Beyond Discovery: A Strategic Framework for Robust Clinical Validation of Novel Inflammatory Biomarkers
This article provides a comprehensive roadmap for researchers, scientists, and drug development professionals aiming to navigate the complex journey of clinically validating novel inflammatory biomarkers.
Beyond Discovery: A Strategic Framework for Robust Clinical Validation of Novel Inflammatory Biomarkers
Abstract
This article provides a comprehensive roadmap for researchers, scientists, and drug development professionals aiming to navigate the complex journey of clinically validating novel inflammatory biomarkers. It covers the foundational principles of biomarker types and roles in precision medicine, details rigorous methodological approaches for analytical and clinical validation, addresses common challenges in reproducibility and standardization, and explores advanced frameworks for regulatory qualification and comparative analysis against established markers. By synthesizing current best practices, regulatory insights, and emerging technological trends, this guide aims to elevate validation standards and accelerate the translation of promising inflammatory biomarkers into clinically useful tools.
Laying the Groundwork: From Biomarker Discovery to Clinical Rationale
Inflammation is a critical driver of many diseases, from cancer to autoimmune disorders. Biomarkers—measurable indicators of biological states—are essential tools for diagnosing, predicting outcomes, and selecting treatments in inflammatory conditions. This technical support center provides troubleshooting guides and FAQs to help researchers navigate the challenges of biomarker research and improve the clinical validation of novel inflammatory biomarkers.
Troubleshooting Guides and FAQs
Pre-Analytical Variables and Sample Integrity
Q: My biomarker data shows high variability between replicates. What are the most common pre-analytical factors I should investigate?
High variability often originates from pre-analytical inconsistencies. The following table summarizes common lab issues and their solutions.
Table 1: Troubleshooting Pre-Analytical Variability in Biomarker Research
| Issue | Potential Impact on Biomarker Data | Corrective & Preventive Actions |
|---|---|---|
| Improper Sample Handling [1] | Degradation of proteins/nucleic acids; unreliable results. | Implement standardized protocols for flash-freezing, consistent thawing on ice, and maintaining cold chain logistics [1]. |
| Inconsistent Sample Preparation [1] | Introduces bias in downstream analyses (e.g., sequencing, PCR). | Standardize extraction methods, use validated reagents, and implement rigorous quality control checkpoints [1]. |
| Sample Contamination [1] | False positives, skewed biomarker profiles, misleading signals. | Use dedicated clean areas, routine equipment decontamination, single-use consumables, and consider automated homogenization [1]. |
| Inadequate Standard Operating Procedures (SOPs) [1] | High error rates and data irreproducibility between operators and batches. | Develop and enforce comprehensive SOPs, provide regular training, and implement barcoding systems to track samples and reagents [1]. |
Experimental Protocol: Validating Sample Preparation Consistency This protocol is designed to identify the source of pre-analytical variability in a protein-based cytokine assay [2].
- Sample Splitting: Split a single, large-volume patient serum or plasma sample into multiple aliquots.
- Variable Introduction: Process the aliquots with intentional, controlled variations:
- Group A: Process immediately after thawing.
- Group B: Leave at room temperature for 30 minutes before processing.
- Group C: Use different lots of the sample collection tube.
- Group D: Use two different technicians to perform the extraction.
- Analysis: Run all samples in the same multiplex cytokine assay (e.g., Luminex or ELISA) [2].
- Data Comparison: Measure the coefficient of variation (CV) across the different groups. A high CV in a specific group pinpoints the source of variability.
Diagnostic Biomarker Panels
Q: A single inflammatory cytokine lacks diagnostic sensitivity and specificity for my disease of interest. What is a more robust approach?
Single-cytokine tests often show limited clinical utility due to the complexity of inflammatory pathways. Combining multiple biomarkers into a panel significantly improves diagnostic performance [2].
Table 2: Diagnostic Performance of Single vs. Combined Inflammatory Cytokines in Gastric Cancer [2]
| Biomarker | Change in GC vs. Control | Reported Diagnostic AUC | Key Limitations as a Single Marker |
|---|---|---|---|
| IL-6 | Increased | 0.72 - 0.90 (varies by study) | Highly variable sensitivity (39%-85.7%) and specificity (50.1%-97%) across populations [2]. |
| IL-8 | Increased | 0.78 | Evidence can be mixed; some studies report no significant difference [2]. |
| IL-1β | Increased | ~0.70 | Low specificity (~43%) when used alone [2]. |
| IFN-γ | Increased | 0.65 (below 0.70) | May reflect general immune activation rather than tumor-specific presence [2]. |
| Multi-Cytokine Panel (e.g., IL-1β + IL-6 + IFN-γ) | - | 0.888 | Combinatorial panels better reflect complex immunobiology and offer superior accuracy [2]. |
Experimental Protocol: Developing a Multiplex Cytokine Diagnostic Panel This methodology outlines the steps for creating and validating a composite biomarker panel [2] [3].
- Discovery Cohort: Use a multiplex assay (e.g., Luminex) to measure a broad panel of cytokines (IL-1β, IL-6, IL-8, IFN-γ, TNF-α, etc.) in a well-characterized patient cohort and matched healthy controls [2].
- Statistical Modeling: Employ multivariable logistic regression or machine learning to identify the smallest combination of biomarkers that best distinguishes the groups. The output is a diagnostic algorithm.
- Validation: Apply this algorithm to an independent, blinded validation cohort to confirm its performance (AUC, sensitivity, specificity).
- Ascitic Fluid Analysis: For abdominal pathologies, measure biomarkers like CEA, CRP, IL-6, and VEGF directly in ascitic fluid, as this can offer better diagnostic insight than serum alone, especially when cytology is inconclusive [3].
Prognostic and Predictive Biomarker Applications
Q: How can I distinguish between a biomarker's prognostic and predictive value in the context of immunotherapy?
A prognostic biomarker provides information about a patient's overall cancer outcome, regardless of therapy. A predictive biomarker provides information about the benefit from a specific therapeutic intervention [4].
Table 3: Key Inflammatory Biomarkers in Cancer Prognosis and Treatment Prediction [4] [5]
| Biomarker | Role & Mechanism | Clinical/Research Utility |
|---|---|---|
| Systemic Inflammatory Indices (SII, SIRI, NLR) [5] | Prognostic: Calculated from peripheral blood counts (neutrophils, lymphocytes, platelets, monocytes), reflecting a pro-tumor systemic inflammatory state. | Elevated levels are strongly associated with worse overall survival in many solid tumors, including prostate cancer. For example, high SIRI was associated with a >6x increased risk of prostate cancer [5]. |
| PD-L1 Expression [4] | Predictive: Tumor cell overexpression of PD-L1 inhibits T-cell function. | Used to identify patients most likely to respond to immune checkpoint inhibitors (anti-PD-1/PD-L1) across various cancers [4]. |
| Tumor Mutational Burden (TMB) [4] | Predictive: Higher TMB suggests more neoantigens, making tumors more visible to the immune system. | Patients with high-TMB tumors are more likely to benefit from immunotherapy [4]. |
| Microsatellite Instability (MSI) [4] | Predictive: A form of high TMB resulting from defective DNA mismatch repair. | A validated biomarker for predicting response to immunotherapy in multiple cancer types [4]. |
Experimental Protocol: Correlating Systemic Inflammatory Biomarkers with Clinical Outcomes
- Cohort Definition: Define a retrospective or prospective cohort of patients with a specific cancer and available baseline clinical data and blood counts.
- Index Calculation: Calculate systemic inflammatory indices (e.g., SII, NLR, PLR, SIRI) from routine blood test data [5].
- Statistical Analysis:
- Prognostic Analysis: Use Cox regression to assess the association between each index (categorized into quartiles) and Overall Survival (OS) or Progression-Free Survival (PFS).
- Predictive Analysis: In a cohort treated with immunotherapy, test for an interaction between the biomarker level and treatment effect on survival.
- Validation: Validate findings in an independent cohort to ensure robustness [5].
Biomarker Assay Validation and Reproducibility
Q: My experimental assay is producing unexpected results. What is a systematic way to troubleshoot this?
Apply a scientific troubleshooting framework to diagnose experimental problems efficiently [6].
- Define the Problem: Clearly state the expected result versus the observed result. (e.g., "My negative control is showing a positive signal.") [7].
- Gather Information & Develop Hypotheses: List all relevant details (reagent lot numbers, equipment used, technician, protocol version). Based on this, develop testable hypotheses (e.g., "The assay buffer is contaminated," "The plate reader was miscalibrated," "The detection antibody is degraded") [7] [6].
- Test Hypotheses Systematically: Test one variable at a time to isolate the cause. Start with the simplest and most likely explanation first (Occam's razor) [6].
- Hypothesis: Contaminated buffer. Test: Use a fresh, aliquoted batch of buffer from a different lot and repeat the control experiment.
- Hypothesis: Faulty equipment. Test: Run a known positive control sample on a different, properly calibrated plate reader.
- Analyze Results and Implement CAPA: Based on the test results, identify the root cause. Implement Corrective and Preventive Actions (CAPA), such as revising the SOP, adding a quality control step, or implementing mandatory equipment calibration logs [6].
The Scientist's Toolkit
Table 4: Essential Research Reagents and Materials for Inflammatory Biomarker Research
| Item | Function/Application |
|---|---|
| Multiplex Immunoassay Kits (Luminex) | Simultaneously measure concentrations of multiple cytokines (e.g., IL-1β, IL-6, IL-8, IFN-γ) from a single small-volume sample [2]. |
| ELISA Kits | Gold-standard for quantifying a specific protein (antigen) in a sample. Useful for validating results from multiplex assays [2]. |
| Next-Generation Sequencing (NGS) | A comprehensive genomic test to assess predictive biomarkers like Tumor Mutational Burden (TMB) and Microsatellite Instability (MSI) from tissue or liquid biopsy samples [4] [8]. |
| Programmed Cell Staining Kits (IHC/IF) | Antibodies for detecting protein expression of biomarkers like PD-L1 in formalin-fixed, paraffin-embedded (FFPE) tumor tissue sections [4]. |
| Cell Separation Kits | Isolate specific immune cell populations (e.g., T cells, monocytes) from peripheral blood mononuclear cells (PBMCs) for functional studies. |
| Automated Homogenizer (e.g., Omni LH 96) | Standardizes the disruption of tissue samples, ensuring uniform extraction of proteins/nucleic acids while minimizing cross-contamination and variability [1]. |
| Mirosamicin | Mirosamicin, CAS:73684-69-2, MF:C37H61NO13, MW:727.9 g/mol |
| Okadaic Acid | Okadaic Acid, CAS:78111-17-8, MF:C44H68O13, MW:805.0 g/mol |
Experimental Workflows and Signaling
Inflammatory Cytokine Signaling in Cancer
This diagram illustrates how key pro-inflammatory cytokines contribute to tumor progression and therapy resistance, forming the biological basis for their use as biomarkers [2].
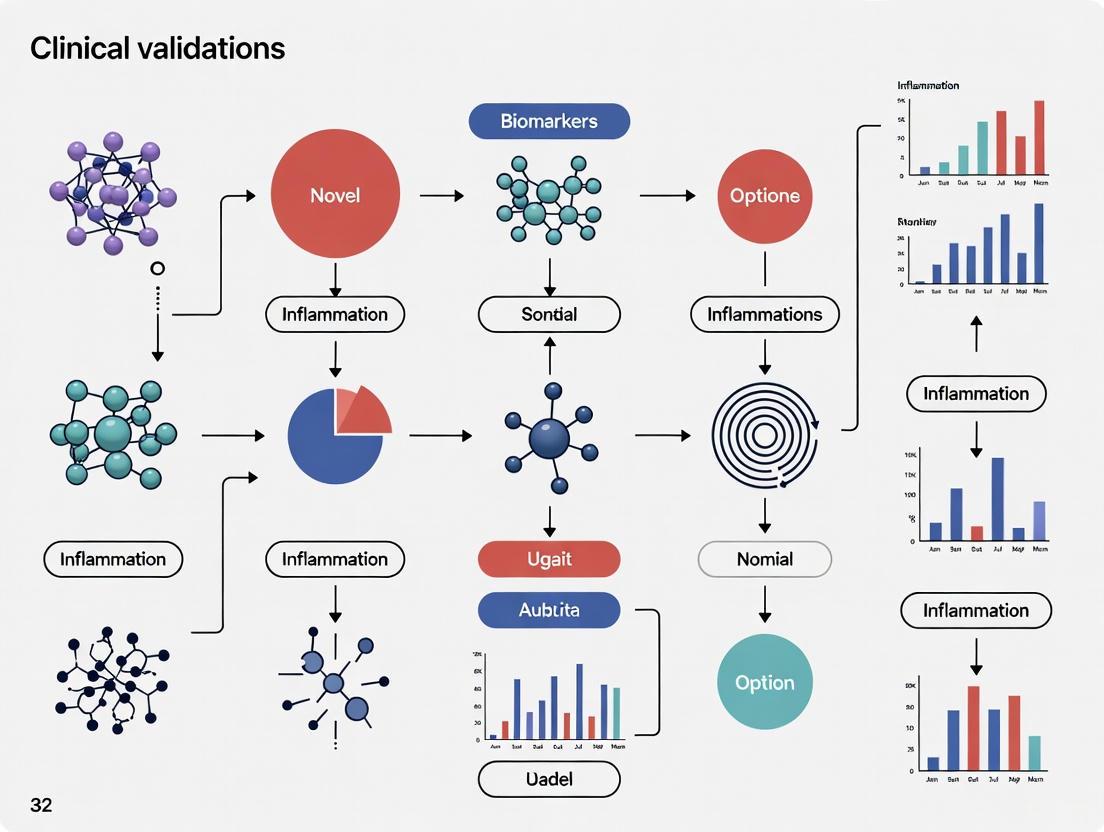
Biomarker Discovery and Validation Workflow
This flowchart outlines a generalized, multi-stage pathway for translating a candidate biomarker from initial discovery into clinical application.
Troubleshooting Guide: Common Biomarker Validation Failures and Solutions
This guide addresses frequent challenges encountered during the validation of novel inflammatory biomarkers, providing targeted solutions to help researchers navigate the complex journey from discovery to clinical implementation.
Stage 1: Discovery and Assay Development
Problem: Candidate biomarkers fail during initial technical validation Symptoms: Inconsistent measurements, poor reproducibility across labs, inability to detect biomarker in different sample matrices. Solutions:
- Implement fit-for-purpose validation early, tailoring stringency to intended use [9].
- Use advanced platforms like LC-MS/MS or Meso Scale Discovery (MSD) which offer greater sensitivity and specificity than traditional ELISA [9].
- Establish standardized SOPs for sample collection, processing, and storage to minimize pre-analytical variability [1] [10].
Problem: Overfitting in biomarker discovery Symptoms: Excellent performance in initial cohort that disappears in independent validation. Solutions:
- Apply rigorous cross-validation methods with proper implementation to avoid inflated performance estimates [11].
- Use statistical methods like LASSO or elastic net that prevent overfitting during feature selection [11].
- Ensure adequate sample size during discovery (minimum 50-200 samples) to identify robust associations [12].
Stage 2: Analytical Validation
Problem: Poor reproducibility across sites Symptoms: Inter-lab variability with coefficients of variation exceeding acceptable thresholds (>15%). Solutions:
- Implement automated sample processing systems (e.g., Omni LH 96 homogenizer) to reduce manual variability [1].
- Establish rigorous quality control measures including standard reference materials [1] [10].
- Conduct interlaboratory studies early to identify sources of technical variability [12].
Problem: Inadequate sensitivity/specificity Symptoms: Cannot distinguish disease states with sufficient accuracy for clinical utility. Solutions:
- Consider multiplex platforms (e.g., MSD U-PLEX) that enable simultaneous measurement of multiple biomarkers, potentially improving classification accuracy [9].
- Evaluate alternative sample types or enrichment strategies to improve signal-to-noise ratio [10].
- Optimize assay conditions through systematic design of experiments (DOE) approaches [10].
Stage 3: Clinical Validation
Problem: Failure to generalize in diverse populations Symptoms: Performance degradation when applied to populations with different demographics, comorbidities, or genetic backgrounds. Solutions:
- Ensure representative patient recruitment from the beginning of validation studies [13] [14].
- Account for within-subject correlation in statistical models when multiple measurements are taken from the same patient [15].
- Test for effect modification by clinical covariates that might impact biomarker performance [13].
Problem: Confusing association with prediction Symptoms: Biomarker correlates with disease presence but cannot predict future outcomes. Solutions:
- Clearly distinguish between diagnostic and predictive claims during study design [13].
- Use prospective study designs for predictive biomarkers rather than retrospective analyses vulnerable to reverse causation [13].
- Ensure the outcome being predicted hasn't already occurred when the biomarker is measured [13].
Stage 4: Clinical Implementation
Problem: Demonstrating clinical utility Symptoms: Biomarker is analytically valid but doesn't change clinical decisions or improve patient outcomes. Solutions:
- Define specific clinical decision thresholds during validation rather than just statistical associations [12] [11].
- Conduct clinical utility studies showing how biomarker use changes management and improves outcomes [12] [16].
- Consider risk-benefit balance - sometimes negative prediction is more valuable than positive prediction depending on clinical context [13].
Problem: Regulatory challenges Symptoms: Inability to gain regulatory approval despite promising clinical data. Solutions:
- Engage regulators early through FDA Biomarker Qualification Program or EMA's Qualification of Novel Methodologies [12] [10].
- Provide comprehensive evidence of analytical validity, clinical validity, and clinical utility [12] [9].
- Demonstrate superiority to existing standards or meaningful additive value to current clinical parameters [14].
Performance Standards and Metrics
Table 1: Key Analytical Validation Performance Requirements
| Parameter | Acceptance Criteria | Common Pitfalls |
|---|---|---|
| Precision (CV) | <15% for repeat measurements | Underestimating inter-operator variability |
| Sensitivity | Sufficient to detect clinically relevant levels | Not establishing LOD/LOQ in relevant matrix |
| Specificity | Demonstrate minimal cross-reactivity | Inadequate testing against related biomarkers |
| Dynamic Range | 80-120% recovery across range | Not validating at clinical decision points |
| Reproducibility | Consistent performance across sites | Inadequate standardization of protocols |
Table 2: Clinical Validation Statistical Requirements
| Metric | Minimum Threshold | Considerations |
|---|---|---|
| AUC-ROC | ≥0.80 for clinical utility [12] | Higher thresholds needed for screening |
| Sensitivity/Specificity | Typically ≥80% depending on indication [12] | Balance depends on clinical context |
| Positive Predictive Value | Varies by disease prevalence | Often overlooked in validation studies |
| Likelihood Ratios | Provide clinical interpretability | More useful than sensitivity/specificity alone |
Essential Research Reagent Solutions
Table 3: Key Research Reagents for Inflammatory Biomarker Validation
| Reagent Type | Function | Considerations |
|---|---|---|
| Multiplex Immunoassay Panels (e.g., MSD U-PLEX) | Simultaneous measurement of multiple inflammatory mediators | More cost-effective than individual ELISAs; $19.20 vs $61.53 per sample for 4-plex [9] |
| Quality Control Materials | Monitor assay performance over time | Should mimic patient sample matrix |
| Standard Reference Materials | Calibration and harmonization across sites | Often overlooked in early development |
| Sample Collection & Stabilization Systems | Preserve biomarker integrity during collection | Critical for labile inflammatory markers |
| Automated Homogenization Systems | Standardize sample preparation | Reduce contamination risk and increase efficiency by up to 40% [1] |
Experimental Protocols for Critical Validation Experiments
Protocol 1: Interlaboratory Reprodubility Study Purpose: Demonstrate consistent performance across multiple sites. Procedure:
- Distribute identical aliquots of 20-30 well-characterized samples to participating laboratories
- Include samples spanning clinical range and controls
- Each site performs measurements in duplicate over 3 separate days
- Analyze results using mixed effects models to partition variability components [15] Key Parameters: Intra-class correlation coefficient (ICC >0.9 excellent), inter-site CV (<15%)
Protocol 2: Longitudinal Stability Assessment Purpose: Establish test-retest reliability for monitoring biomarkers. Procedure:
- Collect serial samples from stable patients (n=minimum 40) over biologically relevant time frame
- Analyze using intraclass correlation coefficient (ICC) appropriate for study design [11]
- Calculate minimum detectable difference to establish sensitivity to change
- Compare to minimal clinically important difference Key Parameters: ICC (select appropriate version based on design [11]), within-subject variance
Protocol 3: Clinical Specificity Evaluation Purpose: Determine biomarker performance in differential diagnosis. Procedure:
- Recruit patients with target condition and relevant differential diagnoses
- Measure biomarker in all groups (minimum 50 per group)
- Calculate sensitivity, specificity, likelihood ratios
- Perform ROC analysis with confidence intervals Key Parameters: Area under ROC curve, positive/negative predictive values, likelihood ratios
Workflow Visualization
Biomarker Validation Pipeline
Statistical Considerations for Validation
Frequently Asked Questions (FAQs)
Q: What is the difference between biomarker validation and qualification? A: Validation is the scientific process of generating evidence that a biomarker is reliable and clinically meaningful, typically taking 3-7 years and resulting in peer-reviewed publications. Qualification is the regulatory process where the FDA or EMA formally recognizes the biomarker for specific uses in drug development, taking 1-3 years and resulting in official qualification letters [12].
Q: Why do over 95% of biomarker candidates fail to reach clinical use? A: Most failures occur due to lack of analytical robustness (assays work in one lab but not others), inadequate clinical validation (failure to generalize across diverse populations), and insufficient clinical utility (doesn't change patient management or outcomes) [17] [12]. Other common reasons include overfitting in discovery, confounding in clinical studies, and inadequate attention to pre-analytical variables [16].
Q: What statistical considerations are most frequently overlooked in biomarker validation? A: Four key issues are commonly neglected: (1) Failure to account for within-subject correlation when multiple measurements come from the same patient; (2) Inadequate control for multiple testing, increasing false discovery rates; (3) Confusing statistical significance with classification accuracy; (4) Selection bias in retrospective studies [15] [11].
Q: How do I determine the appropriate sample size for biomarker validation studies? A: Sample size should be determined by the intended use and required precision. For classification biomarkers, sample size calculations should be based on the probability of classification error rather than just p-values. For reliability studies, much larger sample sizes are needed than for simple group comparisons - often requiring hundreds to thousands of participants depending on the clinical context [11].
Q: When should I transition from traditional ELISA to more advanced platforms like MSD or LC-MS/MS? A: Consider advanced platforms when you need: greater sensitivity for low-abundance biomarkers, multiplexing capability to measure multiple biomarkers simultaneously, broader dynamic range, or when ELISA development is proving challenging due to matrix effects or antibody limitations. The cost savings of multiplexing can be substantial - up to 70% reduction compared to multiple ELISAs [9].
Q: What are the most common reasons regulators reject biomarker submissions? A: A review of EMA biomarker qualifications found that 77% of challenges were linked to assay validity issues, particularly problems with specificity, sensitivity, detection thresholds, and reproducibility [9]. Other common issues include inadequate demonstration of clinical utility and failure to show superiority over existing standards.
Q: How can I demonstrate clinical utility for an inflammatory biomarker? A: Clinical utility requires evidence that using the biomarker improves patient outcomes or decision-making compared to standard care. This can be shown through: (1) Clinical trials where biomarker-guided therapy demonstrates better outcomes; (2) Change in management studies showing clinicians alter treatment based on results; (3) Health economic analyses demonstrating improved efficiency or reduced costs [12] [16].
Frequently Asked Questions
Q1: What is the primary purpose of establishing a clinical rationale for a novel inflammatory biomarker? The primary purpose is to demonstrate the biomarker's biological and clinical relevance by definitively linking it to a specific disease mechanism. This establishes the biomarker's value in addressing an unmet clinical need, such as early disease detection, predicting treatment response, or stratifying patient populations for more effective and targeted therapies [18].
Q2: My biomarker shows strong statistical association with a disease in my cohort. Is this sufficient for clinical validation? A strong statistical association is a crucial first step, but it is not sufficient for full clinical validation. The biological plausibility of the link must be established by elucidating the mechanism of action. Furthermore, you must demonstrate the biomarker's clinical utility by showing how it addresses a specific unmet need, such as diagnosing a condition earlier than current standards, identifying patients who will respond to a specific therapy, or monitoring disease progression more accurately [18].
Q3: What are the key methodological challenges in linking a biomarker to a disease mechanism? Key challenges include:
- Biological Specificity: Distinguishing whether the biomarker is a direct driver of the pathology or a secondary consequence of another process.
- Analytical Validation: Ensuring the assay used to measure the biomarker is robust, reproducible, and accurate across different sample types and laboratories [18].
- Patient Heterogeneity: Accounting for variability in biomarker expression due to genetic diversity, co-morbidities, or environmental factors [19].
Q4: How can I strengthen the evidence for a causal relationship between my biomarker and the disease? Evidence can be strengthened through a multi-faceted approach:
- Experimental Models: Using in vitro (e.g., cell cultures) and in vivo (e.g., animal models) systems to manipulate the biomarker and observe direct effects on disease-relevant pathways.
- Multi-Omics Integration: Correlating your biomarker data with genomic, transcriptomic, or proteomic datasets to place it within a broader biological context [19].
- Clinical Corroboration: Utilizing samples from well-characterized patient cohorts and, where possible, leveraging longitudinal studies to show that changes in the biomarker level precede clinical manifestations of the disease [18].
Q5: What regulatory considerations are critical for biomarker validation in rare inflammatory diseases? For rare diseases, regulators like the FDA acknowledge the challenges of small patient populations. Key considerations include:
- Innovative Trial Designs: Utilizing single-arm trials, Bayesian statistics, and master protocols to maximize data from limited patients [20].
- Use of Real-World Evidence (RWE): Incorporating data from registries and electronic health records to support clinical evidence, provided data reliability and relevance are rigorously addressed [20].
- Clear Biomarker Context of Use: Precisely defining the biomarker's intended role (e.g., prognostic, predictive, pharmacodynamic) in the drug development process [20].
Experimental Protocols & Workflows
Protocol 1: In Vitro Functional Validation of a Novel Inflammatory Biomarker
Objective: To establish a causal link between the biomarker and a key inflammatory pathway in a controlled cell culture system.
Materials and Workflow:
Table 1: Key Research Reagent Solutions for In Vitro Validation
| Research Reagent | Function & Application in Experiment |
|---|---|
| Primary Human Macrophages | Representative human immune cells for studying inflammatory responses in a physiologically relevant model. |
| Lipopolysaccharide (LPS) | A potent inflammatory stimulant used to induce a consistent state of inflammation in the cell culture system. |
| Biomarker-Specific siRNA | Silences the gene encoding the target biomarker to investigate the functional consequences of its knockdown. |
| Neutralizing Monoclonal Antibody | Binds to and blocks the activity of the soluble biomarker protein, allowing assessment of its specific role. |
| Phospho-Specific NF-κB Antibody | Detects activation of the NF-κB signaling pathway, a central regulator of inflammation, via Western Blot. |
Protocol 2: Clinical Correlational Analysis in Patient Cohorts
Objective: To validate the association between the novel biomarker and established clinical metrics of disease activity and unmet needs.
Materials and Workflow:
Table 2: Key Materials for Clinical Cohort Analysis
| Research Reagent / Material | Function & Application in Experiment |
|---|---|
| Validated Immunoassay Kit (ELISA) | Provides a standardized, quantitative method for accurately measuring biomarker concentration in patient serum/plasma. |
| Luminex xMAP Technology | Allows for the multiplexed measurement of the novel biomarker alongside dozens of other analytes from a single small sample volume. |
| Clinical Data Collection Form (CRF) | A standardized document for systematically capturing all relevant patient data, ensuring consistency and quality for analysis. |
| Biobanked Patient Samples | Well-annotated, high-quality samples from retrospective cohorts that can be used for initial discovery and validation studies. |
Data Presentation and Analysis
Table 3: Framework for Summarizing Quantitative Biomarker-Disease Links
| Evidence Category | Experimental Method | Key Quantitative Metric(s) | Interpretation & Link to Unmet Need |
|---|---|---|---|
| Association | Correlation Analysis | Correlation coefficient (r), p-value | Strength of relationship between biomarker and disease activity. |
| Diagnostic Accuracy | Receiver Operating Characteristic (ROC) Analysis | Area Under Curve (AUC), Sensitivity, Specificity | Ability to distinguish patients from healthy controls or other diseases. |
| Predictive Value | Cox Proportional-Hazards Regression | Hazard Ratio (HR), Confidence Interval (CI) | Ability to forecast clinical outcomes like flare-ups or progression. |
| Therapeutic Response | Longitudinal Mixed Models | Mean change from baseline, p-value vs. placebo | Utility in monitoring and predicting response to treatment. |
The Scientist's Toolkit
Table 4: Essential Research Reagent Solutions for Biomarker Validation
| Category | Item | Brief Function & Rationale |
|---|---|---|
| Sample Collection | PAXgene Blood RNA Tubes | Stabilizes intracellular RNA for transcriptomic biomarker analysis from whole blood. |
| Detection & Assay | MSD MULTI-SPOT Assay Plates | Electrochemiluminescence platform for sensitive, multiplexed protein biomarker detection. |
| Signal Transduction | Phospho-Kinase Array Kit | Simultaneously monitor the relative phosphorylation levels of multiple key kinase pathways. |
| Data Analysis | R/Bioconductor Packages (e.g., limma) |
Open-source statistical tools for rigorous analysis of high-throughput biological data. |
| Model Organisms | Transgenic Mouse Models | Genetically engineered to overexpress or lack the biomarker gene for in vivo functional studies. |
| Olaquindox | Olaquindox|Antimicrobial Research Compound|RUO | |
| Mivazerol | Mivazerol, CAS:125472-02-8, MF:C11H11N3O2, MW:217.22 g/mol | Chemical Reagent |
The clinical validation of novel inflammatory biomarkers is a cornerstone of precision medicine, yet its success is heavily dependent on processes that occur before analysis even begins. The pre-analytical phase—encompassing everything from patient preparation to sample storage—is the most vulnerable stage in the laboratory testing process. Research indicates that 60-75% of laboratory errors originate in the pre-analytical phase, with significant implications for data integrity, reproducibility, and clinical validity [21] [22] [23]. For inflammatory biomarker research specifically, pre-analytical conditions can alter biomarker levels, potentially obscuring true biological signals and compromising research outcomes [24]. This technical support center provides troubleshooting guidance and standardized protocols to help researchers maintain sample integrity throughout the pre-analytical workflow, thereby enhancing the reliability of their inflammatory biomarker studies.
Troubleshooting Guides: Addressing Common Pre-Analytical Challenges
Hemolysis: Identification and Prevention
Problem: Hemolyzed samples are the most frequent pre-analytical issue, accounting for 40-70% of all pre-analytical errors [22] [25]. Hemolysis causes spurious release of intracellular analytes (potassium, phosphate, magnesium, LDH, AST, ALT) and can interfere with analytical methods through spectral interference.
Troubleshooting Steps:
- Visually inspect samples for pink-to-red discoloration in serum or plasma. However, note that visual detection is only possible at free hemoglobin concentrations >0.2-0.3 g/L [25].
- Identify the source: Most hemolysis (>98%) occurs in vitro due to collection and handling issues [21].
- Implement preventive measures:
- Minimize tourniquet time (aim for <1 minute) [21].
- Use appropriately sized needles to avoid excessive vacuum [21].
- Ensure disinfectant alcohol has completely dried before venipuncture [21].
- Avoid transferring blood from a syringe to a sample tube through a needle [21].
- Mix collection tubes by gentle inversion only—never shake [21].
- Centrifuge samples promptly after collection clot formation (for serum) [25].
Sample Misidentification and Labeling Errors
Problem: Patient misidentification and improper tube labeling account for a significant portion of pre-analytical errors, creating critical risks for patient safety and data integrity [22].
Troubleshooting Steps:
- Use at least two patient identifiers (e.g., full name and date of birth) to confirm identity before collection [21] [22].
- Label tubes in the presence of the patient after collection to prevent mix-ups. Avoid pre-labeling tubes before drawing blood [21].
- Implement automated identification systems where possible, such as barcoding, which has been shown to reduce mislabeling incidents by up to 85% [1] [22].
Improper Sample Collection Timing
Problem: Collection at incorrect timepoints can skew results for biomarkers with diurnal variation or those affected by metabolic state.
Troubleshooting Steps:
- Consider circadian rhythm: Hormones like cortisol and renin exhibit strong diurnal variation. For inflammatory biomarkers, consistency in collection time across study participants is crucial [21].
- Standardize fasting status: While not all tests require fasting, markers like glucose and triglycerides are profoundly affected. A 10-12 hour fast is standard, but prolonged fasting (>16 hours) should be avoided [21] [22].
- Document timing accurately: Record the time of collection and, for therapeutic drug monitoring, the time of last drug administration [21].
Frequently Asked Questions (FAQs)
Q1: What is the maximum allowable "needle-to-freezer" time for inflammatory biomarker studies?
A: Stability is analyte-specific, but a rapid turnaround is universally recommended. General guidelines suggest separating plasma or serum from cells within 1-2 hours of collection [24] [25]. A 2025 study on inflammation biomarkers found that while many proteins in the Olink Target 96 Inflammation panel were stable across various processing times, delays affected age-related associations for some biomarkers. When possible, standardize processing protocols across all study samples and process immediately for optimal results [24].
Q2: For plasma-based inflammatory biomarkers, which anticoagulant is most appropriate?
A: The choice of anticoagulant is critical and depends on your analytical platform:
- EDTA-plasma: Preferred for most immunochemistry assays and hematology parameters [25].
- Heparin-plasma: Suitable for clinical chemistry and some immunochemistry tests, but can interfere with mass spectrometry and peptide analyses [25].
- Citrate-plasma: Primarily used for coagulation studies, but may be used for other assays with a correction factor [25].
- Serum: Traditionally used for many clinical chemistry tests, but the clotting process can alter the protein profile compared to plasma [25].
Q3: How do repeated freeze-thaw cycles affect inflammatory biomarkers?
A: Multiple freeze-thaw cycles can cause protein degradation or aggregation, leading to inaccurate measurements. Studies indicate that even a single freeze-thaw cycle can affect concentrations of sensitive biomarkers [23]. To minimize this effect:
- Aliquot samples before initial freezing into single-use volumes.
- Establish a standard operating procedure that documents the maximum allowable freeze-thaw cycles for your study (typically 1-3 cycles).
- Maintain detailed records of the freeze-thaw history for each sample [23].
Q4: What strategies can help minimize patient blood loss in longitudinal studies?
A: Patient blood management is especially important in studies requiring repeated sampling. Effective strategies include:
- Using low-volume or pediatric blood collection tubes to reduce draw volume [26].
- Consolidating test requests to avoid unnecessary duplicate testing [26].
- Implementing microsampling techniques or point-of-care testing where possible [26].
The following tables summarize key quantitative data on pre-analytical errors and their impacts, essential for risk assessment and quality control planning in biomarker research.
Table 1: Distribution of Laboratory Errors by Phase
| Testing Phase | Percentage of Total Errors | Common Error Types |
|---|---|---|
| Pre-Analytical | 60% - 75% | Improper sample collection, misidentification, incorrect timing, improper handling [27] [22] [23] |
| Analytical | 7% - 13% | Equipment malfunction, undetected quality control failures [21] [22] |
| Post-Analytical | Not Specified | Test result loss, erroneous validation, transcription errors [22] |
Table 2: Frequency of Specific Pre-Analytical Problems
| Pre-Analytical Issue | Frequency (% of Pre-Analytical Errors) | Primary Impact |
|---|---|---|
| Hemolysis | 40% - 70% | False elevation of intracellular analytes (K+, LDH, AST); spectral interference [22] [25] |
| Insufficient Sample Volume | 10% - 20% | Inability to perform tests; need for recollection [22] |
| Clotted Sample (in anticoagulant tubes) | 5% - 10% | Invalid results for hematology and coagulation tests [22] |
| Improper Container | 5% - 15% | Anticoagulant contamination; incorrect sample matrix [22] |
Table 3: Impact of Pre-Analytical Delays on Inflammation Biomarker Stability [24]
| Stability Metric | Percentage of Proteins Affected | Interpretation |
|---|---|---|
| Proteins with good-excellent correlation (across protocols) | 38% - 83% | A majority of inflammation biomarkers show robustness to variations in pre-analytical processing. |
| Proteins with significant concentration change (>0.5 NPX units) | 18 proteins identified | A subset of biomarkers is highly sensitive to pre-analytical conditions and requires strict protocol adherence. |
| Age-related associations lost due to processing delays | 40% (12 of 30 significant associations) | Pre-analytical variability can obscure biologically significant relationships in epidemiological research. |
Experimental Protocols for Pre-Analytical Validation
Protocol: Evaluating Sample Stability Over Time
Objective: To determine the stability of specific inflammatory biomarkers under different handling conditions before processing.
Materials:
- Blood collection tubes (e.g., Serum, EDTA-plasma, Heparin-plasma)
- Centrifuge
- Refrigerator (4°C)
- Freezer (-80°C)
- Appropriate biomarker analysis platform (e.g., multiplex immunoassay)
Methodology:
- Collect blood from a minimum of 5 healthy volunteers into multiple tube types.
- For each tube type, aliquot whole blood samples and hold them at room temperature for the following time intervals: 0 hours (immediate processing), 1 hour, 2 hours, 4 hours, 8 hours, and 24 hours.
- After each time interval, centrifuge the samples according to standard protocols (e.g., 1500-2000 x g for 10-15 minutes) and aliquot the serum/plasma.
- Store all aliquots at -80°C until batch analysis.
- Analyze all samples from the same donor in the same batch to minimize analytical variance.
- Calculate the percentage change in biomarker concentration relative to the 0-hour baseline for each time point. A change greater than the assay's total allowable error or a statistically significant trend indicates instability.
Protocol: Assessing Freeze-Thaw Stability
Objective: To establish the maximum number of freeze-thaw cycles for specific inflammatory biomarkers.
Materials:
- Previously aliquoted serum or plasma samples
- Freezer (-80°C)
- Water bath or refrigerator for thawing
Methodology:
- Select a pool of well-characterized serum or plasma samples with known concentrations of your target biomarkers.
- Subject aliquots to sequential freeze-thaw cycles (e.g., 1, 2, 3, 5 cycles). One cycle consists of thawing samples completely at 4°C (or room temperature, standardized) and then re-freezing at -80°C for a minimum of 4 hours.
- Include a control aliquot that is thawed only once alongside the maximally cycled samples.
- Analyze all samples in the same batch.
- Compare the measured concentration after each cycle to the control. A significant change (e.g., >10-15%) indicates degradation.
Visual Workflows and Logical Diagrams
Pre-Analytical Workflow for Inflammatory Biomarker Research
The following diagram outlines the critical decision points and standardized procedures in the pre-analytical phase to ensure sample quality for inflammatory biomarker research.
Sample Provenance and Tracking Logic
This diagram visualizes the chain of custody and information flow required to maintain sample provenance from collection to analysis, which is critical for clinical validation studies.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Research Reagent Solutions for Pre-Analytical Work
| Item | Function/Application | Key Considerations |
|---|---|---|
| EDTA Blood Collection Tubes | Inhibits coagulation by chelating calcium. Preferred for plasma and many immunoassays. | Prevents clotting; chelation can interfere with some metal-dependent assays. [21] [25] |
| Serum Separator Tubes (SST) | Contains a gel and clot activator for serum preparation. | Allows for clean serum separation; clotting time must be standardized (30-60 mins). [25] |
| Protease Inhibitor Cocktails | Added to collection tubes to prevent proteolytic degradation of protein biomarkers. | Critical for unstable biomarkers (e.g., ANP, BNP); requires validation. [25] |
| Low-Bind Microcentrifuge Tubes | For sample aliquoting and storage. Minimizes protein adhesion to tube walls. | Essential for low-abundance biomarkers to prevent analyte loss. [23] |
| Stable Isotope Labeled Internal Standards | Used in mass spectrometry-based assays to correct for pre-analytical and analytical variability. | Distinguishes true biomarker changes from artifacts introduced during sample handling. [25] |
| Automated Homogenization Systems | Standardizes sample preparation (e.g., Omni LH 96). | Reduces human error and cross-contamination; increases throughput and reproducibility. [1] |
| Olsalazine | Olsalazine for Research|Anti-inflammatory Compound | Olsalazine is a prodrug of mesalazine for inflammatory bowel disease research. This product is for Research Use Only. Not for human use. |
| Omapatrilat | Omapatrilat | Omapatrilat is a dual ACE/NEP inhibitor for cardiovascular research. This product is for research use only (RUO), not for human consumption. |
Executing Rigorous Validation: Assays, Metrics, and Study Design
For researchers and scientists focused on the clinical validation of novel inflammatory biomarkers, establishing robust analytical methods is a critical step. The reliability of your data, and ultimately the success of your biomarker's translation to clinical use, hinges on a fundamental understanding of three core principles: Sensitivity, Specificity, and Reproducibility. This technical support guide provides clear, actionable protocols and troubleshooting advice to help you assess these parameters effectively, ensuring your analytical methods are fit-for-purpose and generate reliable, defensible data.
Core Principles and Definitions
Before embarking on experimental work, it is crucial to define the key performance characteristics of your analytical method.
- Sensitivity, often referred to as the Limit of Detection (LOD), is the lowest concentration of an analyte that an analytical procedure can reliably detect. It represents the capability of a method to detect trace levels of a biomarker [28] [29].
- Specificity is the ability of the method to measure the analyte unequivocally in the presence of other components that may be expected to be present in the sample matrix, such as other proteins, metabolites, or interfering substances [30] [28] [31]. For biomarker assays, this ensures that the signal measured is due to the target biomarker and not a cross-reacting entity.
- Reproducibility expresses the precision of the method under normal operational conditions and is a measure of its reliability. It is the degree of agreement between the results of measurements conducted on the same homogeneous sample in different laboratories, by different analysts, using different equipment, and over extended time periods [30] [28]. It is often subdivided into:
Experimental Protocols
Protocol 1: Determining Analytical Sensitivity (Limit of Detection)
This protocol outlines the experimental methodology for determining the LOD of your biomarker assay.
1. Principle The LOD is determined by establishing the lowest concentration of the biomarker that can be consistently distinguished from a blank sample. A common approach is based on the signal-to-noise ratio, where the analyte response is compared to the background noise of the system [29] [31].
2. Materials and Reagents
- Reference Standard: Purified and well-characterized target biomarker.
- Assay Buffer: The matrix-matching buffer used in your analytical procedure.
- Sample Matrix: The biological fluid relevant to your biomarker (e.g., serum, plasma) from which the analyte has been stripped or confirmed to be absent.
- Required Equipment: The full analytical instrumentation (e.g., HPLC system, plate reader, PCR cycler) as specified in your method.
3. Step-by-Step Procedure
- Step 1: Prepare a series of analyte samples at concentrations near the expected LOD. A minimum of 5 concentration levels is recommended.
- Step 2: Prepare a minimum of 20 replicates of a blank sample (matrix without the analyte) [29].
- Step 3: Analyze all samples (low concentrations and blanks) using the validated analytical method.
- Step 4: Measure the response for each sample.
4. Data Analysis and Acceptance Criteria
- Calculate the standard deviation (SD) of the responses from the 20 blank replicates.
- The LOD is typically calculated as a concentration that provides a signal-to-noise ratio of 2:1 or 3:1. Alternatively, it can be derived statistically using the formula: LOD = 3.3 × (SD of the blank response / Slope of the calibration curve) [32].
- Acceptance Criterion: The determined LOD should be at or below the concentration required to detect the biomarker in its pathophysiological range.
Protocol 2: Establishing Analytical Specificity
This protocol is designed to confirm that your method is specific for the target inflammatory biomarker.
1. Principle Specificity is demonstrated by showing that the method can distinguish and quantify the biomarker in the presence of other components, such as related biomarkers, potential metabolites, and the sample matrix itself [31]. For stability-indicating methods, specificity is also demonstrated by analyzing samples that have been subjected to stress conditions (heat, light, acid, base, oxidation) [31].
2. Materials and Reagents
- Target Analyte: Your novel inflammatory biomarker.
- Interferents: A panel of structurally similar compounds, common metabolites, and known cross-reactive substances.
- Stressed Samples: Biomarker samples that have been subjected to forced degradation.
- Spiked Matrix Samples: Blank matrix spiked with the target biomarker and potential interferents.
3. Step-by-Step Procedure
- Step 1: Inject a blank or diluent solution to check for interference [31].
- Step 2: Separately inject solutions of each potential interferent.
- Step 3: Inject a solution of the target biomarker (standard).
- Step 4: Inject a spiked solution containing the target biomarker and all potential interferents at their expected concentrations [31].
- Step 5: (For stability-indicating methods) Inject samples of the biomarker that have been stressed under various conditions.
4. Data Analysis and Acceptance Criteria
- Compare the chromatograms or assay readouts from all injections.
- Acceptance Criteria:
- There should be no interference from the blank at the retention time or detection channel of the target biomarker [31].
- The peak or signal for the target biomarker should be baseline-resolved from peaks or signals of any potential interferent [31].
- For chromatographic methods, peak purity assessment (e.g., using a photodiode array detector) should confirm that the main peak is homogeneous and pure [31].
Protocol 3: Assessing Reproducibility
This protocol evaluates the precision of your method across different runs, operators, and instruments.
1. Principle Reproducibility is assessed by analyzing multiple aliquots of the same homogeneous sample under varied but defined conditions and statistically analyzing the results [30] [28].
2. Materials and Reagents
- Homogeneous Sample: A single, well-mixed batch of sample containing the biomarker at a concentration within the quantitative range (typically low, mid, and high levels).
- Multiple Analysts: At least two qualified analysts.
- Multiple Instruments: If available, more than one instrument of the same model.
- Multiple Days: The study should be conducted over several days.
3. Step-by-Step Procedure
- Step 1: Prepare a homogeneous sample pool at a specified concentration.
- Step 2: Have Analyst 1 analyze a minimum of 6 replicates of the sample on Instrument A on Day 1.
- Step 3: Have Analyst 2 analyze another set of 6 replicates of the same sample on Instrument A (or Instrument B) on Day 2.
- Step 4: Ensure that the analytical procedure is followed identically by both analysts.
4. Data Analysis and Acceptance Criteria
- Calculate the mean, standard deviation (SD), and percent relative standard deviation (%RSD) for the results from each analyst/run.
- Use analysis of variance (ANOVA) to determine if there is a statistically significant difference between the results generated by different analysts or on different days.
- Acceptance Criterion: The inter-assay %RSD for reproducibility should be within predefined limits justified by the intended use of the assay. For many bioanalytical methods, an %RSD of ≤15% is often considered acceptable, with more stringent criteria required for critical quality attributes.
Troubleshooting Guides & FAQs
Frequently Asked Questions
Q1: What is the difference between specificity and selectivity?
- Specificity deals with the separation of the peak (or signal) of interest from adjacent components. It ensures there is no interference with your target analyte [31].
- Selectivity deals with the separation between all components in a chromatogram or assay. An assay method is specific, whereas a related substance method is selective because it must resolve all impurities from each other and the main peak [31].
Q2: Our method's reproducibility is poor between two analysts. What could be the cause? Poor reproducibility often points to a method that is not sufficiently robust. Common culprits include:
- Insufficiently Detailed Procedure: Ambiguities in the method protocol that lead to different interpretations (e.g., "vortex briefly" vs. "vortex for 30 seconds at 2000 rpm").
- Variable Sample Preparation: Differences in techniques for steps like pipetting, mixing, or incubation timing.
- Environmental Factors: Uncontrolled room temperature or humidity.
- Solution: Conduct a robustness study during method development to identify critical parameters. Then, tightly control these parameters and specify them explicitly in the written procedure [30] [33].
Q3: How do I demonstrate specificity for a biomarker in a complex matrix like serum? The most effective way is through a spike-and-recovery experiment with interferents:
- Prepare a blank serum sample.
- Prepare a serum sample spiked only with your target biomarker.
- Prepare serum samples spiked with your target biomarker and high concentrations of potential interferents (e.g., related inflammatory cytokines, albumin, immunoglobulins).
- Analyze all samples. The measured concentration of the biomarker in the presence of interferents should be within an acceptable range (e.g., 85-115%) of the concentration measured in the sample without added interferents [31].
Q4: When should method validation be performed? Method validation is required:
- Prior to the use of the method in ongoing or routine testing [34].
- When the method is part of a regulatory submission (e.g., NDA, ANDA) [30] [34].
- When there are changes to previously validated conditions or method parameters that are outside the original validation scope [34].
Troubleshooting Common Issues
| Problem | Potential Causes | Recommended Solutions |
|---|---|---|
| High Background Noise | - Contaminated reagents or buffers.- Dirty instrument optics or flow cell.- Non-specific binding in immunoassays. | - Prepare fresh reagents and use high-purity water.- Perform instrument maintenance as per SOP.- Optimize blocking conditions or include a more specific detergent. |
| Poor Reproducibility Between Runs | - Uncontrolled variation in a critical method parameter (e.g., temperature, pH).- Instability of reagents or analytical standards.- Column degradation in chromatography. | - Perform a robustness study to identify and control key parameters [30].- Document reagent and standard stability and adhere to expiration dates.- Monitor system suitability criteria before each run [32]. |
| Inconsistent Sensitivity (LOD) | - Deterioration of detection source (e.g., lamp in HPLC).- Inconsistent sample preparation technique.- Matrix effects suppressing or enhancing the signal. | - Check and replace consumable instrument parts as needed.- Standardize and meticulously document sample prep steps.- Use a matrix-matched calibration curve and consider stable isotope-labeled internal standards. |
Essential Research Reagent Solutions
The following table details key reagents and materials critical for successful analytical validation experiments.
| Reagent / Material | Function in Validation |
|---|---|
| Certified Reference Standard | Serves as the primary benchmark for establishing method accuracy, preparing calibration curves, and determining sensitivity. Its purity and characterization are foundational [34]. |
| Stripped/Blank Matrix | Essential for assessing specificity (by testing for interference) and for preparing calibration standards and quality control samples in spike-and-recovery experiments to determine accuracy. |
| Stable Isotope-Labeled Internal Standard (for LC-MS) | Corrects for variability in sample preparation, matrix effects, and instrument response, thereby significantly improving the precision and accuracy of the method. |
| Critical Reagents (e.g., Antibodies, Enzymes) | The quality and specificity of these reagents (especially for immunoassays or enzymatic assays) directly determine the method's specificity, sensitivity, and overall robustness. |
Workflow and Relationship Diagrams
Analytical Method Validation Workflow
Relationship Between Validation Parameters
Troubleshooting Guides
FAQ: High Background Signal in MSD Assays
Question: What are the common causes of a high background signal in Meso Scale Discovery (MSD) assays, and how can I resolve them?
Answer: High background is frequently traced to insufficient washing, which fails to remove unbound reagents. To resolve this, ensure thorough washing by increasing the number of wash cycles and incorporating a 30-second soak step between washes to improve the removal of unbound components [35]. Contaminated buffers or reagents can also cause high background; prepare fresh buffers for each experiment [35].
FAQ: Poor Duplicates and Assay Reproducibility
Question: My assays are showing poor duplicate reproducibility. What steps can I take to improve consistency?
Answer: Poor duplicates often result from uneven plate washing or coating. For automated plate washers, check that all ports are clean and unobstructed. Incorporate a soak step and rotate the plate halfway through the washing process [35]. Ensure consistent plate coating by using dedicated ELISA plates (not tissue culture plates) and diluting capture antibodies in PBS without additional protein. Always use fresh plate sealers for each incubation step to prevent cross-contamination from residual HRP enzymes [35].
FAQ: No Signal or Weak Signal When Expected
Question: I am not detecting a signal in my MSD assay, even though I know my sample contains the analyte. What could be wrong?
Answer: First, verify that all reagents were added in the correct order and were prepared correctly according to the protocol [35]. The standard or detection antibody may have degraded; prepare a new standard from a fresh vial and confirm antibody concentrations. If the standard curve appears normal but sample signals are weak, the sample matrix may be interfering with detection. Try diluting your samples at least 1:2 in an appropriate diluent, or perform a dilution series to check for recovery issues [35]. For low-abundance biomarkers, consider switching to an ultra-sensitive platform like the MSD S-PLEX, which can reduce the lower limit of detection by 10- to 1000-fold compared to other methods [36].
FAQ: Platform Selection for Biomarker Analysis
Question: How do I choose between Luminex and MSD platforms for my biomarker study?
Answer: The choice depends on your study's context of use, required sensitivity, and multiplexing needs. The table below compares the two platforms:
| Feature | Luminex Platform | MSD Platform |
|---|---|---|
| Detection Technology | Fluorescence-labeled microspheres (xMAP) [37] | Electrochemiluminescence (ECL) with carbon electrodes [36] [37] |
| Multiplexing Capacity | High (up to 80 targets) [37] | Moderate (typically up to 10 targets) [37] |
| Sensitivity | Good | Superior (e.g., S-PLEX kits can detect biomarkers at femtogram levels) [37] |
| Dynamic Range | Good | Broad dynamic range [36] [37] |
| Ideal Use Case | Early-stage, high-throughput studies requiring a broad panel of targets [37] | Detecting low-abundance analytes in clinical or late-phase samples [37] |
For studies requiring the highest sensitivity for low-abundance inflammatory biomarkers, the MSD S-PLEX platform is often the preferred choice [36] [37].
Experimental Protocols
Protocol: MSD S-PLEX Assay for Inflammatory Cytokines
Context of Use: This protocol is designed for the ultra-sensitive quantification of low-abundance inflammatory cytokines in human serum or plasma to support clinical validation studies [36].
Materials:
- MSD S-PLEX Assay Kit: Contains pre-coated multi-array plates, detection antibodies, and read buffer [36].
- MSD Instrumentation: Imager 6000, Sector S 600, or QuickPlex SQ 120 systems [36].
- SULFO-TAG Labels: Electrochemiluminescent labels conjugated to detection antibodies [36].
- Tripropylamine-containing Buffer: Catalyst for the electrochemical reaction [36].
- Pipettes and Microplates: For precise liquid handling.
Workflow: The following diagram illustrates the key steps and detection mechanism of the MSD S-PLEX assay workflow:
Procedure:
- Plate Preparation: Use the MSD multi-array plate pre-coated with capture antibodies.
- Sample & Incubation: Add standards, controls, and samples to the plate wells. Incubate to allow analyte binding to the capture antibody.
- Detection Antibody: Add a biotinylated detection antibody and incubate.
- SULFO-TAG Streptavidin: Add SULFO-TAG labeled streptavidin, which binds to the biotinylated detection antibody [36].
- Signal Detection: Add MSD Read Buffer containing Tripropylamine. Apply an electric current to the plate electrodes, exciting the SULFO-TAG labels and causing them to emit light at 620 nm. The instrument measures the light intensity, which is quantitatively proportional to the amount of analyte present [36].
The Scientist's Toolkit: Key Research Reagent Solutions
| Reagent/Item | Function in Experiment |
|---|---|
| MSD S-PLEX or V-PLEX Kits | Pre-configured, validated assay kits for specific biomarker panels (e.g., inflammatory cytokines), providing high sensitivity and multiplexing capability [36]. |
| SULFO-TAG Labels | Electrochemiluminescent labels conjugated to detection antibodies; emit light upon electrical stimulation, enabling ultra-sensitive detection with low background [36]. |
| Carbon Electrode Microplates | Specialized plates used in the MSD platform. The electrodes at the bottom initiate the ECL reaction, and the high-binding carbon surface enhances antibody immobilization [37]. |
| Read Buffer with Tripropylamine (TPA) | A crucial chemical catalyst in the ECL buffer that participates in the redox reaction with Ruthenium in the SULFO-TAG, leading to light emission [36]. |
| Luminex xMAP Microspheres | Fluorescent-coded beads that allow for the simultaneous detection of multiple analytes in a single well, ideal for high-plex screening panels [37]. |
| Ombrabulin | Ombrabulin, CAS:181816-48-8, MF:C21H26N2O6, MW:402.4 g/mol |
| Onalespib | Onalespib, CAS:912999-49-6, MF:C24H31N3O3, MW:409.5 g/mol |
Biomarker Validation Framework
Context of Use (COU) in Biomarker Development
Question: Why is defining the "Context of Use" (COU) critical for biomarker validation in clinical research?
Answer: The COU is a concise description of the biomarker's specified purpose, including its category and intended application in drug development or clinical practice [38]. A clearly defined COU is essential because it directly determines the study design, statistical analysis plan, choice of population, and the acceptable performance characteristics of the analytical assay [38]. For example, validating a diagnostic biomarker requires evaluating its accuracy against an accepted clinical standard, while a pharmacodynamic/response biomarker must be tested in patients undergoing the specific treatment to show target engagement [38]. The FDA Biomarker Qualification Program requires a clear COU to begin the submission process [39].
The following diagram outlines the strategic decision-making process for selecting an assay technology based on the biomarker's Context of Use and key performance needs:
Analytical vs. Clinical Validation
It is crucial to distinguish between two key validation stages:
- Analytical Validation: Establishes that the test method itself is reliable and reproducible. It evaluates technical performance characteristics such as sensitivity, specificity, accuracy, precision, and dynamic range [38]. This ensures the assay consistently measures the biomarker accurately.
- Clinical Validation: Evaluates whether the biomarker measurement usefully identifies, measures, or predicts the clinical outcome or biological state for its intended Context of Use [38]. It answers the question: Does the biomarker result correlate with the patient's health, disease, or response to treatment? A robust analytical validation is a prerequisite for a successful clinical validation [38].
Frequently Asked Questions (FAQs)
1. What does the Area Under the ROC Curve (AUC) actually tell me about my biomarker's performance? The AUC is a single metric that summarizes the overall ability of your biomarker to distinguish between diseased and non-diseased individuals across all possible classification thresholds [40]. It represents the probability that a randomly selected diseased individual will have a higher test result than a randomly selected non-diseased individual [41]. AUC values range from 0.5 to 1.0 [40]. The following table provides standard interpretations for AUC values:
| AUC Value | Interpretation | Clinical Usability |
|---|---|---|
| 0.9 - 1.0 | Excellent | Very good diagnostic performance [40] |
| 0.8 - 0.9 | Considerable / Good | Clinically useful [40] |
| 0.7 - 0.8 | Fair | Limited clinical utility [40] |
| 0.6 - 0.7 | Poor | Very limited clinical usability [40] |
| 0.5 - 0.6 | Fail | No better than chance [40] |
2. My biomarker has a statistically significant AUC, but the value is only 0.68. Is it clinically useful? A statistically significant AUC does not automatically imply clinical utility [40]. An AUC of 0.68 falls into the "Poor" interpretation category. While it indicates the biomarker performs better than random chance (AUC=0.5), its discriminatory power is likely too weak for reliable clinical decision-making as a stand-alone test [40]. You should investigate whether the biomarker adds predictive value to existing clinical factors or if its performance can be improved by combining it with other markers.
3. How do I determine the optimal cut-off point for my continuous biomarker? The optimal cut-point is the value that best separates your two groups (e.g., diseased vs. non-diseased) and depends on the clinical context. Several statistical methods can be used, with the Youden index being one of the most common [41]. The Youden index (J) is calculated as J = Sensitivity + Specificity - 1 [41]. The threshold that maximizes this value is considered optimal for balancing sensitivity and specificity. Other methods include the Euclidean index and the Product method, which often yield similar results [41].
4. Why are the Positive and Negative Predictive Values (PPV & NPV) for my biomarker different in a new population? Unlike sensitivity and specificity, PPV and NPV are highly dependent on the prevalence of the disease in the target population [42] [43]. If your initial validation was in a high-prevalence setting (e.g., a specialist clinic) and you apply the test to a low-prevalence setting (e.g., general screening), the PPV will decrease and the NPV will increase [43]. You can recalculate them using Bayes' theorem if you know the new prevalence, as well as your test's sensitivity and specificity [43]:
- PPV = (Sensitivity × Prevalence) / [ (Sensitivity × Prevalence) + (1 - Specificity) × (1 - Prevalence) ]
- NPV = (Specificity × (1 - Prevalence)) / [ (1 - Sensitivity) × Prevalence) + (Specificity × (1 - Prevalence)) ]
5. What does it mean to have a "well-calibrated" prediction model, and how is it assessed? A well-calibrated model means that its predicted probabilities of an outcome accurately match the observed frequencies in the data [44]. For example, if the model predicts a 20% risk for a group of patients, approximately 20% of those patients should experience the event. Calibration is often assessed visually using a calibration plot, which plots the predicted probabilities against the observed proportions [44]. A perfectly calibrated model would follow a 45-degree line on this plot. Statistical tests like the Hosmer-Lemeshow test can also be used, but they are sensitive to sample size.
Troubleshooting Guides
Issue 1: Low Discriminatory Power (AUC < 0.75)
Problem: Your biomarker's AUC is considered "Fair" or "Poor," limiting its clinical utility [40].
Potential Solutions & Diagnostic Steps:
- Re-evaluate Data Distributions: Check if the distributions of your biomarker in the diseased and non-diseased groups overlap significantly. Non-parametric ROC analysis may be more appropriate than a binormal model if the data is skewed [41].
- Explore Feature Engineering: Investigate if transforming the biomarker (e.g., using a logarithm) or creating a ratio with another clinical variable improves discrimination. For instance, studies have found success with ratios like the Monocyte-Lymphocyte Ratio (MLR) or Systemic Immune Inflammation Index (SII) rather than using cell counts alone [45].
- Consider a Multi-Marker Model: A single biomarker is often a weak stand-alone predictor [46]. Use multivariate analysis or machine learning techniques to build a model that combines your biomarker with other clinical or laboratory variables [44] [47]. For example, a study on young-onset colorectal cancer used a Random Forest model incorporating multiple features to achieve an AUC of 0.888 [47].
- Check Data Quality: Ensure there are no errors in data collection, labeling, or adherence to the gold standard diagnosis.
Issue 2: Selecting an Inappropriate Cut-Off Point
Problem: The chosen cut-point leads to unacceptably low sensitivity or specificity for your clinical application.
Potential Solutions & Diagnostic Steps:
- Define the Clinical Goal:
- Is the test for "Rule-Out"? Prioritize high sensitivity to avoid missing diseased individuals (e.g., for screening). You may choose a cut-point that gives >90% sensitivity.
- Is the test for "Rule-In"? Prioritize high specificity to avoid false positives (e.g., confirming a diagnosis before invasive treatment). You may choose a cut-point that gives >90% specificity.
- Compare Methods: Calculate the optimal cut-point using different methods (Youden Index, Euclidean index, etc.) to see if they converge on a similar value, which increases confidence in its validity [41].
- Validate Clinically: The statistically optimal point may not be clinically optimal. Engage with clinical collaborators to determine the acceptable trade-off between false positives and false negatives. Use the ROC curve to visualize the sensitivity and specificity at different thresholds [42].
Issue 3: Model is Poorly Calibrated
Problem: Your risk prediction model's estimated probabilities do not match the observed outcomes (e.g., it systematically over- or under-predicts risk).
Potential Solutions & Diagnostic Steps:
- Inspect the Calibration Plot: This is the first step. The plot will show you if the miscalibration is consistent across all risk levels or only in certain ranges [44].
- Apply Recalibration Techniques:
- Platt Scaling: This method uses logistic regression to transform the output of a model into a probability distribution over classes.
- Isotonic Regression: A more powerful non-parametric method that can learn a non-linear transformation, useful for complex miscalibration patterns.
- Use Bayesian Methods: Incorporate prior knowledge about the expected outcome rates to adjust the model's probabilities, which can be particularly helpful with small datasets.
Experimental Protocols for Key Metrics
Protocol 1: Conducting ROC Curve Analysis
Objective: To evaluate the diagnostic accuracy of a novel inflammatory biomarker.
Materials:
- Dataset with continuous biomarker measurements and a confirmed diagnosis (gold standard) for all subjects.
- Statistical software (e.g., R, SPSS, MedCalc).
Methodology:
- Data Preparation: Ensure your data is clean, with confirmed diseased and non-diseased groups based on a gold standard reference [42].
- Software Command: Run the ROC curve analysis procedure in your chosen software. The algorithm will calculate sensitivity and 1-specificity for every observed value of your biomarker [42].
- Output Generation:
- The ROC Curve: A plot of sensitivity (TPR) vs. 1-specificity (FPR) [48] [49].
- Area Under the Curve (AUC): The primary measure of discriminatory power, including its 95% confidence interval [40] [42].
- Coordinates of the Curve: A table listing all possible thresholds with their corresponding sensitivity and specificity.
Analysis:
- Report the AUC and its 95% CI. An AUC with a narrow confidence interval indicates a more reliable estimate [40].
- Identify the optimal cut-point using the Youden Index [41].
- Report the sensitivity, specificity, PPV, and NPV at the chosen cut-point [40].
Protocol 2: Assessing Model Calibration
Objective: To determine whether the predicted probabilities from a risk stratification model are accurate.
Materials:
- Dataset with model-predicted probabilities and observed binary outcomes.
- Statistical software with calibration plotting capabilities.
Methodology:
- Create Groups: Sort your dataset by the predicted risk and divide it into groups (typically deciles) [44].
- Calculate Averages: For each group, calculate the average predicted probability and the observed event rate.
- Generate Calibration Plot: Create a scatter plot where the x-axis is the average predicted probability for each group and the y-axis is the observed event rate [44].
- Plot Reference Line: Add a diagonal line from (0,0) to (1,1) representing perfect calibration.
Analysis:
- A well-calibrated model will have points that lie close to the diagonal line.
- Points above the line indicate the model is under-predicting risk.
- Points below the line indicate the model is over-predicting risk.
Workflow and Relationship Diagrams
Diagram 1: Biomarker Validation Statistical Workflow
Diagram 2: Relationship Between Prevalence, PPV, and NPV
Research Reagent Solutions
The following table lists key methodological "reagents" — statistical tools and concepts — essential for robust biomarker validation.
| Research "Reagent" | Function & Explanation | Example from Literature |
|---|---|---|
| ROC Curve Analysis | Evaluates the discriminatory ability of a biomarker across all possible thresholds [42]. | Used to assess Systemic Immune Inflammation Index (SII) for ovarian cancer diagnosis (AUC=0.743) [45]. |
| Area Under the Curve (AUC) | Provides a single metric for overall diagnostic performance [40]. | An AUC of 0.80 or above is generally considered clinically useful [40]. |
| Youden Index (J) | A statistical method to identify the optimal cut-point that maximizes both sensitivity and specificity [41]. | Formula: J = Sensitivity + Specificity - 1. The cut-point maximizing J is selected [41]. |
| Bayes' Theorem for PPV/NPV | Allows calculation of predictive values for a new population when prevalence is known [43]. | Crucial for translating test performance from a case-control study to a general screening population [43]. |
| Calibration Plot | A visual tool to check the agreement between predicted probabilities and observed outcomes [44]. | Used in machine learning model validation for neurological deterioration (deviation: 0.116 indicated excellent calibration) [44]. |
| 95% Confidence Interval (CI) | Quantifies the uncertainty around an estimated metric, such as the AUC [40] [42]. | A narrow 95% CI for an AUC suggests a more precise and reliable estimate of performance [40]. |
Distinguishing Prognostic from Predictive Biomarkers in Clinical Trial Design
Foundational Definitions and Regulatory Context
What is the fundamental difference between a prognostic and a predictive biomarker?
A prognostic biomarker provides information about the natural course of a disease, indicating the likelihood of a clinical event (such as disease recurrence or progression) regardless of the specific treatment received. In contrast, a predictive biomarker identifies individuals who are more or less likely to experience a particular effect when exposed to a specific medical product or environmental agent [50] [51].
- Prognostic Biomarker Example: The expression of certain inflammatory gene signatures (e.g., IFI27, CD177) in patients with COVID-19 has been investigated for its ability to predict disease progression to severe outcomes like acute respiratory distress syndrome (ARDS), independent of the treatments administered [52].
- Predictive Biomarker Example: In advanced hepatocellular carcinoma, tumor expression of PD-L1 is a predictive biomarker, as patients with PD-L1 ≥1% showed a different response and improved overall survival when treated with the immunotherapy nivolumab compared to those with lower expression [53].
Why is it often challenging to distinguish between these biomarker types in early development?
At the time of initiating a clinical trial, there is often uncertainty about a biomarker's precise role. A biomarker may be prognostic, predictive, or both, and this ambiguity must be accounted for in the trial design [50]. Furthermore, prognostic biomarkers are often investigated as candidates for predictive properties for a specific therapy, adding to the initial complexity [50].
How do regulatory agencies view these distinctions?
Regulatory discussions, such as those during the European Medicines Agency's (EMA) Scientific Advice procedures, frequently address the role of biomarkers in drug development. Key topics include determining whether a biomarker is predictive or prognostic, which directly impacts patient selection strategies, study design, and the analytical validation of the biomarker test itself [50]. The ultimate goal is to ensure that biomarkers used for patient selection are analytically and clinically validated to support safe and effective use.
Methodological Approaches for Differentiation
Core Study Designs and Analysis
What is the gold-standard study design to test if a biomarker is predictive?
The most robust method involves a randomized controlled trial (RCT) where patients are assigned to different treatment groups (e.g., new therapy vs. control) and biomarker status is measured at baseline. A predictive biomarker is confirmed by a statistically significant treatment-by-biomarker interaction—meaning the effect of the treatment differs depending on the patient's biomarker status [50].
Table 1: Interpreting Outcomes from a Randomized Trial to Distinguish Biomarker Types
| Biomarker Status | Outcome with Treatment A | Outcome with Treatment B | Interpretation |
|---|---|---|---|
| Positive | Better | Worse | The biomarker is predictive. It indicates which treatment is superior. |
| Positive | Better | Better | The biomarker is prognostic. It identifies a group with a generally better (or worse) outcome, regardless of therapy. |
| Negative | Similar | Similar | The biomarker may not be clinically useful for this context. |
How can I analyze data to investigate a biomarker's predictive value? Two common statistical approaches are used [50]:
- Separate Estimation: The treatment effect is estimated separately within the biomarker-positive subgroup and the biomarker-negative subgroup.
- Interaction Testing: A formal statistical test for an interaction term between the biomarker variable and the treatment variable is performed within a regression model. Many early-phase trials are underpowered to detect these interactions, which is a critical consideration in study planning [50].
Practical Experimental Protocol
The following workflow outlines a general protocol for validating a biomarker's predictive value, synthesizing elements from prospective validation studies [52].
Detailed Methodology:
- Patient Cohort & Sampling: Recruit a heterogeneous patient population representing the full spectrum of disease severity (e.g., from outpatient to ICU settings). Collect baseline biospecimens (e.g., peripheral blood in RNA-preserving tubes like PAXgene or Tempus) prior to treatment initiation [52].
- Biomarker Assay: Process samples using standardized protocols. For gene expression biomarkers, this involves total RNA isolation, quality control (e.g., using a Bioanalyzer), cDNA synthesis, and quantitative real-time PCR (qRT-PCR) with primers specific to the candidate biomarkers [52].
- Study Design & Outcome Tracking: In a randomized setting, patients receive either the investigational treatment or the control. All patients are followed prospectively for pre-specified, clinically relevant outcomes (e.g., a composite of disease-specific complications, ICU admission, or survival over 28 days) [52].
- Data Analysis: Evaluate the biomarker's performance by calculating sensitivity, specificity, and predictive values. The key analysis involves testing for a significant interaction between the biomarker (positive/negative or continuous) and the treatment assignment on the clinical outcome, using methods like logistic or Cox regression [50] [52].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Biomarker Research and Development
| Item | Function / Application | Example Products / Methods |
|---|---|---|
| RNA Preservation Tubes | Stabilizes intracellular RNA in blood samples immediately upon drawing, ensuring an accurate snapshot of gene expression. | PAXgene Blood RNA Tubes, Tempus Blood RNA Tubes [52]. |
| Nucleic Acid Extraction Kits | Isulates high-quality, pure RNA from preserved blood or other biospecimens for downstream molecular analysis. | PAXgene Blood RNA Kit (QIAGEN), Tempus Spin RNA Isolation Kit (Thermo Fisher) [52]. |
| qRT-PCR Reagents & Platforms | Quantifies the expression levels of specific candidate biomarker genes with high sensitivity and reproducibility. | TaqMan Gene Expression Master Mix (Thermo Fisher), CFX384 Real-Time PCR Detection System (Bio-Rad) [52]. |
| Immunohistochemistry (IHC) Assays | Detects and localizes specific protein biomarkers (e.g., PD-L1) within formalin-fixed, paraffin-embedded (FFPE) tumor tissue sections. | Validated IHC pharmDx assays (e.g., Dako) [54]. |
| Next-Generation Sequencing (NGS) | Profiles multianalyte biomarker panels, identifies novel genetic mutations, or assesses tumor mutational burden. | Various targeted or whole-exome sequencing platforms [55]. |
| ONO 1603 | ONO 1603, MF:C16H19ClN2O3, MW:322.78 g/mol | Chemical Reagent |
| Opaviraline | Opaviraline, CAS:178040-94-3, MF:C14H17FN2O3, MW:280.29 g/mol | Chemical Reagent |
Troubleshooting Common Scenarios
FAQ 1: Our biomarker appears to be predictive in a single-arm study. Is this sufficient evidence?
No. A single-arm study (where all patients receive the investigational drug) cannot reliably distinguish a predictive from a prognostic biomarker. Observed differences in outcome between biomarker-positive and negative groups could be entirely due to the biomarker's prognostic effect. A randomized controlled design is required to isolate the treatment-specific effect [50] [54].
FAQ 2: How should we handle the selection of a cutoff for a continuous biomarker?
Cutoff selection is a major methodological challenge. Using a data-driven approach (e.g., optimizing the cutoff on the same dataset) can lead to overfitting and unreliable results. Preferred strategies include [50]:
- Using a pre-specified cutoff based on prior biological or clinical evidence.
- Employing a predefined percentile (e.g., median) of the distribution.
- If data-driven methods are unavoidable, use resampling techniques (e.g., bootstrapping) for internal validation and always confirm the cutoff in an independent validation cohort.
FAQ 3: We suspect our biomarker is prognostic, but we want to test its predictive value for our new drug. What is an efficient trial design?
Consider an all-comers design, where you enroll patients regardless of biomarker status and stratify randomization by biomarker status. This allows you to:
- Evaluate the drug's effect in the overall population.
- Test for a treatment-by-biomarker interaction to formally assess predictive properties.
- Estimate the treatment effect within the biomarker-defined subgroups [50]. This design is efficient because it generates evidence for both the general and biomarker-selected populations within one trial.
FAQ 4: What are the key considerations for validating the biomarker assay itself?
Before a biomarker can be used for patient selection, its assay requires rigorous analytical validation. This process establishes key performance characteristics [51]:
- Accuracy: How close the measured value is to the true value.
- Precision: The closeness of repeated measurements (including reproducibility across days, operators, and laboratories).
- Sensitivity: The lowest concentration that can be accurately measured.
- Stability: How the biomarker degrades from sample collection to analysis. For companion diagnostics, this process is critical and is reviewed by regulatory bodies [50].
Frequently Asked Questions
| Question | Answer |
|---|---|
| What are fractional changes (FC) and why are they significant? | Fractional changes (FC) quantify the relative change in a biomarker's level before and after an intervention or over time. Calculated as FC = (Y–X)/X, where X and Y are the values before and after the event, FC provides a more robust prediction of treatment response than single-point measurements [56]. |
| In what clinical context is this approach validated? | This method has been strongly validated in predicting resistance to Intravenous Immunoglobulin (IVIG) treatment in children with Kawasaki disease (KD). Dynamic changes in inflammatory biomarkers like WBC and neutrophil count were superior to pre-treatment scores [56]. |
| Which biomarkers are most predictive when tracked dynamically? | In KD research, the fractional changes in White Blood Cell (WBC) count and Neutrophil Count (NE count) were the strongest individual predictors. A combined model of multiple FCs achieved an Area Under the Curve (AUC) of 0.8307, indicating high predictive accuracy [56]. |
| My predictive model using pre-treatment biomarkers has mediocre performance. How can I improve it? | Incorporate post-treatment laboratory data to calculate fractional changes. Pre-treatment parameters alone often have suboptimal predictive power (e.g., pre-treatment NLR and PLR had a combined AUC of 0.72 in a meta-analysis). Modeling the system's dynamic response significantly enhances accuracy [56]. |
| What is the core mathematical formula for calculating fractional change? | FC = (Y–X)/X, where X is the pre-treatment value and Y is the post-treatment value. This formula is applied to laboratory parameters like WBC, Hb, and NE% [56]. |
Troubleshooting Guides
Issue 1: Low Predictive Power of a Static Biomarker Model
- Problem: Your model, based on a single measurement of a biomarker, fails to accurately predict patient outcomes or treatment response.
- Solution:
- Shift to a Dynamic Framework: Design your experiments to collect biomarker data from at least two critical time points (e.g., pre-treatment and within 24 hours post-treatment).
- Calculate Fractional Changes: Compute the FC for each key biomarker in your study population.
- Validate with Combined Models: Develop a multivariate model that combines the FCs of several biomarkers. Research shows that a combination of FCs (e.g., WBC, Hb, NE%) can achieve an AUC >0.85, far surpassing most static models [56].
Issue 2: Handling Nonlinear Relationships in Biomarker Data
- Problem: You suspect that the relationship between your biomarker and the clinical outcome is not straightforward or linear.
- Solution:
- Statistical Detection: Employ a Restricted Cubic Spline (RCS) analysis to visually and statistically examine the relationship between your predictor and the outcome.
- Model Adjustment: The RCS analysis will reveal if the relationship is nonlinear. If so, you must account for this in your predictive model rather than assuming a simple linear effect [56].
Issue 3: Ensuring Generalizability of Your Predictive Model
- Problem: A model works well in your initial cohort but fails when applied to a new patient population.
- Solution:
- External Validation: Always test your final model, including the FC thresholds you establish, in a separate, independent validation cohort from a different clinical center.
- Proven Example: The predictive power for KD IVIG resistance, established in the Soochow cohort (n=1,796), was successfully validated in an external Anhui cohort (n=636), confirming its reliability [56].
Quantitative Data from Key Research
The table below summarizes the predictive performance of fractional changes in biomarkers for IVIG resistance in Kawasaki disease, as demonstrated in a large-scale study [56].
| Predictive Marker | Area Under the Curve (AUC) | Clinical Context |
|---|---|---|
| WBC (FC) | 0.7677 | IVIG Resistance in Kawasaki Disease |
| Neutrophil Count (FC) | 0.7818 | IVIG Resistance in Kawasaki Disease |
| Combined FC Model | 0.8307 (Soochow Cohort) | IVIG Resistance in Kawasaki Disease |
| Combined FC Model | 0.8564 (Validation Cohort) | IVIG Resistance in Kawasaki Disease |
| Pre-treatment NLR/PLR (from meta-analysis) | ~0.72 | IVIG Resistance in Kawasaki Disease [56] |
Detailed Experimental Protocol
This protocol outlines the methodology for validating fractional changes in inflammatory biomarkers, based on a retrospective clinical cohort study [56].
- Study Design: Two-center, retrospective cohort study.
- Population: Pediatric patients diagnosed with complete or incomplete Kawasaki disease according to the American Heart Association (AHA) criteria.
- Inclusion: Hospitalized patients receiving standard IVIG (2 g/kg) and aspirin treatment.
- Exclusion: Patients who received corticosteroids, non-standard treatment, or had recurrent KD, serious complications, or missing data.
- Data Collection:
- Pre-treatment Labs: Collect blood samples for WBC, NE count, LY count, Hb, CRP, etc., before IVIG administration.
- Post-treatment Labs: Collect blood samples within 24 hours after the completion of IVIG infusion.
- Outcome Definition: IVIG resistance is defined as persistence or recurrence of fever (≥38.0°C) for more than 36 hours after IVIG treatment.
- Data Analysis:
- Calculate Fractional Changes: Compute FC for all laboratory parameters.
- Identify Predictors: Use multivariate logistic regression to find independent predictors of the outcome (e.g., pre-treatment CLR and Hb; post-treatment CLR, LMR; and FCs of WBC, Hb, NE%).
- Assess Performance: Perform Receiver Operating Characteristic (ROC) curve analysis to evaluate the predictive power of each significant variable and combination of variables.
- Test for Nonlinearity: Use Restricted Cubic Spline (RCS) analysis to check for nonlinear associations.
Experimental Workflow and Signaling Pathway
The following diagram illustrates the conceptual workflow for applying a dynamic monitoring framework to biomarker discovery and validation, integrating concepts from observability theory [57].
The Scientist's Toolkit: Research Reagent Solutions
| Essential Material | Function in Research |
|---|---|
| Fully Automated Hematology Analyzer | Measures core inflammatory biomarkers from whole blood samples, including White Blood Cell (WBC) count, Neutrophil count (NE count), Lymphocyte count (LY count), and Hemoglobin (Hb) [56]. |
| Fully Automated Biochemical Analyzer | Measures key plasma/serum biomarkers, most critically C-Reactive Protein (CRP), which is essential for calculating ratios like CLR [56]. |
| EDTA Blood Collection Tubes | Standard tubes for collecting whole blood samples (e.g., 2.0 ml) for hematological analysis [56]. |
| Calculated Inflammatory Ratios | These are not physical reagents but are critical derived metrics. Key examples include the Neutrophil-to-Lymphocyte Ratio (NLR), Lymphocyte-to-Monocyte Ratio (LMR), and C-reactive Protein-to-Lymphocyte Ratio (CLR), which serve as powerful composite biomarkers [56]. |
| Modaline Sulfate | Modaline Sulfate, CAS:2856-75-9, MF:C10H17N3O4S, MW:275.33 g/mol |
| Molindone Hydrochloride | Molindone Hydrochloride, CAS:15622-65-8, MF:C16H25ClN2O2, MW:312.83 g/mol |
Navigating Roadblocks: Strategies for Reproducibility and Standardization
FAQs: Understanding Batch Effects and Reproducibility
Q1: What exactly are batch effects and why are they a major concern for biomarker research?
Batch effects are systematic technical variations introduced when samples are processed or measured in different batches, labs, or using different instruments. These variations are unrelated to the biological variation of interest [58] [59]. In clinical biomarker research, they are a major concern because they can:
- Produce spurious signals or obscure genuine signals, leading to false associations [58] [59].
- Mask actual biological differences between samples, such as between healthy and diseased tissue, impairing the accuracy and generalizability of models intended for clinical use [60].
- Contribute to the reproducibility crisis, where findings from one study cannot be replicated in another, thereby delaying the development of lifesaving therapies and diagnostics [58] [61] [62].
Q2: How can I quickly check if my dataset has batch effects?
You can use a combination of visualization and quantitative metrics to detect batch effects [63].
- Visualization: Perform dimensionality reduction (e.g., PCA, t-SNE, or UMAP) and color the data points by their batch of origin. A clear separation of batches, rather than grouping by biological condition, signals the presence of batch effects [63].
- Quantitative Metrics: Several metrics can help identify batch effects with less human bias. The table below summarizes key metrics and their applications [63].
Table 1: Quantitative Metrics for Batch Effect Detection
| Metric Category | Specific Metric | What it Measures |
|---|---|---|
| Cluster-Based | Adjusted Rand Index (ARI) | Agreement between batch-based clustering and biological-group-based clustering. |
| Normalized Mutual Information (NMI) | The information shared between batch and biological group classifications. | |
| Distance-Based | Average Silhouette Width (ASW) | How similar samples are to their own batch/group compared to other batches/groups [64]. |
| Principal Component Regression (PCR) | The proportion of variance in principal components explained by batch. |
Q3: What are the signs that my batch effect correction has been too aggressive (over-correction)?
Over-correction occurs when a Batch Effect Correction Algorithm (BECA) removes genuine biological signal along with the technical noise. Key signs include [63]:
- Distinct cell types or biological conditions are incorrectly clustered together on dimensionality reduction plots (UMAP, t-SNE).
- A complete overlap of samples from very different biological conditions or experiments, suggesting the method has removed all variation.
- A significant portion of cluster-specific markers are comprised of genes with widespread high expression (e.g., ribosomal genes), indicating a loss of true biological specificity.
Q4: At which data level should I perform batch-effect correction in proteomics studies?
Benchmarking studies using reference materials suggest that protein-level correction is the most robust strategy for MS-based proteomics. The process of protein quantification from precursor and peptide-level intensities can interact with BECAs. Correcting at the protein level, after quantification, has been demonstrated to be more effective in removing unwanted variations while retaining robust biological signals [65].
Troubleshooting Guides
Guide 1: Selecting and Evaluating a Batch Effect Correction Workflow
Problem: A researcher is unsure how to choose and validate a Batch Effect Correction Algorithm (BECA) for their gene expression dataset.
Solution: Follow a structured workflow that prioritizes compatibility and downstream sensitivity analysis.
- Step 1: Consider the Entire Workflow. A BECA does not work in isolation. Ensure the assumptions of the BECA are compatible with all other steps in your data processing workflow (e.g., normalization, imputation) [59].
- Step 2: Test Multiple BECAs. Different tools perform better on different datasets. Begin with methods that are generally well-regarded, such as Harmony or scANVI for single-cell data, or ComBat and limma's removeBatchEffect for bulk data where the source of variation is known [63] [59].
- Step 3: Perform Downstream Sensitivity Analysis. To rigorously assess the impact of different BECAs, use the following protocol [59]:
- Split your data by batch and perform differential expression analysis (DEA) on each batch individually.
- Combine the results to create a union and an intersect of all differentially expressed (DE) features. These serve as reference sets.
- Apply a variety of BECAs to the full dataset, then perform DEA on each corrected dataset.
- For each BECA, calculate performance metrics like recall (using the union set) and check for the preservation of the intersect features. This reveals which BECA best recovers known biological signals.
The following workflow diagram illustrates this troubleshooting process:
Guide 2: Managing Imbalanced Study Designs and Incomplete Data
Problem: Batch effects are confounded with biological groups of interest (e.g., all controls from one batch, all cases from another), or the dataset has a large amount of missing values.
Solution: Employ advanced data integration methods and careful experimental design.
Challenge: Confounded or Imbalanced Design.
- Cause: Biological groups are unevenly distributed across batches, making it difficult to distinguish technical bias from true biological effect [58] [64].
- Solution:
- Causal Methods: Consider causal approaches that focus on conclusions within the range of covariate overlap, rather than extrapolating across the entire dataset. These methods may correctly indicate when the data is inadequate to draw a conclusion [58].
- Leverage References: If available, use internal reference samples (e.g., pooled standards) measured across all batches. Some algorithms like COCONUT or the reference-based mode in BERT can use these to estimate and remove batch effects more robustly [64].
- Account for Imbalance: Be aware that sample imbalance (differences in cell type proportions, etc.) substantially impacts data integration results. Choose integration techniques benchmarked for such settings [63].
Challenge: Incomplete Data (Missing Values).
- Cause: Omic data is often incomplete, with missing values for specific features in specific batches, which many standard BECAs cannot handle.
- Solution: Use data integration frameworks designed for incomplete data, such as HarmonizR or the newer Batch-Effect Reduction Trees (BERT). These methods use matrix dissection or tree-based structures to integrate data without requiring aggressive imputation, thereby retaining more of the original data [64].
Research Reagent Solutions
Table 2: Essential Materials and Tools for Batch-Effect Aware Research
| Item | Function in Batch Effect Management |
|---|---|
| Reference Materials | Commercially available or in-house pooled samples (e.g., Quartet protein reference materials) processed across all batches to monitor and correct for technical variation [65]. |
| Standardized Protocols | Detailed, written procedures for sample preparation, fixation, staining, and analysis to minimize pre-analytical variation [60]. |
| Internal Control Samples | A positive control sample included in every batch run to track performance and signal drift over time. |
| Batch Effect Correction Algorithms (BECAs) | Software tools (e.g., ComBat, Harmony, limma, BERT) specifically designed to model and remove unwanted technical variation from data [58] [59] [64]. |
| Data Management System | A system for meticulously tracking metadata (batch ID, instrument, operator, date, etc.) which is essential for diagnosing and modeling batch effects. |
Experimental Protocols & Data Presentation
Key Experimental Workflow for Robust Data Integration
The diagram below outlines a recommended workflow for handling batch effects in a biomarker discovery pipeline, from experimental design to validation.
Performance Comparison of Data Integration Methods
The following table summarizes benchmark findings for different batch effect correction strategies, particularly in the context of large-scale or incomplete data.
Table 3: Benchmarking Data Integration Methods for Incomplete Omic Data
| Method | Core Approach | Handles Incomplete Data? | Key Performance Findings |
|---|---|---|---|
| BERT | Tree-based integration using ComBat/limma | Yes | Retains up to 5 orders of magnitude more data than other methods; 11x faster runtime; considers covariates and references [64]. |
| HarmonizR | Matrix dissection for parallel integration | Yes | The previous primary method for incomplete data; can suffer from significant data loss depending on blocking strategy [64]. |
| Harmony | Iterative clustering and correction | No | Fast and generally well-performing for single-cell data, but less scalable for very large datasets [63]. |
| scANVI | Deep generative model | No | A top performer in benchmarks but can be complex to implement and run [63]. |
| Protein-Level Correction | Applies BECAs after protein quantification | N/A | In proteomics, this strategy is more robust than correcting at the precursor or peptide level [65]. |
Implementing Fit-for-Purpose Validation Aligned with Intended Use
Core Principles of Fit-for-Purpose Validation
What is the fundamental principle behind "fit-for-purpose" biomarker validation?
The core principle is that validation rigor should be commensurate with the biomarker's specific intended application within clinical development. Validation constitutes "the confirmation by examination and the provision of objective evidence that the particular requirements for a specific intended use are fulfilled." This means you must define the assay's purpose and acceptance criteria before characterizing its performance through experimentation. The assay is validated only if its demonstrated performance meets these pre-defined needs for your specific context [66].
How does intended use influence the validation strategy?
The position of the biomarker on the spectrum from a research tool to a clinical endpoint dictates the stringency of validation. The nature of the analytical technology also influences the level of performance verification required [66]. The validation strategy is driven by the answer to a critical question: How will this biomarker data inform decision-making? The consequences of an incorrect result determine the necessary level of assay robustness.
Biomarker Assay Categorization and Validation Parameters
What are the different categories of biomarker assays, and why does category matter?
The American Association of Pharmaceutical Scientists (AAPS) and the US Clinical Ligand Society have identified five general classes of biomarker assays. The category dictates which performance parameters must be evaluated during validation [66].
Table 1: Biomarker Assay Categories and Key Characteristics
| Assay Category | Calibration Method | Output | Common Examples |
|---|---|---|---|
| Definitive Quantitative | Calibrators & regression model; fully characterized reference standard | Absolute quantitative values | Mass spectrometric analysis [66] |
| Relative Quantitative | Response-concentration calibration with non-representative standards | Relative quantitative values | - |
| Quasi-quantitative | No calibration standard | Continuous response based on a sample characteristic | - |
| Qualitative (Ordinal) | Scoring scales | Discrete scores | Immunohistochemistry (IHC) scoring [66] |
| Qualitative (Nominal) | Presence/Absence | Yes/No | Presence or absence of a gene product [66] |
What validation parameters are required for each assay category?
The performance parameters you need to test are directly tied to your assay's category. The following table summarizes the consensus on which parameters should be investigated [66].
Table 2: Recommended Performance Parameters for Biomarker Method Validation
| Performance Characteristic | Definitive Quantitative | Relative Quantitative | Quasi-quantitative | Qualitative |
|---|---|---|---|---|
| Accuracy | + | |||
| Trueness (Bias) | + | + | ||
| Precision | + | + | + | |
| Reproducibility | + | |||
| Sensitivity | + | + | + | + |
| LLOQ | LLOQ | LLOQ | ||
| Specificity | + | + | + | + |
| Dilution Linearity | + | + | ||
| Parallelism | + | + | ||
| Assay Range | + | + | + | |
| Range Definition | LLOQ–ULOQ | LLOQ–ULOQ |
LLOQ: Lower Limit of Quantitation; ULOQ: Upper Limit of Quantitation.
Troubleshooting Common Validation Challenges
How should I set acceptance criteria for accuracy and precision?
For definitive quantitative assays, more flexibility is allowed compared to standardized bioanalysis of small molecules. While 25% is often a default value for precision and accuracy (30% at the LLOQ), this should be evaluated on a case-by-case basis. Avoid blindly applying fixed criteria without a statistical evaluation of their relevance to your specific assay. Adopting a 4:6:15 rule (where a run is accepted if 4 out of 6 QCs are within 15% of nominal) means 33% of your patient samples could fall outside acceptance limits, which may not be fit-for-purpose [66].
Recommended Approach: Consider using an accuracy profile methodology. This approach accounts for total error (the sum of bias and intermediate precision) against a pre-set acceptance limit you define. It generates a β-expectation tolerance interval, allowing you to visually predict the confidence interval (e.g., 95%) for future measurements and what percentage will fall within your limits [66].
What is the recommended experimental design for building an accuracy profile?
The Societe Francaise des Sciences et Techniques Pharmaceutiques (SFSTP) recommends this design for definitive quantitative methods [66]:
- Run 3–5 different concentrations of calibration standards and 3 different concentrations of validation samples (VS) (high, medium, low) in triplicate.
- Perform this analysis on 3 separate days.
- For biomarker methods, you may need a greater number of calibration standards and VS due to potential nonlinearity in response.
Our novel inflammatory biomarker is for prognosis. What are key validation considerations?
For prognostic biomarkers, as seen in development for DRESS syndrome and stroke, the focus shifts toward clinical validation of the biomarker's ability to predict a specific outcome [67] [68].
- Cohort Selection: Ensure your patient cohort (e.g., critically ill stroke patients) accurately represents the intended-use population [68].
- Model Development and Validation: Use a training cohort to develop your prognostic model and an independent validation cohort to test it. Internal validation techniques like leave-one-out cross-validation can also be employed [67].
- Performance Metrics: For prognostic models, key metrics include the C-index (concordance index) for overall model discrimination, time-dependent Receiver Operating Characteristic (ROC) curves, and Decision Curve Analysis (DCA) to evaluate clinical utility [68].
Experimental Protocols for Key Validation Experiments
Protocol for Establishing Assay Precision (Repeatability and Intermediate Precision)
Objective: To determine the closeness of agreement between multiple measurements of the same sample under defined conditions. Materials: Quality Control (QC) samples at low, mid, and high concentrations within the assay range. Procedure:
- Prepare a batch of each QC level on the same day using the same reagents.
- Analyze each QC level in a minimum of 5 replicates per run.
- Repeat this process for a minimum of 3 different days using fresh reagent preparations where possible.
- Use different analysts or instruments if this variability is expected in routine use. Data Analysis:
- Calculate the mean, standard deviation (SD), and percentage coefficient of variation (%CV) for the replicates within each day (repeatability).
- Pool all data from all days and calculate the overall mean, SD, and %CV (intermediate precision).
- The obtained %CV is compared against your pre-defined acceptance criteria (e.g., <25%).
Protocol for Parallelism Assessment
Objective: To demonstrate that the diluted sample behaves identically to the standard in the assay, ensuring accurate quantification. Materials: Patient or study samples with high levels of the analyte. Procedure:
- Select a minimum of 3 individual patient samples with high analyte concentration.
- Prepare a series of dilutions (e.g., 1:2, 1:4, 1:8) for each sample using the appropriate assay matrix (e.g., pooled plasma).
- Assay the diluted samples and a standard curve in the same run.
- The calculated concentration of each diluted sample should be corrected for the dilution factor. Data Analysis:
- Plot the measured concentration against the dilution factor for each sample.
- Assess the linearity of the response. The data should fit a linear model with an R² value meeting your pre-defined criterion (e.g., >0.95).
- The %CV of the back-calculated concentrations across dilutions should also be within acceptable limits (e.g., <25%). A failure of parallelism indicates potential matrix interference.
Workflow and Pathway Visualizations
Fit-for-Purpose Validation Workflow
The following diagram outlines the iterative, stage-gated process for implementing fit-for-purpose biomarker method validation.
Prognostic Biomarker Development & Validation Pathway
For novel inflammatory biomarkers (e.g., for psoriatic disease or stroke prognosis), the pathway from discovery to clinical application involves distinct phases of validation [69] [68].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Biomarker Validation Experiments
| Item / Reagent | Function / Purpose in Validation | Key Considerations |
|---|---|---|
| Fully Characterized Reference Standard | Serves as the primary calibrator for definitive quantitative assays. | Must be representative of the endogenous biomarker; purity and stability are critical [66]. |
| Quality Control (QC) Samples | Used to monitor assay performance during validation and in-study runs. | Should be prepared in the same matrix as study samples; typically at low, mid, and high concentrations. |
| Authentic Patient/Study Samples | Used for parallelism, stability assessments, and bridging studies. | Ensure an adequate volume is available from donors or a biobank. |
| Appropriate Biological Matrix | (e.g., pooled plasma, serum) Used for preparing calibration standards, QCs, and for dilution linearity. | Should be free of the target analyte or have a known baseline level [66]. |
| Stability-Testing Materials | (e.g., -80°C freezer, benchtop incubator) To assess analyte stability under various conditions. | Conditions should mimic pre-analytical handling (freeze-thaw, room temp, long-term storage) [66]. |
Overcoming Population Diversity Gaps in Validation Cohorts
Frequently Asked Questions (FAQs)
FAQ 1: Why is population diversity a critical issue in biomarker validation?
A lack of diversity in validation cohorts creates a "translational gap," where biomarkers that perform well in controlled, homogenous preclinical studies fail to generalize in broader, heterogeneous patient populations. This can exacerbate health disparities and reduce the generalizability of research findings [70] [71]. Without diverse cohorts, biomarkers may miss critical differences in disease prevalence, genetic background, and treatment responses across racial, ethnic, gender, and age groups [72] [73].
FAQ 2: What are the most common demographic factors affecting enrollment in validation studies?
Research has quantified noticeable differences in enrollment likelihood based on key demographics. A study contacting over 3,500 eligible patients observed the following enrollment ranges [73]:
Table: Enrollment Likelihood by Demographic Factor
| Demographic Factor | Enrollment Likelihood Range |
|---|---|
| Gender | 3.8% - 13.4% |
| Race & Ethnicity | 4.8% - 29.8% |
| Distance to Study Site | 1.1% - 29.2% |
Furthermore, statistical analysis found that patients from White and non-Hispanic backgrounds, as well as those living closer to the study site, were significantly more likely to enroll [73].
FAQ 3: What are the main pitfalls that cause biomarker projects to fail in diverse populations?
Most biomarker projects stall for predictable reasons related to data and methodology [17]:
- Lack of Large, Diverse Datasets: Findings from small, homogenous cohorts often fail to generalize.
- Analytical Variability: Inconsistent methods across labs or teams produce conflicting results.
- Ethical and Privacy Barriers: These can halt collaboration and limit research scope.
- Missing Governance Frameworks: A lack of clear rules on data ownership and use impedes partnership.
- The "Small n, Large p" Problem: Having thousands of potential features (e.g., genes, proteins) but a small number of patients makes it statistically difficult to find reliable signals.
Troubleshooting Guides
Problem 1: My biomarker candidate, identified in a pre-clinical model, does not validate in initial clinical cohorts.
Potential Cause: The pre-clinical model (e.g., traditional animal models, cell lines) may have poor correlation with human clinical disease due to a lack of genetic and physiological diversity, failing to capture human population heterogeneity [71].
Solution Strategy:
- Utilize Human-Relevant Models: Incorporate patient-derived xenografts (PDX), organoids, and 3D co-culture systems that better mimic patient physiology and retain characteristic biomarkers [71].
- Integrate Multi-Omics Data: Use genomics, transcriptomics, and proteomics to identify context-specific, clinically actionable biomarkers that might be missed with a single-method approach [71].
- Employ Functional and Longitudinal Validation: Move beyond single time-point measurements. Use functional assays to confirm biological relevance and longitudinal sampling to capture dynamic biomarker changes over time [71].
Problem 2: My validation cohort does not adequately represent the true disease population.
Potential Cause: Systemic and individual barriers—such as geographic distance to study sites, lack of awareness, and mistrust of the medical establishment—lead to selection bias in enrollment [73].
Solution Strategy:
- Implement Community-Based Participatory Research (CBPR): Involve community partners early in the study design to build public awareness, address health disparities, and improve access [73].
- Use Real-World Data (RWD) for Benchmarking: Develop disease-specific demographic profiles using RWD to set representative enrollment goals for your trials, rather than relying only on general census data [74].
- Adopt Decentralized Trial Elements: Utilize remote patient monitoring and mobile technologies to reduce the burden of travel and make participation easier for a geographically diverse population [70].
Problem 3: I am unable to identify biomarkers that are specific to my disease of interest amidst general inflammation.
Potential Cause: Many inflammatory diseases share common pathways, and identified biomarker signatures may reflect general systemic inflammation rather than being disease-specific [75].
Solution Strategy:
- Incorporate Inflammatory Control Groups: In a study on Inflammatory Bowel Disease (IBD), researchers included samples from patients with Rheumatoid Arthritis (RA) as a positive control for systemic inflammation. This allowed them to filter out non-specific inflammatory genes and identify a focused, IBD-specific biomarker panel [75].
- Apply Advanced Computational Filtering: After differential expression analysis, systematically remove genes that are also differentially expressed in the inflammatory control group. Use machine learning algorithms like LASSO regression to select the most discriminative biomarker candidates from the remaining genes [75].
Table: Experimental Protocol for Disease-Specific Biomarker Identification
| Step | Methodology | Purpose |
|---|---|---|
| 1. Cohort Design | Include patient groups for: a) Target Disease, b) Healthy Controls, c) Inflammatory Disease Controls. | To control for non-specific systemic inflammation. |
| 2. Data Acquisition | Profile samples (e.g., whole blood) using transcriptomics (microarray, RNA-seq) or proteomics. | To generate comprehensive molecular data. |
| 3. Bioinformatics Analysis | Identify Differentially Expressed Genes (DEGs) for each group (e.g., with Limma or DESeq2). Filter out DEGs shared with the inflammatory control group. | To isolate a disease-specific gene set. |
| 4. Biomarker Panel Refinement | Apply machine learning (e.g., LASSO, SVM) on the disease-specific gene set to build a diagnostic model. | To select a minimal, high-performance biomarker panel. |
| 5. Validation | Test the panel's diagnostic accuracy (sensitivity, specificity) in a separate, real-life patient cohort. | To confirm clinical utility and generalizability. |
Problem 4: My biomarker assay is not reproducible across different laboratories or patient cohorts.
Potential Cause: A lack of standardized protocols for measuring and reporting biomarkers, combined with inherent biological variability across diverse populations, leads to inconsistent results [72].
Solution Strategy:
- Adhere to FAIR Principles: Ensure all data and algorithms are Findable, Accessible, Interoperable, and Reusable. This promotes transparency and reproducibility [17].
- Use Open-Source Pipelines: Leverage community-driven, standardized toolkits like the Digital Biomarker Discovery Pipeline (DBDP) to reduce analytical variability and ensure methods are verifiable [17].
- Implement Rigorous Analytical Validation: Before clinical validation, confirm the assay's accuracy, precision, sensitivity, specificity, and reproducibility across the expected range of biological samples [72] [76].
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Materials for Biomarker Discovery and Validation
| Item / Reagent | Function / Explanation |
|---|---|
| PAXgene Blood RNA Tubes | For standardized collection, stabilization, and transport of whole blood RNA for transcriptomic studies [75]. |
| CIBERSORTx Algorithm | A computational tool for deconvoluting immune cell fractions from bulk tissue or blood gene expression data, helping to characterize immune landscape [75]. |
| LASSO (Least Absolute Shrinkage and Selection Operator) Regression | A machine learning algorithm used for variable selection and regularization to identify the most predictive biomarkers from a large pool of candidates [75]. |
| PRM (Parallel Reaction Monitoring) | A high-resolution, high-accuracy mass spectrometry method for targeted quantification of candidate protein biomarkers without the need for antibodies [76]. |
| Digital Biomarker Discovery Pipeline (DBDP) | An open-source toolkit providing standardized methods for processing data from wearables and mobile devices to discover digital biomarkers [17]. |
| Patient-Derived Organoids | 3D cell cultures derived from patient tissues that better recapitulate in vivo biology and biomarker expression than traditional 2D cultures [71]. |
Experimental Workflow and Pathway Diagrams
The following diagram illustrates the core workflow for building a diverse and disease-specific biomarker validation cohort, integrating key steps from troubleshooting guides.
Core Workflow for Diverse Biomarker Validation
The diagram below outlines the analytical pathway for identifying inflammatory response-related biomarkers, a common approach in diseases like stroke and IBD.
Analysis Pathway for Inflammatory Biomarkers
Integrating Multi-Omics Data for Comprehensive Biomarker Signatures
Frequently Asked Questions & Troubleshooting Guides
General Multi-Omics Concepts
What is multi-omics integration and why is it important for biomarker discovery?
Multi-omics integration refers to the combined analysis of different omics data sets—such as genomics, transcriptomics, proteomics, and metabolomics—to provide a more comprehensive understanding of biological systems. This approach is crucial for biomarker discovery because it allows researchers to examine how various biological layers interact and contribute to the overall phenotype or biological response. By correlating information from various omics layers, scientists can generate more holistic insights into disease mechanisms and responses to treatments, ultimately leading to better personalized medicine approaches [77].
How does multi-omics data improve patient stratification in clinical trials?
Multi-omics approaches transform patient stratification by providing a comprehensive view of tumor biology. Each omics layer offers distinct insights: genomics examines the full genetic landscape, transcriptomics analyzes gene expression and pathway activity, and proteomics investigates the functional state of cells by profiling proteins. By integrating these data layers, researchers can identify distinct patient subgroups based on molecular and immune profiles, enabling precise patient selection in trials and improving the chances of detecting true treatment effects [78].
Data Integration Challenges & Solutions
What are the common challenges when integrating multi-omics datasets?
Integrating multi-omics data presents several challenges primarily related to data heterogeneity, dimensionality, and analytical complexity [77]. Specific challenges include:
- Technical variation: Different measurement techniques across omics layers result in varied data types, scales, and noise levels
- Biological variability: Differences among samples can introduce additional noise
- High dimensionality: Can lead to overfitting in statistical models and complicate interpretation
- Data alignment: Requires careful consideration of each dataset's distinct characteristics
How should I handle different data scales in multi-omics datasets?
Handling different data scales requires specific normalization techniques tailored to each data type [77]:
Table: Normalization Methods for Different Omics Data Types
| Omics Data Type | Recommended Normalization Methods | Purpose |
|---|---|---|
| Metabolomics | Log transformation, Total ion current normalization | Stabilize variance and account for differences in sample concentration |
| Transcriptomics | Quantile normalization | Ensure consistent distribution of expression levels across samples |
| Proteomics | Quantile normalization, Z-score normalization | Ensure uniform distribution across samples and standardize to common scale |
| All Types | Z-score normalization | Standardize data to a common scale for cross-omics comparison |
How can I resolve discrepancies between transcriptomics, proteomics, and metabolomics results?
When encountering discrepancies between omics layers, follow this systematic approach [77]:
- Verify data quality from each omics layer, checking for consistency in sample processing
- Consider biological mechanisms such as post-transcriptional or post-translational modifications
- Apply integrative analyses using pathway analysis to identify common biological pathways
- Explore regulatory mechanisms that might reconcile observed differences
Technical Implementation
What are the best practices for preprocessing multi-omics data for joint analysis?
Preprocessing multi-omics data involves several critical steps [77] [79]:
- Data Quality Control: Identify and remove low-quality data points, filter out low-abundance metabolites or proteins, and check for outliers
- Normalization: Account for technical variations using methods appropriate for each data type
- Transformation: Convert data to a common scale or representation to facilitate integration
- Standardization: Ensure data are collected, processed, and stored consistently using agreed-upon standards
- Harmonization: Align data from different sources using domain-specific ontologies or standardized formats
What are the essential bioinformatics tools for multi-omics integration?
Table: Essential Tools for Multi-Omics Data Integration
| Tool Name | Language/Platform | Primary Function | Application Context |
|---|---|---|---|
| mixOmics | R | Multivariate analysis | Multi-omics data integration and visualization |
| INTEGRATE | Python | Data integration | Combining diverse omics datasets |
| IntegrAO | Graph Neural Networks | Classification with incomplete data | Robust patient stratification with partial data |
| NMFProfiler | Not specified | Signature identification | Biomarker discovery and patient subgroup classification |
| GATK Pipeline | Java | Variant calling | Genomic analysis in whole-exome sequencing |
Biomarker Validation
What statistical methods are appropriate for multi-omics biomarker discovery?
Performing statistical tests in multi-omics datasets requires careful consideration of data structure [77]:
- Group comparisons: Use t-tests or ANOVA for comparing means between groups
- Multiple testing correction: Apply Benjamini-Hochberg procedure to control false discovery rate
- Multivariate analysis: Implement PLS-DA or canonical correlation analysis to uncover relationships between omics layers
- Feature selection: Employ machine learning algorithms like Lasso regression or Random Forest to identify informative variables
How can I assess the reproducibility of multi-omics findings?
Assess reproducibility through [77]:
- Technical replicates during sample preparation and analysis
- Independent validation studies with separate cohorts
- Statistical metrics such as coefficient of variation (CV) or concordance correlation coefficient (CCC)
Experimental Protocols & Workflows
Comprehensive Multi-Omics Validation Workflow
The following diagram illustrates a proven workflow for multi-omics biomarker validation, adapted from a PDAC study that successfully identified and validated a four-gene biomarker signature [80]:
Detailed Methodologies for Multi-Omics Analysis
Sample Collection and Ethical Considerations
- Obtain appropriate ethical approval and written informed consent from all patients
- Collect blood samples in EDTA tubes and store at -80°C for downstream processing
- For tissue samples, collect during surgical procedures and immediately transfer in liquid nitrogen for flash freezing
- Ensure normal tissue samples are obtained from pancreas areas confirmed noncancerous by a pathologist [80]
Whole Exome Sequencing Protocol
- DNA Extraction: Use standard phenol-chloroform protocol for genomic DNA isolation
- Quality Assessment: Measure DNA concentration and purity using spectrophotometry
- Library Preparation & Sequencing: Perform WES on Illumina HiSeq platform
- Data Processing:
- Base calling to generate raw reads in FastQ format
- Quality assessment using FastQC and adaptor removal via FastP
- Alignment to human reference genome (GRCh38/hg38) using Burrows-Wheeler Aligner (BWA)
- Variant calling using GATK pipeline and functional annotation with ANNOVAR [80]
Transcriptome Analysis Workflow
- RNA Isolation: Use TRIzol method for total RNA extraction from tissue samples
- cDNA Synthesis: Employ RevertAid Reverse Transcriptase cDNA synthesis kit
- Sequencing: Perform transcriptome sequencing on Illumina platform
- Bioinformatic Analysis: Use R programming with bioinformatics tools for differential expression analysis [80]
RT-qPCR Validation Methodology
- Primer Design: Use PRIMER3 software to design primers spanning exon-exon junctions
- Reaction Setup: Perform quantitative PCR using Syber Green detection system
- Internal Control: Optimize housekeeping gene (GAPDH) as internal control
- Data Analysis: Calculate relative mRNA levels using the 2−ΔΔCt method
- Statistical Analysis: Use Student's t-test with p-value < 0.001 considered statistically significant [80]
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Research Reagents for Multi-Omics Biomarker Validation
| Reagent/Kit | Manufacturer | Specific Function | Application Context |
|---|---|---|---|
| Phenol-chloroform protocol | Standard laboratory suppliers | Genomic DNA extraction from tissue samples | Whole exome sequencing sample preparation |
| RevertAid Reverse Transcriptase cDNA synthesis kit | Thermo Fisher Scientific | cDNA synthesis from isolated RNA | Transcriptome analysis and RT-qPCR validation |
| Syber Green detection system | Bio Molecular System | Quantitative PCR detection | RT-qPCR validation of gene expression |
| TRIzol method reagents | Multiple suppliers | Total RNA isolation from tissue samples | Transcriptome sequencing sample preparation |
| Illumina sequencing reagents | Illumina | Library preparation and sequencing | Whole exome and transcriptome sequencing |
Troubleshooting Common Experimental Issues
Data Quality Problems
Issue: Poor correlation between transcript levels and protein abundance
Solution: This discrepancy is common due to biological factors. Consider that [77]:
- Higher transcript levels indicate potential for increased protein synthesis, but this relationship is influenced by mRNA stability, translation efficiency, and post-translational modifications
- A gene with high mRNA levels might not result in proportionately high protein levels if the protein is rapidly degraded
- Apply pathway analysis to contextualize relationships by mapping gene products to metabolic pathways
Issue: High technical variability across omics platforms
Solution: Implement rigorous standardization [79]:
- Store raw data to ensure full reproducibility of results
- Include complete descriptions of samples, equipment, and software used
- Apply appropriate normalization and batch effect correction methods
- Use style transfer methods based on conditional variational autoencoders for data harmonization
Analytical Challenges
Issue: Difficulty identifying key biomarkers from large multi-omics datasets
Solution: Apply systematic feature selection [77]:
- Data preprocessing to ensure quality and comparability
- Differential expression analysis to identify significant changes between conditions
- Integration techniques such as pathway analysis or machine learning models to prioritize candidates
- Validation of biomarkers showing consistent changes across multiple omics layers
Issue: Challenges linking genomic variation to multi-omics data
Solution: Implement correlation-based approaches [77]:
- Conduct genome-wide association studies (GWAS) to identify trait-associated SNPs
- Explore how genetic variants correlate with transcript levels, protein abundance, or metabolite concentrations
- Use integrative approaches to reveal how genetic variations influence biological pathways
Best Practices for Successful Multi-Omics Integration
Design integrated data resources from the user perspective, not just the data curator's view. Create real use case scenarios to ensure your resource solves actual scientific problems [79].
Value metadata as much as primary data. Comprehensive metadata facilitates data processing, search, and retrieval, similar to how photographic metadata (lenses used, time/date, focal length) enables better image management [79].
Implement spatial biology technologies where appropriate. Spatial transcriptomics and proteomics preserve tissue architecture, revealing how cells interact and how immune cells infiltrate tumors—critical for understanding tumor heterogeneity [78].
Utilize appropriate preclinical models. Patient-derived xenografts (PDX) and organoids recapitulate human tumor biology more accurately than traditional models, enabling better prediction of therapeutic response before clinical testing [78].
Ensure regulatory compliance. Data generated for clinical decision-making must meet CAP and CLIA-accredited standards to ensure integrity, reproducibility, and regulatory compliance [78].
The Role of AI and Machine Learning in Automated Data Interpretation and Predictive Modeling
Technical Support Center: AI in Clinical Biomarker Research
This technical support center provides troubleshooting guides and FAQs for researchers using AI and Machine Learning in the clinical validation of novel inflammatory biomarkers.
Frequently Asked Questions (FAQs)
Q1: What are the most common data-related challenges when training AI models for inflammatory biomarker discovery? The most frequent challenges stem from data heterogeneity and quality. This often includes inconsistent data formats from different omics platforms (e.g., genomics, proteomics), high levels of noise in real-world data, and batch effects from multi-center studies. Incomplete clinical annotations or misaligned sample timing can also severely limit model performance and generalizability [81].
Q2: How can we improve our AI model's generalizability across different patient populations? Improving generalizability requires a proactive strategy. Prioritize incorporating diverse datasets from the earliest stages of model development, ensuring representation across relevant ethnicities, geographies, and clinical settings. Employing techniques like domain adaptation and federated learning can help models adapt to new data distributions without centralizing sensitive data. Continuous validation on external, independent cohorts is essential to test performance robustness [81] [82].
Q3: Our model achieves high accuracy on retrospective data but fails in prospective validation. What might be wrong? This is a classic sign of overfitting or data drift. The model may have learned patterns specific to your historical dataset that are not causally linked to the biology. To address this, rigorously simplify the model to reduce complexity, perform more stringent feature selection to eliminate redundant variables, and implement temporal validation (training on older data and testing on newer data). Furthermore, ensure that the data preprocessing and feature extraction pipelines for prospective data are identical to those used in training [81] [83].
Q4: What are the best practices for integrating multi-omics data (e.g., genomics, proteomics) using AI? Successful multi-omics integration involves a multi-modal data fusion approach. Start by establishing a unified data governance protocol to standardize data from different sources. Instead of simply concatenating datasets, use AI architectures designed for integration, such as multi-view learning or graph neural networks, which can model complex relationships between different types of biological data. The goal is to allow the model to identify complementary signals from each omics layer [81].
Q5: How can we address the "black box" problem and improve model interpretability for regulatory approval? To enhance interpretability, focus on using inherently interpretable models like decision trees or linear models where possible. For complex models like deep learning, utilize post-hoc explanation tools such as SHAP (SHapley Additive exPlanations) or LIME (Local Interpretable Model-agnostic Explanations) to highlight which features most influenced a prediction. Documenting the model's decision-making process with clear, biological rationale is critical for building trust with clinicians and regulators [81] [83].
Troubleshooting Guides
Issue 1: Poor Model Performance on External Validation Cohorts
| Potential Cause | Diagnostic Steps | Solution |
|---|---|---|
| Cohort Shift | Compare summary statistics (mean, variance) of key features between training and validation cohorts. | Apply domain adaptation techniques or re-calibrate the model on a small sample from the new cohort [81]. |
| Data Preprocessing Inconsistency | Audit the data processing pipelines for both cohorts to ensure identical steps (normalization, imputation). | Re-process all data through a single, standardized pipeline before model training and validation [81]. |
| Insufficient Feature Generalizability | Analyze feature importance scores; high importance on technically derived, non-biological features is a red flag. | Re-train the model using a refined feature set focused on biologically relevant variables with known clinical correlation [82]. |
Issue 2: AI Model Fails to Converge or Training is Unstable
| Potential Cause | Diagnostic Steps | Solution |
|---|---|---|
| High-Dimensionality & Multicollinearity | Calculate correlation matrices and variance inflation factors (VIF) for input features. | Apply dimensionality reduction (PCA, autoencoders) or robust feature selection methods (LASSO) before training [81]. |
| Improper Hyperparameter Tuning | Visualize the loss landscape during training to check for oscillations or divergence. | Implement a systematic hyperparameter search (e.g., grid search, Bayesian optimization) to find optimal settings [84]. |
| Data Quality Issues | Check for outliers, missing values, and class imbalance in the training dataset. | Conduct rigorous data cleaning, impute missing values using appropriate methods, and apply sampling techniques to address imbalance [85]. |
Issue 3: Successful Predictive Model Lacks Clinical Utility
| Potential Cause | Diagnostic Steps | Solution |
|---|---|---|
| Poorly Defined Clinical Endpoint | Review if the model's prediction aligns with a clinically actionable decision point for a physician. | Re-align the modeling objective with a clear clinical outcome (e.g., "response to therapy" vs. "change in biomarker level") [83]. |
| Lack of Interpretability | Present model outputs to clinicians and gather feedback on the clarity and actionability of the information. | Integrate explainable AI (XAI) techniques to provide reasoning for predictions and present results through intuitive clinical dashboards [81] [83]. |
| Inadequate Performance Metrics | Evaluate if standard metrics (AUC) are sufficient; calculate clinical utility metrics like NNT (Number Needed to Treat). | Use performance metrics that reflect clinical impact, such as net benefit analysis from decision curve analysis [81]. |
Experimental Protocols for Key Methodologies
Protocol 1: Developing a Digital Biomarker for Inflammatory Flare Prediction
Objective: To develop an AI model that predicts flares in inflammatory bowel disease (IBD) using data from wearable devices.
Materials:
- Patients with confirmed IBD.
- Wearable devices (e.g., Fitbit, Apple Watch) capable of measuring heart rate (HR), resting heart rate (RHR), heart rate variability (HRV), and step count.
- Smartphone application for collecting patient-reported outcomes (PROs) like pain and well-being.
- Standard clinical biomarkers (e.g., C-reactive protein, fecal calprotectin) for ground-truth validation.
Methodology:
- Data Collection: Recruit a longitudinal cohort. Patients continuously wear devices and log PROs daily. Serum and stool samples are collected at regular intervals and during symptomatic flares to measure traditional biomarkers [82].
- Feature Engineering: From the raw device data, calculate daily aggregates (mean, SD) for RHR, HRV, and step count. Create rolling-window averages (e.g., 7-day average) to capture trends.
- Labeling: Define a "flare" event based on a combination of: (a) physician global assessment, (b) rise in traditional biomarkers, and (c) patient-reported symptom escalation.
- Model Training: Train a time-series classification model (e.g., using LSTM networks or Random Forests) to predict the onset of a flare within a pre-defined window (e.g., 7 days). Use the digital features as inputs and the flare event as the output label [82].
- Validation: Validate the model on a held-out test set from the same cohort and subsequently on an independent, external cohort to assess generalizability.
Protocol 2: Multi-Omic Integration for Novel Biomarker Panel Identification
Objective: To identify a robust multi-omics biomarker signature for stratifying patients with autoimmune inflammation.
Materials:
- Patient tissue or serum samples with rich clinical phenotyping.
- Platforms for genomic, transcriptomic, and proteomic profiling.
- High-performance computing infrastructure.
Methodology:
- Data Generation: Perform whole genome sequencing, RNA sequencing, and high-throughput proteomics (e.g., mass spectrometry) on the same set of patient samples.
- Data Harmonization: Normalize and pre-process each omics dataset individually. Use batch correction algorithms to remove technical artifacts. Annotate all features (genes, proteins) consistently.
- Multi-Modal Data Fusion: Employ an AI model capable of integrating the different data types. One effective approach is to use a Multi-Kernel Learning framework, where each omics data type is represented by a separate similarity matrix ("kernel") between patients, and a model learns the optimal combination of these kernels to predict the clinical outcome [81].
- Feature Selection & Interpretation: The model will output a weight for each feature across all omics layers. Features with the highest weights constitute the candidate biomarker panel. Use pathway enrichment analysis to biologically validate the combined signature.
- Experimental Validation: Technically validate the top candidate biomarkers using targeted, clinically applicable assays (e.g., ELISA for proteins, PCR for transcripts) in a new patient cohort.
Workflow and Pathway Visualizations
AI-Driven Biomarker Discovery Workflow
Troubleshooting Poor Model Generalizability
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in AI Biomarker Research |
|---|---|
| High-Parameter Flow Cytometry | Enables deep immunophenotyping of patient samples, generating high-dimensional data on immune cell populations that serve as inputs for AI-based patient stratification [83]. |
| Multiplex Immunofluorescence (MIF) | Allows simultaneous visualization of multiple protein biomarkers on a single tissue section, providing spatial context that is used to train AI models on the tumor microenvironment or inflammatory foci [83]. |
| Single-Cell RNA Sequencing | Reveals transcriptomic heterogeneity at the individual cell level, providing the high-resolution data needed to discover novel cell-type-specific biomarker signatures [81]. |
| Mass Spectrometry Proteomics | Identifies and quantifies thousands of proteins from a sample, generating the large-scale proteomic datasets required for AI-driven biomarker panel identification [81]. |
| Wearable Biosensors | Continuously collect physiological data (e.g., heart rate, activity) as digital biomarkers, which are used to train time-series AI models for predicting disease flares or treatment response [82]. |
Demonstrating Utility: Regulatory Pathways and Competitive Positioning
For researchers developing novel inflammatory biomarkers, navigating the regulatory qualification process is a critical step in transitioning from exploratory research to known valid biomarkers accepted for use in drug development. Regulatory qualification provides a formal acknowledgment that a biomarker is suitable for a specific Context of Use (COU) within drug development and regulatory review, making it a publicly available tool that can be relied upon across multiple drug development programs without needing re-justification in each application [86]. This technical support center guides you through the complexities of the FDA Biomarker Qualification Program (BQP) and the EMA's Qualification of Novel Methodologies (QoNM), helping you troubleshoot common challenges and efficiently advance your biomarker toward regulatory acceptance.
Understanding the Regulatory Frameworks
What is Biomarker Qualification and Why Does It Matter?
Biomarker qualification is a formal regulatory conclusion that within a stated Context of Use, the biomarker can be relied upon to have a specific interpretation and application in drug development and regulatory review [86]. The COU precisely defines the purpose and manner of biomarker application, establishing boundaries within which available data justify its use [86].
For inflammatory biomarker researchers, qualification offers significant advantages:
- Regulatory Efficiency: Once qualified, your biomarker can be included in any drug sponsor's Investigational New Drug (IND), New Drug Application (NDA), or Biologics License Application (BLA) without requiring the FDA to reconfirm its suitability for the qualified COU [86].
- Resource Optimization: Facilitates collaborative development where multiple stakeholders can pool resources, decreasing individual costs and expediting drug development [86].
- Public Health Impact: Increases availability of effective drugs and enables earlier patient access to targeted therapies [86].
Key Regulatory Pathways at a Glance
The FDA and EMA have established parallel but distinct pathways for biomarker qualification. The table below summarizes the core characteristics of each program:
| Feature | FDA Biomarker Qualification Program | EMA Qualification of Novel Methodologies |
|---|---|---|
| Legal Basis | Section 507 of the 21st Century Cures Act [86] | CHMP Regulation (EC) No 726/2004 [87] |
| Primary Goal | Qualify biomarkers as Drug Development Tools (DDTs) for specific Contexts of Use [88] | Provide opinions on acceptability of novel methodologies in medicine development [87] |
| Outcome Documents | Qualified Biomarker Listing [86] | Qualification Opinion (QO) or Qualification Advice (QA) [87] |
| Collaborative Focus | Encourages public-private partnerships and consortia [86] | Consortia more likely to achieve qualification [89] |
| Typical Duration | Multi-stage process with target timelines [90] | Variable; public consultation for QOs [87] |
Step-by-Step Qualification Processes
The FDA's Biomarker Qualification Pathway
The FDA's qualification process follows a structured three-stage approach established by the 21st Century Cures Act, designed to provide increasing levels of detail for biomarker development [86] [91]. The visualization below outlines this pathway:
Engagement and Submission Steps:
Pre-LOI Meeting (Recommended): Before formal submission, request a 30-45 minute teleconference with the Biomarker Qualification Program. Your written request should include a cover letter with three proposed dates, specific questions in PowerPoint format, and a background presentation on your biomarker including its name, proposed COU, and drug development need [91].
Stage 1: Letter of Intent (LOI) Submission: Submit a complete LOI through the NextGen Collaboration Portal. The LOI should include a brief description of the biomarker, its proposed COU, and the drug development need it addresses [91]. The FDA aims to review complete LOIs within 3 months, though actual timelines may vary [90].
Stage 2: Qualification Plan (QP) Development: After LOI acceptance, develop a comprehensive Qualification Plan. The FDA has published a revised QP Content Element Outline (July 2025) with detailed instructions for preparation [86]. Sponsor development of QPs typically takes a median of over 2.5 years, so early planning is essential [90].
Stage 3: Full Qualification Package (FQP) Submission: The FQP contains all supporting data and evidence for your biomarker's proposed COU. Submit through the NextGen Portal, with FDA target review within 10 months [91] [90].
The EMA's Qualification of Novel Methodologies
The EMA offers two primary outcomes through its qualification procedure:
Key EMA Procedural Aspects:
Qualification Advice (QA): A confidential procedure for biomarkers in earlier development stages, focusing on scientific rationale, proposed COU, preliminary data, and evidence generation strategy [92]. Multiple QAs may precede a Qualification Opinion.
Qualification Opinion (QO): Issued when evidence adequately supports the biomarker's targeted COU. Draft QOs undergo a 2-month public consultation before final adoption by the Committee for Medicinal Products for Human Use (CHMP) [87] [89].
Letters of Support: For promising methodologies not yet ready for qualification, the EMA may issue a Letter of Support to encourage data sharing and further studies toward qualification [87].
Troubleshooting Common Challenges
Frequently Asked Questions (FAQs)
Q1: Our inflammatory biomarker research is at an early stage. When should we first engage with regulators?
Engage early through the appropriate preliminary mechanisms. For the FDA, request a Pre-LOI meeting once you have preliminary data and a defined proposed COU [91]. For the EMA, consider an Innovation Task Force (ITF) briefing meeting as a first point of contact for strategic advice on innovative aspects of your project [89]. Research shows that less than half of ITF participants engage in fee-related follow-up procedures, suggesting missed opportunities for continued regulatory guidance [89].
Q2: What are the most common issues raised during biomarker qualification reviews?
Data from EMA qualification procedures (2008-2020) reveal the most frequent issues [92]:
| Issue Category | Frequency in Procedures | Specific Concerns |
|---|---|---|
| Biomarker Properties | 79% | Insufficient evidence of clinical validation, lack of biological/clinical plausibility, inadequate performance characteristics |
| Assay Validation | 77% | Lack of demonstrated reliability, reproducibility, and robustness of measurement assay |
| Context of Use & Rationale | 54% | Inadequate justification for proposed COU, unclear drug development need |
Q3: How long does the qualification process typically take, and how can we manage timeline expectations?
Timelines often exceed targets. Recent analyses show FDA median review times for LOIs and Qualification Plans are more than double the agency's 3- and 6-month targets [90]. Sponsor development of Qualification Plans also takes significant time—a median of over 2.5 years, and nearly 4 years for surrogate endpoint biomarkers [90]. Plan for these extended timelines in your project management and budgeting.
Q4: What organizational structure is most successful for biomarker qualification programs?
Form collaborative consortia rather than pursuing qualification as a single entity. Analysis of EMA procedures shows consortia were more likely to opt for the Qualification of Novel Methodologies procedure and engage in follow-up procedures compared to single companies [89]. The FDA also encourages public-private partnerships, noting that resource requirements often exceed the capabilities of a single entity [86].
Q5: Our biomarker will be measured using a novel assay. What validation standards apply?
The FDA released a finalized "Bioanalytical Method Validation for Biomarkers" guidance in January 2025 [93]. However, the bioanalytical community has raised concerns that this guidance directs applicants to ICH M10, which explicitly states it does not apply to biomarkers [93]. Develop a COU-driven bioanalytical study plan that addresses the specific objectives of your biomarker measurement, rather than applying fixed validation criteria designed for drug analytes [93].
Special Considerations for Inflammatory Biomarkers
Inflammatory biomarkers present unique challenges in qualification. Based on analysis of qualified biomarkers, consider these specific aspects:
Disease Context Specificity: Ensure your COU precisely defines the inflammatory condition and patient population. Biomarkers qualified for one inflammatory condition may not transfer to others without additional validation.
Temporal Dynamics: Address how inflammatory biomarker levels fluctuate over time and in response to various stimuli, not just your investigational therapy.
Standardization Challenges: Implement rigorous assay standardization procedures to account for pre-analytical variables specific to inflammatory markers (e.g., sample processing timing, stability considerations).
Experimental Design and Validation Strategies
Evidence Generation Framework
Building a robust evidence package for inflammatory biomarker qualification requires addressing multiple validation aspects. The following visualization illustrates the interconnected components of a comprehensive validation strategy:
Research Reagent Solutions for Inflammatory Biomarker Development
Successful qualification requires high-quality reagents and materials throughout the development process. The table below outlines essential research reagents and their functions in inflammatory biomarker studies:
| Reagent/Material | Function in Biomarker Development | Specific Considerations for Inflammatory Biomarkers |
|---|---|---|
| Reference Standards | Establish assay calibration and performance metrics | Use well-characterized inflammatory mediators (e.g., cytokines, acute phase proteins) with documented purity and stability |
| Validated Antibodies | Detect and quantify biomarker levels | Verify specificity for target epitope; check cross-reactivity with related inflammatory molecules |
| Control Materials | Monitor assay performance and reproducibility | Include both positive and negative controls relevant to inflammatory conditions |
| Sample Collection Systems | Standardize pre-analytical variables | Use collection tubes with appropriate preservatives for labile inflammatory markers |
| Assay Platforms | Generate quantitative or qualitative measurements | Select platforms with sensitivity appropriate for physiological concentration ranges of inflammatory biomarkers |
| Data Management Tools | Organize, analyze, and document evidence | Implement systems that maintain data integrity and audit trails for regulatory scrutiny |
Navigating the Evolving Regulatory Landscape
Recent Developments and Future Directions
Regulatory science for biomarker qualification continues to evolve. Stay informed about these recent developments:
FDA Bioanalytical Method Validation: The January 2025 FDA guidance on biomarker bioanalysis, while controversial, represents the agency's current thinking on validation standards [93]. Monitor implementation and community feedback.
EMA Action Plan: The EMA has published an action plan for "future-proofing" qualification of novel methodologies, covering actions in 2024 and 2025 aligned with their Regulatory Science Strategy to 2025 [87].
Program Performance Improvements: Both agencies are working to enhance their qualification processes. The FDA's BQP has opportunities for reform, potentially including additional resources through user fees to address timeline issues [90].
Strategic Recommendations for Success
Based on analysis of successful qualification programs and common pitfalls, implement these strategies for your inflammatory biomarker:
Engage Early and Often: Take advantage of preliminary meeting opportunities and maintain regular communication with regulators throughout development.
Form Strategic Consortia: Build diverse collaborations including academic researchers, disease foundations, diagnostic companies, and pharmaceutical partners to pool resources and expertise.
Focus on Unmet Needs: Clearly articulate how your inflammatory biomarker addresses a specific drug development challenge not adequately met by existing tools.
Generate Robust, COU-Driven Evidence: Let your proposed Context of Use dictate the necessary evidence, with particular attention to analytical validation and biological plausibility.
Plan for Extended Timelines: Budget for a multi-year qualification process with adequate resources for evidence generation, regulatory interactions, and potential iterations.
By understanding these regulatory frameworks, anticipating common challenges, and implementing robust validation strategies, researchers can more effectively navigate the complex journey from exploratory inflammatory biomarker discovery to qualified drug development tools that advance precision medicine and patient care.
Frequently Asked Questions (FAQs) on Validation Methods
Q1: What is the core difference between cross-validation and independent replication?
- Cross-validation is a set of data sampling methods used to estimate the generalization performance of an algorithm on a single dataset by repeatedly partitioning it into training and testing sets [94]. Its primary goal is to prevent overoptimism in overfitted models during development [94].
- Independent replication involves validating a model or a finding on a completely new, independent dataset, often collected by a different research team [95] [96]. It is a cornerstone for establishing that a biomarker is "known valid," requiring widespread consensus in the scientific community about its significance [97].
Q2: When during model development should I use each method?
The following table summarizes the distinct roles of these methods:
| Method | Primary Goal | Typical Stage of Use | Key Outcome |
|---|---|---|---|
| Cross-Validation | Performance estimation, algorithm selection, hyperparameter tuning [94]. | Internal development phase on a single dataset. | Provides an estimate of model performance and helps select a robust model before external validation. |
| Independent Replication | Verify that findings generalize beyond the original sample and are not false positives [95] [96]. | Final validation phase, after model is locked. | Establishes robustness and clinical validity, moving a biomarker from "probable valid" to "known valid" [97]. |
Q3: Why might a biomarker fail to replicate in an independent cohort?
Failed replication can stem from discrepancies in several areas, as illustrated by a case in Alzheimer's research where a blood DNA methylation association with neurofilament light chain (NfL) was not replicated [95]:
- Study Design: Differences in cohort sizes, participant recruitment, and population genetics can introduce heterogeneity [95].
- Technical Factors: The use of different analytical platforms (e.g., ELISA vs. Proximity Extension Assay) with varying antibody sensitivities and specificities can lead to inconsistent results [95].
- Biological Factors: Unaccounted for population substructure or genuine biological differences between cohorts (e.g., disease stage) can affect the biomarker's signal [95].
- Statistical Power: The original finding could be a false positive, or the replication study might be underpowered to detect the effect [95].
Troubleshooting Guides
Issue 1: My Model Performs Well in Cross-Validation but Poorly on a New Independent Dataset
Potential Causes and Solutions:
- Cause: Non-Representative Test Sets or Data Shift
The patients in your original dataset are insufficiently representative of the patients in the new deployment domain [94].
- Solution: Ensure your original dataset is as representative as possible of the target population. Use stratified cross-validation for known subclasses (e.g., age groups) to preserve the overall class distribution in each fold [94].
- Cause: Overfitting and "Tuning to the Test Set"
Information from the test set has indirectly influenced how the model was trained, for example, by repeatedly modifying the model based on its holdout test set performance [94].
- Solution: Strictly separate your test set. Use nested cross-validation for hyperparameter tuning and algorithm selection. The final holdout test set should ideally be used only once to obtain an unbiased performance estimate [94].
- Cause: Inadequate Cross-Validation Design The cross-validation method did not properly estimate generalization error.
Issue 2: Planning an Independent Replication Study
A step-by-step protocol to maximize the chances of successful replication:
- Define Scope: Confirm the biomarker's intended use context (e.g., diagnostic, prognostic) as defined in your Quality Target Product Profile (QTPP) [99].
- Harmonize Methods:
- Cohort: Match key clinical and demographic characteristics of the original discovery cohort (e.g., disease stage, age, sex) [95] [96].
- Technology: Use the same analytical platform or demonstrate equivalence between platforms (e.g., Olink, SomaScan, ELISA) [95] [96].
- Analysis: Apply the same pre-processing, normalization, and statistical model. If possible, use the original analytical code [95].
- Ensure Analytical Validity: The assay used in the replication must itself be validated, demonstrating performance characteristics like specificity, accuracy, and precision [97] [100].
- Execute and Compare: Run the pre-specified analysis on the independent cohort and compare the effect size and direction with the original study. High concordance indicates a robust finding [96].
Experimental Protocols
Protocol 1: Implementing a k-Fold Cross-Validation with a Holdout Test Set
This is a robust method for model development and performance estimation [94].
Methodology:
- Initial Split: Randomly split the entire dataset into a training/validation set (e.g., 80%) and a final holdout test set (e.g., 20%). The holdout set is locked away and not used in any model development [94].
- Create Folds: Partition the training/validation set into k disjoint folds (typically k=5 or k=10) [94].
- Cross-Validation Loop: For each of the k iterations:
- Designate one fold as the validation set and the remaining k-1 folds as the training set.
- Train the model on the training set.
- Tune hyperparameters and/or select algorithms based on performance on the validation set.
- Once the model is finalized, assess its performance on the validation set.
- Aggregate Performance: Calculate the average performance across all k folds for a stable estimate.
- Final Model: Train the final model on the entire training/validation set using the optimized hyperparameters.
- Final Test: Evaluate the final model once on the withheld holdout test set to obtain an unbiased estimate of its generalization performance [94].
Protocol 2: Design for a Multi-Cohort Independent Replication Study
This protocol is based on robust practices demonstrated in recent high-impact biomarker studies [95] [96].
Methodology:
- Discovery Phase:
- Replication Phase:
- Apply the model, without retraining or modification, to a fully independent cohort (Cohort B) [96].
- Statistically assess the concordance of effect sizes and directions for the identified biomarkers between Cohort A and Cohort B. Successful replication is characterized by high concordance (e.g., R > 0.8) and consistent directional effects [96].
- Validation and Specificity:
Key Research Reagent Solutions
The following table details essential materials and platforms used in modern biomarker research, as cited in the literature.
| Item | Function in Validation | Exemplar Use Case |
|---|---|---|
| Olink Explore 3072 Platform | High-throughput proteomics for measuring ~3,000 plasma proteins; provides normalized protein expression (NPX) values [96]. | Used to identify a 33-protein signature for Amyotrophic Lateral Sclerosis (ALS) [96]. |
| SomaScan Assay | Alternative proteomic platform using aptamer-based technology to measure thousands of proteins [96]. | Used for cross-platform validation of protein biomarkers in CSF [96]. |
| ELISA Kits | Gold-standard, quantitative immunoassay for validating specific protein biomarkers [95]. | Used to quantify neurofilament light chain (NfL) and YKL-40 levels in validation studies [95] [96]. |
| Bisulfite Conversion Kits | Prepares DNA for methylation analysis by converting unmethylated cytosines to uracils [95]. | Essential for epigenome-wide association studies (EWAS) investigating DNA methylation biomarkers in blood [95]. |
| Genetic Ancestry Panels | Controls for population stratification, a major confounder in genetic and epigenetic association studies [95]. | Included as covariates in regression models to ensure findings are not due to population structure [95]. |
Performance Benchmarks: CRP, ESR, and PCT Across Clinical Conditions
The table below summarizes the diagnostic performance of C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), and procalcitonin (PCT) across various clinical contexts, based on recent research. This data serves as a key benchmark for validating new inflammatory biomarkers.
| Clinical Context | Biomarker | Sensitivity (%) | Specificity (%) | AUC | Cut-off Value | Citation |
|---|---|---|---|---|---|---|
| Pediatric Septic Arthritis | CRP | 89.7 | 88.0 | 0.950 | >10 mg/L | [101] |
| PCT | 17.2 | 96.0 | 0.574 | >0.25 ng/mL | [101] | |
| Late-Onset Neonatal Sepsis | CRP | 77.5 | 87.5 | Not Reported | >5 mg/dL | [102] |
| PCT | 77.5 | 70.0 | Not Reported | >2 ng/mL | [102] | |
| Fracture-Related Infections (Combined) | CRP & PCT | 90.5 | 96.8 | Not Reported | CRP >10 mg/L; PCT >2 ng/mL | [103] |
| Postoperative Spondylodiscitis | CRP | Not Reported | 100.0 | Not Reported | >43.7 mg/L | [104] |
| ESR | 92.9 | Not Reported | Not Reported | >46 mm/h | [104] | |
| PCT | 96.2 | Not Reported | Not Reported | >0.034 ng/mL | [104] | |
| Orthopaedic Infections (General) | ESR or CRP | 52 - 83 | 52 - 83 | Not Reported | Variable | [105] |
Essential Experimental Protocols for Biomarker Comparison
Protocol 1: Retrospective Cohort Study for Diagnostic Accuracy
This methodology is commonly used to establish the diagnostic efficacy of a novel biomarker against gold-standard cultures [101] [103].
- Study Population: Recruit patients suspected of having the target condition (e.g., infection) alongside a control group with non-infectious inflammatory conditions. Strict inclusion/exclusion criteria are critical.
- Gold Standard Reference: Use joint fluid culture for septic arthritis [101] or blood culture for neonatal sepsis [102] to definitively classify patients into "disease" and "non-disease" groups.
- Sample Collection: Collect blood samples for biomarker analysis (CRP, PCT, and the novel biomarker) concurrently with samples for the gold-standard test, prior to initiating antibiotic therapy [101].
- Laboratory Analysis:
- Data Analysis: Perform Receiver Operating Characteristic (ROC) analysis to determine the Area Under the Curve (AUC), optimal cut-off values, sensitivity, and specificity for each biomarker [101] [104].
Protocol 2: Longitudinal Monitoring of Biomarker Kinetics
This protocol assesses a biomarker's utility for monitoring treatment response and predicting clinical outcomes [102] [103].
- Study Design: Prospective observational study in a clinical setting (e.g., NICU or orthopedic ward).
- Sampling Timeline: Collect blood samples at multiple time points:
- Outcome Correlation: Measure biomarker levels at each time point and correlate them with clinical outcomes such as:
The Scientist's Toolkit: Research Reagent Solutions
The table below lists essential materials and their functions for conducting the experiments described in the protocols.
| Item | Function / Application | Example / Specification |
|---|---|---|
| Roche Cobas 8000 Analyzer | Modular clinical chemistry analyzer for performing immunoturbidimetric CRP assays. | Roche Diagnostics [101] |
| Roche Cobas e601 Analyzer | Immunoassay analyzer for performing Electrochemiluminescence (ECLIA) PCT tests. | Roche Diagnostics [101] |
| Roche Elecsys BRAHMS PCT Kit | Commercial kit for specific and quantitative measurement of Procalcitonin. | Roche Diagnostics [102] |
| Blood Culture Bottles | For sterile inoculation and growth of pathogens from joint fluid or blood. | Becton-Dickinson anaerobic or BactecPeds Plus/F bottles [101] |
| Specialized Culture Media | For sub-culturing and identifying bacteria from positive cultures. | Blood agar plates (aerobic), Anaerobic culture media [101] |
| Biochemical Test Strips | For precise bacterial identification from positive cultures via sugar fermentation and enzymatic tests. | Arabinose, Xylose, Catalase, Oxidase, etc. [102] |
| SPSS Software | Statistical software for data analysis, including t-tests, chi-square tests, and ROC analysis. | IBM SPSS version 23 or later [102] [103] |
Frequently Asked Questions (FAQs) for Troubleshooting
Q1: Our novel biomarker shows excellent AUC in a retrospective study, but it fails to correlate with treatment response in a longitudinal design. What could be the issue?
- A: This is a common challenge. The kinetic profile of your biomarker may not align with the clinical recovery timeline. CRP, for instance, rises and falls rapidly, while ESR changes more slowly [106]. Review the fundamental biology of your biomarker—its half-life and the dynamics of its production and clearance. Your sampling frequency may be misaligned with its natural kinetic profile. Furthermore, ensure that the clinical outcomes you are measuring (e.g., "infection control") are objectively defined and consistently applied [103].
Q2: When benchmarking against PCT for bacterial infections, our biomarker's sensitivity is significantly lower. How can we investigate this further?
- A: First, analyze performance within specific patient subgroups. PCT is known to be highly specific for systemic bacterial infections, but its sensitivity can be low in localized infections like early septic arthritis [101]. Stratify your analysis by infection type (localized vs. systemic), causative pathogen (gram-positive vs. gram-negative), and patient factors (immunocompetent vs. immunocompromised). This can reveal contexts where your biomarker may have superior utility despite lower overall sensitivity.
Q3: The diagnostic cut-off values for established biomarkers like CRP and PCT vary widely across the literature. How do we select the appropriate benchmark for our study?
- A: You should not rely on a single value from the literature. The optimal cut-off is context-dependent and influenced by the patient population, the specific clinical question (ruling in vs. ruling out disease), and the assay manufacturer's guidelines. The best practice is to use your own data to determine a population-specific cut-off value via ROC analysis [101] [104]. Clearly report the sensitivity and specificity at this chosen cut-off to allow for direct comparison with other studies.
Q4: A reviewer criticized our study for using ESR as a comparator, calling it a "zombie test." How should we respond, and should we include it in future studies?
- A: This criticism is grounded in recent literature. Some experts argue that ESR and CRP have limited diagnostic accuracy for infections, with sensitivity and specificity often ranging from 52-83%, and that they should not be routinely ordered together [105]. You can acknowledge this limitation and justify ESR's inclusion in your study based on its historical use and continued presence in certain diagnostic criteria (e.g., for rheumatoid arthritis [107]). For future studies, the strongest design benchmarks new biomarkers against the most specific available tests (like PCT for bacterial sepsis) and focuses on clinical outcomes rather than just correlation with older markers.
Incorporating Real-World Evidence (RWE) to Strengthen Clinical Validity
Frequently Asked Questions (FAQs) on RWE for Biomarker Research
Q1: What are the core definitions of Real-World Data (RWD) and Real-World Evidence (RWE)?
- Real-World Data (RWD) is data relating to patient health status and/or the delivery of health care routinely collected from a variety of sources. These sources include electronic health records (EHRs), claims and billing data, product and disease registries, and patient-generated data (including from wearable devices) [108] [109] [110].
- Real-World Evidence (RWE) is the clinical evidence about the usage and potential benefits or risks of a medical product derived from the analysis of RWD [109] [110]. In the context of your research, RWE provides information on how biomarkers perform and predict outcomes in diverse, routine clinical practice settings, beyond the controlled environment of a Randomized Controlled Trial (RCT).
Q2: How can RWE support the clinical validation of novel inflammatory biomarkers?
RWE can strengthen clinical validity by demonstrating a biomarker's performance and prognostic value in broader, more heterogeneous patient populations. It helps answer questions about how a biomarker behaves in patients with comorbidities, different demographics, and in real-world treatment settings. For instance, a study on C-reactive protein (CRP) dynamics in extensive-stage small cell lung cancer used RWE to show that early reduction in CRP levels during treatment was a significant predictor of improved overall survival, thereby validating its utility as a prognostic biomarker in a real-world cohort [111].
Q3: What are the key regulatory considerations for using RWE to support biomarker validation?
Regulatory agencies like the FDA encourage the use of RWE but have specific expectations [109] [112]:
- Early Engagement: It is crucial to engage with regulators early in the process to discuss the appropriateness of the study design and data sources [113] [109] [112].
- Transparency: Be prepared to submit detailed protocols, statistical analysis plans, and patient-level data for review. The FDA emphasizes transparency in data collection and analysis [109].
- Data Quality and Integrity: Regulatory acceptance depends on demonstrating that RWD sources are fit for purpose, with rigorous data governance and validation processes in place [109] [110]. The FDA's Advancing RWE Program is one forum for such discussions [113] [109].
Q4: What are common methodological challenges when incorporating RWE, and how can they be addressed?
A primary challenge is dealing with unobserved confounders—variables that are not measured in the RWD but could influence both the treatment/exposure and the outcome, potentially leading to biased results [108]. Other significant challenges include ensuring data quality and standardization from diverse sources, and managing data privacy and security [110].
Table: Common RWE Challenges and Mitigation Strategies
| Challenge | Potential Mitigation Strategy |
|---|---|
| Unobserved Confounding | Use advanced statistical methods (e.g., propensity score matching, instrumental variables) to balance comparison groups and reduce bias [108] [112]. |
| Data Quality & Standardization | Implement robust data governance frameworks. Use standardized data models (e.g., HL7, FHIR) to harmonize data from different sources like EHRs and registries [110]. |
| Privacy & Security | Adhere to regulations like HIPAA and GDPR. Employ data anonymization and de-identification techniques to protect patient privacy [110]. |
| Regulatory Acceptance | Engage with regulatory agencies early, align study designs with FDA/EMA guidance, and maintain transparent documentation of all processes [109] [112]. |
Troubleshooting Guides for RWE Integration
Guide 1: Addressing Data Quality and Completeness Issues
Problem: Inconsistent, missing, or non-standardized data from Electronic Health Records (EHRs) and other RWD sources.
Steps for Resolution:
- Conduct a Data Provenance Assessment: Before analysis, document the origin of your data, the context of its collection (e.g., for clinical care vs. billing), and any transformations it has undergone. This helps identify potential biases [108].
- Implement a Data Validation Plan:
- Create a checklist for data elements critical to your biomarker study (e.g., lab values, diagnosis codes, medication records).
- Run checks to identify missing values, outliers, and internal inconsistencies.
- Use natural language processing (NLP) techniques to extract and standardize information from unstructured clinical notes [112].
- Apply Data Curation and Harmonization:
- Map local coding systems (e.g., internal lab codes) to common standard terminologies (e.g., LOINC for lab tests, SNOMED CT for diagnoses).
- Develop and document algorithms to define key study variables (e.g., how a "case" of a specific disease is identified from a combination of diagnosis codes, prescriptions, and procedures) [109].
Guide 2: Mitigating Bias and Confounding in RWE Studies
Problem: The non-randomized nature of RWE can lead to biased estimates of a biomarker's effect or association.
Steps for Resolution:
- A Priori Protocol Development: Pre-specify your research question, hypothesis, analysis plan, and methods for confounding control in a protocol. Register the protocol on a site like ClinicalTrials.gov to enhance transparency and reduce the risk of data dredging [109].
- Design and Analysis Techniques:
- Propensity Score Matching: This method creates a balanced cohort by matching each patient in the "exposed" group (e.g., those with a high biomarker level) with a patient in the "unexposed" group (e.g., those with a low biomarker level) who has a similar probability (propensity) of being exposed based on all other observed covariates [112].
- Sensitivity Analyses: Perform additional analyses to test how robust your findings are to potential unmeasured confounding. This assesses how strong an unmeasured confounder would need to be to nullify your observed result [108].
Case Study: Validating CRP Dynamics as a Prognostic Biomarker with RWE
The following workflow and data are based on a real-world study investigating early CRP reduction as a predictor of survival in extensive-stage small cell lung cancer patients treated with immunotherapy [111].
Experimental Protocol
Objective: To determine whether early changes in systemic inflammation markers, particularly CRP, predict overall survival (OS) in a real-world cohort.
Methodology:
- Cohort Definition: Retrospective, single-center study of 35 ES-SCLC patients.
- Intervention: First-line adebrelimab (anti-PD-L1) plus platinum-etoposide or platinum-irinotecan chemotherapy.
- Biomarker Measurement:
- Timepoints: Baseline (pre-treatment) and after 2 months of therapy.
- Markers Assessed: Ten systemic inflammation markers were evaluated, including NLR, PLR, LMR, SII, CRP, and LDH.
- Trend Calculation: The inflammatory trend was quantified as the ratio of the 2-month value to the baseline value (e.g., Trend = CRP~2-month~ / CRP~baseline~).
- Outcome Definition: "Improvement" for CRP was defined as a trend ratio <1 (indicating a decrease from baseline). The primary endpoint was overall survival from 2 months post-treatment initiation (OS2).
- Statistical Analysis: Associations between inflammation dynamics and survival were evaluated using Kaplan-Meier analysis and Cox regression.
Key Experimental Findings
The study successfully generated RWE supporting the prognostic value of dynamic CRP measurement.
Table: Key Efficacy Outcomes from the RWE CRP Study [111]
| Outcome Measure | Result for Patients with CRP Reduction (Trend <1) | Result for Patients without CRP Reduction (Trend ≥1) | Statistical Significance |
|---|---|---|---|
| Median Overall Survival (OS) | 16.2 months | 8.1 months | Hazard Ratio (HR) = 3.49295% CI: 1.239–9.847P = 0.011 |
| Association with Radiologic Response | No significant association found with best overall response or tumor regression (P>0.05) |
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Materials for RWE Biomarker Studies
| Item / Reagent | Function / Application in RWE Context |
|---|---|
| Electronic Health Record (EHR) Data | Provides comprehensive, longitudinal patient data including diagnoses, lab values (e.g., CRP), medications, and outcomes for analysis [110] [112]. |
| Data Harmonization Tools (e.g., HL7 FHIR Standards) | Enable standardization and interoperability of data pulled from disparate EHR systems and other RWD sources, making it analyzable [110]. |
| Statistical Software (e.g., R, Python, SAS) | Performs advanced statistical analyses, including propensity score matching and Cox regression, to handle confounding and test associations in observational data [111] [112]. |
| Propensity Score Models | A statistical method used to simulate randomization by creating balanced comparison groups based on observed covariates, thus reducing selection bias [108] [112]. |
| Natural Language Processing (NLP) Algorithms | Extract and structure relevant clinical information (e.g., disease status, symptom severity) from unstructured physician notes in EHRs [112]. |
Workflow for Integrating RWE into Clinical Validation
The following diagram outlines a systematic approach for incorporating RWE into your inflammatory biomarker research program.
Economic and Operational Considerations for Clinical Integration and Adoption
Troubleshooting Guides and FAQs
This section addresses common operational and economic challenges faced during the clinical validation and integration of novel inflammatory biomarkers.
Frequently Asked Questions
Q1: What is the single most critical factor to define before starting a biomarker validation study? A: The Context of Use (COU). This is a formal, concise description of the biomarker's specified purpose, which dictates every aspect of your study design, from statistical plans to patient populations [38]. The COU includes the biomarker category (e.g., prognostic, diagnostic) and its intended application in drug development or clinical practice.
Q2: Our validation study failed because the biomarker's performance was inconsistent. What could have gone wrong? A: A common root cause is insufficient Analytical Validation preceding Clinical Validation. Before a biomarker's clinical utility can be assessed, the measurement assay itself must be analytically validated to ensure its sensitivity, specificity, accuracy, and precision are acceptable and reliable. Without this, observed variability may stem from the test method rather than the biology [38].
Q3: How can we make a compelling economic case for adopting a novel inflammatory biomarker like IL-6 in heart failure? A: Frame the biomarker as a tool for precision medicine that reduces residual risk. For instance, demonstrate that elevated IL-6 identifies heart failure patients with a higher risk of adverse events despite standard care. This stratification can justify targeted anti-inflammatory therapies or more intensive monitoring, potentially preventing costly hospitalizations and improving outcomes, which is a significant economic driver [114].
Q4: What is a major operational consideration when validating a predictive biomarker? A: Predictive biomarker validation requires an interventional study design. You must test the biomarker in patients exposed to the specific therapeutic intervention to establish its ability to identify responders. This often necessitates running the validation as an ancillary study to an ongoing clinical trial, which requires significant operational coordination and planning [38].
Q5: Why is a biomarker like hsCRP useful even if it is not causally involved in the disease? A: While hsCRP is a downstream marker with no causal role, it serves as a robust and measurable indicator of underlying systemic inflammation. This makes it highly valuable for risk stratification and monitoring treatment response, as evidenced by its use in large trials like JUPITER and CANTOS [114].
Q6: How do we justify the cost of developing a biomarker signature versus a single biomarker? A: While more complex, a composite biomarker signature can provide a more comprehensive assessment of a complex biological process like inflammation. The justification comes from demonstrating a statistically significant improvement in accuracy or predictive power over any single marker or existing standard, leading to better clinical decisions and resource allocation [38] [115].
Quantitative Data on Key Inflammatory Biomarkers
The tables below summarize core and emerging inflammatory biomarkers relevant to clinical research, particularly in cardiovascular disease.
Table 1: Core Clinically Utilized Inflammatory Biomarkers
| Biomarker | Primary Source | Key Clinical Interpretation | Temporal Dynamics |
|---|---|---|---|
| High-Sensitivity CRP (hsCRP) [114] | Liver (induced by IL-6) | Marker of systemic inflammation; used for cardiovascular risk stratification [114]. | Rises and falls rapidly (hours). Good for short-term monitoring [116]. |
| Erythrocyte Sedimentation Rate (ESR) [116] | Influenced by plasma fibrinogen | Non-specific marker of long-term or chronic inflammation [116]. | Changes slowly; can remain elevated after inflammation resolves [116]. |
| Interleukin-6 (IL-6) [114] | Immune cells, endothelial cells | Pro-inflammatory cytokine; causal driver in atherosclerosis and heart failure; key therapeutic target [114]. | Early responder; orchestrates broader inflammatory response [114]. |
| Ferritin [116] | Most cells (iron storage) | Acute-phase reactant; high levels indicate iron overload or inflammation [116]. | Must be interpreted with CRP and iron studies to distinguish causes [116]. |
Table 2: Emerging Research-Based Biomarker Ratios
| Ratio / Index Name | Calculation | Proposed Research Context / Interpretation |
|---|---|---|
| Systemic Immune-Inflammation Index (SII) [115] | (Platelets × Neutrophils) / Lymphocytes | Represents systemic immune activation and inflammation balance [115]. |
| Neutrophil-Lymphocyte Ratio (NLR) [115] | Neutrophils / Lymphocytes | Simple indicator of systemic inflammation; studied in febrile seizures, cancer, CVD [115]. |
| CRP / Albumin Ratio (CAR) [116] | CRP / Albumin | Links inflammatory status with nutritional status [116]. |
| Platelet / Lymphocyte Ratio (PLR) [116] | Platelets / Lymphocytes | Reflects balance between clotting potential and immune status [116]. |
| Monocyte / HDL Ratio (MHR) [116] | Monocytes / HDL Cholesterol | Compares pro-inflammatory immune cells with "protective" HDL cholesterol [116]. |
Experimental Protocols for Biomarker Validation
This section provides detailed methodologies for key experiments in the clinical validation of inflammatory biomarkers.
Protocol 1: Analytical Validation of a Novel Biomarker Assay
Objective: To establish that the assay used to measure the biomarker is technically reliable and reproducible before clinical validation [38].
Materials:
- Calibrators and controls
- Patient sample cohorts (fresh and frozen)
- Assay platform (e.g., ELISA, clinical chemistry analyzer, multiplex immunoassay system)
Procedure:
- Precision: Measure the coefficient of variation (CV) by repeatedly testing pooled samples with low, medium, and high biomarker concentrations within a single run (intra-assay) and across different days, operators, and lots (inter-assay).
- Accuracy/Recovery: Spike known quantities of the biomarker into a sample matrix and measure the percentage recovery by the assay.
- Linearity and Range: Serially dilute high-concentration samples and confirm the measured value is proportional to the expected value across the assay's claimed range.
- Limit of Detection (LoD) & Quantification (LoQ): Determine the lowest concentration distinguishable from zero (LoD) and the lowest concentration that can be measured with acceptable precision and accuracy (LoQ) by repeatedly measuring blank and low-concentration samples.
- Sample Stability: Test biomarker levels in samples subjected to various storage conditions (time, temperature, freeze-thaw cycles) to define handling protocols.
Protocol 2: Clinical Validation of a Prognostic Biomarker (e.g., IL-6 in Heart Failure)
Objective: To evaluate the biomarker's ability to predict the likelihood of a clinical event (e.g., hospitalization or death) in individuals with a specific medical condition (e.g., heart failure) over a defined period [114] [38].
Study Design: Prospective, observational cohort study.
Patient Population: Well-characterized cohort of patients with heart failure (e.g., HFrEF, HFpEF). Sample size must be powered for the expected event rate.
Materials:
- Patient plasma/serum samples
- Validated assay for the biomarker (e.g., hsCRP or IL-6 ELISA)
- Validated assay for a reference standard (e.g., NT-proBNP)
- Clinical data collection system (e.g., electronic health records, case report forms)
Procedure:
- Baseline Sampling: Collect blood samples from all enrolled patients at baseline. Process and store samples according to a standardized, analytically validated protocol.
- Blinded Measurement: Measure the concentration of the novel inflammatory biomarker (e.g., IL-6) and reference standards (e.g., NT-proBNP, hsCRP) in all baseline samples.
- Follow-up: Actively follow all patients for a pre-specified period (e.g., 1-3 years) to record the occurrence of pre-defined primary endpoint events (e.g., HF hospitalization, cardiovascular mortality).
- Statistical Analysis:
- Use Cox proportional hazards models to assess the association between baseline biomarker levels (often log-transformed) and the time to the clinical event.
- Calculate hazard ratios (HR) per standard deviation increase in the biomarker.
- Assess model discrimination using the C-statistic to see if adding the novel biomarker (IL-6) improves the C-statistic over a model containing only established risk factors and standard biomarkers (e.g., NT-proBNP).
- Perform reclassification analysis (NRI - Net Reclassification Index) to determine if the new biomarker correctly reclassifies patients into higher or lower risk categories.
Signaling Pathways and Workflows
Inflammatory Pathway in Heart Failure
This diagram illustrates the central role of IL-6 signaling in the pathogenesis of heart failure, connecting comorbidities to cardiac dysfunction.
Biomarker Validation Workflow
This flowchart outlines the key stages from biomarker discovery to full clinical integration and adoption.
Research Reagent Solutions
Table 3: Essential Materials for Inflammatory Biomarker Research
| Item / Reagent | Function / Application | Example / Notes |
|---|---|---|
| High-Sensitivity ELISA Kits | Quantifying low levels of inflammatory mediators (e.g., IL-6, IL-1β) in serum/plasma [114]. | Critical for measuring baseline levels in chronic diseases; choose kits with validated low limits of detection. |
| Multiplex Immunoassay Panels | Simultaneously measuring multiple cytokines, chemokines, and biomarkers from a single small-volume sample [115]. | Ideal for discovery phases and profiling inflammatory signatures; platforms include Luminex and MSD. |
| CRP and hsCRP Assays | Measuring C-reactive protein for general inflammation and high-sensitivity for cardiovascular risk assessment [114] [116]. | Available on many clinical chemistry analyzers; ensure the hsCRP assay has a reportable range down to ~0.2 mg/L. |
| Anticoagulated Blood Collection Tubes | Obtaining plasma for biomarker analysis. | EDTA tubes are standard for most assays. Consistency in tube type across a study is critical for pre-analytical control. |
| Programmed Freezers (-80°C) | Long-term storage of biological samples for batch analysis and future validation studies [117]. | Maintain sample integrity; monitor freezer temperatures continuously. |
| Clinical Data Management System (CDMS) | Managing and integrating de-identified clinical data with biomarker results [38] [117]. | Essential for statistical analysis of correlations and outcomes; must be compliant with data sharing policies (e.g., NIH DMS). |
Conclusion
The successful clinical validation of novel inflammatory biomarkers hinges on a meticulous, multi-faceted strategy that integrates robust science with pragmatic regulatory and clinical understanding. Key takeaways include the non-negotiable need for rigorous analytical validation, the critical importance of distinguishing between prognostic and predictive utility through appropriate statistical interaction tests, and the value of dynamic, multi-timepoint assessment over single measurements. Looking forward, the field will be shaped by the integration of AI and multi-omics approaches, the expansion of liquid biopsies for non-invasive monitoring, and the growing acceptance of real-world evidence. By adhering to a structured, evidence-based framework, researchers can overcome historical validation hurdles, enhance the predictive power of inflammatory disease management, and ultimately deliver on the promise of precision medicine.
References
- 1. Common Lab Issues That Impact Biomarker Data [https://blog.omni-inc.com/blog/common-lab-issues-that-impact-biomarker-data]
- 2. Rethinking the biomarker landscape in gastric cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12476615/]
- 3. The Diagnostic Role of Tumor and Inflammatory ... [https://pubmed.ncbi.nlm.nih.gov/41010973/]
- 4. The Importance of Predictive Biomarkers and Their ... [https://www.mdpi.com/2227-9059/12/9/2146]
- 5. a population-based (NHANES) and clinical validation study [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1697617/full]
- 6. How to Apply Scientific Troubleshooting Principles to Any ... [https://www.linkedin.com/pulse/how-apply-scientific-troubleshooting-principles-any-problem-yeatman]
- 7. Teaching troubleshooting skills to graduate students - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11407763/]
- 8. Navigating Biomarker Testing: Frequently Asked Questions [https://www.lung.org/lung-health-diseases/lung-disease-lookup/lung-cancer/symptoms-diagnosis/biomarker-testing/biomarker-faqs]
- 9. Beyond ELISA: the future of biomarker validation [https://www.drugtargetreview.com/article/154316/beyond-elisa-the-future-of-biomarker-validation/]
- 10. Biomarker Discovery: Types, Phases and Applications [https://lifesciences.danaher.com/us/en/library/biomarker-discovery.html]
- 11. Biomarkers in Clinical Practice: Challenges & Opportunities [https://esmed.org/biomarkers-in-clinical-practice-challenges-opportunities/]
- 12. Biomarker Validation Guide 2025: Discovery to FDA Approval [https://www.motif.bio/blog/biomarker-discovery-validation-guide-2025]
- 13. Misinterpretation and misapplication of biomarkers in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11974923/]
- 14. BIOMARKERS: HOPES AND CHALLENGES IN THE PATH ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4402218/]
- 15. Biomarker Validation: Common Data Analysis Concerns [https://pmc.ncbi.nlm.nih.gov/articles/PMC4122484/]
- 16. Why Do Biomarkers Fail? [https://sonraianalytics.com/why-do-biomarkers-fail/]
- 17. Biomarker discovery pipeline: 3 Critical Steps 2025 [https://lifebit.ai/blog/biomarker-discovery-pipeline/]
- 18. The Complete Guide to Biomarker Testing [https://superpower.com/library/guide-to-biomarker-testing?srsltid=AfmBOoodaoO6pfoaGOM9Azj9MwF00PwDMWA5QOTRJiKFuPjrVpf1vMR8]
- 19. Orphan Disease Biomarkers Market Size, Report by 2034 [https://www.precedenceresearch.com/orphan-disease-biomarkers-market]
- 20. Rare Disease Focus: FDA's Trio of Cell and Gene Therapy ... [https://www.ropesgray.com/en/insights/alerts/2025/11/rare-disease-focus-fdas-trio-of-cell-and-gene-therapy-draft-guidances-highlight-expedited-programs]
- 21. Preparation for blood tests: what can go wrong before the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12377977/]
- 22. Preanalytical Errors in Clinical Laboratory Testing at a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10981510/]
- 23. Expert Pre-Analytical Work Processing - Sampled [https://sampled.com/the-critical-role-of-pre-analytical-work/]
- 24. The Effect of Preanalytical Conditions on Blood-Based ... [https://pubmed.ncbi.nlm.nih.gov/40531187/]
- 25. Pre-analytical considerations in biomarker research: focu... [https://www.degruyterbrill.com/document/doi/10.1515/cclm-2021-0377/html?lang=en&srsltid=AfmBOooplwBtlsDfR2Br8ZaLAFfmJir_n5GZ_VkxUaNHOoYOb-9IIBr4]
- 26. New insights in preanalytical quality [https://www.degruyterbrill.com/document/doi/10.1515/cclm-2025-0478/html?lang=en&srsltid=AfmBOooAMggd5_oA20sVRXl6N_hJeIQbVnJQY-4H_-sn0Isd8Deiverm]
- 27. Exploring technical aspects of biomarker assays - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK513094/]
- 28. Method Validation Guidelines [https://www.biopharminternational.com/view/method-validation-guidelines]
- 29. Molecular Diagnostics - Part 5: Analytical Sensitivity and ... [https://blog.seracare.com/molecular-serology-blog/verification-part5]
- 30. ICH and FDA Guidelines for Analytical Method Validation [https://www.labmanager.com/ich-and-fda-guidelines-for-analytical-method-validation-34252]
- 31. How To Perform Specificity In Analytical Method Validation [https://pharmaguru.co/specificity-in-analytical-method-validation/]
- 32. ICH Guidelines for Analytical Method Validation Explained [https://amsbiopharma.com/ich-guidelines-analytical-method/]
- 33. Top Mistakes in Analytical Method Validation and How to ... [https://www.pharmoutsourcing.com/Featured-Articles/350046-Top-Mistakes-in-Analytical-Method-Validation-and-How-to-Avoid-Them/]
- 34. Analytical Method Validation Questions and Answers [https://www.complianceonline.com/resources/analytical-method-validation-questions-and-answers.html]
- 35. Troubleshooting Guide: ELISA [https://www.rndsystems.com/resources/troubleshooting-guide-elisa-development]
- 36. MSD Assay Services | Biomarker Analysis [https://www.bioagilytix.com/techniques/instrumentation/msd-assay/]
- 37. Comparative Overview of Luminex and MSD Platforms For ... [https://kcasbio.com/blogs/comparative-overview-of-luminex-and-msd-platforms-for-biomarker-analysis/]
- 38. Biomarker Program FAQs [https://www.ninds.nih.gov/current-research/focus-tools-topics/biomarkers-research/biomarker-program-faqs]
- 39. Biomarker Qualification Program Submission Frequently ... [https://www.fda.gov/drugs/biomarker-qualification-program/biomarker-qualification-program-submission-frequently-asked-questions]
- 40. A guide to interpreting the area under the curve value [https://pmc.ncbi.nlm.nih.gov/articles/PMC10664195/]
- 41. Methods of determining optimal cut-point of diagnostic ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-024-02198-2]
- 42. ROC curve analysis: a useful statistic multi-tool in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11266376/]
- 43. ROC curve analysis: predictive values calculator [https://www.medcalc.org/en/manual/roc-curve-analysis-predictive-values.php]
- 44. Interpretable machine learning for predicting early ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12582914/]
- 45. Systemic Inflammatory Biomarkers as a Predictive Markers for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12050043/]
- 46. Chapter 1 Clinical validation of biomarkers for predicting risk [https://www.sciencedirect.com/science/article/abs/pii/S0065242309480016]
- 47. Development and validation of machine learning models ... [https://www.nature.com/articles/s41698-024-00719-2]
- 48. Receiver operating characteristic [https://en.wikipedia.org/wiki/Receiver_operating_characteristic]
- 49. Evaluating Risk Prediction with ROC Curves [https://www.publichealth.columbia.edu/research/population-health-methods/evaluating-risk-prediction-roc-curves]
- 50. Methodological Insights on Biomarkerâ€Based Patient Selection [https://pmc.ncbi.nlm.nih.gov/articles/PMC11993284/]
- 51. Biomarkers: how to consolidate them in clinical practice [https://www.reumatologiaclinica.org/en-biomarkers-how-consolidate-them-in-avance-S2173574324000947]
- 52. Prospective validation study of prognostic biomarkers to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7789210/]
- 53. Association of inflammatory biomarkers with clinical ... [https://www.sciencedirect.com/science/article/pii/S0168827820304797]
- 54. A Perspective on Challenges and Issues in Biomarker ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2773185/]
- 55. Barriers to biomarker development and clinical translation [https://www.sciencedirect.com/science/article/pii/S0169409X21002465]
- 56. Value of dynamic changes in inflammatory biomarkers for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12515928/]
- 57. Dynamic Sensor Selection for Biomarker Discovery [https://arxiv.org/html/2405.09809v5]
- 58. A causal perspective on batch effects - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12319767/]
- 59. Thinking points for effective batch correction on biomedical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11471903/]
- 60. Understanding and Mitigating Batch Effects in Histopathology [https://www.trillium.de/en/journals/trillium-pathology/archive/2025/tp-1/2025/computational-pathology/image-analysis-understanding-and-mitigating-batch-effects-in-histopathology.html]
- 61. The reproducibility “crisis†- PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC5579390/]
- 62. How to solve the Scientific Reproducibility Crisis [https://sonraianalytics.com/how-to-solve-the-scientific-reproducibility-crisis/]
- 63. 4 Handy Tips For Correcting Batch Effects | ScRNA-seq ... [https://www.pythiabio.com/post/4-handy-tips-for-correcting-batch-effects-scrna-seq-analysis-101]
- 64. High performance data integration for large-scale analyses ... [https://www.nature.com/articles/s41467-025-62237-4]
- 65. Protein-level batch-effect correction enhances robustness ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12586625/]
- 66. Fit-for-purpose biomarker method validation for application ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2990602/]
- 67. Development and validation of prognostic models using ... [https://pubmed.ncbi.nlm.nih.gov/40663026/]
- 68. Development and validation of a novel nutrition ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1658896/full]
- 69. Discovery and Clinical Validation of C1M and C4M as ... [https://www.jrheum.org/content/early/2025/08/25/jrheum.2025-0671]
- 70. Bridging the United States population diversity gaps in clinical ... [https://pubmed.ncbi.nlm.nih.gov/40358454/]
- 71. Bridging the Gap: Translating Preclinical Biomarkers to ... [https://blog.crownbio.com/bridging-the-gap-translating-preclinical-biomarkers-to-clinical-success]
- 72. Understanding biomarker validation, qualification challenges [https://www.techtarget.com/pharmalifesciences/feature/Understanding-biomarker-validation-qualification-challenges]
- 73. Evolving demographics of eligible patient population can ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0323187]
- 74. Demographic clinical trial diversity assessment methods [https://www.sciencedirect.com/science/article/pii/S2451865425000067]
- 75. Biomarker discovery for non-invasive diagnosis of ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1570374/full]
- 76. Proteomics Biomarker Discovery: A Quantitative Workflow ... [https://www.metwarebio.com/proteomics-biomarker-discovery-workflow/]
- 77. Multi-omics Data Analysis FAQ [https://www.metwarebio.com/multi-omics-data-analysis-faq/]
- 78. The Future of Clinical Trials: Incorporating 'Omics for ... [https://blog.crownbio.com/the-future-of-clinical-trials-incorporating-omics-for-enhanced-stratification]
- 79. Ten quick tips for avoiding pitfalls in multi-omics data ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10325053/]
- 80. Integrated Multiomics Validation of Key MUC Gene ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12547622/]
- 81. Applications and challenges of biomarker-based predictive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12399543/]
- 82. Digital biomarkers and artificial intelligence: a new frontier ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1637159/full]
- 83. How AI & Biomarkers Are Reshaping the Next Frontier in ... [https://www.precisionformedicine.com/blog/how-ai-biomarkers-are-reshaping-the-next-frontier-in-drug-development]
- 84. Using AI for Data Analysis: The Ultimate Guide (2025) [https://indatalabs.com/blog/ai-for-data-analysis]
- 85. Using AI for Data Analysis: The Ultimate Guide (2025) [https://www.luzmo.com/blog/ai-data-analysis]
- 86. Drug Development Tool (DDT) Qualification Programs [https://www.fda.gov/drugs/development-approval-process-drugs/drug-development-tool-ddt-qualification-programs]
- 87. Qualification of novel methodologies for medicine development [https://www.ema.europa.eu/en/qualification-novel-methodologies-medicine-development]
- 88. Biomarker Qualification Program [https://www.fda.gov/drugs/drug-development-tool-ddt-qualification-programs/biomarker-qualification-program]
- 89. Biomarkers in Medicines Development—From Discovery to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9086587/]
- 90. AgencyIQ – Sluggish biomarker program offers FDA ... [https://friendsofcancerresearch.org/news/agencyiq-sluggish-biomarker-program-offers-fda-opportunity-for-reform/]
- 91. Resources for Biomarker Requestors [https://www.fda.gov/drugs/biomarker-qualification-program/resources-biomarker-requestors]
- 92. Biomarker Qualification at the European Medicines Agency [https://pmc.ncbi.nlm.nih.gov/articles/PMC9313861/]
- 93. FDA Guidance for Industry on Bioanalytical Method ... [https://labs.iqvia.com/blog/fda-guidance-bioanalytical-method-validation-biomarkers]
- 94. A Guide to Cross-Validation for Artificial Intelligence in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10388213/]
- 95. Delineating blood DNA methylation biomarkers for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12405053/]
- 96. A plasma proteomics-based candidate biomarker panel ... [https://www.nature.com/articles/s41591-025-03890-6]
- 97. Validation of Analytical Methods for Biomarkers Employed in Drug Development - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2744124/]
- 98. Cross-validation approaches for penalized Cox regression - PubMed [https://pubmed.ncbi.nlm.nih.gov/38445300/]
- 99. Q8, Q9, & Q10 Questions and Answers -- Appendix [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/q8-q9-q10-questions-and-answers-appendix-qas-training-sessions-q8-q9-q10-points-consider]
- 100. Frequently Asked Questions about Method Validation [https://www.ofnisystems.com/services/method-validation/frequently-asked-questions-about-method-validation/]
- 101. Comparative analysis of CRP and PCT as biomarkers for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12558828/]
- 102. Comparison of Serum Procalcitonin and C-reactive Protein ... [https://brieflands.com/journals/zjrms/articles/163585]
- 103. Clinical application of combined CRP and PCT detection in ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1563170/full]
- 104. Correlation between Erythrocyte Sedimentation Rate/CRP ... [https://pubmed.ncbi.nlm.nih.gov/40936171/]
- 105. erythrocyte sedimentation rate and C-reactive protein: it is ... [https://www.sciencedirect.com/science/article/abs/pii/S1198743X24004166]
- 106. Inflammation Biomarkers | Learn With Superpower [https://superpower.com/library/inflammation-biomarker-testing?srsltid=AfmBOoq8OR7gdPs5pnRxeWDAfcV6Y7KENocixmv8DvDLDHDxA3G6Poxr]
- 107. Decoding Biomarkers: A Comprehensive Guide to Testing ... [https://www.aiarthritis.org/decoding-biomarkers]
- 108. Examining the Use of Realâ€World Evidence in the Regulatory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7093234/]
- 109. FAQs on FDA Guidance for RWD and RWE in Drug ... [https://polygonhealthanalytics.com/faqs-about-the-fda-guidance-on-the-use-of-real-world-data-and-real-world-evidence-to-support-regulatory-decision-making-for-drug-and-biological-products/]
- 110. A Guide to Real-World Evidence in Clinical Trials [https://www.quanticate.com/blog/real-world-evidence-in-clinical-drug-development]
- 111. Early C-reactive protein reduction predicts survival in real ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1709336/full]
- 112. Real-World Evidence (RWE) | How It Impacts FDA Approval [https://www.crowleylawllc.com/rwe-fda-approval-drug-development/]
- 113. Advancing Real-World Evidence Program [https://www.fda.gov/drugs/development-resources/advancing-real-world-evidence-program-frequently-asked-questions]
- 114. Inflammatory Biomarkers in Heart Failure - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12592283/]
- 115. Special Issue : The Future of Inflammatory Biomarkers [https://www.mdpi.com/journal/jcm/special_issues/F2WY8D472F]
- 116. Inflammation Biomarkers | Learn With Superpower [https://superpower.com/library/inflammation-biomarker-testing?srsltid=AfmBOorLfzOwoFlqy5gabwBqQLlw3LqGoacGVVIAzhoXEqm5FxaRTuxY]
- 117. Alzheimer's disease drug development pipeline: 2025 - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12131090/]