Chronic Low-Grade Inflammation in Metabolic Syndrome: Molecular Mechanisms, Biomarkers, and Novel Therapeutic Targeting
This article provides a comprehensive analysis of the pivotal role chronic low-grade inflammation plays in the pathogenesis and progression of metabolic syndrome (MetS).
Chronic Low-Grade Inflammation in Metabolic Syndrome: Molecular Mechanisms, Biomarkers, and Novel Therapeutic Targeting
Abstract
This article provides a comprehensive analysis of the pivotal role chronic low-grade inflammation plays in the pathogenesis and progression of metabolic syndrome (MetS). Targeting researchers and drug development professionals, it synthesizes foundational knowledge on key molecular drivers, including inflammasome activation, adipokine dysregulation, and mitochondrial dysfunction. It further explores advanced methodological approaches for detecting inflammatory biomarkers, critically examines current and emerging anti-inflammatory therapeutic strategies, and offers a comparative validation of these interventions. The review aims to bridge fundamental research with clinical application, highlighting promising targets for disrupting the inflammatory cascade in MetS.
The Inflammatory Engine of Metabolic Syndrome: Core Mechanisms and Pathways
Defining the Low-Grade Inflammatory State in MetS
Low-grade chronic inflammation is a fundamental pathological process underlying metabolic syndrome (MetS), serving as a critical link between its clinical components and severe complications, including cardiovascular disease (CVD) and type 2 diabetes mellitus (T2DM) [1] [2]. This persistent, subacute inflammatory state is characterized by a measurable increase in circulating pro-inflammatory mediators and immune cell activation, without the classic signs of acute inflammation [3]. Understanding its precise definition, mechanisms, and measurement is essential for researchers and drug development professionals aiming to develop targeted therapeutic interventions.
The significance of this inflammatory state extends beyond mere association to direct causation. Research demonstrates that low-grade inflammation actively contributes to the development of insulin resistance, endothelial dysfunction, and atherosclerosis—core pathological features of MetS [1] [4]. This whitepaper provides a comprehensive technical guide to defining, measuring, and understanding the low-grade inflammatory state in metabolic syndrome, with specific focus on mechanistic insights, standardized assessment protocols, and research applications.
Pathophysiological Mechanisms of Low-Grade Inflammation in MetS
Adipose Tissue as an Inflammatory Organ
The expansion of adipose tissue, particularly visceral fat, initiates the inflammatory cascade in MetS. Hypertrophic adipocytes secrete numerous pro-inflammatory cytokines and chemokines, including tumor necrosis factor-alpha (TNF-α), interleukin-6 (IL-6), interleukin-1β (IL-1β), and monocyte chemoattractant protein-1 (MCP-1) [5] [3]. This process creates a pro-inflammatory milieu that disrupts insulin signaling in peripheral tissues through autocrine and paracrine pathways, establishing a direct link between inflammation and insulin resistance (IR) [5].
Free fatty acids (FFAs) released by expanded adipose tissue further promote insulin resistance and inhibit insulin secretion from pancreatic beta cells [1]. These FFAs inhibit glucose uptake in skeletal muscles while increasing hepatic gluconeogenesis and lipid synthesis through protein kinase induction [1]. The combined effects of insulin resistance and elevated FFAs contribute significantly to hypertension, prothrombotic state, and sustained chronic inflammation [1].
Inflammatory Signaling Pathways
Multiple molecular pathways sustain the chronic inflammatory state in MetS. The nuclear factor kappa B (NF-κB) pathway is activated under hyperglycemic and oxidative stress conditions, contributing to aggravated inflammation by regulating inflammatory gene expression and enhancing endothelial dysfunction [6] [3]. Toll-like receptors (TLRs), particularly TLR4, recognize endogenous ligands released from damaged tissues and activate downstream inflammatory signaling [6] [3].
The involvement of macrophages in MetS-related inflammation is particularly crucial. In adipose tissue, macrophages switch from an anti-inflammatory M2 phenotype to a pro-inflammatory M1 state, secreting large quantities of TNF-α, IL-6, and other inflammatory mediators [3]. This transition creates a vicious cycle of increasing inflammation and metabolic dysfunction.
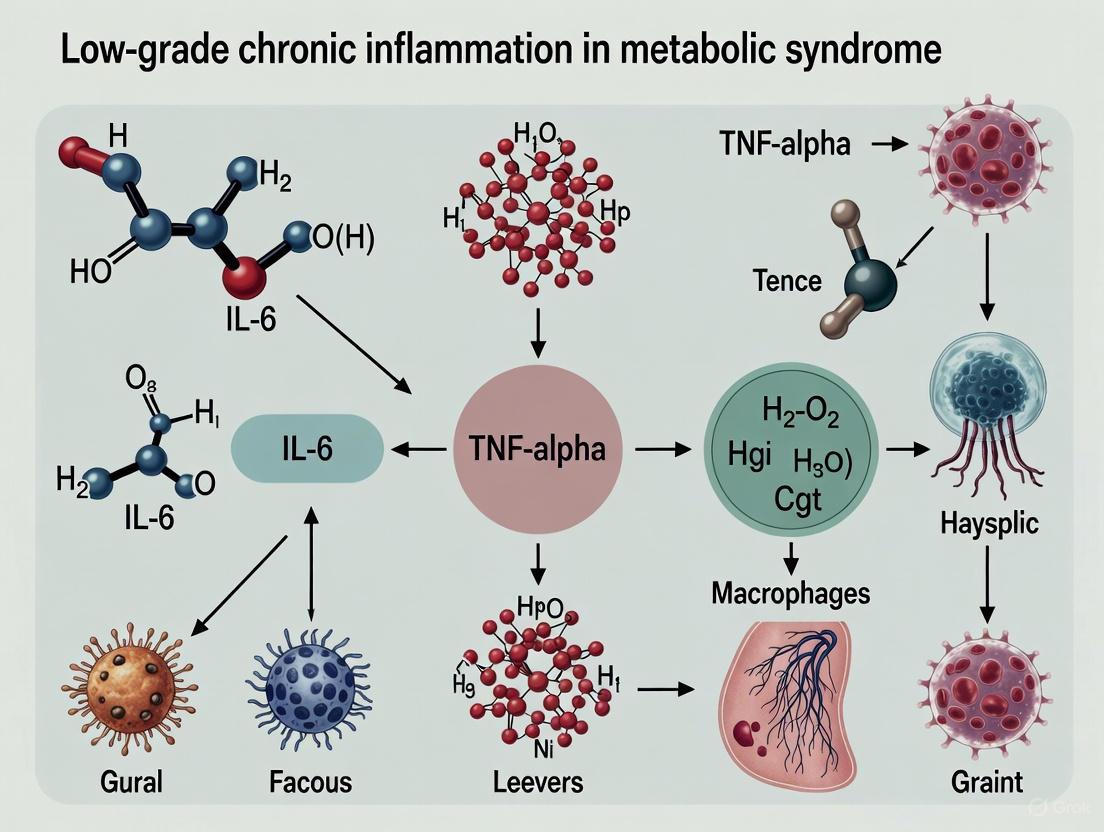
Figure 1: Inflammatory Pathways in Metabolic Syndrome
Systemic Consequences and Clinical Implications
The chronic inflammatory state in MetS adversely impacts multiple organ systems. Insulin resistance causes microvascular damage, predisposing patients to endothelial dysfunction, increased vascular resistance, hypertension, and vessel wall inflammation [1]. Endothelial damage disrupts homeostasis, promoting atherosclerotic disease and hypertension development [1].
The accumulated effects of endothelial dysfunction and hypertension due to metabolic syndrome can result in ischemic heart disease [1]. Endothelial dysfunction from increased levels of plasminogen activator inhibitor-1 and adipokines causes thrombogenicity, while hypertension increases vascular resistance—both processes contributing to coronary artery disease development [1]. Dyslipidemia associated with MetS, particularly elevated triglycerides and reduced HDL cholesterol, drives the atherosclerotic process, leading to symptomatic ischemic heart disease [1] [2].
Biomarkers and Composite Indices for Assessing Low-Grade Inflammation
Individual Inflammatory Biomarkers
Several individual biomarkers have established utility in quantifying the low-grade inflammatory state in MetS. The most consistently associated markers include:
C-reactive protein (CRP), produced by the liver in response to IL-6 stimulation, remains one of the most widely measured inflammatory markers in MetS research and clinical practice [5] [3]. Elevated CRP levels (>3 mg/L) indicate systemic inflammation and strongly correlate with cardiovascular risk [3].
Cytokines and Chemokines including TNF-α, IL-6, IL-1β, and MCP-1 are directly involved in the pathogenesis of insulin resistance and MetS [5] [3]. These molecules are primarily secreted by adipose tissue and infiltrating macrophages, creating autocrine and paracrine inflammatory signaling loops.
Cellular Inflammation Markers including leukocyte count, neutrophil count, and neutrophil-to-lymphocyte ratio (NLR) provide measures of innate immune system activation [5] [4]. These markers are easily obtainable from routine complete blood count (CBC) tests and show consistent associations with MetS components and severity.
Composite Inflammation Indices
Composite indices integrate multiple inflammatory markers to provide a more comprehensive assessment of the low-grade inflammatory state. The most significant indices for MetS research include:
INFLA-Score: This composite score incorporates four biomarkers: CRP, white blood cell (WBC) count, platelet count, and neutrophil-to-lymphocyte ratio (NLR) [5]. The INFLA-score is calculated by assigning values from -4 to +4 based on decile ranks of each component, with the total score ranging from -16 to +16 [5]. Higher scores indicate more pronounced low-grade chronic inflammation.
Advanced Lung Cancer Inflammation Index (ALI): Originally developed for cancer prognosis, ALI has demonstrated significant utility in MetS research. The formula incorporates nutritional and inflammatory parameters: ALI = (Body Mass Index × Albumin) / NLR [7]. Lower ALI values reflect greater inflammatory burden and are associated with increased mortality risk in MetS populations [7].
Table 1: Composite Indices for Low-Grade Inflammation Assessment in MetS
| Index Name | Components | Calculation Formula | Interpretation | Association with MetS |
|---|---|---|---|---|
| INFLA-Score [5] | CRP, WBC, Platelets, NLR | Decile-based scoring (-4 to +4 per component) | Range: -16 to +16Higher score = higher inflammation | OR = 1.08 per unit increase (95% CI: 1.07-1.10)Q4 vs Q1: OR = 3.58 for MetS |
| ALI [7] | BMI, Albumin, Neutrophils, Lymphocytes | (BMI × Albumin) / NLR | Lower values = higher inflammation/mortality risk | L-shaped association with CV mortalityInflection point at 106.24 |
| NLR [7] | Neutrophils, Lymphocytes | Neutrophils / Lymphocytes | Higher ratio = greater inflammatory state | Associated with atherosclerosis in MetS [4] |
| NPAR [7] | Neutrophils, Albumin | Neutrophils / Albumin | Higher ratio = greater inflammatory burden | Predictive of mortality in CMS populations |
Quantitative Relationships Between Inflammation and MetS
Strong epidemiological evidence supports the relationship between inflammatory markers and MetS. A recent study of 1,758 shift workers found that those with higher INFLA-score had significantly greater likelihood of developing MetS (OR = 1.08, 95% CI: 1.07-1.10) [5]. In quartile analyses, participants in the highest INFLA-score quartile had 3.58 times higher risk of MetS compared to those in the lowest quartile [5].
Research involving 6,735 participants for subclinical atherosclerosis found that neutrophils (a marker of inflammation) were independently associated with atherosclerosis (aOR: 1.08, 95% CI: 1.03-1.14), while obesity alone was not after adjusting for metabolic abnormalities and inflammation [4]. This highlights the primacy of inflammation in driving MetS complications.
Analysis of NHANES data including 5,969 participants with MetS revealed distinct mortality patterns based on inflammatory status. The relationship between ALI and mortality demonstrated an L-shaped curve for cardiovascular mortality, with an inflection point at 106.24, below which risk increased dramatically [7].
Standardized Experimental Protocols for Inflammation Assessment
INFLA-Score Determination Protocol
Sample Collection and Handling:
- Collect fasting blood samples in the morning after a 9-hour minimum fast
- Use EDTA tubes for complete blood count analysis
- Use serum separation tubes for CRP analysis
- Process samples within 2 hours of collection for optimal results [5]
Laboratory Analysis:
- Perform complete blood count using automated hematology analyzer (e.g., Sysmex XN-1000, Coulter DxH 800 analyzer) [5] [4]
- Measure CRP using high-sensitivity (hs-CRP) immunoassay
- Ensure all analyses follow standardized laboratory protocols with appropriate quality controls
Calculation Method:
- For each component (CRP, WBC, platelets, NLR), determine decile ranks within the study population
- Assign scores based on decile position: lowest deciles (1-4) receive negative scores (-4 to -1), highest deciles (7-10) receive positive scores (+1 to +4)
- Sum individual component scores for final INFLA-score (range: -16 to +16) [5]
Quality Assurance:
- Exclude individuals with acute infection (CRP > 10 mg/L) [8]
- Standardize sampling conditions (time of day, fasting status)
- Implement batch analysis to minimize inter-assay variability
Peripheral Blood Immune Profiling Protocol
Subject Selection Criteria:
- Include participants meeting standardized MetS criteria (e.g., NCEP ATP III)
- Exclude confounding conditions: acute/chronic infection, inflammatory/autoimmune diseases, recent surgery/trauma (<6 weeks), active malignancy, immunosuppressive medication use [8]
- Consider sex and age matching due to their significant impact on immune parameters [8]
Sample Processing for Immune Phenotyping:
- Collect blood in sodium heparin or EDTA tubes
- Isolate peripheral blood mononuclear cells (PBMCs) using density gradient centrifugation (Ficoll-Paque) within 4 hours of collection
- Cryopreserve cells in liquid nitrogen using controlled-rate freezing
- For flow cytometry, use fresh samples processed within 24 hours
Flow Cytometry Panel Design:
- Include markers for innate immune cells: CD14+ (monocytes), CD15+ (neutrophils), CD56+ (NK cells)
- Include adaptive immune markers: CD3+ (T cells), CD4+ (helper T cells), CD8+ (cytotoxic T cells), CD19+ (B cells)
- Incorporate activation markers: CD38, HLA-DR, CD69
- Analyze using standardized gating strategies and fluorescence minus one (FMO) controls
Data Analysis and Interpretation:
- Calculate absolute cell counts using dual-platform approach
- Determine cell ratios (NLR, lymphocyte-to-monocyte ratio)
- Compare to healthy control population with appropriate demographic matching
- Apply multivariate analysis to adjust for potential confounders
Figure 2: Experimental Workflow for Inflammation Assessment in MetS
Research Reagent Solutions and Essential Materials
Table 2: Essential Research Reagents for MetS Inflammation Studies
| Category | Reagent/Material | Specification | Research Application |
|---|---|---|---|
| Sample Collection | EDTA Blood Collection Tubes | 3mL, 6mL, 10mL | Complete blood count analysis |
| Serum Separator Tubes | 3mL, 6mL, 10mL | CRP and cytokine measurements | |
| Sodium Heparin Tubes | 3mL, 6mL | PBMC isolation for immune phenotyping | |
| Laboratory Analysis | Automated Hematology Analyzer | Sysmex XN-series, Coulter DxH series | Complete blood count with differential [5] [4] |
| High-Sensitivity CRP Assay | Immunoassay, immunoturbidimetric | Quantification of low-grade inflammation | |
| Flow Cytometry Antibodies | CD14, CD15, CD3, CD4, CD8, CD19, CD56 | Immune cell phenotyping [8] | |
| Cell Isolation | Ficoll-Paque PLUS | Density: 1.077 g/mL | PBMC isolation from whole blood |
| Cryopreservation Media | 10% DMSO, 90% FBS | Long-term storage of immune cells | |
| Specialized Assays | Multiplex Cytokine Panels | Luminex-based, electrochemiluminescence | Simultaneous measurement of multiple cytokines |
| ELISA Kits | TNF-α, IL-6, IL-1β, adiponectin | Specific cytokine quantification |
Methodological Considerations and Technical Challenges
Pre-analytical Variables
Timing and Conditions: Diurnal variations significantly affect inflammatory markers, particularly cortisol and certain cytokines. Standardize collection times (typically morning) and participant fasting status (minimum 9 hours) [5]. Recent physical activity, stress, and sleep patterns can transiently alter inflammatory parameters—implement appropriate washout periods and standardized resting protocols.
Sample Processing: Delayed processing (>4 hours) significantly affects immune cell viability and function [8]. Temperature fluctuations during transport and processing can alter cytokine levels and cell surface marker expression. Implement standardized standard operating procedures (SOPs) across all collection sites.
Analytical Considerations
Platform Selection: Different automated hematology analyzers may yield systematically different absolute cell counts [5] [4]. Use the same platform throughout a study or implement cross-platform standardization. For cytokine measurements, multiplex platforms offer comprehensive profiling but may have different sensitivity and dynamic range compared to ELISAs.
Standardization: Implement internal quality controls and participate in external proficiency testing programs. Use standardized calibration materials traceable to international reference standards, particularly for CRP measurements.
Data Interpretation Challenges
Reference Ranges: Establish study-specific reference ranges based on carefully characterized control populations, accounting for age, sex, and ethnic variations [8]. The INFLA-score is inherently population-referenced, requiring appropriate comparator groups [5].
Confounding Factors: Numerous medications impact inflammatory parameters, including statins, metformin, antihypertensive drugs, and anti-inflammatory agents [8]. Document and account for medication use in analyses. Subclinical infections, dental health, and gut microbiome variations can all influence systemic inflammation markers.
The low-grade inflammatory state in MetS represents a critical pathological process with well-defined characteristics, measurement approaches, and technical requirements for rigorous investigation. Composite indices like the INFLA-score and ALI provide robust tools for quantifying this inflammatory state, integrating multiple complementary biomarkers into single metrics that capture the multidimensional nature of chronic inflammation in metabolic disease.
Standardization of protocols—from participant selection through sample processing to analytical methods—is essential for generating comparable, reproducible data across research centers. Attention to pre-analytical variables, appropriate control populations, and comprehensive documentation of potential confounders strengthens the validity of research findings.
As drug development increasingly targets inflammatory pathways in MetS, precise definition and measurement of this low-grade inflammatory state will be crucial for identifying responsive patient populations, validating target engagement, and demonstrating therapeutic efficacy. The frameworks and methodologies outlined in this technical guide provide foundation for advancing these research objectives.
Inflammasomes are cytosolic multiprotein complexes that serve as critical regulators of the innate immune system by responding to pathogenic threats and sterile injury. The NOD-, LRR- and pyrin domain-containing protein 3 (NLRP3) inflammasome is the most extensively characterized of these complexes and functions as a molecular platform for caspase-1 activation, leading to the maturation and secretion of pro-inflammatory cytokines interleukin-1β (IL-1β) and IL-18, while inducing an inflammatory form of cell death known as pyroptosis [9] [10]. The NLRP3-IL-1β axis represents a key signaling pathway that connects cellular stress to systemic inflammation, particularly in the context of metabolic syndrome—a cluster of conditions including obesity, insulin resistance, and dyslipidemia that significantly increases cardiovascular risk [11] [9]. This technical guide examines the molecular mechanisms governing NLRP3 inflammasome activation, its role as a driver of low-grade chronic inflammation in metabolic syndrome, and emerging therapeutic strategies targeting this pathway.
Molecular Mechanisms of NLRP3 Inflammasome Activation
Inflammasome Structure and Components
The NLRP3 inflammasome consists of three core components: the NLRP3 sensor protein, the apoptosis-associated speck-like protein containing a CARD (ASC) adaptor, and procaspase-1 [12]. The NLRP3 protein contains three critical domains: a central NACHT domain that facilitates ATP-dependent oligomerization, C-terminal leucine-rich repeats (LRRs) that sense activating stimuli, and an N-terminal pyrin domain (PYD) that mediates protein-protein interactions [9]. Upon activation, NLRP3 oligomerizes and recruits ASC through PYD-PYD interactions, which then recruits procaspase-1 via CARD-CARD interactions, forming the functional inflammasome complex [9] [10].
Two-Signal Activation Mechanism
NLRP3 inflammasome activation requires two distinct signals [12]:
- Signal 1 (Priming): Pattern recognition receptors (PRRs) such as Toll-like receptors (TLRs) recognize pathogen-associated molecular patterns (PAMPs) or damage-associated molecular patterns (DAMPs), activating the NF-κB signaling pathway. This leads to transcriptional upregulation of NLRP3, pro-IL-1β, and pro-IL-18 [9] [12].
- Signal 2 (Activation): Diverse stimuli including extracellular ATP, pore-forming toxins, crystalline substances, and metabolic danger signals trigger NLRP3 oligomerization and inflammasome assembly, resulting in caspase-1 activation [9] [12].
Activated caspase-1 then cleaves pro-IL-1β and pro-IL-18 into their mature, biologically active forms and cleaves gasdermin D (GSDMD), generating N-terminal fragments that form plasma membrane pores, facilitating cytokine release and initiating pyroptosis [9] [13].
Table 1: NLRP3 Activators in Metabolic Syndrome Context
| Activator Category | Specific Stimuli | Relevance to Metabolic Syndrome |
|---|---|---|
| Crystalline Materials | Cholesterol crystals, monosodium urate crystals | Atherosclerosis development, hyperuricemia |
| Ionic Fluxes | K+ efflux, Ca2+ signaling, Cl- efflux | Cellular stress in hyperglycemic conditions |
| Metabolic Stressors | Saturated fatty acids (palmitate), ceramides, mitochondrial ROS | Obesity, lipotoxicity, insulin resistance |
| DAMPs | Extracellular ATP, HMGB1, cell-free DNA | Tissue injury, chronic inflammation |
| Organelle Dysfunction | Mitochondrial damage, lysosomal disruption, Golgi stress | Oxidative stress, impaired autophagy |
Regulatory Mechanisms
Multiple regulatory mechanisms control NLRP3 inflammasome activation to prevent excessive inflammation:
- Post-translational modifications: Polyubiquitination maintains NLRP3 in an inactive state, while deubiquitination by BRCC3 enables activation [10].
- Intracellular trafficking: NLRP3 translocates from the trans-Golgi network to the microtubule-organizing center along microtubules via dynein and histone deacetylase 6 (HDAC6) [10].
- Ionic fluxes: Potassium efflux represents a common trigger for NLRP3 activation [10].
- Metabolic regulation: Hypoxic conditions and immunometabolic imbalances lower the threshold for inflammasome assembly [10].
The NLRP3-IL-1β Axis in Metabolic Syndrome
Extracellular Vesicle-Mediated Inflammation
Recent evidence demonstrates that NLRP3 can be conveyed via extracellular vesicles (EVs) from metabolic syndrome patients, actively participating in atherosclerosis development [11]. Circulating large EVs carrying NLRP3 correlate with metabolic risk factors associated with obesity and insulin resistance. These EVs from metabolic syndrome patients increase endothelial permeability, monocyte transmigration, smooth muscle cell migration, and secretion of pro-inflammatory molecules by monocyte/macrophages [11]. EVs isolated from advanced human atherosclerotic plaques show accumulation of NLRP3-carrying vesicles, implicating them in vascular inflammation and remodeling [11].
Lipid-Induced Inflammasome Activation
Obesity creates a pathological environment characterized by elevated circulating fatty acids that directly activate the NLRP3 inflammasome. In nucleus pulposus cells, saturated fatty acids like palmitic acid induce NLRP3 inflammasome activation through mitochondrial damage, resulting in mitochondrial double-stranded RNA (mt-dsRNA) release and double-stranded RNA-dependent protein kinase (PKR) activation [14]. This mt-dsRNA-PKR axis represents a novel mechanism linking metabolic stress to inflammasome-driven inflammation in obesity-related conditions, including intervertebral disc degeneration [14].
Systemic Low-Grade Inflammation
In metabolic syndrome, chronic activation of the NLRP3-IL-1β axis creates a state of low-grade systemic inflammation that contributes to insulin resistance, endothelial dysfunction, and cardiovascular complications. IL-1β interferes with insulin signaling in peripheral tissues, promotes lipolysis, and impairs pancreatic β-cell function [9]. The resulting hyperglycemia and dyslipidemia further activate NLRP3, creating a vicious cycle of metabolic dysfunction and inflammation [9].
Table 2: Evidence Linking NLRP3-IL-1β Axis to Metabolic Syndrome Components
| Metabolic Syndrome Component | NLRP3-IL-1β Involvement | Experimental Evidence |
|---|---|---|
| Obesity/Adipose Tissue Inflammation | Macrophage infiltration, adipocyte pyroptosis, reduced adiponectin | Elevated IL-1β in adipose tissue; caspase-1 activation in adipocytes |
| Insulin Resistance | IL-1β-mediated impairment of insulin signaling pathways | NLRP3 inhibition improves insulin sensitivity in rodent models |
| Dyslipidemia | Cholesterol crystal formation, fatty acid-induced activation | LDL promotes NLRP3 activation; cholesterol depletion inhibits inflammasome |
| Atherosclerosis | Endothelial activation, vascular smooth muscle proliferation, plaque instability | NLRP3 detected in human atherosclerotic plaques; colocalization with IL-1β |
| Hypertension | Vascular inflammation, oxidative stress, endothelial dysfunction | NLRP3 deficiency attenuates angiotensin II-induced hypertension |
Experimental Models and Methodologies
In Vitro Models for NLRP3 Activation
Primary Cell Culture of Nucleus Pulposus Cells [14]:
- Cell Isolation: Mouse nucleus pulposus cells isolated from intervertebral discs
- Stimulation: Treatment with 0.5 mmol/L palmitic acid (PA) for 6 hours to mimic lipid overload
- Pharmacological Inhibition: Pre-treatment with PKR inhibitor 2-Aminopurine (2-AP, 0.5 mmol/L) for 60 minutes
- Analysis: Western blot for NLRP3, caspase-1, IL-1β; ELISA for cytokine secretion; immunofluorescence for ASC speck formation
Macrophage NLRP3 Activation Model [9] [10]:
- Cell Lines: Primary human monocytes or murine bone marrow-derived macrophages
- Priming Signal: LPS (100-500 ng/mL) for 3-4 hours
- Activation Signals: ATP (5 mM, 30 min), nigericin (10 μM, 1 hr), monosodium urate crystals (150 μg/mL, 6 hr)
- Readouts: Caspase-1 activity assays, IL-1β secretion by ELISA, LDH release for pyroptosis, Western blot for GSDMD cleavage
In Vivo Models of Metabolic Syndrome
High-Fat Diet Mouse Model [14]:
- Animals: C57BL/6 mice or PKR-deficient (PKR-/-) mice
- Dietary Regimen: High-fat diet (60% kcal from fat) or regular diet starting at 3 weeks of age
- Duration: 6 months (early/medium-term effects) or 14 months (long-term effects)
- Metformin Intervention: Dissolved in drinking water at 205 mg/kg body weight daily for 12 weeks
- Tissue Analysis: Histological assessment of tissues (safranin-O/fast green staining), immunohistochemistry for IL-1β, caspase-1, collagen-II, aggrecan
Assessment of Vascular Inflammation [11]:
- EV Isolation: Circulating large and small EVs isolated from human metabolic syndrome patients
- Functional Assays: Endothelial permeability measurements, monocyte transmigration assays, smooth muscle cell proliferation
- Pharmacological Inhibition: NLRP3 inflammasome inhibitors (MCC950, dapansutrile) to confirm pathway specificity
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for NLRP3-IL-1β Axis Investigation
| Reagent Category | Specific Examples | Application/Function |
|---|---|---|
| NLRP3 Activators | ATP, nigericin, monosodium urate crystals, palmitic acid, cholesterol crystals | Provide Signal 2 for inflammasome activation in experimental models |
| NLRP3 Inhibitors | MCC950, dapansutrile (OLT1177), INF39, thiolutin (BRCC3 inhibitor) | Pharmacological tools to establish NLRP3-specific mechanisms; therapeutic candidates |
| Cytokine Detection | ELISA kits for IL-1β, IL-18; Luminex multiplex assays; Western blot antibodies | Quantify inflammasome activation and cytokine secretion |
| Cell Death Assays | LDH release assay, propidium iodide staining, SYTOX green uptake | Measure pyroptosis and cell membrane integrity |
| Molecular Biology Tools | siRNA for NLRP3, ASC, caspase-1; CRISPR/Cas9 for gene knockout; antibodies for NLRP3 components | Genetic manipulation and protein detection of inflammasome elements |
| Animal Models | NLRP3-deficient mice, ASC-deficient mice, high-fat diet models, ApoE-/- mice | In vivo validation of NLRP3 role in metabolic disease pathogenesis |
| LPA2 antagonist 1 | LPA2 antagonist 1, MF:C20H23Cl2N5O2S2, MW:500.5 g/mol | Chemical Reagent |
| Meclofenoxate Hydrochloride | Meclofenoxate Hydrochloride |
Therapeutic Targeting and Clinical Implications
Pharmacological Inhibition Strategies
Several targeted approaches have emerged for therapeutic inhibition of the NLRP3-IL-1β axis:
Direct NLRP3 Inhibitors:
- MCC950: Potent and selective NLRP3 inhibitor that blocks ASC oligomerization, though hepatotoxicity concerns have limited clinical development [10] [15].
- Dapansutrile (OLT1177): Oral NLRP3 inhibitor that demonstrated efficacy in reducing joint pain and inflammation in a Phase IIa trial for acute gout, with a favorable safety profile [15].
- DFV890: Investigational NLRP3 inhibitor entering early-phase clinical testing for knee osteoarthritis (NCT04886258) [15].
Upstream Pathway Modulators:
- Thiolutin: Inhibits BRCC3 deubiquitinase activity, preventing NLRP3 activation by maintaining its ubiquitinated, inactive state [10].
- Metformin: Attenuates mitochondrial damage and PKR activation, reducing NLRP3 inflammasome activation in nucleus pulposus cells [14].
Cytokine-Targeted Therapies:
- IL-1 Receptor Antagonist (Anakinra): Recombinant version of naturally occurring IL-1Ra that blocks IL-1 signaling.
- Anti-IL-1β Monoclonal Antibodies (Canakinumab): Directly neutralizes IL-1β, shown to reduce cardiovascular events in the CANTOS trial [11].
Non-Pharmacological Modulation
Exercise Interventions: Moderate-intensity aerobic and resistance exercise (≥8 weeks) significantly reduces NLRP3 gene expression, caspase-1 activation, and IL-1β levels across diverse populations [12]. In contrast, high-intensity aerobic exercise can upregulate NLRP3 components, suggesting intensity-dependent effects [12]. Combined aerobic and resistance training appears particularly effective for reducing NLRP3-driven inflammation in metabolic syndrome [12].
Nutritional Approaches:
- Dietary fiber: Metabolized by gut microbiota to short-chain fatty acids that promote regulatory T cells and inhibit NF-κB signaling [16].
- Flavonoids (anthocyanins, quercetin): Decrease NF-κB expression and pro-inflammatory cytokine production [16].
- Vitamin D: Exhibits anti-inflammatory properties by decreasing TLR expression and reactive oxygen species [16].
The NLRP3-IL-1β axis represents a central driver of low-grade chronic inflammation in metabolic syndrome, serving as a critical interface between metabolic dysregulation and immune activation. Extracellular vesicles carrying NLRP3 from metabolic syndrome patients propagate vascular inflammation and contribute to atherosclerosis development, revealing a novel mechanism of intercellular communication in metabolic disease [11]. The mt-dsRNA-PKR activation pathway provides insight into how lipid overload translates into inflammasome activation through mitochondrial damage [14].
Future research should focus on tissue-specific regulation of NLRP3, the role of novel post-translational modifications, and the development of safer, more specific NLRP3 inhibitors for long-term use in chronic metabolic diseases. Additionally, understanding how social determinants of health influence NLRP3 activation may help address disparities in metabolic syndrome prevalence and complications [16]. As our knowledge of inflammasome biology expands, targeting the NLRP3-IL-1β axis holds significant promise for interrupting the vicious cycle of inflammation and metabolic dysfunction in metabolic syndrome.
White adipose tissue (WAT) is no longer considered a passive fat storage depot but a highly active endocrine organ that expresses and secretes a vast array of bioactive molecules called adipokines [17] [18] [19]. These include peptide hormones (adipokines), bioactive lipids (lipokines), and exosomal microRNAs with both local (paracrine) and systemic (endocrine) effects on distant organs including the brain, pancreatic β-cells, liver, skeletal muscle, and cardiovascular system [17]. In healthy states, WAT secretes endocrine factors that maintain organ functions and metabolic homeostasis through precisely regulated signaling networks [17]. However, in obesity, this delicate balance is disrupted, leading to a chronic low-grade inflammatory state characterized by altered secretion of adipokines and pro-inflammatory cytokines that contribute significantly to the pathogenesis of metabolic syndrome and its associated complications [17] [20] [19].
The core of this dysfunction lies in the pathological remodeling of adipose tissue during obesity. As adipocytes undergo hypertrophy and hyperplasia to store excess energy, they generate a plethora of intrinsic signals (e.g., adipocyte death, hypoxia, and mechanical stress) capable of initiating and sustaining an inflammatory response [20]. This creates a self-perpetuating cycle wherein inflamed adipose tissue secretes excessive pro-inflammatory mediators that further exacerbate local and systemic metabolic disturbances, establishing a crucial link between obesity and insulin resistance [20] [21].
The Shift to Pro-Inflammatory Secretion in Obesity
Immune Cell Recruitment and Phenotypic Switching
The healthy adipose tissue microenvironment is maintained by a delicate balance between pro-inflammatory and anti-inflammatory signals, with a predominance of alternatively activated M2 macrophages that secrete anti-inflammatory cytokines like IL-10 [20] [19]. However, obesity triggers a dramatic shift in both the quantity and quality of immune cells within adipose tissue [20]. There is a substantial infiltration of circulating monocytes that differentiate into pro-inflammatory macrophages, alongside a phenotypic switch of resident macrophages from the M2 to the classically activated M1 state [19]. These M1 macrophages aggregate around dead adipocytes, forming characteristic crown-like structures, and become the primary source of pro-inflammatory cytokines within obese adipose tissue [20].
This immune dysregulation extends beyond macrophages to include increased infiltration and activation of other innate and adaptive immune cells. Dendritic cells, mast cells, neutrophils, B cells, and T cells all contribute to the chronic inflammatory milieu by producing additional inflammatory mediators that further amplify the inflammatory cascade [20]. The cumulative effect is a transformation of adipose tissue into a chronically inflamed tissue that systemically influences metabolic homeostasis.
Altered Adipokine Secretion Profile
The dysfunctional adipose tissue in obesity exhibits a marked imbalance in adipokine production, characterized by elevated secretion of pro-inflammatory factors and reduced production of beneficial anti-inflammatory adipokines [18] [19]. This shift creates an endocrine environment that promotes insulin resistance and metabolic dysfunction.
Table 1: Adipokine Dysregulation in Metabolic Syndrome
| Adipokine | Change in Obesity | Primary Metabolic Effects | Impact on Insulin Sensitivity |
|---|---|---|---|
| Leptin | Increased | Appetite regulation, fatty acid oxidation, sympathetic activation | Improves via weight loss (central effect), but leptin resistance develops [18] |
| Adiponectin | Decreased | Improves insulin sensitivity, reduces foam cell formation, anti-inflammatory | Strong improvement [18] [22] |
| Resistin | Increased | Promotes hepatic gluconeogenesis, increases lipolysis | Decreases sensitivity [18] [19] |
| Visfatin | Increased | Mimics insulin, promotes cholesterol accumulation in macrophages | Decreases sensitivity [18] |
| PAI-1 | Increased | Promotes liver steatosis, increases serum cholesterol | Decreases sensitivity [18] |
The ratio of leptin to adiponectin has emerged as a particularly sensitive biomarker of adipose tissue dysfunction and cardiovascular risk profile, with higher ratios strongly correlating with metabolic syndrome components [19]. This altered adipokine secretion profile works in concert with the increased production of pro-inflammatory cytokines to establish the chronic inflammatory state that underpins metabolic syndrome.
Key Pro-inflammatory Cytokines: Mechanisms and Synergistic Actions
Tumor Necrosis Factor-α (TNF-α)
TNF-α was the first pro-inflammatory cytokine definitively linked to obesity-associated insulin resistance [20]. Produced by both adipocytes and adipose tissue macrophages in obesity, TNF-α contributes to insulin resistance through multiple mechanisms. It impairs insulin signaling by serine phosphorylation of insulin receptor substrate-1 (IRS-1), which inhibits normal insulin signal transduction [20] [23]. Additionally, TNF-α stimulates lipolysis in adipocytes, increasing circulating free fatty acids that further exacerbate systemic insulin resistance [23]. The critical role of TNF-α in metabolic dysfunction is supported by studies demonstrating that TNF-α neutralization in obese mice improves insulin sensitivity and glucose metabolism [20].
Interleukin-6 (IL-6)
Adipose tissue contributes significantly to circulating IL-6 levels, producing an estimated 10–35% of systemic IL-6 in resting individuals, with this contribution increasing with adiposity [24]. IL-6 levels are strongly correlated with adiposity, insulin resistance, and lipid abnormalities [24]. Mechanistically, IL-6 inhibits insulin signaling through suppression of insulin receptor tyrosine phosphorylation and downregulation of insulin receptor expression [23]. Furthermore, IL-6 contributes to dyslipidemia by inhibiting hepatic glycogen synthase while activating glycogen phosphorylase and lipolysis, ultimately increasing triglyceride production [24].
Interleukin-1β (IL-1β)
IL-1β plays a dual role in adipose tissue physiology and dysfunction. In the postprandial state, transient IL-1β surges actually promote healthy adipose tissue remodeling by stimulating adipogenesis of precursor cells, thereby facilitating hyperplastic (rather than hypertrophic) expansion [25]. However, in chronic obesity, persistently elevated IL-1β levels contribute to metabolic dysfunction by inducing peripheral insulin resistance and promoting β-cell dysfunction and apoptosis in the pancreas [25]. IL-1β also exerts direct inflammatory effects on adipocytes, further amplifying the pro-inflammatory cascade.
Cytokine Cooperativity in Inflammation
Recent research has revealed that these pro-inflammatory cytokines do not act in isolation but exhibit significant cooperativity in amplifying adipose tissue inflammation. Studies demonstrate that IL-1β and TNF-α together cooperatively enhance IL-6 expression in adipocytes through synergistic effects on CREB binding and histone H3K14 acetylation at the IL-6 promoter region [24]. This cooperative interaction results in significantly greater IL-6 production than would be expected from the additive effects of each cytokine alone, creating an amplification loop that drives chronic inflammation [24].
Table 2: Pro-inflammatory Cytokines in Adipose Tissue Dysfunction
| Cytokine | Primary Cellular Sources in AT | Signaling Pathways | Key Metabolic Consequences |
|---|---|---|---|
| TNF-α | Macrophages, adipocytes | JNK, NF-κB, IRS-1 serine phosphorylation | Insulin resistance, increased lipolysis, reduced adiponectin [20] [23] |
| IL-6 | Macrophages, adipocytes, stromal cells | JAK/STAT, SOCS3, suppress insulin receptor signaling | Hepatic insulin resistance, increased hepatic glucose production, dyslipidemia [24] [23] |
| IL-1β | Macrophages, adipocytes | IL-1R1/MyD88/NF-κB, NLRP3 inflammasome | β-cell dysfunction, insulin resistance, adipogenesis regulation [25] |
The following diagram illustrates the key signaling pathways through which these pro-inflammatory cytokines induce insulin resistance in target tissues:
Experimental Models and Methodologies
In Vitro Models of Adipocyte Biology
The 3T3-L1 murine cell line represents a cornerstone of adipobiology research, providing a standardized model for studying adipocyte differentiation and inflammatory responses [24]. The established differentiation protocol involves maintaining cells in Dulbecco's Modified Eagle Medium (DMEM) supplemented with 10% FBS, 2 mM glutamine, and 1% penicillin-streptomycin at 37°C in 5% CO₂ [24]. At confluence, adipogenesis is induced using a differentiation cocktail containing 5 μg/mL insulin, 0.25 μM dexamethasone, and 0.5 mM IBMX for 48 hours, followed by maintenance in DMEM with 10% FBS for additional differentiation periods [24]. For cytokine stimulation experiments, differentiated adipocytes are treated with specific pro-inflammatory cytokines (typically 10 ng/mL IL-1β, TNF-α, or combinations) to model inflammatory conditions [24].
Primary human adipocytes derived from subcutaneous and omental adipose tissues of both lean and obese individuals provide critical human-relevant data [24]. These cells are commercially available (e.g., ZenBio) and are maintained in specialized preadipocyte growth medium until 80% confluency, followed by differentiation using specific differentiation media for 10 days according to manufacturer protocols [24]. The use of primary cells from both lean and obese donors enables direct comparison of inflammatory responses across metabolic states.
Analytical Methods for Adipokine and Cytokine Assessment
Gene expression analysis typically involves RNA extraction using commercial kits (e.g., RNeasy Mini Kit, Qiagen), followed by cDNA synthesis and quantitative real-time PCR using TaqMan assays specific for target genes (e.g., IL-6, PPARγ, FABP4) with GAPDH as a common housekeeping gene [24]. The 2−ΔΔCT method is standard for calculating relative mRNA expression levels [24].
Protein secretion measurement employs enzyme-linked immunosorbent assays (ELISAs), with commercial kits available for quantitative detection of adipokines and cytokines (e.g., Quantikine ELISA Kits, R&D Systems) in cell culture supernatants or plasma samples [24]. These assays provide sensitive and specific quantification of protein levels, enabling correlation of gene expression with actual secretion.
Functional metabolic assays include glucose uptake measurements using radiolabeled tracers, assessment of insulin signaling through western blot analysis of phosphorylated Akt, and lipid metabolism analysis through Nile Red staining of intracellular lipid droplets [24] [25]. These functional assays provide critical links between inflammatory signaling and metabolic outcomes.
The following diagram illustrates a typical experimental workflow for studying cytokine effects on adipocytes:
Research Reagent Solutions
Table 3: Essential Research Reagents for Adipose Tissue Inflammation Studies
| Reagent Category | Specific Examples | Research Application | Key Functions |
|---|---|---|---|
| Cell Culture Models | 3T3-L1 cell line (ATCC), Primary human preadipocytes (ZenBio) | In vitro differentiation and inflammation studies | Provide standardized and human-relevant models for adipobiology [24] |
| Differentiation Reagents | Insulin, Dexamethasone, IBMX (3-isobutyl-1-methylxanthine) | Adipogenesis induction | Activate transcriptional program for adipocyte differentiation [24] |
| Cytokines & Recombinant Proteins | Recombinant IL-1β, TNF-α, IL-6 (Sigma, R&D Systems) | Cytokine stimulation experiments | Activate inflammatory signaling pathways in adipocytes [24] |
| Analysis Kits | RNeasy Mini Kit (Qiagen), TaqMan Gene Expression Assays, Quantikine ELISA Kits | Gene and protein expression quantification | Enable precise measurement of inflammatory mediators [24] |
| Signaling Inhibitors | Anacardic acid, Curcumin, Trichostatin A | Mechanistic studies | Target specific inflammatory pathways (e.g., histone acetylation) [24] |
Therapeutic Implications and Future Directions
The recognition of adipose tissue as a central player in metabolic inflammation has opened new therapeutic avenues for managing metabolic syndrome. Several strategic approaches have emerged:
Direct cytokine targeting represents a promising intervention strategy. The IL-1 receptor antagonist anakinra has shown potential in modulating WAT morphology and improving metabolic parameters in preclinical models [25]. Similarly, anti-TNF-α therapies, already established for autoimmune conditions, have demonstrated efficacy in improving insulin sensitivity in both animal models and human studies [20] [23]. However, the pleiotropic effects of these cytokines in normal physiology necessitate careful consideration of potential off-target effects.
Lifestyle interventions, particularly regular exercise, consistently demonstrate beneficial effects on adipose tissue inflammation. Exercise training modulates adipokine dysregulation in metabolic syndrome by reducing pro-inflammatory adipokines (e.g., resistin, visfatin) while increasing anti-inflammatory adipokines like adiponectin [22]. These effects are mediated through multiple mechanisms, including reduced visceral adiposity, decreased pro-inflammatory cytokine production, and induction of anti-inflammatory myokines from skeletal muscle that exert cross-talk with adipose tissue [22].
Future research directions should focus on developing more targeted approaches to modulate adipose tissue inflammation without compromising essential immune functions. This includes developing tissue-specific delivery systems for anti-inflammatory agents, identifying key upstream regulators of the inflammatory cascade, and exploring the potential of combination therapies that simultaneously target multiple aspects of adipose tissue dysfunction. Furthermore, personalized approaches based on individual patterns of adipokine secretion and genetic predispositions may enhance therapeutic efficacy while minimizing adverse effects.
The intricate relationship between adipose tissue dysfunction and chronic inflammation represents both a challenge and an opportunity for metabolic disease management. As our understanding of the endocrine functions of adipose tissue continues to evolve, so too will our ability to develop innovative strategies for combating metabolic syndrome and its associated complications.
The Interplay of Oxidative Stress and Mitochondrial Dysfunction in Fuelling Inflammation
The intricate crosstalk between oxidative stress and mitochondrial dysfunction forms a critical vicious cycle that perpetuates chronic low-grade inflammation, particularly in metabolic syndrome (MetS). This review delineates the molecular mechanisms through which mitochondrial-derived reactive oxygen species (ROS) activate inflammatory pathways, including NF-κB and NLRP3 inflammasome signaling, while inflammation simultaneously exacerbates mitochondrial impairment. Within the context of MetS, this self-reinforcing pathway contributes significantly to insulin resistance, endothelial dysfunction, and cardiovascular complications. We provide comprehensive experimental methodologies for investigating these mechanisms, current therapeutic strategies targeting this axis, and essential research tools for advancing drug discovery in this domain.
Mitochondria, the energy production centers in cells, have emerged as central hubs regulating oxidative stress, inflammation, and aging [26]. Their dysfunction induces an imbalance between oxidation and antioxidation, resulting in excessive reactive oxygen species (ROS) generation, which contributes to cell damage and death [26]. Mitochondria are crucial mediators in the occurrence and development of inflammation, with oxidative stress activating damage-associated molecular patterns (DAMPs), primarily mitochondrial DNA (mtDNA), and triggering inflammasome activation [26].
In metabolic syndrome, this interplay becomes particularly detrimental. MetS represents a cluster of metabolic risk factors including central obesity, dyslipidemia, hypertension, and insulin resistance [27] [2]. The link between MetS and its associated diseases is represented by oxidative stress and intracellular redox imbalance, both caused by persistent chronic inflammatory conditions [27]. Understanding the mechanistic basis of this relationship is essential for developing targeted therapies for MetS and its complications.
Molecular Mechanisms of the Oxidative Stress-Inflammation Axis
Mitochondrial Dysfunction and ROS Production
Mitochondrial ROS produced through the respiratory chain is the major source of cellular ROS [26]. The respiratory chain consists of complexes located in the mitochondrial membrane that transfer electrons to oxygen, with Complex I and Complex III being the main sites of ROS generation [26].
- Complex I: The oxidation of NADH produces electrons that are delivered to oxygen, producing superoxide anion (Oâ‚‚â») [26].
- Complex III: Molecular oxygen interacts with semiquinone at the Qo site, producing large amounts of Oâ‚‚â» [26].
- Other sites: Mitochondrial enzymes, including glycerol 3-phosphate dehydrogenase and electron transferring flavoprotein-Q oxidoreductase, also contribute to ROS production [26].
To counteract excessive ROS, mitochondria employ antioxidant systems including the glutathione (GSH) system, superoxide dismutase (SOD), catalase, and substances like melatonin [26]. In metabolic syndrome, this balance is disrupted, leading to oxidative damage.
ROS as Pro-Inflammatory Signaling Molecules
Reactive oxygen species serve dual roles as essential signaling molecules and mediators of cellular damage. They stimulate redox-sensitive transcription factors to express pro-inflammatory mediators [28].
- NF-κB Activation: ROS activate the NF-κB pathway by facilitating IκB kinase (IKK) complex-mediated phosphorylation and degradation of IκBα, leading to nuclear translocation of NF-κB dimers (p65/p50) and transcription of pro-inflammatory genes including TNF-α, IL-6, IL-1β, COX-2, and adhesion molecules [28].
- Inflammasome Activation: Mitochondrial dysfunction and ROS contribute to the activation of the NLRP3 inflammasome, leading to caspase-1 activation and maturation of IL-1β and IL-18 [26] [29].
- Additional Pathways: ROS also modulate other redox-sensitive transcription factors including HIF-1α, FOXO proteins, AP-1, and STAT3, further integrating oxidative stress with inflammatory responses [28].
Inflammatory Signaling-Induced Mitochondrial Dysfunction
This relationship is bidirectional, as inflammatory signals can exacerbate mitochondrial dysfunction:
- Cytokine Effects: Pro-inflammatory cytokines such as TNF-α and IL-1β can impair mitochondrial oxidative phosphorylation, reduce ATP production, and increase mitochondrial ROS generation [29].
- Metabolic Inflammation in Obesity: In obese adipose tissue, macrophage infiltration and polarization toward M1 phenotypes increase production of TNF-α, IL-6, and monocyte chemoattractant protein-1 (MCP-1) [30]. These cytokines induce insulin resistance and further promote mitochondrial oxidative stress [30] [29].
Table 1: Key Molecular Players in the Oxidative Stress-Mitochondrial Dysfunction-Inflammation Axis
| Component | Key Elements | Functional Role in the Axis |
|---|---|---|
| ROS Sources | Complex I & III, mitochondrial enzymes | Generate superoxide and Hâ‚‚Oâ‚‚, initiating oxidative stress |
| Antioxidant Systems | GSH system, SOD, catalase, peroxiredoxins | Scavenge excess ROS to maintain redox balance |
| Inflammatory Transcription Factors | NF-κB, AP-1, STAT3 | Activated by ROS, drive pro-inflammatory gene expression |
| Cytokines & Mediators | TNF-α, IL-6, IL-1β, MCP-1 | Propagate inflammatory signals, can impair mitochondrial function |
| Mitochondrial DAMPs | mtDNA, cardiolipin | Released upon damage, activate innate immune receptors (e.g., NLRP3) |
Experimental Approaches for Mechanistic Investigation
Assessing Mitochondrial Function and ROS Production
Protocol 1: High-Resolution Respirometry to Evaluate Mitochondrial Function
- Objective: To measure mitochondrial oxygen consumption rates (OCR) in cells or isolated mitochondria and assess the impact of inflammatory stimuli.
- Materials: Seahorse XF Analyzer (or equivalent), cell culture media, compounds (oligomycin, FCCP, rotenone/antimycin A), inflammatory cytokines (e.g., TNF-α).
- Procedure:
- Cell Preparation: Plate cells (e.g., adipocytes, hepatocytes, myotubes) at optimal density in XF microplates and culture overnight.
- Treatment: Incubate cells with or without inflammatory cytokines (e.g., 10-50 ng/mL TNF-α) for 6-24 hours.
- Assay Run: Replace media with assay-specific media. Measure baseline OCR, then sequentially inject:
- Oligomycin (1.5 µM): Inhibits ATP synthase, reveals ATP-linked respiration.
- FCCP (1.0 µM): Uncouples mitochondria, reveals maximal respiratory capacity.
- Rotenone/Antimycin A (0.5 µM each): Inhibit Complex I and III, reveal non-mitochondrial respiration.
- Data Analysis: Calculate basal respiration, ATP production, proton leak, maximal respiration, and spare respiratory capacity. Compare treated vs. control groups to determine inflammatory-induced mitochondrial dysfunction [29].
Protocol 2: Flow Cytometric Analysis of Mitochondrial ROS
- Objective: To quantify mitochondrial superoxide production in cells under pro-inflammatory conditions.
- Materials: Flow cytometer, MitoSOX Red mitochondrial superoxide indicator, cell-permeant dyes (e.g., MitoTracker Green for mass), staining buffer.
- Procedure:
- Cell Treatment: Expose cells to pro-inflammatory conditions (e.g., palmitate to mimic lipotoxicity, or cytokine mixture).
- Staining: Harvest cells and load with MitoSOX Red (2-5 µM) and MitoTracker Green (50-100 nM) in serum-free media for 30 minutes at 37°C.
- Analysis: Wash cells, resuspend in buffer, and analyze immediately by flow cytometry. Use MitoTracker Green to gate on cells with healthy mitochondrial mass. Measure MitoSOX fluorescence (excitation/emission ~510/580 nm) as an indicator of mitochondrial superoxide.
- Data Analysis: Report median fluorescence intensity (MFI) of MitoSOX. Compare MFI ratios (treated/control) to quantify ROS induction. Include a positive control (e.g., antimycin A) to validate the assay [29].
Evaluating Inflammatory Activation
Protocol 3: Assessing NLRP3 Inflammasome Activation
- Objective: To determine if mitochondrial dysfunction triggers NLRP3 inflammasome assembly and IL-1β maturation.
- Materials: Macrophage cell line (e.g., THP-1 or BMDMs), LPS, ATP, specific NLRP3 inhibitor (MCC950), antibodies for caspase-1 p20 and IL-1β (Western blot), ELISA kits for IL-1β and IL-18.
- Procedure:
- Priming: Differentiate THP-1 cells with PMA or isolate BMDMs. Prime cells with LPS (100 ng/mL) for 3 hours.
- Activation: Treat cells with a NLRP3 activator. To model mitochondrial involvement, use mtDNA stress inducers (e.g., ethidium bromide pre-treatment) or ROS inducers (e.g., rotenone). Include ATP (5 mM, 30 min) as a positive control.
- Inhibition Control: Pre-treat a group with MCC950 (1 µM) for 1 hour before activation to confirm NLRP3 dependence.
- Analysis:
- Western Blot: Analyze cell lysates (pro-caspase-1, caspase-1 p20) and supernatants (concentrated; caspase-1 p20, mature IL-1β).
- ELISA: Measure secreted mature IL-1β and IL-18 in culture supernatants.
- Data Interpretation: Maturation and secretion of IL-1β/IL-18 in response to mitochondrial stressors, inhibitable by MCC950, confirms NLRP3 activation [26].
The following diagram illustrates the core signaling pathway and the experimental approaches used to investigate it.
The Pathophysiological Context: Metabolic Syndrome
In MetS, the interplay between oxidative stress, mitochondrial dysfunction, and inflammation creates a self-perpetuating cycle that drives disease progression.
Clinical and Biomarker Evidence
Cross-sectional studies demonstrate a clear association between oxidative/inflammatory markers and MetS severity. In a study of 170 females aged 40-45, significant trends were observed across MetS categories (controls, pre-MetS, MetS) [31]:
- Inflammatory Markers: Leukocyte counts, CRP, and IL-6 were significantly lower in healthy controls compared to those with pre-MetS and overt MetS [31].
- Oxidative Status Markers: Levels of uric acid were elevated in MetS, while protective antioxidants like bilirubin and carotenoids were reduced in pre-MetS and MetS groups [31].
- Key Associations: Multivariate regression models identified CRP, uric acid, and IL-6 as consistently associated with MetS components, suggesting a proinflammatory imbalance precedes full MetS manifestation, while oxidative imbalance accompanies overt disease [31].
Table 2: Key Biomarker Changes in Metabolic Syndrome Progression
| Biomarker Category | Specific Marker | Change in Pre-MetS/MetS vs. Control | Clinical/Research Utility |
|---|---|---|---|
| Systemic Inflammation | C-Reactive Protein (CRP) | Increased | Strong, independent predictor of cardiovascular risk; correlates with MetS components [31] [2]. |
| Interleukin-6 (IL-6) | Increased | Pro-inflammatory cytokine; central to insulin resistance pathogenesis [31]. | |
| Leukocyte Count | Increased | Simple, readily available marker of systemic inflammation [31]. | |
| Oxidative Stress & Defense | Uric Acid | Increased | Pro-oxidant; associated with hypertension and insulin resistance [31]. |
| Bilirubin | Decreased | Endogenous antioxidant; lower levels correlate with increased MetS risk [31]. | |
| Carotenoids (/Lipids) | Decreased | Marker of fruit/vegetable intake and antioxidant capacity; lower in MetS [31]. | |
| Adipose Tissue Dysfunction | Adiponectin | Decreased | Anti-inflammatory and insulin-sensitizing adipokine; reduced in obesity/MetS [29]. |
| Leptin | Increased | Satiety hormone; state of leptin resistance in obesity [29]. |
Tissue-Specific Dysfunction in MetS
- Adipose Tissue: Hypertrophied adipocytes release high levels of pro-inflammatory cytokines (TNF-α, IL-6, IL-1β) and elevate circulating free fatty acids (FFAs) [29]. This promotes macrophage infiltration, predominantly toward a pro-inflammatory M1 phenotype, exacerbating local and systemic inflammation [30] [29]. Mitochondrial dysfunction in adipocytes reduces oxidative capacity, leading to incomplete fat oxidation and enhanced FFA release [29].
- Skeletal Muscle: Mitochondrial abnormalities, including reduced oxidative capacity and increased ROS, lead to accumulation of lipid intermediates like diacylglycerols (DAG) and ceramides [29]. These activate stress kinases (e.g., PKCθ), inhibiting insulin receptor signaling and contributing to insulin resistance [29].
- Liver: In metabolic dysfunction-associated steatotic liver disease (MASLD), mitochondrial dysfunction manifests as reduced β-oxidation and increased ROS, which trigger inflammation and fibrosis [29]. The NLRP3 inflammasome is activated by lipotoxicity and mitochondrial DAMPs, driving disease progression from simple steatosis to steatohepatitis [29].
Therapeutic Strategies and Research Reagents
Targeting Mitochondrial Oxidative Stress and Inflammation
Therapeutic approaches aim to break the cycle of oxidative stress and inflammation.
- Antioxidant Therapies: Conventional antioxidants (e.g., Vitamin C, E) have shown limited clinical success. Mitochondria-targeted antioxidants, such as MitoQ (ubiquinone attached to TPP+ cation), accumulate in mitochondria and show promise in preclinical models by reducing mtROS and inflammation [32] [33] [28].
- Enhancing Endogenous Defenses: Activation of the Nrf2 pathway by compounds like sulforaphane or synthetic inducers boosts expression of antioxidant enzymes (HO-1, NQO1), suppressing NF-κB signaling [28]. NAD+ precursors (e.g., Nicotinamide Riboside) improve mitochondrial function and reduce inflammation via sirtuin activation [32].
- Inflammasome Inhibition: Specific NLRP3 inhibitors (e.g., MCC950) potently block IL-1β and IL-18 production and have shown efficacy in animal models of metabolic disease [26] [29].
- Mitochondrial Transplantation: An emerging therapy where functional isolated mitochondria are delivered to damaged tissues, showing promise in ischemic injury models [32].
Table 3: The Scientist's Toolkit: Key Research Reagents for Investigating the Axis
| Reagent/Category | Example(s) | Primary Function in Research |
|---|---|---|
| ROS Detection Probes | MitoSOX Red, H2DCFDA, MitoTracker Red CM-H2XRos | Fluorescent dyes for detecting mitochondrial superoxide and general cellular ROS via microscopy/flow cytometry [29]. |
| Metabolic Phenotyping Systems | Seahorse XF Analyzer | Measures mitochondrial respiration (OCR) and glycolytic rate (ECAR) in live cells in real-time [29]. |
| Cytokines & Induction Agents | Recombinant TNF-α, IL-1β, IL-6; Lipopolysaccharides (LPS), Palmitate (FFA) | Used to induce inflammatory signaling or mimic metabolic stress (lipotoxicity) in cell cultures [29]. |
| Pathway Inhibitors | MCC950 (NLRP3 inhibitor), MitoTEMPO (mitochondrial antioxidant), BAY 11-7082 (IKK/NF-κB inhibitor) | Pharmacological tools to inhibit specific nodes of the pathway and establish mechanistic causality. |
| Mitochondrial Dyes | MitoTracker Green/Deep Red, TMRM, JC-1 | Assess mitochondrial mass, membrane potential (ΔΨm), and morphology. |
| Antibodies for Immunoassays | Anti-phospho-NF-κB p65, Anti-NLRP3, Anti-Caspase-1 (p20), Anti-IL-1β, Anti-4-HNE | Detect protein expression, activation (phosphorylation), cleavage, and oxidative damage markers (4-HNE) via Western blot, ELISA, IHC. |
Experimental Therapy: Mitochondrial-Targeted Photodynamic Therapy
A novel strategy in cancer research that can be adapted for mechanistic studies is Mitochondrial-Targeted Photodynamic Therapy (mt-PDT) [33]. This approach uses photosensitizers (PS) conjugated to mitochondrial targeting moieties (e.g., TPP+ triphenylphosphonium) that accumulate in mitochondria. Upon light irradiation, the PS produces lethal amounts of ROS, selectively disrupting mitochondria and triggering apoptosis [33]. This method can be used as a precise tool to induce mitochondrial oxidative stress and study the subsequent inflammatory consequences.
The interplay between oxidative stress and mitochondrial dysfunction is a fundamental driver of chronic inflammation in metabolic syndrome. This vicious cycle, fueled by metabolic excess, creates a pathological feedback loop that accelerates tissue dysfunction and disease progression. Moving forward, breaking this cycle requires multifaceted strategies that simultaneously target mitochondrial health, redox balance, and specific inflammatory pathways. The experimental methodologies and research tools outlined herein provide a foundation for advancing our understanding and developing novel therapeutics for MetS and other inflammation-driven pathologies.
Gut Microbiota Dysbiosis and Its Role in Systemic Inflammation and MetS Pathogenesis
Metabolic syndrome (MetS) represents a significant global health challenge, a cluster of conditions including abdominal obesity, dyslipidemia, hypertension, and dysglycemia that collectively increase the risk of cardiovascular disease and type 2 diabetes. With an age-adjusted prevalence reaching 34.7% in the United States and 25.0% worldwide, the escalating burden of MetS parallels ongoing obesity pandemic trends, necessitating urgent investigation into its underlying mechanisms [34]. Central to the pathophysiology of MetS is chronic low-grade inflammation (often termed "metainflammation"), which has been extensively linked to disturbances in glucometabolic pathways observed in people with obesity and MetS [35]. A growing body of evidence now positions the gut microbiota as a critical regulator at the intersection of host metabolism and immune function, with microbial dysbiosis emerging as a key driver of the inflammatory processes underlying MetS [36] [35].
The intestinal microbiota, consisting of up to one trillion microorganisms, provides essential metabolic and biological functions that the human host cannot perform independently [37] [38]. Through their metabolic activities, gut microbiota produce various bioactive metabolites, most notably short-chain fatty acids (SCFAs) such as acetate, propionate, and butyrate, which are produced by bacterial fermentation of dietary fibers [37]. These compounds not only provide energy to intestinal epithelial cells but also regulate immune responses, inhibit inflammation, and promote gut barrier integrity [37]. Disruption of the gut microbial ecosystem, termed dysbiosis, has been implicated in the development of obesity, insulin resistance, and systemic inflammation through multiple interconnected mechanisms [35] [38]. This review comprehensively examines the pathological mechanisms linking gut microbiota dysbiosis to systemic inflammation and MetS pathogenesis, providing researchers and drug development professionals with current experimental methodologies, therapeutic insights, and emerging research directions.
Mechanisms Linking Gut Dysbiosis to Systemic Inflammation in MetS
Impairment of Intestinal Barrier Function and Metabolic Endotoxemia
One of the primary mechanisms by which gut dysbiosis contributes to systemic inflammation involves compromised intestinal barrier integrity, leading to increased permeability and translocation of bacterial components into systemic circulation [38]. In healthy states, tight junction proteins (including Zonula Occludens-1 and Occludin) maintain selective permeability of the intestinal epithelium. However, dysbiosis, particularly driven by high-fat diets, disrupts these tight junction complexes [38]. This breach of barrier function facilitates the translocation of microbial components, most notably lipopolysaccharide (LPS), a component of Gram-negative bacteria cell walls and one of the most potent inducers of inflammation [38].
The resulting condition, termed "metabolic endotoxemia," refers to a 2-3 fold increase in circulating LPS levels that triggers low-grade systemic inflammation through activation of pattern recognition receptors [38]. Dietary fat particularly facilitates this process through the transport of LPS from the gut lumen via chylomicrons synthesized by intestinal epithelial cells [38]. Once in circulation, LPS activates the innate immune system through its interaction with the CD14/TLR4 complex, triggering downstream signaling cascades including NF-κB translocation and pro-inflammatory cytokine production [35] [38]. This chronic, low-grade inflammatory state directly contributes to insulin resistance in metabolic tissues including adipose tissue, liver, and muscle [38]. Supporting this mechanistic pathway, studies demonstrate that mice lacking functional LPS receptors (CD14 knockout mice) are resistant to diet-induced obesity, insulin resistance, and inflammation, while antibiotic treatment that reduces bacterial load ameliorates these metabolic disturbances [38].
Alterations in Microbial Metabolite Production
Beyond structural bacterial components, gut microbiota dysbiosis influences host metabolism and inflammation through altered production of key microbial metabolites, particularly SCFAs and trimethylamine N-oxide (TMAO). In MetS states, characteristic microbial shifts include a decline in beneficial SCFA-producing bacteria (such as Blautia, Butyricicoccus, Akkermansia muciniphila, and Faecalibacterium prausnitzii) coupled with an expansion of pro-inflammatory opportunistic pathobionts [39]. This imbalance leads to impaired production of protective SCFAs, resulting in weakened activation of G-protein-coupled receptors (GPR41/43), which are essential for regulating renin release, maintaining endothelial function, and exerting anti-inflammatory effects [39].
Concurrently, dysbiosis promotes the overproduction of trimethylamine (TMA) from dietary choline and L-carnitine, which is subsequently oxidized in the liver to trimethylamine N-oxide (TMAO) [39]. TMAO contributes to elevated blood pressure by promoting endothelial dysfunction, enhancing platelet aggregation, and accelerating atherosclerosis [39]. The net effect of these metabolite alterations is a shift toward pro-inflammatory and pro-atherogenic states that characterize MetS. Clinical evidence demonstrates that HTN patients exhibit depleted levels of butyrate-producing genera including Blautia and Butyricicoccus, with strong correlations between these depleted taxa and circulating inflammatory mediators [39].
Immune System Activation and Crosstalk
The gut microbiota plays a crucial role in educating and modulating the host immune system, with dysbiosis leading to maladaptive immune responses that drive metabolic inflammation. Dysbiosis-associated barrier dysfunction allows bacterial translocation that activates both innate and adaptive immune pathways [35]. This includes TLR4/NF-κB signaling in immune cells, triggering the release of pro-inflammatory cytokines including TNF-α, IL-1β, and IL-17, which collectively promote vascular dysfunction, renal sodium retention, and sympathetic overactivity—all key mechanisms driving hypertension in MetS [39].
In adipose tissue, dysbiosis contributes to a shift in macrophage polarization from alternatively activated M2 macrophages (which secrete anti-inflammatory cytokines like IL-10 that protect against insulin resistance) to classically activated M1 macrophages (which secrete pro-inflammatory cytokines including TNF-α and IL-6 that promote insulin resistance) [35]. This inflammatory milieu in adipose tissue further recruits other immune cells through chemokines like monocyte chemoattractant protein-1 (MCP1), creating a self-perpetuating cycle of inflammation and metabolic dysfunction [35]. Recent evidence suggests that obesity-related insulin resistance may actually precede pro-inflammatory macrophage infiltration, with insulin resistance itself increasing MCP1 expression and monocyte recruitment [35].
Table 1: Key Microbial Metabolites in Metabolic Syndrome Pathogenesis
| Metabolite | Microbial Source | Biological Effect | Impact in MetS |
|---|---|---|---|
| Short-chain fatty acids (Butyrate, Propionate, Acetate) | Blautia, Butyricicoccus, Faecalibacterium, Roseburia | Anti-inflammatory, enhance gut barrier, insulin sensitivity | Decreased in MetS; contributes to inflammation and barrier dysfunction |
| Lipopolysaccharide (LPS) | Gram-negative bacteria (e.g., Escherichia_Shigella) | Pro-inflammatory via TLR4/NF-κB activation | Increased translocation; drives metabolic endotoxemia |
| Trimethylamine N-oxide (TMAO) | Formed from TMA (from Enterobacteriaceae etc.) | Endothelial dysfunction, platelet aggregation | Elevated in MetS; promotes atherosclerosis and hypertension |
| Bile acid metabolites | Multiple bacterial species | regulate glucose/lipid metabolism via FXR/TGR5 | Altered composition affects metabolic homeostasis |
Quantitative Evidence: Dietary Patterns, Gut Microbiota, and MetS Risk
Recent large-scale epidemiological studies have provided compelling quantitative evidence linking dietary patterns, gut microbiota composition, and MetS risk. The Dietary Index for Gut Microbiota (DI-GM) has emerged as a novel assessment metric that quantitatively evaluates the impact of dietary patterns on gut microbiota health [37]. This scoring system, developed through systematic integration of existing literature, incorporates 14 dietary components with significant modulatory effects on gut microbiota: 10 beneficial components (whole grains, dietary fibers, fermented dairy products, broccoli, coffee, polyphenol-rich green tea, avocados, chickpeas, cranberries, soy products) and 4 restrictive components (red meat, processed meats, refined carbohydrates, high-fat diets) [37] [34].
A comprehensive cross-sectional analysis of 59,842 nationally representative participants from the 2007-2018 National Health and Nutrition Examination Survey (NHANES) database revealed a significant negative correlation between DI-GM score and MetS risk (OR = 0.947 [0.921, 0.974]) [37]. As the DI-GM score increases, this protective association becomes more pronounced, with individuals in the highest quartile (Q4) of DI-GM scores exhibiting a 16% lower risk of MetS compared to those in the lowest quartile (Q1) (OR: 0.84; 95%CI: 0.70-1.01) after full adjustment for confounders [34]. Mediation analyses further indicated that inflammatory markers—specifically the systemic immune-inflammation index (SII) and neutrophil-to-lymphocyte ratio (NLR)—mediated 4.63% and 3.83% of the association between DI-GM and MetS, respectively [34]. This suggests that the protective effect of a gut-healthy diet operates in part through modulation of systemic inflammation.
Table 2: Dietary Index for Gut Microbiota (DI-GM) Components and Scoring
| Component Type | Food/Nutrient | Scoring Criteria | Rationale |
|---|---|---|---|
| Beneficial Components (n=10) | Whole grains, Dietary fiber, Fermented dairy, Broccoli, Coffee, Green tea, Avocados, Chickpeas, Cranberries, Soy products | 1 point if intake ≥ sex-specific median | Promote microbial diversity, SCFA production, beneficial taxa (e.g., Bifidobacterium) |
| Restrictive Components (n=4) | Red meat, Processed meats, Refined grains, High-fat diets (≥40% energy from fat) | 1 point if intake < sex-specific median (or <40% energy for high-fat) | Reduce microbial diversity, increase pro-inflammatory taxa, impair barrier function |
| Total Score Range | 0-14 points | Higher scores indicate more favorable diet for gut microbiota |
Analysis of gut microbiota composition in hypertensive patients—a key component of MetS—reveals distinct taxonomic alterations characterized by enriched Escherichia_Shigella, Prevotella_9, and Enterococcus, and depletion of Blautia and other butyrate-producing genera [39]. The Escherichia_Shigella-dominated enterotype is significantly more prevalent in hypertension, while ROC-based biomarker analysis identifies Blautia, Butyricicoccus, Lachnoclostridium, Prevotella_9, and Enterococcus as potential diagnostic biomarkers [39]. These patients simultaneously exhibit elevated pro-inflammatory cytokines including IL-1ra and TNF-α, with strong correlations observed between pathobionts (e.g., Escherichia_Shigella) and pro-inflammatory cytokines, and between butyrate producers (Blautia) and anti-inflammatory mediators [39].
Experimental Models and Methodological Approaches
Human Microbiota Profiling Protocols
Comprehensive understanding of gut microbiota's role in MetS pathogenesis relies on robust experimental methodologies for microbial community analysis. The following protocol, adapted from a case-control study of elderly Chinese hypertensive patients, details standard approaches for 16S rRNA gene sequencing-based microbiota profiling [39]:
Sample Collection and Storage: Approximately 2g of fresh fecal samples are collected in sterile plastic cups and immediately stored at -80°C within 15 minutes of collection to preserve microbial composition and prevent overgrowth.
DNA Extraction: Bacterial genomic DNA is extracted from 300mg of homogenized fecal samples using the QIAamp DNA Stool Mini Kit (Qiagen, Cat. No. 51604) with additional glass-bead beating steps on a Mini-beadbeater to ensure complete cell lysis.
Amplicon Library Preparation: The V3-V4 hypervariable regions of the 16S rRNA gene are amplified using primer pairs 338F (5'-ACTCCTACGGGAGGCAGCAG-3') and 806R (5'-GGACTACHVGGGTWTCTAAT-3'). PCR reactions contain approximately 10ng genomic DNA, forward and reverse primers (1μM each), and high-fidelity PCR master mix.
Sequencing: Purified amplicon libraries are sequenced on the Illumina NovaSeq platform (or similar) using paired-end (2×250) chemistry, generating approximately 50,000-100,000 reads per sample after quality filtering.
Bioinformatic Analysis: Sequences are processed using QIIME2 or similar pipelines, including demultiplexing, quality filtering, denoising, chimera removal, and amplicon sequence variant (ASV) clustering. Taxonomic assignment is performed against reference databases (Silva, Greengenes).
For systemic inflammation assessment, multiplex immunoassays can simultaneously quantify 27+ cytokines (e.g., IL-1ra, TNF-α, IL-6, IL-10) from serum samples, with correlation analysis revealing relationships between specific bacterial taxa and inflammatory mediators [39].
Dietary Intervention Assessment
Assessment of dietary impact on gut microbiota in MetS research employs standardized methodologies:
Dietary Data Collection: The Automated Multiple-Pass Method (AMPA) developed by the USDA provides a standardized 24-hour dietary recall approach, with trained interviewers conducting two independent recalls and averaging intake values [37].
DI-GM Scoring: Each of the 14 dietary components is scored 0 or 1 based on sex-specific median intakes (except high-fat diet using fixed 40% energy threshold), with total scores ranging 0-14 [37] [34].
Clinical MetS Assessment: Based on NCEP-ATPIII criteria, requiring ≥3 of: waist circumference (>102cm men, >88cm women); fasting glucose ≥100mg/dL or diabetes treatment; blood pressure ≥130/85mmHg or antihypertensive medication; triglycerides ≥150mg/dL; HDL-C (<40mg/dL men, <50mg/dL women) [37] [34].
Inflammation Marker Calculation:
- SII = (platelet count × neutrophil count)/lymphocyte count
- NLR = neutrophil count/lymphocyte count Both calculated from complete blood count with differential [34].
Therapeutic Implications and Research Reagent Solutions
Microbiome-Targeted Interventions
Current evidence supports multiple approaches for targeting gut microbiota to ameliorate MetS-associated inflammation:
Prebiotics: Demonstrate the most consistent metabolic and anti-inflammatory benefits across multiple parameters, with significant decreases in fasting glucose in overweight individuals, and improvements in insulin levels and HOMA-IR in MetS patients [40]. Prebiotic interventions produce 31% reduction in C-reactive protein (CRP), alongside decreased IL-6, TNF-α, and LPS levels, while promoting butyrate-producing bacteria [40].
Probiotics: Show significant enhancement of insulin resistance (HOMA-IR), reduced circulating endotoxin levels, decreased visceral fat, BMI, and fat mass, with increased beneficial taxa and reduction in obesity-associated bacteria [40]. However, outcomes for lipid parameters remain inconsistent [40].
Synbiotics: Demonstrate complementary benefits for glucose metabolism and body composition, though require further investigation to establish consistent clinical efficacy [40].
Fecal Microbiota Transplantation (FMT): Shows promise in restoring microbial balance and improving metabolic parameters, with studies indicating improved insulin sensitivity and donor microbiota engraftment in responders [40]. However, application is limited by donor variability, procedural risks, and uncertain long-term safety [41].
Dietary Modifications: Fiber-rich diets markedly improve HbA1c levels in diabetic and prediabetic individuals, while specific dietary patterns quantified by DI-GM scores show significant negative association with MetS risk [37] [40] [34].
Table 3: Research Reagent Solutions for Gut Microbiota-MetS Investigations
| Reagent Category | Specific Examples | Research Application | Key Functions |
|---|---|---|---|
| DNA Extraction Kits | QIAamp DNA Stool Mini Kit (Qiagen #51604) | Microbial community profiling | Comprehensive lysis of diverse bacterial species; inhibitor removal for PCR-compatible DNA |
| 16S rRNA Primers | 338F/806R (V3-V4 regions) | Taxonomic classification | Amplification of hypervariable regions for bacterial identification and diversity assessment |
| Sequencing Platforms | Illumina NovaSeq, MiSeq | High-throughput sequencing | Generation of 50,000-100,000 reads/sample for deep community analysis |
| Cytokine Assays | Multiplex immunoassays (27-plex) | Inflammation quantification | Simultaneous measurement of pro/anti-inflammatory cytokines (IL-1ra, TNF-α, IL-6, IL-10) |
| Bioinformatics Tools | QIIME2, DADA2, SILVA database | Microbiota data analysis | Processing, denoising, taxonomic assignment, and diversity calculations from sequencing data |
| Bacterial Standards | ZymoBIOMICS Microbial Community Standard | Method validation | Quality control for DNA extraction, amplification, and sequencing workflows |
The intricate relationship between gut microbiota dysbiosis, systemic inflammation, and MetS pathogenesis represents a paradigm shift in our understanding of metabolic disease. Evidence from human studies, animal models, and interventional trials consistently demonstrates that gut microbial dysbiosis contributes to MetS through multiple interconnected mechanisms: impairment of intestinal barrier function leading to metabolic endotoxemia; altered production of microbial metabolites including SCFAs and TMAO; and activation of both innate and adaptive immune responses that drive chronic low-grade inflammation [37] [35] [39]. The recently developed DI-GM provides a validated tool for quantifying diet-microbiome interactions, with higher scores significantly associated with reduced MetS risk, partially mediated by inflammatory markers including SII and NLR [37] [34].
Future research should prioritize several key areas: First, personalized microbiome-directed interventions based on individual microbial signatures, dietary patterns, and genetic backgrounds show promise for moving beyond one-size-fits-all approaches [41]. Second, mechanistic insights into specific microbial taxa and their functional genes will enable more targeted therapeutic development, potentially focusing on next-generation probiotics (e.g., Akkermansia muciniphila), postbiotics, or small molecule inhibitors of microbial-host interactions [40] [42]. Third, longitudinal studies tracking microbiota changes relative to MetS development and progression will help establish causal relationships and identify critical windows for intervention. Finally, technical innovations in metagenomics, metabolomics, and computational biology will continue to reveal disease-specific microbial signatures and create novel diagnostic and therapeutic opportunities [41].
The gut microbiota represents both a biomarker for MetS risk stratification and a promising therapeutic target for preventing and managing metabolic syndrome. As research continues to unravel the complex interactions between diet, gut microbes, host immunity, and metabolism, microbiota-targeted interventions may eventually become integrated into standard clinical management for MetS, potentially addressing the root causes of metabolic inflammation rather than merely managing its symptoms.
Inflammaging refers to the chronic, low-grade, and systemic inflammatory state that characterizes aging, serving as a significant risk amplifier for a multitude of age-related pathologies. Unlike acute, beneficial inflammation, inflammaging is a sterile, persistent process driven by a complex interplay of immunological and metabolic mechanisms [43] [44]. It is marked by elevated levels of pro-inflammatory cytokines, acute-phase proteins, and other inflammatory mediators, which contribute to the pathogenesis of conditions such as cardiovascular disease, metabolic syndrome (MetS), neurodegenerative disorders, and reduced immune competence [43] [45] [46]. Within the context of metabolic syndrome research, inflammaging is recognized not merely as a companion phenomenon but as a key driver that accelerates the progression of core metabolic abnormalities, including insulin resistance, dyslipidemia, and central obesity [47] [2] [46].
The interplay between inflammaging and metabolic syndrome creates a vicious cycle. Adipose tissue, particularly in a state of hypertrophy, secretes pro-inflammatory cytokines such as IL-6, TNF-α, and IL-1β, which further fuels systemic inflammation and disrupts insulin signaling in peripheral tissues [47] [2]. This chronic low-grade inflammation is now considered a central pillar in the pathophysiology of MetS, making the understanding of its mechanisms and measurement critical for therapeutic development [47] [2].
Core Mechanisms and Pathways
The development and persistence of inflammaging are underpinned by several interrelated biological hallmarks. The following table summarizes the key mechanisms and their contributions to the inflammatory state.
Table 1: Core Mechanisms Driving Inflammaging
| Mechanism | Key Components | Contribution to Inflammaging |
|---|---|---|
| Immunosenescence [44] [46] | Thymic involution, reduced naive T cells, expanded memory T cells (CD28-), Accumulated Age-associated B cells (ABCs) | Declines in adaptive immune function and reduced ability to clear pathogens and senescent cells |
| Cellular Senescence & SASP [44] | p16/p53 activation, SASP factors (IL-6, IL-1β, CXCL1, MMPs) | Chronic, low-level production of pro-inflammatory cytokines and tissue-remodeling factors |
| Mitochondrial Dysfunction [43] [46] | Reduced calcium uptake, Increased ROS, mtDNA release (DAMPs) | Activation of innate immune sensors (NLRP3 inflammasome) and oxidative stress |
| Gut Dysbiosis [48] [46] | Increased gut permeability, Reduced SCFA-producing bacteria, Elevated TMAO | Systemic entry of microbial products and production of pro-atherogenic metabolites |
These mechanisms do not operate in isolation but form a complex network. The signaling pathways involved can be visualized in the following diagram, which integrates these processes and their connections to metabolic syndrome.
Biomarkers and Measurement in Metabolic Syndrome
Accurately quantifying inflammaging is essential for both research and clinical translation in metabolic syndrome. Biomarkers range from well-established clinical assays to novel composite indices.
Table 2: Key Biomarkers for Assessing Inflammaging in Metabolic Syndrome Research
| Biomarker Category | Specific Marker | Biological Significance & Rationale | Technical & Methodological Considerations |
|---|---|---|---|
| Established Circulating Markers | High-sensitivity CRP (hs-CRP) | Liver-derived acute-phase protein; directly indicates systemic inflammation and strongly predicts cardiovascular risk [49] [50] [51]. | Method: Immunoturbidimetry/ELISA. Kinetics: Rises in 4-6 hrs, peaks at 48 hrs, half-life ~19 hrs. Use hs-CRP for low-grade inflammation [50] [51]. |
| Pro-inflammatory Cytokines (IL-6, TNF-α, IL-1β) | Primary drivers of inflammation; IL-6 is a key regulator of CRP production. Measured in serum/plasma [49] [44]. | Method: Multiplex bead-based immunoassays (Luminex) or ELISA. Challenge: Susceptible to freeze-thaw cycles; requires careful sample handling [49]. | |
| Cellular & Hematological Markers | White Blood Cell (WBC) Count & Differential | Provides a quantitative profile of immune cell populations. Neutrophilia indicates acute stress; lymphopenia is common in chronic inflammation [49] [51]. | Method: Automated hematology analyzers. Neutrophil-to-Lymphocyte Ratio (NLR) is a derived, stable marker of systemic inflammation [47] [51]. |
| Composite & Research Indices | INFLA-Score | A composite score integrating CRP, WBC, platelet count, and NLR. It provides a more robust measure of systemic low-grade inflammation than single markers [47]. | Calculation: Biomarker levels are assigned values based on population deciles. Score range: -16 to +16. A higher score indicates greater inflammatory burden [47]. |
| Oxidative Stress Markers | F2-isoprostanes, 8-OH-dG | F2-isoprostanes are stable products of lipid peroxidation; 8-OH-dG is a marker of oxidative DNA damage. Closely linked to inflammatory pathways [49]. | Method: Gas chromatography-mass spectrometry (GC-MS) or LC-MS/MS for F2-isoprostanes; ELISA or LC-MS/MS for 8-OH-dG. 8-OH-dG is stable in long-term storage [49]. |
The INFLA-Score has demonstrated significant utility in metabolic syndrome research. A 2025 cross-sectional study of 1,758 shift workers found that those in the highest quartile of INFLA-Score had a 3.58 times higher risk of MetS compared to the lowest quartile, demonstrating a clear dose-response relationship [47]. This highlights the power of composite scores in capturing the global inflammatory burden relevant to metabolic dysregulation.
Experimental Protocols for Investigating Inflammaging
Protocol: Immune Cell Profiling in Aging and Metabolic Syndrome
This protocol outlines a comprehensive approach to characterize immunosenescence and immune activation in the context of MetS.
- Sample Collection: Collect peripheral blood in EDTA tubes. Process within 2 hours of collection. Isolate Peripheral Blood Mononuclear Cells (PBMCs) using density gradient centrifugation (e.g., Ficoll-Paque). Plasma can be aliquoted and stored at -80°C for cytokine analysis.
- Cell Staining for Flow Cytometry: Resuspend 1-2 million PBMCs in FACS buffer. Incubate with fluorochrome-conjugated antibodies for 30 minutes at 4°C in the dark. A recommended antibody panel includes:
- T-cell Senescence/Exhaustion: CD3, CD4, CD8, CD28, CD57, KLRG1, PD-1.
- T-cell Differentiation: CD45RA, CCR7 (to define naive, central memory, effector memory subsets).
- Innate Immune Activation: CD14 (monocytes), CD16 (non-classical monocytes), HLA-DR.
- Data Acquisition and Analysis: Acquire data on a flow cytometer capable of detecting at least 8 colors. Analyze using software such as FlowJo. Key analyses include:
- Quantifying the frequency of CD28- T cells within CD4+ and CD8+ populations.
- Calculating the ratio of naive (CD45RA+CCR7+) to memory T cells.
- Assessing monocyte activation via HLA-DR expression.
- Cytokine Measurement: Analyze stored plasma using a high-sensitivity multiplex assay for cytokines including IL-6, TNF-α, IL-1β, and IL-18. Correlate cytokine levels with immune cell phenotypes and clinical parameters of MetS (e.g., HOMA-IR, waist circumference) [44].
Protocol: Ex Vivo Macrophage Stimulation to Assess Functional Phenotype
This methodology evaluates the inflammatory response of innate immune cells from aged or metabolically compromised subjects.
- Macrophage Differentiation: Differentiate isolated human monocytes (from PBMCs) into macrophages by culturing in RPMI-1640 medium supplemented with 10% FBS and 50 ng/mL Macrophage Colony-Stimulating Factor (M-CSF) for 6 days.
- Polarization and Stimulation: Polarize macrophages towards an M1 state with 100 ng/mL IFN-γ for 24 hours, followed by stimulation with 100 ng/mL LPS for an additional 24 hours. Include unstimulated controls.
- Analysis of Response:
- Gene Expression: Harvest RNA and perform RT-qPCR for M1 markers (e.g., TNF-α, IL-6, IL-1β) and M2 markers (e.g., ARG1, MRC1). Calculate fold changes relative to control.
- Protein Secretion: Collect cell culture supernatants. Measure secreted cytokines using ELISA or multiplex immunoassays.
- Metabolic Phenotyping (Seahorse Assay): Analyze mitochondrial respiration and glycolytic function in real-time using an extracellular flux analyzer. Inflammaging is often associated with reduced mitochondrial calcium uptake in macrophages, which can drive pro-inflammatory responses [43].
Research Reagent Solutions
Table 3: Essential Research Reagents for Investigating Inflammaging
| Reagent / Tool Category | Specific Examples | Function & Application |
|---|---|---|
| Antibodies for Flow Cytometry | Anti-human CD3, CD4, CD8, CD28, CD45RA, CCR7, CD14, CD16, HLA-DR, CD57 | Immunophenotyping of T cell subsets, monocyte populations, and identification of senescent/differentiated immune cells [44]. |
| Cytokine Detection Kits | High-sensitivity ELISA or Multiplex Bead Arrays (e.g., Luminex) for IL-6, TNF-α, IL-1β, IL-18 | Quantification of pro-inflammatory cytokines and SASP factors in plasma, serum, or cell culture supernatants [49] [44]. |
| Cell Culture Supplements | Recombinant Human M-CSF, GM-CSF, IFN-γ, LPS | Differentiation and polarization of primary human monocytes into macrophages for functional assays [43]. |
| Senescence & Metabolic Assays | SA-β-Gal Staining Kit (for cellular senescence), Seahorse XFp/Kits (for mitochondrial function), ROS Detection Dyes (e.g., DCFDA) | Direct assessment of cellular senescence, mitochondrial respiration, glycolytic flux, and reactive oxygen species production [43] [44]. |
| Senolytic Compounds | Dasatinib + Quercetin (D+Q), Fisetin, Navitoclax (ABT-263) | Research tools to selectively clear senescent cells and validate the role of cellular senescence and SASP in inflammaging pathways [43] [44]. |
Therapeutic and Intervention Strategies
Targeting inflammaging presents a promising avenue for mitigating metabolic syndrome and other age-related conditions. Interventions can be categorized as follows:
- Lifestyle and Nutritional Interventions: Dietary patterns are a powerful modulator. The Composite Dietary Antioxidant Index (CDAI) has shown a negative association with CVD prevalence, with protective effects being gender-specific [46]. Diets rich in vegetables, fruits, and omega-3 fatty acids (EPA and DHA at 1–2 g/day) consistently lower inflammatory markers like CRP, IL-6, and TNF-α [51]. Regular, moderate-intensity exercise acts as an anti-inflammatory intervention by promoting the release of myokines from muscle [51].
- Pharmacological and Targeted Therapies: Senolytics, such as Dasatinib and Quercetin, have been shown to attenuate inflammation and ameliorate physiologic function in old age by selectively eliminating senescent cells [43]. Other emerging strategies include senomorphic agents that suppress the SASP, telomerase activators to counter immunosenescence, and pre-/probiotic supplementation to correct gut dysbiosis [48] [44].
- Emerging and Experimental Approaches: Cell-based therapies are under investigation, such as senolytic CAR-T cells engineered to target specific senescent cell antigens [43]. Additionally, targeting specific mechanisms like macrophage self-renewal after infection or nutrient-sensing pathways (e.g., Ghrelin receptor GHS-R) are novel strategies to reprogram immune cell function and dampen chronic inflammation [43].
Detecting the Signal: Advanced Biomarkers and Cutting-Edge Profiling Technologies
Metabolic Syndrome (MetS) represents a cluster of abnormalities—including central obesity, dyslipidemia, hypertension, and impaired fasting glucose—that collectively confer significantly increased risk for cardiovascular disease (CVD) and type 2 diabetes mellitus (T2DM) [52]. A central feature underpinning MetS pathophysiology is low-grade chronic inflammation [52]. This persistent, subclinical inflammatory state is increasingly recognized as a critical driver of both insulin resistance and atherogenesis [53]. Consequently, the measurement of systemic inflammatory biomarkers has become essential for risk stratification and understanding disease mechanisms in MetS research. Among the most established clinical markers of this inflammatory state are C-reactive protein (CRP), fibrinogen, and white blood cell (WBC) count. These biomarkers provide objective, measurable parameters of inflammation that are accessible in standard clinical and research settings, making them invaluable tools for investigating the link between metabolic dysfunction and inflammation [54].
The Inflammatory Basis of Metabolic Syndrome
Low-grade inflammation is now considered a hallmark characteristic of MetS [52]. The expansion of adipose tissue, particularly visceral fat, creates a pro-inflammatory environment through the increased production of adipokines and cytokines such as interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α) [52]. These signaling molecules, in turn, stimulate the liver to produce acute-phase reactants, including CRP and fibrinogen, while also promoting leukocytosis [52] [55]. This chronic inflammatory state contributes directly to the development of insulin resistance and endothelial dysfunction, creating a vicious cycle that propagates both metabolic and cardiovascular complications [53].
Large-scale epidemiological studies have consistently demonstrated that individuals with MetS exhibit elevated levels of inflammatory markers. Data from the Third National Health and Nutrition Examination Survey (NHANES III) revealed that people with MetS were significantly more likely to have elevated CRP, fibrinogen, and leukocyte counts compared to those without the syndrome [56]. Furthermore, a dose-response relationship exists between the number of metabolic abnormalities and the degree of inflammation; as the number of MetS components increases, so do the levels of inflammatory biomarkers [54]. This gradient effect provides compelling evidence for the integral role of inflammation in MetS pathophysiology.
Established Inflammatory Markers: Mechanisms and Significance
C-Reactive Protein (CRP)
CRP, particularly when measured by high-sensitivity assays (hs-CRP), is the most extensively characterized and standardized biomarker of inflammation in MetS and cardiovascular disease [52]. Produced primarily by hepatocytes in response to IL-6, CRP serves as a sensitive marker of systemic inflammation. Beyond its role as a biomarker, evidence suggests CRP may actively contribute to atherothrombosis by impairing insulin signaling, promoting endothelial dysfunction, and enhancing monocyte recruitment into the arterial wall [52].
In research settings, hs-CRP has consistently demonstrated superior performance compared to other inflammatory markers for identifying MetS. A Japanese comparative study found the area under the ROC curve (AUC) for hs-CRP was 0.71 in men and 0.74 in women, outperforming WBC count (AUC 0.65 in men, 0.69 in women) for diagnosing MetS [57]. Similarly, a 2022 study in hemodialysis patients reported an AUC of 0.638 for hs-CRP in diagnosing MetS, with an optimal cut-off point of 1.58 mg/L [58]. The diagnostic ability of hs-CRP was significantly better than traditional inflammatory markers like leukocytes, neutrophils, lymphocytes, monocytes, and neutrophil-to-lymphocyte ratio (NLR) in this population [58].
Table 1: CRP Cut-off Values and Diagnostic Performance for Metabolic Syndrome
| Population | Optimal Cut-off | Sensitivity | Specificity | AUC | Citation |
|---|---|---|---|---|---|
| Japanese Men | 0.40 mg/L | 69% | 65% | 0.71 | [57] |
| Japanese Women | 0.35 mg/L | 67% | 72% | 0.74 | [57] |
| Hemodialysis Patients | 1.58 mg/L | - | - | 0.638 | [58] |
Fibrinogen
Fibrinogen is a glycoprotein synthesized in the liver that plays crucial roles in both hemostasis and inflammation [59]. Beyond its well-established function in the coagulation cascade, fibrinogen acts as a key regulator of inflammation in various diseases [55]. It promotes inflammatory responses by facilitating leukocyte adhesion and activation, stimulating cytokine production, and functioning as a bridging molecule in cell-to-cell interactions [55].
In the context of MetS, fibrinogen contributes to a prothrombotic state and has been implicated in vascular complications. Research suggests a potential role for fibrinogen in sudden sensorineural hearing loss (SSHL), which may have a vascular origin. Elevated fibrinogen levels increase blood viscosity and reduce blood flow, potentially compromising circulation in terminal arteries such as those supplying the cochlea [59]. This mechanism highlights how fibrinogen may link MetS to end-organ damage through both inflammatory and rheological pathways.
NHANES III data confirmed that fibrinogen levels are significantly elevated in individuals with MetS compared to those without the syndrome [56]. The proinflammatory properties of fibrinogen, combined with its effects on blood viscosity and coagulation, position it as a multidimensional biomarker that reflects both the inflammatory and prothrombotic components of MetS.
White Blood Cell (WBC) Count
The WBC count represents a convenient, inexpensive, and routinely measured cellular marker of systemic inflammation [54]. Even within normal reference ranges, elevated WBC counts have been consistently associated with MetS and its components across diverse populations [53] [54]. The WBC count reflects the overall inflammatory burden and has demonstrated a significant graded relationship with the number of metabolic abnormalities present [54].
A study of an Iranian population found that mean WBC counts increased progressively with the number of MetS components: from 5.321/µL in those with no components to 6.572/µL in those with all five components (p<0.0001 for trend) [54]. Similarly, research on metabolically healthy obesity (MHO) has demonstrated inverse correlations between WBC count and the MHO phenotype, with an odds ratio of 0.81 (95% CI: 0.76, 0.86) for MHO risk per unit increase in WBC count [60]. This relationship persists across various WBC subtypes, including lymphocytes, monocytes, and neutrophils [60].
Table 2: Association Between Blood Cell Counts and Metabolically Healthy Obesity
| Cell Type | Odds Ratio (95% CI) | P-value | Pattern of Association | Citation |
|---|---|---|---|---|
| WBC | 0.81 (0.76, 0.86) | <0.001 | L-shaped | [60] |
| Lymphocytes | 0.56 (0.47, 0.68) | <0.001 | Linear | [60] |
| Monocytes | 0.41 (0.22, 0.75) | 0.004 | Linear | [60] |
| Neutrophils | 0.82 (0.76, 0.88) | <0.001 | L-shaped | [60] |
While WBC count is generally considered less specific than hs-CRP for MetS diagnosis, it remains a valuable biomarker, particularly in settings where advanced assays are unavailable [57]. Its strengths include wide availability, low cost, and standardization across laboratories.
Comparative Analysis of Inflammatory Markers in Metabolic Syndrome
The inflammatory markers discussed each possess distinct characteristics, advantages, and limitations in the context of MetS research. CRP, particularly hs-CRP, is generally regarded as the most sensitive and specific inflammatory biomarker for MetS, with strong predictive value for cardiovascular events [52] [57]. Its superiority stems from its direct reflection of IL-6 driven inflammation and standardized measurement protocols. However, CRP measurement requires specialized assays that may not be universally available.
Fibrinogen provides unique insights by reflecting both inflammatory and prothrombotic pathways, offering a more comprehensive view of MetS-related pathophysiology [56] [55]. Its association with blood viscosity and flow dynamics connects inflammation to end-organ damage mechanisms, as suggested by research on SSHL [59]. Nevertheless, fibrinogen measurement can be affected by pre-analytical variables and coagulation disorders.
WBC count offers practical advantages as a universally available, inexpensive cellular marker of inflammation that can be easily incorporated into large-scale studies and clinical practice [54]. Its association with MetS components demonstrates a clear dose-response relationship, strengthening its utility for risk stratification [54]. The main limitations of WBC count include lower specificity and susceptibility to various confounders including infections, stress, and other inflammatory conditions.
Table 3: Comparative Characteristics of Established Inflammatory Markers in Metabolic Syndrome Research
| Parameter | CRP/hs-CRP | Fibrinogen | WBC Count |
|---|---|---|---|
| Primary Origin | Hepatocyte (IL-6 driven) | Hepatocyte | Bone marrow |
| Key Functions | Acute phase response, complement activation, endothelial dysfunction | Coagulation, inflammation, blood viscosity | Host defense, inflammation, tissue repair |
| Diagnostic Performance (AUC) | 0.71-0.74 (general population) [57] | - | 0.65-0.69 (general population) [57] |
| Key MetS Associations | Central adiposity, insulin resistance [52] | Prothrombotic state, vascular complications [59] | All MetS components, graded response [54] |
| Advantages | High sensitivity, standardized assays, strong predictive value | Reflects inflammation and coagulation, vascular relevance | Universal availability, low cost, cellular response marker |
| Limitations | Requires specialized assays, moderate cost | Affected by coagulation disorders, pre-analytical variability | Low specificity, confounded by infections |
Methodological Approaches for Inflammatory Marker Assessment
Laboratory Measurement Protocols
hs-CRP Measurement: Serum hs-CRP is typically quantified using immunonephelometric assays on automated analyzers (e.g., Roche/Hitachi 917 analyzer) with a detection limit of 0.01 mg/L [58]. The immunonephelometric method measures the light scatter resulting from antigen-antibody complex formation, providing high sensitivity for low-grade inflammation assessment. For research purposes, blood samples should be collected after an overnight fast (10-12 hours) to minimize dietary influences. Samples are typically centrifuged, and serum aliquots stored at -80°C until analysis to maintain biomarker stability [58].
Fibrinogen Assessment: Plasma fibrinogen can be measured using both functional (clot-based) and immunochemical methods. The Clauss method is widely used for functional fibrinogen assessment, where diluted plasma is clotted with a high concentration of thrombin, and the clotting time is proportional to fibrinogen concentration [59]. For inflammatory studies, enzyme-linked immunosorbent assays (ELISA) may provide additional information about fibrinogen structure and function. Pre-analytical standardization is crucial, as fibrinogen levels can be affected by venipuncture technique, sample processing time, and anticoagulant concentration.
WBC Count Methodology: WBC counts are performed on EDTA-anticoagulated whole blood using automated hematology analyzers (e.g., Sysmex XE-2100) based on the Coulter principle or flow cytometry [58]. These instruments count and size particles by detecting changes in electrical resistance as cells pass through an aperture. The differential count (neutrophils, lymphocytes, monocytes, etc.) is typically determined by peroxidase staining or flow cytometric methods. Quality control includes regular calibration and participation in proficiency testing programs.
Standardized Experimental Workflows
The following diagram illustrates a standardized research workflow for assessing inflammatory markers in metabolic syndrome studies:
Diagram 1: Research Workflow for Inflammatory Marker Assessment in Metabolic Syndrome Studies
Key Methodological Considerations
Population Selection: Studies should clearly define MetS using established criteria (e.g., ATP III, IDF) and consider specific population characteristics (e.g., dialysis patients, ethnic variations) that may influence inflammatory marker levels [58].
Confounder Adjustment: Statistical models should account for potential confounders including age, sex, BMI, smoking status, alcohol intake, physical activity, medication use, and comorbidities [60] [58].
Quality Control: Implement rigorous quality control procedures including standardized sample collection, processing protocols, and blinded laboratory analyses to minimize measurement bias.
Multiple Marker Assessment: Where feasible, measure multiple inflammatory markers to capture different aspects of the inflammatory response and enable comparative analyses.
Signaling Pathways Linking Inflammation to Metabolic Dysfunction
The relationship between inflammatory markers and MetS involves complex signaling pathways that create a vicious cycle of metabolic dysfunction and inflammation. The following diagram illustrates key mechanistic pathways:
Diagram 2: Signaling Pathways Linking Inflammatory Markers to Metabolic Syndrome Pathophysiology
Table 4: Essential Research Reagents and Resources for Inflammatory Marker Studies
| Category | Specific Items | Research Application | Technical Notes |
|---|---|---|---|
| Sample Collection | EDTA tubes (lavender top), Serum separator tubes (SST), Sodium citrate tubes (blue top) | Blood collection for WBC, CRP, and fibrinogen respectively | Maintain sample stability; process within 2h for WBC, 4h for CRP [58] |
| CRP Analysis | hs-CRP immunonephelometric kits, IL-6 ELISA kits, CRP calibrators & controls | Quantifying systemic inflammation, establishing correlation with cytokine drivers | Ensure assay range covers low-grade inflammation (0.1-10 mg/L) [57] |
| Fibrinogen Analysis | Clauss method reagents, Fibrinogen ELISA kits, Thrombin reagents | Measuring fibrinogen concentration & potential structural variants | Functional vs. immunochemical methods may yield different results [59] |
| WBC Analysis | Automated hematology analyzers, Flow cytometers with CD markers, Wright-Giemsa stain | Complete blood count with differential, leukocyte phenotyping | Distinguish neutrophil, lymphocyte, monocyte subsets for refined analysis [60] |
| Data Analysis | Statistical software (R, SPSS), ROC curve analysis packages, Multivariate regression tools | Assessing diagnostic performance, adjusting for confounders, establishing cut-offs | Use weighted analyses for complex survey data (e.g., NHANES) [60] |
CRP (particularly hs-CRP), fibrinogen, and WBC count represent established, clinically relevant inflammatory markers that provide distinct but complementary information in metabolic syndrome research. These biomarkers reflect different aspects of the low-grade chronic inflammatory state that characterizes MetS and contributes to its associated cardiometabolic risks. While hs-CRP generally demonstrates superior diagnostic performance, fibrinogen offers unique insights into prothrombotic mechanisms, and WBC count provides an accessible cellular marker of inflammation. The integration of these biomarkers in research protocols, employing standardized methodologies and appropriate statistical approaches, continues to advance our understanding of the intricate relationship between inflammation and metabolic dysfunction. Future research directions should focus on elucidating the causal mechanisms linking these inflammatory markers to specific metabolic abnormalities and exploring their utility in guiding targeted anti-inflammatory interventions for MetS.
Metabolic syndrome (MetS) is a cluster of conditions—including central obesity, dyslipidemia, hypertension, and hyperglycemia—that collectively increase the risk of type 2 diabetes and cardiovascular disease [61]. Central to its pathophysiology is a state of chronic low-grade inflammation, characterized by abnormal production and signaling of pro-inflammatory cytokines [62]. This inflammatory milieu, driven largely by dysfunctional adipose tissue, creates a self-perpetuating cycle that disrupts insulin signaling and promotes metabolic dysfunction [63]. Among the key mediators are interleukin-1β (IL-1β), interleukin-6 (IL-6), and tumor necrosis factor-alpha (TNF-α), which act through complex receptor-mediated pathways to orchestrate a systemic inflammatory response [64]. Understanding the precise roles, signaling mechanisms, and interactions of these cytokines provides crucial insights for developing targeted therapeutic strategies to disrupt this inflammatory cascade in metabolic disease.
Cytokine Roles and Signaling Pathways in Metabolic Syndrome
TNF-α: A Master Regulator of Metabolic Inflammation
TNF-α plays a pivotal role in initiating and sustaining the inflammatory response in metabolic syndrome. Primarily secreted by adipose tissue macrophages, TNF-α serum levels are significantly elevated in obese individuals with MetS compared to healthy controls (140.69 ± 10.40 pg/ml vs. 15.94 ± 0.89 pg/ml, P < 0.001) [65]. This cytokine inhibits lipoprotein lipase activity and impairs insulin signaling through serine phosphorylation of insulin receptor substrate-1 (IRS-1), a key mechanism in the development of insulin resistance [66] [62]. TNF-α also promotes lipolysis in adipose tissue, increasing circulating free fatty acids that further exacerbate metabolic dysfunction [64]. The cytokine's action extends to inhibiting the expression of critical adipose tissue differentiation regulators CCAAT/enhancer-binding protein α (CEBP-α) and peroxisome proliferator-activated receptor γ-2 (PPARγ-2), thereby altering the expression of multiple adipose tissue proteins involved in lipid and glucose metabolism [66].
IL-6: The Hepatic Inflammatory Mediator
IL-6 serves as a major contributor to the systemic inflammatory state in MetS, with adipose tissue contributing up to 30% of circulating IL-6 levels [66]. Intraperitoneal adipose tissue secretes approximately three times more IL-6 than subcutaneous adipose tissue [66]. Elevated IL-6 levels (98.14 ± 17.94 pg/ml in MetS patients vs. 4.6 ± 0.2 pg/ml in controls, P < 0.001) promote hepatic acute-phase protein production, including C-reactive protein (CRP), which serves as a clinical marker of systemic inflammation [65] [63]. IL-6 induces insulin resistance through multiple mechanisms, including increased expression of suppressor of cytokine signaling 3 (SOCS-3), which inhibits IRS signaling [64]. Furthermore, IL-6 influences hormonal balance and endocrinological abnormalities, potentially affecting free fatty acid levels and contributing to lipid abnormalities commonly observed in MetS [66]. Gender differences in IL-6 regulation have been observed, with obese women showing particularly significant elevations [66].
IL-1β: The β-Cell Toxin
IL-1β plays a specialized role in metabolic syndrome pathogenesis, particularly through its detrimental effects on pancreatic β-cell function [64]. Produced mainly via NLRP3 inflammasome activation in macrophages, IL-1β levels rise in response to metabolic stressors such as free fatty acids and hyperglycemia [63]. In pancreatic islets of type 2 diabetes patients, IL-1β promotes insulin secretory dysfunction and β-cell apoptosis through the induction of endoplasmic reticulum stress [64]. This cytokine also contributes to systemic insulin resistance and endothelial activation, further compounding metabolic dysregulation [63]. Genetic studies have revealed elevated IL-1β expression in human islets from type 2 diabetes patients, highlighting its importance in the progression from obesity to overt diabetes [64].
Emerging Cytokines: PANDER and IL-37
Beyond the classical inflammatory mediators, newer cytokines have emerged as significant players in metabolic syndrome. Pancreatic-derived factor (PANDER), expressed in pancreatic α- and β-cells, shows elevated serum levels in MetS patients and correlates with accumulating MetS components [67]. Conversely, IL-37, a novel anti-inflammatory member of the IL-1 family, demonstrates significantly decreased levels and mRNA expression in MetS patients [67]. IL-37's primary role involves suppressing harmful inflammatory reactions and regulating both innate and adaptive immunity, with potential therapeutic implications for ameliorating insulin resistance in obesity and type 2 diabetes [67].
Table 1: Pro-Inflammatory and Anti-Inflammatory Cytokines in Metabolic Syndrome
| Cytokine | Cellular Source | Receptor | Major Metabolic Effects | Serum Levels in MetS |
|---|---|---|---|---|
| TNF-α | Macrophages, adipocytes | TNFR1, TNFR2 | Serine phosphorylation of IRS-1; inhibits insulin signaling; promotes lipolysis | Significantly elevated (140.69 ± 10.40 pg/ml) [65] |
| IL-6 | Adipocytes, macrophages | IL-6R, gp130 | Hepatic CRP production; induces SOCS-3; inhibits IRS signaling | Significantly elevated (98.14 ± 17.94 pg/ml) [65] |
| IL-1β | Macrophages (via NLRP3 inflammasome) | IL-1R1 | β-cell dysfunction; promotes insulin resistance; endothelial activation | Elevated in tissue inflammation [63] |
| PANDER | Pancreatic α- and β-cells | Not fully characterized | Correlates with accumulation of MetS components | Significantly elevated in MetS [67] |
| IL-37 | Various immune cells | IL-1R8 (SIGIRR) | Suppresses inflammatory reactions; regulates innate/adaptive immunity | Significantly decreased in MetS [67] |
Intracellular Signaling Pathways
The pro-inflammatory cytokines TNF-α, IL-6, and IL-1β activate complex intracellular signaling networks that ultimately converge on insulin resistance. As shown in Figure 1, these pathways center around two key kinases: c-Jun N-terminal kinase (JNK) and inhibitor of nuclear factor kappa-B kinase subunit beta (IKK-β).
Figure 1: Core Inflammatory Signaling Pathways in Metabolic Syndrome. Pro-inflammatory cytokines (TNF-α, IL-6, IL-1β) and free fatty acids (FFAs) activate JNK and IKK-β pathways, leading to serine phosphorylation of IRS-1 and subsequent insulin resistance. These pathways also activate transcription factors NF-κB and AP-1, which induce further pro-inflammatory cytokine production, creating a self-sustaining inflammatory cycle [62] [63] [64].
TNF-α signaling through its receptors activates both JNK and IKK-β pathways, leading to serine phosphorylation of IRS-1 instead of the normal tyrosine phosphorylation required for proper insulin signaling [62]. This aberrant phosphorylation impairs phosphoinositide 3-kinase (PI3K) activation and subsequent Akt2 signaling, ultimately inhibiting translocation of glucose transporter 4 (GLUT-4) to the plasma membrane and reducing cellular glucose uptake [62]. Simultaneously, IL-1β and free fatty acids acting through Toll-like receptor 4 (TLR4) activate IKK-β, which promotes nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB) translocation to the nucleus [63] [64]. NF-κB then induces transcription of numerous pro-inflammatory genes, including those encoding TNF-α, IL-6, and IL-1β, creating a self-sustaining inflammatory feedback loop [62]. Additionally, free fatty acids can be converted to diacylglycerols and ceramides, which activate protein kinase C (PKC) and inhibit Akt activity, respectively, further contributing to insulin resistance [62].
Experimental Methods for Cytokine Analysis
Study Population Designs
Research investigating cytokines in metabolic syndrome typically employs case-control designs with carefully defined participant groups. Studies generally recruit MetS patients based on standardized criteria, most commonly the International Diabetes Federation (IDF) definition in agreement with American Heart Association/National Heart, Lung and Blood Institute (AHA/NHLBI) criteria, which requires the presence of at least three of five metabolic abnormalities: elevated waist circumference, elevated triglycerides, reduced HDL cholesterol, elevated blood pressure, and elevated fasting glucose [68]. Control groups typically consist of healthy individuals with no components of MetS and matched for factors such as age and gender where possible [65]. Sample sizes in recent studies range from approximately 100-300 participants total, with MetS patients and controls often recruited in a 1:1 or 2:1 ratio [65] [68]. Exclusion criteria commonly include autoimmune diseases, acute infectious diseases, neurodegenerative disorders, cancer, cardiovascular diseases, and chronic liver or kidney diseases to minimize confounding inflammatory conditions [67] [68].
Blood Sampling and Cytokine Measurement
Blood collection for cytokine analysis follows standardized protocols to ensure sample integrity. Participants typically fast for 9-12 hours overnight before venous blood collection in the morning [47] [68]. Blood is collected in various tubes depending on subsequent analysis: EDTA tubes for plasma separation, serum separator tubes for cytokine analysis, and fluoride tubes for glucose measurement [67]. For cytokine measurements, samples are centrifuged at specified speeds (typically 2000-3000 × g for 10-15 minutes) to separate plasma or serum, which is then aliquoted and stored at -80°C until analysis to preserve cytokine stability [65].
The primary method for quantifying cytokine levels is enzyme-linked immunosorbent assay (ELISA), which provides sensitive and specific measurement of individual cytokines in serum or plasma. Commercial ELISA kits from manufacturers such as R&D Systems (Quantikine human IL-6 and TNF kits) and Bosterbio are commonly employed with sensitivity ranges of 4.69-300 pg/ml for IL-6 and 7.8-500 pg/ml for TNF-α [66] [65]. The assays are performed according to manufacturer protocols, typically involving incubation of samples in antibody-coated wells, followed by detection with enzyme-conjugated secondary antibodies and colorimetric substrate development [65]. Absorbance is measured using microplate readers such as the Stat Fax 2100, with cytokine concentrations calculated from standard curves [66]. For novel cytokines like IL-37 and PANDER, ELISA kits from specialized manufacturers such as Sunlong Biotech and MyBioSource are utilized [67].
Molecular Biology Techniques
Gene expression analysis of cytokines and their receptors provides complementary data to protein measurements. RNA is typically extracted from blood samples or specific tissues using commercial kits such as the Qiagen tissue extraction kit [67]. Reverse transcription converts RNA to cDNA, which is then amplified using real-time polymerase chain reaction (PCR) systems such as StepOnePlus with EvaGreen Supermix [67]. Primer sequences target specific genes of interest (e.g., for IL-37: Forward 5'-ACAGACCTCCTGCCTCAGAA-3', Reverse 5'-AAGGTGCTGGCAGTTGTTTT-3') with normalization to housekeeping genes like β-actin [67]. The threshold cycle (Ct) values are used to calculate relative mRNA expression using the 2^(-ΔΔCt) method [67].
For genetic association studies, DNA extraction from whole blood is performed using kits such as the Qia-amplification DNA extraction kit, with DNA quantification via spectrophotometry (e.g., NanoDrop 1000) [67]. Single nucleotide polymorphisms (SNPs) in cytokine genes are genotyped using TaqMan allelic discrimination assays on real-time PCR systems, with analysis using GeneMapper software [67].
Table 2: Key Methodologies for Cytokine Analysis in Metabolic Syndrome Research
| Method | Key Reagents/Equipment | Typical Parameters Measured | Advantages | Limitations |
|---|---|---|---|---|
| ELISA | Commercial ELISA kits (R&D Systems, Bosterbio), microplate reader | Serum/plasma concentrations of cytokines (pg/ml) | High specificity and sensitivity; quantitative; relatively simple protocol | Measures single analyte; may not reflect tissue-specific changes |
| Real-time PCR | RNA extraction kits, reverse transcriptase, SYBR Green/ TaqMan chemistry, real-time PCR system | mRNA expression levels of cytokines and receptors (relative expression) | High sensitivity; can detect low abundance transcripts; quantitative | mRNA levels may not correlate with protein levels; post-transcriptional modifications |
| Genetic Analysis | DNA extraction kits, TaqMan SNP genotyping assays, real-time PCR system | Single nucleotide polymorphisms in cytokine genes | Identifies genetic risk factors; can inform personalized medicine approaches | Complex data interpretation; small effect sizes for individual variants |
| Inflammatory Scores | Automated hematology analyzer, CRP measurement | INFLA-score (composite of CRP, WBC, platelets, NLR) | Integrates multiple inflammatory markers; better predictive value than single markers | May miss specific cytokine patterns; requires multiple measurements |
Quantitative Data Synthesis
Multiple studies have consistently demonstrated elevated pro-inflammatory cytokine levels in metabolic syndrome patients compared to healthy controls. As shown in Table 3, TNF-α and IL-6 show the most pronounced elevations, with TNF-α levels in MetS patients reaching nearly 9-fold higher than controls in some studies [65]. The relationship between cytokine levels and specific MetS components follows distinct patterns, with IL-6 showing stronger correlation with CRP levels, while TNF-α demonstrates more consistent elevation across different patient subgroups [66]. Recent research has also highlighted the significance of cytokine ratios and composite inflammation scores, such as the INFLA-score (based on CRP, white blood cell count, platelet count, and neutrophil-to-lymphocyte ratio), which shows a dose-response relationship with MetS and its components [47]. Each unit increase in INFLA-score associates with higher likelihood of developing MetS (OR = 1.08, 95% CI: 1.07-1.10), with those in the highest quartile having 3.58 times higher risk than those in the lowest quartile [47].
Table 3: Cytokine Levels in Metabolic Syndrome Patients vs. Controls
| Cytokine | MetS Patients | Healthy Controls | P-value | Study Population | Reference |
|---|---|---|---|---|---|
| TNF-α | 140.69 ± 10.40 pg/ml | 15.94 ± 0.89 pg/ml | <0.001 | 125 MetS patients vs. 125 controls (Iranian) | [65] |
| IL-6 | 98.14 ± 17.94 pg/ml | 4.6 ± 0.2 pg/ml | <0.001 | 125 MetS patients vs. 125 controls (Iranian) | [65] |
| TNF-α | Significantly higher in obese (P<0.001) | Lower in normal BMI | <0.001 | 80 obese vs. 53 normal BMI (Polish) | [66] |
| IL-6 | Significantly higher in obese women (P=0.001) | Lower in normal BMI | 0.001 (women) | 80 obese vs. 53 normal BMI (Polish) | [66] |
| TNF-α | Significantly elevated in MetS groups | Lower in healthy controls | <0.001 | 200 MetS patients vs. 100 controls (Egyptian) | [67] |
| PANDER | Significantly elevated in MetS groups | Lower in healthy controls | <0.001 | 200 MetS patients vs. 100 controls (Egyptian) | [67] |
| IL-37 | Significantly decreased in MetS groups | Higher in healthy controls | <0.001 | 200 MetS patients vs. 100 controls (Egyptian) | [67] |
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Cytokine Analysis in Metabolic Syndrome
| Reagent/Kit | Manufacturer Examples | Specific Application | Key Features |
|---|---|---|---|
| Quantikine ELISA Kits | R&D Systems | Measurement of human IL-6, TNF-α in serum/plasma | Sensitivity: 4.69-300 pg/ml (IL-6), 7.8-500 pg/ml (TNF-α); validated precision |
| Human PANDER ELISA Kit | Sunlong Biotech | Measurement of pancreatic-derived factor | Specifically detects human PANDER; useful for metabolic studies |
| Human IL-37 ELISA Kit | MyBioSource | Measurement of anti-inflammatory IL-37 | Quantifies this novel anti-inflammatory cytokine; research use only |
| RNA Extraction Kit | Qiagen | Isolation of total RNA from blood samples | High-quality RNA for gene expression studies; includes DNase treatment |
| TaqMan SNP Genotyping Assays | Applied Biosystems | Genetic analysis of cytokine polymorphisms | Designed for specific SNPs; compatible with real-time PCR systems |
| EvaGreen Supermix | Bio-Rad | Real-time PCR for cytokine mRNA quantification | Sensitive detection of amplification; no separate probe required |
| Tanita Body Composition Analyzer | Tanita | Assessment of body fat percentage, visceral fat | Medical grade (MDD CLASS IIa); integrates with metabolic parameters |
| Medifoxamine | Medifoxamine HCl | Medifoxamine is a withdrawn atypical antidepressant for research use only (RUO). Explore its dopaminergic/serotonergic mechanism and applications. Not for human use. | Bench Chemicals |
| Mefruside | Mefruside|Na+-Cl- Symporter Inhibitor|RUO | Bench Chemicals |
The intricate network of pro-inflammatory cytokines, particularly IL-1β, IL-6, and TNF-α, forms a critical pathological foundation in metabolic syndrome, creating self-sustaining inflammatory cycles that drive insulin resistance and metabolic dysfunction [62] [63]. The consistent elevation of these cytokines across diverse populations, along with the emerging roles of newer mediators like PANDER and IL-37, highlights their potential as both biomarkers and therapeutic targets [67] [65]. Future research should focus on developing multi-cytokine profiling panels that can better stratify MetS patients according to their inflammatory status, potentially guiding personalized treatment approaches [47] [68]. Furthermore, the development of specific antagonists targeting cytokine signaling pathways, particularly those downstream of TNF-α and IL-1β, represents a promising frontier for breaking the cycle of inflammation and insulin resistance in metabolic disease [62] [64]. As our understanding of the complex cytokine networks in MetS deepens, so too will our ability to intervene therapeutically in this widespread and debilitating condition.
Oxidative stress, characterized by an imbalance between the production of reactive oxygen species (ROS) and the body's antioxidant defenses, is a fundamental component in the pathogenesis of metabolic syndrome (MetS) and its related complications [69]. This biochemical phenomenon results in measurable damage to lipids, proteins, and DNA, driving chronic low-grade inflammation and tissue dysfunction [69] [70]. In MetS, a cluster of interrelated metabolic risk factors including abdominal obesity, dyslipidemia, hypertension, and insulin resistance creates a pro-oxidant state that perpetuates a vicious cycle of cellular damage and metabolic deterioration [71] [69]. The biomarkers of this damage—notably malondialdehyde (MDA) and F2-isoprostanes from lipid peroxidation, and 8-hydroxy-2'-deoxyguanosine (8-OHdG) from DNA oxidation—serve as critical objective indicators of oxidative stress intensity and have emerged as valuable tools for risk stratification, disease monitoring, and therapeutic development in metabolic disorder research [72] [71] [73].
Biomarker Profiles and Pathophysiological Significance
Lipid Peroxidation Biomarkers
Malondialdehyde (MDA) is one of the most extensively studied secondary products of polyunsaturated fatty acid peroxidation. It accumulates in tissues and biological fluids when oxidative stress overwhelms cellular defenses and serves as a reliable indicator of lipid peroxidation intensity [71] [73]. In metabolic syndrome research, MDA levels have demonstrated significant predictive value. A 2025 prospective study revealed that individuals with higher baseline MDA levels faced increased odds of developing incident chronic kidney disease (CKD) within one year, highlighting its prognostic relevance in MetS complications [71]. The study further identified positive correlations between urinary albumin-to-creatinine ratio (UACR)—a marker of renal damage—and both MDA and pro-inflammatory cytokines (IL-1β, TNFα), situating MDA within the inflammatory-oxidative cascade that characterizes MetS pathophysiology [71].
F2-isoprostanes are prostaglandin-like compounds formed through the non-enzymatic, free radical-mediated peroxidation of arachidonic acid. Their formation is not dependent on cyclooxygenase enzymes, making them specific markers of oxidative lipid damage [74] [73]. These stable compounds provide a more specific and reliable measure of lipid peroxidation than MDA in various pathological states [74] [73]. In recent research, F2-isoprostanes have shown diagnostic utility across multiple conditions linked to oxidative stress. A 2025 comparative cross-sectional study documented significantly elevated serum F2-isoprostanes in Alzheimer's disease patients (179.38 ± 3.01 pg/mL) compared to controls (85.89 ± 0.97 pg/mL), underscoring their sensitivity as oxidative stress markers in degenerative pathologies [73]. Additionally, their potential as markers in reproductive pathologies with an inflammatory basis, such as genitourinary infections and varicocele, is under investigation, suggesting broad applicability across tissue types and disease states [74].
DNA Damage Biomarkers
8-Hydroxy-2'-deoxyguanosine (8-OHdG) represents one of the most abundant and well-characterized products of DNA oxidation, formed when hydroxyl radicals and singlet oxygen attack the C8 position of deoxyguanosine in DNA [72] [75]. This modified nucleoside is excised and released into circulation and urine during DNA repair processes, making it a valuable non-invasive marker of cumulative oxidative DNA damage and cellular repair activity [72] [76]. As a biomarker, 8-OHdG provides critical insights into the genotoxic consequences of oxidative stress in metabolic disorders. Elevated 8-OHdG levels have been consistently documented in type 2 diabetes and even in prediabetic states, often with greater sensitivity than traditional metabolic indicators [72]. The marker increases further in patients with advanced diabetic complications like proliferative retinopathy and nephropathy, positioning it as a potential tool for monitoring disease progression and complication risk in MetS [72].
Table 1: Characteristic Values of Oxidative Stress Biomarkers in Health and Disease
| Biomarker | Healthy Controls | Disease States | Significance |
|---|---|---|---|
| MDA | 2.23 ± 0.16 nmol/mL (controls) [73] | 5.73 ± 0.31 nmol/mL (Alzheimer's patients) [73] | Increases with oxidative stress intensity; predicts CKD risk in MetS [71] |
| F2-Isoprostanes | 85.89 ± 0.97 pg/mL (controls) [73] | 179.38 ± 3.01 pg/mL (Alzheimer's patients) [73] | Specific marker of lipid peroxidation; elevated in degenerative diseases [74] [73] |
| 8-OHdG (Urinary) | 29.6 ± 24.5 ng/mg creatinine (men); 43.9 ± 42.1 ng/mg creatinine (women) [72] | >1.5 nmol/mmol creatinine associated with 3.68× higher colorectal cancer risk [72] | Marker of oxidative DNA damage; elevated in cancer, diabetes, neurodegeneration [72] |
| 8-OHdG (Optimal) | 0-5.2 ng/mg creatinine [72] | N/A | Target range for optimal health [72] |
Analytical Methodologies
Sample Preparation and Extraction
Robust sample preparation is fundamental to reliable quantification of oxidative stress biomarkers. For MDA measurement, collection of fasting serum or plasma samples in appropriate anticoagulant tubes is standard, with immediate processing and storage at -80°C to prevent ex vivo oxidation [71]. For F2-isoprostanes analysis, blood should be collected in serum separator tubes, allowed to clot at room temperature for 30 minutes, centrifuged at 1000 × g for 15 minutes, with aliquoted serum stored at -80°C [73]. 8-OHdG can be measured in both urine and plasma, with urine collection being particularly advantageous for non-invasive assessment of cumulative DNA damage [72] [75]. For urinary 8-OHdG, samples should be centrifuged to remove particulates, and creatinine correction should be applied to account for variations in urine concentration [72].
Solid-phase extraction (SPE) has emerged as a powerful sample preparation technique, particularly for simultaneous analysis of multiple biomarkers. A validated protocol for cotinine and 8-OHdG quantification illustrates this approach: 100 μL of urine is mixed with 100 μL of internal standard (e.g., 8-OHdG-15N5 at 5 ng/mL) and 800 μL of 10 mM ammonium formate in 0.1% formic acid [75]. The SPE cartridge (Oasis HLB 30 μm, 30 mg) is preconditioned with 1 mL methanol and equilibrated with 1 mL water before sample loading. After loading, the cartridge is washed with 1 mL water and analytes are eluted with 1 mL methanol. The eluate is evaporated under nitrogen and reconstituted in 300 μL of 50% acetonitrile, followed by filtration (0.2 μm) prior to analysis [75].
Quantification Techniques
Chromatographic Methods offer superior specificity and sensitivity for biomarker quantification. Liquid chromatography-tandem mass spectrometry (LC-MS/MS) has become the gold standard for 8-OHdG and F2-isoprostanes measurement due to high selectivity and low detection limits [75] [76]. A recently developed LC-MS/MS method for simultaneous 8-OHdG and cotinine analysis achieved detection limits of 0.5 ng/mL for 8-OHdG and 0.23 ng/mL for cotinine, with excellent reproducibility across laboratories (Pearson correlation and intraclass correlation coefficients >0.9) [75]. The analytical conditions employed a HILIC column (150 × 2.1 mm) with gradient elution (5-40% ammonium formate in 0.1% formic acid over 2.5 minutes) at 0.25 mL/min flow rate [75]. Multiple reaction monitoring (MRM) in positive ion mode tracked transitions of m/z 284.30→167.90 for 8-OHdG and m/z 177.20→97.90 for cotinine [75].
Immunoassays provide accessible alternatives for high-throughput analysis. Enzyme-linked immunosorbent assays (ELISA) are widely used for MDA, F2-isoprostanes, and 8-OHdG quantification, offering practical advantages in clinical settings without requiring sophisticated instrumentation [73] [76]. Recent advances include the development of highly specific antibodies against 8-OHdG that enable automated evaluation via fluorescence and confocal microscopy in cells and tissues, expanding applications to histological samples [76]. However, immunoassays may show greater variability and cross-reactivity compared to chromatographic methods, necessitating careful validation against established reference methods.
Table 2: Advanced Analytical Methods for Oxidative Stress Biomarkers
| Method | Biomarkers | Key Parameters | Advantages | Limitations |
|---|---|---|---|---|
| LC-MS/MS [75] | 8-OHdG, F2-isoprostanes, MDA | LOD: 0.5 ng/mL (8-OHdG); 0.23 ng/mL (cotinine); Column: HILIC; MRM detection | High specificity and sensitivity; simultaneous multi-analyte quantification | Expensive instrumentation; technical expertise required |
| GC-MS [75] | MDA, F2-isoprostanes | Requires derivatization; electron impact ionization | High resolution; excellent sensitivity for volatile compounds | Complex sample preparation; thermal degradation possible |
| HPLC-ECD/UV [75] | 8-OHdG, MDA | Electrochemical or UV detection; C18 columns | Widely accessible; good sensitivity for targeted analysis | Limited multiplexing capability; potential interferences |
| ELISA [73] [76] | All three biomarkers | Commercial kits; colorimetric/fluorimetric detection | High throughput; minimal technical training required | Antibody cross-reactivity; less quantitative than MS |
Signaling Pathways in Metabolic Syndrome
The interplay between oxidative stress biomarkers and metabolic syndrome pathophysiology involves complex signaling pathways that create and perpetuate chronic low-grade inflammation. The diagram below illustrates key mechanistic relationships between lipid peroxidation products, DNA damage markers, and metabolic dysfunction.
Oxidative Stress Pathways in Metabolic Syndrome. This diagram illustrates how metabolic syndrome creates an oxidative microenvironment that drives lipid peroxidation (MDA, F2-isoprostanes) and DNA damage (8-OHdG), perpetuating chronic inflammation and metabolic complications through interconnected pathways. The self-amplifying cycle between ROS production, inflammation, and impaired Nrf2 signaling creates a pathological feedback loop that accelerates tissue damage and disease progression [71] [69] [70].
Within this framework, specific mechanistic interactions warrant emphasis. MDA promotes dysfunctional high-density lipoprotein (HDL) particles and correlates positively with urinary albumin-to-creatinine ratio (UACR) and pro-inflammatory cytokines (IL-1β, TNFα) in MetS, contributing directly to renal impairment in CKD progression [71]. F2-isoprostanes act as potent vasoconstrictors and amplify inflammatory signaling through receptor-dependent mechanisms, creating a feed-forward loop of oxidative damage and inflammation [74] [73]. 8-OHdG accumulation reflects the genotoxic consequences of this microenvironment, with elevated levels signifying inadequate DNA repair capacity and increased mutation risk—particularly dangerous when damage escapes repair before cell division, leading to permanent genetic alterations that drive cancer development and disease progression in MetS [72].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Oxidative Stress Biomarker Analysis
| Reagent/Category | Specific Examples | Research Application | Technical Notes |
|---|---|---|---|
| Internal Standards | Cotinine-d3, 8-OHdG-15N5 [75] | Isotope dilution for LC-MS/MS quantification | Corrects for extraction efficiency and matrix effects; essential for precision |
| SPE Cartridges | Oasis HLB 96-well plate 30 μm (30 mg) [75] | Sample clean-up and analyte concentration | Precondition with methanol, equilibrate with water; enables high-throughput processing |
| Chromatography Columns | Kinetex 2.6 μm HILIC (100 Å, 150 × 2.1 mm) [75] | Hydrophilic interaction liquid chromatography | Ideal for polar biomarkers like 8-OHdG; compatible with MS detection |
| ELISA Kits | Commercial F2-isoprostanes, MDA, 8-OHdG kits [73] [76] | High-throughput screening | Validate against reference methods; watch for cross-reactivity in complex matrices |
| Antibodies | Anti-8-OHdG (self-developed and commercial) [76] | Immunohistochemistry and immunofluorescence | Enable cellular localization; suitable for automated microscopy in cells/tissues |
| Mobile Phase Additives | Ammonium formate, formic acid [75] | LC-MS/MS analysis | Enhance ionization efficiency; 10 mM ammonium formate in 0.1% formic acid recommended |
| Antioxidant Supplements | Vitamin E, Vitamin C, Coenzyme Q10 [72] | Intervention studies | Vitamin E (200 IU daily) reduced 8-OHdG by 33.8% in smokers; demonstrates biomarker utility |
| Megazol | Megazol, CAS:19622-55-0, MF:C6H6N6O2S, MW:226.22 g/mol | Chemical Reagent | Bench Chemicals |
| Meleagrin | Meleagrin is a natural alkaloid for research into cancer, pulmonary fibrosis, and antibiotic mechanisms. For Research Use Only. Not for human use. | Bench Chemicals |
Experimental Workflow: From Sample to Data
The comprehensive analysis of oxidative stress biomarkers requires systematic workflows that ensure sample integrity and analytical validity. The following diagram outlines a standardized approach from specimen collection through data interpretation, integrating methodologies from recent studies.
Biomarker Analysis Workflow. This diagram outlines the standardized pathway from biological sample collection through data interpretation for oxidative stress biomarker quantification, incorporating methodologies validated in recent studies [72] [73] [75]. The workflow emphasizes critical pre-analytical steps that significantly impact biomarker stability, particularly immediate processing and storage at -80°C to prevent ex vivo oxidation.
For researchers implementing this workflow, several technical considerations are paramount. The sample collection phase should involve fasting blood draws for serum/plasma biomarkers and first-morning urine collections for 8-OHdG measurement, with appropriate additives (EDTA, citrate) for plasma separation [72] [71]. During solid-phase extraction, maintaining consistent flow rates (<1 mL/min) and complete cartridge preconditioning (1 mL methanol followed by 1 mL water) is critical for reproducible recovery rates [75]. For LC-MS/MS analysis, the use of HILIC chromatography with gradient elution (5-40% aqueous phase over 2.5 minutes) provides optimal separation of hydrophilic biomarkers like 8-OHdG, while MRM monitoring of specific transitions (m/z 284.30→167.90 for 8-OHdG) ensures high specificity in complex biological matrices [75]. Data processing must include appropriate normalization—creatinine correction for urinary biomarkers and volume adjustment for serum/plasma biomarkers—with quality controls spanning the analytical range to monitor assay performance [72] [75].
The integration of MDA, F2-isoprostanes, and 8-OHdG as complementary oxidative stress biomarkers provides a powerful framework for investigating the molecular pathophysiology of metabolic syndrome. These biomarkers offer distinct yet interconnected perspectives on the oxidative damage landscape: MDA reflecting general lipid peroxidation, F2-isoprostanes providing specific assessment of arachidonic acid oxidation, and 8-OHdG quantifying cumulative DNA damage. Their measurement through validated methodologies—particularly LC-MS/MS for reference analysis and ELISA for high-throughput applications—enables precise quantification of oxidative stress intensity in research and clinical contexts. As the understanding of low-grade chronic inflammation in MetS deepens, these biomarkers will play increasingly important roles in patient stratification, therapeutic monitoring, and the development of targeted interventions that address the underlying oxidative mechanisms driving metabolic disease progression.
Metabolomics has emerged as a powerful analytical approach for systematically studying the unique chemical fingerprints left by specific cellular processes, providing unparalleled insights into inflammatory pathways. This field comprehensively measures small molecule metabolites (<1,500 Da) that represent the functional outputs of biological systems, capturing the dynamic metabolic state influenced by genetics, environment, and disease pathology. In the context of inflammation, metabolomic analyses reveal how immune activation and inflammatory mediators reprogram cellular metabolism, offering crucial insights into disease mechanisms and potential therapeutic targets. The integration of mass spectrometry (MS) and nuclear magnetic resonance (NMR) spectroscopy has proven particularly valuable for identifying metabolic signatures of low-grade chronic inflammation, a key driver in metabolic syndrome and related disorders [77].
Chronic low-grade inflammation represents a persistent, subclinical immune activation that serves as a fundamental pathological process underlying many metabolic disorders. Unlike acute inflammation that resolves rapidly, this sustained inflammatory state creates a self-perpetuating cycle of metabolic dysregulation and tissue damage. Metabolomic technologies now enable researchers to detect subtle alterations in metabolic pathways long before clinical symptoms of metabolic syndrome manifest, providing opportunities for early intervention [78]. The application of MS and NMR to biofluids and tissues offers a window into the intricate relationships between nutrient metabolism, immune cell function, and inflammatory signaling, making these technologies indispensable for modern metabolic research [2].
Technical Foundations of Metabolomic Technologies
Nuclear Magnetic Resonance (NMR) Spectroscopy
NMR spectroscopy exploits the magnetic properties of atomic nuclei to determine the structure and concentration of metabolites in complex biological samples. When placed in a strong magnetic field, nuclei such as 1H, 13C, or 31P absorb and re-emit electromagnetic radiation at frequencies characteristic of their molecular environment. 1H-NMR is particularly valuable for metabolomic studies because of its ability to detect all protons in a sample, providing a comprehensive metabolic profile without requiring prior knowledge of metabolite composition [79].
Modern NMR systems for metabolomics typically employ high-field magnets (500-900 MHz) equipped with cryogenically cooled probes that significantly enhance sensitivity by reducing thermal noise. The Carr-Purcell-Meiboom-Gill (CPMG) pulse sequence is routinely applied to suppress signals from macromolecules like proteins and lipoproteins, thereby highlighting small molecule metabolites [79] [80]. For sample preparation, minimal processing is required—often just dilution with deuterated buffer (e.g., 200 mM sodium phosphate pH 7.4 in 20% 2H2O) to provide a field frequency lock, followed by centrifugation to remove particulates [79]. This straightforward preparation makes NMR highly reproducible and ideal for high-throughput clinical applications.
A significant advantage of NMR is its non-destructive nature, allowing repeated analysis of the same sample or subsequent analysis using other techniques. NMR provides direct quantitative information based on peak intensities, requires no chromatographic separation, and excels at identifying isomers and structurally similar compounds. Recent methodological advances include dynamic nuclear polarization for sensitivity enhancement and 2D NMR experiments (e.g., 1H-1H COSY, 1H-13C HSQC) for resolving overlapping signals in complex biological mixtures [81].
Mass Spectrometry (MS) Platforms
Mass spectrometry-based metabolomics measures the mass-to-charge ratio (m/z) of ionized metabolites, providing exceptional sensitivity and specificity for comprehensive metabolic profiling. MS platforms typically couple liquid chromatography (LC) or gas chromatography (GC) separation with mass detection, enabling analysis of thousands of metabolites in a single run. LC-MS is particularly well-suited for polar and thermally labile compounds, while GC-MS offers superior separation efficiency for volatile and chemically derivatizable metabolites [81].
The technical workflow begins with metabolite extraction using organic solvents (e.g., methanol, acetonitrile) to precipitate proteins while maintaining metabolic integrity. Following chromatographic separation, metabolites are ionized using techniques such as electrospray ionization (ESI) or atmospheric pressure chemical ionization (APCI). The mass analyzers then separate ions based on their m/z ratios, with time-of-flight (TOF), Orbitrap, and triple quadrupole instruments being most common in metabolomics. TOF and Orbitrap systems provide high mass accuracy and resolution for untargeted discovery, while triple quadrupole instruments offer superior sensitivity for targeted quantification using selected reaction monitoring (SRM) [81].
Key advantages of MS include its exceptional sensitivity (detecting metabolites at femtomolar to attomolar concentrations), high throughput capability, and broad dynamic range. Recent technological innovations such as ion mobility separation add an additional dimension of separation based on molecular shape and size, while imaging MS enables spatial resolution of metabolite distributions in tissues [81]. The primary limitations include more extensive sample preparation, matrix effects that can suppress ionization, and the challenge of annotating unknown metabolites from complex spectra.
Table 1: Comparison of NMR and MS Platforms for Metabolomic Analysis
| Feature | NMR Spectroscopy | Mass Spectrometry |
|---|---|---|
| Detection Limit | μM-mM range | pM-nM range |
| Sample Preparation | Minimal (dilution) | Extensive (extraction, derivatization) |
| Quantitation | Absolute without standards | Relative (requires standards for absolute) |
| Reproducibility | High (<2% variance) | Moderate (5-20% variance) |
| Structural Insight | High (determines structure) | Limited (requires standards/MSn) |
| Throughput | Moderate (10-20 min/sample) | High (1-10 min/sample) |
| Key Strengths | Non-destructive, reproducible, identifies unknowns | Highly sensitive, comprehensive coverage, imaging capability |
| Primary Limitations | Lower sensitivity, limited dynamic range | Matrix effects, destructive, annotation challenges |
Complementary Applications in Inflammation Research
NMR and MS provide complementary insights when applied to inflammatory conditions. NMR excels at detecting and quantifying abundant metabolites involved in central carbon metabolism, such as organic acids, amino acids, and carbohydrates, making it ideal for monitoring energetic pathways reprogrammed during inflammation [80]. MS extends coverage to low-abundance signaling molecules, including eicosanoids, specialized pro-resolving mediators, and oxidative stress markers that play crucial roles in inflammatory processes [78].
Integrated approaches that combine both technologies maximize metabolic coverage. For example, NMR can provide rapid metabolic phenotyping of biofluids to identify samples of interest, which are then subjected to deep molecular profiling via MS. This synergistic application has proven particularly powerful for elucidating the complex metabolic adaptations in chronic inflammatory diseases, including the interplay between glycolysis, TCA cycle flux, and phospholipid metabolism in activated immune cells [77].
Metabolomic Signatures in Inflammatory Diseases
Rheumatoid Arthritis and Autoimmune Inflammation
Rheumatomic studies of rheumatoid arthritis (RA) reveal profound disturbances in energy and lipid metabolism that correlate with disease activity and treatment response. NMR-based analysis of RA synovial fluid demonstrates significant depletion of key metabolites in energy pathways compared to osteoarthritis, including reduced glucose, pyruvate, and lactate, reflecting the highly metabolic nature of inflamed synovium with increased nutrient consumption [80]. Additionally, RA synovial fluid shows elevated levels of acetate, succinate, and branched-chain amino acids, suggesting increased protein catabolism and mitochondrial dysfunction [80].
Serum metabolomics has identified distinct signatures that differentiate TNF inhibitor responders from non-responders prior to treatment initiation. Key predictive metabolites include 2-hydroxyisovaleric acid, acetoacetic acid, mobile lipids, alanine, and leucine, which collectively achieved 83.1% balanced accuracy in classifying future response [79]. These findings suggest that pre-treatment metabolic states influence therapeutic outcomes, potentially due to underlying differences in inflammatory pathways or mitochondrial function. FTIR spectroscopy further complements these findings by identifying spectral differences in the 1000-1200 cm−1 region (carbohydrates and nucleic acids) that distinguish RA patients from healthy controls, and in the 1600-1700 cm−1 region that predicts TNF inhibitor response [79].
Table 2: Key Metabolite Alterations in Inflammatory Diseases
| Metabolite | Inflammatory Condition | Direction of Change | Biological Interpretation |
|---|---|---|---|
| Lactate | RA, Crohn's disease, Multiple sclerosis | Increased | Enhanced glycolysis (Warburg effect) in immune cells |
| Succinate | RA, Obesity | Increased | TCA cycle disruption, HIF-1α stabilization |
| BCAAs | RA, Metabolic syndrome | Increased/Decreased | Muscle proteolysis, insulin resistance |
| Taurine | Osteoarthritis | Increased | Subchondral bone sclerosis, antioxidant response |
| N-acetyl glycoprotein | Crohn's disease | Increased | Acute phase protein glycosylation |
| Arachidonic acid | Chronic inflammation | Increased | Eicosanoid precursor, pro-inflammatory signaling |
| EPA-derived lipids | Chronic inflammation | Decreased | Reduced anti-inflammatory mediators |
Crohn's Disease and Inflammatory Bowel Disease
In Crohn's disease, NMR-based plasma metabolomics identifies a distinct inflammatory signature characterized by elevated N-acetyl glycoprotein, glycerol, and phenylalanine that strongly correlates with C-reactive protein levels (R² = 0.62) [82]. This metabolic signature was independently validated using machine learning approaches to classify patients with active inflammation (CRP ≥ 5 mg/L), confirming its robustness as an indicator of disease activity. Importantly, integration of metabolomic data with whole exome sequencing revealed that this inflammatory metabolomic profile correlates with pathogenic mutation burden in genes regulating pro-inflammatory signaling pathways, particularly those functioning within "intrinsic component of membrane" and "inflammatory bowel disease" pathways [82].
The study further demonstrated that specific spectral regions in NMR profiles could non-invasively monitor treatment response and disease progression, offering potential clinical utility for managing therapeutic interventions. The correlation between metabolic profiles and genetic markers highlights how integrating multi-omics data can elucidate the functional consequences of genetic susceptibility variants in complex inflammatory diseases [82].
Low-Grade Inflammation in Metabolic Syndrome
Metabolic syndrome represents a cluster of conditions characterized by central obesity, dyslipidemia, hypertension, and insulin resistance, with chronic low-grade inflammation as a common pathogenic thread. The INFLA-score, a composite index based on C-reactive protein, white blood cell count, platelet count, and neutrophil-to-lymphocyte ratio, provides a integrated measure of this inflammatory state [5]. Research demonstrates that each unit increase in INFLA-score corresponds to an 8% higher likelihood of metabolic syndrome (OR = 1.08, 95% CI: 1.07–1.10), with those in the highest INFLA-score quartile having a 3.58-fold increased risk compared to the lowest quartile [5].
Metabolomic studies reveal that this low-grade inflammatory state associates with distinct alterations in phospholipid metabolism, including elevated lysophosphatidylcholines, sphingomyelins, and ceramides that promote insulin resistance through inhibition of insulin signaling pathways [29]. Additionally, shifts in mitochondrial metabolism reduce fatty acid β-oxidation and increase diacylglycerol accumulation, further exacerbating metabolic dysfunction. The interplay between inflammation and mitochondrial function creates a self-reinforcing cycle where inflammatory cytokines impair mitochondrial oxidative capacity, leading to increased reactive oxygen species production that further amplifies inflammatory signaling through activation of the NLRP3 inflammasome [29].
Methodological Protocols for Inflammation-Focused Metabolomics
Sample Preparation Protocols
Serum Collection for NMR Analysis (adapted from [79]):
- Collect approximately 9 mL whole blood into Z serum clot activator tubes
- Rest at room temperature (20-25°C) for 30 minutes for clot formation
- Centrifuge at 1,500 ×g for 15 minutes to separate serum
- Aliquot 1 mL supernatant and snap-freeze in liquid nitrogen
- Store at -80°C until analysis
- Prior to NMR, thaw samples on ice for 30 minutes
- Mix 120 μL serum with 120 μL buffer master mix (200 mM sodium phosphate pH 7.4 in 20% 2H2O and 2.4 mM NaN3)
- Centrifuge at 21,500 ×g for 5 minutes at 4°C
- Transfer 200 μL supernatant to 3 mm NMR tubes
Synovial Fluid Preparation for NMR (adapted from [80]):
- Aspirate synovial fluid into heparinized tubes
- Process within 1 hour of collection
- Centrifuge at >2,000 ×g for 5 minutes to remove cells and debris
- Aliquot and store cell-free supernatant at -20°C
- For NMR analysis, thaw 100 μL synovial fluid on ice
- Dilute with 80 μL ddH2O (18.2 MΩ), 20 μL 1 M PO43- pH7.4 buffer in deuterium oxide, and 0.005 μL sodium azide
- Vortex for 1 minute, centrifuge at 13,000 ×g for 2 minutes at 4°C
- Transfer 190 μL to 3 mm NMR tubes
Plasma Preparation for MS-Based Metabolomics (adapted from [82]):
- Collect peripheral venous blood in EDTA tubes
- Centrifuge at 2,000 RPM for 10 minutes at 4°C
- Carefully extract plasma layer above buffy coat
- Immediately snap-freeze and store at -80°C
- For MS analysis, thaw plasma on ice
- Precipitate proteins with cold methanol (3:1 ratio)
- Vortex vigorously for 30 seconds, incubate at -20°C for 1 hour
- Centrifuge at 14,000 ×g for 15 minutes at 4°C
- Collect supernatant and evaporate under nitrogen stream
- Reconstitute in MS-compatible solvent for analysis
Instrumental Analysis Parameters
NMR Spectroscopy Conditions (adapted from [79] [80]):
- Instrument: Bruker 700 MHz spectrometer with TCI Cryoprobe
- Temperature: 37°C for serum, 297°K for plasma
- Pulse sequence: 1D CPMG (cpmgpr1d) with presaturation for water suppression
- Spectral width: 19,607 Hz (15 ppm)
- Data points: 32-65K
- Scans: 256 transients with 8 dummy scans
- Echo time: 9.6 ms (CPMG)
- Relaxation delay: 3.1 seconds
- Reference: Glucose anomeric proton at δ 5.223 ppm
LC-MS Typical Conditions (representative parameters):
- Chromatography: Reversed-phase C18 column (100 × 2.1 mm, 1.7-1.8 μm)
- Mobile phase: A) Water with 0.1% formic acid; B) Acetonitrile with 0.1% formic acid
- Gradient: 1-99% B over 15-20 minutes
- Flow rate: 0.3-0.4 mL/min
- Ionization: ESI positive/negative switching mode
- Mass analyzer: Q-TOF or Orbitrap
- Resolution: >30,000 FWHM
- Mass range: m/z 50-1,200
Data Processing and Statistical Analysis
Raw NMR data processing typically includes:
- Fourier transformation with exponential line broadening (0.3-1.0 Hz)
- Phase and baseline correction
- Chemical shift referencing to internal standard or known metabolite
- Spectral binning/bucketing (0.01-0.04 ppm regions)
- Normalization (probabilistic quotient normalization, median normalization)
- Scaling (unit variance, Pareto scaling)
MS data processing workflow:
- Raw data conversion to open formats (mzML, mzXML)
- Peak picking, alignment, and retention time correction
- Feature detection and deisotoping
- Peak integration and quantification
- Missing value imputation (KNN, minimum value)
- Normalization (internal standards, probabilistic quotient)
Multivariate statistical analysis:
- Unsupervised methods: Principal Component Analysis (PCA) for quality control and outlier detection
- Supervised methods: Partial Least Squares-Discriminant Analysis (PLS-DA), Orthogonal Projections to Latent Structures (OPLS) for class separation
- Validation: Cross-validation (7-fold, leave-one-out) and permutation testing
- Univariate statistics: Student's t-test with False Discovery Rate (FDR) correction
- Machine learning: Random Forest, Support Vector Machines for classification
Metabolic Pathways in Inflammation
Inflammatory signaling reprograms cellular metabolism through multiple interconnected pathways that support immune cell function and tissue remodeling. The Warburg effect, characterized by increased glycolysis even under normoxic conditions, provides rapid ATP generation and biosynthetic precursors for proliferating immune cells [77]. This metabolic adaptation is driven by stabilization of hypoxia-inducible factor (HIF)-1α under inflammatory conditions, which upregulates glycolytic enzymes and lactate dehydrogenase A, resulting in lactate accumulation—a consistent finding in inflammatory environments ranging from rheumatoid joints to diabetic foot ulcers [77].
Mitochondrial dysfunction represents another hallmark of chronic inflammation, with impaired oxidative phosphorylation and increased reactive oxygen species production creating a feed-forward loop that sustains inflammatory signaling. In obesity-driven metabolic disorders, this manifests as reduced fatty acid β-oxidation and accumulation of lipid intermediates (diacylglycerols, ceramides) that activate stress kinases and inhibit insulin signaling [29]. Additionally, disturbances in amino acid metabolism, particularly increased catabolism of tryptophan and branched-chain amino acids, contribute to both immune dysfunction and metabolic impairments in chronic inflammatory states.
The NLRP3 inflammasome serves as a critical integrator of metabolic and inflammatory signals, becoming activated by mitochondrial reactive oxygen species, ceramides, and other metabolic danger signals. This activation triggers IL-1β and IL-18 maturation, propagating inflammatory responses that further disrupt metabolic homeostasis [29]. Understanding these interconnected pathways provides opportunities for therapeutic interventions targeting metabolic-inflammatory cross-talk.
Diagram 1: Metabolic-Inflammatory Cross-talk in Chronic Disease. This diagram illustrates the key feedback loops connecting metabolic dysregulation and chronic inflammation, highlighting the central roles of glycolytic shift, mitochondrial dysfunction, and NLRP3 inflammasome activation.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for Inflammation Metabolomics
| Reagent/Material | Application | Function | Example Specifications |
|---|---|---|---|
| Deuterated Solvents | NMR spectroscopy | Provides field frequency lock; minimizes solvent signal | D2O (99.9% deuterium); deuterated methanol, chloroform |
| Internal Standards | Quantitation (MS/NMR) | Normalization; quality control; retention time markers | DSS-d6, TSP-d4 (NMR); isotopically labeled internal standards (MS) |
| Protein Precipitation Reagents | Sample preparation | Remove proteins; stabilize metabolites | Cold methanol, acetonitrile (MS); organic solvents |
| Chemical Derivatization Kits | GC-MS analysis | Enhance volatility; improve detection | MSTFA, BSTFA + TMCS; methoxyamine hydrochloride |
| Solid Phase Extraction | Sample cleanup | Fractionate; concentrate; remove interferents | C18, HILIC, ion exchange cartridges |
| Quality Control Pools | Method validation | Monitor instrument performance; normalize data | Pooled reference serum/plasma; NIST SRM 1950 |
| Metabolite Libraries | Compound identification | Annotate peaks; quantify metabolites | Commercial libraries (HMDB, MassBank); in-house databases |
| Chromatography Columns | LC-MS separation | Resolve metabolite mixtures | C18, HILIC, phenyl columns (1.7-2.1mm ID) |
| Buffer Systems | NMR sample prep | Maintain pH; provide reference | Sodium phosphate buffer (pH 7.4) in D2O |
| Cryogenic Probes | NMR sensitivity | Enhance signal-to-noise; reduce detection limits | Bruker TCI CryoProbe; Agilent OneProbe |
| Melianol | Melianol, CAS:16838-01-0, MF:C30H48O4, MW:472.7 g/mol | Chemical Reagent | Bench Chemicals |
| Memoquin | Memoquin, MF:C38H56N4O4, MW:632.9 g/mol | Chemical Reagent | Bench Chemicals |
Future Directions and Clinical Applications
The integration of metabolomics with other omics technologies (genomics, transcriptomics, proteomics) represents the next frontier in understanding inflammatory diseases. This multi-omics approach enables researchers to connect genetic susceptibility variants with functional metabolic consequences, providing a systems-level view of disease pathogenesis [82]. For example, combining whole exome sequencing with plasma metabolomics has revealed how pathogenic mutations in pro-inflammatory signaling genes correlate with specific metabolic signatures in Crohn's disease [82]. Similar approaches applied to metabolic syndrome could elucidate how genetic risk factors interact with environmental triggers to drive disease progression through inflammatory mechanisms.
Advanced machine learning and artificial intelligence algorithms are increasingly being applied to metabolomic data to develop predictive models of disease progression and treatment response. Random Forest classifiers have successfully identified inflammatory status in Crohn's disease patients based on NMR metabolic profiles [82], while OPLS modeling has predicted TNF inhibitor response in rheumatoid arthritis with over 83% accuracy [79]. As these computational methods mature, they offer the potential for clinically actionable tools to guide personalized treatment strategies for inflammatory conditions.
The concept of precision nutrition represents another promising application, where metabolomic profiling could guide dietary interventions to modulate inflammatory pathways. Research has demonstrated that high-fiber and fermented-food-enriched diets modulate gut microbiota composition and reduce serum inflammatory proteins [78], while omega-3 fatty acids compete with arachidonic acid metabolism to produce less inflammatory derivatives [77]. Metabolomic monitoring could potentially identify individuals most likely to benefit from specific nutritional interventions and track their biochemical responses, moving beyond one-size-fits-all dietary recommendations.
Diagram 2: Integrated Workflow for Inflammation Metabolomics. This diagram outlines the comprehensive pipeline from sample collection to clinical application, highlighting the integration of multi-omics data and machine learning for precision medicine approaches.
From a clinical translation perspective, metabolomics offers significant potential for developing biomarker panels that can detect early-stage metabolic syndrome before overt clinical manifestations appear. The INFLA-score demonstrates how integrating multiple inflammatory markers provides superior risk stratification compared to individual measurements [5]. Similarly, metabolic signatures could complement existing clinical parameters to improve diagnosis, prognosis, and therapeutic monitoring of chronic inflammatory conditions. The ongoing development of portable analytical technologies such as FTIR spectroscopy [79] may eventually enable point-of-care metabolic profiling, making metabolomic insights more accessible in routine clinical practice.
In conclusion, MS and NMR spectroscopy provide complementary and powerful approaches for elucidating the complex metabolic adaptations in inflammatory states. The continued refinement of these technologies, combined with advanced computational methods and multi-omics integration, promises to accelerate our understanding of the fundamental connections between metabolism and inflammation, ultimately enabling more effective strategies for preventing and treating metabolic syndrome and related disorders.
Metabolic syndrome (MetS) is a cluster of conditions—including central obesity, dyslipidemia, hypertension, and insulin resistance—that significantly elevates the risk of cardiovascular disease and type 2 diabetes [2]. A key pathophysiological feature underpinning MetS is chronic low-grade inflammation, characterized by a persistent, systemic increase in pro-inflammatory mediators [29] [7]. Traditional methods for monitoring this inflammatory state rely heavily on blood-based biomarkers, which involve invasive collection procedures that can be stressful for patients and unsuitable for frequent monitoring [83].
Saliva is emerging as a compelling alternative diagnostic medium, reflecting the body's physiological status through a complex mixture of biomarkers [84] [85]. Salivary glands are highly vascularized, allowing molecules from the blood to enter saliva via passive diffusion or active transport, thereby creating a close correlation between salivary and serum concentrations for many analytes [84] [86]. The non-invasive, cost-effective, and simple nature of saliva collection presents a significant advantage for both clinical diagnostics and large-scale research, particularly for the repeated measurements needed to track the chronic inflammatory processes in MetS [84] [83] [86]. This whitepaper details the latest salivary biomarkers and technologies for detecting chronic inflammation, providing a technical guide for researchers and drug development professionals working within the context of metabolic syndrome.
Salivary Biomarkers of Chronic Inflammation
Chronic inflammation associated with Metabolic Syndrome can be detected and monitored through several classes of biomarkers present in saliva. The following table summarizes the key inflammatory biomarkers, their mechanisms, and their significance in the context of MetS.
Table 1: Key Salivary Biomarkers for Chronic Inflammation in Metabolic Syndrome
| Biomarker Category | Specific Biomarkers | Pathophysiological Role in Inflammation/MetS | Detection Methods |
|---|---|---|---|
| Inflammatory Cytokines | IL-6, IL-1β, TNF-α, IL-8 [84] [87] | Produced by immune and adipose tissues; promote insulin resistance, endothelial dysfunction, and atherosclerosis [84] [29]. | ELISA, Multiplex Immunoassays, Biosensors [86] [87] |
| Acute Phase Proteins | C-Reactive Protein (CRP) [84] | A classic systemic inflammation marker; elevated in obesity and correlates with cardiovascular risk in MetS [84] [7]. | ELISA, Latex-enhanced Immunoassays |
| Pro-inflammatory Enzymes | Matrix Metalloproteinases (MMP-8, MMP-9) [86] [87] | Involved in tissue remodeling and inflammation; elevated levels linked to periodontitis (a common comorbidity in MetS) and systemic inflammation [86]. | Gel Zymography, Fluorescent Peptide Assays |
| Oxidative Stress Markers | Malondialdehyde (MDA), 8-isoprostane [84] [86] | Products of lipid peroxidation; indicate oxidative damage, which is a key driver of inflammation and insulin resistance in MetS [84] [29]. | Spectrophotometry, Mass Spectrometry, ELISA |
| Genetic & Epigenetic Markers | miRNA (e.g., miR-146a, miR-155), DNA Methylation patterns [84] [85] | Regulate gene expression in inflammatory pathways; potential for early risk stratification and understanding epigenetic influences on MetS [84] [85]. | qRT-PCR, Microarrays, Bisulfite Sequencing |
The application of these biomarkers is moving beyond single-analyte detection. Composite scores, such as the low-grade inflammation score (INFLA-score), which integrates CRP, white blood cell count, platelet count, and neutrophil-to-lymphocyte ratio (NLR), have been validated in blood and show promise for salivary application [5]. Research on oilfield shift workers demonstrated that a higher INFLA-score was strongly associated with a greater likelihood of having MetS, with those in the highest quartile of INFLA-score having a 3.58 times higher risk than those in the lowest quartile [5]. This multi-analyte approach provides a more robust assessment of the body's overall inflammatory state.
Experimental Protocols for Salivary Biomarker Analysis
Saliva Sample Collection and Pre-processing
Standardized protocols are critical for generating reliable and reproducible data. The following workflow is recommended for research settings.
Title: Saliva Sample Processing Workflow
Detailed Protocol:
- Participant Preparation: Subjects should refrain from eating, drinking (except water), smoking, and performing oral hygiene for at least 60 minutes prior to collection to avoid contamination and dilution [83] [86].
- Sample Collection: Collect unstimulated whole saliva via the passive drool method. Participants should allow saliva to pool in the mouth floor and expel it through a sterile funnel into a pre-chilled, DNA-/RNA-free polypropylene tube. The process is typically conducted over 5-15 minutes [83] [88]. The use of saliva collection aids (e.g., SalivaBio Oral Swabs) is acceptable, especially in field studies, though the material may influence analyte recovery [83].
- Pre-processing: Centrifuge the collected saliva at 2,600 × g for 15 minutes at 4°C. This step separates the clear supernatant (cell-free saliva) from the pellet containing cellular debris, bacteria, and exfoliated epithelial cells [88].
- Aliquoting and Stabilization: Immediately aliquot the supernatant into cryovials. To preserve biomarker integrity, add appropriate stabilizers—such as protease inhibitors for protein analysis or RNase inhibitors for RNA/DNA analysis [85] [88].
- Storage: Store aliquots at -80°C until analysis. Avoid repeated freeze-thaw cycles.
Validation of Salivary mRNA Biomarkers via qRT-PCR
The following protocol, adapted from a validated oral cancer biomarker study, outlines a robust method for quantifying inflammatory mRNA biomarkers in saliva [88].
Detailed Protocol:
RNA Extraction:
- Use 300 μL of supernatant saliva.
- Extract total RNA using a commercial kit (e.g., MagMAX Viral RNA Isolation Kit) on a semi-automated magnetic particle processor (e.g., KingFisher) to minimize variability and increase throughput [88].
- Treat the eluted RNA with DNase I (e.g., from Ambion) for 30 minutes at 37°C to remove genomic DNA contamination.
cDNA Synthesis:
- Use gene-specific primers for the reverse transcription reaction to increase specificity and sensitivity.
- Perform the reaction using 50 U of MuLV reverse transcriptase in a 20 μL reaction volume. Incubation conditions: 25°C for 10 min, 42°C for 45 min, followed by enzyme inactivation at 95°C for 5 min [88].
Quantitative Real-Time PCR (qPCR):
- Perform reactions in triplicate for each sample.
- Use a 20 μL reaction mix containing SYBR Green I Master Mix and 400 nM of each primer.
- Run on a standard thermal cycler (e.g., ABI 7500 Fast) with a three-step protocol: denaturation at 95°C, followed by 40 cycles of 95°C for 15s, 60°C for 30s, and 72°C for 30s, concluding with a melting curve analysis to verify amplicon specificity [88].
Quantification:
- Generate absolute standard curves using known copy numbers of in vitro transcribed RNA for each target biomarker. This allows for precise copy number quantification in the sample [88].
Technological Advances in Salivary Biomarker Detection
Emerging sensing technologies are overcoming historical challenges in salivary diagnostics, such as low biomarker concentration and sample complexity.
Table 2: Advanced Sensing Platforms for Salivary Biomarker Detection
| Technology Platform | Core Principle | Key Advantages for MetS Research |
|---|---|---|
| Electrochemical Biosensors [87] | Measures electrical signal (current, impedance) from antigen-antibody or aptamer-target binding on an electrode surface. | High sensitivity for low-abundance biomarkers; potential for miniaturization and continuous monitoring; direct detection in complex fluids. |
| Optical Biosensors (e.g., Surface Plasmon Resonance - SPR) [87] | Detects changes in refractive index or light emission upon biomarker binding to a sensor surface. | Label-free, real-time kinetic analysis of biomarker levels; high throughput capability. |
| Microfluidic & Lab-on-a-Chip Systems [87] | Integrates sample preparation and analysis into a single, miniaturized device. | Automates processing, reduces reagent use and human error; ideal for point-of-care testing and large cohort screening. |
| Wearable Oral Sensors [87] | Miniaturized devices (e.g., tooth-mounted, intraoral patches) for continuous in situ monitoring. | Unprecedented capability for real-time, dynamic tracking of inflammatory fluctuations in response to diet, sleep, or medication. |
These platforms often employ nanomaterials (e.g., graphene, gold nanoparticles) to enhance signal amplification and biorecognition elements (e.g., monoclonal antibodies, DNA aptamers) for high specificity [87]. The integration of these sensors with smartphones for data readout is a key trend, paving the way for decentralized health monitoring.
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful research into salivary biomarkers for inflammation requires a suite of reliable reagents and tools. The following table details essential components for a typical workflow.
Table 3: Research Reagent Solutions for Salivary Biomarker Analysis
| Reagent / Kit | Function / Specific Role | Example Use-Case in Protocol |
|---|---|---|
| Protease Inhibitor Cocktail | Inhibits proteolytic degradation of protein biomarkers (e.g., cytokines, CRP) in saliva. | Added to saliva supernatant immediately after centrifugation to preserve analyte integrity during storage [85]. |
| RNase Inhibitor & SUPERASE-In | Preserves RNA integrity by inhibiting ubiquitous RNases, crucial for mRNA/miRNA analysis. | Used as a preservative during saliva collection or added post-collection for transcriptomic studies [88]. |
| Magnetic-Bead Based RNA/DNA Kits (e.g., MagMAX) | Isolate high-purity nucleic acids from complex saliva samples; amenable to automation. | Used with a KingFisher system for automated, high-throughput RNA extraction from saliva supernatants [88]. |
| SYBR Green qPCR Master Mix | Fluorescent dye for detecting PCR amplicons during qRT-PCR cycles. | Used for the quantification of inflammatory gene transcripts (e.g., IL-1β, IL-8) with high sensitivity [88]. |
| Recombinant Cytokine Proteins & Antibody Pairs | Serve as positive controls and capture/detection reagents in immunoassays (ELISA). | Essential for developing and validating in-house ELISA or biosensor assays for TNF-α, IL-6, etc. [86]. |
| Multiplex Immunoassay Panels (Luminex-based) | Simultaneously quantify multiple protein biomarkers from a single, small-volume sample. | Profiling a panel of inflammatory cytokines (IL-6, IL-1β, TNF-α) in a saliva sample from a MetS cohort study [86]. |
| Men 10207 | Men 10207, CAS:126050-12-2, MF:C57H68N14O10, MW:1109.2 g/mol | Chemical Reagent |
| Masitinib Mesylate | Masitinib Mesylate, CAS:1048007-93-7, MF:C29H34N6O4S2, MW:594.8 g/mol | Chemical Reagent |
Salivary diagnostics represent a paradigm shift in the monitoring of chronic low-grade inflammation in metabolic syndrome. The rich biomarker content of saliva, coupled with standardized collection protocols and rapidly advancing detection technologies, provides researchers and drug developers with a powerful, non-invasive tool. The ability to perform frequent, stress-free sampling allows for dynamic tracking of inflammatory status and therapeutic responses in real-time, offering significant potential for advancing personalized medicine approaches in MetS management. Future efforts will focus on validating large-scale, multi-biomarker panels and integrating them with intelligent, point-of-care devices to translate this promising research into clinical and therapeutic reality.
Composite Indices and -Omics Approaches for a Holistic Inflammatory Profile
Metabolic Syndrome (MetS) represents a cluster of conditions—including obesity, hypertension, hyperglycemia, and dyslipidemia—that collectively increase the risk of coronary heart disease, cardiovascular disease, type 2 diabetes mellitus, stroke, and all-cause mortality [5]. With a global prevalence of 25%, MetS poses a significant challenge to public health worldwide [5]. The pathogenesis of MetS is complex and multifactorial, involving insulin resistance, genetic predisposition, and environmental influences, with chronic low-grade inflammation recognized as a key driver in its development and progression [5].
The traditional approach of measuring single inflammatory biomarkers has limitations in capturing the complexity of the inflammatory processes underlying MetS. Obesity, particularly visceral adiposity, leads to adipocyte hyperplasia and hypertrophy, triggering the secretion of numerous pro-inflammatory factors such as interleukin-6 (IL-6), tumor necrosis factor α (TNF-α), and interleukin-1β (IL-1β) [5]. These factors disrupt insulin signaling in peripheral tissues through autocrine and paracrine pathways, leading to metabolic disorders and insulin resistance, which in turn promotes the development of MetS [5]. This understanding has driven the development of more comprehensive assessment methods, including composite inflammatory indices and multi-omics approaches, to better characterize the inflammatory landscape in MetS and facilitate targeted interventions.
Established Composite Indices for Low-Grade Inflammation
The INFLA-Score: A Validated Composite Measure
The low-grade inflammation score (INFLA-score) is a composite index that integrates four routinely measured hematological parameters: high-sensitivity C-reactive protein (hs-CRP), leukocyte count, platelet count, and the neutrophil-to-lymphocyte ratio (NLR) or granulocyte-to-lymphocyte ratio (GrL) [5] [89]. This index provides a multidimensional assessment of inflammatory status by capturing different components of the inflammatory response process.
Table 1: Components of the INFLA-Score
| Biomarker | Biological Significance | Scoring Method |
|---|---|---|
| High-sensitivity C-reactive protein (hs-CRP) | Acute phase protein indicating systemic inflammation | Values in highest deciles (7-10): +1 to +4 |
| Leukocyte count | Overall immune cell mobilization | Values in middle deciles (5-6): 0 |
| Platelet count | Involvement in inflammatory pathways | Values in lowest deciles (1-4): -1 to -4 |
| Neutrophil-to-lymphocyte ratio (NLR) | Balance between innate and adaptive immunity | Total score range: -16 to +16 |
The calculation method involves assigning scores based on biomarker decile distributions, with values in the highest deciles (7th to 10th) receiving positive scores (+1 to +4), measurements in the middle deciles (5th and 6th) scoring zero, and values in the lowest deciles (1st to 4th) receiving negative scores (-1 to -4) [89]. The total INFLA-score represents an individual's level of low-grade inflammation, with higher scores indicating a more pronounced inflammatory status [89].
Clinical Validation and Predictive Value
Recent large-scale studies have demonstrated the significant predictive value of the INFLA-score for metabolic syndrome and cardiometabolic diseases. In a cross-sectional study of 1,758 shift workers in China's oilfield operations, multifactorial logistic regression analysis showed that those with higher INFLA-score had a significantly increased likelihood of developing MetS (OR = 1.08, 95% CI: 1.07–1.10) [5]. When comparing the highest INFLA-score quartile (Q4) to the lowest (Q1), the risk of developing MetS was 3.58 times higher in the Q4 group [5]. The study also found a positive association between INFLA-score and all individual components of MetS, including elevated blood glucose, blood pressure, waist circumference, triglyceride levels, and lower HDL levels (p < 0.001) [5].
A prospective cohort study involving 79,160 participants with obesity (BMI ≥ 30 kg/m²) from the UK Biobank further validated the INFLA-score's clinical utility [89]. Over a median follow-up of 161.41 months, Cox regression analysis revealed that each unit increase in the INFLA-score corresponded to a 1.5% increase in overall cardiometabolic disease risk (HR: 1.015, 95% CI 1.013–1.018), with particularly strong associations for type 2 diabetes mellitus risk (HR: 1.024, 95% CI 1.020–1.028) [89]. Restricted cubic spline analysis indicated a non-linear relationship between cumulative INFLA-score and cardiometabolic disease risk (P = 0.044) [89].
Other Composite Inflammatory Indices
Beyond the INFLA-score, several other composite inflammatory indices have demonstrated prognostic value in cardiovascular and metabolic conditions:
- Systemic Immune-Inflammation Index (SII): Calculated as platelet count × neutrophil count/lymphocyte count, this index reflects the balance between inflammatory and immune response [90].
- Systemic Inflammatory Response Index (SIRI): Derived from monocyte × neutrophil/lymphocyte counts, this index integrates multiple leukocyte subtypes [90].
- Neutrophil-to-High-density Lipoprotein Ratio (NHR): Combines inflammatory and lipid parameters [90].
- Platelet-to-Lymphocyte Ratio (PLR) and Monocyte-to-Lymphocyte Ratio (MLR): Simpler ratios with demonstrated prognostic value [90].
In a study of heart failure patients, these composite inflammatory markers showed a significant positive linear relationship with 180-day mortality, with the Inflammatory Prognostic Index (IPI) - combining CRP and albumin - showing the most significant incremental predictive value [91]. Similarly, in acute ischemic stroke patients, SIRI, NLR, and PLR emerged as independent risk factors for poor short-term prognosis [90].
Table 2: Predictive Performance of Inflammatory Indices in Clinical Studies
| Clinical Context | Most Predictive Indices | Performance Metrics |
|---|---|---|
| Metabolic Syndrome in Shift Workers | INFLA-score | Q4 vs Q1: OR = 3.58 for MetS risk |
| Cardiometabolic Diseases in Obesity | INFLA-score | Per unit increase: HR = 1.015 for CMDs |
| Heart Failure Mortality | IPI (CRP + Albumin) | Strongest incremental predictive value |
| Acute Ischemic Stroke Prognosis | SIRI, NLR, PLR | Independent risk factors (OR: 5.912, 1.334, 1.02) |
Multi-Omics Approaches for Inflammatory Profiling
Genomics and Genetic Risk Scores
Genomic approaches have identified numerous susceptibility loci for metabolic diseases, with familial aggregation, ethnic differences, and higher concordance rates in monozygotic versus dizygotic twins all indicating a strong genetic component to conditions like type 2 diabetes [92]. Early genetic studies identified associations with genes such as peroxisome proliferator-activated receptor gamma (PPARG) and transcription factor 7-like 2 (TCF7L2) [92]. Genome-wide association studies (GWAS) have further expanded the list of T2DM-associated loci to include SLC30A8, CDKAL1, and IGF2BP2 [92].
Given that single genetic variants typically offer limited predictive power, Genetic Risk Scores (GRS) that combine information from multiple variants have emerged as more powerful tools. Researchers have constructed various GRS containing different loci to explore their contribution to diabetes incidence during long-term follow-up [92]. One study demonstrated that the hazard for T2DM incidence was 3.45 times higher in the highest GRS quintile compared with the lowest quintile [92]. The addition of genetic information to conventional risk factor-based models has been shown to improve the area under the curve (AUC) for T2DM prediction from 0.78 to 0.79 [92].
For NAFLD, genetic variants in patatin-like phospholipase domain-containing protein 3 (PNPLA3), transmembrane 6 superfamily member 2 (TM6SF2), and membrane-bound O-acyltransferase 7-transmembrane channel like 4 (MBOAT7-TMC4) loci have been associated with disease susceptibility [92]. A meta-analysis showed that the PNPLA3 rs738409 variant exerts a strong influence on liver fat accumulation [92].
Chromatin Accessibility Profiling
Chromatin accessibility refers to the physical contact permissibility of nuclear macromolecules with chromatinized DNA, primarily determined by nucleosome distribution and occupancy [93]. The dynamic regulation of chromatin accessibility represents a prominent characteristic of the eukaryotic genome, with accessible regions comprising only ~2–3% of the whole genome [93]. These accessible loci are predominantly located in euchromatin regions with less nucleosome occupancy and higher regulatory activity, while inaccessible regions are mainly found in heterochromatin that is more densely packed [93].
Multiple high-throughput methods have been developed to profile chromatin accessibility genome-wide:
- ATAC-seq (Assay for Transposase-Accessible Chromatin using sequencing): Uses a hyperactive Tn5 transposase to simultaneously fragment and tag accessible genomic regions with sequencing adapters [93]. This method significantly simplified and flourished chromatin accessibility investigation, particularly with its application to small cell numbers and single cells [93].
- DNase-seq (DNase I hypersensitive sites sequencing): Identifies regions susceptible to DNase I enzyme cleavage [93].
- MNase-seq (Micrococcal Nuclease sequencing): Maps nucleosome positions based on MNase digestion patterns [93].
- FAIRE-seq (Formaldehyde-Assisted Isolation of Regulatory Elements): Isoles nucleosome-depleted regions based on their differential solubility [93].
The emergence of multimodal detection techniques now enables direct detection of epigenetic modifications, chromatin states, and gene expression in the same sample at single-cell resolution [93]. This integration provides unprecedented insights into the relationship between chromatin architecture and transcriptional regulation in inflammatory states.
Chromatin Accessibility Regulation
In inflammatory bowel disease, chromatin profiling has revealed distinct chromatin landscapes in Crohn's disease and ulcerative colitis, uncovering stable regulatory shifts independent of inflammation [94]. These findings suggest that chromatin accessibility patterns may serve as biomarkers for disease classification and therapeutic targets.
Transcriptomics and Proteomics in Inflammation Research
Transcriptomic and proteomic approaches provide complementary layers of information to genomic studies, capturing dynamic changes in gene expression and protein abundance in response to inflammatory stimuli. While not the primary focus of the current search results, these approaches are integral to comprehensive multi-omics profiling of inflammatory states.
Multi-omics studies that integrate genetic, transcriptomic, epigenetic, proteomic, and metabolomic data have demonstrated powerful capabilities in reclassifying metabolic diseases into molecularly and clinically distinct subgroups, revealing intra-disease heterogeneity and inter-disease similarities [92]. This refined classification provides a valuable reference for precision medicine approaches to inflammatory metabolic disorders.
Advanced Computational and Machine Learning Approaches
AI-Driven Phenotypic Characterization
Artificial intelligence approaches are increasingly applied to inflammatory disease research, providing unprecedented insights into the relationship between cellular morphology and inflammatory states. Advanced imaging modalities combined with computational algorithms can accurately discriminate between healthy, inflamed, degenerating, and diseased chondrocytes, and predict macrophage phenotypes with different functional states ranging from homeostatic to anti-/pro-inflammatory and tissue repair phenotypes [95]. These approaches can also predict the immunogenic potential (cytokine production) of cells at the single-cell level based on morphological features [95].
Machine learning techniques have been applied to multiple biomarker bioprofiling in serum to predict disease severity and triage patients with conditions like COVID-19 [95]. Similarly, diagnostic models for ischemic stroke using inflammation-related genes identified through machine learning have been developed and validated [95]. These models demonstrate the potential of AI approaches to extract clinically meaningful patterns from complex inflammatory biomarker data.
Novel Computational Frameworks for Peptide Identification
The NeXtMD framework represents a novel dual-module stacked approach that integrates both machine learning (ML) and deep learning (DL) components for accurate identification of anti-inflammatory peptides (AIPs) [96]. This system systematically extracts four functionally relevant sequence-derived descriptors:
- Dipeptide Deviation Encoding (DDE): Captures residue composition
- Composition of K-Spaced Amino Acid Pairs (CKSAAP): Measures inter-residue correlation
- Physicochemical Properties grouped into 16 classes (PP16): Encodes biochemical characteristics
- Auto-Correlation of Hydrophobicity (ACH): Quantifies sequence patterns
The framework employs a two-stage prediction strategy where the first stage generates preliminary predictions using an ensemble of four ML classifiers (Random Forest, XGBoost, LightGBM, and GBDT), and the second stage employs a multi-branch residual network (ResNeXt) to refine these predictions [96]. Benchmark evaluations demonstrate that NeXtMD outperforms current state-of-the-art methods, achieving an AUC of 0.8607, precision of 0.8062, and F1-score of 0.7513 [96].
NeXtMD AIP Identification Workflow
Experimental Protocols for Comprehensive Inflammatory Profiling
Protocol 1: INFLA-Score Calculation and Validation
Objective: To calculate and validate the INFLA-score as a composite measure of low-grade inflammation in population studies.
Materials and Reagents:
- EDTA-treated blood collection tubes
- Automated hematology analyzer (e.g., Coulter DxH 800 analyzer or Sysmex XT-1800i)
- Immunoturbidimetric assay reagents for hs-CRP quantification
- Standard laboratory centrifuges
Methodology:
- Collect fasting blood samples in EDTA-treated tubes
- Perform complete blood count analysis within 24 hours of collection using an automated hematology analyzer
- Quantify hs-CRP levels using high-sensitivity immunoturbidimetric analysis
- Calculate granulocyte count as the sum of neutrophils, eosinophils, and basophils
- Determine NLR or GrL ratio from differential counts
- Categorize each biomarker into deciles based on the population distribution
- Assign scores as follows:
- Deciles 1-4: -4 to -1 points
- Deciles 5-6: 0 points
- Deciles 7-10: +1 to +4 points
- Sum the scores for all four biomarkers to obtain the INFLA-score (range: -16 to +16)
Validation Steps:
- Assess association with MetS components using logistic regression models
- Evaluate predictive value for cardiometabolic outcomes using Cox proportional hazards models
- Perform subgroup analyses by sex, age, and medication use
- Conduct sensitivity analyses to test robustness of findings
Protocol 2: Chromatin Accessibility Profiling via ATAC-seq
Objective: To profile genome-wide chromatin accessibility patterns in immune cell populations relevant to inflammatory states.
Materials and Reagents:
- Nuclei isolation buffer (e.g., 10 mM Tris-HCl, 10 mM NaCl, 3 mM MgClâ‚‚, 0.1% IGEPAL CA-630)
- Tagmentase enzyme (Tn5 transposase)
- DNA clean-up beads or columns
- PCR amplification reagents
- High-sensitivity DNA quantification assay
- Next-generation sequencing platform
Methodology:
- Isolate nuclei from target cells (e.g., peripheral blood mononuclear cells)
- Count nuclei and assess viability
- Perform tagmentation reaction using Tn5 transposase to simultaneously fragment and tag accessible genomic regions
- Purify tagmented DNA using solid-phase reversible immobilization beads
- Amplify library via limited-cycle PCR with barcoded primers
- Quantify library concentration and quality using fluorometric methods
- Sequence libraries on appropriate NGS platform (e.g., Illumina)
- Process sequencing data through bioinformatic pipeline:
- Quality control (FastQC)
- Adapter trimming (Trimmomatic, Cutadapt)
- Alignment to reference genome (Bowtie2, BWA)
- Peak calling (MACS2)
- Differential accessibility analysis (DESeq2, diffBind)
- Motif enrichment analysis (HOMER, MEME)
Integration with Multi-omics:
- Combine with RNA-seq data to correlate accessibility with gene expression
- Integrate with ChIP-seq data for histone modifications
- Compare with GWAS data to contextualize disease-associated variants
Protocol 3: Inflammatory Resilience Assessment Using Challenge Tests
Objective: To quantify inflammatory resilience through response to standardized metabolic challenges.
Materials and Reagents:
- PhenFlex Challenge Test (PFT) drink: 75 g glucose, 60 g fat, 18 g protein concentrate
- EDTA plasma collection tubes
- Multiplex immunoassay panels (e.g., Meso Scale Discovery for cytokines)
- Centrifuges for plasma separation
- -80°C freezer for sample storage
Methodology:
- After a 12-hour overnight fast, administer PFT drink within 5 minutes
- Collect blood samples at baseline (t=0) and postprandially (t=30, 60, 120, 240 minutes)
- Separate plasma immediately by centrifugation and store at -80°C
- Measure inflammatory markers using multiplex immunoassays:
- Pro-inflammatory: IL-6, IL-8, TNF-α, IL-12p70
- Anti-inflammatory: IL-10, IL-13
- Additional markers: IFN-γ, MPO, leptin, adiponectin, CRP, SAA
- Calculate composite inflammatory resilience scores using health space modeling
- Compare trajectories to reference populations (young lean vs. older obese)
Analysis Approach:
- Model postprandial inflammatory responses as trajectories
- Calculate area under the curve for pro- and anti-inflammatory markers
- Develop composite scores reflecting dynamic response capacity
- Assess intervention effects by comparing pre- and post-treatment responses
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Essential Research Tools for Inflammatory Profiling
| Tool Category | Specific Products/Platforms | Application in Inflammation Research |
|---|---|---|
| Hematology Analyzers | Coulter DxH 800 analyzer, Sysmex XT-1800i | Complete blood count parameters for composite indices |
| Immunoassay Platforms | Beckman Coulter AU5800, Meso Scale Discovery Multiplex | Quantification of CRP and cytokine panels |
| Chromatin Profiling | Illumina sequencing platforms, Tn5 transposase | ATAC-seq for chromatin accessibility mapping |
| Machine Learning | Random Forest, XGBoost, LightGBM, ResNeXt | Predictive modeling of inflammatory states and peptide identification |
| Bioinformatic Tools | FastQC, Bowtie2, MACS2, DESeq2, HOMER | Analysis of sequencing data and motif enrichment |
| Challenge Tests | PhenFlex Challenge Test (PFT) | Assessment of inflammatory resilience through metabolic perturbation |
| Mavacoxib | Mavacoxib | Mavacoxib is a long-acting, selective COX-2 inhibitor for research use only. Explore its applications in anti-inflammatory and oncology studies. RUO, not for human use. |
| Maytansine | Maytansine, CAS:35846-53-8, MF:C34H46ClN3O10, MW:692.2 g/mol | Chemical Reagent |
The integration of composite inflammatory indices with multi-omics approaches represents a paradigm shift in how researchers and clinicians assess and interpret low-grade inflammation in metabolic syndrome. The INFLA-score and similar composite measures offer practical, cost-effective methods for risk stratification that outperform single biomarkers in predicting cardiometabolic outcomes [5] [89]. Meanwhile, advanced omics technologies—including genomics, chromatin accessibility profiling, and transcriptomics—provide unprecedented resolution for understanding the molecular mechanisms underlying inflammatory dysregulation [92] [93].
The emerging field of artificial intelligence and machine learning further enhances these approaches by identifying complex patterns in high-dimensional data, enabling more accurate prediction of inflammatory phenotypes and therapeutic responses [95] [96]. As these technologies continue to evolve and become more accessible, they hold tremendous promise for advancing precision medicine approaches to inflammatory metabolic disorders, ultimately enabling more targeted and effective interventions for patients with metabolic syndrome and related conditions.
Breaking the Cycle: Overcoming Challenges in Anti-Inflammatory Therapy for MetS
The NLRP3 inflammasome, a cytosolic multiprotein complex, acts as a critical sensor of metabolic stress and a central driver of the chronic low-grade inflammation that characterizes metabolic syndrome. Its activation leads to caspase-1-mediated maturation of pro-inflammatory cytokines IL-1β and IL-18 and induction of pyroptosis, contributing to insulin resistance, cardiovascular disease, and other metabolic sequelae. This whitepaper evaluates the efficacy, mechanisms, and limitations of emerging NLRP3 inhibitors. While repurposed drugs like colchicine demonstrate clinical utility, a new generation of selective small-molecule inhibitors—such as NT-0796, ML345, and others in clinical development—show superior target specificity and promising preclinical and early clinical results. However, challenges related to selectivity, tissue-specific delivery, and long-term safety remain significant hurdles in the path to clinical approval. Targeted inhibition of the NLRP3 inflammasome represents a paradigm shift from symptom management to disease-modifying interventions for metabolic syndrome and its associated conditions.
Metabolic syndrome is increasingly recognized as a chronic inflammatory disease whose mechanisms involve macrophage and neutrophil activation, initiation of the nod-like receptor protein 3 (NLRP3) inflammasome, and IL-1β secretion [97]. The NLRP3 inflammasome serves as an essential component of the innate immune system, a molecular platform that detects diverse danger signals including metabolic stress, infections, and structural cellular disruptions [10]. Beyond pathogen defense, inflammasomes influence tissue regeneration, cell death pathways, and sterile inflammation, highlighting their role as integrative immune hubs [10].
In the context of metabolic syndrome, chronic activation of the NLRP3 inflammasome occurs in response to various metabolic danger signals, including cholesterol or uric acid crystals, extracellular ATP, and aggregated proteins [98]. This sustained activation creates a persistent state of low-grade inflammation that impairs insulin signaling, promotes atherosclerotic plaque development, and contributes to the pathogenesis of obesity, type 2 diabetes, and cardiovascular disease [97] [99]. The central role of NLRP3 in these interconnected conditions makes it an attractive therapeutic target for addressing the underlying inflammatory pathology of metabolic syndrome rather than merely managing its symptoms.
Molecular Mechanisms of NLRP3 Inflammasome Activation
The NLRP3 inflammasome is a high-molecular-weight intracellular multi-protein complex consisting of three core components: the NLRP3 sensor protein, the ASC (apoptosis-associated speck-like protein containing a CARD) adaptor protein, and the pro-caspase-1 effector protein [100]. NLRP3 contains three domains: an N-terminal pyrin domain (PYD), a central NACHT domain, and a C-terminal leucine-rich repeat (LRR) domain [100].
Activation Pathways
The activation of the NLRP3 inflammasome occurs through three distinct pathways:
- Canonical Pathway: Requires two signals. The priming signal (Signal 1) from TLR ligands triggers NF-κB activation, upregulating pro-IL-1β and NLRP3 expression. The activation signal (Signal 2) from PAMPs or DAMPs induces inflammasome assembly, leading to caspase-1 activation [100].
- Non-canonical Pathway: Involves intracellular LPS detection by caspase-11 (in mice) or caspase-4/5 (in humans), indirectly activating NLRP3 [10] [98].
- Alternative Pathway: Activated by LPS through TLR4 without requiring cell death, resulting in a more gradual but sustained inflammatory response [10].
Table 1: Key Molecular Events in NLRP3 Inflammasome Activation
| Event | Components Involved | Functional Outcome |
|---|---|---|
| Priming Signal | TLRs, NF-κB | Upregulation of NLRP3, pro-IL-1β, and pro-IL-18 |
| Activation Signal | PAMPs/DAMPs (ATP, crystals, etc.) | Oligomerization of inflammasome components |
| Inflammasome Assembly | NLRP3, ASC, pro-caspase-1 | Formation of functional inflammasome complex |
| Caspase Activation | Caspase-1 | Cleavage of pro-IL-1β, pro-IL-18, and gasdermin D |
| Effector Phase | Mature IL-1β, IL-18, GSDMD-NT | cytokine secretion and pyroptotic cell death |
Regulatory Mechanisms
Multiple regulatory mechanisms modulate NLRP3 activation, including BRCC3-mediated deubiquitination, lysine carbamylation, intracellular trafficking to the microtubule-organizing center, and endolysosomal localization via PI4P [10]. Dysregulation of these checkpoints contributes to inflammatory, neurodegenerative, hepatic, metabolic, and infectious diseases [10].
The following diagram illustrates the molecular regulation and activation pathways of the NLRP3 inflammasome:
Established and Emerging NLRP3 Inhibitors: Efficacy and Mechanisms
Repurposed Therapeutics: Colchicine
Colchicine, a lipid-soluble tricyclic alkaloid, has been used medicinally for millennia but has recently gained attention for its NLRP3 inhibitory effects in cardiovascular disease [97]. Its mechanism extends beyond direct NLRP3 suppression to include sirtuin and AMP-activated protein kinase (AMPK) pathway regulation, and downregulation of cellular stress signals that promote atherosclerotic plaque rupture, insulin resistance, and obesity [97].
Key Pharmacological Properties:
- Single doses range from 0.5 to 1.2 mg with rapid absorption in the jejunum and ileum
- Peak plasma concentrations approximately 1 hour after ingestion
- Bioavailability of 24-88%, with 40% binding to albumin in circulation
- Preferentially accumulates inside neutrophils, which lack the P-glycoprotein efflux pump
- Narrow therapeutic index with gastrointestinal side effects affecting 5-20% of individuals
Colchicine's proven efficacy in preventing cardiovascular disease led to its inclusion in the 2023 American College of Cardiology treatment guidelines, representing a promising development for NLRP3-targeted therapy in metabolic syndrome [97].
Novel Small-Molecule Inhibitors in Development
Recent years have seen significant advances in developing selective NLRP3 inhibitors with improved specificity and safety profiles. The following table summarizes key investigational agents:
Table 2: Novel Small-Molecule NLRP3 Inhibitors in Development
| Inhibitor | Developer | Mechanism of Action | Development Stage | Key Indications |
|---|---|---|---|---|
| NT-0796 | NodThera | Brain-penetrant NLRP3 inhibitor | Phase 2 trials | Obesity, CVD, Parkinson's |
| NT-0150 | NodThera | Pyridazinone-based NLRP3 inhibitor | Phase 1 SAD/MAD studies | Neurodegeneration |
| NT-0249 | NodThera | Peripheral NLRP3 inhibitor | Preclinical | Inflammatory & neuropathic pain |
| ML345 | Academic | Disrupts NLRP3-NEK7 interaction | Preclinical | Systemic inflammation, miscarriage |
| MCC950/Inzomelid | Industry/Academic | Direct NLRP3 inhibitor | Phase 2 completed | CAPS, inflammatory diseases |
| Thiolutin | Academic | BRCC3 deubiquitinase inhibitor | Preclinical | Broad-spectrum inflammasome inhibition |
Notable Candidate Profiles:
NT-0796: NodThera's lead candidate is a potent, highly selective small-molecule brain-penetrant NLRP3 inhibitor that crosses the blood-brain barrier to target immune cells in the central nervous system [101]. In mouse diet-induced obesity models, NT-0796 monotherapy reduced body weight, inflammation, and neuroinflammation, and reset multiple endocrine hormones [101]. When combined with GLP-1 receptor agonist semaglutide, NT-0796 demonstrated additive weight loss, reversing the obese phenotype. Furthermore, switching from combination therapy to NT-0796 monotherapy maintained weight loss [101]. NT-0796 is currently in two phase 2 clinical studies for obesity (RESOLVE-1 and RESOLVE-2), with topline data expected in 2Q 2026 [101].
ML345: Originally identified as an insulin-degrading enzyme inhibitor, ML345 has been characterized as a highly potent and selective NLRP3 inhibitor [98]. It effectively suppresses canonical, noncanonical, and alternative NLRP3 inflammasome activation pathways without affecting other inflammasomes. Mechanistically, ML345 binds to NLRP3 in a non-covalent manner and directly targets tyrosine 381 (Y381), disrupting its essential interaction with NIMA-related kinase 7 (NEK7), consequently preventing inflammasome complex formation [98]. In vivo, ML345 is well tolerated and markedly alleviates inflammatory responses in mouse models of NLRP3-associated disorders. Compared with several previously reported NLRP3 inhibitors, ML345 exhibits superior selectivity and comparable or greater inhibitory potency [98].
MCC950 and Analogs: MCC950 represents one of the most potent NLRP3 inhibitors discovered to date, though clinical development faced challenges related to hepatotoxicity [102] [98]. Its derivatives inzomelid and IZD334 have completed phase I studies, demonstrating the ongoing interest in this chemical series [98].
Experimental Approaches for Evaluating NLRP3 Inhibitors
Standardized In Vitro Methodologies
Primary Cell-Based Assays:
- Cell Source: Primary bone marrow-derived macrophages (BMDMs) from wild-type and NLRP3-deficient mice; human peripheral blood mononuclear cells (PBMCs) [98]
- Priming Signal: LPS (100-500 ng/mL for 2-4 hours) to induce pro-IL-1β and NLRP3 expression
- Activation Signals: Nigericin (5-10 μM), ATP (1-5 mM), monosodium urate crystals (100-250 μg/mL), silica particles (100-200 μg/mL) [98]
- Readouts: IL-1β and IL-18 secretion by ELISA, caspase-1 cleavage by Western blot, LDH release for pyroptosis quantification [98]
Specificity Assessment:
- Alternative Inflammasome Activation: AIM2 (poly(dA:dT) transfection), NLRC4 (Salmonella Typhimurium infection), NLRP1 (Val-boroPro), Pyrin (Clostridium difficile toxin B) [98]
- Priming Phase Evaluation: NF-κB activation and pro-IL-1β expression via Western blot after LPS stimulation with inhibitor treatment [98]
In Vivo Disease Models
Metabolic Syndrome Models:
- Diet-Induced Obesity: C57BL/6J mice fed high-fat diet (45-60% kcal from fat) for 12-20 weeks [101]
- Cardiovascular Disease: ApoE-/- mice on Western diet for atherosclerotic plaque assessment
- Type 2 Diabetes: db/db mice or high-fat diet with low-dose streptozotocin
Inflammatory Challenge Models:
- Systemic Inflammation: LPS-induced endotoxemia (10-20 mg/kg intraperitoneal) with cytokine measurement in serum [98]
- Peritonitis: MSU crystal-induced peritonitis with neutrophil influx quantification
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for NLRP3 Investigations
| Reagent/Category | Specific Examples | Research Application | Key Function |
|---|---|---|---|
| Cell Models | Primary BMDMs, iBMDMs, THP-1 cells, PBMCs | In vitro screening | Cellular context for inflammasome studies |
| Activation Agents | Nigericin, ATP, MSU crystals, SiO2, alum | Inflammasome activation | Provide specific triggers for NLRP3 assembly |
| Cytokine Detection | IL-1β ELISA, IL-18 ELISA, Luminex multiplex | Efficacy assessment | Quantify inhibitor effects on cytokine release |
| Cell Death Assays | LDH release, propidium iodide staining | Pyroptosis measurement | Evaluate gasdermin D-mediated cell death |
| Western Blot Antibodies | Anti-caspase-1, anti-NLRP3, anti-ASC, anti-IL-1β | Mechanism confirmation | Detect protein cleavage and complex formation |
| Animal Models | Diet-induced obesity, LPS challenge, CAPS models | In vivo validation | Preclinical efficacy and safety assessment |
| Butyrolactone 3 | Butyrolactone 3, CAS:778649-18-6, MF:C9H12O4, MW:184.19 g/mol | Chemical Reagent | Bench Chemicals |
| Mericitabine | Mericitabine, CAS:940908-79-2, MF:C18H26FN3O6, MW:399.4 g/mol | Chemical Reagent | Bench Chemicals |
Limitations and Challenges in Clinical Translation
Selectivity and Safety Concerns
Despite promising preclinical results, clinical translation of NLRP3 inhibitors has faced challenges related to selectivity, limited efficacy, and potential toxicity [102]. The narrow therapeutic index of first-generation inhibitors like MCC950, which demonstrated hepatotoxicity in clinical trials, highlights the importance of thorough safety profiling [98]. NLRP3's role in host defense against pathogens raises theoretical concerns about increased infection risk, though targeted inhibition may preserve sufficient immune function due to redundant cytokine production pathways [101].
Pharmacological Limitations
Tissue-Specific Delivery: Many inflammatory processes in metabolic syndrome occur within specific tissue compartments that may be difficult to access. NodThera has addressed this by developing both brain-penetrant (NT-0796, NT-0150) and peripheral (NT-0249) inhibitors tailored to different disease contexts [101].
Dosing and Bioavailability: The optimal dosing regimen for chronic conditions like metabolic syndrome remains undefined. While colchicine requires multiple daily doses, next-generation inhibitors like NT-0249 demonstrate pharmacokinetics commensurate with once-daily dosing [101].
Clinical Development Hurdles
The heterogeneous nature of metabolic syndrome presents challenges for clinical trial design and patient selection. Additionally, the lack of validated biomarkers for NLRP3 activation in specific tissues makes target engagement and dose optimization difficult. While hsCRP reduction has been used as a surrogate, more specific biomarkers are needed [101].
The following diagram illustrates the current developmental pipeline and associated challenges for NLRP3 inhibitors:
Future Perspectives and Research Directions
The field of NLRP3 inhibition is rapidly evolving, with several promising directions emerging:
Combination Therapies: Evidence suggests NLRP3 inhibitors may enhance the efficacy of existing metabolic therapies. NodThera's research demonstrates additive weight loss when NT-0796 is combined with GLP-1 receptor agonists like semaglutide [101]. Similarly, colchicine's effects on multiple inflammatory pathways may complement standard cardiovascular therapies [97].
Precision Medicine Approaches: As our understanding of NLRP3 biology deepens, opportunities emerge for patient stratification based on specific inflammasome activation signatures. Genetic profiling of NLRP3 variants and related regulatory proteins may identify subgroups most likely to respond to targeted inhibition.
Novel Therapeutic Strategies: Beyond direct NLRP3 inhibition, alternative approaches targeting upstream regulators (e.g., BRCC3 with thiolutin) or downstream effectors offer additional therapeutic entry points [10]. Carbamylation-mediated suppression and disruption of endocytic dynamics represent innovative strategies under investigation [10].
Expanding Indications: While metabolic syndrome remains a primary focus, NLRP3 inhibitors show promise for neurodegenerative diseases, autoimmune conditions, and other chronic inflammatory states [101] [100]. The brain-penetrant properties of compounds like NT-0796 open possibilities for addressing neuroinflammation in Parkinson's disease and related conditions [101].
Targeting the NLRP3 inflammasome represents a transformative approach to addressing the chronic low-grade inflammation underlying metabolic syndrome. From the repurposed drug colchicine to novel selective inhibitors like NT-0796 and ML345, therapeutic strategies are evolving toward greater specificity and improved safety profiles. While challenges in clinical translation remain, compelling preclinical and early clinical data support continued investment in this target. As understanding of NLRP3 biology deepens and clinical trial results mature, NLRP3 inhibitors hold significant potential to shift the treatment paradigm for metabolic syndrome from symptomatic management to fundamentally addressing the underlying inflammatory pathology. The coming years will be critical in determining whether these promising therapeutic candidates can overcome existing limitations and deliver on their potential to modify disease progression in metabolic syndrome and related conditions.
Metabolic syndrome (MetS) represents a cluster of conditions—including central obesity, dyslipidemia, hypertension, and insulin resistance—that collectively amplify the risk of cardiovascular disease (CVD), type 2 diabetes mellitus (T2DM), and all-cause mortality [2]. The global prevalence of MetS continues to rise, currently affecting approximately 25% of adults worldwide and presenting substantial challenges to public health systems [2]. Central to the pathophysiology of MetS is chronic low-grade inflammation, a persistent, subclinical immune activation state that drives metabolic dysfunction through complex signaling pathways [5] [2] [29]. This inflammatory state is characterized by elevated levels of pro-inflammatory cytokines including interleukin-1β (IL-1β), IL-6, and tumor necrosis factor-α (TNF-α), which disrupt insulin signaling, promote endothelial dysfunction, and accelerate atherosclerosis [2] [29].
The recognition of inflammation as a fundamental driver of metabolic disease has catalyzed the investigation of anti-inflammatory therapies for repurposing in this context. Among the most promising candidates are IL-1 blockers and colchicine, established agents with potent immunomodulatory properties. This review provides a comprehensive assessment of the current clinical trial evidence evaluating these drugs, with a specific focus on their efficacy, safety profiles, and potential integration into treatment strategies for inflammation-driven metabolic disorders.
Mechanistic Insights: Inflammation at the Crossroads of Metabolic Dysfunction
The Inflammatory Network in Metabolic Syndrome
Chronic low-grade inflammation in MetS originates primarily from dysfunctional adipose tissue. Hypertrophied adipocytes release elevated levels of pro-inflammatory cytokines, including TNF-α, IL-6, and IL-1β, while reducing the production of anti-inflammatory adiponectin [29]. This process creates a systemic pro-inflammatory state that disrupts insulin signaling in peripheral tissues, leading to insulin resistance—a core defect in MetS [2] [29]. Furthermore, obesity-induced mitochondrial dysfunction generates excessive reactive oxygen species (ROS), which activate the NLRP3 inflammasome, a multiprotein complex responsible for the cleavage and secretion of mature IL-1β [29]. This establishes a vicious cycle wherein metabolic stress fuels inflammation, which in turn exacerbates metabolic dysfunction.
The INFLA-score, a composite inflammatory index based on C-reactive protein (CRP), leukocyte count, platelet count, and the neutrophil-to-lymphocyte ratio (NLR), has emerged as a valuable tool for quantifying low-grade inflammation in clinical research [5]. Recent studies demonstrate a strong positive association between elevated INFLA-score and the prevalence of MetS, with a clear dose-response relationship observed across its components, including elevated blood glucose, blood pressure, waist circumference, and triglyceride levels [5].
Molecular Targets: IL-1 Signaling and Colchicine's Mechanisms
Table 1: Molecular Mechanisms of Action of Repurposed Anti-inflammatory Drugs
| Drug Class | Specific Agent | Primary Molecular Target | Key Downstream Effects | Impact on Inflammatory Pathways |
|---|---|---|---|---|
| IL-1 Blockers | Canakinumab | IL-1β | Neutralizes circulating IL-1β; inhibits IL-1β signaling | Reduces systemic inflammation; attenuates NLRP3 inflammasome-mediated damage |
| IL-1 Blockers | Anakinra | IL-1 Receptor | Competitively inhibits IL-1α and IL-1β binding | Blocks IL-1 signal transduction; decreases production of IL-6 and other cytokines |
| Microtubule Inhibitor | Colchicine | Tubulin heterodimers | Inhibits microtubule assembly and polymerization | Disrupts NLRP3 inflammasome activation; reduces neutrophil chemotaxis and adhesion |
IL-1 blockers directly target the IL-1 signaling axis, a cornerstone of innate immunity and inflammatory responses. Canakinumab is a fully human monoclonal antibody that selectively neutralizes IL-1β, preventing its interaction with IL-1 receptors [103]. Anakinra, a recombinant form of the naturally occurring IL-1 receptor antagonist (IL-1Ra), competitively inhibits the binding of both IL-1α and IL-1β to the IL-1 type I receptor [104]. By attenuating IL-1 signaling, these agents reduce the production of downstream inflammatory mediators, including IL-6, and mitigate IL-1-driven pathological processes.
Colchicine, an ancient alkaloid derived from Colchicum autumnale, exerts pleiotropic anti-inflammatory effects primarily through binding to tubulin and inhibiting microtubule polymerization [103]. This disruption of microtubule dynamics impairs multiple cellular processes critical to inflammation, including neutrophil chemotaxis, adhesion, and recruitment to sites of inflammation. Furthermore, colchicine potently inhibits the NLRP3 inflammasome, thereby reducing the activation of caspase-1 and the subsequent conversion of pro-IL-1β and pro-IL-18 into their active, secreted forms [103]. This dual mechanism positions colchicine as a compelling therapeutic option for countering inflammation in MetS.
Diagram Title: Inflammation in Metabolic Syndrome and Drug Targets
Clinical Trial Evidence: Efficacy and Safety Profiles
Colchicine in Cardiovascular Disease
The potential of low-dose colchicine (typically 0.5 mg daily) for reducing cardiovascular events has been evaluated in several landmark randomized controlled trials (RCTs), predominantly in patients with established coronary artery disease (CAD). A recent updated meta-analysis of 16 RCTs, encompassing data from 20,601 patients, provides a comprehensive overview of its efficacy and safety [105].
Table 2: Efficacy and Safety Outcomes of Colchicine from a 2025 Meta-Analysis of 16 RCTs (n=20,601) [105]
| Outcome | Relative Risk (RR) | 95% Confidence Interval (CI) | Statistical Significance |
|---|---|---|---|
| All-cause death | 0.97 | 0.78 - 1.22 | Non-significant |
| Cardiovascular death | 0.98 | 0.79 - 1.21 | Non-significant |
| Myocardial Infarction | 0.74 | 0.59 - 0.93 | Significant |
| Ischemia-driven Revascularization | 0.72 | 0.53 - 0.99 | Significant |
| Stroke | 0.67 | 0.39 - 1.15 | Non-significant |
| Gastrointestinal Adverse Events | 1.83 | 1.38 - 2.43 | Significant |
The pooled analysis demonstrates that colchicine does not significantly reduce the relative risk of all-cause or cardiovascular death [105]. However, it confers a significant 26% reduction in the risk of myocardial infarction and a 28% reduction in the risk of ischemia-driven revascularization [105]. This suggests that colchicine's benefit may lie more in preventing atherosclerotic plaque instability and ischemic events rather than in reducing mortality in the studied populations. The most notable safety concern is a significant 83% increased risk of gastrointestinal adverse events, though these are typically manageable and rarely lead to treatment discontinuation [105].
IL-1 Blockers in Inflammatory and Cardiovascular Conditions
The clinical evidence for IL-1 blockade comes from both autoimmune and cardiovascular trials. The CANTOS (Canakinumab Anti-Inflammatory Thrombosis Outcome Study) was a pivotal trial that proved the concept of targeting inflammation to reduce CVD risk. It demonstrated that canakinumab significantly reduced recurrent cardiovascular events in patients with prior myocardial infarction and elevated high-sensitivity CRP (hsCRP), independent of lipid-level lowering [103]. A prespecified analysis further showed that the cardiovascular benefit was confined to patients whose on-treatment hsCRP was reduced below 2.0 mg/L [103].
In the context of autoinflammatory diseases, the Eurofever observational study provides long-term data on the use of colchicine and anti-IL-1 blockers (canakinumab and anakinra) in Familial Mediterranean Fever (FMF) [106]. The study found that both drug classes were generally effective and well-tolerated over a mean follow-up of 2.9±3.1 years, with adverse events typically characterized as mild [106]. This long-term safety data from rheumatology supports the potential for repurposing these agents for chronic conditions like MetS.
The Researcher's Toolkit: Key Reagents and Methodologies
Table 3: Essential Research Reagents and Analytical Tools for Investigating Low-Grade Inflammation
| Reagent / Tool | Primary Function | Research Application | Example Context in Search Results |
|---|---|---|---|
| High-sensitivity CRP (hsCRP) | Biomarker of systemic inflammation | Quantifying low-grade inflammation; risk stratification | Used in CANTOS to identify eligible patients and track response [103]. |
| INFLA-Score | Composite index (CRP, WBC, Platelets, NLR) | Holistic assessment of chronic low-grade inflammation | Validated in a cohort of 1,758 shift workers to assess Mets risk [5]. |
| Advanced Lung Cancer Inflammation Index (ALI) | Composite index (BMI, Albumin, Lymphocyte/Neutrophil) | Assessing integrated nutritional-inflammation status | Identified as a strong predictor of mortality in Mets patients [7]. |
| Canakinumab | Human monoclonal anti-IL-1β antibody | Mechanistic studies of IL-1β pathway inhibition; clinical trial therapeutic | Primary intervention in the CANTOS trial [103]. |
| Low-Dose Colchicine | Microtubule and NLRP3 inflammasome inhibitor | Intervention for reducing inflammatory cardiovascular events | Dosed at 0.5 mg daily in recent CVD outcomes trials [105] [103]. |
Core Experimental Protocols
Protocol 1: Calculating and Applying the INFLA-Score in Cohort Studies. The INFLA-score is calculated from four blood-based biomarkers: high-sensitivity CRP, white blood cell count, platelet count, and the neutrophil-to-lymphocyte ratio (NLR) [5]. Each component is transformed by assigning values from -4 (lowest decile) to +4 (highest decile). The scores are summed to generate a final INFLA-score ranging from -16 to +16, where higher scores indicate greater inflammatory status [5]. In analytical models, this continuous score can be used to assess its association with Mets incidence or components via logistic regression, often employing restricted cubic splines to evaluate non-linear dose-response relationships [5].
Protocol 2: Assessing Cardiovascular Outcomes in RCTs of Anti-inflammatory Agents. Clinical trials evaluating drugs like colchicine and IL-1 blockers typically enroll patients with established atherosclerotic cardiovascular disease (e.g., prior myocardial infarction, CAD) [105] [103]. Participants are randomized to receive the active drug or a matching placebo on a background of standard guideline-directed medical therapy. The primary endpoint is usually a composite major adverse cardiovascular event (MACE) outcome, such as cardiovascular death, non-fatal myocardial infarction, and non-fatal stroke [103]. Key secondary endpoints often include ischemia-driven revascularization and hospitalization for unstable angina. Safety monitoring, with particular attention to infections (for IL-1 blockers) and gastrointestinal symptoms (for colchicine), is essential [105] [103].
The repurposing of anti-inflammatory drugs like colchicine and IL-1 blockers represents a paradigm shift in addressing the residual inflammatory risk prevalent in patients with metabolic syndrome. Robust evidence from cardiovascular outcomes trials confirms that targeting specific inflammatory pathways can significantly reduce ischemic events, although mortality benefits remain elusive and safety considerations, particularly regarding gastrointestinal effects with colchicine, warrant attention [105] [103].
Future research should focus on several critical areas: (1) identifying specific biomarkers, such as a high INFLA-score or elevated hsCRP, to pinpoint the patient subgroups most likely to benefit from therapy; (2) designing trials specifically within MetS populations to evaluate the impact of these drugs on the development and progression of core metabolic parameters, not just cardiovascular outcomes; and (3) exploring potential synergistic effects of combining anti-inflammatory therapies with existing metabolic drugs. As our understanding of the intricate links between metabolism and immunity deepens, the strategic inhibition of inflammatory pathways with repurposed drugs holds significant promise for improving the management of metabolic syndrome and its devastating complications.
Addressing Mitochondrial Dysfunction as a Strategy to Reduce Oxidative Stress and Inflammation
Within the context of metabolic syndrome, a state of low-grade chronic inflammation is a key pathological driver that accelerates disease progression. Central to this process is mitochondrial dysfunction, which serves as a critical link between metabolic overload and the activation of pro-inflammatory pathways [30]. Mitochondria are not merely energy-producing organelles but also function as central signaling hubs that coordinate cellular stress responses. In metabolic syndrome, nutrient excess and metabolic derangements disrupt mitochondrial efficiency, leading to excessive reactive oxygen species (ROS) generation and the release of mitochondrial damage-associated molecular patterns (mtDAMPs) [26] [107]. These events create a self-perpetuating cycle of oxidative stress and inflammation that characterizes the chronic inflammatory state observed in metabolic disorders. This technical review examines the mechanistic basis of mitochondrial dysfunction in metabolic inflammation and evaluates targeted therapeutic strategies to disrupt this cycle, with particular relevance for researchers and drug development professionals working in the field of immunometabolism.
Molecular Mechanisms Linking Mitochondrial Dysfunction to Inflammation
Mitochondrial ROS Production and Oxidative Stress
The electron transport chain (ETC) is a primary site of ROS generation under conditions of metabolic stress. Complex I and III are recognized as the main sites of superoxide (Oâ‚‚â») production, with electron leakage occurring particularly during states of high membrane potential and reduced coenzyme Q pool [26] [108]. During pathological conditions such as metabolic syndrome, this ROS production becomes exacerbated, overwhelming the mitochondrial antioxidant systems that include:
- Glutathione (GSH) system: GSH is converted to oxidized glutathione (GSSG) by glutathione peroxidase (GPx), simultaneously reducing Hâ‚‚Oâ‚‚ to Hâ‚‚O. GSSG is then recycled back to GSH by glutathione reductase [26].
- Enzymatic antioxidants: Superoxide dismutase (SOD) catalyzes the conversion of Oâ‚‚â» to Hâ‚‚Oâ‚‚, which is subsequently scavenged to Hâ‚‚O by peroxiredoxin or catalase [26].
- Small molecule antioxidants: Melatonin and coenzyme Q10 directly neutralize ROS and upregulate antioxidant enzymes [26] [32].
In metabolic syndrome, chronic nutrient excess disrupts this balance, leading to persistent oxidative stress that damages cellular components and activates inflammatory cascades.
mtDNA Damage and DAMP Signaling
Mitochondrial DNA is particularly vulnerable to ROS-mediated damage due to its proximity to the ETC and lack of histone protection [108]. Oxidative damage to mtDNA results in:
- Mutation accumulation: Increased mutational burden that further compromises ETC function
- mtDNA release: Displacement of damaged mtDNA into the cytosol and extracellular space
- DAMP activation: Released mtDNA acts as a damage-associated molecular pattern through its hypomethylated CpG motifs, which are recognized by pattern recognition receptors including TLR9 and NLRP3 inflammasome [107]
This mechanism establishes a direct connection between mitochondrial quality control failure and sterile inflammation that characterizes metabolic syndrome.
Imbalances in Mitochondrial Dynamics and Quality Control
Mitochondria exist in dynamic networks that undergo continuous fusion and fission, processes essential for maintaining functional integrity. Key regulators include:
- Fission proteins: Drp1 is recruited to the mitochondrial outer membrane by adaptor proteins (Mff, Fis1, MiD49, MiD51) where it forms constricting rings to divide mitochondria [26] [32]
- Fusion proteins: Mitofusins 1/2 mediate outer membrane fusion, while OPA1 facilitates inner membrane fusion [26]
In metabolic syndrome, this balance shifts toward excessive fission, generating fragmented mitochondrial networks with impaired bioenergetic capacity [30]. Simultaneously, mitophagic clearance of damaged mitochondria becomes impaired, allowing accumulation of dysfunctional organelles that perpetuate ROS production and DAMP release [32].
Table 1: Key Mitochondrial Dysfunction Mechanisms in Metabolic Syndrome
| Mechanism | Key Components | Consequence in Metabolic Syndrome |
|---|---|---|
| ROS Production | Complex I & III, RET, Antioxidant systems | Chronic oxidative stress, Protein/lipid damage |
| mtDNA Damage | Oxidized mtDNA, TFAM, Repair enzymes | DAMP signaling, Inflammasome activation |
| Mitochondrial Dynamics | Drp1, Mff, OPA1, Mitofusins | Fragmented network, Bioenergetic failure |
| Quality Control | PINK1-Parkin, LC3, Lysosomes | Accumulation of damaged mitochondria |
Therapeutic Strategies Targeting Mitochondrial Dysfunction
Direct Mitochondrial-Targeted Compounds
Several therapeutic approaches directly address mitochondrial oxidative stress and bioenergetic deficits:
- MitoQ: A mitochondria-targeted antioxidant that accumulates in the mitochondrial matrix and neutralizes ROS [32]
- Elamipretide (SS-31): Targets the inner mitochondrial membrane, protecting cardiolipin and improving ETC efficiency [109]
- Nicotinamide Riboside (NR): NAD+ precursor that enhances sirtuin activity and mitochondrial biogenesis [32]
- Coenzyme Q10: Electron carrier that also functions as a lipid-soluble antioxidant [32]
These compounds aim to directly interrupt the cycle of oxidative damage and bioenergetic decline at the level of the organelle itself.
Modulators of Mitochondrial Biogenesis and Dynamics
Therapeutic strategies also target the regulatory systems that control mitochondrial quantity and quality:
- AMPK activators: Metformin and other AMPK agonists stimulate mitochondrial biogenesis and mitophagy [30]
- PPAR-α/γ agonists: Improve fatty acid oxidation and mitochondrial biogenesis [110]
- Drp1 inhibitors: Prevent pathological mitochondrial fragmentation [111]
These approaches work by enhancing the cell's innate quality control systems to maintain a healthier mitochondrial population.
Table 2: Selected Mitochondria-Targeted Therapies in Development
| Therapeutic Agent | Molecular Target | Development Stage | Primary Indication |
|---|---|---|---|
| Elamipretide | Cardiolipin stabilization | FDA Approved (Barth) [109] | Barth Syndrome |
| KL1333 | NAD+ metabolism | Phase I/II (Actively Recruiting) [109] | KSS-CPEO, MELAS, MERRF |
| Sonlicromanol (KH176) | ROS metabolism | Phase II (Active, not yet recruiting) [109] | MELAS, MIDD |
| Zagociguat | sGC stimulator | Phase II (Actively Recruiting) [109] | MELAS |
| MT1621 | Deoxynucleotide metabolism | FDA Approved (TK2d) [109] | TK2 Deficiency |
Experimental Approaches for Assessing Mitochondrial Function
Biomarker Assessment in Preclinical and Clinical Studies
Validated biomarkers are essential for evaluating mitochondrial function in metabolic syndrome research:
- Growth Differentiation Factor-15 (GDF-15): Currently shows the greatest diagnostic value for mitochondrial dysfunction, outperforming traditional markers [112]
- Fibroblast Growth Factor-21 (FGF-21): Second most valuable biomarker, particularly responsive to mitochondrial stress [112]
- Lactate and lactate:pyruvate ratio: Classic markers of increased anaerobic metabolism due to OXPHOS impairment [112]
- Oxidative stress markers: Malondialdehyde (MDA), protein carbonyls, and 3-nitrotyrosine provide evidence of ROS-mediated damage [113]
These biomarkers should be measured in combination to provide a comprehensive assessment of mitochondrial status.
Functional and Imaging-Based Assessments
Advanced methodologies for evaluating mitochondrial function include:
- High-Resolution Respirometry: Direct measurement of OXPHOS capacity in isolated mitochondria or permeabilized cells using substrates targeting specific ETC complexes
- Mitochondrial Membrane Potential Assessment: Using fluorescent probes (JC-1, TMRM) to evaluate the proton gradient essential for ATP production
- Live-Cell Imaging of Mitochondrial Dynamics: Time-lapse microscopy to quantify fusion/fission rates and mitochondrial network morphology
- ATP Production Rates: Luciferase-based assays to measure ATP generation capacity from different metabolic substrates
These techniques provide direct functional readouts that complement biomarker measurements.
Integrated Signaling Pathways in Mitochondrial Dysfunction
The diagram below illustrates the core signaling pathways connecting mitochondrial dysfunction to oxidative stress and inflammation in metabolic syndrome.
Figure 1: Signaling Pathways in Mitochondrial Dysfunction and Therapeutic Targets. This diagram illustrates the vicious cycle linking metabolic syndrome to mitochondrial dysfunction, oxidative stress, and inflammation, with key points for therapeutic intervention indicated.
Research Reagent Solutions for Mitochondrial Studies
Table 3: Essential Research Reagents for Mitochondrial Function Assessment
| Reagent/Category | Specific Examples | Research Application |
|---|---|---|
| Mitochondrial Stains | MitoTracker dyes, TMRM, JC-1 | Visualization and membrane potential assessment |
| ROS Detection Probes | MitoSOX Red, H2DCFDA | Specific detection of mitochondrial superoxide |
| Oxygen Consumption Assays | Seahorse XF Analyzers, Oxygraphs | Real-time measurement of OXPHOS function |
| Antibodies for Mitochondrial Proteins | Anti-TOMM20, Anti-COX IV, Anti-HSP60 | Mitochondrial quantification and localization |
| mtDNA Damage Assays | Long-range PCR, QPCR-based damage quantitation | Assessment of mtDNA integrity and copy number |
| Metabolite Assays | Lactate/pyruvate, Acylcarnitine profiles | Evaluation of mitochondrial metabolic function |
Mitochondrial dysfunction represents a pathogenic nexus connecting metabolic overload to the oxidative stress and chronic inflammation that characterizes metabolic syndrome. Therapeutic strategies that target specific aspects of mitochondrial biology—including ROS production, bioenergetic capacity, dynamics, and quality control—offer promising approaches for breaking this cycle. The continued development of sensitive biomarkers and advanced assessment methodologies will be essential for translating these targeted approaches into effective clinical interventions for metabolic syndrome and its associated complications. For researchers in this field, focusing on the intersection between mitochondrial health and immune metabolism provides fertile ground for discovering novel therapeutic strategies to address the growing burden of metabolic disease.
The human gut microbiota, a complex ecosystem of trillions of microorganisms, plays a pivotal role in maintaining metabolic homeostasis and immune function. Within the context of metabolic syndrome (MetS)—a constellation of interrelated metabolic abnormalities including central obesity, dyslipidemia, hypertension, and dysglycemia—the gut microbiome has emerged as a critical mediator of low-grade chronic inflammation, a fundamental pathophysiological process driving disease progression [34] [114]. Dysbiosis, an imbalance in gut microbial composition and function, disrupts intestinal barrier integrity, promotes translocation of bacterial endotoxins such as lipopolysaccharide (LPS), and activates pro-inflammatory signaling pathways that sustain a state of systemic inflammation [115] [114]. This chronic inflammatory state directly contributes to insulin resistance, adipose tissue dysfunction, and the cardiovascular complications associated with MetS.
Targeted modulation of the gut microbiota represents a promising therapeutic strategy for breaking the cycle of inflammation and metabolic dysfunction. This whitepaper provides an in-depth technical analysis of three cornerstone intervention approaches: probiotics (live beneficial microorganisms), prebiotics (selectively fermented substrates that confer health benefits), and polyphenols (bioactive plant compounds abundant in traditional medicines). We synthesize current scientific evidence, detail mechanistic insights into their anti-inflammatory actions within the context of MetS, summarize key quantitative findings, and provide standardized experimental protocols for preclinical and clinical investigation. The overarching goal is to equip researchers and drug development professionals with a comprehensive framework for advancing microbiome-targeted therapies for metabolic syndrome.
Mechanisms of Action in Modulating Inflammation
Probiotics: Immunomodulation and Barrier Fortification
Probiotics, primarily strains of Lactobacillus and Bifidobacterium, exert their beneficial effects through multiple direct and indirect mechanisms to counteract low-grade inflammation.
- Direct Immunomodulation: Probiotics can influence the gut's immune landscape by promoting the differentiation of anti-inflammatory T-cells. Specific strains drive the development of T-helper 2 (Th2) cells and increase the production of anti-inflammatory cytokines such as IL-4 and IL-10 [116]. Concurrently, they can suppress the activation of pro-inflammatory pathways, including those mediated by Th17 cells [116].
- Enhancement of Gut Barrier Function: A key mechanism in reducing inflammation is the preservation of intestinal barrier integrity. Probiotics strengthen this barrier by increasing mucus secretion and preventing the degradation of tight junction proteins (e.g., occludin, ZO-1) [116] [117]. This action reduces the translocation of LPS into the systemic circulation, thereby blunting the activation of immune cells and the subsequent production of inflammatory markers like TNF-α, IL-6, and IL-1β [116] [114].
- Pathogen Inhibition and Microbiome Regulation: Through competitive exclusion, probiotics can prevent the adhesion of pathogenic bacteria to the intestinal epithelium. Some strains also produce bacteriocins and other antimicrobial compounds that directly inhibit the growth of harmful organisms, thereby helping to restore a balanced microbial community [115].
Prebiotics: Fueling Beneficial Bacteria and SCFA Production
Prebiotics, typically non-digestible carbohydrates like dietary fibers, are selectively utilized by host microorganisms to confer a health benefit. Their primary mode of action is indirect, through the stimulation of beneficial gut bacteria.
- Selective Stimulation of Beneficial Taxa: Prebiotics serve as a fermentable fuel for beneficial bacterial groups such as Bifidobacterium and Lactobacillus, promoting their growth and metabolic activity [117]. This selective stimulation helps to counter dysbiosis associated with metabolic syndrome.
- Generation of Anti-inflammatory Metabolites: The fermentation of prebiotics by gut microbiota leads to the production of short-chain fatty acids (SCFAs), including acetate, propionate, and butyrate [115] [114]. These SCFAs are crucial for maintaining gut health and systemic metabolism. Butyrate serves as the primary energy source for colonocytes, reinforcing the gut barrier [114]. Furthermore, SCFAs bind to receptors like GPR43 on immune cells, promoting the expansion of regulatory T-cells (Tregs) and the secretion of IL-10, which collectively suppress inflammation [118].
Polyphenols: Prebiotic-like Effects and Microbial Metabolites
Polyphenols, a heterogenous group of compounds found in plants, exhibit "prebiotic-like" properties and their health effects are heavily dependent on microbial transformation.
- Modulation of Microbial Composition: Similar to prebiotics, polyphenols can promote beneficial bacteria (e.g., Lactobacillus, Bifidobacterium, Akkermansia muciniphila) and inhibit harmful ones (e.g., Escherichia–Shigella) [119] [120] [121]. For instance, cranberry polyphenols have been shown to create a favorable niche for A. muciniphila by stimulating host mucin production [121].
- Bioactivation by Gut Microbiota: An estimated 95% of dietary polyphenols reach the colon intact, where they are metabolized by gut microbial enzymes into bioavailable and often more active metabolites [121]. These microbial metabolites exhibit enhanced antioxidant and anti-inflammatory activities compared to their parent compounds [119].
- Multi-faceted Mechanisms: The resulting metabolites, along with the polyphenols themselves, can directly scavenge free radicals, inhibit pro-inflammatory enzymes, and modulate key signaling pathways such as NF-κB and MAPK, which are central to the expression of inflammatory cytokines [117]. They also help strengthen the intestinal barrier, reducing LPS-induced inflammation [120] [121].
The following diagram illustrates the core mechanisms through which these interventions target gut microbiota to ameliorate low-grade inflammation in metabolic syndrome.
Robust epidemiological studies and clinical trials have established compelling associations between dietary interventions targeting the gut microbiome and reduced risk of metabolic syndrome. The following tables summarize key quantitative findings from recent research.
Table 1: Association between Dietary Index for Gut Microbiota (DI-GM) and Metabolic Syndrome Risk
| Study Parameter | Details | Quantitative Finding | Reference |
|---|---|---|---|
| Study Population | NHANES 2007-2018 (n=339,242 adults) | N/A | [34] |
| Exposure Variable | DI-GM Score (Quartiles: Q1 lowest, Q4 highest) | 14-component score (0-13) | [34] |
| Primary Outcome | Metabolic Syndrome (ATP III criteria) | Adjusted Odds Ratio (OR) | [34] |
| Risk Association | Q4 (Highest DI-GM) vs. Q1 (Lowest DI-GM) | OR: 0.84 (95% CI: 0.70–1.01) | [34] |
| Mediation Analysis | Systemic Immune-inflammation Index (SII) | 4.63% mediation of DI-GM/MetS association | [34] |
| Mediation Analysis | Neutrophil-to-lymphocyte ratio (NLR) | 3.83% mediation of DI-GM/MetS association | [34] |
Table 2: Effects of Specific Interventions on Gut Microbiota and Metabolic Markers
| Intervention Category | Specific Example | Observed Effect on Microbiota / Metabolism | Reference |
|---|---|---|---|
| Probiotics | Various Strains (Lactobacillus, Bifidobacterium) | Improved blood sugar control & lipid profiles; Increased Akkermansia & Blautia | [115] [120] |
| Prebiotics | Dietary Fiber | Promoted SCFA production (butyrate); Improved gut barrier integrity & insulin sensitivity | [115] [114] |
| Polyphenols (Cranberry) | Cranberry Flavan-3-ols | Microbial metabolites defended against E. coli; Increased Akkermansia muciniphila | [121] |
| Herbal Medicine | Berberis kansuensis (Berberis Cortex) | Significantly increased abundance of Akkermansia in T2D rats | [120] |
| Herbal Medicine | Gynostemma pentaphyllum | Reduced abundance of pro-inflammatory Proteobacteria in NAFLD mice | [120] |
| Herbal Formulation | Jiangzhi Granules | Increased SCFA-producing Lachnospiraceae; Reduced Proteobacteria | [120] |
Experimental Protocols for Preclinical and Clinical Research
To ensure reproducibility and translational validity in gut microbiome research, standardized experimental protocols are essential. The following section outlines detailed methodologies for investigating the effects of microbiota-targeted interventions.
Preclinical Animal Model Protocol
This protocol is designed to evaluate the efficacy of interventions in a well-established rodent model of diet-induced metabolic syndrome.
Animal Model and Induction of MetS:
- Subjects: Use C57BL/6J male mice (6-8 weeks old) or equivalent model. A sample size of n=10-12 per group provides sufficient statistical power.
- Diet: Administer a High-Fat Diet (HFD) containing 45-60% kcal from fat (e.g., lard) and 20-30% kcal from fructose or sucrose for a duration of 12-16 weeks to induce obesity, insulin resistance, and low-grade inflammation. The control group receives a standard chow diet (10-15% kcal from fat).
Intervention Administration:
- Probiotics: Administer a daily oral gavage of a defined probiotic strain (e.g., Lactobacillus rhamnosus GG, Akkermansia muciniphila) at a dose of 1x10^9 CFU in 200 µL of sterile PBS or vehicle. Vehicle control group receives PBS alone.
- Prebiotics: Incorporate the prebiotic (e.g., Inulin, Fructooligosaccharides - FOS) into the HFD at a concentration of 5-10% (w/w).
- Polyphenols/Herbal Extracts: Administer via oral gavage. The dose should be determined from prior literature; for a plant extract, a common range is 100-400 mg/kg body weight daily, dissolved in an appropriate vehicle (e.g., water, carboxymethyl cellulose).
Sample Collection and Analysis:
- Metabolic Phenotyping: Conduct weekly monitoring of body weight and food intake. Perform an Oral Glucose Tolerance Test (OGTT) and Insulin Tolerance Test (ITT) at the end of the intervention period after a 6-hour fast.
- Tissue and Blood Collection: At sacrifice, collect blood via cardiac puncture. Isolate serum for biomarker analysis. Excise and weigh key metabolic tissues (epididymal fat, liver). Collect colon and ileum tissues, flash-freeze for molecular analysis, or preserve in formalin for histology.
- Fecal Sample Collection: Collect fecal pellets at baseline, mid-point, and endpoint. Store immediately at -80°C for subsequent microbiome analysis.
Downstream Analyses:
- Gut Microbiome Analysis: Extract genomic DNA from fecal samples and perform 16S rRNA gene sequencing (V3-V4 region) on an Illumina MiSeq platform. Analyze data using QIIME 2 or Mothur to determine alpha/beta diversity and differential taxonomic abundance.
- Inflammatory Markers: Quantify serum levels of LPS, TNF-α, IL-6, IL-1β, and adiponectin using ELISA kits.
- Gut Permeability: Assess in vivo using the FITC-dextran assay; administer 4.4 kDa FITC-dextran and measure fluorescence in serum after 4 hours.
- Histology and Gene Expression: Perform H&E and Oil Red O staining on liver sections for steatosis scoring. Analyze mRNA expression of tight junction proteins (e.g., Zo-1, Occludin) and inflammatory genes (e.g., Tnf-α, Il-6) in colon tissue via qRT-PCR.
Clinical Trial Protocol
This framework outlines a randomized, controlled, double-blind trial to assess the impact of a defined intervention on patients with metabolic syndrome.
Study Population and Design:
- Participants: Recruit adults (age 18-65) meeting the ATP III criteria for MetS. Key exclusion criteria include: use of antibiotics/probiotics within 2 months, history of IBD, major cardiovascular event, or diabetes requiring insulin.
- Trial Design: A randomized, double-blind, placebo-controlled, parallel-arm trial. After a 2-week run-in period, participants are randomized to receive either the active intervention or an identical placebo for 12 weeks.
Intervention and Compliance:
- Active Product: This could be a specific probiotic strain, prebiotic fiber, polyphenol-rich extract, or a synbiotic combination. The dose must be justified by prior clinical evidence (e.g., 10^9-10^10 CFU/day for probiotics; 5-15 g/day for prebiotics).
- Placebo: An indistinguishable product (e.g., maltodextrin for a prebiotic).
- Compliance: Monitored through returned product logs, periodic video check-ins, and measurement of specific biomarkers in plasma or urine (e.g., polyphenol metabolites).
Outcome Measures and Sampling:
- Primary Outcomes: Change from baseline in HOMA-IR (Homeostatic Model Assessment of Insulin Resistance) and serum LPS-binding protein (LBP) or high-sensitivity C-reactive protein (hs-CRP).
- Secondary Outcomes: Changes in individual MetS components (waist circumference, blood pressure, lipid profile, fasting glucose), body composition (DEXA scan), and gut microbiota composition (16S rRNA sequencing of fecal samples).
- Sampling Schedule: Collect blood and fecal samples at baseline (week 0) and endpoint (week 12). A 3-day dietary record should be completed at both time points to account for dietary confounders.
The following workflow diagram visualizes the key stages of the clinical trial protocol.
The Scientist's Toolkit: Key Research Reagents and Materials
Table 3: Essential Reagents and Materials for Gut Microbiota Research
| Category | Reagent / Material | Function / Application | Technical Notes |
|---|---|---|---|
| Animal Models | C57BL/6J Mice | Standardized model for diet-induced obesity & MetS | Ensure consistent genetic background; control for microbiome via co-housing. |
| Induction Diets | High-Fat Diet (HFD) with Fructose/Sucrose | Induces metabolic syndrome phenotypes (obesity, IR, inflammation) | Common formulations: D12451 (45% fat) or D12492 (60% fat) from Research Diets. |
| Probiotic Strains | Lactobacillus rhamnosus GG (LGG)Akkermansia muciniphila | Live beneficial microorganisms for intervention studies | Verify viability (CFU count) and purity. A. muciniphila requires specialized culture. |
| Prebiotics | Inulin, Fructo-oligosaccharides (FOS) | Selective substrates to stimulate growth of beneficial bacteria | Incorporate into diet at 5-10% (w/w) or administer via gavage. |
| Molecular Kits | 16S rRNA Gene Sequencing Kit (e.g., Illumina) | Profiling gut microbiota composition & diversity | Standardize DNA extraction method; target V3-V4 hypervariable regions. |
| Biomarker Assays | ELISA Kits for LPS, TNF-α, IL-6, Adiponectin | Quantifying systemic inflammation & metabolic parameters | Use high-sensitivity kits for detecting low-grade inflammation. |
| Permeability Assay | FITC-labeled Dextran (4.4 kDa) | Assessing intestinal barrier integrity in vivo | Standard dose: 400-600 mg/kg; measure serum fluorescence after 4 hours. |
| Cell Culture Models | Caco-2 cell line | In vitro model of human intestinal epithelium | Used for studying barrier function (Transepithelial Electrical Resistance - TEER). |
The strategic modulation of the gut microbiota through probiotics, prebiotics, and polyphenols presents a powerful, multifaceted approach to mitigating the chronic low-grade inflammation that underpins metabolic syndrome. The evidence synthesized in this whitepaper underscores that these interventions work in concert through complementary mechanisms: probiotics directly engage with host immunity and barrier function, prebiotics selectively nourish a beneficial microbial ecosystem to generate anti-inflammatory metabolites, and polyphenols, often derived from traditional medicinal plants, are bio-transformed by the microbiota into potent therapeutic compounds. The consistent observation that these approaches can increase the abundance of keystone species like Akkermansia muciniphila, reduce systemic inflammatory markers, and improve metabolic parameters provides a compelling rationale for their continued investigation.
For researchers and drug developers, the path forward requires a commitment to rigor and personalization. Standardized experimental protocols, as detailed herein, are crucial for generating reproducible and comparable data. Future success will hinge on leveraging multi-omics technologies to move beyond correlative analyses and establish causative links between specific microbial functions and host metabolism. Furthermore, the significant inter-individual variability in gut microbiome composition demands a shift toward personalized nutrition and medicine. By integrating deep microbial phenotyping with clinical data, it will be possible to match specific intervention types—and specific strains or compounds—to the individuals most likely to benefit, ultimately enabling more effective and targeted therapies for combating metabolic syndrome and its inflammatory complications.
Metabolic Syndrome (MetS) represents a cluster of cardiometabolic risk factors—including abdominal obesity, dyslipidemia, hypertension, and hyperglycemia—that collectively confer a significantly elevated risk for type 2 diabetes and cardiovascular disease [122]. The global prevalence of MetS is estimated to affect approximately one-quarter of the world's adult population, making it a pressing public health challenge [123]. Central to the pathophysiology of MetS is chronic low-grade systemic inflammation, which serves as a critical mechanistic link between obesity, insulin resistance, and associated metabolic disturbances [122].
This inflammatory state, sometimes termed "metaflammation" (metabolic inflammation), is characterized by abnormal production of adipokines and cytokines, activation of inflammatory signaling pathways, and elevated circulating levels of inflammatory biomarkers such as C-reactive protein (CRP), interleukin-6 (IL-6), and tumor necrosis factor-alpha (TNF-α) [124] [125]. The expanded understanding of inflammation's role has shifted therapeutic focus toward modifiable lifestyle factors, particularly diet and physical activity, which can directly modulate inflammatory tone independent of pharmaceutical interventions [126] [124]. This technical review examines the evidence for lifestyle interventions targeting inflammatory pathways within MetS, providing researchers and drug development professionals with mechanistic insights and methodological frameworks for future investigations.
Dietary Interventions and Inflammatory Potential
Quantifying Dietary Inflammatory Potential
The inflammatory potential of diet can be systematically quantified using several validated indices. The Dietary Inflammatory Index (DII) and Empirical Dietary Inflammatory Pattern (EDIP) are the most widely employed tools for this purpose [123]. The DII is a literature-derived, nutrient-based index that assesses a diet's overall inflammatory potential, with higher scores indicating a more pro-inflammatory dietary pattern [127]. In contrast, the EDIP is an empirically-derived index based on food groups that directly explains variation in inflammatory biomarkers, making it particularly useful for reflecting real-world dietary patterns [123].
Recent research has adapted these tools for specific populations. The EDIP-Asian (EDIP-A) score, for instance, was developed and validated in multi-ethnic Asian cohorts in Singapore and significantly predicts MetS incidence (OR: 1.13, 95% CI: 1.02-1.26) [123]. This adaptation highlights the importance of culturally relevant dietary assessment tools in nutrition research.
Table 1: Dietary Indices for Assessing Inflammatory Potential
| Index Name | Basis of Development | Key Components | Associated Biomarkers |
|---|---|---|---|
| Dietary Inflammatory Index (DII) | Literature-derived, nutrient-based | Overall nutrient inflammatory potential | CRP, IL-6, TNF-αR2, adiponectin |
| Empirical Dietary Inflammatory Pattern (EDIP) | Food group-based, empirical | Pro- and anti-inflammatory food groups | CRP, IL-6, GlycA |
| EDIP-Asian (EDIP-A) | Adapted for Asian populations | Culturally relevant food groups | hsCRP, IL-6 |
Pro-Inflammatory Dietary Patterns
Diets characterized by high consumption of ultra-processed foods (UPF), refined carbohydrates, saturated fats, and processed meats consistently demonstrate pro-inflammatory effects [126] [125]. A recent scoping review of 24 studies found that higher UPF consumption was most consistently associated with elevated CRP levels in both adults and pediatric populations [125]. Proposed mechanisms for these effects include:
- Gut barrier disruption: Emulsifiers and artificial additives in UPF can impair intestinal tight junction function, increasing permeability and facilitating bacterial translocation [125].
- Microbiome alterations: UPF typically lacks fermentable fiber, reducing production of anti-inflammatory short-chain fatty acids by gut microbiota [125].
- Advanced glycation end-products (AGEs): Heating and processing techniques generate AGEs that can activate inflammatory pathways through receptor binding [126].
The Western dietary pattern exemplifies a pro-inflammatory diet, with its characteristic high levels of processed meats, high-fat dairy, refined grains, sugar-sweetened beverages, and corresponding low intake of fruits, vegetables, and whole grains [126]. This pattern is associated with elevated levels of CRP, IL-6, and TNF-α, creating an inflammatory milieu that promotes insulin resistance and metabolic dysfunction [126].
Anti-Inflammatory Dietary Patterns
In contrast, anti-inflammatory dietary patterns such as the Mediterranean diet, DASH (Dietary Approaches to Stop Hypertension) diet, and traditional Asian diets share common features: abundant fruits and vegetables, whole grains, unsaturated fats (particularly olive oil), legumes, and lean protein sources with minimal red meat and processed foods [126]. These patterns are rich in bioactive compounds with anti-inflammatory properties, including:
- Polyphenols and flavonoids: Found in colorful fruits and vegetables, these compounds can inhibit NF-κB signaling and reduce pro-inflammatory cytokine production [126].
- Omega-3 fatty acids: Present in fish, nuts, and seeds, they serve as precursors to specialized pro-resolving mediators that actively resolve inflammation [126].
- Fiber and resistant starch: Promote gut health and production of anti-inflammatory short-chain fatty acids like butyrate [125].
Intervention studies demonstrate that adherence to anti-inflammatory dietary patterns significantly reduces circulating inflammatory markers. A study of children with obesity found that those with more anti-inflammatory diets had significantly lower DII scores and corresponding reductions in inflammatory biomarkers, though some associations were attenuated after adjustment for confounders [127].
Diagram 1: Dietary influence on inflammatory pathways. The diagram illustrates how pro- and anti-inflammatory dietary patterns modulate different mechanistic pathways and ultimately affect inflammatory biomarker levels. SCFA: short-chain fatty acids; PPAR: peroxisome proliferator-activated receptor gamma.
Exercise as an Anti-Inflammatory Intervention
Exercise Modalities and Metabolic Health
Physical activity represents a powerful non-pharmacological strategy for reducing chronic inflammation. Different exercise modalities induce distinct but complementary physiological adaptations that collectively improve metabolic health and reduce inflammatory tone [128].
Table 2: Exercise Modalities and Their Effects on Metabolic and Inflammatory Markers
| Exercise Modality | Primary Physiological Adaptations | Impact on Inflammatory Markers | Effect on Metabolic Parameters |
|---|---|---|---|
| Aerobic Training | ↑ AMPK activation, ↑ fatty acid oxidation, ↑ mitochondrial biogenesis, ↓ visceral adipose tissue | ↓ CRP, ↓ TNF-α, ↓ IL-6 | ↓ Fasting glucose, ↓ triglycerides, ↓ LDL-C, ↑ HDL-C |
| Resistance Training | ↑ mTOR activation, ↑ muscle hypertrophy, ↑ resting energy expenditure, ↑ glucose uptake | ↓ CRP, ↓ IL-6, ↑ adiponectin | Improved insulin sensitivity, favorable body composition changes |
| Combined Training | Combined benefits of aerobic and resistance exercise; potential synergistic effects | ↓ CRP, ↓ TNF-α, improved inflammatory profile | ↓ Fasting glucose, ↓ fasting insulin, ↓ HOMA-IR, improved lipid profile |
A comprehensive meta-analysis of 10 clinical trials demonstrated that different exercise modalities produce distinct effects on MetS indicators. Aerobic training significantly reduced total cholesterol (-23.70 mg/dL, p=0.003), fasting blood glucose (-0.66 mg/dL, p=0.02), and diastolic blood pressure (-0.79 mmHg, p=0.02), while combined training significantly improved HDL (0.12 mg/dL, p=0.004) and fasting blood glucose (-1.42 mg/dL, p=0.01) [128].
Mechanistic Basis for Exercise-Induced Anti-Inflammatory Effects
The anti-inflammatory effects of exercise training are mediated through multiple interconnected mechanisms:
Visceral adipose tissue reduction: Exercise training, particularly aerobic exercise, preferentially reduces visceral adipose tissue mass, a major source of pro-inflammatory cytokines [124]. This reduction decreases the production of adipokines such as TNF-α and IL-6 while increasing anti-inflammatory adiponectin secretion [124] [129].
Myokine production: Contracting skeletal muscle functions as an endocrine organ, releasing myokines including IL-6, which induces an anti-inflammatory environment by stimulating the production of IL-10 and IL-1ra while inhibiting TNF-α production [124].
Toll-like receptor (TLR) regulation: Exercise training downregulates the expression of pattern recognition receptors such as TLR4 on monocytes and macrophages, reducing their responsiveness to inflammatory stimuli [124].
Improved glucose metabolism: By enhancing insulin sensitivity and glucose disposal, exercise reduces hyperglycemia-induced oxidative stress and inflammatory pathway activation [129].
Autonomic nervous system regulation: Exercise training increases vagal tone, which exerts anti-inflammatory effects through the cholinergic anti-inflammatory pathway [124].
Recent evidence confirms that these anti-inflammatory effects occur independently of body weight changes, suggesting that exercise has direct body fat-independent anti-inflammatory properties [124]. This is particularly relevant for drug development, as it highlights distinct mechanisms that might be targeted pharmacologically.
Protocol for Combined Exercise Training Intervention
For researchers designing exercise interventions to study inflammatory outcomes in MetS, the following protocol exemplifies current best practices based on recent meta-analyses:
Program Design:
- Duration: 12-24 weeks
- Frequency: 3-5 sessions per week
- Session Structure: Combined aerobic and resistance training
Aerobic Component:
- Intensity: Moderate to vigorous (50-80% VOâ‚‚ max or heart rate reserve)
- Duration: 30-45 minutes per session
- Modality: Walking, cycling, or other continuous rhythmic activities
Resistance Component:
- Exercises: 6-8 multi-joint exercises targeting major muscle groups
- Intensity: 60-80% of one-repetition maximum (1RM)
- Volume: 2-4 sets of 8-15 repetitions per exercise
- Progression: Systematic increase in load (5-10%) when target repetitions are achieved
This combined exercise approach has demonstrated significant effects on both inflammatory markers and metabolic parameters in sedentary adults. A systematic review and meta-analysis of 24 randomized controlled trials found that combined training significantly decreased fasting glucose (SMD: -0.474, p=0.009), fasting insulin (SMD: -1.024, p<0.001), HOMA-IR (SMD: -0.946, p<0.001), TNF-α (SMD: -0.972, p<0.001), and CRP (SMD: -0.507, p=0.001) [129].
Diagram 2: Exercise-induced anti-inflammatory pathways. The diagram illustrates acute and chronic mechanisms through which different exercise modalities reduce systemic inflammation. TLR: Toll-like receptor; IL-1ra: interleukin-1 receptor antagonist.
Synergistic Effects of Combined Lifestyle Interventions
Emerging evidence suggests that diet and exercise interventions may have synergistic effects on inflammatory tone and metabolic health. A cross-sectional study of 2,349 elderly participants found that moderate-intensity physical activity was negatively correlated with CRP (r=-0.129) and blood glucose (r=-0.127) levels, and that these relationships were mediated by specific dietary components [130]. Mediation analysis revealed that the intake of dark green leafy vegetables significantly mediated the relationship between physical activity and CRP levels, while vitamin B12 intake mediated the relationship between physical activity and blood glucose levels [130].
This suggests that the anti-inflammatory effects of physical activity may be partially explained by associated improvements in dietary patterns, highlighting the complex interplay between these lifestyle factors. The same study found that moderate-intensity physical activity was positively associated with intake of dark green leafy vegetables (β=0.174) and negatively associated with consumption of unprocessed red meat (β=-0.112) and deep-fried foods (β=-0.117) [130].
From a drug development perspective, understanding these synergistic pathways may inform combination therapies that target multiple mechanisms simultaneously. The finding that lifestyle interventions can reduce inflammation through both dependent and independent pathways suggests potential for multi-target pharmacological approaches in MetS treatment.
Research Toolkit: Methodologies and Biomarkers
Essential Methodologies for Lifestyle Intervention Research
For researchers investigating lifestyle interventions in MetS, several methodological approaches are essential:
Dietary Assessment Methods:
- Food Frequency Questionnaires (FFQ): Validated, semi-quantitative instruments (e.g., 168-item FFQ) to assess habitual dietary intake [127] [123].
- 24-hour dietary recalls: Multiple recalls (including weekdays and weekends) to estimate specific nutrient intakes [130].
- Dietary Inflammatory Indices: Calculation of DII or EDIP scores to quantify overall inflammatory potential of diet [127] [123].
Physical Activity Assessment:
- International Physical Activity Questionnaire (IPAQ): Validated tool for categorizing activity levels as low, moderate, or vigorous based on MET-minutes/week [130].
- Exercise Intervention Protocols: Standardized programs with precise specification of type, intensity, duration, and progression [128] [129].
Body Composition Analysis:
- Anthropometric measurements: Body mass index, waist circumference [128].
- Advanced body composition: DEXA or other methods to quantify visceral adipose tissue reduction [124].
Key Biomarkers for Assessing Inflammatory Tone
A comprehensive assessment of inflammatory tone in MetS should include the following biomarkers:
Table 3: Essential Biomarkers for Assessing Inflammatory Tone in Metabolic Syndrome Research
| Biomarker Category | Specific Markers | Biological Significance | Assessment Methods |
|---|---|---|---|
| Acute Phase Proteins | High-sensitivity CRP (hs-CRP) | Hepatic production induced by IL-6; independent cardiovascular risk predictor | Immunoassays (ELISA, immunoturbidimetric) |
| Pro-inflammatory Cytokines | IL-6, TNF-α, IL-1β | Central mediators of inflammatory signaling; correlate with insulin resistance | Multiplex immunoassays, ELISA |
| Anti-inflammatory Cytokines | IL-10, IL-1ra | Counter-regulatory cytokines that limit inflammation | Multiplex immunoassays, ELISA |
| Adipokines | Leptin, Adiponectin | Adipose tissue-derived hormones; link obesity to inflammation | ELISA |
| Novel Inflammatory Indices | Systemic Immune-Inflammation Index (SII), Systemic Inflammation Response Index (SIRI) | Composite markers incorporating multiple cell counts | Calculated from complete blood count |
| Metabolic-Inflammatory Cross-talk Markers | Triglyceride-glucose index (TyG), NHHR (non-HDL-C/HDL-C ratio) | Integrated measures of metabolic and inflammatory dysfunction | Calculated from lipid profiles and glucose |
Experimental Considerations for Clinical Trials
When designing clinical trials to evaluate lifestyle interventions for inflammatory tone in MetS, several key considerations emerge from recent research:
Population characteristics: Age significantly influences intervention response, with younger populations often showing more pronounced improvements in inflammatory markers [131]. Sex differences in adipokine responses should also be accounted for in study design [130].
Intervention duration: Most exercise interventions of 12 weeks or longer demonstrate significant effects on inflammatory markers, though some changes in glucose metabolism may be detectable earlier [129].
Control for confounding: Careful adjustment for body composition changes is necessary to distinguish direct anti-inflammatory effects from those mediated through fat mass reduction [124].
Novel biomarker inclusion: Incorporating emerging markers such as GlycA (glycoprotein acetylation) may provide additional insight into inflammatory processes [123].
Lifestyle interventions targeting diet and physical activity represent powerful approaches for modulating inflammatory tone in Metabolic Syndrome. The evidence reviewed demonstrates that both anti-inflammatory dietary patterns and regular exercise produce significant reductions in systemic inflammation through distinct but complementary mechanisms. For drug development professionals, understanding these mechanisms provides valuable insights for target identification and validation. Future research should focus on elucidating the synergistic effects of combined lifestyle interventions, identifying personalized approaches based on genetic and phenotypic characteristics, and developing more targeted anti-inflammatory strategies based on the mechanistic pathways engaged by diet and exercise.
Challenges in Drug Specificity, Systemic Side Effects, and Patient Stratification
Metabolic syndrome (MetS) is a complex condition characterized by a cluster of metabolic disorders, including central obesity, dyslipidemia, hypertension, and insulin resistance [2]. A key pathophysiological feature of MetS is chronic low-grade inflammation, which serves as a critical driver of disease progression and associated complications [47] [2]. This inflammatory state, primarily originating from adipose tissue, involves the secretion of numerous pro-inflammatory factors such as interleukin-6 (IL-6), tumor necrosis factor α (TNF-α), and interleukin-1β (IL-1β) that disrupt insulin signaling and promote metabolic dysfunction [47]. Within this context, drug development faces three fundamental challenges: achieving sufficient specificity for inflammatory targets within the metabolic landscape, minimizing systemic side effects from therapeutic interventions, and developing precise patient stratification strategies to identify those most likely to respond to anti-inflammatory approaches. These challenges are particularly pronounced in MetS, where the inflammatory processes are systemic, chronic, and intricately intertwined with core metabolic pathways.
The relationship between inflammatory biomarkers and MetS can be quantified to establish robust associations and stratification parameters. Recent research has validated the Low-grade Inflammation Score (INFLA-score), a composite index based on C-reactive protein (CRP), white blood cell count (WBC), platelet count, and neutrophil-to-lymphocyte ratio (NLR), as a significant predictor of MetS and its components [47].
Table 1: Association between INFLA-Score and Metabolic Syndrome Risk
| Study Population | INFLA-Score Metric | Risk Association with MetS | Key Findings |
|---|---|---|---|
| Oilfield Shift Workers (n=1,758) [47] | Per 1-unit increase | OR = 1.08 (95% CI: 1.07-1.10) | Positive dose-response relationship established |
| Oilfield Shift Workers (n=1,758) [47] | Highest Quartile (Q4) vs. Lowest (Q1) | OR = 3.58 | Q4 group had 3.58x higher risk of MetS than Q1 group |
| Oilfield Shift Workers (n=1,758) [47] | Sex-based Analysis | Men: OR = 1.07 (95% CI: 1.05-1.09)Women: OR = 1.13 (95% CI: 1.09-1.16) | Significant interaction, with women at higher risk |
Table 2: INFLA-Score Associations with Individual Components of Metabolic Syndrome
| MetS Component | Association with INFLA-Score | Statistical Significance |
|---|---|---|
| Elevated Blood Glucose | Positive Association | p < 0.001 |
| Elevated Blood Pressure | Positive Association | p < 0.001 |
| Increased Waist Circumference | Positive Association | p < 0.001 |
| Elevated Triglyceride Levels | Positive Association | p < 0.001 |
| Reduced HDL Cholesterol | Positive Association | p < 0.001 |
Challenge 1: Drug Specificity in Targeting Inflammatory Pathways
The Specificity Problem in Metabolic Inflammation
Achieving drug specificity in MetS is challenging due to the pleiotropic nature of inflammatory signaling pathways and their extensive crosstalk with metabolic processes. In the context of MetS, inflammatory mediators such as TNF-α and IL-6 not only promote systemic inflammation but also directly interfere with insulin signaling through the inhibition of insulin receptor substrate (IRS) proteins and downstream kinase pathways [47] [2]. This creates a complex network of interactions where targeted inhibition of a single inflammatory mediator may be insufficient to reverse metabolic dysfunction, while broad anti-inflammatory approaches risk disrupting essential immune surveillance and defense mechanisms.
Experimental Approaches for Specificity Validation
Protocol 1: Specificity Profiling for Novel Anti-inflammatory Compounds
- Objective: To evaluate the binding specificity and functional selectivity of candidate compounds for inflammatory targets relevant to MetS.
- Methodology:
- Target Panel Screening: Utilize kinase profiling assays (e.g., radiometric or mobility shift assays) and cytokine receptor binding panels to quantify compound affinity against 50+ related kinases and receptors.
- Cellular Pathway Mapping: Treat cultured adipocytes, hepatocytes, and macrophages with candidate compounds and measure phosphorylation states of key signaling nodes (e.g., JNK, IKKβ, p38 MAPK) via multiplex immunoassays.
- Transcriptomic Analysis: Perform RNA sequencing on treated cells to assess global changes in gene expression, specifically monitoring off-target effects on metabolic genes.
- Key Outputs: Dose-response curves (IC50 values for intended vs. off-targets), a selectivity score, and a pathway modulation index.
Challenge 2: Mitigating Systemic Side Effects
Origins of Systemic Toxicity
Systemic side effects arising from anti-inflammatory therapies in MetS patients often stem from the ubiquitous expression of inflammatory targets and their roles in normal physiological processes. For instance, glucocorticoids, while potent anti-inflammatory agents, exacerbate metabolic abnormalities like insulin resistance and dyslipidemia, directly counteracting therapeutic goals in MetS [2]. Furthermore, the liver's central role in both drug metabolism and the pathogenesis of MetS (e.g., in non-alcoholic fatty liver disease) creates a vulnerability to hepatotoxicity, a common side effect of systemically administered drugs.
Model-Informed Drug Development (MIDD) for Safety Optimization
Model-Informed Drug Development (MIDD) integrates quantitative modeling and simulation to predict and mitigate side effects early in the development process [132]. Key methodologies include:
- Physiologically Based Pharmacokinetic (PBPK) Modeling: Simulates drug absorption, distribution, metabolism, and excretion (ADME) to predict tissue-specific exposure, particularly in metabolically active tissues like liver and adipose [132].
- Quantitative Systems Pharmacology (QSP): Builds computational models that integrate drug action with disease pathophysiology (e.g., the interplay between inflammation and insulin signaling) to simulate both efficacy and adverse outcomes in virtual patient populations [132].
Protocol 2: Preclinical Safety and Tolerability Assessment in MetS Context
- Objective: To characterize the potential metabolic side effects of a novel anti-inflammatory agent in a physiologically relevant model system.
- In Vivo Model: Diet-induced obese (DIO) rodent model or a transgenic model (e.g., leptin-deficient ob/ob mice) that recapitulates key features of human MetS.
- Dosing Regimen: 4-8 weeks of treatment with the candidate drug, including a positive control (e.g., a known anti-inflammatory with metabolic side effects) and a vehicle control.
- Core Metabolic Phenotyping Endpoints:
- Glucose Homeostasis: Intraperitoneal glucose tolerance test (IPGTT) and insulin tolerance test (ITT).
- Systemic Metabolism: Indirect calorimetry to measure energy expenditure and respiratory exchange ratio.
- Serum Biomarkers: Comprehensive plasma lipid profiling (triglycerides, HDL, LDL), liver enzymes (ALT, AST), and adipokine levels (leptin, adiponectin).
- Histopathology: Analysis of liver, adipose tissue, and pancreas for signs of steatosis, inflammation, and cellular integrity.
Challenge 3: Patient Stratification for Targeted Therapies
The Imperative for Precision in MetS
MetS represents a highly heterogeneous condition, and individual variability in the inflammatory drivers of metabolic dysfunction means that anti-inflammatory therapies will not be universally effective. The INFLA-score study demonstrated that the relationship between inflammation and MetS risk is not uniform, with a significantly stronger association observed in women compared to men [47]. This underscores the critical need for robust stratification biomarkers to identify patient subpopulations most likely to benefit from a given therapy, thereby increasing clinical trial success rates and maximizing therapeutic benefit.
Advanced Stratification Methodologies
Multi-Omics Integration: A powerful approach involves the integration of data from multiple molecular layers to define patient subtypes [133].
- Genomics: Identifies single-nucleotide polymorphisms (SNPs) and structural variations in genes related to inflammation and metabolism (e.g., APOC3 variants associated with MetS risk) [2] [134].
- Transcriptomics: Reveals gene expression signatures in blood or adipose tissue that reflect the activity of specific inflammatory pathways.
- Proteomics: Quantifies circulating levels of proteins (e.g., CRP, IL-6, TNF-α, adiponectin) to provide a functional readout of the inflammatory state [47].
Artificial Intelligence in Histopathology: Advanced AI algorithms, particularly deep learning models applied to histopathology images, can identify complex morphological patterns in tissue biopsies (e.g., liver or adipose) that are predictive of treatment response and are invisible to the human eye [135]. These models can be trained using self-supervised learning on large image repositories, reducing the need for manual annotation.
Protocol 3: Developing a Stratification Biomarker Signature
- Objective: To derive and validate a biomarker signature that predicts response to an anti-inflammatory therapy in MetS patients.
- Study Design: A prospective, randomized clinical trial with a pre-specified biomarker analysis plan. Baseline samples (plasma, serum, PBMCs) are collected from all participants.
- Methodology:
- Discovery Cohort: Use untargeted proteomics and transcriptomics on baseline samples from responders vs. non-responders to identify a candidate panel of biomarkers.
- Assay Development: Develop a targeted, clinically applicable assay (e.g., multiplex immunoassay or qPCR) for the candidate biomarkers.
- Validation: Lock down the algorithm (e.g., a weighted score combining INFLA-score with specific protein biomarkers) and test its predictive performance in a blinded, independent validation cohort.
- Key Outputs: A validated biomarker signature with defined cut-off values, associated with a probability of response to therapy.
Table 3: Key Research Reagent Solutions for Investigating Inflammation in Metabolic Syndrome
| Reagent / Tool | Primary Function | Application in MetS Research |
|---|---|---|
| Multiplex Immunoassay Panels | Simultaneous quantification of multiple cytokines/chemokines (e.g., IL-6, TNF-α, IL-1β, leptin, adiponectin) | Profiling inflammatory and adipokine signatures in patient serum or cell culture supernatants [47]. |
| Phospho-Specific Antibodies | Detection of phosphorylated signaling proteins (e.g., p-IRS-1, p-JNK, p-IKK) via Western Blot or ELISA | Interrogating insulin signaling and inflammatory pathway activation in tissue lysates [2]. |
| Patient-Derived Organoids (PDOs) | 3D in vitro models derived from human tissues (e.g., liver, adipose). | Studying cell-type-specific responses to drug treatments and modeling patient-specific disease pathophysiology [133]. |
| INFLA-Score Components (CRP, WBC, Platelet Count, NLR) | Calculation of a composite low-grade inflammation score. | Stratifying patient cohorts for clinical studies and linking systemic inflammation to MetS components [47]. |
| Liquid Chromatography-Mass Spectrometry (LC-MS) | Global and targeted analysis of metabolites and lipids. | Identifying lipid species and metabolic intermediates linked to inflammation and insulin resistance [133]. |
Integrated Workflow and Future Directions
Addressing the interconnected challenges of specificity, safety, and stratification requires an integrated workflow that leverages modern computational and experimental tools. The future of drug development in MetS lies in combining Model-Informed Drug Development (MIDD) approaches with advanced patient stratification techniques from the earliest stages of research [132] [135] [133]. This includes using QSP models to simulate clinical trials in virtual populations defined by multi-omics data, thereby de-risking and informing the design of actual clinical studies. Furthermore, the application of AI for the discovery of novel digital biomarkers from histopathology images or other clinical data holds the promise of further refining patient stratification, ensuring that the right patients receive the right anti-inflammatory therapy, ultimately improving success rates in the clinic and patient outcomes.
Bench to Bedside: Comparative Analysis of Therapeutic Strategies and Clinical Validation
The management of low-grade chronic inflammation, a cornerstone of metabolic syndrome (MetS), presents a critical therapeutic challenge. This in-depth technical review provides a systematic comparison of two foundational strategies: lifestyle modification and pharmacological anti-inflammatory therapy. We synthesize current molecular evidence, detailing the mechanisms by which dietary interventions, physical activity, and weight loss counteract inflammation through pathways such as AMPK activation and gut microbiota modulation. Concurrently, we evaluate advanced pharmacological agents, including glucagon-like peptide-1 receptor agonists (GLP-1 RAs) and natural compounds like berberine, which target inflammation via direct receptor-mediated and systemic effects. By integrating quantitative data from recent clinical trials, experimental protocols, and mechanistic diagrams, this review serves as a comprehensive resource for researchers and drug development professionals navigating the complexities of anti-inflammatory therapeutic development for MetS.
Metabolic syndrome (MetS) is a cluster of conditions—including central obesity, insulin resistance, dyslipidemia, and hypertension—that collectively increase the risk of type 2 diabetes (T2D) and cardiovascular disease (CVD) [136] [137]. A key underlying feature of MetS is a state of chronic, low-grade inflammation, which is now recognized as a fundamental pathogenetic event rather than a mere association [138] [122]. This proinflammatory state is characterized by elevated circulating levels of inflammatory cytokines such as TNF-α, IL-6, and C-reactive protein (CRP), and is driven by complex interactions between adipose tissue dysfunction, immune cell activation, and gut microbiota alterations [136] [138].
The triggers for this inflammatory cascade are multifaceted. In obesity, expanding adipose tissue undergoes significant remodeling, leading to adipocyte hypertrophy, hypoxia, and mechanical stress [138]. This promotes the secretion of proinflammatory adipokines and chemokines, which in turn drive the infiltration and activation of immune cells, particularly M1-polarized macrophages [138]. Concurrently, disturbances in gut microbiota composition and function can increase intestinal permeability, leading to elevated systemic levels of bacterial lipopolysaccharide (LPS) and other microbial products that perpetuate inflammation through pattern recognition receptor (PRR) signaling [136] [138]. This inflammatory signaling directly impairs insulin action in metabolic tissues and promotes endothelial dysfunction, creating a vicious cycle that exacerbates MetS components [138] [122].
Targeting this inflammatory basis provides a rational therapeutic strategy. This review conducts a head-to-head comparison of the two primary approaches: multifaceted lifestyle modification and targeted pharmacological anti-inflammatory therapy, framing this analysis within the context of a broader thesis on managing chronic inflammation in MetS.
Lifestyle Modification: Mechanisms and Protocols
Lifestyle modification, which encompasses dietary changes, increased physical activity, and weight management, represents the first-line intervention for MetS and its associated inflammatory state. Its effects are mediated through a multitude of interconnected physiological pathways.
Molecular Anti-Inflammatory Mechanisms of Lifestyle Intervention
Lifestyle interventions counteract inflammation through several key mechanisms:
- Reduction of Adipose Tissue Inflammation: Weight loss, particularly a reduction in visceral adipose tissue, decreases the production of pro-inflammatory adipokines (e.g., TNF-α, IL-6) and reduces macrophage infiltration into adipose depots, shifting the balance from a pro-inflammatory M1 phenotype to an anti-inflammatory M2 phenotype [138] [139].
- Enhancement of Gut Microbiome Homeostasis: Dietary components like prebiotic fibers and polyphenols serve as substrates for beneficial gut bacteria, promoting the production of anti-inflammatory metabolites, particularly short-chain fatty acids (SCFAs) like butyrate [136] [140]. SCFAs strengthen the intestinal barrier, reducing endotoxin translocation, and signal through G protein-coupled receptors (GPCRs) to exert anti-inflammatory and insulin-sensitizing effects [136].
- Activation of Key Signaling Pathways: Polyphenols from plant-based foods and traditional medicines can activate AMP-activated protein kinase (AMPK) and silence sirtuin 1 (SIRT1), pathways that improve mitochondrial function and suppress NF-κB–driven inflammation [136] [141]. Physical exercise similarly activates these pathways, enhancing oxidative metabolism and reducing oxidative stress [139].
Experimental Evidence and Quantitative Outcomes
Recent clinical trials provide robust quantitative data on the efficacy of lifestyle-related interventions in reducing inflammatory biomarkers.
Table 1: Anti-Inflammatory Effects of Specific Lifestyle-Related Interventions from Clinical Studies
| Intervention | Study Details | Key Inflammatory Marker Reductions | Effect Size (Cohen's d or β with 95% CI) |
|---|---|---|---|
| Synbiotic (Kefir + Prebiotic Mix) [140] | 6-week RCT; n=20 (Synbiotic) vs n=20 (Control) | IL-6 | d = -0.882 (-1.36 to -0.17) |
| IFN-γ | d = -0.940 (-2.03 to -0.31) | ||
| TNF-α | Significant reduction (p<0.05) | ||
| Inulin Fibre [140] | 6-week RCT; n=31 | TNF-α | d = -1.012 (-0.71 to -0.20) |
| Omega-3 Fatty Acids [140] | 6-week RCT; n=33 | TNF-α | d = -0.618 (-0.73 to -0.09) |
| Combined Adverse Lifestyle Score Deterioration [142] | 2-month observational; n=179 | Increase in IL-17A (per 1-pt score increase) | β = 0.98 (0.23 to 1.73) pg/mL |
| Increase in IFN-γ (per 1-pt score increase) | β = 1.79 (0.39 to 3.18) pg/mL | ||
| Decreased Daily Activity [142] | 2-month observational; n=179 | Increase in IL-17A | β = 1.83 (0.53 to 3.13) pg/mL |
| Increase in IFN-γ | β = 2.59 (0.9 to 4.98) pg/mL |
The data in Table 1 demonstrate that targeted dietary supplements can produce significant anti-inflammatory effects over a relatively short period. The synbiotic intervention, in particular, showed a broad effect on multiple cytokines. Furthermore, the observational data underscores that deteriorations in lifestyle, especially in physical activity, are directly linked to a quantifiable increase in pro-inflammatory cytokines [142].
Longer-term studies focused on weight loss confirm these findings. In a 2-year study, obese patients who achieved a weight loss of ≥10% saw the prevalence of MetS drop dramatically, whereas it remained high in those who lost <10% [137]. This highlights that the magnitude of lifestyle change directly correlates with metabolic and inflammatory improvement.
Detailed Experimental Protocol: 6-Week Synbiotic Intervention
The following protocol is adapted from the study that demonstrated broad anti-inflammatory effects [140] and serves as a template for designing clinical interventions.
- Objective: To evaluate the effects of a 6-week synbiotic supplementation on systemic inflammatory biomarkers in adults.
- Study Design: Randomized controlled trial (RCT) with a parallel control group.
- Participants:
- Inclusion Criteria: Adults aged >18 years with a Body Mass Index (BMI) between 20 and 39.9 kg/m².
- Exclusion Criteria: Gastrointestinal conditions (IBS, IBD, coeliac), lactose intolerance, diabetes, other inflammatory conditions (e.g., asthma, psoriasis), use of fibre/probiotic supplements, use of prescribed medication, and pregnancy.
- Intervention Arm:
- Synbiotic Preparation: 170 ml of kefir (containing 27 live bacterial cultures) combined with 10 g of a proprietary prebiotic mix (including arabinoxylan, beta-glucans, FOS, inulin, GOS, etc.).
- Administration: Consumed daily as a smoothie for 6 weeks.
- Control Arm: No intervention for 6 weeks.
- Data Collection (Baseline and 6-week follow-up):
- Blood Sample Collection: Fasting venous blood drawn into serum separation tubes. Samples are left to clot at room temperature for 15 minutes, centrifuged at 3000 RCF for 10 minutes, aliquoted, and stored at -80°C.
- Inflammatory Biomarker Profiling: Serum analysis using the Olink Target 96 Inflammation panel (Olink Bioscience, Uppsala, Sweden), which utilizes Proximity Extension Assay (PEA) technology for high-sensitivity multiplex quantification of 92 proteins.
- Anthropometric Measures: Height, weight, and BMI.
- Statistical Analysis: Changes in inflammatory markers from baseline are analyzed using parametric methods. Effect sizes (e.g., Cohen's d) are calculated, and a False Discovery Rate (FDR) adjusted p-value < 0.05 is considered significant.
The following workflow diagram visualizes this experimental protocol.
Pharmacological Anti-Inflammatory Therapy: Mechanisms and Protocols
Pharmacological strategies offer a targeted approach to mitigating inflammation in MetS, ranging from repurposed diabetes medications to novel natural compounds.
Molecular Mechanisms of Pharmacological Agents
Key drug classes exert anti-inflammatory effects through distinct and overlapping pathways:
- GLP-1 Receptor Agonists (GLP-1 RAs): Drugs like liraglutide, semaglutide, and tirzepatide reduce inflammation via both weight loss-dependent and independent mechanisms [143]. They directly modulate immune cells; for instance, intraepithelial lymphocytes express GLP-1 receptors, and their activation can suppress pro-inflammatory cytokine production. GLP-1 RAs also inhibit critical pro-inflammatory signaling pathways, including NF-κB DNA binding and downstream TNF-α and IL-1β expression [143].
- Natural Bioactive Compounds (e.g., Berberine): Berberine (BBR) is a multi-target agent with demonstrated anti-obesity and anti-inflammatory effects. Its mechanisms include:
- AMPK Activation: Enhances lipolysis and fatty acid β-oxidation while inhibiting inflammation [141].
- PPAR-γ Suppression: Inhibits adipogenesis, reducing the source of inflammatory adipokines [141].
- Gut Microbiota Modulation: Improves the integrity of the gut barrier and reduces metabolic endotoxemia [136] [141].
- NF-κB Pathway Inhibition: Directly suppresses a master regulator of inflammation [141].
Experimental Evidence and Quantitative Outcomes
Clinical trials have quantified the significant anti-inflammatory impact of these pharmacological agents.
Table 2: Anti-Inflammatory Effects of Pharmacological Agents from Clinical Studies
| Intervention | Study Details | Key Outcomes & Inflammatory Marker Reductions | Notes |
|---|---|---|---|
| Semaglutide (GLP-1 RA) [143] | SUSTAIN & PIONEER RCTs (T2D) | CRP reduced by 30% in PIONEER 2 | Only 20-60% of CRP reduction explained by glucose/weight loss. |
| Tirzepatide (GIP/GLP-1 RA) [143] | RCTs (T2D/Obesity) | Significant reduction in CRP | - |
| Oral Semaglutide vs. Empagliflozin [143] | PIONEER 2 RCT (T2D) | Semaglutide reduced CRP by 30%; Empagliflozin had no effect | Despite similar ~4% weight loss in both groups. |
| Berberine (BBR) [141] | Preclinical & Clinical studies | Dose-dependent reduction in body weight and inflammation. | Multi-target action on AMPK, gut microbiota, and NF-κB pathways. |
The data underscores the weight-loss independent anti-inflammatory properties of GLP-1 RAs. A single dose of exenatide or semaglutide was shown to reduce TNF-α levels in LPS-challenged mice within hours, precluding weight loss as a primary mechanism [143]. Similarly, the comparison with empagliflozin provides a compelling clinical control, isolating the potent anti-inflammatory effect of GLP-1 RAs [143].
Detailed Experimental Protocol: Assessing GLP-1 RA Anti-Inflammatory Action
This protocol outlines a method to dissect the weight loss-independent anti-inflammatory effects of GLP-1 RAs, a key area of research interest [143].
- Objective: To investigate the acute, weight loss-independent anti-inflammatory effects of a GLP-1 RA in an LPS-challenge model.
- In Vivo Model:
- Animals: C57BL/6J mice.
- Groups: (1) Vehicle + Saline, (2) Vehicle + LPS, (3) GLP-1 RA (e.g., exenatide or semaglutide) + LPS.
- Dosing: A single dose of GLP-1 RA or vehicle is administered intraperitoneally, followed by an IP injection of LPS (e.g., 1 mg/kg from E. coli) 1 hour later.
- Sample Collection: Blood and tissues (e.g., spleen, adipose tissue) are collected 3 hours post-LPS injection for analysis.
- In Vitro Model:
- Cell Culture: Human Peripheral Blood Mononuclear Cells (PBMCs) isolated from healthy donors.
- Treatment: PBMCs are pre-treated with a GLP-1 RA (e.g., exenatide, 100 nM) or vehicle for 1 hour, then stimulated with LPS (100 ng/mL) for 6-24 hours.
- Primary Outcome Measures:
- Plasma Cytokines: TNF-α, IL-6, and IL-1β levels measured by ELISA or multiplex immunoassay.
- NF-κB Pathway Activation: In PBMCs, nuclear translocation of NF-κB p65 subunit is assessed by immunofluorescence or western blot. DNA binding of NF-κB can be measured by Electrophoretic Mobility Shift Assay (EMSA).
- Gene Expression: mRNA levels of TNF, IL1B, and NFKBIA (IκBα) in PBMCs or tissues quantified by RT-qPCR.
The diagram below illustrates the key signaling pathways targeted by these pharmacological interventions.
The Scientist's Toolkit: Key Research Reagents and Models
This section details essential tools and models for investigating anti-inflammatory therapies in the context of MetS.
Table 3: Key Research Reagent Solutions for Metabolic Inflammation Studies
| Reagent / Model | Specification / Example | Primary Research Application |
|---|---|---|
| High-Sensitivity Multiplex Immunoassay | Olink Target 96 Inflammation Panel (PEA technology) [140] | Simultaneous, high-precision quantification of 92 human inflammatory proteins from low-volume serum samples. |
| Lipopolysaccharide (LPS) Challenge Model | E. coli LPS, 1 mg/kg (mouse, IP) [143] | A robust model for inducing acute systemic inflammation to test the rapid, direct anti-inflammatory efficacy of compounds independent of metabolic changes. |
| Diet-Induced Obese (DIO) Mouse Model | C57BL/6J mice fed High-Fat Diet (60% kcal from fat) for 12-16 weeks [141] | A gold-standard preclinical model that recapitulates the key features of human MetS, including obesity, insulin resistance, and chronic low-grade inflammation. |
| Gut Microbiota Profiling | 16S rRNA gene sequencing (e.g., Illumina MiSeq) [136] | To assess compositional changes in the gut microbiome (e.g., Firmicutes/Bacteroidetes ratio, abundance of Akkermansia) in response to prebiotic, probiotic, or drug interventions. |
| GLP-1 Receptor Agonists | Semaglutide, Liraglutide, Exenatide [143] | Pharmacological tools to probe the intersection of incretin signaling and immune regulation, using both in vivo and in vitro (e.g., PBMC) models. |
| Natural Bioactive Compounds | Berberine (BBR) [141] | A multi-target natural product to investigate pathways like AMPK activation, PPAR-γ suppression, and gut microbiota modulation in metabolic inflammation. |
Integrated Discussion and Future Directions
The evidence presented demonstrates that both lifestyle modification and pharmacological therapy exert potent anti-inflammatory effects in MetS, albeit through different primary mechanisms and timescales. Lifestyle interventions, particularly those incorporating synbiotics, fiber, and omega-3 fatty acids, work through a systems-level approach, modulating gut microbiota, reducing adiposity, and activating broad-spectrum anti-inflammatory pathways like AMPK [136] [140]. The strength of this approach lies in its multi-target nature and foundation in overall health. In contrast, pharmacological agents like GLP-1 RAs and berberine offer more direct and potent targeting of specific inflammatory nodes, such as GLP-1 receptors on immune cells or the NF-κB signaling cascade [143] [141]. This often results in a more rapid and pronounced reduction in specific inflammatory biomarkers, as seen with semaglutide's potent effect on CRP.
A critical consideration for drug development is the weight loss-dependent versus independent effects. GLP-1 RAs demonstrate that a significant portion of their anti-inflammatory action is independent of weight loss, pointing to direct immunomodulatory properties [143]. This separation of mechanisms is a key area for future research, as it could lead to therapies that decouple metabolic improvement from inflammation reduction. Furthermore, the gut microbiome emerges as a central player, being modulated effectively by both high-fiber dietary interventions and agents like berberine [136] [141]. Targeting the gut-inflammatory axis represents a promising frontier for both lifestyle and pharmacological strategies.
Future research should prioritize several key areas:
- Combination Therapy Trials: Rigorous RCTs investigating the synergistic potential of combining lifestyle modification (e.g., Mediterranean diet with exercise) with GLP-1 RAs or berberine.
- Personalized Medicine Approaches: Exploring biomarkers, including microbiome profiles and genetic polymorphisms, that predict individual responsiveness to different anti-inflammatory interventions.
- Pharmacokinetic Optimization: For natural compounds like berberine, developing novel delivery systems (e.g., nanoparticles, phytosomes) to overcome poor oral bioavailability is crucial for translating preclinical efficacy to clinical success [141].
In conclusion, the choice between lifestyle and pharmacological interventions is not necessarily binary. An evolved understanding of their distinct and complementary mechanisms will pave the way for integrated, personalized treatment paradigms to effectively quell the chronic inflammation that fuels metabolic syndrome.
Evaluating the Therapeutic Potential of Natural Compounds (e.g., TCM Polyphenols) vs. Synthetic Drugs
The global burden of metabolic syndrome (MetS) and its associated complications underscores the critical need for effective therapeutic strategies. This whitepaper provides a comprehensive evaluation of natural compounds, specifically Traditional Chinese Medicine (TCM) polyphenols, against synthetic drugs for managing MetS, with a focused examination of their mechanisms in modulating low-grade chronic inflammation. We present a detailed analysis of efficacy, mechanisms of action, safety profiles, and research methodologies to inform drug discovery professionals and scientists. By integrating quantitative data comparisons with visual mechanistic pathways and experimental protocols, this review aims to bridge traditional knowledge and modern scientific validation for developing next-generation MetS therapeutics.
Metabolic syndrome (MetS) represents a cluster of metabolic abnormalities—including central obesity, dyslipidemia, hypertension, and insulin resistance—that significantly increase the risk of cardiovascular disease (CVD) and type 2 diabetes [2]. The global prevalence of MetS is approximately 25%, creating a substantial economic burden on healthcare systems worldwide [2]. Central to MetS pathophysiology is chronic low-grade inflammation, now recognized as a key driver connecting its various components [5] [2].
The inflammatory basis of MetS manifests through multiple mechanisms. Obesity, particularly visceral adiposity, triggers adipocyte hyperplasia and hypertrophy, leading to secretion of pro-inflammatory cytokines including interleukin-6 (IL-6), tumor necrosis factor α (TNF-α), and interleukin-1β (IL-1β) [5] [2]. These inflammatory mediators disrupt insulin signaling in peripheral tissues through autocrine and paracrine pathways, promoting metabolic disorders and insulin resistance [5]. This chronic inflammatory state can be quantitatively assessed through the low-grade inflammation score (INFLA-score), a composite index based on C-reactive protein (CRP), white blood cell count (WBC), platelet count, and neutrophil-to-lymphocyte ratio (NLR) that provides a more comprehensive assessment of inflammatory status than individual biomarkers [5]. Recent research demonstrates that elevated INFLA-score strongly correlates with MetS prevalence, with those in the highest INFLA quartile having a 3.58 times higher risk of developing MetS compared to the lowest quartile [5].
Natural Compounds versus Synthetic Drugs: Comparative Analysis
The following tables provide a systematic comparison between natural compounds and synthetic drugs across multiple dimensions relevant to MetS treatment and drug development.
Table 1: Mechanism of Action and Therapeutic Applications
| Aspect | Natural Compounds (TCM Polyphenols) | Synthetic Drugs |
|---|---|---|
| Primary Mechanisms | Multi-target effects: Antioxidant, cytokine suppression, NLRP3 inhibition, metabolism modulation [144] [145] [146] | Single-target precision: Receptor agonism, enzyme inhibition [147] |
| Therapeutic Advantages | Lower toxicity profiles, dual advantage of intrinsic antimicrobial and immunomodulatory effects [144] [145] | Consistent chemical composition, predictable pharmacokinetics, standardized dosing [144] [147] |
| Key Applications in MetS | • Icariin: Promotes osteogenic differentiation [146]• Geraniol: Multifunctional antifungal with antibiofilm effects [144]• Echinacea: Reduces respiratory infection likelihood [144] | • Semaglutide: GLP-1 analog for glycemic control and weight loss [147]• Antihypertensives: Target blood pressure regulation• Statins: Cholesterol management |
| Representative Agents | Flavonoids (Icariin), phenolic acids, lignans, stilbenes [146] | Semaglutide, liraglutide, exenatide [147] |
Table 2: Research and Development Considerations
| Consideration | Natural Compounds | Synthetic Drugs |
|---|---|---|
| Chemical Complexity | Highly diverse structures; ~8000 polyphenolic structures identified [145] | Defined, reproducible structures |
| Standardization Challenges | Efficacy varies based on source, preparation, and dosage [144] | Consistent manufacturing processes |
| Bioavailability Issues | Dependent on food matrix, processing, and digestive enzymes [145] | Optimized through formulation technologies |
| Research Advancements | High-throughput screening, genomic analysis, computational screening [144] | Structure-based drug design, nanoparticle encapsulation |
| Development Timeline | Lengthy due to complexity of identification and standardization | Streamlined through synthetic protocols |
Table 3: Quantitative Comparison of Anti-inflammatory Efficacy
| Parameter | Natural Compounds | Synthetic Drugs | Research Evidence |
|---|---|---|---|
| Cytokine Reduction | Icariin blocks NF-κ B activation, inhibiting osteoclast formation [146] | Semaglutide reduces TNF-α, IL-6, IL-1β [147] | In vitro and animal studies for both classes |
| Oxidative Stress Modulation | Scavenges free radicals, chelates transition metals [145] | Indirect effects through metabolic improvement | Demonstrated in rat models [145] |
| Clinical Efficacy Metrics | Fuzheng Jiedu granules reduce COVID-19 progression in high-risk patients [144] | Semaglutide improves glycemic control (HbA1c reduction ~1.5-2.0%) [147] | Human clinical trials |
| Dosing Considerations | Variable bioavailability (e.g., Icariin effects at µM concentrations) [146] | Fixed dosing regimens (e.g., semaglutide 0.5-1.0 mg weekly) [147] | Established through pharmacokinetic studies |
Mechanistic Pathways in Inflammation Regulation
Natural Compounds: Multi-Targeted Approach
Natural polyphenols from TCM exert their therapeutic effects through simultaneous modulation of multiple inflammatory pathways, as illustrated in the following mechanistic diagram:
Diagram 1: Polyphenol anti-inflammatory mechanisms. Natural polyphenols target multiple inflammatory pathways including NF-κB signaling, RANK/RANKL system, and antioxidant defense.
Key mechanisms include:
- NF-κB Pathway Modulation: Polyphenols like icariin inhibit NF-κB activation, reducing downstream pro-inflammatory cytokines including TNF-α and IL-6 [146]. This pathway is crucial in connecting inflammation with insulin resistance in MetS.
- RANK/RANKL System Regulation: Certain flavonoids suppress receptor activator of nuclear factor kappa-B ligand (RANKL)-induced osteoclastogenesis, preserving bone density during inflammatory states [146].
- Antioxidant Defense Enhancement: Through free radical scavenging and metal chelation, polyphenols reduce oxidative stress that amplifies inflammatory cascades in MetS [145].
Synthetic Drugs: Targeted Pathway Engagement
Synthetic GLP-1 receptor agonists like semaglutide employ more specific molecular targeting:
Diagram 2: Semaglutide anti-inflammatory actions. The synthetic GLP-1 receptor agonist semaglutide modulates inflammation through metabolic improvement and direct immune regulation.
Primary mechanisms include:
- Direct Cytokine Suppression: Semaglutide reduces levels of TNF-α, IL-6, IL-1β, and MCP-1, breaking the cycle of inflammation and insulin resistance [147].
- Immune Cell Polarization: It promotes a shift in macrophage polarization from pro-inflammatory M1 to anti-inflammatory M2 phenotypes [147].
- NF-κB Pathway Inhibition: Like natural compounds, semaglutide also suppresses NF-κB signaling, though through distinct receptor-mediated mechanisms [147].
Experimental Protocols for Efficacy Evaluation
INFLA-Score Assessment in Metabolic Syndrome
The INFLA-score provides a quantitative measure of low-grade inflammation relevant for both natural product and synthetic drug evaluation [5]:
Protocol Objectives: To calculate INFLA-score and evaluate its association with MetS components in research populations.
Methodology Details:
- Biomarker Measurement:
- Collect fasting blood samples after a 9-hour fast
- Measure CRP, WBC, platelet count, and NLR using standardized automated analyzers
- For NLR, calculate from differential white blood cell count
INFLA-Score Calculation:
- Divide each biomarker into deciles based on population distribution
- Assign values from -4 (lowest decile) to +4 (highest decile) for each biomarker
- Sum values across all four biomarkers for total INFLA-score (range: -16 to +16)
- Higher scores indicate greater inflammatory burden
Statistical Analysis:
- Employ multivariable logistic regression models adjusting for confounders (age, sex, smoking status)
- Use restricted cubic splines to evaluate dose-response relationships
- Conduct subgroup analyses with interaction tests
Applications in Drug Development: This protocol enables quantification of anti-inflammatory effects of both natural compounds and synthetic drugs, providing a standardized metric for comparing intervention efficacy.
Osteoblast Differentiation Assay for Bone-Related Inflammation
This protocol evaluates the effects of natural compounds on bone formation, particularly relevant given the connection between MetS, inflammation, and bone health [146]:
Protocol Objectives: To assess the osteogenic potential of TCM polyphenols using in vitro models.
Methodology Details:
- Cell Culture:
- Utilize bone marrow stromal cells (BMSCs) or mesenchymal stem cells (MSCs)
- Maintain in α-MEM medium supplemented with 10% fetal bovine serum
- Culture at 37°C in 5% CO₂ humidified atmosphere
Osteogenic Differentiation:
- Seed cells at 10,000 cells/cm² in differentiation plates
- Treat with test compounds (e.g., icariin at 1-10 μM) in osteogenic medium
- Include positive controls (BMP-2) and vehicle controls
- Refresh medium every 3 days for 21-day differentiation period
Outcome Measurements:
- Alkaline Phosphatase (ALP) Activity: Measure at day 7-10 using pNPP substrate
- Mineralization Assessment: Visualize at day 21-28 using Alizarin Red S staining
- Gene Expression Analysis: Quantify osteogenic markers (Runx2, Osterix, Osteocalcin) via RT-qPCR
- Protein Expression: Evaluate signaling pathway activation (BMP/Smad, Wnt/β-catenin) via western blot
Mechanistic Studies:
- Employ pathway-specific inhibitors to confirm mechanism of action
- Utilize siRNA knockdown for critical transcription factors
- Conduct epigenetic analyses where appropriate (e.g., promoter methylation status)
Research Significance: This protocol enables evaluation of natural compounds' multi-target effects on bone formation pathways relevant to the inflammatory components of MetS.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 4: Key Research Reagents for Investigating Inflammation in Metabolic Syndrome
| Reagent Category | Specific Examples | Research Applications | Technical Notes |
|---|---|---|---|
| Inflammation Biomarkers | CRP, WBC, platelet count, NLR [5] | INFLA-score calculation; systemic inflammation assessment | Automated hematology analyzers (e.g., Coulter DxH 800) [5] |
| Cell Culture Models | Bone marrow stromal cells (BMSCs), mesenchymal stem cells (MSCs) [146] | Osteogenic differentiation assays; compound screening | Use early passages (P3-P8) for consistent results [146] |
| Cytokine Detection Kits | TNF-α, IL-6, IL-1β ELISA kits [147] | Quantifying inflammatory mediators in conditioned media | Validate with appropriate standards and controls |
| Natural Compound Libraries | Flavonoids (icariin), phenolic acids, stilbenes [146] | Screening for bioactivity; structure-activity relationship studies | Consider solubility issues; use DMSO stocks with final concentration <0.1% |
| Pathway Reporters | NF-κB luciferase constructs, BMP/Smad responsive elements [146] | Mechanism of action studies; pathway activation quantification | Normalize to constitutive promoters (e.g., CMV, SV40) |
| Animal Models | High-fat diet induced MetS models, genetic obesity models | In vivo efficacy and toxicity evaluation | Monitor INFLA-score equivalent biomarkers [5] |
The therapeutic management of metabolic syndrome requires addressing its fundamental inflammatory components. Both natural compounds and synthetic drugs offer distinct advantages: natural TCM polyphenols provide multi-targeted effects with lower toxicity profiles, while synthetic drugs offer precise targeting and standardized dosing. The future of MetS treatment likely lies in integrated approaches that combine the strengths of both paradigms.
Emerging research directions include:
- Hybrid Molecules: Developing synthetic compounds inspired by natural product scaffolds
- Personalized Medicine Approaches: Utilizing inflammation biomarkers like INFLA-score to identify responders
- Advanced Delivery Systems: Nanoparticle encapsulation to improve bioavailability of natural compounds
- Synergistic Combinations: Rational pairing of natural compounds with synthetic drugs to enhance efficacy while reducing side effects
As drug discovery continues to evolve, the integration of traditional knowledge with modern scientific validation will be crucial for developing effective, safe, and sustainable therapies for metabolic syndrome and its inflammatory complications.
Analyzing Clinical Trial Data for IL-1 Inhibition and Colchicine in T2DM and CVD Risk Reduction
Metabolic syndrome (MetS) is a complex condition characterized by central obesity, dyslipidemia, hypertension, and insulin resistance, with chronic low-grade inflammation recognized as a key pathophysiological driver [2]. This inflammatory state is characterized by elevated levels of acute-phase proteins, pro-inflammatory cytokines, chemokines, and adipokines, which occur even before the onset of overt type 2 diabetes mellitus (T2DM) [148]. The interconnection between MetS, T2DM, and cardiovascular disease (CVD) forms a dangerous triad wherein inflammation serves as a common biological pathway [2]. Among the key inflammatory mediators, interleukin-1β (IL-1β) has emerged as a critical cytokine that regulates chemokines and cytokines in patients with T2DM, with its release dependent on activation of the NLRP3 inflammasome [148]. This understanding has prompted investigation into anti-inflammatory therapies, particularly IL-1 inhibitors and colchicine, for reducing cardiovascular risk in patients with T2DM and metabolic syndrome.
Theoretical Foundations: Inflammatory Pathways in T2DM and Atherosclerosis
Key Inflammatory Mechanisms in T2DM
The development of T2DM involves a complex interplay between metabolic disturbances and inflammatory processes. White adipose tissue (WAT), particularly visceral WAT in the trunk and abdomen, serves as the primary source of inflammatory markers in T2DM [148]. Hypertrophied adipocytes due to excessive caloric intake lead to increased accumulation of immune cells and activation of genes encoding pro-inflammatory molecules. This process triggers multiple inflammatory pathways through:
- Increased NF-κB and JNK activity in hypertrophied adipocytes
- Altered unfolded protein response due to endoplasmic reticulum stress
- Hypoxic stress from vasculature insufficiency in enlarged adipocytes
- Activation of Toll-like receptors by excess free fatty acids
- Macrophage polarization from anti-inflammatory M2 to pro-inflammatory M1 phenotype [148]
These mechanisms collectively promote a pro-inflammatory state characterized by elevated levels of C-reactive protein (CRP), IL-1β, TNF-α, IL-6, and monocyte chemoattractant protein-1 (MCP-1) [148].
The NLRP3 Inflammasome and IL-1β in T2DM Pathogenesis
The NLRP3 inflammasome plays a central role in bridging metabolic dysfunction with inflammation in T2DM. Activation of this multiprotein complex leads to caspase-1 activation, which subsequently processes pro-IL-1β and pro-IL-18 into their active forms [148]. IL-1β then contributes to insulin resistance through multiple mechanisms:
- Impairment of insulin signaling in peripheral tissues
- Promotion of β-cell apoptosis in the pancreas
- Induction of chemokine production that recruits additional immune cells
- Synergistic action with other cytokines to amplify inflammatory responses
The central role of IL-1β in T2DM pathophysiology provides the rational basis for therapeutic targeting of this cytokine and its upstream regulators.
Diagram 1: Inflammatory pathway in T2DM pathogenesis.
Clinical Trial Data Analysis: IL-1 Inhibition and Colchicine in T2DM
Colchicine Cardiovascular Outcomes
Colchicine, an ancient anti-inflammatory medication, exhibits broad anti-inflammatory effects including inhibition of the NLRP3 inflammasome and polymerization of tubulin that affects leukocyte function [149]. Recent randomized controlled trials have investigated its potential for cardiovascular risk reduction in patients with established cardiovascular disease, with subanalyses focusing on diabetic populations.
Table 1: Colchicine Cardiovascular Outcome Trials in Diabetic Populations
| Trial | Population | Sample Size | Follow-up | Primary Endpoint Results | DM Subgroup Analysis |
|---|---|---|---|---|---|
| LoDoCo2 [149] | Chronic coronary artery disease | 5,522 total (1,007 with T2DM) | Median 28.6 months | HR 0.69 (95% CI 0.57-0.83) for overall population | HR 0.87 (95% CI 0.61-1.25) in T2DM vs HR 0.64 (95% CI 0.51-0.80) in non-DM (pinteraction=0.14) |
| COLCOT [148] | Recent myocardial infarction | 4,745 | Median 22.6 months | HR 0.77 (95% CI 0.61-0.96) | Greater effect in patients with diabetes |
| Korean Cohort Study [150] | T2DM and gout | 38,724 after PS matching | 2011-2022 | HR 0.94 (95% CI 0.65-1.36) for MACE | No significant reduction in MACE vs NSAIDs |
The LoDoCo2 trial demonstrated that participants with T2DM had a significantly higher risk for the primary composite endpoint (cardiovascular death, spontaneous myocardial infarction, ischemic stroke, or ischemia-driven revascularization) compared to those without diabetes (adjusted HR 1.52, 95% CI 1.15-2.01, p < 0.01) [149]. Despite this elevated baseline risk, the beneficial effects of colchicine appeared consistent regardless of diabetes status, though the point estimate suggested a potentially attenuated effect in the diabetic subgroup.
A recent real-world study from South Korea (2025) investigated colchicine versus NSAIDs in patients with T2DM and gout, finding no significant difference in major adverse cardiovascular events (MACE) between the treatments (HR 0.94, 95% CI 0.65-1.36) [150]. This null finding highlights the need for further research on colchicine for primary cardiovascular prevention in specific diabetic subpopulations.
IL-1 Inhibitor Clinical Evidence
IL-1 inhibition represents a more targeted anti-inflammatory approach for T2DM and associated cardiovascular risk. The Canakinumab Anti-Inflammatory Thrombosis Outcomes Study (CANTOS) provided proof-of-concept for the inflammation hypothesis of atherosclerosis, though with mixed results in diabetic populations.
Table 2: IL-1 Targeted Therapies in T2DM and CVD
| Therapy | Mechanism | Trial/Study | Population | Glycemic Outcomes | Cardiovascular Outcomes |
|---|---|---|---|---|---|
| Canakinumab [148] [149] | Monoclonal antibody against IL-1β | CANTOS | 10,061 patients with prior MI and hsCRP ≥2mg/L | No improvement in glycemic control or reduction in new-onset T2DM | Significant reduction in cardiovascular events independent of lipid lowering |
| Colchicine [148] [149] | NLRP3 inflammasome inhibition, microtubule disruption | LoDoCo2 | Chronic CAD with and without T2DM | New-onset T2DM: 1.5% (colchicine) vs 2.2% (placebo), p=0.10 | Consistent risk reduction regardless of DM status |
| Other IL-1 Inhibitors [148] | IL-1 receptor antagonism | Small mechanistic studies | T2DM patients | Improved beta-cell function and glycemic control | Insufficient data |
While small studies suggested that IL-1 targeted therapy could improve glycemic control in T2DM, the larger CANTOS substudy did not demonstrate better glycemic control or reduction in new-onset T2DM with canakinumab treatment [148] [149]. This dissociation between inflammatory pathway inhibition and metabolic improvement highlights the complexity of these interconnected biological systems.
Methodological Approaches for Investigating IL-1 Pathways in T2DM
Assessing Low-Grade Inflammation in Metabolic Syndrome
The low-grade inflammation score (INFLA-score) has emerged as a valuable composite metric for quantifying systemic inflammatory burden in metabolic syndrome research. This score incorporates four hematological parameters:
- C-reactive protein (CRP) - Acute phase inflammatory marker
- White blood cell count (WBC) - General inflammatory activity
- Platelet count - Involvement in inflammatory processes
- Neutrophil-to-lymphocyte ratio (NLR) - Systemic inflammatory response
The INFLA-score is calculated by assigning values from -4 to +4 based on decile rankings of each component, with the total score ranging from -16 to +16 [5]. Higher scores indicate greater inflammatory status. Recent research demonstrated that each unit increase in INFLA-score was associated with an 8% higher likelihood of having metabolic syndrome (OR=1.08, 95% CI: 1.07-1.10), with those in the highest quartile having a 3.58 times higher risk than those in the lowest quartile [5].
Diagram 2: INFLA-score assessment workflow.
Experimental Protocols for NLRP3 Inflammasome Activation Studies
Research into IL-1 inhibition requires standardized methodologies for assessing NLRP3 inflammasome activation and its inhibition. Key experimental approaches include:
In vitro Macrophage Activation Model:
- Cell culture: THP-1 monocytic cell line differentiated into macrophages using PMA (phorbol 12-myristate 13-acetate)
- Priming signal: Incubation with LPS (lipopolysaccharide) for 3-4 hours to upregulate NLRP3 and pro-IL-1β expression
- Activation signal: Exposure to NLRP3 activators (ATP, nigericin, crystalline particulates) for 30-60 minutes
- IL-1β measurement: Quantification of mature IL-1β in supernatant by ELISA
- Inhibitor testing: Pre-treatment with colchicine or IL-1 inhibitors during priming/activation phases
Ex vivo Monocyte Assay from Patient Blood:
- PBMC isolation: Density gradient centrifugation to isolate peripheral blood mononuclear cells
- Stimulation: Direct stimulation with NLRP3 activators in the presence/absence of inhibitors
- Cytokine profiling: Multiplex cytokine analysis of IL-1β, IL-18, IL-6, TNF-α
- Gene expression: qRT-PCR analysis of NLRP3, CASP1, IL1B mRNA levels
These methodologies allow for the evaluation of compound effects on specific steps of the inflammasome activation pathway and their potential therapeutic application in T2DM.
Research Reagent Solutions for IL-1 Pathway Investigation
Table 3: Essential Research Reagents for IL-1 and NLRP3 Studies
| Reagent/Category | Specific Examples | Research Application | Technical Notes |
|---|---|---|---|
| Cell Lines | THP-1 (human monocytic), J774A.1 (mouse macrophage), Primary human macrophages | In vitro modeling of inflammasome activation | THP-1 requires PMA differentiation for macrophage phenotype |
| NLRP3 Activators | ATP, Nigericin, Monosodium urate crystals, Silica particles, Imiquimod | Inducing inflammasome assembly and IL-1β secretion | Concentration and timing critical for specific activation |
| Cytokine Detection | ELISA kits (IL-1β, IL-18), Luminex multiplex arrays, Western blot (caspase-1) | Quantifying inflammatory responses | Pro- vs mature IL-1β distinction important for activity assessment |
| IL-1 Inhibitors | Anakinra (IL-1Ra), Canakinumab (anti-IL-1β), Gevokizumab (anti-IL-1β) | Positive controls for inhibition studies | Different mechanisms: receptor blockade vs cytokine neutralization |
| Colchicine Formulations | Pharmaceutical grade colchicine, fluorescent conjugates | Microtubule disruption and inflammasome inhibition studies | Dose-response critical (nM to μM range) |
| Gene Expression Analysis | qPCR primers (NLRP3, CASP1, IL1B, PYCARD), RNA isolation kits | Transcriptional regulation assessment | LPS priming typically increases NLRP3 and IL1B expression |
The investigation of IL-1 inhibition and colchicine for cardiovascular risk reduction in T2DM represents a promising frontier in cardiometabolic medicine. Current evidence suggests that while colchicine provides consistent cardiovascular benefits in patients with established coronary disease regardless of diabetes status, its effects may be attenuated in diabetic populations [149]. The potential for colchicine to reduce new-onset diabetes, though not statistically significant in the LoDoCo2 trial (1.5% vs 2.2% in placebo, p=0.10), warrants further investigation in dedicated prevention trials [149].
Future research should focus on identifying specific inflammatory endotypes within the broad T2DM population that may derive particular benefit from anti-inflammatory therapies. Additionally, the development of more targeted NLRP3 inhibitors with improved safety profiles may unlock the full potential of this therapeutic approach without the gastrointestinal side effects associated with colchicine. As our understanding of the intricate connections between metabolic disturbances and chronic inflammation deepens, anti-inflammatory strategies are poised to become important adjuncts to standard care for reducing cardiovascular risk in patients with type 2 diabetes and metabolic syndrome.
Assessing the Additive Benefit of Anti-Inflammatory Agents on Top of Standard MetS Care
Metabolic syndrome (MetS) represents a cluster of conditions—including central obesity, dyslipidemia, hypertension, and insulin resistance—that collectively increase the risk of cardiovascular disease (CVD) and type 2 diabetes mellitus (T2DM) [2] [151]. The global prevalence of MetS is approximately 25%, making it a significant public health challenge with substantial economic implications for healthcare systems worldwide [2]. While standard care focuses on managing individual components through lifestyle modifications and pharmacotherapy targeting blood pressure, lipids, and glucose, a growing body of evidence suggests that chronic low-grade inflammation serves as a key pathophysiological driver underlying MetS [152] [5] [2]. This inflammatory state, characterized by elevated pro-inflammatory cytokines and acute-phase reactants, not only contributes to insulin resistance but also promotes endothelial dysfunction and atherosclerosis [2] [151] [29]. This whitepaper examines the scientific rationale and clinical evidence for targeting inflammation as an additive strategy to standard MetS care, with particular focus on mechanisms, therapeutic agents, and experimental approaches relevant to researchers and drug development professionals.
The Inflammatory Basis of Metabolic Syndrome
Chronic low-grade inflammation is now recognized as a fundamental mechanism linking obesity to metabolic dysfunction. In expanded adipose tissue, particularly visceral fat, hypertrophied adipocytes and infiltrating immune cells—primarily macrophages—secrete an array of pro-inflammatory cytokines and chemokines, including tumor necrosis factor-alpha (TNF-α), interleukin-6 (IL-6), and interleukin-1 beta (IL-1β) [5] [151] [29]. These mediators disrupt insulin signaling in peripheral tissues through autocrine and paracrine pathways, leading to systemic insulin resistance [5]. Specifically, TNF-α phosphorylates serine residues on insulin receptor substrate (IRS) proteins, rendering them unable to activate downstream phosphatidylinositol 3-kinase (PI3K) and protein kinase B (Akt) pathways essential for glucose transporter type 4 (GLUT-4) translocation and glucose uptake [151]. IL-6 contributes to hepatic acute-phase protein production, including C-reactive protein (CRP), while IL-1β impairs pancreatic β-cell function and insulin secretion [152] [151].
The INFLA-score, a composite inflammatory index based on CRP, white blood cell count, platelet count, and neutrophil-to-lymphocyte ratio (NLR), provides a comprehensive assessment of low-grade inflammation and has demonstrated strong associations with MetS and its components [5]. In a cross-sectional study of 1,758 oilfield shift workers, participants in the highest INFLA-score quartile had a 3.58-fold increased risk of MetS compared to those in the lowest quartile (OR = 3.58, Q4 v Q1) after adjusting for confounders [5]. The INFLA-score showed positive associations with elevated blood glucose, blood pressure, waist circumference, triglyceride levels, and reduced high-density lipoprotein (HDL) cholesterol (p < 0.001), with a notable dose-response relationship [5]. This inflammatory scoring system offers researchers a valuable tool for quantifying inflammatory burden and assessing intervention efficacy in MetS studies.
Figure 1: Inflammatory Pathways in Metabolic Syndrome Pathogenesis. This diagram illustrates the central role of chronic inflammation in driving insulin resistance and metabolic dysfunction, highlighting key molecular mediators and their effects on insulin signaling.
Current Anti-Inflammatory Therapeutic Strategies
Targeted Pharmacological Approaches
Several targeted anti-inflammatory strategies have been investigated in clinical trials for MetS and related conditions, with varying mechanisms and levels of evidence supporting their efficacy (Table 1).
Table 1: Anti-Inflammatory Agents Investigated for Metabolic Syndrome
| Therapeutic Target | Agent(s) | Mechanism of Action | Metabolic Effects | Clinical Trial Evidence |
|---|---|---|---|---|
| IKK-β/NF-κB pathway | Salsalate | Inhibits IKK-β, reducing NF-κB activation and inflammatory gene expression | Improved insulin sensitivity, β-cell function, and glucose control | Modest improvements in glycemic parameters [152] |
| TNF-α | Etanercept, Infliximab, Adalimumab | Neutralizes TNF-α, a key inflammatory cytokine | Improved insulin sensitivity in patients with inflammatory rheumatoid diseases | Effects in MetS/T2DM remain relatively modest [152] |
| IL-1β | Anakinra, Canakinumab | Blocks IL-1β signaling, reducing inflammation | Improved insulin sensitivity, β-cell function, glycemic control | Canakinumab associated with reduced cardiovascular events in CANTOS trial [152] |
| IL-6 | Tocilizumab | Inhibits IL-6 receptor signaling | Improved insulin sensitivity in inflammatory conditions | Potential for worsening lipid profiles noted [152] |
| CCR2 | CCR2 antagonists | Blocks monocyte recruitment to adipose tissue | Reduced adipose tissue inflammation, improved insulin sensitivity | Preclinical and early clinical studies show promise [152] |
The IL-1β axis has emerged as a particularly promising target, with canakinumab (a monoclonal antibody against IL-1β) demonstrating not only improved glycemic control but also significantly reduced cardiovascular event rates in the CANTOS trial, independent of lipid-lowering effects [152]. This provides compelling evidence that targeting inflammation can yield cardiovascular benefits beyond conventional risk factor management. However, most anti-inflammatory agents have shown relatively modest metabolic effects when used as monotherapy, suggesting that combination approaches or patient stratification based on inflammatory biomarkers may be necessary to optimize therapeutic outcomes [152].
Nutritional and Lifestyle Interventions
Beyond pharmacological agents, dietary patterns significantly influence inflammatory status in MetS. The Dietary Inflammatory Index (DII) quantifies the inflammatory potential of an individual's diet based on intake of 45 nutrients and food components that affect inflammatory biomarkers, including CRP, IL-1β, IL-6, and TNF-α [153]. In a cross-sectional study of 1,936 elderly adults in Northern China, participants with the most pro-inflammatory diets (highest DII quartile) had a 1.28-fold increased risk of MetS compared to those with the most anti-inflammatory diets (fully adjusted model) [153]. Pro-inflammatory diets were significantly associated with hyperglycemia, hypertriglyceridemia, hypertension, and abdominal obesity, with these associations being particularly pronounced in obese individuals (BMI ≥ 28 kg/m²) [153]. These findings suggest that adopting anti-inflammatory dietary patterns may represent a foundational strategy for reducing inflammatory burden in MetS, potentially enhancing the efficacy of subsequent pharmacological interventions.
Experimental Design and Methodological Considerations
Assessing Inflammatory Status in MetS Research
Accurate quantification of inflammatory status is essential for evaluating the additive benefit of anti-inflammatory interventions in MetS. The following methodologies provide comprehensive assessment:
INFLA-Score Calculation Protocol:
- Biomarker Measurement: Obtain fasting blood samples for:
- High-sensitivity CRP (immunoturbidimetric assay)
- Complete blood count with differential (automated hematology analyzer)
- Platelet count
- Calculate neutrophil-to-lymphocyte ratio (NLR)
- Decile Assignment: For each biomarker, assign values based on population deciles:
- Deciles 1-4: Assign values from -4 to -1
- Deciles 7-10: Assign values from +1 to +4
- Deciles 5-6: Assign value of 0
- Score Calculation: Sum values across all four biomarkers to generate INFLA-score (range: -16 to +16) [5]
Additional Methodological Considerations:
- Cytokine Profiling: Multiplex immunoassays for TNF-α, IL-6, IL-1β, IL-10, adiponectin, leptin
- Transcriptomic Analysis: RNA sequencing of peripheral blood mononuclear cells (PBMCs) for inflammatory pathway activation
- Adipose Tissue Biopsy: Immunohistochemistry for macrophage infiltration (CD68+ staining) and cytokine production
Preclinical Experimental Workflow
Figure 2: Preclinical Experimental Workflow for Evaluating Anti-Inflammatory Therapies in Metabolic Syndrome. This diagram outlines a comprehensive experimental approach for investigating the additive benefits of anti-inflammatory agents in relevant animal models of MetS.
Clinical Trial Design Considerations
For clinical validation, a randomized, double-blind, placebo-controlled trial design is recommended with the following key elements:
- Population: Adults meeting ATP III criteria for MetS with elevated inflammatory markers (e.g., INFLA-score ≥2 or hs-CRP ≥2 mg/L)
- Intervention: Standard MetS care (lifestyle counseling + metformin/statins/antihypertensives as needed) ± anti-inflammatory agent
- Primary Endpoints: Change in insulin sensitivity (hyperinsulinemic-euglycemic clamp), composite MetS severity score
- Secondary Endpoints: Inflammatory biomarkers (INFLA-score, cytokines), body composition, endothelial function, adipokine profile
- Duration: Minimum 6 months to assess sustained metabolic effects
The Scientist's Toolkit: Key Research Reagents and Platforms
Table 2: Essential Research Tools for Investigating Inflammation in Metabolic Syndrome
| Category | Specific Reagents/Assays | Research Application | Key Considerations |
|---|---|---|---|
| Inflammatory Biomarker Panels | Multiplex cytokine arrays (Luminex/MSD), hs-CRP ELISA, leukocyte differential count | Comprehensive inflammatory profiling | Standardize sample collection processing; account for diurnal variation |
| Metabolic Phenotyping | Hyperinsulinemic-euglycemic clamps, oral glucose tolerance tests, indirect calorimetry | Assessment of insulin sensitivity and energy metabolism | Consider using stable isotopes for precise flux measurements |
| Adipose Tissue Analysis | Stromal vascular fraction isolation, adipocyte culture systems, histology (H&E, CD68 IHC) | Evaluation of adipose tissue remodeling and inflammation | Preserve tissue rapidly for RNA/protein analysis; optimize digestion protocols |
| Molecular Pathway Analysis | Phospho-specific antibodies for insulin signaling (p-AKT, p-IRS), NF-κB pathway reporters, RNA-seq | Mechanistic studies of inflammatory signaling | Use pathway-focused PCR arrays for targeted gene expression analysis |
| Animal Models | High-fat diet-induced obesity, ob/ob, db/db mice; Zucker fatty rats | Preclinical efficacy and safety testing | Monitor metabolic parameters regularly; consider sex differences in response |
The integration of anti-inflammatory agents with standard MetS care represents a promising therapeutic strategy grounded in the fundamental role of chronic inflammation in metabolic disease pathogenesis. Current evidence suggests that targeting specific inflammatory pathways, particularly the IL-1β axis, can provide additive benefits for both metabolic parameters and cardiovascular outcomes. However, several research gaps remain, including the optimal patient selection criteria based on inflammatory phenotypes, the potential superiority of combination anti-inflammatory approaches, and the long-term safety profile of immunomodulatory therapies in MetS populations. Future research should focus on personalized anti-inflammatory strategies based on comprehensive inflammatory profiling (e.g., INFLA-score), development of novel therapeutic combinations that target multiple inflammatory pathways simultaneously, and exploration of nutritional interventions as adjuncts to pharmacological approaches. Furthermore, greater understanding of the interplay between inflammation and mitochondrial dysfunction—a key feature of obesity-related metabolic disorders—may reveal novel therapeutic targets for more effective MetS management [29]. As research in this field advances, targeting inflammation promises to move beyond symptomatic management toward addressing the root causes of metabolic dysfunction.
Validation of Novel Biomarkers as Predictive Tools for Treatment Response and Patient Outcomes
The integration of novel biomarkers into metabolic syndrome (MetS) research represents a paradigm shift in understanding the intricate relationship between low-grade chronic inflammation and metabolic dysregulation. This technical guide provides a comprehensive framework for the development, analytical validation, and clinical application of inflammatory biomarkers as predictive tools for treatment response and patient outcomes. By synthesizing current evidence and methodologies, we outline standardized protocols for biomarker qualification, emphasizing a fit-for-purpose approach tailored to the specific context of use in metabolic syndrome management. The whitepaper establishes that multimarker inflammatory scores, particularly the INFLA-score and Systemic Inflammation Response Index (SIRI), demonstrate superior predictive capability compared to single-marker approaches, with INFLA-score showing a dose-response relationship with MetS risk (OR = 1.08, 95% CI: 1.07–1.10 per unit increase) and the highest SIRI quartile associated with 1.61-fold increased odds (95% CI: 1.25–2.08) for advanced cardiometabolic disease stages. Furthermore, machine learning frameworks incorporating inflammatory markers achieve area under the curve values of 0.80-0.89 for MetS prediction, enabling robust risk stratification. This resource provides researchers and drug development professionals with actionable methodologies to advance biomarker validation from discovery to clinical implementation within the context of low-grade inflammation in metabolic syndrome.
Metabolic syndrome represents a cluster of interrelated metabolic abnormalities—including abdominal obesity, hypertension, dyslipidemia, and hyperglycemia—that collectively increase risk for cardiovascular disease, type 2 diabetes, and all-cause mortality. The global prevalence of MetS has reached approximately 25%, creating a substantial public health burden worldwide [5]. Central to MetS pathophysiology is chronic low-grade inflammation, characterized by persistent activation of innate immune pathways and elevated circulating inflammatory mediators. Adipose tissue dysfunction, particularly in visceral depots, drives this inflammatory state through hyperplasia, hypertrophy, and secretion of pro-inflammatory factors including interleukin-6 (IL-6), tumor necrosis factor-α (TNF-α), and interleukin-1β (IL-1β) [5] [154]. These inflammatory mediators disrupt insulin signaling in peripheral tissues through autocrine and paracrine pathways, establishing a mechanistic link between inflammation and metabolic dysfunction [5].
Biomarkers serve as objectively measurable indicators of biological processes, pathological states, or pharmacological responses to therapeutic interventions [155]. In the context of MetS, biomarkers transition from traditional univariate measures to multidimensional combinations that more comprehensively capture disease heterogeneity. The validation of novel biomarkers specifically addressing low-grade inflammation provides critical tools for early detection, risk stratification, and monitoring of therapeutic interventions in MetS [156] [154]. The escalating prevalence of metabolic disorders necessitates refined approaches to patient stratification and treatment personalization, positioning inflammatory biomarkers as essential components of precision medicine frameworks in cardiometabolic disease [157].
Biomarker Categories and Context of Use Framework
Regulatory Definitions and Classification
The U.S. FDA-NIH Biomarkers, EndpointS, and other Tools (BEST) resource establishes standardized terminology for biomarker categorization, which is fundamental to their appropriate application in drug development and clinical research [155]. Understanding these categories ensures proper validation and implementation strategies aligned with the biomarker's intended purpose.
Table 1: Biomarker Categories Based on FDA-NIH BEST Resource
| Category | Primary Use | Example in Metabolic Syndrome |
|---|---|---|
| Susceptibility/Risk | Identify individuals with increased disease risk | Genetic markers for insulin resistance |
| Diagnostic | Detect or confirm disease presence | HbA1c for diabetes diagnosis |
| Monitoring | Assess disease status or response to treatment | Serial CRP measurements during anti-inflammatory therapy |
| Prognostic | Identify likelihood of disease recurrence or progression | INFLA-score for MetS complication risk |
| Predictive | Identify individuals more likely to respond to specific treatment | Inflammatory markers for response to IL-6 antagonists |
| Pharmacodynamic/Response | Show biological response to therapeutic intervention | Changes in adiponectin following TZD administration |
| Safety | Monitor potential adverse effects of treatment | Serum creatinine for renal function during medication |
The same biomarker may fulfill multiple categories depending on context. For instance, hemoglobin A1c serves as both a diagnostic biomarker for diabetes and a monitoring biomarker for glycemic control [155]. This multifunctionality necessitates careful consideration of the specific context of use (COU) during validation.
Context of Use in Metabolic Syndrome Research
The COU defines the specific application of a biomarker within drug development or clinical practice. For metabolic syndrome with underlying low-grade inflammation, distinct COUs include:
- Early Risk Stratification: Identifying individuals with subclinical inflammation who are at elevated risk for developing full MetS, enabling preemptive interventions [156].
- Treatment Selection: Using inflammatory profiles to match patients with specific pathophysiological subtypes to targeted therapies, such as anti-inflammatory interventions [154].
- Dose Optimization: Employing pharmacodynamic biomarkers to establish optimal dosing for medications targeting inflammatory pathways in MetS [155].
- Safety Monitoring: Detecting inflammatory exacerbations or off-target effects during therapeutic interventions for MetS [155].
The validation requirements vary substantially based on the COU. For example, a biomarker intended for early risk stratification requires extensive epidemiological validation across diverse populations, while a pharmacodynamic biomarker primarily necessitates establishing a direct relationship between drug exposure and biomarker changes [155].
Promising Inflammatory Biomarkers in Metabolic Syndrome
Composite Inflammatory Scores
Single-marker approaches have limitations in capturing the complexity of low-grade inflammation in MetS. Composite scores integrating multiple inflammatory parameters demonstrate enhanced predictive capability:
INFLA-Score: This composite index combines four hematological parameters: C-reactive protein (CRP), white blood cell count (WBC), platelet count, and neutrophil-to-lymphocyte ratio (NLR). The score is calculated by assigning values from -4 to +4 based on decile rankings of each component, with the total score ranging from -16 to +16. Higher scores indicate greater inflammatory burden [5].
In a study of 1,758 oilfield shift workers, each unit increase in INFLA-score was associated with 8% higher odds of MetS (OR = 1.08, 95% CI: 1.07–1.10). Those in the highest INFLA-score quartile had 3.58 times greater MetS risk compared to the lowest quartile [5]. The INFLA-score demonstrated positive associations with all MetS components—elevated blood glucose, blood pressure, waist circumference, triglycerides, and reduced HDL—with statistically significant dose-response relationships (p<0.001) [5].
Systemic Inflammation Response Index (SIRI): This index integrates neutrophil, monocyte, and lymphocyte counts using the formula: (monocyte count × neutrophil count)/lymphocyte count. SIRI has demonstrated superior discriminative ability for advanced cardiometabolic stages compared to established inflammatory indices like NLR or platelet-to-lymphocyte ratio [158].
In an NHANES analysis of 10,405 adults with cardiovascular-kidney-metabolic (CKM) syndrome, individuals in the highest SIRI quartile had 1.61-fold increased odds (95% CI: 1.25–2.08) of advanced CKM stages (3 or 4) compared to the lowest quartile, with each unit increase in SIRI associated with 14% higher risk [158].
Emerging Circulating and Imaging Biomarkers
Beyond composite scores, several specific inflammatory markers show promise in MetS research:
Growth Differentiation Factor 15 (GDF-15): A member of the transforming growth factor-β superfamily, GDF-15 is upregulated under cellular stress conditions. In a study of 2,083 participants, GDF-15 levels were significantly higher in males (580.6 vs. 519.3 ng/L, p<0.001) and positively correlated with BMI, waist circumference, blood pressure, insulin, and triglycerides, while inversely correlating with HDL cholesterol [154].
MicroRNAs: Circulating microRNAs, particularly miR-484, show potential as biomarkers linking environmental exposures (e.g., diet) with metabolic regulation. Research from the Di@bet.es cohort demonstrates associations between serum miR-484, fruit intake frequency, and type 2 diabetes risk [154].
Liver Function Tests and hs-CRP: Integration of liver enzymes (ALT, AST) with high-sensitivity CRP improves MetS prediction accuracy. Machine learning models incorporating these biomarkers achieve specificity rates of 77-83% in identifying MetS [157].
Table 2: Performance Characteristics of Inflammatory Biomarkers in Metabolic Syndrome
| Biomarker | Population | Predictive Performance | Key Associations |
|---|---|---|---|
| INFLA-Score | 1,758 shift workers | OR 1.08 (95% CI: 1.07-1.10) per unit increase for MetS; Q4 vs Q1: OR 3.58 | All MetS components (WC, BP, TG, HDL, FPG) |
| SIRI | 10,405 NHANES participants | OR 1.61 (95% CI: 1.25-2.08) for advanced CKM syndrome; 14% risk increase per unit | Superior to NLR, PLR for advanced stages |
| hs-CRP + Liver Enzymes | 8,972 MASHAD participants | Specificity 77-83%; Error rate 27% in gradient boosting model | ALT, direct bilirubin, sex as key predictors |
| GDF-15 | 2,083 KDEP participants | Significant associations with obesity (p<0.001) and diabetic traits | Male gender, older age, Arab ethnicity |
Validation Methodologies and Experimental Protocols
Analytical Validation Procedures
Analytical validation establishes that biomarker measurement assays perform reliably according to their specified requirements. Key components include:
Precision and Accuracy Assessment: For inflammatory biomarkers like CRP, precision is evaluated through intra-assay and inter-assay coefficients of variation (CV). Acceptable precision typically requires CV <15% for biomarker measurements in validation studies [155]. Accuracy is determined through recovery experiments using spiked samples with known analyte concentrations.
Linearity and Reportable Range: Establishing the range of analyte concentrations over which the assay provides linearly proportional results. For NLR and other cellular ratios, this involves verifying linearity across clinically relevant ranges for each cell type [158].
Reference Interval Establishment: Determining normal ranges for novel inflammatory biomarkers in healthy control populations, with stratification by age, sex, and ethnicity when appropriate. For example, GDF-15 reference intervals differ significantly by age (563.4 ng/L for <50 years vs. 781.4 ng/L for >50 years) and sex [154].
Sample Handling Protocols: Standardizing pre-analytical variables including fasting requirements, sample processing timelines, and storage conditions. For cytokine measurements, samples typically require processing within 2 hours of collection with storage at -80°C [159].
Clinical Validation Study Designs
Clinical validation demonstrates that a biomarker accurately identifies or predicts clinical outcomes of interest. Recommended study designs include:
Cross-Sectional Studies: Initial validation establishing associations between biomarker levels and concurrent disease status. For example, the association between INFLA-score and MetS prevalence was initially established in a cross-sectional study of 1,758 shift workers [5].
Longitudinal Cohort Studies: Assessing biomarker performance for predicting future outcomes. The RaNCD cohort study followed 9,602 adults aged 35-65 years to validate predictive models for MetS development [160].
Randomized Controlled Trials (RCTs): Evaluating biomarkers as monitoring or response tools in therapeutic interventions. A meta-analysis of 8 RCTs (n=444) demonstrated that magnesium supplementation significantly reduced CRP levels (SMD = -0.327; 95% CI: -0.602 to -0.053; p=0.048) in MetS patients [159].
Method Comparison Studies: Establishing concordance between different measurement platforms. For body composition assessments, dual-energy X-ray absorptiometry (DEXA) serves as the gold standard against which bioelectrical impedance analysis (BIA) is validated for obesity-related inflammation markers [161].
Statistical Analysis Frameworks
Robust statistical methodologies are essential for biomarker validation:
Discriminatory Performance Assessment: Receiver operating characteristic (ROC) analysis determines area under the curve (AUC) values with 95% confidence intervals. SIRI demonstrated superior discriminative ability for advanced CKM syndrome compared to other inflammatory indices [158].
Multivariable Regression Modeling: Logistic regression models adjusted for confounders (age, sex, smoking status) quantify independent associations between biomarkers and outcomes. INFLA-score associations with MetS components remained significant after full adjustment (p<0.001) [5].
Machine Learning Approaches: Advanced algorithms like gradient boosting and convolutional neural networks validate biomarker predictive utility. These models achieve AUC values of 0.80-0.89 for MetS prediction using inflammatory and metabolic markers [157] [161].
Mediation Analysis: Partitioning direct and indirect effects of biomarkers on outcomes. For SIRI and CKM syndrome, hs-CRP accounted for only 4.94% of the association, indicating SIRI captures distinct inflammatory pathways [158].
The following diagram illustrates the comprehensive biomarker validation workflow from discovery to clinical implementation:
Biomarker Validation Workflow
Technological Advances in Biomarker Research
Multi-Omics Integration
The integration of genomics, transcriptomics, proteomics, and metabolomics data provides comprehensive molecular profiling for biomarker discovery. In metabolic-associated fatty liver disease (MAFLD), integrated multi-omics analysis identified five glycolysis-related key genes (ALDH3A1, CDK1, DEPDC1, HKDC1, and SOX9) driving disease progression and interacting with immune infiltration patterns [154]. Spatial transcriptomics further revealed colocalization of CDK1, SOX9, and HKDC1 with the monocyte-derived macrophage marker CCR2, illuminating the hepatocyte–fibroblast–macrophage axis as the predominant glycolysis-active niche in inflammatory metabolic disease [154].
Artificial Intelligence and Machine Learning
AI and machine learning revolutionize biomarker analysis through:
Predictive Analytics: Sophisticated models forecast disease progression and treatment responses based on biomarker profiles. Gradient boosting and convolutional neural networks achieve specificity rates of 77-83% for MetS prediction using liver function tests and hs-CRP [157].
Automated Data Interpretation: Machine learning algorithms facilitate automated analysis of complex datasets, significantly reducing time required for biomarker discovery and validation. The Boruta algorithm effectively identifies the most important anthropometric, biochemical, and nutritional predictors of MetS from high-dimensional data [160].
Personalized Treatment Planning: AI analysis of individual patient data alongside biomarker information supports tailored treatment strategies. SHAP (SHapley Additive exPlanations) analysis identifies hs-CRP, direct bilirubin, ALT, and sex as the most influential predictors in MetS models, enabling personalized risk assessment [157].
Single-Cell and Spatial Analysis Technologies
Single-cell analysis technologies enable unprecedented resolution in characterizing cellular heterogeneity within metabolic tissues. These approaches:
- Reveal insights into tumor microenvironments and their parallels in metabolic disease
- Identify rare cell populations that may drive disease progression or therapy resistance
- When integrated with multi-omics data, provide comprehensive views of cellular mechanisms
Spatial transcriptomics has proven particularly valuable in metabolic liver disease, demonstrating colocalization of metabolic genes with inflammatory cell markers [154].
Pathophysiological Framework: Inflammation in Metabolic Syndrome
Chronic low-grade inflammation in metabolic syndrome originates primarily from adipose tissue dysfunction. Hypertrophic adipocytes secrete pro-inflammatory cytokines including TNF-α, IL-6, and IL-1β, which disrupt insulin signaling through autocrine and paracrine pathways [5]. This inflammatory milieu promotes hepatic steatosis, muscle insulin resistance, and pancreatic β-cell dysfunction, creating a self-perpetuating cycle of metabolic deterioration.
The following diagram illustrates key inflammatory pathways in metabolic syndrome:
Inflammatory Pathways in Metabolic Syndrome
Research Reagent Solutions for Biomarker Validation
Table 3: Essential Research Reagents for Inflammatory Biomarker Studies
| Reagent Category | Specific Examples | Research Application | Technical Considerations |
|---|---|---|---|
| Immunoassays | ELISA kits for CRP, IL-6, TNF-α, adiponectin | Quantification of circulating inflammatory mediators | Validate cross-reactivity; check recovery in biological matrix |
| Automated Hematology Analyzers | Beckman Coulter DxH 800 analyzer | Complete blood count parameters for cellular indices | Standardize sample processing timelines; establish QC procedures |
| Genomic Analysis Tools | RNA-seq platforms, single-cell RNA-seq | Transcriptomic profiling of inflammatory pathways | Preserve RNA integrity; normalize for cellular heterogeneity |
| Proteomic Platforms | Mass spectrometry, Olink panels | Multiplexed protein biomarker quantification | Implement normalization strategies; validate dynamic range |
| Spatial Biology Reagents | Multiplexed immunofluorescence, spatial transcriptomics | Tissue context for inflammatory processes | Optimize antibody panels; validate signal specificity |
| Metabolomic Profiling | LC-MS/MS, NMR platforms | Assessment of inflammatory metabolites | Standardize sample extraction; use internal standards |
Regulatory Considerations and Qualification Pathways
Fit-for-Purpose Validation Framework
Biomarker validation should follow a fit-for-purpose approach, with evidence requirements tailored to the specific context of use. The level of validation needed varies substantially based on biomarker category and application [155]:
- Susceptibility/Risk Biomarkers: Require epidemiological evidence, biological plausibility, and established causality
- Diagnostic Biomarkers: Prioritize sensitivity and/or specificity with proof of accurate disease identification across diverse populations
- Monitoring Biomarkers: Need validation of ability to reflect disease status changes over time
- Predictive Biomarkers: Emphasize sensitivity, specificity, and mechanistic links to treatment response
- Pharmacodynamic/Response Biomarkers: Require evidence of direct relationship between drug action and biomarker changes
- Safety Biomarkers: Must demonstrate consistent indication of potential adverse effects across populations
Regulatory Engagement Strategies
Several pathways exist for regulatory acceptance of biomarkers in drug development:
Early Engagement: Through Critical Path Innovation Meetings (CPIM) or pre-Investigational New Drug (IND) consultations, developers can discuss biomarker validation plans with regulatory agencies [155].
IND Process: Biomarkers can be validated within specific drug development programs through the IND application process, including Type C surrogate endpoint meetings for efficacy claim support [155].
Biomarker Qualification Program (BQP): The FDA's structured framework for broader biomarker acceptance across multiple drug development programs involves three stages: Letter of Intent, Qualification Plan, and Full Qualification Package [155].
The optimal pathway depends on factors including biomarker maturity, intended application scope, and available supporting evidence. BQP qualification, while more resource-intensive, enables biomarker use across multiple development programs without re-review [155].
The validation of novel inflammatory biomarkers for metabolic syndrome represents a critical advancement in personalized medicine approaches to cardiometabolic disease. Composite scores like INFLA-score and SIRI demonstrate superior performance compared to single markers, reflecting the multidimensional nature of low-grade inflammation in MetS. Machine learning frameworks further enhance predictive accuracy by integrating diverse biomarker classes with clinical parameters.
Future directions should focus on several key areas: First, expanding multi-omics integration to capture the full complexity of inflammatory-metabolic interactions. Second, strengthening longitudinal cohort studies to establish temporal relationships between biomarker dynamics and disease progression. Third, advancing point-of-care testing technologies to translate validated biomarkers into clinical practice. Finally, standardizing regulatory frameworks to facilitate efficient biomarker qualification across diverse populations.
The systematic validation of inflammatory biomarkers according to rigorous methodological standards will enable more precise risk stratification, earlier intervention, and personalized treatment approaches for metabolic syndrome, ultimately mitigating the substantial global burden of cardiometabolic disease.
Cost-Benefit and Risk-Benefit Analysis of Integrating Anti-Inflammatory Therapies into MetS Management
Metabolic syndrome (MetS), a cluster of conditions including central obesity, dyslipidemia, hypertension, and insulin resistance, represents a significant global health challenge with a prevalence of approximately 25% worldwide [2]. Chronic low-grade inflammation has been identified as a central pathogenic driver that connects these components and accelerates the progression to serious comorbidities, including cardiovascular disease (CVD) and type 2 diabetes (T2D) [162] [163]. This whitepaper provides a comprehensive analysis of the therapeutic rationale, cost-benefit considerations, and risk-benefit profiles of integrating targeted anti-inflammatory strategies into MetS management. Evidence from recent clinical trials and meta-analyses demonstrates that anti-inflammatory approaches—spanning pharmacological agents, dietary patterns, and emerging drug therapies—can significantly mitigate cardiovascular risk factors and address the residual inflammatory risk that persists despite current standard care. For researchers and drug development professionals, this analysis underscores the compelling value proposition of targeting inflammation as a modifiable pathway in MetS, while highlighting critical gaps in biomarker-guided personalization and long-term outcome studies that warrant further investigation.
MetS is fundamentally a pro-inflammatory state characterized by chronic, low-grade activation of innate immune pathways that promotes its core metabolic abnormalities and associated complications [162] [163]. The pathophysiology centers on adipose tissue dysfunction, where hypertrophied adipocytes in visceral fat depots secrete pro-inflammatory cytokines and chemokines, including interleukin-6 (IL-6), tumor necrosis factor-alpha (TNF-α), and interleukin-1 beta (IL-1β) [163]. This creates a systemic inflammatory milieu that induces insulin resistance in peripheral tissues, disrupts endothelial function, and promotes atherogenic dyslipidemia—establishing a direct link between inflammation and cardiometabolic disease [2] [162].
The recognition of inflammation as a unifying pathogenic mechanism represents a paradigm shift in MetS research and therapeutic development. Despite optimal management of traditional risk factors such as LDL cholesterol and blood pressure, a substantial residual cardiovascular risk persists in many patients, driven largely by ongoing inflammation [162]. This residual risk presents both a clinical challenge and an opportunity for novel therapeutic interventions. Biomarkers such as high-sensitivity C-reactive protein (hs-CRP) have emerged as valuable tools for quantifying this inflammatory risk and identifying patients who may benefit most from anti-inflammatory strategies [162]. Research indicates that nearly 50% of patients with coronary heart disease exhibit elevated hs-CRP (≥2 mg/L) despite optimal LDL control, underscoring the pervasiveness of residual inflammation [162].
Quantitative Analysis of Anti-Inflammatory Interventions
Anti-Inflammatory Dietary Patterns
A comprehensive meta-analysis of 18 randomized controlled trials demonstrated that anti-inflammatory dietary patterns significantly improve key cardiovascular risk factors in MetS [164]. The table below summarizes the quantitative benefits of these dietary interventions compared to omnivorous control diets.
Table 1: Cardiovascular Risk Reduction with Anti-Inflammatory Diets
| Outcome Measure | Mean Difference (95% CI) | P-value | Clinical Significance |
|---|---|---|---|
| Systolic BP | -3.99 mmHg (-6.01 to -1.97) | 0.0001 | Equivalent to many first-line antihypertensives |
| Diastolic BP | -1.81 mmHg (-2.73 to -0.88) | 0.0001 | Clinically meaningful reduction |
| LDL-C | -0.23 SMD (-0.39 to -0.07) | 0.004 | Modest but significant improvement |
| Total Cholesterol | -0.31 SMD (-0.43 to -0.18) | <0.00001 | Significant improvement |
| hs-CRP | -0.16 SMD (-0.31 to -0.00) | 0.04 | Direct anti-inflammatory effect |
These dietary patterns include the Mediterranean diet (characterized by extra-virgin olive oil ≥60 mL/day, fatty fish ≥2 servings/week, and polyphenol-rich plant foods), DASH diet (emphasizing sodium restriction <2,300 mg/day with potassium-rich foods), Nordic diet (featuring berries ≥100 g/day and cruciferous vegetables), and vegetarian diets [164]. The anti-inflammatory mechanisms of these diets involve suppression of the NF-κB signaling pathway, reduced secretion of pro-inflammatory cytokines, enhanced antioxidant intake, and modulation of gut microbiota to increase production of anti-inflammatory short-chain fatty acids [164].
Pharmacological Agents with Anti-Inflammatory Properties
Table 2: Anti-Inflammatory Pharmacotherapies for MetS Components
| Therapeutic Class | Representative Agents | Primary Indications | Anti-Inflammatory Mechanisms | Cardiovascular Risk Reduction |
|---|---|---|---|---|
| GLP-1 RAs | Liraglutide, Semaglutide, Dulaglutide | T2D, Obesity | ↓ IL-6, IL-1β, TNFα; ↓ CRP; inhibition of NF-κB and NLRP3 inflammasome | MACE reduction: 12-27% [162] |
| SGLT2 Inhibitors | Empagliflozin, Canagliflozin | T2D | ↓ Oxidative stress; improved endothelial function; ↓ inflammation | Heart failure hospitalization reduction: ~30% |
| Statins | Atorvastatin, Rosuvastatin | Dyslipidemia | ↓ Isoprenoid intermediates; inhibition of NF-κB; ↓ cytokines (IL-6, TNFα, CRP) | MACE reduction: up to 37% [162] |
| Targeted Anti-Inflammatories | Colchicine, IL-1β/IL-6 inhibitors | CVD risk reduction | Direct inhibition of specific inflammatory pathways (NLRP3 inflammasome, IL-1β/IL-6 signaling) | COLCHICINE: MACE reduction ~30% in CVD patients |
The pleiotropic anti-inflammatory effects of GLP-1 receptor agonists are particularly noteworthy. These agents demonstrate both weight loss-dependent and independent anti-inflammatory properties, with acute administration reducing TNF-α levels within hours in LPS-challenged mice—far preceding any meaningful weight loss [165]. Clinical trial data further support these direct anti-inflammatory effects; in the SUSTAIN and PIONEER trials, improvements in glucose and weight explained only 20-60% of the observed CRP reductions with semaglutide [165].
Experimental Methodologies for Assessing Anti-Inflammatory Efficacy
Clinical Trial Protocols for Anti-Inflammatory Interventions
Meta-Analysis Protocol for Dietary Interventions [164]
- Search Strategy: Systematic literature review across five databases (PubMed, Web of Science, Cochrane Library, Embase, and CNKI) using PRISMA guidelines
- Inclusion Criteria: Randomized controlled trials (including crossover designs) comparing anti-inflammatory dietary patterns (Mediterranean, DASH, Nordic, ketogenic, vegetarian) versus omnivorous diets
- Outcome Measures: Primary outcomes include systolic and diastolic blood pressure, lipid profiles (LDL-C, HDL-C, triglycerides, total cholesterol), and inflammatory markers (hs-CRP)
- Statistical Analysis: Meta-analysis utilizing RevMan 5 and Stata 18 software with random effects models. Calculation of mean differences (MD) for blood pressure and standardized mean differences (SMD) for lipid parameters and inflammatory markers with 95% confidence intervals
GLP-1 RA Anti-Inflammatory Assessment [165]
- In vitro Models: Human PBMCs stimulated with LPS or other inflammasome activators, treated with GLP-1 RAs, followed by measurement of NF-κB DNA binding, cytokine gene expression (TNF, IL1B), and cytokine secretion
- In vivo Models: Mice challenged with LPS with or without GLP-1 RA pretreatment, followed by serial measurement of circulating TNF-α, IL-6, and other inflammatory mediators
- Clinical Translation: Proteomic analyses of plasma from clinical trial participants (e.g., STEP trials) to identify inflammatory and immune regulatory pathway modifications independent of weight loss
Signaling Pathways in Metabolic Inflammation
Figure 1: Inflammatory Signaling in MetS and Therapeutic Targets
Risk-Benefit Analysis of Anti-Inflammatory Approaches
Comparative Risk Profiles
Anti-Inflammatory Diets
- Benefits: Favorable safety profile, additional nutritional benefits beyond inflammation reduction, synergistic effects with pharmacological therapies
- Risks: Minimal beyond potential dietary adherence challenges and nutrient deficiencies if poorly planned (e.g., vegetarian diets requiring B12 supplementation)
- Risk-Benefit Assessment: Overwhelmingly positive with high benefit-risk ratio, suitable as foundational therapy for all MetS patients [164]
GLP-1 Receptor Agonists
- Benefits: Potent anti-inflammatory effects, significant weight loss (10-23% with newer agents), direct cardiovascular and renal protection, glucose-lowering
- Risks: Gastrointestinal side effects (nausea, vomiting, diarrhea), cost and access limitations, potential muscle mass loss without exercise
- Risk-Benefit Assessment: Favorable for high-risk MetS patients, particularly those with obesity and elevated inflammatory markers despite standard care [166] [165]
Targeted Anti-Inflammatory Biologics
- Benefits: Specific pathway inhibition, potent inflammation reduction, proven cardiovascular event reduction in high-risk patients
- Risks: Immunosuppression potential, infection risk, cost constraints, limited long-term safety data in MetS populations without established CVD
- Risk-Benefit Assessment: Reserved for MetS patients with established CVD and elevated inflammatory markers despite optimal conventional therapy [162]
Cost-Benefit Considerations
The economic burden of MetS and its complications is substantial, with direct medical costs attributed to obesity alone exceeding $260 billion in the US [166]. When evaluating anti-inflammatory therapies, several cost dimensions must be considered:
- Direct Drug Costs: GLP-1 RAs and biologic anti-inflammatories represent significant budget impacts but may yield downstream savings through event reduction
- Monitoring Costs: Anti-inflammatory therapies require baseline and periodic assessment of inflammatory biomarkers (hs-CRP, IL-6), renal function, and hepatic parameters
- Event-Related Cost Avoidance: Successful inflammation reduction translates to fewer myocardial infarctions, strokes, heart failure hospitalizations, and diabetes complications
- Implementation Costs: Dietary interventions require nutrition education and counseling resources but offer favorable long-term cost-effectiveness
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Metabolic Inflammation Studies
| Reagent/Category | Specific Examples | Research Application | Key Findings Enabled |
|---|---|---|---|
| Cytokine Assays | hs-CRP, IL-6, IL-1β, TNF-α ELISA kits | Quantification of systemic inflammation | Correlation of cytokine levels with MetS components and CVD outcomes [162] |
| Cell Culture Models | Human PBMCs, adipocyte cell lines | In vitro screening of anti-inflammatory compounds | GLP-1 RA inhibition of NF-κB DNA binding [165] |
| Animal Models | LPS-challenged mice, genetic obesity models | In vivo efficacy and mechanism studies | Acute anti-inflammatory effects of exenatide/semaglutide [165] |
| Omics Technologies | Proteomics, metabolomics platforms | Unbiased biomarker discovery | Semaglutide-induced changes in inflammatory pathways independent of weight loss [165] |
| Flow Cytometry | Macrophage polarization markers (CD86, CD206) | Immune cell phenotyping | M1/M2 macrophage balance in adipose tissue inflammation [163] |
Future Directions and Research Agenda
The integration of anti-inflammatory approaches into MetS management represents a promising frontier for reducing residual cardiovascular risk. Several key areas warrant prioritized investigation:
Precision Medicine Approaches
- Development of biomarker-guided algorithms for selecting patients most likely to benefit from specific anti-inflammatory therapies
- Identification of genetic polymorphisms influencing response to anti-inflammatory interventions
- Integration of multi-omics data (proteomic, metabolomic, microbiomic) for personalized inflammation targeting
Novel Therapeutic Targets
- Combination therapies targeting multiple inflammatory pathways simultaneously
- Gut microbiome modulation through prebiotics, probiotics, and postbiotics
- miRNA-based therapeutics for epigenetic regulation of inflammation [167]
- Activin receptor inhibitors and myostatin antibodies for preserving muscle mass during weight loss [166]
Clinical Trial Design Innovations
- Standardized inflammatory biomarker panels across trials to enable cross-study comparisons
- Inclusion of early-stage MetS patients to assess potential for disease modification
- Long-term safety and efficacy studies of targeted anti-inflammatories in MetS populations
The compelling evidence supporting inflammation as a core pathogenic mechanism in MetS necessitates a fundamental re-evaluation of therapeutic strategies. Anti-inflammatory interventions—spanning dietary patterns, established pharmacotherapies with pleiotropic anti-inflammatory properties, and emerging targeted biologics—offer significant potential for addressing the residual cardiovascular risk that persists despite current standard care. The cost-benefit and risk-benefit profiles of these approaches vary considerably, with dietary interventions providing a foundational low-risk strategy, while targeted anti-inflammatories offer potent effects for high-risk populations but with greater cost and potential safety considerations.
For drug development professionals and researchers, the inflammation-centered paradigm in MetS presents numerous opportunities for innovation. Prioritizing biomarker-driven patient selection, developing novel targeted therapies with favorable safety profiles, and demonstrating long-term value through comprehensive health economic outcomes research will be critical for advancing this field. As precision medicine approaches mature, the optimal integration of anti-inflammatory strategies into MetS management holds promise for meaningfully reducing the global burden of cardiometabolic disease.
Conclusion
Chronic low-grade inflammation is an established cornerstone of Metabolic Syndrome pathophysiology, driven by a complex network of interactions between inflammasome activation, adipose tissue dysfunction, oxidative stress, and gut microbiota. Targeting this inflammatory network offers a promising, multi-faceted approach for therapeutic intervention beyond managing individual MetS components. Future directions for biomedical research must focus on developing highly specific inflammasome inhibitors, validating non-invasive biomarker panels for early detection and monitoring, and conducting large-scale, long-term clinical trials to firmly establish the role of anti-inflammatory strategies in preventing T2DM and cardiovascular complications. A personalized medicine approach, based on a patient's unique inflammatory signature, represents the next frontier in combating MetS.
References
- 1. Metabolic Syndrome - StatPearls - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK459248/]
- 2. Metabolic syndrome: epidemiology, mechanisms, and ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1661603/full]
- 3. Update on Biomarkers of Chronic Inflammatory Processes ... [https://www.mdpi.com/1422-0067/25/19/10395]
- 4. Obesity, metabolic abnormalities and low-grade inflammation [https://www.frontiersin.org/journals/cardiovascular-medicine/articles/10.3389/fcvm.2025.1607399/full]
- 5. Low-grade inflammation score (INFLA - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12495778/]
- 6. Update on Biomarkers of Chronic Inflammatory Processes ... [https://pubmed.ncbi.nlm.nih.gov/39408723/]
- 7. The association of nutritional and inflammatory status with ... [https://www.nature.com/articles/s41598-025-94061-7]
- 8. “Recommendations for clinical study protocols for immune ... [https://www.nature.com/articles/s41531-025-01146-1]
- 9. molecular mechanisms via inflammasome signaling - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12362934/]
- 10. NLRP3 and beyond: inflammasomes as central cellular ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1624770/full]
- 11. NLRP3, conveyed via extracellular vesicles from metabolic ... [https://pubmed.ncbi.nlm.nih.gov/40517251/]
- 12. Assembly and activation of the NLRP3 inflammasome and ... [https://www.frontiersin.org/journals/sports-and-active-living/articles/10.3389/fspor.2025.1602208/full]
- 13. IL-1 family cytokines in inflammation and immunity [https://www.nature.com/articles/s41423-025-01358-8]
- 14. Obesity-induced NLRP3 inflammasome activation in nucleus ... [https://josr-online.biomedcentral.com/articles/10.1186/s13018-025-06382-y]
- 15. Promising Molecular Therapeutic Targets for Drug ... [https://www.mdpi.com/2077-0383/14/16/5827]
- 16. Molecular connections between inflammation and social ... [https://www.frontiersin.org/journals/epidemiology/articles/10.3389/fepid.2025.1683955/full]
- 17. The endocrine function of adipose tissues in health and ... [https://www.nature.com/articles/s41574-019-0230-6]
- 18. The Roles and Associated Mechanisms of Adipokines in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8781412/]
- 19. Pathophysiology of Obesity - StatPearls - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK572076/]
- 20. Chronic Adipose Tissue Inflammation Linking Obesity to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7000657/]
- 21. Pathophysiology of obesity and its associated diseases [https://www.sciencedirect.com/science/article/pii/S2211383523000126]
- 22. Exercise training modulates adipokine dysregulations in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9219261/]
- 23. Pro-inflammatory cytokines: The link between obesity and ... [https://www.sciencedirect.com/science/article/abs/pii/S1359610118301199]
- 24. IL-1β and TNFα Cooperativity in Regulating IL-6 Expression in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8619559/]
- 25. IL-1β promotes adipogenesis by directly targeting ... [https://www.nature.com/articles/s41467-024-51938-x]
- 26. Mitochondria in oxidative stress, inflammation and aging [https://www.nature.com/articles/s41392-025-02253-4]
- 27. Biomarkers of Oxidative Stress in Metabolic Syndrome and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6525823/]
- 28. Therapeutic Strategies Targeting Oxidative Stress and ... [https://www.mdpi.com/2673-6411/5/4/35]
- 29. Obesity-Driven Metabolic Disorders: The Interplay of ... [https://www.mdpi.com/1422-0067/26/19/9715]
- 30. Mitochondrial Dysfunction: A Basic Mechanism in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3603328/]
- 31. Association of Inflammatory and Oxidative Status Markers ... [https://www.mdpi.com/2076-3921/12/6/1221]
- 32. Mitochondrial dysfunction: mechanisms and advances in ... [https://www.nature.com/articles/s41392-024-01839-8]
- 33. Therapeutic Strategies for Regulating Mitochondrial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7023101/]
- 34. Association between dietary index for gut microbiota and ... [https://www.nature.com/articles/s41598-025-99396-9]
- 35. Gut Microbiota as a Trigger for Metabolic Inflammation in ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2020.571731/full]
- 36. Gut microbiota, low-grade inflammation, and metabolic ... [https://pubmed.ncbi.nlm.nih.gov/24285672/]
- 37. Association Between the Dietary Index for Gut Microbiota and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12603787/]
- 38. Involvement of gut microbiota in the development of low-grade ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3463487/]
- 39. Gut microbiota dysbiosis and systemic inflammation in ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1662578/full]
- 40. Efficacy of Gut Microbiome-Targeted Therapies in Modulating ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12541121/]
- 41. Gut microbiota dysbiosis and the gut–liver–brain axis [https://www.sciencedirect.com/science/article/pii/S2590097825000382]
- 42. Pharmacological modulation of the gut microbiota and ... [https://www.sciencedirect.com/science/article/pii/S3050567425000094]
- 43. Inflammaging: Mechanisms, Markers, and Intervention ... [https://www.nia.nih.gov/research/dab/workshops/inflammaging-mechanisms-markers-and-intervention-strategies]
- 44. Targeting immunosenescence and inflammaging [https://www.nature.com/articles/s12276-025-01527-9]
- 45. Inflammageing, a targetable pathway for preventing ... [https://pubmed.ncbi.nlm.nih.gov/39530590/]
- 46. Editorial: Inflammaging and immunosenescence: role in ... [https://www.frontiersin.org/journals/cardiovascular-medicine/articles/10.3389/fcvm.2025.1616623/full]
- 47. Low-grade inflammation score (INFLA- score) associated with ... [https://dmsjournal.biomedcentral.com/articles/10.1186/s13098-025-01850-1]
- 48. Cardiovascular inflammaging: Mechanisms, consequences ... [https://www.sciencedirect.com/science/article/pii/S2666379125003374]
- 49. Common and Novel Markers for Measuring Inflammation and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8001241/]
- 50. Diagnostics: Inflammatory Markers [https://www.tamingthesru.com/blog/diagnostics/inflammatory-markers]
- 51. Inflammation Biomarkers | Learn With Superpower [https://superpower.com/library/inflammation-biomarker-testing?srsltid=AfmBOorswGLr88xUVRSHGnV18L8ndUVmt8chv1oHfbWo72eApaZsjbOD]
- 52. Human C-reactive protein and the metabolic syndrome - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2921825/]
- 53. Association of white blood cell count with metabolic ... [https://www.sciencedirect.com/science/article/abs/pii/S0026049509001644]
- 54. White blood cell count and clustered components of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7919179/]
- 55. Fibrinogen as a key regulator of inflammation in disease [https://pubmed.ncbi.nlm.nih.gov/22037947/]
- 56. The metabolic syndrome and C-reactive protein, fibrinogen ... [https://www.sciencedirect.com/science/article/abs/pii/S0021915003001345]
- 57. between high-sensitivity C-reactive protein (hs- Comparison ) and... CRP [https://pubmed.ncbi.nlm.nih.gov/20075574/]
- 58. in the diagnosis of Inflammatory markers metabolic syndrome [https://www.dovepress.com/comparison-of-inflammatory-markers-in-the-diagnosis-of-metabolic-syndr-peer-reviewed-fulltext-article-DMSO]
- 59. The Role of Fibrinogen, Homocysteine and Metabolic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10673203/]
- 60. The association between white blood cell counts and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11784339/]
- 61. Developmental Trends of Metabolic Syndrome in the Past ... [https://www.mdpi.com/2077-0383/14/7/2402]
- 62. TARGETING INFLAMMATION IN METABOLIC SYNDROME [https://pmc.ncbi.nlm.nih.gov/articles/PMC6800061/]
- 63. The Mechanisms of Chronic Inflammation in Obesity and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12110701/]
- 64. Inflammation in Metabolic Diseases and Insulin Resistance [https://e-jcpp.org/journal/view.php?doi=10.36011/cpp.2021.3.e5]
- 65. Clinical Significance of Serum IL-6 and TNF-α Levels in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5643447/]
- 66. Proinflammatory cytokines IL-6 and TNF-α and the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4360270/]
- 67. Relationship between Cytokines and Metabolic Syndrome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10784435/]
- 68. Assessment of metabolic syndrome predictors in relation to ... [https://www.nature.com/articles/s41598-022-27269-6]
- 69. Frontiers | Editorial: Cellular and molecular mechanisms in metabolic ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1580553/full]
- 70. Biomarkers of Oxidative Stress, Inflammation, and Brain ... [https://www.sciencedirect.com/science/article/pii/S0034837625001950]
- 71. Association Between Oxidative–Inflammation Biomarkers ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12383110/]
- 72. 8-OHdG Test: Measuring DNA Damage and Oxidative Stress [https://www.jinfiniti.com/8-ohdg-test/?srsltid=AfmBOorNG8XOnpUu5rMECAIzcoqo35yBEqSHFH01cXDqdgG5bWgXUzJi]
- 73. Role of Oxidative Stress Markers F2-Isoprostanes and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12156724/]
- 74. Are F2-isoprostanes a better marker of semen lipid ... [https://www.sciencedirect.com/science/article/pii/S1043466625000365]
- 75. Simultaneous analysis of cotinine and 8-OHdG in urine [https://pmc.ncbi.nlm.nih.gov/articles/PMC12623111/]
- 76. Automated determination of 8-OHdG in cells and tissue via ... [https://www.sciencedirect.com/science/article/pii/S2215017X24000067]
- 77. Metabolomics in the Analysis of Inflammatory Diseases - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK402338/]
- 78. Review Early nutritional interventions for chronic low-grade ... [https://www.sciencedirect.com/science/article/abs/pii/S1043276025001249]
- 79. Serum metabolomics identifies unique inflammatory ... [https://link.springer.com/article/10.1007/s11306-025-02310-7]
- 80. 1H NMR Metabolomics Identifies Underlying Inflammatory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6220363/]
- 81. ISMRM 2025 Workshop on Frontiers in Metabolomics & ... [https://www.ismrm.org/workshops/2025/MMI/]
- 82. Evidence of a genetically driven metabolomic signature in ... [https://www.nature.com/articles/s41598-022-18178-9]
- 83. Salivary Biomarkers: Toward Future Clinical and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3811231/]
- 84. Salivary biomarkers: novel noninvasive tools to diagnose ... [https://www.nature.com/articles/s41368-023-00231-6]
- 85. Promising applications of human-derived saliva biomarker ... [https://www.nature.com/articles/s41368-022-00209-w]
- 86. Salivary Biomarkers Identification: Advances in Standard ... [https://www.mdpi.com/2673-6373/5/2/26]
- 87. Sensing strategies for disease biomarkers in saliva [https://www.sciencedirect.com/science/article/abs/pii/S001085452500921X]
- 88. Pre-Validation of Salivary Biomarkers for Oral Cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3319329/]
- 89. INFLA score: a novel inflammatory marker for assessing ... [https://dmsjournal.biomedcentral.com/articles/10.1186/s13098-024-01396-8]
- 90. Correlation analysis of inflammatory markers with the short- ... [https://www.nature.com/articles/s41598-024-66279-4]
- 91. The relationship between composite inflammatory ... [https://www.sciencedirect.com/science/article/abs/pii/S0167527324013779]
- 92. Multi-omics profiling: the way toward precision medicine in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8697344/]
- 93. Chromatin accessibility: biological functions, molecular ... [https://www.nature.com/articles/s41392-024-02030-9]
- 94. Chromatin profiling to identify biomarkers in inflammatory ... [https://pubmed.ncbi.nlm.nih.gov/40304726/]
- 95. Editorial: Artificial intelligence in predicting, determining ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11217532/]
- 96. NeXtMD: a new generation of machine learning and deep ... [https://bmcbiol.biomedcentral.com/articles/10.1186/s12915-025-02314-8]
- 97. New perspectives on the NLRP3 inflammasome ... [https://www.explorationpub.com/Journals/emd/Article/1007104]
- 98. ML345 is a potent and selective NLRP3 inflammasome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12615901/]
- 99. Immuno-metabolic diseases and therapeutics: molecular ... [https://biosignaling.biomedcentral.com/articles/10.1186/s12964-025-02368-9]
- 100. NLRP3 inflammasome in health and disease (Review) [https://www.spandidos-publications.com/10.3892/ijmm.2025.5489]
- 101. inhibiting the NLRP3 inflammasome to treat chronic ... [https://www.nature.com/articles/d43747-025-00093-3]
- 102. Overcoming roadblocks to anti-inflammatory NLRP3 ... [https://www.nature.com/articles/d41573-025-00156-1]
- 103. Low-dose colchicine for management of coronary artery ... [https://www.ccjm.org/content/92/10/609]
- 104. Blockade of IL-1 family cytokines in the treatment ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1577628/full]
- 105. Efficacy and safety of colchicine in patients with coronary ... [https://pubmed.ncbi.nlm.nih.gov/41019029/]
- 106. Long-term efficacy and safety of colchicine and anti-IL-1 ... [https://pubmed.ncbi.nlm.nih.gov/40252570/]
- 107. Mitochondrial Dysfunction, Oxidative Stress, and Neuroinflammation: Intertwined Roads to Neurodegeneration - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7466131/]
- 108. Mitochondrial Oxidative Stress—A Causative Factor and Therapeutic Target in Many Diseases - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8707347/]
- 109. Mitochondrial Disease Therapeutic Pipeline [https://umdf.org/clinical-trials/therapeutic-pipeline/]
- 110. Mitochondrial Dysfunction as a Therapeutic Nexus in HFpEF [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1676988/abstract]
- 111. Mitochondrial dysfunction as a therapeutic nexus in HFpEF [https://pubmed.ncbi.nlm.nih.gov/41089829/]
- 112. Biomarkers of mitochondrial disorders - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC10903091/]
- 113. Frontiers | Mitochondrial Dysfunction and Oxidative Stress in Alzheimer’s Disease [https://www.frontiersin.org/journals/aging-neuroscience/articles/10.3389/fnagi.2021.617588/full]
- 114. Physiological Mechanisms of and Therapeutic Approaches ... [https://www.mdpi.com/1467-3045/47/8/637]
- 115. Microbiome-based therapeutics for metabolic disorders [https://pmc.ncbi.nlm.nih.gov/articles/PMC12613280/]
- 116. Anti-Inflammatory and Immunomodulatory Effects of Probiotics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7953067/]
- 117. Medicinal Plants for a Healthy Gut Microbiome [https://www.mdpi.com/1422-0067/26/22/10875]
- 118. Dietary Component-Induced Inflammation and Its ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2022.931458/full]
- 119. The role of phytochemicals in modulating the gut microbiota [https://www.sciencedirect.com/science/article/pii/S2590097825000060]
- 120. The interplay between herbal medicines and gut ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10079915/]
- 121. Do polyphenols qualify as prebiotics? The latest scientific ... [https://isappscience.org/do-polyphenols-qualify-as-prebiotics-the-latest-scientific-perspectives/]
- 122. The metabolic syndrome and inflammation: association or ... [https://pubmed.ncbi.nlm.nih.gov/15673055/]
- 123. An empirical dietary inflammatory pattern increases the ... [https://link.springer.com/article/10.1007/s00394-025-03770-2]
- 124. The Anti-Inflammatory Actions of Exercise Training - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4243532/]
- 125. Ultra-Processed Food Consumption and Systemic ... [https://www.mdpi.com/2072-6643/17/18/3012]
- 126. Anti-Inflammatory Diets - StatPearls - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK597377/]
- 127. Association between the dietary inflammatory index and ... [https://pubmed.ncbi.nlm.nih.gov/41210113/?utm_source=FeedFetcher&utm_medium=rss&utm_campaign=None&utm_content=1PqbW6kGMDP8-zIcBV2yY2WdP1bM_inG00MO_jW7aT_OdqWEu3&fc=None&ff=20251111082100&v=2.18.0.post22+67771e2]
- 128. Effectiveness of Physical Exercise on Indicators of Metabolic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12286169/]
- 129. The effects of combined exercise training on glucose ... [https://www.nature.com/articles/s41598-024-51832-y]
- 130. The impact of physical activity and dietary habits on ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1600038/full]
- 131. Exercise effects on the link between inflammation, metabolic ... [https://lipidworld.biomedcentral.com/articles/10.1186/s12944-025-02713-4]
- 132. Advancing drug development with “Fit-for-Purpose†modeling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12436579/]
- 133. The Future of Clinical Trials: Incorporating 'Omics for ... [https://blog.crownbio.com/the-future-of-clinical-trials-incorporating-omics-for-enhanced-stratification]
- 134. Metabolic syndrome: epidemiology, mechanisms, and current ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12441046/]
- 135. Advanced AI Unlocks Precision Patient Stratification ... [https://pixelscientia.com/articles/advanced-ai-unlocks-precision-patient-stratification-for-drug-development/]
- 136. Metabolic syndrome: molecular mechanisms and therapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12378851/]
- 137. Lifestyle modification in the management of the metabolic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3047997/]
- 138. Inflammatory mechanisms linking obesity and metabolic disease [https://pmc.ncbi.nlm.nih.gov/articles/PMC5199709/]
- 139. Anti-Inflammation Lifestyle [https://www.brighamandwomens.org/patients-and-families/meals-and-nutrition/bwh-nutrition-and-wellness-hub/special-topics/anti-inflammatory-lifestyle]
- 140. The anti-inflammatory effects of three different dietary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12529832/]
- 141. Berberine as a multi-target therapeutic agent for obesity [https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-025-02738-6]
- 142. Lifestyle deterioration linked to elevated inflammatory ... [https://www.nature.com/articles/s41598-024-69967-3]
- 143. Antiinflammatory actions of glucagon-like peptide-1–based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12578379/]
- 144. Natural Remedies Repositioned: Advancing Drug ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1655921/abstract]
- 145. Possible Side Effects of Polyphenols and Their Interactions ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10058246/]
- 146. A mechanistic review of chinese medicine polyphenols on ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2022.1017538/full]
- 147. Anti-inflammatory benefits of semaglutide: State of the art [https://pmc.ncbi.nlm.nih.gov/articles/PMC10992717/]
- 148. Emerging insights into the role of IL-1 inhibitors and colchicine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11197348/]
- 149. Colchicine and diabetes in patients with chronic coronary ... [https://www.frontiersin.org/journals/cardiovascular-medicine/articles/10.3389/fcvm.2023.1244529/full]
- 150. Colchicine and the risk of major adverse cardiovascular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12617512/]
- 151. Research advances in the therapy of metabolic syndrome [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2024.1364881/full]
- 152. Anti-inflammatory agents to treat or prevent type 2 diabetes ... [https://pubmed.ncbi.nlm.nih.gov/25345753/]
- 153. Association of dietary inflammatory index and metabolic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9381302/]
- 154. A Focus on Obesity and Type 2 Diabetes Mellitus [https://www.mdpi.com/2227-9059/13/10/2443]
- 155. Use of Biomarkers in Drug Development for Regulatory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12489174/]
- 156. Applications and challenges of biomarker-based predictive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12399543/]
- 157. A machine learning-based framework for predicting ... [https://www.nature.com/articles/s41598-025-06723-1]
- 158. a cross-sectional study using NHANES 2015–2020 data [https://bmccardiovascdisord.biomedcentral.com/articles/10.1186/s12872-025-05109-5]
- 159. The effect of long-term magnesium intake on inflammatory ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1692937/full]
- 160. Machine learning-driven predictions of metabolic syndrome in ... [https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-025-03139-5]
- 161. Development of a Predictive Model for Metabolic ... [https://www.jmir.org/2025/1/e67525]
- 162. Role of Residual Inflammation as a Risk Factor Across ... [https://link.springer.com/article/10.1007/s13300-025-01743-6]
- 163. New Advances in Metabolic Syndrome, from Prevention to ... [https://www.mdpi.com/2072-6643/15/3/640]
- 164. Impact of anti-inflammatory diets on cardiovascular disease ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11965126/]
- 165. Antiinflammatory actions of glucagon-like peptide-1–based ... [https://www.jci.org/articles/view/194751]
- 166. A glimpse into the pipeline of anti-obesity medication ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1630199/full]
- 167. New discoveries in therapeutic targets and drug development ... [https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-025-02682-5]