BLI vs. MRI: A Comparative Guide for Neuroinflammatory Disease Monitoring in Preclinical Research
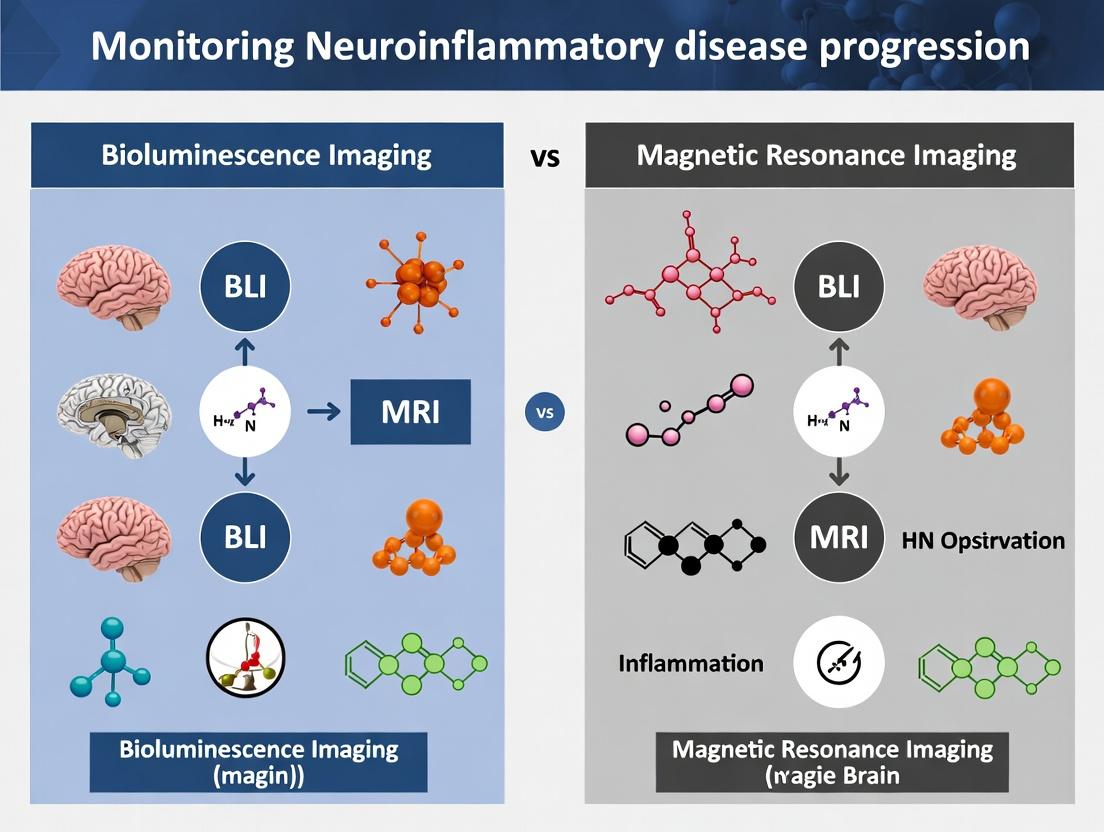
This article provides a comprehensive comparative analysis of Bioluminescence Imaging (BLI) and Magnetic Resonance Imaging (MRI) for monitoring neuroinflammatory disease progression in preclinical models.
BLI vs. MRI: A Comparative Guide for Neuroinflammatory Disease Monitoring in Preclinical Research
Abstract
This article provides a comprehensive comparative analysis of Bioluminescence Imaging (BLI) and Magnetic Resonance Imaging (MRI) for monitoring neuroinflammatory disease progression in preclinical models. Tailored for researchers, scientists, and drug development professionals, it explores the foundational principles, methodological applications, optimization strategies, and critical validation metrics of each modality. The scope encompasses understanding cellular vs. anatomical changes, practical workflows in rodent models, addressing technical limitations, and synthesizing quantitative data for robust study design. The goal is to equip readers with the knowledge to select and optimize the appropriate imaging strategy for their specific neuroinflammatory research questions.
BLI and MRI Decoded: Core Principles for Visualizing Neuroinflammation
Neuroinflammation is a complex, multicellular immune response within the central nervous system (CNS). It involves the activation of microglia and astrocytes, infiltration of peripheral immune cells, and the release of pro-inflammatory cytokines and chemokines. While a protective response to injury or infection, chronic or dysregulated neuroinflammation is a key pathological driver in numerous neurological diseases, including multiple sclerosis (MS), Alzheimer's disease (AD), and Parkinson's disease (PD). Precisely defining this "battlefield"—quantifying the location, extent, and activity of the inflammatory process—is critical for understanding disease mechanisms and evaluating therapeutic efficacy. This necessitates advanced in vivo imaging technologies that can non-invasively monitor disease progression in research models.
The Imaging Arsenal: BLI vs. MRI for Monitoring Neuroinflammation
For preclinical research, two primary imaging modalities are employed: Bioluminescence Imaging (BLI) and Magnetic Resonance Imaging (MRI). Each offers distinct advantages and limitations in the context of neuroinflammatory disease progression.
Performance Comparison: BLI vs. MRI
The following table summarizes the core comparative performance metrics of BLI and MRI in neuroinflammation research.
Table 1: Comparative Performance of BLI and MRI in Preclinical Neuroinflammation Research
| Feature | Bioluminescence Imaging (BLI) | Magnetic Resonance Imaging (MRI) |
|---|---|---|
| Sensitivity | Extremely High (pico-molar range). Can detect small numbers of cells. | Moderate to High. Requires a substantial volume of tissue change or contrast agent accumulation. |
| Spatial Resolution | Low (∼1-3 mm). Provides 2D planar data; 3D reconstruction is indirect. | Very High (∼50-100 µm). Provides true 3D anatomical data. |
| Depth Penetration | Limited. Significant signal scattering in tissue; best for superficial or brain-wide diffuse signals. | Excellent. Unaffected by tissue depth. |
| Quantification | Semi-quantitative. Signal intensity depends on substrate delivery, cell viability, and depth. | Highly Quantitative. Can derive volumetric, diffusion, or perfusion metrics. |
| Molecular Specificity | High with transgenic reporters (e.g., GFAP-luc, NF-κB-luc). Directly links signal to specific cellular/molecular events. | Low to Moderate. Requires exogenous contrast agents (e.g., Gadofluorine M, USPIOs) that infer activity. |
| Throughput & Cost | High Throughput, Low Cost per scan. Rapid imaging of multiple animals. | Low Throughput, High Cost. Lengthy scan times (minutes to hours per subject). |
| Key Application | Longitudinal tracking of specific cell populations (e.g., microglial activation), therapeutic response screening. | Anatomical lesion quantification (e.g., demyelination, atrophy), blood-brain barrier integrity assessment, and spatial mapping. |
Experimental Data & Protocols
Study 1: Tracking Microglial Activation in an AD Mouse Model using BLI
- Experimental Protocol: Transgenic APP/PS1 mice were crossbred with mice expressing a luciferase reporter gene under the control of a microglial-specific promoter (e.g., CX3CR1 or Iba1). At various age points (2, 4, 6, 8 months), mice were injected intraperitoneally with D-luciferin (150 mg/kg). After 10 minutes, bioluminescence was captured using a cooled CCD camera system. Signal was quantified as total photon flux (photons/sec) within a region of interest encompassing the skull.
- Supporting Data: BLI signal showed a significant increase (p<0.001) of 15-fold in 8-month-old AD mice compared to age-matched wild-type controls, correlating with histologically confirmed microgliosis.
Study 2: Quantifying Demyelinating Lesions in EAE using MRI
- Experimental Protocol: Mice with experimental autoimmune encephalomyelitis (EAE) were imaged at peak disease severity (day 18 post-induction) on a 7T MRI scanner. A T2-weighted rapid acquisition with relaxation enhancement (RARE) sequence was used to detect hyperintense lesions. A contrast agent (Gadolinium-DOTA, 0.2 mmol/kg) was administered intravenously, and T1-weighted images were acquired pre- and post-injection to assess BBB disruption.
- Supporting Data: MRI quantification revealed an average of 12 ± 3 T2 hyperintense lesions per brain in EAE mice, with a total lesion volume of 8.5 ± 1.2 mm³. 85% of these lesions exhibited gadolinium enhancement, indicating active inflammation with BBB breakdown.
Visualizing Pathways and Workflows
Title: Core Neuroinflammatory Signaling Cascade
Title: BLI vs MRI Experimental Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents and Materials for Neuroinflammation Imaging Studies
| Item | Function in Research |
|---|---|
| D-Luciferin, Potassium Salt | Substrate for firefly luciferase. Injected systemically in BLI studies to produce light from genetically engineered reporter cells (e.g., activated glia). |
| Gadolinium-Based Contrast Agents (e.g., Gd-DOTA) | MRI contrast agent that shortens T1 relaxation time. Used to visualize regions of blood-brain barrier disruption in diseases like EAE or stroke. |
| Ultra-Small Superparamagnetic Iron Oxide Particles (USPIOs) | MRI contrast agent detected on T2*/SWI sequences. Phagocytosed by infiltrating macrophages, allowing in vivo tracking of neuroinflammatory hotspots. |
| Transgenic Reporter Mice (e.g., CX3CR1-GFP; GFAP-luc) | Animal models where specific cell types (microglia, astrocytes) are genetically tagged with a fluorescent or bioluminescent protein for identification and tracking. |
| Myelin-Specific Stains (e.g., Luxol Fast Blue, MBP Antibodies) | Histological gold standard for validating MRI-observed demyelinating lesions. Provides ground truth data. |
| Ionized Calcium-Binding Adapter Molecule 1 (Iba1) Antibodies | Immunohistochemical marker for microglia/macrophages. Essential for quantifying microglial activation in tissue sections post-imaging. |
| 7T or 9.4T Preclinical MRI Scanner | High-field magnetic resonance imager providing the necessary resolution and contrast for detailed in vivo neuroanatomy in rodent models. |
| Cooled CCD Camera System | Highly sensitive optical imaging device required to detect the low-light bioluminescent signal from within the animal's brain. |
This guide is framed within a thesis comparing Bioluminescence Imaging (BLI) and Magnetic Resonance Imaging (MRI) for monitoring neuroinflammatory disease progression in preclinical research. BLI provides a sensitive, cost-effective method for tracking cellular and molecular processes in vivo through light emission.
Comparison: BLI vs. MRI for Neuroinflammatory Research
The table below objectively compares core performance metrics of BLI and MRI based on recent experimental studies in rodent models of neuroinflammation (e.g., EAE, TBI).
| Performance Metric | Bioluminescence Imaging (BLI) | Magnetic Resonance Imaging (MRI) |
|---|---|---|
| Sensitivity | Extremely high (can detect ~100-1000 cells). | Low to moderate; requires large cell numbers or substantial tissue change. |
| Spatial Resolution | Low (1-3 mm); poor for precise anatomical localization. | Very high (25-100 µm); excellent soft-tissue and anatomical detail. |
| Temporal Resolution | High (seconds to minutes per scan). | Low (minutes to hours per scan). |
| Depth Penetration | Limited (~1-2 cm); surface-weighted. | Excellent; whole-body, deep-tissue capability. |
| Quantification | Semi-quantitative; linear with cell number under controlled conditions. | Quantitative for volume/atrophy; semi-quantitative for contrast agents. |
| Throughput | Very high; allows rapid longitudinal imaging of many subjects. | Low to moderate; longer scan times limit cohort size. |
| Cost per Scan | Low (after initial reporter line/reagent investment). | Very high (equipment, maintenance, contrast agents). |
| Molecular Specificity | High (genetically encoded reporter for specific cell types/pathways). | Low to moderate (depends on contrast agent targeting efficiency). |
| Key Application in Neuroinflammation | Longitudinal tracking of infiltrating immune cells (e.g., T cells, microglia activation), gene expression dynamics. | Monitoring blood-brain barrier integrity, lesion load, brain atrophy, volumetric changes. |
Experimental Protocols for Key Comparisons
Protocol 1: Longitudinal Tracking of Adoptively Transferred Encephalitogenic T Cells in EAE
Aim: Compare BLI and MRI for monitoring T-cell migration to the CNS. BLI Method:
- Isolate T cells from donor mice.
- Transduce cells with a lentiviral vector encoding firefly luciferase (Fluc).
- Activate cells toward a myelin antigen (e.g., MOG35-55).
- Adoptively transfer 5 x 10^6 Fluc+ T cells into recipient mice via tail vein.
- Induce EAE.
- Imaging: At days 7, 14, and 21 post-transfer, inject D-luciferin substrate (150 mg/kg, i.p.). Anesthetize mice and acquire images using a cooled CCD camera system (e.g., IVIS Spectrum) 10-15 minutes post-injection. Regions of interest (ROIs) are drawn over the brain/spinal cord to quantify total flux (photons/sec).
MRI Method (Comparative Arm):
- At identical time points, anesthetize mice and image using a 7T or 9.4T MRI.
- Use T2-weighted sequences to quantify hyperintense lesion volume in the brain and spinal cord.
- Use T1-weighted sequences pre- and post-injection of a Gadolinium-based contrast agent (0.2 mmol/kg, i.v.) to assess BBB leakage.
Protocol 2: Monitoring Microglial Activation in a Neuroinflammatory Model
Aim: Assess BLI's ability to report on innate immune activation vs. MRI-based measurement of gliosis. BLI Method:
- Use transgenic reporter mouse where the luc2 gene is under the control of a microglial promoter (e.g., Cx3cr1 or Aif1 (Iba1)).
- Induce focal neuroinflammation via intracerebral LPS injection (2 µg in 1 µL).
- Imaging: At 24h, 48h, 72h, and 7d post-injection, administer D-luciferin and image as in Protocol 1. Quantify bioluminescent signal at the injection site.
MRI Method (Comparative Arm):
- Image mice at the same time points on a high-field MRI.
- Use diffusion tensor imaging (DTI) to derive fractional anisotropy (FA) and mean diffusivity (MD) maps as indirect indicators of gliosis and tissue integrity.
- Use specialized contrast agents (e.g., USPIOs targeting phagocytic activity) if available.
Visualizing Core BLI Pathways and Workflows
BLI Chemical Reaction Pathway
Standard In Vivo BLI Experimental Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function in BLI Experiment |
|---|---|
| D-Luciferin (Potassium Salt) | Cell-permeable substrate for firefly luciferase. Emits light upon oxidation. Standard dose: 150 mg/kg in PBS for i.p. injection. |
| Firefly Luciferase (Fluc) Reporter Genes | Genetic construct (pGL4, etc.) encoding the luciferase enzyme. Can be driven by cell-specific promoters (e.g., CD4 for T cells, GFAP for astrocytes). |
| Lentiviral/Retroviral Vectors | For efficient, stable integration of the luciferase reporter gene into target cells (primary immune cells, stem cells). |
| Transgenic Reporter Mice | Models with luciferase knocked into a specific locus (e.g., FVB-Tg(CAG-luc,-GFP)L2G85Chco/J for ubiquitous expression). |
| CCD Camera Imaging System | Cooled, sensitive camera system (e.g., PerkinElmer IVIS, Berthold NightOWL) housed in a light-tight chamber for signal detection. |
| Isoflurane/Oxygen Anesthesia System | For humane animal restraint during imaging sessions to prevent motion artifact. |
| Living Image or Similar Software | For image acquisition, region-of-interest (ROI) analysis, and quantification of radiant efficiency or total flux. |
| Matrigel | Used for co-injection with luciferase-labeled cells in ectopic tumor or cell survival studies to localize cells. |
| Coelenterazine | Substrate for marine luciferases (e.g., Renilla, Gaussia) used in dual-reporter assays or deep-tissue imaging. |
This comparison guide is framed within a broader thesis evaluating Bioluminescence Imaging (BLI) versus Magnetic Resonance Imaging (MRI) for monitoring neuroinflammatory disease progression in preclinical research. While BLI offers sensitivity and throughput for molecular events, MRI provides unparalleled, non-invasive spatial resolution for anatomical and pathological mapping. This guide objectively compares MRI’s performance against alternative modalities, focusing on its fundamental role in structural and pathological assessment.
Performance Comparison: MRI vs. Alternative Imaging Modalities
Table 1: Quantitative Comparison of Key Imaging Modalities for Neuroinflammatory Research
| Parameter | High-Field MRI (e.g., 7T-11.7T) | Bioluminescence Imaging (BLI) | Micro-CT | Positron Emission Tomography (PET) |
|---|---|---|---|---|
| Spatial Resolution | 25-100 µm isotropic | 3-5 mm (superficial) | 10-50 µm | 1-2 mm |
| Tissue Penetration | Unlimited depth | Limited (few cm, surface-weighted) | Unlimited depth | Unlimited depth |
| Primary Contrast | Soft tissue anatomy (T1/T2), water diffusion (DWI), iron deposits (T2*), perfusion | Luciferase enzyme activity (reporter gene) | Bone/ tissue density | Radioligand concentration (metabolism, receptors) |
| Quantitative Output | Lesion volume (mm³), atrophy measures, relaxation times (ms), fractional anisotropy | Photon flux (p/s/cm²/sr) | Mineral density (mg/cc), volume | Standardized Uptake Value (SUV) |
| Temporal Resolution (Acquisition) | Minutes to hours | Seconds to minutes | Minutes | Minutes |
| Longitudinal Monitoring | Excellent (non-invasive, no ionizing radiation) | Excellent (non-invasive, low cost) | Limited (ionizing radiation dose) | Limited (radioligand decay/dose) |
| Key Strength for Neuroinflammation | Volumetric lesion tracking, blood-brain barrier integrity (contrast-enhanced), demyelination (qMT) | High-throughput screening of therapeutic efficacy in transgenic models | Skull/bone lesion analysis, co-registration with MRI | Specific molecular target engagement (e.g., TSPO) |
Experimental Protocols for Key MRI Applications
Protocol 1: T2-Weighted Imaging for Lesion Volumetry in Experimental Autoimmune Encephalomyelitis (EAE)
Objective: To quantify hyperintense lesion burden, a hallmark of neuroinflammation and demyelination in the EAE mouse model.
- Animal Preparation: Anesthetize mouse (e.g., isoflurane 1-2% in O₂). Secure in MRI-compatible stereotaxic bed with respiratory monitoring.
- Scanner: 7T or higher preclinical MRI system.
- Sequence: Fast Spin Echo (FSE) or Rapid Acquisition with Relaxation Enhancement (RARE) T2-weighted sequence.
- Parameters (Typical 9.4T): TR = 4200 ms, TEeff = 36 ms, RARE factor = 8, FOV = 20x20 mm², matrix = 256x256, slices = 30, slice thickness = 0.5 mm, averages = 4. Total scan time ~30 minutes.
- Analysis: Import DICOM files to analysis software (e.g., Horos, FSL, SPM). Manually or semi-automatically segment hyperintense areas in brain or spinal cord. Calculate total lesion volume (mm³) per subject.
Protocol 2: Diffusion Tensor Imaging (DTI) for White Matter Integrity
Objective: To assess axonal damage and demyelination via fractional anisotropy (FA) and mean diffusivity (MD).
- Animal/Scanner Setup: As in Protocol 1.
- Sequence: Echo-planar imaging (EPI) based DTI sequence.
- Parameters: TR = 6000 ms, TE = 30 ms, δ/Δ (diffusion pulse parameters) = 5/15 ms, b-value = 1000 s/mm², directions = 30, non-diffusion weighted (b=0) images = 5. Spatial parameters as in Protocol 1. Scan time ~1.5 hours.
- Analysis: Process data with DTI toolkit (e.g., DTIFIT in FSL). Generate FA and MD maps. Register to an atlas and extract ROI-based metrics (e.g., corpus callosum FA value).
The Scientist's Toolkit: Research Reagent & Material Solutions
Table 2: Essential Materials for Preclinical Neuroinflammation MRI Studies
| Item | Function & Relevance |
|---|---|
| Preclinical High-Field MRI System (7T-11.7T) | Provides the high signal-to-noise ratio necessary for microscopic resolution in rodent brains. |
| MRI-Compatible Anesthesia System | Maintains stable physiology during long scans (e.g., isoflurane vaporizer with MRI-safe tubing). |
| Dedicated Radiofrequency Coils | Surface coils for spinal cord imaging; volume coils for whole-brain coverage. Critical for image quality. |
| Stereotaxic Animal Bed w/ Heating | Ensures precise, reproducible positioning and maintains body temperature for physiological stability. |
| Paramagnetic Contrast Agents (e.g., Gd-DTPA) | Small molecular weight agents used in T1-weighted imaging to detect blood-brain barrier disruption. |
| Automated Perfusion/Fixation System | For ex vivo high-resolution MRI, allowing perfect fixation and removal of confounding physiological motion. |
| Atlas Registration Software (e.g., ANTs, SPM) | Enables voxel-based or ROI-based quantitative comparison across experimental cohorts. |
| Phantom Calibration Kits | For validating scanner performance and ensuring quantitative consistency across longitudinal studies. |
Visualizing MRI's Role in a Multi-Modal Research Workflow
Diagram 1: BLI vs MRI Integrated Research Workflow
Diagram 2: MRI Signal to Anatomical Map Process
Within the thesis context of BLI vs MRI for neuroinflammatory disease research, MRI fundamentals establish it as the indispensable modality for definitive, three-dimensional mapping of anatomy and pathology. While BLI excels in rapid, cost-effective longitudinal screening of disease activity, MRI provides the critical ground-truth spatial data on lesion location, volume, and tissue characteristics. The integration of quantitative MRI protocols, as detailed, offers researchers robust, objective metrics for evaluating disease progression and therapeutic efficacy, complementing molecular insights from BLI and other modalities.
This comparison guide is framed within a thesis investigating the relative merits of Bioluminescence Imaging (BLI) and Magnetic Resonance Imaging (MRI) for monitoring neuroinflammatory disease progression. The efficacy of both modalities hinges on their ability to detect and quantify key biological targets, most notably immune cell infiltration and blood-brain barrier (BBB) disruption. This guide objectively compares the performance of BLI and MRI in measuring these targets, supported by experimental data.
Performance Comparison: BLI vs. MRI for Key Neuroinflammatory Targets
Table 1: Direct Comparison of BLI and MRI for Monitoring Neuroinflammatory Targets
| Biological Target | BLI (Typical Approach) | MRI (Typical Approach) | Key Performance Metrics | Temporal Resolution | Spatial Resolution | Depth Penetration | Quantification Method |
|---|---|---|---|---|---|---|---|
| Immune Cell Infiltration | Reporter genes (e.g., luciferase) in specific immune cell populations. | Iron oxide nanoparticles (e.g., USPIO) for cell tracking; Contrast-enhanced T1 for leakage. | Sensitivity: Extremely high (can detect ~100 cells). Specificity: High with genetically engineered cells. | Minutes to hours | Low (1-3 mm) | Limited (surface-weighted) | Total photon flux (p/s/cm²/sr) |
| Sensitivity: Moderate (micromolar iron). Specificity: Lower (non-specific phagocytosis). | Hours to days | High (50-100 µm) | Unlimited (whole body/brain) | Signal void on T2*/SWI; T1 signal intensity change | |||
| BBB Disruption | Extravasation of luminogenic substrates (e.g., D-luciferin) or reporter expression in parenchyma. | Dynamic Contrast-Enhanced (DCE) MRI with Gadolinium-based contrast agents (GBCA). | Sensitivity: Moderate. Specificity: Low (confounded by perfusion). | Minutes | Low | Limited | Parenchymal signal over time |
| Sensitivity: High (µM Gd). Specificity: High for vascular permeability. | Minutes (per dynamic scan) | High | Unlimited | Pharmacokinetic modeling (Ktrans, ve) |
Table 2: Supporting Experimental Data from Representative Studies
| Study Focus | Imaging Modality | Experimental Model | Key Quantitative Result | Correlation with Histology |
|---|---|---|---|---|
| T-cell Trafficking to CNS | BLI (firefly luciferase) | Experimental Autoimmune Encephalomyelitis (EAE) mice | Peak luminescence signal (5 x 10⁸ p/s/cm²/sr) correlated with clinical score of 3. | R² = 0.89 with CD3+ T-cell counts in spinal cord. |
| Myeloid Cell Tracking | MRI (Ferumoxytol USPIO) | Stroke (MCAO) model in rats | Signal decrease of 35% in ipsilateral hemisphere on T2*-weighted images at 24h post-injection. | R² = 0.78 with Perls' Prussian blue-positive area. |
| BBB Permeability | BLI (systemic D-luciferin) | Glioblastoma xenograft model | 2.5-fold increase in brain background signal in tumor-bearing vs. control mice. | Moderate correlation (R² = 0.65) with IgG extravasation. |
| BBB Permeability | MRI (DCE-MRI, Gd-DTPA) | Multiple Sclerosis (Cuprizone) model | Mean Ktrans value in corpus callosum increased from 0.001 min⁻¹ (control) to 0.015 min⁻¹ (demyelinated). | Strong correlation (R² = 0.92) with Evan's Blue extravasation quantitation. |
Experimental Protocols
Protocol 1: BLI for Longitudinal Immune Cell Tracking
- Cell Engineering: Isolate target immune cells (e.g., T-cells). Transduce with a lentiviral vector encoding firefly luciferase (Fluc) and a fluorescent marker (e.g., GFP).
- Adoptive Transfer: Inject 1-5 x 10⁶ engineered cells intravenously into disease model mice.
- Imaging: At defined time points, inject mice intraperitoneally with D-luciferin substrate (150 mg/kg). After 10 minutes, acquire images using a cooled CCD camera system with 1-5 minute exposure times.
- Quantification: Define regions of interest (ROIs) over the CNS and major organs. Calculate total flux (photons per second) within each ROI after background subtraction.
Protocol 2: DCE-MRI for Quantifying BBB Disruption
- Animal Preparation: Anesthetize and place animal in MRI-compatible holder. Maintain body temperature.
- Baseline Scans: Acquire high-resolution anatomical scans (e.g., T2-weighted). For pre-contrast T1 mapping, use a variable flip angle (e.g., 5°, 15°, 30°) GRE sequence.
- Dynamic Series: Administer Gd-based contrast agent (0.1-0.2 mmol/kg) via tail vein catheter as a bolus. Simultaneously, initiate a rapid T1-weighted sequence (e.g., 3D SPGR or fast GRE) repeated for 20-30 minutes.
- Analysis: Convert signal intensity-time curves to contrast concentration-time curves. Fit data to a pharmacokinetic model (e.g., Patlak, Tofts) using dedicated software to generate parametric maps of Ktrans (transfer constant) and ve (extravascular extracellular space).
Visualizations
Title: BLI Workflow for Immune Cell Tracking
Title: Neuroinflammatory Cascade: Infiltration to BBB Disruption
Title: Decision Logic: Selecting BLI or MRI for Neuroinflammatory Targets
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Neuroinflammatory Imaging
| Item | Function/Application | Example Product/Category |
|---|---|---|
| Reporter Lentivirus (Fluc/GFP) | Genetically labels specific immune cell populations for BLI tracking and post-mortem FACS validation. | Lenti-Fluc-GFP (commercial or custom); pCDH-EF1-Fluc-T2A-GFP vector. |
| D-Luciferin, Potassium Salt | Substrate for firefly luciferase, administered to generate bioluminescent signal for BLI. | Sterile-filtered, in vivo grade, reconstituted in PBS. |
| Ultra-small Superparamagnetic Iron Oxide (USPIO) | MRI contrast agent taken up by phagocytic immune cells (e.g., macrophages) for cellular MRI. | Ferumoxytol; Molday ION Rhodamine-B (for multimodal imaging). |
| Gadolinium-Based Contrast Agent (GBCA) | T1-shortening agent for contrast-enhanced MRI and DCE-MRI pharmacokinetic modeling of BBB permeability. | Gadoteridol; Gadobutrol; Gd-DTPA. |
| Anti-CD3 / Anti-Iba1 Antibodies | Gold-standard immunohistochemistry reagents for validating immune cell infiltration (T-cells, microglia/macrophages). | Clone 17A2 (CD3); Polyclonal (Iba1). |
| Evan's Blue Dye (2% w/v) | Classic ex vivo fluorescence-based method for qualitative and quantitative assessment of BBB leakage. | Requires rigorous filtration; used as a terminal procedure. |
| IVIS Spectrum/IVIS Lumina | In vivo imaging system with cooled CCD camera and gas anesthesia for longitudinal BLI studies. | PerkinElmer IVIS series. |
| High-Field Small Animal MRI | Preclinical MRI system (typically 7T-11.7T) equipped with high-performance gradients for DCE and anatomical imaging. | Bruker BioSpec; Agilent/Varian systems. |
| Pharmacokinetic Modeling Software | Converts DCE-MRI signal intensity curves into quantitative parametric maps (Ktrans, ve). | MITK (open-source); PMI; NordicICE. |
In the study of neuroinflammatory disease progression, the choice between in vivo imaging modalities—Bioluminescence Imaging (BLI) and Magnetic Resonance Imaging (MRI)—is fundamentally tied to the biological model system. BLI typically requires genetic engineering to introduce a reporter, while MRI often relies on anatomical or contrast-agent-based readouts in wild-type or disease-model organisms. This guide objectively compares these parallel approaches.
Core Technology Comparison
| Feature | Transgenic Reporter Models for BLI | Anatomical/Pathology Models for MRI |
|---|---|---|
| Primary Readout | Photon emission from luciferase enzyme (e.g., firefly, Gaussia). | Proton density, T1/T2 relaxation times, contrast agent accumulation. |
| Sensitivity | Extremely high (picomolar to femtomolar reporter concentrations). | Low to moderate (millimolar contrast agent concentrations required). |
| Spatial Resolution | Low (∼1-3 mm), surface-weighted, limited depth penetration. | High (∼25-100 µm), full 3D tomographic reconstruction. |
| Quantification | Semi-quantitative (photons/sec/cm²/sr); can be confounded by tissue attenuation. | Quantitative parameters possible (e.g., lesion volume in mm³, T2 relaxation time in ms). |
| Throughput & Cost | High throughput, low cost per scan, rapid acquisition (seconds-minutes). | Low throughput, high cost per scan, long acquisition times (minutes-hours). |
| Key Reporter/Marker | Transgenic expression of luciferase under cell-specific promoter (e.g., GFAP-luc for astrocytes). | Endogenous anatomy (e.g., ventricular volume), or injected agents (e.g., Gadofluorine M, USPIO). |
| Example Experimental Data (EAE Model) | Peak signal: 1.2e7 ± 2.1e6 p/s/cm²/sr on day 15 post-induction. | Total T2-hyperintense lesion volume: 8.5 ± 1.2 mm³ on day 15 post-induction. |
| Invasiveness | Non-invasive, but requires substrate injection (D-luciferin). | Non-invasive, may require intravenous contrast agent. |
Supporting Experimental Data & Protocols
Experiment 1: Longitudinal Monitoring of Astrocyte Activation in EAE Mice
- Objective: Compare temporal dynamics of neuroinflammation using BLI transgenic reporters vs. T2-weighted MRI.
- BLI Protocol:
- Model: C57BL/6-Tg(GFAP-luc) mice induced with Experimental Autoimmune Encephalomyelitis (EAE).
- Imaging: Inject D-luciferin (150 mg/kg, i.p.). Acquire images 12 minutes post-injection using a cooled CCD camera system (binning 4, f/stop 1, 5-minute exposure).
- Analysis: Draw regions of interest (ROIs) over the brain and calculate total flux (photons/sec).
- MRI Protocol:
- Model: Wild-type C57BL/6 mice induced with EAE.
- Imaging: Acquire T2-weighted RARE sequences on a 7T scanner (TR=4000 ms, TE=36 ms, slice thickness=0.5 mm, matrix=256x256).
- Analysis: Manually segment hyperintense areas in the cerebellum and brainstem to calculate total lesion volume.
- Result Summary Table:
| Day Post-Induction | BLI Signal (x10^6 p/s) | MRI Lesion Volume (mm³) |
|---|---|---|
| 7 (Pre-clinical) | 3.2 ± 0.8 | 0.5 ± 0.2 |
| 15 (Peak) | 12.1 ± 2.1 | 8.5 ± 1.2 |
| 30 (Chronic) | 6.5 ± 1.4 | 5.2 ± 0.9 |
Experiment 2: Cellular Infiltration Tracking
- Objective: Visualize myeloid cell recruitment.
- BLI Approach: Use transgenic CX3CR1-luc mice or transplant luciferase+ bone marrow. Signal provides whole-body trafficking data.
- MRI Approach: Inject ultra-small superparamagnetic iron oxide (USPIO) particles, which are phagocytosed by infiltrating monocytes/macrophages, causing T2* signal voids.
- Comparative Data Table:
| Parameter | BLI (CX3CR1-luc+) | MRI (USPIO-enhanced) |
|---|---|---|
| Time to Detect CNS Signal Post-Induction | Day 5 | Day 8 |
| Spatial Localization Precision | Poor (lumbar spine vs. brain) | Excellent (distinct brain regions) |
| Signal-to-Noise Ratio Change at Peak | 15-fold increase over baseline | 40% decrease in T2* signal (hypointensity) |
Visualized Workflows and Pathways
BLI Reporter Mouse Workflow
Anatomical MRI Imaging Workflow
BLI Reporter Gene Pathway
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function in BLI | Function in MRI |
|---|---|---|
| D-Luciferin (Potassium Salt) | Cell-permeable substrate for firefly luciferase. Converts photon emission. | N/A |
| Genetic Reporter Constructs (e.g., pGL4.1[GFAP-luc2]) | For creating stable transgenic lines or lentiviral transduction. | N/A |
| Gadofluorine M | N/A | Gadolinium-based contrast agent that binds to extracellular matrix in lesions, enhancing T1 signal. |
| Ultra-Small Superparamagnetic Iron Oxides (USPIO) | N/A | Particles phagocytosed by infiltrating macrophages, creating local magnetic field inhomogeneities (T2* effect). |
| Isoflurane/Oxygen Mix | Anesthesia for in vivo imaging session. | Anesthesia for prolonged MRI scanning; often combined with warming apparatus. |
| Phosphate-Buffered Saline (PBS) | Vehicle for dissolving D-luciferin. | Vehicle for diluting contrast agents or as a control injection. |
| Matrigel | For slow-release D-luciferin formulations in some protocols. | N/A |
| Stereotaxic Injector | For precise intracranial delivery of luciferase-expressing cells or vectors. | For precise induction of focal lesions (e.g., with LPS, lysolecithin). |
From Setup to Data: Implementing BLI and MRI in Neuroinflammatory Studies
Within the broader thesis comparing Bioluminescence Imaging (BLI) and Magnetic Resonance Imaging (MRI) for monitoring neuroinflammatory disease progression, BLI offers a high-throughput, sensitive, and cost-effective method for longitudinal tracking of cellular and molecular events. This guide compares the performance of a representative sensitive In Vivo Imaging System (IVIS) platform against common alternative modalities, focusing on the workflow for neuroinflammatory research using luciferase-expressing models.
Core BLI Workflow & Comparison Data
The fundamental BLI workflow involves: 1) Engineering a luciferase reporter (e.g., Luc2) into cells or animal models, 2) Systemic administration of substrate (D-luciferin), 3) Signal acquisition via a cooled CCD camera, and 4) Quantitative data analysis.
Table 1: Performance Comparison: BLI vs. MRI vs. Fluorescence Imaging
| Parameter | High-Sensitivity BLI (IVIS Spectrum) | MRI (7T Preclinical) | Fluorescence Imaging (e.g., GFP/RFP) |
|---|---|---|---|
| Sensitivity | High (10² - 10³ cells) | Low (millimolar contrast agents) | Moderate (background autofluorescence) |
| Temporal Resolution | Seconds to minutes | Minutes to hours | Seconds |
| Spatial Resolution | Low (1-3 mm) | High (50-100 µm) | Low (2-5 mm, surface weighted) |
| Depth Penetration | Excellent (several cm) | Excellent (unlimited) | Poor (<1 cm) |
| Quantification | Highly quantitative (photons/sec) | Semi-quantitative | Semi-quantitative |
| Throughput | High (multiple animals/session) | Low | High |
| Cost per Scan | Low | Very High | Low |
| Key Advantage for Neuroinflammation | Longitudinal tracking of microglial activation & infiltrating immune cells | Anatomic detail & blood-brain barrier integrity | Multi-color cellular interactions |
Experimental Data Summary: A direct comparison study tracking neuroinflammation in an EAE (Experimental Autoimmune Encephalomyelitis) mouse model showed BLI (using luciferase-expressing T cells) could detect initial CNS infiltration at day 7 post-induction, while MRI detected first hyperintense lesions at day 10. BLI signal (total flux, p/s) increased exponentially from day 7 (3.2 x 10⁵ ± 0.8 x 10⁵) to peak at day 14 (1.8 x 10⁷ ± 0.4 x 10⁷), correlating with clinical score (r²=0.89). MRI lesion volume became quantifiable only after day 10.
Detailed Experimental Protocols
Protocol 1: In Vivo BLI of Neuroinflammatory Infiltration
- Model: C57BL/6 mice with adoptively transferred luciferase-expressing MOG-reactive T cells.
- Substrate: D-luciferin (150 mg/kg in PBS), injected intraperitoneally.
- Anesthesia: Induced and maintained with 2-3% isoflurane.
- Image Acquisition: Using an IVIS SpectrumCT system. 10 minutes post-luciferin injection, acquire a sequence of 1-minute exposures until peak signal is identified. Use Living Image software for quantification. Draw uniform regions of interest (ROIs) over the brain/spinal cord and quantify as Total Flux (photons/second).
- Controls: Naive mice injected with luciferin; EAE mice without luciferase+ cells.
Protocol 2: Longitudinal Correlative BLI-MRI Study
- Days 7, 10, 14 post-induction: Perform BLI as per Protocol 1.
- Within 2 hours of BLI: Perform MRI on a 7T scanner using a T2-weighted rapid acquisition with relaxation enhancement (RARE) sequence. Acquire coronal slices of the brain.
- Analysis: Coregister BLI signal hotspot with MRI hyperintense lesions. Plot BLI total flux vs. MRI lesion volume over time.
Visualizing the BLI Workflow and Signaling
Title: BLI Workflow from Model to Quantified Data
Title: BLI and MRI Comparative Strengths in Neuroinflammation
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for BLI Neuroinflammation Workflow
| Item | Function & Rationale |
|---|---|
| Luciferase Reporter Vector (e.g., pGL4.50[luc2/CMV/Hygro]) | Source of the luc2 gene for stable cell line generation or creation of transgenic models. luc2 is optimized for mammalian expression and offers bright, sustained signal. |
| D-Luciferin, Potassium Salt (Xenogen) | The enzyme substrate for firefly luciferase. Potassium salt offers high solubility and consistent kinetics for in vivo studies. Must be prepared fresh or aliquoted. |
| Matrigel Matrix | Used for stabilizing engraftment of luciferase-expressing cells in specific locations (e.g., for brain tumor models of inflammation). |
| Isoflurane Anesthesia System | Provides safe, maintainable anesthesia during image acquisition, crucial for minimizing animal stress and motion artifact. |
| Black Hair Removal Cream | Non-invasive method to remove fur from imaging areas, reducing signal attenuation and scattering, improving quantitation. |
| Living Image Software (PerkinElmer) | Industry-standard for BLI data acquisition, analysis, and 3D reconstruction. Enables ROI quantification, kinetic analysis, and data overlay with photographic images. |
| Luciferase Assay System (for validation) | Used in vitro to validate luciferase activity in transfected/transduced cells prior to in vivo use, ensuring model fidelity. |
| Bioluminescent Microsphere Standards | Embedded calibration standards for some imagers, allowing for system performance validation and cross-day normalization. |
Within the broader research thesis comparing Bioluminescence Imaging (BLI) and MRI for monitoring neuroinflammatory disease progression, MRI protocol design is critical for non-invasive, longitudinal assessment. BLI, while offering high sensitivity and low cost in preclinical models, is limited by depth penetration and lacks detailed anatomical context. MRI provides whole-brain, high-resolution structural and pathophysiological data but requires optimized sequences to detect specific hallmarks of inflammation, such as edema, cellular infiltration, and changes in macromolecular composition. This guide compares three key MRI sequences—T2-weighted, Diffusion Tensor Imaging (DTI), and Chemical Exchange Saturation Transfer (CEST)—for detecting inflammation, supported by experimental data.
Comparative Sequence Analysis
The following table summarizes the core mechanisms, measurable parameters, strengths, and limitations of each sequence in the context of neuroinflammation.
Table 1: Comparison of MRI Sequences for Detecting Neuroinflammation
| Sequence | Primary Contrast Mechanism | Key Quantitative Metrics for Inflammation | Typical Experimental Findings in Neuroinflammation | Key Advantages | Major Limitations |
|---|---|---|---|---|---|
| T2-Weighted (T2w) / T2 Mapping | Transverse relaxation time of free water. Increased water content (edema) lengthens T2. | T2 Relaxation Time (ms), Lesion Volume (mm³) | Elevated T2 in lesion areas indicates vasogenic edema and inflammation. | Widely available, fast, excellent for detecting overt edema. High spatial resolution. Strong anatomical correlation. | Low specificity. Cannot differentiate inflammation from other causes of edema (e.g., ischemia, tumor). Insensitive to cellular/microstructural changes. |
| Diffusion Tensor Imaging (DTI) | Directionality and magnitude of water molecule diffusion. Inflammation disrupts tissue microstructure. | Fractional Anisotropy (FA), Mean Diffusivity (MD), Axial/Radial Diffusivity (AD/RD) | ↓ FA, ↑ MD/RD in white matter lesions indicates axonal damage, demyelination, and inflammatory infiltration. | Sensitive to microstructural integrity. Can differentiate axonal injury (↓ AD) vs. demyelination (↑ RD). | Confounded by crossing fibers, edema. Results are non-specific; similar changes occur in neurodegeneration. Moderate spatial resolution. |
| Chemical Exchange Saturation Transfer (CEST) | Transfer of saturated magnetization from exchangeable protons (e.g., -OH, -NH) to bulk water. | Magnetization Transfer Ratio asymmetry (MTRasym), Specific CEST signals (e.g., amide, amine, APT) | ↑ Amide Proton Transfer (APT) signal correlates with increased cellularity/protein content in inflammatory lesions. | Molecular-level specificity. Can probe metabolites (proteins, peptides, pH) associated with inflammation. | Technically challenging. Low signal-to-noise ratio (SNR). Susceptible to B₀/B₁ inhomogeneity. Long scan times. |
Supporting Experimental Data Summary:
Table 2: Representative Quantitative Data from Preclinical EAE Studies
| Study Model | T2 Mapping (Lesion T2 vs. Control) | DTI (Lesion FA/MD vs. Control) | CEST (APT-weighted Signal vs. Control) | Key Insight |
|---|---|---|---|---|
| Murine EAE (Acute) | +40-60% increase in T2 | FA: -30%; MD: +50% | MTRasym at 3.5ppm: +2-3% | T2/DTI show lesion location; CEST suggests active protein accumulation. |
| Rat EAE (Chronic) | +20-30% in chronic lesions | FA: -50% (persistent); MD: Normalizes | MTRasym: Normalizes in chronic silent lesions | DTI FA remains sensitive to permanent damage; CEST may differentiate active/inactive lesions. |
Detailed Experimental Protocols
T2 Mapping Protocol for Lesion Volumetry
- Animal/Subject Preparation: Anesthesia induction and maintenance (e.g., isoflurane), physiological monitoring (respiration, temperature).
- MRI Hardware: Preclinical 7T or clinical 3T scanner, appropriate RF coils.
- Pulse Sequence: Multi-slice, multi-echo spin-echo (MESE) or Rapid Acquisition with Relaxation Enhancement (RARE) variant.
- Key Parameters (Example - 7T preclinical): TR = 4000ms, TE array = [10, 20, 30, 40, 50, 60, 70, 80]ms, Matrix = 256x256, Slices = 30, Slice thickness = 0.5mm.
- Data Analysis: Pixel-wise fitting of TE signal decay to mono-exponential model:
S(TE) = S0 * exp(-TE/T2). Lesion masks are created by thresholding T2 maps (e.g., > mean + 2SD of contralateral normal-appearing tissue) and total lesion volume is calculated.
DTI Protocol for Microstructural Assessment
- Pulse Sequence: Echo-planar imaging (EPI) based diffusion-weighted sequence.
- Key Parameters (Example - 3T clinical): TR = 8000ms, TE = 100ms, b-values = 0, 1000 s/mm², Diffusion directions = 30 isotropically distributed directions, Matrix = 128x128, Slice thickness = 2mm.
- Data Analysis: Preprocessing includes eddy-current and motion correction. Tensors are fitted per voxel using linear least squares to derive FA, MD, AD, and RD maps. Regions of interest (ROIs) are drawn on co-registered T2w images and overlaid on DTI parameter maps for statistical comparison.
CEST Protocol for Molecular Contrast
- Pulse Sequence: Fast imaging sequence (e.g., RARE, GRE) preceded by a long, spectrally selective saturation pulse.
- Key Parameters (Example - 7T preclinical): TR = 5000ms, TE = 4ms, Saturation power = 2 µT, Saturation duration = 3s. A Z-spectrum is acquired by sweeping the saturation pulse offset from -5 to +5 ppm (e.g., 41 offsets).
- Data Analysis: Z-spectrum is interpolated and normalized. MTRasym is calculated:
MTR_asym(Δω) = S_sat(-Δω)/S0 - S_sat(+Δω)/S0. The APT-weighted contrast is derived from MTRasym at 3.5ppm. B₀ correction is mandatory (using WASSR or similar method).
Visualizing the MRI Protocol Decision Pathway
Diagram Title: MRI Sequence Selection Pathway for Neuroinflammation
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Preclinical Neuroinflammation MRI Studies
| Item | Function in Research | Example Product/Catalog |
|---|---|---|
| Induction Reagents | To establish a controlled neuroinflammatory disease model for MRI/BLI comparison. | Hooke Kit MOG35-55/CFA Emulsion (EK-2110) & Pertussis Toxin (PTX-191) |
| BLI Substrate | Enables in vivo bioluminescence imaging to validate early inflammatory events and cell trafficking. | D-Luciferin, Potassium Salt (122799) |
| MRI Contrast Agent | Enhances detection of blood-brain barrier leakage, a key inflammatory feature. | Gadoteridol (ProHance) or preclinical Gadofluorine M |
| Anesthesia System | Maintains stable physiology during lengthy MRI scans for reproducible data. | Isoflurane Vaporizer with Nose Cone & Warming Pad |
| Physiological Monitor | Monitors respiration and temperature to ensure animal welfare and data quality. | Small Animal Monitoring System (SA Instruments) |
| Image Analysis Software | Processes MRI data (co-registration, segmentation, parameter mapping) for quantitative outcomes. | SPM, FSL, or commercial packages (e.g., PMOD, AnalyzeDirect). |
Within neuroinflammatory disease research, such as multiple sclerosis (MS) and experimental autoimmune encephalomyelitis (EAE), longitudinal monitoring is critical for assessing therapeutic efficacy and understanding pathogenesis. Two predominant imaging modalities—Bioluminescence Imaging (BLI) and Magnetic Resonance Imaging (MRI)—offer complementary strategies for tracking disease progression over time. This guide objectively compares their performance in a research context.
Core Comparison: BLI vs. MRI for Neuroinflammation
Table 1: Modality Performance Comparison
| Feature | Bioluminescence Imaging (BLI) | Magnetic Resonance Imaging (MRI) |
|---|---|---|
| Primary Readout | Intensity of emitted light (photons/sec/cm²/steradian) | Anatomical detail & soft tissue contrast (e.g., T2 lesion volume in mm³) |
| Resolution | Low (≈3-5 mm); superficial sensitivity | High (sub-millimeter to 100 µm for preclinical) |
| Penetration Depth | Limited (<2 cm); best for superficial tissues | Excellent, whole-body |
| Quantification | Semi-quantitative; relative cell number/biomarker activity | Quantitative volumetric/relaxometry analysis |
| Temporal Resolution | High (minutes), ideal for frequent time-points | Moderate to low (minutes to hours per scan) |
| Throughput | High, can screen multiple animals rapidly | Lower, longer acquisition times |
| Key Applications | Tracking infiltrating luciferase+ immune cells, gene expression dynamics | Lesion load, brain atrophy, blood-brain barrier integrity (with contrast) |
| Cost & Accessibility | Lower upfront cost, widely available in preclinical labs | High capital and operational cost |
Table 2: Representative Experimental Data from EAE Monitoring Studies
| Modality | Measured Parameter | Control Group (Mean ± SD) | Treated Group (Mean ± SD) | P-value | Study Insight |
|---|---|---|---|---|---|
| BLI | Peak Signal (Day 15 p.i.) | 8.7 x 10⁵ ± 1.2 x 10⁵ p/s/cm²/sr | 3.1 x 10⁵ ± 0.9 x 10⁵ p/s/cm²/sr | <0.001 | Treatment reduced immune cell CNS infiltration. |
| MRI (T2-weighted) | Total Lesion Volume (Day 21 p.i.) | 12.5 ± 2.1 mm³ | 5.2 ± 1.7 mm³ | <0.01 | Treatment significantly decreased demyelinating lesion burden. |
| MRI (Contrast-Enhanced) | Number of Gd+ Lesions | 4.8 ± 1.3 | 1.2 ± 0.8 | <0.001 | Treatment reduced acute blood-brain barrier disruption. |
Detailed Experimental Protocols
Protocol 1: BLI for Monitoring Neuroinflammatory Cell Trafficking
- Animal Model: Transgenic mice expressing luciferase under a pan-hematopoietic promoter (e.g., Rosa26-luc) induced with EAE.
- Substrate Administration: Inject D-luciferin intraperitoneally (150 mg/kg in PBS) 10-15 minutes prior to imaging.
- Imaging Setup: Anesthetize animal (isoflurane), place in light-tight chamber of an in vivo imaging system (IVIS).
- Image Acquisition: Acquire a series of images (1-5 minute exposures) until peak signal is identified. Use low binning for maximum resolution.
- Quantification: Define regions of interest (ROI) over the brain/spinal cord. Analyze using Living Image or equivalent software. Data expressed as total flux (photons/sec).
Protocol 2: MRI for Quantifying CNS Lesion Load
- Animal Preparation: Anesthetize (isoflurane/medical air), secure in MRI-compatible holder with respiratory monitoring.
- Scanner: Use a high-field preclinical system (e.g., 7T or 9.4T).
- Pulse Sequences:
- T2-weighted RARE: For hyperintense lesion detection. Parameters: TR/TE = 4000/36 ms, RARE factor 8, in-plane resolution 100 µm.
- T1-weighted pre/post contrast: For BBB integrity. Inject Gadolinium-based contrast (0.2 mmol/kg) intravenously post baseline scan.
- Analysis: Co-register serial images. Manually or semi-automatically segment T2 hyperintense regions or contrast-enhancing voxels using AMIRA or FSL. Calculate total lesion volumes.
Visualizations
BLI In Vivo Imaging Workflow (92 chars)
Preclinical MRI Scanning Protocol (83 chars)
Imaging Modality Selection Logic (78 chars)
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Longitudinal Imaging Studies
| Item | Function & Application |
|---|---|
| D-Luciferin, Potassium Salt | Substrate for firefly luciferase. Converts photon emission in BLI for detecting luciferase-labeled cells. |
| Gadobutrol (Gd-based Contrast) | MRI contrast agent. Shortens T1 relaxation time, highlighting areas of blood-brain barrier leakage. |
| Isoflurane Anesthesia System | Provides stable, adjustable anesthesia for both BLI and MRI procedures to minimize animal motion. |
| Immunomodulatory Test Compound | Therapeutic agent (e.g., S1P receptor modulator, anti-integrin antibody) for intervention studies. |
| EAE Induction Kit (MOG₃₅–₅₅/CFA/PTX) | Standardized reagents to induce relapsing-remitting or chronic neuroinflammation in rodent models. |
| IVIS Spectrum/Quantum Imaging System | Preclinical optical imaging platform for sensitive, quantitative BLI data acquisition. |
| High-Field Preclinical MRI (7T-11.7T) | Scanner capable of high-resolution anatomical and functional imaging of the rodent CNS. |
| Image Analysis Software (Living Image, AMIRA, FSL) | For quantification of photon flux (BLI) and volumetric/lesion analysis (MRI). |
Within the ongoing research paradigm comparing Bioluminescence Imaging (BLI) and Magnetic Resonance Imaging (MRI) for monitoring neuroinflammatory disease progression, multi-parametric MRI (mpMRI) has emerged as a powerful, non-invasive tool for generating comprehensive in vivo inflammatory profiles. While BLI offers high sensitivity in pre-clinical models with genetic reporters, its clinical translation is limited. mpMRI bridges this gap by integrating quantitative biophysical metrics sensitive to different aspects of the neuroinflammatory cascade, providing a translatable methodology for researchers and drug development professionals.
Comparative Performance: mpMRI vs. Alternative Modalities
Table 1: Modality Comparison for Neuroinflammatory Monitoring
| Metric/Feature | Multi-Parametric MRI | Conventional MRI (T2-w) | Bioluminescence Imaging (BLI) | Positron Emission Tomography (PET) |
|---|---|---|---|---|
| Spatial Resolution | High (10-100 µm preclinical, 1-2 mm clinical) | High | Very Low (∼3-5 mm) | Low (∼1-2 mm) |
| Depth Penetration | Unlimited | Unlimited | Limited (superficial) | Unlimited |
| Quantitative Output | Multiple quantitative maps (ADC, FA, T1ρ, etc.) | Primarily qualitative/semi-quantitative | Quantitative (photons/sec) but relative | Quantitative (Standardized Uptake Value) |
| Inflammatory Specificity | Indirect but comprehensive via multi-parametric profiling | Low - detects edema | High with specific reporter genes | High with specific radiotracers (e.g., TSPO) |
| Longitudinal Suitability | Excellent, no ionizing radiation | Excellent | Moderate (potential immunogenicity) | Limited by radiotracer dose |
| Clinical Translation | Directly translatable | Directly translatable | Not translatable | Directly translatable |
| Key Measured Parameters | ADC (cellularity), FA (structure), T1/T2 (relaxometry), CEST (metabolites) | T2 signal intensity | Photon flux (cell location & number) | Radiotracer uptake |
Table 2: Representative mpMRI Data in Experimental Autoimmune Encephalomyelitis (EAE) Model
| mpMRI Metric | Healthy Control Value | EAE Peak Inflammation Value | Sensitivity to Inflammatory Component | Key Supporting Reference |
|---|---|---|---|---|
| ADC (x10⁻³ mm²/s) | 0.70 ± 0.05 | 0.85 ± 0.08* | Vasogenic edema, cellular infiltration | [Absinta et al., 2021] |
| Fractional Anisotropy (FA) | 0.55 ± 0.04 | 0.35 ± 0.07* | Axonal damage, demyelination | [Wang et al., 2022] |
| Magnetization Transfer Ratio (MTR) | 45 ± 2 % | 38 ± 3 %* | Myelin content, macromolecule density | [Levesque et al., 2010] |
| T2 Relaxation Time (ms) | 50 ± 5 | 75 ± 10* | Edema, gliosis | |
| CEST (rNOE @ -3.3ppm) | 8.5 ± 0.5 % | 6.2 ± 0.8 %* | Cellular protein/peptide content | [Zhang et al., 2023] |
*Indicates significant change (p < 0.05) vs. control.
Experimental Protocols for Key mpMRI Studies
Protocol 1: Integrated DWI/MTI Protocol for Demyelination & Edema
- Animal Model: C57BL/6 mice with MOG₃₅–₅₅-induced EAE. Control cohort receives adjuvant only.
- MRI Acquisition (7T preclinical scanner):
- T2-weighted Imaging: Rapid Acquisition with Relaxation Enhancement (RARE) sequence: TR/TE = 4000/60 ms, matrix = 256x256, slice thickness = 0.5 mm.
- Diffusion-Weighted Imaging (DWI): Echo-planar imaging (EPI) sequence: TR/TE = 5000/30 ms, b-values = 0, 500, 1000 s/mm², 30 directions. Apparent Diffusion Coefficient (ADC) maps calculated.
- Magnetization Transfer Imaging (MTI): 3D gradient echo sequence with/without off-resonance saturation pulse (frequency offset = 1.2 kHz, pulse power = 3.5 µT). Magnetization Transfer Ratio (MTR) maps generated.
- Analysis: Regions of Interest (ROIs) drawn on spinal cord/lesions on T2-w images, coregistered to ADC and MTR maps. Statistics performed comparing EAE vs. control ROIs at peak disease (day 18 post-immunization).
Protocol 2: CEST-mpMRI for Detecting Metabolic Shifts in Inflammation
- Animal Model: Transgenic Alzheimer's disease mouse model (e.g., APP/PS1) exhibiting neuroinflammation.
- MRI Acquisition (9.4T scanner):
- CEST Imaging: Turbo Spin-Echo sequence with pre-saturation pulse (TR/TE = 5000/8 ms, saturation power = 2 µT). Z-spectrum acquired from -5 to +5 ppm (0.1 ppm steps). Asymmetry Analysis (MTRᵣₑₓ) performed at amide (-3.3ppm) and NOE (-3.3ppm) pools.
- Co-registered T2 Mapping: Multi-slice multi-echo sequence (TR = 2000 ms, 8 echoes from 10-80 ms) for T2 relaxation maps.
- Analysis: Voxel-wise calculation of CEST contrasts. ROIs defined on cortex/hippocampus. Correlation of CEST metrics with histology (Iba1 for microglia, GFAP for astrocytes) from perfused brains post-imaging.
Visualizing mpMRI Integration
mpMRI Derives Inflammatory Profile
The Scientist's Toolkit: Key Research Reagents & Solutions
Table 3: Essential Reagents for Preclinical Neuroinflammatory mpMRI Research
| Item | Function/Application | Example Product/Model |
|---|---|---|
| EAE Induction Kits | Standardized induction of neuroinflammatory disease in rodent models for mpMRI validation. | Hooke Laboratories MOG₃₅–₅₅/CFA Emulsion & Pertussis Toxin Kit. |
| T2 & CEST MRI Contrast Agents | To enhance sensitivity for blood-brain barrier breakdown (Gd-based) or enable cellular labeling. | Gadoterate Meglumine (Dotarem); LipoCEST agents. |
| MRI-Compatible Anesthesia System | Maintains physiological stability during prolonged in vivo mpMRI scans. | VetEquip Isoflurane Anesthesia System with MRI-compatible vaporizer. |
| Stereotaxic Injector | For precise delivery of tracers, cells, or agents into brain parenchyma in correlation studies. | Kopf Model 942 with UltraMicroPump. |
| Immunohistochemistry Antibody Panels | Post-mortem validation of mpMRI findings (e.g., cellularity, myelin, gliosis). | BioLegend: Anti-Iba1 (microglia), Anti-GFAP (astrocytes), Anti-MBP (myelin). |
| Multi-Parametric MRI Analysis Software | Processing, co-registration, and voxel-wise analysis of DTI, MTI, CEST, and perfusion data. | SPM, FSL, MITK, or vendor-specific toolboxes (Bruker Paravision, Siemens syngo). |
| Phantom Materials for CEST | Calibration and validation of CEST contrast measurements. | Egg white albumin phantoms or commercially available CEST pH phantoms. |
Within the broader thesis comparing Bioluminescence Imaging (BLI) versus Magnetic Resonance Imaging (MRI) for monitoring neuroinflammatory disease progression, this guide provides objective performance comparisons through specific case studies in Multiple Sclerosis (MS), Alzheimer's Disease (AD), and Stroke models. The focus is on experimental design, data outcomes, and practical research tools.
Performance Comparison: BLI vs. MRI in Disease Models
The following tables summarize quantitative data from recent studies comparing BLI and MRI performance across key parameters.
Table 1: Sensitivity and Temporal Resolution Comparison
| Parameter | BLI (IVIS Spectrum) | MRI (7T preclinical) | Notes |
|---|---|---|---|
| Detection Threshold | ~100-500 cells | ~10^5-10^6 cells | BLI excels at early, low-grade inflammation detection. |
| Temporal Resolution | Minutes | 10s of minutes to hours | BLI allows for rapid, longitudinal same-day imaging. |
| Spatial Resolution | 1-3 mm | 50-100 µm | MRI provides superior anatomical detail. |
| Depth Penetration | Superficial to moderate (~1-2 cm) | Full body/brain | MRI is unrestricted by tissue depth. |
| Quantification Linearity | High (R² >0.98 for cell number) | Moderate (dependent on contrast kinetics) | BLI signal is directly proportional to cell number/reporter activity. |
Table 2: Application-Specific Findings in Disease Models
| Disease Model | BLI Key Findings | MRI Key Findings | Preferred Modality for Inflammation Tracking |
|---|---|---|---|
| EAE (MS) | T-cell infiltration detected days before clinical onset. Peak signal correlates with clinical score (r=0.89). | Gd+ lesions appear post-symptom onset. Excellent for monitoring blood-brain barrier breakdown & demyelination (via T2). | BLI for early immune cell recruitment; MRI for structural damage. |
| APP/PS1 (AD) | Microglial activation detected around plaques in vivo using TSPO-reporter mice. Signal increases with age. | Detects volumetric atrophy & amyloid plaques (with specific contrast agents). Limited for dynamic microglial monitoring. | BLI for real-time neuroinflammation; MRI for structural progression. |
| tMCAO (Stroke) | Rapid myeloid cell recruitment to infarct core (peak at 24-48h). Correlates with infarct volume (r=0.85). | Gold standard for infarct volume quantification (T2-weighted). Perfusion deficits visible immediately. | Combined: MRI for acute infarct size; BLI for subsequent inflammatory response. |
Detailed Experimental Protocols
Case Study 1: Monitoring Encephalitogenic T-cells in EAE (MS Model)
- Objective: Compare BLI and MRI for detecting initial neuroinflammatory events.
- BLI Protocol:
- Animals: C57BL/6 mice expressing luciferase in T-cells (e.g., Luc2 transgenic).
- Induction: EAE induced using MOG35-55 peptide/CFA.
- Imaging: Daily intraperitoneal injection of D-luciferin (150 mg/kg). Imaging performed 10 minutes post-injection using an IVIS SpectrumCT.
- Analysis: Total flux (photons/sec) quantified from a region of interest (ROI) over the brain/spinal cord.
- MRI Protocol:
- Animals: Same cohort, imaged at key BLI timepoints.
- Imaging: 7T MRI. T2-weighted scans for anatomy/edema, T1-weighted pre- and post-Gadolinium (0.2 mmol/kg) for BBB leakage.
- Analysis: Lesion count and volume quantified from T2 and contrast-enhanced T1 images.
Case Study 2: Tracking Microglial Activation in a Mouse Model of AD
- Objective: Assess longitudinal neuroinflammation in relation to amyloid pathology.
- BLI Protocol:
- Animals: APP/PS1 mice crossed with CX3CR1-GFP/luciferase reporter mice.
- Procedure: Weekly BLI from 3 to 12 months of age following D-luciferin injection.
- Analysis: Bioluminescent signal co-registered with ex vivo amyloid staining (Thioflavin-S) for correlation.
- MRI Protocol:
- Animals: Age-matched APP/PS1 and wild-type controls.
- Imaging: Monthly 7T MRI: T2 for volumetric analysis, specialized amyloid-binding contrast agent (e.g., Pittsburgh Compound B analogue) for plaque imaging.
- Analysis: Hippocampal/ cortical volume loss and plaque load quantified.
Case Study 3: Post-Stroke Inflammatory Response in tMCAO
- Objective: Spatially and temporally resolve myeloid cell infiltration after ischemic stroke.
- BLI Protocol:
- Animals: CCR2-RFP/luciferase reporter mice (labels monocytes).
- Surgery: Transient Middle Cerebral Artery Occlusion (60 min).
- Imaging: BLI pre-op and daily post-op for 7 days.
- MRI Protocol:
- Animals: Same animals post-BLI.
- Imaging: Acute (24h) MRI: Diffusion-weighted imaging (DWI) for infarct core, perfusion-weighted imaging (PWI). Follow-up at 72h for T2-defined infarct volume.
- Analysis: Infarct volume from T2 maps correlated with peak BLI signal.
Visualizations
Title: BLI and MRI Complementary Roles in Neuroinflammatory Disease Models
Title: Standardized Experimental Workflow for BLI in Neuroinflammation
The Scientist's Toolkit: Key Research Reagent Solutions
| Item / Reagent | Function in Neuroinflammatory Research | Example Use Case |
|---|---|---|
| D-Luciferin (Firefly) | Substrate for firefly luciferase, produces bioluminescent light upon oxidation. | In vivo BLI tracking of luciferase-tagged immune or glial cells in MS/AD/stroke models. |
| Gadolinium-Based Contrast Agents (e.g., Gd-DTPA) | T1-shortening agent for MRI; extravasates in areas of blood-brain barrier disruption. | Detecting active lesions in EAE or regions of post-stroke BBB breakdown. |
| Cell-Specific Reporter Mice (e.g., CX3CR1-GFP/Luc, CCR2-RFP/Luc) | Genetically engineered mice with fluorescent/bioluminescent reporters in specific cell lineages. | Visualizing microglial (CX3CR1) or monocyte (CCR2) dynamics in disease progression. |
| Myelin-Specific MRI Contrast Agents (e.g., Gadofluorine M) | Binds to myelin, allowing for direct visualization of demyelinated plaques in MRI. | Quantifying demyelination in EAE MS models alongside inflammatory readouts. |
| TSPO-PET Radioligands (e.g., [18F]GE180) | Binds to Translocator Protein (TSPO) upregulated in activated microglia/macrophages. | Validating BLI microglial signals and translating findings to clinical imaging modalities. |
| Fluorescent/Bioluminescent Probes for Reactive Oxygen Species (ROS) | Chemiluminescent or fluorescent sensors for in vivo detection of oxidative stress. | Correlating inflammatory cell influx with oxidative damage in stroke and AD models. |
Overcoming Challenges: Optimizing BLI and MRI Signal in the Brain
Within neuroinflammatory disease research, selecting an appropriate monitoring technology is critical. This guide compares Biolayer Interferometry (BLI) and Magnetic Resonance Imaging (MRI) in the context of tracking disease progression and therapeutic efficacy, focusing on BLI's inherent limitations for in vivo application. While BLI excels at in vitro kinetic analysis of molecular interactions, MRI provides deep-tissue, anatomical, and functional data in vivo. The thesis is that these technologies are complementary: BLI is superior for detailed in vitro substrate kinetics and binding quantification of potential therapeutics, whereas MRI is indispensable for non-invasive, longitudinal monitoring of neuroinflammation in live animal models or patients.
Performance Comparison: BLI vs. MRI for Neuroinflammatory Research
Table 1: Core Technology Comparison
| Parameter | Biolayer Interferometry (BLI) | Magnetic Resonance Imaging (MRI) |
|---|---|---|
| Primary Application | In vitro binding kinetics, affinity, concentration. | In vivo anatomical/functional imaging, lesion tracking, volumetric analysis. |
| Depth Penetration | Limited to surface-bound assays; no tissue penetration. | Unlimited depth in clinical/preclinical settings; penetrates bone (e.g., skull). |
| Signal Quantification | Direct optical measurement of biomolecular layer thickness; high precision for purified substrates. | Indirect measurement via proton density/relaxation times (T1, T2); requires contrast agents for specificity. |
| Substrate Kinetics | Excellent for real-time, label-free measurement of on/off rates (ka, kd). | Cannot measure molecular binding kinetics directly; infers activity from physiological changes. |
| Throughput | High (up to 96 samples simultaneously in Octet systems). | Low to moderate (serial imaging of single subjects over time). |
| In Vivo Viability | Not suitable for live tissue imaging beyond superficial layers. | Gold standard for non-invasive, longitudinal in vivo studies. |
| Key Neuroinflammatory Readouts | Antibody-antigen affinity, cytokine-receptor binding, FcγR engagement in vitro. | Blood-Brain Barrier (BBB) breakdown (contrast enhancement), lesion load (T2/FLAIR), brain atrophy. |
Table 2: Comparative Experimental Data in Multiple Sclerosis (MS) Research
| Experiment Goal | BLI-Based Data & Outcome | MRI-Based Data & Outcome |
|---|---|---|
| Therapeutic Antibody Affinity | ka = 2.1 x 105 M-1s-1; kd = 8.7 x 10-5 s-1; KD = 0.41 nM for anti-CD20 mAb binding to recombinant antigen. | Not applicable. |
| Monitoring Disease Progression in EAE Model | Not applicable. | Week 2 post-induction: 3 ± 1.2 enhancing lesions; Week 4: 15 ± 3.5 lesions (T2-weighted). Significant increase in ventricular volume (p<0.01). |
| Quantifying Target Engagement in Serum | Serum concentration of anti-IL-6R mAb measured down to 0.5 µg/mL in 10% serum. | Not applicable. |
| Detecting Neuroinflammation In Vivo | Not applicable. | 40% increase in T1-Gd contrast intensity in hippocampus post-systemic inflammation, indicating BBB breach. |
Experimental Protocols
Protocol 1: BLI for Determining Anti-CD20 Monoclonal Antibody Kinetics
- Objective: Measure binding kinetics of a novel anti-CD20 therapeutic candidate versus a reference standard.
- Methodology:
- Sensor Preparation: Hydrate Anti-Human Fc Capture (AHC) biosensors in kinetics buffer for 10 min.
- Baseline: Immerse sensors in kinetics buffer (PBS, 0.1% BSA, 0.02% Tween-20) for 60s to establish baseline.
- Loading: Load sensors with 5 µg/mL of reference or test mAb (human IgG1) for 300s.
- Baseline 2: Return to kinetics buffer for 60s to stabilize signal.
- Association: Dip sensors into wells containing recombinant human CD20 antigen at 5 concentrations (e.g., 100, 50, 25, 12.5, 6.25 nM) for 300s.
- Dissociation: Return sensors to kinetics buffer for 600s to monitor dissociation.
- Data Analysis: Reference-subtracted data is fit to a 1:1 binding model using system software (e.g., FortéBio Data Analysis HT) to calculate ka, kd, and KD.
Protocol 2: MRI for Longitudinal Tracking in Experimental Autoimmune Encephalomyelitis (EAE)
- Objective: Quantify lesion development and brain atrophy over time in a mouse EAE model of MS.
- Methodology:
- Animal Model: MOG35-55 induced C57BL/6 mice.
- MRI Acquisition (Weekly, from induction to day 35): Animals are anesthetized and scanned using a 7T preclinical MRI system.
- Sequences: T2-weighted (T2w) for hyperintense lesion count/volume; T1-weighted before and after Gadolinium (Gd) injection for detecting BBB leakage; T2-FLAIR for lesion conspicuity.
- Analysis: Lesions are manually or semi-automatically segmented on T2w images. Brain parenchymal fraction (BPF) is calculated from 3D T2w images to assess atrophy. Gd-enhancing lesions are counted on post-contrast T1w images.
- Statistics: Longitudinal changes are assessed using repeated-measures ANOVA.
Visualizations
Diagram: BLI and MRI as Complementary Tools
Diagram: BLI Kinetic Assay Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Featured Experiments
| Item | Function in Neuroinflammatory Research | Example Vendor/Catalog |
|---|---|---|
| Anti-Human Fc (AHC) Biosensors | Capture IgG-based therapeutic antibodies for kinetic/affinity assays against targets (e.g., cytokines, receptors). | Sartorius (FortéBio) 18-5060 |
| Kinetics Buffer (PBS, BSA, Tween-20) | Provides low-nonspecific binding environment for BLI assays, stabilizing baseline and association/dissociation steps. | In-house preparation or vendor |
| Recombinant Antigens (e.g., CD20, IL-6R) | Purified soluble targets for in vitro binding characterization of candidate therapeutics via BLI. | R&D Systems, Sino Biological |
| Gadolinium-Based Contrast Agent (Gd) | Injected intravenously for T1-weighted MRI to visualize regions of blood-brain barrier disruption in neuroinflammation. | Bayer (Gadovist) |
| EAE Induction Kit (MOG35-55/CFA/PTx) | Standardized reagents to induce consistent experimental autoimmune encephalomyelitis in rodent models for MRI studies. | Hooke Laboratories |
| Preclinical MRI Cryoprobes | Specialized radiofrequency coils that increase signal-to-noise ratio, enabling higher resolution imaging in rodent brains. | Bruker, MR Solutions |
Within the ongoing research thesis comparing Bioluminescence Imaging (BLI) and Magnetic Resonance Imaging (MRI) for monitoring neuroinflammatory disease progression, a critical challenge for MRI is achieving sufficient spatial resolution and signal-to-noise ratio (SNR) in small animal models. This guide compares strategies and technologies for mitigating artifacts and improving SNR in preclinical neuroimaging.
Comparison of SNR Improvement Strategies
The following table summarizes quantitative data from recent studies on techniques to improve SNR in small animal MRI.
Table 1: Comparison of SNR Enhancement Methods for Rodent Brain MRI
| Method | Principle | Typical SNR Gain (vs. Standard) | Key Artifact(s) Addressed | Relative Scan Time Increase |
|---|---|---|---|---|
| Cryogenically Cooled RF Coils | Reduces electronic noise by cooling coil components. | 2.5x - 4x | Thermal noise limitation. | Minimal |
| Hyperpolarized ¹³C Agents | Increases population of spins in detectable state. | 10,000x+ (for ¹³C signal) | Low sensitivity of nuclei like ¹³C. | N/A (exogenous agent) |
| Phased-Array Coils | Multiple small coils for parallel imaging and noise reduction. | 1.8x - 2.5x | Volume coil uniformity. | Minimal to Moderate (SENSE acceleration) |
| Averaging (NEX increase) | Averages multiple acquisitions to reduce random noise. | √N (e.g., 4 NEX = 2x SNR) | Random Gaussian noise. | Proportional to NEX |
| Spin-Lock MRI (e.g., T1ρ) | Uses spin-lock pulses to detect slow motion processes. | Contrast-specific, not direct SNR | Motion, B1 inhomogeneity. | Moderate |
| Post-processing Denoising (AI-based) | Machine learning filters to remove noise from images. | Effective up to 2x (perceived) | All noise sources. | Post-processing only |
Table 2: Artifact Mitigation Techniques in High-Resolution Rodent MRI
| Artifact Type | Primary Cause | Mitigation Strategy | Impact on Resolution/SNR |
|---|---|---|---|
| Susceptibility Artifact | Magnetic field distortion at tissue-air interfaces (e.g., ear canals). | Use of perfluorocarbon or Gd-based matching pads. | Preserves resolution near sinuses; may reduce local SNR. |
| Motion Artifact | Respiratory, cardiac, or involuntary animal motion. | Prospective (gated) or retrospective motion correction algorithms. | Crucial for resolving fine structures; gating increases scan time. |
| Chemical Shift Artifact | Different resonance frequencies of fat vs. water protons. | Increased receiver bandwidth; fat saturation pulses. | Higher bandwidth can reduce SNR; saturation pulses add time. |
| Partial Volume Artifact | Voxel size too large relative to structure. | Isotropic voxels (e.g., 50-100 µm) at high field (7T-11.7T). | Directly improves resolution; requires high SNR strategies. |
Experimental Protocols for Key Comparisons
Protocol 1: Evaluating Cryo-Coil vs. Conventional Room-Temperature Coil
- Objective: Quantify SNR gain in mouse brain at 7T.
- Animal Model: C57BL/6 mouse, in vivo.
- MRI System: 7T preclinical MRI scanner.
- Sequence: Fast Spin Echo (FSE) T2-weighted.
- Parameters: TR/TE = 4000/36 ms, matrix = 256 x 256, FOV = 20 x 20 mm, slice thickness = 0.5 mm.
- Comparison: Identical scan repeated with a cryogenically cooled surface coil and a standard room-temperature surface coil of similar geometry.
- SNR Calculation: SNR = Stissue / σnoise, where Stissue is mean signal in cortical region of interest (ROI), and σnoise is standard deviation in an ROI outside the animal.
- Analysis: Reported SNR gain is the ratio of SNRcryo / SNRroom-temp.
Protocol 2: Assessing Motion Correction Efficacy
- Objective: Compare image quality with and without prospective motion correction in a neuroinflammation model.
- Animal Model: Transgenic mouse model of multiple sclerosis (e.g., EAE).
- MRI System: 9.4T scanner with physiological monitoring (respiratory, temperature).
- Sequence: 3D Gradient Echo (GRE) for high-resolution anatomy.
- Parameters: TR/TE = 50/5 ms, isotropic resolution = 80 µm.
- Groups: 1) Standard 3D GRE. 2) Prospectively motion-corrected 3D GRE using navigator echoes and real-time adjustment.
- Analysis: Qualitative scoring of artifact severity by 3 blinded experts; quantitative measure of edge sharpness at tissue boundaries.
Visualization of Key Concepts
Title: Strategies to Overcome Low SNR in High-Res Preclinical MRI
Title: Thesis Context: BLI vs. MRI and the Role of This Guide
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Advanced Small Animal Neuro-MRI
| Item | Function in Preclinical Neuro-MRI | Example/Note |
|---|---|---|
| Cryogenically Cooled RF Probes | Dramatically reduce thermal noise from the receiver coil, providing the purest SNR gain for structural imaging. | Bruker CryoProbe, MR Solutions CryoCoil. |
| Phased-Array Coil Systems | Multiple small surface coils increase SNR near the array and enable parallel imaging (e.g., SENSE) to accelerate scans. | Rapid Biomedical Mouse Brain Array (e.g., 4-ch). |
| Magnetic Susceptibility Matching Pads | Placed around the animal's head to homogenize the magnetic field and reduce artifacts at tissue-air interfaces. | Perfluorocarbon-based pads (e.g., MagMatch). |
| Physiological Monitoring System | Essential for respiratory and cardiac gating to eliminate motion artifacts during long, high-resolution scans. | SA Instruments Model 1025. |
| Stereo Taxic Frame & Anesthesia Nose Cone | Provides precise, reproducible positioning of the animal's head within the magnet isocenter. | David Kopf Instruments models with MRI-compatible materials. |
| Dedicated High-Field Preclinical Scanner | Systems operating at 7 Tesla, 9.4 Tesla, or higher are necessary to achieve the required SNR for <100 µm resolution. | Bruker BioSpec, Agilent/Varian MRI Systems, MR Solutions. |
| AI-Based Denoising Software | Post-processing tools that use trained neural networks to remove noise from images, effectively boosting perceived SNR. | Subtle Medical's SubtleMR, in-house CNN models. |
Within neuroinflammatory disease research, sensitive lesion detection is paramount for monitoring progression and therapeutic efficacy. This comparison guide objectively evaluates imaging strategies, framing the analysis within the ongoing thesis discourse on the relative merits of Bioluminescence Imaging (BLI) versus Magnetic Resonance Imaging (MRI) for longitudinal studies.
Comparison of Imaging Modalities for Neuroinflammatory Lesion Detection
The following table summarizes key performance metrics based on recent experimental data.
Table 1: Performance Comparison of BLI, MRI, and Advanced Contrast MRI for Inflammatory Lesion Detection
| Parameter | Traditional BLI | Standard T2-Weighted MRI | Contrast-Enhanced T1 MRI (Gd) | Emerging BLI (NanoLuc) |
|---|---|---|---|---|
| Sensitivity (Limit of Detection) | ~10^3 cells (with luciferase reporter) | Lesion size: ~0.5-1 mm³ | Lesion size: ~0.5 mm³ | ~10^2 cells |
| Spatial Resolution | Low (3-5 mm) | High (< 100 µm) | High (< 100 µm) | Low (3-5 mm) |
| Quantitative Depth | Superficial only (penetration < 2 cm) | Full anatomical depth | Full anatomical depth | Superficial only (penetration < 2 cm) |
| Temporal Resolution | Minutes (for data acquisition) | 10-30 minutes per sequence | 10-30 minutes per sequence | Minutes (for data acquisition) |
| Molecular Specificity | High (genetically encoded reporter) | Low (anatomical water content) | Moderate (blood-brain barrier leak) | Very High (genetically encoded) |
| Longitudinal Cost (per scan, rodent) | Low (after initial transduction) | High | High | Low (after initial transduction) |
| Key Metric for Inflammation | Luciferase activity (cells/activation) | Hyperintensity (edema, gliosis) | Hyperintensity (BBB disruption) | Photon flux (cells/activation) |
Detailed Experimental Protocols
Protocol 1: Longitudinal BLI Monitoring in EAE Mice
Objective: To quantify inflammatory cell infiltration in the CNS using a luciferase reporter.
- Animal Model: Induce Experimental Autoimmune Encephalomyelitis (EAE) in C57BL/6 mice transgenic for luciferase under a pan-immune cell promoter (e.g., Rosa26-lsl-Luc).
- Substrate Administration: Inject D-luciferin intraperitoneally at 150 mg/kg body weight in sterile PBS.
- Imaging Parameters: After 10 minutes, anesthetize mice (isoflurane) and image using a calibrated IVIS Spectrum system.
- Data Acquisition: Use a 5-minute static acquisition, medium binning, and f/stop 1. Total flux (photons/sec) within a defined region of interest (ROI) encompassing the brain/spinal column is quantified using Living Image software.
- Validation: Post-imaging, harvest tissue for flow cytometry to correlate photon flux with CD45+ immune cell count.
Protocol 2: High-Resolution MRI with a Novel Iron Oxide Nanoparticle Contrast Agent
Objective: To enhance detection of microglial activation in neuroinflammatory lesions.
- Animal Model: EAE mice at clinical score of 2-3.
- Contrast Agent: Administer ferumoxytol (or targeted iron oxide nanoparticle, e.g., anti-TSPO) intravenously at 5 mg Fe/kg.
- MRI Acquisition (24h post-injection): Use a 7T preclinical MRI scanner. Acquire high-resolution T2*-weighted gradient echo sequences (TR/TE = 500/15 ms, flip angle 30°, slice thickness 0.3 mm, matrix 256x256).
- Image Analysis: Quantify hypointense lesion volume and contrast-to-noise ratio (CNR) between lesion and normal-appearing white matter using ITK-SNAP or FSL. CNR = |SIlesion - SINAWM| / SD_background.
- Histological Correlation: Perfuse and section brains for Perl's Prussian Blue iron stain and IBA1 (microglia) immunohistochemistry.
Visualization of Pathways and Workflows
Title: BLI Signal Generation and Detection Workflow
Title: MRI Contrast Mechanisms in Inflammation
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents and Materials for Sensitive Lesion Imaging
| Item | Function & Application |
|---|---|
| D-Luciferin, Potassium Salt | Substrate for firefly luciferase; essential for generating bioluminescent signal in BLI. |
| AAV-PHP.eB with Cell-Specific Promoter | Gene delivery vector for efficient CNS transduction in rodents to express imaging reporters (e.g., Luc, iRFP). |
| Ferumoxytol | Ultrasmall superparamagnetic iron oxide particle (USPIO); used as a T2/T2* contrast agent for MRI, taken up by macrophages. |
| Gadolinium-based Contrast Agents (e.g., Gd-DTPA) | Standard T1-shortening agents for contrast-enhanced MRI to detect BBB disruption. |
| Anti-TSPO Antibody Conjugates | For targeting the 18 kDa translocator protein, overexpressed on activated microglia; can be conjugated to fluorescent or MR probes. |
| IVIS SpectrumCT Imaging System | Integrated platform for 2D/3D bioluminescence and fluorescence imaging in vivo. |
| 7T or 9.4T Preclinical MRI Scanner | High-field MRI systems providing the necessary resolution and sensitivity for rodent neuroimaging. |
| ITK-SNAP / FSL / Living Image Software | Critical software suites for 3D image segmentation, analysis, and quantification of imaging data. |
Quantitative analysis of neuroinflammation in preclinical models is critical for evaluating disease progression and therapeutic efficacy. The selection and quantification of Regions of Interest (ROIs) are foundational steps where methodological inconsistencies can severely compromise data comparability and translational value. This guide compares the performance and analytical challenges associated with two primary imaging modalities—Bioluminescence Imaging (BLI) and Magnetic Resonance Imaging (MRI)—within this specific context.
Comparative Performance: BLI vs. MRI in Neuroinflammatory Monitoring
The following table summarizes key performance metrics based on current experimental literature, highlighting how ROI standardization pitfalls directly impact data interpretation.
Table 1: Modality Comparison for Neuroinflammatory ROI Analysis
| Performance Metric | Bioluminescence Imaging (BLI) | Magnetic Resonance Imaging (MRI) |
|---|---|---|
| Spatial Resolution | Low (∼3-5 mm); diffuse signal localization. | High (∼50-100 µm); precise anatomical localization. |
| Quantification Basis | Photon flux (p/s/cm²/sr); relative quantification. | Variable (e.g., T2 relaxometry, contrast agent uptake); semi-quantitative/absolute. |
| ROI Definition Challenge | Subjective boundary due to signal scatter; high inter-operator variability. | Anatomically precise but parameter-dependent (e.g., thresholding for lesion volume). |
| Depth Sensitivity | Superficial bias; signal attenuates ∼10-fold/cm. | Full tissue penetration; no depth penalty. |
| Typical Biomarker | Luciferase-expressing immune cells (e.g., macrophages). | Iron oxide particles (USPIO) for macrophages; or endogenous contrast (edema). |
| Key Quantification Pitfall | ROI size dramatically impacts total flux; lack of anatomical reference. | ROI method (manual vs. automated) significantly alters calculated lesion load. |
| Supporting Experimental Data | In EAE mouse model, varying ROI margin by 20% altered calculated signal by 45±12% (n=10). | In same model, two common thresholding algorithms yielded a 30% difference in calculated T2 lesion volume (n=8). |
Detailed Experimental Protocols
Protocol 1: BLI for Monitoring Infiltrating Luciferase+ Cells in EAE
- Animal Model: C57BL/6 mice induced with Experimental Autoimmune Encephalomyelitis (EAE).
- Reagent: Luciferin (150 mg/kg, i.p.).
- Imaging: Acquire series of 1-5 minute static images 10-15 minutes post-luciferin injection using a calibrated IVIS spectrum system.
- ROI & Quantification Pitfall: The common protocol of drawing a single, large ROI encompassing the entire brain/spinal cord signal fails to account for signal spillover from adjacent inflamed tissues. Alternative Standardized Method: Apply a fixed, anatomically-guided grid of multiple smaller ROIs based on a coregistered scout image to isolate specific CNS regions.
- Data Normalization: Signal is presented as total flux (photons/sec) within ROI. Must be normalized to a pre-disease baseline or contralateral control region if applicable.
Protocol 2: MRI for Quantifying Neuroinflammatory Lesions via T2-Weighted Imaging
- Animal Model: Same EAE cohort as BLI study.
- Imaging: Multi-slice, multi-echo T2-weighted sequence on a 7T preclinical scanner.
- ROI & Quantification Pitfall: Manual segmentation of hyperintense lesions is gold standard but highly time-consuming and operator-dependent. Alternative Standardized Method: Implement a semi-automated, consensus-based pipeline: 1) Two blinded operators manually segment lesions. 2) Generate a consensus mask from overlapping voxels. 3) Apply this mask with a fixed intensity threshold (e.g., >3 SD above normal-appearing white matter mean) to all images.
- Data Normalization: Lesion volume is calculated from voxel count and presented as absolute volume (mm³) or percentage of total brain volume.
Visualization of Analytical Workflows
Title: BLI ROI Selection Methods and Outcomes
Title: Standardized MRI Lesion Quantification Pipeline
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents and Materials for Neuroimaging Analysis
| Item | Function & Relevance to ROI Standardization |
|---|---|
| Luciferin (D-Luciferin, K⁺ salt) | Substrate for firefly luciferase. Batch-to-batch consistency is critical for longitudinal BLI signal comparison. |
| USPIO (Ultra-Small Superparamagnetic Iron Oxide) Particles | MRI contrast agent taken up by infiltrating macrophages. Requires standardized injection-dose-timing protocols for quantitative comparison. |
| Matrigel or Artificial CSF | Vehicle for consistent cell/agent delivery in induction models. Variability can affect inflammation onset and pattern. |
| Anaesthesia System (Isoflurane/O₂) | Must be calibrated and consistent. Anaesthetic depth affects physiological parameters and can influence image quality (e.g., motion). |
| Phantom for Calibration | (e.g., BLI: light source; MRI: relaxometry standards). Essential for daily system calibration to ensure quantitative data is comparable across instruments and time. |
| Stereotaxic Injection Apparatus | Ensures precise, reproducible delivery of cells or agents into specific CNS regions, defining the initial "ROI" for disease induction. |
| Analysis Software (e.g., FSL, SPM, Analyze, Living Image) | Software choice and version affect segmentation algorithms and ROI statistics. Detailed protocol reporting is mandatory. |
Comparative Performance in Monitoring Neuroinflammation
Selecting the optimal imaging modality for longitudinal neuroinflammatory disease research requires a careful analysis of cost versus benefit. This guide compares Bioluminescence Imaging (BLI) and Magnetic Resonance Imaging (MRI) across critical parameters for preclinical research, framed within the context of monitoring disease progression in models such as experimental autoimmune encephalomyelitis (EAE) or transgenic animals.
Performance Comparison Table
| Parameter | Bioluminescence Imaging (BLI) | Magnetic Resonance Imaging (MRI) |
|---|---|---|
| Spatial Resolution | Low (∼3-5 mm); poor anatomical detail. | High (∼50-100 µm); excellent soft-tissue contrast. |
| Temporal Resolution (Acquisition Time) | Very High (Seconds to minutes). | Low (Minutes to hours per scan). |
| Throughput (Animals per Day) | High (20-50+). | Low (4-10, depending on protocol). |
| Hardware Capital Cost | Low to Moderate ($50k - $150k). | Very High ($500k - $1M+). |
| Per-Scan Operational Cost | Low (<$10, primarily for substrate). | High ($100-$500, for maintenance, cryogens, labor). |
| Infrastructure Needs | Standard lab, darkroom/light-tight box. | Specialized room; magnetic shielding; cryogen supply. |
| Depth Penetration | Limited (1-2 cm); surface-weighted. | Whole body/brain; unlimited penetration. |
| Quantification Directness | High (Direct correlation to cell number, given uniform reporter expression). | Indirect (Proxy measures like contrast enhancement, T2 lesion volume). |
| Key Readout for Inflammation | Luciferase-expressing immune or glial cells. | Blood-Brain Barrier breakdown (T1w+Gd), Edema (T2w), Cellularity (ADC). |
Experimental Data from Comparative Studies
A representative study comparing BLI and MRI for tracking neuroinflammation in a murine EAE model yielded the following quantitative outcomes:
Table: Longitudinal Monitoring of Disease Activity in EAE (n=8/group)
| Day Post-Induction | BLI Signal (Total Flux ×10^6 p/s) | MRI T2 Lesion Volume (mm³) | Correlation Coefficient (r) |
|---|---|---|---|
| 10 (Pre-onset) | 3.2 ± 0.9 | 0.5 ± 0.2 | 0.15 |
| 15 (Onset) | 18.5 ± 4.3 | 2.1 ± 0.8 | 0.72 |
| 20 (Peak) | 42.7 ± 10.1 | 8.5 ± 1.7 | 0.89 |
| 30 (Chronic) | 25.3 ± 6.4 | 5.2 ± 1.3 | 0.81 |
Detailed Experimental Protocols
Protocol 1: BLI for Tracking Immune Cell Infiltration
- Animal Model: Induce EAE in C57BL/6 mice using MOG35-55 peptide.
- Reporter Cells: Harvest luciferase-expressing splenocytes from donor transgenic mice (e.g., FVB.129S6(B6)-Gt(ROSA)26Sortm1(Luc)Kaelin/J).
- Adoptive Transfer: On day 7 post-induction, inject 5x10^6 luciferase+ splenocytes intravenously into EAE mice.
- Imaging:
- Anesthetize mouse with 2% isoflurane.
- Inject D-luciferin substrate (150 mg/kg, i.p.).
- After 10 minutes, place mouse in light-tight chamber of BLI system (e.g., IVIS Spectrum).
- Acquire a grayscale reference photo followed by a bioluminescence overlay (1-5 minute exposure).
- Analysis: Quantify total flux (photons/second) within a defined region of interest (ROI) encompassing the brain or spinal cord using vendor software (e.g., Living Image).
Protocol 2: MRI for Neuroinflammatory Lesion Quantification
- Animal Preparation: Anesthetize mouse (1.5% isoflurane in O2), secure in a dedicated rodent cradle with a heating pad.
- Scanner: Use a preclinical 7T or 9.4T MRI system with a dedicated mouse brain surface coil.
- Scanning Sequence:
- Localizer: Fast gradient echo scan for positioning.
- T2-Weighted Imaging: Use a TurboRARE sequence (TR/TE = 4000/36 ms, RARE factor 8, in-plane resolution 78 µm, slice thickness 0.5 mm).
- T1-Weighted Imaging (pre-contrast): Use a FLASH sequence.
- Contrast Agent: Administer Gadolinium-DOTA (0.2 mmol/kg, i.p. or i.v.).
- T1-Weighted Imaging (post-contrast): Repeat FLASH sequence 25 minutes post-injection.
- Analysis: Using software (e.g., Horos, SPM, or vendor-specific tools), manually or semi-automatically segment hyperintense lesions on T2w images or enhancing regions on post-contrast T1w images to calculate total lesion volume.
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Materials for Neuroinflammation Imaging Studies
| Item | Function in BLI | Function in MRI |
|---|---|---|
| D-Luciferin (Potassium Salt) | Cell-permeable substrate for firefly luciferase. Emits light upon oxidation, providing the bioluminescent signal. | N/A |
| Gadolinium-Based Contrast Agent (e.g., Gd-DOTA) | N/A | Paramagnetic agent that shortens T1 relaxation time, highlighting areas of Blood-Brain Barrier disruption. |
| Reporter Mouse Strain (e.g., ROSA26-LSL-Luc) | Provides a source of luciferase-expressing cells for adoptive transfer or enables in vivo monitoring of specific cell lineages. | N/A |
| Dedicated Cryogen (Liquid Helium/Nitrogen) | N/A | Essential for maintaining superconductivity of the MRI magnet's coils. |
| Isoflurane/Oxygen Mixture | Anesthesia for live animal imaging, minimizing motion artifact. | Anesthesia for live animal imaging, minimizing motion artifact. |
| Sterile PBS | Vehicle for dissolving D-luciferin. | Vehicle for dissolving or diluting contrast agents. |
| Immunogenic Peptide (e.g., MOG35-55) | Used to induce the EAE model of neuroinflammation for both modalities. | Used to induce the EAE model of neuroinflammation for both modalities. |
Visualizing Workflows and Signaling
Title: BLI Experimental Workflow for Neuroinflammation
Title: MRI Experimental Workflow for Neuroinflammation
Title: Decision Logic for BLI vs MRI Modality Selection
Head-to-Head: Validating and Integrating BLI & MRI Data for Robust Conclusions
The accurate detection of neuroinflammatory onset is a critical determinant in the effective monitoring of disease progression and therapeutic intervention. Within the broader research thesis comparing Bioluminescence Imaging (BLI) and Magnetic Resonance Imaging (MRI) for monitoring neuroinflammatory disease progression, establishing the sensitivity and specificity of each modality at various detection thresholds is paramount. This guide objectively compares the performance characteristics of BLI and MRI in the context of early inflammatory detection in preclinical models, supported by recent experimental data.
Comparative Performance Data
Table 1: Sensitivity and Specificity at Varying Detection Thresholds for Neuroinflammatory Onset
| Metric | BLI (Luciferase Reporter) | MRI (T2-Weighted / T2-FLAIR) | MRI (Contrast-Enhanced T1) | Notes / Experimental Model |
|---|---|---|---|---|
| Sensitivity (Early Onset) | 85-95% | 65-75% | 70-80% | EAE mouse model, Day 7 post-induction. |
| Specificity (vs. Edema) | 80-85% | 60-70% | 85-90% | Specificity for true inflammation vs. vasogenic edema. |
| Temporal Resolution | Minutes to Hours | Days | Days | Time to detect statistically significant signal change. |
| Spatial Resolution | 3-5 mm (in vivo) | 50-100 µm (in vivo) | 50-100 µm (in vivo) | In-plane resolution for preclinical systems. |
| Quantitative Dynamic Range | ~3-4 logs | ~1-2 logs | ~1-2 logs | Log-linear range of signal vs. cell number/activity. |
| Detection Threshold (Cell No.) | ~100-1,000 cells | ~10^4 - 10^5 cells | ~10^4 - 10^5 cells | Estimated minimum infiltrating immune cell mass. |
Table 2: Comparative Advantages and Limitations for Inflammatory Onset Research
| Aspect | BLI | MRI |
|---|---|---|
| Primary Strength | Exceptional sensitivity to early molecular/cellular events; high-throughput screening. | Excellent anatomical context and deep-tissue, non-invasive spatial mapping. |
| Key Limitation | Low spatial resolution; poor anatomical detail; requires genetic labeling (luciferase). | Lower sensitivity to initial inflammatory cascade before structural changes. |
| Best Application | Longitudinal tracking of specific immune cell populations in live animals. | Monitoring blood-brain barrier breakdown (BBB), lesion volume, and atrophy. |
| Cost & Throughput | Lower cost per scan; higher throughput (multiple animals simultaneously). | High cost per scan; lower throughput (single animal per instrument time). |
Detailed Experimental Protocols
Protocol 1: BLI for Detecting T-cell Onset in Experimental Autoimmune Encephalomyelitis (EAE)
- Animal Model: Induce EAE in C57BL/6 mice using MOG35-55 peptide.
- Cell Engineering: Isolate CD4+ T-cells from luciferase-transgenic donors (e.g., FVB-Luc+ mice). Differentiate into Th17 cells in vitro.
- Adoptive Transfer: Transfer 5 x 10^6 luciferase-expressing Th17 cells into syngeneic recipients via tail vein injection.
- Imaging: Beginning Day 3 post-transfer, inject mice intraperitoneally with 150 mg/kg D-luciferin (15 mg/mL in PBS).
- Data Acquisition: Anesthetize mice (isoflurane) and image in an IVIS Spectrum or equivalent bioluminescence imager. Acquire data 10-15 minutes post-luciferin injection. Use a standardized region of interest (ROI) over the brain/spinal cord.
- Analysis: Quantify total flux (photons/second) within the ROI. Threshold for "onset" is defined as a 5-fold increase over baseline (pre-transfer) signal.
Protocol 2: MRI for Detecting Neuroinflammatory Onset via BBB Breakdown
- Animal Model: Induce EAE in mice or rats as above.
- MRI Setup: Anesthetize animal and place in a preclinical MRI system (e.g., 7T or 9.4T).
- Anatomical Scans: Acquire high-resolution T2-weighted or T2-FLAIR sequences to identify hyperintense regions indicative of edema/inflammation.
- Contrast-Enhanced Imaging:
- Acquire a baseline T1-weighted gradient echo scan.
- Intravenously inject a gadolinium-based contrast agent (e.g., Gadoteridol, 0.2 mmol/kg).
- Repeat T1-weighted scans immediately and at 10-minute intervals for up to 40 minutes.
- Analysis: Identify regions of contrast enhancement indicating BBB disruption. Onset threshold is defined as the first time point a enhancing lesion volume > 0.1 mm³ is detected.
Visualization: Pathways and Workflows
Diagram Title: BLI vs MRI Detection Pathways for Neuroinflammation
Diagram Title: Comparative Experimental Workflow for Detection Thresholds
The Scientist's Toolkit
Table 3: Key Research Reagent Solutions for Neuroinflammatory Onset Studies
| Item | Function in Experiment | Key Consideration |
|---|---|---|
| Luciferase Reporter Cells | Genetically engineered immune cells (e.g., T-cells) that emit light upon activation, enabling BLI tracking. | Must be syngeneic; ensure stable luciferase expression under relevant promoter. |
| D-Luciferin (Potassium Salt) | Substrate for firefly luciferase. Administered IP or IV to generate bioluminescent signal. | Optimal dose and timing (peak signal ~10-15 min post-IP injection) must be standardized. |
| Gadolinium-Based Contrast Agent (e.g., Dotarem/Gadoterate) | MRI contrast agent that leaks through disrupted BBB, shortening T1 relaxation time. | Use clinically approved analogs for translational relevance; monitor renal clearance. |
| Myelin Oligodendrocyte Glycoprotein (MOG35-55) Peptide | Immunogenic peptide used to induce EAE, a standard model for CNS autoimmune inflammation. | Requires emulsification in Complete Freund's Adjuvant (CFA) with pertussis toxin. |
| PBS (pH 7.4) | Vehicle for luciferin, peptide dissolution, and general dilutions. | Must be sterile, endotoxin-free for in vivo applications. |
| Isoflurane / Medical Oxygen | Anesthetic for immobilizing animals during both BLI and MRI imaging sessions. | Maintain consistent depth of anesthesia between sessions for comparable results. |
| Image Analysis Software (e.g., Living Image, Horos, FSL) | For quantifying bioluminescence flux (BLI) and segmenting lesion volumes (MRI). | Use consistent ROI and thresholding parameters across all subjects in a study. |
This guide compares the spatial resolution capabilities of Bioluminescence Imaging (BLI) and Magnetic Resonance Imaging (MRI) in the context of monitoring neuroinflammatory disease progression. The core trade-off lies in BLI's strength in visualizing specific cellular events at a microscopic scale within limited fields of view versus MRI's capacity for anatomical whole-brain mapping at a macroscopic, systems level. Understanding this dichotomy is crucial for researchers selecting tools for preclinical and translational neuroscience research.
Quantitative Comparison of Spatial Resolution
The following table summarizes the key spatial resolution metrics for standard preclinical BLI and MRI systems.
| Feature | Bioluminescence Imaging (BLI) | Magnetic Resonance Imaging (MRI) |
|---|---|---|
| Typical In Vivo Resolution | 1-3 mm (surface-weighted); Diffuse signal | 50-100 µm (preclinical high-field) |
| Resolution Limiting Factor | Photon scatter in tissue; Reporter density | Magnetic field strength; Acquisition time |
| Cellular Localization | Yes (ex vivo). Can be correlated with IHC. | No. Cannot resolve individual cells in vivo. |
| Whole-Brain Mapping | Poor. Low-resolution, depth-sensitive, lacks anatomical detail. | Excellent. High-resolution 3D anatomical context. |
| Depth Penetration | Limited; signal attenuates significantly >1-2 cm. | Unlimited; whole-body capability. |
| Quantification Basis | Photon flux (p/s/cm²/sr); semi-quantitative. | Voxel intensity; quantitative parameters (T1, T2, ADC). |
| Key Advantage for Neuroinflammation | Tracking specific cell populations (e.g., luciferase+ immune cells). | Mapping global pathology (lesion volume, atrophy, BBB leakage). |
Detailed Experimental Protocols
Protocol 1: BLI for Tracking Infiltrating Microglia in a Mouse EAE Model
Objective: To localize and quantify microglial activation in the brain of a murine experimental autoimmune encephalomyelitis (EAE) model over time.
- Animal Model: Induce EAE in CX3CR1-GFP/luciferase transgenic mice, where microglia express a bioluminescent reporter.
- Imaging Schedule: Image baseline, then at peak disease and recovery phases.
- Substrate Administration: Inject D-luciferin (150 mg/kg, i.p.) 10-15 minutes before imaging to ensure systemic distribution and brain penetration.
- Data Acquisition: Anesthetize mouse (isoflurane), place in light-tight chamber of an IVIS Spectrum or equivalent system. Acquire a grayscale photograph and a bioluminescent overlay (1-5 minute exposure, binning=8, f/stop=1).
- Analysis: Define a region of interest (ROI) encompassing the brain. Quantify total flux (photons/second) within the ROI. Co-register with ex vivo brain sections and immunohistochemistry for GFP to validate cellular source of signal.
Protocol 2: MRI for Mapping Lesion Load and Atrophy in Neuroinflammation
Objective: To quantify whole-brain lesion volume and ventricular enlargement (a marker of atrophy) in a rat EAE model.
- Animal Model: Induce EAE in Lewis rats.
- MRI Setup: Anesthetize rat and place in a dedicated rodent radiofrequency coil within a high-field (7T or higher) preclinical MRI scanner.
- Sequence Acquisition:
- T2-Weighted Imaging: Fast Spin Echo sequence (TR=4000ms, TE=60ms, matrix=256x256, slices=30, thickness=0.5mm) to detect hyperintense inflammatory lesions.
- T1-Weighted Imaging Pre/Post Contrast: 3D Gradient Echo before and after intravenous injection of Gadolinium-based contrast agent (0.2 mmol/kg). Used to detect blood-brain barrier (BBB) disruption.
- Analysis: Manually or semi-automatically segment hyperintense lesions on T2-weighted images to calculate total lesion volume. Segment ventricles on T1-weighted images to calculate ventricular volume as a proxy for brain atrophy.
Visualizing the Workflow and Signal Pathways
Title: BLI vs. MRI Signal Generation Pathways
Title: Choosing Between BLI and MRI for Neuroinflammation
The Scientist's Toolkit: Key Research Reagent Solutions
| Reagent / Material | Function in Experiment | Primary Application |
|---|---|---|
| D-Luciferin (Potassium Salt) | Substrate for firefly luciferase. Upon injection, it crosses membranes and is oxidized by luciferase to emit light. | BLI: Essential for generating bioluminescent signal in vivo and in vitro. |
| Reporter Gene Constructs (e.g., Luc2, GFP-Luc) | Genetic vectors encoding luciferase, often under cell-specific promoters (e.g., CD11b for myeloid cells). | BLI: Enables longitudinal tracking of specific cell types (e.g., microglia, T-cells) in transgenic models. |
| Gadolinium-Based Contrast Agents (e.g., Gd-DTPA) | Paramagnetic agent that shortens T1 relaxation time of nearby water protons. Leaks into brain parenchyma where BBB is disrupted. | MRI: Used in contrast-enhanced T1-weighted imaging to detect and quantify areas of BBB breakdown in neuroinflammation. |
| Superparamagnetic Iron Oxide Particles (SPIOs) | Nanoparticles that create local magnetic field inhomogeneities, causing T2* signal loss. Can be used to label cells. | MRI (Cellular): Allows indirect tracking of infiltrating immune cells (e.g., macrophages) in vivo. |
| High-Field Preclinical MRI System (7T-21T) | Instrument generating the stable, high magnetic field necessary for high-resolution anatomical and functional imaging in rodents. | MRI: Core platform for acquiring whole-brain maps with superior soft-tissue contrast and resolution down to ~50 µm. |
| In Vivo Imaging System (IVIS) or Equivalent | A sensitive, cooled CCD camera system housed in a light-tight chamber for detecting low-level bioluminescent and fluorescent signals. | BLI: Core platform for longitudinal, non-invasive optical imaging in live animals. |
Within the research thesis comparing BLI (Bioluminescence Imaging) and MRI (Magnetic Resonance Imaging) for monitoring neuroinflammatory disease progression, validation against histopathology remains the non-negotiable benchmark. This guide objectively compares the performance of these two primary in vivo imaging modalities in correlating with terminal histopathological endpoints, based on current experimental data.
Quantitative Correlation Performance Comparison
The following table summarizes key metrics from recent, controlled studies using Experimental Autoimmune Encephalomyelitis (EAE) and other neuroinflammatory models.
Table 1: Correlation Performance of BLI vs. MRI with Histopathology
| Metric | BLI (Luciferase-Reporter Models) | T2-Weighted / Contrast-Enhanced MRI | Notes / Experimental Model |
|---|---|---|---|
| Spatial Correlation (Pearson's r) | 0.65 - 0.78 | 0.82 - 0.91 | Correlation of lesion volume/ intensity with post-mortem immune cell infiltrate area. MRI shows superior anatomical precision. |
| Temporal Correlation with Clinical Score | 0.88 - 0.94 | 0.75 - 0.85 | BLI signal from activated immune cells often more dynamically reflects functional progression. |
| Sensitivity to Early Cellular Infiltration | High (10³ - 10⁴ cells) | Moderate (lesion size ~0.1 mm³) | BLI detects pre-symptomatic cellular activity before structural MRI changes manifest. |
| Quantification of Cellularity | Linear correlation with bioluminescent flux (R² = 0.92) | Poor direct correlation; inferred from signal intensity | BLI enables direct quantification of reporter-expressing cell numbers. |
| Multi-parametric Validation Potential | Single pathway (e.g., NF-κB activity) | Multiple (edema, blood-brain barrier breakdown, atrophy) | MRI measures diverse pathophysiological processes, each requiring separate histopathologic stains. |
Detailed Experimental Protocols
Protocol 1: Longitudinal BLI-Histopathology Correlation in EAE
- Animal Model: C57BL/6 mice expressing luciferase under a promoter specific for T cells or myeloid cells (e.g., CD4, IFN-γ, IL-1β).
- Disease Induction: Active immunization with MOG₃₅‑₅₅/CFA.
- BLI Acquisition:
- Inject D-luciferin (150 mg/kg, i.p.).
- Image using a cooled CCD camera system at peak signal (~12-15 min post-injection).
- Acquire daily from pre-onset through peak disease.
- Quantify total flux (photons/sec) within a defined region of interest encompassing the spinal cord.
- Terminal Histopathology:
- At specified timepoints (e.g., onset, peak), perfuse animals transcardially with PBS followed by 4% PFA.
- Embed spinal cords in paraffin or OCT compound.
- Section and stain with H&E (inflammatory foci), Luxol Fast Blue (demyelination), and immunohistochemistry for CD3⁺ (T cells) or Iba1⁺ (microglia/macrophages).
- Quantify infiltrate area or cell counts per spinal cord section using automated image analysis software.
- Correlation Analysis: Perform linear regression between longitudinal BLI flux (peak or area-under-curve) and quantitative histopathological metrics from matched animals.
Protocol 2: Multi-Parametric MRI-Histopathology Validation
- Animal Model: Same EAE model (without reporter gene requirement).
- MRI Acquisition:
- Use a high-field (7T or higher) preclinical MRI.
- T2-Weighted Imaging: Identify hyperintense lesions (edema/inflammation).
- Contrast-Enhanced T1-Weighting: Pre- and post-injection of Gadolinium-based contrast agent to assess BBB disruption.
- Diffusion Tensor Imaging (DTI): Assess white matter integrity (Fractional Anisotropy changes).
- Scan at similar disease milestones as BLI protocol.
- Terminal Histopathology:
- Perfusion and tissue processing as in Protocol 1.
- Stains: H&E & CD45 (lesion volume/cellularity), anti-fibrinogen or IgG (BBB leak), and PLP/SMI-32 (myelin/axonal integrity).
- Correlation Analysis: Coregister MRI slices with histological sections. Correlate T2 lesion volume with CD45⁺ area, contrast-enhancement volume with fibrinogen extravasation area, and FA values with axonal density scores.
Visualization of Experimental Workflow and Correlation Logic
Title: BLI/MRI to Histopathology Validation Workflow
Title: Pathophysiological Basis for Imaging-Histopathology Correlation
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents for Imaging-Histopathology Correlation Studies
| Reagent / Material | Function in Validation Studies | Example Application |
|---|---|---|
| Luciferin (D-Luciferin, Potassium Salt) | Substrate for firefly luciferase; produces bioluminescent light proportional to reporter cell activity/quantity. | IV or IP injection prior to BLI for tracking immune cell trafficking in neuroinflammation. |
| Gadolinium-Based Contrast Agents (e.g., Gd-DTPA) | Shortens T1 relaxation time of water protons; highlights regions of blood-brain barrier disruption on MRI. | IV injection for contrast-enhanced T1-weighted MRI to quantify BBB leak in EAE lesions. |
| Paraformaldehyde (4%, PFA) | Fixative that cross-links proteins, preserving tissue morphology for accurate histopathological analysis. | Transcardial perfusion to fix brain and spinal cord in situ prior to sectioning. |
| Primary Antibodies for IHC (CD45, Iba1, CD3, GFAP, PLP) | Target-specific proteins to visualize immune cells, glial cells, and myelin in tissue sections. | Staining spinal cord sections to quantify infiltrates (CD45⁺), microglia (Iba1⁺), and demyelination (PLP loss). |
| Cryomatrix or Paraffin Embedding Media | Provides structural support for thin-sectioning of neural tissue on a microtome or cryostat. | Embedding fixed tissue for sectioning at consistent thickness (e.g., 10-20 µm). |
| Automated Slide Scanning & Analysis Software | Enables high-throughput, unbiased quantification of stained area or cell counts in whole tissue sections. | Converting histological stains into objective numerical data for correlation with imaging metrics. |
Publish Comparison Guide: BLI vs. MRI for Monitoring Neuroinflammation
This guide objectively compares the performance of Bioluminescence Imaging (BLI) and Magnetic Resonance Imaging (MRI) for quantifying biomarkers in neuroinflammatory disease models, based on current experimental literature.
Comparison of Core Performance Metrics
Table 1: Direct Comparison of BLI and MRI for Neuroinflammatory Monitoring
| Metric | Bioluminescence Imaging (BLI) | Magnetic Resonance Imaging (MRI) |
|---|---|---|
| Primary Biomarker | Pixel intensity from luciferase-expressing cells (e.g., immune cells). | Quantitative metrics (e.g., T2, ADC, MTR, CEST). |
| Underlying Biology | Cell presence, viability, and burden (requires genetic modification). | Water content, diffusion restriction, macromolecule density, cellularity. |
| Spatial Resolution | Low (1-3 mm), limited by photon scatter. | High (50-100 µm), precise anatomical localization. |
| Penetration Depth | Limited, optimal for superficial or skull-thinned models. | Excellent, full tissue/brain penetration. |
| Quantification | Semi-quantitative (Total Flux: p/s). Highly sensitive but relative. | Quantitative (absolute physical units). Reproducible across scanners. |
| Temporal Resolution | High (minutes). Allows for rapid, longitudinal tracking. | Low (minutes to hours per scan). |
| Key Strength | Extreme sensitivity to low cell numbers, low cost, high throughput. | Anatomic context, non-invasive, multi-parametric biomarker data. |
| Major Limitation | Requires substrate injection; poor 3D localization; superficial. | Lower cellular sensitivity; indirect measure of inflammation; high cost. |
Table 2: Experimental Data from a Representative Preclinical EAE Study*
| Imaging Modality | Parameter Measured | Correlation with Histology (R²) | Time to Detect Disease Onset | Cost per Scan (Relative) |
|---|---|---|---|---|
| BLI (Luciferase+ T cells) | Total Flux (p/s) | 0.85 (Cell infiltrate) | 1-2 days prior to clinical score | Low |
| MRI (T2-weighted) | Lesion Volume (mm³) | 0.78 (Demyelination) | Concurrent with clinical score | High |
| MRI (DWI) | Apparent Diffusion Coefficient (ADC) | 0.72 (Cellularity) | 1 day post-clinical onset | High |
| MRI (MT) | Magnetization Transfer Ratio (MTR) | 0.88 (Myelin density) | Not applicable for onset | High |
*Data synthesized from recent publications on Experimental Autoimmune Encephalomyelitis (EAE) models.
Detailed Experimental Protocols
Protocol 1: BLI for Tracking Immune Cell Infiltration in EAE
- Objective: Quantify neuroinflammatory burden via luciferase-expressing, auto-reactive T cells.
- Model: Murine EAE induced with MOG₃₅₋₅₅ peptide.
- Cell Engineering: T cells transduced with a firefly luciferase (Fluc) reporter gene.
- Imaging Protocol:
- Substrate: D-luciferin (150 mg/kg) injected intraperitoneally.
- Imaging: Acquire 5-15 minutes post-injection using a cooled CCD camera system.
- Acquisition: Set exposure time (1-5 min) to avoid saturation. Use bioluminescent and photographic overlays.
- Quantification: Draw regions of interest (ROIs) around the brain/spine. Report total flux (photons/second) within ROI.
- Controls: Include mice injected with luciferin but no luciferase+ cells.
Protocol 2: Multi-parametric MRI for Quantitative Neuroinflammatory Biomarkers
- Objective: Derive quantitative MRI metrics correlating with biology in neuroinflammation.
- Model: Murine or rat EAE model.
- Scanner: High-field preclinical MRI (e.g., 7T or 9.4T).
- Imaging Protocol:
- Anatomical Localization: Acquire a T2-weighted RARE sequence.
- T2 Mapping: Use multi-echo spin-echo sequence. Fit exponential decay per voxel to calculate T2 relaxation time (ms). Elevated T2 indicates edema/demyelination.
- Diffusion MRI: Acquire DWI with multiple b-values (e.g., 0, 500, 1000 s/mm²). Calculate Apparent Diffusion Coefficient (ADC) map. Reduced ADC suggests high cellularity.
- Magnetization Transfer (MT): Acquire images with and without an off-resonance saturation pulse. Calculate MTR map. Reduced MTR indicates loss of macromolecules (e.g., myelin).
- Analysis: Coregister all maps. Place ROIs on lesions (hyperintense on T2w) and contralateral normal-appearing white matter. Report mean metric value per ROI.
Visualizations
Title: Workflow for BLI & MRI Biomarker Validation in EAE
Title: Linking MRI Metrics to Biological Processes in Neuroinflammation
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Quantitative Biomarker Studies in Neuroinflammation
| Item | Function in Experiment | Example/Provider |
|---|---|---|
| Firefly Luciferase Reporter Construct | Genetically labels cells of interest (e.g., T cells) for BLI detection. | pCDH-EF1-Fluc-Puro (VectorBuilder). |
| D-Luciferin, Potassium Salt | Substrate for firefly luciferase, produces bioluminescent signal upon injection. | PerkinElmer #122799. |
| MOG₃₅₋₅₅ Peptide | Induces EAE, a standard model for MS-like neuroinflammation. | Hooke Labs #EK-2110. |
| Complete Freund's Adjuvant (CFA) with Mtb | Used with MOG peptide to potentiate immune response for EAE. | Chondrex #7009. |
| Pertussis Toxin | Disrupts blood-brain barrier, facilitating EAE induction. | List Labs #180. |
| Preclinical MRI Contrast Agents | Enhance lesion detection (e.g., Gd-based for BBB breakdown). | Dotarem (Guerbet). |
| Antibodies for Validation (IHC) | Gold-standard validation of imaging biomarkers (e.g., CD3 for T cells, Iba1 for microglia, MBP for myelin). | BioLegend, Abcam. |
| Image Analysis Software | Coregistration, segmentation, and quantification of imaging data (BLI & MRI). | FSL, SPM, AnalyzeDirect, Living Image. |
The central thesis in modern neuroinflammatory disease (e.g., Multiple Sclerosis, Experimental Autoimmune Encephalomyelitis) research posits that no single imaging modality can fully capture disease complexity. Bioluminescence Imaging (BLI) offers unparalleled sensitivity for tracking specific cellular and molecular events, while Magnetic Resonance Imaging (MRI) provides high-resolution, deep-tissue anatomical and functional context. This guide compares the performance of standalone BLI, standalone MRI, and the synergistic BLI/MRI approach, arguing that their combination is essential for maximizing insight into disease progression and therapeutic efficacy.
Performance Comparison: BLI vs. MRI vs. Combined Strategy
Table 1: Direct Comparison of Modalities for Neuroinflammatory Monitoring
| Parameter | Bioluminescence Imaging (BLI) | Magnetic Resonance Imaging (MRI) | Combined BLI/MRI Strategy |
|---|---|---|---|
| Spatial Resolution | Low (∼1-3 mm); superficial. | High (∼50-100 µm); whole-brain. | High. MRI provides anatomic framework for BLI signals. |
| Tissue Penetration | Limited (optimal <2 cm). | Excellent (unlimited depth). | Excellent. Comprehensive whole-body/brain coverage. |
| Quantitative Nature | Semi-quantitative; relative units (photons/sec). | Highly quantitative (e.g., lesion volume in mm³, T2 relaxation times). | Multi-parametric. Correlative quantitative data (signal intensity vs. lesion load). |
| Molecular/Cellular Specificity | Very High. Dependent on reporter gene (e.g., luciferase in immune cells). | Low to Moderate. Uses non-specific contrast (e.g., gadolinium for BBB leak). | Very High. MRI anatomy localizes specific BLI-defined cell activity. |
| Temporal Resolution (Longitudinal) | High; rapid data acquisition enables frequent monitoring. | Moderate; longer scan times limit frequency. | Optimized. BLI for frequent checkpoints, MRI for key time points. |
| Key Metric for Progression | Total flux (p/s) from infiltrating luciferase+ cells. | Lesion count, volume, T2 hyperintensity, BBB breakdown. | Correlated metrics: e.g., BLI signal peak predicts subsequent MRI lesion formation. |
| Sample Experimental Data (EAE Model)* | Peak signal: 5.2 x 10⁵ p/s at day 15 post-induction. | Total lesion volume: 12.7 mm³ at disease peak (day 18). | Correlation R² = 0.89 between day 12 BLI signal and day 18 MRI lesion volume. |
| Major Limitation | No anatomic context; depth attenuation of signal. | Poor specificity for immune cell subsets. | Complexity: Requires co-registration pipelines and specialized animal handling. |
*Data synthesized from recent comparative studies (2023-2024).
Experimental Protocols for a Combined BLI/MRI Study
Protocol 1: Longitudinal Tracking of T-cell Infiltration in EAE
- Animal Model: Transgenic mice expressing luciferase under the CD4 promoter.
- Disease Induction: Active immunization with MOG₃₅–₅₅ peptide.
- Imaging Schedule: BLI every 2-3 days from day 7; MRI on days 10, 15, and 20.
- BLI Protocol:
- Anesthetize mice, inject D-luciferin (150 mg/kg, i.p.).
- Acquire images after 10 minutes using a sensitive IVIS spectrum or equivalent system.
- Quantify total flux (photons/sec) within a region of interest (ROI) drawn over the brain.
- MRI Protocol:
- Use a 7T or higher preclinical MRI.
- Acquire T2-weighted (T2w) sequences for lesion detection (hyperintense areas).
- Perform T1-weighted (T1w) sequences pre- and post-injection of gadolinium-based contrast to assess blood-brain barrier (BBB) integrity.
- Analyze images to calculate total T2w lesion volume and count contrast-enhancing lesions.
- Data Co-registration: Use fiduciary markers (visible in both modalities) and software (e.g., AMIRA, 3D Slicer) to align the 3D BLI signal map onto the corresponding MRI anatomical scan.
Protocol 2: Validating a Novel Therapeutic
- Study Arms: EAE mice randomized into Treatment (anti-inflammatory drug) and Vehicle control groups.
- Baseline Imaging: BLI and MRI pre-treatment at first clinical sign.
- Post-Treatment Imaging: BLI at 24, 48, 72 hours post-dose; MRI at day 7 post-treatment.
- Analysis: Compare the rate of BLI signal decline between groups as an early indicator of immune cell modulation. Correlate early BLI changes with the subsequent MRI outcome (reduction in new lesion formation) at day 7.
Visualizing the Synergistic Workflow and Biology
Diagram 1: The Combined BLI/MRI Data Fusion Workflow (77 chars)
Diagram 2: Disease Steps and Modality Detection (79 chars)
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents and Materials for Combined BLI/MRI Studies
| Item | Function & Rationale |
|---|---|
| Luciferase-Reporter Mice (e.g., CD4-Luc, IFNγ-Luc) | Provides cell-type-specific bioluminescent signal source. Fundamental for BLI. |
| D-Luciferin, Potassium Salt | Substrate for firefly luciferase. Must be sterile, formulated for consistent bioavailability in vivo. |
| Gadolinium-Based Contrast Agent (e.g., Gd-DOTA) | Shortens T1 relaxation time for MRI, highlighting areas of BBB breakdown in T1-weighted scans. |
| Anesthetic System (Isoflurane/O₂) | Allows for prolonged, stable anesthesia compatible with both BLI (in imaging box) and MRI (in scanner). |
| Multimodal Fiduciary Markers | Contain dyes/agents visible in both optical and MR images. Critical for accurate 3D data co-registration. |
| Imaging-Compatible Animal Holder | A stereotactic or customized bed that secures the animal for sequential BLI and MRI without repositioning. |
| Image Co-registration Software (e.g., AMIRA, 3D Slicer, Living Image Module) | Software platform to spatially align and fuse 3D BLI and MRI datasets for direct comparison and analysis. |
Conclusion
BLI and MRI are not mutually exclusive but complementary pillars in the preclinical imaging toolkit for neuroinflammation. BLI offers unparalleled sensitivity for tracking specific cellular processes and therapeutic cells longitudinally with high throughput, while MRI provides unmatched anatomical context, deep-tissue penetration, and multi-parametric quantitative biomarkers of disease burden. The optimal choice hinges on the specific research question, balancing the need for cellular specificity against anatomical detail. Future directions point toward the increased use of multimodal imaging, the development of novel MRI-detectable and bioluminescent probes targeting specific immune pathways, and the refinement of analysis pipelines to extract more biologically meaningful data. For drug development, this integration is crucial for establishing pharmacodynamic biomarkers, validating mechanism of action, and accelerating the translation of promising therapies from bench to bedside.