Comprehensive Flow Cytometry Guide for Macrophage M1/M2 Polarization Analysis
This article provides a complete framework for analyzing macrophage M1/M2 polarization using flow cytometry, tailored for researchers and drug development professionals.
Comprehensive Flow Cytometry Guide for Macrophage M1/M2 Polarization Analysis
Abstract
This article provides a complete framework for analyzing macrophage M1/M2 polarization using flow cytometry, tailored for researchers and drug development professionals. It covers foundational principles of macrophage biology and polarization markers, detailed protocols for human and mouse models, critical troubleshooting for reproducibility, and advanced validation techniques including machine learning and label-free methods. The content synthesizes current best practices to enable accurate immunophenotyping in basic research and therapeutic development.
Understanding Macrophage Polarization: From Basic Biology to Marker Selection
Macrophages are fundamental components of the innate immune system, capable of adopting diverse functional programs in response to signals within their microenvironment. This process, known as macrophage polarization, enables them to perform a wide array of immune functions, from host defense against pathogens to tissue repair and homeostasis maintenance [1]. The classification of macrophages into classically activated (M1) and alternatively activated (M2) phenotypes provides a fundamental framework for understanding their functional diversity, though it's important to recognize that this represents a simplification of a broad continuum of activation states [2] [1].
The M1/M2 paradigm originated from early observations of how macrophages respond to different stimuli. M1 macrophages were first described by G.B. Mackaness in the 1960s as cells activated during cell-mediated immune responses, while M2 macrophages were identified later in the early 1990s in relation to Th2 cell-mediated anti-inflammatory responses [1]. This classification system has persisted as a utilitarian shorthand for describing the pro-inflammatory and anti-inflammatory extremes of macrophage polarization, despite ongoing recognition of its limitations in capturing the full complexity of macrophage phenotypes in vivo [2].
From a technical perspective, the M1/M2 paradigm provides a valuable foundation for flow cytometry-based research, offering defined surface markers and intracellular targets that enable researchers to identify and quantify macrophage subpopulations in various experimental and disease contexts [3]. The polarization process involves significant transcriptional reprogramming, altering the expression of over 1,000 genes and activating distinct signaling pathways, metabolic programs, and effector functions [2].
Biological Foundations of M1 and M2 Macrophages
M1 Macrophages: Pro-inflammatory Mediators
M1 macrophages, or classically activated macrophages, function as powerful effector cells in direct host defense against pathogens. They are typically polarized in vitro through treatment with TLR ligands such as bacterial lipopolysaccharide (LPS) combined with interferon-gamma (IFN-γ), or through stimulation with granulocyte-macrophage colony-stimulating factor (GM-CSF) [1] [4]. In vivo, classically activated macrophages arise in response to IFN-γ produced by Th1 lymphocytes or natural killer cells, along with tumor necrosis factor (TNF) produced by antigen-presenting cells [1].
The activation of M1 macrophages is governed by specific transcription factors including STAT1, IRF5, NF-κB, and AP-1 [2] [1]. These regulators drive a characteristic gene expression profile that enhances microbicidal capacity through several mechanisms. M1 macrophages produce high levels of pro-inflammatory cytokines including IFN-γ, IL-1, IL-6, IL-12, and IL-23, and TNFα [1]. They also generate increased amounts of reactive oxygen species (ROS) and nitrogen radicals through upregulation of inducible nitric oxide synthase (iNOS) [1]. Additionally, they demonstrate enhanced antigen presentation capabilities and express high levels of co-stimulatory molecules [5].
M1 macrophages preferentially utilize glycolysis for energy production, which supports their rapid inflammatory responses and production of antimicrobial compounds [6] [7]. This metabolic reprogramming is essential for their function, allowing prompt generation of energy and reactive oxygen species [6]. During bacterial infections, M1 polarization is crucial for phagocytosis and intracellular killing of pathogens, as demonstrated in infections with Listeria monocytogenes, Salmonella species, and Mycobacterium tuberculosis [1].
M2 Macrophages: Immunoregulatory and Repair Functions
M2 macrophages, or alternatively activated macrophages, function primarily in immune regulation, tissue repair, and resolution of inflammation. They are polarized in vitro by exposure to cytokines such as IL-4, IL-10, or IL-13 [5] [1]. The M2 category encompasses considerable heterogeneity, with several subtypes identified including M2a (wound-healing), M2b (regulatory), and M2c (acquired deactivation) macrophages, each with distinct activation stimuli and functional characteristics [1].
The polarization of M2 macrophages is controlled by transcription factors such as STAT6, STAT3, IRF4, and PPARγ [2] [4]. These regulators drive expression of characteristic M2 markers including arginase 1 (Arg1), chitinase-like proteins (Ym1), resistin-like molecule alpha (Fizz1), and the mannose receptor CD206 [1] [4]. M2 macrophages typically produce high levels of anti-inflammatory cytokines such as IL-10 and TGF-β, which help suppress inflammatory responses and promote tissue repair [1].
Unlike their M1 counterparts, M2 macrophages preferentially rely on oxidative phosphorylation for energy production, utilizing fatty acid oxidation and an intact tricarboxylic acid (TCA) cycle to support their long-term functions in tissue homeostasis and repair [6] [7]. This metabolic profile supports their role in extracellular matrix formation, angiogenesis, and regulation of immune responses [5]. M2 macrophages do not typically produce nitric oxide or present antigen to T cells as effectively as M1 macrophages, reflecting their different functional priorities [5].
Table 1: Core Characteristics of M1 and M2 Macrophages
| Characteristic | M1 Macrophages | M2 Macrophages |
|---|---|---|
| Activation Type | Classical | Alternative |
| Polarizing Stimuli | IFN-γ, LPS, GM-CSF | IL-4, IL-13, IL-10, M-CSF |
| Key Transcription Factors | STAT1, IRF5, NF-κB | STAT6, STAT3, IRF4, PPARγ |
| Characteristic Markers | CD86, CD80, HLA-DR, iNOS | CD206, CD163, Arg1, Ym1 |
| Metabolic Pathway | Glycolysis | Oxidative Phosphorylation |
| Primary Functions | Pathogen killing, Pro-inflammatory response | Tissue repair, Immunoregulation |
Experimental Protocols for Macrophage Polarization
Human Monocyte-Derived Macrophage Polarization
This protocol details the polarization of human monocyte-derived macrophages toward M1 and M2 phenotypes, adapted from established methodologies with specific reagent information [3].
Monocyte Isolation and Differentiation
Begin with negatively selected monocytes cultured in complete RPMI medium. For M1 precursor differentiation, supplement medium with 20 ng/mL human GM-CSF. For M2 precursor differentiation, supplement with 20 ng/mL human M-CSF. Incubate cells for 6 days, adding fresh media with respective factors on day 3. On day 6, cells become M0 undifferentiated macrophages ready for polarization [3].
Macrophage Polarization
- M1 Polarization: Activate M0 macrophages with 100 ng/mL human IFN-γ and 50 ng/mL LPS. Incubate for 24 hours. For enhanced M1 characterization, additional stimulation with 100 ng/mL LPS for 4 hours can be performed [3].
- M2 Polarization: Activate M0 macrophages with 20 ng/mL IL-13 and 20 ng/mL IL-4. Incubate for 24 hours [3].
Characterization via Flow Cytometry
For flow cytometry analysis, seed monocytes at a density of 1 × 10^6 cells/mL in tissue culture-treated 6-well plates. After polarization on day 7, process cells as follows:
- Wash twice with DPBS without Ca²⺠and Mg²âº
- Detach using DPBS with 10 mM EDTA
- Wash twice with DPBS containing 2% FBS
- Resuspend in BSB with human and mouse serum and incubate for 30 minutes on ice
- Stain with surface markers for M1 (CD14+, HLA-DR+, CD274+, CD86+) and M2 (CD14+, HLA-DR-, CD206+) for 30 minutes on ice
- Wash, pellet, fix, and permeabilize for 20 minutes on ice
- Stain intracellular markers (IL-10 and TNF)
- Perform final wash and resuspend in BSB in FACS collection tubes [3]
Murine Bone Marrow-Derived Macrophage Polarization
This protocol describes the generation and polarization of bone marrow-derived macrophages from mice, suitable for investigating macrophage biology in experimental models [6].
Bone Marrow Cell Isolation
Extract long bones from hind limbs under sterile conditions. Flush bone marrow channels with 5 mL medium using a 25-G needle. Pass the aspirate through needles of decreasing sizes (18G, 21G, 23G, 25G) to obtain a single-cell suspension. Resuspend to a concentration of 10^6 cells/mL for further experiments [6].
Monocyte Purification
Isolate monocytes using immunomagnetic separation according to manufacturer protocols. Resuspend approximately 60 × 10^6 cells from bone marrow aspirate in EasySep buffer. Incubate with antibody cocktail targeting non-monocytic cells. Add magnetic particles and separate using a magnet. Transfer unmarked monocytes to a new tube, wash, count, and proceed to differentiation [6].
Macrophage Differentiation and Polarization
Seed isolated monocytes at 40,000 cells/cm² in differentiation medium consisting of high-glucose DMEM supplemented with 20% fetal bovine serum (FBS) and 30% L929-conditioned medium (source of M-CSF). Culture for 7 days, refreshing medium on day 3. For M2 polarization, treat cells with 20 ng/mL IL-4 for 72 hours. Maintain control wells under identical conditions without IL-4 treatment [6].
Signaling Pathways in Macrophage Polarization
M1 Polarization Signaling Pathways
The polarization of M1 macrophages is governed by well-defined signaling cascades initiated by specific stimuli. The binding of IFN-γ to its receptor (IFNGR) activates Janus kinase (JAK) adapters, leading to phosphorylation and activation of STAT1 [4]. Activated STAT1 dimerizes and translocates to the nucleus, where it drives expression of pro-inflammatory genes including major histocompatibility complex (MHC) II, IL-12, and nitric oxide synthase 2 (NOS2) [4].
Simultaneously, microbial products such as LPS activate TLR4, initiating signaling through two main adapter proteins: MyD88 and TRIF [4]. The MyD88-dependent pathway activates IKK complex, leading to NF-κB activation and translocation to the nucleus. NF-κB promotes expression of various inflammatory genes including TNF, IL-1β, and IL-12 [4]. The TRIF-dependent pathway activates IRF3, which induces production of type I interferons (IFN-α and IFN-β) [4]. These signaling cascades converge to establish the characteristic M1 transcriptional program and functional phenotype.
M2 Polarization Signaling Pathways
M2 macrophage polarization is primarily driven by cytokines IL-4 and IL-13, which bind to the IL-4Rα receptor [4]. This binding activates JAK1 and JAK3, leading to phosphorylation and activation of STAT6 [4]. Activated STAT6 translocates to the nucleus and modulates expression of M2-associated genes including arginase 1 (Arg1), chitinase-like 3 (Ym1), and CD206 [4].
Other transcription factors involved in M2 polarization include IRF4 and PPARγ [4]. The IL-10 signaling pathway also contributes to M2 polarization through activation of STAT3, which modulates expression of anti-inflammatory genes and suppresses pro-inflammatory cytokine signaling [4]. Glucocorticoid signaling represents another pathway influencing M2 polarization, with glucocorticoid receptors directly regulating transcription of anti-inflammatory genes like IL-10 [4].
Research Reagent Solutions for Macrophage Studies
Table 2: Essential Research Reagents for Macrophage Polarization Studies
| Reagent Category | Specific Examples | Function in Macrophage Research |
|---|---|---|
| Growth Factors | GM-CSF (20 ng/mL), M-CSF (20 ng/mL) | Directs precursor differentiation toward M1 (GM-CSF) or M2 (M-CSF) predisposition [3] |
| Polarizing Cytokines | IFN-γ (100 ng/mL), IL-4 (20 ng/mL), IL-13 (20 ng/mL) | Induces polarization toward specific phenotypes; IFN-γ for M1, IL-4/IL-13 for M2 [3] |
| TLR Agonists | LPS (50-100 ng/mL) | Synergizes with IFN-γ to promote strong M1 polarization [3] |
| Surface Markers (Flow Cytometry) | CD14, HLA-DR, CD86, CD274 for M1; CD14, CD206 for M2 | Enables identification and quantification of polarized populations via flow cytometry [3] |
| Intracellular Markers | iNOS, TNF for M1; Arg1, IL-10 for M2 | Provides intracellular validation of polarization status [3] |
| Metabolic Probes | Glycolysis inhibitors, OXPHOS modulators | Investigates metabolic differences between M1 (glycolytic) and M2 (OXPHOS) phenotypes [6] [7] |
Flow Cytometry Analysis of Polarized Macrophages
Panel Design and Gating Strategy
Comprehensive flow cytometry analysis is essential for characterizing macrophage polarization states. A well-designed panel should include markers that distinguish between M1 and M2 phenotypes while accounting for potential intermediate states. The gating strategy should follow a logical progression from live cell identification through population characterization [8].
Begin by gating on live cells using a viability dye, followed by singlet discrimination using FSC-H vs FSC-A to exclude doublets. Next, gate on CD14+ monocytes/macrophages to focus on the population of interest. Subsequently, analyze expression of M1 markers (HLA-DR, CD86, CD274) and M2 markers (CD206) to identify polarized subpopulations [3]. For more detailed characterization, include intracellular staining for cytokines (TNF for M1, IL-10 for M2) and metabolic enzymes (iNOS for M1, Arg1 for M2) [3].
Data Presentation and Publication Standards
When presenting flow cytometry data for publication, adhere to established guidelines to ensure reproducibility and clarity [8]. Include detailed information about experimental design, sample preparation, and instrumentation. Specify the flow cytometer manufacturer, model, and software used for acquisition [8]. Describe the sample preparation process including proteases, filtration approaches, red blood cell lysis reagents, permeabilization procedures, and fixatives utilized [8].
For data presentation, clearly outline the gating strategy with all light scatter gates, live-dead gates, doublet gates, and fluorescence-detecting gates [8]. The method used to define gates should be stated, whether using unstained controls, biological controls, isotype controls, or fluorescence minus one controls [8]. Ensure proper compensation is performed and documented, especially for multi-color panels [8]. When presenting plots, label both axes clearly, display proper quantitation for scales, and avoid piling up events on the axis [8].
Table 3: Flow Cytometry Markers for Macrophage Polarization
| Marker | M1 Expression | M2 Expression | Function |
|---|---|---|---|
| CD14 | + | + | Monocyte/macrophage lineage marker [3] |
| HLA-DR | High | Low/Negative | Antigen presentation capability [3] |
| CD86 | High | Low | Co-stimulatory molecule, T cell activation [3] |
| CD274 (PD-L1) | High | Variable | Immune checkpoint molecule [3] |
| CD206 | Low | High | Mannose receptor, endocytosis [3] |
| TNF | High | Low | Pro-inflammatory cytokine [3] |
| IL-10 | Low | High | Anti-inflammatory cytokine [3] |
Advanced Concepts and Recent Developments
Beyond the Binary Paradigm
While the M1/M2 classification provides a useful framework, contemporary research recognizes that macrophage phenotypes exist along a continuum rather than as discrete binary states [2] [1]. In vivo, macrophages display remarkable plasticity, with the ability to transition between functional states in response to changing microenvironmental cues [2]. This continuum includes hybrid states that co-express both M1 and M2 markers, as well as distinct activation patterns driven by tissue-specific factors [2].
The M1/M2 system may be particularly inadequate for describing certain tissue-resident macrophage populations. For example, alveolar macrophages minimally express many canonical M1 markers and often display intermediate M1/M2 phenotypes [2]. Similarly, tumor-associated macrophages (TAMs) frequently exhibit mixed phenotypes that don't neatly align with the classical M1/M2 dichotomy [1]. These observations highlight the importance of comprehensive phenotyping approaches that go beyond simple M1/M2 classification.
Metabolic Regulation of Polarization
Emerging research has illuminated the crucial role of metabolic reprogramming in macrophage polarization. M1 macrophages preferentially utilize glycolysis even under aerobic conditions, a metabolic shift that supports their rapid inflammatory responses and production of antimicrobial compounds [6] [7]. This glycolytic preference is driven by stabilization of hypoxia-inducible factor 1-alpha (HIF1α), which promotes expression of glycolytic enzymes and pro-inflammatory genes [4].
In contrast, M2 macrophages rely primarily on oxidative phosphorylation and fatty acid oxidation to support their long-term functions in tissue repair and immunoregulation [6] [7]. The metabolic differences between M1 and M2 macrophages are not merely consequences of polarization but actively contribute to establishing and maintaining their functional states [6]. Therapeutic targeting of these metabolic pathways represents a promising approach for modulating macrophage function in disease contexts.
Therapeutic Implications and Targeting Strategies
The manipulation of macrophage polarization states holds significant therapeutic potential across various disease contexts. In cancer, strategies to reprogram tumor-associated macrophages from pro-tumorigenic M2-like states to anti-tumorigenic M1-like states are being actively investigated [9]. Similarly, in chronic inflammatory diseases and fibrosis, promoting a shift from pro-inflammatory M1 to anti-inflammatory M2 phenotypes may help resolve inflammation and limit tissue damage [1].
Recent advances have identified multiple molecular targets for modulating macrophage polarization, including transcription factors, metabolic enzymes, and signaling pathway components [2] [4]. For example, disruption of CDK5 regulatory subunit p35 has been shown to limit immunosuppressive M2 macrophages while maintaining functional M1 macrophages, suggesting a potential therapeutic strategy for enhancing anti-tumor immunity [7]. Similarly, microRNAs such as miR-210 have been implicated in regulating macrophage polarization and may represent promising therapeutic targets [6].
Key Surface and Intracellular Markers for M1 (CD86, MHC II, TNF-α) and M2 (CD206, Arginase 1) Identification
Macrophages are fundamental components of the innate immune system, exhibiting remarkable plasticity that allows them to adopt diverse functional phenotypes in response to environmental cues. The classification of macrophages into classically activated (M1) and alternatively activated (M2) polarization states provides a framework for understanding their roles in health and disease. Flow cytometry has emerged as an indispensable tool for discriminating these subsets based on surface and intracellular marker expression, offering single-cell resolution and multi-parameter analysis capabilities that are essential for modern immunological research and drug development [10] [11]. The accurate identification of macrophage polarization states is particularly crucial in oncology, where tumor-associated macrophages (TAMs) can constitute up to 50% of the tumor mass and significantly influence therapeutic outcomes [12].
The M1/M2 paradigm represents a continuum of activation states rather than discrete entities, with macrophages often exhibiting mixed or intermediate phenotypes. M1 macrophages typically emerge in response to interferon-gamma (IFN-γ) and microbial products like lipopolysaccharide (LPS), driving pro-inflammatory responses and anti-tumor immunity. In contrast, M2 macrophages polarized by interleukin-4 (IL-4) and IL-13 promote immunosuppression, tissue repair, and angiogenesis, frequently contributing to tumor progression [12] [13]. This application note provides a comprehensive framework for identifying these functionally distinct populations using optimized flow cytometry panels, with particular emphasis on the key surface markers CD86 and CD206, and intracellular proteins including MHC II, TNF-α, and Arginase 1.
Marker Profiles and Phenotypic Characterization
Comprehensive Marker Panels for M1 and M2 Macrophages
Table 1: Key Surface and Intracellular Markers for Macrophage Polarization
| Marker Type | Marker | M1 Expression | M2 Expression | Cellular Location | Primary Function |
|---|---|---|---|---|---|
| Surface | CD86 | High [14] | Low [14] | Cell membrane | Co-stimulatory molecule for T-cell activation |
| Surface | CD206 | Low/Absent [15] | High [15] [16] | Cell membrane | Phagocytosis, endocytic receptor |
| Surface | MHC Class II | High [14] | Low/Medium [14] | Cell membrane | Antigen presentation |
| Intracellular | TNF-α | High [14] | Low [14] | Cytoplasmic | Pro-inflammatory cytokine |
| Intracellular | Arginase-1 | Low/Absent [17] | High [16] [17] | Cytosolic enzyme | L-arginine metabolism, inhibits NO production |
| Surface | CD14 | Medium [14] | Low (M2a) / Medium (M2c) [14] | Cell membrane | LPS receptor component |
| Surface | F4/80 | High (M1, M2a) [14] | Variable (Low on M2c) [14] | Cell membrane | Scavenger receptor |
The characterization of macrophage polarization states requires a multi-parameter approach, as no single marker provides definitive classification. The markers highlighted in Table 1 represent well-established indicators, but macrophage phenotypes exist along a spectrum with considerable heterogeneity. CD86 and MHC Class II serve as robust surface indicators of M1 polarization, facilitating antigen presentation and T-cell co-stimulation [14]. Conversely, CD206 (mannose receptor) functions as a highly specific marker for M2 macrophages, particularly those polarized by IL-4, and mediates endocytic clearance and immunoregulatory functions [13] [15]. For intracellular proteins, TNF-α production is characteristic of M1 macrophages following inflammatory stimulation, while Arginase-1 expression represents a defining metabolic enzyme for M2 macrophages that modulates the tumor microenvironment through arginine depletion [16] [17].
Table 2: Additional Markers for Comprehensive Macrophage Subtyping
| Macrophage Subset | Polarizing Stimuli | Additional Characteristic Markers | Functional Specialization |
|---|---|---|---|
| M1 | IFN-γ ± LPS [14] | CD80, iNOS, IL-12, IL-23 [12] | Pro-inflammatory responses, microbial killing |
| M2a | IL-4, IL-13 [14] | CD209, CCL17, CCL22 [13] | Tissue repair, fibrosis, immunoregulation |
| M2b | Immune complexes, TLR/IL-1R ligands | CD64, CD86 (low), IL-10 | Immunoregulation |
| M2c | IL-10 [14] | CD163, CD14 (med), TGF-β, MER TK [12] | Matrix deposition, tissue remodeling |
| M2d | TLR antagonists, adenosine | VEGF, IL-10, TGF-β [14] | Angiogenesis, tumor promotion |
Context-Dependent Marker Variability
The expression patterns of macrophage markers demonstrate significant context-dependent variability that researchers must consider during experimental design and data interpretation. Studies of bronchoalveolar lavage fluid (BALF) from lung cancer patients revealed macrophages co-expressing CD68+bright, CD206+bright, CD163+bright, CD80+, CD86+, and CD40+bright, challenging the simplistic M1/M2 binary and highlighting the intermediate phenotypes prevalent in human disease [12]. Similarly, investigations of murine renal mononuclear phagocytes identified CD86+MHCII+CD206- and CD206+ subpopulations across five distinct MNP subsets, demonstrating that functional heterogeneity exists within conventionally defined macrophage populations [15].
Technical factors also significantly impact marker expression. The polarization method itself influences phenotype, as plastic adhesion during monocyte isolation tends to push cells toward pro-inflammatory states, while CD14 positive selection with magnetic beads favors anti-inflammatory phenotypes [18]. Furthermore, stimulation with LPS can induce TLR4 ectodomain shedding from the cell surface and alter phagocytic capacity, potentially confounding results if not properly controlled [18] [14]. These findings underscore the importance of using multi-marker panels with partially redundant markers to ensure accurate classification despite context-dependent variability.
Experimental Protocols and Workflows
Macrophage Differentiation and Polarization
Table 3: Standardized Protocol for Generating M1 and M2 Macrophages from Bone Marrow Mononuclear Cells (BMNCs)
| Step | Procedure | Duration | Key Reagents | Quality Control |
|---|---|---|---|---|
| BMNC Isolation | Aspirate bone marrow from femurs/tibiae; isolate mononuclear cells using Histopaque-1083 density gradient centrifugation | 60-90 minutes | High-glucose DMEM with 10% FBS, Histopaque-1083 [19] | Cell viability >95% by trypan blue exclusion |
| Macrophage Differentiation | Culture BMNCs in complete medium supplemented with M-CSF (50ng/mL) | 6-7 days | Recombinant M-CSF [19] | Adherent, elongated morphology |
| M1 Polarization | Treat differentiated macrophages with IFN-γ (100ng/mL) + LPS (100ng/mL) | 24 hours | Recombinant IFN-γ, LPS [14] | Verify via TNF-α ELISA (significant increase) [14] |
| M2 Polarization | Treat differentiated macrophages with IL-4 (20ng/mL) ± IL-13 (20ng/mL) | 24-48 hours | Recombinant IL-4, IL-13 [19] [14] | Verify via CD206 and Arginase-1 expression |
This standardized protocol for generating polarized macrophages from mouse and rat BMNCs provides a high-throughput, reproducible method that minimizes technical variability. The approach yields approximately 200% cell expansion while complying with 3R principles (Replace, Reduce, Refine) through efficient cell utilization [19]. For human macrophage studies, peripheral blood mononuclear cells (PBMCs) can be isolated via Ficoll-Paque density gradient centrifugation, with monocytes subsequently differentiated using M-CSF (50ng/mL) for 6-7 days before polarization with identical cytokine regimens.
Flow Cytometry Staining and Analysis
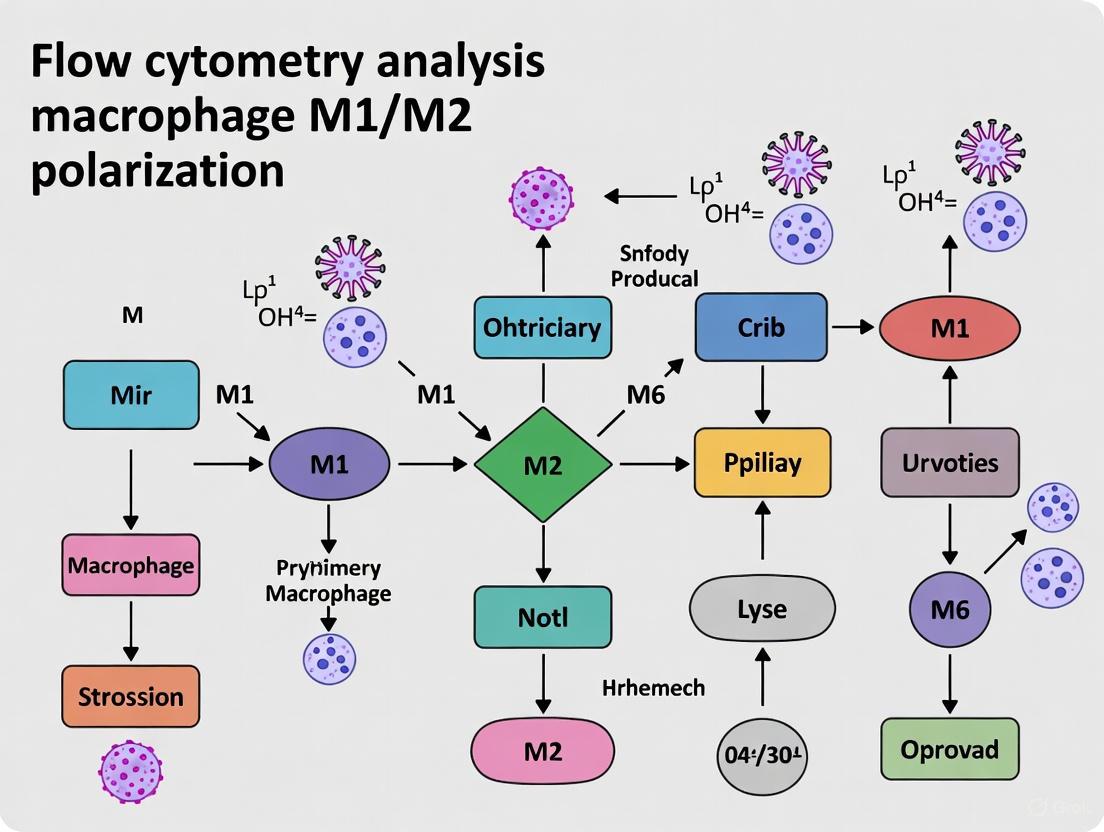
Diagram 1: Flow cytometry staining workflow for M1/M2 macrophage identification.
The staining protocol proceeds through sequential steps critical for preserving marker integrity and antibody accessibility. Surface antigen staining should be performed on live, unfixed cells using fluorochrome-conjugated antibodies against CD86, CD206, and MHC Class II in staining buffer containing Fc receptor block to minimize non-specific binding. Following surface staining, cells require fixation and permeabilization before intracellular staining—a step where specific buffer selection significantly impacts results. For optimal Arginase-1 detection, the Intracellular Fixation & Permeabilization Buffer Set (Invitrogen, 88-8824-00) provides superior performance, though the Foxp3/Transcription Factor Staining Buffer Set (00-5523-00) represents a viable alternative [17]. Simultaneous intracellular staining for TNF-α and Arginase-1 enables direct correlation of M1 and M2 signatures at the single-cell level.
Compensation controls must include singly stained samples for each fluorochrome used, while fluorescence-minus-one (FMO) controls are essential for establishing accurate gating boundaries, particularly for markers with continuous expression patterns like CD206 and CD86 [15]. For analysis, researchers should first identify the macrophage population based on forward/side scatter properties and lineage markers (e.g., F4/80, CD11b), then subsequently gate on M1 (CD86+MHCII+CD206-) and M2 (CD206+) subpopulations before assessing intracellular TNF-α and Arginase-1 expression within these predefined subsets.
Data Interpretation and Analytical Considerations
Quantitative Expression Profiles
Table 4: Expected Marker Expression Patterns in Polarized Macrophage Subsets
| Marker | Naïve (M0) | M1 (IFN-γ + LPS) | M2a (IL-4) | M2c (IL-10) |
|---|---|---|---|---|
| CD86 | Low [14] | Medium/High [14] | Low [14] | Low [14] |
| CD206 | Low [15] | Low/Absent [15] | High [15] [16] | Medium [14] |
| MHC Class II | Very Low [14] | Low [14] | Low [14] | Medium [14] |
| TNF-α | Very Low [14] | Medium (surface) [14] | Low [14] | Low [14] |
| Arginase-1 | Very Low [14] | Low/Absent [17] | High [16] [17] | Medium [14] |
| F4/80 | High [14] | High [14] | High [14] | Low [14] |
Data interpretation must account for the quantitative expression patterns detailed in Table 4, recognizing that these represent general guidelines rather than absolute thresholds. M1 macrophages typically demonstrate medium to high expression of CD86 and MHC Class II with minimal CD206, while producing substantial TNF-α upon stimulation [14]. Conversely, M2a macrophages exhibit high CD206 and Arginase-1 expression with low CD86 and MHC Class II [15] [16] [14]. The M2c subset induced by IL-10 displays a distinct pattern with medium MHC Class II and CD206 expression but low CD86 and TNF-α [14].
Researchers should note that marker expression exists along a continuum, with intermediate phenotypes commonly observed in disease contexts. For instance, studies of lung cancer BALF revealed macrophages simultaneously expressing both M1 (CD80, CD86) and M2 (CD206, CD163) markers, underscoring the limitations of rigid classification schemes [12]. Similarly, investigations using an optimized eleven-color flow cytometry panel identified substantial heterogeneity in marker expression within nominally polarized populations, highlighting the importance of multi-parameter analysis for comprehensive phenotypic characterization [14].
Technical Validation and Quality Control
Robust experimental design requires implementation of systematic quality control measures throughout the workflow. Polarization efficiency should be verified through functional assays, with M1 polarization confirmed via TNF-α ELISA (expecting ~1552 ± 80.1 pg/mL for IFN-γ + LPS stimulation in RAW264.7 cells) and M2 polarization validated through Arginase-1 detection and phagocytosis assays (M2 macrophages typically exhibit higher phagocytic capacity than M1) [18] [14]. Technical variance assessments have demonstrated that standardized protocols yield highly reproducible results with minimal inter-experimenter variability when processing identical samples [15].
Potential technical pitfalls necessitate specific controls. LPS stimulation can completely clear TLR4 from the cell surface through ectodomain shedding, potentially confounding analyses that include this marker [14]. Additionally, F4/80 expression decreases substantially on M2c macrophages, potentially leading to underestimation of this subset if used as the sole identification marker [14]. Researchers should therefore implement multi-marker gating strategies that do not rely exclusively on a single marker for population identification.
Applications in Disease Research and Therapeutic Development
The precise identification of macrophage polarization states using flow cytometry has profound implications for both basic research and translational applications. In oncology, detailed characterization of tumor-associated macrophages (TAMs) provides critical insights into disease progression and therapeutic response. Studies investigating the origin of metastatic cancer cells have revealed that M2 macrophages phagocytosing apoptotic tumor cells can undergo a "change of loyalty," potentially becoming the source of distal tissue tumor metastasis [13]. This paradigm-shifting hypothesis underscores the therapeutic potential of targeting M2 macrophages, with experiments demonstrating that CD206 knockdown significantly suppresses tumor growth and metastasis in murine models [13].
Beyond oncology, macrophage polarization plays crucial roles in renal pathology, where distinct MNP subsets and their functional segmentation vary between different mouse models of kidney injury and are dynamically regulated in a time-dependent manner [15]. The refinement of macrophage subpopulations has revealed that CD206+ cells from multiple MNP subsets exhibit significantly higher ex vivo phagocytic capacity than their CD86+MHCII+CD206- counterparts, indicating functional specialization within the macrophage compartment [15].
Pharmacological modulation of macrophage polarization represents an emerging therapeutic strategy. Recent investigations have demonstrated that CDK8/19 inhibitors such as BRD6989 enhance IL-4-induced Arginase-1 expression in macrophages via STAT6 and p38 MAPK activation, simultaneously increasing CD206 surface expression [16]. This chemical promotion of M2 polarization suggests novel approaches for treating inflammatory disorders and highlights the importance of accurate macrophage phenotyping in drug development pipelines.
The Scientist's Toolkit: Essential Research Reagents
Table 5: Essential Reagents for Macrophage Polarization and Flow Cytometry Analysis
| Reagent Category | Specific Examples | Function/Application | Considerations |
|---|---|---|---|
| Polarization Cytokines | Recombinant IFN-γ, LPS, IL-4, IL-13, IL-10, M-CSF | Direct macrophage polarization toward specific phenotypes | Species-specific variants required; optimize concentrations empirically |
| Flow Cytometry Antibodies | Anti-CD86, CD206, MHC II, F4/80, CD11b, TNF-α, Arginase-1 (clone A1exF5) | Marker identification and population discrimination | Fluorochrome selection critical for panel design; validate clones for specific applications |
| Intracellular Staining Reagents | Intracellular Fixation & Permeabilization Buffer Set (88-8824-00), Foxp3/Transcription Factor Staining Buffer Set (00-5523-00) | Enable detection of intracellular antigens | Buffer selection affects signal intensity; optimize for specific targets |
| Cell Isolation Reagents | Histopaque-1083, Ficoll-Paque, magnetic bead separation kits | Isolation of mononuclear cells from blood or bone marrow | Method affects basal activation state; plastic adhesion promotes inflammation |
| Validation Assays | TNF-α ELISA, phagocytosis assays (E. coli bioparticles), quantitative PCR | Verify polarization efficiency and functional status | Implement alongside flow cytometry for comprehensive characterization |
| Egfr-IN-44 | Egfr-IN-44, MF:C27H29ClN6O2S, MW:537.1 g/mol | Chemical Reagent | Bench Chemicals |
| PfPKG-IN-1 | PfPKG-IN-1|cGMP-Dependent Protein Kinase Inhibitor | Bench Chemicals |
This curated reagent list provides foundational components for establishing robust macrophage polarization and characterization workflows. The Arginase-1 antibody clone A1exF5 warrants particular emphasis as it recognizes both human and mouse Arginase-1 and represents the only clone validated for flow cytometry detection of this crucial M2 marker in both species [17]. When designing flow cytometry panels, researchers should prioritize antibodies with minimal spectral overlap and include viability dyes (e.g., Fixable Viability Stain 780) to exclude dead cells from analysis, thereby reducing non-specific binding and false positives.
The comprehensive flow cytometry-based framework presented herein enables precise identification of macrophage polarization states through simultaneous assessment of surface (CD86, CD206, MHC II) and intracellular (TNF-α, Arginase-1) markers. When implemented alongside standardized polarization protocols and appropriate analytical approaches, these panels provide powerful tools for elucidating macrophage heterogeneity in health and disease. The integration of multi-parameter flow cytometry with functional assays offers unprecedented resolution for dissecting macrophage biology, facilitating advances in both basic immunology and the development of macrophage-targeted therapeutics across diverse pathological contexts.
Macrophages exhibit remarkable functional plasticity, dynamically polarizing into distinct phenotypes in response to microenvironmental cues. While the classical M1/M2 dichotomy provides a foundational framework, the M2 phenotype encompasses a spectrum of specialized subtypes—M2a, M2b, M2c, and M2d—each with unique activation mechanisms, marker expression, and functional roles [20] [21]. This heterogeneity underpins their diverse functions in immune regulation, tissue homeostasis, and disease progression, presenting both challenges and opportunities for research and therapeutic development.
Understanding these subtypes is particularly crucial in the context of tumor microenvironments, where M2-like tumor-associated macrophages (TAMs) play pivotal roles in facilitating angiogenesis, metastasis, and immunosuppression [22]. Similarly, in chronic inflammatory and autoimmune conditions, specific M2 subsets contribute to pathology resolution or progression. For researchers employing flow cytometry to study macrophage polarization, recognizing the complexity beyond the M1/M2 paradigm is essential for accurate experimental design and data interpretation. This article provides a comprehensive resource for distinguishing these subtypes through their defining characteristics, signaling pathways, and practical methodologies for identification and functional assessment.
Characterization of M2 Subtypes
The M2 macrophage classification extends beyond a uniform anti-inflammatory profile to encompass functionally distinct subsets. The table below summarizes the key inducters, surface markers, and primary functions for each M2 subtype.
Table 1: Characterization of M2 Macrophage Subtypes
| Subtype | Primary Inducers | Characteristic Markers | Secreted Factors | Primary Functions |
|---|---|---|---|---|
| M2a | IL-4, IL-13 [20] [21] | CD206, CD209 [20] | CCL17, CCL18, CCL22, CCL24 [20] | Tissue repair, fibrosis, immunoregulation [20] |
| M2b | Immune complexes (ICs), TLR agonists, IL-1R ligands [20] | --- | High IL-10, low IL-12 [20] | Immunoregulation, Th2 activation |
| M2c | IL-10, glucocorticoids [21] [4] | --- | --- | Phagocytosis, matrix deposition, tissue remodeling |
| M2d | --- | --- | IL-10, VEGF [22] | Angiogenesis, tumor progression |
M2a Macrophages
The M2a subtype, induced by IL-4 and IL-13, represents a primary phenotype associated with Th2-type immune responses [20] [21]. These macrophages are characterized by elevated expression of the scavenger receptor CD206 and the C-type lectin CD209, along with production of chemokines such as CCL17, CCL18, CCL22, and CCL24 [20]. Functionally, M2a macrophages exhibit potent profibrotic activity and play critical roles in wound healing and tissue repair processes [20]. Their polarization is primarily mediated through the IL-4 receptor-STAT6 signaling axis, with additional contributions from the PI3K/Akt pathway and peroxisome proliferator-activated receptor gamma (PPARγ) [20] [4].
M2b Macrophages
M2b macrophages, identified by their unique immunoregulatory profile, are polarized by combined exposure to immune complexes (ICs) and TLR agonists or IL-1 receptor ligands [20]. This subtype is distinguished by a high IL-10 to IL-12 secretion ratio, positioning them as key modulators of immune activation [20]. While sometimes categorized separately as M2b, regulatory macrophages (Mreg) share functional similarities in their ability to control excessive inflammation and support tissue homeostasis [21].
M2c Macrophages
The M2c phenotype, induced by IL-10 and glucocorticoids, specializes in phagocytic clearance of apoptotic cells and tissue remodeling [21] [4]. These macrophages contribute to resolution phases of inflammation through extracellular matrix deposition and suppression of proinflammatory immune responses. The anti-inflammatory effects of IL-10 are mediated through activation of the STAT3 signaling pathway [4].
M2d Macrophages
The M2d subtype, often associated with tumor-promoting functions, is stimulated by factors that induce the production of IL-10 and vascular endothelial growth factor (VEGF) [22]. These macrophages promote angiogenesis and create an immunosuppressive microenvironment conducive to tumor progression [22]. In cancer contexts, M2d macrophages represent a significant component of tumor-associated macrophages (TAMs) that correlate with poor clinical outcomes.
Signaling Pathways Regulating M2 Polarization
The polarization of macrophages toward M2 subtypes is governed by distinct yet interconnected signaling pathways. The following diagram illustrates the core signaling networks for the M2a, M2b, and M2c subtypes.
Diagram Title: Core Signaling Pathways in M2 Macrophage Polarization
The diagram above illustrates the principal signaling cascades driving M2 macrophage polarization. For M2a macrophages, IL-4 and IL-13 binding to the IL-4 receptor activates JAK-STAT6 signaling, alongside IRS-PI3K/Akt and PPARγ pathways, inducing characteristic M2a gene expression [20] [4]. M2b polarization involves immune complexes, TLR agonists, and IL-1R ligands converging on MyD88 and NF-κB signaling, resulting in a high IL-10/low IL-12 secretory profile [20]. M2c macrophages respond to IL-10 through JAK-STAT3 activation and SOCS3 induction, promoting anti-inflammatory gene expression and phagocytic activity [4].
Flow Cytometry Analysis of M2 Subtypes
Flow cytometry represents a powerful tool for discerning macrophage subsets based on surface and intracellular markers. However, accurate identification requires carefully designed panels and standardized methodologies to overcome technical challenges associated with macrophage analysis.
Comprehensive Marker Panels
The complex nature of macrophage polarization necessitates multiparameter flow cytometry panels capable of distinguishing subtle phenotypic differences. An optimized eleven-color polychromatic panel has been developed to prevent mischaracterization due to stimulus-induced changes in individual markers [23]. This panel incorporates:
- Lineage and Identification Markers: F4/80 for general macrophage identification
- M1-Associated Markers: CD86, MHC Class II, TNF-α
- M2-Associated Markers: CD206, Arginase 1
- Activation and Toll-like Receptors: TLR4, CD14
- Functional Markers: VEGF
This multi-marker approach provides redundant characterization to ensure accurate subset identification even when individual marker expression is altered by inflammatory stimuli [23]. The inclusion of partially redundant markers—where at least one marker remains stable under common inflammatory conditions like LPS exposure—enhances the reliability of polarization assessment [23].
Critical Methodological Considerations
Macrophage analysis by flow cytometry presents unique technical challenges that must be addressed to ensure data integrity and reproducibility:
- Cell Detachment Methods: Enzymatic treatments like trypsin can alter surface marker expression and are generally not recommended. EDTA treatment or manual scraping preserve surface epitopes better, though EDTA may increase cell aggregation [24].
- Gating Strategies: Comprehensive single-cell gating is essential to exclude doublets and aggregates that can skew results. Strategies should include FSC-H vs FSC-W and SSC-H vs SSC-W plots for doublet discrimination, with careful attention to viable cell populations [24].
- Standardized Processing: Consistent sample handling, fixation, and staining protocols minimize technical variability. Inclusion of viability dyes helps exclude apoptotic and necrotic cells from analysis [24].
Table 2: Essential Research Reagents for M2 Macrophage Flow Cytometry
| Reagent Category | Specific Examples | Application Purpose | Technical Notes |
|---|---|---|---|
| Polarizing Cytokines | IL-4, IL-13 (M2a); IL-10 (M2c) [21] | In vitro differentiation | Use research-grade reagents; validate concentrations |
| Flow Antibodies | Anti-F4/80, CD206, CD86, CD14, MHC-II [23] | Surface marker detection | Titrate antibodies; include Fc receptor block |
| Intracellular Staining Reagents | Arginase 1, TNF-α antibodies [23] | Functional marker detection | Requires cell permeabilization |
| Cell Line Models | RAW 264.7 (mouse) [23] [24] | In vitro screening | Validate findings with primary cells |
| Cell Processing Reagents | EDTA solution [24] | Gentle cell detachment | Preferred over trypsin for surface marker preservation |
Experimental Protocols
In Vitro M2 Macrophage Polarization
This protocol details the generation of M2 macrophage subsets from human monocytic cell lines for subsequent flow cytometric analysis.
Cell Culture and Differentiation:
- Culture THP-1 cells in RPMI-1640 medium supplemented with 10% fetal bovine serum (FBS).
- Differentiate THP-1 monocytes into macrophages using 100 ng/mL Phorbol 12-myristate 13-acetate (PMA) for 24-48 hours [25].
- Replace with fresh complete medium and rest cells for 24 hours before polarization.
M2 Polarization Conditions:
Validation of Polarization:
- Confirm polarization status by measuring TNF-α secretion (typically low in M2 subsets) via ELISA [23].
- Analyze characteristic marker expression by flow cytometry or RT-PCR before proceeding to experimental assays.
Flow Cytometry Staining and Acquisition
This protocol ensures reproducible staining and acquisition for macrophage polarization analysis.
Cell Harvesting:
- Use EDTA solution (recommended concentration: 2-5 mM) for cell detachment to preserve surface epitopes [24].
- Alternatively, employ careful manual scraping if EDTA significantly affects marker expression.
- Wash cells with cold FACS buffer (PBS with 1-2% FBS).
Surface Staining:
- Resuspend cells in FACS buffer containing Fc receptor blocking antibody.
- Aliquot cells and add fluorochrome-conjugated antibodies against target surface markers (e.g., CD206, CD86, MHC-II).
- Incubate for 30 minutes at 4°C protected from light.
- Wash twice with cold FACS buffer.
Intracellular Staining (if required):
- Fix cells with 4% paraformaldehyde for 10-15 minutes at room temperature.
- Permeabilize cells using ice-cold methanol or commercial permeabilization buffers.
- Incubate with intracellular antibodies (e.g., Arginase 1, TNF-α) for 30-60 minutes at 4°C.
- Wash twice with permeabilization buffer, then resuspend in FACS buffer.
Data Acquisition:
- Pass cells through a cell strainer to remove aggregates.
- Acquire data on a flow cytometer capable of detecting all fluorochromes in the panel.
- Include single-stained controls for compensation and fluorescence minus one (FMO) controls for gate setting.
Data Analysis and Gating Strategy
The workflow below outlines a systematic approach for analyzing macrophage polarization data, emphasizing the critical steps to ensure accurate subset identification.
Diagram Title: Macrophage Flow Cytometry Data Analysis Workflow
Functional Significance in Disease and Therapy
The specialized functions of M2 subtypes have profound implications in various pathological contexts, particularly in cancer, autoimmune disorders, and tissue repair processes.
Tumor-Associated Macrophages (TAMs)
M2-like TAMs, particularly the M2d subtype, play multifaceted roles in tumor progression through several mechanisms [22]:
- Angiogenesis Promotion: Secretion of VEGF and other pro-angiogenic factors enhances tumor vascularization [22].
- Immunosuppression: Production of IL-10 and TGF-β inhibits cytotoxic T lymphocyte function while recruiting regulatory T cells via CCL22 [22].
- Metastasis Facilitation: Expression of matrix metalloproteinases (MMPs) remodels the extracellular matrix, enabling tumor cell invasion [22].
- Therapy Resistance: TAMs contribute to resistance against chemotherapy and checkpoint blockade immunotherapy [22].
Spatial distribution analyses reveal that M2-like TAMs predominantly infiltrate hypoxic and stromal regions within tumors, where they establish specialized niches conducive to tumor survival and progression [22]. The density of M2 TAM infiltration often correlates with poor prognosis across multiple cancer types, including breast, lung, and prostate cancers [26] [22].
Therapeutic Targeting Strategies
The functional significance of M2 subtypes has inspired several therapeutic approaches:
- CSF-1R Inhibitors: Target macrophage recruitment and survival by blocking colony-stimulating factor 1 receptor signaling [20] [22].
- CCL2 Antagonists: Disrupt monocyte recruitment to tumors by interfering with the CCL2-CCR2 axis [22].
- Repolarization Strategies: Use nanoparticles, TLR agonists, or metabolic modulators to shift M2-like TAMs toward tumor-suppressive M1 phenotypes [22] [21].
- Genetic Approaches: Employ CRISPR-Cas9 editing to disrupt protumorigenic pathways in TAMs [22].
The refined classification of M2 macrophage subtypes represents a significant advancement beyond the traditional M1/M2 dichotomy, offering deeper insights into their diverse functional roles in health and disease. For researchers applying flow cytometry to macrophage polarization studies, incorporating comprehensive marker panels, standardized methodologies, and appropriate analytical frameworks is essential for accurate subset discrimination. The growing understanding of M2 heterogeneity continues to reveal novel therapeutic opportunities, particularly in oncology, where targeting specific TAM subpopulations holds promise for overcoming treatment resistance. As single-cell technologies further elucidate macrophage plasticity, the integration of these findings with robust phenotypic analysis will continue to drive both basic research and translational applications.
Macrophages are versatile cells of the immune system that play an indispensable role in both advancing and resolving inflammation. Their remarkable plasticity allows them to adopt diverse functional phenotypes in response to environmental signals. The classification of macrophages into classically activated (M1) and alternatively activated (M2) phenotypes provides a foundational framework for understanding macrophage biology in health and disease. M1 macrophages, typically induced by interferon-gamma (IFN-γ) and lipopolysaccharide (LPS), exhibit pro-inflammatory, microbicidal, and anti-tumor functions. In contrast, M2 macrophages, polarized by interleukin-4 (IL-4) and interleukin-13 (IL-13), display immunoregulatory, pro-reparative, and pro-angiogenic activities. This application note details standardized protocols for inducing and validating these polarization states, with particular emphasis on analysis through flow cytometry, to ensure reproducible and accurate research outcomes.
Polarization Inducers and Signaling Pathways
Standard Polarization Stimuli
The induction of macrophage polarization relies on specific cytokine combinations that trigger distinct intracellular signaling cascades, leading to defined transcriptional and functional programs. The table below summarizes the core inducers and their primary effects.
Table 1: Standard Macrophage Polarization Inducers and Key Markers
| Phenotype | Standard Inducers | Primary Signaling Pathway | Characteristic Surface Markers | Functional Role |
|---|---|---|---|---|
| M1 | IFN-γ + LPS | STAT1, IRF activation [27] | CD86, CD80, MHC Class II [27] [28] | Pro-inflammatory, microbicidal, anti-tumor [12] |
| M2 | IL-4 / IL-13 | STAT6, STAT3 activation [27] [29] | CD206, CD163, Arginase-1 [27] [29] [12] | Immunoregulatory, tissue repair, pro-angiogenic [12] |
Signaling Pathway Diagrams
The following diagrams illustrate the core signaling pathways involved in M1 and M2 macrophage polarization.
Diagram 1: M1 Polarization Signaling Pathway. Stimulation with IFN-γ and LPS activates the STAT1 and IRF pathways, leading to the expression of characteristic surface markers and a pro-inflammatory phenotype [27].
Diagram 2: M2 Polarization Signaling Pathway. Stimulation with IL-4 and/or IL-13 engages the Type II receptor, leading to activation of STAT6 and STAT3, which drive the expression of canonical M2 markers and a reparative phenotype [27] [29].
Detailed Experimental Protocols
Protocol 1: Polarization of Human Monocyte-Derived Macrophages
This protocol is adapted from studies utilizing human primary cells and is suitable for investigating human-specific macrophage biology [29] [28].
Key Reagent Solutions:
- Monocyte Isolation: Human pan monocyte isolation kit.
- Differentiation Medium: RPMI 1640 GlutaMAX, supplemented with 10% FBS, 1% penicillin/streptomycin, 1 mM sodium pyruvate, 1x Non-Essential Amino Acids, and 50 ng/mL M-CSF.
- Polarization Cytokines: Recombinant human IFN-γ, LPS, IL-4, and IL-13.
Procedure:
- Monocyte Isolation: Isolate primary human monocytes from buffy coats or PBMCs using a human pan monocyte isolation kit according to the manufacturer's instructions. Monocyte purity of at least 85% (CD14+/CD16+) is recommended [29].
- Macrophage Differentiation: Seed isolated monocytes at a density of 2x10ⶠcells/well in 6-well plates. Differentiate them into macrophages by culturing for 7 days in complete differentiation medium. Replace the medium every 2-3 days [29].
- Macrophage Polarization:
- Harvesting and Analysis: After the polarization period, detach cells using a gentle cell dissociation reagent. Harvest cells and proceed with flow cytometric analysis or other downstream applications.
Protocol 2: Polarization of Mouse Bone Marrow-Derived Macrophages (BMDMs)
This protocol is widely used in murine models and provides a robust system for studying macrophage polarization in vitro [27].
Key Reagent Solutions:
- Differentiation Medium: DMEM or RPMI 1640, supplemented with 10-20% FBS, 1% penicillin/streptomycin, and 20-30% L929-conditioned medium (as a source of M-CSF) or recombinant M-CSF.
- Polarization Cytokines: Recombinant mouse IFN-γ, LPS, IL-4, and IL-13.
Procedure:
- Bone Marrow Cell Isolation: Flush bone marrow cells from the femurs and tibiae of mice. Lyse red blood cells using an appropriate lysis buffer.
- BMDM Differentiation: Seed the bone marrow cells and culture them for 5-7 days in complete differentiation medium. Replace the medium on day 3 or 4.
- Macrophage Polarization:
- Harvesting and Analysis: Scrape or gently detach the adherent BMDMs. Harvest cells and proceed with flow cytometric analysis.
Table 2: Quantitative Stimulus Ranges for Murine BMDM Polarization [27]
| Phenotype | Stimulus | Common Concentration Range | Key Marker Expression (Example) |
|---|---|---|---|
| M1 | LPS / IFN-γ | 0.1 - 0.3 ng/mL (low) to 100 ng/mL (saturating) | CD86: Tenfold increase with 0.3 ng/mL LPS/IFN-γ [27] |
| M2 | IL-4 / IL-13 | 0.1 - 1 ng/mL (low) to 50 ng/mL (saturating) | CD206: Threefold increase with 1 ng/mL IL-4/IL-13 [27] |
Flow Cytometry Analysis of Polarization
Panel Design and Gating Strategy
Flow cytometry is the gold standard for validating macrophage polarization states. A well-designed multicolor panel is critical for accurately identifying phenotypes, especially given the plasticity and potential for mixed phenotypes.
Essential Markers for a Comprehensive Panel: An optimized panel should include markers for positive identification of macrophages and for distinguishing M1 and M2 states. Using partially redundant markers guards against stimulus-induced changes in individual markers [14].
Table 3: Essential Markers for Macrophage Polarization Flow Cytometry Panels
| Target | Phenotype Association | Function / Note | Recommendation |
|---|---|---|---|
| F4/80 | Pan-macrophage (mouse) | Adhesion glycoprotein; expression can vary with polarization [14] | Essential for mouse models |
| CD68 | Pan-macrophage (human) | Scavenger receptor protein | Essential for human models [12] |
| CD86 | M1 | Co-stimulatory molecule | Core M1 marker [27] [12] |
| MHC Class II | M1 | Antigen presentation | Core M1 marker [12] [14] |
| CD206 | M2 | Mannose receptor | Core M2 marker [27] [12] |
| CD163 | M2 | Scavenger receptor | M2 marker [12] |
| Arginase-1 | M2 | Intracellular enzyme | M2 marker (intracellular staining) [14] |
Gating Strategy:
- Singlets: Use FSC-H vs FSC-A to exclude cell doublets.
- Live Cells: Use a viability dye (e.g., Zombie Aqua) to exclude dead cells.
- Macrophage Population: Gate on F4/80⺠(mouse) or CD68⺠(human) cells.
- Phenotype Identification: Analyze the expression of M1 (e.g., CD86, MHC II) and M2 (e.g., CD206, CD163) markers on the macrophage population. Visualization in a biaxial plot (CD86 vs CD206) is highly informative [27].
Critical Considerations and Validation
- Phenotype Continuum and Plasticity: Macrophages exposed to combined M1 and M2 signals can acquire a mixed activation state, with individual cells co-expressing both CD86 and CD206, rather than polarizing to discrete phenotypes [27]. Phenotypic markers also evolve with time; for instance, co-stimulated macrophages may lose CD86 and increase CD206 expression over several days [27].
- Functional Validation: Surface marker analysis should be complemented with functional assays to confirm polarization.
- M1 Validation: Measure pro-inflammatory cytokine secretion (e.g., TNF-α, IL-12) in cell supernatant via ELISA. M1 polarization with IFN-γ + LPS potently boosts TNF-α production [14].
- M2 Validation: Measure the expression of genes associated with M2 polarization, such as ARG1 and MRC1 (encodes CD206), via RT-qPCR [28].
Advanced Concepts and Applications
Complex Polarization Dynamics
Research has moved beyond simple M1/M2 dichotomies. Key advanced concepts include:
- Sequential Polarization: Cellular history impacts response. Exposure to LPS/IFN-γ potentiates the subsequent response to IL-4/IL-13, whereas pre-polarization with IL-4/IL-13 can inhibit the response to LPS/IFN-γ [27].
- Metabolic Reprogramming: M1 and M2 polarization are underpinned by distinct metabolic states. M1 macrophages favor glycolysis, while M2 macrophages upregulate oxidative phosphorylation (OXPHOS) [30]. Counterintuitively, IL-4/IL-13 pre-activation can induce a form of innate training that enhances pro-inflammatory responses to a secondary mycobacterial challenge, a state that retains heightened OXPHOS rather than switching to glycolysis [30].
- IL-4 vs. IL-13 Specificity: While IL-4 and IL-13 induce highly overlapping M2 marker expression with equivalent potency in human macrophages [29], subtle differences exist. IL-4 can enhance reactive oxygen species (ROS) generation more potently than IL-13, and differential receptor usage (IL-4 can signal through both Type I and Type II receptors, while IL-13 uses only the Type II) may lead to context-specific functional differences [29].
Troubleshooting Guide
Table 4: Common Polarization Issues and Solutions
| Problem | Potential Cause | Suggested Solution |
|---|---|---|
| Weak M1/M2 marker expression | Suboptimal cytokine concentration or duration | Perform a dose-response and time-course experiment. Use concentrations from published literature as a starting point (see Table 2). |
| High variability between replicates | Inconsistent cell seeding density or poor monocyte differentiation | Ensure uniform cell counting and seeding. Verify monocyte purity and health before differentiation. |
| Unexpected marker co-expression | Genuine mixed phenotype | Consider the biological context; mixed phenotypes are common in vivo and with mixed stimuli [27]. Analyze data on single-cell level via flow cytometry. |
| Low cell viability after polarization | Cytotoxicity of stimuli (especially high-dose LPS) | Titrate LPS to find a balance between efficacy and cytotoxicity. Check serum quality and use endotoxin-free reagents. |
Practical Flow Cytometry Panels and Protocols for Reliable Polarization
Deep immunophenotyping via multi-parametric flow cytometry serves as a crucial methodological approach for unraveling the complexity of the immune system in health and disease. This application note provides a detailed framework for designing robust 10-11 color flow cytometry panels, with specific application to the study of macrophage M1/M2 polarization—a critical process in inflammatory responses, tissue repair, and cancer immunotherapy. The standardized protocols outlined herein ensure high data quality and reproducibility, enabling researchers to capture comprehensive immune profiles at single-cell resolution.
Panel Design Fundamentals
Marker Selection Strategy
Effective panel design requires careful consideration of marker expression patterns and biological context. Target antigens generally fall into two categories: lineage markers with known expression patterns used to define major immune populations, and function markers related to cell activation, proliferation, and metabolic states with potentially unknown expression patterns [31].
For macrophage polarization studies, key surface markers include:
When selecting antibody clones, note that different clones against the same target antigen may exhibit distinct staining patterns, necessitating consultation of validated resources such as the Optimized Multicolor Immunofluorescence Panels (OMIPs) collection [31].
Fluorochrome Configuration
Strategic fluorochrome assignment is paramount for panel performance. The general principle is to assign bright fluorochromes (e.g., PE, BV421) to markers with low expression levels or unknown expression patterns, while dim fluorochromes (e.g., FITC, PerCP/Cy5.5) should be reserved for brightly expressed lineage markers [31].
Table 1: Fluorochrome Brightness Classification
| Brightness Category | Example Fluorochromes | Recommended Application |
|---|---|---|
| Bright | PE, BV421 | Low-abundance functional markers (e.g., cytokine receptors) |
| Medium | APC, PE/Cy7 | Moderately expressed markers |
| Dim | FITC, PerCP/Cy5.5 | Bright lineage markers (e.g., CD45, CD3) |
Comprehensive 11-Color Panel for Macrophage Studies
Panel Configuration
This optimized 11-color panel enables deep immunophenotyping of macrophage populations and their polarization states, adapted from standardized methodologies [33] [31].
Table 2: 11-Color Macrophage Immunophenotyping Panel
| Marker | Fluorochrome | Expression Profile | Primary Function in Panel |
|---|---|---|---|
| CD45 | PerCP/Cy5.5 | Pan-hematopoietic | Leukocyte identification |
| CD11b | BV510 | Myeloid cells | Myeloid lineage gate |
| F4/80 | PE/Cy7 | Macrophages | Macrophage identification |
| CD86 | BV421 | M1-associated | Pro-inflammatory phenotype |
| CD206 | PE | M2-associated | Anti-inflammatory phenotype |
| CD64 | APC | M1-associated | Fcγ receptor signaling |
| HLA-DR | BV605 | Antigen-presenting cells | Activation status |
| CD14 | FITC | Monocytes/Macrophages | Subset discrimination |
| CD163 | PE/Dazzle594 | M2-associated | Scavenger receptor |
| CD80 | Alexa Fluor 700 | M1-associated | Co-stimulatory marker |
| Live/Dead | Near-IR | N/A | Viability discrimination |
Gating Strategy for Macrophage Polarization
- Singlets: FSC-H vs FSC-A to exclude aggregated cells
- Live cells: Gate on Near-IR negative population
- Leukocytes: CD45+ events
- Myeloid lineage: CD11b+ population
- Macrophages: F4/80+ CD11b+ events
- Polarization states: Concurrent assessment of M1 (CD86+ CD64+ CD80+) and M2 (CD206+ CD163+) markers [32] [9]
Experimental Protocols
Instrument Characterization and Detector Gain Optimization
Proper instrument setup is foundational for reproducible high-dimensional flow cytometry data [31].
Materials
- 8-peaks Rainbow Calibration Particles (RCPs; Spherotech, Cat#RCP-30-5A)
- Anti-Mouse Ig, κ/Negative Control Compensation Particles Set (BD, Cat#552843)
- Flow cytometer with minimum 3-laser configuration (e.g., CytoFLEX LX)
Procedure
- Daily Quality Control: Perform instrument-specific startup and quality control procedures
- Detector Linearity Assessment:
- Vortex RCPs vigorously and add 2-3 drops to 1 mL ddHâ‚‚O
- Adjust FSC/SSC gain to place beads on scale
- Set gains for all fluorescence detectors to 25V (except FSC/SSC)
- Acquire 5,000 events for both RCPs and negative control compensation particles
- Increase gain by 50V for each detector and repeat acquisition
- Export data in FCS3.1 format and calculate median fluorescence intensity (MFI)
- Linearity Calculation:
- Calculate detector linearity as:
(P8_MFI - P7_MFI)/P7_MFIwhere P7 and P8 represent the second brightest and brightest bead peaks, respectively [31]
- Calculate detector linearity as:
- Optimal Gain Determination:
- For each detector, identify the gain point showing the highest signal-to-background ratio co-occurring with the lowest robust coefficient of variance and a slope of zero on the linearity curve
Antibody Titration and Sample Staining
Precise antibody titration ensures optimal staining with minimal background [31].
Reagent Setup
- Stain buffer: PBS with 2% fetal bovine serum (store at 2-8°C for up to 2 weeks)
- 1× Lysing Solution: Dilute 10× concentrate FACS Lysing Solution 1:10 with ddH₂O
- 1% PFA: Dilute 4% PFA 1:4 with PBS for cell fixation
- Antibody premixes: Combine titrated antibodies in 20 μL stain buffer per sample
Staining Protocol for Human Whole Blood or PBMCs
- Sample Preparation:
- Collect fresh human peripheral whole blood in heparin or EDTA tubes
- Isolate PBMCs using density gradient centrifugation if required
- Cell Staining:
- Aliquot 100 μL whole blood or 1-2×10ⶠPBMCs per test
- Add antibody cocktail and incubate 30 minutes at 4°C in the dark
- Add 2 mL 1× Lysing Solution, incubate 10 minutes at RT
- Centrifuge at 500× g for 5 minutes, discard supernatant
- Wash twice with 2 mL stain buffer
- Resuspend cells in 200-300 μL 1% PFA for fixation
- Data Acquisition:
- Acquire samples on calibrated flow cytometer within 24 hours
- Collect minimum 100,000 events per sample for rare population detection
Spectral Flow Cytometry Considerations
For spectral flow cytometry systems (e.g., Cytek Aurora):
- Include cell-based or bead-based single-color controls for optimal unmixing
- Add Brilliant Stain Buffer to mitigate polymer dye-dye interactions [34]
- Use blocking reagents such as CellBlox Blocking Buffer to reduce non-specific cell binding [34]
Advanced Applications in Macrophage Polarization Research
Integration with Functional Assays
Complement surface marker analysis with functional assessments for comprehensive macrophage characterization:
Metabolic Profiling:
Cytokine Production:
Phagocytic Capacity:
- Assess using pH-sensitive probes or fluorescent beads [36]
Autofluorescence as a Metabolic Indicator
Autofluorescence flow cytometry enables label-free assessment of macrophage metabolic states based on intrinsic fluorescence of NADH and FAD [35]. This approach reveals that:
- M1 polarization induces a red shift in autofluorescence spectra, indicating membrane depolarization [32]
- M2 polarization shows a blue shift (hyperpolarization) [32]
- Autofluorescence profiles can distinguish atherosclerosis patients from healthy controls with high accuracy (ROC-AUC: 0.84 ± 0.09) [35]
Research Reagent Solutions
Table 3: Essential Reagents for Deep Immunophenotyping
| Reagent/Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| Flow Cytometry Instruments | CytoFLEX LX, Cytek Aurora (5-laser) | Sample acquisition | Cytek Aurora enables high-parameter spectral cytometry [34] |
| Validation Particles | 8-peaks RCPs (Spherotech), Negative Control Compensation Particles (BD) | Instrument calibration, compensation controls | Essential for standardized protocol implementation [31] |
| Cell Processing Reagents | FACS Lysing Solution (BD), Brilliant Stain Buffer (BD) | Red blood cell lysis, reducing dye interactions | Critical for whole blood processing and polymer dye performance [34] |
| Viability Markers | Near-IR fixable viability dyes | Exclusion of dead cells | Improves data quality by reducing non-specific binding |
| Data Analysis Software | FlowJo v10.8.1, Cytek SpectroFlo | Data analysis, spectral unmixing | FlowJo is industry standard for conventional flow data [31] [34] |
Workflow Visualization
Diagram 1: Comprehensive immunophenotyping workflow from panel design to data analysis.
Troubleshooting and Quality Assurance
Spillover Spreading Minimization
Spillover spreading error significantly impacts high-dimensional panel sensitivity [31]. Mitigation strategies include:
- Assign weak markers to channels receiving less spread
- Place backbone markers in channels contributing less spread
- Regularly consult spillover spreading matrices for your specific instrument configuration
Data Reproducibility Measures
- Standardized Protocols: Implement identical procedures across experiments
- Longitudinal Monitoring: Include control samples for batch-to-batch normalization
- Reference Samples: Use preserved patient samples or calibration beads for instrument performance tracking
The standardized 10-11 color flow cytometry panels detailed in this application note provide a robust framework for deep immunophenotyping with specific utility in macrophage polarization research. By adhering to these meticulously optimized protocols—encompassing instrument calibration, reagent validation, and systematic gating strategies—researchers can generate high-quality, reproducible data that advances our understanding of macrophage biology in health and disease. The integration of surface marker analysis with functional metabolic assessments through autofluorescence and cytokine profiling offers a comprehensive approach to elucidating the dynamic nature of macrophage polarization in various pathological contexts.
Macrophages are versatile immune cells that play a central role in innate and adaptive immunity, wound repair, and tissue remodeling. Their remarkable functional plasticity allows them to adopt different activation states, or phenotypes, in response to specific microenvironmental cues. The classical M1/M2 paradigm represents a simplified but useful framework for understanding macrophage polarization, where M1 macrophages exhibit pro-inflammatory, antimicrobial functions, while M2 macrophages demonstrate immunoregulatory and tissue-repair capabilities [23] [12]. The characterization of these phenotypes is particularly relevant in cancer immunology, where tumor-associated macrophages (TAMs) often exhibit M2-like properties that support tumor progression and suppress anti-tumor immunity [12] [28].
Flow cytometry has emerged as a powerful tool for discriminating macrophage phenotypes due to its ability to simultaneously measure multiple surface and intracellular markers at the single-cell level. However, accurate classification requires carefully optimized panels that account for the spectrum of activation states and potential marker co-expression [12]. This protocol provides a detailed methodology for polarizing human monocyte-derived macrophages and analyzing their phenotypes using multicolor flow cytometry, framed within the broader context of macrophage biology research and its applications in therapeutic development.
Materials and Reagents
Research Reagent Solutions
Table 1: Essential reagents for human monocyte-derived macrophage culture and polarization
| Reagent Category | Specific Examples | Function/Purpose |
|---|---|---|
| Cell Isolation | Anti-human CD14 magnetic beads, Lympholyte-H density gradient medium | Isolation of monocytes from peripheral blood mononuclear cells (PBMCs) |
| Culture Media | RPMI 1640, Fetal Bovine Serum (FBS), Human Serum, Penicillin/Streptomycin, L-glutamine | Maintenance and growth of macrophages |
| Differentiation Factor | Macrophage Colony-Stimulating Factor (M-CSF/CSF-1) | Drives monocyte-to-macrophage differentiation |
| Polarizing Cytokines | IFN-γ, IL-4, IL-10, IL-13 | Induce specific macrophage activation states |
| Polarizing Agents | Lipopolysaccharides (LPS) | Synergizes with IFN-γ for M1 polarization |
| Flow Cytometry Antibodies | Anti-CD68, CD80, CD86, CD40, CD64, CD163, CD206, MHC Class II, Arginase-1 | Detection of macrophage surface and intracellular markers |
Equipment
- Biological safety cabinet
- CO₂ incubator (37°C, 5% CO₂)
- Centrifuge
- Flow cytometer with multiple laser configurations (capable of detecting at least 11 colors)
- Brightfield microscope
- Hemocytometer or automated cell counter
Methodology
Monocyte Isolation and Macrophage Differentiation
- PBMC Isolation: Collect peripheral blood from healthy donors following appropriate ethical guidelines and informed consent [28]. Isolate PBMCs using density gradient centrifugation with Lympholyte-H or similar medium.
- CD14⺠Monocyte Separation: Purify monocytes from PBMCs using magnetic-activated cell sorting (MACS) with anti-human CD14-conjugated magnetic beads according to manufacturer's instructions [28] [37].
- Macrophage Differentiation: Culture sorted CD14⺠monocytes (at 1×10ⵠcells/mL) in complete RPMI 1640 medium supplemented with 10% FBS, 5% human serum, antibiotics, and 25 ng/mL M-CSF for 6 days to generate non-polarized (M0) macrophages [28]. Refresh media with M-CSF every 2-3 days.
Macrophage Polarization
After 6 days of differentiation, polarize M0 macrophages using the following cytokine conditions:
- M1 Polarization: Treat M0 macrophages with IFN-γ (10 ng/mL) plus LPS (100 ng/mL) for 48 hours [28].
- M2a Polarization: Treat M0 macrophages with IL-4 (20 ng/mL) for 48 hours [28].
- M2c Polarization: Treat M0 macrophages with IL-10 (20 ng/mL) for 48 hours [23].
- Tumor-Associated Macrophage (TAM) Model: As an alternative approach, polarize monocytes using tumor cell-conditioned media to generate TAM-like cells [37].
Figure 1: Experimental workflow for macrophage differentiation and polarization.
Flow Cytometry Panel Design and Staining
Based on recent optimization studies [23], the following eleven-color panel provides comprehensive characterization of macrophage phenotypes:
Table 2: Optimized flow cytometry panel for human macrophage phenotyping
| Marker | Specificity | Polarization Association | Function/Biological Significance |
|---|---|---|---|
| CD68 | Macrophage lineage | Pan-macrophage | Lysosomal marker, identifies macrophagic lineage |
| CD80/CD86 | Co-stimulatory molecules | M1 [12] | T-cell activation, antigen presentation capability |
| CD64 | FcγRI | M1 [32] | High-affinity IgG receptor, pro-inflammatory function |
| MHC Class II | Antigen presentation | M1 [23] [12] | Antigen presentation capability |
| CD163 | Scavenger receptor | M2 [12] | Hemoglobin scavenger, anti-inflammatory function |
| CD206 | Mannose receptor | M2 [12] [28] [32] | Pattern recognition receptor, endocytosis |
| CD40 | Co-stimulatory molecule | M1/M2 [12] | Activation marker, context-dependent expression |
| Arginase-1 | Metabolic enzyme | M2 [23] [12] | Ornithine pathway, associated with tissue repair |
| TNF-α | Pro-inflammatory cytokine | M1 [23] | Key inflammatory mediator |
Staining Procedure:
- Harvesting: Gently scrape polarized macrophages and transfer to flow cytometry tubes. Centrifuge at 300 × g for 5 minutes and discard supernatant.
- Surface Staining: Resuspend cell pellets in 100 μL FACS buffer (PBS + 2% FBS) containing optimally titrated fluorochrome-conjugated antibodies against surface markers (CD80, CD86, CD64, CD163, CD206, CD40, MHC Class II). Incubate for 30 minutes at 4°C in the dark.
- Intracellular Staining (if required):
- Fix cells with 4% paraformaldehyde for 10 minutes at room temperature.
- Permeabilize with 0.1% Triton X-100 or commercial permeabilization buffer.
- Incubate with intracellular antibodies (CD68, Arginase-1, TNF-α) for 30 minutes at 4°C in the dark.
- Washing and Acquisition: Wash cells twice with FACS buffer, resuspend in 200-300 μL FACS buffer, and acquire data on a flow cytometer within 24 hours. Include appropriate single-stained controls for compensation.
Quality Control and Validation
- Polarization Verification: Validate polarization states by measuring TNF-α concentration in cell supernatants using ELISA for M1 macrophages [23].
- Alternative Validation Methods:
Expected Results and Data Interpretation
Marker Expression Patterns
Table 3: Expected expression patterns of key markers across polarization states
| Marker | M1 (IFN-γ + LPS) | M2a (IL-4) | M2c (IL-10) |
|---|---|---|---|
| CD80/CD86 | High [12] | Low/Moderate [12] | Low/Moderate [12] |
| CD64 | High [32] | Low | Low |
| MHC Class II | High [23] [12] | Low/Moderate | Low |
| CD163 | Low | High [12] | High [12] |
| CD206 | Low | High [12] [28] [32] | Moderate |
| CD40 | High [12] | Moderate [12] | Moderate [12] |
| Arginase-1 | Low | High [23] [12] | High [23] |
| TNF-α | High [23] | Low | Low |
Figure 2: Characteristic marker expression patterns for M1 and M2 polarized macrophages.
Data Analysis Guidelines
- Gating Strategy: Begin by gating on single cells using FSC-A/FSC-H, then identify macrophages using CD68 expression. Subsequent analysis should evaluate combination marker expression rather than relying on single markers.
- Multidimensional Analysis: Utilize t-SNE, UMAP, or FlowSOM algorithms to visualize high-dimensional data and identify potential subpopulations.
- Phenotype Assignment: Assign M1 or M2 phenotypes based on composite profiles rather than individual markers. Recognize that macrophages may exist on a spectrum with intermediate phenotypes.
Technical Considerations and Troubleshooting
- Marker Redundancy: The included partially redundant markers (e.g., multiple M1 and M2 markers) prevent misclassification due to stimulus-induced changes in individual markers [23].
- Activation State Stability: Be aware that macrophage phenotypes are plastic and may shift during handling. Process samples promptly after harvesting.
- Species Considerations: This protocol is optimized for human macrophages. Murine macrophages may require different markers (e.g., CD38, Egr2) [38].
- Tumor Microenvironment Modeling: For TAM studies, consider validating findings using tumor-conditioned media polarization models [37].
Applications in Research and Drug Development
This standardized protocol enables:
- Tumor Immunophenotyping: Characterize macrophage populations in patient-derived samples, potentially identifying prognostic biomarkers [12].
- Therapeutic Screening: Evaluate candidate immunotherapies designed to modulate macrophage polarization (e.g., TAM-repolarizing agents).
- Mechanistic Studies: Investigate signaling pathways and metabolic programs underlying macrophage plasticity.
- Personalized Medicine: Assess individual variations in macrophage responses that may influence treatment outcomes.
The comprehensive flow cytometry panel presented here provides researchers with a robust toolset for delineating human macrophage phenotypes, advancing our understanding of their role in health and disease, and facilitating the development of macrophage-targeted therapeutics.
Bone marrow-derived macrophages (BMDMs) are primary macrophage cells differentiated in vitro from mouse bone marrow progenitor cells. They represent a essential tool in immunological research, providing a homogeneous population of naïve macrophages that closely mimic in vivo biology without the activation state variations often encountered in tissue-resident macrophages [39] [40]. Within the context of macrophage polarization research, BMDMs serve as a robust platform for investigating the molecular mechanisms driving M1 (pro-inflammatory) and M2 (anti-inflammatory) polarization, a critical process in immunity, homeostasis, and disease pathogenesis [41] [42]. The reliability and scalability of BMDM cultures make them particularly valuable for flow cytometry-based phenotyping, enabling quantitative assessment of polarization states at the single-cell level.
Generation of Bone Marrow-Derived Macrophages
Principle
This protocol establishes a method for generating mature macrophages through the in vitro differentiation of bone marrow hematopoietic stem and progenitor cells, using L929-cell conditioned medium (LCCM) as a source of Macrophage Colony-Stimulating Factor (M-CSF) [39] [40]. The procedure can be performed using either fresh or cryopreserved bone marrow cells, offering significant operational flexibility [39].
Materials and Reagents
- Mice: C57BL/6 mice, 6-12 weeks old [39]
- Dissection Tools: Sterile scissors and forceps
- Basal Medium: RPMI 1640 [39] [40]
- Complete Differentiation Medium (R20/30): RPMI 1640 supplemented with 20% Fetal Bovine Serum (FBS), 30% LCCM, 100 U/mL penicillin, 100 µg/mL streptomycin, and 2 mM L-glutamine [39]
- Freezing Medium: 90% FBS + 10% DMSO [39]
- LCCM Preparation: Supernatant from L929 cells cultured for 7-10 days, filtered (0.45 µm), and stored at -20°C [40]
Protocol
Harvesting of Bone Marrow Cells
- Euthanize 6-12 week old mouse following institutional animal care guidelines [39].
- Dissect femurs and tibias, removing adjacent muscle tissue thoroughly [40].
- Sterilize bones in 70% ethanol for 1 minute, followed by a wash in sterile RPMI 1640 [39].
- Remove both epiphyses using sterile scissors [39].
- Flush marrow cavity with RPMI 1640 using a syringe (25-27 gauge) into a sterile collection tube [40].
- Prepare single-cell suspension by gently pipetting or passing through a 70 µm cell strainer. Centrifuge at 200× g for 5 minutes at 4°C [39] [40].
- Resuspend cell pellet in appropriate medium for counting and subsequent culture or cryopreservation.
Optional: Cryopreservation of Bone Marrow Cells
- Resuspend fresh bone marrow cells at 4-6×10^6 cells/mL in freezing medium (90% FBS, 10% DMSO) [39].
- Aliquot 1 mL per cryovial and place at -80°C for 24 hours in a freezing container.
- Transfer vials to liquid nitrogen for long-term storage.
- To thaw: Rapidly warm cryovial in 37°C water bath, transfer cells to pre-warmed PBS, centrifuge at 200× g for 5 minutes, and resuspend in differentiation medium [39].
In Vitro Differentiation to Macrophages
- Seed bone marrow cells in non-tissue culture treated Petri dishes or plates at appropriate density (e.g., 1×10^6 cells/mL) in R20/30 differentiation medium [39].
- Incubate at 37°C in a 5% CO2 atmosphere for 4 days [39].
- Add an equal volume of fresh R20/30 medium on day 4 without removing the original medium [39].
- Continue incubation for an additional 3 days. By day 7, a confluent layer of adherent, mature BMDMs should be visible [39] [40].
- Harvest BMDMs by discarding supernatant, washing with sterile PBS, and incubating with ice-cold PBS for 10 minutes at 4°C. Gently pipette across the dish surface to detach cells [39].
- Count cells and resuspend in appropriate medium for subsequent experiments.
Macrophage Polarization
Polarization Protocol
- Seed harvested BMDMs in tissue culture-treated plates at desired density (e.g., 1×10^6 cells/well) in cultivation medium (R10/5: RPMI 1640, 10% FBS, 5% LCCM, 2 mM L-glutamine) [39].
- Allow cells to adhere for 12 hours before polarization [39].
- Stimulate with polarization cytokines for 24-48 hours [41] [42]:
- Harvest polarized macrophages for downstream analysis by flow cytometry.
Key Signaling Pathways in Macrophage Polarization
The molecular mechanisms driving macrophage polarization involve distinct signaling pathways and metabolic reprogramming. Quantitative proteomic and phosphoproteomic analyses have revealed that M1 and M2 polarization are controlled by specific signaling networks [43].
Flow Cytometry Analysis of Polarized Macrophages
Sample Preparation
- Harvest polarized macrophages using PBS containing 2 mM EDTA or gentle cell scraping [41].
- Wash cells twice with FACS buffer (PBS + 2% BSA) [41].
- Stain with viability dye (e.g., DAPI or Zombie Aqua) for 30 minutes at 4°C to exclude dead cells [41].
- Block Fc receptors using anti-CD16/32 antibody for 20 minutes at 4°C to reduce nonspecific binding [41].
- Stain with fluorophore-conjugated antibodies for 30 minutes at 4°C in the dark [41].
- Wash cells twice with FACS buffer and resuspend in fixation buffer if not acquiring immediately [41].
- Acquire data on flow cytometer and analyze using appropriate software (e.g., FlowJo) [41].
Marker Expression in Polarized Macrophages
The table below summarizes key surface and intracellular markers for identifying M1 and M2 polarized macrophages:
Table 1: Characteristic Markers of Polarized Macrophages
| Marker | M1 Expression | M2 Expression | Function | Reference |
|---|---|---|---|---|
| CD80 | Increased [41] | Low/Negative | Co-stimulatory molecule for T cell activation | [41] |
| CD86 | Increased [41] | Low/Negative | Co-stimulatory molecule for T cell activation | [41] |
| MHC-II | High | Variable | Antigen presentation | [40] |
| CD206 | Low/Negative | Increased [41] [44] | Mannose receptor, phagocytosis | [41] [44] |
| CD300A | Not Reported | Specific Expression [41] | Immunoregulatory receptor | [41] |
| LILRB2 | Not Reported | Specific Expression [41] | Immunoregulatory receptor | [41] |
| Siglec-10 | Not Reported | Specific Expression [41] | Immunoregulatory receptor | [41] |
| CD109 | Not Reported | Specific Expression [41] | GPI-anchored protein | [41] |
| iNOS | High [42] | Low/Negative | Nitric oxide production | [42] |
| Arg1 | Low/Negative | High [42] | Arginine metabolism | [42] |
Advanced Analytical Approaches
Autofluorescence Flow Cytometry
Recent advances in multispectral flow cytometry enable analysis of macrophage polarization through autofluorescence (AF) profiles without extrinsic labels. Macrophage AF signatures change significantly under M1/M2 polarization and stress conditions, primarily reflecting alterations in metabolic cofactors (NADH and FAD) [35]. This label-free approach can distinguish immune states in clinical samples, with leukocyte AF profiles discriminating atherosclerosis patients from healthy controls (ROC-AUC: 0.84 ± 0.09) when combined with advanced predictive models [35].
Transcriptional Plasticity Assessment
Trajectory analysis of time-course transcriptomic data demonstrates that polarized macrophages exhibit remarkable plasticity. When polarizing cytokines are removed, macrophages largely revert to a baseline (M0) state within 72 hours [42]. Furthermore, macrophages completely repolarize when switched between M1 and M2 conditions, adopting phenotypes dictated by their current microenvironment with minimal memory of prior polarization states [42].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagent Solutions for BMDM Generation and Polarization
| Reagent Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| Growth/Polarization Cytokines | M-CSF (100 ng/mL) [41] | Drives macrophage differentiation from progenitors | Source: Recombinant protein or L929-cell conditioned medium [39] |
| IFN-γ (50 ng/mL) [41] | M1 polarization signal | Synergizes with TLR agonists like LPS [41] [42] | |
| IL-4 (20 ng/mL) [41] | M2 polarization signal | Canonical alternative activation stimulus [41] [42] | |
| Cell Culture Media | RPMI 1640 [39] | Basal culture medium | Supports hematopoietic cell growth |
| X-VIVO15 [41] | Serum-free medium | Used for defined culture conditions | |
| Flow Cytometry Antibodies | Anti-CD80 [41] | M1 marker detection | Co-stimulatory molecule |
| Anti-CD86 [41] | M1 marker detection | Co-stimulatory molecule | |
| Anti-CD206 [41] [44] | M2 marker detection | Mannose receptor | |
| Anti-CD300A [41] | M2-associated marker | Novel M2 marker identified by proteomics [41] | |
| Specialized Reagents | LCCM [39] | Source of M-CSF | 20-30% concentration for differentiation [39] |
| LPS [41] [42] | TLR4 agonist | Used at 10-100 ng/mL for M1 polarization [41] [42] | |
| Grp78-IN-1 | Grp78-IN-1, MF:C21H23FO3, MW:342.4 g/mol | Chemical Reagent | Bench Chemicals |
| Dulcite-13C-1 | Dulcite-13C-1, MF:C6H14O6, MW:183.16 g/mol | Chemical Reagent | Bench Chemicals |
Functional Validation of Polarized Macrophages
Phagocytosis Assay
- Wash polarized macrophages twice with PBS and add serum-free RPMI medium [41].
- Add FITC-conjugated Zymosan A particles (5 particles per cell) and incubate at 37°C for 1 hour [41].
- Wash with PBS and add trypan blue (250 µg/mL) to quench extracellular fluorescence [41].
- Analyze internalized fluorescence by flow cytometry or fluorescence microscopy [41].
Metabolic Profiling
Global proteomic and phosphoproteomic analyses reveal distinct metabolic signatures in polarized macrophages. M1 macrophages typically upregulate glycolytic pathways, while M2 macrophages enhance oxidative phosphorylation and other metabolic pathways including glycosaminoglycan metabolism and retinoic acid signaling [43]. These metabolic differences can be assessed using extracellular flux analyzers to measure glycolytic and mitochondrial respiration rates.
Troubleshooting and Technical Considerations
- Differentiation Efficiency: Ensure LCCM quality and potency through regular quality control testing. Incomplete differentiation may result in heterogeneous cultures with non-adherent cells [40].
- Polarization Specificity: Validate polarization protocols using multiple markers rather than relying on a single identifier, as macrophage activation exists along a spectrum [42] [45].
- Cryopreservation Impact: BMDMs generated from cryopreserved bone marrow cells show similar functional capacity to those from fresh cells, including equivalent expression of CD80 and CD86 in response to LPS and comparable restriction of intracellular pathogens [39].
- Plasticity Considerations: When designing sequential polarization experiments, note that macrophages demonstrate minimal memory of prior polarization states and primarily respond to current environmental cues [42].
This comprehensive protocol provides a foundation for reliable generation, polarization, and flow cytometric analysis of bone marrow-derived macrophages, enabling robust investigation of macrophage biology in health and disease.
Macrophage polarization is a critical process in the immune response, with classically activated (M1) and alternatively activated (M2) macrophages playing distinct and often opposing roles in disease pathogenesis [46]. The M1/M2 balance influences disease progression, therapeutic responses, and patient outcomes in conditions ranging from cancer to infectious and chronic inflammatory diseases [12] [47]. Flow cytometry has emerged as a powerful tool for dissecting macrophage heterogeneity due to its ability to simultaneously measure multiple surface and intracellular markers at single-cell resolution [23] [48]. This application note provides detailed protocols and analytical frameworks for studying macrophage polarization in cancer, tuberculosis, and fibrosis research, supporting the broader thesis that precise immunophenotyping is essential for understanding disease mechanisms and developing targeted therapies.
Macrophage Polarization in Disease Models
Cancer Microenvironment
In the lung cancer microenvironment, tumor-associated macrophages (TAMs) display a complex polarization state that contributes to immunosuppression and tumor progression. Flow cytometric analysis of bronchoalveolar lavage fluid (BALF) from patients with confirmed lung cancer reveals a unique macrophage immunophenotype characterized by bright expression of CD68, CD206, CD163, and CD40, along with positive expression of CD80, CD86, and CD45 [12]. These TAMs frequently express Arginase-1 and exist in a mixed polarization state that differs significantly from macrophages in healthy lung tissue from the same patients [12].
The cytokine profile in the cancerous lung environment shows high concentrations of IL-1RA and IL-6, with complex correlations between pro- and anti-inflammatory cytokines that likely contribute to the immunosuppressive tumor microenvironment [12]. This mixed polarization state represents a potential therapeutic target, as TAMs constitute up to 50% of the tumor mass in solid tumors and significantly influence treatment outcomes [12].
Table 1: Key Macrophage Markers in Lung Cancer Microenvironment
| Marker Category | Specific Markers | Expression in Lung TAMs | Functional Significance |
|---|---|---|---|
| Pan-Macrophage | CD68, CD45 | Bright (CD68), Positive (CD45) | Cell identification and quantification |
| M2-Associated | CD206, CD163, Arginase-1 | Bright (CD206, CD163), Positive (Arginase-1) | Immunosuppression, tissue remodeling |
| Costimulatory | CD80, CD86, CD40 | Positive (CD80, CD86), Bright (CD40) | Antigen presentation, T cell activation |
| Cytokines | IL-1RA, IL-6 | High concentration | Immunoregulation, inflammation |
Tuberculosis Infection
Mycobacterium tuberculosis (Mtb) infection induces distinct macrophage polarization patterns that influence bacterial control and disease progression. Research demonstrates that M1-polarized macrophages, characterized by elevated CD64, CD86, TLR2, HLA-DR, and CCR7 expression, exhibit superior control of Mtb infection compared to M2-polarized cells [48] [47]. At 4 hours post-infection, M1 macrophages show significantly lower bacterial uptake (19.3%) compared to M2 macrophages (82.7%) [47].
However, Mtb infection promotes a mixed M1/M2 activation state, with infection modulating polarization marker expression [48]. Notably, vitamin D-polarized macrophages demonstrate enhanced control of intracellular Mtb growth, associated with high mRNA levels of pro-inflammatory cytokines and the antimicrobial peptide LL-37, without upregulation of the immunosuppressive enzyme IDO [47]. This polarization state represents a promising therapeutic target for host-directed therapies against tuberculosis.
Table 2: Macrophage Polarization in Tuberculosis Infection
| Polarization State | Key Markers | Mtb Control | Characteristic Features |
|---|---|---|---|
| M1 | CD64, CD86, TLR2, HLA-DR, CCR7 | Strong | Pro-inflammatory cytokines, reactive nitrogen intermediates |
| M2 | CD163, CD200R, CD206, CD80 | Weak | Th2 immunoregulation, tissue remodeling |
| Vitamin D-Polarized | LL-37, HLADR, CD80 | Strongest | Pro-inflammatory cytokines + IL-10, low IDO |
| Mtb-Infected Mixed | Variable M1/M2 markers | Intermediate | Downregulation of polarization markers |
Hypoxia and Fibrosis Models
Hypoxia serves as a critical regulator of macrophage polarization in fibrotic environments, promoting a shift toward M2-like phenotypes that drive tissue remodeling and fibrosis. In human macrophage models, hypoxia (1% O2) hinders M1 polarization while promoting acquisition of M2 phenotypic and secretory features [46]. This hypoxic environment decreases expression of T cell costimulatory molecules and proinflammatory cytokines while enhancing alternative activation markers.
The triggering receptor expressed on myeloid cells-1 (TREM-1) emerges as a key hypoxia-inducible gene that can reverse M2 polarization, imparting an M1-skewed phenotype when engaged by an agonist antibody [46]. In oligoarticular juvenile idiopathic arthritis, a condition characterized by hypoxic synovial environments and tissue fibrosis, synovial fluid macrophages express high TREM-1 levels associated with predominant M1 polarization, suggesting its role in counterregulatory mechanisms in hypoxic, fibrotic microenvironments [46].
Experimental Protocols
Macrophage Differentiation and Polarization
Human Monocyte-Derived Macrophage Differentiation:
- Isolate peripheral blood mononuclear cells (PBMCs) from buffy coats by density gradient centrifugation using Lympholyte-H or Ficoll [28] [47].
- Purify CD14+ monocytes by magnetic-activated cell sorting (MACS) using anti-human CD14 microbeads, achieving ≥95% purity [28] [46].
- Culture monocytes in RPMI 1640 medium supplemented with 10% FBS, 2 mM L-glutamine, and appropriate cytokines for 6 days:
- Replace half of the medium on day 3 with fresh medium containing cytokines [46].
Macrophage Polarization:
- M1 Polarization: Treat differentiated macrophages with 50 ng/mL IFN-γ and 10 ng/mL LPS for 24-48 hours [48] [28] [47].
- M2 Polarization: Treat with 20 ng/mL IL-4 for 24-48 hours [28] [46].
- Vitamin D Polarization: Treat undifferentiated monocytes with 10 nM 1,25(OH)2D3 for 6 days during differentiation [47].
- For hypoxia studies: Perform differentiation and polarization at 1% O2 in a hypoxic chamber [46].
Flow Cytometry Panel Design and Staining
Optimized Multicolor Panel Design: Comprehensive macrophage characterization requires panels that capture the spectrum of polarization states. An optimized 11-color panel for mouse macrophages includes F4/80, Arginase 1, TLR4, CD86, VEGF, CD14, CD206, MHC Class II, and TNF-α, providing redundant markers to prevent mischaracterization when individual markers are affected by inflammatory stimuli [23]. For human macrophages, a 10-color panel assessing CD64, CD86, TLR2, HLA-DR, CCR7 (M1), and CD163, CD200R, CD206, CD80 (M2) enables deep characterization [48].
Staining Protocol:
- Harvest macrophages using non-enzymatic cell dissociation buffer or FACS buffer with 0.5 mM EDTA [48] [49].
- For surface staining: Resuspend cells in fluorochrome-conjugated antibody cocktail and incubate for 30 minutes at 4°C protected from light [48] [49].
- For intracellular staining: Fix cells with 4% PFA for 10 minutes, permeabilize with 0.1% Triton X-100, then stain with intracellular antibodies (e.g., TNF-α, Arginase-1) [28] [38].
- For cytokine staining: Activate cells with LPS (100 ng/mL) for 4 hours in the presence of protein transport inhibitor (Golgi-Plug, 1 μL/mL) for the final 20 hours [50].
- Acquire data on a flow cytometer capable of detecting 10+ parameters, collecting a minimum of 50,000 events per sample [48] [49].
Data Analysis Approaches
Conventional Gating Strategy:
- Begin by gating on single cells using FSC-A/FSC-H [48].
- Identify live cells using viability dyes [49].
- Gate on macrophage population using CD68 or F4/80 [12] [38].
- Analyze M1/M2 markers using bi-axial plots to identify co-expression patterns [48].
- Use fluorescence minus one (FMO) controls to establish positive populations [48].
Advanced Analysis Techniques:
- Employ dimensionality reduction tools like UMAP and t-SNE to visualize high-dimensional data [48].
- Use clustering algorithms (PhenoGraph) to identify distinct subpopulations [48].
- Analyze at least 50,000 cells per sample to ensure adequate representation of rare subsets [49].
- Include isotype controls and compensation controls for multicolor panels [28].
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for Macrophage Polarization Studies
| Reagent Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| Growth Factors | M-CSF, GM-CSF | Drives monocyte to macrophage differentiation | Use 50-100 ng/mL for 6 days; GM-CSF predisposes to M1, M-CSF to M2 |
| Polarizing Cytokines | IFN-γ, IL-4, IL-10 | Induces specific polarization states | IFN-γ + LPS for M1; IL-4 for M2a; IL-10 for M2c |
| Polarizing Agents | 1,25(OH)2D3, LPS | Modulates polarization | Vitamin D promotes antimicrobial activity; LPS for classical activation |
| Surface Markers (Human) | CD64, CD86, HLA-DR (M1); CD163, CD206, CD200R (M2) | Phenotype identification | Use in combination for reliable classification |
| Surface Markers (Mouse) | CD38, Gpr18, Fpr2 (M1); Egr2, c-Myc (M2) | Phenotype identification | CD38 and Egr2 provide better distinction than classic markers |
| Intracellular Markers | iNOS, Arginase-1, TNF-α, IL-1β (M1); IL-10, TGF-β (M2) | Functional characterization | Requires cell permeabilization after surface staining |
| Inhibition Reagents | TREM-1 inhibitor (LP17), Brefeldin A | Pathway manipulation, intracellular staining | LP17 blocks TREM-1 signaling; BFA enables cytokine detection |
| Scp1-IN-2 | Scp1-IN-2|SCP1 Covalent Inhibitor|REST Degradation | Scp1-IN-2 is a potent, selective covalent SCP1 inhibitor that promotes REST degradation for glioblastoma research. For Research Use Only. Not for human use. | Bench Chemicals |
| Topoisomerase II inhibitor 4 | Topoisomerase II inhibitor 4, MF:C25H25N5O4, MW:459.5 g/mol | Chemical Reagent | Bench Chemicals |
Signaling Pathways and Molecular Regulation
Macrophage polarization is regulated by complex signaling networks that integrate environmental cues. The following diagram illustrates key signaling pathways involved in M1/M2 polarization and their modulation in disease environments:
Flow cytometric analysis of macrophage polarization provides critical insights into disease mechanisms across cancer, tuberculosis, and fibrosis models. The protocols and frameworks presented here enable researchers to capture the complexity of macrophage phenotypes in these diverse pathological contexts. Key considerations for successful implementation include: (1) using comprehensive marker panels with redundant markers to account for stimulus-induced changes; (2) standardizing differentiation and polarization protocols across experiments; and (3) employing advanced analytical approaches to decipher the spectrum of macrophage activation states. As research in this field advances, flow cytometry will continue to be an indispensable tool for understanding macrophage biology and developing macrophage-targeted therapies.
Solving Common Challenges: Ensuring Reproducibility and Data Quality
Within the context of macrophage M1/M2 polarization research for flow cytometry, the cell detachment step is a critical pre-analytical variable that can significantly influence experimental outcomes. The integrity of key surface markers defining macrophage phenotypes is highly vulnerable to the enzymatic and mechanical stresses of cell harvesting [51]. The selection of an inappropriate detachment method can cleave specific surface receptors, leading to inaccurate phenotypic data and potentially flawed scientific conclusions [51]. This application note provides detailed, evidence-based protocols and quantitative comparisons to guide researchers in selecting optimal cell detachment strategies to preserve the surface marker integrity essential for reliable macrophage polarization analysis.
Quantitative Comparison of Cell Detachment Methods
The choice of detachment method directly impacts the viability, recovery, and most importantly, the surface marker integrity of cells. The following table summarizes key performance metrics for common methods used for adherent macrophages, based on empirical data.
Table 1: Quantitative Comparison of Cell Detachment Methods for Macrophage Surface Marker Preservation
| Detachment Method | Mechanism of Action | Impact on Surface FasL/FasR (MFI) | Impact on Macrophage Marker F4/80 | Relative Cell Viability Post-Detachment | Typical Incubation Time | Required Recovery Time |
|---|---|---|---|---|---|---|
| Scraping (Mechanical) | Physical dislodgement | Minimal decrease (Best preservation) [51] | Unaltered [51] | Variable; can be low due to shear stress | Immediate | Minimal |
| EDTA-Based Buffer (e.g., Versene) | Calcium Chelation (Non-enzymatic) | Slight decrease [51] | Unaltered [51] | Good | 20-30 minutes [51] | Minimal |
| Accutase | Mild Enzymatic & Chelation | Significant decrease [51] | Unaltered [51] | Excellent (Best viability) [51] | 10-30 minutes [51] | ~20 hours [51] |
| Trypsin | Proteolytic Enzymatic Cleavage | Expected severe decrease (General protein degradation) [51] | Expected alteration | Moderate to Poor | 5-15 minutes | Expected prolonged |
Detailed Experimental Protocols for Cell Detachment
Protocol A: Non-Enzymatic Detachment using EDTA-Based Buffer
This method is recommended for preserving sensitive surface markers like FasL and Fas receptor during flow cytometry analysis of macrophage polarization [51].
Reagents:
- EDTA-based cell dissociation solution (e.g., Versene, commercial non-enzymatic buffer)
- Mg2+/Ca2+-free Phosphate-Buffered Saline (PBS)
- Flow Buffer (2% FBS in PBS)
Procedure:
- Aspirate and Wash: Gently aspirate the culture medium from the adherent macrophage culture. Wash the cells once with a pre-warmed (37°C), Mg2+/Ca2+-free PBS to remove residual media and divalent cations [52].
- Apply Detachment Solution: Add enough EDTA-based dissociation solution to completely cover the cell layer (e.g., 3 mL for a 6-well plate, 5 mL for a T75 flask) [52].
- Incubate: Incubate the culture vessel at 37°C for 20-30 minutes. Do not mechanically agitate by tapping or scraping, as this can be performed but is not required for this method [51].
- Confirm Detachment: Periodically check under a microscope. Adherent cells will round up but may not fully detach into suspension.
- Collect Cells: Gently pipet the dissociation solution across the cell layer to dislodge the cells. Transfer the cell suspension to a conical tube.
- Neutralize and Wash: Add twice the volume of flow buffer (2% FBS in PBS) to neutralize the solution. Centrifuge at 300-400 x g for 5 minutes. Aspirate the supernatant and resuspend the cell pellet in flow buffer for counting and subsequent staining [52].
Protocol B: Mild Enzymatic Detachment using Accutase
Use this protocol when high cell viability is a priority, but plan for a significant recovery period to allow surface protein re-expression [51].
Reagents:
- Accutase solution
- Mg2+/Ca2+-free PBS
- Complete cell culture medium
Procedure:
- Aspirate and Wash: Aspirate the culture medium and wash the cells once with pre-warmed (37°C), Mg2+/Ca2+-free PBS [52].
- Apply Accutase: Add sufficient pre-warmed Accutase to cover the cell layer.
- Incubate: Incubate at 37°C for 10-30 minutes. Monitor microscopically for cell detachment. Accutase is typically gentler and may require a longer incubation than trypsin.
- Collect Cells: Once the majority of cells are detached and floating, gently pipet the solution to dislodge any remaining cells. Transfer the suspension to a conical tube.
- Neutralize: Add a volume of complete culture medium that is at least equal to the volume of Accutase used. The serum in the medium will neutralize the enzyme.
- Wash and Count: Centrifuge at 300-400 x g for 5 minutes. Aspirate the supernatant and resuspend the cell pellet in complete medium or an appropriate buffer.
- Critical Recovery Step: For flow cytometry analysis of surface markers compromised by Accutase (e.g., FasL/FasR), you must allow the cells to recover in culture for approximately 20 hours before analysis to enable surface protein re-expression [51].
Experimental Workflow for Optimal Cell Detachment
The following diagram outlines the key decision-making process for selecting and applying the optimal cell detachment method in macrophage polarization studies.
The Scientist's Toolkit: Key Reagents for Cell Detachment & Staining
Table 2: Essential Research Reagent Solutions for Cell Preparation and Flow Cytometry
| Reagent / Material | Function / Purpose | Example Usage & Notes |
|---|---|---|
| EDTA-Based Dissociation Buffer | Non-enzymatic cell detachment via calcium chelation; ideal for preserving sensitive surface proteins like FasL/FasR [51]. | Use for flow cytometry of macrophages when analyzing easily cleaved markers. Incubate 20-30 min at 37°C [51]. |
| Accutase | Mild enzymatic/chelating detachment solution; provides excellent cell viability but can compromise specific surface markers [51]. | Best for applications requiring high viability post-detachment. Requires ~20h recovery for surface marker re-expression before analysis [51]. |
| Flow Buffer (2% FBS in PBS) | Standard buffer for cell washing, staining, and resuspension; FBS helps block non-specific antibody binding. | Used throughout staining protocol to wash and quench enzymatic reactions after cell detachment [52]. |
| Viability Dye (e.g., PI, Sytox) | Fluorescent dye that stains dead cells (impermeant to live cells), allowing for their exclusion during flow cytometry gating. | Added to sorting buffer to exclude dead cells, improving sort purity and data quality [53]. |
| Fluorescence Minus One (FMO) Controls | Critical controls for accurate gating where cells are stained with all antibodies except one. | Essential for setting positive/negative gates for surface markers, especially in multicolor panels for M1/M2 markers [53]. |
| Cell Strainer (35-70 µm) | Used to filter cell suspensions immediately before analysis to ensure a single-cell suspension and prevent clogging. | Filter samples just prior to sort/analysis, even if filtered after staining, to remove aggregates [53]. |
| Hsp90-IN-17 hydrochloride | Hsp90-IN-17 hydrochloride, MF:C21H21ClN4O7, MW:476.9 g/mol | Chemical Reagent |
| Carpro-AM1 | Carpro-AM1|FAAH/COX Inhibitor | Carpro-AM1 is a dual FAAH and substrate-selective COX inhibitor (IC50=94 nM). For Research Use Only. Not for human or veterinary diagnostic or therapeutic use. |
In macrophage polarization research, the accuracy of flow cytometry data hinges on a robust gating strategy. Proper gating selectively targets viable, single cells, ensuring that subsequent analysis of M1 and M2 phenotypes is based on clean, interpretable events [54]. This protocol details a step-by-step gating strategy to isolate live, single macrophages for consistent and reproducible results in immunophenotyping studies.
Step-by-Step Gating Strategy
The following workflow is essential for isolating your target macrophage population prior to M1/M2 analysis.
Excluding Debris and Identifying Cells
The initial step involves distinguishing intact cells from electronic noise and debris using light scatter properties [54] [55].
- Create a dot plot of Forward Scatter-Area (FSC-A) versus Side Scatter-Area (SSC-A).
- Adjust photomultiplier tube (PMT) settings to ensure all expected cell populations are visible [56].
- Set an FSC threshold to remove most debris, air bubbles, and laser noise, which typically appear as FSC-low events [56].
- Draw a region (R1) around the cell population of interest. For primary cells like PBMCs, this gate may separate lymphocytes, monocytes, and granulocytes. For macrophage cell lines, one main population is typically visible [54].
Gating for Single Cells
To prevent clumps of cells from being analyzed as a single event and skewing results, a "singlets" gate is critical [57].
- Create a plot of FSC-Height (FSC-H) versus FSC-Area (FSC-A). Using FSC-Width (FSC-W) is also valid [54] [56].
- Apply the initial "R1" gate from the FSC-A/SSC-A plot to this new plot.
- Gate the population along the diagonal. Single cells will have proportional pulse height and area, forming a diagonal line. Events that fall off this diagonal represent doublets or multiplets and should be excluded [54] [57].
Excluding Non-Viable Cells
Dead cells can non-specifically bind antibodies and dyes, leading to inaccurate data. Their exclusion is paramount [54].
- Incorporate a viability dye (e.g., propidium iodide, 7-AAD, or a fixable viability dye) into your staining panel [56].
- Create a plot of FSC-A versus the viability dye channel.
- Apply the singlets gate ("R2") to this plot.
- Draw a region around the viability dye-negative population to select live cells for further analysis [54] [56].
Identifying Leukocytes with CD45
When working with complex samples like dissociated tissues, staining with a pan-leukocyte marker like CD45 helps gate out residual non-immune cells [56].
- Create a plot of FSC-A versus CD45.
- Apply the live cells gate ("R3") to this plot.
- Draw a region around the CD45-positive population to isolate leukocytes [56].
Gating Controls and Panel Design for Macrophage Polarization
Essential Gating Controls
To ensure gates are set accurately and minimize background fluorescence, specific controls are non-negotiable.
- Fluorescence Minus One (FMO) Controls: A sample stained with all antibodies in your panel except one. This control accounts for background fluorescence spread into the channel of interest and is essential for accurately determining positive and negative populations, especially for low-abundance markers [56].
- Isotype Controls: These control for non-specific antibody binding but must be carefully matched to the specific antibody in terms of immunoglobulin isotype, fluorophore-to-protein ratio, and concentration [56].
- Compensation Controls: Use samples stained with a single fluorophore-conjugated antibody or compensation beads to correct for spectral overlap between fluorophores in multicolor panels [56].
Application in Macrophage Phenotyping
For M1/M2 polarization studies, the final analysis-ready population (derived from the sequential gating above) is analyzed for phenotype-specific markers. Common markers include CD64 and CD86 for M1 macrophages and CD206 for M2 macrophages, which can be distinguished via flow cytometry [32]. The use of FMO controls is particularly critical for accurately resolving these populations.
Research Reagent Solutions
The table below lists essential reagents for implementing this gating strategy in macrophage research.
Table 1: Key Reagents for Flow Cytometry Gating
| Reagent Type | Specific Examples | Function in Gating Strategy |
|---|---|---|
| Viability Dyes | Propidium Iodide (PI), 7-AAD, Fixable Viability Dyes | Distinguishes live cells from dead cells to reduce non-specific binding and improve data quality [54] [56]. |
| Pan-Leukocyte Marker | Anti-CD45 Antibody (various conjugates) | Gates out non-immune cells (e.g., from tissue digests), ensuring analysis is focused on the immune cell lineage [56]. |
| "Dump Channel" Antibodies | Biotinylated antibodies against non-target cells (e.g., CD3, CD19) with Streptavidin conjugate | A panel of antibodies against irrelevant lineages, combined with a viability dye in the same channel, to efficiently exclude unwanted cells [57]. |
| M1 Macrophage Markers | Anti-CD64, Anti-CD86 | Identifies pro-inflammatory, classically activated macrophages for polarization studies [32]. |
| M2 Macrophage Markers | Anti-CD206 | Identifies anti-inflammatory, alternatively activated macrophages for polarization studies [32]. |
| Compensation Beads | Ultraviolet-reactive polystyrene beads | Used with single-color stained samples to set accurate compensation matrices and correct for spectral overlap in multicolor panels [56]. |
| Fc Receptor Block | Human or Mouse Fc Block | Reduces non-specific, Fc-mediated antibody binding, lowering background signal and improving resolution. |
In the field of macrophage polarization research, accurate phenotyping of M1 and M2 subsets is fundamental to understanding immune responses, tissue repair, and disease progression. However, a significant methodological challenge persists: the expression of commonly used polarization markers can be substantially altered by the very inflammatory or immunological stimuli used to induce polarization, potentially leading to mischaracterization [14]. This Application Note details the implementation of a robust flow cytometry strategy employing partially redundant markers to overcome this limitation, ensuring reliable classification of macrophage polarization states for research and drug development applications.
The core principle of this approach involves designing marker panels where, for each macrophage subset, at least one identifying marker is not substantially affected by common inflammatory stimuli such as lipopolysaccharide (L1). By providing built-in verification, this strategy mitigates the risk of misinterpreting data due to stimulus-induced artifact, thereby increasing the validity and reproducibility of experimental results.
The Core Concept: Partial Redundancy as a Safeguard
The Problem of Stimulus-Induced Marker Alteration
Traditional flow cytometry panels for macrophage polarization often rely on a minimal number of markers, typically three or fewer, due to constraints of time, cost, and technical complexity [14]. This minimalist approach carries inherent risks, as key surface and intracellular markers can undergo dynamic changes in response to experimental conditions.
A critical example is the complete clearance of TLR4 from the cell surface of macrophages polarized using IFN-γ + LPS, a phenomenon linked to TLR4 ectodomain shedding [14]. Similarly, the expression of F4/80, frequently used as a universal macrophage marker, decreases significantly in M2c macrophages polarized with IL-10 [14]. Relying solely on such malleable markers can lead to an incomplete or incorrect assessment of macrophage subsets present in a sample.
The Solution: A Partially Redundant Marker Panel
The optimized solution is an eleven-color polychromatic flow cytometry panel that incorporates partial redundancy. For each target macrophage subset (M1, M2a, M2c), the panel includes multiple markers, ensuring that at least one marker remains stable and reliably detectable even when others are altered by the polarization stimulus [14].
This strategy functions as an internal control system. If the primary marker for a subset is downregulated or altered by the stimulus, a secondary (redundant) marker provides a confirmatory signal, preventing the misclassification of that cell population.
The following diagram illustrates the logical relationship between the problem, the strategic solution, and its experimental implementation:
Optimized Marker Panel and Phenotypic Profiles
The optimized eleven-color panel was developed and validated using the murine RAW 264.7 macrophage cell line. Cells were polarized toward M1, M2a, and M2c phenotypes using specific cytokines, and polarization was confirmed via ELISA measurement of TNF-α in cell supernatants [14]. The panel was designed to avoid antibody interference and complex color compensation issues.
Comprehensive Marker Panel
Table 1: Optimized Eleven-Color Flow Cytometry Panel for Macrophage Polarization
| Target | Category | Specificity & Rationale |
|---|---|---|
| F4/80 | Pan-macrophage | General macrophage identification. Note: Expression decreases in M2c [14]. |
| CD14 | Surface Marker | Coreceptor for TLR4; shows medium expression on M1 macrophages [14]. |
| TLR4 | Surface Marker | LPS receptor. Cleared from surface in IFN-γ + LPS stimulated M1 cells [14]. |
| CD86 | Surface Marker | Costimulatory molecule; expressed on M1 and some M2 subsets [14] [58]. |
| MHC Class II | Surface Marker | Antigen presentation; expression varies by subset [14]. |
| CD206 | Surface Marker | Mannose receptor; canonical M2a marker [14]. |
| TNF-α | Intra/Extra-cellular | Pro-inflammatory cytokine; measured on surface and intracellularly in M1 [14]. |
| Arginase 1 | Intracellular Enzyme | Involved in arginine metabolism; associated with M2 polarization [14] [38]. |
| VEGF | Intracellular Factor | Vascular endothelial growth factor; highly expressed in M1 macrophages [14]. |
Definitive Phenotypic Profiles
The combination of markers in this panel creates unique fingerprints for each polarization state, allowing for clear distinction even when individual markers are altered.
Table 2: Characteristic Marker Expression Profiles of Polarized Macrophages
| Macrophage Subset | Polarizing Stimulus | Surface Marker Profile | Intracellular Marker Profile |
|---|---|---|---|
| M0 (Naïve) | None | F4/80Hi, TLR4Lo, CD86Lo, MHC IILo | VEGFMed, Arg-1Lo |
| M1 | IFN-γ ± LPS | CD14Med, MHC IILo, CD86Med, TLR4Lo/Cleared (with LPS) | VEGFHi, TNF-αMed (internal) |
| M2a | IL-4 | CD206Hi, TLR4Hi | Arg-1Hi |
| M2c | IL-10 | F4/80Lo | VEGFLo |
The power of redundancy is exemplified in M1 identification: while LPS stimulation clears surface TLR4, the M1 population can still be reliably identified by its concurrent profile of CD14Med, CD86Med, and high intracellular VEGF [14]. Similarly, the drop in F4/80 expression in M2c macrophages is compensated for by their low VEGF signature.
Detailed Experimental Protocol
Macrophage Culture and Polarization
This protocol is adapted from established methodologies for in vitro polarization of murine macrophage cell lines [14].
- Cell Line: RAW 264.7 (ATCC TIB-71).
- Complete Culture Medium: RPMI 1640 supplemented with 10% heat-inactivated Fetal Bovine Serum (FBS), 100 U/mL penicillin, and 100 µg/mL streptomycin.
- Culture Conditions: Maintain cells in a humidified incubator at 37°C with 5% CO2. Subculture at 90% confluence.
Polarization Protocol:
- Seed cells at a density of 3 x 105 cells per well in an appropriate tissue culture plate.
- Allow cells to adhere overnight in complete culture medium.
- Replace medium with fresh complete medium containing the following polarizing agents:
- M1 Polarization: IFN-γ (20-50 ng/mL) with or without a low dose of LPS (e.g., 10-100 ng/mL).
- M2a Polarization: IL-4 (20 ng/mL).
- M2c Polarization: IL-10 (20 ng/mL).
- M0 (Control): Complete culture medium only.
- Incubate for 24-48 hours. The optimal duration may require empirical determination.
Polarization Verification (ELISA):
- Collect cell-free supernatant post-polarization.
- Measure TNF-α concentration using a commercial ELISA kit as a functional validation of M1 polarization. A significant increase in TNF-α should be observed in IFN-γ ± LPS-treated samples compared to M0, M2a, and M2c supernatants [14].
Flow Cytometry Staining and Acquisition
Materials:
- Antibodies listed in Table 1, titrated for optimal signal-to-noise ratio.
- Flow cytometry staining buffer (e.g., PBS with 1-2% FBS).
- Cell fixation and permeabilization buffers (for intracellular staining).
- Fixable Viability Dye (e.g., eFluor 506) to exclude dead cells.
Staining Workflow:
- Harvesting: Gently detach adherent cells using enzyme-free dissociation buffer or careful scraping. Transfer to flow cytometry tubes.
- Viability Staining: Resuspend cell pellets in buffer containing a fixable viability dye. Incubate for 20-30 minutes at 4°C in the dark. Wash.
- Surface Staining: Resuspend cells in staining buffer containing pre-titrated cocktails of antibodies against surface markers (F4/80, CD14, TLR4, CD86, MHC Class II, CD206). Incubate for 30 minutes at 4°C in the dark. Wash twice.
- Fixation and Permeabilization: Fix cells using a commercial fixation buffer (e.g., 4% PFA) for 20 minutes at room temperature. Wash, then permeabilize cells using a commercial permeabilization buffer (e.g., saponin-based or methanol-based).
- Intracellular Staining: Resuspend fixed and permeabilized cells in permeabilization buffer containing antibodies against intracellular targets (TNF-α, Arginase 1, VEGF). Incubate for 30-60 minutes at 4°C in the dark. Wash twice with permeabilization buffer, then once with standard staining buffer.
- Acquisition: Resuspend cells in staining buffer and acquire data immediately on a flow cytometer capable of detecting 11 colors. Compensation controls (e.g., ultracomp beads or single-stained cells) are essential for accurate results.
The following workflow provides a visual summary of the key experimental steps:
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for Macrophage Polarization Studies
| Reagent / Material | Function / Application | Example & Notes |
|---|---|---|
| Polarizing Cytokines | Directs macrophage differentiation into specific subsets. | Recombinant murine IFN-γ (for M1), IL-4 (for M2a), IL-10 (for M2c). Aliquot and store at -80°C to avoid loss of activity. |
| Flow Cytometry Antibodies | Detection of surface and intracellular markers. | Pre-conjugated, titrated antibodies from Table 1. Critical for building an 11-color panel without interference. |
| Fixation & Permeabilization Buffers | Enables intracellular staining by making the cell membrane permeable. | Commercial kits (e.g., Foxp3/Transcription Factor Staining Buffer Set). Ensure compatibility with your target intracellular epitopes. |
| Cell Dissociation Reagent | Harvesting adherent macrophages for analysis. | Enzyme-free solutions are preferred to prevent cleavage of surface epitopes of interest. |
| Viability Dye | Distinguishes live cells from dead cells in analysis. | Fixable Viability Dye (e.g., eFluor 506). Must be used prior to fixation for accurate dead cell exclusion. |
| Antibacterial agent 124 | Antibacterial Agent 124|Research Grade | Antibacterial agent 124 is a research compound for in vitro studies. This product is For Research Use Only. Not for human, veterinary, or household use. |
Data Analysis and Interpretation
The analysis should leverage the strength of the redundant panel. Gating strategies should sequentially identify single cells, live cells, and macrophages (via F4/80, with the caveat of its variability in M2c). Subsequent analysis should use biaxial plots to visualize co-expression patterns.
For instance, M1 macrophages can be identified as F4/80+ cells that are CD14+ CD86+ and/or VEGFhigh, providing multiple avenues for correct identification even if one pathway is compromised. M2a macrophages can be robustly identified as CD206high Arg-1high, while M2c cells are F4/80low VEGFlow. The use of partially redundant markers not only confirms subset identity but also allows researchers to make functional inferences about the macrophages based on their comprehensive marker profile [14].
Implementing a partially redundant marker strategy is a critical advancement for ensuring accuracy in macrophage polarization research. The optimized eleven-color flow cytometry panel detailed herein provides a robust framework that safeguards against the common pitfall of stimulus-induced marker alteration. By adopting this comprehensive and confirmatory approach, researchers and drug developers can generate more reliable, reproducible, and insightful data on macrophage biology, ultimately strengthening the foundation for future therapeutic discoveries.
Flow cytometry is an indispensable tool for delineating complex cellular populations, and its application in macrophage polarization research is paramount for advancing our understanding of innate immunity, inflammatory diseases, and cancer. The technology's power lies in its ability to perform multi-parameter analysis of single cells in suspension, providing high-throughput quantitative data on both surface and intracellular markers that define the pro-inflammatory M1 and anti-inflammatory M2 states [52] [32]. However, the path to reliable data is fraught with technical challenges, including spectral overlap requiring compensation, cellular autofluorescence that can obscure weak signals, and the particular difficulties of preparing adherent cells like macrophages for analysis. This application note provides detailed protocols and strategies, framed within macrophage M1/M2 polarization research, to navigate these pitfalls, ensuring the generation of precise, reproducible, and biologically meaningful data for researchers, scientists, and drug development professionals.
The Macrophage Polarization Model: An Experimental System
A foundational understanding of the macrophage polarization model is critical for designing appropriate flow cytometry experiments. Macrophages are highly plastic immune cells that differentiate into distinct functional phenotypes in response to specific environmental cues.
- M0 (Naïve) State: Bone marrow-derived macrophages (BMDMs) or human monocyte-derived macrophages (MDMs) are first differentiated from their precursors to establish a baseline, naïve state (M0) [59].
- M1 (Pro-inflammatory) Polarization: Treatment of M0 macrophages with Lipopolysaccharide (LPS) and/or Interferon-gamma (IFN-γ) drives polarization towards the M1 phenotype. These cells are characterized by high expression of pro-inflammatory cytokines (e.g., IL-1β, IL-6) and surface markers like CD64 and CD86 [59] [32]. They play key roles in pathogen clearance and antitumor immunity.
- M2 (Anti-inflammatory) Polarization: Treatment with Interleukin-4 (IL-4) and/or IL-13 drives polarization towards the M2 phenotype. These cells express high levels of markers such as CD206 (mannose receptor) and CD163, and are involved in tissue repair, angiogenesis, and immunoregulation [59] [32].
The protein landscapes of M1 and M2 macrophages are unique, underpinning their specialized functions. Recent proteomic studies have identified novel surface biomarkers, such as Clec4e for murine M1 and Cd72 for murine M2 macrophages, which facilitate their detection via flow cytometry [59].
Key Biomarkers for Macrophage Phenotyping
The following table summarizes critical biomarkers used to distinguish macrophage phenotypes via flow cytometry and other methods.
Table 1: Key Biomarkers for Macrophage M1 and M2 Polarization
| Phenotype | Surface Markers (Flow Cytometry) | Intracellular/Cytokine Markers | Novel Proteomic Biomarkers |
|---|---|---|---|
| M1 | CD64, CD86 [32] | IL-1β, IL-6, iNOS [59] [32] | Clec4e, Gbp2, Acod1 [59] |
| M2 | CD206, CD163 [59] [32] | IL-10, Arg1 [59] | Cd72 [59] |
Experimental Protocols for Macrophage Flow Cytometry
Protocol 1: Harvesting and Preparing Adherent Macrophage Cultures
Generating a viable single-cell suspension from adherent macrophages is a critical first step. The following protocol is adapted from established methods for neural and general adherent cells [52] [60].
Materials:
- Differentiated and polarized adherent macrophages (e.g., BMDMs or MDMs)
- Phosphate-buffered saline (PBS), Mg2+/Ca2+ free
- Pre-warmed cell dissociation agent (e.g., Accutase, trypsin replacement, or EDTA)
- Flow Cytometry Staining Buffer (e.g., 2% FBS in PBS)
- 15 mL or 50 mL conical centrifuge tubes
- Cell strainer (70 µm nylon mesh)
Procedure:
- Assessment: Prior to harvesting, observe the macrophage culture using phase-contrast microscopy to confirm health and confluence [52].
- Washing: Gently wash the culture dish/flask with PBS to remove serum and debris. For macrophages, which can be loosely adherent, this step must be gentle to avoid premature detachment [52] [60].
- Detachment: Add a pre-warmed, gentle dissociation agent like Accutase to cover the entire surface. Enzymatic digestion with trypsin replacement is also effective, but note that it may negatively affect some surface epitopes [52] [60]. Incubate at 37°C for 2-5 minutes. Macrophages typically detach readily; avoid over-digestion.
- Quenching and Collection: Gently tap the vessel to dislodge cells. Quench the enzyme by adding twice the volume of Flow Cytometry Staining Buffer. Collect the cell suspension into a conical tube [52].
- Filtering and Washing: Pass the cell suspension through a cell strainer to remove any clumps or debris [60]. Centrifuge at 300-400 x g for 4-5 minutes at 4°C. Carefully decant the supernatant.
- Cell Counting and Viability: Resuspend the cell pellet in a known volume of buffer and perform a cell count and viability analysis. Adjust the cell concentration to 1 x 10^7 cells/mL for staining [60].
Protocol 2: Surface and Intracellular Antigen Staining
This protocol allows for the simultaneous detection of surface markers (e.g., CD64, CD206) and intracellular antigens (e.g., cytokines), combining established methodologies [52] [61].
Materials:
- Prepared single-cell macrophage suspension
- Conjugated antibodies against surface antigens
- Conjugated antibodies against intracellular antigens
- Flow Cytometry Staining Buffer
- Fixation solution (e.g., 4% paraformaldehyde)
- Permeabilization buffer (e.g., 0.1% Triton X-100 in PBS or commercial saponin-based buffer)
- Fc receptor blocking agent (optional, but recommended)
Procedure:
- Surface Antigen Staining (Live Cells):
- Aliquot 100 µL of cell suspension (1 x 10^6 cells) into a flow cytometry tube.
- (Optional) Add Fc receptor block to reduce non-specific binding. Incubate on ice for 10 minutes.
- Add titrated antibodies against surface markers (e.g., CD64, CD206). Vortex gently.
- Incubate in the dark on ice for 30 minutes [52] [61].
- Add 2 mL of Flow Cytometry Staining Buffer and centrifuge at 300-400 x g for 5 minutes. Decant the supernatant.
- Repeat the wash step.
Fixation and Permeabilization:
- Resuspend the cell pellet in 100-200 µL of fixation buffer (e.g., 4% PFA). Incubate in the dark at room temperature for 15-20 minutes.
- Add 2 mL of permeabilization buffer and centrifuge. Decant the supernatant.
- Wash the cells once more with 2 mL of permeabilization buffer.
Intracellular Antigen Staining:
- Resuspend the fixed and permeabilized cells in 100 µL of permeabilization buffer.
- Add titrated antibodies against intracellular targets (e.g., cytokines, iNOS).
- Incubate in the dark on ice for 30-60 minutes.
- Add 2 mL of permeabilization buffer and centrifuge. Decant the supernatant.
- Perform a final wash with Flow Cytometry Staining Buffer to remove the permeabilization agent.
- Resuspend the final cell pellet in 200-300 µL of Flow Cytometry Staining Buffer for acquisition on the flow cytometer [52].
Managing Technical Pitfalls
Compensation and Spectral Overlap
The simultaneous detection of multiple fluorochromes is complicated by their broad emission spectra, which can overlap into the detection channels of other fluorochromes. This "spillover" must be corrected electronically through a process called compensation to ensure the accuracy of quantitative measurements [52] [62].
Strategy and Protocol:
- Single-Color Controls: For each fluorochrome used in the panel, prepare a control sample stained with that fluorochrome alone. These controls are essential for the flow cytometer's software to calculate the correct compensation matrix [52].
- Proper Gating: Use the target population of interest (e.g., live, single macrophages) for setting compensation, not a generic cell or bead population, as fluorescence spillover can vary between cell types.
- Instrument Calibration: Use calibration microspheres with known fluorescence intensities to ensure instrument performance and quantitative comparability over time and across different platforms [62].
Autofluorescence
Macrophages are particularly prone to autofluorescence due to their high metabolic activity and endogenous molecules like flavins and NADPH. This intrinsic signal can mask weakly expressed antigens and lead to false positives [61] [32].
Strategy and Protocol:
- Fluorochrome Selection: Use bright fluorochromes with emissions in the red and far-red spectrum (e.g., Allophycocyanin (APC)), as cellular autofluorescence is typically strongest in the green-yellow wavelengths. In cells with high autofluorescence, APC can yield more relative brightness than PE [61].
- Use a "No Stain" Control: Always include an unstained, but otherwise identically processed, sample of macrophages. This control defines the level of autofluorescence, which can be used to set negative gates accurately.
- Spectral Unmixing: If using a spectral flow cytometer, the full spectrum of autofluorescence can be measured from the unstained control and mathematically subtracted from the stained samples.
Analysis of Adherent Cells
The analysis of adherent macrophages introduces specific challenges related to the harvesting process and sample quality.
Strategy and Protocol:
- Viability Staining: Always include a viability dye (e.g., propidium iodide, DAPI) to exclude dead cells from the analysis. Dead cells are a major source of non-specific antibody binding and increased autofluorescence [52] [60].
- Gentle Harvesting: Optimize enzymatic digestion to balance cell yield with epitope preservation. Over-digestion can cleave surface antigens of interest and increase cell clumping [52] [60].
- Debris Exclusion: Carefully gate on forward scatter (FSC) vs. side scatter (SSC) plots to exclude cellular debris and small particles. The initial gating strategy is crucial for clean data [52].
The Scientist's Toolkit: Essential Reagents and Materials
A successful flow cytometry experiment relies on the appropriate selection of reagents and materials. The following table details key solutions used in the protocols above.
Table 2: Research Reagent Solutions for Macrophage Flow Cytometry
| Item | Function / Purpose | Example / Notes |
|---|---|---|
| Accutase / Trypsin | Enzymatic cell detachment from adherent culture. Gentle on surface epitopes. | Pre-warmed to 37°C; incubation time must be optimized [60]. |
| Flow Cytometry Staining Buffer | Washing and antibody dilution buffer. Preserves cell viability and reduces non-specific binding. | Typically PBS with 1-2% Fetal Bovine Serum (FBS) and optional sodium azide [52] [60]. |
| Fc Receptor Block | Blocks non-specific binding of antibodies to Fc receptors on macrophages. | Crucial for reducing background fluorescence in myeloid cells [61]. |
| Fixation Solution | Preserves cellular structure and cross-links antibodies in place for intracellular staining. | 4% Paraformaldehyde (PFA) is common. Avoid acidic buffers with FITC [52] [61]. |
| Permeabilization Buffer | Disrupts the cell membrane to allow antibodies access to intracellular antigens. | Saponin-based or detergent-based (Triton X-100) [52]. |
| Viability Dye | Distinguishes live from dead cells during analysis. Dead cells must be excluded. | Propidium Iodide, DAPI, or fixable viability dyes [52] [60]. |
| Calibration Beads | Microspheres for instrument quality control, standardization, and quantitative fluorescence. | Enables traceable measurements and cross-platform comparisons [62]. |
The rigorous application of flow cytometry to macrophage polarization research demands a methodical approach to overcome inherent technical challenges. By implementing the detailed protocols for cell preparation and staining, and by proactively managing the pitfalls of compensation, autofluorescence, and adherent cell analysis through careful experimental design and controls, researchers can achieve a high level of data quality and reproducibility. This precision is foundational for advancing our understanding of macrophage biology and for the successful development of therapeutics that target specific immune phenotypes.
Advanced Techniques and Validation: Beyond Traditional Flow Cytometry
In macrophage polarization research, a comprehensive validation strategy is crucial for confirming phenotypic states beyond surface marker expression. This application note details a correlative analytical framework that integrates gene expression data from Reverse Transcription Quantitative Polymerase Chain Reaction (RT-qPCR) with functional metabolic outputs from Griess (nitric oxide) and Arginase activity assays. The concurrent use of these methods allows researchers to obtain a multi-layered validation of macrophage M1/M2 polarization states by connecting transcriptional regulation with downstream biochemical consequences [63] [64] [7].
The core of this approach lies in monitoring the critical metabolic shift in L-arginine utilization, a well-established hallmark of macrophage polarization. M1 macrophages upregulate inducible nitric oxide synthase (iNOS), catalyzing the production of nitric oxide (NO) from L-arginine, while M2 macrophages upregulate Arginase-1 (ARG1), which hydrolyzes L-arginine to ornithine and urea [64] [7]. This protocol provides standardized methodologies to quantitatively capture these distinct functional profiles, thereby offering a robust system for validating polarization status in various research contexts, including drug development and immunotoxicity testing.
Background and Scientific Rationale
The Metabolic Switch in Macrophage Polarization
Macrophage polarization toward the M1 or M2 phenotype orchestrates a profound rewiring of cellular metabolism, with the amino acid L-arginine serving as a key metabolic node. The competition for this common substrate determines the functional outcome of the immune response [64] [7].
- M1 Phenotype (Pro-inflammatory): Classical activation via stimuli like IFN-γ and LPS robustly induces the expression of NOS2, the gene encoding iNOS. This enzyme generates nitric oxide (NO), a key signaling molecule with antimicrobial and tumoricidal properties. NO and its stable oxidation products, nitrite and nitrate, can be quantified using the Griess assay [7] [65].
- M2 Phenotype (Anti-inflammatory): Alternative activation via IL-4 or IL-13 induces the expression of ARG1, the gene encoding Arginase-1. This enzyme diverts L-arginine away from NO production and toward the polyamine and proline synthesis pathways, which are essential for cell proliferation and tissue repair. Arginase activity can be measured by detecting the urea byproduct of its reaction [64] [7].
The complementary nature of these pathways allows researchers to cross-validate polarization states. For instance, a successful M1 polarization should demonstrate high NOS2 expression, high NO production, and low ARG1 expression/activity, and vice-versa for the M2 phenotype [63] [64].
Key Molecular Targets and Expected Outcomes
The table below summarizes the core molecular targets analyzed in this integrated workflow and their expression across polarization states.
Table 1: Key Analytical Targets in Macrophage Polarization
| Target | Assay Type | M1 Phenotype | M2 Phenotype | Biological Role |
|---|---|---|---|---|
| iNOS / NOS2 | RT-qPCR / Griess Assay | ↑↑↑ (High) | ↓ (Low/Baseline) | Pro-inflammatory mediator, antimicrobial defense [7] [65] |
| Arginase-1 / ARG1 | RT-qPCR / Arginase Activity | ↓ (Low/Baseline) | ↑↑↑ (High) | Immunosuppression, tissue repair [64] [7] |
| CD86 / CD80 | Flow Cytometry | ↑↑↑ (High) | ↓ (Low/Baseline) | M1 surface markers, co-stimulation [64] [7] |
| CD206 | Flow Cytometry | ↓ (Low/Baseline) | ↑↑↑ (High) | M2 surface marker, endocytosis [64] [7] |
This multi-target approach is exemplified in recent research. A study on Toxoplasma gondii infection demonstrated that the parasite protein TgCDPK3 interacts with host Arginase-1, suppressing its activity and shifting macrophages toward an M1-biased phenotype, a discovery validated using the very assays described herein [63]. Conversely, the disruption of the CDK5 regulatory subunit p35 was shown to limit M2 macrophages, evidenced by decreased Arginase-1 production, while maintaining M1 functional responses [7].
Experimental Workflow and Protocols
Integrated Workflow for Correlative Analysis
The following diagram outlines the sequential and parallel processes of the integrated validation workflow, from macrophage culture to final data correlation.
Macrophage Polarization Protocol
3.2.1 Cell Culture and Differentiation
- Cell Models: Human monocytic THP-1 or HL-60 cell lines are commonly used. Differentiate into naive macrophages (M0) by treating with Phorbol 12-myristate 13-acetate (PMA) for THP-1 cells (e.g., 100 nM for 48 hours) or with M-CSF for primary human monocytes (e.g., 50 ng/mL for 6-7 days) [64] [66].
- Polarization Stimuli:
3.2.2 Cell Harvesting and Lysis
- Wash polarized cells with cold PBS.
- Lyse cells using an appropriate lysis buffer. A typical buffer for parallel RNA and protein/activity analysis contains:
- 10 mM Tris-HCl (pH 7.4)
- 1% Triton X-100
- 1 μM pepstatin A, 1 μM leupeptin (protease inhibitors)
- 1 mM PMSF [63]
- Critical Step: Gently scrape the cells and transfer the lysate to a microcentrifuge tube. Vortex briefly and centrifuge at 12,000 × g for 10 minutes at 4°C. Aliquot the supernatant for the different downstream assays to avoid repeated freeze-thaw cycles.
RT-qPCR Protocol for Gene Expression Analysis
3.3.1 RNA Isolation and cDNA Synthesis
- Isolate total RNA from a cell lysate aliquot using a commercial kit (e.g., TRIzol reagent). Determine RNA concentration and purity by spectrophotometry (A260/A280 ratio ~2.0 is ideal) [67] [68].
- Perform reverse transcription on 1 μg of total RNA using a cDNA synthesis kit with random hexamers and/or oligo(dT) primers. A typical 20 μL reaction includes:
- 1 μg RNA
- 4 μL 5x Reaction Buffer
- 1 μL Reverse Transcriptase (200 U/μL)
- 1 μL dNTP Mix (10 mM each)
- 1 μL Primer Mix
- Nuclease-free water to 20 μL
- Incubate as per manufacturer's instructions (e.g., 25°C for 5 min, 50°C for 45 min, 70°C for 5 min). Dilute the resulting cDNA and store at -20°C.
3.3.2 Quantitative PCR (qPCR)
- Prepare qPCR reactions in a 96-well plate. A standard 20 μL reaction contains:
- 10 μL 2x SYBR Green PCR Master Mix
- 1 μL Forward Primer (10 μM)
- 1 μL Reverse Primer (10 μM)
- 2 μL cDNA template (or water for NTC)
- 6 μL Nuclease-free water
- Primer Sequences: Use validated primer pairs for human genes.
Table 2: Example qPCR Primer Sequences
Gene Forward Primer (5'→3') Reverse Primer (5'→3') Amplicon Size NOS2 CAGCTGGGCTGTACAAACCTT CATTGGAAGTGAAGCGTTTCG ~150 bp ARG1 GTGGAAACTTGCATGGACAAC AATCCTGGTACATCTGGGAACT ~120 bp GAPDH GGAGCGAGATCCCTCCAAAAT GGCTGTTGTCATACTTCTCATGG ~100 bp - Run the qPCR with the following cycling conditions:
- Step 1: 95°C for 3 min (Initial Denaturation)
- Step 2: 95°C for 10 sec (Denaturation)
- Step 3: 60°C for 30 sec (Annealing/Extension) — Repeat Steps 2-3 for 40 cycles.
- Perform a melt curve analysis at the end (65°C to 95°C, increment 0.5°C).
- Data Analysis: Calculate fold changes in gene expression using the 2^(-ΔΔCt) method, normalizing to housekeeping genes (e.g., GAPDH, β-actin) and relative to the control group (e.g., M0 macrophages) [67].
Functional Assay Protocols
3.4.1 Griess Assay for Nitric Oxide (NO) Production The Griess reaction measures nitrite (NOâ‚‚â»), a stable end product of NO, in cell culture supernatants [63] [65].
- Reagent Preparation: Prepare Griess reagent by mixing equal volumes of 1% sulfanilamide in 5% phosphoric acid and 0.1% N-(1-Naphthyl)ethylenediamine dihydrochloride in water. Protect from light.
- Procedure:
- Collect cell culture supernatant from polarized macrophages after 24-48 hours of stimulation. Centrifuge to remove any cells or debris.
- In a 96-well plate, add 50 μL of supernatant and 50 μL of Griess reagent.
- Incubate at room temperature for 10-15 minutes, protected from light.
- Measure the absorbance at 540 nm using a microplate reader.
- Quantification: Generate a standard curve using sodium nitrite (NaNO₂) diluted in culture medium (e.g., 0-100 μM). Calculate the nitrite concentration in samples by interpolating from the standard curve. Express results as μM nitrite or normalized to total cellular protein.
3.4.2 Arginase Activity Assay This assay quantifies urea produced by the arginase-mediated hydrolysis of L-arginine [63] [7].
- Reagent Preparation:
- Substrate Buffer: 50 mM Tris-HCl (pH 7.5), containing 10 mM MnClâ‚‚.
- Arginine Substrate: 0.5 M L-arginine (pH 9.7).
- Urea Detection Reagents:
- Acid Solution: H₂SO₄: H₃PO₄: H₂O (1:3:7)
- Colorimetric Agent: α-Isonitrosopropiophenone (ISPF, 9% in 100% ethanol)
- Procedure:
- Activation: Mix 50 μL of cell lysate with 50 μL of Substrate Buffer. Heat at 55-60°C for 10 minutes to activate arginase.
- Enzymatic Reaction: Add 25 μL of Arginine Substrate to the activated lysate. Incubate at 37°C for 60-120 minutes.
- Reaction Termination: Stop the reaction by adding 400 μL of the Acid Solution.
- Color Development: Add 25 μL of ISPF and mix. Heat samples at 100°C for 45 minutes. Cool to room temperature in the dark.
- Absorbance Measurement: Read the absorbance at 540 nm.
- Quantification: Generate a standard curve using urea (0-100 μg/mL). The arginase activity is proportional to the amount of urea produced and can be expressed as mU/mL or normalized to total protein content (e.g., mU/mg protein).
The Scientist's Toolkit: Research Reagent Solutions
The table below catalogues essential reagents and kits for implementing this integrated validation strategy.
Table 3: Essential Research Reagents and Kits
| Item | Function/Application | Example Product/Source |
|---|---|---|
| M-CSF (Macrophage Colony-Stimulating Factor) | Differentiation of primary human monocytes into M0 macrophages [7] | Recombinant Human M-CSF (PeproTech) |
| LPS (Lipopolysaccharide) & IFN-γ | Key cytokines for classical M1 macrophage polarization [64] [7] | LPS from E. coli (Sigma-Aldrich), Recombinant Human IFN-γ (BioLegend) |
| IL-4 & IL-13 | Key cytokines for alternative M2 macrophage polarization [64] [7] | Recombinant Human IL-4 / IL-13 (R&D Systems) |
| RNA Extraction Kit | Isolation of high-quality total RNA for RT-qPCR | TRIzol Reagent (Invitrogen) or RNeasy Kit (Qiagen) |
| cDNA Synthesis Kit | Reverse transcription of RNA to cDNA for qPCR analysis | High-Capacity cDNA Reverse Transcription Kit (Applied Biosystems) |
| SYBR Green qPCR Master Mix | Fluorescence-based detection of amplified DNA in real-time PCR | PowerUp SYBR Green Master Mix (Applied Biosystems) |
| Griess Reagent Kit | Colorimetric detection and quantification of nitrite, a stable NO metabolite [63] | Griess Reagent Kit (Beyotime, S0024) |
| Arginase Activity Assay Kit | Colorimetric measurement of arginase activity via urea production [63] | Arginase Activity Assay Kit (Boxbio, AKAM022M) |
Data Interpretation and Correlation Analysis
Expected Quantitative Outcomes
When successfully implemented, this integrated approach yields a quantitative profile that clearly distinguishes M1 and M2 macrophages. The table below provides representative data from published studies to illustrate expected outcomes.
Table 4: Representative Data from Polarized Macrophages
| Assay | M0 Macrophages (Baseline) | M1-Polarized Macrophages | M2-Polarized Macrophages | Reference Context |
|---|---|---|---|---|
| NOS2 mRNA (RT-qPCR) | 1.0 (Reference) | 50 - 200 fold increase | 0.5 - 2 fold change | CFIm25 overexpression drove M1 polarization [64] |
| ARG1 mRNA (RT-qPCR) | 1.0 (Reference) | 0.1 - 0.5 fold change | 20 - 100 fold increase | M2 polarization with IL-4/IL-13 [64] |
| Nitrite (Griess Assay) | 1 - 5 μM | 20 - 60 μM | 2 - 8 μM | LPS-stimulated BV2 microglial cells [65] |
| Arginase Activity | 5 - 15 mU/mg | 2 - 10 mU/mg | 50 - 200 mU/mg | Loss of p35 reduced ARG1 in M2 cells [7] |
Correlation and Pathway Integration
The final, critical step is to correlate transcriptional and functional data to build a coherent narrative. Strong positive correlations between NOS2 expression and NO production, and between ARG1 expression and arginase activity, confirm a successfully polarized and functionally active macrophage population.
The molecular pathways underlying the measured targets and their role in polarization can be visualized as follows:
Discrepancies between gene expression and functional output can reveal post-transcriptional regulation, enzyme inhibition, or substrate limitation. For example, the TgCDPK3 protein of Toxoplasma gondii was shown to interact directly with host Arginase-1, suppressing its activity without necessarily affecting ARG1 mRNA levels [63]. Such findings highlight the indispensable value of this multi-layered validation strategy in uncovering complex regulatory mechanisms in macrophage biology.
The analysis of macrophage polarization into classically activated (M1) and alternatively activated (M2) phenotypes is crucial for understanding immune responses in health and disease. Traditional methods for identifying these cellular states rely on fluorescent labels or antibodies that target specific surface and intracellular markers. While informative, these approaches are costly, time-consuming, and alter native cell physiology. Emerging label-free techniques leverage intrinsic cellular autofluorescence signatures, which arise from metabolic co-factors like NAD(P)H and FAD, combined with machine learning to classify macrophage phenotypes rapidly and non-invasively. This Application Note details the protocols and data analysis pipelines for implementing these cutting-edge methods in macrophage polarization research, providing researchers with frameworks to accelerate discovery in immunology and drug development.
Autofluorescence Signatures as Phenotypic Indicators
Macrophage polarization drives distinct metabolic reprogramming: M1 macrophages typically rely on glycolysis, while M2 phenotypes favor oxidative phosphorylation. These metabolic differences alter the concentrations and protein-binding states of intrinsic fluorophores, creating unique autofluorescence "fingerprints" that can be exploited for classification [69].
- NAD(P)H and FAD: The primary sources of autofluorescence, these coenzymes provide insights into cellular metabolic states. Their fluorescence intensity and lifetime change depending on the metabolic pathway a cell utilizes [69] [70].
- Morphological Features: Polarized macrophages also exhibit differences in cell size, granularity, and structural details, which can be captured through techniques like flow cytometry and reflectance confocal microscopy [71] [28].
The following table summarizes the key autofluorescence parameters used in different analytical platforms to distinguish macrophage phenotypes.
Table 1: Key Autofluorescence Parameters for Macrophage Phenotype Classification
| Analytical Platform | Key Measured Parameters | Phenotypic Correlations |
|---|---|---|
| Multispectral Flow Cytometry [71] | 45 optical signals (FSC, SSC, fluorescence height/area/width) | Distinct six-phenotype (M0, M1, M2a, M2b, M2c, M2d) fingerprint |
| Two-Photon FLIM (2P-FLIM) [69] | NAD(P)H fluorescence lifetimes (τ1, τ2, α1, α2, τavg), Optical Redox Ratio (ORR) | Shorter lifetimes associated with M1; Longer lifetimes associated with M2 |
| Hyperspectral Reflectance Confocal Microscopy [28] | Reflectance spectral profile at each pixel | High accuracy (>98%) for M1 vs. M2 classification |
Experimental Protocols
Protocol 1: Label-Free Classification Using Multispectral Flow Cytometry
This protocol is adapted from the work profiling six macrophage phenotypes using a conventional flow cytometer equipped with multiple lasers [71].
Workflow
The following diagram illustrates the key stages of this protocol, from cell preparation to result validation.
Key Materials and Reagents
Table 2: Essential Reagents for Multispectral Flow Cytometry Protocol
| Reagent / Material | Function / Application |
|---|---|
| Polarization Cytokines (IFN-γ, IL-4, etc.) | Generation of specific macrophage phenotypes (M1, M2a, etc.) [71] |
| DAPI (4',6-diamidino-2-phenylindole) | Viability dye for excluding dead cells from analysis [71] |
| Multi-Laser Flow Cytometer | Instrument for acquiring multi-parameter autofluorescence data (e.g., 6 lasers, 20 fluorescence detectors) [71] |
| Cell Culture Media & Supplements | For macrophage differentiation and maintenance |
Step-by-Step Procedure
- Cell Polarization: Generate six macrophage phenotypes (M0, M1, M2a, M2b, M2c, M2d) from primary human monocytes or cell lines using established polarization protocols [71] [71]. Include parallel cultures for validation.
- Validation of Polarization: Validate the polarization status of the cells using traditional methods before autofluorescence analysis. This typically involves:
- Immunostaining and polychromatic flow cytometry for canonical surface markers.
- Functional assays: Griess assay to measure nitric oxide (M1-associated) and arginase assay (M2-associated) [71].
- Sample Preparation for Autofluorescence Cytometry: Prepare a single-cell suspension of viable macrophages. Stain cells with a viability dye like DAPI to allow for the exclusion of dead cells during analysis. Note: No other fluorescent labels are used.
- Flow Cytometry Data Acquisition: Acquire data on a flow cytometer equipped with multiple lasers. For each cell event, collect the following parameters:
- Forward scatter (FSC) height, area, and width.
- Side scatter (SSC) height and area.
- Height and area signals from all available fluorescence detectors (e.g., 40 signals from 20 detectors) [71]. This creates a 45-dimensional response vector for each cell, forming its autofluorescence fingerprint.
- Data Preprocessing and Model Training:
- Data Splitting: Pool all single-cell events and randomly split the dataset into three subsets: 60% for training, 20% for validation, and 20% for testing [71].
- Model Training: Train a Fully Connected Neural Network (FCNN) using the training set. The input layer should match the number of extracted parameters (e.g., 45 nodes). Use the validation set to tune hyperparameters and prevent overfitting.
- Performance Evaluation: Use the held-out test set to evaluate the final model's classification accuracy. The FCNN has been shown to achieve 75.8% accuracy for six-phenotype classification, with higher accuracies (averaging 92.0%) for binary classification tasks [71].
Protocol 2: Phenotype Classification via Two-Photon FLIM (2P-FLIM) and Machine Learning
This protocol utilizes fluorescence lifetime imaging of NAD(P)H to classify macrophage polarization states based on metabolic activity [69].
Workflow
The diagram below outlines the workflow for the 2P-FLIM-based classification protocol.
Key Materials and Reagents
Table 3: Essential Reagents for 2P-FLIM Protocol
| Reagent / Material | Function / Application |
|---|---|
| Polarization Cytokines (IFN-γ, IL-4) | Generation of M1 and M2 macrophage phenotypes [69] |
| Carbonyl cyanide-p-trifluoromethoxyphenylhydrazone (FCCP) | Mitochondrial uncoupler used for metabolic challenge to stratify phenotypes [69] |
| Two-Photon Fluorescence Lifetime Microscope | System for exciting NAD(P)H and measuring fluorescence decay kinetics |
Step-by-Step Procedure
- Macrophage Polarization and Metabolic Perturbation: Polarize human monocyte-derived macrophages towards M1 (using IFN-γ) and M2 (using IL-4) states. To enhance phenotypic stratification, challenge the cells during imaging with small molecules like FCCP, which uncouples mitochondrial oxidative phosphorylation [69].
- 2P-FLIM Image Acquisition: Acquire large field-of-view images of individual polarized macrophages using a two-photon microscope configured for FLIM. Excite NAD(P)H with a pulsed laser (e.g., ~740 nm) and record the fluorescence decay curve at every pixel in the image.
- FLIM Parameter Extraction: Fit the fluorescence decay data to a multi-exponential model to extract key quantitative parameters for each cell or image region:
- Fluorescence lifetimes (Ï„1, Ï„2).
- Fractional amplitudes (α1, α2).
- Mean lifetime (Ï„avg).
- Optical Redox Ratio (ORR), calculated as FAD/(NAD(P)H + FAD) [69].
- Data Analysis and Machine Learning:
- Dimensionality Reduction: Use techniques like Uniform Manifold Approximation and Projection (UMAP) to visualize the high-dimensional FLIM data and observe natural clustering of M1 and M2 phenotypes.
- Classifier Training: Employ a Random Forest algorithm to build a classification model. This model can distinguish M1 and M2 phenotypes with high accuracy (ROC-AUC of 0.944) and also identify the most important FLIM parameters driving the classification [69].
Performance Comparison and Technical Considerations
The performance of label-free autofluorescence classification varies based on the technology and the complexity of the classification task.
Table 4: Performance Comparison of Label-Free Classification Methods
| Method | Classification Task | Reported Performance | Key Advantages |
|---|---|---|---|
| Multispectral Flow Cytometry + FCNN [71] | 6 phenotypes (M0, M1, M2a, M2b, M2c, M2d) | 75.8% accuracy | High-throughput, multi-parameter single-cell data |
| Pool of 2 phenotypes | ~92.0% accuracy | ||
| 2P-FLIM + Random Forest [69] | M1 vs. M2 (Human, full FoV) | 94.4% AUC | Provides spatial information and direct metabolic readout |
| Hyperspectral Reflectancy Confocal + LDA [28] | M1 vs. M2 (Human, single-cell) | >98% accuracy | High single-cell accuracy, simple optical setup |
The Scientist's Toolkit
Table 5: Key Research Reagent Solutions for Label-Free Macrophage Analysis
| Tool / Reagent | Function in the Workflow |
|---|---|
| Multispectral Flow Cytometer | Captures high-dimensional autofluorescence fingerprints from single cells in suspension [71] [35]. |
| Two-Photon FLIM System | Enables label-free imaging of metabolic states via NAD(P)H fluorescence lifetime measurements in live cells and tissues [69] [72]. |
| Hyperspectral Confocal Microscope | Collects full reflectance spectra at each image pixel for label-free single-cell classification [28]. |
| Polarization Cocktails (IFN-γ, LPS, IL-4, IL-13) | Standardized reagents for generating specific and consistent macrophage phenotypes in vitro [71] [69] [73]. |
| Metabolic Inhibitors (e.g., FCCP) | Used to perturb cell metabolism and amplify autofluorescence differences between phenotypes [69]. |
The integration of autofluorescence measurements with machine learning classifiers provides a robust, label-free framework for identifying macrophage polarization states. These methods offer significant advantages in speed, cost, and the preservation of native cell function compared to traditional antibody-based techniques. The protocols outlined here for multispectral flow cytometry and 2P-FLIM provide actionable pathways for researchers to implement these approaches, facilitating deeper investigation into macrophage biology and accelerating therapeutic discovery in immunology and related fields.
Within the broader scope of macrophage polarization research, flow cytometry has served as a cornerstone technique for identifying M1 and M2 phenotypes based on surface marker expression. However, the requirement for cell labeling, fixation, and destruction limits its application for dynamic, live-cell studies and fails to provide intrinsic biochemical information. Hyperspectral Imaging (HSI) and Raman spectroscopy have emerged as powerful, label-free alternatives that enable non-invasive, live-cell characterization of macrophage phenotype based on their intrinsic biochemical and morphological properties [74] [28]. These techniques provide a complementary approach to flow cytometry, offering the potential for kinetic studies of polarization dynamics without perturbing the cellular environment.
This Application Note details the experimental protocols and analytical frameworks for implementing these label-free technologies, specifically for discriminating between pro-inflammatory M1 and anti-inflammatory M2 macrophage phenotypes. The methodologies outlined herein are designed to integrate seamlessly with existing flow cytometry workflows, providing researchers with a multimodal approach to macrophage polarization analysis.
Key Performance Metrics for Label-Free Phenotype Discrimination
The following table summarizes the demonstrated performance of Raman spectroscopy and hyperspectral imaging in distinguishing macrophage phenotypes, as validated against traditional methods like flow cytometry and RT-qPCR.
Table 1: Performance Metrics of Label-Free Techniques for Macrophage Phenotyping
| Technique | Macrophage Model | Phenotypes Discriminated | Classification Accuracy | Key Discriminatory Features | Reference Method Validation |
|---|---|---|---|---|---|
| Raman Spectroscopy | Human monocyte-derived macrophages | M0, M1, M2 | High accuracy (model validated) [74] | Lipid droplet content, nucleic acids, protein profiles [74] | Flow cytometry (CD80, CD206) [74] |
| Raman Spectroscopy | Human alveolar macrophages in PCLS | SARS-CoV-2 infected vs. uninfected | 83% [75] | Intracellular RNA, carotenoids, triacylglycerides, glucose [75] | Cytokine quantification (IFN-γ, IL-18) [75] |
| Hyperspectral Reflectance Confocal Microscopy | Human monocyte-derived macrophages | M1 vs. M2 | >98% (cells from same donor) [28] | Reflectance spectra related to cellular refractive index and morphology [28] | Flow cytometry (CD80, CD86, CD163, CD206) and RT-qPCR [28] |
Experimental Protocols
Protocol 1: Raman Spectroscopic Analysis of Polarized Macrophages
This protocol describes the procedure for label-free discrimination of macrophage phenotypes using single-cell Raman spectroscopic imaging [74].
Sample Preparation
- Cell Culture & Polarization: Differentiate human monocytes isolated from PBMCs into macrophages (M0) using GM-CSF or M-CSF (e.g., 25 ng/mL M-CSF for 6 days) [74] [28].
- Induce Polarization:
- Validation of Polarization: Validate polarization states using flow cytometry for M1 markers (e.g., CD80, CD86) and M2 markers (e.g., CD206, CD163) [74] [28].
- Sample for Raman: Seed polarized macrophages on suitable substrates (e.g., CaF₂ slides) and chemically fix with 4% PFA for 15 minutes at 37°C [74].
Data Acquisition
- Instrument Setup: Use a confocal Raman microscope equipped with a 532 nm or 785 nm laser source.
- Spectral Collection: Acquire Raman spectra or hyperspectral images from single cells. Typical acquisition parameters might include a 1-2 second integration time per spectrum [74].
- Spatial Imaging: For Raman imaging, collect spectra in a raster-scan pattern across the cell to create a hyperspectral data cube.
Data Analysis
- Pre-processing: Perform cosmic ray removal, background subtraction, and vector normalization on all spectra.
- Spectral Unmixing: Apply algorithms like N-FINDR to identify and visualize the distribution of major biochemical components (lipids, proteins, nucleic acids) within the cells [74].
- Classification Modeling:
- Use Principal Component Analysis (PCA) to reduce the dimensionality of the spectral data.
- Build a Linear Discriminant Analysis (LDA) model on the PCA scores to create a classifier for M0, M1, and M2 phenotypes [74].
- Model Validation: Employ leave-one-donor-out cross-validation to ensure the model's robustness and generalizability [74].
Protocol 2: Hyperspectral Reflectance Confocal Microscopy for Live-Cell Phenotyping
This protocol outlines the use of label-free HSI for classifying macrophage polarization in living cells [28].
Sample Preparation
- Cell Culture & Polarization: Follow steps 1-3 from Protocol 3.1.1 to generate validated M1 and M2 macrophages.
- Live-Cell Preparation: Seed polarized macrophages onto glass-bottom culture dishes suitable for live-cell imaging. Perform HSI measurements in live cells without fixation.
Data Acquisition
- Instrument Setup: Use a laser scanning confocal microscope equipped with a white-light laser source and a hyperspectral detector.
- Spectral Collection: Acquire a complete reflectance spectrum (e.g., from 450 nm to 800 nm) for every pixel in the field of view to generate a hyperspectral data cube [28].
Data Analysis
- Pre-processing: Normalize spectra and correct for instrumental effects.
- Semi-Automatic Classification:
- Perform PCA on the hyperspectral data to identify major sources of variance.
- Use LDA on the principal components to build a classifier that automatically discriminates M1 from M2 macrophages at the single-cell level [28].
Signaling Pathways in Macrophage Polarization
The transition between macrophage phenotypes is regulated by complex intracellular signaling pathways. The following diagram illustrates the key pathways involved in M1 and M2 polarization, which underpin the biochemical changes detected by label-free techniques.
Diagram 1: Signaling pathways governing macrophage polarization, highlighting metabolic shifts and surface marker expression. In disease contexts such as lymphoma relapse, a shift toward the M2 phenotype is promoted [9].
Experimental Workflow for Integrated Analysis
The following diagram outlines a comprehensive workflow that integrates label-free techniques with established molecular biology methods for robust macrophage phenotyping.
Diagram 2: Integrated experimental workflow from cell preparation to phenotype validation.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of these protocols requires specific biological and analytical reagents. The following table lists key materials and their functions.
Table 2: Essential Research Reagents and Materials for Macrophage Polarization and Label-Free Analysis
| Category | Item | Function / Application | Example Citations |
|---|---|---|---|
| Cell Culture & Polarization | Recombinant Human/Mouse M-CSF | Differentiation of monocytes into naïve M0 macrophages. | [74] [28] |
| Polarizing Cytokines: IFN-γ, LPS, IL-4 | Induction of M1 (IFN-γ + LPS) and M2 (IL-4) phenotypes. | [59] [74] [28] | |
| Validation Reagents | Flow Cytometry Antibodies: anti-CD80, anti-CD86, anti-CD206, anti-CD163 | Validation of macrophage phenotype by surface marker expression. | [12] [74] [28] |
| qPCR Primers: iNOS (NOS2), ARG1, TNF-α, IL-10, CD206 (MRC1) | Validation of macrophage phenotype by gene expression. | [28] [36] | |
| Label-Free Analysis | CaFâ‚‚ Slides or Quartz Bottom Dishes | Optically suitable substrates for Raman spectroscopy and HSI. | [74] |
| Supercontinuum Laser Source | White-light laser for hyperspectral reflectance confocal microscopy. | [28] | |
| Data Analysis | Multivariate Analysis Software (e.g., Python with Scikit-learn, MATLAB, PLS_Toolbox) | For performing PCA, LDA, and other classification analyses on spectral data. | [75] [74] [28] |
The classical M1/M2 paradigm of macrophage polarization has provided a valuable but simplified framework for understanding immune responses in health and disease. However, this binary classification often fails to capture the complex spectrum of macrophage activation states present in physiological environments. Flow cytometry, while powerful for high-throughput cellular analysis, relies on a limited set of surface and intracellular markers that may not resolve the full heterogeneity of macrophage populations. Single-cell RNA sequencing (scRNA-seq) has emerged as a transformative validation tool that comprehensively resolves macrophage heterogeneity, enabling researchers to identify novel subpopulations, define unique transcriptional signatures, and develop more refined flow cytometry panels for macrophage polarization studies.
ScRNA-Seq Reveals Complex Macrophage Heterogeneity Beyond M1/M2
Identification of Novel Macrophage Subsets
Single-cell RNA sequencing has consistently demonstrated that tissue macrophages exist as multiple distinct subpopulations with specialized functional roles, moving beyond the traditional M1/M2 classification:
Table 1: Novel Macrophage Subpopulations Identified by ScRNA-Seq Across Diseases
| Disease Context | Identified Subsets | Key Marker Genes | Functional Characteristics |
|---|---|---|---|
| Ulcerative Colitis [76] | APOEâº, S100A8âº, LSP1âº, IGHMâº, IL1B⺠| S100A4, S100A6, VCAN | S100A8⺠and IL1B⺠subsets expanded in inflamed tissue; non-classical M1/M2 polarization |
| Colon Cancer [77] | Macrophages_SPP1 | SPP1, FTL, FTH1 | Enhanced glycolytic metabolism, lysosomal activity, angiogenesis, and immunosuppression |
| Atherosclerosis [78] | IL1BâºAPOE⺠inflammatory foam cells, IL1Bâ»APOE⺠non-inflammatory foam cells, LYVE1⺠macrophages | IL1B, APOE, LYVE1, TREM2 | Inflammatory foam cells predominant in carotid plaques; non-inflammatory in femoral plaques |
| Gastric Cancer [79] | TAM-APOE, TAM-IDO1, TAM-SKAP1, TAM-POLB | APOE, IDO1, SKAP1, POLB | TAM-APOE subset interacts with tumor cells via MIF-CD74 axis; lipid metabolism enrichment |
These findings demonstrate that scRNA-seq can resolve macrophage heterogeneity with unprecedented resolution, identifying disease-specific subpopulations that may represent new therapeutic targets.
Key Technological Advantages of ScRNA-Seq for Macrophage Studies
The application of scRNA-seq to macrophage biology provides several distinct advantages over traditional methods:
- Unbiased identification of novel cellular states without prior knowledge of marker genes
- Resolution of continuous phenotypic transitions through pseudotime trajectory analysis [76]
- Discovery of cellular communication networks via ligand-receptor interaction analysis [79]
- Identification of key transcriptional regulators using gene regulatory network analysis [80]
- Integration with other modalities including spatial transcriptomics and proteomics
Experimental Protocols for ScRNA-Seq in Macrophage Research
Standardized ScRNA-Seq Workflow for Macrophage Analysis
The following protocol outlines a comprehensive approach for utilizing scRNA-seq to resolve macrophage heterogeneity and validate flow cytometry panels:
Sample Preparation and Cell Isolation
- Obtain tissue samples (e.g., colonic mucosa, tumors, atherosclerotic plaques) in appropriate preservation medium
- Process tissues using gentle dissociation protocols to maintain macrophage viability and integrity
- For in vitro studies, differentiate monocyte-derived macrophages (MDMs) with M-CSF (25 ng/mL, 6 days) [28]
- Polarize macrophages with M1 (IFN-γ 10 ng/mL + LPS 100 ng/mL, 48h) or M2 (IL-4 20 ng/mL, 48h) stimuli
- Include viability staining (e.g., propidium iodide) to exclude dead cells during sorting
- Target cell recovery of 5,000-10,000 macrophages per sample for optimal sequencing depth
Library Preparation and Sequencing
- Use 10X Genomics Chromium platform for single-cell partitioning
- Target 20,000-50,000 reads per cell with 3' or 5' gene expression libraries
- Include unique molecular identifiers (UMIs) to correct for amplification bias
- Sequence to a depth ensuring detection of low-abundance transcripts
Computational Analysis Pipeline
- Process raw data using Cell Ranger or equivalent pipeline
- Perform quality control: retain cells with 300-6,000 detected genes, <10% mitochondrial reads [80]
- Normalize data using SCTransform (Seurat) or similar methods
- Conduct principal component analysis (PCA) and graph-based clustering
- Visualize using UMAP or t-SNE dimensionality reduction
- Annotate macrophage clusters using reference databases (CellMarker2.0) [81]
- Perform differential expression analysis (FindMarkers in Seurat, logfc.threshold = 0.25, min.pct = 0.25)
- Construct gene regulatory networks using pySCENIC [80]
- Analyze cell-cell communication with CellChat or CellPhoneDB [79]
Integration with Flow Cytometry Validation
Marker Validation Pipeline
- Identify significantly enriched surface markers from scRNA-seq clusters
- Select candidates with clear differential expression and commercial antibody availability
- Design polychromatic flow cytometry panels incorporating novel and canonical markers
- Include at least 2-3 redundant markers per subset to account for stimulus-induced changes [23]
- Validate panels using defined polarization conditions and tissue macrophages
Functional Correlations
- Correlate scRNA-seq-defined macrophage subsets with functional assays (phagocytosis, cytokine production)
- Validate putative subpopulation functions through sorted population analysis
- Establish transcription factor relationships with surface marker expression [80]
ScRNA-Seq Informed Flow Cytometry Panel Design
Optimized Marker Panels for Resolving Macrophage Heterogeneity
The integration of scRNA-seq findings with flow cytometry enables the development of refined panels that better capture macrophage diversity:
Table 2: ScRNA-Seq Informed Flow Cytometry Markers for Macrophage Subsets
| Marker Category | Specific Markers | Utility in Macrophage Subsetting | Validation Evidence |
|---|---|---|---|
| Novel Surface Markers | CD38, Gpr18, Fpr2 (M1); Egr2, c-Myc (M2) [38] | Improved discrimination beyond classical markers; CD38 labels 71% of M1 macrophages; Egr2 labels 70% of M2 macrophages | scRNA-seq with flow cytometry validation in murine models |
| Comprehensive Polarization Panel | F4/80, Arginase 1, TLR4, CD86, VEGF, CD14, CD206, MHC Class II, TNF-α [23] | Eleven-color panel with redundant markers to prevent misclassification due to stimulus-induced changes | Validation in RAW 264.7 cells with IFN-γ+LPS (M1), IL-4 (M2a), IL-10 (M2c) |
| Tissue-Resident Macrophage Markers | CD9, CD5 (B-1a cells) [82] | Identification of tissue-resident B-1a cells that spatially co-localize with and regulate macrophages | Parabiosis experiments confirming tissue residency |
| Metabolic/Functional Markers | SPP1, APOE, LYVE1, TREM2 [78] [77] | Resolution of functionally distinct foam cell and tissue-repair macrophages | scRNA-seq with functional validation in disease contexts |
Research Reagent Solutions for Macrophage Studies
Table 3: Essential Research Reagents for Integrated ScRNA-Seq and Flow Cytometry Workflows
| Reagent Category | Specific Products | Application | Technical Considerations |
|---|---|---|---|
| Cell Isolation | Gentle MACS Dissociator, collagenase IV, DNase I | Tissue processing for macrophage isolation | Gentle protocols preserve viability and surface epitopes |
| Polarization Cytokines | M-CSF, GM-CSF, IFN-γ, IL-4, IL-10, IL-13, LPS | In vitro polarization controls | Concentration and timing critical for reproducible polarization |
| scRNA-Seq Platforms | 10X Genomics Chromium, Parse Biosciences | Single-cell partitioning | 10X suitable for fresh cells; Parse for fixed samples |
| Antibody Panels | CD38-PE/Cy7, Egr2-Alexa647, CD206-BV711, CD86-BV605 [23] [38] | Polychromatic flow cytometry | Include viability dye and Fc block for clean results |
| Bioinformatics Tools | Seurat, Scanpy, Monocle, CellChat | scRNA-seq data analysis | Seurat most widely used; harmony for batch correction |
| Validation Assays |
Conclusion
Flow cytometry remains the cornerstone technique for macrophage polarization analysis, but requires carefully designed panels and standardized protocols to overcome reproducibility challenges. The integration of traditional marker-based staining with novel label-free methods and machine learning represents the future of high-content, high-throughput immunophenotyping. These advanced approaches will accelerate drug discovery by providing deeper insights into macrophage plasticity in cancer, chronic inflammation, and fibrosis, ultimately enabling the development of therapies that target specific macrophage subsets. Future directions should focus on standardizing panels across laboratories and translating in vitro findings to complex in vivo environments.
References
- 1. Macrophage polarization [https://en.wikipedia.org/wiki/Macrophage_polarization]
- 2. Editorial: Exploring the molecular mechanisms that regulate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12041800/]
- 3. M1/M2 Macrophage Polarization [https://bio-protocol.org/exchange/minidetail?id=6319488&type=30]
- 4. Macrophages in immunoregulation and therapeutics [https://www.nature.com/articles/s41392-023-01452-1]
- 5. Differences Between M1 and M2 Macrophages [https://www.criver.com/eureka/ask-scientist-whats-difference-between-m1-and-m2-macrophages]
- 6. miR-210 promotes the anti-inflammatory phenotype and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12361208/]
- 7. Disruption of CDK5 regulatory subunit 1, p35, limits ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1584791/full]
- 8. Publishing flow cytometry data - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2822558/]
- 9. The transition between M1 and M2 macrophage ... [https://www.nature.com/articles/s41419-025-07610-3]
- 10. Applications of Flow Cytometry in Drug Discovery and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11011675/]
- 11. Flow cytometry markers guide [https://www.abcam.com/en-us/knowledge-center/flow-cytometry/flow-cytometry-markers]
- 12. Flow Cytometric Analysis of Macrophages and Cytokines ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10650702/]
- 13. CD206 modulates the role of M2 macrophages in the origin of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10861823/]
- 14. An optimized flow cytometry panel for classifying ... [https://www.sciencedirect.com/science/article/abs/pii/S002217592200165X]
- 15. A flow cytometry approach reveals heterogeneity in ... [https://www.nature.com/articles/s41598-021-92784-x]
- 16. CDK8/19 inhibitor enhances arginase-1 expression in ... [https://www.sciencedirect.com/science/article/abs/pii/S0014299924005417]
- 17. Arginase 1: A novel macrophage marker for flow cytometry [https://www.thermofisher.com/blog/behindthebench/a1exf5-a-novel-arginase-1-monoclonal-antibody-for-flow-cytometry/]
- 18. P17-13 Optimization of Macrophage Polarization and ... [https://www.sciencedirect.com/science/article/abs/pii/S0378427425020247]
- 19. A generalized protocol for the induction of M2-like ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11964487/]
- 20. Macrophage Signaling Pathways in Health and Disease [https://pmc.ncbi.nlm.nih.gov/articles/PMC12171086/]
- 21. Reprogram to heal: Macrophage phenotypes as living ... [https://www.sciencedirect.com/science/article/abs/pii/S0024320525002358]
- 22. Dual roles and therapeutic targeting of tumor-associated ... [https://www.nature.com/articles/s41392-025-02325-5]
- 23. An optimized flow cytometry panel for classifying macrophage ... [https://pubmed.ncbi.nlm.nih.gov/36265578/]
- 24. Systematic approach in macrophage polarization ... [https://www.sciencedirect.com/science/article/abs/pii/S0022175921000144]
- 25. Biomarker identification associated with M2 tumor ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2025.1545608/full]
- 26. Development and Validation of Novel Biomarkers Related to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8276177/]
- 27. Regulation of macrophage polarization and plasticity by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5148158/]
- 28. Classification of M1/M2-polarized human macrophages by ... [https://www.nature.com/articles/s41598-017-08121-8]
- 29. IL-4 and IL-13 induce equivalent expression of traditional ... [https://www.nature.com/articles/s41598-023-46237-2]
- 30. Macrophage innate training induced by IL-4 and IL-13 ... [https://elifesciences.org/articles/74690]
- 31. of Human Whole Blood by Standardized... Deep Immunophenotyping [https://link.springer.com/article/10.1007/s43657-022-00092-9]
- 32. Comparative analysis of RT-qPCR, flow cytometry, and Di- ... [https://www.sciencedirect.com/science/article/pii/S2405580825003127]
- 33. of Human Whole Blood by Standardized... Deep Immunophenotyping [https://pubmed.ncbi.nlm.nih.gov/37325713/]
- 34. Human B Cell Panel – 10 | Thermo Fisher Scientific - CA color [https://www.thermofisher.com/ca/en/home/life-science/cell-analysis/flow-cytometry/flow-cytometry-learning-center/flow-cytometry-resource-library/flow-cytometry-multiplex-panels/human-b-cell-panel-10.html]
- 35. Autofluorescence Flow Cytometry for Macrophages Analysis [https://pubmed.ncbi.nlm.nih.gov/40926303/]
- 36. miR-210 promotes the anti-inflammatory phenotype and ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1633163/full]
- 37. Protocol to drive human monocyte-to-macrophage ... [https://www.sciencedirect.com/science/article/pii/S2666166722005469]
- 38. Novel Markers to Delineate Murine M1 and M2 Macrophages [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0145342]
- 39. A Method for Generation of Bone - Marrow from... Derived Macrophages [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0015263]
- 40. of Derivation from Macrophages | SpringerLink Mouse Bone Marrow [https://link.springer.com/protocol/10.1007/978-1-4939-9167-9_3]
- 41. Quantitative Proteomics of Polarised Macrophages Derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8869710/]
- 42. Trajectory analysis quantifies transcriptional plasticity ... [https://www.nature.com/articles/s41598-020-68766-w]
- 43. Global characterization of macrophage polarization ... [https://www.sciencedirect.com/science/article/pii/S2211124721014327]
- 44. M2 polarization of macrophage protects the lung cancer ... [https://www.nature.com/articles/s41420-025-02775-4]
- 45. Novel macrophage polarization model: from gene ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11114961/]
- 46. Regulation of Human Macrophage M1–M2 Polarization ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2017.01097/full]
- 47. Polarization of Human Monocyte-Derived Cells With ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2019.03157/full]
- 48. Polarization of M1 and M2 Human Monocyte-Derived Cells ... [https://pubmed.ncbi.nlm.nih.gov/33016941/]
- 49. Polarization of M1 and M2 Human Monocyte-Derived Cells ... [https://www.jove.com/v/61807/polarization-m1-m2-human-monocyte-derived-cells-analysis-with-flow]
- 50. An optimized flow cytometry protocol for simultaneous ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9957341/]
- 51. Different methods of detaching adherent cells and their ... [https://www.nature.com/articles/s41598-022-09605-y]
- 52. Flow Cytometry Protocols for Surface and Intracellular Antigen ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4396953/]
- 53. Sample Guidelines & Protocols | Flow Cytometry and Cell ... [https://www.uthsc.edu/research/institutional-cores/fccs/protocols.php]
- 54. Flow Cytometry Gating for Beginners [https://www.ptglab.com/news/blog/flow-cytometry-gating-for-beginners/?srsltid=AfmBOopO_woi2CVlJOitAYfBtDca9b9Vbb9fRBGcRkB6B0IuyAFuCsOn]
- 55. Flow Cytometry: An Overview - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5939936/]
- 56. Considerations for Flow Cytometry Gating | FACS Analysis [https://www.stemcell.com/considerations-for-facs-gating.html]
- 57. The Gate of Flow Cytometry To Improve Your FACS Data ... [https://expertcytometry.com/3-flow-cytometry-gates-that-will-improve-the-accuracy-of-your-facs-data-analysis/]
- 58. A consensus surface activation marker signature is partially ... [https://retrovirology.biomedcentral.com/articles/10.1186/1742-4690-10-155]
- 59. Identification of novel protein biomarkers of macrophage ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12576133/]
- 60. BestProtocols: Cell Preparation for Flow Cytometry Protocols | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/references/protocols/cell-and-tissue-analysis/protocols/cell-preparation-flow-cytometery.html]
- 61. Flow cytometry (FACS) staining protocol (Cell surface staining) [https://medicine.yale.edu/immuno/flowcore/protocols/analysis/]
- 62. Quantitative Flow Cytometry Measurements | NIST [https://www.nist.gov/programs-projects/quantitative-flow-cytometry-measurements]
- 63. Toxoplasma calcium-dependent protein kinases 3 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12090600/]
- 64. CFIm25-Dependent Alternative Polyadenylation in AKT2 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12262724/]
- 65. Validation of Hv1 channel functions in BV2 microglial cells ... [https://www.frontiersin.org/journals/cellular-neuroscience/articles/10.3389/fncel.2025.1624224/full]
- 66. Apoptotic vesicles of mesenchymal stem cells promote M2 ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04546-5]
- 67. Multi-omics profiling identifies M1 macrophage polarization ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12504312/]
- 68. Discovering Biomarkers for Chronic Sinusitis with Nasal ... [https://www.frontiersin.org/journals/bioinformatics/articles/10.3389/fbinf.2025.1613136/abstract]
- 69. Non-invasive classification of macrophage polarisation by ... [https://elifesciences.org/articles/77373]
- 70. Detecting immune cells with label-free two-photon ... [https://arxiv.org/html/2506.14449v1]
- 71. Label-free macrophage phenotype classification using ... [https://www.nature.com/articles/s41598-023-32158-7]
- 72. Label-free imaging of M1 and M2 macrophage phenotypes ... [https://elifesciences.org/articles/72819]
- 73. The role of M1/M2 macrophage polarization in primary ... [https://arthritis-research.biomedcentral.com/articles/10.1186/s13075-024-03340-7]
- 74. Label-Free Characterization of Macrophage Polarization ... [https://www.mdpi.com/1422-0067/24/1/824]
- 75. Investigating alveolar macrophages in an human ex vivo ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12399784/]
- 76. Dissecting macrophage heterogeneity in ulcerative colitis [https://pubmed.ncbi.nlm.nih.gov/41242266/]
- 77. Single-cell transcriptomic analysis reveals the ... [https://link.springer.com/article/10.1007/s12672-025-04002-z]
- 78. Single-cell profiling reveals inflammatory polarization of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10544225/]
- 79. Single-cell RNA sequencing analysis revealed the ... [https://www.nature.com/articles/s41598-025-10301-w]
- 80. Integrative analysis of single-cell and microarray data ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2025.1617834/full]
- 81. Single-cell RNA sequencing and in vitro validation reveal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12613610/]
- 82. Tissue-resident B cells orchestrate macrophage ... [https://www.nature.com/articles/s41467-023-42625-4]