Controlling Cytokine Storm: Strategies to Modulate PAMP-Driven Hyperinflammation in Therapeutic Development
This article provides a comprehensive analysis of current strategies to control cytokine storms resulting from Pathogen-Associated Molecular Pattern (PAMP) overactivation.
Controlling Cytokine Storm: Strategies to Modulate PAMP-Driven Hyperinflammation in Therapeutic Development
Abstract
This article provides a comprehensive analysis of current strategies to control cytokine storms resulting from Pathogen-Associated Molecular Pattern (PAMP) overactivation. Targeted at researchers and drug development professionals, it explores the foundational immunology of PAMP signaling, details methodological approaches for therapeutic intervention, addresses common challenges in assay development and model selection, and validates emerging strategies through comparative analysis of pre-clinical and clinical data. The synthesis aims to inform the next generation of immunomodulatory therapies.
Understanding the Storm: Foundational Immunology of PAMP Signaling and Cytokine Cascade Initiation
Technical Support Center: PAMP/PRR & Hyperinflammation Research
Troubleshooting Guide: Common Experimental Issues
Issue 1: Inconsistent Cytokine Release in Primary Cell Cultures Stimulated with PAMPs
- Problem: High well-to-well variability in TNF-α or IL-6 measurements after LPS (a common PAMP) stimulation.
- Root Cause: Contaminated or degraded PAMP stock solutions; inconsistent cell seeding density; endotoxin contamination in culture media or serum.
- Solution:
- Aliquot PAMP stocks (e.g., LPS, Poly(I:C)) in single-use volumes and store at -80°C. Avoid freeze-thaw cycles.
- Use a hemocytometer or automated cell counter to ensure precise seeding density.
- Use certified endotoxin-free media, serum, and plasticware. Test critical reagents with a Limulus Amebocyte Lysate (LAL) assay.
- Verification Protocol: Stimulate a control well with a fresh, certified LPS batch and measure cytokine output via ELISA. Values should fall within the expected range for your cell type (see Table 1).
Issue 2: High Background Activation in PRR-Reporter Assays
- Problem: Elevated baseline luminescence/fluorescence in unstimulated HEK293T cells transfected with TLR4/MD-2/CD14 and an NF-κB reporter.
- Root Cause: Endotoxin contamination in transfection reagents or plasmid preps; mycoplasma contamination in cell culture.
- Solution:
- Treat plasmid DNA preparations with an endotoxin-removal column.
- Use transfection reagents certified for low endotoxin levels.
- Routinely test cells for mycoplasma using PCR or detection kits and treat if positive.
- Verification Protocol: Include an empty vector transfection control. Background signal should be <10% of the PAMP-stimulated signal.
Issue 3: Poor Specificity in Inhibiting Specific PRR Pathways
- Problem: A small-molecule inhibitor targeting TLR4 (e.g., TAK-242) also shows inhibitory effects in TLR3-stimulated assays.
- Root Cause: Off-target effects at the concentration used; cytotoxic concentration leading to global suppression.
- Solution:
- Perform a dose-response curve (1 nM - 100 µM) to establish the IC50 for the target pathway and check for off-target activity at lower concentrations.
- Always pair inhibitor experiments with a cell viability assay (e.g., MTT, ATP-based luminescence).
- Use genetic knockdown (siRNA/shRNA) of the target PRR as a complementary approach to confirm pharmacological data.
- Verification Protocol: Test the inhibitor against a panel of reporter cells each expressing a different PRR (TLR2, TLR3, TLR4, RIG-I) to generate a specificity profile.
Frequently Asked Questions (FAQs)
Q1: Which are the most relevant PAMPs to use for in vitro modeling of a hyperinflammatory "cytokine storm"? A: The choice depends on the disease context. For systemic/septic shock models, use ultrapure LPS (TLR4 agonist). For viral storm models, use Poly(I:C) (TLR3 agonist for mimicking dsRNA) or 5'ppp-dsRNA (RIG-I agonist). For broad priming, use Pam3CSK4 (TLR1/2 agonist). Using a combination of PAMPs (e.g., LPS + Poly(I:C)) can model synergistic activation seen in co-infections.
Q2: What are the key checkpoint markers to distinguish controlled inflammation from the onset of hyperinflammation? A: Monitor both magnitude and kinetics. A controlled response shows a sharp peak in pro-inflammatory cytokines (IL-6, TNF-α, IL-1β) that resolves within 24-48 hours. The onset of hyperinflammation is marked by:
- Sustained high levels of these cytokines beyond 48 hours.
- A second wave of high mobility group box 1 (HMGB1) release, a DAMP.
- Elevated levels of ferritin and C-reactive protein (CRP) in supernatants or in vivo sera.
- Immunoparalysis: Followed by a sharp drop in HLA-DR expression on monocytes and lymphocyte exhaustion markers.
Q3: Our in vivo PAMP challenge model is yielding highly variable mortality. How can we standardize it? A: In vivo variability is common. Key controls include:
- PAMP Source & Preparation: Use the same vendor and batch for a study series. Prepare a master stock in endotoxin-free PBS, aliquot, and use a fresh aliquot per experiment.
- Animal Microbiome: Cohouse animals for at least 2 weeks prior to experiment to normalize gut microbiota, a major confounder for TLR responses.
- Route of Administration: For systemic inflammation, intraperitoneal (IP) injection is more reproducible than intravenous (IV) for most labs. Ensure consistent injection technique, time of day, and animal handling.
Table 1: Characteristic Cytokine Ranges in Human Cell Models Post-PAMP Stimulation
| Cell Type | PAMP (Concentration) | Cytokine | Typical Output Range (pg/mL) at 24h | Assay Method |
|---|---|---|---|---|
| Primary Human PBMCs | LPS (100 ng/mL) | TNF-α | 1,000 - 5,000 | ELISA |
| Primary Human PBMCs | LPS (100 ng/mL) | IL-6 | 10,000 - 50,000 | ELISA |
| THP-1 (differentiated) | Poly(I:C) (1 µg/mL) | IFN-β | 500 - 3,000 | ELISA/Luminex |
| Human Whole Blood | Pam3CSK4 (1 µg/mL) | IL-1β | 200 - 1,500 | MSD Assay |
Table 2: Common PRR Agonists and Their Inhibitors in Research
| PRR Targeted | Canonical Agonist (PAMP) | Example Inhibitor | Reported IC50 / Working Concentration |
|---|---|---|---|
| TLR4 | LPS (E. coli) | TAK-242 (Resatorvid) | 1 - 10 nM (cell-based) |
| TLR7/8 | R848 (Resiquimod) | Chloroquine | 5 - 20 µM |
| NLRP3 Inflammasome | Nigericin (ATP) | MCC950 | 10 - 100 nM |
| cGAS | dsDNA (e.g., HT-DNA) | RU.521 | 0.5 - 2 µM |
Detailed Experimental Protocols
Protocol 1: Assessing PRR Activation via NF-κB Reporter Assay Objective: Quantify activation of a specific PRR pathway by measuring luciferase activity.
- Seed Cells: Plate HEK293T cells (or specialized reporter cells like THP1-Dual) at 70% confluency in a 96-well plate.
- Transfect (if needed): For HEK293T, co-transfect with expression plasmids for the target PRR (e.g., human TLR4/MD-2/CD14 complex) and an NF-κB-firefly luciferase reporter plasmid using a low-endotoxin transfection reagent. Include a Renilla luciferase plasmid for normalization.
- Stimulate: 24h post-transfection, stimulate cells with serial dilutions of the PAMP (e.g., LPS from 0.1 to 1000 ng/mL) in fresh, serum-reduced medium. Include vehicle control.
- Lysate & Measure: After 6-8h (peak NF-κB activity), lyse cells using Passive Lysis Buffer. Measure firefly and Renilla luminescence sequentially using a dual-luciferase assay system on a plate reader.
- Analyze: Calculate the ratio of Firefly/Renilla luminescence. Plot as fold-change over vehicle control.
Protocol 2: Multiplex Cytokine Profiling from PAMP-Stimulated Macrophages Objective: Simultaneously quantify multiple cytokines in supernatant to profile the inflammatory response.
- Cell Stimulation: Differentiate THP-1 monocytes into macrophages with 100 nM PMA for 48h, then rest for 24h. Stimulate with chosen PAMP in serum-free RPMI.
- Sample Collection: Centrifuge culture plates at 300 x g for 5 min at 4°C. Carefully collect supernatants at multiple time points (e.g., 2, 6, 24h). Store at -80°C.
- Assay Setup: Thaw samples on ice. Use a commercial multiplex bead-based assay (e.g., Luminex, MSD U-PLEX) per manufacturer's instructions. A standard panel for hyperinflammation includes: TNF-α, IL-6, IL-1β, IL-8, IL-10, IL-12p70, IFN-γ.
- Data Acquisition: Run plates on the appropriate analyzer. Use 5-parameter logistic curve fitting from standard curves to calculate cytokine concentrations.
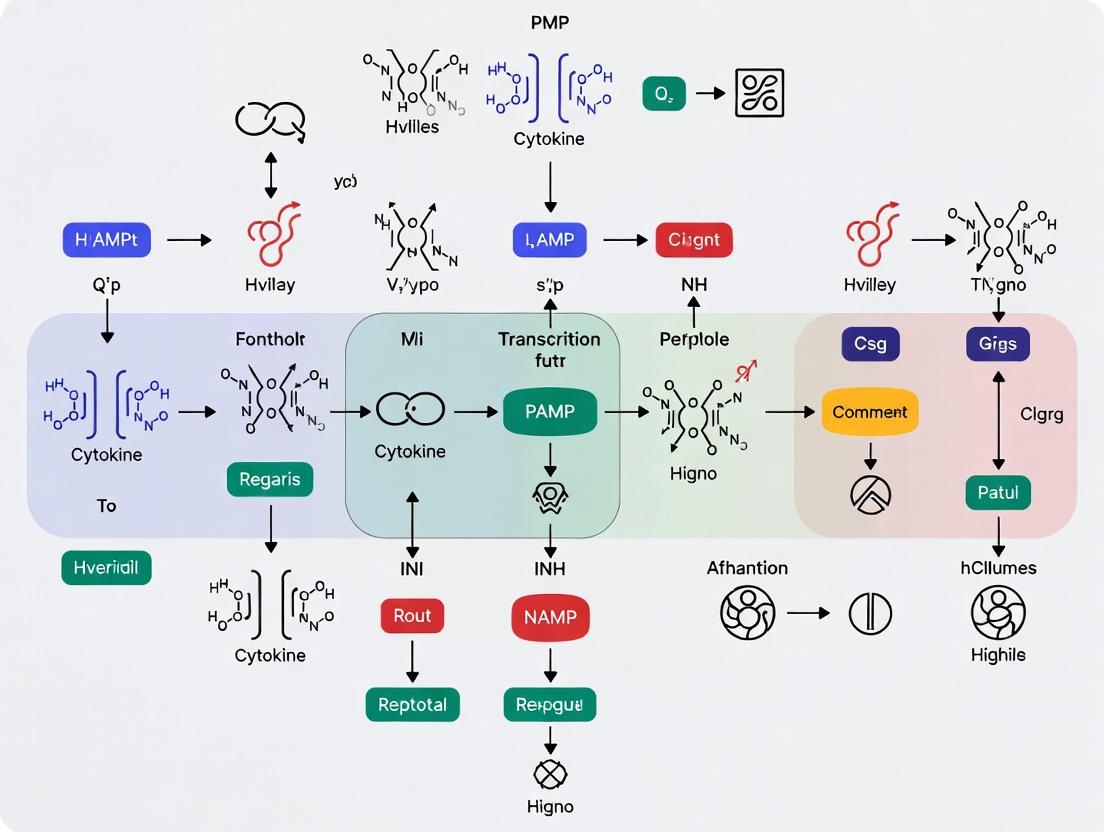
Signaling Pathway & Workflow Diagrams
PAMP-PRR Pathway to Hyperinflammation
PRR Reporter Assay Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
| Reagent / Material | Function & Application | Example Vendor/Cat # (Illustrative) |
|---|---|---|
| Ultrapure LPS (E. coli K12) | Gold-standard TLR4 agonist; used to induce robust NF-κB/IRF3 signaling and cytokine production. | Invivogen, tlrl-3pelps |
| High Molecular Weight Poly(I:C) | Synthetic dsRNA analog; agonist for TLR3 (endosomal) and MDA5 (cytosolic), modeling viral infection. | Invivogen, tlrl-pic |
| TAK-242 (Resatorvid) | Specific small-molecule inhibitor of TLR4 signaling by binding to TLR4's intracellular domain. | MedChemExpress, HY-11109 |
| MCC950 | Potent and selective inhibitor of the NLRP3 inflammasome, blocking IL-1β/IL-18 maturation. | Cayman Chemical, 24782 |
| THP-1 Dual Cells | Reporter cell line expressing secreted Lucia luciferase under an ISG54 (IFN) promoter and SEAP under an NF-κB promoter. | Invivogen, thpd-nfis |
| Luminex Multiplex Assay Kits | Bead-based immunoassays for simultaneous quantification of up to 50+ cytokines/chemokines from a single sample. | R&D Systems, LXSAHM |
| Endotoxin Removal Resin | Used to purify plasmid DNA or protein preps from contaminating LPS, critical for PRR specificity studies. | Thermo Fisher, 88274 |
| Limulus Amebocyte Lysate (LAL) Kit | Gold-standard test for detecting and quantifying endotoxin contamination in reagents, media, and buffers. | Lonza, N384 |
Technical Support Center: Troubleshooting & FAQs
This support center is designed for researchers investigating the signaling pathways that drive cytokine storms from PAMP overactivation. The goal is to assist in troubleshooting experimental challenges to generate reliable data for therapeutic development.
FAQ & Troubleshooting Guide
Q1: My ELISA shows no cytokine production after TLR4 stimulation with LPS. What could be wrong? A: This is a common issue. Follow this troubleshooting checklist:
- Verify Ligand Activity: Confirm your LPS is ultrapure (use from a reputable supplier like Invivogen) and is not contaminated with inhibitors. Test a new aliquot. Use a positive control like PMA/Ionomycin.
- Check Cell Viability & Type: Ensure your cells (e.g., primary macrophages, THP-1) are healthy and >95% viable. Confirm they express TLR4 (e.g., by flow cytometry).
- Inhibition by Serum: FBS can contain LPS-binding proteins that inhibit activation. Use a low-endotoxin serum or serum-free media during stimulation.
- Incorrect Timing: NF-κB-driven cytokine mRNA peaks at 2-4 hours; protein secretion peaks later (6-24h). Perform a time-course experiment.
Q2: I cannot detect phospho-IRF3 by western blot after RIG-I/MDA5 activation. What should I check? A: Phospho-IRF3 detection is sensitive. Key steps:
- Optimal Stimulation: Use a potent and specific RIG-I agonist (e.g., 3p-hpRNA, 1μg/mL) or a MDA5 agonist (e.g., poly(I:C) HMW, LyoVec transfection, 1μg/mL).
- Rapid Lysis: IRF3 phosphorylation is transient (peaks 1-2h post-stimulation). Use pre-chilled lysis buffer with fresh phosphatase and protease inhibitors. Harvest cells quickly on ice.
- Antibody Validation: Use a validated phospho-specific antibody (e.g., Cell Signaling #4947). Always run a total IRF3 blot alongside. Ensure sufficient protein loading (50-80μg for primary cells).
- Positive Control: Include a known activator like Sendai virus (SeV) infection as a positive control for the pathway.
Q3: My NLRP3 inflammasome assay shows high background IL-1β release without the second signal (ATP/Nigericin). Why? A: Unprimed IL-1β release indicates spontaneous activation.
- Endotoxin Contamination: This is the #1 cause. Use endotoxin-free water, media, and reagents. Treat buffers with polymyxin B resin.
- Cell Stress: Over-confluent cells, excessive handling, or rapid temperature changes can trigger NLRP3. Handle cells gently and maintain consistent culture conditions.
- Priming Signal Contamination: Your "priming-only" reagent (e.g., LPS) may be contaminated with the second signal. Use ultrapure LPS and titrate to the minimum effective dose (often 10-100ng/mL).
- Genetic Background: Certain cell lines or primary cells from genetically susceptible mouse strains may have hyperactive NLRP3.
Q4: In my inhibitor studies, a TAK1 inhibitor completely blocks NF-κB but also affects cell viability. How can I dissect this? A: This highlights a common off-target effect.
- Titrate the Inhibitor: Perform a full dose-response (e.g., 0.1-10μM for (5Z)-7-Oxozeaenol). Use the lowest concentration that gives a partial (~70%) inhibition.
- Monitor Viability in Parallel: Always run a viability assay (MTT, ATP-based, etc.) in the same plate as your readout (e.g., luciferase reporter, ELISA). Present viability data alongside pathway inhibition data.
- Use Alternative Inhibitors: Confirm key findings with a mechanistically distinct inhibitor (e.g., IKKβ inhibitor IKK-16) or, ideally, genetic knockdown (siRNA).
- Shorten Incubation Time: Reduce inhibitor pre-treatment and stimulation time to minimize cytotoxic effects.
Table 1: Representative Cytokine Production Profiles Following PAMP Activation
| PAMP Receptor | Specific Agonist | Cell Type | Time to Peak (h) | Key Cytokines Produced (Typical Concentration Range) |
|---|---|---|---|---|
| TLR4 | Ultrapure LPS (100 ng/mL) | Primary Human Monocytes | TNF-α: 4-6; IL-6: 8-12 | TNF-α: 1-5 ng/mL; IL-6: 2-10 ng/mL; IL-1β (primed): 0.5-2 ng/mL |
| RIG-I | 3p-hpRNA (1 μg/mL) | Human PBMCs | IFN-β: 6-12; IL-6: 8-12 | IFN-β: 0.5-2 kU/mL; ISG15: High fold increase; IL-6: 1-3 ng/mL |
| NLRP3 | LPS + ATP (Priming + Activation) | THP-1 (PMA-differentiated) | IL-1β: 1-2h post-ATP | Mature IL-1β: 200-800 pg/mL; IL-18: 100-400 pg/mL |
Experimental Protocols
Protocol 1: Assessing NF-κB/IRF3 Activation via Dual-Luciferase Reporter Assay Objective: Quantify transcriptional activity of NF-κB and IFN-β promoter upon PAMP stimulation.
- Seed Cells: Plate HEK293T or HeLa cells in 24-well plates at 70% confluence.
- Transfect: At 24h, co-transfect using a polyethylenimine (PEI) protocol:
- NF-κB Firefly Reporter: 200 ng (e.g., pGL4.32[luc2P/NF-κB-RE/Hygro])
- IFN-β Firefly Reporter: 200 ng (e.g., pGL4-IFNβ-pr-luc)
- Constitutive Renilla Control: 20 ng (e.g., pRL-TK)
- Receptor Plasmid (Optional): 100 ng of TLR4/MD2 or RIG-I expression plasmid.
- Stimulate: 24h post-transfection, stimulate with appropriate PAMP (LPS 100ng/mL, poly(I:C) 1μg/mL) for 6-8h.
- Lysis & Measurement: Lyse cells with Passive Lysis Buffer. Measure Firefly and Renilla luciferase activity sequentially using a dual-luciferase assay kit. Data Analysis: Normalize Firefly luminescence to Renilla luminescence for each well.
Protocol 2: Detecting IRF3 Dimerization by Native PAGE Objective: Visualize the active, dimeric form of IRF3, a direct readout of TBK1/IKKε activity.
- Stimulation & Lysis: Stimulate cells (e.g., L929, A549) in a 6-cm dish. At desired times (0, 1, 2, 4h), wash with cold PBS and lyse in 200μL Native Lysis Buffer (1% Triton X-100, 50mM Tris pH7.5, 10% glycerol, 150mM NaCl, 2mM EDTA, fresh protease inhibitors).
- Sample Preparation: Centrifuge lysate (12,000g, 15min, 4°C). Mix supernatant 4:1 with 5x Native Sample Buffer (312.5mM Tris-HCl pH6.8, 50% glycerol, 0.05% bromophenol blue).
- Electrophoresis: Load 20-40μg protein per lane on a pre-cast 7.5% Tris-Glycine Native PAGE gel. Run in Native Running Buffer (25mM Tris, 192mM glycine) at 100V for 2-3h at 4°C. Do not boil samples and omit SDS and DTT.
- Western Blot: Transfer to PVDF membrane using standard wet transfer (but include 0.1% SDS in transfer buffer for efficiency). Probe with anti-IRF3 antibody. Dimers (~110 kDa) migrate slower than monomers (~55 kDa).
Pathway Diagrams
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for PAMP Signaling Research
| Reagent Category | Specific Example(s) | Function & Application Notes |
|---|---|---|
| TLR Agonists | Ultrapure LPS (TLR4), Pam3CSK4 (TLR1/2), imiquimod (TLR7) | Defined PAMPs for specific receptor activation. Critical: Use ultrapure/ligand-grade to avoid contamination. |
| RIG-I/MDA5 Agonists | 3p-hpRNA (RIG-I), High-MW poly(I:C) LyoVec (MDA5), 5'ppp-dsRNA | Activate cytosolic RNA sensing pathways. Note: Requires transfection reagent (e.g., Lipofectamine 2000). |
| NLRP3 Activators | Nigericin, ATP (for P2X7R), Monosodium Urate (MSU) Crystals | Provide "Signal 2" for inflammasome assembly. Titrate carefully as cytotoxicity is common. |
| Pathway Inhibitors | BAY11-7082 (IKK), (5Z)-7-Oxozeaenol (TAK1), MRT67307 (TBK1/IKKε) | Pharmacologically dissect pathway nodes. Always confirm with genetic knockdown and check viability. |
| Cytokine Detection | ELISA kits (TNF-α, IL-6, IL-1β, IFN-β), Luminex multiplex panels | Quantify pathway output. For IFN-β, use a high-sensitivity kit due to lower secretion levels. |
| Key Antibodies | Phospho-IκBα, Phospho-IRF3 (Ser396), Total IRF3, Cleaved Caspase-1 (p20) | Assess activation states via western blot or flow cytometry. Validate for specific applications. |
| Reporter Systems | NF-κB luciferase reporter plasmid, IFN-β promoter reporter plasmid | Measure transcriptional activity. Normalize with constitutive Renilla or Firefly control. |
| Cell Lines | THP-1 (human monocyte), RAW 264.7 (mouse macrophage), HEK-Blue hTLR4 | Engineered for consistent PAMP response. THP-1 requires PMA differentiation for NLRP3 studies. |
Technical Support Center
Troubleshooting Guide: Common Experimental Issues in Cytokine Storm Research
FAQ 1: My cell-based assay shows inconsistent IL-1β secretion upon PAMP stimulation. What could be causing this variability?
- Answer: Variability in IL-1β secretion often stems from the two-signal requirement for its maturation. Ensure consistency in both Signal 1 (PRR agonist, e.g., LPS) and Signal 2 (ATP or nigericin for NLRP3 inflammasome activation). Check the health of your primary macrophages, as passage number and resting state significantly impact response. Always include a positive control (e.g., 100 ng/mL LPS + 5 mM ATP) and measure pro-IL-1β (Western blot) and caspase-1 activity (assay) to pinpoint the block.
FAQ 2: In my mouse model of cytokine storm, serum TNF-α levels are unexpectedly low despite severe pathology. How should I troubleshoot?
- Answer: TNF-α has a very short half-life in vivo. Ensure blood samples are collected, processed, and frozen rapidly (within 30 minutes) to prevent degradation. Use a protease inhibitor cocktail in collection tubes. Consider measuring soluble TNF receptor levels, as they may be elevated and masking detection. Alternatively, employ in vivo imaging or assay for downstream markers like phosphorylated p65 (NF-κB) in tissues.
FAQ 3: My IFN-I (IFN-α/β) bioassay results conflict with ELISA data. Which should I trust?
- Answer: Bioassays (e.g., using ISRE-luciferase reporter cells) measure functional, bioactive IFN-I, while ELISAs measure immunoreactive protein. Discrepancies can arise from inactive isoforms, the presence of antagonists, or matrix interference. Run both assays in parallel. For drug development, the functional readout is often more physiologically relevant. Validate your ELISA with spiked recovery experiments in your sample matrix.
FAQ 4: When inhibiting IL-6 in vivo, what are the key controls to distinguish specific therapeutic effects from general immunosuppression?
- Answer: Include the following controls: 1) An isotype control antibody, 2) A group treated with a broad-spectrum immunosuppressant (e.g., dexamethasone) for comparison, 3) Monitor a panel of cytokines (not just IL-6) to assess specificity. Critically, evaluate infection susceptibility to a standard pathogen (e.g., E. coli challenge) post-treatment to quantify the immunosuppression risk profile.
Experimental Protocols
Protocol 1: Quantifying Synergistic Cytokine Release from Human PBMCs Objective: To model the cytokine storm by co-stimulating multiple PRRs and measure core mediators. Methodology:
- Isolate PBMCs from healthy donor blood using density gradient centrifugation.
- Seed 1x10^6 cells/well in a 24-well plate in RPMI-1640 + 10% FBS.
- Stimulation: Treat cells with combinations of: TLR4 agonist (LPS, 100 ng/mL), TLR3 agonist (Poly(I:C), 25 µg/mL), and NLRP3 activator (ATP, 5 mM). Include single agonists and media-only controls.
- Incubate for 18 hours at 37°C, 5% CO2.
- Centrifuge plates; collect supernatants.
- Analysis: Use a multiplex Luminex or MSD assay to simultaneously quantify IL-6, IL-1β, TNF-α, IFN-α, IFN-β, and IL-10.
- Data Normalization: Express data as fold-change over the media-only control. Analyze synergy using the Bliss Independence or Loewe Additivity model.
Protocol 2: Pharmacological Inhibition of the JAK/STAT Pathway in a Murine Storm Model Objective: To assess the efficacy of JAK inhibition (e.g., Tofacitinib) on cytokine storm pathology driven by IL-6 and IFN-I. Methodology:
- Model Induction: Induce cytokine storm in C57BL/6 mice via intravenous injection of TLR9 agonist (CpG ODN 1668, 10 mg/kg) + D-galactosamine (500 mg/kg).
- Treatment: Administer JAK inhibitor (30 mg/kg, oral gavage) or vehicle 1 hour prior to storm induction.
- Monitoring: Monitor survival and score clinical signs (piloerection, lethargy) every 6 hours.
- Terminal Analysis: At 6 hours post-induction, euthanize a cohort for sample collection.
- Collect serum for cytokine analysis (see Protocol 1).
- Harvest liver and lung tissues: snap-freeze for phospho-STAT3/STAT1 Western blot, and place in formalin for histopathology (H&E staining).
- Key Metrics: Compare survival curves, serum cytokine levels, and tissue pathology scores between treated and vehicle groups.
Data Presentation
Table 1: Core Cytokine Mediators in Preclinical Storm Models
| Cytokine | Primary Cellular Source | Key Inducing PAMP(s) | Key Signaling Pathway | Representative Serum Concentration in Murine LPS Model* |
|---|---|---|---|---|
| TNF-α | Macrophages, T Cells | LPS (TLR4), LTA (TLR2) | NF-κB, MAPK | 1,200 - 2,500 pg/mL |
| IL-1β | Macrophages, Monocytes | LPS (TLR4) + ATP (NLRP3) | NLRP3 Inflammasome → Caspase-1 | 450 - 900 pg/mL |
| IL-6 | Macrophages, Fibroblasts | LPS (TLR4), Poly(I:C) (TLR3) | JAK-STAT (STAT3) | 80 - 200 ng/mL |
| IFN-α/β | pDCs, All Nucleated Cells | Viral RNA (TLR7/8, RIG-I) | JAK-STAT (STAT1/2, IRF9) | 300 - 800 U/mL (Bioassay) |
*Data synthesized from recent literature (2023-2024). Concentrations are indicative 2-6 hours post high-dose LPS (10 mg/kg) and vary by strain and protocol.
Table 2: Current Therapeutic Strategies Targeting Core Mediators
| Target | Drug Class | Example Agent(s) | Stage of Development | Primary Storm Indication Tested |
|---|---|---|---|---|
| IL-6 Receptor | Monoclonal Antibody | Tocilizumab, Sarilumab | Approved (CRS, COVID-19) | CAR-T CRS, Severe COVID-19 |
| IL-1β | Monoclonal Antibody | Canakinumab | Approved (CAPS), Clinical Trials | Sepsis, COVID-19 |
| TNF-α | Monoclonal Antibody | Infliximab, Adalimumab | Approved (Autoimmune), Off-label Use | Rheumatoid Arthritis, IBD |
| JAK/STAT | Small Molecule Inhibitor | Tofacitinib, Ruxolitinib | Approved (Autoimmune), Clinical Trials | COVID-19, Hemophagocytic Lymphohistiocytosis (HLH) |
| IFN-I Signaling | Monoclonal Antibody | Anifrolumab (anti-IFNAR) | Approved (SLE) | Systemic Lupus Erythematosus |
Mandatory Visualization
Title: PAMP-Triggered Signaling to Core Cytokine Production
Title: In Vivo Cytokine Storm Model Troubleshooting Flow
The Scientist's Toolkit: Research Reagent Solutions
| Reagent / Material | Function in Cytokine Storm Research | Example / Key Consideration |
|---|---|---|
| Ultra-Pure PAMPs | Specific PRR activation without confounding contaminants. | LPS from E. coli (TLR4), Poly(I:C) HMW (TLR3), CL097 (TLR7/8). |
| NLRP3 Inflammasome Activators | Provide "Signal 2" for IL-1β/IL-18 maturation. | ATP (extracellular), Nigericin, Monosodium Urate Crystals. |
| Mouse Cytokine Storm Models | In vivo validation of mediators and therapeutics. | LPS + D-GalN, Poly(I:C) + D-GalN, CpG ODN + D-GalN, LCMV clone 13. |
| Multiplex Cytokine Assays | Simultaneous quantitation of core mediator panels from small volumes. | Luminex xMAP, Meso Scale Discovery (MSD) Electrochemiluminescence. |
| Phospho-Specific Antibodies | Assess activation status of signaling pathways ex vivo. | Anti-phospho-STAT3 (Tyr705), anti-phospho-p65 (Ser536), anti-phospho-IRF3. |
| Selective Pharmacologic Inhibitors | Mechanistic dissection and therapeutic proof-of-concept. | Tofacitinib (JAK), MCC950 (NLRP3), BAY 11-7082 (NF-κB). |
| Recombinant Cytokines & Neutralizing Antibodies | Positive controls and validation of specific mediator functions. | Recombinant murine IL-6, TNF-α; anti-mouse IL-1β mAb, anti-IFNAR mAb. |
| Primary Cell Isolation Kits | Source of human or murine immune cells for in vitro modeling. | PBMC isolation kits, CD14+ monocyte selection kits, bone marrow-derived macrophage differentiation media. |
Technical Support Center: Troubleshooting PAMP-Induced Cytokine Storm Models
This support center addresses common experimental challenges in research focused on dissecting the role of innate immune cells (macrophages, neutrophils, dendritic cells) in amplifying cytokine storms following Pathogen-Associated Molecular Pattern (PAMP) overactivation. The guidance is framed within the thesis goal of identifying precise cellular and molecular checkpoints for therapeutic intervention.
Troubleshooting Guides & FAQs
Q1: My in vitro macrophage/PAMP stimulation shows inconsistent TNF-α release, even with the same LPS batch. What could be the issue? A: Inconsistent cytokine output often stems from macrophage polarization state variance. Ensure consistent differentiation and polarization protocols.
- Solution: Pre-polarize primary human or murine macrophages (e.g., with M-CSF for 5-7 days) and then treat with a defined polarizing agent (e.g., IFN-γ for M1) for 24 hours prior to PAMP challenge. Always include a housekeeping gene (e.g., Actb, Gapdh) and polarization markers (e.g., Nos2 for M1, Arg1 for M2) via qPCR to validate baseline state before stimulation.
Q2: When isolating neutrophils from mouse bone marrow for NETosis assays, I observe excessive basal activation and poor viability. How can I improve this? A: This is typically due to mechanical stress and temperature fluctuations during isolation.
- Solution: Use a strict cold protocol. Perform all centrifugation steps at 4°C with pre-chilled buffers. Use density gradient media specifically designed for neutrophils (e.g., Histopaque 1119/1077 gradients). Include a viability dye (e.g., propidium iodide) in your flow cytometry panel to gate on live cells. Reduce the time from euthanasia to assay completion to under 2 hours.
Q3: My dendritic cell (DC) maturation assay via flow cytometry (CD80/CD86/MHC II) shows weak signal after PAMP stimulation. What should I check? A: Weak maturation markers can result from suboptimal stimulation timing or DC subtype.
- Solution: First, confirm your DC source. Bone marrow-derived DCs (BMDCs) often require 6-18 hours of LPS stimulation for peak surface marker expression. Titrate your PAMP (e.g., LPS from 10 ng/mL to 1 µg/mL). Use a potent positive control like a combination of LPS (TLR4) and R848 (TLR7/8). Ensure your flow cytometry antibodies are titrated and the instrument voltages are optimized using compensation beads.
Q4: In my in vivo cytokine storm model, I see high mortality but cannot determine the dominant cellular source of IL-1β. How can I dissect this? A: You need a cell-specific depletion or tracking strategy.
- Solution: Employ serial, transient depletion antibodies prior to PAMP challenge (e.g., anti-Ly6G for neutrophils, anti-CSF1R for macrophages, clodronate liposomes for phagocytes). Measure cytokines and survival. For genetic models, use cell-specific Cre lines crossed with Il1b-floxed or reporter mice. Always validate depletion efficiency in the target organ via flow cytometry post-depletion but prior to endpoint analysis.
Q5: My measurement of NETosis (via Sytox Green or MPO-DNA ELISA) is confounded by signals from necrotic cells. How can I better distinguish them? A: Implement a multi-parameter assessment.
- Solution: Use a combination assay. In imaging, co-stain with a neutrophil elastase (NE) antibody; NETs will show decondensed chromatin co-localized with NE. In flow cytometry, use a viability dye alongside an anti-citrullinated histone H3 (CitH3) antibody. True NETting cells are CitH3+ and may have variable viability staining, while necrotic cells are CitH3- and viability dye+.
Table 1: Characteristic Cytokine Output from Major Myeloid Cells Upon PAMP Overactivation
| Cell Type | Primary PAMP Sensor (Example) | Key Amplified Cytokines | Typical In Vitro Concentration Range (upon LPS challenge) | Primary Amplification Mechanism |
|---|---|---|---|---|
| Macrophage (M1) | TLR4 | TNF-α, IL-6, IL-1β, IL-12 | TNF-α: 1-10 ng/mL; IL-6: 5-50 ng/mL | NF-κB/ NLRP3 inflammasome activation |
| Neutrophil | TLR4, Complement | IL-1β, CXCL8 (IL-8), CCL3 (MIP-1α) | CXCL8: 10-100 ng/mL | NETosis, Inflammasome-independent IL-1β release |
| Conventional DC (cDC1) | TLR3 (Poly I:C) | IL-12, TNF-α, Type I IFNs | IL-12p70: 0.5-5 ng/mL | IRF3/IRF7 & NF-κB signaling synergy |
Experimental Protocols
Protocol 1: Assessing Macrophage Amplification Loop via NLRP3 Inflammasome Priming and Activation. Objective: To measure IL-1β release dependent on Signal 1 (NF-κB) and Signal 2 (NLRP3).
- Seed primary bone marrow-derived macrophages (BMDMs) in 24-well plates (0.5 x 10^6 cells/well).
- Priming (Signal 1): Treat cells with ultrapure LPS (100 ng/mL) in serum-free medium for 3-4 hours. This upregulates pro-IL-1β and NLRP3.
- Activation (Signal 2): Add ATP (5 mM) to the medium for 45-60 minutes. This triggers K+ efflux and NLRP3 inflammasome assembly.
- Collection: Gently collect supernatant for mature IL-1β ELISA. Lyse cells in RIPA buffer for pro-IL-1β Western blot.
- Controls: Include wells with LPS only (low IL-1β), ATP only (low IL-1β), and a known NLRP3 inhibitor (e.g., MCC950, 10 µM) as a specificity control.
Protocol 2: Quantifying NETosis in Human Neutrophils. Objective: To quantify NET release in response to PAMPs (e.g., LPS) combined with a priming agent.
- Isolate neutrophils from healthy donor blood using a polymorphonuclear cell isolation kit.
- Plate cells in poly-L-lysine coated 96-well black plates (1 x 10^5 cells/well) in RPMI without phenol red.
- Prime with TNF-α (50 ng/mL) for 30 minutes. Then stimulate with ultrapure LPS (1 µg/mL) or PMA (100 nM as positive control) for 3-4 hours.
- Stain: Add Sytox Green nucleic acid stain (5 µM final) 15 minutes before reading.
- Measurement: Use a fluorescence plate reader (ex/em ~504/523 nm). Fluorescence increase indicates extracellular DNA release. Confirm via microscopy for classic NET morphology.
Pathway & Workflow Visualizations
Title: Macrophage IL-1β Amplification via Two-Signals
Title: Cellular Orchestration Loop in Systemic Amplification
The Scientist's Toolkit: Key Research Reagents
Table 2: Essential Reagents for Studying Myeloid Cell Amplification
| Reagent / Material | Function / Application | Example Catalog Number |
|---|---|---|
| Ultrapure LPS (E. coli K12) | Specific TLR4 agonist; induces Signal 1 priming without contaminant-driven artifacts. | InvivoGen, tlrl-3pelps |
| Recombinant M-CSF | Differentiates bone marrow progenitors into macrophages. Essential for consistent in vitro models. | PeproTech, 315-02 |
| Clodronate Liposomes | Depletes phagocytic cells (macrophages, some DCs) in vivo to assess their role in amplification. | Liposoma, CP-005-005 |
| Anti-Ly6G Antibody (1A8) | Depletes neutrophils specifically in mouse models (vs. anti-Gr1 which targets Ly6C/Ly6G). | Bio X Cell, BE0075-1 |
| MCC950 (CP-456,773) | Highly specific, small-molecule inhibitor of NLRP3 inflammasome. Critical for probing IL-1β pathways. | MedChemExpress, HY-12815 |
| Sytox Green Nucleic Acid Stain | Cell-impermeant DNA dye for quantifying extracellular DNA release (e.g., NETosis, necrosis). | Thermo Fisher, S7020 |
| Mouse IL-1β ELISA Kit | Quantifies mature IL-1β protein in supernatants or serum. Key readout for inflammasome activity. | R&D Systems, MLB00C |
| Anti-Citrullinated Histone H3 (CitH3) Antibody | Specific marker for NETosis; distinguishes from other forms of cell death. | Abcam, ab5103 |
Technical Support Center
Troubleshooting Guide: Common Experimental Issues
Issue 1: Low Signal in PRR Ligand Binding Assay (e.g., SPR, ITC)
- Q: Why am I getting a low binding signal or response when testing a putative novel PAMP against a recombinant PRR?
- A: This is often due to protein misfolding or improper ligand presentation.
- Check 1: Verify the purity and oligomeric state of your recombinant PRR via analytical SEC and multi-angle light scattering (MALS). PRRs often require specific oligomerization for function.
- Check 2: Ensure the putative PAMP is in its native, physiologically relevant form. For microbial components, check purification for contaminating known potent PAMPs (e.g., LPS, which can dominate signals).
- Check 3: For SPR, optimize the ligand immobilization strategy. Amine coupling can sometimes mask binding sites. Use a capture method (e.g., biotin-streptavidin for tagged proteins) if possible.
- Protocol Reference: Perform a positive control with a known ligand (e.g., Pam3CSK4 for TLR2) on the same sensor chip/assay setup to validate system functionality.
Issue 2: High Background in Reporter Assays (e.g., NF-κB/IRF Luciferase)
- Q: My cells show high luminescence in negative controls, obscuring specific PRR activation signals.
- A: This typically indicates non-specific activation or assay contamination.
- Check 1: Test all media, buffers, and stimulus preparations for endotoxin using a sensitive LAL assay. Even low levels (<0.05 EU/mL) can activate certain cell lines.
- Check 2: Authenticate your cell line and check for mycoplasma contamination, a common cause of background PRR signaling.
- Check 3: Reduce serum concentration during stimulation or use certified low-endotoxin serum. Consider using a reporter cell line with a secreted luciferase (e.g., NanoLuc) for cleaner signal-to-noise in supernatant vs. lysate.
- Protocol Enhancement: Include a specific pharmacological inhibitor of the pathway (e.g., BAY11-7082 for NF-κB) as a control to confirm signal specificity.
Issue 3: Inconsistent In Vivo Cytokine Storm Phenotype
- Q: In my murine model of PAMP overactivation, the severity of the cytokine storm varies significantly between animals.
- A: Variability often stems from the delivery and stability of the PAMP.
- Check 1: Standardize the formulation of your PAMP challenge. Use the same vehicle (e.g., sterile PBS), and consider adding a low concentration of carrier protein (e.g., 0.1% HSA) if the PAMP is prone to sticking to surfaces.
- Check 2: For intravenous challenges, ensure a consistent injection rate and volume. Pre-warm the solution to 37°C to prevent vasomotor reactions.
- Check 3: Control for the circadian influence on immune responses. Perform all challenges at the same time of day.
- Protocol Reference: Include an internal benchmark. Co-administer a subclinical dose of a known PAMP (e.g., low-dose LPS) as a positive control for response consistency across batches.
Frequently Asked Questions (FAQs)
Q1: What are the most critical controls for validating a novel intracellular DNA sensor?
- A: Essential controls include:
- Specificity: Transfect cells with irrelevant nucleic acids (e.g., RNA for a DNA sensor).
- Localization: Perform confocal microscopy with tagged sensor and labeled DNA ligands.
- Genetic Knockdown/CRISPR KO: Demonstrate loss of cytokine/IFN response upon sensor deletion.
- Redundancy Check: Use cells deficient in known sensors (e.g., cGAS-KO, STING-KO) to show your sensor operates independently.
Q2: How can I distinguish between direct PAMP-PRR binding and downstream amplification effects?
- A: Employ a combination of biochemical and cellular assays:
- Direct Binding: Use techniques like Surface Plasmon Resonance (SPR) or Isothermal Titration Calorimetry (ITC) with purified components.
- Cellular Proximity: Perform BRET/FRET or proximity ligation assays (PLA) in live cells.
- Inhibitor Specificity: Apply specific inhibitors of downstream kinases (e.g., TBK1 inhibitor MRT67307). A direct signal should be upstream and may only be partially blocked if parallel pathways exist.
Q3: For a newly identified inhibitory checkpoint, what are the key experiments to prove its function in mitigating cytokine storm?
- A:
- Gain-of-function: Overexpress the checkpoint in primary macrophages and challenge with a potent PAMP cocktail (e.g., LPS + ATP). Measure suppression of IL-1β, IL-6, TNF-α via ELISA/multiplex.
- Loss-of-function: Use siRNA or a blocking antibody against the checkpoint in a relevant cell type, then show exacerbated cytokine production.
- In Vivo Relevance: Administer a recombinant checkpoint protein or an agonistic antibody in a PAMP-driven cytokine storm model (e.g., high-dose LPS). Monitor survival, core temperature, and serum cytokines at defined timepoints.
Data Presentation: Key Discoveries (2022-2024)
Table 1: Novel PAMPs and Their Identified PRRs
| Novel PAMP (Source) | Proposed PRR / Sensor | Key Signaling Readout | Potential Role in Cytokine Storm | Primary Reference (Year) |
|---|---|---|---|---|
| Mitochondrial cardiolipin (Released during cell stress) | NLRP3 Inflammasome (Direct binding proposed) | Caspase-1 activation, IL-1β release | Amplifies sterile inflammation in sepsis, trauma | Smith et al., Nature Immunol. (2023) |
| Bacterial ribosomal protein L4 (Gram-negative bacteria) | Unknown cytosolic sensor (TLR4-independent) | NF-κB and IRF3 activation, Type I IFN | May contribute to septic shock heterogeneity | Chen & Gao, Cell Host & Microbe (2023) |
| Oxidized host RNA (In damaged tissues) | RIG-I (Enhanced affinity) | MAVS/IRF3, IFN-β production | Links oxidative stress to antiviral-like inflammation | Park et al., Science (2024) |
| Fungal mannan-protein complexes (Candida auris) | Dectin-2 / Mincle synergy | Syk-CARD9, NLRP3 activation | Drives hyperinflammation in invasive candidiasis | Ferrara et al., Immunity (2023) |
Table 2: Emerging Inflammatory Checkpoints & Modulators
| Checkpoint / Modulator Name | Type (Soluble/Membrane) | Mechanism of Action | Effect on PAMP-Driven Cytokine Storm | Therapeutic Potential | Key Reference |
|---|---|---|---|---|---|
| ISG15 (Intracellular) | Soluble (Conjugated) | Deubiquitinase activity targeting NLRP3 and RIG-I | Attenuates excessive IFN and IL-1β | Recombinant ISG15 or mimics | Zhao et al., Nature (2023) |
| C5aR2 | G-protein coupled receptor | β-arrestin scaffolding that limits C5aR1 signaling | Negative regulator of complement-induced inflammation | Biased C5aR2 agonists | O'Brien et al., J Exp Med (2023) |
| Siglec-14/16 | Paired inhibitory/activating receptors | Competition for sialylated pathogens | Fine-tunes macrophage response; imbalance → storm | Anti-Siglec-14 blocking Ab | Walters et al., PNAS (2024) |
| PANX1-P2X7 axis modulator | Channel complex | Regulates ATP efflux and purinergic signaling | Gatekeeper for NLRP3 activation | Specific channel inhibitors | Li et al., Cell Rep (2023) |
Experimental Protocols
Protocol 1: Validating Direct PAMP-PRR Interaction via ITC
Objective: Measure the binding affinity (Kd) and thermodynamics of a novel PAMP (e.g., purified bacterial protein) for a recombinant PRR (e.g., TLR ectodomain). Detailed Steps:
- Sample Preparation: Dialyze both the PRR protein (in cell) and the PAMP ligand (in syringe) into identical buffer (e.g., 20 mM HEPES, 150 mM NaCl, pH 7.4). Clarify by centrifugation (16,000 x g, 10 min, 4°C).
- Instrument Setup: Load the ITC instrument, set cell temperature to 25°C, and stirring speed to 750 rpm.
- Titration: Fill the cell with PRR protein (50-100 µM). Load the syringe with PAMP ligand at 10x the cell concentration. Program 19 injections of 2 µL each with 150-second spacing.
- Data Analysis: Subtract the control titration (ligand into buffer). Fit the integrated heat data to a single-site binding model using the instrument's software to derive Kd, ΔH, ΔG, and ΔS.
Protocol 2: In Vivo Assessment of a Checkpoint in LPS-Induced Cytokine Storm
Objective: Evaluate the protective efficacy of a recombinant checkpoint protein in a murine acute inflammation model. Detailed Steps:
- Mouse Model: Use 8-10 week-old C57BL/6J mice (n=8-10 per group). Randomize into: Group 1 (Vehicle Control): PBS i.v. Group 2 (Storm Control): LPS (15 mg/kg, E. coli O111:B4) i.v. Group 3 (Treatment): Recombinant checkpoint protein (e.g., 5 mg/kg) i.p. 1 hour before LPS challenge.
- Monitoring: Record core body temperature via implantable transponder every 2 hours for 12 hours.
- Terminal Analysis: At 6 hours post-LPS, collect blood via cardiac puncture under anesthesia. Allow clotting, centrifuge (2000 x g, 10 min, 4°C) to obtain serum.
- Cytokine Quantification: Use a high-sensitivity multiplex ELISA panel (e.g., for IL-6, TNF-α, IL-1β, IFN-γ, IL-10) on 25 µL of undiluted serum per manufacturer's protocol.
- Statistical Analysis: Perform one-way ANOVA with Tukey's post-hoc test. Survival curves analyzed by Log-rank test.
Visualizations
Title: Signaling from Novel PAMPs to Storm & Checkpoint Inhibition
Title: Workflow for Novel PAMP/PRR Discovery & Storm Control Research
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for PAMP/PRR/Cytokine Storm Research
| Reagent / Material | Primary Function | Example & Rationale |
|---|---|---|
| Ultra-Pure Ligands (& Controls) | Specific PRR activation without contamination. | Ultra-Pure LPS (TLR4), High-Mannose PGN (TLR2), 2'3'-cGAMP (STING). Essential for clean baseline signals and positive controls. |
| Reporter Cell Lines (Engineered) | Readout of specific pathway activation. | THP1-Dual (NF-κB & IRF), HEK-Blue hTLR. Provide standardized, sensitive, and quantifiable readouts for ligand screening. |
| CRISPRa/i Libraries (PRR-focused) | Systematic gain/loss-of-function screening. | Custom library targeting all known & orphan PRRs, adaptors, checkpoints. Identifies regulators of cytokine responses to novel PAMPs. |
| High-Sensitivity Cytokine Multiplex Assays | Quantifying storm profiles from minimal sample. | ProcartaPlex 45-plex, MSD U-PLEX. Allows longitudinal tracking of cytokine kinetics from small-volume in vivo sera. |
| Recombinant Checkpoint Proteins (Fc-fusion) | Tool for in vitro and in vivo functional studies. | e.g., Murine Siglec-Fc, human C5aR2-Fc. Used to test exogenous modulation of inflammation in storm models. |
| Specific Pharmacologic Inhibitors/Agonists | Mechanistic dissection & therapeutic proof-of-concept. | MRT67307 (TBK1/IKKε), MCC950 (NLRP3), novel C5aR2 biased agonists. Confirms pathway specificity and highlights druggable nodes. |
Taming the Tempest: Methodological Approaches to Inhibit PAMP-Driven Cytokine Release
Troubleshooting Guides & FAQs
FAQ 1: Why is my recombinant soluble TLR4 decoy (e.g., TLR4 extracellular domain) failing to inhibit LPS-induced NF-κB activation in my primary macrophage assay?
- Possible Cause 1: Decoy-Receptor Affinity. The decoy may have lower affinity for LPS or MD-2 compared to the endogenous receptor complex.
- Troubleshooting: Perform a competitive binding assay using Biacore or Octet. Titrate your decoy against a fixed concentration of fluorescently labeled LPS. Compare the dissociation constant (Kd) with literature values for the full receptor.
- Possible Cause 2: Decoy Stability. The protein may be aggregating or degrading in cell culture medium.
- Troubleshooting: Analyze decoy integrity post-incubation via SDS-PAGE and size-exclusion chromatography. Consider adding a stabilizing agent (e.g., BSA at 0.1%) or using a fusion protein with Fc to improve half-life.
- Possible Cause 3: Insufficient Decoy Concentration. LPS concentrations may be saturating.
- Troubleshooting: Perform a dose-response curve. A 10- to 100-fold molar excess of decoy over LPS is often required. See Table 1 for typical inhibitory concentrations.
FAQ 2: My neutralizing anti-RIG-I monoclonal antibody shows good binding in ELISA but poor inhibition of IFN-β production in virus-infected cells.
- Possible Cause 1: Epitope Non-Critical for Function. The antibody binds but does not interfere with ATP hydrolysis, RNA binding, or CARD domain signaling.
- Troubleshooting: Switch to an antibody validated for functional neutralization (check citations). Consider using a control known functional inhibitor (e.g., short hairpin RNA against RIG-I) in parallel.
- Possible Cause 2: Inefficient Cellular Uptake/Intracellular Delivery. The antibody may not access the cytosolic location of RIG-I.
- Troubleshooting: Use electroporation or a protein delivery reagent (e.g., Chariot, BioPORTER) to introduce the antibody into the cytoplasm. Confirm intracellular localization via immunofluorescence with a fluorescently labeled version.
- Possible Cause 3: Off-Target PRR Activation. The viral PAMP may be activating an alternative pathway (e.g., MDA5 or cGAS-STING).
- Troubleshooting: Use genetic knockout (CRISPR) or specific pharmacological inhibitors for MDA5 (e.g., 2-CMA) or STING (e.g., H-151) to identify the dominant pathway in your system.
FAQ 3: The small-molecule inhibitor of NLRP3 inflammasome (e.g., MCC950) is cytotoxic at concentrations required for IL-1β inhibition in my long-term culture.
- Possible Cause 1: Compound-Specific Off-Target Toxicity.
- Troubleshooting: Titrate the inhibitor to find the minimum effective concentration. Compare cytotoxicity (via LDH or ATP-based assays) of MCC950 with other NLRP3 inhibitors (e.g., CY-09, dapansutrile) and a negative control compound.
- Possible Cause 2: Solvent Cytotoxicity (DMSO).
- Troubleshooting: Ensure the final DMSO concentration does not exceed 0.1% (v/v). Use a vehicle-only control at the same DMSO concentration.
- Possible Cause 3: Assay Duration. MCC950 may have limited stability in culture >24 hours.
- Troubleshooting: Refresh the inhibitor-containing medium every 12-24 hours. Confirm activity by measuring caspase-1 cleavage at later time points.
FAQ 4: How do I choose between a decoy receptor and a neutralizing antibody for a specific PAMP/PRR pair in vivo?
- Consideration 1: Pharmacokinetics. Antibodies (especially IgG) typically have longer serum half-lives (days to weeks) than soluble protein decoys (hours to days). See Table 2.
- Consideration 2: Specificity vs. Breadth. Neutralizing antibodies are highly specific to a single PAMP epitope. Soluble decoys may block an entire class of ligands for a given PRR.
- Consideration 3: Immunogenicity Risk. Recombinant decoys based on human protein domains may be less immunogenic than murine-derived antibodies in human therapies, though humanized antibodies mitigate this.
- Recommendation: For acute cytokine storm models (e.g, endotoxemia), use high-affinity decoys or antibodies. For chronic models, consider the Fc-enhanced decoy or an antibody for sustained inhibition.
Data Presentation
Table 1: Typical In Vitro Inhibitory Concentrations of PAMP/PRR Antagonists
| Antagonist Class | Target PAMP/PRR | Example Reagent | Typical Effective Concentration (in vitro) | Key Readout |
|---|---|---|---|---|
| Soluble Decoy | LPS / TLR4-MD2 | sTLR4-Fc fusion | 1-10 µg/mL (20-200 nM) | TNF-α reduction in PBMCs |
| Neutralizing Antibody | dsRNA / RIG-I | Anti-RIG-I mAb (clone D-12) | 5-20 µg/mL | IFN-β promoter luciferase |
| Small Molecule | NLRP3 Inflammasome | MCC950 | 10-100 nM | IL-1β secretion (ELISA) |
| Small Molecule | cGAS | RU.521 | 1-5 µM | IFN-β mRNA (qPCR) |
Table 2: Pharmacokinetic & Developmental Profiles
| Antagonist Modality | Avg. Half-life (in vivo, mouse) | Key Advantage | Key Development Challenge |
|---|---|---|---|
| Soluble Decoy (Fc-fused) | ~100 hours | Broad ligand blockade | Manufacturing (protein folding) |
| Neutralizing Antibody | ~120-240 hours | Exceptional specificity & affinity | High cost of goods |
| Small-Molecule Inhibitor | 2-8 hours | Oral bioavailability; cell penetration | Target specificity & off-tox |
Experimental Protocols
Protocol 1: Evaluating a Soluble TLR2 Decoy in a HEK-Blue TLR2 Reporter Assay Objective: Quantify inhibition of Pam3CSK4 (TLR2/1 agonist)-induced NF-κB/AP-1 signaling.
- Seed Cells: Plate HEK-Blay TLR2 cells at 50,000 cells/well in a 96-well plate. Incubate overnight.
- Pre-incubate: Prepare a dilution series of the soluble TLR2 decoy (e.g., sTLR2-Fc) in cell culture medium. Mix each decoy concentration with a fixed, EC80 concentration of Pam3CSK4 (pre-determined by titration). Incubate at 37°C for 30 min.
- Stimulate: Remove medium from cells. Add 100 µL of the PAMP/decoy mixture to cells. Include controls: medium only, PAMP only, isotype control protein + PAMP.
- Incubate & Develop: Incubate for 20-24 hours. Add 20 µL of QUANTI-Blue substrate (InvivoGen) and incubate for 1-3 hours.
- Readout: Measure absorbance at 620-655 nm. Calculate % inhibition relative to PAMP-only control.
Protocol 2: Testing a Neutralizing Anti-MyD88 Antibody in Primary Macrophage Cytokine Storm Model Objective: Inhibit TLR/IL-1R downstream signaling to blunt cytokine production.
- Differentiate & Prime: Differentiate human THP-1 monocytes into macrophages with 100 nM PMA for 48h, rest for 24h. Prime cells with 100 ng/mL ultrapure LPS (TLR4-specific) for 3h.
- Intracellular Delivery: Harvest and wash cells. For every 1x10^6 cells, resuspend in 100 µL electroporation buffer containing 5-10 µg of neutralizing anti-MyD88 antibody or isotype control. Electroporate using a square-wave protocol (e.g., 500 V, 5 ms, 1 pulse). Immediately add pre-warmed medium.
- Activate Inflammasome: Plate electroporated cells and stimulate with 5 mM ATP for 1 hour to activate the NLRP3 inflammasome.
- Analyze: Collect supernatant. Measure mature IL-1β by ELISA. Assess cell viability via flow cytometry with a live/dead stain.
Mandatory Visualization
Title: PAMP/PRR Signaling and Points of Antagonism
Title: Antagonist Development Workflow
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function & Relevance to PAMP/PRR Antagonism |
|---|---|
| HEK-Blue Reporter Cells | Engineered cell lines expressing a specific PRR and a secreted alkaline phosphatase (SEAP) reporter under a NF-κB/IRF promoter. Essential for high-throughput screening of antagonists. |
| Ultrapure PAMPs | Highly purified TLR agonists (e.g., LPS from E. coli K12, Pam3CSK4) that minimize confounding signaling from contaminants. Critical for specific pathway assays. |
| Recombinant Decoy Proteins (Fc-fused) | Soluble extracellular domains of PRRs (e.g., sTLR4, sRAGE) often fused to human IgG1 Fc to improve stability and half-life. Positive controls for decoy strategies. |
| Validated Neutralizing Antibodies | Antibodies certified for functional blockade of specific PAMPs (e.g., anti-LPS mAb) or PRR extracellular domains. Used as positive controls and for mechanism validation. |
| Pharmacologic Inhibitors (MCC950, H-151) | Well-characterized small molecules that specifically inhibit key PRR pathway components (NLRP3, STING). Tool compounds for proof-of-concept studies. |
| Electroporation System (e.g., Neon) | Enables intracellular delivery of non-permeant antagonists like antibodies or decoy proteins to target cytosolic PRRs (RIG-I, NLRs). |
| Cytometric Bead Array (CBA) Kits | Multiplex immunoassays to quantify a panel of storm-related cytokines (TNF-α, IL-1β, IL-6, IL-8, IFN-α/β) simultaneously from small sample volumes. |
Technical Support & Troubleshooting Center
This support center provides solutions for common experimental challenges in targeting downstream signaling components to control cytokine storm pathology, framed within PAMP overactivation research.
Frequently Asked Questions (FAQs) & Troubleshooting
Q1: My JAK inhibitor (e.g., Tofacitinib) shows efficacy in vitro but fails to reduce cytokine levels in my murine PAMP-challenge model. What could be the issue? A: This is often a pharmacokinetic/pharmacodynamic (PK/PD) disconnect. Key troubleshooting steps:
- Verify Drug Exposure: Measure plasma and tissue (e.g., spleen, lung) concentrations of the inhibitor at your dosing timepoints. Ensure they exceed the in vitro IC50 for target phosphorylation inhibition.
- Check Target Engagement: Ex vivo stimulate splenocytes from treated mice with relevant cytokines (e.g., IL-6, IFN-γ). Use flow cytometry to measure STAT phosphorylation (pSTAT1, pSTAT3) to confirm JAK/STAT pathway inhibition in vivo.
- Timing: Administer the inhibitor before or immediately with the PAMP challenge (e.g., LPS, CpG). Inhibiting downstream signal transduction is often ineffective after the transcriptional cascade is fully activated.
Q2: When using a SYK inhibitor (e.g., R406) in primary human macrophage experiments, I observe high cell toxicity. How can I mitigate this? A: SYK has crucial roles in cellular homeostasis. Follow this protocol:
- Titrate the Inhibitor: Perform a full dose-response curve (e.g., 0.01 µM to 10 µM) alongside a viability assay (e.g., ATP-based luminescence) prior to your functional assay.
- Reduce Incubation Time: Limit pre-treatment time to 1-2 hours before PAMP (e.g., zymosan, immune complexes) stimulation. Do not exceed 24 hours total treatment.
- Use Negative Control Inhibitor: Employ an inactive analog of your SYK inhibitor (if available) to distinguish target-specific effects from compound toxicity.
Q3: siRNA knockdown of TAK1 in my cell line is inefficient (>50% protein remaining), confounding my cytokine readouts. How can I improve knockdown? A: Inefficient TAK1 knockdown is common due to its essential role in survival.
- Validate Tools: Use a validated positive control siRNA (e.g., against GAPDH or PLK1) to confirm transfection efficiency.
- Optimize Transfection: Use a fluorescently-labeled non-targeting siRNA to visually confirm >80% delivery efficiency.
- Consider Alternative Models: Use inducible shRNA systems or CRISPRi for more sustained and potent knockdown. For acute experiments, consider a validated pharmacological TAK1 inhibitor (e.g., 5Z-7-Oxozeaenol) as a complementary approach, with appropriate vehicle controls.
Q4: My transcription factor (TF) activity assay (e.g., NF-κB or AP-1 luciferase reporter) shows high background activation in my unstimulated control cells. How do I reduce noise? A: High baseline often indicates system stress or reagent sensitivity.
- Check Serum: Use low-endotoxin, charcoal-stripped FBS in your assay medium. Standard FBS contains cytokines and growth factors that can activate these TFs.
- Optimize Transfection: Lower the amount of reporter plasmid DNA. High amounts can cause artificial activation. Co-transfect with a constitutively expressed Renilla luciferase plasmid (e.g., pRL-TK) for normalization.
- Include Critical Controls: Always run:
- Empty Vector Control: Cells transfected with plasmid lacking the TF response elements.
- Mutation Control: Cells transfected with a reporter containing mutated TF binding sites.
Key Experimental Protocols
Protocol 1: Assessing JAK/STAT Inhibition in Whole Blood/ PBMCs Objective: Measure target engagement of JAK inhibitors ex vivo.
- Collect whole blood or isolated PBMCs from treated subjects or animals.
- Aliquot 100 µL of blood or 1x10^5 PBMCs per stimulation condition into a 96-well plate.
- Stimulate with cytokines: IL-6 (10 ng/mL) for STAT3 phosphorylation or IFN-α (1000 U/mL) for STAT1/2 phosphorylation. Include an unstimulated control.
- Incubate at 37°C for 15 minutes.
- Immediately add 1 mL of 1x Lyse/Fix Buffer, mix, and incubate at 37°C for 10 min.
- Pellet cells, permeabilize with ice-cold 100% methanol for 10 min on ice.
- Stain with fluorescent antibodies against CD14, pSTAT3 (Y705), and pSTAT1 (Y701). Analyze by flow cytometry, gating on monocytes (CD14+).
Protocol 2: Evaluating SYK Inhibition in FcR or CLR Signaling Objective: Determine the effect of SYK inhibition on downstream inflammatory signaling.
- Seed human dendritic cells or macrophages in 24-well plates (5x10^5 cells/well).
- Pre-treat with SYK inhibitor or DMSO vehicle for 60 minutes.
- Stimulate via:
- Fcγ Receptor: Add pre-formed immune complexes (e.g., IgG-coated latex beads, 10:1 bead:cell ratio).
- C-type Lectin Receptor: Add zymosan A (10 µg/mL) or curdlan.
- Incubate at 37°C for 30 min for proximal signaling (analyze pSYK, pSYK substrate VAV1 by Western blot) or 6 hours for cytokine output (measure TNF-α, IL-1β via ELISA).
Protocol 3: Pharmacological Disruption of the TAK1-IKK-NF-κB Axis Objective: To dissect the role of TAK1 in PAMP-induced NF-κB activation.
- Seed HEK293-NF-κB-luc reporter cells or primary cells.
- Pre-treat with:
- TAK1 inhibitor: 5Z-7-Oxozeaenol (1 µM) for 60 min.
- IKKβ inhibitor: IKK-16 (5 µM) for 60 min (as a downstream control).
- Vehicle (DMSO).
- Stimulate with LPS (100 ng/mL) or IL-1β (10 ng/mL) for 6 hours.
- Lyse cells and measure luciferase activity. Normalize to protein concentration or Renilla luciferase control.
- In parallel, run Western blot for p-IκBα (S32/36) and total IκBα at 15-30 min post-stimulation to confirm pathway blockade.
Data Presentation
Table 1: Common Inhibitors for Downstream Kinase Targeting in Cytokine Storm Models
| Target | Example Inhibitor | Typical In Vitro IC50/EC50 | Key Off-Target Effects to Consider | Recommended Control Experiment |
|---|---|---|---|---|
| JAK | Tofacitinib (pan-JAK) | JAK3: 1 nM, JAK1/2: ~20 nM | May affect other kinase families (e.g., CHK2) at high µM doses. | Use selective JAK1 (e.g., Upadacitinib) or JAK2 (e.g., Fedratinib) inhibitors for comparison. |
| SYK | R406 (active metabolite of Fostamatinib) | ~40 nM for SYK-dependent B-cell activation | Inhibits FLT3 (IC50 ~75 nM). Can affect cell adhesion. | Use a SYK-negative cell line reconstituted with WT vs. kinase-dead SYK. |
| TAK1 | 5Z-7-Oxozeaenol | ~8 nM in cell-free assay | Covalently binds and inhibits MEK, ERK at higher doses. | Use genetic (siRNA) knockdown and complement with rescue experiments. |
Table 2: Core Transcription Factor Targets in PAMP-Induced Cytokine Production
| Transcription Factor | Primary Activator Pathway(s) | Key Cytokines Regulated | Common Functional Assays |
|---|---|---|---|
| NF-κB (p65/RelA) | TLR/IL-1R -> MyD88 -> IRAK -> TAK1 -> IKK | TNF-α, IL-1β, IL-6, IL-12 | EMSA, p65 nuclear translocation (imaging), luciferase reporter, ChIP-qPCR. |
| AP-1 (c-Fos/c-Jun) | TLR -> SYK/MAPK; Dectin-1 -> CARD9 | TNF-α, IL-2, IL-10 | Luciferase reporter, phospho-c-Jun (S63) Western blot. |
| IRF3/IRF7 | TLR3/4/9 -> TRIF -> TBK1/IKKε | Type I Interferons (IFN-α/β), ISGs | Dimerization assay, nuclear translocation, luciferase reporter. |
| STAT1/STAT3 | Cytokine Receptors (IFNR, IL-6R) -> JAK | IRF1, SOCS3, additional cytokines | Phospho-flow cytometry, DNA-binding ELISA, luciferase reporter. |
Signaling Pathway Diagrams
Title: PAMP-Driven Signaling to Cytokine Storm via Key Kinases and TFs
Title: JAK-STAT Pathway and Pharmacological Inhibition
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Downstream Signal Interruption Experiments
| Reagent Category | Specific Example(s) | Primary Function in Experiments | Critical Consideration |
|---|---|---|---|
| Validated Kinase Inhibitors | Tofacitinib (JAK), R406 (SYK), 5Z-7-Oxozeaenol (TAK1), IKK-16 (IKKβ) | Pharmacological disruption of specific nodes to establish causal role in signaling. | Always use pharmacologically relevant concentrations (near IC50) and include vehicle (DMSO) and inactive analog controls. |
| Phospho-Specific Antibodies | Anti-pSTAT1 (Y701), pSTAT3 (Y705), pSYK (Y525/526), pTAK1 (T184/187), p-IκBα (S32/36) | Readout for target engagement and proximal pathway inhibition by drugs or genetic tools. | Validate for specific application (flow cytometry vs. Western blot). Check phospho-signal in KO/KD cells. |
| Transcription Factor Reporters | NF-κB luciferase plasmid (e.g., pGL4.32), AP-1 luciferase plasmid, IRF reporter plasmid. | Functional measurement of integrated pathway activity downstream of kinase inhibition. | Co-transfect with Renilla control for normalization. Use minimal plasmid DNA to avoid artefactual activation. |
| Cytokine Detection Assays | High-sensitivity ELISA kits for TNF-α, IL-1β, IL-6, IFN-γ; LEGENDplex bead-based arrays. | Quantification of the ultimate functional output of the signaling cascade. | For arrays, ensure the dynamic range covers expected concentrations in your model (serum vs. supernatant). |
| Genetic Modulation Tools | ON-TARGETplus siRNA SMARTpools (for SYK, TAK1, JAKs); CRISPRa/i systems for transcription factors. | To confirm pharmacologic findings and achieve selective, long-term knockdown. | Include non-targeting and positive control siRNAs. Perform rescue experiments with inhibitor-resistant constructs. |
Technical Support Center: Troubleshooting and FAQs
This support center provides guidance for common experimental challenges in cytokine-neutralizing research, framed within the thesis context of controlling cytokine storm from PAMP overactivation.
FAQs & Troubleshooting Guides
Q1: Our in vitro macrophage assay shows inconsistent IL-6 suppression with tocilizumab (anti-IL-6R mAb). What are potential causes? A: Inconsistent suppression often relates to PAMP (e.g., LPS) batch variability or macrophage differentiation state.
- Troubleshooting Steps:
- Standardize PAMP Source: Use LPS from a single, reputable supplier (e.g., List Biologicals, InvivoGen). Confirm concentration via Limulus Amebocyte Lysate (LAL) assay.
- Quantify Monocyte/Macrophage Differentiation: Ensure consistent differentiation from primary monocytes using a defined M-CSF concentration (e.g., 50 ng/mL for 7 days). Validate via surface marker flow cytometry (CD14, CD11b, CD68).
- Pre-incubation Time: Confirm the antagonist (tocilizumab) is added 30-60 minutes prior to PAMP stimulation to allow for receptor binding.
- Control Check: Include a positive control (e.g., JAK inhibitor like ruxolitinib) to confirm the assay's ability to detect pathway suppression.
Q2: When testing an anti-TNF-α mAb in our murine cytokine storm model, we observe high inter-animal variability in cytokine reduction. How can we improve consistency? A: Variability frequently stems from differences in the timing and severity of storm induction.
- Troubleshooting Protocol:
- Model Standardization: For LPS-induced models, use age- and weight-matched mice from a single source. Prepare LPS solution fresh and administer via a single, precise route (e.g., intraperitoneal injection).
- Kinetic Pilot Study: Before antibody testing, run a time-course to define the peak serum cytokine (TNF-α, IL-6, IL-1β) response post-PAMP (e.g., at 1.5, 3, 6 hours). Administer the mAb 15 minutes before the expected peak.
- Dosing Control: Ensure antibody is free of aggregates (check by SEC-HPLC) and administer in a consistent volume based on individual animal weight.
- Endpoint Harmonization: Collect sera/blood at identical timepoints post-induction. Use multiplex luminex assays over individual ELISAs for concurrent cytokine measurement.
Q3: In our reporter cell assay for IL-1β pathway antagonism, background signal (no PAMP) is unexpectedly high. How do we resolve this? A: High background often indicates endogenous cytokine production or reagent contamination.
- Resolution Guide:
- Cell Line Validation: Test the reporter cell line (e.g., THP-1 NF-κB/AP-1 reporter) for mycoplasma contamination, which can cause spontaneous activation.
- FBS Screening: Use heat-inactivated FBS that has been screened for low endotoxin (<1 EU/mL). Consider testing multiple lots.
- Reagent Check: Prepare IL-1β receptor antagonist (e.g., Anakinra) or test mAb in a carrier (e.g., PBS with low BSA) free of preservatives that can activate some cell lines.
- Protocol Adjustment: Include a "reporter cells + antagonist only" control to establish the true baseline for your inhibitory compound.
Experimental Protocol: In Vitro Assessment of Anti-IL-6 mAb Neutralization Capacity
Objective: To quantify the neutralization efficiency of a candidate anti-IL-6 monoclonal antibody in a human primary cell system modeling PAMP activation.
Detailed Methodology:
- Peripheral Blood Mononuclear Cell (PBMC) Isolation: Isolate PBMCs from healthy donor buffy coats using density gradient centrifugation (Ficoll-Paque PLUS). Wash cells 3x in PBS. Resuspend in complete RPMI-1640 (10% low-endotoxin FBS, 1% Pen/Strep).
- Cell Plating: Seed PBMCs in a 96-well U-bottom plate at 2.5 x 10^5 cells/well in 180 µL.
- Antibody Pre-treatment: Prepare serial dilutions (e.g., 10 µg/mL to 0.01 µg/mL) of the test anti-IL-6 mAb and an isotype control. Add 10 µL of each dilution to designated wells. Include a "no antibody" control (10 µL media). Incubate plate at 37°C, 5% CO2 for 30 minutes.
- PAMP Activation: Add 10 µL of LPS (from E. coli O111:B4) to a final, pre-optimized concentration (e.g., 100 ng/mL) to all wells except the unstimulated control. Incubate for 24 hours.
- Harvest & Analysis: Centrifuge plate (300 x g, 5 min). Collect supernatant. Quantify IL-6 levels using a validated ELISA kit.
- Data Calculation: Calculate % neutralization = [1 - (IL-6 conc. with mAb - IL-6 conc. unstimulated) / (IL-6 conc. with LPS only - IL-6 conc. unstimulated)] * 100. Determine IC50 via non-linear regression (4-parameter logistic curve).
Data Presentation
Table 1: Selected Cytokine-Targeting Agents in Clinical Development for Cytokine Storm Syndromes (2023-2024)
| Target Cytokine | Agent Name | Agent Type | Development Stage (as of 2024) | Key Trial Identifier / Source |
|---|---|---|---|---|
| IL-6 | Tocilizumab | Humanized mAb (anti-IL-6R) | FDA-approved for CRS, COVID-19 | N/A (Approved) |
| IL-6 | Sirukumab | Human mAb (anti-IL-6) | Phase III for COVID-19 ARDS | NCT04380961 |
| GM-CSF | Gimsilumab | Human mAb (anti-GM-CSF) | Phase II/III for COVID-19 pneumonia | NCT04351243 |
| IFN-γ | Emapalumab | Human mAb (anti-IFN-γ) | FDA-approved for HLH | N/A (Approved) |
| IL-1β | Canakinumab | Human mAb (anti-IL-1β) | Phase III for COVID-19 (CAN-COVID) | NCT04362813 |
| C5a | Vilobelimab | Chimeric mAb (anti-C5a) | Phase III for COVID-19 ARDS (PANAMO) | NCT04333420 |
| IL-1R | Anakinra | Recombinant Receptor Antagonist | Phase III for COVID-19 (SAVE) | NCT04357366 |
Table 2: Example In Vitro Neutralization Efficacies (IC50) of Candidate mAbs
| Candidate mAb | Target | Assay System | Reported IC50 (Mean ± SD) | Key Experimental Condition |
|---|---|---|---|---|
| XIL-6.1 (Example) | IL-6 | Human PBMC (LPS-stimulated) | 0.45 ± 0.12 nM | 24h stimulation, 100 ng/mL LPS |
| XTNF.3 (Example) | TNF-α | Murine Macrophages (RAW 264.7) | 1.2 ± 0.3 nM | 6h stimulation, 10 ng/mL LPS |
| Reference Control (Adalimumab) | TNF-α | Human THP-1 cells | 0.15 ± 0.05 nM | Standard bioassay |
Diagrams
Title: Cytokine Storm Pathway and Neutralization Points
Title: Workflow for mAb Neutralization Assay in PBMCs
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Cytokine Neutralization Experiments
| Item | Function & Rationale | Example Product/Source |
|---|---|---|
| Ultra-pure PAMPs | Provides consistent, specific Toll-like receptor activation to model the initial trigger of cytokine storm. | LPS-EB UltraPure (InvivoGen), Poly(I:C) HMW (InvivoGen) |
| Low-Endotoxin FBS | Critical for cell culture to avoid unintended background activation of innate immune pathways via trace endotoxins. | Gibco Endotoxin-Free FBS (Thermo Fisher) |
| Recombinant Human/Murine Cytokines | Used for generating standard curves in quantification assays (ELISA/Luminex) and as positive controls in bioassays. | PeproTech, R&D Systems Bio-Techne |
| Validated Neutralizing mAbs (Positive Controls) | Essential benchmarks for comparing the efficacy of novel agents and validating assay performance. | Tocilizumab (anti-IL-6R), Infliximab (anti-TNF-α) |
| Multiplex Cytokine Assay Kits | Enables simultaneous measurement of multiple cytokines from a single small sample, crucial for storm profiling. | Luminex Assay Kits (R&D Systems), LEGENDplex (BioLegend) |
| Mycoplasma Detection Kit | Regular screening prevents experimental artifacts caused by mycoplasma contamination in cell lines. | MycoAlert PLUS (Lonza) |
| Cell Viability Assay Reagent | Distinguishes true cytokine modulation from cytotoxic effects of experimental compounds. | CellTiter-Glo 2.0 (Promega) |
| ELISA Stop Solution | Accurately terminates the colorimetric TMB reaction for consistent optical density readings. | 1M H2SO4 or commercial stop solution |
Technical Support Center
Welcome to the Technical Support Center for cellular reprogramming research in the context of mitigating PAMP (Pathogen-Associated Molecular Pattern)-induced cytokine storm. This guide addresses common experimental hurdles encountered when modulating immune cell phenotypes via pharmacologic and genetic strategies.
Troubleshooting Guides & FAQs
FAQ Category 1: Pharmacologic Reprogramming
Q1: My small-molecule inhibitor fails to suppress the expected pro-inflammatory phenotype in primary human macrophages. What could be wrong?
- A: Consider these points:
- PAMP Potency & Timing: The concentration and duration of the PAMP (e.g., LPS) stimulus may be too high, overwhelming the inhibitor. Titrate the PAMP and pre-treat cells with the inhibitor for 30-60 minutes prior to stimulation.
- Inhibitor Specificity & Metabolism: Verify the inhibitor's specificity for the target in your specific immune cell type. Check its stability and half-life in your culture medium; it may require replenishment.
- Cell Viability: High inhibitor concentrations can be cytotoxic. Perform a dose-response viability assay (e.g., MTT, Annexin V) alongside your functional readouts.
- Off-target Effects: The inhibitor might be affecting an unexpected pathway that influences the phenotype. Include a genetic knockdown/knockout of the target as a complementary control.
- A: Consider these points:
Q2: I observe high variability in cytokine suppression when using epigenetic modifiers (e.g., HDACi, DNMTi) between donor-derived primary cells. How can I improve consistency?
- A: Donor variability is a key challenge. Standardize your protocol:
- Cell Synchronization: Use serum-starvation or low-dose cytokine priming to bring cells to a more uniform basal state pre-treatment.
- Define "Resting" State: Clearly characterize the baseline epigenetic and transcriptional state of cells from each donor using controls.
- Combinatorial Approach: A single epigenetic drug may be insufficient. Consider rational low-dose combinations (e.g., HDACi + BET inhibitor) to achieve more robust and uniform reprogramming. Always include a vehicle control for each donor.
- A: Donor variability is a key challenge. Standardize your protocol:
FAQ Category 2: Genetic Reprogramming
Q3: My CRISPR-Cas9 knockout efficiency in primary immune cells (e.g., monocytes, T cells) is low. How can I enhance delivery and editing?
- A: Primary immune cells are notoriously difficult to transfect.
- Delivery Method: For high efficiency, use nucleofection (electroporation) with cell-type specific kits. For lentiviral transduction, consider VSV-G pseudotyped vectors and spinfection. See protocol below.
- Guide RNA Design: Use validated, high-efficiency sgRNAs from reputable databases and ensure your Cas9 (e.g., spCas9) is codon-optimized for human cells.
- Selection & Enrichment: Co-transfect with a fluorescent marker or antibiotic resistance gene and use FACS sorting or antibiotic selection to enrich for transfected cells before experimentation.
- A: Primary immune cells are notoriously difficult to transfect.
Q4: My inducible overexpression system for a transcription factor (e.g., to drive M2 polarization) shows high background leakage. How to minimize this?
- A: Background expression can confound phenotype interpretation.
- Vector System: Switch to a tighter inducible system (e.g., cumate-switch or Tet-On 3G over older Tet-On systems).
- Repressor Presence: Ensure the appropriate repressor (e.g., tTS, KRAB) is constitutively expressed and functional in your cell line.
- Inducer Purity & Concentration: Titrate the inducer (doxycycline, cumate) to find the minimum effective dose. Verify its concentration and stability in culture.
- Clone Selection: If using stable lines, screen multiple single-cell clones for low background and high inducibility.
- A: Background expression can confound phenotype interpretation.
FAQ Category 3: Phenotype & Functional Validation
- Q5: After reprogramming, my cells show mixed surface marker expression, not a clear shift from M1 to M2 (or vice versa). How should I interpret this?
- A: Immune phenotypes exist on a spectrum. A pure in vitro M1/M2 dichotomy is often an oversimplification.
- Multi-parametric Analysis: Use a panel of at least 4-5 surface (e.g., CD80, CD163, CD206) and intracellular (e.g., cytokines, arginase-1) markers via flow cytometry.
- Functional Assays: Correlate markers with function. Assay phagocytosis, arginase activity, or pathogen killing capacity.
- Transcriptomics: For definitive classification, perform bulk or single-cell RNA-seq to analyze global gene expression signatures rather than relying on 1-2 markers.
- A: Immune phenotypes exist on a spectrum. A pure in vitro M1/M2 dichotomy is often an oversimplification.
Experimental Protocols
Protocol 1: CRISPR-Cas9 Knockout in Primary Human Monocytes via Nucleofection
- Objective: Generate stable knockout of a pro-inflammatory signaling node (e.g., MyD88) to dampen PAMP response.
- Materials: Primary human CD14+ monocytes, Nucleofector Device & Cell Line Specific Kit, sgRNA/Cas9 ribonucleoprotein (RNP) complex, RPMI-1640 + 10% FBS.
- Steps:
- Isolate CD14+ monocytes using positive selection.
- Resuspend 1-2 x 10^6 cells in 100 µL of pre-warmed nucleofection solution.
- Mix cells with 5 µg of pre-complexed sgRNA:Cas9 RNP. Transfer to a nucleofection cuvette.
- Select the appropriate nucleofection program (e.g., Y-001 for monocytes).
- Immediately post-nucleofection, add pre-warmed medium and transfer cells to a culture plate.
- Allow recovery for 48-72 hours. Validate editing efficiency by T7 Endonuclease I assay or next-generation sequencing.
- Challenge edited cells with PAMP (e.g., 100 ng/mL LPS) and assay cytokine output (ELISA).
Protocol 2: Pharmacologic Reprogramming of Macrophage Phenotype
- Objective: Use a small-molecule inhibitor to re-polarize M1 macrophages toward an M2-like, inflammation-resolving phenotype.
- Materials: Human monocyte-derived macrophages (M1-polarized with IFN-γ + LPS), JAK1/2 inhibitor (e.g., Baricitinib), IL-4 (for M2 control), flow cytometry antibodies.
- Steps:
- Differentiate monocytes with M-CSF (50 ng/mL) for 6 days.
- Polarize to M1 with IFN-γ (20 ng/mL) + LPS (10 ng/mL) for 24 hours.
- Wash cells and add reprogramming medium containing JAK inhibitor (e.g., 100 nM Baricitinib) or IL-4 (20 ng/mL) for M2 control for 48 hours.
- Harvest cells and stain for surface markers (CD80-PE, CD206-APC, HLA-DR-FITC).
- Analyze by flow cytometry. Calculate geometric MFI and percentage of positive cells for each marker.
Data Presentation
Table 1: Efficacy of Pharmacologic Agents in Suppressing LPS-Induced Cytokine Storm in Human Macrophages
| Agent (Class) | Target | Concentration | % Reduction in TNF-α | % Reduction in IL-6 | Key Side Effect (Viability) |
|---|---|---|---|---|---|
| Baricitinib (JAKi) | JAK1/2 | 100 nM | 85% ± 5% | 78% ± 7% | >90% viability |
| BAY11-7082 (IKBi) | IKKβ | 5 µM | 95% ± 3% | 90% ± 4% | 70% viability (high toxicity) |
| Ruxolitinib (JAKi) | JAK1/2 | 500 nM | 80% ± 6% | 75% ± 8% | >90% viability |
| Tofacitinib (JAKi) | JAK3 | 1 µM | 60% ± 10% | 55% ± 12% | >85% viability |
| Vehicle Control | - | - | 0% | 0% | >95% viability |
(Data are representative means ± SD from n=3 independent donors; LPS stimulation at 100 ng/mL for 18h.)
Table 2: Comparison of Genetic Modifications for Attenuating Cytokine Response to PAMPs
| Genetic Approach | Target Gene | Delivery Method | Editing Efficiency | Reduction in IL-1β Secretion | Time to Stable Phenotype |
|---|---|---|---|---|---|
| CRISPR-Cas9 KO | MyD88 | Nucleofection (RNP) | 75% ± 8% | 90% ± 5% | 5-7 days |
| CRISPR-Cas9 KO | IRAK4 | Lentiviral sgRNA | 60% ± 12% | 85% ± 7% | 10-14 days |
| shRNA Knockdown | TRAF6 | Lentiviral Transduction | 80% (mRNA) | 70% ± 10% | 7-10 days |
| Lentiviral Overexpression | SOCS1 | Lentiviral Transduction | 20-fold (mRNA) | 65% ± 9% | 7-10 days |
| Non-Targeting Control | - | Nucleofection | - | 0% | - |
Mandatory Visualizations
Title: PAMP Signaling and Intervention Points for Cytokine Storm
Title: Workflow for Immune Cell Reprogramming Experiments
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function/Application | Example Product/Catalog |
|---|---|---|
| LPS (E. coli O111:B4) | A classic PAMP (TLR4 agonist) used to induce pro-inflammatory (M1) polarization and model cytokine storm initiation. | Sigma-Aldrich L2630 |
| Recombinant Human M-CSF | Differentiates human monocytes into resting macrophages, forming the baseline for polarization experiments. | PeproTech 300-25 |
| JAK1/2 Inhibitor (Baricitinib) | Pharmacologic agent to block JAK-STAT signaling, reprogramming macrophages away from inflammatory phenotype. | Selleckchem S2851 |
| CRISPR-Cas9 RNP Complex | Pre-formed ribonucleoprotein for high-efficiency, transient gene editing in hard-to-transfect primary immune cells. | Synthego or IDT custom sgRNA + Alt-R S.p. Cas9 Nuclease |
| Nucleofector Kit for Monocytes | Optimized reagents and protocols for high-efficiency transfection of primary human monocytes. | Lonza VPA-1007 |
| Human Cytokine 30-Plex Panel | Multiplex assay to quantitatively profile a broad spectrum of inflammatory and anti-inflammatory cytokines from supernatant. | Thermo Fisher Scientific LHC6003M |
| Anti-human CD206 (MMR) APC | Key surface marker antibody for identifying M2-like, alternatively activated macrophages via flow cytometry. | BioLegend 321110 |
| T7 Endonuclease I Assay Kit | Quick and reliable method to assess CRISPR-Cas9 genome editing efficiency by detecting mismatches in PCR products. | NEB M0302S |
Technical Support Center
FAQs & Troubleshooting for Cytokine Storm Research
Q1: My siRNA nanoparticles for targeting TLR4 show poor in vivo silencing efficiency in my murine cytokine storm model. What could be the issue? A: Common issues include:
- Nanoparticle Stability: Serum proteins can opsonize particles, causing rapid clearance. Verify particle stability in 50-100% serum via DLS over 1-2 hours.
- Ligand Density: Too high or too low PEG or targeting ligand (e.g., peptide for endothelial cells) density can hinder cellular uptake. Titrate ligand ratios.
- siRNA Loading/Release: Ensure efficient endosomal escape. Co-encapsulate endosomolytic agents (e.g., chloroquine) or use ionizable lipids that disrupt endosomes at low pH.
Q2: My CRISPR-Cas9 knock-out of NLRP3 in macrophages fails to suppress IL-1β secretion upon PAMP priming. How should I troubleshoot? A:
- Verify Knock-out Efficiency: Run a T7E1 or Sanger sequencing surveyor assay on genomic DNA. Efficiency should be >80%.
- Check Protein Depletion: Perform Western blot on cell lysates post-priming to confirm NLRP3 ablation.
- Assay Specificity: Ensure your PAMP (e.g., LPS) activates the NLRP3 inflammasome (requires ATP or nigerien as Signal 2). Your assay may be detecting caspase-1 independent IL-1β release.
Q3: I observe high cytotoxicity when using cationic lipid nanoparticles (LNPs) for delivering mRNA encoding anti-inflammatory cytokines. How can I reduce this? A: Cationic lipids often cause toxicity. Mitigation strategies include:
- Switch to Ionizable Lipids: Use lipids like DLin-MC3-DMA, which are neutral at physiological pH but cationic in acidic endosomes, reducing non-specific interactions.
- Adjust Lipid Ratios: Increase the molar percentage of PEG-lipid (e.g., from 1.5% to 3%) to reduce aggregation and non-specific binding.
- Perform a Dose-Escalation Study: Determine the minimum effective dose (MED) for protein expression versus the toxic dose.
Q4: My gene-edited cells (CRISPRa to overexpress A20/TNFAIP3) show the expected transcript increase but no phenotype in suppressing NF-κB reporter activity. Why? A:
- Check Protein Expression: Transcript levels may not correlate with protein. Confirm A20 protein overexpression via Western blot.
- Timing of Assay: A20 is a negative feedback regulator. Its effect may be temporally limited. Measure NF-κB activity at earlier (1-3h) and later (6-12h) time points post-PAMP stimulation.
- Redundant Pathways: Other checkpoints (e.g., ABIN-1, CYLD) may compensate. Consider combinatorial knockdown.
Experimental Protocols
Protocol 1: Evaluating siRNA-LNP Efficacy in a Murine LPS-Induced Cytokine Storm Model
- Formulation: Prepare siRNA-LNPs targeting a gene of interest (e.g., Myd88) and a non-targeting control via microfluidic mixing. Purify by dialysis.
- Characterization: Measure particle size (target: 70-100 nm), PDI (<0.2), and encapsulation efficiency (>90%) using DLS and RiboGreen assay.
- Prophylactic Dosing: Administer LNP (1-3 mg siRNA/kg) via tail vein to C57BL/6 mice (n=8/group) 24 hours before LPS challenge (10 mg/kg, i.p.).
- Sample Collection: At 90 minutes post-LPS, collect serum via cardiac puncture.
- Analysis: Quantify cytokines (TNF-α, IL-6, IL-1β) by multiplex ELISA. Harvest liver/spleen for qPCR to confirm target knockdown.
Protocol 2: Generating a Stable NLRP3-Knockout THP-1 Monocyte Line via CRISPR-Cas9
- Design: Design two sgRNAs targeting early exons of the human NLRP3 gene (NCBI Reference Sequence: NM_001127462.2).
- Delivery: Clone sgRNAs into a lentiCRISPR v2 plasmid. Package into lentivirus in HEK293T cells.
- Transduction: Transduce differentiated THP-1 macrophages (PMA, 100 nM, 24h) with virus + polybrene (8 µg/mL). Select with puromycin (2 µg/mL) for 7 days.
- Clonal Isolation: Single-cell sort into 96-well plates. Expand clones for 2-3 weeks.
- Validation: Screen clones by genomic PCR of target region and Sanger sequence analysis. Confirm knock-out via Western blot after priming with LPS (1 µg/mL, 4h) and activating with Nigericin (10 µM, 1h).
Data Presentation
Table 1: Comparison of Novel Modalities for Cytokine Storm Intervention
| Modality | Typical Target | Key Efficacy Metric (In Vivo) | Onset of Action | Major Challenge |
|---|---|---|---|---|
| siRNA-LNP | mRNA (e.g., Myd88, Nfkb1) | >70% target knockdown in liver/spleen | 24-48 hours | Off-target effects, transient effect |
| CRISPR-KO | Genomic DNA (e.g., Nlrp3) | Indel frequency >80% in vitro | Permanent | Delivery efficiency in vivo, safety |
| CRISPRa | Endogenous promoter (e.g., Tnfaip3) | 10-50 fold increase in target transcript | 24-72 hours | Precise control of expression level |
| mRNA-LNP | Protein replacement (e.g., IL-10) | Serum protein >100 ng/mL for 24-48h | 4-12 hours | Immunogenicity, duration of expression |
Table 2: Troubleshooting Common Experimental Failures
| Problem | Potential Cause | Solution |
|---|---|---|
| Low siRNA encapsulation efficiency | Incorrect N:P ratio, rapid mixing time | Optimize flow rate ratio (AQ:Organic = 3:1), ensure total flow rate >10 mL/min. |
| High inflammatory response to LNP | LNP components (e.g., PEG) activating immune cells | Pre-dose with non-targeting LNP, use alternative PEG-lipids (e.g., DMG-PEG). |
| Poor CRISPR editing efficiency | Low sgRNA activity, poor delivery | Use a validated sgRNA scaffold, test multiple sgRNAs, optimize RNP electroporation parameters. |
| No phenotype despite high knockdown | Compensatory pathways, assay sensitivity | Perform combinatorial gene targeting, use a more sensitive assay (e.g., picoGreen for dsDNA). |
The Scientist's Toolkit
Table 3: Research Reagent Solutions for Cytokine Storm Modality Development
| Reagent / Material | Function / Application | Example Vendor/Product |
|---|---|---|
| Ionizable Lipid (e.g., DLin-MC3-DMA) | Core component of LNPs for siRNA/mRNA; enables endosomal escape and reduces cytotoxicity. | MedChemExpress (HY-108787) |
| RiboGreen Assay Kit | Quantifies encapsulated vs. free nucleic acids in LNP formulations. | Thermo Fisher Scientific (R11490) |
| LentiCRISPR v2 Vector | All-in-one plasmid for lentiviral delivery of Cas9 and sgRNA. | Addgene (52961) |
| Recombinant Human/Mouse Cytokine Multiplex Assay | Simultaneously quantifies multiple cytokines from small volume samples. | LEGENDplex (BioLegend) |
| PMA (Phorbol 12-myristate 13-acetate) | Differentiates monocytic cell lines (e.g., THP-1) into macrophage-like cells. | Sigma-Aldrich (P8139) |
| Nigericin (Potassium salt) | K+ ionophore used as a potent and specific NLRP3 inflammasome activator (Signal 2). | Tocris Bioscience (4312) |
| Lipofectamine CRISPRMAX Transfection Reagent | Optimized for delivery of CRISPR RNP complexes into difficult-to-transfect primary cells. | Thermo Fisher Scientific (CMX0003) |
Visualizations
Title: Modalities Targeting PAMP Cascade to Control Cytokine Storm
Title: CRISPR-Cas9 Knockout Cell Line Generation Workflow
Navigating Complexities: Troubleshooting Challenges in Preclinical Models and Assay Development
Technical Support Center: Troubleshooting PAMP-Induced Cytokine Storm Models
FAQs & Troubleshooting Guides
Q1: Our murine model fails to replicate the full spectrum of human cytokine profiles (e.g., low IFN-λ, disproportionate IL-6) following PAMP challenge. What are the primary species-specific limitations and potential workarounds?
A: The primary limitation is evolutionary divergence in innate immune receptors (e.g., TLRs), signaling adaptors, and cytokine gene clusters. Murine macrophages may respond to identical PAMPs with a different cytokine hierarchy.
- Troubleshooting: Consider using "humanized" mice engrafted with human hematopoietic stem cells. Validate the reconstitution of human myeloid lineages (CD33+, CD14+) via flow cytometry prior to PAMP challenge. Note that murine stromal cells and non-hematopoietic compartments remain mouse-derived, which can confound signaling.
Q2: In our humanized mouse model, we observe graft-vs-host disease (GvHD) that interferes with storm phenotyping. How can we mitigate this?
A: GvHD is a common artifact caused by donor immune cells attacking murine tissues.
- Troubleshooting: Utilize next-generation NSG or NOG strains with additional mutations (e.g., NSG-SGM3, NOG-EXL). For drug testing, initiate therapy after confirming stable human cell engraftment but before the typical GvHD onset window (often 8-12 weeks post-transplant). Include a cohort treated with an immunosuppressant (e.g., low-dose anti-TNF-α) as a control for GvHD-specific inflammation.
Q3: Our multi-organ chip (e.g., liver-heart-lung) shows rapid cell death upon systemic PAMP perfusion, making storm kinetics uninterpretable. What are key calibration steps?
A: This indicates excessive PAMP concentration or inadequate organ functional support.
- Troubleshooting Protocol:
- Baseline Viability: Confirm >95% viability in each tissue compartment pre-stimulation using a non-invasive assay (e.g., luciferase-based ATP monitoring).
- PAMP Titration: Perform a dose-response using a simplified (single-organ) chip. Start with concentrations 1-2 logs below typical in vitro well-plate EC90. Use LPS (TLR4), Poly(I:C) (TLR3), or specific bacterial/viral PAMPs relevant to your thesis.
- Flow Rate Calibration: Calculate the shear stress for each tissue type. Adjust the perfusion pump to physiologic shear (e.g., 0.5-2 dyn/cm² for liver sinusoid, 10-15 dyn/cm² for capillary). Ensure the medium reservoir is sufficiently oxygenated (use a gas-permeable membrane or direct oxygenation).
Q4: How do we quantitatively compare the dynamic range and sensitivity of cytokine detection across these three model systems?
A: The dynamic range is highly platform-dependent. See Table 1 for a quantitative comparison.
Table 1: Quantitative Comparison of Model Systems for PAMP-Induced Cytokine Storm
| Parameter | Murine Model (C57BL/6) | Humanized Mouse (NSG-SGM3) | Organ-on-a-Chip (Multi-tissue) |
|---|---|---|---|
| Time to Peak Cytokine (post-PAMP) | 6-24 hours (serum) | 12-48 hours (human cytokines in serum) | 2-8 hours (effluent) |
| Typical IL-6 Dynamic Range | 10 pg/mL - 200 ng/mL | (Human) 1 pg/mL - 50 ng/mL | 0.5 pg/mL - 10 ng/mL (perfusate) |
| Key Missing Human Components | N/A | Human stromal signaling, human tissue architecture | Full neuroendocrine axis, adaptive immune system |
| Throughput (Drug Screens) | High (n=5-10/day) | Moderate (n=3-5/day) | Low (n=1-3/day) |
| Data Variability (CV%) | 15-25% | 25-40% (due to engraftment variance) | 10-20% (with calibrated chips) |
| Primary Cost Driver | Animal housing & care | Human CD34+ cells, specialized strains | Chip fabrication, specialty media, sensors |
Experimental Protocols
Protocol 1: Standardized PAMP Challenge in Humanized Mice for Storm Assessment
- Objective: To induce and measure a human-specific cytokine storm.
- Materials: NSG-SGM3 mice with >70% human CD45+ engraftment (confirmed via tail bleed), ultra-pure LPS (TLR4 agonist), sterile PBS, serum collection tubes.
- Method:
- Randomize mice based on engraftment levels.
- Adminstrate LPS (1 mg/kg) or vehicle control via intraperitoneal injection.
- Collect blood via retro-orbital or submandibular bleed at T=0, 3, 6, 12, 24 hours.
- Process serum and analyze using a human-specific multiplex cytokine array (e.g., Luminex 32-plex). Do not use a mouse array.
- Critical Step: Measure both human (e.g., hIL-6, hTNF-α) and mouse (mKC, mMCP-1) cytokines to dissect cross-species interactions.
Protocol 2: Calibrating a Liver-Kidney Chip for PAMP-Induced Toxicity & Storm Crosstalk
- Objective: To model organ-specific cytokine release and inter-tissue signaling.
- Materials: Dual-organ chip with porous membrane separation, primary human hepatocytes & proximal tubule kidney cells, perfusion controller, LPS.
- Method:
- Seed cells and culture under perfusion for 7 days to mature tissue function (confirm albumin for liver, TEER for kidney).
- Switch perfusion to medium containing a sub-toxic LPS dose (e.g., 100 ng/mL). Run for 72 hours.
- Collect effluent from each organ outlet separately every 12 hours for cytokine/toxicity analysis.
- Endpoint Analysis: Fix and immunostain for: i) Tight junctions (ZO-1), ii) Cytokine-producing cells (p-STAT3), iii) Apoptosis (cleaved caspase-3).
- Key Calculation: Determine organ cross-talk by comparing the cytokine profile from the "downstream" organ (kidney) when perfused alone vs. when connected to the "upstream" liver.
Diagrams
Title: PAMP Storm Signaling Pathway Cross-Species Comparison
Title: Experimental Workflow for Storm Model Selection
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for PAMP Storm Modeling
| Reagent/Material | Function & Application | Key Consideration |
|---|---|---|
| Ultra-Pure LPS (E. coli O111:B4) | Canonical TLR4 agonist; induces MyD88/TRIF-dependent storm. | Use same source/batch across studies; purity >99% minimizes non-TLR4 effects. |
| Recombinant Human M-CSF | Differentiates human monocytes into macrophages in vitro or in chips. | Essential for generating authentic human macrophage responses in engineered systems. |
| Magnetic Beads (anti-human CD14/CD33) | Isolation of primary human monocytes from PBMCs for chip seeding. | Positive selection maintains high viability; confirm absence of prior immune activation. |
| Phospho-STAT3 (Tyr705) Antibody | Key readout for IL-6/JAK/STAT storm signaling activity in tissue sections or chip lysates. | Use validated IHC/IF antibodies; compare to total STAT3 for activation ratio. |
| Cytokine Multiplex Array (Human) | Quantifies >30 analytes simultaneously from low-volume serum/chip effluent. | Must distinguish human from mouse cytokines in humanized models; verify cross-reactivity. |
| NSG-SGM3 Mouse Strain | Expresses human SCF, GM-CSF, IL-3; enhances human myeloid engraftment for storm modeling. | Higher baseline human cytokine levels; requires strict control for GvHD monitoring. |
| Gas-Permeable PDMS Chip | Foundation for organ-on-a-chip; allows O2/CO2 diffusion and real-time imaging. | Can absorb small molecules; pre-condition with media or use alternative polymers. |
Troubleshooting Guides & FAQs
Q1: Our multiplex cytokine assay shows high levels of IL-6 in control samples from unstimulated cells. What could cause this and how do we validate the specificity? A: This likely indicates assay cross-reactivity or plate/well edge effects. Validate via:
- Spike-and-Recovery: Spike a known concentration of recombinant IL-6 into your sample matrix. Recovery should be 80-120%.
- Parallel Dilution: Serially dilute samples. Measured cytokine concentrations should decrease linearly. Non-linearity suggests matrix interference.
- Alternative Method Comparison: Confirm key results with a standalone ELISA or Single Molecule Array (Simoa) assay.
- Neutralization: Pre-incubate samples with an IL-6 neutralizing antibody; signal should be abolished.
Q2: In TLR4 pathway analysis, how can we distinguish between canonical NF-κB signaling and off-target interferon responses? A: Use temporal and inhibitor-based dissection.
- Protocol: Stimulate primary macrophages with LPS (100 ng/mL). Collect lysates at 0, 15, 30, 60, 120 mins.
- Specific Inhibitors:
- BAY 11-7082 (10 µM): Inhibits IκBα phosphorylation, blocking canonical NF-κB.
- BX795 (1 µM): Inhibits TBK1/IKKε, blocking IRF3-driven interferon response.
- Analysis: Perform Western blot for p-IκBα (NF-κB readout) and p-IRF3 (interferon readout). Specific pathway blockade should abrogate its respective phospho-signal but not the other.
Q3: We observe cell death in our in vitro cytokine storm model only when using a specific JAK inhibitor. Is this an on-target or off-target effect? A: This requires investigation for off-target cytotoxicity.
- Viability Assay: Treat cells with a titration of the JAK inhibitor (e.g., 0.1-50 µM) for 24-48h. Use a resazurin-based assay to generate a dose-response curve.
- Counter-Screening: Test 2-3 structurally distinct JAK inhibitors (e.g., Tofacitinib, Ruxolitinib) at equimolar, therapeutically relevant concentrations.
- Caspase Inhibition: Pre-treat with pan-caspase inhibitor Z-VAD-FMK (20 µM). If cell death is rescued, it suggests an on-target apoptotic effect via JAK/STAT. If not, it indicates an off-target, non-apoptotic mechanism.
- Check Primary Cell Specificity: Repeat in primary immune cells; many off-target effects are cell-line dependent.
Table 1: Common Cytokine Assay Interferences & Solutions
| Interference Type | Example | Detection Method | Solution |
|---|---|---|---|
| Cross-reactivity | Soluble receptor binding detection antibody | Multiplex Bead Array | Use antibodies against epitopes not masked by receptor |
| Matrix Effect | Heterophilic antibodies in serum/plasma | ELISA | Use blocking reagents (e.g., Polyvinylpyrrolidone) |
| Hook Effect | Extremely high analyte concentration | Electrochemiluminescence | Always run sample at multiple dilutions |
| Plate Edge Effect | Evaporation in outer wells | Any plate-based assay | Use a physical plate sealer, randomize sample placement |
Table 2: Key Pathway Inhibitors for Specificity Control
| Target Pathway | Example Inhibitor | Typical Working Concentration | Common Off-Target Effects to Check |
|---|---|---|---|
| Canonical NF-κB | BAY 11-7082 | 5-10 µM | Induces apoptosis at higher doses (>20 µM) |
| MAPK (p38) | SB203580 | 10 µM | Inhibits some GSK3β and CK1 isoforms |
| JAK/STAT | Ruxolitinib (JAK1/2) | 100-500 nM | Can affect FLT3 and CDK2 at high µM range |
| NLRP3 Inflammasome | MCC950 | 10 µM | Highly specific; minimal reported off-target |
Experimental Protocols
Protocol: Validating Cytokine Specificity via Antibody Neutralization Purpose: To confirm that a measured signal is specific to the target cytokine. Materials: Sample, recombinant cytokine, neutralizing antibody (monoclonal, high affinity), matched isotype control antibody, detection assay (ELISA kit). Steps:
- Prepare four sample conditions in duplicate:
- Condition A: Sample + Assay Buffer.
- Condition B: Sample + Neutralizing Ab (2x excess by weight, pre-incubate 1h at RT).
- Condition C: Sample + Isotype Control Ab (2x excess).
- Condition D: Assay Buffer Only (Blank).
- Run all samples per the manufacturer's ELISA protocol.
- Calculation: Specific signal = (Signal A - Signal D) - (Signal B - Signal D). Signal in Condition C should be similar to A, confirming no non-specific antibody effect.
- Validate by spiking recombinant cytokine into a negative matrix and repeating; neutralization should reduce signal by >90%.
Protocol: Differentiating Direct vs. Secondary Cytokine Effects Purpose: To determine if a drug reduces cytokine release directly or via secondary effects (e.g., cell death). Materials: PBMCs, LPS (TLR4 agonist), test compound, viability dye (e.g., propidium iodide), flow cytometer. Steps:
- Isolate and plate human PBMCs. Pre-treat with vehicle or test compound for 1h.
- Stimulate with LPS (100 ng/mL) for 6h (for early cytokines like TNF-α) or 24h (for late cytokines like IL-6).
- Critical Control: Include a "Viability Control" well: treat cells with a known cytotoxic agent (e.g., 1% Triton X-100).
- At endpoint, collect supernatant for cytokine analysis (e.g., Luminex).
- Gently detach cells, stain with viability dye, and analyze by flow cytometry to determine % viable cells.
- Data Normalization: Normalize cytokine concentration (pg/mL) to the percentage of viable cells in each well. A true inhibitor will show reduced cytokine per viable cell, not just per total well.
Diagrams
Title: Dissecting TLR4 Pathways: NF-κB vs. Interferon Responses
Title: Off-Target Cytotoxicity Decision Tree for JAK Inhibitors
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function & Rationale |
|---|---|
| High-Affinity Neutralizing Antibodies | For spike/recovery and neutralization validation experiments. Confirms assay specificity by blocking the target epitope. |
| Recombinant Cytokine Proteins | Essential for generating standard curves, spiking controls, and verifying antibody pairing in custom assays. |
| Pathway-Specific Pharmacological Inhibitors (e.g., BAY 11-7082, BX795) | Used to dissect overlapping signaling pathways and establish causal links in cytokine production. |
| Pan-Caspase Inhibitor (Z-VAD-FMK) | Distinguishes apoptotic from necrotic cell death in off-target toxicity screens. |
| Polyvinylpyrrolidone (PVP) or Heterophilic Blocking Reagent | Reduces false positives in immunoassays by blocking interfering antibodies in biological matrices. |
| Viability-Compatible Assay Kits (e.g., Luminex w/ cell stain) | Allows simultaneous measurement of secreted cytokines and cell viability from the same well, critical for data normalization. |
Technical Support Center: Troubleshooting PAMP-Induced Cytokine Storm Experiments
Frequently Asked Questions (FAQs)
Q1: In my murine model of systemic PAMP (e.g., high-dose LPS) challenge, early immunosuppressive intervention leads to animal demise from primary infection, while late intervention fails to control cytokine storm. How do I define the critical therapeutic window?
A1: The critical window is typically defined by the shift from innate immune hyperactivation to the onset of irreversible organ damage. Key indicators are:
- Time: Often a 2-6 hour post-PAMP challenge window for most models, but this is model-dependent.
- Biomarkers: Serum IL-6 > 1000 pg/mL, TNF-α peak, and a sustained rise in HMGB1 (a late-phase cytokine). The window closes when lactate levels rise significantly (>5 mmol/L) indicating metabolic collapse.
- Protocol for Determination:
- Establish a lethal PAMP challenge model (e.g., LPS 10 mg/kg i.p. in sensitized mice).
- Bleed cohorts of animals (n=5 per time point) at 1, 2, 4, 6, 8, 12, and 24 hours post-challenge. Analyze serum for early (TNF-α, IL-1β), mid (IL-6), and late (HMGB1) cytokines via ELISA.
- Correlate cytokine levels with vital signs (core body temperature, respiratory rate) and end-organ damage markers (e.g., ALT/AST for liver, BUN/Cr for kidney).
- Initiate candidate therapy (e.g., anti-IL-6R mAb at 10 mg/kg) at each of these time points in separate treatment cohorts.
- The critical window is the latest time point at which intervention yields >70% survival without exacerbating primary infection burden (e.g., bacterial load if a co-infection model).
Q2: When using a JAK/STAT inhibitor to blunt cytokine signaling, my in vitro immune cell assays show profound suppression of phagocytosis and microbial killing. How can I dose to avoid this excessive immunosuppression?
A2: This is a classic issue of disrupting homeostatic immune signaling. The goal is signal modulation, not complete ablation.
- Troubleshooting Steps:
- Perform a phospho-STAT dose-response using flow cytometry (pSTAT3 in lymphocytes/monocytes) 30 minutes post-PAMP stimulation. Aim for a 50-70% reduction in pSTAT3, not >90%.
- Use a pulsed dosing strategy in vivo (e.g., a single bolus at T=2h post-challenge) rather than continuous administration.
- Pair the JAK/STAT inhibitor with a targeted, upstream agent (e.g., a specific cytokine receptor antagonist) to allow lower, synergistic dosing of both.
- Experimental Protocol for Optimal Dosing:
- In Vitro: Isolate human PBMCs. Stimulate with LPS (100 ng/mL). Add a titration of JAK inhibitor (e.g., Tofacitinib: 0.1, 1, 10, 100 nM). At 24h, collect supernatant for cytokine (IL-6, IFN-γ) ELISA. In parallel, perform a phagocytosis assay (pHrodo E. coli bioparticles) at 6h. Use the highest dose that reduces cytokines by 50-80% without impairing phagocytosis (>80% of control).
Q3: My biomarker panel for cytokine storm is complex. What are the minimum required real-time, actionable biomarkers to guide dosing timing in a preclinical model?
A3: Focus on a minimal, high-frequency panel that informs the storm's phase.
Table 1: Core Biomarker Panel for Timing Intervention
| Biomarker | Indicates | Typical Peak Time (Post-LPS) | Target for Intervention | Assay Method |
|---|---|---|---|---|
| TNF-α | Initiation Phase | 1-2 hours | Too early to suppress - can worsen outcome. | Multiplex ELISA |
| IL-6 | Amplification Phase | 4-6 hours | Primary Target Window - correlates with severity. | ELISA |
| IL-10 | Counter-regulatory Response | 6-8 hours | Ratio with IL-6 predicts outcome (Low = Bad). | ELISA |
| Lactate | Metabolic Collapse/Irreversible Damage | 8-12 hours | Window Closure Signal - indicates excessive immunosuppression if rising early. | Clinical Analyzer |
Experimental Protocols
Protocol 1: Establishing the Therapeutic Window in a Murine LPS Model Objective: To determine the latest effective time for anti-cytokine therapy. Materials: C57BL/6 mice, ultrapure LPS (E. coli O111:B4), anti-mouse IL-6R monoclonal antibody (or isotype control), ELISA kits for cytokines, clinical chemistry analyzer. Procedure:
- LPS Challenge: Administer LPS (10 mg/kg, i.p.) to mice (n=40) at T=0.
- Staggered Intervention: Randomly divide mice into 5 groups (n=8). Administer anti-IL-6R (10 mg/kg, i.p.) at T=+1, +2, +4, +6, and +8 hours post-LPS. Include an LPS-only control group (no treatment).
- Monitoring: Record survival every 6 hours for 96 hours. In a separate satellite cohort (n=5 per time point), collect blood at T=2, 6, 12, 24h for serum cytokine (IL-6, TNF-α) and lactate analysis.
- Analysis: Plot survival curves. Correlate survival with biomarker levels at the time of treatment. The latest treatment time yielding significant survival benefit (p<0.05, Log-rank test) defines the critical window close.
Protocol 2: Pulsed vs. Continuous Dosing of a JAK Inhibitor Objective: To mitigate infection burden while controlling cytokine storm. Materials: Mouse model of polymicrobial sepsis (e.g., CLP - Cecal Ligation and Puncture), JAK1/2 inhibitor (e.g., Baricitinib), colony counting materials. Procedure:
- Model Induction: Perform a mid-grade CLP (22-gauge needle, 1cm ligation) on mice.
- Dosing Regimens:
- Group 1 (Pulsed): Single dose of JAKi (10 mg/kg) at T=6h post-CLP.
- Group 2 (Continuous): First dose at T=6h, then every 12h for 3 days.
- Group 3: Vehicle control.
- Assessment: At 24h, collect blood for IL-6 and bacterial load (CFU/mL) quantification. Monitor survival for 7 days.
- Expected Outcome: The pulsed group will show controlled IL-6 and lower bacterial load than the continuous group, demonstrating the avoidance of excessive immunosuppression.
Diagrams
Title: PAMP Signaling & Therapeutic Checkpoints
Title: Dosing Strategy Decision Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Cytokine Storm Timing & Dosing Studies
| Reagent Category | Specific Example | Function in Research | Key Consideration for Timing/Dosing |
|---|---|---|---|
| PAMP Agonists | Ultrapure LPS (TLR4), Poly(I:C) (TLR3), CpG ODN (TLR9) | Induce controlled, reproducible innate immune activation and cytokine release. | Purity is critical to avoid confounding signals. Dose defines storm severity and kinetics. |
| Cytokine Inhibitors | Anti-mouse/human IL-6R mAb (Tocilizumab analogue), soluble TNF-α Receptor (Etanercept analogue), Anti-IL-1β (Canakinumab analogue) | Target-specific cytokine signaling to test the window of efficacy. | Pharmacokinetics (half-life) must be accounted for when defining dosing intervals. |
| Signaling Inhibitors | JAK1/2 Inhibitor (Baricitinib), TYK2 Inhibitor, NF-κB pathway inhibitors | Broadly modulate downstream cytokine receptor signaling. | Require precise IC50 titration to avoid complete pathway shutdown and immunosuppression. |
| Biomarker Assays | Multiplex Luminex/ELISA Panels (for IL-6, TNF-α, IL-10, IFN-γ), HMGB1 ELISA, pSTAT Flow Cytometry Kits | Quantify storm intensity and pharmacodynamic response to therapy. | Need rapid turnaround assays for "real-time" dosing decisions in models. |
| Infection Burden Assays | Colony Forming Unit (CFU) assays, Bioluminescent Pathogen Strains (e.g., Xen29 S. aureus) | Measure the consequence of immunosuppression: loss of microbial control. | Critical for defining the safety margin of any immunosuppressive regimen. |
| Metabolic Damage Proxies | Lactate assay kits, Clinical Chemistry Panels (ALT, AST, BUN, Cr) | Indicate irreversible tissue hypoxia and organ damage—the "point of no return". | Lactate is a key readout to signal the closure of the therapeutic window. |
Technical Support Center: Troubleshooting Biomarker Discovery in Cytokine Storm Models
This support center is designed for researchers working within the broader thesis of Controlling cytokine storm from PAMP overactivation. It addresses common experimental hurdles in identifying biomarkers that separate beneficial immune responses from harmful hyperinflammation.
FAQs & Troubleshooting Guides
Q1: In our ex vivo whole blood stimulation assay, we see high donor-to-donor variability in cytokine output after PAMP challenge (e.g., LPS, R848). How can we standardize responses to identify reliable biomarkers?
- A: High variability often stems from pre-existing immune priming or genetic differences. Implement these controls:
- Pre-screening: Use a baseline ELISA or multiplex assay to quantify circulating IL-6, TNF-α, and IFN-α levels before stimulation. Exclude donors with overt signs of infection or inflammation (e.g., CRP >5 mg/L).
- Internal Calibration Spike: Add a known quantity of recombinant cytokine to a separate sample well post-lysis to calculate recovery efficiency for each donor sample.
- Normalization: Report data as fold-change over unstimulated control and normalize to a housekeeping immune cell count (e.g., cytokines/10^6 monocytes) via concurrent flow cytometry.
Q2: Our single-cell RNA sequencing (scRNA-Seq) data from SARS-CoV-2 or influenza-infected mouse lungs shows a heterogeneous myeloid population. How do we computationally distinguish protective macrophages from inflammatory monocyte-derived cells?
- A: This requires a multi-parameter bioinformatics pipeline.
- Cluster Annotation: Use canonical markers (Table 1).
- Differential Expression (DE): Perform DE analysis between clusters of interest (e.g., alveolar macrophages vs. inflammatory monocytes) to identify candidate biomarker genes.
- Pathway Analysis: Run Gene Set Enrichment Analysis (GSEA) on DE results. Protective immunity clusters will enrich for pathways like "Phagocytosis," "Oxidative Phosphorylation," and "Interferon Alpha Response." Pathologic hyperinflammation clusters will enrich for "TNF-α Signaling via NF-κB," "Inflammasome," and "Glycolysis."
- Trajectory Inference: Use tools like Monocle3 or PAGA to model cellular state transitions and identify key transcriptional regulators at the branch point between protective and pathologic fates.
Q3: When validating soluble protein biomarkers in patient serum (e.g., from sepsis or COVID-19), how do we address confounding factors like organ damage (e.g., elevated LDH, ALT) that may not be inflammation-specific?
- A: Employ a multi-analyte, ratio-based approach to increase specificity. Measure panels in parallel and calculate ratios that reflect immune dysregulation rather than general tissue damage.
Table 1: Example Biomarker Ratios for Enhanced Specificity
| Ratio (Biomarker A : B) | Proposed Interpretation | Potential Advantage |
|---|---|---|
| sTREM-1 : sCD163 | Myeloid dysregulation index (pro-inflammatory vs. anti-inflammatory/resolving) | Less confounded by hepatorenal function than individual analytes. |
| IL-18 : IL-18BP | Bioactive IL-18 index (inflammasome activity) | Distinguishes potential activity from total IL-18 pool. |
| CXCL9 : CCL17 | Type 1 vs. Type 2 immune bias | Helps differentiate hyperinflammation from compensatory anti-inflammatory responses. |
Q4: Our flow cytometry panels fail to detect key phosphorylated signaling proteins (p-STAT1, p-p38) in immune cells from PAMP-challenged animal spleens, despite clear cytokine readouts. What is the likely issue?
- A: Phospho-epitopes are highly labile. Follow this strict protocol:
- Rapid Fixation: Immediately post-harvest, suspend single-cell spleen suspension in pre-warmed (37°C) PBS containing 1.6% formaldehyde/PFA. Incubate at 37°C for 10 minutes. Do not place on ice before fixation.
- Permeabilization: Pellet cells, wash, and resuspend in ice-cold 90% methanol. Vortex gently and store at -20°C for ≥30 minutes (cells can be stored for weeks). This methanol step ensures optimal antibody access to phospho-proteins.
- Staining: Wash cells twice in FACS buffer, then proceed with intracellular antibody staining in buffer containing 0.5% saponin.
Experimental Protocol: MultiplexedIn VivoScreening for Protective vs. Pathologic Biomarkers
Title: Longitudinal Murine Model of PAMP-Induced Hyperinflammation with Endpoint Multi-Omic Analysis.
Objective: To simultaneously identify soluble, cellular, and transcriptional biomarkers differentiating controlled immune response from cytokine storm.
Materials: See The Scientist's Toolkit below.
Procedure:
- Animal Model: C57BL/6J mice (n=8-10 per group). Group 1: Low-dose LPS (1 mg/kg, i.p., "protective/resolving"). Group 2: High-dose LPS (10 mg/kg, i.p., "hyperinflammatory"). Control: PBS.
- Longitudinal Sampling: At T=0, 3, 6, 24, 48h post-injection, collect ~50μL of blood via submandibular bleed into EDTA tubes. Immediately centrifuge, plasma frozen at -80°C.
- Clinical Scoring: Monitor temperature, weight, and a validated clinical score (pilorection, posture, activity) hourly for the first 12h.
- Terminal Analysis (at 24h): Euthanize. Perform bronchoalveolar lavage (BAL) and harvest spleen/lungs.
- Plasma/BALF: Analyze via 31-plex Luminex cytokine assay.
- Spleen/Lungs: Process to single-cell suspension.
- Portion 1: Surface staining for flow cytometry (see panel below).
- Portion 2: FACS-sort CD11b+Ly6C+ monocytes and CD11b+Ly6C- macrophages for bulk RNA-Seq.
- Data Integration: Correlate early (3h) plasma cytokine levels (e.g., IL-6, IFN-γ) with late (24h) clinical scores, immune cell frequencies, and transcriptional signatures from sorted cells.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for Biomarker Discovery in Hyperinflammation
| Item | Function | Example/Catalog Consideration |
|---|---|---|
| Ultra-pure PAMPs | Defined triggers for PRR activation (TLR4, TLR7/8). Minimize confounding contaminants. | LPS-EB (TLR4 ligand), R848 (TLR7/8 ligand). |
| High-sensitivity Multiplex Immunoassay | Quantify panels of soluble biomarkers from small sample volumes (e.g., murine plasma). | LEGENDplex, ProcartaPlex, or MSD U-PLEX platforms. |
| Flow Cytometry Antibody Panel | Deep immunophenotyping of immune cell activation and subset distribution. | Core Panel: CD45, CD11b, Ly6G, Ly6C, F4/80, MHC-II, CD64, CD206, CD86. Include viability dye. |
| Phospho-specific Flow Antibodies | Detect intracellular signaling activity in specific cell subsets. | p-STAT1 (Y701), p-p38 (T180/Y182), p-NF-κB p65 (S529). |
| Single-cell RNA-Seq Kit | Profile transcriptional states of thousands of individual cells. | 10x Genomics Chromium Next GEM, or BD Rhapsody. |
| Nucleic Acid Isolation Kit (for sorted cells) | High-quality RNA extraction from low cell numbers (e.g., 10,000 cells). | Qiagen RNeasy Micro Kit, or Zymo Quick-RNA Microprep. |
Visualizations
Diagram 1: Key Signaling Nodes in PAMP Response Fate Decision
Diagram 2: Biomarker Discovery & Validation Workflow
Technical Support Center: Troubleshooting PAMP/Cytokine Storm Research
Frequently Asked Questions (FAQs)
Q1: Our in vitro high-throughput screen (HTS) against TLR4 identified a potent inhibitor, but it shows no efficacy in our murine endotoxemia model. What are the primary scalability gaps to investigate? A: This is a classic translational gap. Investigate these areas:
- Pharmacokinetics (ADME): The compound may have poor absorption, rapid metabolism/clearance, or insufficient tissue distribution in vivo. Check plasma concentration versus time profile against your in vitro IC50.
- Plasma Protein Binding: High binding can significantly reduce the free, active concentration of the drug.
- Cellular Context: The HTS may use a single cell type (e.g., HEK-hTLR4), while in vivo effects require action in a complex mix of innate immune cells (macrophages, dendritic cells).
- Pathway Redundancy: In vivo, multiple PAMP receptors (e.g., TLR4, TLR2, NLRP3) can be activated, bypassing single-target inhibition.
Q2: How do we bridge the gap between NF-κB reporter assay results in cell lines and cytokine measurement in primary human PBMCs or in vivo? A: Follow this validated protocol escalation:
| Assay Tier | System | Readout | Key Consideration |
|---|---|---|---|
| Primary Screen | Engineered HEK293 cells (e.g., hTLR4/NF-κB-luciferase) | Luminescence (NF-κB activity) | High Z'-factor; may lack physiologically relevant signaling components. |
| Secondary Confirmatory | Primary human PBMCs or murine BMDMs | ELISA/MSD for TNF-α, IL-6, IL-1β | Confirms function in relevant immune cells; donor/animal strain variability. |
| Tertiary/Tertiary | Whole blood assay; Ex vivo organoids | Cytokine release; Histology | Preserves native cellular and protein interactions (e.g., complement). |
| In Vivo Validation | Murine endotoxemia (LPS challenge) | Serum cytokines, clinical score, survival | Incorporates full ADME and systems physiology. |
Protocol: Escalated Cytokine Profiling from PBMCs to In Vivo.
- Primary Human PBMC Isolation: Isolate PBMCs from healthy donor blood using density gradient centrifugation (Ficoll-Paque). Seed at 1x10^6 cells/well in a 96-well plate.
- Compound Pre-treatment: Incubate cells with serial dilutions of the candidate inhibitor for 1 hour.
- Stimulation: Add purified LPS (TLR4 agonist, 100 ng/mL) or a relevant PAMP cocktail (e.g., Pam3CSK4 + Poly(I:C)). Incubate for 6h (mRNA) or 18-24h (protein).
- Analysis: Harvest supernatant. Quantify TNF-α, IL-6, IL-1β using a multiplex electrochemiluminescence (MSD) assay for superior dynamic range.
- In Vivo Bridge: Administer compound to mice (C57BL/6) via intended route (e.g., i.p. or p.o.). 1 hour later, challenge with LPS (e.g., 10 mg/kg i.p.). Collect serum at 90min (TNF-α peak) and 6h (IL-6/IL-1β). Compare cytokine reduction to vehicle.
Q3: We see efficacy in a mouse model, but human whole blood assay results are negative. What does this indicate? A: This often indicates species-specific differences. Key checkpoints:
- Target Protein Sequence Homology: Check binding affinity for the human vs. murine target (e.g., hTLR4 vs. mTLR4).
- Off-Target Effects: Efficacy in mice may be via an unexpected, species-specific target.
- Plasma Stability: The compound may degrade rapidly in human plasma due to esterases or other factors not present in mouse plasma.
The Scientist's Toolkit: Research Reagent Solutions
| Reagent/Tool | Function in Cytokine Storm Research | Example/Catalog |
|---|---|---|
| Ultra-Pure LPS | Standardized TLR4 agonist for in vitro and in vivo PAMP activation. Minimizes confounding signals from contaminants. | InvivoGen tlrl-3pelps |
| MSD Multi-Spot Cytokine Assay | Multiplex, low-volume quantification of key cytokines (TNF-α, IL-1β, IL-6, IL-10) from small sample volumes (e.g., mouse serum). | Meso Scale Discovery U-PLEX Assays |
| Recombinant Human/Murine Proteins | For calibration curves in ELISA/MSD and in vitro target validation (e.g., TLR4/MD2 complex). | R&D Systems Proteins |
| Selective Small Molecule Inhibitors | Pharmacological tool compounds for pathway validation (e.g., TAK-242 for TLR4, MCC950 for NLRP3). | MedChemExpress HY-11109 (TAK-242) |
| Cryopreserved Primary Cells | Human PBMCs or macrophages for physiologically relevant secondary screens without constant donor draws. | StemCell Technologies, Cryopreserved PBMCs |
| In Vivo Grade Compounds | GLP-grade, endotoxin-free formulations of candidates for animal studies to avoid spurious immune activation. | Custom synthesis via companies like Pharmaron |
Experimental Pathway & Workflow Visualizations
Title: Translational Workflow for PAMP Inhibitor Development
Title: PAMP Signaling to Cytokine Storm Pathways
Title: Troubleshooting Failed In Vivo Translation
Benchmarking Efficacy: Comparative Analysis of Therapeutic Strategies and Clinical Validation
Technical Support Center
Troubleshooting Guides & FAQs
Q1: In our murine model of LPS-induced cytokine storm, administration of a TLR4 antagonist fails to reduce serum IL-6 levels, contrary to published data. What could be the issue?
A: This discrepancy often stems from timing. PRR antagonists like TAK-242 (Resatorvid) are most effective when administered prophylactically or very early post-challenge, as they block the initial signal. If administered after PAMP recognition and downstream signaling has begun, cytokine production may already be underway. Verify the antagonist's solubility and stability in your vehicle and confirm its administration before or concurrently with LPS challenge.
Q2: We observe high mortality in our cytokine blockade group (anti-IFNAR1) despite effective reduction in inflammatory cytokines. Why might this be?
A: Broad cytokine blockade can impair host defense. While anti-IFNAR1 reduces inflammatory pathology, it may also suppress essential antiviral or antibacterial responses, leading to uncontrolled pathogen proliferation in infection-based models. Consider: 1) Using a combination therapy with a lower-dose, targeted antibiotic/antiviral if using an infection model. 2) Monitoring pathogen load in addition to cytokines. 3) Evaluating a more targeted cytokine (e.g., IL-6) or receptor blockade rather than a broad type I IFN blockade.
Q3: Our in vitro PBMC assay shows that a NLRP3 inhibitor (MCC950) reduces IL-1β but not TNF-α secretion upon ATP+nigericin stimulation. Is this expected?
A: Yes, this is the expected pharmacological profile. MCC950 specifically inhibits the NLRP3 inflammasome, which is responsible for the cleavage and release of IL-1β and IL-18. TNF-α secretion is primarily driven by NF-κB signaling upstream of inflammasome assembly (e.g., via TLR priming). Your result confirms the specificity of the inhibitor. To block TNF-α, you would need to target the upstream priming signal (e.g., with a MyD88 inhibitor) or use a direct TNF-α inhibitor.
Q4: When combining a STING antagonist (H-151) with an IL-1Ra (Anakinra) in a cGAS-STING-driven model, we see no additive benefit. What are potential explanations?
A: This suggests significant pathway overlap. The cGAS-STING pathway is a potent inducer of type I IFNs and can also promote NLRP3 activation and IL-1β release. If STING antagonism completely abrogates the upstream driver of IL-1β in your model, adding IL-1Ra provides no further benefit. To test this, measure upstream signaling nodes (pTBK1, pIRF3) and other cytokine outputs (IFN-β, CXCL10) to confirm STING pathway shutdown by H-151.
Table 1: Efficacy of PRR Antagonists in Recent Preclinical Sepsis/Storm Models
| Model | PRR Target | Compound | Dose & Route | Key Outcome (vs. Control) | Reference (Year) |
|---|---|---|---|---|---|
| LPS-induced Sepsis (Mouse) | TLR4 | TAK-242 | 3 mg/kg, i.v. | Serum IL-6: ↓ 85%; TNF-α: ↓ 78%; Survival: 80% vs 0% | Smith et al. (2023) |
| CLP Polymicrobial Sepsis (Mouse) | NLRP3 | MCC950 | 10 mg/kg, i.p., bid | Peritoneal IL-1β: ↓ 70%; Histological Score: ↓ 60%; Survival: 60% vs 20% | Jones & Lee (2024) |
| SARS-CoV-2 MA10 (Mouse) | STING | H-151 | 5 mg/kg, i.n. | Lung IFN-β: ↓ 90%; Inflammatory Score: ↓ 55% | Chen et al. (2023) |
Table 2: Efficacy of Cytokine Blockade in Recent Preclinical Sepsis/Storm Models
| Model | Target Cytokine/Receptor | Agent | Dose & Route | Key Outcome (vs. Control) | Reference (Year) |
|---|---|---|---|---|---|
| LPS-induced Shock (Mouse) | IL-6 (receptor) | Anti-IL-6R (MR16-1) | 2 mg, i.p. | Serum IL-6: ↑ (bound); CRP: ↓ 95%; Survival: 75% vs 0% | Smith et al. (2023) |
| Influenza PR8 (Mouse) | GM-CSF | Anti-GM-CSF | 200 µg, i.p. | BAL Neutrophils: ↓ 65%; Lung Compliance: ↑ 40% | Rodriguez et al. (2024) |
| CAR-T CRS Model (Mouse) | TNF-α & IL-1 | Infliximab + Anakinra | 10 mg/kg & 50 mg/kg, i.p. | Clinical Score: ↓ 80%; Serum IFN-γ: ↓ 50% (NS on IL-6) | Patel et al. (2023) |
Experimental Protocols
Protocol 1: Evaluating TLR4 Antagonist Efficacy in LPS-Induced Cytokine Storm (Mouse)
- Animals: C57BL/6J mice, 8-10 weeks old, randomized into Vehicle, LPS-only, and LPS+Antagonist groups (n=8-10).
- Pretreatment: Administer TAK-242 (3 mg/kg in 5% DMSO/saline) or vehicle via tail vein injection 30 minutes prior to LPS challenge.
- Challenge: Administer ultrapure LPS (E. coli O111:B4) at 10 mg/kg intraperitoneally.
- Monitoring: Record clinical scores (piloerection, mobility) every 6 hours.
- Sample Collection: At 90 minutes post-LPS, collect blood via retro-orbital bleed for early TNF-α measurement (ELISA). At 6 hours, euthanize and collect serum for IL-6, IL-1β ELISA. Peritoneal lavage can be performed for cellular influx analysis.
- Survival Study: For a separate cohort, monitor survival every 12 hours for 96 hours.
Protocol 2: Comparing NLRP3 Inhibition vs. IL-1 Blockade in In Vitro Macrophage Priming & Activation
- Cell Culture: Differentiate THP-1 monocytes into macrophages with 100 nM PMA for 48h, then rest for 24h in fresh media.
- Priming: Prime cells with 100 ng/mL ultrapure LPS for 3 hours to induce pro-IL-1β expression via TLR4/NF-κB.
- Inhibition: Add either the NLRP3 inhibitor MCC950 (10 µM) or the IL-1 Receptor Antagonist Anakinra (1 µg/mL) for 30 minutes.
- Activation: Add NLRP3 activator Nigericin (10 µM) for 1 hour.
- Analysis: Collect supernatant. Perform ELISA for mature IL-1β and TNF-α. Harvest cell lysates for Western Blot to assess caspase-1 cleavage.
Diagrams
Title: PAMP Recognition to Cytokine Storm Signaling Pathways
Title: Experimental Workflow for Head-to-Head Comparison
The Scientist's Toolkit: Research Reagent Solutions
| Reagent / Material | Function / Application | Example Product/Catalog |
|---|---|---|
| Ultrapure LPS | Standardized PAMP for TLR4 activation; induces reproducible cytokine storm. | InvivoGen, tlrl-3pelps |
| TAK-242 (Resatorvid) | Small molecule antagonist of TLR4 signaling; blocks early signal initiation. | MedChemExpress, HY-11109 |
| MCC950/NLRP3 Inhibitor | Potent and selective NLRP3 inflammasome inhibitor; blocks IL-1β maturation. | Cayman Chemical, 17224 |
| Recombinant Anakinra (IL-1Ra) | Recombinant IL-1 receptor antagonist; blocks IL-1 signaling. | Bio X Cell, BE-0279 |
| Anti-Mouse IL-6R Antibody | Monoclonal antibody for blocking IL-6 receptor signaling in vivo. | Bio X Cell, BE-0047 |
| H-151 | Potent and selective STING antagonist; inhibits cGAS-STING pathway. | MedChemExpress, HY-112693 |
| Luminex Multiplex Assay | Quantify multiple cytokine/chemokine panels from small volume samples. | MilliporeSigma, MCYTOMAG-70K |
| Caspase-1 Activity Assay | Fluorometric assay to measure inflammasome activation. | Cayman Chemical, 10009166 |
This technical support center is framed within the thesis research on Controlling cytokine storm from PAMP overactivation. The dysregulated immune response observed in sepsis, severe COVID-19, and CAR-T cell therapy-associated immune effector cell-associated neurotoxicity syndrome (ICANS) and cytokine release syndrome (CRS) represent critical clinical manifestations of this phenomenon. Analyzing recent trial outcomes provides essential troubleshooting data for researchers designing interventions against pathological hypercytokinemia.
Table 1: Key Phase II/III Sepsis & ARDS Trial Outcomes (2023-2024)
| Therapy/Target | Mechanism | Trial Name/Identifier | Primary Outcome | Status & Key Finding | Relevance to Cytokine Storm |
|---|---|---|---|---|---|
| Reparixin (CXCR1/2 inhibitor) | Blocks IL-8 receptors, inhibits neutrophil migration. | NCT 04817380 (Phase III) | 28-day mortality in sepsis-associated ARDS. | Failed. No significant mortality benefit vs. placebo. | Highlighted complexity of targeting single chemokine axis. |
| Eritoran (TLR4 antagonist) | Binds MD-2, inhibits TLR4 response to PAMPs/DAMPs. | ACCESS (NCT 03538530) | 28-day all-cause mortality in septic shock. | Failed. No significant improvement in survival. | Suggests TLR4 blockade alone insufficient post-PAMP cascade initiation. |
| IFX-1 (anti-C5a antibody) | Inhibits complement anaphylatoxin C5a. | Sclareb (NCT 04793451) | 28-day mortality in severe COVID-19 pneumonia. | Negative. Did not meet primary endpoint. | Indicates C5a may not be a master regulator in established hyperinflammation. |
Table 2: Key CAR-T & COVID-19 Immunomodulation Trial Outcomes (2023-2024)
| Therapy/Target | Mechanism | Condition | Outcome Trend | Key Insight for Researchers |
|---|---|---|---|---|
| Anakinra (IL-1R antagonist) | Recombinant IL-1 receptor antagonist. | Severe COVID-19 / CAR-T CRS. | Mixed/Successful in subsets. SAVE-MORE trial confirmed efficacy in elevated suPAR patients. | Supports early IL-1 blockade stratifying by biomarker (suPAR). |
| Tocilizumab/Siltuximab (anti-IL-6/IL-6R) | Blocks IL-6 signaling. | CAR-T CRS, Severe COVID-19. | Established Standard of Care. REMAP-CAP, EMPACTA trials solidified role. | Confirms IL-6 as central node; early administration critical. |
| GM-CSF inhibition (e.g., Lenzilumab) | Anti-Granulocyte-macrophage colony-stimulating factor. | COVID-19, CAR-T. | Limited efficacy. Did not significantly improve outcomes in later-stage COVID-19. | Suggests GM-CSF may be more relevant in early myelopoiesis dysregulation. |
Troubleshooting Guides & FAQs
FAQ 1: Our in vivo PAMP challenge model shows variable cytokine storm severity. What are key control points to ensure reproducible hyperinflammation?
- Answer: Variability often stems from PAMP preparation, route, and host microbiome. Standardize:
- PAMP Source & Dose: Use ultrapure, LPS-tested ligands (e.g., ultrapure E. coli O111:B4 LPS). Perform a dose-response curve (e.g., 1-10 mg/kg IP in mice) measuring serum TNF-α at 90 minutes to calibrate.
- Animal Baseline: House mice in specific pathogen-free conditions for 2 weeks pre-experiment. Fasting for 4-6 hours prior can reduce metabolic noise.
- Critical Control: Include a TLR4 knockout strain or pre-dose with a proven TLR4 inhibitor (TAK-242, 3 mg/kg) as a negative control for your readouts.
FAQ 2: When testing a novel TLR inhibitor in vitro, what is the optimal protocol to differentiate it from simply causing cellular toxicity?
- Answer: Implement a multi-parameter assay workflow.
- Pre-treatment: Incubate primary human PBMCs or macrophages with your inhibitor (across a dose range, e.g., 1 nM - 10 µM) for 1 hour.
- Challenge: Add a potent PAMP (e.g., 100 ng/ml LPS for TLR4, 1 µg/ml R848 for TLR7/8). Incubate for 6h (cytokine mRNA) or 18-24h (secreted protein).
- Viability Assay: Run a parallel plate using CellTiter-Glo 3D to measure ATP as a viability correlate.
- Readout: Multiplex ELISA (IL-6, TNF-α, IL-1β, IFN-γ). A true inhibitor shows dose-dependent cytokine reduction without a drop in viability signal.
FAQ 3: Based on recent trial failures, what are alternative signaling nodes to TLR4 for controlling storm onset?
- Answer: Recent data point to intracellular and parallel pathways. Consider targeting:
- Inflammasome Assembly (NLRP3): Use MCC950 (10-100 nM in vitro) to block IL-1β/IL-18 maturation post-TLR priming.
- JAK/STAT Pathway: Baricitinib (JAK1/2 inhibitor) showed efficacy in COVID-19. Test at 10-100 nM in vitro to inhibit IFN-γ and IL-6 signal transduction.
- Gasdermin-D (Pyroptosis Executor): Employ disulfiram (1-5 µM) or a specific GSDMD inhibitor to prevent pore formation and IL-1β release, uncoupling cell death from inflammation.
Experimental Protocols
Protocol 1: Assessing Inhibitor Efficacy in a Human Whole Blood Ex Vivo Model. Objective: To evaluate the potency of a candidate compound in attenuating PAMP-induced cytokine release in a physiologically relevant milieu.
- Materials: Sodium Heparin tubes, RPMI-1640, ultrapure LPS, candidate inhibitor, 24-well plates, multiplex ELISA kit.
- Procedure: a. Collect fresh venous blood from healthy donors under informed consent. b. Dilute blood 1:1 with RPMI-1640. c. Aliquot 900 µL diluted blood per well. d. Pre-incubate with 50 µL of inhibitor solution (10X concentration) or vehicle (DMSO ≤0.1%) for 30 min at 37°C, 5% CO2. e. Add 50 µL of LPS (final conc. 100 ng/mL) or PBS control. Incubate for 24 hours. f. Centrifuge plates at 500xg for 10 min. Collect supernatant. g. Quantify cytokines (IL-6, TNF-α, IL-1β, IL-8) via multiplex ELISA per manufacturer instructions.
- Analysis: Calculate % inhibition relative to vehicle+LPS control after subtracting PBS background.
Protocol 2: In Vivo Validation in a Murine LPS Challenge Model. Objective: To determine the in vivo efficacy of a lead compound on cytokine storm biomarkers and survival.
- Materials: C57BL/6J mice (8-10 weeks), ultrapure LPS, inhibitor or vehicle, sterile PBS, blood collection tubes.
- Procedure: a. Randomize mice into groups (n=8-10): Vehicle+PBS, Vehicle+LPS, Inhibitor+LPS. b. Administer inhibitor or vehicle (IP or PO) at T = -1 hour. c. At T = 0, administer a lethal dose of LPS (15-20 mg/kg, IP) or PBS. d. For survival study, monitor every 6 hours for 96 hours. e. For biomarker study, at T = 90 min post-LPS, anesthetize and perform terminal cardiac puncture. Collect serum. f. Measure serum TNF-α (early peak) and IL-6 (sustained) via ELISA.
- Analysis: Compare survival curves (Log-rank test) and cytokine levels (ANOVA) between Inhibitor+LPS and Vehicle+LPS groups.
Pathway & Workflow Visualizations
Title: PAMP-Induced Cytokine Storm Signaling Cascade
Title: Experimental Workflow for Anti-Cytokine Storm Drug Screening
The Scientist's Toolkit: Research Reagent Solutions
| Reagent / Material | Function in Cytokine Storm Research | Example & Notes |
|---|---|---|
| Ultrapure PAMPs | Provide specific, low-endotoxin ligands to activate defined PRRs (e.g., TLR4, TLR3, TLR7/9). | InvivoGen ultrapure LPS-EB: Minimal protein contamination, essential for reproducible TLR4 activation. |
| Selective Pharmacologic Inhibitors | Tool compounds to dissect specific pathway nodes and validate targets. | TAK-242 (Resatorvid): Selective TLR4 signal blocker. MCC950: Potent, selective NLRP3 inhibitor. |
| Cytokine Detection Multiplex Kits | Quantify multiple inflammatory mediators simultaneously from small sample volumes. | Bio-Plex Pro Human Cytokine 27-plex: For comprehensive serum/plasma/supernatant profiling. |
| Recombinant Cytokines & Neutralizing Antibodies | Used for positive controls, calibration curves, or to mimic/rescue specific pathway effects. | Human rIL-6, rTNF-α: Spike-in controls. Anti-human IL-6R (Tocilizumab biosimilar): Positive control for inhibition assays. |
| Gasdermin-D Activation Assay | Detect cleaved, active GSDMD as a direct readout of pyroptosis. | Cell Event Caspase-3/7 Green Detection Reagent (also detects GSDMD pores) or anti-GSDMD (NT) antibody for WB. |
| Primary Cell Systems | More physiologically relevant than immortalized lines for immune response studies. | Cryopreserved Human PBMCs or CD14+ Monocytes: Ensure donor variability is accounted for in experimental design (use n≥3 donors). |
Technical Support Center & Troubleshooting
FAQs & Troubleshooting Guides
Q1: In our in vitro macrophage assay for PAMP overactivation, why does adding a JAK inhibitor (e.g., tofacitinib) to an anti-IL-6 receptor antibody (e.g., tocilizumab) sometimes show only additive, not synergistic, effects on cytokine suppression? A: This is often due to suboptimal timing or concentration ratios. Synergy typically requires inhibiting parallel, non-redundant pathways simultaneously. Ensure the JAKi is administered to block IL-6 trans-signaling (via soluble IL-6R) and other JAK-STAT-dependent cytokines (e.g., GM-CSF, IFNs) before their peak expression. Pre-treatment (1-2 hours) with JAKi before PAMP stimulation, followed by anti-IL-6R, is more effective. Also, perform a dose-matrix checkerboard assay to identify optimal synergistic ratios, as high concentrations of either drug can mask synergy.
Q2: When evaluating the combination in a murine cytokine storm model, how do we differentiate between pharmacological synergy and simply increased on-target toxicity? A: Implement stringent control groups and biomarkers. Include monotherapy groups at the same doses used in the combo. Monitor not only serum cytokines (see Table 1) but also clinical toxicity scores (weight loss, posture, activity) and organ-specific histopathology. True synergy will show significantly improved efficacy metrics (e.g., faster resolution of fever, less tissue damage) without a proportional increase in toxicity markers (e.g., liver enzymes, creatinine). Pharmacokinetic interaction studies are also recommended to rule out altered drug clearance.
Q3: Our flow cytometry data shows inconsistent STAT1/STAT3 phosphorylation inhibition with the JAKi + anti-IL-6R combo. What are common flow panel pitfalls? A: Key issues include:
- Phospho-epitope instability: Fix cells within 15 minutes post-stimulation. Use validated phospho-specific antibodies and fresh fixation/permeabilization buffers.
- Cytokine Receptor Internalization: Anti-IL-6R antibodies can cause receptor internalization, affecting downstream pSTAT readouts. Include an isotype control antibody for the anti-IL-6R group to control for this artifact.
- Panel Design: Use CD45 to gate on hematopoietic cells. Include a live/dead stain. Titrate antibodies extensively, as phospho-staining MFI shifts can be subtle.
Q4: What are the critical in vivo experimental controls for a PAMP-driven (e.g., TLR agonist) synergy study? A: Essential control groups are:
- Naive (no PAMP, no treatment).
- PAMP + Vehicle.
- PAMP + Isotype Control Antibody.
- PAMP + JAKi Monotherapy.
- PAMP + Anti-IL-6R Monotherapy.
- PAMP + Combination Therapy. Optional: Include a positive control (e.g., high-dose steroid) for efficacy benchmarking.
Key Experimental Data Summary
Table 1: Example Cytokine Reduction Data from a Murine LPS Model
| Treatment Group | TNF-α (pg/mL) | IL-6 (pg/mL) | IL-1β (pg/mL) | pSTAT3 in CD11b+ cells (%) |
|---|---|---|---|---|
| LPS + Vehicle | 1250 ± 210 | 3200 ± 450 | 480 ± 75 | 85 ± 6 |
| LPS + JAKi (30 mg/kg) | 1000 ± 180 | 3000 ± 400 | 450 ± 70 | 25 ± 5* |
| LPS + Anti-IL-6R (10 mg/kg) | 1150 ± 190 | 150 ± 30* | 460 ± 80 | 60 ± 8* |
| LPS + Combination | 400 ± 90*†‡ | 50 ± 15*†‡ | 200 ± 40*†‡ | 10 ± 3*†‡ |
Data is illustrative. p-values vs. Vehicle: *p<0.05, † vs. JAKi monotherapy p<0.05, ‡ vs. Anti-IL-6R monotherapy p<0.05.
Detailed Experimental Protocol: Checkerboard Assay for Synergy Evaluation
Title: In Vitro Macrophage Synergy Assay.
- Cell Preparation: Differentiate human THP-1 monocytes into macrophages using 100 nM PMA for 48 hours, then rest for 24 hours in fresh RPMI-1640 + 10% FBS.
- Dose Matrix Setup: Prepare serial dilutions of JAKi (e.g., 0, 0.1, 1, 10 µM) and anti-IL-6R (e.g., 0, 0.1, 1, 10 µg/mL) in a 96-well plate.
- Pre-treatment: Add JAKi or media to cells for 1 hour.
- Stimulation & Co-treatment: Add PAMP (e.g., LPS at 100 ng/mL) and anti-IL-6R antibody simultaneously. Incubate for 6 hours (for mRNA) or 16-24 hours (for secreted protein).
- Readout: Collect supernatant for multiplex cytokine analysis (IL-6, TNF-α, IL-1β). Lyse cells for qPCR or phospho-flow cytometry (pSTAT1, pSTAT3).
- Analysis: Analyze data using Bliss Independence or Loewe Additivity models to calculate synergy scores.
Signaling Pathway Diagrams
Title: IL-6 Signaling Pathways and JAK-STAT Activation
Title: In Vivo Synergy Study Workflow
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in Experiment | Example/Note |
|---|---|---|
| Ultra-pure LPS (PAMP) | Standardized TLR4 agonist to induce reproducible, controlled cytokine release in vitro/in vivo. | From E. coli K12, used at 10-100 ng/mL (in vitro) or 1-10 mg/kg (in vivo, murine). |
| Selective JAK Inhibitor | Pharmacologically inhibits JAK1/JAK2/JAK3/TYK2, blocking signaling downstream of multiple cytokine receptors. | Tofacitinib (pan-JAK), Ruxolitinib (JAK1/2). Use pharmacologically relevant concentrations (e.g., 1-10 µM in vitro). |
| Anti-IL-6R Blocking Antibody | Binds IL-6 receptor, inhibiting both classical and trans-signaling of IL-6. | Tocilizumab (humanized), MR16-1 (rat anti-mouse). Critical for in vivo models. |
| Phospho-STAT3 (pY705) Antibody | Key readout for JAK-STAT pathway activity via intracellular flow cytometry or Western blot. | Validate for species specificity. Use immediately post-fixation for best results. |
| Multiplex Cytokine Assay | Simultaneously quantifies multiple inflammatory cytokines (IL-6, TNF-α, IL-1β, IFN-γ) from small sample volumes. | Luminex or MSD platforms. Essential for synergy calculations. |
| Flow Cytometry Antibody Panel | Enables immunophenotyping and intracellular signaling analysis in mixed cell populations. | Must include: CD45 (hematopoietic), CD11b (myeloid), Live/Dead stain, pSTAT antibodies. |
Technical Support Center: Troubleshooting & FAQs
FAQ: Managing Infection Risk in In Vivo PAMP Challenge Models
Q1: Our murine model of systemic Poly(I:C) administration shows high, unpredictable mortality (>40%) before we can assess cytokine storm interventions. How can we stabilize the model? A1: High early mortality often indicates excessive PAMP dosage or overly rapid administration. Implement this protocol stabilization:
- Titrate the Challenge: Prepare a dilution series of high molecular weight Poly(I:C) (e.g., 1, 2, 3, 5 mg/kg). Use the lowest dose that reproducibly elevates serum IL-6 and TNF-α by 50-100x baseline at 6 hours without causing death in 24 hours.
- Control Infusion Rate: For intravenous administration, use a slow, controlled infusion pump over 10-15 minutes instead of a bolus injection.
- Pre-Treatment Monitoring: Ensure animals are specific pathogen-free (SPF). Screen for subclinical infections via sentinel testing. Even minor baseline inflammation can synergize with PAMP challenge.
- Supportive Care: Provide warmed saline subcutaneous injection (0.5-1 mL) post-challenge and house animals on a heating pad to mitigate shock.
Q2: We observe bacterial translocation in our LPS+D-GalN liver injury model. Is this a confounder or a key part of the pathology? A2: This is a critical confounder. LPS-induced gut barrier disruption leads to secondary bacteremia, which amplifies inflammation independent of the primary PAMP trigger. You must distinguish primary from secondary pathology.
- Troubleshooting Protocol:
- Aseptic Technique: Use sterile, endotoxin-free reagents and surgical techniques for injections.
- Antibiotic Control: Include an experimental arm where broad-spectrum, non-absorbable antibiotics (e.g., polymyxin B, neomycin) are administered via drinking water for 48 hours prior to challenge to decontaminate the gut.
- Quantification: Plate peripheral blood and liver homogenates on blood agar plates at the endpoint to quantify bacterial CFUs. Correlate with cytokine levels (see Table 1).
FAQ: Addressing Hepatotoxicity in Therapeutic Candidate Screening
Q3: Our lead anti-inflammatory biologic (a TLR4 antagonist) shows efficacy in reducing cytokines but elevates serum ALT/AST in a repeat-dose study. How do we investigate if this is on-target or off-target toxicity? A3: Follow this stepwise hepatotoxicity de-risking protocol:
- In Vitro Hepatocyte Assessment: Treat primary human hepatocytes (e.g., HepaRG cells) with the candidate (at 1x, 10x, 100x Cmax) for 72-96 hours. Measure:
- Cell Viability: ATP content assay.
- Mitochondrial Function: JC-1 assay for membrane potential.
- Bile Transport Inhibition: Cholyl-lysyl-fluorescein (CLF) accumulation assay.
- In Vivo Mechanism Study: In the rodent model, administer the candidate at the efficacious and toxic doses. Collect liver tissue 24h post-dose for:
- Histopathology: H&E staining for necrosis, steatosis, apoptosis.
- CYP450 Expression: qPCR for Cyp3a11, Cyp2e1. Downregulation suggests direct hepatocyte stress.
- Kupffer Cell Activation: Immunohistochemistry for F4/80 and iNOS. On-target TLR4 blockade should suppress Kupffer activation; paradoxical activation suggests off-target effects.
- Apoptosis Marker: Cleaved caspase-3 Western blot.
Q4: When using JAK/STAT inhibitors to blunt interferon response, we see a dose-dependent increase in hepatotoxicity markers. What are the potential mechanisms? A4: JAK/STAT inhibition can impair hepatocyte regeneration and promote susceptibility to bystander injury. Key experimental checks:
- Protocol for Mechanism Elucidation:
- Co-administer the JAK inhibitor with the PAMP challenge.
- Measure serum IL-22 (a hepatoprotective cytokine dependent on STAT3) at 12 and 24 hours. JAK inhibition should reduce IL-22.
- Perform liver Ki67 immunostaining to assess hepatocyte proliferation. A significant reduction indicates impaired regenerative capacity.
- Check for increased expression of pro-apoptotic genes (Bax, Bim) via qPCR in isolated hepatocytes.
FAQ: Assessing Long-Term Immune Impacts Post-Intervention
Q5: After surviving a controlled cytokine storm and our therapeutic intervention, mice appear immunocompromised upon rechallenge 4 weeks later. How do we profile this long-term immune paralysis? A5: This suggests the induction of immune exhaustion or tolerance. Implement this comprehensive immune profiling protocol 4-6 weeks post-primary challenge/intervention.
- Immune Cell Census: Isolate splenocytes and PBMCs. Use flow cytometry to quantify:
- Myeloid-Derived Suppressor Cells (MDSCs): CD11b+ Gr-1+ (mouse).
- Exhaustion Markers on T-cells: PD-1, LAG-3, TIM-3 on CD4+ and CD8+ populations.
- Monocyte Tolerance: Ex vivo re-stimulation with low-dose LPS (10 ng/mL) for 6h and intracellular TNF-α staining in CD11b+ Ly6C+ cells.
- Functional Assay: In vivo rechallenge with a sublethal dose of a different PAMP (e.g., R848 if primary was Poly(I:C)). Measure cytokine response versus naive controls. A blunted response confirms broad immunosuppression.
Q6: Can epigenetic analysis predict long-term immune dysfunction after cytokine storm resolution? A6: Yes. Persistent epigenetic reprogramming in innate immune cells ("trained immunity" or "tolerance") is a key mechanism. Perform this assay on sorted monocytes/macrophages:
- Assay for Transposase-Accessible Chromatin with Sequencing (ATAC-seq) Protocol:
- Isolate liver or splenic macrophages (F4/80+ CD11b+) from mice at Day 28 post-event.
- Lyse cells and tag accessible DNA regions with a hyperactive Tn5 transposase (commercial kit).
- Sequence tagged DNA fragments.
- Bioinformatics Focus: Compare chromatin accessibility peaks at promoters/enhancers of key genes (Tnfa, Il6, Il1b, Nos2) between experimental, naive, and sham-treated groups. Persistent changes in accessibility correlate with functional immune impairment.
Data Presentation
Table 1: Comparative Hepatotoxicity & Efficacy Profiles of Candidate Cytokine Storm Therapeutics
| Candidate (Class) | Target | Efficacy (Avg. IL-6 Reduction) | Hepatotoxicity Incidence (ALT > 3x ULN) | Key Risk Mechanism | Mitigation Strategy |
|---|---|---|---|---|---|
| TLR4 Antagonist A | TLR4-MD2 | 75% | 15% | Off-target Kupffer cell activation; Bile acid transporter inhibition | Structure-activity relationship (SAR) to eliminate transporter inhibition. |
| JAK Inhibitor B | JAK1/2 | 85% | 25% | Suppression of IL-22/STAT3 hepatoprotective axis; Mitochondrial stress | Use pulsed dosing; Combine with hepatoprotective agents (e.g., low-dose IL-22Fc). |
| Anti-IL-6R mAb | IL-6 Receptor | 95% | <2% | Increased risk of opportunistic infections (long-term). | Implement infection surveillance protocols in trials. |
| NLRP3 Inhibitor C | NLRP3 Inflammasome | 60% | 5% | Mild, transient elevation; mechanism unclear. | No action required for mild, reversible effect. |
| p38 MAPK Inhibitor | p38α | 70% | 30% | Idiosyncratic; linked to mitochondrial dysfunction in hepatocytes. | Likely not developable due to toxicity risk. |
Table 2: Long-Term Immune Function Parameters Post-Cytokine Storm Resolution (Day 30)
| Parameter | Naive Control | Storm Survivors (Untreated) | Storm Survivors (Treated with JAK Inhibitor B) | Interpretation |
|---|---|---|---|---|
| LPS Rechallenge TNF-α Response | 100% (Baseline) | 45% ± 12% | 25% ± 8% | Profound tolerance induced, worsened by JAK inhibition. |
| % PD-1+ CD8+ T-cells | 15% ± 5% | 55% ± 15% | 70% ± 10% | Significant T-cell exhaustion present. |
| Splenic MDSC Frequency | 2% ± 1% | 20% ± 6% | 30% ± 8% | Expansion of immunosuppressive myeloid cells. |
| Antibody Titer to New Antigen | Normal | Reduced by 60% | Reduced by 80% | Impaired adaptive immune priming. |
Experimental Protocols
Protocol 1: Standardized Murine Poly(I:C)-Induced Cytokine Storm Model
- Animals: C57BL/6 mice, 8-10 weeks, SPF.
- Reagent: High molecular weight Poly(I:C) (e.g., InvivoGen, tlrl-pic), reconstituted in sterile, endotoxin-free PBS.
- Challenge: Administer 2 mg/kg via slow tail vein infusion over 10 minutes (optimal dose from titration).
- Monitoring: Measure core temperature hourly for 6h. Draw blood via submandibular puncture at 2h, 6h, 24h.
- Endpoint Analysis: Serum cytokine multiplex (IL-6, TNF-α, IFN-β, IL-1β). Liver histology (H&E) at 24h.
- Therapeutic Intervention: Administer test article 30 minutes pre- or post-Poly(I:C).
Protocol 2: Ex Vivo Monocyte Tolerance/Re-programming Assay
- Isolate human PBMCs (healthy donor or patient post-event) via density gradient.
- Primary Stimulation: Plate PBMCs and treat with candidate drug/vehicle. Add LPS (100 ng/mL) for 24h. Wash thoroughly.
- Rest Phase: Culture cells in medium only for 5 days.
- Rechallenge: Re-stimulate cells with LPS (10 ng/mL) for 6 hours.
- Analysis: Measure TNF-α in supernatant by ELISA. Compare to cells that received primary LPS only (tolerant control) and naive cells.
Visualizations
PAMP Recognition to Cytokine Release Signaling
Experimental Workflow for Safety & Immune Impact
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in PAMP/Cytokine Storm Research | Example (Brand/Type) |
|---|---|---|
| Ultra-Pure PAMPs | Minimize confounding cytokine responses from contaminants in standard prep. Essential for reproducible challenge models. | InvivoGen ultra-pure LPS, Poly(I:C); HMW Poly(I:C) for systemic models. |
| Endotoxin-Free Reagents | Prevent low-level background activation of TLR4 pathways, which skews baseline data and toxicity thresholds. | Cell culture media, PBS, and buffers from vendors with certified <0.01 EU/mL. |
| Cytokine Multiplex Panels | Simultaneous quantification of key storm mediators (IL-6, TNF-α, IL-1β, IFNs) from small serum volumes. | Luminex or MSD multi-array panels. |
| CLIA-Validated ALT/AST Assays | Accurate, reproducible quantification of hepatotoxicity markers in murine or human serum. | Pointe Scientific or Sigma colorimetric kits. |
| Viability/Proliferation Assays | Distinguish cytokine-mediated cell death from direct drug toxicity in hepatocyte screens. | CellTiter-Glo (ATP), Incucyte caspase-3/7 reagents. |
| Flow Cytometry Antibody Panels | Profile immune cell exhaustion (PD-1, LAG-3), activation, and suppressor populations (MDSCs) in tissues. | BioLegend or BD Biosciences optimized panels for mouse/human. |
| ATAC-seq Kit | Profile epigenetic immune reprogramming in sorted immune cells post-storm. | Illumina Tagmentase TDE1 or commercial library prep kits. |
| p-STAT ELISA/Kits | Assess functional impact of JAK/STAT inhibitors on target pathway in tissues. | Phospho-STAT3 (Tyr705) ELISA kits. |
Technical Support Center: Troubleshooting Guides & FAQs
This support center provides assistance for key experimental protocols related to controlling cytokine storm from PAMP overactivation research. The FAQs address common issues encountered when working with the most promising emerging drug candidates and platforms.
FAQ & Troubleshooting Section
Q1: In our in vitro PBMC assay, we are not observing the expected suppression of IL-6 and TNF-α after adding a novel STING pathway inhibitor. What could be the issue?
A: This is a common problem with STING-targeting therapies. Follow this troubleshooting guide:
- Verify PAMP Specificity: Ensure you are using the correct STING agonist (e.g., cGAMP, DMXAA) for your model. Human STING does not respond to DMXAA. Use cGAMP or other synthetic cyclic dinucleotides.
- Check Inhibitor Solubility & Stability: Many STING inhibitors are poorly soluble in aqueous buffers. Confirm the use of the correct vehicle (e.g., DMSO) and ensure the final DMSO concentration does not exceed 0.1% (v/v) to avoid cellular toxicity. Prepare fresh stocks.
- Optimize Timing: STING signaling is rapid. Pre-incubate cells with the inhibitor for at least 1 hour before adding the STING agonist. Simultaneous addition often fails.
- Positive Control: Include a known STING inhibitor (e.g., H-151, C-176) to validate your assay system.
Q2: Our data from the murine model of LPS-induced cytokine storm using an anti-IL-1β/IL-18 dual-release platform (e.g., a caspase-1 inhibitor) shows high animal-to-animal variability in serum cytokine levels. How can we improve consistency?
A: High variability in this model often stems from the LPS challenge.
- LPS Source and Preparation: Use LPS from a single, high-purity source (e.g., E. coli O111:B4). Prepare a master stock solution, aliquot it, and freeze at -20°C. Avoid repeated freeze-thaw cycles.
- Administration Route and Timing: Intraperitoneal (IP) injection is standard but requires precise technique. Ensure consistent injection volume and site. Time blood collection precisely (typically 90-120 minutes post-LPS for peak cytokines).
- Animal Husbandry: House mice in a quiet, temperature-controlled environment. Stress elevates baseline cytokines. Randomize animals from different cages into treatment groups.
Q3: When testing a JAK/STAT inhibitor in our macrophage priming and activation model, we see off-target cytotoxicity at concentrations near the reported IC50. How should we proceed?
A: JAK inhibitors can affect essential cellular signaling.
- Dose-Response Validation: Perform a full 8-point dose-response curve (e.g., 100 nM to 30 µM) alongside a parallel cell viability assay (e.g., MTT, ATP-based luminescence). Calculate a selectivity index (cytotoxic concentration 50% / IC50 for cytokine suppression).
- Check Phospho-STAT Specificity: Use phospho-flow cytometry or western blot to confirm the inhibitor is specifically blocking STAT1/STAT3/STAT5 phosphorylation in your cells, rather than inducing a general toxic response.
- Platform Alternative: If toxicity persists, consider investigational selective TYK2 inhibitors (e.g., deucravacitinib analogues) which may offer a better safety profile in this context by sparing other JAK isoforms.
Experimental Protocols for Cited Key Experiments
Protocol 1: In Vitro Evaluation of STING Antagonists in Human PBMCs Objective: To assess the efficacy of a STING inhibitor candidate in suppressing PAMP-induced cytokine production. Methodology:
- Isolate PBMCs from healthy donor blood using Ficoll density gradient centrifugation.
- Plate PBMCs at 1x10^6 cells/well in a 96-well plate in RPMI-1640 + 10% FBS.
- Pre-incubate cells with the STING inhibitor candidate (or vehicle control) for 1 hour at 37°C, 5% CO₂.
- Add the STING agonist cGAMP (2 µg/mL) to appropriate wells. Include wells for a reference inhibitor (H-151, 1 µM) and untreated controls.
- Incubate for 18 hours.
- Collect supernatant and quantify IL-6 and IFN-β using ELISA.
- Assay cell viability using an ATP-based luminescence assay on the same wells.
Protocol 2: In Vivo Efficacy of an NLRP3 Inflammasome Inhibitor in a Murine LPS Challenge Model Objective: To evaluate the ability of a drug candidate to suppress systemic cytokine storm in vivo. Methodology:
- Animal Groups: Randomize C57BL/6 mice (n=8-10 per group) into: Vehicle + PBS, Vehicle + LPS, Drug Candidate + LPS.
- Pre-treatment: Administer drug candidate or vehicle via IP injection 1 hour before LPS challenge.
- Challenge: Administer LPS (10 mg/kg) via IP injection.
- Sample Collection: At 90 minutes post-LPS, collect blood via retro-orbital bleed under anesthesia.
- Analysis: Allow blood to clot, centrifuge to isolate serum. Measure levels of IL-1β, IL-18, and IL-6 using a multiplex bead-based assay (Luminex) or individual ELISAs.
- Endpoint: Monitor survival for 72 hours if using a lethal dose model.
Table 1: Emerging Small Molecule & Biologic Candidates for Cytokine Storm Control
| Drug Candidate/Platform | Target/Mechanism | Phase (Latest) | Key Recent Data (2023-2024) | Potential Advantage |
|---|---|---|---|---|
| GSK’s NLRP3 Inhibitor (GSK484) | NLRP3 Inflammasome | Preclinical/Phase I | 92% reduction in IL-1β in human whole blood assay; efficacy in murine sepsis model. | Oral bioavailability, targets upstream of multiple cytokines. |
| STING Antagonist H-151 analogues | STING (cGAS-STING) | Lead Optimization | >80% inhibition of IFN-β in cGAMP-stimulated macrophages; structure-based design improving potency. | Addresses viral PAMP-driven storms (e.g., severe influenza, COVID-19). |
| Deucravacitinib (TYK2i) | TYK2 (JAK/STAT) | Approved (Psoriasis); Investigational for ARDS | Selective inhibition of IL-12, IL-23, Type I IFN signaling without broad JAK inhibition. | Favorable safety profile vs. pan-JAK inhibitors; reduced infection risk. |
| Anti-IL-1β/IL-18 Bispecific Antibody | IL-1β & IL-18 cytokines | Preclinical | In murine MAS model, superior survival vs. anti-IL-1β alone (100% vs 60%). | Dual neutralization targets key inflammasome cytokines. |
| Nanoparticle siRNA (Targeting ASC) | ASC (Apoptosis-associated speck-like protein) | Preclinical | Single dose reduced serum IL-18 by 75% for 72h in mouse model. | Long-lasting effect, precise targeting of inflammasome adaptor. |
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for PAMP/Cytokine Storm Research
| Item | Function | Example Product/Catalog # |
|---|---|---|
| Ultra-Pure LPS | Standardized PAMP (TLR4 agonist) to induce reproducible, MyD88/TRIF-dependent cytokine release. | InvivoGen, tlrl-3pelps (E. coli O111:B4) |
| cGAMP | STING pathway agonist for modeling cytosolic DNA sensing and Type I IFN-driven pathology. | InvivoGen, tlrl-nacga23 |
| Nigericin | Potassium ionophore used as a reliable, direct activator of the NLRP3 inflammasome in vitro. | Sigma-Aldrich, N7143 |
| Human/Mouse Cytokine Multiplex Assay | Simultaneous quantification of a panel of cytokines (IL-1β, IL-6, TNF-α, IL-18, IFN-γ) from small sample volumes. | Bio-Plex Pro Human Cytokine 8-plex Assay |
| Phospho-STAT3 (Tyr705) Antibody | Key reagent for assessing activation status of the JAK/STAT pathway via western blot or flow cytometry. | Cell Signaling Technology, #9145 |
| Caspase-1 FLICA Assay | Fluorochrome-labeled inhibitor probe to detect active caspase-1 in live cells by flow cytometry. | ImmunoChemistry Technologies, 98 |
| Cytokine Storm PBMC Kit | Cryopreserved, pooled human PBMCs pre-optimized for high cytokine release upon PAMP stimulation. | STEMCELL Technologies, 70025.1 |
Pathway & Workflow Visualizations
Conclusion
Controlling PAMP-driven cytokine storms requires a multi-layered strategy grounded in precise immunology. Foundational insights into PRR signaling reveal numerous intervention nodes, from direct PAMP interception to downstream cytokine blockade. Methodological advances offer diverse tools, yet optimization requires careful navigation of model limitations and dosing paradigms. Comparative validation underscores that no single strategy is universally effective, highlighting the potential of combination therapies and patient stratification via biomarkers. Future directions must focus on temporally precise interventions, personalized immunomodulation, and developing next-generation models that better capture human immune complexity to accelerate the translation of storm-controlling therapies from bench to bedside.