Microfluidic DEP Trapping [51] | Electrical Impedance Sensing [51] |
|---|---|---|---|
| Detection Limit | 8-20 ng/mL for cytokines (IL-8, TNF-α) | Single-cell capture | Single-cell resolution |
| Dynamic Range | 0-150 ng/mL for multiplexed protein detection | N/A | N/A |
| Trapping Efficiency | N/A | >90% with optimized parameters | N/A |
| Multiplexing Capacity | 5+ biomarkers simultaneously | N/A | N/A |
| Analysis Time | ~5 minutes post-calibration | Minutes for array loading | Real-time monitoring |
| Measurement Error | ~8 ng/mL average across biomarkers | N/A | N/A |
The sensitivity of these platforms is particularly suited to inflammatory cytokine monitoring, as plasma cytokine concentrations can rise from less than 100 pg/mL in healthy adults to over 1000 pg/mL during inflammatory responses [49]. This dynamic range comfortably falls within the detection capabilities of microcavity array systems.
Table 2: Inflammatory Cytokine Concentrations in Health and Disease States
| Cytokine | Healthy Levels (pg/mL) | Inflammatory Conditions (pg/mL) | Signaling Mode |
|---|---|---|---|
| IL-6 | Often undetectable [49] | Up to 1000 pg/mL post-surgery [49] | Autocrine/Paracrine |
| IL-8 | <100 pg/mL [49] | Elevated in sepsis, trauma [49] | Paracrine |
| TNF-α | <100 pg/mL [49] | Elevated in cytokine storm [31] | Paracrine |
| IL-10 | <100 pg/mL [49] | Elevated in CARS phase of sepsis [31] | Autocrine/Paracrine |
Experimental Protocols
Array Functionalization for Cytokine Capture
Materials:
- Silicon photonic microring resonator chip with 32+ sensors [50]
- 6-hydrazinonicotinamide (S-HyNic) for surface functionalization [50]
- Monoclonal mouse IgG antibodies specific to target cytokines (anti-IL-6, anti-IL-8, anti-TNF-α, etc.) modified with 4-formylbenzamide (4FB) moieties [50]
- PDMS microfluidic device with six channels [50]
- Phosphate-buffered saline (PBS) with 0.1 mg/mL bovine serum albumin (BSA-PBS) [50]
- Glycine buffer (pH 2.2) for surface regeneration [50]
Procedure:
- Mount the microcavity array chip and align the PDMS microfluidic device to create distinct flow channels over sensor groups.
- Functionalize the sensor surface with S-HyNic to enable covalent attachment of antibodies.
- Introduce antibody solutions through designated channels, immobilizing specific antibodies to distinct sensor regions (4 sensors per antibody type).
- Reserve one channel for isotype control antibodies to monitor non-specific binding.
- Validate functionalization by flowing control solutions containing 1 μg/mL of non-target proteins in BSA-PBS to confirm minimal cross-reactivity.
- Store functionalized arrays in PBS at 4°C until use (within 48 hours recommended).
Single-Cell Loading and Cytokine Secretion Profiling
Materials:
- Single-cell suspension of immune cells (e.g., monocytes, T-cells) at 1-5×10ⶠcells/mL
- Microcavity array with integrated dielectrophoresis electrodes [51]
- AC signal generator for DEP manipulation (1-10 MHz, 5-15 Vpp) [51]
- Cell culture medium appropriate for cell type
- Temperature-controlled stage (37°C, 5% CO₂)
Procedure:
- Introduce cell suspension into the microcavity array at controlled flow rates (0.5-2 μL/min).
- Apply AC electric field to activate DEP trapping mechanisms. For pDEP-based capture, use higher frequency fields (>5 MHz) to trap cells at electrode edges [51].
- Monitor trapping efficiency microscopically, optimizing voltage and flow rate to achieve >90% single-cell occupancy.
- Once cells are trapped, replace flow with fresh culture medium or specific stimulants (e.g., LPS for immune activation).
- Monitor cytokine secretion in real-time using the functionalized sensors, recording resonance wavelength shifts every 10-30 seconds.
- For temporal profiling, continue measurements for 2-24 hours depending on experimental objectives.
- Regenerate sensor surfaces between experiments using glycine buffer (pH 2.2) for 1-2 minutes [50].
Data Analysis and Quantification
Initial Slope Analysis Method:
- For sensors far from saturation (e.g., CEA, TNF-α), fit real-time response curves to linear functions.
- For sensors approaching equilibrium (e.g., IL-8, AFP), fit responses to exponential functions and calculate initial slopes from the first derivative at t=0 [50].
- Construct calibration curves for each sensor using initial slope data from standard solutions.
- Determine unknown concentrations by interpolating sample slopes against calibration curves.
- Apply drift correction using control sensor responses to account for bulk refractive index changes.
Signaling Pathways in Inflammatory Cytokine Research
The investigation of autocrine and paracrine signaling is fundamental to understanding inflammatory processes. Biofunctional microcavity arrays enable precise dissection of these signaling modes, which are often dysregulated in conditions such as sepsis, autoimmune diseases, and cancer.
Autocrine Signaling in Inflammation: Autocrine signaling occurs when a cell responds to its own secreted cytokines, creating self-amplifying loops that can drive sustained inflammatory responses. In the context of sepsis, monocytes and macrophages exhibit autocrine signaling through IL-1β and TNF-α, reinforcing their activated state and contributing to the initial hyperinflammatory phase [31]. Microcavity arrays capture these autocrine circuits by monitoring simultaneous cytokine secretion and downstream signaling events within individual cells, revealing heterogeneity in autocrine amplification across cell populations.
Paracrine Signaling in Inflammation: Paracrine signaling mediates communication between different cell types within inflammatory microenvironments. For example, endothelial cells responding to IL-6 secreted by nearby immune cells represents a classic paracrine interaction that increases vascular permeability during inflammation [49]. Microcavity arrays with patterned co-cultures enable controlled investigation of these directional signaling events, quantifying the spatial range and magnitude of paracrine effects.
Cytokine Storm Dynamics: The pathological transition from controlled inflammation to cytokine storm involves a breakdown in the regulatory balance between autocrine and paracrine signaling, leading to excessive production of proinflammatory cytokines including IL-6, IL-8, and TNF-α [49] [31]. Microcavity arrays provide unique insights into the cellular origins and propagation patterns of cytokine storms by tracking which cell subpopulations initiate the cascade and how the signaling spreads through autocrine and paracrine mechanisms.
Diagram 1: Autocrine and Paracrine Signaling Pathways
Integrated Experimental Workflow
A comprehensive approach to studying inflammatory signaling using biofunctional microcavity arrays involves multiple integrated steps from device preparation to data analysis. The following workflow diagram illustrates the complete experimental pipeline:
Diagram 2: Integrated Experimental Workflow
Research Reagent Solutions
Successful implementation of biofunctional microcavity array experiments requires specific reagents and materials optimized for single-cell analysis. The following table details essential research reagents and their functions:
Table 3: Essential Research Reagents for Microcavity Array Experiments
| Reagent/Material | Function | Specifications | Application Notes |
|---|---|---|---|
| Silicon Photonic Chips | Optical detection platform | 32+ microring resonators [50] | Reusable after regeneration |
| Cytokine-Specific Antibodies | Target capture agents | Monoclonal, 4FB-modified [50] | Multiplexing requires distinct epitopes |
| S-HyNic Crosslinker | Surface functionalization | 6-hydrazinonicotinamide [50] | Enables covalent attachment |
| DEP Buffer | Cell manipulation medium | Low conductivity, isotonic [51] | Optimized Clausius-Mossoti factor |
| Glycine Regeneration Buffer | Surface regeneration | pH 2.2 [50] | Removes bound analytes |
| Microfluidic Components | Fluid delivery system | PDMS, 6-channel design [50] | Enables parallel processing |
Technological Integration and Future Perspectives
The convergence of biofunctional microcavity arrays with advanced single-cell analysis techniques represents a powerful paradigm for inflammatory cytokine research. Emerging directions include the integration of multi-omics approaches, where cytokine secretion data is correlated with transcriptional and proteomic profiles from the same individual cells. Additionally, the incorporation of advanced biosensing modalities such as graphene energy transfer (GET) systems promises to enhance spatial resolution to the Ångström scale for studying molecular interactions [52].
Future developments will likely focus on increasing multiplexing capabilities to simultaneously monitor larger panels of inflammatory mediators, thereby capturing the complexity of cytokine networks rather than individual signals. The integration of long-term culture capabilities will enable the investigation of how autocrine and paracrine signaling evolves during chronic inflammation and resolution phases. As these platforms become more accessible, they will undoubtedly accelerate both fundamental understanding of inflammatory processes and the development of targeted immunomodulatory therapies.
Optogenetic Modulation of Calcium Signaling in Non-Neuronal Cells
Calcium ions (Ca²âº) function as ubiquitous intracellular messengers, governing diverse cellular processes including proliferation, migration, secretion, and gene expression. In non-neuronal cells, Ca²⺠signaling exerts particularly profound effects on immune responses and inflammatory pathways through the regulation of cytokine release and cellular differentiation. The emergence of optogenetics has revolutionized our ability to dissect these complex signaling networks with unprecedented spatial and temporal precision. By leveraging light-sensitive proteins, researchers can now manipulate specific Ca²⺠signaling pathways in targeted cell populations, enabling causal relationships to be established between Ca²⺠dynamics and functional outcomes such as autocrine and paracrine signaling of inflammatory mediators.
This technical guide provides a comprehensive framework for implementing optogenetic approaches to modulate Ca²⺠signaling in non-neuronal cells, with particular emphasis on applications within inflammatory cytokine research. We detail the molecular tools, experimental methodologies, and analytical techniques required to investigate how Ca²⺠influx regulates the secretion of cytokines and other signaling molecules that coordinate intercellular communication in physiological and pathological contexts. The integration of optogenetics with advanced imaging and molecular biology techniques now enables researchers to move beyond correlation to establish causation in complex inflammatory signaling networks, providing new insights for therapeutic intervention in inflammatory diseases.
Optogenetic Tools for Calcium Modulation
Core Optogenetic Actuators
The selection of appropriate optogenetic actuators is fundamental to experimental design. These tools can be categorized based on their ion selectivity, spectral properties, and operational mechanisms. The most widely utilized optogenetic tools for Ca²⺠modulation are channelrhodopsins engineered for enhanced calcium permeability.
CapChR2 (Calcium-permeable Channelrhodopsin-2) represents a breakthrough optogenetic tool for Ca²⺠manipulation. This engineered channelrhodopsin variant demonstrates significantly improved Ca²⺠permeability compared to wild-type Channelrhodopsin-2 while maintaining rapid kinetics and light sensitivity [53] [54]. CapChR2 is activated by blue light (∼470 nm) and enables precise temporal control of Ca²⺠influx without engaging endogenous signaling pathways that might confound interpretation. In Schwann cells, optogenetic activation of CapChR2 has been shown to trigger Ca²âº-dependent release of neurotrophic factors, demonstrating its utility for studying secretome regulation [53]. The tool is particularly valuable for investigating Ca²âº-triggered secretomes and their effects on neighboring cells through paracrine signaling mechanisms.
For experiments requiring simultaneous optogenetic stimulation and calcium imaging, red-shifted channelrhodopsins such as Chrimson or ReaChR offer distinct advantages. These actuators are activated by longer wavelength light (590-650 nm), which minimizes spectral overlap with commonly used green calcium indicators (e.g., GCaMP) and reduces phototoxicity [55]. This spectral separation enables all-optical experiments where Ca²⺠dynamics can be monitored while simultaneously manipulating cellular activity. The development of these tools has been particularly impactful for studying inflammatory cytokine networks where feedback loops and complex cellular interactions necessitate precise perturbation and observation.
Advanced and Specialized Optogenetic Tools
Beyond core channelrhodopsins, several specialized optogenetic tools expand experimental possibilities for Ca²⺠research:
PhoCl (Photo-cleavable protein) is a recently developed optogenetic tool that undergoes irreversible cleavage upon violet light (405 nm) activation [56]. While not directly a Ca²⺠channel, PhoCl can be incorporated into engineered systems to control protein localization and function, including Ca²⺠signaling components. Its nuclear localization variant enables single-cell manipulation in vivo with minimal background interference, making it valuable for studies of cell-autonomous inflammatory responses [56].
Pisces (Photo-inducible single-cell labeling system) represents a sophisticated tool that combines the photo-cleavage capability of PhoCl with a photoconvertible fluorescent protein (mMaple) and balanced nuclear localization/export signals [56]. This system enables complete morphological tracing of individual cells following activation, which can be correlated with Ca²⺠signaling dynamics and cytokine secretion profiles. For inflammatory research, this permits direct investigation of how cellular morphology influences secretory capacity and intercellular communication range.
Table 1: Optogenetic Tools for Calcium Manipulation in Non-Neuronal Cells
| Tool Name | Activation Wavelength | Key Features | Primary Applications | Considerations |
|---|---|---|---|---|
| CapChR2 | ~470 nm blue light | High Ca²⺠permeability, rapid kinetics | Ca²⺠influx studies, secretome release, autocrine/paracrine signaling | Endogenous Opsin expression may cause background |
| Red-shifted Opsins (Chrimson, ReaChR) | 590-650 nm red light | Minimal spectral overlap with GCaMP indicators | All-optical stimulation and imaging, deep tissue applications | Lower Ca²⺠permeability than CapChR2 |
| PhoCl | 405 nm violet light | Irreversible cleavage, nuclear localization | Protein translocation studies, pathway dissection | Permanent activation, not reversible |
| Pisces | 405 nm violet light | Combines PhoCl with mMaple, full morphology labeling | Correlating structure-function in secretory cells | Complex construct design and validation |
Experimental Design and Implementation
Integrated Optical Systems for Simultaneous Stimulation and Imaging
The investigation of Ca²âº-mediated inflammatory signaling requires specialized instrumentation that enables simultaneous optogenetic manipulation and quantitative readouts. Integrated microscope systems have been developed that incorporate multiple light sources for independent control of optogenetic actuators and calcium indicators [55]. These systems typically feature two independently controlled LED modules: a blue LED (435-460 nm) for exciting green calcium indicators (e.g., GCaMP), and a red LED (590-650 nm) for activating red-shifted opsins [55].
A critical consideration in system design is minimizing crosstalk between stimulation and imaging pathways. Optical filters must be carefully selected to prevent optogenetic activation light from contaminating the calcium imaging channel, and vice versa. Although some residual crosstalk may occur, proper filter selection and temporal separation of stimulation and imaging sequences can mitigate these effects [55]. Additionally, thermal management is essential during prolonged experiments, as high-intensity LED illumination can generate sufficient heat to affect cellular physiology. Modern systems incorporate heat sinks and temperature monitoring to maintain stable experimental conditions [55].
For studies investigating inflammatory cytokine dynamics in complex tissues, gradient-index (GRIN) lenses enable optical access to deep structures while maintaining cellular resolution. When coupled with miniaturized integrated microscopes, these systems allow for Ca²⺠imaging and optogenetic manipulation in freely behaving models, providing insights into how inflammatory states affect physiological processes [55].
Protocol: Simultaneous Optogenetic Stimulation and Calcium Imaging
This protocol details the methodology for investigating Ca²âº-dependent inflammatory signaling in non-neuronal cells using integrated optogenetic and imaging approaches.
Step 1: Cell Preparation and Optogenetic Tool Expression
- Culture target non-neuronal cells (e.g., immune cells, epithelial cells, or glial cells) on appropriate imaging-compatible substrates.
- Deliver optogenetic construct (e.g., CapChR2) using lentiviral or adenoviral transduction, ensuring appropriate promoter selection for cell-type specific expression.
- Include a calcium indicator (e.g., GCaMP6f for rapid kinetics or GCaMP8f for enhanced sensitivity) either co-expressed with the opsin or introduced as a separate construct.
- Allow 48-72 hours for sufficient transgene expression before imaging.
Step 2: System Configuration and Calibration
- Configure integrated microscope system with appropriate excitation filters (435-460 nm for calcium imaging, 590-650 nm for optogenetic stimulation).
- Set imaging parameters: 30 Hz frame rate typically provides sufficient temporal resolution for Ca²⺠dynamics.
- Calibrate optogenetic LED intensity using a power meter; typical irradiance ranges from 1-10 mW/mm² depending on opsin expression level.
- Establish stimulation paradigm: light pulses of 100-1000 ms duration effectively trigger Ca²⺠influx without excessive photodamage.
Step 3: Experimental Execution and Data Acquisition
- Perform baseline calcium imaging for 1-2 minutes to establish pre-stimulation Ca²⺠levels.
- Deliver optogenetic stimulation pulses according to experimental design while continuing calcium imaging.
- Include control groups expressing calcium indicator but not opsin to account for potential photodynamic effects.
- For inflammatory signaling studies, collect supernatant at specified timepoints post-stimulation for cytokine analysis via ELISA or multiplex assays.
Step 4: Data Analysis and Interpretation
- Extract calcium transients from regions of interest corresponding to individual cells.
- Quantify response parameters: amplitude, rise time, decay kinetics, and area under the curve.
- Correlate Ca²⺠dynamics with subsequent cytokine secretion profiles to establish functional relationships.
- Employ statistical analyses to determine significance across experimental conditions.
Figure 1: Experimental workflow for optogenetic modulation of calcium signaling with cytokine analysis.
Calcium Signaling in Inflammatory Contexts
The Calci-Inflammatory Network
The concept of a "Calci-Inflammatory Network" provides a framework for understanding the bidirectional relationship between Ca²⺠signaling and inflammatory processes [57]. In this paradigm, Ca²⺠operates as both a regulator and effector of inflammatory pathways, creating feedback loops that can either resolve or amplify inflammatory responses. In immune cells and tissue-resident cells, Ca²⺠influx triggers the activation of transcription factors such as NFAT and NF-κB, which subsequently drive the expression of pro-inflammatory cytokines including IL-1β, IL-6, and TNF-α [58] [59].
The calcium-sensing receptor (CaSR) plays a pivotal role in this network by translating extracellular Ca²⺠fluctuations into intracellular inflammatory responses. Activation of CaSR on immune cells can modulate cytokine production and cellular differentiation, thereby shaping the overall inflammatory milieu [57]. Interestingly, emerging evidence suggests that hypocalcemia may represent an adaptive response to limit excessive inflammation by reducing CaSR activation and subsequent cytokine production [57]. This perspective reframes calcium dysregulation not merely as a pathological consequence but as a potential modulatory mechanism within inflammatory circuits.
Optogenetic approaches are uniquely positioned to dissect this complex network by enabling precise manipulation of specific Ca²⺠signaling nodes without concurrently affecting other inflammatory parameters. For instance, selective activation of Ca²⺠influx in macrophages via CapChR2 allows researchers to determine the sufficiency of Ca²⺠signals for driving specific cytokine production profiles, independently of pattern recognition receptor activation.
Cytokine Signaling and Calcium Interdependence
Inflammatory cytokines both regulate and are regulated by Ca²⺠signaling, creating intricate feedback loops that optogenetic tools can help disentangle. Pro-inflammatory cytokines such as IL-1β and IL-6 can enhance the expression of Ca²âº-permeable channels, including transient receptor potential (TRP) channels and store-operated Ca²⺠entry (SOCE) components, thereby sensitizing cells to subsequent Ca²⺠signals [60] [59]. This positive feedback loop may contribute to the hyperinflammatory state characteristic of cytokine storm conditions.
The JAK/STAT pathway, activated by multiple cytokines including IL-6, interfaces with Ca²⺠signaling through several mechanisms. STAT transcription factors can regulate the expression of Ca²⺠channels and pumps, while Ca²âº-dependent enzymes such as calmodulin kinase II (CaMKII) can phosphorylate JAK/STAT components to modulate their activity [59]. This molecular crosstalk enables integration of inflammatory signals with Ca²⺠dynamics to fine-tune cellular responses. In the context of cytokine release syndrome (CRS), excessive activation of this interconnected network leads to pathological Ca²⺠dysregulation and organ dysfunction [59].
Table 2: Key Inflammatory Cytokines and Their Relationship with Calcium Signaling
| Cytokine | Primary Sources | Calcium Signaling Effects | Therapeutic Targeting |
|---|---|---|---|
| IL-1β | Macrophages, monocytes | Activates NLRP3 inflammasome, enhances SOCE | Anakinra (IL-1 receptor antagonist) |
| IL-6 | Macrophages, T cells, endothelial cells | Modulates TRP channel expression, regulates CaSR sensitivity | Tocilizumab (IL-6 receptor antibody) |
| TNF-α | Macrophages, mast cells, T cells | Potentiates store-operated calcium entry, activates NF-κB | Infliximab (TNF antibody) |
| IFN-γ | T cells, NK cells | Upregulates STIM/Orai expression, enhances SOCE | Emapalumab (IFN-γ antibody) |
| IL-17 | Th17 cells, γδ T cells | Increases expression of TRPV channels | Secukinumab (IL-17A antibody) |
Data Analysis and Interpretation
Quantifying Calcium Dynamics and Cytokine Output
Robust quantification of Ca²⺠dynamics is essential for correlating optogenetic stimulation with functional inflammatory outputs. Calcium imaging data should be analyzed to extract key parameters that characterize the spatiotemporal pattern of Ca²⺠signals:
Amplitude reflects the magnitude of Ca²⺠elevation and may correlate with the intensity of downstream responses such as vesicle fusion and cytokine release. Rise time indicates how rapidly Ca²⺠increases following optogenetic stimulation, which may influence the selective activation of downstream effectors with varying Ca²⺠affinity. Decay kinetics represent Ca²⺠clearance mechanisms and can affect the frequency response of Ca²âº-dependent processes. Oscillation frequency, when present, can encode information that selectively activates specific transcriptional programs.
For comprehensive analysis, these parameters should be correlated with cytokine secretion profiles quantified from supernatant samples. Multiplex immunoassays (e.g., Luminex) enable simultaneous measurement of multiple inflammatory mediators, providing a holistic view of the secretory response to optogenetically induced Ca²⺠signals. Advanced computational approaches, including machine learning algorithms, can identify patterns in high-dimensional datasets to predict inflammatory outputs based on Ca²⺠dynamics.
Table 3: Quantitative Parameters of Calcium Dynamics and Their Biological Significance
| Parameter | Measurement Method | Biological Interpretation | Relationship to Cytokine Secretion |
|---|---|---|---|
| Amplitude (ΔF/F0) | Fluorescence intensity change | Strength of calcium signal | Correlates with quantity of immediate release |
| Rise time (tau) | Exponential fit of rising phase | Speed of calcium influx | Faster rise may promote rapid secretion |
| Decay constant (tau) | Exponential fit of decay phase | Calcium clearance efficiency | Slower decay may sustain transcription |
| Area under curve | Integral of ΔF/F0 over time | Total calcium load | Predicts sustained secretory responses |
| Oscillation frequency | Peak detection algorithm | Encoded information | May selectively activate specific genes |
Modeling Calcium-Dependent Inflammatory Signaling
Computational modeling provides a powerful approach for interpreting experimental data and generating testable hypotheses about the Calci-Inflammatory Network. Mathematical models can integrate experimental measurements of Ca²⺠dynamics with known biochemical pathways to predict inflammatory outcomes. A minimal model might incorporate:
Ca²⺠influx through optogenetically activated channels, buffering and extrusion mechanisms that shape Ca²⺠signals, Ca²âº-dependent activation of kinases and phosphatases, transcription factor activation and nuclear translocation, and cytokine gene expression and protein secretion.
Parameterizing such models with experimental data enables in silico prediction of how manipulating specific nodes (e.g., inhibiting a particular Ca²⺠channel or kinase) might affect the overall inflammatory response. These models can also help identify critical control points in the network that might represent therapeutic targets for modulating pathological inflammation without completely suppressing protective immune function.
Figure 2: Core signaling pathway from optogenetic stimulation to cytokine secretion.
The Scientist's Toolkit
Essential Research Reagent Solutions
Successful implementation of optogenetic Ca²⺠modulation requires carefully selected reagents and tools. The following table comprehensively details essential materials and their applications in experimental workflows:
Table 4: Essential Research Reagents for Optogenetic Calcium Studies
| Reagent Category | Specific Examples | Function/Application | Key Considerations |
|---|---|---|---|
| Optogenetic Actuators | CapChR2, Chrimson, ReaChR | Mediates light-controlled calcium influx | Select based on calcium permeability, kinetics, and excitation spectrum |
| Calcium Indicators | GCaMP6/7/8 series, R-GECO | Reports intracellular calcium dynamics | Match kinetics to biological process; consider spectral overlap with actuator |
| Expression Systems | Lentivirus, AAV, stable cell lines | Delivers genetic constructs to target cells | Optimize for cell type-specific expression and appropriate expression levels |
| Cytokine Detection | ELISA, Luminex, Western blot | Quantifies inflammatory outputs | Sensitivity and multiplexing capacity should match experimental needs |
| Cell Type-Specific Markers | CD antibodies, GFP reporters | Identifies and isolates specific cell populations | Essential for heterogeneous cultures or tissue samples |
| Pathway Inhibitors | BAPTA-AM, 2-APB, KN-93 | Perturbs specific signaling nodes | Use to establish necessity of specific pathways |
| Optogenetic Control Tools | DREADDs, chemogenetic receptors | Provides non-optical control conditions | Important for distinguishing light effects from calcium effects |
| Mesendogen | Mesendogen|TRPM6 Inhibitor|Stem Cell Differentiation | Bench Chemicals | |
| Metacavir | Metacavir, CAS:120503-45-9, MF:C11H15N5O3, MW:265.27 g/mol | Chemical Reagent | Bench Chemicals |
Optogenetic modulation of Ca²⺠signaling represents a transformative approach for investigating inflammatory cytokine networks in non-neuronal cells. The precision and temporal control afforded by these techniques enable researchers to move beyond correlative observations to establish causal relationships between specific Ca²⺠signaling patterns and functional inflammatory outputs. As optogenetic tools continue to evolve with improved specificity, sensitivity, and minimal invasiveness, their application to the study of autocrine and paracrine signaling in inflammation will undoubtedly yield novel insights into disease mechanisms and potential therapeutic interventions.
The integration of optogenetics with complementary approaches—including advanced imaging, omics technologies, and computational modeling—promises to unravel the extraordinary complexity of the Calci-Inflammatory Network. By systematically dissecting how Ca²⺠signals are decoded into inflammatory responses, researchers can identify critical nodes for therapeutic intervention in conditions characterized by dysregulated inflammation, from autoimmune disorders to cytokine release syndromes. The experimental frameworks and methodologies detailed in this technical guide provide a foundation for exploiting these powerful approaches to advance both basic science and translational applications in inflammatory disease research.
High-Throughput Cytokine Profiling and Secretome Analysis
Cytokines are signaling proteins that act as crucial chemical messengers within the immune system, controlling inflammation and coordinating immune responses [2]. These proteins facilitate complex cell-to-cell communication through autocrine signaling (binding to receptors on the same cell), paracrine signaling (affecting nearby cells), and endocrine signaling (influencing distant cells) [2]. The complete set of secreted proteins released by cells—the secretome—provides a dynamic snapshot of cellular communication, offering valuable insights for both basic research and drug development [61] [62]. In inflammatory processes, the balance between pro-inflammatory cytokines (which initiate or heighten inflammation) and anti-inflammatory cytokines (which reduce inflammation) determines immunological outcomes, with dysregulation leading to autoimmune diseases, metabolic disorders, and cancer [2].
High-throughput cytokine profiling enables researchers to systematically quantify these secreted proteins across thousands of samples, revealing how inflammatory signals propagate through autocrine and paracrine mechanisms. This technical guide explores cutting-edge platforms, detailed methodologies, and analytical frameworks for comprehensive secretome analysis, with particular emphasis on their application to inflammatory cytokine research.
High-Throughput Profiling Technologies
Technology Platforms and Principles
Advanced technologies have transformed our capacity to quantify cytokines across extensive sample sets. The core challenge in multiplexed immunoassays—reagent-driven cross-reactivity (rCR)—occurs when noncognate antibodies mixed in solution form mismatched sandwich complexes, increasing background noise and reducing sensitivity exponentially with more antibody pairs [63]. The following table compares major high-plex protein measurement technologies:
Table 1: Comparison of High-Throughput Protein Profiling Technologies
| Technology | Multiplexing Capacity | Sensitivity | Key Mechanism | Advantages | Limitations |
|---|---|---|---|---|---|
| nELISA [63] | 191-plex (demonstrated) | Sub-pg/mL across 7 orders of magnitude | DNA-mediated sandwich immunoassay with bead barcoding | Minimal rCR, cost-efficient, high-throughput | Requires specialized detection system |
| Mass Cytometry (CyTOF) [64] | 42+ parameters simultaneously | High (single-cell level) | Metal isotope-tagged antibodies with mass spectrometry detection | Minimal channel overlap, no compensation needed | Low throughput compared to flow cytometry, complex data analysis |
| Proximity Extension Assay (PEA) [63] | Thousands of proteins per assay | High | Proximity-dependent DNA amplification and sequencing | High specificity and sensitivity | Costly, lower throughput, less flexible for customization |
| Aptamer-based (SomaScan) [63] | Thousands of proteins per assay | High | Aptamer-based capture with DNA microarray detection | High multiplexing capability | Multiple capture-release steps, not ideal for post-translational modifications |
Next-Generation nELISA Platform
The nELISA platform represents a significant advancement by addressing fundamental limitations of conventional immunoassays. Its core innovation, CLAMP (Colocalized-by-Linkage Assays on Microparticles), incorporates three key features [63]:
- Preassembled antibody pairs spatially confined to individual beads prevent noncognate interactions
- Releasable detection antibodies tethered via flexible single-stranded DNA enable efficient ternary sandwich formation
- Conditional signal generation through toehold-mediated strand displacement, where fluorescently labeled DNA oligos simultaneously untether and label detection antibodies
When combined with emFRET bead barcoding—which uses varying ratios of four fluorophores to generate thousands of spectral signatures—nELISA achieves high-throughput, high-plex capability without rCR [63]. This platform has demonstrated practical utility in profiling 7,392 peripheral blood mononuclear cell samples, generating approximately 1.4 million protein measurements and revealing over 440 robust cytokine responses in under one week [63].
Experimental Design and Protocols
Sample Preparation and Secretome Collection
Standardized protocols for secretome production are critical for reproducible results. Key considerations include [61]:
- Cell Culture Conditions: Maintain consistent cell density, media composition, and incubation parameters to minimize variability in cytokine secretion profiles.
- Stimulation Agents: Use appropriate immune stimuli such as concanavalin A (T-cell stimulus), lipopolysaccharide (TLR4 agonist), or CpG DNA (TLR9 agonist) to elicit cytokine responses relevant to your research questions [63] [3].
- Collection Timing: Temporal dynamics significantly impact cytokine measurements; some cytokines appear within hours while others require longer stimulation periods.
- Protein Transport Inhibitors: For intracellular cytokine staining, add brefeldin A and monensin during the final 4 hours of stimulation to retain cytokines within cells [64].
Table 2: Essential Research Reagents for Cytokine Profiling
| Reagent Category | Specific Examples | Function & Application |
|---|---|---|
| Immune Cell Stimuli | Concanavalin A, LPS, CpG DNA, PMA + Ionomycin | Activate specific immune signaling pathways (TLR, NF-κB) to elicit cytokine responses [63] [3] |
| Protein Transport Inhibitors | Brefeldin A, Monensin | Block cytokine secretion for intracellular cytokine staining and detection [64] |
| Detection Antibodies | Metal-conjugated antibodies (CyTOF), DNA-tethered antibodies (nELISA) | Enable target protein detection through various readout systems [63] [64] |
| Cell Surface Markers | CD3, CD14, CD19, CD4, CD8, CD56, CD16 | Identify and characterize specific immune cell populations during analysis [64] |
| Cytokine/Chemokine Panels | 191-plex inflammation panel (nELISA), custom NK cell panels (CyTOF) | Simultaneously measure multiple inflammatory mediators [63] [64] |
High-Throughput Intracellular Cytokine Staining Protocol for Mass Cytometry
The following protocol adapts established methodology for functional analysis of immune cells [64]:
Cell Stimulation:
- Resuspend cells at 1-2×10^6 cells/mL in complete medium.
- Add stimulation cocktail (PMA + ionomycin, cytokine mixture, or pathogen-infected cells).
- Add anti-CD107a antibodies to measure degranulation.
- Incubate for 12-16 hours at 37°C, 5% CO₂.
Inhibition of Protein Transport:
- Add brefeldin A (1:1000) and monensin (1:1500) for the final 4 hours of stimulation.
Cell Staining:
- Transfer cells to metal-free tubes and wash with CyFACS buffer.
- Stain with viability marker (e.g., cisplatin) for 5 minutes.
- Wash with CyFACS buffer, then incubate with surface antibody panel for 30 minutes at room temperature.
- Wash cells, then fix and permeabilize using FoxP3/Transcription Factor Staining Buffer Set.
- Stain with intracellular antibody panel for 30-60 minutes at room temperature.
Sample Acquisition:
- Wash cells with CyFACS buffer, then resuspend in water with EQ Four Element Calibration Beads.
- Acquire data on mass cytometer, collecting 100,000+ events per sample.
Figure 1: Intracellular Cytokine Staining Workflow for Mass Cytometry
nELISA Protocol for Secreted Cytokine Detection
The nELISA platform uses a different approach optimized for secreted protein measurement [63]:
CLAMP Bead Preparation:
- Preassemble target-specific antibody pairs on barcoded beads.
- Hybridize detection antibodies via flexible single-stranded DNA tethers.
Sample Incubation:
- Pool assembled CLAMPs and dispense into 384-well plates.
- Add samples and incubate to allow ternary sandwich complex formation.
Detection by Strand Displacement:
- Add fluorescently tagged displacer-oligo to simultaneously release and label detection antibodies.
- Wash away unbound probes to minimize background signal.
Flow Cytometric Analysis:
- Analyze beads using flow cytometry with emFRET decoding.
- Process data to quantify cytokine concentrations based on fluorescent signals.
Signaling Pathways in Inflammatory Cytokine Production
TNF Production and NF-κB Signaling
Tumor necrosis factor (TNF) serves as a cornerstone inflammatory cytokine with complex regulation and signaling capabilities. Research reveals that TNF exhibits stimulus-specific functions, acting primarily through paracrine signaling in response to lipopolysaccharide (LPS) but demonstrating autocrine amplification in response to CpG DNA [3]. This specificity is determined by the underlying signaling network dynamics of TNF production and NF-κB response.
Macrophages exposed to pathogens initiate TNF production through Toll-like receptors (TLRs) that engage adaptor proteins MyD88 and TRIF, leading to activation of transcription factors NF-κB and IRF3 [3]. TNF production is regulated through multiple mechanisms:
- Transcriptional Control: MyD88-dependent signaling primarily drives early TNF mRNA synthesis through NF-κB activation [3].
- Post-transcriptional Regulation: TRIF-dependent signaling extends TNF mRNA half-life by inactivating mRNA destabilizing proteins [3].
- Translational and Post-translational Control: Both MyD88 and TRIF contribute to translational efficiency and protein processing through regulation of eIF4E and TACE enzyme activity [3].
Figure 2: TNF Production and Signaling Pathways
Autocrine and Paracrine Signaling Networks
The physical interaction network between immune cells creates a complex wiring diagram that coordinates inflammatory responses. Systematic mapping of surface protein interactions reveals that immune cells dynamically adjust their connectivity based on activation status [65]. In resting states, immune cells favor transient interactions, while inflamed conditions promote higher-affinity connections—an "affinity switch" that may support more dynamic threat responses [65].
Myeloid-lineage cells frequently serve as interaction hubs across tissues, adapting their receptor repertoire to integrate local immune communications [65]. This network perspective explains how autocrine and paracrine signaling are spatially and temporally coordinated, with implications for both physiological inflammation and pathological states like autoimmunity and cancer.
Data Analysis and Bioinformatics
Computational Tools for Secretome Analysis
Bioinformatics platforms are essential for interpreting complex secretome datasets. Specialized tools include:
- AUDACY (AUtomated Data Analysis of CYtokines): Processes secretomic data to identify key proteins and map biological pathways, offering human-specific data extraction for clinical relevance [66].
- FindYourPath: Performs differential gene expression and pathway analysis on transcriptomic data, generating customizable graphical outputs to visualize immune pathways and cellular communication [66].
- Integrated Atlases: Web-accessible platforms that contextualize receptor-ligand pairs across single-cell expression datasets from multiple tissues, helping researchers identify potential functional contexts for interactions [65].
These tools enable researchers to move from raw data to biological insights by identifying differentially expressed cytokines, mapping enriched pathways, and constructing interaction networks that reveal how cellular communication is rewired in different physiological states.
Data Normalization and Statistical Considerations
Robust secretome analysis requires careful statistical design:
- Multiplate Normalization: Include reference standards and controls across plates to correct for technical variability in large-scale studies.
- Batch Effect Correction: Account for run-to-run variability using removeUnwantedVariation or similar algorithms.
- False Discovery Control: Apply multiple testing corrections (e.g., Benjamini-Hochberg) when conducting numerous statistical comparisons.
- Pathway Enrichment Analysis: Use overrepresentation analysis or gene set enrichment methods to identify biologically meaningful patterns beyond individual cytokine changes.
Applications in Research and Drug Development
High-throughput cytokine profiling enables diverse applications in basic research and pharmaceutical development:
- Compound Screening: nELISA integration with Cell Painting allows phenotypic screening of reference compounds, simultaneously capturing cytokine responses and morphological changes [63].
- Biomarker Discovery: Secretome analysis identifies diagnostic, prognostic, and predictive biomarkers for autoimmune diseases, cancer, and metabolic disorders [2] [62].
- Mechanism of Action Studies: Cytokine profiling reveals how therapeutic interventions modulate immune pathways, supporting target validation and lead optimization.
- Toxicity Assessment: Comprehensive cytokine measurement detects potential immunotoxicity earlier in drug development pipelines.
These applications demonstrate how high-throughput cytokine profiling bridges basic research on autocrine/paracrine signaling and therapeutic development, offering insights into both disease mechanisms and intervention strategies.
High-throughput cytokine profiling and secretome analysis provide powerful frameworks for investigating inflammatory signaling in physiological and pathological contexts. The integration of advanced technological platforms like nELISA and mass cytometry with sophisticated bioinformatics tools enables researchers to decode the complex language of intercellular communication. As these methodologies continue to evolve, they will further illuminate the intricate networks of autocrine and paracrine signaling that coordinate immune responses, offering new opportunities for understanding and therapeutic intervention in inflammatory diseases.
Genetic manipulation technologies are foundational tools for dissecting the complex roles of inflammatory cytokines in autocrine and paracrine signaling. These signaling mechanisms, where cells release cytokines that act upon themselves (autocrine) or on nearby cells (paracrine), are critical in maintaining immune homeostasis and driving inflammatory pathologies [29]. Precise genetic interventions enable researchers to systematically unravel the contributions of specific genes to these processes. The evolution from traditional knockout models to advanced CRISPR-based technologies represents a paradigm shift in our ability to conduct functional genomics research with unprecedented precision and scalability [67] [68].
This technical guide provides an in-depth comparison of established and emerging genetic manipulation strategies, with particular emphasis on their application in inflammatory cytokine research. We detail methodologies for implementing zinc finger nucleases (ZFNs), transcription activator-like effector nucleases (TALENs), CRISPR-Cas9 knockout systems, and CRISPR interference (CRISPRi) technologies, focusing on experimental design considerations for studying IL-6, TNF-α, and other clinically relevant cytokines within autocrine and paracrine signaling contexts [29] [69].
Traditional Gene Knockout Methods
Historical Context and Mechanistic Principles
Traditional gene knockout methods rely on protein-based DNA recognition domains fused to non-specific nuclease domains. Zinc Finger Nucleases (ZFNs) utilize engineered zinc finger proteins, where each finger recognizes approximately 3 base pairs of DNA; multiple fingers are assembled to create a specific DNA-binding array fused to the FokI nuclease domain [67]. The FokI nuclease must dimerize to become active, requiring two ZFN subunits to bind opposite DNA strands with precise orientation and spacing (typically 5-7 bp apart) to create a double-strand break (DSB) [67].
Transcription Activator-Like Effector Nucleases (TALENs) employ TALE proteins derived from Xanthomonas bacteria, where each TALE repeat recognizes a single DNA base pair through highly variable repeat region di-residues. Like ZFNs, TALENs use the FokI nuclease domain that requires dimerization for activity [67]. The primary advantage of TALENs over ZFNs lies in their more straightforward design principles: a direct one-repeat-to-one-base-pair correspondence eliminates context-dependent effects that complicate zinc finger array design.
Applications in Cytokine Signaling Research
Traditional knockouts have been instrumental in establishing foundational knowledge of cytokine signaling pathways. ZFNs have demonstrated high specificity in creating stable cell lines with targeted disruptions in cytokine receptors, effectively dissecting autocrine signaling loops [67]. TALENs have been successfully employed to generate knockouts in primary immune cells, enabling functional validation of paracrine signaling mechanisms in physiologically relevant models [67]. These approaches remain valuable for applications requiring highly validated, specific edits with minimal off-target effects, particularly when investigating critical cytokines like IL-6 and TNF-α whose dysregulation has profound pathological consequences [29].
Table 1: Comparison of Traditional Gene Knockout Platforms
| Feature | Zinc Finger Nucleases (ZFNs) | TALENs |
|---|---|---|
| DNA Recognition Mechanism | Protein-based (3 bp per zinc finger) | Protein-based (1 bp per TALE repeat) |
| Nuclease Domain | FokI (requires dimerization) | FokI (requires dimerization) |
| Targeting Flexibility | Limited by DNA context effects | High flexibility |
| Development Timeline | Several weeks to months | Several weeks |
| Relative Cost | High | High |
| Scalability | Limited | Limited |
| Best Applications | Stable cell line generation, therapeutic knockouts | Primary cell editing, high-specificity requirements |
CRISPR-Cas Systems for Gene Knockout
Mechanism of Action
The CRISPR-Cas9 system has revolutionized genetic manipulation through its RNA-guided DNA targeting mechanism. The system comprises two core components: the Cas9 endonuclease and a single-guide RNA (sgRNA) that combines the functions of the CRISPR RNA (crRNA) and trans-activating crRNA (tracrRNA) [67] [68]. The sgRNA contains a 20-nucleotide sequence complementary to the target DNA, which directs Cas9 to specific genomic loci adjacent to a protospacer adjacent motif (PAM, typically 5'-NGG-3' for Streptococcus pyogenes Cas9) [69] [68].
Upon binding to the target DNA, Cas9 induces a double-strand break (DSB) three base pairs upstream of the PAM sequence [67]. Cellular repair of DSBs occurs primarily through two pathways: non-homologous end joining (NHEJ) often results in small insertions or deletions (indels) that can disrupt the reading frame, creating functional knockouts, or homology-directed repair (HDR) which can be harnessed for precise edits using donor DNA templates [69] [68].
Experimental Design for Cytokine Research
For investigating autocrine and paracrine cytokine signaling, CRISPR knockouts require careful experimental design. sgRNAs should target early exons of cytokine or receptor genes (e.g., IL6, IL6R, TNF, TNFR) to maximize probability of functional disruption [69]. Multiple sgRNAs per gene (typically 3-4) should be screened to identify the most efficient editors. For paracrine signaling studies, consider cell-type-specific delivery systems to dissect signaling contributions from different cellular components within complex co-culture systems [29].
Protocol: CRISPR-Cas9 Knockout in Mammalian Cells
- sgRNA Design: Design 3-4 sgRNAs per target gene using established algorithms (CRISPick, CHOPCHOP). For cytokine genes, consider targeting signal peptide regions or critical functional domains.
- Vector Construction: Clone sgRNA sequences into appropriate expression vectors (e.g., lentiCRISPRv2, Addgene #52961).
- Delivery: Transfect or transduce target cells. For hard-to-transfect primary immune cells, consider nucleofection or lentiviral delivery.
- Selection: Apply appropriate selection (e.g., puromycin 1-5 μg/mL, 48-72 hours) 24 hours post-delivery.
- Validation: Assess editing efficiency 72-96 hours post-delivery via T7E1 assay or tracking of indels by decomposition (TIDE) analysis.
- Functional Assays: Establish clonal populations and validate knockout via Western blotting and functional cytokine signaling assays [67] [68].
CRISPR Interference (CRISPRi) for Gene Suppression
Principles and Advantages
CRISPR interference (CRISPRi) represents a refined approach for reversible gene silencing without permanent DNA alteration. The system utilizes a catalytically "dead" Cas9 (dCas9) protein, generated through point mutations (D10A and H840A for SpCas9) that abolish nuclease activity while preserving DNA-binding capability [69]. When targeted to gene promoters by sgRNAs, dCas9 creates a steric block that physically impedes RNA polymerase binding or progression, resulting in transcriptional repression [69].
For enhanced suppression, dCas9 is often fused to transcriptional repressor domains such as the Krüppel-associated box (KRAB), which recruits additional chromatin-modifying complexes to establish a repressive chromatin state [69]. This approach typically achieves 70-99% gene repression without altering the underlying DNA sequence, making it ideal for studying essential genes where complete knockout would be lethal, or for transiently dissecting cytokine signaling dynamics [69].
Implementing CRISPRi in Signaling Studies
CRISPRi is particularly valuable for investigating the temporal dynamics of autocrine and paracrine signaling. The reversible nature of CRISPRi enables researchers to probe how acute versus chronic cytokine suppression differentially impacts signaling networks. For cytokine genes regulated by feedback loops, such as IL-6 and TNF-α, CRISPRi can dissect these regulatory mechanisms without the compensatory adaptations that may occur in stable knockout models [29] [69].
Protocol: CRISPRi Knockdown for Cytokine Signaling Studies
- dCas9-KRAB Expression: Establish stable cell lines expressing dCas9-KRAB or deliver via lentiviral vectors.
- sgRNA Design: Design sgRNAs targeting transcription start sites (-50 to +300 bp relative to TSS). Multiple sgRNAs per gene often yield improved repression.
- Delivery: Introduce sgRNAs via lentiviral transduction at low MOI to ensure single-copy integration.
- Validation: Assess knockdown efficiency 72-96 hours post-transduction via qPCR and/or Western blot.
- Functional Assays: Evaluate effects on cytokine secretion (ELISA), signaling pathway activation (phospho-flow cytometry), and transcriptomic responses (RNA-seq) [69].
Table 2: Research Reagent Solutions for Genetic Manipulation
| Reagent Type | Specific Examples | Function & Application |
|---|---|---|
| Nuclease Systems | SpCas9, FokI-dCas9, ZFNs, TALENs | Creates DSBs or binds DNA targets for editing or repression |
| Delivery Vectors | Lentiviral vectors (lentiCRISPRv2), Adenoviral vectors, Plasmid DNA | Delivers genetic editing components to target cells |
| Selection Markers | Puromycin N-acetyltransferase, Neomycin resistance | Enriches for successfully modified cells |
| Reporter Systems | GFP, RFP, Luciferase | Tracks editing efficiency and validates targeting |
| dCas9 Fusion Proteins | dCas9-KRAB, dCas9-VPR | Enables transcriptional repression (KRAB) or activation (VPR) |
Comparative Analysis of Platforms
Technical Performance Metrics
Each genetic manipulation platform offers distinct advantages and limitations for cytokine research. Traditional methods (ZFNs, TALENs) provide high specificity with lower off-target effects but require substantial protein engineering expertise and time [67]. CRISPR-Cas9 enables rapid prototyping and multiplexed screening but may have higher off-target activity, though high-fidelity Cas9 variants (e.g., HiFi Cas9) have mitigated this concern [67] [68]. CRISPRi offers reversible, titratable suppression without genomic damage but achieves incomplete knockdown compared to complete knockout [69].
Table 3: Platform Comparison for Cytokine Research Applications
| Parameter | CRISPR-Cas9 | CRISPRi | ZFNs/TALENs |
|---|---|---|---|
| Mechanism | DNA cleavage | Transcriptional repression | DNA cleavage |
| Efficiency | High (often >70%) | Variable (70-99%) | Moderate to high |
| Permanence | Permanent | Reversible | Permanent |
| Multiplexing Capacity | High (multiple gRNAs) | High (multiple gRNAs) | Limited |
| Development Time | Days | Days | Weeks to months |
| Off-Target Effects | Moderate (improved with HiFi variants) | Low to moderate | Low |
| Best for Cytokine Studies | Complete pathway disruption, essential gene analysis | Signaling dynamics, essential genes, reversible manipulation | High-specificity requirements, therapeutic applications |
Application to Autocrine and Paracrine Signaling Research
The investigation of inflammatory cytokine networks requires careful platform selection based on specific research questions. For definitive establishment of a cytokine's role in autocrine signaling, CRISPR-Cas9 knockout provides unambiguous evidence through complete gene disruption [29]. When studying cytokines with pleiotropic effects or essential cellular functions, CRISPRi enables researchers to titrate suppression levels and observe dose-dependent signaling effects [69].
In complex co-culture systems modeling paracrine interactions between immune cell subsets, CRISPRi offers particular advantages by allowing transient, cell-type-specific suppression without permanently altering cellular identity or function. For high-throughput screening of cytokine signaling components, multiplexed CRISPR-Cas9 libraries enable systematic identification of novel regulators within autocrine and paracrine networks [68].
Advanced Applications and Future Directions
Multiplexed Genetic Screens
Multiplexed CRISPR screening enables comprehensive functional analysis of cytokine signaling networks at unprecedented scale. By delivering pooled sgRNA libraries targeting hundreds or thousands of genes simultaneously, researchers can identify both known and novel regulators of specific cytokine responses [68]. For autocrine signaling studies, positive selection screens can identify genes whose knockout confers resistance to cytokine-mediated effects. For paracrine signaling, co-culture screening models can identify genes in producer cells required for cytokine production and genes in responder cells required for cytokine sensing and signal transduction [68].
The CDKO (combinatorial double-knockout) library approach enables systematic mapping of genetic interactions within cytokine signaling pathways, revealing synthetic lethal interactions and compensatory mechanisms that maintain signaling fidelity [68]. When integrated with single-cell RNA sequencing (CRISPR-seq), these approaches can simultaneously capture genetic perturbations and transcriptional responses, providing deep insights into cytokine-mediated gene regulatory networks [68].
Therapeutic Applications
Genetic manipulation technologies hold significant promise for developing novel therapies targeting dysregulated cytokine signaling in autoimmune and inflammatory diseases. CRISPR-Cas9 has been explored for directly disrupting pathogenic cytokine genes or their receptors in adoptive cell therapies [69]. CRISPRi offers a potentially safer approach for reversible suppression of cytokine production without permanent genomic alteration [69].
In rheumatoid arthritis, CRISPR-based approaches have targeted TNF-α signaling components, while in inflammatory bowel disease, interventions have focused on IL-23 and other cytokines critical to disease pathogenesis [69]. For systemic lupus erythematosus, researchers have used CRISPR to modulate B-cell function and autoantibody production [69]. As delivery technologies advance, particularly nanoparticle-based systems capable of cell-type-specific targeting, in vivo genetic manipulation may become feasible for directly modulating pathological cytokine signaling in human patients [69].
Co-culture Systems for Studying Cell-Cell Communication
Cell-cell communication is a cornerstone of physiological and pathological processes, enabling multicellular organisms to coordinate complex functions. Co-culture systems, defined as the in vitro cultivation of multiple distinct cell types, have emerged as indispensable tools for deconstructing these intricate communication networks. Within the specific context of inflammatory cytokine research, these systems allow researchers to move beyond simplistic monocultures to model the dynamic paracrine and autocrine signaling loops that characterize in vivo inflammatory environments [70] [71]. Such models are crucial for bridging the gap between traditional cell culture and complex animal models, offering enhanced physiological relevance while maintaining experimental control [72] [71].
The study of inflammatory cytokines exemplifies the necessity of co-culture approaches. Inflammation is rarely mediated by a single cell type in isolation; rather, it arises from a cascade of signals exchanged between immune cells, stromal cells, and tissue-specific parenchymal cells [70] [73]. For instance, in rheumatoid arthritis, a pathological feedback loop between fibroblast-like synoviocytes and macrophages drives disease progression [73]. Similarly, in ocular inflammation, communication between corneal epithelial cells and neutrophils amplifies the production of IL-6, IL-8, and MCP-1 [70]. Co-culture systems provide the platform necessary to interrogate these specific cellular interactions, enabling the dissection of key signaling pathways and the identification of novel therapeutic targets for inflammatory diseases.
Core Concepts of Cell Signaling in Co-culture Systems
To effectively utilize co-culture systems, one must first understand the fundamental modes of cellular crosstalk these models are designed to capture. Cell signaling can be broadly classified based on the distance over which the signal acts, and co-culture configurations can be tailored to study each of these mechanisms.
Paracrine Signaling: This involves a signaling cell releasing ligands that act on nearby target cells. The signals are rapidly degraded or taken up, ensuring a localized effect [39] [1]. A canonical example is the release of neurotransmitters across a synaptic cleft [39]. In inflammatory co-cultures, this is the primary mode by which immune cells, such as macrophages, activate surrounding stromal cells through the release of cytokines like TNF-α, IL-1β, and IL-6 [73].
Autocrine Signaling: A cell secretes a signaling molecule that then binds to receptors on its own surface, leading to a self-regulatory response [39] [1]. This mechanism is critical in processes like pain sensation, inflammatory responses, and early developmental patterning [1]. In a co-culture context, autocrine signaling can work in concert with paracrine signaling to amplify an inflammatory response within a single cell population.
Juxtacrine Signaling: This direct contact-mediated signaling occurs through interactions between membrane-bound proteins on adjacent cells. While not always categorized separately from direct contact, it is a vital mechanism in feeder cell co-culture systems and immune cell recognition [74].
Endocrine Signaling: Involving hormones released into the bloodstream to act on distant target organs, this is less commonly the primary focus of standard in vitro co-cultures but can be modeled in advanced body-on-a-chip systems that link multiple tissue modules [39] [71].
The following table summarizes these key signaling types and their relevance to co-culture model design.
Table 1: Forms of Cell-Cell Communication and Their Modeling in Co-culture Systems
| Signaling Type | Signaling Distance | Key Characteristics | Relevance to Co-culture Models |
|---|---|---|---|
| Paracrine | Local (diffusion through extracellular matrix) | Fast response, short duration; ligands degraded locally [39] [1]. | Modeled in both direct and indirect (e.g., Transwell) co-cultures; key for cytokine/chemokine studies [70] [73]. |
| Autocrine | Self-signaling | Regulates cell survival, differentiation, and inflammatory responses [39] [1]. | Occurs within each cell type in a co-culture; can be studied using specific receptor blockers. |
| Juxtacrine | Direct cell-cell contact | Requires physical contact via gap junctions or membrane ligand-receptor pairs [1] [74]. | Modeled in direct contact co-cultures; studied in feeder-layer systems or with direct cell mixing [74]. |
| Endocrine | Long-distance (via bloodstream) | Slow response, long-lasting effect; hormones diluted in circulation [39] [1]. | Modeled in advanced multi-organ microfluidic "body-on-a-chip" platforms [71] [75]. |
Figure 1: Logical workflow for selecting a co-culture system based on the primary signaling mode of interest.
Designing a Co-culture System for Inflammatory Research
The transition from principle to practice requires careful consideration of the physical configuration of the co-culture system. The choice of model depends on the research question, specifically whether the cell-cell communication of interest requires direct physical contact or is mediated solely by soluble factors.
Direct Contact Co-culture Systems
In this configuration, two or more cell types are cultured in direct physical contact within the same compartment. This is achieved by seeding the cells simultaneously as a mixed population or by layering one cell type onto a pre-established monolayer of another [74].
- Applications: This system is ideal for investigating juxtacrine signaling and the combined effects of direct contact and soluble factor exchange. It is particularly useful for studying processes like immune synapse formation, cell migration, and the differentiation of stem cells when in contact with a feeder layer [74]. For example, a direct contact co-culture of neurons and glial cells allows for the study of contact-dependent mechanisms that influence neuronal differentiation and survival [74].
- Workflow: The typical workflow involves preparing single-cell suspensions of each cell type, mixing them in a specific, optimized ratio, and then seeding the mixture into a culture vessel. Alternatively, for feeder-layer systems, one cell type is treated with a mitotic inhibitor and then used as a substrate for the second cell type [74].
Figure 2: Direct contact co-culture workflow.
Indirect Contact Co-culture Systems
Indirect co-culture systems physically separate the different cell types while allowing them to share the same culture medium or communicate via soluble factors. This separation is most commonly achieved using Transwell inserts, which are permeable membrane filters that fit into standard multi-well plates [70] [72] [76].
- Applications: This setup is perfectly suited for the specific study of paracrine and autocrine signaling without the confounding variable of direct cell contact [74]. It is the system of choice for modeling inflammatory cytokine loops, such as the interaction between macrophages and fibroblasts in rheumatoid arthritis [73] or between neutrophils and corneal epithelial cells in ocular inflammation [70]. It is also widely used to study barrier function, as in gut-immune [76] or vascular models.
- Workflow: One cell type (e.g., macrophages) is seeded on the permeable membrane of the Transwell insert, while the other (e.g., fibroblasts) is seeded in the bottom of the well. The insert is then placed into the well, creating a shared fluidic compartment. Soluble factors secreted by one cell type can diffuse through the membrane to influence the other cell type, and vice-versa [72] [76].
Figure 3: Indirect contact co-culture using a Transwell system.
Advanced Model Systems: From 2D to 3D and Microfluidics
While 2D co-cultures are a mainstay, the field is rapidly advancing towards more physiologically relevant 3D models.
- Three-Dimensional (3D) Co-culture Systems: Cells are cultured within a 3D scaffold or hydrogel (e.g., Matrigel, collagen, alginate) that more closely mimics the in vivo extracellular matrix (ECM) [71] [74]. This 3D context influences cell morphology, polarity, and signaling, often leading to more authentic cellular responses. 3D systems are used to model tissues like the brain, liver, and tumors with high fidelity [71] [74].
- Organoid and Spheroid Co-cultures: These are complex, self-organizing 3D structures that can contain multiple cell types from a specific tissue or organ. Tumor organoids, for instance, can be co-cultured with cancer-associated fibroblasts (CAFs) or immune cells to study tumor-stromal interactions in a highly representative TME [71].
- Microfluidic "Organ-on-a-Chip" Systems: These devices incorporate continuous perfusion of culture medium through micro-chambers containing living cells. They provide dynamic fluid flow (shear stress), improved mass transport, and the ability to create stable chemical gradients [71] [75]. Chips can be designed to model the gut-immune axis [76] or the neurovascular unit [72], and multiple chips can be linked to create a "body-on-a-chip" for systemic studies [71] [75].
Table 2: Comparison of Co-culture Model Complexities
| Model Type | Key Features | Pros | Cons | Best for Studying |
|---|---|---|---|---|
| 2D Co-culture | Cells grow on a flat, rigid surface [77]. | Simple, scalable, highly reproducible, easy to image and analyze [77]. | Low physiological relevance; abnormal cell morphology and polarity [74]. | Initial screening of cell-cell interactions; paracrine signaling. |
| 3D Co-culture | Cells embedded in hydrogel or ECM scaffold [71] [74]. | More physiologically relevant cell morphology, signaling, and drug responses [71]. | More complex, less scalable, potential batch variability of ECM [71]. | Complex tissue modeling (tumors, neural tissue); microenvironmental effects. |
| Organ-on-a-Chip | Microfluidic channels with perfusable cell chambers [71] [75]. | Mechanical forces (shear stress), improved nutrient/waste exchange, gradient formation [75]. | Technically challenging, requires specialized equipment, low throughput [75]. | Barrier function, vascular interactions, systemic effects in linked systems. |
Detailed Experimental Protocol: A Macrophage-Fibroblast Inflammatory Co-culture
The following protocol, adapted from a recent rheumatoid arthritis (RA) study, provides a concrete example of establishing a 2D Transwell co-culture to investigate paracrine signaling in inflammation [73].
Materials and Cell Preparation
- Research Reagent Solutions:
- THP-1 Human Monocytes: Maintain in RPMI-1640 + 10% FBS. Differentiate into M0 macrophages with 100 nM PMA for 24 hours. Polarize to M1 phenotype with 100 ng/mL LPS for 48 hours [73].
- Fibroblast-like Synoviocytes (FLS): Use either a human cell line (e.g., SW982) or primary cells isolated from synovial tissue via collagenase digestion. Culture in DMEM + 10% FBS [73].
- Transwell Inserts: Use inserts with a 0.4 µm or 0.8 µm pore membrane, suitable for 24-well or 96-well plates [76] [73].
- Key Reagents: PMA, LPS, Methotrexate (for therapeutic validation), ELISA kits for TNF-α, IL-6, IL-1β, MMPs, RNA extraction kit, primers for qPCR.
Co-culture Establishment and Stimulation
- Differentiate and Activate Macrophages: Differentiate THP-1 monocytes in a culture dish to generate M0 macrophages using PMA. Subsequently, polarize them to an M1 pro-inflammatory state using LPS. After polarization, thoroughly wash the cells to remove all LPS [73].
- Seed the Co-culture:
- Detach the differentiated M1 macrophages and seed them onto the permeable membrane of the Transwell insert.
- Seed the FLS in the bottom well of the culture plate.
- Allow both cell types to adhere adequately (e.g., 4-6 hours).
- Assemble the System: Carefully place the Transwell insert containing the macrophages into the well containing the FLS. This creates a shared medium compartment, allowing soluble factors to diffuse between the two cell populations.
- Stimulation and Intervention: To model disease, the system can be further stimulated. For therapeutic testing, add drugs like Methotrexate to the culture medium. Incubate for the desired timeframe (e.g., 24-48 hours) [73].
Readouts and Analysis
- Inflammatory Cytokine Production: Collect conditioned medium and quantify levels of key cytokines (e.g., TNF-α, IL-1β, IL-6) using ELISA. This directly measures paracrine signaling output [70] [73].
- Gene Expression Analysis: After co-culture, separately lyse cells from the insert (macrophages) and the well bottom (FLS). Perform RNA extraction and qPCR to measure expression of pro-inflammatory genes, matrix metalloproteinases (MMPs), and other markers of interest [73].
- Functional Assays:
- Fibroblast Invasion: Use a Matrigel-coated transwell invasion assay. Place serum-free medium in the top chamber and FLS in the bottom chamber. Activated FLS from the co-culture will exhibit enhanced invasion through the Matrigel, which can be quantified after staining [73].
- Barrier Integrity: For epithelial/endothelial models, measure Transepithelial/Endothelial Electrical Resistance (TEER) using an volt-ohm meter to assess barrier function in real-time [76].
Quantitative Insights from Co-culture Models
Co-culture models consistently reveal a significant amplification of inflammatory responses compared to monocultures, underscoring the critical role of cell-cell communication in driving pathology.
Table 3: Quantitative Amplification of Inflammatory Markers in Co-culture Systems
| Disease/Model Context | Cell Types Co-cultured | Key Inflammatory Markers | Fold-Change in Co-culture vs. Control | Citation |
|---|---|---|---|---|
| Rheumatoid Arthritis | M1 Macrophages / Fibroblast-like Synoviocytes (FLS) | IL-1β | 6.30-fold increase | [73] |
| IL-6 | 4.94-fold increase | [73] | ||
| TNF-α | 1.57-fold increase | [73] | ||
| MMP9 | 37.61-fold increase | [73] | ||
| Ocular Inflammation | Corneal Epithelial Cells (HCE-T) / Neutrophils (dHL-60) + PM | IL-8, IL-6, MCP-1 | Production enhanced in co-culture | [70] |
| Diabetic Retinopathy | Retinal Vascular Endothelial Cells (RRMECs) / Ganglion Cells (RGCs) + High Glucose | Endothelial Migration & Lumen Formation | Significantly lower in co-culture vs. monoculture | [72] |
| Ganglion Cell Apoptosis Index | Higher in co-culture vs. monoculture | [72] |
These quantitative data validate that co-culture systems capture synergistic interactions where the combined response is greater than the sum of individual cell responses. The dramatic upregulation of IL-1β and MMP9 in the RA model [73] highlights a powerful inflammatory and tissue-destructive loop that would be missed in macrophage-only or fibroblast-only cultures.
Co-culture systems are powerful and versatile platforms that have fundamentally advanced our ability to study cell-cell communication, particularly the paracrine and autocrine signaling of inflammatory cytokines. By moving from simple 2D setups to sophisticated 3D and microfluidic models, researchers can now capture the multicellular complexity of physiological and pathological processes with increasing fidelity. The quantitative data generated from these models, such as the dramatic amplification of cytokine production, provides compelling evidence for the critical role of cellular crosstalk in diseases like rheumatoid arthritis and diabetic retinopathy.
As the field progresses, the integration of co-culture with patient-derived cells, including organoids and primary immune cells, will further enhance the personalization and predictive power of these models. This will be invaluable for drug development professionals aiming to screen novel anti-inflammatory therapies in human-relevant systems before advancing to costly clinical trials, ultimately accelerating the delivery of new treatments for inflammatory diseases.
Live-Cell Imaging of Spatiotemporal Signaling Dynamics
The ability to visualize and quantify cellular communication in real-time is paramount to understanding complex biological processes, from immune responses to cancer progression. Live-cell imaging has emerged as a cornerstone technique for elucidating the spatiotemporal dynamics of signaling molecules, particularly those involved in autocrine and paracrine signaling. Autocrine signaling occurs when a cell secretes signaling molecules that bind to receptors on its own surface, while paracrine signaling involves the communication between neighboring cells over short distances. These signaling modes are especially significant in the context of inflammatory cytokines, which shape the tumor microenvironment (TME) and drive critical processes including cancer initiation, proliferation, metastasis, and therapeutic resistance [78].
Inflammatory cytokines such as IL-6, IL-8, and various chemokines function within dynamic, self-perpetuating feedback loops that are challenging to capture with endpoint measurements alone [78]. The stromal cell-derived factor-1α (SDF-1α)/CXCR4 chemokine/receptor pair exemplifies this complexity, guiding neural stem cell recruitment to injury sites and contributing to metastatic cancer cell migration through autocrine/paracrine mechanisms [79]. Understanding these signaling dynamics requires not only advanced imaging technologies but also sophisticated computational models to interpret the resulting data. This technical guide provides a comprehensive framework for designing and executing live-cell imaging studies to decode these intricate spatiotemporal signaling dynamics, with particular emphasis on methodologies relevant to inflammatory cytokine research in drug development.
Key Applications in Autocrine/Paracrine Signaling Research
Mapping Inflammatory Cytokine Networks
Live-cell imaging enables researchers to track the secretion and diffusion of inflammatory cytokines that shape the tumor microenvironment. These cytokines, including IL-6, IL-8, TNF, IL-17, and various chemokines such as CCL-5, are known to promote tumor growth through both autocrine and paracrine mechanisms [78]. For instance, cancer cells can secrete cytokines that in an autocrine fashion generate a forward-feedback loop to stimulate self-proliferation, expansion, and drug resistance. Simultaneously, these same cytokines act in a paracrine manner to induce recruitment, activation, and differentiation of other cells in the TME [78]. The senescence-associated secretary phenotype (SASP), which includes pro-inflammatory cytokines like IL-1α, IL-1β, IL-6, IL-8, CXCL-1, and CXCL-2, can induce tumorigenesis in a paracrine fashion [78]. Live-cell imaging allows researchers to capture these dynamic interactions, revealing how cytokine gradients form and evolve over time to influence cellular behavior.
Visualizing SDF-1α/CXCR4 Signaling Dynamics
The SDF-1α/CXCR4 chemokine/receptor pair serves as a paradigm for studying spatiotemporal signaling dynamics in live cells. This signaling axis is responsible for the migration of various cell types, including neural stem cells toward injury sites and metastatic cancer cells [79]. Research has demonstrated that SDF-1α/CXCR4 autocrine/paracrine signaling contributes to long-distance migration of numerous cell types outside the central nervous system, including skin, breast, and ovarian cancers [79]. A key study revealed that exogenous SDF-1a administration led to significantly increased Schwann cell migration and upregulation of SDF-1a compared to non-treated controls, suggesting a self-reinforcing autocrine loop [79]. Live-cell imaging of this signaling pathway can reveal how cells detect gradients of SDF-1α through spatial and temporal sensing of occupied receptors, thereby guiding cells along chemotactic gradients—a process fundamental to both physiological repair mechanisms and pathological processes like metastasis.
Table 1: Key Inflammatory Cytokines in Autocrine/Paracrine Signaling and Their Functions
| Cytokine/Chemokine | Primary Signaling Mode | Biological Functions in Cancer | Live-Cell Imaging Approaches |
|---|---|---|---|
| SDF-1α (CXCL12) | Autocrine/Paracrine | Stem cell recruitment, Metastatic cell migration, Schwann cell migration | Gradient visualization, Receptor internalization tracking |
| IL-6 | Autocrine/Paracrine | Tumor cell proliferation, Forward-feedback loops, Drug resistance | FRET-based activation sensors, Secretion assays |
| IL-8 | Autocrine/Paracrine | Angiogenesis, Neutrophil recruitment, Tumor cell migration | Gradient mapping, Cell migration tracking |
| TNF | Paracrine | NF-κB activation, Cell survival/proliferation, Inflammation | NF-κB translocation assays, Signaling activation reporters |
| SASP Factors (IL-1α/β, IL-6, IL-8, CXCL-1/2) | Paracrine | Tumorigenesis, Microenvironment remodeling, Chronic inflammation | Multiplexed imaging, Secretion kinetics analysis |
Quantitative Live-Cell Imaging Platforms and Technologies
Advanced Imaging Systems for Spatial Dynamics
The selection of appropriate imaging technology is critical for capturing the rapid, often subtle dynamics of autocrine and paracrine signaling. Widefield fluorescence microscopy provides a foundational approach for live-cell imaging, offering fast acquisition speeds suitable for tracking rapid signaling events. However, this technique may suffer from out-of-focus light, which can limit spatial resolution in thick samples. Confocal microscopy, particularly spinning disk confocal systems, eliminates out-of-focus light through optical sectioning, providing improved spatial resolution while maintaining the speed necessary for live-cell imaging [80]. For ultra-high resolution imaging, techniques such as super-resolution radial fluctuations (SRRF) enable visualization of subcellular structures and protein localization beyond the diffraction limit, as demonstrated in the PRISMS platform which can perform automated repeated frame imaging for SRRF reconstructions [80].
Recent advancements in spatial transcriptomics technologies have bridged the gap between molecular profiling and spatial context, with platforms like Stereo-seq v1.3, Visium HD FFPE, CosMx 6K, and Xenium 5K offering subcellular resolution [81]. These platforms can be broadly categorized into sequencing-based spatial transcriptomics (sST) and imaging-based spatial transcriptomics (iST), each with distinct advantages. sST platforms like Stereo-seq and Visium HD enable unbiased whole-transcriptome analysis by capturing poly(A)-tailed transcripts with poly(dT) oligos on spatially barcoded arrays, while iST platforms such as CosMx and Xenium utilize iterative hybridization of fluorescently labeled probes followed by sequential imaging to profile gene expression in situ at single-molecule resolution [81]. Systematic benchmarking of these platforms has revealed differences in sensitivity, specificity, and diffusion control, with Xenium 5K demonstrating superior sensitivity for multiple marker genes including the epithelial cell marker EPCAM [81].
The PRISMS Open-Source Platform
The Python-based Robotic Imaging and Staining for Modular Spatial Omics (PRISMS) platform represents a significant advancement in democratizing spatial omics by providing an open-source, automated multiplexing pipeline [80]. PRISMS utilizes a liquid handling robot with thermal control to enable rapid and automated staining of RNA and protein samples, addressing the high costs and technical barriers associated with proprietary spatial omics platforms. The platform's modular sample holders and Python control facilitate high-throughput, single-molecule fluorescence imaging on both widefield and confocal microscopes [80].
A key innovation of PRISMS is its compatibility with Nikon NIS Elements Basic Research software, enabling custom image acquisition through command-level commands, autofocus correction for Z drift, and generation of Fiji/ImageJ macros to stitch overlapping images for large scan imaging [80]. This custom pipeline is particularly valuable for super-resolved acquisitions such as SRRF, which requires repeated frame imaging (~100 frames) of single Z coordinates—a capability not typically available in standard imaging software [80]. By providing an open-source, customizable workflow, PRISMS enables researchers to tailor acquisition and analysis parameters to their specific autocrine/paracrine signaling questions, moving beyond the "black box" limitations of proprietary systems.
Table 2: Technical Comparison of Spatial Omics Platforms for Signaling Dynamics Research
| Platform/Technology | Spatial Resolution | Gene Detection Capacity | Key Advantages | Limitations |
|---|---|---|---|---|
| PRISMS (Open-source) | Subcellular (with SRRF) | Customizable panels | Open-source, Cost-effective, Customizable acquisition | Requires technical expertise for implementation |
| Xenium 5K (10x Genomics) | Subcellular | 5,001 genes | High sensitivity, Commercial support, Integrated analysis | Proprietary platform, Higher cost |
| CosMx 6K (NanoString) | Single-molecule | 6,175 genes | Comprehensive panel, High-plex protein capability | Lower correlation with scRNA-seq than other platforms |
| Visium HD FFPE (10x Genomics) | 2 μm | 18,085 genes | Whole-transcriptome, Unbiased detection | Lower resolution than imaging-based methods |
| Stereo-seq v1.3 (BGI) | 0.5 μm | Whole-transcriptome | Highest resolution for sequencing-based, Unbiased detection | Computational intensity for data processing |
Experimental Protocols for Signaling Dynamics
Protocol: Live-Cell Imaging of SDF-1α/CXCR4 Autocrine/Paracrine Signaling
This protocol outlines a methodology for investigating SDF-1α/CXCR4 signaling dynamics, based on established approaches with modifications for enhanced spatiotemporal resolution [79].
Materials:
- CXCR4-EGFP transgenic mice or cell lines expressing CXCR4-EGFP
- Recombinant SDF-1α conjugated with AlexaFluor647 (AFSDF-1α)
- Poly(lactic-co-glycolic) acid (PLGA) nanoparticles for controlled SDF-1α release
- Primary microglia, astrocytes, and brain endothelial cells
- Live-cell imaging chamber with environmental control (37°C, 5% CO₂)
- Confocal or spinning disk microscope system with temperature and COâ‚‚ control
Methods:
- Sample Preparation:
- Isolate primary microglia, astrocytes, and brain endothelial cells from neonatal CXCR4-EGFP mice (aged P0-P2) using magnetic bead separation for CD11b (microglia) or Glast (astrocytes) [79].
- Culture cells in appropriate growth media on glass-bottom dishes or coverslips compatible with live-cell imaging.
- For SDF-1α stimulation, prepare either bolus injections (30 ng) or SDF-1α-loaded PLGA nanoparticles designed to release approximately 30 ng in the first 24 hours followed by 9 ng over the next 6 days [79].
Imaging Setup:
- Configure microscope for simultaneous detection of EGFP (CXCR4 receptor) and AlexaFluor647 (SDF-1α ligand).
- Set up time-lapse acquisition with appropriate intervals (e.g., 30-second to 5-minute intervals depending on experimental question).
- Define multiple positions for automated imaging across different conditions.
- For gradient analysis, implement tiling or large-area scanning to capture broader spatial contexts.
Image Acquisition:
- Acquire baseline images for 10-30 minutes before SDF-1α stimulation to establish baseline dynamics.
- Add SDF-1α (either bolus or nanoparticle-released) and continue time-lapse acquisition for 4-24 hours depending on experimental goals.
- For autocrine/paracrine signaling assessment, include conditions with CXCR4 inhibitors (e.g AMD3100) to disrupt the feedback loop.
Data Analysis:
- Quantify CXCR4-EGFP redistribution and internalization in response to SDF-1α stimulation.
- Track SDF-1α gradient formation and dissipation over time using fluorescence intensity profiles.
- Apply mathematical models that incorporate autocrine/paracrine mechanisms to accurately capture SDF-1α temporal trends and spatial distribution [79].
Protocol: Multiplexed Cytokine Signaling Dynamics with PRISMS
This protocol leverages the open-source PRISMS platform for automated, multiplexed imaging of inflammatory cytokine signaling dynamics [80].
Materials:
- PRISMS-compatible microscope (Nikon widefield or Cephla spinning disk confocal)
- Opentrons OT-2 liquid handling robot
- Temperature modules for thermal control during staining
- DNAse I enzyme (for RNA label removal) or LiBH4 (for protein photobleaching)
- Custom 3D-printed mount for tissue slides or laser-cut acrylic holders for coverslips
- Fluorescently labeled probes for target cytokines or their receptors
Methods:
- System Setup:
- Install PRISMS Python package and dependencies (Jupyter notebook environment).
- Configure microscope integration through Nikon NIS Elements Basic Research software.
- Calibrate liquid handling robot for automated staining procedures.
Automated Staining:
- Program OT-2 robot for rapid, multiplex staining of up to 12 slides or coverslips in a single run.
- Utilize temperature modules to facilitate both hybridization chain reaction (HCR) RNA and immunofluorescence (IF) protein staining.
- Implement cyclic multiplexing by removing labeled fluorescence with DNAse I enzyme (RNA) or LiBH4 photobleaching (protein), followed by repeated staining and imaging [80].
Image Acquisition:
- Use PRISMS to write command-level NIS Elements commands for custom image acquisition.
- Implement automated focus correction by computing autofocus correction for Z drift.
- Acquire images using tiling patterns (individual FOVs, contiguous FOVs for stitching, or combination patterns).
- For super-resolution applications, acquire repeated frames (~100) for SRRF reconstruction.
Image Processing and Analysis:
- Execute Fiji/ImageJ macros generated by PRISMS for stitching overlapping images.
- Perform SRRF reconstruction for super-resolved imaging when applicable.
- Conduct automated post-processing including background subtraction, thresholding, and individual channel rendering.
- Extract single-cell statistics and expression patterns for correlation with signaling dynamics.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagent Solutions for Live-Cell Imaging of Signaling Dynamics
| Reagent/Material | Function | Example Application | Technical Notes |
|---|---|---|---|
| CXCR4-EGFP transgenic models | Visualize receptor localization and trafficking | Real-time tracking of CXCR4 dynamics in response to SDF-1α | Available as mouse models or can be introduced via transfection/transduction |
| AFSDF-1α (AlexaFluor647-conjugated) | Track ligand distribution and gradient formation | Monitor SDF-1α diffusion and binding in live cells | Distinguishes exogenous from endogenous SDF-1α [79] |
| PLGA nanoparticles | Controlled release of signaling molecules | Sustain SDF-1α presentation to simulate physiological release | Can be engineered for specific release kinetics [79] |
| Opentrons OT-2 robot | Automated liquid handling | High-throughput, reproducible staining for multiplexed imaging | Integrated with PRISMS platform for spatial omics [80] |
| Modular sample holders | Adapt various sample formats for imaging | Accommodate tissue slides, coverslips, or well plates | 3D-printed mounts for slides; laser-cut acrylic for coverslips [80] |
| DNAse I enzyme | Remove RNA labels between cycles | Enable cyclic multiplexing in RNA detection | Allows repeated staining and imaging rounds [80] |
| LiBH4 | Photobleaching agent for protein labels | Reset fluorescence between imaging cycles in protein detection | Enables cyclic multiplexing for protein targets [80] |
| Quantitative calibration standards | Convert fluorescence to absolute units | Standardize measurements across instruments and time | Enables definitive quantitative analysis rather than relative measurements [82] |
| Metergoline | Metergoline, CAS:17692-51-2, MF:C25H29N3O2, MW:403.5 g/mol | Chemical Reagent | Bench Chemicals |
| Metesind Glucuronate | Metesind Glucuronate, CAS:157182-23-5, MF:C29H34N4O10S, MW:630.7 g/mol | Chemical Reagent | Bench Chemicals |
Data Analysis and Computational Modeling
Quantitative Analysis of Spatiotemporal Data
The transformation of raw imaging data into quantitative biological insights requires rigorous analytical approaches. Flow cytometry represents a powerful complementary technique that, when properly calibrated, can provide definitive quantitative data rather than the quasi-quantitative or qualitative data typically reported [82]. Embracing quantitative flow cytometry through instrument standardization, calibration with commercially available multi-intensity beads with Equivalent Reference Fluorophore (ERF) assigned SI-traceable values, and proper antigen quantitation approaches enables researchers to generate data that can be trusted, compared, and built upon across experiments and laboratories [82].
For spatial analysis, the cytofast R-package provides valuable tools for visualization and quantification of cell clusters, enabling efficient discovery of cell populations associated with diseases or physiology [83]. This approach is particularly valuable for analyzing multiparametric cytometric data to reveal immune signatures and correlations, such as discovering macrophage subsets that significantly decrease upon cancer immunotherapy [83]. When analyzing signaling gradients, it's essential to move beyond simple fluorescence intensity measurements and implement spatial autocorrelation analysis, gradient quantification algorithms, and temporal tracking of signal propagation.
Mathematical Modeling of Signaling Dynamics
Computational models are indispensable for interpreting complex spatiotemporal signaling data and generating testable hypotheses. Research on SDF-1α signaling has demonstrated that diffusion-only based mathematical models are unable to accurately capture in vivo SDF-1α spatial distribution [79]. However, incorporating autocrine/paracrine mechanisms into these models allows for accurate recapitulation of SDF-1α temporal trends, indicating these dynamics play an essential role in SDF-1α sustainment [79].
The creation of mathematical models using platforms like COMSOL Multiphysics enables researchers to study spatiotemporal dynamics by simulating both the diffusion of signaling molecules and the cellular responses to those signals [79]. These models should incorporate parameters such as ligand-receptor binding kinetics, receptor internalization and recycling, feedback mechanisms that enhance or suppress signal production, and the spatial constraints of the cellular environment. By iteratively refining these models with experimental data, researchers can develop increasingly accurate representations of autocrine/paracrine signaling networks that predict cellular behaviors under novel conditions.
Signaling Pathways and Experimental Workflows
Computational Modeling of Cytokine Networks and Feedback Loops
Cytokine networks form the core communication infrastructure of the immune system, enabling cells to coordinate responses through autocrine (self-signaling) and paracrine (neighbor-signaling) mechanisms [84]. These networks exhibit remarkable complexity, with over one hundred cytokines existing in families that share receptor components and signal transduction pathways [85]. In inflammatory contexts, dysregulation of these networks can lead to a "cytokine storm" with potentially fatal consequences, making computational modeling essential for understanding their dynamics and identifying therapeutic interventions [86].
The integration of experimental and computational approaches has advanced our understanding of how cytokines like TNFα, IL-6, IL-1β, IL-10, and TGFβ orchestrate inflammatory responses through complex feedback loops [85] [87] [88]. Computational models provide a robust set of tools to analyze these complex interactions, creating novel insights that can be experimentally validated [85]. This technical guide explores the mathematical frameworks, experimental protocols, and computational tools essential for modeling cytokine networks within the broader context of autocrine and paracrine signaling research.
Mathematical Frameworks for Cytokine Network Modeling
Fundamental Modeling Approaches
Computational models of cytokine networks generally fall into two main categories: knowledge-based (theory-driven) and data-driven (empirical) approaches [85]. Knowledge-based models utilize prior biological understanding to construct mathematical representations, while data-driven models analyze complex experimental datasets to generate new hypotheses [85].
Table 1: Comparison of Mathematical Modeling Approaches for Cytokine Networks
| Model Type | Key Features | Typical Applications | Examples in Cytokine Research |
|---|---|---|---|
| Ordinary Differential Equations (ODEs) | Describe rates of change in cytokine concentrations; continuous deterministic modeling | Dynamics of cytokine production, degradation, and signaling | TNFα adaptation to LPS; Th cell differentiation [85] [87] [88] |
| S-system Models | Power-law representation of biochemical systems; variant of ODE formalism | Autocrine/paracrine signaling networks | Microglial cytokine interactions (TNFα, TGFβ, IL-10) [87] |
| Logical Network Models | Discrete, qualitative representation of network interactions | Large-scale network analysis where kinetic parameters are unavailable | CD4+ T cell differentiation pathways [85] |
| Rule-based Modeling | Explicit representation of molecular structures and interactions | Detailed intracellular signaling networks | BioNetGen platform for complex immune signaling [89] |
Core Mathematical Formalisms
The S-system model formulation has proven particularly valuable for modeling autocrine/paracrine cytokine networks. This approach models the expression dynamics of each cytokine using a variant of the classic S-systems formulation [87]:
Where:
Cₓ = Cₓ(t)is the expression of cytokine x at time tkₓis the production rate upon activation by cytokineCᵢat timet - τd,ixτd,ixis the time delay between activation ofCᵢand subsequent activation ofCₓγₓandγₛₛ,ₓare degradation rate constants [87]
For intracellular signaling, ordinary differential equation (ODE) models typically describe the activation of immune cells and cytokine release in response to inflammatory stimuli like LPS. These models incorporate mRNA expression, translation to proteins, and cytokine release into plasma, each with specific half-lives and regulatory interactions [88].
Key Signaling Pathways and Feedback Loops
Microglial Cytokine Network
In central nervous system inflammation, microglia coordinate neuroinflammation through a complex cytokine network. Computational modeling has revealed critical autocrine and paracrine feedback loops involving TNFα, TGFβ, and IL-10 [87].
Microglial Cytokine Feedback Network
This network illustrates how LPS stimulation induces TNFα production, which subsequently stimulates both TGFβ and IL-10 expression. These anti-inflammatory cytokines then inhibit TNFα through negative feedback loops, with each also exhibiting autoregulation [87]. Global sensitivity analysis has revealed that TGFβ- and IL-10-mediated inhibition of TNFα is critical for regulating network behavior, with these parallel negative feedback loops exhibiting differential kinetics that explain their non-intuitive effects when perturbed [87].
Inflammatory Response to Acute and Prolonged Stimulation
Mathematical modeling of the human inflammatory response has revealed distinct dynamics under acute versus prolonged LPS exposure, with implications for understanding sepsis pathophysiology [88]. A multiscale ODE model simulating processes at both cellular and organism levels can capture these differential responses.
Table 2: Key Model Parameters for Inflammatory Response Simulation
| Parameter | Description | Value/Range | Biological Significance |
|---|---|---|---|
| kTNFmRNA, kIL6mRNA, kIL10mRNA | mRNA half-life parameters | Model-specific | Determines rapidity of cytokine response to stimulus [88] |
| sTNF, sIL6, sIL10 | Compounded scaling parameters | Model-specific | Incorporates translation rate and arbitrary scaling factors [88] |
| Ï„d,ix | Time delay between cytokine activation | Variable | Represents signaling cascade delays [87] |
| Kix, nix | Half-maximal activation constant and cooperativity | Network-dependent | Determines sensitivity of cytokine production to regulators [87] |
Multiscale Inflammatory Response Model
This model illustrates how LPS activates immune cells to express mRNA coding for pro- and anti-inflammatory cytokines, which are then translated and released [88]. IL-10 provides negative feedback inhibition of TNF, IL-1β, and IL-6 mRNA expression [88]. At the organism level, IL-1β and IL-6 increase body temperature, which subsequently elevates heart rate, while TNF, IL-1β, and IL-6 cause tissue damage that decreases blood pressure [88].
Experimental Protocols and Methodologies
Parameter Estimation and Model Calibration
Parameter estimation for cytokine network models typically follows a systematic approach combining literature-derived values with experimental data fitting:
- Initialization: Coupling constants (Kix and Kjx) are initiated based on available biochemical data [87].
- Model Fitting: The entire parameter set is fitted to normalized experimental waveforms, with primary focus on recapitulating relative kinetics rather than absolute concentrations [87].
- Constraint Application: Model outputs are constrained to the same order of magnitude to maintain biological plausibility [87].
- Sensitivity Analysis: Global sensitivity analysis identifies parameters with greatest influence on model outputs [88].
- Parameter Estimation: Sensitive parameters are estimated using experimental data, with justification for re-estimating literature-derived values based on in vivo complexity [88].
Model Validation Using Experimental Endotoxemia
Human experimental endotoxemia provides valuable data for model validation. The protocol involves:
- LPS Administration: Healthy human volunteers receive either bolus injections or continuous infusion of bacterial endotoxin (LPS) [88].
- Cytokine Measurement: Serial blood samples are collected to measure TNFα, IL-6, IL-1β, and IL-10 concentrations over time [88].
- Clinical Parameter Monitoring: Body temperature, heart rate, and blood pressure are recorded continuously [88].
- Data Integration: Experimental time-concentration curves are used to validate model predictions [88].
This approach has revealed that models must account for differential responses to acute versus prolonged LPS exposure, with continuous infusion better mimicking the protracted nature of real infections compared to bolus injections [88].
Research Reagent Solutions Toolkit
Table 3: Essential Research Reagents for Cytokine Network Studies
| Reagent/Cell System | Function/Application | Key Features | Representative Use |
|---|---|---|---|
| Primary Microglia | Model system for CNS inflammation | Resident brain macrophages; key regulators of neuroimmune functions | Studying autocrine/paracrine TNFα, TGFβ, IL-10 networks [87] |
| Experimental Endotoxemia | Human inflammatory response model | Intravenous LPS administration; measures cytokine dynamics and vital signs | Model calibration and validation [88] |
| BioNetGen Software | Rule-based modeling of biochemical networks | Graph-based syntax for building reaction models from structured objects | Intracellular signaling network modeling [89] |
| NatE MESA Receptors | Synthetic cytokine biosensors | Converted natural cytokine receptors into orthogonal biosensors | Engineering T cells to sense immunosuppressive cues [90] |
| CD4+ T Cell Differentiation Systems | Modeling T helper cell fate decisions | In vitro polarization of naïve T cells to specific subsets | Studying Th1/Th2/Th17 differentiation networks [85] |
| Methasulfocarb | Methasulfocarb | Methasulfocarb is a thiocarbamate fungicide for rice disease research. This product is for research use only and not for human consumption. | Bench Chemicals |
| Methisazone | Methisazone|Antiviral Research Compound|1910-68-5 | Bench Chemicals |
Advanced Applications and Therapeutic Implications
Engineering Synthetic Cytokine Receptors
Recent advances enable conversion of natural cytokine receptors into orthogonal synthetic biosensors using modular extracellular sensor architecture (MESA). This approach co-opts natural cytokine receptor ectodomains into synthetic receptors that sense soluble cues through mechanisms independent of native pathways [90]. The development process involves:
- Receptor Selection: Choosing human cytokine receptors representing various classes and signaling mechanisms (e.g., VEGFR, IL-10R, TNFR, TGFβR) [90].
- Domain Engineering: Pairing natural receptor ectodomains with MESA intracellular signaling domains, including split tobacco etch virus protease and synthetic transcription factors [90].
- Validation: Testing surface expression and ligand-inducible signaling across design variants [90].
This technology enables engineering of T cells that sense immunosuppressive cues and respond with customized transcriptional output to support chimeric antigen receptor T cell activity, particularly in the tumor microenvironment [90].
Single-Cell Analysis of Cytokine Production
Single-cell technologies have revolutionized understanding of cytokine networks by revealing heterogeneity in cytokine production that was masked in population-level measurements. Key insights include:
- Stable Production Patterns: Individual T cells make stable decisions to produce IFN-γ or not, correlated with T-bet expression and methylation status of relevant loci [85].
- Quantitative Memory: T cells retain quantitative memory of IFN-γ production levels for up to one month in vivo [85].
- Continuum States: Th1/Th2 differentiation occurs through continuous tunable transcription factor expression that drives binary stochastic cytokine secretion, challenging traditional binary fate models [85].
These findings necessitate computational models that account for cellular heterogeneity and memory effects in cytokine responses.
Future Directions and Implementation Considerations
The field of cytokine network modeling is advancing toward multiscale models that integrate intracellular signaling with tissue-level and organism-level responses. Key challenges include parameter identifiability, model reduction while preserving predictive power, and integration of single-cell heterogeneity into population-level models.
Implementation of the models and protocols described requires careful consideration of biological context, as cytokine networks exhibit significant tissue-specific and disease-specific variations. The tools and frameworks presented provide a foundation for developing targeted therapeutic strategies that modulate pathological cytokine networks while preserving essential immune function, particularly in the context of autocrine and paracrine signaling in inflammatory diseases.
Addressing Research Challenges and Technical Limitations
Overcoming Signal Specificity Issues in Complex Microenvironments
In the study of autocrine and paracrine signaling of inflammatory cytokines, researchers face a fundamental challenge: signal specificity in complex microenvironments. Cells residing in tissues like the tumor microenvironment (TME) are simultaneously exposed to multiple overlapping cytokine signals, yet they execute specific and appropriate responses. This precision occurs despite the fact that many inflammatory cytokines share common signaling pathways, particularly the JAK-STAT and NF-κB cascades [91] [31]. The molecular mechanisms that enable discrete signaling outcomes from promiscuous pathways remain a central focus in inflammatory cytokine research.
This technical guide examines the current understanding of how specificity is maintained in these crowded signaling landscapes, with particular emphasis on the spatiotemporal dynamics of signal encoding. We explore experimental approaches for deconvoluting these complex interactions and provide methodological frameworks for researchers investigating autocrine and paracrine inflammatory signaling. The insights gained from these investigations are critical for developing targeted therapeutic interventions that can modulate specific aspects of inflammatory responses without disrupting protective immunity.
Molecular Mechanisms of Signal Encoding
Temporal Patterning of Signaling Output
The timing and duration of cytokine signals represent a primary layer of encoding specificity. Research reveals that identical signaling components can produce distinct transcriptional outcomes based on their activation kinetics [88]. The NF-κB pathway, for instance, exhibits oscillatory behavior in response to certain stimuli while demonstrating sustained activation following other signals. These temporal patterns are decoded by the nucleus to activate specific gene expression programs.
Key temporal encoding mechanisms include:
- Signal pulse frequency: Brief, high-amplitude TNF-α pulses versus sustained IL-1β exposure trigger different NF-κB nuclear translocation dynamics [88]
- Oscillatory patterns: The NLRP3 inflammasome activation creates pulsed IL-1β release, encoding danger signals temporally [91]
- Feedback loop timing: Negative feedback regulators like SOCS proteins exhibit distinct expression kinetics that shape signaling duration and output specificity [91]
Spatial Compartmentalization of Signaling Components
Spatial organization within cells and tissues provides another critical layer of signal specificity. Signaling components are not uniformly distributed but are organized into signalosomes and spatially restricted compartments that dictate interaction specificity.
Spatial regulation mechanisms include:
- Receptor compartmentalization: TLR4 localization to lipid rafts versus non-raft membrane regions creates signaling platforms with distinct adapter protein recruitment capabilities [31]
- Scaffold protein-mediated complex formation: Intracellular scaffolds organize specific MAPK signaling modules that determine response specificity to different inflammatory stimuli [91]
- Tissue-level spatial gradients: Inflammatory cytokines form concentration gradients across tissue compartments, creating zones of differential activation that guide immune cell positioning and function [92]
Table 1: Strategies for Maintaining Signaling Specificity in Shared Pathways
| Specificity Mechanism | Molecular Components | Outcome Examples |
|---|---|---|
| Temporal encoding | Oscillatory NF-κB, pulsed IL-1β release, SOCS feedback | Distinct gene expression programs from same pathway |
| Spatial compartmentalization | Lipid raft localization, signalosomes, tissue gradients | Differential signaling from shared receptors |
| Receptor combinatoriality | Heterodimeric receptor assemblies, coreceptor usage | Context-specific responses to cytokine families |
| Cross-pathway integration | MAPK-NF-κB crosstalk, metabolic-inflammatory integration | Signal processing that incorporates microenvironmental context |
Experimental Approaches for Deconvoluting Specificity
Single-Cell Analysis of Signaling Heterogeneity
Traditional bulk measurements obscure the heterogeneity of signaling responses across cell populations within complex microenvironments. Single-cell technologies enable researchers to capture the diversity of autocrine and paracrine signaling states.
Methodology: Mass Cytometry (CyTOF) for Phospho-Signaling Analysis
Experimental workflow:
- Prepare single-cell suspensions from tissue microenvironments (e.g., tumor digests, lymph node cells)
- Stimulate with cytokine combinations (e.g., IFN-γ + TNF-α, IL-4 + IL-13) for precise timepoints (0, 5, 15, 30, 60 min)
- Fix cells immediately with 1.6% PFA to preserve phosphorylation states
- Permeabilize (ice-cold methanol) and stain with metal-tagged antibodies against phospho-STAT1 (Y701), phospho-STAT3 (Y705), phospho-STAT5 (Y694), phospho-STAT6 (Y641)
- Acquire data on CyTOF instrument, analyzing 50,000+ cells per condition
- Use dimensionality reduction (t-SNE, UMAP) and clustering (PhenoGraph) to identify signaling states
Key considerations:
- Include a viability marker (cisplatin-based) to exclude dead cells
- Use a reference sample stained with all antibodies for batch normalization
- Spike-in calibration beads for signal normalization across runs
This approach revealed that macrophages in the TME exhibit heterogeneous STAT activation profiles despite uniform cytokine exposure, with distinct subpopulations showing preferential STAT1 versus STAT3 phosphorylation in response to IFN-γ [91].
Live-Cell Imaging of Spatiotemporal Signaling Dynamics
Direct visualization of signaling events in real-time provides unparalleled insight into the dynamic nature of inflammatory signaling.
Methodology: FRET Biosensor Imaging of NF-κB Dynamics
- Biosensor design: Implement a CFP-YFP FRET pair flanking NF-κB's nuclear localization sequence (NLS) and an NF-κB binding domain
Experimental workflow:
- Transduce cells with lentiviral NF-κB FRET biosensor (validated for minimal baseline nuclear localization)
- Seed into microfluidic chambers permitting precise cytokine stimulation and imaging
- Serum-starve cells (4-6 hours) to reduce baseline activation
- Stimulate with TNF-α (10 ng/mL), IL-1β (10 ng/mL), or LPS (100 ng/mL) while acquiring images every 2 minutes for 8 hours
- Calculate nuclear-to-cytoplasmic FRET ratio to quantify NF-κB activation kinetics
- Analyze oscillation frequency, amplitude, and duration using Fourier transform and peak detection algorithms
Technical considerations:
- Maintain environmental control (37°C, 5% CO₂) throughout live imaging
- Include a non-stimulated control to assess baseline oscillations
- Express biosensor at low levels to avoid signaling perturbation
This methodology demonstrated that TNF-α induces damped oscillations in NF-κB nuclear translocation, while IL-1β generates sustained nuclear localization, explaining how different cytokines produce distinct transcriptional outputs through the same pathway [88].
Technical Solutions and Research Reagent Toolkit
Research Reagent Solutions for Signaling Studies
Table 2: Essential Research Reagents for Investigating Signaling Specificity
| Reagent Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| Pathway inhibitors | JAK1/2 inhibitor (ruxolitinib), IKKβ inhibitor (IKK-16), NLRP3 inflammasome inhibitor (MCC950) | Dissecting pathway contributions to specific outputs | Assess selectivity through kinome screening; monitor compensatory signaling |
| Cytokine stimulation | Recombinant human TNF-α, IL-1β, IL-6, IFN-γ, IL-4, IL-13 | Controlled pathway activation | Use carrier proteins (0.1% BSA) to prevent adsorption; verify species specificity |
| Phospho-specific antibodies | Anti-pSTAT1 (Y701), pSTAT3 (Y705), pSTAT5 (Y694), pSTAT6 (Y641), pNF-κB p65 (S536) | Monitoring pathway activation states | Optimize fixation/permeabilization for each epitope; include positive controls |
| Live-cell biosensors | FRET-based NF-κB, kinase activity reporters (AKAR), calcium indicators (GCaMP) | Real-time signaling dynamics | Control for biosensor expression level effects; verify dynamic range |
| Scaffold disruptors | Targeted degradation (dTAG) of AKAPs, JIP proteins | Testing spatial organization requirements | Monitor acute versus chronic disruption effects |
| Mezlocillin | Mezlocillin, CAS:51481-65-3, MF:C21H25N5O8S2, MW:539.6 g/mol | Chemical Reagent | Bench Chemicals |
Computational Modeling Approaches
Mathematical modeling provides a powerful framework for understanding how signal specificity emerges from complex biochemical networks.
Methodology: ODE Modeling of Inflammatory Signaling Crosstalk
Model structure: Develop a system of ordinary differential equations capturing:
- Extracellular cytokine concentrations (LPS, TNF-α, IL-1β)
- Receptor binding and activation kinetics
- Intracellular signaling cascades (NF-κB, MAPK, JAK-STAT)
- Negative feedback regulators (SOCS, IκB, DUSPs)
- Transcriptional and translational dynamics
- Secreted cytokine feedback (autocrine/paracrine loops)
Parameter estimation:
- Extract kinetic parameters from literature (binding constants, catalytic rates)
- Calbrate unknown parameters against experimental data (phospho-flow, ELISA)
- Use global optimization algorithms (particle swarm, genetic algorithms) for parameter fitting
- Validate models with independent data not used in calibration
Model analysis:
- Perform local sensitivity analysis (partial rank correlation coefficient)
- Conduct bifurcation analysis to identify bistable switches
- Simulate knockout/knockdown conditions to predict perturbation outcomes
This approach successfully modeled the biphasic inflammatory response in sepsis, capturing the transition from initial hyperinflammation to subsequent immunosuppression based on feedback dynamics within cytokine networks [88] [31].
Pathway Visualization and Experimental Design
Inflammatory Signaling Network Integration
The following diagram illustrates the core signaling pathways discussed in this guide and their points of crosstalk, which represent both challenges and opportunities for maintaining signal specificity.
Diagram 1: Inflammatory signaling network with crosstalk. This diagram illustrates the core pathways discussed and their integration points, which are critical for understanding specificity challenges. Dashed red lines indicate key crosstalk points that complicate signal specificity.
Experimental Workflow for Specificity Analysis
The following diagram outlines a comprehensive experimental approach for investigating signal specificity in complex microenvironments.
Diagram 2: Experimental workflow for specificity analysis. This integrated approach combines primary cell models, single-cell technologies, live imaging, and computational modeling to deconvolute signaling specificity mechanisms.
Overcoming signal specificity issues in complex microenvironments requires integrated experimental and computational approaches that capture the dynamic, heterogeneous nature of inflammatory signaling. The methodologies outlined in this guide provide a framework for investigating how autocrine and paracrine cytokine signals maintain specificity despite pathway promiscuity.
Future research directions should focus on developing next-generation tools with enhanced temporal and spatial resolution, including:
- Optogenetic cytokine receptors for precise spatiotemporal control of signaling initiation
- Multiplexed biosensors capable of simultaneously monitoring multiple signaling pathways in single cells
- Spatial transcriptomics integration to correlate signaling states with tissue position
- Microfluidic organ-on-chip platforms that preserve native microenvironmental architecture
As these technologies mature, they will enable researchers to progressively decode the logic of inflammatory signaling specificity, facilitating the development of targeted interventions for cancer, autoimmune diseases, and other conditions driven by dysregulated inflammation.
Strategies for Disentangling Convoluted Signaling Mechanisms
Inflammatory cytokines operate within a complex web of autocrine and paracrine signaling that defines the immune response in health and disease. This network is characterized by three fundamental properties that create substantial research challenges: extensive crosstalk between signaling pathways, multiple feedback and feedforward loops, and cell-context specific behaviors [93]. In cancer biology, this complexity is particularly evident, where cytokines can play paradoxical roles—either promoting or inhibiting tumor growth—depending on their concentration, timing, and cellular context [94]. The hepatocyte growth factor (HGF) signaling pathway exemplifies this challenge, where researchers have identified at least 17 potential feedback and crosstalk mechanisms between the PI3K and MAPK pathways alone, creating over 130,000 possible network structures that must be evaluated [93].
Disentangling these convoluted mechanisms requires sophisticated methodologies that combine computational modeling with rigorous experimental validation. The dynamic, non-linear nature of these networks means traditional linear approaches to pathway analysis are insufficient. Furthermore, the spatial and temporal dimensions of autocrine and paracrine signaling add additional layers of complexity, as the same signals can produce different effects depending on their localization and timing [95]. This technical guide outlines comprehensive strategies to address these challenges, providing researchers with a systematic framework for deconstructing and understanding complex signaling networks in inflammatory cytokine research.
Core Analytical Framework: A Hybrid Modeling Approach
Foundational Principles
A hybrid mathematical modeling strategy that combines qualitative and quantitative approaches has emerged as a powerful framework for dissecting complex signaling networks [93]. This methodology capitalizes on the complementary strengths of different modeling paradigms: qualitative models can efficiently handle large combinatorial spaces of potential interactions, while quantitative models precisely capture dynamic signaling behaviors. The implementation of this framework follows a systematic workflow that progressively refines network models from initial literature-based reconstruction to experimentally validated, cell-context specific networks.
The fundamental challenge this approach addresses is the combinatorial explosion of possible network configurations. In the case of HGF signaling, starting with literature-derived knowledge of 17 potential interactions generates 2^17 (131,072) possible network structures [93]. Through iterative modeling and experimental validation, researchers can reduce this complexity to identify the specific network topology operative in their experimental system. This process is particularly valuable for understanding cytokine signaling, where the same ligand-receptor interaction can produce different outcomes in different cellular contexts or physiological states.
Implementation Workflow
Table: Hybrid Modeling Workflow for Signaling Network Reconstruction
| Phase | Key Activities | Outputs | Validation Approaches |
|---|---|---|---|
| Network Reconstruction | Compile literature-derived interactions; Construct initial interaction graphs | Comprehensive list of potential feedback and crosstalk mechanisms; Qualitative network model | Literature mining; Expert curation; Database integration |
| Qualitative Modeling | Apply interaction graphs; Generate testable predictions using dependency matrix concept | Predictions of network behavior under specific perturbations; Inconsistency identification | Comparison of predicted vs. observed qualitative behaviors; Identification of missing interactions |
| Quantitative Modeling | Develop ordinary differential equation (ODE) models; Parameter estimation from time-resolved data | Dynamic network models capable of simulating signal amplitude and duration | Parameter fitting; Sensitivity analysis; Model selection criteria (AIC, BIC) |
| Experimental Validation | Design combinatorial perturbation experiments; Measure pathway activation dynamics | Refined, cell-context specific network structure; Validated model predictions | Immunoblotting with phospho-specific antibodies; High-throughput phosphoproteomics |
Computational Methodologies
Qualitative Modeling with Interaction Graphs
Interaction graphs serve as the foundational qualitative modeling formalism for initial network reconstruction [93]. These graphs represent signaling components as nodes and their interactions as directed edges, providing a computationally tractable approach for managing large combinatorial spaces. The primary strength of interaction graphs lies in their ability to make qualitative predictions about network behavior that can be tested experimentally. When these predictions contradict experimental observations, researchers gain crucial insights into missing or inactive interactions within their network models.
The implementation of interaction graphs begins with comprehensive literature mining to identify all potential interactions within the signaling network of interest. For cytokine signaling networks, this includes documenting all known ligands, receptors, adaptor proteins, signaling intermediates, and transcription factors. The resulting graph represents the universe of possible interactions, which must then be refined through iterative experimentation. A key analytical tool used with interaction graphs is the dependency matrix [93], which systematically maps the relationships between network perturbations and their effects on signaling outputs, enabling researchers to identify inconsistencies between model predictions and experimental data.
Quantitative Dynamic Modeling
Ordinary differential equation (ODE) models provide the quantitative complement to qualitative interaction graphs [93]. These dynamic models excel at capturing essential features of signaling behavior, including signal amplitude, duration, and adaptation dynamics. Where interaction graphs identify which interactions are present, ODE models quantify how these interactions collectively determine system behavior. The development of ODE models requires time-resolved quantitative data, typically obtained through techniques such as immunoblotting with phospho-specific antibodies or high-throughput phosphoproteomics.
Parameter estimation represents a significant challenge in ODE modeling, particularly for large networks. Modern approaches address this through systematic model reduction and hierarchical modeling strategies. For cytokine signaling networks, this often involves developing separate modules for specific subsystems (e.g., JAK-STAT signaling, MAPK activation, PI3K-Akt signaling) that are subsequently integrated into a comprehensive network model. The resulting models enable researchers to simulate the effects of targeted perturbations, including pharmacological inhibition and genetic modifications, providing testable hypotheses about network regulation.
Diagram: Hybrid Modeling Workflow for Network Identification. This framework combines qualitative and quantitative approaches to systematically reduce combinatorial complexity and identify cell-context specific network structures.
Experimental Design and Validation
Combinatorial Perturbation Strategies
Combinatorial perturbation experiments represent the cornerstone of experimental validation for complex signaling networks [93]. Single perturbations often produce minimal effects due to network robustness, while strategically designed combinatorial interventions can reveal critical network structures and dependencies. For cytokine signaling networks, this typically involves combining receptor-level perturbations (e.g., neutralizing antibodies, receptor antagonists) with pathway-specific inhibitors targeting key intracellular signaling nodes. The experimental design must include appropriate controls and dose-response characteristics to ensure interpretable results.
The selection of perturbation agents should be guided by the specific signaling network under investigation. For inflammatory cytokine networks focusing on autocrine and paracrine signaling, essential perturbations include:
- Receptor-blocking antibodies for target cytokines (e.g., anti-IL-6R, anti-TNF-R)
- Ligand-neutralizing antibodies to disrupt autocrine/paracrine loops
- Small molecule inhibitors targeting key signaling kinases (JAK, MAPK, PI3K inhibitors)
- Genetic perturbations (CRISPR, RNAi) targeting adaptor proteins and signaling intermediates
Measurement endpoints should include time-resolved phosphorylation data for key signaling nodes, ideally employing multiplexed approaches such as phospho-flow cytometry or Luminex arrays to capture network-level responses rather than isolated pathway readouts.
Measurement and Analytical Techniques
Time-resolved quantitative data collection is essential for capturing the dynamic features of signaling networks [93]. Experimental designs should include dense timepoint sampling, particularly during the initial signaling response (typically 0-120 minutes post-stimulation), to adequately capture signaling dynamics. Primary measurements should focus on phosphorylation states of key signaling proteins, as these provide direct readouts of pathway activation.
For cytokine signaling studies, essential analytical techniques include:
- Immunoblotting with phospho-specific antibodies for validated targets
- High-throughput phosphoproteomics for unbiased network discovery
- Cytokine bead arrays for measuring autocrine/paracrine ligand production
- Single-cell RNA sequencing to capture heterogeneous cellular responses
- Spatial transcriptomics to contextualize paracrine signaling networks
Data quality controls should include verification of antibody specificity, normalization to housekeeping proteins, and demonstration of linear dynamic range for quantitative assays. For perturbation studies, it is critical to verify inhibitor specificity and efficacy through direct measurement of target phosphorylation.
Research Reagent Solutions
Table: Essential Research Reagents for Signaling Network Analysis
| Reagent Category | Specific Examples | Primary Applications | Key Considerations |
|---|---|---|---|
| Pathway Inhibitors | LY29004 (PI3K inhibitor), Wortmannin (PI3K inhibitor), U0126 (MEK inhibitor), PD 98059 (MEK inhibitor) | Targeted pathway perturbation; Network validation | Specificity validation; Dose-response characterization; Off-target effects assessment |
| Clinical Grade Inhibitors | PX-866 (PI3K inhibitor), CAL-101 (PI3K inhibitor), MK-2206 (Akt inhibitor), PD 0325901 (MEK inhibitor) | Translationally relevant perturbation; Combination therapy modeling | Clinical relevance; Pharmacodynamic properties; Therapeutic index considerations |
| Neutralizing Antibodies | Anti-IL-6R, Anti-TNF-α, Anti-HGF, Anti-VEGF | Disruption of autocrine/paracrine loops; Receptor-level perturbation | Epitope characterization; Neutralization efficacy; Species cross-reactivity |
| Detection Reagents | Phospho-specific antibodies, Luminex bead arrays, Proximity ligation assay reagents | Signal transduction measurement; Network activity mapping | Specificity validation; Dynamic range; Multiplexing capability |
| Engineered Cell Tools | Reporter cell lines, CRISPR-modified cells, Inducible expression systems | Pathway activity monitoring; Specific node perturbation | Functional validation; Stability assessment; Leakiness controls |
Case Study: HGF Signaling Network Analysis
A comprehensive example of this methodology comes from the analysis of HGF-stimulated PI3K and MAPK signaling in primary mouse hepatocytes [93]. This study demonstrated how hybrid modeling could resolve the combinatorial complexity of 131,072 possible network structures to identify the specific topology operative in hepatocytes. The research employed interaction graph modeling to represent potential crosstalk and feedback mechanisms, followed by ODE-based dynamic modeling to quantitatively describe pathway dynamics.
The experimental validation involved systematic combinatorial perturbations using PI3K inhibitors (LY29004, Wortmannin), Akt inhibitor VIII, and MEK inhibitors (PD 98059, U0126) [93]. Time-resolved measurements of Akt and ERK phosphorylation provided the quantitative data necessary for model selection and validation. The resulting network model revealed that the hepatocyte-specific signaling network was robust to single perturbations but highly sensitive to specific combinatorial interventions, demonstrating how this approach can identify optimal targeting strategies for therapeutic intervention.
This case study illustrates several key principles for disentangling convoluted signaling mechanisms: (1) the importance of primary cell systems for physiological relevance, (2) the power of combinatorial perturbations to reveal network properties, and (3) the value of iterative modeling and experimentation to progressively refine network models. The methodologies established in this study provide a template for investigating other complex cytokine signaling networks in inflammatory and neoplastic contexts.
Diagram: HGF Signaling Network Complexity. This network illustrates the multiple feedback and crosstalk mechanisms between PI3K and MAPK pathways that create combinatorial complexity in signaling networks.
Advanced Computational Tools
Next-Generation CCI Analysis
The emergence of single-cell transcriptomics has enabled the development of next-generation computational tools for analyzing cell-cell interactions (CCIs) and cell-cell communication (CCC) [95]. These tools have evolved to address four key aspects of signaling complexity: (1) finer resolution through single-cell analysis, (2) spatial contextualization, (3) deeper characterization of multiple ligand types and intracellular events, and (4) broader scaling across multiple biological conditions. For cytokine researchers focusing on autocrine and paracrine signaling, these tools provide unprecedented capability to deconvolute complex signaling networks.
Core computational tools include CellPhoneDB and CellChat, which establish fundamental methods for inferring CCIs from transcriptomic data [95]. These tools use expression-based formulas to evaluate ligand-receptor interactions between cell types, then employ statistical tests to identify significant interactions. Next-generation tools have expanded these capabilities to address cellular heterogeneity, spatial organization, and complex intracellular signaling events. These advancements are particularly valuable for understanding inflammatory cytokine networks, where the same ligand-receptor pair can mediate different functions in different cellular contexts.
Rule-Based and Data-Driven Strategies
Computational tools for CCI analysis employ two complementary strategies: rule-based approaches that incorporate prior knowledge about signaling behavior, and data-driven approaches that use statistical tests or machine learning to interpret gene expression patterns [95]. Rule-based tools (e.g., SoptSC, NICHES, ICELLNET) implement assumptions about CCI behavior using principles associated with ligand and receptor quantity, providing consistent results due to their formula-based nature. Data-driven tools (e.g., DIALOGUE, MISTy, scITD) can reveal unexpected correlations and hidden patterns within large datasets, even when underlying mechanisms are poorly understood.
For cytokine signaling research, hybrid approaches that combine both strategies often provide the most powerful solutions. These methods leverage the consistency of rule-based approaches while capitalizing on the pattern-discovery capabilities of data-driven methods. The selection of specific tools should be guided by research objectives: hypothesis-driven studies may benefit from rule-based approaches, while discovery-focused research may prioritize data-driven methods. In practice, employing multiple complementary tools provides the most robust insights into complex autocrine and paracrine signaling networks.
Emerging Methodologies and Future Directions
The field of signaling network analysis is rapidly evolving, with several emerging methodologies offering new capabilities for disentangling complex cytokine networks. Spatial transcriptomics technologies enable researchers to contextualize paracrine signaling within tissue architecture, providing crucial spatial constraints for network models [95]. Live-cell biosensors permit real-time monitoring of signaling activity in individual cells, capturing the dynamic heterogeneity of cellular responses. Multiplexed perturbation screens using CRISPR-based approaches enable systematic mapping of genetic interactions within signaling networks.
Future methodological developments will likely focus on multi-omic data integration, combining transcriptomic, proteomic, phosphoproteomic, and metabolomic data to build more comprehensive network models. Mechanistic machine learning approaches that incorporate prior biological knowledge into flexible learning architectures show particular promise for managing the complexity of cytokine signaling networks. As these methodologies mature, they will increasingly enable researchers to move beyond descriptive network models to predictive models that can accurately forecast system behavior under novel perturbations, ultimately accelerating therapeutic development for inflammatory diseases and cancer.
Addressing Drug Resistance in Cytokine-Targeted Therapies
Cytokine-mediated communication, operating through autocrine (self-signaling) and paracrine (neighbor-signaling) pathways, represents a fundamental mechanism by which cells coordinate immune responses and maintain tissue homeostasis [96]. In the context of cancer and inflammatory diseases, these signaling modes are frequently co-opted to promote survival and resistance to therapeutic interventions. The tumor microenvironment (TME) becomes a rich source of cytokine networks that drive pathogenesis, with cytokines including IL-6, TNF-α, TGF-β, and IL-10 playing particularly prominent roles [97]. Understanding the quantitative dynamics of cytokine production and consumption is essential for developing effective therapeutic strategies, as the functional relevance of a cytokine depends on its concentration, spatial distribution, and temporal persistence within tissues [96].
Drug resistance remains a defining challenge in oncology and immunology, limiting the durability of current therapies and contributing to disease relapse and poor patient outcomes [98]. Resistance to cytokine-targeted therapies emerges through complex adaptations involving genetic alterations, epigenetic reprogramming, post-translational modifications, and non-coding RNA networks that cooperate with metabolic reprogramming and tumor microenvironment remodeling to sustain resistant phenotypes [98]. This review integrates recent progress in understanding the molecular, cellular, and ecological foundations of drug resistance, with a particular focus on how autocrine and paracrine cytokine signaling circuits confer treatment resistance across diverse therapeutic contexts.
Mechanisms of Cytokine-Mediated Drug Resistance
Key Cytokines and Their Signaling Pathways in Resistance
Cytokines function by binding to specific receptors on target cells and activating cascades of downstream signaling events that culminate in gene expression programs promoting cell survival, proliferation, and therapeutic evasion [96]. The resistance mechanisms are multifaceted and affect drug metabolism, target expression, DNA repair capacity, and apoptotic threshold [99].
Table 1: Key Cytokines Implicated in Therapeutic Resistance
| Cytokine | Primary Signaling Pathways | Role in Resistance | Experimental EC50 Range (pM) |
|---|---|---|---|
| IL-6 | JAK-STAT3, MAPK, PI3K-AKT | Promotes survival, dedifferentiation, and chemoresistance across multiple cancers | 0.38–38.00 [96] |
| TNF-α | NF-κB, JNK, p38 MAPK | Drives inflammatory programming and resistance to CDK4/6 inhibitors in breast cancer | 2.9–44.0 [96] [97] |
| IL-1β | NF-κB, JNK, p38 MAPK | Enhances stemness properties and therapeutic evasion | 0.008–0.710 [96] |
| IL-8 | p38 MAPK-ERK-AKT, NF-κB, JAK-STAT | Promotes angiogenesis and survival in colorectal cancer | 62.5–312.5 [96] |
| IL-10 | TYK2, JAK1, STAT3, STAT1 | Induces immunosuppressive microenvironment | 8.06–53.80 [96] |
| IL-17 | NF-κB, ERK1/2, p38 MAPK | Shapes immunosuppressive niche in HR+HER2- breast cancer | 129–387 [96] |
Resistance Mechanisms in Specific Cancer Types
The autocrine and paracrine functions of cytokines in promoting resistance manifest differently across cancer types, reflecting tissue-specific signaling contexts and microenvironmental influences:
Breast Cancer: In HR+HER2- breast cancer, autocrine/paracrine IL-6 signaling confers resistance to CDK4/6 inhibitors by favoring STAT3-dependent genetic programs that promote dedifferentiation alongside acquisition of immunoevasive traits [100]. Recent data show circulating IL-6 levels increase at progression compared to baseline in patients receiving CDK4/6 inhibitors, correlating with STAT3 phosphorylation in tumor samples [100]. In triple-negative breast cancer (TNBC), pro-inflammatory cytokines including TNF-α, TGF-β, IL-6, and IL-10 orchestrate a complex network of cellular interactions that remodel the TME into an immunosuppressive niche, compromising antitumor immune responses and contributing to therapeutic resistance [97].
Colorectal Cancer: Inflammation and cytokines are strongly linked to colorectal cancer, with a specific subtype (colitis-associated colorectal cancer) arising from chronic inflammation in inflammatory bowel disease patients [101]. Cytokines including IL-6, TNFα, IFN, IL1, IL8, IL-17, IL-10, and IL-22 significantly impact chemo-resistance mechanisms in colorectal cancer cells [101]. These cytokines modulate ABC transporter expression, enhance DNA repair, inhibit apoptosis, and strengthen cancer stemness through activation of pathways like NF-κB and STAT3 [101].
Ovarian Cancer: Cytokines like IL-6 and IL-11 are associated with complex tumor microenvironments and chemoresistance in ovarian cancer [102]. IL-6 signaling can reprogram and alter T-cell immune responses to tumors, and may serve as a biomarker to distinguish between malignant and non-malignant lesions and predict chemoresistance [102]. The complexity of cytokine networks in ovarian cancer resistance likely necessitates multi-targeted therapeutic approaches rather than single inhibition strategies [102].
Cholangiocarcinoma: This aggressive malignancy exhibits primary chemoresistance mediated by autocrine and paracrine cues released in the tumor microenvironment [99]. Cholangiocytes are constitutively endowed with multiple membrane carriers that mediate both uptake and extrusion of therapeutic compounds, including ABC family transporters that regulate drug extrusion against concentration gradients [99]. Additionally, intracellular enzymatic functions promoting chemoresistance include either decreased activation of pro-drug compounds or enhanced inactivation of active metabolites [99].
Experimental Approaches for Studying Cytokine-Mediated Resistance
Quantitative Analysis of Cytokine Signaling Dynamics
A systematic understanding of the quantitative rules that govern cytokine-mediated cell-to-cell communication is essential for deciphering resistance mechanisms [96]. The accumulation of a soluble cytokine in tissues results from two fundamental biochemical and cellular events: production and consumption. Mathematical modeling of these dynamics can predict whether a given cytokine will function primarily through autocrine or paracrine mechanisms in specific pathological contexts [96].
Advanced methodologies for quantifying cytokine signaling include:
- Cytometric bead arrays for multiplex cytokine quantification in conditioned media [103]
- Single-cell RNA sequencing to resolve cellular heterogeneity in cytokine production and response [96]
- Phospho-flow cytometry to measure signaling pathway activation in complex cell mixtures
- Microfluidic devices to control spatial organization and analyze paracrine communication
In Vitro and In Vivo Models for Resistance Studies
Table 2: Experimental Model Systems for Studying Cytokine-Mediated Resistance
| Model System | Applications | Key Readouts | Considerations |
|---|---|---|---|
| 3D Co-culture Systems | Studying paracrine signaling between cancer cells and stromal components | Cytokine secretion profiles, drug penetration, spatial organization | Better recapitulates TME than 2D cultures |
| Patient-Derived Xenografts (PDXs) | Evaluating therapeutic responses and resistance mechanisms in human tumors | Tumor growth kinetics, cytokine levels, phospho-signaling | Maintains tumor heterogeneity but lacks functional immune system |
| Genetically Engineered Mouse Models | Investigating cytokine function in intact immune system | Immune cell infiltration, metastasis, autocrine vs. paracrine effects | Species-specific cytokine differences may limit translation |
| Organoid Cultures | High-throughput drug screening in patient-specific contexts | Viability, differentiation status, cytokine secretion | Variable stromal component depending on culture method |
For example, in a recent study investigating IL-6 mediated resistance to CDK4/6 inhibitors in HR+HER2- breast cancer, researchers employed multiple model systems: (1) in vitro cultures of resistant MCF7 or T47D cells for IL-6 depletion experiments; (2) long-term resistance development models where cells were exposed to palbociclib over extended periods; and (3) PDX models established from human HR+HER2- metastatic breast cancers relapsing early versus late after CDK4/6 inhibitor initiation [100]. This multi-faceted approach enabled both mechanistic insights and therapeutic validation.
Figure 1: Cytokine Signaling Networks in Therapeutic Resistance. Cytokines activate intracellular signaling pathways that drive expression of genes promoting multiple resistance mechanisms. These mechanisms reinforce cytokine production through autocrine and paracrine loops, creating self-sustaining resistance circuits.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Investigating Cytokine-Mediated Resistance
| Reagent Category | Specific Examples | Research Applications | Key Considerations |
|---|---|---|---|
| Cytokine Inhibitors | Tocilizumab (IL-6R), TTI-101 (STAT3), Infliximab (TNF-α) | Pathway inhibition studies, combination therapies | Specificity, pharmacokinetics, tissue penetration |
| Neutralizing Antibodies | Anti-IL-6, Anti-TNF-α, Anti-IL-1β | Blocking autocrine/paracrine signaling, mechanistic studies | Epitope recognition, species cross-reactivity |
| Recombinant Cytokines | rhIL-6, rhTNF-α, rhIL-1β | Pathway activation, rescue experiments | Bioactivity, endotoxin levels, formulation |
| Signal Transduction Inhibitors | JAK inhibitors (Ruxolitinib), IKK inhibitors, p38 MAPK inhibitors | Dissecting signaling hierarchies | Off-target effects, compensatory pathways |
| Gene Editing Tools | CRISPR/Cas9, shRNA vectors | Knockout/knockdown of cytokine genes or receptors | Efficiency, delivery method, complete vs partial knockdown |
| Cytokine Detection Assays | ELISA, Luminex, ELISpot, Cytometric bead array | Quantifying cytokine production and consumption | Sensitivity, dynamic range, multiplex capability |
Detailed Experimental Protocols
Protocol 1: Assessing Autocrine versus Paracrine Signaling in Vitro
Background: Determining whether cytokine signaling occurs primarily through autocrine (same cell) versus paracrine (neighboring cell) mechanisms is essential for understanding resistance dynamics and designing appropriate interventions [3] [104].
Materials:
- Transwell inserts (0.4μm and 8.0μm pore sizes)
- Conditioned media collection tubes
- Cytokine-specific neutralizing antibodies
- Cytokine detection ELISA or multiplex array
- Target cells with CRISPR-mediated cytokine receptor knockout
Procedure:
- Culture Setup: Plate cytokine-producing cells in the lower chamber of a Transwell system.
- Conditioned Media Preparation: Culture cells for 24-48 hours, then collect and filter-sterilize conditioned media.
- Signaling Inhibition: Apply cytokine-specific neutralizing antibodies to either producer or receiver cells.
- Spatial Separation Experiments:
- For paracrine signaling assessment: Place responder cells in upper chamber with 0.4μm pores (allows cytokine passage but not cells)
- For autocrine signaling assessment: Use receptor-deficient producer cells to eliminate autocrine signaling
- Response Measurement: Quantify pathway activation (e.g., phospho-STAT3/STAT5) after 24 hours using Western blot or phospho-flow cytometry.
- Data Analysis: Compare signaling in:
- Direct co-culture (autocrine + paracrine)
- Transwell separation (paracrine only)
- Neutralizing antibody conditions (autocrine only when paracrine blocked)
Interpretation: This experimental approach enables dissection of the relative contributions of autocrine versus paracrine signaling to therapeutic resistance, informing whether cell-autonomous versus microenvironment-targeting strategies would be most effective.
Protocol 2: Evaluating Cytokine-Mediated Resistance in Patient-Derived Xenografts
Background: PDX models maintain tumor heterogeneity and microenvironmental interactions more effectively than conventional cell line xenografts, providing a clinically relevant system for studying cytokine-mediated resistance [100].
Materials:
- Immunodeficient mice (NSG, NOG, or similar)
- Patient-derived tumor tissue
- Cytokine-targeting therapeutic agents
- Blood collection supplies for serial monitoring
- Multiplex cytokine detection platform
Procedure:
- PDX Establishment: Implant patient-derived tumor fragments subcutaneously or orthotopically into immunodeficient mice.
- Treatment Cohorts: Randomize mice into control, standard therapy, cytokine-targeting agent, and combination groups once tumors reach 150-200mm³.
- Serial Monitoring:
- Measure tumor dimensions 3 times weekly
- Collect blood samples weekly for cytokine level analysis
- Perform small biopsy specimens at predetermined timepoints for phospho-signaling analysis
- Endpoint Analysis:
- Process tumors for IHC staining of cytokine receptors, phospho-proteins, and proliferation markers
- Isolate cells for single-cell RNA sequencing to characterize heterogeneity
- Bank tumor tissues for subsequent organoid generation
- Validation Experiments: Test insights from PDX models in organoid cultures with genetic manipulation of cytokine signaling components.
Interpretation: PDX models enable evaluation of cytokine dynamics throughout therapeutic response and resistance development, providing insights into temporal regulation of autocrine/paracrine signaling and predictive biomarkers for treatment success.
Figure 2: Experimental Workflow for Investigating Cytokine-Mediated Resistance. A systematic approach combining multiple model systems enables comprehensive understanding of cytokine-driven resistance mechanisms and translation to clinical strategies.
Emerging Therapeutic Strategies to Overcome Cytokine-Mediated Resistance
Targeted Interventions Against Cytokine Signaling Networks
Advances in understanding cytokine networks in therapeutic resistance have revealed several promising intervention strategies:
Combination Targeting: Simultaneous inhibition of cytokine production and signaling pathways shows enhanced efficacy. For example, in HR+HER2- breast cancer resistant to CDK4/6 inhibitors, combining the STAT3 inhibitor TTI-101 with palbociclib demonstrated synergistic effects in PDX models of late progression [100]. Similar results were obtained with the FDA-approved IL-6 inhibitor tocilizumab, pointing to the IL-6/STAT3 axis as a potential target for restoring sensitivity [100].
Microenvironment Reprogramming: Rather than directly targeting cancer cells, approaches that modify the tumor microenvironment to reduce pro-survival cytokine signaling show promise. This includes repolarizing tumor-associated macrophages, targeting cancer-associated fibroblasts, and modulating extracellular matrix composition to reduce cytokine retention and signaling [98] [97].
Vertical Pathway Inhibition: Concurrent targeting of multiple nodes in a cytokine signaling pathway can prevent compensatory activation and overcome resistance. For instance, in TNBC, combined inhibition of cytokine production (e.g., IL-6, TNF-α) and their downstream effectors (e.g., STAT3, NF-κB) may provide more durable responses than single-agent approaches [97].
Sequential Therapy Strategies: Based on the temporal evolution of resistance mechanisms, treatment sequencing that anticipates and preempts cytokine-mediated resistance may improve outcomes. For example, in colorectal cancer, early introduction of cytokine pathway inhibitors during chemotherapy may prevent the establishment of resistant niches [101].
Biomarker Development for Personalized Resistance Management
The heterogeneity of cytokine-mediated resistance mechanisms necessitates biomarker-driven treatment approaches:
Circulating Cytokine Profiles: Longitudinal monitoring of circulating cytokines may provide early indicators of emerging resistance. In HR+HER2- breast cancer, increased plasma IL-6 levels at progression on CDK4/6 inhibitors suggest potential utility as a dynamic biomarker [100].
Tissue-Based Signaling Signatures: Multiplexed immunohistochemistry or digital spatial profiling of cytokine signaling pathway activation (e.g., phospho-STAT3, NF-κB localization) in tumor biopsies can identify dominant resistance pathways for targeted intervention [97].
Single-Cell Transcriptomic Classifiers: Resolution of cellular heterogeneity in cytokine production and response using single-cell RNA sequencing enables identification of resistant subpopulations and their characteristic signaling dependencies [96].
The pervasive role of autocrine and paracrine cytokine signaling in therapeutic resistance represents both a fundamental challenge and a promising opportunity in cancer therapeutics. Resistance emerges not merely through cell-autonomous genetic adaptations but through complex, dynamically evolving networks of communication between cancer cells and their microenvironment. Successful targeting of these resistance mechanisms will require sophisticated understanding of cytokine dynamics, spatial organization, and temporal evolution throughout the therapeutic journey.
Future progress will depend on several key advances: (1) development of more sophisticated experimental models that capture the complexity of cytokine networks in human tumors; (2) advanced computational approaches to model and predict resistance dynamics; (3) biomarker strategies to match patients with appropriate cytokine-targeting approaches; and (4) clinical trial designs that incorporate longitudinal monitoring of cytokine signaling and adaptive treatment interventions. By addressing cytokine-mediated resistance through integrated experimental and computational approaches, the field can overcome current limitations and achieve more durable therapeutic responses for cancer patients.
Optimizing Culture Conditions to Maintain Physiological Relevance
The fidelity of in vitro research in immunology and drug development is fundamentally constrained by the physiological relevance of cell culture systems. This whitepaper provides a technical guide for optimizing culture conditions, with a specific focus on preserving the nuanced dynamics of autocrine and paracrine signaling of inflammatory cytokines. We detail refined culture methodologies, quantitative assessment protocols, and advanced visualization techniques essential for researchers aiming to bridge the gap between traditional cell culture and in vivo physiology. By implementing these strategies, scientists can significantly enhance the predictive value of their experimental models in areas such as innate immunity, inflammatory disease modeling, and therapeutic agent development.
Cell culture remains the primary platform for modeling human diseases and biological processes for research purposes. However, standard in vitro techniques often fail to adequately reflect physiological conditions, raising concerns about the translational potential of acquired data [105]. The communication between cells—through direct contact or at a distance via ligand–receptor interactions—is a cornerstone of multicellular existence, influencing growth, development, differentiation, and physiological regulation [11]. These interactions are particularly critical in the study of inflammatory cytokines, such as Tumor Necrosis Factor (TNF), which coordinates innate and adaptive immune responses by functioning in an autocrine manner (affecting the same cell) or a paracrine manner (affecting neighboring cells) [3]. Deciphering these intercellular communication networks is therefore essential for understanding cell differentiation, development, and metabolism, and for discovering new therapeutic targets [11]. This guide outlines a systematic approach to refining cell culture conditions to increase their modeling adequacy, thereby ensuring that critical signaling pathways, like those mediated by TNF, are accurately represented in experimental models.
Core Principles of Physiological Media and Culture Environment
Traditional culture media often rely on non-physiological components, such as high concentrations of fetal calf serum and supraphysiological nutrient levels, which can obscure authentic cell signaling. Transitioning to refined, physiologically relevant media is a fundamental first step.
Composition of Refined Physiological Media
Refined physiological media are formulated to mimic the metabolite and nutrient composition of human blood plasma. This involves adjusting glucose levels, amino acids, vitamins, and hormones to concentrations found in vivo. The use of defined, human-derived supplements is favored over fetal calf serum to reduce batch-to-batch variability and provide a more human-relevant signaling environment [105]. The goal is to create a culture condition that forces cells to rely on physiological metabolic pathways, thereby uncovering oncogene-dependent metabolic signatures and other disease-relevant phenotypes that may be masked in standard media [105].
Table 1: Key Components of Physiologically Relevant Media
| Component Category | Physiological Consideration | Impact on Cell Signaling |
|---|---|---|
| Energy Substrates | Glucose at human plasma levels (~5 mM) | Prevents artificial hyperglycemia-induced signaling; promotes oxidative phosphorylation. |
| Serum Replacement | Defined growth factor mixes, human platelet lysates | Eliminates confounding animal-derived cytokines; provides human-specific ligand context. |
| Inorganic Salts & Buffers | Physiological oxygen (1-10%), bicarbonate buffer | Recapitulates tissue-level hypoxia and pH; influences HIF signaling and cytokine production. |
Advanced Culture Models: 3D Spheroids
Moving beyond two-dimensional monolayers to three-dimensional (3D) culture models is crucial for maintaining physiological relevance. Spheroid cultures restore cell-cell and cell-matrix interactions that are absent in 2D systems, creating diffusion gradients for oxygen, nutrients, and metabolites that more closely mimic a tissue microenvironment [105]. These gradients are instrumental in establishing autocrine and paracrine signaling niches. For instance, a cytokine like TNF secreted by a macrophage in the core of a spheroid will have a vastly different effect profile compared to its uniform distribution in a 2D monolayer, thereby replicating the spatial dynamics of an inflammatory focus in vivo.
Diagram 1: 2D vs. 3D culture models for signaling studies.
Autocrine and Paracrine Signaling in Inflammation Research
The network dynamics of cytokine signaling are complex and stimulus-specific. A systems biology approach, combining experimental data with computational models, has been instrumental in revealing that the autocrine and paracrine functions of a key cytokine like TNF are determined by the underlying signaling network dynamics of its production and the subsequent NFκB response [3].
TNF as a Model Inflammatory Cytokine
TNF is a hallmark of the inflammatory response to pathogen exposure. Its production in macrophages is controlled by Toll-like Receptors (TLRs), which engage adaptor proteins MyD88 and TRIF. These adaptors mediate a multi-tiered control of TNF production, regulating its mRNA synthesis, half-life, translation, and secretion [3]. Critically, research has shown that the role of TNF signaling is not universal; it depends on the initial stimulus. For example, in response to lipopolysaccharide (LPS), TNF does not have a significant autocrine function in amplifying the NFκB response in the producing cell but plays a potent paracrine role in neighboring cells. In contrast, in response to CpG DNA, autocrine TNF extends the duration of NFκB activity and shapes subsequent gene expression programs [3]. This highlights the critical importance of context, which is dictated by the culture environment.
Diagram 2: Stimulus-specific TNF autocrine and paracrine signaling.
Quantitative Assessment of Cytokine Signaling
To accurately capture these dynamics, robust quantitative methods are required. Enzyme-Linked Immunosorbent Assay (ELISA) is a standard technique for measuring secreted TNF protein in supernatant. However, a complete picture requires analysis at multiple levels:
- Nascent mRNA Transcription: Measured via intron-specific probes in RT-PCR, revealing immediate transcriptional responses [3].
- Mature mRNA Stability: Assessed through half-life measurements, often controlled by p38 MAPK/MK2 pathways downstream of TLRs [3].
- Protein Secretion: Quantified by ELISA, which represents the final, functional output of the production cascade.
Table 2: Quantitative Profiling of TNF Production in BMDMs Stimulated with LPS
| Time Post-Stimulation | TNF Secreted Protein (ELISA) | Mature TNF mRNA | Nascent TNF Transcript |
|---|---|---|---|
| 1 hour | 350 ± 45 pg/mL | 105 ± 12 AU | 25 ± 5 AU |
| 2 hours | 1250 ± 180 pg/mL | 220 ± 25 AU | 32 ± 6 AU |
| 4 hours | 850 ± 95 pg/mL | 150 ± 18 AU | 15 ± 3 AU |
| Key Regulatory Insight | TRIF & MyD88 dependent [3] | MyD88 dominant at early times [3] | MyD88- NFκB axis controlled [3] |
Methodologies for Analyzing Cell Communication
Modern technologies enable researchers to deconstruct the complexity of cell-cell communication with unprecedented depth.
High-Dimensional Single-Cell Analysis
Mass cytometry, or CyTOF (cytometry by time-of-flight), allows for the simultaneous quantification of over 30 cellular parameters at the single-cell level [106]. This technology, when integrated with high-dimensional analysis algorithms, can reveal extraordinary cellular diversity and heterogeneity within a population, such as identifying distinct immune cell subtypes participating in a paracrine dialogue. Key analysis algorithms include:
- viSNE: A dimensionality reduction technique that maps high-dimensional data into two dimensions for visualization.
- PhenoGraph: An algorithm that automatically identifies communities of cells (clusters) based on their phenotypic similarity [106]. These tools shift analysis away from user-defined, Boolean gating strategies to automated, unbiased identification of cell clusters and phenotypes, providing a systems-level view of cellular responses [106].
Computational Reconstruction of Interaction Networks
Ligand-receptor interaction (LRI) analysis based on single-cell RNA sequencing (scRNA-Seq) data has become a standard practice for inferring intercellular communication. Computational tools leverage curated databases of ligand-receptor pairs to predict active communication channels between different cell types in a tissue [11]. These inferred networks can be visualized and further analyzed using network visualization software like Cytoscape [107]. Cytoscape allows users to map quantitative data (e.g., expression levels) onto visual properties of the network (node color, size, edge thickness), enabling an intuitive understanding of complex signaling networks [107] [108]. For instance, nodes (cells) can be colored based on their TNF expression, and edges (predicted interactions) can be weighted based on the combined ligand-receptor expression score.
Experimental Protocols
Protocol: Establishing Murine Bone Marrow-Derived Macrophage (BMDM) Spheroids for TNF Signaling Studies
This protocol outlines the process of generating 3D macrophage spheroids to study autocrine/paracrine TNF signaling in response to TLR agonists.
Key Research Reagent Solutions:
- Bone Marrow-Derived Macrophages (BMDMs): Primary cells isolated from murine bone marrow and differentiated with M-CSF for 7 days to yield mature macrophages.
- Physiological Culture Media: Base DMEM/F12, adjusted to 5 mM glucose, supplemented with 5% human platelet lysate, and defined growth factors.
- Spheroid Formation Matrix: A commercially available hydrogel or 1.35 mg/mL Matrigel in Hank's Buffered Salt Solution (HBSS) to support 3D structure [106].
- TLR Agonists: Ultrapure LPS (TLR4 agonist) and CpG DNA (TLR9 agonist) to provide specific inflammatory stimuli.
Methodology:
- BMDM Differentiation: Isolate progenitor cells from C57BL/6J mouse femurs and tibias. Differentiate in standard culture dishes with complete media containing 20 ng/mL M-CSF for 7 days.
- Harvest and Resuspend: Detach differentiated BMDMs using gentle cell dissociation reagent. Resuspend the cell pellet at a density of 1×10^5 cells/mL in the refined physiological media.
- Spheroid Formation:
- Mix the cell suspension with the spheroid formation matrix (e.g., Matrigel) on ice.
- Plate 100 µL drops onto a pre-changed culture dish lid. Invert the lid and place over the dish containing PBS to create a hanging drop culture.
- Culture for 48-72 hours to allow spheroid aggregation.
- Stimulation and Analysis:
- Carefully transfer formed spheroids to a low-adhesion 96-well plate.
- Stimulate with LPS (100 ng/mL) or CpG DNA (1 µM) for defined time periods (1, 2, 4, 8 hours).
- Harvest supernatant for TNF ELISA.
- Collect spheroids for RNA extraction and qPCR analysis of TNF and NFκB-target genes.
Protocol: High-Dimensional Analysis of Macrophage Heterogeneity via Mass Cytometry
This protocol details sample processing and staining for CyTOF analysis to dissect macrophage heterogeneity and signaling states.
Key Research Reagent Solutions:
- Metal-Conjugated Antibodies: Antibodies targeting surface (CD11b, F4/80) and intracellular markers (phospho-p38, phospho-NFκB p65), conjugated to rare earth metals.
- Cell Viability Stain: Cisplatin (Fluidigm) to label non-viable cells for exclusion during analysis.
- Intercalator: Cell-ID Intercalator-Ir (Fluidigm) to label DNA and identify nucleated cells.
- Fixation and Permeabilization Buffers: FoxP3 Fix/Perm buffer (eBioscience) or similar for intracellular antigen staining.
Methodology:
- Cell Processing: Following stimulation, dissociate spheroids using collagenase D (Roche) for 1 hour at 37°C. Form a single-cell suspension and perform red blood cell lysis if necessary.
- Cell Staining:
- Viability Staining: Resuspend cells in cisplatin solution for 5 minutes. Quench with cell culture media.
- Surface Staining: Incubate with Fc receptor blocking antibody (2.4G2), then with the metal-conjugated surface antibody panel for 30 minutes (15 mins at 37°C, 15 mins at 22°C).
- Fixation and Permeabilization: Fix and permeabilize cells using the FoxP3 buffer kit.
- Intracellular Staining: Incubate with metal-conjugated intracellular antibodies (e.g., anti-phospho-proteins) for 2 hours at 4°C.
- Data Acquisition and Normalization:
- Resuspend cells in intercalator solution. Acquire data on a Helios mass cytometer with normalization beads spiked into each sample.
- Normalize data using software like Normalizer (Nolan Lab) to correct for instrument drift.
- Data Analysis:
- Export normalized, singlet, live cell data.
- Use a combination of algorithms (e.g., PhenoGraph in R for clustering, followed by viSNE in Cytobank for visualization) to identify distinct macrophage subpopulations and their activated signaling states [106].
The Scientist's Toolkit
Table 3: Essential Research Reagents for Physiological Signaling Studies
| Reagent / Tool | Function / Purpose | Technical Considerations |
|---|---|---|
| Defined Physiological Media | Mimics human plasma composition; reduces serum-derived confounding signals. | Formulate in-house or use commercial blends; critical for metabolic and signaling studies. |
| 3D Culture Matrices (e.g., Matrigel) | Provides a scaffold for spheroid formation; enables cell-matrix interactions. | Lot variability is a concern; use consistent batches for an experiment [106]. |
| Ultrapure TLR Agonists | Specific activation of pattern recognition receptors to induce defined inflammatory responses. | Essential for studying MyD88 vs. TRIF pathway-specific effects on TNF production [3]. |
| Mass Cytometry (CyTOF) | High-dimensional, single-cell analysis of phenotype and signaling states. | Requires specialized instrumentation and metal-conjugated antibodies [106]. |
| Computational Analysis Algorithms (PhenoGraph, viSNE) | Unbiased identification and visualization of cell populations from high-dimensional data. | Choice of algorithm can reveal complementary biological insights [106]. |
| Network Visualization Software (Cytoscape) | Reconstructs and visualizes ligand-receptor interaction networks from scRNA-seq data. | Use built-in style functions to map data (e.g., expression) to visual properties (color, size) [107] [108]. |
Troubleshooting Problems in Signal Amplification and Detection
Signal amplification and detection are fundamental processes in biological research, particularly in the study of complex cell-to-cell communication systems such as those mediated by inflammatory cytokines. Within the broader context of autocrine and paracrine signaling research, accurate signal measurement is frequently compromised by technical challenges that can obscure biological reality. Inflammatory cytokines, including tumor necrosis factor (TNF), interleukin-1β (IL-1β), and various interferons, coordinate immune responses through intricate networks where a single cytokine can elicit dramatically different responses depending on the cellular source, target, and timing [3] [109]. The pleiotropic nature of these signaling molecules, combined with the potential for redundancy in their actions, creates a system where signal amplification and detection problems can lead to fundamentally flawed interpretations of cytokine biology [22] [109].
This technical guide addresses the core challenges in accurately measuring and interpreting cytokine-mediated signaling events, with a specific focus on autocrine and paracrine loops in inflammatory contexts. We provide a systematic framework for troubleshooting common experimental pitfalls, validated through case studies from recent research that has successfully navigated these complexities using iterative systems biology approaches and single-cell resolution technologies [3] [109].
Core Principles of Cytokine Signaling in Inflammation
Autocrine and Paracrine Signaling Dynamics
Inflammatory cytokines function through distinct spatial signaling modalities. Autocrine signaling occurs when a cytokine acts on the same cell that produced it, potentially amplifying the initial inflammatory signal. Paracrine signaling involves cytokine communication between neighboring cells, enabling the spatial propagation of inflammatory responses [22]. The functional consequences of these signaling modes are context-dependent, as demonstrated by the finding that TNF exhibits potent paracrine functions but surprisingly lacks autocrine amplification effects in response to lipopolysaccharide (LPS) in macrophages [3].
The dynamics of cytokine production and consumption fundamentally govern signal detection challenges. The accumulation of any soluble cytokine in tissues or experimental systems results from the balance between production rates by secreting cells and consumption rates by target cells expressing appropriate receptors [96]. This relationship can be represented as:
Accumulation = Production - Consumption
In experimental systems, failures to account for consumption effects can lead to significant underestimation of true production rates, particularly for cytokines with rapid turnover.
Quantitative Parameters of Major Inflammatory Cytokines
Table 1: Key biochemical properties of inflammatory cytokines relevant to signal detection
| Cytokine | Molecular Mass (kDa) | Signaling Pathways | EC50 Range (pM) | Primary Producing Cells | Primary Target Cells |
|---|---|---|---|---|---|
| TNF | 17 | NF-κB, JNK, p38 MAPK | 2.9-44.0 [96] | Macrophages, T cells, NK cells | Macrophages, T cells, monocytes [96] |
| IL-1β | 17.5 | NF-κB, JNK, p38 MAPK | 0.008-0.710 [96] | Monocytes, epithelial cells | Macrophages [96] |
| IL-6 | 21 | JAK1, STAT3, STAT1, STAT5 | 0.38-38.00 [96] | T cells, macrophages, fibroblasts | B cells, T cells, thymocytes [96] |
| IFNγ | 17 | JAK1, JAK2, STAT1 | 2.9-44.0 [96] | T cells, NK cells, NKT cells | T cells, monocytes, macrophages [96] |
| IL-18 | 18 | NF-κB, JNK, p38 MAPK | 83.33-500.00 [96] | Macrophages | T cells, NK cells [96] |
Common Signal Amplification and Detection Problems
Autocrine Signaling Artifacts and Masking
A fundamental challenge in cytokine research is the accurate detection of autocrine signaling events, which are frequently masked by experimental conditions or overshadowed by paracrine effects. Studies of TNF production in macrophages have revealed that autocrine functions are stimulus-specific, with TNF failing to amplify NFκB responses in an autocrine manner after LPS stimulation despite robust production, while demonstrating clear autocrine effects in response to CpG DNA [3]. This stimulus-specificity underscores the importance of network dynamics in determining autocrine functionality, where the relative timing and magnitude of signaling events through adaptor proteins like MyD88 and TRIF determine whether autocrine loops become established [3].
The "consumption problem" represents another key challenge in detection, where rapid cytokine uptake by target cells prevents accumulation in the extracellular space. This effect is particularly pronounced for cytokines with high-affinity receptors or those produced in low quantities. Recent quantitative analyses have demonstrated that cytokine consumption follows saturable kinetics, with detection thresholds being strongly influenced by the density of target cells in the experimental system [96].
Signal Specificity and Cross-Talk Issues
The pleiotropy and redundancy inherent to cytokine networks create significant challenges for attributing specific effects to individual cytokines. Single-cell transcriptomic analyses have revealed that most cytokines induce highly cell-type-specific responses, with the same cytokine producing dramatically different gene expression patterns across immune cell types [109]. For example, IL-1β induces distinct gene programs in neutrophils, migratory dendritic cells, and T regulatory cells, potentially leading to misinterpretation if cellular heterogeneity is not accounted for [109].
Secondary signaling effects present another detection challenge, where the cytokine being measured actually functions to induce production of other mediators. Studies of IL-2, IL-12, IL-15, and IL-18 have demonstrated that these cytokines can induce IFNγ production in NK cells, which subsequently activates bystander cell populations, creating the false appearance of direct action on these secondary targets [109].
Troubleshooting Methodologies
Experimental Design Solutions
Controlled Genetic Perturbation Models
Genetic knockout systems provide powerful tools for dissecting complex cytokine networks. Studies of TNF regulation have successfully employed myd88â»â„â» and trifâ»â„â» bone marrow-derived macrophages (BMDMs) to delineate adaptor-specific contributions to TNF production [3]. The experimental workflow involves:
- Generate knockout cells: Create genetic knockouts of specific signaling components (e.g., MyD88, TRIF) using CRISPR/Cas9 or derived from knockout animals.
- Stimulate with specific agonists: Treat wild-type and knockout cells with TLR agonists such as LPS (MyD88+TRIF) or CpG DNA (MyD88-only).
- Measure multi-level responses: Quantify TNF production at transcriptional (nascent RNA), translational (secreted protein), and functional (NFκB activation) levels.
- Incorporate receptor blockade: Use neutralizing antibodies against cytokines (e.g., anti-TNF) to distinguish autocrine versus paracrine effects.
Table 2: Key research reagents for cytokine signal detection studies
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| TLR Agonists | LPS (TLR4), CpG DNA (TLR9) | Selective pathway activation to probe adaptor-specific signaling [3] |
| Neutralizing Antibodies | Anti-TNF, Anti-IL-1β, Anti-IFNγ | Block specific cytokine actions to dissect autocrine/paracrine functions [3] |
| Genetic Models | myd88â»â„â», trifâ»â„â» BMDMs | Disrupt specific signaling branches to determine component necessity [3] |
| Signaling Inhibitors | IKK inhibitors, p38 MAPK inhibitors | Block specific intracellular signaling pathways to map transduction events |
| Cytokine Detection | ELISA, Single-cell RNA-seq, Phospho-flow cytometry | Measure cytokine production at protein, transcriptional, and signaling levels [3] [109] |
Quantitative and Computational Approaches
Systems Biology Modeling
Iterative mathematical modeling combined with experimental validation provides a powerful framework for troubleshooting signal detection problems. The systems biology approach applied to TNF regulation involves:
- Develop modular mathematical models: Create separate models for TNF mRNA synthesis, mRNA half-life, translation, and protein secretion, then link these to established models of TLR, TNFR, and NFκB signaling [3].
- Parameterize with kinetic data: Use quantitative time-course measurements of TNF production at multiple regulatory levels (transcription, translation, secretion) in wild-type and knockout cells.
- Validate predictions experimentally: Test model predictions (e.g., absence of autocrine function in LPS response) using specific experimental perturbations [3].
Single-Cell Resolution Technologies
Bulk measurement approaches mask cell-to-cell variability and obscure detection of autocrine signaling events. Recent advances in single-cell technologies enable unprecedented resolution of cytokine responses:
- Single-cell RNA sequencing (scRNA-seq): The "Immune Dictionary" approach systematically profiled transcriptomic responses to 86 cytokines across 17 immune cell types, revealing extensive cell-type-specific responses that would be masked in bulk measurements [109].
- High-dimensional mass cytometry: Simultaneously measure multiple signaling pathways, cytokine production, and surface markers at single-cell resolution to deconvolve complex signaling networks.
- Microfluidic devices: Use compartmentalized systems to isolate individual cells or defined cell populations while controlling cytokine exposure.
Case Study: Resolving TNF Signaling Controversies
The application of these troubleshooting methodologies has resolved longstanding controversies regarding TNF's autocrine functions. Earlier studies presented conflicting evidence about whether TNF amplifies NFκB responses in an autocrine manner, with some reports supporting this model and others contradicting it [3]. Through systematic analysis using the integrated approaches described above, researchers determined that these apparent contradictions stemmed from stimulus-specific network dynamics rather than technical artifacts.
Specifically, the combination of mathematical modeling with targeted experiments in genetic knockout models revealed that:
- LPS stimulation activates both MyD88 and TRIF pathways, producing strong TNF secretion but without establishing autocrine amplification
- CpG DNA stimulation activates only MyD88, resulting in autocrine TNF signaling that extends NFκB duration
- The differential behavior stems from the relative timing and magnitude of signaling events through the distinct adaptor proteins [3]
This case study illustrates how applying rigorous troubleshooting methodologies can transform apparent contradictions into mechanistic understanding of network regulation.
Future Directions and Emerging Solutions
Emerging technologies are providing new approaches for addressing persistent challenges in cytokine signal detection. The development of cytokine secretion assays with single-cell resolution, such as time-resolved capture systems, enables direct measurement of autocrine signaling events without disruption of native cellular contexts. Spatial transcriptomics technologies now permit mapping cytokine production and response within tissue architecture, resolving paracrine signaling networks with unprecedented spatial resolution.
Computational methods continue to advance, with multi-scale modeling frameworks now capable of integrating intracellular signaling dynamics with tissue-level cytokine diffusion and consumption. These models are particularly valuable for predicting how pharmacological interventions might alter autocrine/paracrine balance in inflammatory diseases. Finally, the ongoing expansion of reference datasets like the Immune Dictionary provides essential benchmarks for distinguishing true biological effects from technical artifacts in cytokine signaling studies [109].
Accurate signal amplification and detection in autocrine and paracrine cytokine research requires integrated methodological approaches that address the fundamental complexities of these signaling systems. The troubleshooting framework presented here—combining genetic perturbations, quantitative measurements, computational modeling, and single-cell technologies—provides a systematic path for overcoming common detection problems. As cytokine-targeted therapies continue to emerge for inflammatory diseases, cancer, and immune disorders, the rigorous application of these principles will be essential for developing accurate mechanistic understanding and effective therapeutic strategies.
Managing Cytokine Pleiotropy and Redundancy in Experimental Design
Cytokines exhibit inherent pleiotropy (multiple biological actions) and redundancy (shared biological actions), presenting significant challenges in experimental immunology and therapeutic development [110]. These properties are deeply embedded within the context of autocrine and paracrine signaling networks that coordinate inflammatory responses [3] [2]. This technical guide provides a structured framework for designing experiments that effectively disentangle these complex signaling dynamics, enabling more precise mechanistic studies and therapeutic interventions. We present quantitative data analysis methodologies, detailed experimental protocols, and specialized reagent solutions to address these challenges systematically.
Fundamental Concepts
Cytokines are signaling proteins that function as crucial chemical messengers in the immune system, controlling inflammation, cell differentiation, and proliferation [2]. Their operational challenges stem from two key properties:
- Pleiotropy: A single cytokine can exert multiple, sometimes seemingly unrelated, biological effects on different target cells [110]. For instance, interleukin-6 (IL-6) exhibits both pro-inflammatory and anti-inflammatory effects depending on cellular context [111].
- Redundancy: Multiple cytokines often share overlapping functions, enabling robust system performance but complicating mechanistic studies [110]. This redundancy frequently arises from related cytokines sharing common receptor subunits, particularly beta-subunits, while maintaining ligand-specific alpha-subunits [110].
Signaling Context: Autocrine and Paracrine Dynamics
Cytokines operate through distinct spatial signaling modalities that influence experimental outcomes:
- Autocrine signaling: Cytokines bind to receptors on the same cell that released them, enabling self-amplification or self-regulation of cellular responses [2].
- Paracrine signaling: Cytokines signal to nearby cells, facilitating localized immune coordination within tissues [2].
- Endocrine signaling: Cytokines travel through circulation to distant target cells, mediating systemic effects [2].
Critically, the functional impact of these signaling modes depends on specific pathological contexts. For example, in response to lipopolysaccharide (LPS), tumor necrosis factor (TNF) does not significantly function in autocrine amplification of NFκB in the producing cell but plays a potent paracrine role in neighboring cells [3]. Conversely, in response to CpG DNA, autocrine TNF signaling extends the duration of NFκB activity and shapes subsequent gene expression programs [3].
Quantitative Analysis of Cytokine Signaling Networks
Systematic Profiling Approaches
Modern approaches to dissecting cytokine pleiotropy and redundancy employ large-scale transcriptional profiling to map cytokine-response relationships across diverse cellular contexts.
Table 1: CytoSig Platform Analysis of Cytokine Response Signatures [16]
| Cytokine | Number of Profiles | Representative Target Genes | Correlation with Ligand Expression (TCGA) | Key Functional Associations |
|---|---|---|---|---|
| IL-10 | 16 | SOCS3, IL1RN, CD163 | 0.68 | Anti-inflammatory response |
| IL-27 | 8 | CXCL10, IDO1, PD-L1 | 0.72 | Th1 differentiation, antiviral |
| BMP6 | 5 | ID1, SMAD6, HEY1 | 0.61 | Anti-inflammatory factor |
| CXCL8 | 23 | MMP9, CXCR1, BC2L1 | 0.75 | Neutrophil recruitment |
The CytoSig platform represents a significant advancement, having curated 20,591 transcriptome profiles of human cytokine, chemokine, and growth factor responses [16]. This resource enables researchers to predict cytokine signaling activities from transcriptomic data and identify context-specific functions.
Network-Level Interactions
Cytokines operate within a complex network where one cytokine can influence the production and activity of others, creating feedback loops that complicate experimental interpretation [111].
Table 2: Pro-inflammatory and Anti-inflammatory Cytokine Profiles [111]
| Cytokine Class | Representative Members | Primary Cellular Sources | Major Functions | Therapeutic Targeting |
|---|---|---|---|---|
| Pro-inflammatory | IL-1β, IL-6, IL-8, IL-12, TNF-α, IFN-γ | Macrophages, T cells, Dendritic cells | Drive inflammatory processes, activate immune cells | TNF-α inhibitors, IL-17 inhibitors |
| Anti-inflammatory | IL-4, IL-10, IL-11, IL-13, IL-1RA, TGF-β | Regulatory T cells, Macrophages, B cells | Inhibit inflammation, suppress immune responses | IL-10 therapy, TGF-β modulation |
The balance between these opposing cytokine classes is crucial for immune homeostasis, with imbalances leading to chronic inflammation, autoimmunity, or immunosuppression [111].
Experimental Design Strategies
Controlling for Pleiotropy
Pleiotropy requires that cytokine receptors exert differential activities on different cells, potentially explained by several molecular mechanisms [110]:
- Usage of different beta-subunits in various cell types
- Unique signaling capacities of ligand-specific alpha-subunits
- Differential signaling capacities of distinct regions of receptor complexes
- Differential cellular machinery that responds to the same signal in different ways
Experimental Protocol 1: Cell-Type-Specific Response Profiling
- Stimulus Application: Treat purified primary cell populations (e.g., macrophages, T cell subsets, epithelial cells) with standardized cytokine concentrations.
- Multi-parameter Readouts: Simultaneously measure phosphorylation events, gene expression changes, and functional outputs across cell types.
- Receptor Characterization: Quantify receptor subunit expression patterns (both alpha and beta chains) across cell types using flow cytometry or Western blot.
- Pathway Inhibition: Apply specific inhibitors (e.g., JAK/STAT, MAPK, NFκB inhibitors) to identify utilized signaling modules in each cell type.
This approach reveals how the same cytokine elicits different responses across cellular contexts, addressing pleiotropy through systematic comparison.
Addressing Redundancy
Functional redundancy arises when multiple cytokines signal through shared receptor components and downstream pathways [110]. The IL-10 cytokine family exemplifies this challenge, with multiple members (IL-19, IL-20, IL-22, IL-24, IL-26) signaling through shared receptor complexes and commonly activating STAT3 transcription factors [112].
Experimental Protocol 2: Redundancy Dissection Through Combinatorial Perturbation
- Single Cytokine Knockout: Using CRISPR/Cas9 or neutralizing antibodies, individually inhibit each cytokine in a functionally related family.
- Combinatorial Knockout: Progressively inhibit multiple cytokines in combination to identify redundancy thresholds.
- Receptor Blockade: Inhibit shared receptor subunits to determine which cytokine functions are abolished.
- Rescue Experiments: Add back individual cytokines to establish sufficiency for specific functions.
This systematic approach identifies which cytokines are truly redundant versus those with unique non-overlapping functions despite shared signaling components.
Advanced Methodologies and Visualization
Signaling Pathway Mapping
The IL-10 family cytokine signaling pathway demonstrates shared and distinct signaling components that underlie both redundancy and specific actions:
IL-10 Family Signaling Network Diagram
This visualization illustrates how different IL-10 family cytokines utilize shared receptor components and signaling pathways while maintaining specificity through unique receptor combinations.
Experimental Workflow for Autocrine/Paracrine Analysis
The following experimental workflow systematically distinguishes autocrine versus paracrine cytokine functions:
Autocrine/Paracrine Experimental Workflow
This workflow enables researchers to deconstruct complex cytokine networks by experimentally isolating specific signaling modalities. The approach revealed that TNF functions predominantly through paracrine signaling in LPS response but acquires significant autocrine functions in CpG DNA response [3].
Research Reagent Solutions
Table 3: Essential Research Reagents for Cytokine Pleiotropy and Redundancy Studies
| Reagent Category | Specific Examples | Research Application | Experimental Considerations |
|---|---|---|---|
| Neutralizing Antibodies | Anti-TNF, Anti-IL-6R, Anti-IFN-γ | Block specific cytokine functions to assess necessity | Potential cross-reactivity; validate specificity |
| Recombinant Cytokines | rhIL-10, rhTNF-α, rhIL-1β | Stimulate pathways to assess sufficiency | Dose-response critical; consider physiological concentrations |
| Signaling Inhibitors | JAK Inhibitors (Tofacitinib), STAT Inhibitors, p38/MAPK Inhibitors | Block specific downstream pathways | Off-target effects; use multiple inhibitors for confirmation |
| Receptor Blockers | Anti-IL-10R, Anti-TNFR, Soluble cytokine receptors | Prevent ligand-receptor interactions | May not distinguish between receptor subtypes |
| CRISPR/Cas9 Systems | Knockout models for cytokines and receptors | Generate defined genetic backgrounds | Compensatory mechanisms may develop |
| Cytokine ELISA/Kits | Multiplex cytokine arrays, High-sensitivity ELISA | Quantify cytokine production | Dynamic range limitations; validate with spike-in controls |
Discussion and Future Perspectives
Managing cytokine pleiotropy and redundancy requires sophisticated experimental designs that account for the contextual nature of cytokine signaling. The development of comprehensive databases like CytoSig, which contains 20,591 transcriptomic profiles of cytokine responses, enables more predictive modeling of cytokine activities in diverse biological contexts [16]. Future research directions should include:
- Single-cell resolution analyses to uncover cell-to-cell variability in cytokine responses within seemingly homogeneous populations
- Spatiotemporal mapping of cytokine activities in tissues to understand localized concentration gradients and their functional impacts
- Computational modeling approaches that integrate multi-omics data to predict emergent behaviors in cytokine networks
- Advanced perturbation tools that enable precise manipulation of specific cytokine-receptor interactions in complex cellular environments
As these methodologies mature, researchers will gain increasingly precise control over cytokine pleiotropy and redundancy, enabling more effective therapeutic interventions for inflammatory diseases, autoimmune disorders, and cancer.
Technical Considerations for Primary Cell vs Cell Line Models
The investigation of autocrine and paracrine signaling of inflammatory cytokines presents unique challenges for in vitro model selection. The choice between primary cells and immortalized cell lines directly impacts the physiological relevance, translational validity, and ultimate success of research outcomes. Within the specific context of inflammatory signaling, where complex intercellular communication networks dictate biological responses, model selection becomes particularly critical. These communication mechanisms—autocrine (self-signaling) and paracrine (neighbor-signaling)—underpin fundamental inflammatory processes including leukocyte recruitment, immune cell activation, and tissue remodeling [113] [114]. This technical guide provides a comprehensive comparison of primary cells and cell lines, offering detailed methodologies and analytical frameworks to inform model selection for research on inflammatory cytokine signaling.
Comparative Analysis: Primary Cells vs. Cell Lines
Fundamental Characteristics and Research Applications
Table 1: Fundamental Characteristics of Primary Cells and Cell Lines
| Characteristic | Primary Cells | Immortalized Cell Lines |
|---|---|---|
| Origin | Directly isolated from human or animal tissues [115] [116] | Derived from primary cultures; often cancer-derived (e.g., HeLa, MCF-7) [117] |
| Lifespan | Finite; undergo a limited number of cell divisions before senescence [116] [118] | Infinite (continuous) due to spontaneous or induced transformation [118] [119] |
| Genetic Profile | Retain in vivo genetic makeup with minimal drift; donor-specific variations [115] [116] | Subject to genetic drift and selective pressure over passages; often exhibit anomalies [117] [115] |
| Physiological Relevance | High; maintain native morphology, cell-type specific functions, and key markers [115] [120] [116] | Low to moderate; often exhibit altered morphology and optimized for proliferation, not function [117] [120] |
| Key Advantages | • Human-specific biology• Retention of tissue-specific functions• Relevant for personalized medicine [115] [121] [122] | • Ease of culture and transfection• High scalability and reproducibility• Suitable for high-throughput screening [117] [118] |
| Key Limitations | • Technically complex culture• Donor-to-donor variability• Limited scalability and lifespan [117] [116] | • Poor predictive power for human biology• Contamination and misidentification risks• Often cancer-derived [117] [115] |
| Typical Time to Assay | Several weeks post-dissection [117] | Can be assayed within 24-48 hours of thawing [117] |
Quantitative Comparison of Key Parameters
Table 2: Quantitative and Functional Comparison for Signaling Research
| Parameter | Primary Cells | Cell Lines | Implication for Cytokine Signaling Research |
|---|---|---|---|
| Biological Relevance | High ( Closer to native morphology/function) [117] | Low ( Often non-physiological) [117] | Primary cells maintain authentic receptor expression and response profiles crucial for cytokine studies. |
| Reproducibility | Low ( High donor-to-donor variability) [117] | High ( Reliable, but prone to drift) [117] | Cell lines offer lower experimental noise, but primary cells better reflect human population diversity. |
| Scalability | Low ( Difficult to expand) [117] | High ( Easily scalable) [117] | Cell lines are superior for large-scale screening, while primary cells are limited by yield. |
| Species Relevance | Human (if using human primary cells) | Often non-human or cancer-derived [117] | Human primary cells avoid species-specific signaling pathway discrepancies. |
| Contamination Risk | Lower risk of cross-contamination [115] | Higher risk (e.g., HeLa contamination widespread) [115] | Misidentification can invalidate signaling studies, favoring primary cells. |
| Cost & Technical Demand | High (specialized media, limited passages) [116] | Low (standardized protocols, robust growth) [118] | Cell lines are more practical for routine assays; primary cells require expertise and resources. |
Experimental Workflows and Protocols
Establishing Primary Cultures for Signaling Studies
Protocol 1: Isolation and Culture of Primary Cells from Tissue
The process of establishing a primary culture requires careful attention to technique to maintain cell viability and function, which is paramount for subsequent signaling studies [121] [116].
- Tissue Acquisition and Dissection: Obtain tissue from surgical resection or biopsy, preserving structure in tissue-specific transport media. Under sterile conditions, mince tissue into 1-2 mm³ fragments using surgical scissors or blades [121] [122].
- Tissue Dissociation: Select an appropriate dissociation method based on tissue type:
- Enzymatic Dissociation: Incubate tissue fragments with a optimized enzyme cocktail (e.g., collagenase, trypsin, DNase) at 37°C with agitation. Enzymatic selection is critical; collagenase is often used for intestine, liver, and kidney, while papain may be used for muscle tissue [121] [122].
- Chemical Dissociation: Use agents like EDTA or EGTA to chelate cations (Ca²âº, Mg²âº) and weaken intercellular connections, often combined with enzymatic methods [121] [122].
- Mechanical Dissociation: Involves repeated cutting, homogenization, and filtration. Note: This method generally yields a higher number of non-viable cells and is less preferred for cultivation [121] [122].
- Cell Separation and Seeding: Neutralize the enzyme activity with complete growth medium. Filter the cell suspension through a 70-100 μm mesh to remove debris. Centrifuge and resuspend the cell pellet in specialized, serum-free or low-serum growth media optimized for the specific primary cell type. Seed cells onto culture vessels, which may be pre-coated with a physiologically relevant substrate (e.g., collagen, gelatin, fibronectin) to improve attachment and growth [120] [116] [119].
- Maintenance and Subculturing: Culture cells at 37°C in a 5% CO₂ humidified incubator. Change medium 24 hours post-seeding to remove non-adherent cells and residual DMSO if thawed from cryopreservation. Subculture cells at 70-80% confluence using a gentle dissociation reagent to avoid damaging cell surface receptors critical for cytokine signaling [116].
Diagram 1: Primary Cell Culture Workflow
Workflow for Autocrine/Paracrine Signaling Analysis
Integrating cell culture with modern analytical techniques is essential for deconstructing complex signaling networks.
Protocol 2: Analyzing Autocrine/Paracrine Signaling in Heterocellular Cultures
This multiscale inference-based approach integrates single-cell transcriptomic data to predict how intercellular communication influences cell phenotypes and population dynamics, with particular relevance to inflammatory processes [113].
- Experimental Model Setup: Establish a co-culture system containing multiple cell types involved in the inflammatory response. Alternatively, use conditioned media from one cell population to treat another to isolate soluble factor effects.
- Single-Cell RNA Sequencing (scRNA-seq): Harvest cells from the culture system. Prepare libraries using a platform such as 10x Genomics and sequence to obtain transcriptome-wide data at single-cell resolution. This data will form the foundation for all subsequent inferences [113].
- Cell State Annotation and Classification: Process raw sequencing data (alignment, normalization, clustering). Classify cells into distinct states or subtypes based on their transcriptomic profiles (e.g., using known marker genes for different immune cell states) [113].
- Ligand-Receptor Interaction Inference: Input the processed scRNA-seq data and cell state annotations into a computational tool like CellChat to infer intercellular communication networks. CellChat uses a curated database of ligand-receptor interactions to identify significantly active signaling pathways between different cell states and is robust to noise [113].
- Intracellular Signaling Network Reconstruction: Use a tool like decoupleR to estimate transcription factor (TF) activity from the gene expression data. Then, employ a causal network reconstruction tool (e.g., CORNETO) to integrate the ligand-receptor interactions, TF activities, and differential expression results. This step connects external signals to intracellular signaling nodes and downstream transcriptional outputs, identifying key regulatory TFs [113].
- Validation and Functional Analysis: Correlate inferences with protein-level data (e.g., phospho-protein flow cytometry) for key signaling nodes. Perturb predicted key ligands, receptors, or downstream TFs (e.g., using siRNA or small molecules) and measure the impact on cellular phenotypes (e.g., cytokine production, migration) to validate the model's predictions [113].
Diagram 2: Signaling Analysis Workflow
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Research Reagent Solutions for Signaling Studies
| Reagent Category | Specific Examples | Function & Application in Signaling Research |
|---|---|---|
| Specialized Growth Media | Endothelial Cell Medium, Airway Epithelial Cell Medium | Provides tissue-specific nutrients, hormones, and growth factors to maintain differentiated cell function and receptor expression [120] [116]. |
| Dissociation Reagents | Collagenase, Trypsin/EDTA, Accutase | Enzymatically cleaves cell-cell and cell-matrix adhesions to generate single-cell suspensions from tissues while preserving receptor integrity [121] [116]. |
| Extracellular Matrix (ECM) | Collagen I, Matrigel, Fibronectin, Gelatin | Provides a physiologically relevant substrate for cell attachment, spreading, and polarization, which influences cytokine secretion and response [116] [119]. |
| Cell Culture Supplements | Foetal Bovine Serum (FBS), Defined Growth Supplements (e.g., EGF, FGF) | Supports cell growth and viability. For signaling studies, defined, low-serum supplements are preferred to minimize confounding external signals [118] [119]. |
| Cryopreservation Media | Complete medium with 10% DMSO | Allows long-term storage of primary cells and cell lines while maintaining high post-thaw viability and functionality [116]. |
| Cytokine & Signaling Reagents | Recombinant Cytokines, Neutralizing Antibodies, Receptor Antagonists | Used to stimulate or inhibit specific signaling pathways to dissect autocrine/paracrine mechanisms and validate computational predictions [113]. |
Special Considerations for Autocrine/Paracrine Signaling Research
The study of autocrine and paracrine signaling introduces specific requirements for model systems, where the limitations of traditional models become particularly pronounced.
Preservation of Native Signaling Networks: Primary cells maintain authentic receptor expression levels and stoichiometry, which is critical for accurate modeling of cytokine signaling cascades. In contrast, cell lines often shift resources toward proliferation, altering their signaling networks and making them poor predictors of human immune responses [117] [115]. For example, studies show that findings in immortalized lines frequently fail to translate to human tissue or in vivo models, contributing to the high failure rate (∼97%) of CNS-targeted drug candidates [117].
Modeling Heterocellular Communication: Inflammatory environments consist of multiple interacting cell types. Primary cells, by retaining their native characteristics, are better suited for modeling these complex interactions. Research using scRNA-seq analysis of cancers, including small cell lung cancer, has revealed that signaling interactions between different cancerous cell subtypes result in reinforcement of phenotypic transitions and maintenance of population-level heterogeneity [113]. This complexity is difficult to recapitulate with homogeneous, immortalized cell lines.
Technical Considerations for Signaling Studies: When investigating specific autocrine/paracrine mechanisms, such as the lysophosphatidylserine (LysoPS) signaling in B cells, the use of models that accurately reflect in vivo receptor expression and coupling is essential. For instance, activated B cells produce LysoPS, which then acts via Gα13-coupled receptors in an autocrine/paracrine fashion to regulate cell adhesive properties and germinal center formation [114]. Such nuanced regulatory mechanisms may be lost or altered in immortalized cell lines.
The selection between primary cells and immortalized cell lines for the study of autocrine and paracrine inflammatory signaling is a fundamental decision that carries significant implications for research validity and translational potential. Primary cells offer superior physiological relevance and are indispensable for modeling human-specific signaling pathways and heterocellular communication, despite their technical challenges and higher cost. Immortalized cell lines provide practical advantages of scalability, reproducibility, and ease of use that make them suitable for high-throughput screening and preliminary investigations. A strategic approach often involves using cell lines for initial discovery and primary cell-based models for validation and mechanistic studies. As the field advances, emerging technologies like human iPSC-derived cells and standardized, ready-to-use primary cells (e.g., ioCells) are promising alternatives that aim to bridge the gap between relevance and practicality, potentially offering a path toward more predictive and human-relevant models for inflammatory cytokine research [117].
Approaches for Controlling Temporal Dynamics in Signaling Studies
The precise control of temporal dynamics in cell signaling has emerged as a critical frontier in biological research and therapeutic development. Unlike traditional approaches that focus on steady-state behaviors, understanding and manipulating the time-dependent aspects of signaling pathways offers unprecedented opportunities for targeted interventions. This is particularly relevant in the context of inflammatory cytokine research, where autocrine and paracrine signaling dynamics determine functional outcomes in health and disease [3] [11]. Cells employ complex temporal codes to transmit information through dynamic signaling patterns, where the timing, duration, and oscillatory characteristics of pathway activation encode specific instructions that dictate downstream biological responses [123]. The ability to measure, model, and manipulate these temporal patterns provides researchers with powerful tools to decipher pathological mechanisms and develop novel therapeutic strategies with enhanced specificity and reduced side effects.
In inflammatory processes, the dynamics of cytokine-mediated communication between cells create complex feedback loops that can either resolve inflammation or lead to chronic pathological states. Single-cell studies have revealed that stimulus-specific dynamics of key signaling molecules such as NFκB determine ligand-specific gene expression programs, and loss of this specificity is linked to autoimmune and inflammatory diseases [123] [3]. This understanding has sparked the development of innovative approaches to control these dynamics for research and therapeutic purposes. This technical guide comprehensively outlines the current methodologies for controlling temporal dynamics in signaling studies, with particular emphasis on their application to inflammatory cytokine research, providing researchers with practical frameworks for implementing these approaches in their experimental systems.
Computational and Modeling Approaches
Quantitative Metrics for Temporal Dynamics Analysis
Computational methods provide powerful, non-invasive approaches for analyzing and predicting temporal dynamics in signaling pathways. These approaches enable researchers to simulate perturbations and observe system behaviors that may be difficult to capture experimentally. A key advancement in this area is the development of quantitative metrics specifically designed to evaluate temporal patterns in signaling data.
The Stimulus Response Specificity (SRS) score is a computational metric developed to quantify how effectively a signaling system retains stimulus-specific information under pharmacological or genetic perturbations [123]. This score measures the capacity of temporal dynamics to accurately encode ligand identity and dose despite perturbations to the system. The SRS framework evaluates whether specific dynamic features are maintained, compromised, or altered in ways that affect signaling fidelity. Complementing the SRS score, the stimulus confusion map provides a visualization tool that represents how pharmacological treatments affect the discrimination between different stimuli based on their signaling dynamics [123]. This approach employs epsilon network clustering in trajectory space and various dimensionally reduced spaces to map the degree to which originally distinct signaling responses become confused under different experimental conditions.
For analyzing chromatin dynamics, methods like ChromTime utilize probabilistic mixture models to detect expanding, contracting, and steady peaks in time-course chromatin sequencing data [124]. This approach models spatial changes of chromatin mark peaks over time, predicting boundaries and their movements between consecutive time points. ChromTime has demonstrated that expanding and contracting peaks mark regulatory regions associated with transcription factor binding and gene expression changes, providing insights into the temporal regulation of gene expression programs downstream of signaling events [124].
Mathematical Modeling of Signaling Networks
Mathematical modeling represents a cornerstone approach for understanding and controlling temporal dynamics in complex signaling systems. Ordinary differential equation (ODE)-based models have proven particularly valuable for simulating the dynamic behavior of signaling pathways over time. For the NFκB signaling system, an established model consisting of 94 biochemical reactions controlled by 126 kinetic parameters can simulate temporal trajectories in response to various ligands and pharmacological treatments [123]. This model incorporates receptor-associated signaling modules for different ligands (TNF, LPS, CpG, Poly(I:C), and Pam3CSK) and a common core module including kinases TAK1 and IKK and the IκBα-NFκB negative feedback loop.
For cytokine dynamics, coupled partial differential equation (PDE) and ODE models have been developed to simulate cellular and cytokine responses during immune activation [125]. These models can predict the dynamics of key inflammatory cytokines including TNF-α, IL-6, IL-8, and IL-10 in response to pathogens such as S. aureus, capturing the interconnectivity between cellular and cytokine responses [125]. The integration of these modeling frameworks enables researchers to simulate how perturbations at different levels of the system affect overall temporal dynamics and functional outcomes.
Table 1: Computational Approaches for Analyzing Temporal Signaling Dynamics
| Method | Key Features | Applications in Inflammatory Signaling | Technical Requirements |
|---|---|---|---|
| Stimulus Response Specificity (SRS) Scoring | Quantifies retention of stimulus-specific information under perturbation | Evaluating drug effects on NFκB signaling specificity; identifying treatments that maintain signaling fidelity | Single-cell signaling data; computational implementation of SRS algorithm |
| Stimulus Confusion Mapping | Visualizes how perturbations affect discrimination between stimuli | Mapping how drugs alter capacity to distinguish between different immune threats | High-dimensional temporal data; dimensionality reduction techniques |
| ChromTime Analysis | Detects expanding, contracting, and steady chromatin peaks | Linking temporal changes in chromatin marks to inflammatory gene expression | Time-course chromatin sequencing data (ChIP-seq, ATAC-seq) |
| ODE/PDE Modeling | Simulates system dynamics using differential equations | Predicting cytokine dynamics in response to pathogens; simulating NFκB trajectories | Kinetic parameters; computational modeling expertise |
Experimental and Imaging Techniques
Live-Cell Imaging and Single-Cell Analysis
Advanced live-cell imaging technologies have revolutionized our ability to capture temporal dynamics in signaling processes with high resolution. The quantitative live-cell imaging of secretion activity (qLCI-S) technology enables high-throughput, dual-color monitoring of secretion activity at the single-cell level over several days [126]. This approach combines long-term imaging with subsequent transcriptomic analysis of phenotypically defined cells, allowing researchers to directly link dynamic secretory profiles with gene expression patterns. For inflammatory cytokine research, qLCI-S has been used to visualize characteristic temporal patterns of cytokine secretion in rare immune cell populations, such as group 2 innate lymphoid cells, and to reveal minor subpopulations with enhanced cytokine production [126].
The effectiveness of live-cell imaging approaches depends on the availability of specific reagents and technologies designed to capture dynamic processes. The following research toolkit outlines key resources for implementing these methodologies:
Table 2: Research Reagent Solutions for Temporal Dynamics Studies
| Research Tool | Function in Temporal Studies | Example Applications |
|---|---|---|
| qLCI-S Technology | Long-term, dual-color tracking of secretion activity | Dynamic cytokine secretion profiling in rare immune cell populations |
| GFP Reconstitution Across Synaptic Partners (GRASP) | Detects cell-cell contacts and communication events | Mapping synaptic connections; visualizing transient cell interactions |
| Split Fluorescent Protein Fragments (YFP, CFP) | Simultaneous imaging of multiple interaction factors | Tracking multiple signaling pathways or interaction networks concurrently |
| Photoactivated Localization Microscopy | Nanometer-resolution imaging of fluorescent proteins | Super-resolution tracking of protein localization and movement |
Signaling Codon Analysis for Feature Extraction
A powerful framework for analyzing complex temporal signaling data involves decomposing dynamic trajectories into discrete, informative features termed signaling codons [123]. This approach, particularly developed for NFκB signaling, identifies six key dynamic features that collectively encode stimulus-specific information:
- Speed: Captures the activation speed of the signaling response
- Peak Amplitude (Amp): The highest level of signaling activity reached
- Duration (Dur): The total time the signaling molecule remains above an activation threshold
- Total Activity (AUC): The overall accumulation of signaling activity over time
- Early vs. Late (EvL): Represents the front-loading of signaling activity
- Oscillatory Power (Osc): Quantifies the oscillation properties of the signaling trajectory
By quantifying these features under different experimental conditions, researchers can develop a feature-based representation of complex temporal patterns that facilitates comparison across conditions and identification of critical control points. This approach has demonstrated that temporal coding capacity of the NFκB signaling network is generally robust to various pharmacological perturbations, enabling targeted manipulation of specific dynamic features without causing broad side-effects [123].
Applications in Inflammatory Cytokine Research
Analyzing Autocrine and Paracrine Signaling Loops
The control of temporal dynamics is particularly relevant for understanding autocrine and paracrine signaling of inflammatory cytokines, where timing and feedback loops critically determine system behavior. Research on TNF production and signaling has revealed that network dynamics govern stimulus-specific autocrine and paracrine functions [3]. Contrary to initial expectations, systems biology approaches combining experimental studies with computational models demonstrated that in response to lipopolysaccharide (LPS), TNF does not have an autocrine function in amplifying the NFκB response in the same cell, although it plays a potent paracrine role in neighboring cells [3]. However, in response to CpG DNA, autocrine TNF extends the duration of NFκB activity and shapes CpG-induced gene expression programs [3].
This stimulus-specificity of autocrine functions highlights the importance of temporal dynamics in determining cytokine signaling outcomes. The integration of TNF production models with models of TLR, TNFR, and NFκB signaling modules has enabled researchers to simulate and predict these complex temporal relationships [3]. These approaches have revealed that the differential engagement of signaling adapters (MyD88 and TRIF) by various TLR agonists creates distinct temporal patterns that determine whether autocrine TNF signaling will occur and what functions it will serve.
Diagram 1: Temporal dynamics in autocrine and paracrine inflammatory signaling networks. The diagram illustrates how initial stimuli engage different adapter pathways that create distinct temporal signaling patterns, leading to cytokine production that feeds back through autocrine and paracrine loops. These feedback mechanisms are regulated by dynamic processes with specific timing characteristics.
Pharmacological Perturbation of Temporal Dynamics
Therapeutic targeting of temporal dynamics represents a promising approach for treating inflammatory diseases while minimizing side effects. Computational workflows have been developed to assess how drugs affect stimulus-specific signaling dynamics, using the NFκB system as a model [123]. This approach involves simulating dynamic NFκB trajectories in response to multiple stimuli (representing various immune threats) under treatment with representative drugs across different dosage levels.
The pharmacological perturbation strategy involves:
- Target Selection: Identifying key signaling nodes that control dynamic features without completely disrupting pathway function
- Dose Optimization: Determining concentration ranges that modulate without abrogating temporal patterns
- Specificity Assessment: Evaluating whether interventions maintain the system's capacity to generate stimulus-specific responses
This approach has revealed that the temporal coding capacity of the NFκB signaling network is generally robust to various pharmacological perturbations, enabling targeted manipulation of specific dynamic features without causing broad side-effects [123]. This robustness suggests that drugs can be designed to target pathological signaling dynamics while preserving physiological responses to different stimuli.
Implementation Framework
Integrated Workflow for Temporal Dynamics Studies
Implementing a comprehensive approach to control temporal dynamics requires the integration of computational and experimental methods. The following workflow provides a structured framework for designing studies focused on inflammatory cytokine dynamics:
Diagram 2: Integrated workflow for temporal dynamics studies in inflammatory signaling. The framework progresses from system characterization through perturbation design, experimental implementation, and data analysis, with iterative refinement based on validation results.
Protocol for Pharmacological Perturbation of NFκB Temporal Dynamics
Based on established computational workflows [123], the following detailed protocol can be implemented to assess drug effects on temporal signaling dynamics:
Step 1: System Modeling and Simulation
- Implement the NFκB signaling model comprising 94 biochemical reactions controlled by 126 kinetic parameters
- Simulate dynamic NFκB trajectories in response to 15 stimuli representing various immune threats
- Generate data for 10 representative drugs across 20 dosage levels for each stimulus condition
- Establish baseline dynamics and identify the six key signaling codons for each condition
Step 2: Dynamic Feature Extraction
- For each simulated trajectory, quantify the six signaling codons:
- Speed: Calculate activation speed using time to reach 50% of peak amplitude
- Peak Amplitude: Identify maximum NFκB activation level
- Duration: Determine time NFκB remains above activation threshold (typically 30% of maximum)
- Total Activity: Compute area under the curve (AUC) for the entire trajectory
- Early vs. Late: Calculate ratio of activity in first 60 minutes to remaining trajectory
- Oscillatory Power: Quantify using power spectral analysis of the detrended signal
- Compile features into a multidimensional dataset for analysis
Step 3: Stimulus Response Specificity Assessment
- Implement SRS score calculation to quantify retention of stimulus-specific information
- Construct stimulus confusion maps using epsilon network clustering in:
- Full trajectory space
- Canonical polyadic decomposition-reduced space
- Functional principal component analysis-reduced space
- Signaling codon space
- Compare confusion patterns across reduction methods to identify optimal analysis space
Step 4: Experimental Validation (Optional)
- For selected perturbations, validate predictions using live-cell imaging of NFκB dynamics
- Implement qLCI-S for correlated secretion dynamics and transcriptomic analysis
- Confirm that pharmacological effects match computational predictions
This protocol enables systematic evaluation of how drug treatments affect stimulus-specificity of NFκB activation dynamics and its ability to accurately code ligand identity and dose, providing a framework for developing temporal dynamics-targeted therapies.
The approaches outlined in this technical guide provide researchers with comprehensive methodologies for controlling and analyzing temporal dynamics in signaling studies, with particular relevance to inflammatory cytokine research. The integration of computational modeling, live-cell imaging, and feature-based analysis creates a powerful framework for understanding how timing and dynamics shape biological responses in health and disease. As these methods continue to evolve, they offer the potential to develop more precise therapeutic interventions that target pathological signaling dynamics while preserving physiological functions, ultimately leading to more effective treatments for inflammatory diseases with reduced side effects.
Therapeutic Targeting and Clinical Translation Assessment
Validation Frameworks for Autocrine/Paracrine Signaling Loops
The precise validation of autocrine and paracrine signaling loops represents a critical challenge in molecular biology, particularly in the context of inflammatory cytokine research. Autocrine signaling occurs when cells respond to signaling molecules they themselves secrete, while paracrine signaling involves cellular responses to molecules secreted by neighboring cells [22]. These communication modes are fundamental to coordinated immune responses, tissue homeostasis, and disease pathogenesis, yet their experimental distinction requires sophisticated methodological approaches. The complexity of these systems is exemplified by findings that the same cytokine, such as Tumor Necrosis Factor (TNF), can function primarily through paracrine mechanisms in response to certain stimuli (e.g., lipopolysaccharide, LPS) while utilizing autocrine signaling in response to others (e.g., CpG DNA) [3]. This stimulus-specificity highlights that network dynamics of adaptor proteins like MyD88 and TRIF govern the autocrine and paracrine functions of cytokines, necessitating validation frameworks that can capture these nuanced biological behaviors [3].
Advancements in single-cell technologies and computational biology have revolutionized our ability to dissect these complex communication networks. Researchers can now move beyond traditional bulk population studies to investigate signaling heterogeneity at cellular resolution, enabling more precise validation of autocrine/paracrine mechanisms [113] [11]. This technical guide provides a comprehensive overview of contemporary validation frameworks, integrating both experimental and computational approaches to address the unique challenges associated with establishing bona fide autocrine and paracrine signaling loops in inflammatory contexts.
Core Principles and Biological Significance
Defining Autocrine and Paracrine Signaling
In multicellular organisms, cell-cell communication (CCC) represents a fundamental process that profoundly influences an organism's homeostasis, development, and disease processes [11]. Cytokines, as key signaling molecules, can exert their effects through three primary modes: autocrine signaling (acting on the same cell that produced them), paracrine signaling (acting on nearby cells), and endocrine signaling (acting on distant cells) [22]. The functional distinction between autocrine and paracrine mechanisms has profound implications for understanding inflammatory processes, as these signaling modes can generate qualitatively different network behaviors including positive feedback loops, signal amplification, and tissue-level response coordination.
From a technical perspective, autocrine signaling creates potential for self-reinforcing circuits that can drive bistable switches in cell fate, while paracrine signaling enables coordinated responses across cell populations. The biological significance of properly distinguishing these mechanisms is underscored by findings that aberrant autocrine/paracrine loops contribute to various pathological states, including cancer metastasis, chronic inflammation, and autoimmune disorders [3] [113]. For instance, in cancer biology, autocrine/paracrine signaling of lysophosphatidylserine (LysoPS) through Gα13-coupled receptors has been shown to inhibit B cell aggregation, thereby affecting germinal center and tertiary lymphoid structure formation [114].
Analytical Challenges in Loop Validation
Validating autocrine and paracrine loops presents unique methodological challenges that stem from several biological complexities. Ligand-receptor binding kinetics, receptor compartmentalization, and signal integration with other pathways create a dynamic signaling landscape that is difficult to capture with single-timepoint or bulk measurements [3] [127]. Additionally, inflammatory cytokines often exhibit significant redundancy and pleiotropy, where multiple cytokines activate overlapping signaling pathways and single cytokines elicit diverse effects in different cellular contexts [22].
The technical challenge is further compounded by the spatiotemporal dynamics of cytokine secretion, diffusion, binding, and degradation—parameters that are difficult to measure directly in living tissues. Computational models have revealed that the same cytokine-receptor system can function primarily through autocrine or paracrine mechanisms depending on relative expression levels, tissue architecture, and the presence of negative regulators [3]. These findings emphasize that validation frameworks must move beyond simple ligand-receptor co-expression analyses to incorporate dynamic and quantitative assessments of signaling activity.
Computational Validation Frameworks
Multiscale Inference Approaches
Advanced computational methods have emerged that leverage single-cell RNA sequencing (scRNA-seq) data to infer autocrine/paracrine communication patterns. These multiscale inference approaches integrate multiple analytical layers to connect intercellular signaling with intracellular responses, enabling more robust prediction of autocrine/paracrine loops [113]. A prominent workflow integrates ligand-receptor interaction inference (using tools like CellChat), transcription factor activity estimation (using decoupleR), and causal signaling network reconstruction (using CORNETO) to analyze scRNA-seq data and investigate how intercellular interactions influence cell phenotypes [113].
This integrated framework addresses a key limitation of earlier methods by not only identifying potential ligand-receptor interactions but also determining whether these interactions produce measurable downstream signaling effects. The application of this approach to small cell lung cancer (SCLC) revealed that signaling interactions between cancerous cells reinforce phenotypic transitions and maintain population-level intratumoral heterogeneity through defined autocrine/paracrine circuits [113]. Validation of these predictions requires orthogonal experimental approaches, but the computational framework provides critical hypotheses for testing.
Table 1: Computational Tools for Signaling Loop Validation
| Tool Name | Primary Function | Application in Loop Validation | Strengths |
|---|---|---|---|
| CellChat | Ligand-receptor interaction inference from scRNA-seq data | Identifies potential autocrine/paracrine interactions based on co-expression patterns | Robust to noise; incorporates heteromeric complexes; high specificity |
| decoupleR | Transcription factor activity estimation | Connects extracellular signaling to intracellular responses through TF activation | Uses multiple statistical methods; integrates with prior knowledge networks |
| CORNETO | Causal signaling network reconstruction | Reconstructs context-specific signaling networks from perturbation data | Finds minimal consistent networks; integrates multiple data types |
| GRASP (GFP reconstitution across synaptic partners) | Detection of cell-cell contacts | Visualizes physical interactions between cells in complex tissues | Provides spatial information; can be used with multiple fluorescent proteins |
Machine Learning Applications
Machine learning (ML) approaches offer promising avenues for enhancing the validation of signaling loops, particularly through their ability to identify complex patterns in high-dimensional data. Supervised ML models such as Gradient Boosted Trees have been successfully applied to related validation challenges in biology, demonstrating accuracies of 83-86% in classification tasks [128]. In the context of autocrine/paracrine validation, similar models could be trained to distinguish autocrine-dominant from paracrine-dominant signaling patterns based on features derived from single-cell or spatial transcriptomics data.
A critical consideration for ML applications in this domain is model interpretability. Methods such as SHapley Additive exPlanations (SHAP) analysis can mitigate the "black box" effect of complex ensemble models by identifying the key features driving predictions [128]. This approach not only validates model performance but can also reveal novel biological insights into the molecular determinants of autocrine versus paracrine signaling dominance.
Experimental Validation Methodologies
Genetic Perturbation Strategies
Genetic approaches provide powerful tools for dissecting autocrine/paracrine signaling mechanisms. Knockout models of specific cytokines, their receptors, or downstream signaling components can establish necessity for specific communication modes. For example, studies using trif−/− and myd88−/− bone marrow-derived macrophages (BMDMs) demonstrated that TRIF and MyD88 adaptor proteins differentially regulate TNF production through distinct mechanisms, with MyD88 primarily controlling early transcriptional responses and TRIF influencing post-transcriptional and post-translational events [3].
The experimental workflow for genetic validation typically involves a series of sequential experiments:
- Cell culture validation using primary cells or cell lines to establish baseline signaling responses
- Genetic perturbation using CRISPR/Cas9, siRNA, or stable knockout systems
- Stimulus application using specific ligands (e.g., LPS, CpG DNA) to activate defined pathways
- Multi-level response measurement assessing transcriptional, translational, and secretory events
- Coculture experiments to distinguish cell-autonomous from non-cell-autonomous effects
This approach was instrumental in demonstrating that TNF does not have significant autocrine function in amplifying the NFκB response to LPS, despite its potent paracrine role in neighboring cells [3]. The same study revealed that in response to CpG DNA, autocrine TNF extends the duration of NFκB activity and shapes gene expression programs, highlighting the stimulus-specific nature of these signaling modes.
Spatial Localization Techniques
The spatial dimension is fundamental to distinguishing autocrine from paracrine signaling, as these modes are defined by the relative positions of signal source and target cells. Advanced imaging techniques enable visualization of cytokine secretion, diffusion, and receptor engagement with high spatiotemporal resolution. Methods such as GFP reconstitution across synaptic partners (GRASP) employ split fluorescent protein fragments fused to interacting partners on opposing cells [11]. When cells make contact, the split proteins associate and reconstitute fluorescence, providing direct visual evidence of cell-cell communication.
Super-resolution microscopy techniques, including stimulated emission depletion (STED) and structured illumination microscopy (SIM), have further enhanced our ability to visualize signaling events at nanometer resolution [11]. These approaches can reveal the subcellular localization of cytokine receptors, internalization events, and downstream signaling complexes that define autocrine versus paracrine responses. When combined with genetic reporters for pathway activity (e.g., NFκB translocation assays), these methods provide powerful validation of predicted autocrine/paracrine loops.
Table 2: Key Research Reagent Solutions for Signaling Validation
| Reagent Category | Specific Examples | Experimental Function | Considerations for Use |
|---|---|---|---|
| Primary cell models | Bone marrow-derived macrophages (BMDMs) | Physiological relevance for inflammatory signaling | Require specialized isolation protocols; donor variability |
| Genetic perturbation tools | CRISPR/Cas9, siRNA, knockout mice | Establish necessity of specific components | Off-target effects; compensation mechanisms |
| Pathway agonists/antagonists | LPS, CpG DNA, cytokine inhibitors | Selective pathway activation/inhibition | Specificity concerns; dose optimization required |
| Detection antibodies | Phospho-specific antibodies, cytokine ELISA | Measure pathway activation and cytokine production | Validation for specific applications needed |
| Live-cell reporters | FRET biosensors, NFκB-GFP reporters | Real-time monitoring of signaling dynamics | Potential perturbation of native signaling |
| Single-cell platforms | scRNA-seq, CyTOF, high-content imaging | Resolution of cellular heterogeneity | Cost; computational expertise required |
Integrated Workflows and Case Studies
Iterative Systems Biology Approach
The complexity of autocrine/paracrine signaling demands integrated validation strategies that combine computational and experimental methods. An iterative systems biology approach has proven particularly effective, wherein mathematical models of signaling networks generate testable predictions that are subsequently validated experimentally [3]. This approach typically follows a cyclic workflow:
- Quantitative model development based on existing literature and preliminary data
- Model simulation to predict network behaviors under specific conditions
- Experimental design to test key model predictions
- Data collection using appropriate analytical methods
- Model refinement based on experimental results
This framework was successfully applied to understand the multitier control of TNF production, leading to the counterintuitive finding that TNF does not function autocrinally in LPS signaling despite potent paracrine effects [3]. The model integrated regulatory modules controlling TNF mRNA synthesis and processing, mRNA half-life, translation, and protein processing and secretion, then linked these to established models of TLR, TNFR, and NFκB signaling modules.
Inflammatory Cytokine Case Study: TNF Signaling
TNF represents a paradigmatic example of the complexities in validating autocrine/paracrine loops, with studies revealing stimulus-specific behaviors that challenge simplistic categorization. In response to LPS, which engages both MyD88 and TRIF adaptor proteins, TNF primarily functions through paracrine mechanisms with minimal autocrine amplification of NFκB signaling [3]. In contrast, in response to CpG DNA, which engages only MyD88, autocrine TNF signaling extends the duration of NFκB activity and shapes subsequent gene expression programs.
The validation of these distinct behaviors required multiple orthogonal approaches:
- Cell culture systems with controlled stimulation conditions
- Genetic models including trif−/− and myd88−/− macrophages
- Secreted protein quantification using ELISA at multiple timepoints
- Transcriptional analysis measuring nascent RNA production
- Computational modeling to integrate data and generate testable hypotheses
- Coculture experiments to separate donor and responder cells
This multifaceted approach revealed that network dynamics of MyD88 and TRIF signaling determine the stimulus-specific autocrine and paracrine functions of TNF, providing a framework for understanding similar complexities with other inflammatory cytokines [3].
Quantitative Assessment and Data Analysis
Performance Metrics for Validation
Robust validation of autocrine/paracrine loops requires quantitative assessment using appropriate performance metrics. Control performance monitoring (CPM) methods, adapted from engineering applications, provide valuable frameworks for evaluating signaling system performance [129]. These include both model-based approaches (requiring detailed system modeling) and model-free approaches (based solely on operational data).
For signaling loop validation, particularly relevant model-free CPM methods include:
- Integral-based indices: Integral Squared Error (ISE), Integral of Time-weighted Absolute Error (ITAE)
- Statistical divergence measures: Kullback-Leibler divergence, Histogram Intersection, Euclidean Distance
- Oscillation detection methods: Cross-correlation, autocorrelation-based approaches
In comparative studies, Kullback-Leibler divergence, Euclidean distance, histogram intersection, and Overall Controller Efficiency (OCE) performed well in identifying fault scenarios in control systems, suggesting similar utility for detecting perturbations in signaling loops [129]. These metrics enable quantitative comparison of signaling behaviors under different conditions (e.g., wild-type vs. knockout, different stimuli), providing statistical rigor to validation efforts.
Data Integration and Visualization
The complexity of autocrine/paracrine signaling data demands sophisticated integration and visualization approaches. Multiscale inference frameworks that connect ligand-receptor interactions to downstream transcriptional responses enable more holistic interpretation of validation experiments [113]. These approaches typically incorporate multiple data types:
- Ligand-receptor interaction data from tools like CellChat
- Transcription factor activity from algorithms like decoupleR
- Gene expression patterns from single-cell or bulk RNA-seq
- Protein localization and abundance from imaging or proteomics
- Phenotypic readouts from functional assays
Effective visualization of these integrated datasets often requires specialized approaches such as circos plots for ligand-receptor interactions, heatmaps for coordinated expression patterns, and network graphs for signaling pathways. These visualizations not only aid in data interpretation but can also reveal emergent patterns that might be missed in reductionist analyses.
Future Directions and Concluding Remarks
The validation of autocrine/paracrine signaling loops continues to evolve with technological advancements. Emerging methods in spatial transcriptomics, live-cell biosensors, and multiplexed proteomics promise to provide increasingly comprehensive views of cytokine signaling in relevant physiological contexts. Additionally, the integration of machine learning approaches with mechanistic modeling offers exciting opportunities for discovering novel autocrine/paracrine circuits and predicting their functional consequences [128].
A critical future direction involves moving beyond simplified cell culture systems to validate autocrine/paracrine loops in complex tissue environments. The development of organoid and tissue-on-chip platforms that preserve native tissue architecture while allowing experimental manipulation will be essential for this transition. Similarly, advances in in vivo biosensors and perturbation tools will enable more direct testing of autocrine/paracrine mechanisms in physiological contexts.
The validation frameworks outlined in this guide provide a foundation for rigorous assessment of autocrine/paracrine signaling loops, with particular relevance to inflammatory cytokine research. By combining computational, genetic, spatial, and quantitative approaches, researchers can overcome the historical challenges associated with distinguishing these fundamentally different signaling modes. As these methods continue to mature, they will undoubtedly reveal new insights into the organization of cytokine networks and their roles in health and disease.
Comparative Analysis of Monoclonal Antibodies and Small Molecule Inhibitors
The therapeutic landscape for modulating pathological signaling pathways, particularly those involving inflammatory cytokines in autocrine and paracrine loops, is dominated by two distinct classes of pharmacological agents: monoclonal antibodies (mAbs) and small molecule inhibitors. These therapeutic modalities employ fundamentally different strategies for interrupting disease-driving signals. Monoclonal antibodies are large, complex proteins typically produced in living systems that target specific antigens with high precision, while small molecule inhibitors are low molecular weight compounds designed to interact with specific molecular targets, often intracellular enzymes such as protein kinases [130] [131]. The selection between these modalities requires careful consideration of their respective properties, mechanisms, and therapeutic applications, especially within the context of cytokine signaling research where autocrine and paracrine mechanisms perpetuate disease states [132] [133] [99].
Autocrine signaling occurs when cells respond to signaling molecules that they themselves secrete, creating a self-stimulatory loop, while paracrine signaling involves communication between neighboring cells through locally secreted mediators [133]. These signaling mechanisms are particularly relevant in inflammatory diseases and cancer, where they can drive pathological processes and confer resistance to therapies [99]. Understanding the distinct capabilities of mAbs and small molecules in disrupting these signaling paradigms is essential for advancing targeted therapeutic interventions.
Molecular Properties and Mechanisms of Action
Fundamental Structural Characteristics
The structural divergence between monoclonal antibodies and small molecule inhibitors underlies their distinct pharmacological behaviors. Monoclonal antibodies are large biological molecules with molecular weights typically ranging from 150-200 kDa, characterized by a complex Y-shaped structure comprising two heavy chains and two light chains organized into constant (Fc) and variable (Fab) regions [134] [131]. The Fab region contains complementarity-determining regions (CDRs) that confer exquisite antigen specificity, while the Fc region mediates immune effector functions. Their substantial size and proteinaceous nature generally restricts them to extracellular targets and necessitates administration via injection or infusion [130] [131].
In contrast, small molecule inhibitors are synthetically produced chemical compounds with molecular weights typically below 900 Daltons [130] [131]. Their compact size and chemical nature enable them to readily cross cell membranes and target intracellular proteins, including kinases and other enzymes. This property makes them particularly suitable for targeting cytosolic and nuclear targets inaccessible to biologics. Most small molecule drugs can be administered orally and exhibit favorable stability at room temperature, significantly simplifying their storage, distribution, and patient use [130].
Table 1: Fundamental Properties of Monoclonal Antibodies and Small Molecule Inhibitors
| Property | Monoclonal Antibodies | Small Molecule Inhibitors |
|---|---|---|
| Molecular Size | 150-200 kDa (large proteins) | <900 Daltons (low molecular weight) [130] |
| Structural Complexity | Complex tertiary and quaternary structure | Simple chemical structures [131] |
| Production Method | Living cell systems (CHO, bacterial) [131] | Chemical synthesis [131] |
| Typical Administration Route | Injection/Infusion (IV, SC) [130] | Oral (tablets, capsules) [130] |
| Storage Requirements | Refrigeration (2-8°C) often required [130] | Typically stable at room temperature [130] |
| Cellular Permeability | Poor (limited to extracellular targets) [130] | Excellent (access intracellular targets) [130] |
Mechanisms of Action in Signaling Pathways
Monoclonal antibodies and small molecule inhibitors employ distinct mechanisms to modulate disease-relevant signaling pathways. mAbs typically exert their effects through highly specific target engagement, which can result in several downstream consequences: (1) neutralization of soluble ligands like inflammatory cytokines, preventing receptor activation; (2) blockade of receptor-ligand interactions; (3) induction of antibody-dependent cellular cytotoxicity (ADCC) via Fc receptor engagement on immune cells; (4) complement-dependent cytotoxicity (CDC); and (5) receptor internalization and degradation [134] [135]. For example, anti-TNFα antibodies such as infliximab and adalimumab bind soluble and membrane-bound TNFα, effectively disrupting its interaction with TNF receptors and thereby attenuating inflammatory signaling in conditions like rheumatoid arthritis and inflammatory bowel disease [136].
Small molecule inhibitors typically function by competitively or allosterically inhibiting enzymatic activity within cells. The most prominent class—protein kinase inhibitors—often targets the ATP-binding pocket of kinases, preventing phosphorylation of downstream substrates and interrupting signal transduction cascades [137] [138]. For instance, imatinib (Gleevec) binds to the ATP-binding site of the BCR-ABL fusion kinase, inhibiting its constitutive activity and producing remarkable efficacy in chronic myeloid leukemia [137]. Their intracellular access allows them to target signaling components throughout the cytoplasmic and nuclear compartments.
Diagram 1: Therapeutic Targeting of Inflammatory Signaling Pathways. Monoclonal antibodies (blue) primarily target extracellular components such as cytokines and their receptors, while small molecule inhibitors (green) penetrate cells to inhibit intracellular kinases and downstream signaling events.
Therapeutic Applications in Autocrine/Paracrine Signaling
Targeting Autocrine and Paracrine Signaling Loops
Autocrine and paracrine signaling mechanisms play crucial roles in various pathological conditions, including cancer, autoimmune diseases, and inflammatory disorders. Autocrine signaling occurs when cells respond to signaling molecules that they themselves secrete, creating self-stimulatory loops, while paracrine signaling involves communication between neighboring cells through locally secreted mediators [133]. These mechanisms are particularly relevant in the context of inflammatory cytokines, where they can establish and perpetuate disease states.
In cancer, autocrine signaling loops can drive uncontrolled proliferation and confer resistance to therapies. For example, many tumor cells secrete growth factors such as epidermal growth factor (EGF) or vascular endothelial growth factor (VEGF) that bind to receptors on their own surface, creating a self-sustaining growth signal [133]. Similarly, in cholangiocarcinoma, autocrine and paracrine signals originating in the tumor microenvironment promote chemoresistance by activating pro-survival pathways that protect cancer cells from drug-induced apoptosis [99]. Embryonic stem cells also utilize autocrine signaling through factors like Fgf4 and Wnt to maintain self-renewal and regulate differentiation timing [132].
Modality-Specific Therapeutic Approaches
Monoclonal antibodies excel at intercepting autocrine/paracrine signaling by targeting extracellular components—either the soluble ligands themselves or their cognate receptors. This approach effectively neutralizes the signaling molecules before they can engage cellular receptors, thereby disrupting both autocrine and paracrine communication. For instance, anti-IL-6 antibodies can disrupt IL-6-mediated autocrine loops that drive tumor growth in lung adenocarcinoma [133]. Similarly, anti-VEGF antibodies like bevacizumab block VEGF-driven paracrine signaling between tumor cells and vascular endothelial cells, inhibiting angiogenesis [136].
Small molecule inhibitors are particularly effective against intracellular kinases that function as critical signal transducers in autocrine/paracrine loops. Their ability to penetrate cell membranes allows them to target key signaling nodes within the cytoplasm. For example, EGFR tyrosine kinase inhibitors like gefitinib and osimertinib effectively disrupt autocrine signaling in non-small cell lung cancers with EGFR mutations, where the EGFR pathway is constitutively activated [137]. JAK inhibitors represent another important class that targets signal transduction downstream of multiple cytokine receptors, effectively dampening inflammatory responses in autoimmune conditions [137].
Table 2: Therapeutic Applications in Autocrine/Paracrine Signaling Pathways
| Signaling Context | Monoclonal Antibody Approach | Small Molecule Inhibitor Approach |
|---|---|---|
| Inflammatory Cytokines (TNFα, IL-6) | Neutralize soluble cytokines (infliximab, adalimumab) [136] | Intracellular kinase inhibition (JAK inhibitors) [137] |
| Growth Factor Signaling (EGFR, HER2) | Receptor blockade (cetuximab, trastuzumab) [136] [135] | Tyrosine kinase inhibition (gefitinib, osimertinib) [137] |
| Angiogenesis (VEGF) | Ligand neutralization (bevacizumab) [136] | Receptor kinase inhibition (sunitinib) [138] |
| Immune Checkpoints (PD-1/PD-L1) | Blockade of immune inhibitory signals (nivolumab) [136] | Limited application due to extracellular nature of targets |
| Intracellular Oncogenic Kinases | Not accessible to conventional mAbs | Direct kinase inhibition (imatinib targeting BCR-ABL) [137] |
Comparative Strengths and Limitations
Therapeutic Advantages and Challenges
Both therapeutic modalities present distinct profiles of advantages and limitations that influence their clinical application. Monoclonal antibodies offer exceptional target specificity, typically resulting in fewer off-target effects and reduced toxicity compared to conventional small molecule therapies [135]. Their long half-life, often ranging from days to weeks, enables less frequent dosing intervals—a particular advantage in chronic conditions requiring sustained therapy [130]. Additionally, the Fc-mediated effector functions of mAbs, including ADCC and CDC, can engage the immune system directly in eliminating target cells, providing a therapeutic mechanism beyond simple target neutralization [134].
However, mAbs face significant limitations including poor oral bioavailability, necessitating parenteral administration, and the potential for immunogenicity, which can lead to the development of anti-drug antibodies that reduce efficacy or cause adverse reactions [136] [135]. Their complex structure demands stringent storage conditions, typically requiring refrigeration, and complicates manufacturing, resulting in substantially higher production costs compared to small molecules [130]. Perhaps most importantly, their large size and polarity generally restrict them to extracellular targets, leaving intracellular signaling components inaccessible.
Small molecule inhibitors offer the significant advantage of oral administration, greatly enhancing patient convenience and compliance [130]. Their small size enables penetration of cell membranes to reach intracellular targets, including kinases and other enzymes involved in signal transduction cascades [137]. Manufacturing processes for small molecules are generally more established and scalable than biologics production, resulting in lower production costs and ultimately reduced treatment expenses, especially after patent expiration when generics become available [130].
The limitations of small molecules include a typically shorter half-life, often requiring more frequent dosing, and a higher propensity for off-target effects and drug-drug interactions due to less exquisite specificity compared to mAbs [130]. They can be susceptible to rapid metabolism and elimination, and pathogens or cancer cells may develop resistance through mutation of the target binding site [130]. Additionally, their ability to cross the blood-brain barrier, while advantageous for CNS targets, can increase the risk of neurological side effects when targeting peripheral tissues.
Development and Commercial Considerations
The development pathways for these two therapeutic classes differ substantially in timeline, cost, and regulatory considerations. Small molecule development typically requires 8-10 years at an average cost of $1-2 billion, while biologics development averages 10-12 years with costs ranging from $2-4 billion [131]. This discrepancy stems from the more complex manufacturing processes and analytical characterization required for biologics.
Regulatory protection also differs between the classes. Small molecules typically receive 5 years of market exclusivity before facing generic competition, while biologics are granted 12 years of exclusivity before biosimilars can enter the market [130]. However, the pathway for biosimilar approval remains more complex than for generic small molecules, requiring extensive comparative studies rather than simple bioequivalence demonstrations [131].
Table 3: Comparative Development and Clinical Profiles
| Parameter | Monoclonal Antibodies | Small Molecule Inhibitors |
|---|---|---|
| Development Timeline | 10-12 years [131] | 8-10 years [131] |
| Development Cost | $2-4 billion [131] | $1-2 billion [131] |
| Market Exclusivity | 12 years [130] | 5 years [130] |
| Dosing Frequency | Less frequent (days to weeks) [130] | More frequent (daily to weekly) [130] |
| Immunogenicity Risk | Higher (anti-drug antibodies) [136] | Lower |
| Manufacturing Complexity | High (living systems, stringent controls) [130] | Lower (chemical synthesis) [130] |
| Follow-on Competition | Biosimilars (complex development) [131] | Generics (straightforward approval) [130] |
Research Methodologies and Experimental Protocols
Investigating Autocrine/Paracrine Signaling in Therapeutic Development
Research into autocrine and paracrine signaling mechanisms requires specialized methodologies that can elucidate complex cell-cell communication networks. Microfluidic technologies have emerged as particularly valuable tools in this context, enabling precise control over the spatial and temporal cellular microenvironment with resolution down to single cells and subsecond timescales [132]. These systems allow researchers to create defined gradients of signaling molecules, manipulate cell organization, and monitor autocrine/paracrine signaling dynamics in real-time.
For investigating therapeutic modulation of these pathways, several established experimental approaches are employed. Conditional medium transfer experiments can distinguish autocrine from paracrine effects by transferring medium from donor cells to recipient cultures and monitoring responses [132]. Receptor blockade studies using neutralizing antibodies help identify specific ligand-receptor interactions, while genetic approaches using RNA interference or CRISPR-Cas9 can validate target involvement in signaling pathways [134]. Advanced imaging techniques including live-cell microscopy and fluorescence resonance energy transfer (FRET) reporters enable visualization of signaling dynamics in real-time within individual cells.
Assessment of Therapeutic Efficacy and Resistance
Evaluating the functional effects of mAbs and small molecule inhibitors on autocrine/paracrine signaling requires multifaceted assessment strategies. For signaling pathway analysis, phospho-specific flow cytometry and Western blotting can quantify changes in phosphorylation states of pathway components following treatment [99]. Gene expression profiling using RNA sequencing or RT-qPCR monitors transcriptional responses to pathway modulation, while functional assays such as cell proliferation, apoptosis, and migration measurements document phenotypic consequences [99].
In the context of cancer therapeutics, clonogenic assays and 3D spheroid models provide insights into effects on self-renewal capacity and tissue-level organization, particularly relevant for assessing disruption of autocrine/paracrine survival signals [99]. For immune-mediated diseases, co-culture systems incorporating multiple cell types (e.g., T cells, B cells, and antigen-presenting cells) better recapitulate the paracrine signaling networks operating in vivo [136]. Assessment of therapeutic resistance mechanisms should include evaluation of alternative pathway activation, target mutation analysis, and expression changes in drug transporters and metabolizing enzymes [99].
Diagram 2: Experimental Workflow for Evaluating Therapeutic Modulation of Signaling Pathways. This generalized protocol outlines key steps for investigating how monoclonal antibodies and small molecule inhibitors affect autocrine and paracrine signaling mechanisms.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 4: Essential Research Tools for Investigating Therapeutic Targeting of Signaling Pathways
| Research Tool | Application/Function | Relevance to Signaling Studies |
|---|---|---|
| Microfluidic Platforms | Precise control of cellular microenvironment and gradient formation [132] | Enables study of autocrine/paracrine signaling with spatiotemporal control |
| Neutralizing Antibodies | Block specific ligand-receptor interactions [136] | Tool for dissecting specific pathway components and mechanism validation |
| Phospho-Specific Flow Cytometry | Multiplexed quantification of signaling pathway activation [99] | Allows monitoring of intracellular signaling dynamics in mixed cell populations |
| CHO Cell Lines | Mammalian expression system for mAb production [131] | Standard platform for recombinant monoclonal antibody expression |
| Receptor Binding Assays | Measure affinity and kinetics of drug-target interactions | Fundamental for characterizing binding properties of both mAbs and small molecules |
| Kinase Activity Assays | Quantify inhibition of enzymatic activity [138] | Essential for profiling small molecule inhibitors against kinase targets |
| ADCC/CDC Reporter Assays | Evaluate Fc-mediated effector functions [134] | Assess immune-engaging capabilities of therapeutic antibodies |
| 3D Spheroid Cultures | Model tissue-level signaling and drug penetration [99] | More physiologically relevant system for studying autocrine/paracrine signaling |
| Mass Spectrometry | Characterize post-translational modifications and drug metabolism | Comprehensive analysis of signaling modifications and compound stability |
Future Perspectives and Emerging Trends
The therapeutic landscape for targeting signaling pathways continues to evolve with emerging technologies and novel approaches. Bispecific antibodies represent a promising advancement, enabling simultaneous targeting of two different antigens or engaging immune effector cells directly to target cells [130] [134]. Antibody-drug conjugates (ADCs) combine the targeting specificity of mAbs with the potent cytotoxic effects of small molecules, creating hybrid modalities that deliver payloads directly to target cells [130]. In the small molecule domain, targeted protein degradation approaches such as PROTACs (proteolysis-targeting chimeras) offer the potential to catalytically degrade disease-driving proteins rather than merely inhibiting their activity.
The integration of artificial intelligence and machine learning in drug discovery is accelerating the development of both therapeutic classes, improving prediction of drug-target interactions for small molecules and optimizing protein engineering for biologics [131]. There is also growing interest in combination approaches that leverage the complementary strengths of mAbs and small molecules, particularly in oncology where simultaneous targeting of multiple pathway components can enhance efficacy and circumvent resistance mechanisms [131]. The field is also moving toward increasingly personalized approaches, with biomarker-driven patient selection becoming standard for both therapeutic classes, exemplified by companion diagnostics for drugs like trastuzumab (HER2 testing) and EGFR inhibitors (EGFR mutation testing) [137] [135].
As our understanding of autocrine and paracrine signaling networks deepens, therapeutic interventions will likely become more sophisticated, potentially targeting multiple nodes within these networks simultaneously or sequentially based on dynamic changes in signaling pathway activation. The continued evolution of both monoclonal antibodies and small molecule inhibitors will undoubtedly provide researchers and clinicians with an expanding arsenal of targeted therapeutics for disrupting pathological signaling in inflammatory diseases, cancer, and beyond.
Biomarker Development for Patient Stratification and Treatment Response
Biomarker development represents a cornerstone of modern precision medicine, enabling a paradigm shift from a one-size-fits-all treatment approach to targeted therapies tailored to individual patient profiles. Within inflammatory disease research, biomarkers derived from the autocrine and paracrine signaling networks of inflammatory cytokines provide a powerful framework for understanding disease heterogeneity, predicting treatment response, and stratifying patient populations for clinical trial enrollment. The global blood-based biomarkers market, projected to grow from USD 8.2 billion in 2025 to USD 15.3 billion by 2035 at a compound annual growth rate (CAGR) of 6.5%, underscores the accelerating adoption and economic significance of these tools in clinical development [139]. Genetic biomarkers currently command the largest market share (33.9%), driven by their predictive diagnostic capabilities and utility in hereditary risk assessment [139].
The clinical utility of biomarkers spans the entire therapeutic development continuum, from early target discovery to post-market surveillance. In the context of inflammatory cytokines, which operate through complex autocrine (self-signaling) and paracrine (neighbor-signaling) mechanisms, biomarkers can quantify pathway activity, identify patient subpopulations with distinct molecular drivers, and monitor pharmacological intervention effects. This technical guide outlines the complete workflow for developing, validating, and implementing biomarkers for patient stratification and treatment response monitoring, with specific emphasis on methodologies relevant to inflammatory cytokine research.
Biomarker Types and Clinical Applications in Inflammatory Signaling
Biomarkers are categorized based on their specific clinical application, with each type requiring distinct validation approaches. The FDA-NIH Biomarker Working Group's BEST (Biomarkers, EndpointS, and other Tools) resource provides a standardized classification that is essential for regulatory alignment [140].
Table: Biomarker Types and Applications in Inflammatory Cytokine Research
| Biomarker Type | Clinical Application | Example in Cytokine Research |
|---|---|---|
| Susceptibility/Risk | Identifies likelihood of developing a condition | Germline variants in cytokine receptor genes (e.g., IL23R) associated with increased inflammatory disease risk |
| Diagnostic | Detects or confirms presence of a disease | Elevated serum IL-6 or TNF-α levels confirming active inflammatory state |
| Monitoring | Assesses disease status or evidence of exposure to an intervention | Serial measurements of CRP or IL-1β to track disease activity |
| Prognostic | Identifies likelihood of a clinical event or disease progression | High baseline IL-17A signature predicting more rapid disease progression in autoimmune conditions |
| Predictive | Identifies individuals more likely to respond to a specific therapy | Presence of specific autoantibodies predicting response to B-cell depletion therapy |
| Response | Indicates a biological response to a therapeutic intervention | Reduction in IL-6 or IFN-γ levels following anti-cytokine therapy |
| Safety | Indicates the likelihood of an adverse event | Development of neutralizing antibodies against biologic therapies |
Functional magnetic resonance imaging drug cue reactivity (FDCR) studies, while primarily used in substance use disorders, exemplify the biomarker development pathway. A systematic review of 415 FDCR studies found that most could potentially support biomarker development, including diagnostic (32.7%), treatment response (32.3%), and severity (19.2%) biomarkers [140]. This demonstrates the widespread potential for translating research assays into clinically useful tools.
Technical Framework for Biomarker Development
Context of Use Definition and Analytical Validation
The initial critical step in biomarker development is defining the precise Context of Use (COU)—the specific circumstances under which the biomarker will be employed and interpreted [140]. For inflammatory cytokine biomarkers intended for patient stratification, the COU must explicitly state whether the biomarker will be used for clinical trial enrichment, as a companion diagnostic, or for treatment selection in clinical practice.
Following COU definition, analytical validation establishes that the biomarker test accurately and reliably measures the intended analyte. Key performance characteristics must be demonstrated under the specified COU:
- Accuracy and Precision: For cytokine quantification assays, this requires demonstrating low intra-assay and inter-assay coefficient of variation (<15%) across the measurable range.
- Sensitivity and Specificity: Establish limits of detection (LOD) and quantification (LOQ) for cytokine measurements, particularly challenging for low-abundance analytes in complex biological matrices.
- Repeatability and Reproducibility: Demonstrate consistent performance across operators, instruments, and laboratories, especially for multisite clinical trials.
Clinical Validation and Qualification
Clinical validation establishes that the biomarker reliably predicts or measures the clinical endpoint of interest. For stratification biomarkers in inflammatory diseases, this typically requires demonstrating:
- Associations with clinical phenotypes (e.g., high IL-23 pathway activity with specific psoriatic arthritis subtypes)
- Differential treatment responses between biomarker-positive and biomarker-negative populations
- Prognostic significance independent of treatment
The clinical qualification process involves amassing evidence across multiple studies to justify use of the biomarker for its proposed COU. Regulatory agencies increasingly recognize real-world evidence alongside data from controlled clinical trials for biomarker qualification [141].
Implementation and Integration into Clinical Workflows
Successful biomarker translation requires consideration of practical implementation factors:
- Sample collection and stability for cytokine measurements in clinical settings
- Turnaround time compatible with treatment decision timelines
- Cost-effectiveness and reimbursement landscape
- Interpretation guidelines for clinicians
- Integration with electronic health records and clinical decision support systems
Experimental Methodologies for Biomarker Development
Multi-Omics Approaches for Biomarker Discovery
Comprehensive biomarker discovery requires integration of multiple analytical platforms to capture the complexity of inflammatory signaling networks. Multi-omics approaches provide complementary layers of biological information that collectively enable robust patient stratification.
Table: Multi-Omics Platforms for Inflammatory Biomarker Discovery
| Platform | Analytical Focus | Application in Cytokine Research | Key Technologies |
|---|---|---|---|
| Genomics | DNA sequence variation | Identify genetic polymorphisms in cytokine genes and receptors associated with disease susceptibility or treatment response | Whole genome sequencing, SNP arrays, targeted NGS panels |
| Transcriptomics | Gene expression patterns | Profile expression of cytokine genes and downstream signaling pathway components in patient tissues or blood | RNA sequencing, single-cell RNA-seq, nanostring |
| Proteomics | Protein abundance and modifications | Quantify cytokine protein levels and post-translational modifications in serum/plasma and tissues | Mass spectrometry, Olink, Somalogic, ELISA |
| Metabolomics | Small molecule metabolites | Identify metabolic signatures downstream of cytokine receptor activation | LC-MS, GC-MS, NMR spectroscopy |
| Epigenomics | DNA and histone modifications | Assess epigenetic regulation of cytokine gene expression in immune cell subsets | ATAC-seq, ChIP-seq, methylation arrays |
Next-generation sequencing currently leads technology utilization in the biomarkers sector with 35.2% market share, followed by PCR at 25.0% and immunoassays at 20.0% [139]. The integration of these platforms enables identification of comprehensive biomarker signatures that reflect the complexity of inflammatory diseases.
Liquid Biopsy Technologies for Minimal Invasive Monitoring
Liquid biopsies have emerged as powerful tools for non-invasive biomarker assessment, particularly valuable for serial monitoring of treatment response. By 2025, advancements are expected in:
- Enhanced sensitivity and specificity through improved circulating tumor DNA (ctDNA) analysis and exosome profiling
- Real-time monitoring of disease progression and treatment responses
- Broader applications beyond oncology into inflammatory and autoimmune diseases [141]
For cytokine research, liquid biopsies enable quantification of:
- Circulating cytokine and receptor levels
- Extracellular vesicles carrying cytokine signaling complexes
- Immune cell gene expression patterns in peripheral blood
- Proteolytic fragments generated by inflammatory processes
Single-Cell Analysis for Cellular Heterogeneity Mapping
Single-cell technologies provide unprecedented resolution for dissecting cellular heterogeneity in inflammatory diseases, enabling:
- Deeper insights into tumor microenvironments by examining individual cells within inflammatory lesions
- Identification of rare cell populations that may drive disease progression or resistance to therapy
- Integration with multi-omics data for a comprehensive view of cellular mechanisms [141]
Application to cytokine research includes:
- Single-cell cytokine secretion profiling using technologies like IsoCode or 10X Genomics
- Surface receptor expression mapping on immune cell subsets
- Transcriptional profiling of cytokine-producing cells
- Epigenetic landscape analysis of cytokine-responsive cell populations
Research Reagent Solutions for Cytokine Biomarker Development
Table: Essential Research Reagents for Inflammatory Biomarker Development
| Reagent Category | Specific Examples | Research Application |
|---|---|---|
| Cytokine Detection Antibodies | Anti-IL-6, Anti-TNF-α, Anti-IL-17, Anti-IL-23 | Quantification of cytokine levels in serum, plasma, and tissue extracts via ELISA, Luminex, or Western blot |
| Phospho-Specific Antibodies | Phospho-STAT3, Phospho-NF-κB p65 | Assessment of cytokine signaling pathway activation in patient samples |
| Recombinant Cytokines & Antagonists | Human recombinant IL-1β, IL-6, TNF-α; Anakinra (IL-1Ra) | Assay controls, pathway stimulation experiments, target validation studies |
| ELISA & Multiplex Immunoassay Kits | High-sensitivity IL-6 ELISA, 65-plex cytokine panels | Simultaneous quantification of multiple inflammatory mediators in limited sample volumes |
| Gene Expression Panels | RT² Profiler PCR Arrays for Human Cytokines & Receptors | Targeted profiling of cytokine pathway gene expression |
| Single-Cell Analysis Platforms | 10X Genomics Immune Profiling, IsoCode STAT Signaling | Characterization of cytokine responses at single-cell resolution |
| Cell-Based Reporter Assays | NF-κB luciferase reporter, STAT-responsive elements | Functional assessment of cytokine pathway activity |
| Proteomic Sample Preparation Kits | Magnetic bead-based cytokine enrichment, TMTpro 16plex | Preparation of samples for mass spectrometry-based cytokine quantification |
Signaling Pathway Visualization
Inflammatory Cytokine Signaling Network
Inflammatory Cytokine Signaling Network: This diagram illustrates the autocrine and paracrine signaling mechanisms of inflammatory cytokines, showing how initial stimuli trigger cytokine release that acts on both producer cells (autocrine) and neighboring cells (paracrine), ultimately leading to measurable biomarker production.
Biomarker Development Workflow
Biomarker Development Workflow: This flowchart outlines the key stages in translating biomarker discoveries from initial multi-omics discovery through analytical and clinical validation to regulatory qualification and clinical implementation for patient stratification.
Emerging Trends and Future Directions
Artificial Intelligence and Machine Learning Integration
By 2025, AI and ML are poised to revolutionize biomarker development through:
- Predictive Analytics: Sophisticated models that forecast disease progression and treatment responses based on biomarker profiles [141]
- Automated Data Interpretation: ML algorithms facilitating automated analysis of complex datasets, significantly reducing time required for biomarker discovery and validation [141]
- Personalized Treatment Plans: AI-driven analysis of individual patient data alongside biomarker information to develop tailored treatment approaches [141]
Application to inflammatory cytokine research includes:
- Deep learning models predicting treatment response from baseline cytokine profiles
- Natural language processing extracting biomarker-disease relationships from scientific literature
- Neural networks identifying novel biomarker combinations from high-dimensional omics data
Regulatory Science Advancements and Standardization
Regulatory frameworks are evolving to accommodate innovative biomarker approaches:
- Streamlined Approval Processes for biomarkers validated through large-scale studies and real-world evidence [141]
- Standardization Initiatives establishing validated protocols for biomarker analytical and clinical validation [141]
- Emphasis on Real-World Evidence in evaluating biomarker performance across diverse populations [141]
Patient-Centric Biomarker Development
Future biomarker development will increasingly incorporate patient perspectives:
- Informed Consent and Data Sharing practices that educate patients about biomarker testing implications [141]
- Patient-Reported Outcomes integrated into biomarker studies to provide insights into treatment effectiveness [141]
- Community Engagement ensuring diverse population representation in biomarker research [141]
The development of robust biomarkers for patient stratification and treatment response monitoring represents a critical enabling technology for precision medicine in inflammatory diseases. The complex autocrine and paracrine signaling networks of inflammatory cytokines provide both challenges and opportunities for biomarker discovery. Successful implementation requires rigorous analytical validation, clear clinical utility demonstration, and practical integration into clinical workflows. Emerging technologies—including AI-driven analysis, multi-omics integration, and advanced liquid biopsy platforms—are poised to accelerate biomarker development and validation. As these tools mature, they will enable more precise patient stratification, earlier assessment of treatment response, and ultimately improved clinical outcomes across a spectrum of inflammatory conditions.
The translation of preclinical findings into successful clinical applications remains a formidable challenge in biomedical research, particularly in the context of autocrine and paracrine signaling of inflammatory cytokines. While preclinical models have yielded invaluable insights into cytokine biology and identified promising therapeutic targets, the complex, context-dependent nature of cytokine signaling networks has contributed to numerous translational failures. This review examines the key successes and failures in this domain, analyzes the cellular and molecular mechanisms underlying translational challenges, and provides detailed experimental methodologies for enhancing the predictive validity of preclinical studies. By synthesizing evidence from recent advances in cancer immunotherapy, stromal biology, and systems immunology, we offer a framework for improving the robustness and clinical relevance of preclinical research on inflammatory cytokine networks.
Inflammatory cytokines function as critical mediators of intercellular communication through autocrine (self-signaling), paracrine (neighboring cell signaling), and endocrine (distant signaling) mechanisms [2]. The translation of preclinical discoveries targeting these pathways has proven exceptionally challenging due to the profound complexity of cytokine networks, their pleiotropic effects, and significant interspecies differences in cytokine biology [142] [127]. The failure rate of Phase III clinical trials remains notably high, with estimates suggesting that a majority fail despite promising preclinical data [142]. This challenge is particularly acute in the context of cancer immunotherapy, where inflammatory cytokines within the tumor microenvironment (TME) create complex signaling networks that influence treatment response and resistance [143] [144] [97].
A critical insight from systems biology approaches is that cytokine functions are highly context-dependent. For instance, tumor necrosis factor (TNF) exhibits stimulus-specific roles, where it functions primarily as a paracrine signal in response to lipopolysaccharide (LPS) but acquires significant autocrine functions in response to CpG DNA, extending NFκB activity duration and shaping gene expression programs [3]. This nuanced regulation underscores why targeted interventions against seemingly straightforward cytokine pathways frequently yield unexpected clinical outcomes. Understanding the network dynamics, crosstalk mechanisms, and feedback loops in cytokine signaling is therefore essential for improving translational success [3] [127].
Autocrine and Paracrine Signaling Mechanisms in the Tumor Microenvironment
Fundamental Signaling Mechanisms
Cell-cell communication (CCC) represents a fundamental process governing multicellular organism homeostasis, development, and disease pathogenesis [11]. In the context of cancer and inflammation, two primary cytokine signaling modalities operate:
Autocrine signaling: When a cell secretes cytokines that bind to receptors on its own surface, creating self-stimulatory loops that amplify inflammatory responses [3] [2]. For example, in response to CpG DNA, autocrine TNF signaling extends the duration of NFκB activity in macrophages [3].
Paracrine signaling: When cytokines secreted by one cell type exert effects on neighboring cells, enabling complex multicellular communication networks [6] [2]. Cancer-associated fibroblasts (CAFs) extensively utilize paracrine signaling through cytokines including TGF-β, IL-6, and CXCL12 to remodel the TME and promote immunosuppression [6].
The distinction between these signaling modes has profound therapeutic implications, as autocrine pathways may be targeted through cell-intrinsic mechanisms while paracrine pathways require consideration of multicellular networks.
Key Cell Types and Their Cytokine Networks
Different cell populations within the TME employ distinct autocrine and paracrine signaling programs that collectively shape the immune landscape:
Myeloid Cells: Tumor-associated macrophages (TAMs), myeloid-derived suppressor cells (MDSCs), and dendritic cells (DCs) utilize extensive paracrine signaling to suppress antitumor immunity. TAMs secrete IL-10, TGF-β, and VEGF, inhibiting T cell function and promoting angiogenesis [143] [144]. MDSCs employ metabolic reprogramming through arginase-1 (ARG1) and indoleamine 2,3-dioxygenase (IDO) to deplete essential amino acids and suppress T cell proliferation [143].
Cancer-Associated Fibroblasts (CAFs): CAFs establish a complex paracrine signaling network that orchestrates immunosuppression through multiple subtypes:
- myCAFs upregulate TGF-β to suppress T-cell activation and promote Treg differentiation [6]
- iCAFs mediate upregulation of IL-6 and CXCL12, recruiting immunosuppressive cells [6]
- apCAFs express MHC Class II molecules and induce Treg formation [6]
Tumor Cells: Cancer cells themselves frequently establish autocrine signaling loops that drive proliferation and survival. In triple-negative breast cancer (TNBC), tumor cells produce pro-inflammatory cytokines including TNF-α, TGF-β, and IL-6 that maintain chronic inflammation and support drug resistance [97].
Table 1: Key Cytokines in Autocrine and Paracrine Signaling Networks
| Cytokine | Primary Sources | Signaling Mode | Major Functions | Therapeutic Targeting Status |
|---|---|---|---|---|
| TGF-β | TAMs, CAFs, MDSCs | Paracrine | Treg differentiation, ECM remodeling, EMT | Phase III (galunisertib) [6] |
| IL-6 | iCAFs, TAMs, tumor cells | Autocrine/Paracrine | Inflammation, angiogenesis, drug resistance | Preclinical/Phase I (antibodies) [6] [97] |
| TNF-α | Macrophages, lymphocytes | Autocrine/Paracrine | NFκB activation, inflammation, cell survival | Clinical (infliximab) but limited in cancer [3] [97] |
| CXCL12 | iCAFs, endothelial cells | Paracrine | Immunosuppressive cell recruitment, metastasis | Phase II (CXCR4 antagonists) [6] |
| IL-10 | TAMs, Tregs, MDSCs | Paracrine | Immunosuppression, T cell inhibition | Preclinical development [143] [97] |
Analysis of Translational Failures: Mechanisms and Case Studies
Biological Complexity as a Barrier to Translation
The transition from promising preclinical results to failed clinical trials can frequently be attributed to oversimplified models of biological complexity:
Network Redundancy and Compensation: Cytokine networks contain extensive feedback loops and compensatory mechanisms that are frequently unmasked in clinical settings but not in simplified preclinical models. For example, targeting individual cytokines like TNF-α in rheumatoid arthritis demonstrated efficacy, but similar approaches in oncology have faced challenges due to network redundancy [3] [127].
Context-Dependent Signaling Outcomes: The same cytokine can exert opposing effects in different tissue contexts or disease stages. TNF-α signaling illustrates this principle, where it can promote antitumor immunity or drive tumor progression depending on cellular context and timing [3] [97].
Species-Specific Differences: Fundamental differences in immune system organization and cytokine responses between mice and humans significantly impact translational success. For instance, the composition and kinetics of inflammatory responses often differ substantially, leading to unexpected clinical outcomes [142].
Limitations of Preclinical Model Systems
Current preclinical models suffer from several inherent limitations that compromise their predictive value:
Immune-Compromised Models: Many xenograft models utilize immunodeficient mice that cannot recapitulate human immune responses to therapeutic interventions, particularly for immunotherapies targeting cytokine networks [142].
Simplified Microenvironments: Conventional 2D cell culture systems fail to capture the complex three-dimensional architecture and stromal components of native tissues, where paracrine signaling occurs [142] [6].
Genetic Homogeneity: Preclinical models often utilize genetically identical animals or cell lines that do not reflect the heterogeneity of human patient populations [142].
Table 2: Limitations of Preclinical Models and Potential Solutions
| Model Limitation | Impact on Translation | Enhanced Modeling Approaches |
|---|---|---|
| Syngeneic tumor models in immunocompetent mice | Limited human immune system relevance | Humanized mouse models with engrafted human immune cells |
| 2D monoculture systems | Inadequate paracrine signaling representation | 3D organoid co-culture systems with multiple cell types |
| Genetically homogeneous models | Failure to predict variable clinical responses | Diverse genetic background panels, patient-derived xenografts |
| Endpoint analyses only | Missing dynamic network adaptations | Real-time imaging, longitudinal sampling protocols |
| Standardized laboratory conditions | Lack of environmental variability | Introduction of controlled challenges and stressors [142] |
Successful Translational Strategies: Case Studies and Methodologies
Overcoming Myeloid-Mediated Immunosuppression
Strategic targeting of myeloid cells in the TME represents a promising approach that has advanced to clinical testing based on robust preclinical evidence:
CSF1R Inhibition: Preclinical studies demonstrated that colony-stimulating factor 1 receptor (CSF1R) signaling maintains immunosuppressive TAM populations in tumors. CSF1R inhibitors successfully depleted these populations in mouse models, enhancing T cell responses and improving outcomes with checkpoint blockade [143]. This approach has advanced to multiple clinical trials, with evidence of TAM modulation and potential efficacy in select malignancies.
PI3Kγ Targeting: Phosphoinositide 3-kinase gamma (PI3Kγ) was identified as a key regulator of immunosuppressive macrophage polarization in tumors. PI3Kγ inhibition reprogrammed TAMs toward an immunostimulatory phenotype and sensitized tumors to checkpoint blockade in preclinical models [143] [144]. This strategy has progressed to clinical evaluation based on these mechanistic insights.
Systems Biology Approaches to Cytokine Network Analysis
Iterative systems biology approaches have demonstrated improved predictive validity by comprehensively modeling cytokine network dynamics:
Quantitative Modeling of TNF Production: Researchers developed mathematical models of TNF production incorporating regulatory modules controlling mRNA synthesis, half-life, translation, and secretion [3]. By linking these to models of TLR and NFκB signaling networks, they predicted and experimentally validated that TNF's autocrine function is stimulus-specific—minimal in LPS response but significant in CpG DNA response [3]. This approach exemplifies how computational modeling can yield non-intuitive biological insights with translational relevance.
Single-Cell Analysis of TME Communication: Advanced single-cell RNA sequencing technologies enable comprehensive mapping of ligand-receptor interactions and communication patterns within the TME [11]. These approaches have revealed previously unappreciated heterogeneity in stromal and immune cell populations, identifying distinct CAF subsets with unique paracrine signaling programs [6].
Experimental Protocols for Enhanced Translational Predictivity
Comprehensive Cytokine Signaling Validation Workflow
Diagram 1: Experimental workflow for validating cytokine signaling interventions
Step 1: In Vitro Model Development
- Establish 3D co-culture systems incorporating relevant stromal components (CAFs, endothelial cells) and immune cells (macrophages, T cells) at physiologically relevant ratios [142] [6]
- Utilize patient-derived primary cells whenever possible to maintain genetic and phenotypic heterogeneity
- Implement conditioned media transfer experiments to distinguish paracrine from autocrine effects
Step 2: Autocrine/Paracrine Signaling Validation
- Employ cytokine neutralization antibodies in transwell systems to discriminate autocrine versus paracrine mechanisms [3]
- Implement GRASP (GFP Reconstitution Across Synaptic Partners) techniques to visualize and quantify cell-cell contacts and signaling events [11]
- Utilize phospho-specific flow cytometry to map signaling network activation in different cell populations simultaneously
Step 3: Mechanistic Studies in Relevant Preclinical Models
- Utilize orthotopic tumor models that preserve tissue-specific stromal interactions [142]
- Employ inducible genetic models to temporally control cytokine or receptor expression
- Implement intravital imaging to visualize cytokine signaling dynamics in real-time
Step 4: Systems Biology Modeling
- Develop quantitative models of cytokine production and signaling networks [3]
- Incorporate parameter variability from multiple experimental replicates and conditions
- Validate model predictions using orthogonal experimental approaches
Step 5: Robustness Assessment Under Challenge Conditions
- Test therapeutic interventions in models with varying genetic backgrounds [142]
- Introduce concurrent inflammatory challenges or metabolic stressors
- Assess efficacy across different disease stages (early versus advanced)
Research Reagent Solutions for Cytokine Signaling Studies
Table 3: Essential Research Reagents for Autocrine/Paracrine Signaling Studies
| Reagent Category | Specific Examples | Research Application | Technical Considerations |
|---|---|---|---|
| Cytokine Neutralizing Antibodies | Anti-TGF-β, Anti-IL-6, Anti-TNF-α | Discriminate autocrine vs. paracrine functions | Validate specificity; assess incomplete neutralization |
| Pathway Inhibitors | CSF1R inhibitors (PLX3397), PI3Kγ inhibitors (IPI-549) | Target specific cytokine signaling pathways | Monitor compensatory pathway activation |
| Conditioned Media Collection Systems | Serum-free collection, protease inhibition | Analyze secreted factors mediating paracrine signaling | Standardize cell numbers and collection timing |
| Cytokine Reporter Systems | NFκB-GFP, STAT3-luciferase reporters | Monitor pathway activation in live cells | Account for reporter half-life and sensitivity |
| Advanced Culture Systems | Transwell inserts, 3D organoid platforms | Segregate cellular compartments while allowing signaling | Validate barrier integrity and molecular transfer |
Visualization of Signaling Networks and Experimental Approaches
Autocrine and Paracrine Signaling Network
Diagram 2: Autocrine and paracrine signaling networks in the TME
Signaling Crosstalk and Feedback Mechanisms
Diagram 3: Signaling crosstalk and feedback mechanisms in cytokine networks
The translation of preclinical findings on autocrine and paracrine cytokine signaling into clinical success requires a fundamental shift in experimental approach. Moving beyond simplified models to embrace complexity, heterogeneity, and dynamic network regulation is essential for improving translational outcomes. Key principles for future progress include:
Embracing Systems-Level Approaches: Comprehensive computational modeling of cytokine networks that incorporates cell-type specific signaling, feedback mechanisms, and non-linear dynamics will enhance predictive accuracy [3] [127].
Incorporating Tumor Microenvironment Complexity: Preclinical models must recapitulate the multicellular ecosystems where autocrine and paracrine signaling occur, including relevant stromal components and immune populations [143] [6].
Implementing Robustness Challenges: Therapeutic candidates should be validated under diverse conditions that stress-test their efficacy, including genetic variability, concurrent inflammation, and different disease stages [142].
Leveraging Humanized Model Systems: Advanced models incorporating human immune systems and patient-derived tissue samples will better predict clinical responses [142] [145].
Developing Multi-Targeted Intervention Strategies: Given the redundancy and adaptability of cytokine networks, rational combination therapies targeting complementary pathways may prove more effective than single-target approaches [144] [6].
By adopting these principles and methodologies, the field can bridge the translational gap and more effectively harness autocrine and paracrine signaling pathways for therapeutic benefit across cancer, inflammatory diseases, and beyond.
Assessing Therapeutic Efficacy Across Autoimmune Indications
The therapeutic landscape for autoimmune diseases is undergoing a profound transformation, moving from broad immunosuppression toward targeted immunomodulation. This shift is driven by an increasingly sophisticated understanding of the autocrine and paracrine signaling networks of inflammatory cytokines that orchestrate disease pathogenesis. Assessing therapeutic efficacy in this new paradigm requires multidimensional approaches that capture not only clinical symptom reduction but also fundamental alterations in underlying immune pathways. Current strategies aim to achieve sustained drug-free remission by "resetting" the immune system through precise cellular and molecular interventions, representing a radical departure from conventional lifelong immunosuppressive regimens [146] [147]. The integration of advanced biomarker technologies and high-resolution immune monitoring now enables researchers to track these therapeutic effects with unprecedented precision, accelerating the development of next-generation autoimmune therapies.
Current Therapeutic Landscape and Efficacy Metrics
Emerging Drug Classes and Clinical Performance
Recent clinical advances have yielded several promising therapeutic classes with distinct mechanisms of action targeting specific autoimmune indications. The table below summarizes key emerging therapies and their documented efficacy profiles from recent clinical investigations.
Table 1: Recent Advancements in Autoimmune Disease Therapeutics
| Therapeutic Agent | Mechanism of Action | Autoimmune Indication | Reported Efficacy Outcomes | Stage of Development |
|---|---|---|---|---|
| Rosnilimab [148] | Depletes pathogenic T cells | Rheumatoid Arthritis | Meaningful improvement in joint pain and swelling with strong safety profile | Phase 2b Trial |
| Ianulimab [148] | Targets B-cells | Sjögren's Disease | Significant reduction in disease activity in phase III trials (NEPTUNUS-1 & NEPTUNUS-2) | Phase 3 |
| Deucravacitinib [148] | TYK2 inhibitor | Psoriatic Arthritis | Sustained benefit through full year of treatment | Phase 3 |
| CD19 CAR-T [149] [146] | B-cell depletion | SLE, Systemic Sclerosis, IIM | Sustained clinical improvement, elimination of autoantibodies, drug-free remission | Early Clinical Trials |
| BCMA-CD19 CAR-T [146] | Dual-target B-cell depletion | Multiple Autoimmune Indications | Clinical improvement in refractory patients | Early Clinical Trials |
Cardiovascular Comorbidity Monitoring in Autoimmune Disorders
Beyond disease-specific symptoms, comprehensive efficacy assessment must encompass systemic manifestations, particularly cardiovascular complications. A nationwide case-control study presented at ACR Convergence 2025 revealed that individuals with systemic lupus erythematosus (SLE) face a significantly elevated risk of cardiovascular disease and heart tissue damage compared to the general population [148]. This finding underscores the critical importance of incorporating routine cardiac monitoring into therapeutic management plans for autoimmune conditions, particularly SLE, as cardiovascular manifestations may not correlate directly with conventional disease activity metrics.
Methodologies for Efficacy Assessment in Clinical Research
Autoantibody Profiling Techniques
Serial autoantibody monitoring has emerged as a powerful methodology for predicting and assessing treatment responses across multiple autoimmune conditions and therapeutic modalities.
Table 2: Autoantibody Profiling Methodologies for Therapeutic Response Assessment
| Methodology | Technical Approach | Applications | Key Findings |
|---|---|---|---|
| REAP (Rapid Extracellular Antigen Profiling) [150] | High-throughput assay screening >6,000 autoantibodies | Cancer immunotherapy (with implications for autoimmunity) | Specific autoantibodies (e.g., interferon-blocking) associated with 5-10 fold improved response |
| MUSCAT Assay [151] | Bead-based array with 130 antigens using Luminex technology | NSCLC patients receiving immunotherapies | "Spark response" post-ICI predicts superior progression-free survival |
| SeroTag Multiplex Antibody Discovery [152] | 1,168-antigen array for autoantibody profiling | Predicting response to anti-PD-1 therapy | Baseline autoantibodies against specific targets (e.g., LIG3) associated with clinical benefit |
The experimental protocol for comprehensive autoantibody assessment typically involves:
- Sample Collection: Serial serum samples obtained at baseline, during treatment, and at follow-up intervals
- Antigen Preparation: High-purity antigen immobilization on bead-based arrays or chip platforms
- Incubation and Detection: Serum incubation with antigen panels followed by detection with fluorescent-conjugated secondary antibodies
- Data Analysis: Quantification of mean fluorescence intensity (MFI) and calculation of fold-changes across timepoints
- Response Categorization: Classification of antibody dynamics into no response (NR), weak response (WR), spark response (SR), or hyper-spark response (HSR) based on established cutoff values [151]
Cellular Reconstitution Monitoring Post-CAR-T Therapy
For cellular therapies, assessment extends beyond autoantibody reduction to comprehensive immune cell profiling. The standard protocol includes:
- Flow Cytometry: Tracking B-cell, T-cell, and plasma cell populations pre- and post-treatment
- Cytokine Measurement: Multiplex arrays to quantify inflammatory and regulatory cytokines
- Immunoglobulin Quantification: Serial measurement of immunoglobulin isotypes
- Autoantibody Specificity Testing: Monitoring pathogen-specific autoantibodies to assess immunocompetence
In patients receiving CD19 CAR-T therapy for autoimmune diseases, research has demonstrated the emergence of a naïve, non-class-switched B-cell phenotype following treatment, with most autoantibodies either disappearing or showing reduced titers [149] [146]. This reconstitution pattern correlates with sustained clinical improvement while maintaining immunocompetence.
Cytokine Signaling Pathways in Autoimmunity and Therapeutic Targeting
The Dual Nature of Cytokine Networks
Inflammatory cytokines operate through complex autocrine and paracrine signaling networks that exhibit considerable functional plasticity in autoimmune pathogenesis. The "double-edged sword" effect of cytokines represents a fundamental consideration for therapeutic targeting, as the same cytokine can mediate both protective and pathological effects depending on context, concentration, and temporal aspects of signaling [153].
Table 3: Dual-Role Cytokines in Autoimmunity and Cancer
| Cytokine | Protective/Anti-Tumor Effects | Pathological/Pro-Tumor Effects |
|---|---|---|
| IFN-γ [153] | Inhibits tumor cell growth, promotes apoptosis, upregulates MHC I, activates M1 macrophages and NK cells | Chronic exposure exhausts immune system, upregulates immunosuppressive checkpoints |
| IL-2 [153] | Drives clonal expansion of CD4+ and CD8+ T cells, enhances cytotoxic activity | |
| TGF-β [153] [94] | Early tumor suppression, reduces cell proliferation, triggers apoptosis | Promotes EMT, enhances migration/invasion, induces Treg differentiation, creates immunosuppressive microenvironment |
| IL-6 [153] [154] | Promotes B-cell differentiation, Th17 development, acute phase response, tumor proliferation via JAK/STAT3, chemoresistance | |
| IL-10 [153] | Inhibits antigen presentation, suppresses Th1 responses, promotes Treg differentiation |
Signaling Pathway Visualization
Cytokine Signaling Pathways
The diagram above illustrates the core IL-6 signaling pathway, demonstrating both classical signaling (through membrane-bound IL-6R) and trans-signaling (through soluble IL-6R), converging on JAK/STAT3 activation and culminating in pro-inflammatory and proliferative responses [154].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 4: Essential Research Reagents for Autoimmunity Therapeutic Development
| Reagent/Platform | Function | Application in Efficacy Assessment |
|---|---|---|
| Luminex Bead-Based Arrays [151] | Multiplex quantification of soluble analytes | Simultaneous measurement of cytokine profiles, autoantibody specificities |
| REAP Technology [150] | High-throughput autoantibody discovery | Comprehensive autoantibody profiling across thousands of antigens |
| MUSCAT Assay [151] | Denatured antigen immobilization for autoantibody detection | Enhanced detection of autoantibodies against unstable or aggregation-prone antigens |
| Flow Cytometry Panels [149] | Immunophenotyping of cell populations | Tracking immune cell reconstitution post-therapy, quantifying target engagement |
| CD19 CAR-T Cells [149] [146] | B-cell depletion therapy | Investigating deep B-cell depletion as therapeutic strategy for multiple autoimmune diseases |
| BCMA-CD19 CAR-T Cells [146] | Dual-target B-cell and plasma cell depletion | Targeting broader pathogenic B-cell lineage for refractory autoimmune conditions |
The assessment of therapeutic efficacy across autoimmune indications is evolving from symptom-based metrics toward multidimensional evaluation encompassing molecular resetting of immune networks, normalization of autoimmune responses, and restoration of immunologic homeostasis. The emerging toolkit of high-resolution immune monitoring technologies, coupled with increasingly sophisticated therapeutic modalities, enables researchers to quantify therapeutic effects with unprecedented precision. As our understanding of the autocrine and paracrine signaling networks in autoimmunity deepens, efficacy assessment will continue to incorporate more nuanced biomarkers of immune function, ultimately enabling truly personalized therapeutic approaches for autoimmune diseases. Future directions will likely focus on real-time immune monitoring, multi-omic integration for response prediction, and dynamic treatment adaptation based on evolving biomarker profiles.
Comparative Safety Profiles of Cytokine-Targeting Biologics
Cytokine-targeting biologics, primarily monoclonal antibodies, have revolutionized the treatment of immune-mediated diseases by offering high target specificity. Their safety profiles are intrinsically linked to the physiological roles of the cytokines they inhibit and the resulting immunomodulatory effects [155]. This whitepaper provides a comparative analysis of the safety profiles of these therapeutics, detailing the mechanisms underpinning both shared and target-specific adverse events. It further presents standardized experimental methodologies for evaluating the safety of novel biologic agents during pre-clinical and clinical development, providing a critical resource for researchers and drug development professionals working within the context of inflammatory cytokine signaling research.
Cytokines are small glycoproteins that act as pivotal mediators of cell communication, operating through autocrine and paracrine signaling pathways to regulate cellular processes including differentiation, proliferation, and activation [155]. The dysregulation of these signaling networks is a hallmark of numerous pathological states, including autoimmune diseases, chronic inflammation, and cancer [155] [29]. For instance, chronic inflammatory environments, often driven by cytokine loops involving IL-6 and TNF-α, promote cancer initiation and progression through the sustained activation of transcription factors like STAT-3 and NF-κB [29].
Biologics, such as monoclonal antibodies (mAbs), are therapeutic molecules derived from biological sources designed to intervene in these pathways with high specificity [155]. By selectively neutralizing cytokines or their receptors, these agents can precisely modulate dysregulated immune responses. However, the very precision of these therapies means that their safety profiles are directly influenced by the critical homeostatic functions of their target molecules. Blocking a cytokine with a broad physiological role, such as IL-4 or IL-6, inevitably carries a different risk profile compared to inhibiting a cytokine with a more specialized function. Understanding these profiles is essential for the rational design and clinical application of cytokine-targeting therapies.
Comparative Safety Profiles of Major Cytokine-Targeting Biologics
The safety of cytokine-targeting biologics varies significantly based on their mechanism of action and the specific cytokine pathway they inhibit. The table below summarizes the safety profiles of several key biologics, highlighting their mechanisms and associated adverse events.
Table 1: Comparative Safety Profiles of Select Cytokine-Targeting Biologics
| Biologic (Target) | Mechanism of Action | Primary Indications | Common Adverse Events | Serious/Specific Safety Concerns |
|---|---|---|---|---|
| Dupilumab (IL-4Rα) | Human IgG4 mAb; blocks shared IL-4Rα subunit, inhibiting IL-4 and IL-13 signaling [155] [156]. | Atopic dermatitis, asthma, chronic rhinosinusitis with nasal polyps [155]. | Conjunctivitis, injection site reactions, headaches [156]. | Herpetic keratitis, significant eosinophilia in some patients [156]. |
| Ustekinumab (IL-12/IL-23) | Human IgG1κ mAb; binds the p40 subunit shared by IL-12 and IL-23, reducing Th1 and Th17 inflammation [156]. | Psoriasis, psoriatic arthritis, Crohn's disease. | Upper respiratory infections, headache, fatigue. | Increased risk of serious infections; requires screening for latent tuberculosis [156]. |
| TNF-α Inhibitors (e.g., Infliximab, Adalimumab) | Neutralize TNF-α (a soluble and transmembrane protein), impeding its interaction with receptors [156]. | Rheumatoid arthritis, inflammatory bowel disease, psoriasis. | Infusion/injection site reactions, increased risk of infections. | Boxed Warning: Serious infections (e.g., reactivation of TB), malignancy (e.g., lymphoma), heart failure; paradoxical new/worsened psoriasis [156]. |
| Secukinumab (IL-17A) | Human IgG1κ mAb; selectively binds and neutralizes IL-17A [156]. | Plaque psoriasis, ankylosing spondylitis, psoriatic arthritis. | Upper respiratory tract infections, candidiasis, diarrhea. | Increased incidence of mucocutaneous candidiasis due to role of IL-17 in antifungal immunity [156]. |
| JAK Inhibitors (e.g., Tofacitinib) | Small molecules; inhibit Janus kinases (JAKs) downstream of multiple cytokine receptors, including γc family cytokines [155]. | Rheumatoid arthritis, alopecia areata. | Headache, diarrhea, nausea, upper respiratory infections. | Boxed Warning: Serious infections, malignancy, major adverse cardiovascular events (MACE), thrombosis, and death [156]. |
Analysis of Safety Profile Trends
The data reveals several key trends. First, the inhibition of broadly acting cytokines or key signaling nodes (e.g., TNF-α, JAKs) is associated with more systemic and serious safety concerns, such as elevated risks of opportunistic infections and malignancy [156]. Second, safety profiles often reflect the physiological role of the targeted pathway; for example, IL-17 inhibition predisposes patients to candidiasis, while IL-4/IL-13 blockade with dupilumab is uniquely linked to ocular surface inflammation [156]. Finally, the human or humanized nature of most mAbs generally minimizes immunogenic reactions, though injection site reactions remain common.
Experimental Protocols for Safety Assessment
A comprehensive safety assessment for cytokine-targeting biologics requires a multi-faceted experimental approach spanning from in vitro systems to clinical trials.
In Vitro Binding and Specificity Assays
Objective: To confirm the biologic's target specificity and affinity, minimizing off-target effects.
- Surface Plasmon Resonance (SPR): Used to quantify binding kinetics (KD, Kon, Koff) between the biologic and its purified target cytokine/receptor [155].
- Cell-Based ELISA/FACS: Cells expressing the target receptor are treated with the biologic and stimulated with the cytokine. Binding and blockade are detected via specific antibodies to confirm functional inhibition of the intended pathway [155].
In Vitro Functional and Cytotoxicity Assays
Objective: To evaluate the functional consequences of cytokine blockade and assess potential direct cellular toxicity.
- PBMC Proliferation/Cytokine Secretion Assay: Human Peripheral Blood Mononuclear Cells (PBMCs) are stimulated with mitogens or specific antigens in the presence of the biologic. Suppression of proliferation and cytokine release (measured by Luminex or ELISA) confirms intended immunosuppressive effects and helps identify potential cytokine release syndrome (CRS) risks [31].
- Cell Viability Assays: Representative cell lines (e.g., hepatic, renal) are cultured with a range of concentrations of the biologic. Viability is measured using MTT or AlamarBlue assays after 72 hours to screen for direct cytotoxicity unrelated to target engagement.
Ex Vivo and In Vivo Models
Objective: To assess safety in a physiologically relevant, integrated immune system.
- Human Whole Blood Assay: The biologic is added to fresh, heparinized human whole blood, which is then stimulated with LPS or other TLR agonists. The subsequent release of pro-inflammatory cytokines (e.g., TNF-α, IL-6, IL-1β) is quantified to model systemic immunosuppression and potential for increased infection risk [31].
- Repeated-Dose Toxicity Studies in Non-Human Primates (NHPs): NHPs are administered the biologic weekly for 4-13 weeks at multiples of the clinical dose. Endpoints include clinical pathology (hematology, clinical chemistry), histopathology of major organs, immunophenotyping by flow cytometry, and anti-drug antibody (ADA) assessment to gauge immunogenicity.
Clinical Trial Safety Monitoring
Objective: To identify and quantify adverse events in the target patient population.
- Phase I-III Protocols: Safety is evaluated by monitoring the incidence of Adverse Events (AEs), Serious Adverse Events (SAEs), and laboratory abnormalities. Specific attention is paid to:
- Infections: Recording all infections, with special focus on opportunistic infections.
- Malignancies: Documenting any new or recurrent malignancies.
- Cardiovascular Events: Monitoring for MACE (Major Adverse Cardiovascular Events) [156].
- Organ Function: Regular testing of hepatic, renal, and hematological function.
- Disease-Specific Biomarkers: For instance, in trials for Dupilumab, blood eosinophil counts are monitored due to the association with eosinophilia [156].
Signaling Pathways and Immunobiology
The γc family of cytokines, including IL-2, IL-4, IL-7, IL-9, IL-15, and IL-21, are critical regulators of immune cell development and function. They signal through receptor complexes that share the common gamma chain (γc) subunit, engaging the JAK-STAT pathway, primarily JAK1 and JAK3, to mediate their effects [155]. Dysregulation of this signaling is implicated in a range of diseases, from immunodeficiencies to autoimmunity and cancer [155]. The following diagram illustrates the key signaling pathways of two major cytokine families, the γc family and the IL-1/TNF-α family, which are central to the action of many biologics.
Diagram 1: Key Cytokine Signaling Pathways Targeted by Biologics. Blockade of these pathways (dashed lines) leads to therapeutic immunosuppression but also carries the class-level safety risk of increased infection.
The Scientist's Toolkit: Research Reagent Solutions
The study of cytokine biology and the development of novel biologics rely on a standardized set of research tools and reagents. The following table details essential materials and their applications in this field.
Table 2: Key Research Reagents for Investigating Cytokine-Targeting Biologics
| Reagent / Material | Function and Application in Research |
|---|---|
| Recombinant Cytokines & Antibodies | Purified human cytokines are used in in vitro stimulation assays to map signaling pathways. Target-specific antibodies (neutralizing and detecting) are crucial for ELISA, Western Blot, and Immunoprecipitation to measure cytokine levels and pathway activity [155]. |
| Engineered Cell Lines | Reporter cell lines (e.g., STAT-GFP) are engineered to express a fluorescent protein under the control of a specific transcription factor's response element (e.g., STAT6). They provide a high-throughput method to screen for biologic activity and specificity by quantifying pathway inhibition [155]. |
| JAK/STAT Pathway Inhibitors | Small-molecule inhibitors of JAKs (e.g., Tofacitinib) serve as critical tool compounds in mechanistic studies. They help delineate the contribution of specific JAK-STAT pathways to a biological effect and provide a comparator for biologic-based therapies [155] [156]. |
| Multiplex Cytokine Arrays (Luminex) | These kits allow simultaneous quantification of dozens of cytokines, chemokines, and growth factors from small volume samples (e.g., cell culture supernatant, serum). This is essential for profiling the immunomodulatory effects and potential cytokine release syndrome (CRS) risk of a candidate biologic [31]. |
| Human PBMCs and Immune Cell Subsets | Fresh or cryopreserved PBMCs from healthy donors or patients provide a physiologically relevant ex vivo system. Isolated T cell subsets (e.g., Th1, Th2, Th17, Treg), B cells, and monocytes allow for detailed cell-type-specific analysis of biologic effects on proliferation, differentiation, and function [155]. |
Emerging Targets in the Cytokine Signaling Cascade
Cytokines are a broad category of small signaling proteins (typically 5-25 kDa) that are critical for intercellular communication, particularly in immune responses, inflammation, and cellular homeostasis [22]. These molecules, which include interleukins (ILs), interferons (IFNs), tumor necrosis factors (TNFs), chemokines, and growth factors, operate through autocrine, paracrine, and occasionally endocrine mechanisms to regulate target cell functions including differentiation, proliferation, apoptosis, and survival [96] [111]. The cytokine signaling network is characterized by significant pleiotropy (where a single cytokine can have multiple effects) and redundancy (where multiple cytokines can mediate similar functions), creating a complex regulatory landscape [16] [157]. In the context of inflammatory diseases, cancer, and autoimmune disorders, the precise balance between pro-inflammatory and anti-inflammatory cytokines becomes disrupted, making specific nodes within this network attractive targets for therapeutic intervention [94] [111] [31].
Table: Major Cytokine Families and Their Primary Functions
| Cytokine Family | Key Representatives | Primary Signaling Functions |
|---|---|---|
| Interleukins (ILs) | IL-1, IL-2, IL-6, IL-10, IL-17 | Immunomodulation; T-cell differentiation; inflammation |
| Interferons (IFNs) | IFN-α, IFN-β, IFN-γ | Antiviral defense; anti-tumor immunity; immune activation |
| Tumor Necrosis Factor (TNF) Superfamily | TNF-α | Pro-inflammatory signaling; apoptosis; cell survival |
| Chemokines | CXCL8, CCL2, CCL5 | Chemoattraction; leukocyte trafficking |
| Growth Factors | TGF-β, VEGF, EGF | Cell growth; differentiation; tissue repair |
Key Emerging Targets in the Cytokine Cascade
The cGAS-STING Signaling Pathway
The cyclic GMP-AMP synthase-stimulator of interferon genes (cGAS-STING) pathway is a central mediator of innate immunity, serving as a cytosolic DNA sensor [158]. Upon binding double-stranded DNA (dsDNA), cGAS synthesizes the second messenger 2'3'-cGAMP, which activates STING on the endoplasmic reticulum membrane. Activated STING then traffics to the Golgi, recruiting and activating TBK1 kinase, which phosphorylates IRF3, leading to the production of type I interferons and pro-inflammatory cytokines [158]. This pathway is emerging as a critical target in cancer immunotherapy, inflammatory dermatoses, and autoimmune diseases. In cancer, STING agonists are being developed to enhance anti-tumor immunity, while in conditions like psoriasis and systemic lupus erythematosus (SLE), cGAS-STING inhibitors may ameliorate pathogenic inflammation driven by self-DNA [158]. The pathway's role is complex, as chronic STING activation can lead to a suppressive tumor microenvironment, highlighting the need for context-specific modulation.
Pleiotropic Cytokines with Dual Roles: TGF-β and IL-6
Transforming Growth Factor-beta (TGF-β) and Interleukin-6 (IL-6) exemplify the contextual duality of cytokine function, presenting both challenges and opportunities for therapeutic targeting. TGF-β signaling switches from a tumor-suppressive role in healthy and early-stage tumor cells to a pro-tumorigenic factor in advanced cancers, promoting epithelial-to-mesenchymal transition (EMT), metastasis, and fibrosis [94]. Similarly, IL-6, through its classic and trans-signaling pathways, can drive both pro- and anti-inflammatory responses. In chronic inflammatory diseases and cancer, IL-6 contributes to pathologic inflammation, immune evasion, and resistance to therapy [94] [111]. Emerging strategies aim to selectively inhibit the pathogenic arms of these cytokines' signaling, such as using TGF-β traps or IL-6 trans-signaling inhibitors, while preserving their homeostatic functions, thereby improving therapeutic windows and reducing off-target effects.
Chemokine Networks in the Tumor Microenvironment
Chemokines such as CXCL8, CCL2, and CXCL12 are critical organizers of immune cell infiltration into tumors [94]. These molecules and their receptors (e.g., CXCR2, CCR2, CXCR4) establish spatial networks within the tumor microenvironment (TME) that can either promote or inhibit anti-tumor immunity. For instance, CXCL8 attracts pro-tumorigenic neutrophils and promotes angiogenesis, while CCL2 recruits immunosuppressive tumor-associated macrophages (TAMs) [94]. Emerging therapeutic approaches include small-molecule receptor antagonists and neutralizing antibodies designed to disrupt these protumorigenic chemokine gradients, thereby re-engineering the TME to be more permissive to immune attack. In idiopathic pulmonary fibrosis (IPF), recent proteomic analyses have identified CXCL8 as a central hub protein, further underscoring its broad role in fibro-inflammatory disease [159].
Novel Agonists for Immunostimulatory Cytokines
There is a renewed interest in harnessing the power of endogenous immunostimulatory cytokines like IL-2, IL-12, IL-15, and IFN-α for cancer therapy [94]. However, their clinical application has been limited by severe toxicity and poor pharmacokinetics. Emerging strategies focus on engineering novel agonists with improved safety profiles. These include:
- Cytokine variants with mutated receptor-binding domains to bias signaling toward desired immune subsets (e.g., IL-2 mutants with reduced CD25 binding to avoid Treg expansion).
- Fusion proteins that tether cytokines to tumor-specific antibodies or extracellular matrix components to localize activity.
- PEGylated formulations to extend half-life and reduce dosing frequency, as seen with approved IFN-α therapies [94].
These engineered molecules seek to maximize the antitumor effects of cytokine therapy—such as enhanced NK and CD8+ T cell activation—while minimizing systemic toxicity.
Table: Emerging Cytokine Targets and Their Therapeutic Modalities
| Emerging Target | Associated Pathway | Therapeutic Approach | Clinical Context |
|---|---|---|---|
| STING | cGAS-STING | Agonists (e.g., cGAMP analogs); Inhibitors (e.g., palmitoylation blockers) | Cancer immunotherapy, Inflammatory skin diseases |
| TGF-β | SMAD-dependent & independent | Neutralizing antibodies, Receptor kinase inhibitors, "Trap" molecules | Cancer, Fibrotic diseases |
| IL-6 | JAK-STAT | mAbs (e.g., Tocilizumab), trans-signaling inhibitors | Rheumatoid arthritis, Cytokine release syndrome |
| CXCL8/CXCR2 | Chemokine signaling | Small molecule antagonists (e.g., CXCR2 inhibitors) | Cancer (e.g., IPF), Chronic inflammation |
| Engineered IL-2 | JAK-STAT, PI3K-AKT | Mutated cytokines with biased receptor affinity | Cancer |
Quantitative Analysis and Systematic Investigation of Cytokine Activity
The study of cytokine signaling is being revolutionized by systematic, data-driven approaches. The Cytokine Signaling Analyzer (CytoSig) platform addresses the challenges of pleiotropy and redundancy by leveraging a large compendium of 20,591 transcriptomic profiles from human cytokine response experiments [16] [157]. This resource enables researchers to infer cytokine signaling activity from bulk or single-cell RNA-sequencing data of patient samples, moving beyond simple cytokine concentration measurements to a more functional understanding of pathway activity. In severe COVID-19, for example, CytoSig analysis identified CXCL8 signaling as a primary driver of adverse inflammation, nominating it as a therapeutic target [16] [157]. Furthermore, integrative proteomic studies in diseases like IPF are mapping entire cytokine interaction networks, identifying central "hub" proteins like FGF2, HGF, and ANGPT2 that coordinate profibrotic signaling and represent promising targets for multi-ligand inhibition strategies [159].
Experimental Protocols for Profiling Cytokine Signaling
Transcriptomic Profiling of Cytokine Responses
A primary method for systematically investigating cytokine signaling involves generating and analyzing transcriptomic profiles from cytokine-stimulated cells [16] [157].
Detailed Methodology:
- Cell Model Selection: Use relevant primary human cells (e.g., peripheral blood mononuclear cells - PBMCs, specific T cell subsets, monocytes) or appropriate cell lines. The choice of cell model is critical as the response is highly cell-type-specific.
- Cytokine Stimulation: Treat cells with a single cytokine or a defined combination. A range of physiologically relevant concentrations (e.g., pM to nM) and time points (e.g., 30 min to 24 hours) should be tested to capture both early and late response genes.
- RNA Extraction and Sequencing: Harvest cells and extract total RNA. Prepare RNA-sequencing (RNA-seq) libraries following standard protocols (e.g., poly-A selection) and sequence on an appropriate platform (e.g., Illumina) to a sufficient depth (e.g., 20-30 million reads per sample).
- Data Processing and Signature Generation: Align sequence reads to a reference genome (e.g., GRCh38). Perform differential expression analysis (e.g., using DESeq2 or edgeR) comparing treated samples to untreated controls. The resulting list of genes with their log2 fold changes constitutes the cytokine response signature.
Predicting Signaling Activity from Transcriptomic Data
The CytoSig platform provides a protocol to infer active cytokine pathways from custom transcriptomic datasets [16] [157].
Detailed Methodology:
- Input Data Preparation: Prepare a gene expression matrix (counts or TPMs) from bulk tissue or single-cell RNA-seq data.
- Activity Inference: Submit the data to the CytoSig web platform (https://cytosig.ccr.cancer.gov/) or use the standalone software. The algorithm compares the input gene expression profile against its database of known cytokine response signatures.
- Result Interpretation: The output is a Z-score for each cytokine, indicating the level of enrichment for its target genes in the sample. A high positive Z-score suggests active signaling for that specific cytokine pathway in the sampled tissue or cell population.
Validating Hub Protein Function in Complex Tissues
For targets identified via proteomics or bioinformatics, such as in IPF, functional validation is key [159].
Detailed Methodology:
- Spatial Localization: Perform immunohistochemistry (IHC) or immunofluorescence (IF) on formalin-fixed paraffin-embedded (FFPE) patient tissue sections using validated antibodies against the hub protein (e.g., HGF, FGF2).
- Cellular Source Identification: Integrate with single-cell RNA-sequencing (scRNA-seq) data from the same disease context to identify the specific cell populations expressing the hub protein and its receptor.
- Functional Blocking: In ex vivo or in vivo models, apply specific neutralizing antibodies or small-molecule inhibitors against the hub protein and assess phenotypic outcomes (e.g., reduction in fibroblast activation or collagen deposition).
Visualization of Signaling Pathways and Experimental Workflows
cGAS-STING Signaling Pathway
cGAS-STING Pathway Diagram
CytoSig Experimental and Analytical Workflow
CytoSig Workflow Diagram
The Scientist's Toolkit: Key Research Reagent Solutions
Table: Essential Research Reagents for Cytokine Signaling Studies
| Reagent / Solution | Primary Function | Example Application |
|---|---|---|
| Recombinant Cytokines | To stimulate signaling pathways in vitro | Treatment of cell cultures to generate reference transcriptomic signatures [16] [157] |
| Phospho-Specific Antibodies | Detect activation of signaling intermediates | Western blot for p-IRF3, p-STATs to confirm pathway engagement [158] |
| Neutralizing Antibodies | Block specific cytokine-receptor interactions | Functional validation of target identity in vitro and in vivo [94] [159] |
| Multiplex Immunoassays (Luminex) | Quantify multiple cytokine concentrations simultaneously | Measuring cytokine release in patient serum or cell culture supernatant [16] |
| scRNA-seq Kits | Profile gene expression at single-cell resolution | Identifying cellular sources and targets of cytokines in complex tissues [159] |
| cGAS/STING Inhibitors & Agonists | Modulate the cGAS-STING pathway | Probing the role of cytosolic DNA sensing in disease models [158] |
| JAK/STAT Inhibitors | Block downstream signaling from multiple cytokine receptors | Functional dissection of cytokine signaling dependencies [94] |
Novel Delivery Systems for Localized Cytokine Modulation
Cytokines are potent signaling proteins, typically under 30 kDa, that orchestrate immune responses by binding to specific cell surface receptors in autocrine (same cell) and paracrine (neighboring cell) fashions [160]. This local signaling is crucial for maintaining immune homeostasis, but its pleiotropic and concentration-dependent nature means that systemic administration for therapeutic purposes often leads to significant challenges, including rapid degradation, short serum half-life, and severe dose-limiting toxicities [161] [162]. The clinical translation of cytokine therapies has therefore been hampered by the fundamental conflict between delivering effective doses and avoiding harmful side effects [161].
The paradigm is shifting from systemic delivery to localized modulation, aligning with the physiological context of autocrine and paracrine signaling. Novel delivery systems are being engineered to target cytokines to specific tissues, cell types, or even subcellular compartments, thereby reactivating or suppressing immune responses precisely where needed [163] [162]. This whitepaper provides an in-depth technical guide to the leading platforms in this field, detailing their mechanisms, experimental validation, and application within immuno-oncology and inflammatory disease research.
Platform Technologies for Cytokine Delivery
Advanced delivery systems are designed to overcome the pharmacokinetic and pharmacodynamic limitations of native cytokines. The following table summarizes the key characteristics of the major platforms.
Table 1: Comparison of Novel Cytokine Delivery Systems
| Delivery System | Core Mechanism | Key Advantages | Primary Challenges | Therapeutic Context |
|---|---|---|---|---|
| Pegylated Cytokines [161] | Covalent bonding of cytokines to polyethylene glycol (PEG) polymers. | Prolongs circulating half-life, reduces dosing frequency. | Pegylation can alter cytokine conformation and bioactivity. | Oncology (e.g., NKTR-214, a pegylated IL-2) [161]. |
| Immuno-cytokine Drug Conjugates [163] | Fusion of cytokines with tumor-specific antibodies (e.g., L19). | Enables specific targeting to tumor microenvironments (TME). | Requires well-defined, tumor-specific cell surface markers. | Solid tumors (e.g., L19-IL-2 for glioblastoma) [163]. |
| Activity-on-Target Cytokines (AcTakines) [161] | Modified cytokines attached to delivery systems targeting cell-specific markers. | Dramatically limits systemic exposure and off-target effects. | Requires tumor-specific antigens or cell-specific markers. | Pre-clinical development for targeted immunotherapy. |
| Liposomes [164] [162] | Cytokine encapsulation within lipid bilayer vesicles. | Protects cargo from degradation; biocompatible; allows sustained release. | Stability, encapsulation efficiency, potential lysosomal degradation. | Cancer vaccines, intratumoral injection, T-cell priming [162]. |
| Polymeric Nanoparticles (e.g., PLGA) [162] [165] | Cytokine encapsulation within biodegradable polymer matrices. | Controlled release kinetics; tunable degradation; protection of cargo. | Exposure to organic solvents during synthesis can denature proteins. | Sustained release depot for vaccines and cancer therapy [162] [165]. |
| Cell Membrane-Coated Nanoparticles (CNPs) [163] | Nanoparticles coated with native cell membranes. | Inherent bio-interfaces for cytokine neutralization or targeted delivery. | Complex fabrication process; batch-to-batch consistency. | Cytokine neutralization in sepsis and autoimmune diseases [163]. |
Detailed Methodologies and Experimental Protocols
Synthesis of Cytokine-Loaded PLGA Nanoparticles
The water-in-oil-in-water (W/O/W) double emulsion solvent evaporation technique is a standard method for encapsulating hydrophilic cytokines like IL-2 or IL-12 within PLGA nanoparticles [162] [165]. The following protocol details the critical steps for reproducibility and maintaining cytokine bioactivity.
Experimental Protocol: W/O/W Double Emulsion
- Primary Emulsion (W/O): Dissolve 50-100 mg of PLGA (e.g., 50:50 lactide:glycolide ratio) in 2 mL of dichloromethane (DCM) as the organic phase. The aqueous phase consists of 0.1-0.5 mL of an aqueous solution containing 10-50 µg of the recombinant cytokine (e.g., IL-12) stabilized with 1% (w/v) bovine serum albumin (BSA). Add the aqueous cytokine solution to the PLGA/DCM solution and emulsify using a high-speed homogenizer (e.g., 10,000 rpm for 60 seconds) or a probe sonicator (e.g., 50 W for 30 seconds) on ice to form the primary water-in-oil emulsion.
- Secondary Emulsion (W/O/W): Pour the primary emulsion immediately into 10 mL of an external aqueous phase containing 2-5% (w/v) polyvinyl alcohol (PVA) as a stabilizer. Homogenize this mixture a second time (e.g., 5,000 rpm for 120 seconds) to form a stable double emulsion.
- Solvent Evaporation: Transfer the double emulsion to a beaker containing 50-100 mL of a 0.1-0.3% PVA solution. Stir continuously for 3-4 hours at room temperature to allow the organic solvent (DCM) to evaporate, solidifying the nanoparticles.
- Nanoparticle Collection: Collect the nanoparticles by ultracentrifugation (e.g., 20,000 × g for 30 minutes at 4°C). Wash the pellet 2-3 times with purified water to remove residual PVA and unencapsulated cytokine.
- Lyophilization: Resuspend the final nanoparticle pellet in a cryoprotectant solution (e.g., 5% trehalose) and lyophilize for long-term storage. The encapsulation efficiency can be determined by quantifying the unencapsulated cytokine in the supernatant using an ELISA kit [162] [165].
Engineering and Evaluation of Immunocytokines
Immunocytokines, such as the L19-IL-2 fusion, are designed for targeted delivery to the tumor microenvironment [163].
Experimental Protocol: L19-IL-2 Fusion Protein Evaluation
- Genetic Construction and Expression: Clone the gene sequences for the single-chain variable fragment (scFv) of the L19 antibody (specific for the EDB domain of fibronectin) and human IL-2 into an appropriate expression vector, separated by a flexible peptide linker. Transfect the construct into a mammalian expression system like CHO or HEK293 cells.
- Protein Purification: Harvest the culture supernatant and purify the fusion protein using affinity chromatography (e.g., Ni-NTA resin if a His-tag is incorporated) followed by size-exclusion chromatography to ensure purity and correct oligomeric state.
- In Vitro Binding Assay: Validate target binding using ELISA. Coat a 96-well plate with recombinant EDB-fibronectin. After blocking, add serially diluted L19-IL-2 fusion protein. Detect binding using an antibody against the IL-2 moiety or the Fc region of the fusion construct. The L19 antibody moiety should confer high-affinity binding to EDB-fibronectin compared to an irrelevant control antibody fusion.
- In Vivo Biodistribution: Inject tumor-bearing mice intravenously with the purified L19-IL-2 fusion protein. After 24-48 hours, harvest organs (tumor, liver, spleen, kidney, lung) and analyze cytokine concentration in tissue homogenates by ELISA. The L19-IL-2 construct is expected to show significantly higher accumulation in EDB-positive tumor tissue compared to healthy organs [163].
- In Vivo Efficacy: Administer the L19-IL-2 fusion protein to mice with established syngeneic or xenograft tumors. Monitor tumor volume over time and compare to groups treated with saline, free IL-2, or a non-targeted IL-2 fusion. A significant reduction in tumor growth in the L19-IL-2 group demonstrates targeted efficacy [163].
Diagram 1: Immunocytokine targeting tumor vasculature.
The Scientist's Toolkit: Essential Research Reagents
Successful research in this field relies on a suite of specialized reagents and materials. The following table lists key items for developing and testing novel cytokine delivery systems.
Table 2: Essential Research Reagents for Cytokine Delivery Studies
| Reagent / Material | Function / Purpose | Technical Notes |
|---|---|---|
| PLGA (Poly(lactic-co-glycolic acid)) [162] [165] | Biodegradable polymer matrix for nanoparticle formation; enables controlled release. | Vary lactide:glycolide ratio (e.g., 50:50, 75:25) to tune degradation rate from weeks to months. |
| DSPC / Cholesterol [164] [162] | Lipid components for forming stable liposomal bilayers. | Cholesterol incorporation (30-50 mol%) enhances membrane stability and modulates cytokine release kinetics. |
| Polyvinyl Alcohol (PVA) [162] [165] | Stabilizer and surfactant in W/O/W emulsion synthesis of polymeric nanoparticles. | Critical for controlling nanoparticle size and polydispersity during formulation. |
| PEG Derivatives (e.g., mPEG-NHS) [161] [162] | For pegylation to extend half-life or create "stealth" nanoparticles that evade immune clearance. | "Stealth" liposomes/Particles with PEG coatings exhibit longer circulation times. |
| Recombinant Cytokines (IL-2, IL-12, IFN-γ) [162] | The active therapeutic cargo for encapsulation or conjugation. | Bioactivity must be verified post-encapsulation; sensitive to organic solvents and interfaces. |
| ELISA Kits (Cytokine-specific) [162] | Quantifying cytokine concentration in supernatants, serum, and tissue homogenates. | Used to determine encapsulation efficiency, release profiles, and biodistribution. |
| Target-Specific Antibodies (e.g., anti-EDB) [163] | Targeting moieties for constructing immunocytokines or functionalized nanoparticles. | scFv formats are commonly used for genetic fusion to cytokines. |
Advanced Engineering Strategies
Prodrug Approaches and Activity-on-Target Cytokines
To achieve maximal specificity, "masked" cytokines or prodrugs are engineered to become active only within the target microenvironment. A prime example is an IL-2 prodrug where the cytokine is fused to its receptor β (IL2Rβ) via a tumor protease-sensitive linker [163]. In this inactive state, the IL-2 is blocked by its own soluble receptor. Upon encountering tumor-specific proteases (e.g., matrix metalloproteinases), the linker is cleaved, releasing active IL-2 to stimulate local T-cells and NK cells. This strategy has demonstrated superior tumor accumulation and reduced systemic toxicity compared to active IL-2 administration [163].
Nanocarrier Functionalization for Targeted Delivery
Beyond encapsulation, nanocarriers can be surface-functionalized with targeting ligands. For instance, the von Willebrand factor's A3 collagen-binding domain (CBD) has been fused with IL-2, directing the cytokine to collagen proteins that are abundantly exposed in the leaky vasculature of tumors [163]. In vivo studies showed selective accumulation of CBD-IL-2 in tumor sites and significantly reduced off-target accumulation in organs like the liver and kidneys, enhancing the therapeutic index [163].
Diagram 2: Experimental workflow for nanoparticle evaluation.
The evolution of cytokine therapeutics is inextricably linked to advances in delivery technologies. The platforms discussed—from targeted immunocytokines and smart prodrugs to versatile nanocarriers—represent a powerful toolkit for achieving localized cytokine modulation that mirrors physiological autocrine and paracrine signaling. These systems directly address the historical limitations of systemic toxicity and rapid clearance, enabling the full therapeutic potential of cytokines to be harnessed in oncology, regenerative medicine, and the treatment of inflammatory diseases. As these technologies mature, the focus will shift towards optimizing their clinical scalability, manufacturing reproducibility, and navigating regulatory pathways, ultimately paving the way for a new generation of precise and effective immunotherapies.
Conclusion
The intricate networks of autocrine and paracrine inflammatory cytokine signaling represent fundamental mechanisms governing immune homeostasis, disease pathogenesis, and therapeutic responses. This synthesis reveals how foundational understanding of these pathways, combined with advanced methodological approaches, enables researchers to overcome technical challenges and develop targeted interventions. The future of this field lies in leveraging emerging technologies—from sophisticated microfluidic platforms to optogenetic tools—to achieve unprecedented spatial and temporal control in studying these complex systems. For drug development professionals, the key implication is the growing potential for highly specific therapeutic strategies that target pathological autocrine/paracrine loops while preserving physiological signaling. Future research should focus on understanding context-dependent signaling outcomes, developing next-generation models that better recapitulate human disease microenvironments, and advancing personalized approaches that account for inter-patient variability in cytokine network architecture. The continued elucidation of these sophisticated communication systems promises to unlock novel therapeutic paradigms across autoimmune diseases, cancer, and chronic inflammatory conditions.
References
- 1. Types of Signals | Biology for Majors I [https://courses.lumenlearning.com/wm-biology1/chapter/reading-types-of-signals/]
- 2. What are Cytokines? Types & Function [https://my.clevelandclinic.org/health/body/24585-cytokines]
- 3. Network dynamics determine the autocrine and paracrine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4180974/]
- 4. Distinguishing autocrine and paracrine signals in ... [https://www.nature.com/articles/srep31951]
- 5. Quantitative variation in autocrine signaling and pathway ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3084603/]
- 6. Paracrine signaling in cancer-associated fibroblasts [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06744-4]
- 7. Dynamic allostery: a novel mechanism regulating autocrine ... [https://www.nature.com/articles/s41392-024-02099-2]
- 8. Inflammatory cytokine - Wikipedia [https://en.wikipedia.org/wiki/Inflammatory_cytokine]
- 9. Inflammatory Cytokines | Sino Biological [https://www.sinobiological.com/resource/cytokines/all-proinflammatory-cytokines]
- 10. Pro-Inflammatory Cytokines Overview | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/life-science/cell-analysis/cell-analysis-learning-center/immunology-at-work/proinflammatory-cytokines-overview.html]
- 11. Cell–cell communication: new insights and clinical ... [https://www.nature.com/articles/s41392-024-01888-z]
- 12. Ten simple rules for creating reusable pathway models for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8375987/]
- 13. Immunomodulatory Mechanisms of Chronic Wound Healing [https://pmc.ncbi.nlm.nih.gov/articles/PMC12538007/]
- 14. The emerging role of tissue regulatory T cells in ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1640113/full]
- 15. Dictionary of immune responses to cytokines at single-cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10781646/]
- 16. Systematic investigation of cytokine signaling activity at the ... [https://www.nature.com/articles/s41592-021-01274-5]
- 17. Dynamic allostery drives autocrine and paracrine TGF-β ... [https://www.sciencedirect.com/science/article/pii/S0092867424009656]
- 18. Inflammatory Cytokines That Enhance Antigen ... [https://www.mdpi.com/1422-0067/23/22/14122]
- 19. CellNEST reveals cell–cell relay networks using attention ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12240806/]
- 20. Editorial: Autoimmunity: novel insights and future perspectives [https://pmc.ncbi.nlm.nih.gov/articles/PMC12615490/]
- 21. Immune cell senescence in autoimmunity: implications for ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1596686/full]
- 22. Cytokine [https://en.wikipedia.org/wiki/Cytokine]
- 23. Mathematical modeling in autoimmune diseases [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1371620/full]
- 24. Research trends and visualization analysis of autoimmune ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12214184/]
- 25. The “double-edged sword†effect of cytokines in cancer [https://www.frontiersin.org/articles/10.3389/fimmu.2025.1701405/full]
- 26. The cytokines in tumor microenvironment: from cancer ... [https://www.sciencedirect.com/science/article/abs/pii/S1040842824000544]
- 27. Dynamics of inflammatory signals within the tumor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12019612/]
- 28. Paracrine Signalling - an overview [https://www.sciencedirect.com/topics/medicine-and-dentistry/paracrine-signalling]
- 29. Chronic Stress Mediates Inflammatory Cytokines Alterations ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11769853/]
- 30. Dual roles and therapeutic targeting of tumor-associated ... [https://www.nature.com/articles/s41392-025-02325-5]
- 31. Cytokines in sepsis: a critical review of the literature on ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1682306/full]
- 32. Advancing Biomedical Data Visualization for ... [https://www.elucidata.io/blog/data-visualization-connecting-the-dots-in-biomedical-research]
- 33. An explorable model of an adverse outcome pathway ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12371706/]
- 34. An NF-kB/TNF-alpha signalling feedback loop acts to ... [https://www.nature.com/articles/s41536-025-00414-1]
- 35. A body–brain circuit that regulates body inflammatory ... [https://www.nature.com/articles/s41586-024-07469-y]
- 36. Positioning of negative feedback loops within immune ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12157479/]
- 37. Paracrine Signalling - an overview [https://www.sciencedirect.com/topics/agricultural-and-biological-sciences/paracrine-signalling]
- 38. The Hippo pathway kinase MST1 mediates a feedback ... [https://www.sciencedirect.com/science/article/pii/S2211124725008472]
- 39. 9.2: Signaling Molecules and Cellular Receptors - Forms of ... [https://bio.libretexts.org/Bookshelves/Introductory_and_General_Biology/General_Biology_(Boundless)/09%3A_Cell_Communication/9.02%3A_Signaling_Molecules_and_Cellular_Receptors_-_Forms_of_Signaling]
- 40. Physiology, Cellular Messengers - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK538154/]
- 41. Auto Paracrine Signaling Mechanism & Stem Cell ... [https://stemcellthailand.org/paracrine-signaling/]
- 42. Comparison of methods and resources for cell ... [https://www.nature.com/articles/s41467-022-30755-0]
- 43. Pancreatic endocrine and exocrine signaling and crosstalk ... [https://www.nature.com/articles/s41392-024-02098-3]
- 44. Reconfigurable open microfluidics for studying the spatiotemporal dynamics of paracrine signalling - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7543914/]
- 45. B-Cell Populations in Focus: A New Flow Cytometry Assay ... [https://cellcarta.com/science-hub/bcell-flow-cytometry-autoimmune-research/]
- 46. Microfluidic platform for the study of intercellular communication via soluble factor-cell and cell-cell paracrine signaling - PubMed [https://pubmed.ncbi.nlm.nih.gov/25379089/]
- 47. Recovery of phenotypically sorted cells using droplet-digital ... [https://pubs.rsc.org/en/content/articlehtml/2025/lc/d5lc00415b]
- 48. Empowering single-cell analysis with emerging active ... [https://www.sciencedirect.com/science/article/abs/pii/S0142961225005368]
- 49. Tracking inflammation status for improving patient prognosis [https://pmc.ncbi.nlm.nih.gov/articles/PMC12173025/]
- 50. Quantitative, Label-Free Detection of Five Protein ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2800857/]
- 51. Microfluidic-Based Electrical Operation and Measurement ... [https://www.mdpi.com/1424-8220/24/19/6359]
- 52. Volume 22 Issue 1, January 2025 [https://www.nature.com/nmeth/volumes/22/issues/1]
- 53. Optogenetic and Endogenous Modulation of Ca 2 ... [https://pubmed.ncbi.nlm.nih.gov/41009647/]
- 54. Optogenetic and Endogenous Modulation of Ca 2 ... [https://www.mdpi.com/1422-0067/26/18/9082]
- 55. Simultaneous Optogenetics and Cellular Resolution ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6066578/]
- 56. Designed optogenetic tool for bridging single-neuronal ... [https://www.nature.com/articles/s41467-025-62938-w]
- 57. The Calci-Inflammatory Network: A Paradigm Shift in ... [https://www.mdpi.com/2624-862X/6/3/22]
- 58. Understanding chronic inflammation: couplings between ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1558263/full]
- 59. Deep insight into cytokine storm: from pathogenesis to ... [https://www.nature.com/articles/s41392-025-02178-y]
- 60. Research progress on the mechanisms of interleukin and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12463896/]
- 61. Method standardization of secretome production, collection ... [https://www.sciencedirect.com/science/article/pii/S2352320425000811]
- 62. Bioinformatics tools for secretome analysis [https://pubmed.ncbi.nlm.nih.gov/23395702/]
- 63. nELISA: a high-throughput, high-plex platform enables ... [https://www.nature.com/articles/s41592-025-02861-6]
- 64. Application of Mass Cytometry (CyTOF) for Functional and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5304457/]
- 65. A physical wiring diagram for the human immune system [https://www.nature.com/articles/s41586-022-05028-x]
- 66. Bioinformatics analysis [https://genoskin.com/bioinformatics-analysis/]
- 67. Comparing Gene Editing Platforms: CRISPR vs. Traditional ... [https://blog.crownbio.com/comparing-gene-editing-platforms-crispr-vs-traditional-methods]
- 68. Applications of multiplexed CRISPR–Cas for genome ... [https://www.nature.com/articles/s12276-025-01500-6]
- 69. The role of CRISPR-Cas9 and CRISPR interference ... [https://www.sciencedirect.com/science/article/abs/pii/S156899722500076X]
- 70. Inflammatory Cytokines and Chemokines Are ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11047649/]
- 71. Key aspects for conception and construction of co-culture ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10119418/]
- 72. Comparative analysis of co-culture and monoculture models ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10515208/]
- 73. A 2D inflammatory co-culture model for investigating ... [https://www.nature.com/articles/s41598-025-16007-3]
- 74. From 2D to 3D Co-Culture Systems: A Review of Co- ... [https://www.mdpi.com/1422-0067/23/21/13116]
- 75. A quantitative meta-analysis comparing cell models in ... [https://www.nature.com/articles/s41598-023-35043-5]
- 76. A scalable human gut-immune co-culture model for ... [https://www.sciencedirect.com/science/article/pii/S2472555225000413]
- 77. A review of co-culture models to study the oral ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7448840/]
- 78. Frontiers | Tumor-Induced Inflammatory and the Emerging... Cytokines [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2021.692142/full]
- 79. Stromal Cell -Derived Factor-1a Autocrine / Paracrine ... Signaling [https://pmc.ncbi.nlm.nih.gov/articles/PMC7878637/]
- 80. Modular, open-sourced multiplexing for democratizing spatial ... [https://pubs.rsc.org/en/content/articlehtml/2025/lc/d5lc00286a]
- 81. Systematic benchmarking of high-throughput subcellular ... [https://www.nature.com/articles/s41467-025-64292-3]
- 82. Flow Cytometry: From Arbitrary Units to Quantitative Science [https://www.sepscience.com/flow-cytometry-from-arbitrary-units-to-quantitative-science-12122]
- 83. Cytofast: A workflow for visual and quantitative analysis of ... [https://www.sciencedirect.com/science/article/pii/S200103701830059X]
- 84. Autocrine Signalling - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/neuroscience/autocrine-signalling]
- 85. Demystifying the cytokine network: Mathematical models point ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5457394/]
- 86. Fostering experimental and computational synergy to ... [https://www.sciencedirect.com/science/article/pii/S1471490621002404]
- 87. Computational modeling of cytokine signaling in microglia [https://pmc.ncbi.nlm.nih.gov/articles/PMC5520540/]
- 88. Mathematical model of the inflammatory response to acute ... [https://www.nature.com/articles/s41540-024-00473-y]
- 89. BioNetGen: Home [https://bionetgen.org/]
- 90. Conversion of natural cytokine receptors into orthogonal ... [https://www.nature.com/articles/s41589-025-01986-1]
- 91. Macrophage Signaling Pathways in Health and Disease [https://pmc.ncbi.nlm.nih.gov/articles/PMC12171086/]
- 92. Reprogramming the tumor microenvironment to boost ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1677548/full]
- 93. Disentangling the Complexity of HGF Signaling by Combining ... [https://journals.plos.org/ploscompbiol/article%3Fid%3D10.1371/journal.pcbi.1004192]
- 94. Targeting cytokine and chemokine signaling pathways for ... [https://www.nature.com/articles/s41392-024-01868-3]
- 95. The diversification of methods for studying cell–cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11139546/]
- 96. Cytokine-mediated communications: a quantitative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8126146/]
- 97. Inflammation-associated drug resistance and tumor growth ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1623137/full]
- 98. Drug resistance in cancer: molecular mechanisms and ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12623568/]
- 99. Autocrine and Paracrine Mechanisms Promoting ... [https://www.mdpi.com/1422-0067/18/1/149]
- 100. Cytokine signaling and resistance to CDK4/6 inhibitors in ... [https://www.nature.com/articles/s41698-025-01108-z]
- 101. Targeting cytokine and chemokine signaling pathways for ... [https://biosignaling.biomedcentral.com/articles/10.1186/s12964-025-02235-7]
- 102. Cytokines Linked With Drug Resistance in Ovarian Cancer ... [https://www.ajmc.com/view/cytokines-linked-with-drug-resistance-in-ovarian-cancer-but-underlying-mechanisms-remain-unclear]
- 103. Comparative analysis of cytokines and growth factors in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8176054/]
- 104. Article Autocrine and paracrine IL-2 signals collaborate to ... [https://www.sciencedirect.com/science/article/pii/S2211124722003849]
- 105. Refined culture conditions with increased physiological ... [https://www.sciencedirect.com/science/article/pii/S2667237525000025]
- 106. A Beginner's Guide To Analyzing and Visualizing Mass ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5765874/]
- 107. 12. Styles — Cytoscape User Manual 3.10.4 documentation [https://manual.cytoscape.org/en/stable/Styles.html]
- 108. Advanced Visualization: Working with Palettes [https://cytoscape.org/cytoscape-tutorials/protocols/advanced-palettes/]
- 109. Dictionary of immune responses to cytokines at single-cell ... [https://www.nature.com/articles/s41586-023-06816-9]
- 110. Cytokine pleiotropy and redundancy: a view from the receptor [https://pubmed.ncbi.nlm.nih.gov/7696967/]
- 111. Cytokine network pathway [https://www.abcam.com/en-us/technical-resources/pathways/cytokine-network-pathway]
- 112. IL-10 Cytokine Family Signaling Pathway [https://www.rndsystems.com/pathways/il-10-cytokine-family-signaling-pathway]
- 113. Intercellular signaling reinforces single-cell level phenotypic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12392621/]
- 114. Autocrine/paracrine lysophosphatidylserine signaling ... [https://www.sciencedirect.com/science/article/pii/S2589004225006819]
- 115. Cell Lines vs. Primary Cells [https://www.stemcell.com/physiological-relevance-of-human-primary-cells-vs-cell-lines]
- 116. Primary Cell Culture Guide [https://www.atcc.org/resources/culture-guides/primary-cell-culture-guide]
- 117. Primary cells vs. cell lines: Is it not time for something better? [https://www.bit.bio/blog/primary-cells-vs-cell-lines]
- 118. Introduction to Cell Culture [https://www.thermofisher.com/us/en/home/references/gibco-cell-culture-basics/introduction-to-cell-culture.html]
- 119. Cell Culture Guide - Techniques and Protocols [https://www.assaygenie.com/cell-culture-guide-techniques-and-protocols/?srsltid=AfmBOorHOP0xxWOIG8QfkYpMlRO1-d6zDurLNG8LIVNctrv7LvVA5n8B]
- 120. Primary Cells Versus Cell Lines [https://sciencellonline.com/en/blog/post/primary-cells-versus-cell-lines?srsltid=AfmBOooyjILfjPEdTjfX-cl1OWLM0nAJzN2QUOcUQuA58jI5IWlKz_GZ]
- 121. Comparison of primary and passaged tumor cell cultures and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11220317/]
- 122. Comparison of primary and passaged tumor cell cultures ... [https://www.explorationpub.com/Journals/etat/Article/1002237]
- 123. A computational workflow for assessing drug effects on ... [https://journals.plos.org/ploscompbiol/article?id=10.1371/journal.pcbi.1013344]
- 124. ChromTime: modeling spatio-temporal dynamics of chromatin ... [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-018-1485-2]
- 125. A Mathematical Model of the Dynamics of Cytokine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8633844/]
- 126. Quantitative live-cell imaging of secretion activity reveals ... [https://www.sciencedirect.com/science/article/pii/S2589004224010629]
- 127. Signal integration, crosstalk mechanisms and networks in ... [https://www.sciencedirect.com/science/article/pii/S0167488911001844]
- 128. Supervised Machine Learning-Based Decision Support for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9114067/]
- 129. Comparison of Single Control Loop Performance ... [https://www.mdpi.com/2076-3417/13/12/6945]
- 130. From Small Molecules to Biologics, New Modalities in Drug ... [https://chemaxon.com/blog/small-molecules-vs-biologics]
- 131. Biologics vs Small Molecules: A New Era in Drug ... [https://synergbiopharma.com/biologics-vs-small-molecules/]
- 132. Probing embryonic stem cell autocrine and paracrine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4030416/]
- 133. Autocrine Signalling - an overview [https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/autocrine-signalling]
- 134. A Comprehensive Review of Monoclonal Antibodies in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11231668/]
- 135. The Benefits and Limitations of Monoclonal Antibody Therapy [https://www.mybiosource.com/learn/the-benefits-and-limitations-of-monoclonal-antibody-therapy/]
- 136. The Molecular Mechanisms That Underlie the Immune ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7461797/]
- 137. FDA approves 100th small-molecule kinase inhibitor [https://www.nature.com/articles/d41573-025-00188-7]
- 138. Properties of FDA-approved small molecule protein kinase ... [https://www.sciencedirect.com/science/article/pii/S1043661825001483]
- 139. Blood Based Biomarkers Market [https://www.factmr.com/report/blood-based-biomarkers-market]
- 140. Parameter Space and Potential for Biomarker Development in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11304510/]
- 141. Challenges and Future Trends in Biomarker Analysis for ... [https://blog.crownbio.com/challenges-and-future-trends-in-biomarker-analysis-for-clinical-research-whats-ahead-in-2025]
- 142. Uncertainty in the Translation of Preclinical Experiments to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2864134/]
- 143. Targeting myeloid cells to improve cancer immune therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC12350267/]
- 144. Harnessing innate immune pathways for therapeutic ... [https://www.nature.com/articles/s41392-024-01765-9]
- 145. Advances and clinical challenges of mesenchymal stem cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11294097/]
- 146. Innovations in immunotherapy for autoimmune diseases [https://pmc.ncbi.nlm.nih.gov/articles/PMC12485509/]
- 147. The race to reset autoimmune diseases [https://www.nature.com/articles/d41573-025-00085-z]
- 148. Breakthrough Autoimmune Findings at ACR 2025 [https://www.autoimmuneinstitute.org/research_updates/breakthrough-autoimmune-findings-at-acr-2025/]
- 149. Cellular Therapy for Systemic Autoimmune Diseases [https://pmc.ncbi.nlm.nih.gov/articles/PMC12637278/]
- 150. Patients' own autoantibodies may hold key to boosting ... [https://www.fredhutch.org/en/news/releases/2025/07/patient-antibodies-may-hold-key-to-boost-cancer-immunotherapy-response.html]
- 151. Autoantibody spark response predicts treatment outcome ... [https://www.nature.com/articles/s41598-025-12069-5]
- 152. Autoantibody profiling to predict response to the anti-PD-1 ... [https://pubmed.ncbi.nlm.nih.gov/40768895/]
- 153. The "Double-Edged Sword" Effect of Cytokines in Cancer [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1701405/full]
- 154. The Diverse Function of IL-6 in Biological Processes ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12226255/]
- 155. Targeting γc family cytokines with biologics - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC11845063/]
- 156. Cytokine-Targeting Biologic Therapies for Alopecia Areata [https://www.mdpi.com/2673-8449/5/2/11]
- 157. Systematic Investigation of Cytokine Signaling Activity at the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8493809/]
- 158. Targeting the cGAS-STING pathway: emerging strategies and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12183253/]
- 159. New Proteomic Analysis Maps Cytokine Signatures Driving ... [https://www.ajmc.com/view/new-proteomic-analysis-maps-cytokine-signatures-driving-ipf]
- 160. Nanotechnology Solutions for Controlled Cytokine Delivery [https://www.mdpi.com/2076-3417/10/20/7098]
- 161. Development of Delivery Systems for Local Administration of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10466172/]
- 162. Particle-mediated delivery of cytokines for immunotherapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC3395888/]
- 163. Nanoparticle approaches for manipulating cytokine ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1592795/full]
- 164. Nanocarrier system: An emerging strategy for bioactive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9760884/]
- 165. Recent Advances in Peptide-Loaded PLGA Nanocarriers ... [https://www.mdpi.com/1424-8247/18/1/127]