Cytokine Detection Sensitivity: A Comprehensive Comparison of Methods for Biomarker Research and Drug Development
Accurate cytokine quantification is crucial for understanding immune responses, disease mechanisms, and therapeutic efficacy in biomedical research and drug development.
Cytokine Detection Sensitivity: A Comprehensive Comparison of Methods for Biomarker Research and Drug Development
Abstract
Accurate cytokine quantification is crucial for understanding immune responses, disease mechanisms, and therapeutic efficacy in biomedical research and drug development. This article provides a systematic comparison of cytokine detection methods, evaluating sensitivity, dynamic range, and practical application across platforms including ELISA, ELISPOT, Luminex, MSD, and digital immunoassays like Simoa. It addresses foundational principles, methodological selection criteria, troubleshooting for pre-analytical variables, and validation strategies to ensure data reliability. Targeting researchers and drug development professionals, this review synthesizes current evidence to guide optimal technology selection for specific research scenarios, from basic discovery to clinical trials, while highlighting emerging trends in ultra-sensitive multiplex cytokine profiling.
Why Sensitivity Matters: The Critical Role of Cytokine Detection in Biomedical Research
Cytokines are small, secreted proteins that orchestrate immune responses through complex cell-cell communication networks. Their precise detection and quantification are fundamental to understanding immune function in health and disease, from autoimmune disorders like rheumatoid arthritis to cancer and infectious diseases [1] [2] [3]. The accurate measurement of cytokine signaling activity provides critical insights into disease mechanisms, patient stratification, and therapeutic monitoring, making the choice of detection methodology a pivotal decision for researchers and clinicians [1] [4].
This guide provides an objective comparison of major cytokine detection technologies, focusing on their sensitivity, multiplexing capability, and practical applications. We present experimental data and detailed protocols to help researchers select the most appropriate method for their specific needs, framed within the broader context of sensitivity comparison in cytokine detection research.
Comparative Analysis of Cytokine Detection Methods
The evolution from single-plex to multiplex technologies represents a paradigm shift in cytokine detection, enabling researchers to capture the complex, interconnected nature of cytokine networks from limited sample volumes.
Table 1: Performance Comparison of Major Cytokine Detection Technologies
| Method | Sensitivity Range | Multiplex Capacity | Sample Volume | Throughput | Key Applications |
|---|---|---|---|---|---|
| Traditional ELISA | pg/mL (~0.5 pM) [5] | Single-plex [5] | 50-100 μL [5] | Low (4+ hours) [1] | Targeted cytokine analysis, validation studies |
| Multiplex Bead Arrays (FlowCytomix) | ~1.2-43.3 pg/mL [1] | 13+ plex [1] | 25-50 μL [1] | Medium-high | Comprehensive cytokine profiling, clinical studies |
| AI-Enhanced POC Biosensors | 0.01-100 pg/mL [4] | 10+ plex [4] | 1-50 μL [4] | Very high (5-30 min) [4] | Rapid diagnostics, therapeutic monitoring |
| Transcriptomic Analysis (CytoSig) | N/A (indirect activity) [3] | 40+ cytokines [3] | Varies | Computational | Signaling activity inference, pathway analysis |
Table 2: Practical Considerations for Method Selection
| Parameter | ELISA | Multiplex Bead Arrays | Transcriptomic Approaches |
|---|---|---|---|
| Equipment Requirements | Standard plate reader [5] | Flow cytometer [1] | Sequencing infrastructure, computational resources [3] |
| Cost per Data Point | High for multiple targets [1] | Moderate for multiplexed data [1] | High initial, decreasing with scale |
| Technical Expertise | Moderate laboratory skills [5] | Flow cytometry expertise [1] | Bioinformatics expertise [6] [3] |
| Sample Type Compatibility | Serum, plasma, supernatant [5] [1] | Serum, plasma, supernatant [1] | Tissue, single cells [2] [3] |
| Standardization | Well-established protocols [5] | Kit-based, platform-dependent [1] | Evolving standards, method-dependent [6] |
Experimental Protocols and Methodologies
Indirect Sandwich ELISA Protocol
The indirect sandwich ELISA remains a gold standard for sensitive, specific quantification of individual cytokines, with a typical sensitivity of pg/mL or approximately 0.5 pM for a 15 kDa protein [5].
Day 1: Plate Coating
- Dilute capture antibody in PBS to optimal concentration determined by checkerboard titration.
- Coat 96-well high-binding microplate with 50 μL/well of diluted capture antibody.
- Tap plate gently to ensure complete coverage of well bottom.
- Incubate plate overnight at 4°C [5].
Day 2: Assay Procedure
- Wash coated plate with automatic plate washer (5 washes, 250 μL/wash, 15-second soaks).
- Add 150 μL/well blocking buffer (e.g., 2% BSA in PBS) and incubate 1 hour at ambient temperature on orbital shaker.
- Prepare cytokine standards in dilution buffer (e.g., PBS with 0.005% Tween-20 and 2% FCS) across appropriate concentration range.
- After blocking, wash plate and add 50 μL/well of standards or samples. Incubate 2 hours.
- Prepare biotinylated detection antibody in dilution buffer.
- Wash plate and add 50 μL/well of detection antibody. Incubate 2 hours.
- Prepare streptavidin-conjugated HRP (typically 1:20,000 in PBS with 0.1% BSA and 0.005% Tween-20).
- Wash plate and add 50 μL/well of SA-HRP. Incubate 30 minutes.
- Wash plate and add 100 μL/well TMB substrate. Incubate in dark without shaking for 20-30 minutes.
- Stop reaction with 1.5 N sulfuric acid and measure optical density at 450-590 nm [5].
Multiplex Bead-Based Assay Protocol
Bead-based multiplex assays like FlowCytomix enable simultaneous quantification of multiple cytokines from limited sample volumes, significantly enhancing efficiency for comprehensive immune profiling.
Sample Preparation
- Collect serum samples by centrifuging blood at 800×g for 10 minutes. Aliquot and store at -80°C.
- For PBMC supernatants: isolate PBMCs using Ficoll-Hypaque density gradient centrifugation.
- Culture PBMCs at 2×10^6 cells/mL in complete medium with or without stimulation (e.g., 5 μg/mL PHA).
- Incubate cells 24 hours at 37°C, collect supernatant, and store at -80°C until assay [1].
Assay Procedure
- Bring all reagents and samples to room temperature.
- Prepare standards by serial dilution of recombinant cytokine standards.
- Add 25 μL of standards or samples to appropriate wells.
- Add 25 μL of mixed bead suspension to each well.
- Incubate plate for 2 hours in dark on orbital shaker.
- Wash plate twice with wash buffer.
- Add 25 μL of detection antibody mixture to each well.
- Incubate for 1 hour in dark on orbital shaker.
- Wash plate twice and add 25 μL of streptavidin-PE to each well.
- Incubate for 30 minutes in dark on orbital shaker.
- Wash plate twice and resuspend beads in wash buffer.
- Analyze on flow cytometer using instrument-specific software [1].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagent Solutions for Cytokine Detection
| Reagent/Category | Function/Purpose | Examples/Specifications |
|---|---|---|
| Matched Antibody Pairs | Capture and detect specific cytokines with high specificity | Monoclonal capture with biotinylated detection antibody [5] |
| Cytokine Standards | Quantification through standard curve generation | Recombinant proteins in known concentrations [5] |
| Blocking Buffers | Prevent non-specific binding to assay surfaces | 2% BSA in PBS, Blotto, Casein, SuperBlock [5] |
| Detection Amplification | Signal enhancement for improved sensitivity | Streptavidin-conjugated HRP or infrared dyes [5] |
| Multiplex Bead Kits | Simultaneous detection of multiple analytes | FlowCytomix, LEGENDplex with distinct bead populations [1] [7] |
| Plerixafor | Plerixafor (AMD3100) | |
| Pluripotin | Pluripotin, CAS:839707-37-8, MF:C27H25F3N8O2, MW:550.5 g/mol | Chemical Reagent |
Advanced Technologies and Future Directions
Transcriptomic Approaches to Cytokine Activity
Beyond direct protein detection, transcriptomic approaches like CytoSig and the Immune Dictionary model cytokine signaling activity by analyzing downstream gene expression patterns, providing insights into functional signaling networks rather than mere protein presence [2] [3].
The CytoSig platform utilizes a database of 20,591 transcriptome profiles of human cytokine responses to predict cytokine signaling activities from bulk or single-cell transcriptomic data. This approach captures the functional consequences of cytokine signaling by identifying regulated target genes, addressing limitations of direct protein measurement where cytokine release can be transient compared to longer-lasting transcriptional responses [3].
Single-Cell Resolution and Computational Methods
Recent advances enable cytokine activity estimation at single-cell resolution using methods like MouSSE (Mouse-Specific Single cell cytokine activity prediction and Estimation), which leverages the Immune Dictionary containing single-cell transcriptomic profiles of over 17 immune cell types responding to 86 cytokines [2] [6].
MouSSE uses a gene set scoring approach with a modification of the Variance-adjusted Mahalanobis method to estimate cell-level activity of 86 distinct cytokines from scRNA-seq data, addressing the challenges of sparsity and technical noise in single-cell data while accounting for the pleiotropic and redundant nature of cytokine functions [6].
Emerging Trends: AI and Point-of-Care Biosensing
The cytokine detection landscape is rapidly evolving with the integration of artificial intelligence and point-of-care biosensing technologies. AI-enabled multiplex POC platforms now achieve limits of detection as low as 0.01-100 pg/mL using just 1-50 μL of sample and delivering results within 5-30 minutes [4].
These systems leverage machine learning algorithms, including convolutional neural networks and decision-tree models, for autonomous signal processing and decision support. This convergence of multiplexed biosensing with AI enhances analytical performance, interpretability, and clinical utility for real-time immune monitoring in precision medicine applications [4].
The optimal cytokine detection method depends on specific research requirements. Traditional ELISA provides reliable, sensitive quantification of individual cytokines with well-established protocols. Multiplex bead arrays offer superior efficiency for comprehensive cytokine profiling from limited samples. Transcriptomic approaches infer functional signaling activity beyond protein detection, while emerging AI-enhanced biosensors enable rapid, decentralized cytokine monitoring.
Understanding the comparative strengths, limitations, and experimental requirements of each platform empowers researchers to select the most appropriate technology for their specific applications, from basic immune research to clinical diagnostics and therapeutic development. As cytokine detection continues evolving toward higher multiplexing capacity, single-cell resolution, and computational integration, researchers will gain increasingly powerful tools to decipher the complex language of immune communication in health and disease.
The accurate measurement of low-abundance cytokines in complex biological matrices represents a significant challenge in biomedical research and clinical diagnostics. These signaling proteins, crucial for understanding immune responses, often exist at ultra-low concentrations—in the picogram (pg) to femtogram (fg) per milliliter range—within serum, plasma, and other biological fluids [8]. Their detection is further complicated by matrix effects, the presence of binding proteins, and the dynamic nature of cytokine secretion [9] [10]. This comparison guide objectively evaluates the performance of current cytokine detection technologies, focusing on their sensitivity, dynamic range, and suitability for complex matrices to inform researchers and drug development professionals in selecting the optimal platform for their specific applications.
Key Cytokine Detection Technologies and Their Operational Principles
Understanding the fundamental working principles of various cytokine detection platforms is essential for appreciating their performance characteristics and limitations. The technologies can be broadly categorized into traditional immunoassays, multiplexed arrays, and emerging next-generation platforms.
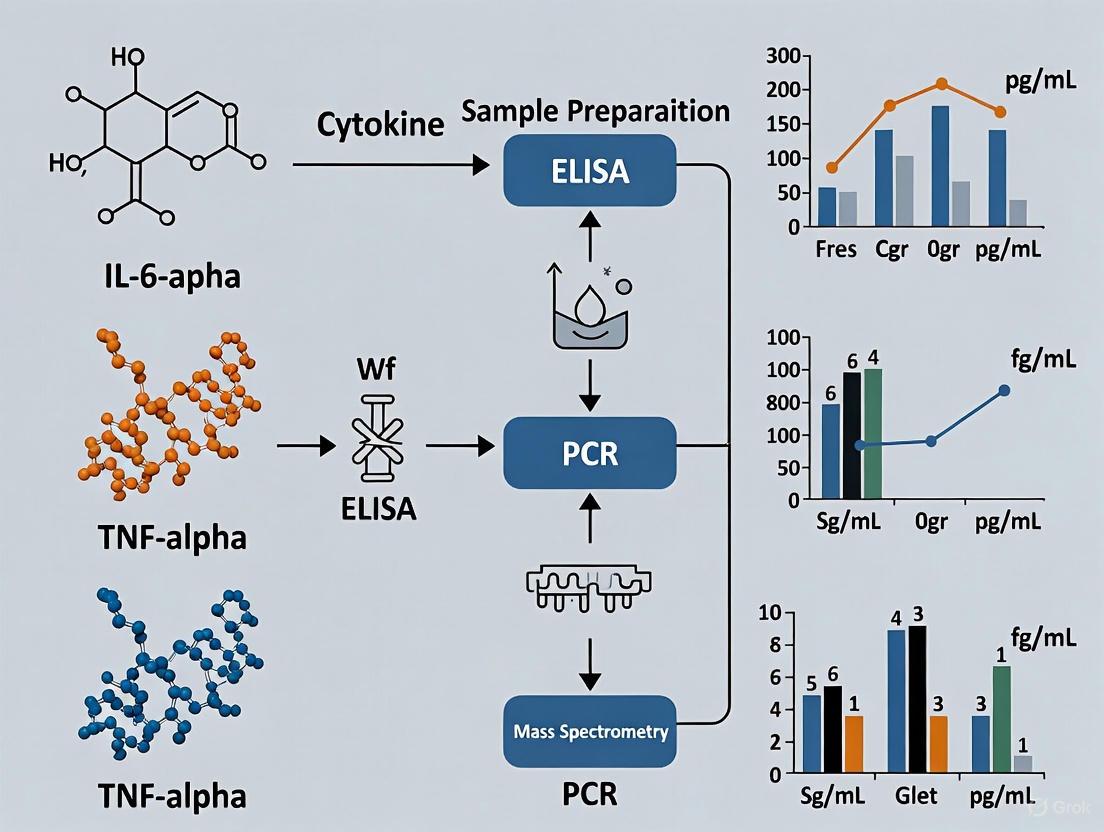
Technology Workflows and Signaling Mechanisms
The following diagram illustrates the core operational workflows and detection signaling mechanisms for the primary classes of cytokine detection technologies discussed in this guide.
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful cytokine detection requires carefully selected reagents and materials. The following table details key components essential for conducting these sensitive measurements.
Table: Essential Research Reagents for Cytokine Detection
| Reagent/Material | Function & Importance | Application Notes |
|---|---|---|
| Matched Antibody Pairs | Pairs of capture and detection antibodies specific to the target cytokine; form the core of sandwich immunoassays [8]. | Critical for assay specificity; validated pairs minimize cross-reactivity. |
| Ultra-Sensitive Detection Chemistry | Enzymes (e.g., HRP), fluorophores (e.g., PE), or luciferase systems that generate the measurable signal [8] [11]. | Signal amplification is key for detecting low-abundance targets. |
| Matrix-Matched Standards & Controls | Cytokine standards diluted in a solution that mimics the sample matrix (e.g., serum, plasma) [10]. | Accounts for matrix effects, enabling accurate quantification in biological samples. |
| Blocking Buffers | Protein-based solutions (e.g., BSA) used to coat unused binding sites on plates or beads [12]. | Reduces non-specific binding, a major source of background noise. |
| Solid-Phase Supports | Microplates, magnetic beads, or sensor chips that serve as the solid support for the immunoassay [8] [13]. | Beads enable multiplexing; specialized sensor chips are used for label-free platforms. |
| Sample Dilution Buffers | Buffers designed to dilute complex samples while preserving cytokine integrity and minimizing interference [10]. | Specific buffers can help overcome matrix inhibition effects. |
| PluriSIn 1 | N'-phenylisonicotinohydrazide|RUO|Research Compound | N'-phenylisonicotinohydrazide is a chemical reagent for research use only (RUO). Explore its applications in antimicrobial and medicinal chemistry studies. |
| PMX-53 | PMX-53, MF:C47H65N11O7, MW:896.1 g/mol | Chemical Reagent |
Comparative Performance Analysis of Leading Platforms
A critical comparison of sensitivity, dynamic range, and throughput reveals significant differences between platforms, directly impacting their suitability for detecting low-abundance cytokines.
Quantitative Performance Metrics
The following table summarizes key performance data for various cytokine detection technologies, as reported in the literature.
Table: Sensitivity and Dynamic Range Comparison of Cytokine Detection Platforms
| Technology/Platform | Reported Sensitivity (LOD/LLOQ) | Dynamic Range | Sample Volume | Multiplexing Capability |
|---|---|---|---|---|
| Simoa (HD-X) | Single-digit fg/mL for IL-17A [8] | >4 logs [8] | 50 µL [8] | Single-plex and multiplex (e.g., 4-plex) [8] |
| MSD (Electrochemiluminescence) | Best sensitivity in low detection limit [13] | Broadest dynamic range [13] | Not specified | Up to 10-plex [14] [15] |
| Luminex (Bead-Based) | Variable; some cytokines clearly detected, others not (e.g., IL-1β) [14] | Broad [13] | 35-50 µL [14] | High (e.g., 13-plex to 51-plex) [14] [10] |
| LSPRi (Peptide Aptamer) | 4.6 pg/mL for IL-6 [9] | ~6 orders of magnitude [9] | 3 µL [9] | Typically low (developing) |
| Electrochemical Immunosensor | 9.8 pg/mL for OSM in serum [12] | 20 - 140 pg/mL (linear range) [12] | Not specified | Typically low |
| Lumit Immunoassay | <10 pg/mL (MDD) [11] | >3 logs [11] | Suited for 384-well | Medium (developing) |
Analysis of Platform Strengths and Limitations
Ultra-Sensitive Digital ELISA (Simoa): This platform demonstrates superior sensitivity, outperforming conventional methods by orders of magnitude. Its key innovation is the isolation of immunocomplexes on beads in femtoliter wells, enabling digital counting of single molecules. This allows for precise quantification of cytokines like IL-17A in the single-digit fg/mL range, making it ideal for detecting ultra-low abundance targets in clinical samples [8]. A validation study demonstrated intra- and inter-assay coefficients of variation (CVs) under 10%, confirming high precision in complex matrices like serum [8].
Electrochemiluminescence (Meso Scale Discovery - MSD): MSD consistently ranks high in comparative studies for sensitivity and broad dynamic range [13]. Its electrode-integrated plates allow for efficient capture and low-background signal detection. However, a multisite comparison highlighted that absolute cytokine concentrations can vary significantly between laboratories and kit lots, suggesting caution for long-term multi-site studies [14].
Bead-Based Multiplex (Luminex): The primary advantage of Luminex is high-throughput multiplexing, allowing for the simultaneous measurement of dozens of cytokines from a single small-volume sample [14] [15]. However, its sensitivity for specific low-abundance cytokines can be inconsistent. For instance, in a multisite evaluation, IL-1β was only clearly detected with one of several tested kits, and significant inter-laboratory variability was observed [14]. This platform may be best for studies where relative changes, rather than absolute concentrations, are the focus [14].
Emerging and Niche Platforms:
- LSPR with Peptide Aptamers: This label-free approach uses engineered peptide aptamers, which are smaller than antibodies, on a nanoplasmonic sensor surface. This design enhances the mass ratio of the captured analyte to the probe, achieving a record-breaking LOD of 4.6 pg/mL for IL-6 and a wide dynamic range. It shows promise for rapid, small-volume testing [9].
- Electrochemical Immunosensors: These sensors translate antibody-antigen binding directly into an electrical signal. A label-free sensor for Oncostatin M (OSM) demonstrated a LOD of 9.8 pg/mL in human serum, with high specificity against interfering biomarkers. Its advantages include potential for miniaturization and point-of-care use [12].
- Lumit Bioluminescent Immunoassays: This homogeneous, no-wash assay uses NanoLuc Binary Technology (NanoBiT). Antibodies labeled with SmBiT and LgBiT subunits reassemble into a functional luciferase upon binding the target cytokine, producing a luminescent signal. It is optimized for high-throughput screening in 384-well formats, with a minimal detectable dose (MDD) under 10 pg/mL and a broad linear range, offering a compelling solution for automated, high-throughput workflows [11].
The Critical Impact of Biological Matrices
The choice of biological matrix (e.g., serum vs. plasma) profoundly impacts assay performance and must be considered during experimental design.
Matrix Inhibition and Interference: Both serum and plasma inhibit the detection of many cytokines, with serum typically causing greater inhibition than plasma [10]. This matrix effect is attributed to non-specific binding, the presence of soluble cytokine receptors, and other interfering proteins. The extent of inhibition varies by cytokine and between individual donors [10].
Serum vs. Plasma Comparison: While cytokine levels in matched serum and plasma samples are generally correlated, several key differences exist:
- Higher Background in Serum: Non-specific background signals are significantly increased in serum compared to plasma [10].
- Sensitivity for Low-Abundance Cytokines: For certain low-abundance cytokines, plasma may be a more sensitive matrix because its lower background allows for better detection of subtle, disease-related changes [10].
- Impact of Dilution: Diluting samples can help overcome matrix inhibition, but the dilution is not linear for all cytokines. Therefore, comparisons must be made between samples diluted to the same degree [10].
Detailed Experimental Protocols
To ensure reproducibility, detailed methodologies from key cited studies are provided below.
- Objective: To validate an ultra-sensitive IL-17A assay on the Simoa HD-X platform for clinical and CRO use.
- Sample Preparation: Serum samples were used. The protocol emphasizes rigorous validation in complex biological matrices.
- Assay Procedure:
- Capture: Cytokines are captured by antibodies conjugated to paramagnetic beads.
- Detection: Binding of an enzyme-labeled detection antibody (β-galactosidase) forms an immunocomplex.
- Wash and Seclusion: Beads are washed and resuspended in a substrate solution, then loaded into a single-well array disk where each bead is sealed in a femtoliter-sized well.
- Signal Generation and Imaging: The substrate is hydrolyzed, generating a fluorescent product. The presence or absence of a single enzyme molecule per well is counted digitally.
- Validation Parameters: The study measured:
- Dynamic Range & LOD: Achieved single-digit fg/mL sensitivity.
- Precision: Intra- and inter-assay CVs were under 10%.
- Matrix Effects: Specifically evaluated in serum.
- Recovery: Assessed via spike-and-recovery and dilution linearity tests.
- Objective: Simultaneously quantify multiple cytokines in serum or plasma.
- Sample Preparation: Serum (clotted) or plasma (anti-coagulated) is centrifuged and aliquoted to avoid repeated freeze-thaw cycles.
- Assay Procedure (as performed in multisite comparison):
- Incubation: A 50 μL sample is mixed with antibody-linked polystyrene or magnetic beads in a 96-well filter plate and incubated for 2 hours at room temperature, followed by an overnight incubation at 4°C with shaking.
- Washing: Plates are vacuum-filtered and washed twice with wash buffer.
- Detection: Beads are incubated with a biotinylated detection antibody for 2 hours.
- Signal Amplification: After washing, beads are incubated with streptavidin-phycoerythrin (SA-PE) for 30-40 minutes.
- Washing and Reading: A final wash is performed, and beads are resuspended in reading buffer. The plate is read on a Luminex instrument, which uses lasers to identify the bead set (and thus the cytokine) and quantify the PE signal.
- Data Analysis: A 5-parameter logistic (5PL) curve with 1/Y² weighting is often used to fit the standard curve, giving better quantitation at the low end.
The challenge of measuring low-abundance cytokines in complex matrices is met with a diverse and evolving technological landscape. The choice of platform involves a careful trade-off between ultimate sensitivity, multiplexing capability, throughput, and cost. Digital ELISA platforms like Simoa currently offer the highest sensitivity, which is critical for detecting ultra-low level cytokines in clinical serum samples. Multiplexed bead-based assays like Luminex provide an unparalleled broad profile of the immune response from a small sample volume, though with potentially variable sensitivity for some analytes. Emerging technologies, including label-free LSPR and electrochemical sensors, promise rapid, minimal-volume testing with point-of-care potential. Ultimately, the selection of a method must be guided by the specific research question, the required sensitivity, the number of analytes, the available sample volume, and the experimental budget. Researchers must also carefully standardize sample collection and matrix choice, preferably using plasma for low-abundance targets, to ensure reliable and interpretable data.
Cytokines are secreted proteins that play critical roles in cell signaling within immune responses, functioning as key mediators in processes ranging from pathogen defense to inflammation regulation [16]. Their concentrations in biological fluids provide valuable information about in vivo immune status, making accurate detection essential for biological studies, disease diagnosis, and drug development [13]. The evolution from traditional bioassays to modern immunoassays represents a significant advancement in the field, with current technologies offering dramatically improved sensitivity, specificity, and multiplexing capabilities. Dysregulation of cytokines is implicated in a diverse array of pathophysiological conditions, including autoimmune disorders, cancer, infectious diseases like COVID-19, and neurological conditions, underscoring the clinical relevance of precise cytokine measurement [17] [18] [16].
The fundamental principle underlying most cytokine detection methods involves the specific binding of antibodies to target cytokine molecules, but the technologies diverge significantly in their detection mechanisms, sensitivity ranges, and practical applications. This guide provides an objective comparison of current cytokine detection platforms, presenting experimental data on their performance characteristics to assist researchers, scientists, and drug development professionals in selecting appropriate methodologies for their specific applications. As the field continues to advance, understanding the strengths and limitations of each technology becomes increasingly important for generating reliable, reproducible data in both basic research and clinical contexts.
Comparative Analysis of Major Cytokine Detection Platforms
Table 1: Comprehensive Comparison of Cytokine Detection Platforms
| Technology | Detection Mechanism | Sensitivity (Lower Detection Limit) | Dynamic Range | Multiplexing Capability | Key Advantages | Key Limitations |
|---|---|---|---|---|---|---|
| MSD (Meso Scale Discovery) | Electrochemiluminescence | Best sensitivity in low detection limit [13] | Broadest dynamic range [13] | High | Superior sensitivity, broad dynamic range [13] | Higher cost, specialized equipment required |
| CBA (Cytometric Bead Array) | Flow cytometry with bead-based capture | Superior performance [13] | Superior performance [13] | High | Suitable for high-throughput screening with multiplexing [13] | Requires flow cytometry expertise and equipment |
| Luminex | Fluorescent bead-based (xMAP) | Good performance [13] [14] | Good performance [13] | High | Well-established, widely available | Variable performance between kits and laboratories [14] |
| Simoa (Single Molecule Array) | Digital ELISA | Highest sensitivity for sub-pg/mL detection [19] [18] | Wide | Low to moderate | Exceptional sensitivity, detects endogenous cytokines [19] [18] | Limited multiplexing, higher cost per analyte |
| Olink | Proximity Extension Assay (PEA) | High detectability [17] | Moderate | High | High specificity, good correlation with other sensitive methods [17] | Requires specialized equipment and DNA-tagged antibodies |
| Alamar NULISAseq | Proximity Ligation Assay (PLA) | Highest overall detectability [17] | Moderate to Wide | High (200-plex) | Exceptional detectability, broad panel [17] | Complex workflow, newer platform with less established track record |
| ELLA | Microfluidic immunoassay | Good sensitivity for TNF and IFNγ [20] | 4-5 log10 dynamic range [20] | Moderate | Rapid, automated, minimal user intervention [20] | Limited single-cell resolution, lower multiplexing capacity |
| ELISpot | Enzyme-linked immunospot | Cell-level detection [20] | 2 log10 dynamic range [20] | Low to moderate | Single-cell resolution, detects cytokine-secreting cells [20] | Variable results between laboratories, lower dynamic range [20] |
| Traditional ELISA | Enzyme-linked immunosorbent assay | Moderate | Moderate | Low (typically single-plex) | Well-established, widely available | Lower throughput, limited multiplexing capability [13] |
Experimental Validation and Cross-Platform Comparisons
Independent studies have consistently demonstrated significant variability in performance across different cytokine detection platforms. A comprehensive evaluation of nine technology platforms for quantitative measurements of cytokines at sub-pg/mL levels in human serum revealed that the Simoa and Erenna platforms showed the highest frequency of endogenous analyte detection (FEAD), followed by Milliplex and Imperacer platforms [19]. However, only Simoa and Erenna results showed high correlation across all evaluated cytokine assays, while other platforms exhibited poor correlation with each other, highlighting the critical importance of platform selection for biomarker quantification [19].
A separate cross-platform comparison focusing on Luminex, Olink, and Alamar NULISAseq demonstrated that detectability differences across platforms often translated to differences in differential expression findings [17]. The study revealed that the Alamar platform showed the highest overall detectability, followed by Olink and then Luminex. Furthermore, correlation of protein measurements between the Alamar and Olink platforms tended to be stronger than the correlation of either platform with Luminex [17]. These findings emphasize that the choice of immunoassay technology can substantially impact research findings and clinical interpretations.
Table 2: Cross-Platform Performance Assessment from Independent Studies
| Study Focus | Platforms Compared | Key Findings | Reference |
|---|---|---|---|
| Sensitivity for Inflammation Biomarkers | Simoa, MSD, Luminex (multiple vendors), Quantikine ELISA | Simoa demonstrated highest sensitivity in detecting endogenous analytes across all cytokines and clinical populations; MSD and R&D Luminex showed variable performance; Myriad Luminex exhibited low FEAD | [18] |
| Multisite Reproducibility | Bio-Rad Luminex, BioSource Luminex, Linco Luminex, MSD | Significant differences between laboratories and/or lots with all kits; no single multiplex panel detected all cytokines reliably; kits detected similar patterns of cytokine perturbation during primary HIV viremia | [14] |
| COVID-19 Cohort Analysis | Luminex, Olink, Alamar NULISAseq | Alamar showed highest detectability; correlation stronger between Alamar and Olink than with Luminex; detectability differences affected differential expression findings | [17] |
| Functional Immune Phenotyping | ELLA, ELISpot | ELLA provided more precise measurement with 4-5 log10 dynamic range vs. ELISpot's 2 log10 range; ELLA correctly identified stimulants in 90% of samples vs. 72% for ELISpot | [20] |
| Sub-pg/mL Detection | Simoa, Erenna, Milliplex, V-plex, Ella, AMMP, Imperacer | Simoa and Erenna showed highest sensitivity and correlation; V-plex and Ella showed acceptable parallelism; Milliplex, AMMP, and Imperacer showed poor correlation with other platforms | [19] |
Experimental Protocols for Cytokine Detection
Standardized Procedures Across Platforms
Luminex Assay Protocol: The Luminex methodology employs fluorescent bead-based technology where capture antibodies are coated on color-coded microbeads. The standard protocol involves: (1) Incubation of 35-50μL of sample with antibody-coated beads for 2 hours; (2) Washing steps to remove unbound material; (3) Addition of biotinylated detection antibody and incubation for 1 hour; (4) Addition of streptavidin-phycoerythrin reporter; (5) Analysis on Luminex instrumentation which identifies each bead by its fluorescent signature and quantifies the bound cytokine via the PE signal [17] [14]. Sensitivity can be enhanced through optimized washing procedures and non-specific binding correction using control beads like the Assay Chex system [17].
Olink PEA Protocol: The Olink proximity extension assay utilizes DNA-tagged antibodies in a highly specific workflow: (1) Incubation of sample with pairs of oligonucleotide-labeled antibodies to each protein for 16 hours at 4°C; (2) Proximity extension where bound antibody pairs generate a double-strand oligonucleotide PCR target; (3) Microfluidic qPCR using a Dynamic Array Integrated Fluidic Circuit (IFC) chip pre-loaded with protein-specific primers; (4) Quantification using real-time PCR analysis via ΔΔCt method with results reported in Normalized Protein Expression (NPX) units, where one NPX unit difference represents a doubling of protein concentration [17].
MSD Electrochemiluminescence Protocol: Meso Scale Discovery's platform employs: (1) Coating of carbon electrode-containing plates with capture antibodies; (2) Sample incubation followed by washing; (3) Addition of detection antibodies labeled with SULFO-TAG ruthenium derivatives; (4) Application of voltage to induce electrochemiluminescence emission; (5) Light signal quantification which correlates to analyte concentration. This technology demonstrates particular strength in detecting low-abundance cytokines without interference from sample matrix components [13] [18].
Sample Preparation and Handling Considerations
Proper sample handling is critical for reliable cytokine measurements across all platforms. Standard protocols recommend: (1) Processing serum or plasma within 6 hours of collection; (2) Immediate freezing at -80°C without repeated freeze-thaw cycles; (3) Centrifugation of samples after thawing to remove precipitates or debris; (4) Adherence to recommended sample dilution factors specific to each technology [17] [14]. The number of freeze-thaw cycles significantly impacts cytokine stability, with most protocols recommending minimal freeze-thaw cycles (optimally one cycle or fewer) to prevent analyte degradation [17].
For specialized applications like single-cell cytokine activity estimation from transcriptomic data, computational methods like MouSSE (Mouse-Specific Single cell transcriptomics level cytokine activity prediction and Estimation) have been developed. This approach uses gene set scoring of cytokine-specific signatures constructed from perturbation data, employing a modification of the Variance-adjusted Mahalanobis (VAM) method to account for technical noise and sparsity in single-cell RNA-sequencing data [16].
Visualizing Cytokine Detection Workflows
Cytokine Detection Technology Workflow
Cytokine Detection Sensitivity Spectrum
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for Cytokine Detection
| Reagent/Material | Function | Example Applications | Technical Considerations |
|---|---|---|---|
| Capture Antibodies | Bind specific cytokines in solution | All immunoassay platforms; coated on plates, beads, or DNA-tagged | Specificity validation critical; lot-to-lot variability affects results [14] |
| Detection Antibodies | Generate measurable signal upon binding | Typically biotinylated or fluorophore-conjugated; DNA-tagged for PEA/PLA | Epitope should differ from capture antibody; cross-reactivity must be minimized |
| Fluorescent Beads | Solid phase for multiplexed capture | Luminex, CBA platforms; spectrally distinct bead sets | Bead stability and uniform coating essential for reproducibility [21] |
| Electrochemiluminescence Labels | Signal generation in applied electric field | MSD platform; SULFO-TAG labels | Enables broad dynamic range with minimal background [13] [18] |
| DNA Reporters | Proximal binding generates amplifiable signal | Olink, NULISAseq platforms; enables PCR quantification | High specificity through dual recognition requirement [17] |
| Reference Standards | Quantification and standard curve generation | All quantitative platforms; recombinant cytokines | Lack of universal reference standards contributes to platform variability [19] [14] |
| Matrix Buffers | Mimic sample environment for standards | Diluent for standards; sample preservation | Proper matrix matching essential for accurate quantification [14] |
| Quality Controls | Monitor assay performance and reproducibility | Inter-plate controls, process monitoring | Essential for identifying lot and laboratory variability [14] |
| Nimustine Hydrochloride | Nimustine Hydrochloride, CAS:55661-38-6, MF:C9H14Cl2N6O2, MW:309.15 g/mol | Chemical Reagent | Bench Chemicals |
| Nintedanib esylate | Nintedanib esylate, MF:C33H39N5O7S, MW:649.8 g/mol | Chemical Reagent | Bench Chemicals |
The landscape of cytokine detection technologies has evolved significantly from traditional bioassays to sophisticated immunoassays capable of detecting sub-picogram concentrations of multiple cytokines simultaneously. Based on comprehensive cross-platform comparisons, MSD demonstrates superior sensitivity and dynamic range, while CBA and Luminex offer robust performance for high-throughput screening with multiplexing capability [13]. For applications requiring exceptional sensitivity to detect low-abundance cytokines, Simoa and Alamar NULISAseq platforms show the highest detectability [17] [19] [18].
The integration of cytokine detection with advanced computational methods represents an emerging frontier in the field. Machine learning approaches applied to cytokine profiling data have demonstrated remarkable capability in classifying patient disease status, with one study achieving 95.6% sensitivity and 98.1% specificity for COVID-19 status prediction using combined clinical data and cytokine profiles [22]. Similarly, computational methods like MouSSE enable cytokine activity estimation from single-cell RNA-sequencing data, expanding the analytical framework beyond protein detection to transcriptomic-level activity inference [16].
As the field advances, key considerations for technology selection include required sensitivity, multiplexing needs, sample volume constraints, available instrumentation, and project budget. Researchers should be aware that significant variability exists between platforms and even between lots from the same manufacturer, underscoring the importance of rigorous validation and implementation of appropriate controls [14]. The ongoing development of standardized reference materials and improved assay reproducibility will further enhance the utility of cytokine detection across both basic research and clinical applications.
Impact of Accurate Quantification on Disease Diagnosis and Therapeutic Monitoring
The accurate quantification of cytokines has emerged as a cornerstone of precision medicine, providing indispensable insights into disease mechanisms, diagnostic stratification, and therapeutic monitoring. These small, soluble proteins function as crucial immunoregulators that form the communication network for the immune system, offering valuable mechanistic data for numerous inflammatory and immune disease states [23]. The profiling of multiple cytokines represents a more robust approach to predicting disease progression than single-cytokine measurements, as patterns of biomolecules provide a more comprehensive depiction of disease than individual biomarkers [21] [24]. This comparative guide examines the performance characteristics of major cytokine detection technologies, providing researchers and drug development professionals with experimental data and methodologies to inform their analytical strategies. As the focus of biomarker studies shifts toward deciphering complex biomolecular patterns, the validation of multiplexing technologies for reproducibility and precision becomes increasingly crucial for accurate protein identification and clinical implementation [24].
Technical Comparison of Major Cytokine Detection Platforms
The selection of an appropriate cytokine detection method fundamentally shapes the reliability, depth, and interpretation of research outcomes. Each major technology offers distinct advantages and limitations that must be aligned with specific research objectives.
Table 1: Performance Characteristics of Major Cytokine Detection Methods
| Method | Sensitivity | Multiplexing Capacity | Dynamic Range | Sample Volume | Throughput | Best Applications |
|---|---|---|---|---|---|---|
| ELISA | Low pg/mL range [25] | Single-plex [25] | 2-3 logs [25] | 100-200 μL [25] | Moderate [25] | Validating specific cytokines; studies with limited budget [25] |
| Flow Cytometry | Similar to ELISA [23] | 12-plex+ [21] | Similar to ELISA [23] | 50-100 μL [21] | Moderate to High [21] | Immune profiling; clinical research [21] [23] |
| Luminex xMAP | Low pg/mL to fg/mL [25] | Up to 500-plex [25] | 3-5 logs [25] | 25-50 μL [25] | High [25] | Biomarker discovery; large cohort studies [25] |
| MSD-ECL | High (ECL advantage) [25] | High-plex available [25] | 3-5 logs [25] | 25-50 μL [25] | High [25] | Sensitivity-critical applications [25] |
Enzyme-Linked Immunosorbent Assay (ELISA)
As one of the most widely used techniques, ELISA offers simplicity, well-established protocols, and high specificity through its sandwich assay format where a capture antibody binds the cytokine and a detection antibody produces a measurable signal [5]. The four basic steps include: (1) capturing analyte with immobilized antibody; (2) detecting captured analyte with biotinylated detection antibody; (3) amplification with enzyme-conjugated streptavidin; and (4) substrate addition and optical density measurement [5]. While ELISA provides good sensitivity for many cytokines, it is generally less sensitive than newer technologies and has limited multiplexing capability, making it most suitable for studies focusing on a small number of predefined cytokines rather than discovery research [25].
Flow Cytometry-Based Multiplex Assays
Flow cytometry platforms have gained significant traction for cytokine detection due to their balance of performance and accessibility in clinical and research institutions [21]. Recent innovations have further enhanced their utility, such as one-step assay formats that reduce operation and reaction times. In these advanced systems, all reagents including capture-antibody-modified beads and phycoerythrin-labeled detection antibodies are mixed in the same reaction system, achieving similar performance to conventional approaches while significantly simplifying the procedure [21]. Additionally, lyophilization techniques have been successfully implemented to remove the need for cold storage of reagents, further streamlining the assay process and enhancing its practicality for diverse research environments [21].
Luminex xMAP Technology
Luminex technology utilizes color-coded microspheres that allow for simultaneous detection of multiple cytokines in a single sample [25]. Each microsphere set is labeled with distinct fluorescent ratios and coated with capture antibodies specific to different cytokines, enabling multiplexed quantification through flow cytometry or specialized readers [25]. This platform's key advantage lies in its extensive multiplexing capacity while maintaining high sensitivity and requiring minimal sample volume, making it particularly valuable for pediatric studies or animal model research where sample availability is limited [25].
Experimental Protocols and Methodological Considerations
Conventional Flow Cytometry-Based Cytokine Assay Protocol
The conventional flow cytometry-based multiple cytokine assay follows a multi-step process requiring several hours to complete. The detailed methodology consists of: (1) combining 50 μL of sample or standard with 50 μL of capture microspheres in a 96-well plate and incubating with shaking at room temperature for 2 hours; (2) removing unbound material by washing with buffer (0.15 M PBS, 0.05% Tween-20, pH 7.4), followed by addition of a biotinylated secondary antibody and incubation for 30 minutes; (3) after additional washing to remove unconjugated secondary antibody, adding streptavidin-PE conjugate and incubating with shaking at room temperature for 30 minutes; and (4) following a final wash step, adding reading buffer and analyzing the plate using a flow cytometer [21].
Advanced One-Step Flow Cytometry Assay Protocol
Recent methodological innovations have led to simplified protocols that maintain analytical performance while significantly reducing complexity. The one-step assay protocol is substantially more efficient: (1) 100 μL of sample or standard is added to a 96-well plate containing lyophilized reagent beads and incubated with shaking at room temperature for 1.5 hours; (2) following washing to remove unbound components, reading buffer is added, and the plate is analyzed using a flow cytometer [21]. This streamlined approach reduces hands-on time and total assay duration while maintaining analytical performance, demonstrating how methodological refinements can enhance practical utility in research settings.
Lyophilization Optimization for Assay Simplification
The development of stable lyophilized reagents represents a significant advancement in cytokine detection technology. Optimization of lyophilization buffers has been systematically evaluated using different formulations: (1) 0.15 M PBS buffer (pH 7.4) containing 0.1% BSA; (2) 0.15 M PBS buffer (pH 7.4) supplemented with 0.1% BSA and 5% trehalose; and (3) 0.15 M PBS buffer (pH 7.4) containing 0.1% BSA, 5% mannitol, and 3% trehalose [21]. The capture-antibody-containing microspheres and corresponding detection antibodies are mixed in one of these lyophilization buffer systems, with microsphere concentrations of 100,000 particles/mL and detection antibody concentrations of 2 μg/mL [21]. Using an automated dispensing system, 250 μL aliquots are rapidly dispensed into liquid nitrogen, where they crystallize within approximately 10 seconds, followed by immediate transfer to a pre-cooled vacuum freeze-dryer for lyophilization over 12 hours to obtain stable freeze-dried reagent spheres [21].
Diagram 1: Workflow comparison of conventional versus advanced one-step cytokine detection assays.
Comparative Validation Studies and Method Agreement
Statistical Approaches for Method Comparison
When evaluating different cytokine detection platforms, researchers must employ appropriate statistical methods to assess agreement between technologies. Traditional regression analysis and correlation coefficients have been widely used but are subject to limitations, as they measure the strength of linear relationships rather than actual agreement between methods [23]. The Bland-Altman plot has emerged as a more informative approach for method comparison, quantifying agreement between two quantitative measurements by studying the mean difference and constructing limits of agreement [23]. This method visualizes differences in measurements against the average of the two methods, computing the average difference and standard deviation to establish 95% limits of agreement (mean difference ± 1.96 SD), with smaller ranges between limits indicating better concordance [23].
Empirical Comparison of ELISA and Flow Cytometry
A focused comparison study examining IL-1β, IL-6, and TNF-α measurements demonstrated that while regression analysis showed general compatibility between ELISA and flow cytometry for all three cytokines, Bland-Altman plots revealed important differences [23]. The two methods showed better agreement for IL-6 measurements compared to IL-1β and TNF-α, highlighting how statistical approach selection can significantly impact interpretation of method compatibility [23]. This underscores the importance of utilizing multiple statistical approaches when validating new cytokine detection platforms or transitioning between methodologies.
Table 2: Clinical Applications of Cytokine Profiling in Disease Management
| Disease Area | Cytokines Measured | Clinical Utility | Detection Platform | Reference |
|---|---|---|---|---|
| COVID-19 | 12-plex panel | Disease severity stratification; outcome prediction | One-step flow cytometry | [21] |
| HBV Infection | 12-plex panel + ALT/AST | Viral load prediction; treatment monitoring | Flow cytometry with machine learning | [21] |
| Cancer Diagnosis | sEV protein markers | Non-invasive cancer detection; treatment response | Enzymatic optical reporter | [26] |
| Hypercholesterolemia | IL-1β, IL-6, TNF-α | Inflammation monitoring | ELISA vs. Flow cytometry comparison | [23] |
| Parkinson's Disease | Digital biomarkers | Early detection; progression monitoring | Wearable sensors | [27] |
Integration with Advanced Analytical Approaches
Machine Learning-Enhanced Cytokine Analysis
The integration of machine learning algorithms with multiplex cytokine data has significantly enhanced the diagnostic and prognostic value of cytokine profiling. In the context of HBV infection, supervised machine learning approaches including logistic regression, random forest, and support vector machines have been successfully applied to cytokine data along with ALT and AST measurements to predict viral load [21]. These algorithms utilize random search coupled with 5-fold cross-validation to identify optimal hyperparameters, with performance compared according to accuracy and Area Under the Curve (AUC) metrics [21]. Additionally, unsupervised machine learning models such as t-SNE have demonstrated utility in clustering COVID-19 patients based on their cytokine profiles, providing deeper insights into disease heterogeneity and progression [21].
Emerging Technologies and Future Directions
The cytokine detection landscape continues to evolve with several emerging technologies enhancing measurement capabilities. Digital biomarkers represent a novel class of biomarkers acquired through portable, wearable, implantable, or ingestible digital devices, enabling longitudinal, continuous measurement beyond traditional clinical environments [27]. Additionally, enzymatic optical reporter deposition-based liquid biopsy assays have demonstrated exceptional sensitivity for small extracellular vesicle detection, achieving a limit of 6.4 × 10³ particles mLâ»Â¹ with a linear range of 10â´-10¹Ⱐparticles mLâ»Â¹ while consuming minimal biofluid volumes (10 μL) [26]. When combined with dimensionality reduction techniques like principal coordinates analysis, these approaches have achieved remarkable diagnostic accuracy, reaching 100% in distinguishing between cancer and noncancer controls in a clinical cohort of 84 patients across 6 cancer types [26].
Diagram 2: Integration of multiplex cytokine data with machine learning for enhanced clinical insights.
The Researcher's Toolkit: Essential Reagents and Materials
Successful cytokine detection requires careful selection and optimization of reagents and materials. The following toolkit compiles essential components for establishing robust cytokine detection assays across different platforms.
Table 3: Essential Research Reagent Solutions for Cytokine Detection
| Reagent/Material | Function | Examples/Specifications | Considerations |
|---|---|---|---|
| Matched Antibody Pairs | Capture and detection of specific cytokines | Monoclonal capture with biotinylated detection | Varying affinity between pairs affects sensitivity [5] |
| Recombinant Protein Standards | Quantification standard curve | BioLegend; range: 3-log dilution series | Must match native protein structure and activity [21] [5] |
| Blocking Buffers | Prevent non-specific binding | BSA, Blotto, Casein, Superblock | Optimal buffer varies by assay; empirical testing required [5] |
| Coated Microspheres | Solid phase for multiplex detection | Fluorescently encoded beads (Spherotech) | Coupling via EDC/sulfo-NHS chemistry [21] |
| Lyophilization Stabilizers | Reagent preservation without cold storage | Trehalose, mannitol in PBS buffer | Maintains antibody stability and assay performance [21] |
| Signal Amplification Systems | Enhanced detection sensitivity | Streptavidin-HRP, streptavidin-PE, IR dyes | Choice affects dynamic range and background [5] [25] |
| Niraxostat | Niraxostat, CAS:206884-98-2, MF:C16H17N3O3, MW:299.32 g/mol | Chemical Reagent | Bench Chemicals |
| Nitecapone | Nitecapone, CAS:116313-94-1, MF:C12H11NO6, MW:265.22 g/mol | Chemical Reagent | Bench Chemicals |
Accurate cytokine quantification continues to play an increasingly vital role in disease diagnosis and therapeutic monitoring, with technology advancements steadily enhancing the sensitivity, multiplexing capability, and practical utility of detection platforms. The integration of streamlined methodologies such as one-step assays and lyophilized reagents with advanced computational approaches including machine learning represents the future of cytokine profiling, enabling more precise disease stratification and treatment monitoring across diverse clinical and research applications. As these technologies continue to evolve, researchers must maintain rigorous validation practices employing appropriate statistical approaches to ensure data reliability and translational relevance, ultimately advancing both fundamental understanding of disease mechanisms and clinical management of complex inflammatory conditions.
Cytokine Detection Technologies: From ELISA to Digital Immunoassays
Within the field of immunology and biomedical research, accurately measuring cytokine levels is crucial for understanding immune responses, disease mechanisms, and the efficacy of therapeutic interventions. Among the array of available techniques, the Enzyme-Linked Immunosorbent Assay (ELISA) has long been considered a fundamental and reliable workhorse. This guide provides an objective comparison of ELISA's performance against modern alternative platforms, focusing on its characteristic moderate sensitivity within the broader context of cytokine detection methods. We will summarize key quantitative data, detail standard experimental protocols, and position ELISA within the current technological landscape to aid researchers, scientists, and drug development professionals in making informed methodological choices.
Technology Comparison: Positioning ELISA Among Alternatives
The selection of a cytokine detection method is a critical decision that shapes project conclusions, budgets, and follow-up plans. Cross-platform studies consistently reveal significant differences in detectability, dynamic range, and agreement across overlapping cytokines due to fundamental variations in assay physics [28]. The table below provides a high-level overview of how ELISA sits alongside other common technologies.
Table 1: Core Characteristics of Major Cytokine Detection Platforms
| Method | How It Detects Protein | Multiplexing Capability | Sensitivity | Sample Volume per Panel | Key Strengths | Key Constraints |
|---|---|---|---|---|---|---|
| ELISA | Sandwich immunoassay with enzyme-linked colorimetric or chemiluminescent readout [15] | Single-plex (one analyte per well) [29] | Moderate (typically low pg/mL) [25] | 100-200 μL [25] | High specificity; well-validated; widely available; cost-effective [15] [29] | Not efficient for many analytes; higher sample volume; moderate dynamic range [15] [25] |
| Luminex (Bead-Based) | Fluorescent detection on spectrally distinct beads [28] | High-plex (up to 500 analytes) [25] | Good (low pg/mL) [28] [25] | ~25-50 μL [25] | Good for profiling many cytokines; well-understood; flexible panels [28] | Potential for background fluorescence/cross-reactivity; some low-abundance targets may be missed [28] |
| MSD (Electrochemiluminescence) | Sandwich immunoassay with electrochemiluminescent readout [28] [15] | Moderate-plex (e.g., 10-plex per spot) [28] [15] | High; very sensitive [28] [25] | ~20-40 μL [28] | Excellent sensitivity and broad dynamic range; good performance in complex matrices [28] [25] | Limited multiplex capacity compared to high-plex options; higher sample volume than some platforms [28] |
| Olink (Proximity Extension Assay) | Dual antibody binding with DNA oligonucleotide hybridization and PCR amplification [28] | High-plex | High (low pg/mL possible) [28] | ~1 μL [28] | High specificity; very low sample requirement; high multiplex capability [28] | Relative quantification; may have lower sensitivity for some very low-abundance analytes [28] |
Quantitative data from platform comparison studies highlight critical performance differences. A key differentiator is sample volume requirement. For a single panel, Olink uses approximately 1 μL, Luminex requires about 12.5 μL, while traditional ELISA needs 100-200 μL, making it less suitable for volume-limited studies [28] [25]. Regarding sensitivity and detectability, in the IMPACC COVID-19 cohort study, platforms were ranked for detectability as follows: Alamar NULISAseq had the highest overall detectability, followed by Olink, with Luminex having lower detectability for some low-abundance cytokines [28]. ELISA typically offers sensitivity in the low picogram per milliliter (pg/mL) range, which is sufficient for many cytokines but may be less sensitive than ECL-based platforms (like MSD) or ultra-sensitive methods for very low-abundance targets [25].
Table 2: Cross-Platform Performance Metrics from Comparative Studies
| Performance Metric | ELISA | Luminex | MSD | Olink |
|---|---|---|---|---|
| Typical Dynamic Range | 2-3 logs [25] | 3-5 logs [25] | 3-5 logs [25] | Robust over its range [28] |
| Correlation Between Platforms | Good correlation with flow cytometry for IL-1β, IL-6; less for TNF-α [30] | Varies by target; lower for low-abundance cytokines [28] | Often correlates well with other platforms for medium-abundance analytes [28] | Better agreement with other PEA than bead-based methods [28] |
| Data Output | Absolute quantification (pg/mL) [28] | Absolute quantification (pg/mL) [28] | Absolute quantification (pg/mL) [28] | Relative quantification (NPX) [28] |
Experimental Protocols: Core Methodology and Comparisons
Detailed Protocol: Sandwich ELISA for Cytokine Detection
The sandwich ELISA is the most common format for cytokine detection due to its high specificity [31] [32]. The following protocol details the critical steps, which are also visualized in the workflow diagram.
- Plate Coating: A high-binding 96-well microtiter plate is coated with a capture antibody specific to the target cytokine. The antibody is diluted in a coating buffer, and an appropriate volume is added to each well. The plate is then sealed and incubated overnight at 4°C or for a shorter period (e.g., 1-2 hours) at room temperature [32].
- Blocking: After washing the plate multiple times with a wash buffer (e.g., PBS containing 0.05% Tween 20, PBST) to remove unbound capture antibody, the remaining protein-binding sites on the plastic are "blocked" to prevent non-specific binding. This is typically done by incubating the wells with a blocking agent like 5% skim milk or Bovine Serum Albumin (BSA) in PBST for 1-2 hours at room temperature [33] [32].
- Sample and Standard Incubation: After another wash cycle, the plate is ready for sample addition. The blocking buffer is discarded, and the test samples—serum, plasma, or cell culture supernatant—are added to the wells. It is crucial to include a dilution series of a known concentration of the recombinant cytokine (standard) to generate a standard curve for quantification. The plate is incubated, allowing the target cytokine in the samples and standards to be captured by the immobilized antibody [32].
- Detection Antibody Incubation: The plate is washed again to remove unbound protein. A biotin-conjugated detection antibody, specific to a different epitope on the target cytokine, is then added to the wells and incubated. This forms the "sandwich" [31] [32].
- Enzyme Conjugate Incubation: Following another wash step to remove excess detection antibody, a streptavidin conjugate linked to an enzyme such as Horseradish Peroxidase (HRP) is added. The streptavidin binds with high affinity to the biotin on the detection antibody [31] [32].
- Signal Development and Readout: In the final step, after a final thorough wash to remove unbound conjugate, a colorimetric substrate solution (e.g., TMB for HRP) is added to the wells. The enzyme catalyzes the conversion of the substrate into a colored product. The reaction is stopped after a defined period with a stop solution (e.g., acid). The intensity of the color, measured as Optical Density (OD) by a plate reader, is proportional to the amount of cytokine present in the well [31] [32].
- Data Analysis: The OD values of the standard concentrations are used to generate a standard curve (often a 5-parameter logistic curve). The concentration of the cytokine in the unknown samples is then interpolated from this curve [31].
Comparative Protocol: Flow Cytometry for Cytokine Measurement
Flow cytometry offers an alternative approach, often used for intracellular cytokine staining in specific cell populations. A typical protocol for bead-based soluble cytokine measurement (e.g., CBA Flex Set) is summarized below for contrast with ELISA:
- Bead Preparation: A mixture of multiple bead populations is prepared, each with a distinct fluorescence intensity and coated with a capture antibody specific to a different cytokine.
- Incubation: The mixed beads, recombinant standards or test samples (e.g., serum), and PE-conjugated detection antibodies are combined and incubated to form sandwich complexes.
- Acquisition: The reaction mixture is resolved on a flow cytometer. One laser identifies the specific bead (and thus the analyte), while a second laser quantifies the PE fluorescence on the bead, which is proportional to the amount of bound cytokine.
- Analysis: Using specialized software, the concentration of each cytokine in the sample is determined by comparing the PE fluorescence to the standard curve [30].
The Scientist's Toolkit: Essential Reagent Solutions
Successful cytokine detection, regardless of platform, relies on a core set of high-quality reagents. The following table details these essential materials.
Table 3: Essential Research Reagents for Cytokine Detection Assays
| Reagent / Material | Function / Role in the Assay | Key Considerations |
|---|---|---|
| Matched Antibody Pairs | A capture antibody to immobilize the target and a detection antibody to bind a different epitope, providing high specificity [32]. | Antibodies must be well-matched and tested for pairing. Monoclonal antibodies offer high specificity; polyclonals can increase signal but may raise background noise [32]. |
| Titrated Standards | A purified recombinant protein of known concentration used to generate a standard curve for quantitative interpolation of sample concentrations [32]. | Critical for assay accuracy. Must be diluted precisely to create the curve. The quality of the standard directly impacts data reliability [32]. |
| Detection Enzyme Conjugate | An enzyme (e.g., HRP) linked to a secondary antibody or streptavidin, which catalyzes the substrate conversion to generate a detectable signal [32]. | Streptavidin-HRP is common when using biotinylated detection antibodies. The enzyme's activity and conjugate stability are vital for consistent results. |
| Chromogenic/ECL Substrate | A chemical compound (e.g., TMB) that the enzyme converts into a colored, fluorescent, or luminescent product [33] [32]. | Choice depends on the enzyme and required sensitivity. Precipitating TMB is used for dot-blot visualization [33], while soluble TMB is common for plate-based ELISA. |
| Plate Washer and Reader | Specialized instrumentation to automate washing steps and to measure the optical density (OD) of each well at specific wavelengths [31]. | Proper washer calibration ensures consistent washing. The plate reader must be compatible with the assay format (e.g., 96-well plate) and substrate type. |
| Blocking Agent | A protein solution (e.g., BSA, skim milk) used to cover any non-specific binding sites on the solid phase after coating [33]. | Prevents false positive signals. The agent must be inert and not interfere with antibody-antigen binding. |
| Nithiamide | Nithiamide, CAS:140-40-9, MF:C5H5N3O3S, MW:187.18 g/mol | Chemical Reagent |
| Nitracrine | Nitracrine, CAS:4533-39-5, MF:C18H20N4O2, MW:324.4 g/mol | Chemical Reagent |
Sensitivity in Context: Understanding Key Metrics
When evaluating ELISA's "moderate sensitivity," it is essential to distinguish between specific technical terms often used interchangeably.
- Sensitivity vs. Limit of Detection (LOD): In analytical chemistry, sensitivity is formally defined as the slope of the calibration curve, indicating how the signal changes with concentration. In practice, the ELISA industry commonly uses "sensitivity" to refer to the LOD. The LOD is the minimum concentration of an analyte that can be reliably distinguished from a blank sample, typically defined as the mean blank signal plus 3 standard deviations [34].
- Limit of Quantification (LOQ): The LOQ is a more practical metric. It is the lowest concentration that can be quantitatively measured with acceptable precision and accuracy (often defined as the mean blank signal plus 10 standard deviations). Results between the LOD and LOQ may be considered qualitatively detected but not reliably quantifiable [34]. The lower limit of the range provided in most commercial ELISA kits is typically aligned with the LOQ, ensuring data within the stated range is quantitatively robust [34].
ELISA remains a cornerstone technology for cytokine detection, prized for its specificity, robustness, and accessibility. Its position as a "workhorse" is well-earned. However, as this guide has detailed through quantitative comparisons and methodological breakdowns, its moderate sensitivity and single-plex nature present clear limitations. The choice between ELISA and modern multiplex or ultra-sensitive platforms like Luminex, MSD, and Olink is not about identifying a single superior technology, but about matching the tool to the task. For targeted analysis of a few cytokines with sufficient abundance, ELISA is an excellent and cost-effective choice. For discovery-phase research requiring a broad profile from minimal sample volume, newer high-plex technologies offer compelling and often necessary advantages. Understanding these trade-offs empowers scientists to design better studies and generate more reliable data in the complex field of cytokine biology.
In the field of immunology, accurately measuring cellular immune responses is crucial for advancing vaccine development, cancer immunotherapy, and infectious disease research. While various methods exist for cytokine detection, the Enzyme-Linked ImmunoSpot (ELISPOT) assay stands apart by providing exceptional sensitivity and single-cell resolution. This technique enables researchers to enumerate individual cytokine-secreting cells, offering insights into immune function that bulk measurement methods cannot provide. Unlike assays that measure the total concentration of analytes in solution, ELISPOT captures the secretory activity of individual cells, making it uniquely valuable for detecting rare antigen-specific T-cells and B-cells. This capability is particularly important in monitoring low-frequency immune responses where the number of responding cells is limited but biologically significant. As research increasingly focuses on precise immune monitoring, understanding ELISPOT's technical advantages, proper implementation, and performance relative to other methods becomes essential for designing robust experimental strategies.
Technology Comparison: ELISPOT Versus Alternative Cytokine Detection Platforms
Key Characteristics of Major Cytokine Detection Methods
Various platforms are available for cytokine detection, each with distinct strengths and limitations. The table below provides a systematic comparison of ELISPOT with other commonly used technologies.
| Method | Detection Principle | Sensitivity | Resolution | Multiplexing Capacity | Sample Requirements | Key Applications |
|---|---|---|---|---|---|---|
| ELISPOT | Immunoassay with membrane-bound capture and enzymatic/fluorescent detection [31] [35] | Very high (single-cell level) [31] [36] | Single-cell | Moderate (1-4 analytes with FluoroSpot) [37] | Live cells (e.g., PBMCs) [31] | Vaccine development, T-cell monitoring, cancer immunology [31] [38] |
| ELISA | Immunoassay with plate-bound capture and enzymatic detection in solution [31] [28] | Moderate to high | Bulk protein measurement | Limited (single-plex or low-plex) [28] | Serum, plasma, supernatant [31] | Biomarker validation, antibody titer measurement [31] |
| Flow Cytometry (ICS) | Intracellular staining with fluorescent antibodies and cell analysis [37] [21] | Moderate | Single-cell | High (multiple cytokines + phenotyping) [37] [21] | Live cells | Immune cell profiling, functional characterization [39] [21] |
| Luminex | Bead-based immunoassay with fluorescent detection [28] | Moderate | Bulk protein measurement | High (up to 50+ analytes) [28] | Serum, plasma | Biomarker discovery, cytokine profiling [28] |
| MSD | Electrochemiluminescence with plate-bound capture [28] | High | Bulk protein measurement | Moderate (typically 10-plex) [28] | Serum, plasma (20-40 μL/panel) [28] | Biomarker validation, pharmacokinetic studies [28] |
Sensitivity and Performance Characteristics
Quantitative performance data reveals significant differences between platforms. In a direct comparison study of SARS-CoV-2 T-cell responses, ELISPOT demonstrated superior sensitivity to intracellular cytokine staining (ICS), detecting responses in 67% of paucisymptomatic patients compared to 44% with ICS [39]. This enhanced sensitivity for rare cell detection is further evidenced by ELISPOT's ability to detect frequencies as low as 1 in 100,000 cells [31].
Sample requirement differences are also substantial. ELISPOT typically requires 250,000 PBMCs per well for human IFN-γ detection [39], while miniaturized 384-well formats can function with only 33,000 PBMCs per well, enabling up to 30 data points from 1 mL of blood [40]. This economy of cell usage is particularly valuable when working with limited clinical samples.
ELISPOT Protocol: Detailed Methodology for Robust Results
Plate Preparation and Coating
The ELISPOT procedure begins with plate preparation, typically using 96-well plates with PVDF membranes. The membrane is first activated with 35% ethanol for 30 seconds, followed by thorough washing with PBS to remove any residual ethanol that could compromise cell viability [35]. Coating with a capture antibody specific to the target cytokine (e.g., IFN-γ, IL-2, Granzyme B) is performed overnight at 4°C, typically using 0.5-1 μg antibody per well in phosphate-buffered saline [35]. After coating, plates are blocked with protein-based blocking buffers such as 2% skim milk or 1% BSA for 2 hours at room temperature to prevent nonspecific binding [35]. Properly prepared plates can be stored at 4°C for up to two weeks in sealed pouches with desiccant [35].
Cell Preparation and Stimulation
Peripheral blood mononuclear cells (PBMCs) are the most common sample type for ELISPOT assays. Both freshly isolated and cryopreserved PBMCs can be used, though proper handling is critical. Fresh blood samples should be processed within 8 hours of collection to prevent granulocyte activation and preserve T-cell function [35]. For frozen PBMCs, an optimized thawing protocol followed by a resting period of at least 1-4 hours helps remove cell debris and restore cellular function [39] [38] [35]. Cell viability should exceed 95% as determined by trypan blue exclusion [35].
During assay setup, cells are counted and plated at appropriate densities, typically ranging from 100,000 to 400,000 cells per well in 96-well plates [39]. Antigenic stimulation is achieved using peptide pools (e.g., CEF pool, SARS-CoV-2 spike peptides) at concentrations typically ranging from 1-2 μg/mL [39] [38]. Positive control wells contain mitogens such as phytohemagglutinin (PHA), while negative control wells contain equivalent concentrations of the peptide solvent (usually DMSO) [38]. The plate is then incubated for 18-24 hours at 37°C with 7% CO₂ to allow for cytokine secretion and capture [39] [38].
Detection and Visualization
Following incubation, cells are removed by washing, and a biotinylated detection antibody is added, which binds to the captured cytokine [31] [35]. After incubation and washing, a streptavidin-enzyme conjugate (typically alkaline phosphatase or horseradish peroxidase) is added [31] [35]. A precipitating substrate solution is then added, which produces insoluble colored spots at the sites of cytokine secretion [31]. For fluorescent detection (FluoroSpot), enzyme-conjugated antibodies are replaced with fluorophore-conjugated detection reagents [37]. The reaction is stopped by water rinsing, and plates are air-dried prior to analysis [35].
Image Acquisition and Analysis
Proper spot enumeration requires specialized ELISPOT readers with high-resolution imaging capabilities. Spot size and morphology provide important information about secretory activity, with IFN-γ spots typically measuring 25-50 μm in diameter [41]. High-resolution imaging (achieving pixel sizes of 2.5 μm or smaller) is essential for accurate spot detection and enumeration, particularly for smaller cytokines like TNF-α with spots as small as 15 μm [41]. Automated readers use sophisticated algorithms to distinguish true spots from background artifacts, providing counts of spot-forming units (SFU) per well, which are typically normalized to SFU per million input cells [31] [40].
Essential Research Reagents and Equipment
Successful ELISPOT implementation requires specific reagents and equipment optimized for the assay's requirements.
| Category | Specific Items | Function & Importance |
|---|---|---|
| Consumables | PVDF membrane plates [35] | Provides matrix for antibody coating and spot formation |
| Coating antibodies [31] [35] | Capture specific cytokines at secretion site | |
| Detection antibodies (biotinylated) [31] [35] | Bind captured cytokine for detection | |
| Enzyme conjugates (Streptavidin-HRP/ALP) [31] [35] | Catalyze substrate conversion for signal generation | |
| Precipitating substrates [31] [35] | Form insoluble colored products at secretion sites | |
| Cell Culture | PBMC isolation materials (Ficoll, separation tubes) [40] [35] | Isolate mononuclear cells from whole blood |
| Cell culture media (RPMI, CTL-Test medium) [40] [38] | Support cell viability during stimulation | |
| Peptide pools/antigens [39] [38] | Stimulate antigen-specific cytokine secretion | |
| Equipment | ELISPOT plate reader [31] [41] | Automated spot enumeration with high resolution |
| Biological safety cabinet [35] | Maintain sterile conditions for cell culture | |
| COâ‚‚ incubator [39] [38] | Maintain optimal temperature, humidity, and COâ‚‚ |
Advanced Applications and Protocol Variations
FluoroSpot for Multiplexed Detection
FluoroSpot represents an advanced extension of ELISPOT technology, enabling simultaneous detection of 2-4 different cytokines from the same cell population [37]. This multiplexing capability provides insights into polyfunctional T-cells capable of producing multiple effector molecules simultaneously. By using detection antibodies conjugated to different fluorophores rather than enzymes, FluoroSpot allows discrimination of cells secreting different cytokine combinations [37]. This approach is particularly valuable for comprehensive immune monitoring, allowing researchers to characterize Th1 (IFN-γ), Th2 (IL-4, IL-5), and Th17 (IL-17) responses simultaneously from limited cell numbers.
Miniaturized Formats for Limited Samples
For studies with limited cell availability, ELISPOT assays can be performed in 384-well formats, which require only one-third of the reagents and cells compared to standard 96-well plates [40]. This miniaturization enables comprehensive immune monitoring from small blood volumes, making the technology applicable to pediatric, geriatric, and immunosuppressed patient populations where sample collection is limited [40]. Despite the reduced well size, 384-well formats maintain equivalent spot sizes and detection sensitivity to conventional formats [40].
Regulatory Compliance and Assay Validation
For regulated studies, ELISPOT assays require formal validation to ensure reliability and reproducibility. Key validation parameters include limit of detection (LOD), precision (intra-assay, inter-assay, and inter-analyst), specificity, and linearity [38]. Establishing appropriate cut points using statistical methods is essential for determining positive responses in biological samples [38]. Such rigorous validation is particularly important in gene therapy studies and clinical trials where cellular immune responses against viral vectors or transgene products must be accurately monitored [38].
ELISPOT remains a cornerstone technology for detecting cytokine-secreting cells at single-cell resolution, offering unparalleled sensitivity for monitoring rare antigen-specific immune responses. Its unique ability to quantify functionally active cells rather than bulk protein concentration provides critical insights in vaccine development, cancer immunotherapy, and infectious disease research. While newer multiplexing technologies offer advantages for certain applications, ELISPOT's combination of sensitivity, quantitative accuracy, and functional relevance ensures its continued importance in comprehensive immune monitoring strategies. Proper implementation following optimized protocols, coupled with appropriate reagent selection and validation, enables researchers to leverage this powerful technology to advance our understanding of immune function in health and disease.
The measurement of soluble cytokines and other analytes is crucial for understanding immune responses, disease progression, and the efficacy of therapeutic interventions. Traditional methods like the enzyme-linked immunosorbent assay (ELISA) have long been the standard for quantitative analysis of cytokines and other biomarkers but are not well-suited for high-throughput multiplex analyses. Multiplex bead array assays address this limitation by enabling the simultaneous quantification of numerous analytes in a single small-volume sample. Among these, Luminex xMAP technology has emerged as a leading platform, combining advanced fluidics, optics, and digital signal processing with proprietary microsphere technology to deliver both high-density and high-throughput multiplexed assay capabilities. This technology is particularly valuable in research and clinical laboratories where rapid, precise, and cost-effective measurement of multiple analytes is required, from basic research in immunology to applied drug development and clinical trial support [42] [43] [44].
Luminex xMAP Technology: Core Principles and Workflow
Fundamental Technology Components
The Luminex platform leverages xMAP (Multi-Analyte Profiling) technology, which utilizes fluorescently-coded microspheres as the solid support for immunoassays. The system integrates four core technologies:
- xMAP Microspheres: These are 6.45 µm magnetic or 5.6 µm polystyrene microspheres impregnated with varying ratios of fluorescent dyes, creating up to 500 distinct spectral signatures. Each bead set can be coated with a unique capture molecule (e.g., antibody, antigen, oligonucleotide), allowing it to specifically bind a different target analyte [44].
- Bead-Based Immunoassays: Assays such as the MILLIPLEX panels consist of analyte-specific capture antibodies conjugated to xMAP beads, enabling multivariate analysis of complex biological states using minimal sample volumes (as low as 25 µL) [44].
- Luminex Detection Platforms: Instruments like the Luminex 200, FLEXMAP 3D, and xMAP INTELLIFLEX systems use flow cytometry-based detection with integrated lasers, optics, advanced fluidics, and high-speed digital signal processors to identify the bead set and quantify the bound analyte [44].
- Software: xPONENT software handles data acquisition, while Belysa software provides sophisticated data analysis capabilities for curve fitting and concentration determination [44].
Assay Workflow and Detection Mechanism
The typical workflow for a Luminex multiplex immunoassay involves several key steps, visualized in the diagram below.
Fig. 1 Luminex Multiplex Assay Workflow
During the reading process, the Luminex analyzer uses two lasers: a classification laser (often a 635 nm red laser) which excites the dyes inside the beads to identify which bead set is being Interrogated, and a reporter laser (532 nm green laser) which excites the phycoerythrin (PE) fluorescent label to quantify the amount of bound analyte. The resulting data provides both the identity of the analyte (from the bead spectral address) and its concentration (from the PE fluorescence intensity) for each individual bead, with statistical rigor derived from analyzing numerous beads per analyte [42] [44].
Performance Comparison of Luminex with Alternative Platforms
Direct Technology Comparison: Luminex vs. ELISA vs. MSD
When selecting a platform for cytokine detection, researchers commonly evaluate key performance parameters including sensitivity, dynamic range, multiplexing capacity, and throughput. The table below provides a direct comparison of Luminex with two other widely used technologies: traditional ELISA and Meso Scale Discovery (MSD) electrochemiluminescence platforms.
Table 1: Platform Comparison for Cytokine Detection
| Parameter | Luminex xMAP | Traditional ELISA | Meso Scale Discovery (MSD) |
|---|---|---|---|
| Detection Technology | Fluorescence-labeled microspheres [45] | Colorimetric reaction [43] | Electrochemiluminescence (ECL) [45] |
| Multiplexing Capacity | High (Up to 80-500 analytes) [45] [44] | Single-plex only [43] | Moderate (Up to 10 analytes) [45] |
| Sample Volume | Low (25-50 µL) [42] [44] | High (Often >100 µL per analyte) | Low (Similar to Luminex) |
| Sensitivity | Higher than ELISA [43] | Lower than Luminex [43] | Highest (e.g., S-PLEX assays at femtogram level) [45] |
| Dynamic Range | 3-4 log [44] | 1-2 log | >4 log [45] |
| Throughput | High (96- or 384-well format) [44] | Low (Multiple plates for multiple analytes) | High (96-well format) |
| Best Application Fit | Large-scale multiplex studies, immune profiling [45] | Single-analyte studies with limited budget | Low-abundance biomarkers, late-phase drug development [45] |
Supporting Experimental Data and Cross-Platform Studies
The comparative performance outlined in Table 1 is supported by numerous experimental studies. A key advantage of Luminex is its higher sensitivity and multiplexing capability compared to ELISA. One study noted that Luminex technology can detect cytokine levels that are several orders of magnitude lower than those detectable by ELISA, with generally higher accuracy due to the bead-based assay system and reduced potential for cross-reactivity [43].
However, performance can vary based on the specific kit manufacturer and bead type. A 12-year multi-site proficiency testing program analyzing data from over 15,500 measurements found that switching from polystyrene to paramagnetic beads significantly improved performance, yielding better precision and accuracy [46]. Furthermore, a comparative study of three commercial Luminex kits (Bio-Rad, Millipore, Ozyme) using supernatants from antigen-stimulated peripheral blood mononuclear cells (PBMC) revealed that Millipore kits showed a better working range and lower overall mean pooled coefficients of variation (CV) for all donors and cytokines (19.4%) compared to Bio-Rad (17.2%) and Ozyme (26.7%) [47].
When compared directly to MSD in another study, both platforms demonstrated strong correlation, but MSD generally exhibited a broader dynamic range and higher sensitivity, making it more suitable for detecting very low-abundance analytes [45]. This makes MSD particularly valuable for later-phase clinical trials where detecting subtle changes in biomarker levels is critical.
Experimental Protocols for Luminex-Based Detection
Key Methodological Considerations for Optimal Performance
To ensure reliable and reproducible results from Luminex assays, particularly when profiling cytokines from cell culture models, several experimental parameters require careful optimization:
- Cell Culture Protocol Optimization: When using supernatants from antigen-stimulated PBMCs, the culture duration and cell density significantly impact cytokine measurements. Kinetic studies have shown that the optimal culture duration for maximal specific cytokine concentration (stimulated minus background) varies by analyte. For instance, IL-2 peaks at 2 days, while IFNγ, IL-5, and IL-17 peak at 5 days. This suggests that a protocol with a single round of stimulation but with two time points (e.g., day 2 and day 5) yields the best results for a comprehensive cytokine profile [47].
- Cell Density: Using 0.5 million PBMCs per well provides similar levels of specific cytokine secretion as 1.0 million cells, making it a suitable and efficient choice, especially when working with limited patient samples [47].
- Bead Type: Magnetic bead-based kits demonstrate better precision than polystyrene bead-based kits, with lower mean coefficients of variation for both standards and samples [47].
Detailed Protocol: Evaluating SARS-CoV-2 Antibody Responses
Recent applications of Luminex technology include the evaluation of immune responses to infectious diseases. The following protocol, adapted from a 2023 study comparing Luminex-based assays for SARS-CoV-2 antibody detection, outlines a typical workflow [48]:
Sample Collection and Preparation:
- Collect human serum samples and store at -40°C or lower prior to testing.
- Include pre-characterized positive and negative control samples, as determined by a reference method (e.g., Roche Elecsys immunoassay).
Assay Procedure (MULTICOV-AB Assay):
- Bead Preparation: Use Luminex MagPlex magnetic beads conjugated with SARS-CoV-2 antigens (Spike (S), Receptor Binding Domain (RBD), and Nucleocapsid (N)).
- Sample Incubation: Incubate the bead mixture with test samples in a 96-well plate. Include a standard curve for quantification, if available.
- Washing: Wash the beads to remove unbound proteins.
- Detection: Incubate with a biotinylated detection antibody (anti-human IgG), followed by incubation with streptavidin-phycoerythrin (SA-PE).
- Final Wash and Resuspension: Wash the beads to remove unbound SA-PE and resuspend them in reading buffer.
Data Acquisition and Analysis:
- Read the plate using a Luminex 200 analyzer or comparable instrument with xPONENT software.
- Report results as Net Median Fluorescence Intensity (MFI) or convert to concentration units using the standard curve.
- Define positivity criteria; for example, a sample is considered positive for SARS-CoV-2 IgG when its net MFI values for both S and RBD beads exceed the net MFI values of the respective cut-off controls [48].
In the cited study, this protocol enabled the MULTICOV-AB Assay to achieve 100% sensitivity in detecting antibodies to S trimer and RBD in known positive samples, outperforming other Luminex-based assays evaluated [48].
Essential Research Reagent Solutions
Successful implementation of Luminex technology relies on a suite of specialized reagents and materials. The following table details key components essential for performing multiplex bead-based assays.
Table 2: Essential Research Reagents for Luminex Assays
| Reagent/Material | Function | Examples & Notes |
|---|---|---|
| xMAP Microspheres | Solid support for assay; spectral signature identifies the specific analyte. | Magnetic (e.g., MagPlex) or traditional polystyrene beads. Choose the bead set based on the target analyte panel [44]. |
| MILLIPLEX Multiplex Kits | Complete analyte-specific assay kits. | Include lyophilized or liquid bead sets, standards, detection antibodies, and assay buffers. Kits are available for cytokines, chemokines, phosphoproteins, and more [44]. |
| Biotinylated Detection Antibody | Binds to the captured analyte on the bead surface. | Analyte-specific antibody that is biotinylated. Quality and clone are pivotal for assay performance [42] [47]. |
| Streptavidin-Phycoerythrin (SA-PE) | Fluorescent reporter molecule for quantification. | Binds to the biotin on the detection antibody. PE is excited by the reporter laser to generate the signal [44]. |
| Assay Buffers | Facilitate specific binding and minimize background. | Include sample diluent, wash buffer, and matrix solution to counteract interference from complex sample types like serum. |
| Luminex Analyzer | Instrument for bead interrogation and signal detection. | Platforms include Luminex 200, FLEXMAP 3D, and xMAP INTELLIFLEX. The choice affects throughput and multiplexing capacity [44]. |
| Analysis Software | Data acquisition and analysis for concentration determination. | xPONENT for acquisition and Belysa for curve fitting and data analysis [44]. |
Luminex xMAP technology represents a powerful solution for high-throughput, multiplex biomarker profiling, offering significant advantages in speed, sample conservation, and data richness over traditional methods like ELISA. While platform choice depends on specific research needs—with MSD holding an advantage for ultra-sensitive detection of low-abundance analytes—Luminex remains a premier platform for comprehensive immunophenotyping and large-scale studies. As with any sophisticated methodology, careful attention to experimental protocol, reagent selection, and validation is paramount for generating reliable and meaningful data. The continued evolution of bead-based multiplexing ensures its critical role in advancing biomedical research and drug development.
Within cytokine detection research, the analytical performance of immunoassay platforms directly determines the quality and reliability of experimental data. The measurement of cytokines—key signaling proteins in immune responses—is crucial for understanding disease pathogenesis, monitoring immune status, and developing therapeutic interventions [14] [49]. However, researchers face significant challenges due to the low abundance of many cytokines in biological samples and their wide concentration ranges during biological responses [14]. This comparison guide objectively evaluates the Meso Scale Discovery (MSD) electrochemiluminescence platform against alternative technologies, with particular focus on its dynamic range and sensitivity—two critical parameters for comprehensive cytokine profiling. The assessment is grounded in experimental data from comparative studies and technical specifications to provide evidence-based guidance for researchers, scientists, and drug development professionals working in this field.
Fundamental Principles of Electrochemiluminescence Detection
The MSD platform employs electrochemiluminescence (ECL) technology, which fundamentally differs from conventional optical detection methods. This approach utilizes electrochemical stimulation to generate light signals only from labels in immediate proximity to the electrode surface [50]. The core mechanism involves applying electricity to carbon electrode-containing plates, which triggers a light-emitting reaction from SULFO-TAG labels in the presence of a co-reactant solution containing tripropylamine (TPrA) [50] [51]. This spatial decoupling of the stimulation method (electricity) from the detected signal (light) creates a significant advantage by dramatically reducing background noise, as only labels near the electrode surface are excited and detected [50].
Key Platform Components and Workflow
The MSD system incorporates several specialized components that contribute to its analytical performance. High-binding carbon electrodes in the bottom of MULTI-ARRAY and MULTI-SPOT microplates provide substantially greater binding capacity (approximately 10×) than conventional polystyrene surfaces, enabling enhanced capture of biological reagents [50]. The platform uses SULFO-TAG labels conjugated to detection antibodies, which generate light upon electrical stimulation [50]. A typical assay follows a sandwich immunoassay format where a capture antibody specific to the target protein (e.g., TDP-43, cytokines) is immobilized on the electrode surface, followed by sample addition, and subsequent binding of a detection antibody that is recognized by a species-specific SULFO-TAG-labeled antibody [51]. The complete experimental workflow can be visualized as follows:
Comparative Performance Analysis
Sensitivity and Dynamic Range Comparisons
Multiple independent studies have consistently demonstrated MSD's superior performance characteristics for cytokine detection. A comprehensive comparison of multiple immunoassay technologies revealed that MSD exhibits the best sensitivity in the low detection limit and the broadest dynamic range among the platforms tested [13]. Similarly, a 2020 study published in Frontiers in Immunology directly comparing bead-based fluorescence (Luminex) versus planar electrochemiluminescence (MSD) multiplex immunoassays found that the MSD platform had lower lower limits of quantification (LLoQs) than Luminex for 14 out of 16 shared cytokines, with similar performance for IL-6 and superior Luminex performance only for IL-17 [49].
Table 1: Comparison of Lower Limits of Quantification (LLoQ) for Shared Cytokines Between MSD and Luminex Platforms
| Cytokine | MSD LLoQ (pg/mL) | Luminex LLoQ (pg/mL) | Sensitivity Advantage |
|---|---|---|---|
| IL-1β | Lower | Higher | MSD |
| IL-2 | Lower | Higher | MSD |
| IL-4 | Lower | Higher | MSD |
| IL-5 | Lower | Higher | MSD |
| IL-6 | Similar | Similar | Equivalent |
| IL-7 | Lower | Higher | MSD |
| IL-8 | Lower | Higher | MSD |
| IL-10 | Lower | Higher | MSD |
| IL-12 (p70) | Lower | Higher | MSD |
| IL-13 | Lower | Higher | MSD |
| IL-17 | Higher | Lower | Luminex |
| TNF-α | Lower | Higher | MSD |
| IFN-γ | Lower | Higher | MSD |
| GM-CSF | Lower | Higher | MSD |
| MIP-1α | Lower | Higher | MSD |
| MIP-1β | Lower | Higher | MSD |
The dynamic range of MSD assays typically spans 4-6 orders of magnitude, significantly broader than conventional ELISA methods [52] [49]. This extensive range enables researchers to quantify both low-abundance and high-concentration analytes within the same sample without requiring multiple dilutions, thereby conserving valuable samples and reducing processing time [50]. For example, a recently developed TDP-43 assay on the MSD platform demonstrated a working range of 4–20,000 pg/mL, representing a dynamic range exceeding 4 orders of magnitude [51].
Platform Comparison Table
Table 2: Comprehensive Comparison of Multiplex Immunoassay Platforms for Cytokine Detection
| Parameter | MSD ECL | Luminex Bead-Based Fluorescence | Traditional ELISA |
|---|---|---|---|
| Detection Technology | Electrochemiluminescence | Fluorescence-labeled microspheres | Colorimetric or chemiluminescence |
| Multiplexing Capacity | Up to 10 analytes simultaneously [45] [53] | Up to 80 analytes simultaneously [45] | Typically single-plex |
| Sensitivity | Highest (femtogram level with S-PLEX kits) [45] | Variable (generally lower than MSD) [49] | Moderate to high |
| Dynamic Range | Broadest (typically 4-6 logs) [50] [49] | Broad (>4.5 logs) [49] | Limited (typically 2-3 logs) |
| Sample Volume | Small (as little as 25 μL) [53] | Moderate to large | Large |
| Background Signal | Lowest (decoupled stimulation and detection) [50] | Moderate | Moderate to high |
| Throughput | High | Highest | Low to moderate |
| Best Application | Low-abundance biomarkers, clinical samples with limited volume | Large-scale exploratory studies with broad panels | Single-analyte measurements with sufficient sample |
Experimental Protocols and Methodologies
Standard MSD Assay Protocol for Cytokine Detection
The experimental methodology for MSD-based cytokine detection follows a standardized procedure that leverages the platform's unique characteristics. A typical protocol begins with plate preparation, where MSD multi-spot plates are coated with capture antibodies specific to target cytokines [51]. Following overnight coating at 4°C or 1-2 hours at room temperature, plates are blocked with blocking buffers to minimize non-specific binding. Samples and standards are then added to the plates, with recommended sample volumes typically ranging from 25-50 μL [49] [53]. The plate is incubated with shaking for 2 hours at room temperature or overnight at 4°C for enhanced sensitivity [49].
After sample incubation and washing, a detection antibody solution containing SULFO-TAG labeled antibodies is added and incubated for an additional 1-2 hours [51]. Following final washes, Read Buffer containing tripropylamine is added to the plates, which are then immediately read on an MSD instrument [51]. The instrument applies an electrical current to the plate electrodes, triggering light emission from SULFO-TAG labels in proximity to the electrodes. The emitted light is detected and quantified, with signal intensity directly proportional to the amount of captured analyte [51].
Key Research Reagent Solutions
Table 3: Essential Research Reagents for MSD Electrochemiluminescence Assays
| Reagent / Material | Function | Application Example |
|---|---|---|
| SULFO-TAG Label | Ruthenium-based label that emits light upon electrochemical stimulation | Signal generation for all MSD assays [50] [51] |
| Carbon Electrode Plates | Solid matrix with high binding capacity for biomolecule immobilization | MULTI-ARRAY and MULTI-SPOT plates for assay setup [50] |
| Read Buffer | Contains tripropylamine co-reactant essential for ECL reaction | Final step before plate reading to enable light emission [51] |
| Assay Diluent | Matrix for reconstituting standards and diluting samples | Iron Horse Assay Diluent used in TDP-43 assay development [51] |
| Capture Antibodies | Target-specific antibodies immobilized on electrode surface | TDP-43 Rabbit Polyclonal antibody for neurodegenerative biomarker assays [51] |
| Detection Antibodies | Target-specific antibodies conjugated to SULFO-TAG or recognized by SULFO-TAG secondary | Human TDP-43/TARDBP Mouse monoclonal antibody for sandwich immunoassay [51] |
Applications in Biomedical Research
The combination of high sensitivity and broad dynamic range makes the MSD platform particularly valuable for detecting low-abundance biomarkers in complex biological matrices. In neurodegenerative disease research, MSD-based assays have been developed for proteins like neurofilament heavy chain (NfH) and TDP-43, demonstrating superior sensitivity and smaller sample volume requirements compared to conventional ELISA methods [52] [51]. For example, the MSD NfH assay showed enhanced performance with a broad dynamic range while requiring only 25 μL of cerebrospinal fluid, approximately half the volume needed for traditional ELISA [52].
In metabolic research, a novel MSD-based sandwich immunoassay for glucagon demonstrated exceptional sensitivity with a detection range of 0.14 pmol/L to 1950 pmol/L, significantly outperforming existing methods for this clinically important hormone [54]. The assay showed excellent specificity, distinguishing glucagon from closely related peptides like oxyntomodulin, which is crucial for accurate physiological assessment [54].
The platform's performance has also been validated in large-scale studies. A multisite comparison of high-sensitivity multiplex cytokine assays found that while absolute cytokine concentrations differed across testing platforms, MSD assays generally detected similar patterns of cytokine perturbation during primary HIV viremia, suggesting utility for longitudinal studies where relative changes in cytokines are important [14].
The MSD electrochemiluminescence platform demonstrates distinct advantages in sensitivity and dynamic range compared to alternative cytokine detection methods. These performance characteristics stem from its fundamental detection mechanism, which decouples signal stimulation from detection, resulting in lower background and enhanced sensitivity. While the platform offers more limited multiplexing capacity compared to bead-based systems like Luminex, its ability to detect low-abundance analytes across wide concentration ranges makes it particularly valuable for applications where sample volume is limited or analyte concentrations vary substantially. The experimental data from comparative studies supports MSD as the optimal choice for researchers requiring the highest sensitivity and broadest dynamic range, particularly in later-phase clinical studies and biomarker verification where accurate quantification of low-abundance cytokines is essential for robust scientific conclusions.
The accurate quantification of protein biomarkers is fundamental to advancing biomedical research, drug development, and clinical diagnostics. For many conditions, particularly neurological disorders, autoimmune diseases, and early-stage cancer, critically important protein biomarkers circulate at exceptionally low concentrations—often in the femtomolar (10â»Â¹âµ) to attomolar (10â»Â¹â¸) range—making them undetectable with conventional immunoassay technologies. Traditional methods like enzyme-linked immunosorbent assays (ELISAs) typically offer sensitivities only down to the picomolar (10â»Â¹Â²) level, creating a significant detection gap for low-abundance proteins. This limitation has spurred the development of digital immunoassays, which aim to achieve single-molecule counting for ultimate sensitivity. Among these, the Single Molecule Array (Simoa) technology has emerged as a revolutionary platform, enabling researchers to detect proteins with up to 1,000-fold greater sensitivity than conventional ELISA. This guide provides an objective comparison of Simoa's performance against other leading immunoassay platforms, supported by experimental data and detailed methodologies, to inform researchers, scientists, and drug development professionals in their technology selection process.
The Fundamental Principle of Digital Detection
Single-molecule immunoassays represent a paradigm shift from analog measurement to digital counting. Traditional immunoassays measure the average signal from millions of molecules in a bulk solution. In contrast, digital immunoassays isolate individual immunocomplexes into separate containers, allowing for the precise counting of single molecules. This transition from measuring a continuous signal to counting discrete events dramatically improves sensitivity and reduces background noise. These methods can be broadly categorized into in situ assays, which generate and detect immune complexes in a predetermined fixed area, and random assignment assays, which randomly assign immune complexes to designated detection areas. Random assignment methods, including microarray-based (e.g., Simoa) and microdroplet-based techniques, are more suitable for widespread clinical application due to their automation and throughput [55].
Simoa Technology: How It Works
The Simoa platform, commercialized by Quanterix, utilizes microarray technology with thousands of femtoliter-sized wells (approximately 40 fL volume) inscribed on a millimeter-sized chip. The assay follows a sandwich ELISA principle but with a critical enhancement: magnetic beads coated with capture antibodies form immunocomplexes with the target analyte and an enzyme-labeled detector antibody. These beads are then resuspended in a enzymatic substrate solution and loaded onto the chip, where they are randomly distributed into the microwells. A proprietary sealing oil traps individual beads in their respective wells. If a bead contains a target molecule, the enzyme converts the substrate into a fluorescent product that accumulates within the confined well, creating a bright fluorescent signal detectable by a high-resolution fluorescence microscope. The system then digitally counts the ratio of fluorescent ("on") wells to total wells to determine the original analyte concentration [55]. This process allows Simoa to achieve a typical sensitivity of 10â»Â¹â¸ mol/L, making it the first single-molecule immunoassay technology to be fully automated and commercialized [55].
Alternative Digital Platforms
While Simoa is a well-established commercial platform, other digital approaches are also emerging. Droplet Digital ELISA represents a further evolution, using droplet microfluidics to achieve even greater sensitivity. One study reported this approach as being up to 25-fold more sensitive than Simoa, detecting proteins in the low attomolar range [56]. However, this technology is less mature and not yet as widely automated or commercialized for routine use. Another alternative, the Ella automated immunoassay (ProteinSimple, Bio-techne), is a cartridge-based microfluidic system designed for automated and high-throughput quantification [57]. It is important to note that these platforms, while all aiming for high sensitivity, employ different technological principles, which leads to measurable differences in their performance characteristics, as detailed in the following sections.
Comparative Performance Analysis
Sensitivity and Limit of Detection
The primary advantage of Simoa is its exceptional sensitivity, which enables the detection of previously unmeasurable biomarkers. For instance, in the detection of interferon-alpha (IFN-α), a key cytokine in autoimmune diseases, a Simoa-based assay demonstrated a 5,000-fold increase in sensitivity compared to a commercial ELISA [58]. The lower limit of detection for IFN-α using Simoa can be as low as 0.0035 pg/mL, making it possible to quantify this cytokine even in healthy individuals [59]. This level of sensitivity is crucial for studying diseases like systemic lupus erythematosus (SLE) and dermatomyositis, where IFN-α plays a pathogenic role but circulates at ultralow levels.
Table 1: Comparison of Detection Limits for Key Biomarkers Across Platforms
| Biomarker | Simoa (LoD) | Ella (LoD) | MSD HPE (LoD) | CBA (LoD) | Clinical Significance |
|---|---|---|---|---|---|
| IFN-α | 0.0035 pg/mL [59] | Information Missing | Information Missing | Information Missing | Autoimmunity (SLE, Dermatomyositis) |
| IFN-γ | 0.026 pg/mL [59] | Information Missing | Information Missing | Information Missing | Viral defense, Autoimmunity |
| Neurofilament Light Chain (NfL) | Information Missing | Information Missing | Information Missing | Information Missing | Neuroaxonal injury (MS, Alzheimer's) |
| P-tau181 (Plasma) | Information Missing | Information Missing | Information Missing | Information Missing | Alzheimer's Disease Pathology |
| Abbreviations: LoD (Limit of Detection), MSD HPE (Meso Scale Discovery High-Performance Electrochemiluminescence), CBA (Cytometric Bead Array). |
Platform Concordance and Absolute Quantification
Direct comparison studies reveal that while different high-sensitivity platforms can effectively distinguish clinical groups, their absolute concentration measurements are not directly interchangeable. A landmark study comparing Simoa and Ella for measuring serum Neurofilament Light Chain (NfL) in hereditary amyloidosis patients found a strong positive correlation between the two methods (r = 0.8, p < 0.001). However, the Ella platform consistently overestimated NfL concentrations by 42% compared to Simoa. The median NfL concentration was 27.5 pg/mL on Ella versus 15.9 pg/mL on Simoa. Bland-Altman analysis confirmed a mean bias of 15.4 pg/mL, with the overestimation being more pronounced at higher concentrations [57].
Similarly, a comparison of Simoa and Meso Scale Discovery (MSD) HPE for cytokine measurement in plasma showed comparable detectability for most analytes, but Simoa yielded higher absolute concentrations for IL-10, IL-6, and TNFα. The correlation for the same cytokine measured across both platforms varied from small to moderate (r = 0.26 for IL-10 to r = 0.64 for IL-6), indicating that a significant portion of the variance is platform-specific [60]. These findings underscore a critical point for researchers: absolute concentrations derived from one platform cannot be directly applied to reference intervals established by another.
Clinical Discrimination Power
Despite differences in absolute quantification, all high-sensitivity platforms demonstrate robust power to distinguish between clinical populations, which is their primary utility in research and diagnostics.
- Neurodegenerative Disease: Both Simoa and Ella platforms effectively differentiated between presymptomatic and symptomatic patients with hereditary amyloidosis (p < 0.001 for both), despite the absolute concentration differences [57].
- Alzheimer's Disease: The Cytometric Bead Array (CBA) method, a more accessible and less expensive bead-based immunoassay, showed excellent performance for plasma P-tau181. It differentiated amyloid-positive from amyloid-negative cognitively impaired patients with an Area Under the Curve (AUC) in Receiver Operating Characteristic (ROC) analysis, demonstrating its potential as a cost-effective alternative for specific biomarkers [61].
- Autoimmune Myopathies: Simoa-enabled IFN-α measurement served as a reliable biomarker of disease activity in dermatomyositis. Patients with active disease had significantly higher median IFN-α levels (0.49 pg/mL) than non-active patients (0.03 pg/mL), with an AUC of 0.90, indicating outstanding diagnostic accuracy [59].
Table 2: Platform Performance in Different Disease Contexts
| Platform | Biomarker | Clinical Context | Key Performance Finding |
|---|---|---|---|
| Simoa | IFN-α | Dermatomyositis Activity | AUC = 0.90 for distinguishing active vs. non-active disease [59]. |
| Simoa vs. Ella | NfL | ATTRv Amyloidosis (Symptomatic vs. Presymptomatic) | Both effective (p < 0.001), but Ella overestimated concentrations by 42% [57]. |
| CBA | P-tau181 | Alzheimer's Disease (Aβ+ vs. Aβ- CI) | Showed excellent performance in differentiating groups [61]. |
| Simoa vs. MSD HPE | IL-6, TNFα, IL-10 | Healthy Aging | Showed similar patterns of association with vascular/brain health, despite concentration differences [60]. |
Detailed Experimental Protocols
Protocol: Comparative Analysis of Simoa and Ella for Serum NfL
This protocol is based on the study by Gagliardi et al. (2025) that directly compared the two platforms [57].
1. Sample Collection and Preparation:
- Collect peripheral blood in additive-free vacutainers with a separating gel.
- Centrifuge samples at 3,000 rpm for 10 minutes at room temperature to separate serum.
- Aliquot the serum into sterile polypropylene tubes and store at -80°C until analysis.
2. Simoa Assay Execution:
- Use the commercial NF-Light Advantage Kit (Quanterix) on a semi-automated SR-X Biomarker Detection System.
- Dilute samples 1:4 and load them randomly onto 96-well plates.
- Include kit-provided quality control (QC) samples on each plate. Maintain the inter-plate coefficient of variance (CV) below 10%.
- The lower limit of detection (LLoD) for Simoa NfL is 0.071 pg/mL, with an upper limit of 2,000 pg/mL.
3. Ella Assay Execution:
- Use the Simple Plex cartridge-based assay on the Ella platform (ProteinSimple).
- Dilute samples 1:2, according to the manufacturer's instructions.
- The Ella cartridge contains an internal factory-standard curve for calibration.
- The LLoD for Ella NfL is 1.09 pg/mL, with an upper limit of 10,290 pg/mL.
4. Data and Statistical Analysis:
- Compare NfL concentrations from both methods using the Wilcoxon signed-rank test.
- Assess correlation using the Spearman correlation coefficient.
- Evaluate agreement and bias using Bland-Altman analysis and Passing-Bablok regression.
Protocol: Simoa-based IFN-α Measurement in Dermatomyositis
This protocol is adapted from the study by Roubille et al. (2025) [59].
1. Patient Cohort and Serum Isolation:
- Enroll patients meeting classification criteria for idiopathic inflammatory myopathies (IIM). Exclude patients who received high-dose corticosteroids (>0.5 mg/kg) within one week prior to sampling, as this can rapidly reduce IFN levels.
- Collect blood samples and separate serum by centrifugation within 3 hours of draw.
- Freeze serum aliquots rapidly at -80°C, ensuring they are thawed only once before analysis to prevent protein degradation.
2. Simoa Immunoassay:
- Use the Quanterix Simoa IFN-α Reagent Kit on the HD-X Analyzer.
- A volume of 400 µL of serum per well is required for the analysis.
- The established limit of detection (LOD) for this assay is 0.0035 pg/mL.
- Define a positivity threshold based on the mean plus three standard deviations of measurements from healthy donor controls (e.g., 0.22 pg/mL).
3. Clinical Correlation:
- Clinicians assess disease activity at the time of blood collection using standardized tools like the Physician Global Activity (PGA) score and Manual Muscle Testing (MMT8).
- Perform statistical analyses (e.g., Spearman's rank correlation) to correlate serum IFN-α levels with clinical disease activity scores.
- Generate ROC curves to evaluate the biomarker's power to distinguish active from non-active disease.
Signaling Pathways and Workflow Visualization
The following diagram illustrates the core technological workflow of the Simoa platform, from sample to digital result.
Simoa Digital ELISA Workflow
The pathological role of cytokines like IFN-α, which are detectable by Simoa, can be understood within the broader context of the interferon signaling pathway, as shown below.
The Scientist's Toolkit: Essential Research Reagents
For researchers aiming to implement or understand these ultra-sensitive assays, the following table details key reagents and their functions.
Table 3: Key Reagents for Ultra-Sensitive Immunoassays
| Reagent / Solution | Critical Function | Technical Notes |
|---|---|---|
| Capture Antibody-Bead Conjugates | Immobilizes the target analyte from the sample. | High affinity and specificity are paramount. Beads are magnetic for washing and manipulation (Simoa) [55]. |
| Biotinylated Detection Antibody | Binds to a different epitope on the captured analyte, enabling detection. | Streptavidin-enzyme conjugates (e.g., Streptavidin-β-galactosidase in Simoa) subsequently bind to the biotin [55]. |
| Enzyme Substrate (Fluorogenic) | Converted by the enzyme label into a fluorescent product for signal generation. | Must generate a stable, bright fluorescent signal upon enzymatic conversion (e.g., Resorufin β-D-galactopyranoside for β-gal) [55]. |
| Sealing Oil | Traps single beads in femtoliter wells, creating isolated reaction chambers. | This confinement is key to digital detection, allowing fluorescent product accumulation [55]. |
| Assay-Specific Calibrators | A series of solutions with known analyte concentrations. | Used to generate the standard curve for interpolating sample concentrations. Quality is critical for accuracy. |
| Quality Control (QC) Samples | Monitor assay precision, accuracy, and reproducibility across runs. | Should be run at low, medium, and high concentrations within the assay's dynamic range [57]. |
| Pocapavir | Pocapavir, CAS:146949-21-5, MF:C21H17Cl3O3, MW:423.7 g/mol | Chemical Reagent |
| Poloppin | Poloppin, MF:C20H15BrF3NO2, MW:438.2 g/mol | Chemical Reagent |
Digital immunoassays, with Simoa at the forefront, have irrevocably changed the landscape of protein biomarker detection by providing single-molecule sensitivity. The experimental data clearly shows that while platforms like Simoa, Ella, and MSD HPE are all capable of robustly distinguishing clinical states, their absolute quantitative results are not directly interchangeable. This underscores the necessity for researchers to consider platform-specific reference ranges and to maintain methodological consistency within longitudinal studies.
Future developments in the field are likely to focus on several key areas: achieving even higher levels of multiplexing to conserve valuable samples, further reducing costs to enable wider adoption, standardizing measurements across platforms to allow for data pooling and meta-analyses, and developing more point-of-care-friendly formats based on microdroplet technologies. As these technologies continue to evolve and mature, their role in validating novel biomarkers for early disease diagnosis, monitoring treatment efficacy, and stratifying patient populations will become increasingly central to both biomedical research and clinical diagnostics.
The selection of an appropriate cytokine detection method is a critical decision that directly influences data quality, interpretability, and ultimately, research conclusions. This guide provides a systematic comparison of current technologies based on quantifiable performance metrics, experimental data, and application-specific considerations to enable informed method selection aligned with research objectives and sample constraints.
Table 1: Core Performance Metrics of Major Cytokine Detection Platforms
| Technology | Sensitivity (Typical LOD) | Dynamic Range | Sample Volume per Panel | Multiplexing Capacity | Key Strengths |
|---|---|---|---|---|---|
| Digital ELISA (Simoa) | Femtogram/mL range (e.g., single-digit fg/mL for IL-17A) [8] | 3-4 logs [8] | ~50 μL for multiplex [8] | Low to moderate (e.g., 4-plex panels) [8] | Ultra-sensitive detection for low-abundance cytokines; robust in complex matrices [8] |
| Proximity Extension Assay (Olink) | Low pg/mL possible [28] | Not specified | ~1 μL [28] | High (e.g., 48-plex panels) [28] | High specificity with minimal sample requirement; excellent performance in overlapping analytes [28] |
| Electrochemiluminescence (MSD) | Superior sensitivity at low end [13] [28] | Broadest dynamic range [13] | 20-40 μL [28] | Moderate (e.g., 10-plex) [28] | Excellent sensitivity and broad dynamic range; reliable for medium to low abundance cytokines [13] [28] |
| Bead-Based Multiplex (Luminex) | Picogram/mL range [28] | Not specified | ~12.5-60 μL [28] | High (e.g., 20-80 plex) [28] | Good for profiling many cytokines simultaneously; widely available and understood [28] |
| Traditional ELISA | Picogram/mL range [5] [28] | Limited [28] | Higher volume per analyte [28] | Single-analyte or limited multiplex [28] | High specificity per analyte; widely available and validated; lower technical complexity [5] [28] |
| Digital PLA (dPLA) | Femtomolar (e.g., 0.73 fM for IL-6) [62] | 5 orders of magnitude [62] | Not specified | Compatible with protein and nucleic acid targets [62] | Ultrasensitive simultaneous measurement of proteins and bacterial DNA; single-molecule resolution [62] |
| Microfluidic ELISA (ELLA) | Sub-picogram [20] | 4-5 log10 [20] | Not specified | Moderate multiplexing [20] | Rapid, precise measurement with minimal user intervention; reduced bias [20] |
Technology-Specific Experimental Protocols and Validation
Digital Immunoassays (Simoa)
Experimental Protocol for IL-17A Validation [8]:
- Platform: Simoa HD-X Analyzer with Cytokine Advantage PLUS kits
- Sample Preparation: Serum samples validated for matrix effects
- Assay Procedure: Single-plex or multiplex (e.g., IL-6, IL-8, IL-10, TNF-α) assays run on a single instrument
- Validation Metrics:
- Precision: Intra- and inter-assay CVs <10%
- Recovery tests: Spike-and-recovery and dilution linearity assessments
- Limit of Detection: Single-digit femtogram/mL range achieved
- Throughput: Up to 288 samples per day [8]
Proximity Extension Assay (Olink)
Experimental Workflow [28]:
- Principle: Dual antibody-DNA oligonucleotide binding to target protein followed by hybridization, polymerase extension, and qPCR/NGS readout
- Sample Input: 1μL of sample per panel
- Data Output: Normalized Protein Expression (NPX) values
- Cross-Platform Validation: In the IMPACC COVID-19 cohort, Olink showed higher detectability than Luminex for many shared targets, though some low-abundance cytokines (IL-2, IL-4, IL-10, IL-13) were poorly correlated across platforms [28]
Flow Cytometry-Based Multiplex Assay
One-Step Protocol Development [21]:
- Innovation: Lyophilized capture-antibody-modified beads and PE-labeled detection antibodies premixed
- Procedure: 100μL sample added to lyophilized reagent beads, incubated 1.5 hours with shaking, washed, and analyzed on flow cytometer
- Lyophilization Optimization: Three buffer formulations tested, with PBS containing 0.1% BSA, 5% mannitol, and 3% trehalose proving optimal
- Validation: Applied to COVID-19 and HBV patient sera with machine learning models to predict disease severity and viral load [21]
Digital Proximity Ligation Assay (dPLA)
Experimental Design for Septic Shock Monitoring [62]:
- Targets: IL-6, TNF-α proteins combined with GN/GP bacterial 16S rRNA genes and blaTEM resistance gene
- Methodology: Combines droplet digital PCR with proximity ligation assay
- Sensitivity Achieved: 0.02 pg/mL (0.73 fM) for IL-6 and 0.08 pg/mL (4.33 fM) for TNF-α in BALF samples
- Clinical Application: Longitudinal plasma analysis from septic shock patients revealed association between IL-6 dynamics and patient outcomes [62]
Method Selection Framework
Decision Workflow
Application-Specific Recommendations
Drug Discovery and Development
Recommended Platform: MSD or Simoa [63] [8]
- Rationale: MSD provides the broadest dynamic range essential for pharmacokinetic studies, while Simoa offers the sensitivity required for early biomarker detection in clinical trials [13] [8]
- Supporting Data: Frontage Laboratories validated Simoa for clinical phase I-III studies, demonstrating precision (CVs <10%) sufficient for regulatory submissions [8]
Clinical Diagnostics and Patient Stratification
Recommended Platform: Multiplex platforms (Luminex, Olink) or functional assays (ELISpot/ELLA) [20]
- Rationale: Balance between comprehensive profiling and practical implementation
- Supporting Data: ELLA demonstrated superior precision (4-5 log10 dynamic range) compared to ELISpot (2 log10) for functional immune phenotyping in sepsis [20]
Basic Immune Research with Limited Sample
Recommended Platform: Olink or flow cytometry-based multiplex [21] [28]
- Rationale: Minimal sample requirements (1μL for Olink) with high multiplex capability
- Supporting Data: Olink provided reliable detection using ~1μL sample volume versus 12.5μL for Luminex and 20-40μL for MSD [28]
Infectious Disease and Sepsis Biomarker Discovery
Recommended Platform: Digital PLA or Simoa [62] [8]
- Rationale: Unparalleled sensitivity for detecting early cytokine shifts and correlating with bacterial load
- Supporting Data: dPLA enabled prediction of septic shock outcomes with >90% accuracy by tracking IL-6 and bacterial DNA dynamics [62]
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Reagents and Materials for Cytokine Detection Workflows
| Reagent/Material | Function/Purpose | Application Examples | Technical Considerations |
|---|---|---|---|
| Matched Antibody Pairs | Capture and detection of specific cytokines | ELISA, Luminex, MSD platforms [5] | Require checkerboard titration for optimal concentrations [5] |
| Carboxylated Fluorescent Microspheres | Bead-based analyte discrimination | Luminex, flow cytometry multiplex assays [21] | Coupled via EDC/sulfo-NHS chemistry; spectral encoding enables multiplexing [21] |
| Lyophilization Stabilizers | Preserve reagent stability without cold storage | Trehalose (5%), mannitol (5%) in PBS with BSA (0.1%) [21] | Enables single-step assays and simplifies reagent transport [21] |
| DNA-Oligo Conjugated Antibodies | Proximity-based detection with nucleic acid amplification | Olink PEA, digital PLA [62] [28] | Enables high specificity through dual recognition and PCR amplification [28] |
| Electrochemiluminescent Tags | Signal generation in applied electric fields | MSD platforms [13] [28] | Provides low background and enhanced sensitivity compared to colorimetric detection [13] |
| Blocking Buffers | Prevent non-specific binding | All solid-phase immunoassays [5] | Various formulations: BSA, Blotto, Casein, Superblock; require optimization [5] |
| Poloxin | Poloxin|PLK1 PBD Inhibitor|CAS 321688-88-4 | Poloxin is a polo-like kinase 1 (PLK1) Polo-Box Domain (PBD) inhibitor (IC50 = 4.8 µM). For research use only. Not for human or veterinary use. | Bench Chemicals |
| N-Methylparoxetine | N-Methylparoxetine, CAS:110429-36-2, MF:C20H22FNO3, MW:343.4 g/mol | Chemical Reagent | Bench Chemicals |
Emerging Technologies and Future Directions
The cytokine detection landscape is evolving toward higher sensitivity, greater multiplex capability, and computational integration. Ultra-sensitive platforms like Simoa and digital PLA are pushing detection limits to the femtomolar range, enabling measurement of previously undetectable low-abundance cytokines [62] [8]. Simultaneously, integration with machine learning approaches, as demonstrated in COVID-19 and HBV studies, enhances the predictive power of cytokine profiles for disease outcomes [21].
The market is concurrently shifting toward point-of-care testing formats and automated systems that reduce operator-dependent variability, addressing a key limitation of traditional methods like ELISpot that showed up to 35-fold inter-laboratory variation [20]. As these technologies mature, researchers should consider both current performance metrics and platform scalability for their specific application needs.
Optimizing Cytokine Measurements: Overcoming Pre-analytical and Analytical Challenges
In the field of cytokine research, particularly within sensitivity comparisons of detection methodologies, the integrity of experimental data is heavily dependent on robust sample collection and processing protocols. Pre-analytical variables represent the most significant source of variability in biomarker measurements, often surpassing technical differences between assay platforms themselves [64]. These variables—encompassing sample collection, processing, and storage conditions—can profoundly alter the measurable concentration of cytokines, potentially leading to erroneous conclusions in both basic research and clinical drug development.
The critical importance of standardizing these pre-analytical factors is magnified when comparisons are made across different detection technologies, such as enzyme-linked immunosorbent assay (ELISA), multiplex arrays, and electrochemiluminescence-based platforms. A cytokine profile that appears differentially expressed between patient cohorts or experimental conditions may simply reflect inconsistencies in sample handling rather than true biological variation. Therefore, a comprehensive understanding and control of these variables is not merely a procedural formality but a fundamental prerequisite for generating reliable, reproducible, and biologically meaningful data in cytokine research.
Key Pre-analytical Variables and Their Effects
Experimental data from controlled studies reveal that specific pre-analytical handling steps can significantly alter measured cytokine levels. The following variables are among the most critical to control.
Blood Collection Tube Type
The choice of anticoagulant or blood collection media is a primary decision that systematically influences cytokine measurements. A 2021 study investigating COVID-19-relevant cytokines found that different tube types resulted in significantly different blood cytokine levels [65]. While the exact magnitude of effect is cytokine-dependent, this underscores that absolute cytokine concentrations cannot be directly compared when measured from different sample types, such as serum versus plasma or plasma with different anticoagulants.
Time to Centrifugation
The delay between blood collection and plasma separation is a well-documented source of variability. Holding EDTA plasma tubes at room temperature for 3 hours before centrifugation led to declining levels of IL-17A and IL-6 [65]. This degradation or consumption of cytokines over time in unprocessed whole blood necessitates a standardized and minimized processing window to ensure accurate quantification.
Sample Storage Delays and Freeze-Thaw Cycles
Stability studies indicate that cytokines vary in their susceptibility to storage conditions. For instance, IFN-γ levels declined when plasma samples were stored at room temperature for 24 hours after centrifugation [65]. Furthermore, IL-17A levels were sensitive to storage delays, showing declines after a 2-week storage period at higher temperatures [65]. Repeated freeze-thaw cycles are another major concern, as they can lead to irreversible cytokine degradation or aggregation, thereby lowering apparent concentrations.
Table 1: Summary of Pre-analytical Variable Effects on Specific Cytokines
| Pre-analytical Variable | Affected Cytokines | Observed Effect | Citation |
|---|---|---|---|
| Collection Tube Type | Multiple cytokines (e.g., IL-6, IFN-γ, TNF-α) | Significant differences in absolute measured levels | [65] |
| Centrifugation Delay (3h at RT) | IL-6, IL-17A | Decline in measured concentration | [65] |
| Post-Centrifugation Storage Delay (24h at RT) | IFN-γ | Decline in measured concentration | [65] |
| Extended Storage (2 weeks) | IL-17A | Decline in measured concentration | [65] |
Comparative Analysis of Cytokine Detection Technologies
Understanding pre-analytical variables is essential for a fair comparison of the performance of different cytokine detection methods. Each platform possesses unique strengths and limitations in sensitivity, dynamic range, and multiplexing capability, which must be matched to the research objective.
The journey from a biological sample to a quantitated cytokine profile involves a standardized workflow, regardless of the detection technology chosen. The initial, critical steps are the pre-analytical phase, which directly impacts the quality of the input material for any downstream assay.
Performance Comparison of Major Platforms
ELISA (Enzyme-Linked Immunosorbent Assay): As the traditional gold standard, ELISA provides high specificity and good sensitivity for a single analyte. However, it is limited by moderate throughput, a dynamic range of typically 2-3 logs, and a relatively high sample volume consumption of 100–200 μL per test [15] [25]. Its single-plex nature makes it inefficient for comprehensive immune profiling.
Luminex xMAP Technology: This bead-based multiplex array allows for the simultaneous measurement of dozens to hundreds of analytes from a single small sample volume (25–50 μL) [14] [25]. It offers high throughput, a broad dynamic range (3–5 logs), and good sensitivity, making it a powerful tool for discovery research. However, it can be sensitive to interfering substances in serum/plasma and requires careful validation to manage potential cross-reactivity [15] [14].
Meso Scale Discovery (MSD): Utilizing electrochemiluminescence detection, MSD platforms are often noted for their excellent sensitivity and very broad dynamic range, which can minimize the need for sample re-runs [13] [25]. MSD assays also require small sample volumes and have a good multiplexing capacity (e.g., up to 10-plex per well). A comparative analysis highlighted MSD as having the best sensitivity in the low detection limit and the broadest dynamic range among commonly used technologies [13].
Simoa (Single Molecule Array): An emerging technology, Simoa provides exceptional sensitivity, capable of detecting cytokines in the femtogram per milliliter range. This makes it suitable for measuring very low-abundance cytokines that are undetectable by other methods [65].
Table 2: Technical Comparison of Cytokine Detection Methods
| Feature | ELISA | Luminex xMAP | Meso Scale Discovery (MSD) | Simoa |
|---|---|---|---|---|
| Multiplexing | Single-plex | High (up to 500-plex) | Medium (up to ~10-plex per well) | Low to Medium |
| Sensitivity | Good (Low pg/mL) | Good to Excellent (Low pg/mL to fg/mL) | Excellent (Broadest dynamic range) | Highest (fg/mL range) |
| Sample Volume | High (100–200 μL) | Low (25–50 μL) | Low | Low |
| Throughput | Moderate | High | High | Moderate |
| Dynamic Range | 2-3 logs | 3-5 logs | >5 logs | 3-4 logs |
| Best For | Validating specific targets | Discovery, large-scale profiling | Sensitive quantitation, kinetic studies | Ultra-low abundance targets |
Experimental Protocols for Validating Pre-analytical Variables
To establish a reliable standard operating procedure (SOP) for a specific research context, it is necessary to empirically determine the impact of pre-analytical variables on the cytokines and detection platform of choice. The following protocol, adapted from a 2021 stability study, provides a template for such an investigation [65].
Protocol: Evaluating Centrifugation Delay and Storage Stability
Objective: To determine the effect of pre-centrifugation delay and short-term storage temperature on the stability of a panel of cytokines in plasma.
Materials:
- Kâ‚‚EDTA blood collection tubes.
- Centrifuge capable of 1800× g.
- Freezer at -80°C.
- Aliquoting tubes.
- Validated cytokine detection platform (e.g., Simoa, MSD, or Luminex).
Method:
- Sample Collection: Collect venous blood from consented donors into Kâ‚‚EDTA tubes.
- Pre-centrifugation Delay (Variable): Divide tubes into groups and hold at room temperature for different time intervals: 30 minutes (reference), 1 hour, 3 hours, and 24 hours.
- Centrifugation: Centrifuge all tubes at 1800× g for 10 minutes at room temperature to obtain plasma.
- Aliquot and Storage (Variable): Immediately aliquot plasma into polypropylene tubes. For the storage variable, create subgroups: aliquots stored immediately at -80°C (reference), stored at 2-8°C for 24 hours, or held at room temperature for 24 hours before final storage at -80°C.
- Analysis: Measure cytokine concentrations (e.g., IFN-γ, IL-6, IL-10, TNF-α, IL-17A) in all samples in a single batch to minimize inter-assay variability.
- Data Analysis: Normalize cytokine levels in experimental conditions to the reference condition (30 min delay, immediate -80°C storage). A change of ≥15% from the reference is often considered biologically significant in such stability studies [65].
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table details key materials and reagents essential for conducting rigorous cytokine analysis, with a focus on mitigating pre-analytical variability.
Table 3: Essential Reagents and Materials for Cytokine Analysis
| Item | Function/Description | Critical Considerations |
|---|---|---|
| Kâ‚‚EDTA Tubes | Standard tube for plasma collection; binds calcium to prevent clotting. | Often used as a reference anticoagulant in validation studies. Consistency in brand and lot is key. |
| Serum Separator Tubes | Tubes containing a gel that separates serum from clotted blood after centrifugation. | Serum and plasma cytokine levels are not directly comparable [15]. |
| Polypropylene Storage Tubes | For aliquoting and long-term storage of samples. | Polypropylene is preferred over other plastics as it minimizes analyte adhesion. |
| Validated Cytokine Panel | A pre-configured multiplex panel for a specific platform (e.g., Luminex, MSD). | Use panels that provide data on cross-reactivity. For absolute quantitation, ensure the standard curve is matrix-matched. |
| Cytokine Standards | Calibrators of known concentration used to generate a standard curve. | Standards provided by kit manufacturers may yield different absolute concentrations than international standards [14]. |
| Assay Diluent | Matrix used to dilute samples and standards. | Should mimic the biological sample matrix (e.g., serum, plasma) to minimize matrix effects and ensure accuracy. |
| PP121 | PP121, CAS:1092788-83-4, MF:C17H17N7, MW:319.4 g/mol | Chemical Reagent |
| Prenylamine Lactate | Prenylamine Lactate, CAS:69-43-2, MF:C27H33NO3, MW:419.6 g/mol | Chemical Reagent |
In the context of comparing cytokine detection method sensitivities, the data generated is only as reliable as the sample from which it was derived. As evidenced by numerous studies, pre-analytical variables such as collection tube type, processing delays, and storage conditions exert a profound influence on measured cytokine levels, an effect that can easily obscure or exaggerate the performance differences between technological platforms. Therefore, the path to robust and comparable data requires the implementation of standardized, well-validated SOPs for sample handling that are tailored to the specific cytokines and assays of interest. By rigorously controlling the pre-analytical phase, researchers can ensure that the sensitivity, dynamic range, and multiplexing capabilities of modern detection technologies are leveraged to reveal true biological signals, not procedural artifacts.
For researchers and drug development professionals, the choice between serum and plasma is a critical pre-analytical variable that can fundamentally impact the reliability and interpretation of cytokine data. Serum and plasma, while both derived from blood, are distinct matrices with different protein compositions and properties. Plasma is the liquid portion of blood that remains when clotting is prevented through the use of anticoagulants, preserving the full complement of proteins, including clotting factors. In contrast, serum is the fluid obtained after blood has clotted, a process that depletes clotting factors like fibrinogen but may also lead to the release of additional cellular components [66].
Understanding the effects of these matrices is essential within the broader context of comparing the sensitivity of cytokine detection methods. The matrix effect—how the sample background inhibits or enhances the detection of target analytes—can vary significantly between serum and plasma, influencing assay sensitivity, dynamic range, and ultimately, the accuracy of measured cytokine concentrations [10]. This guide provides an objective comparison of serum and plasma performance, supported by experimental data, to inform robust experimental design in biomarker discovery and clinical research.
Fundamental Differences Between Serum and Plasma
The core distinction between serum and plasma lies in the presence or absence of the clotting process. This fundamental difference impacts not only composition but also sample handling, stability, and suitability for different analytical goals.
Compositional and Handling Differences
The table below summarizes the key practical differences between these matrices.
| Characteristic | Plasma | Serum |
|---|---|---|
| Composition | Contains all blood proteins, including clotting factors (e.g., fibrinogen) [66]. | Lacks clotting factors consumed in the clot; may have proteins released from platelets [66]. |
| Preparation Method | Blood drawn into anticoagulant tube, mixed, and centrifuged. Quick preparation [66]. | Blood drawn into plain tube, allowed to clot (~30 mins), then centrifuged. Slower process [66]. |
| Key Handling Considerations | Less pre-analytical variability due to immediate processing [66]. | Clotting time and temperature must be standardized to avoid variability [66]. |
| Inherent Matrix Effects | Generally exhibits lower non-specific background in immunoassays [10]. | Typically has higher non-specific background, potentially masking low-abundance cytokines [10]. |
Impact of the Clotting Process
The act of clotting does not merely remove proteins; it can actively alter the proteome. During clot formation, platelets and other blood cells become activated and release various factors into the serum. A prominent example is Vascular Endothelial Growth Factor (VEGF), which one source notes can be nearly six-fold higher in serum than in plasma from the same donor due to platelet degranulation [66]. This means that for certain analytes, serum levels may reflect a combination of in vivo circulation and ex vivo release, potentially confounding biological interpretation. A study on extracellular vesicles further confirmed that serum-derived fractions contain more particles enriched with platelet-associated proteins compared to plasma [67].
Comparative Experimental Data: Serum vs. Plasma
Empirical comparisons consistently reveal that the choice of matrix leads to quantifiable differences in measured cytokine levels, with implications for assay sensitivity.
Spike-recovery experiments are a standard method to evaluate matrix effects. One study found that both serum and plasma can inhibit the detection of many cytokines, but serum often causes greater inhibition than plasma [10]. This inhibition means that the measured concentration is lower than the actual concentration, compromising quantitative accuracy. The same study also reported that the non-specific background, a key factor in limiting sensitivity, was "significantly increased in serum versus plasma" [10]. This higher background can obscure the signal of low-abundance cytokines, reducing the effective sensitivity of the assay.
Relative Performance of Serum and Plasma Matrices
The following table summarizes findings from a 72-plex Luminex study that compared serum and different plasma types [68].
| Analytic Category | Representative Cytokines/Chemokines | Observed Difference in Serum vs. Plasma |
|---|---|---|
| Significantly Higher in Serum | PDGF-bb, IL-4, IL-8, IL-9, VEGF, CCL-5 (RANTES), CD40L [68] | Concentrations were markedly elevated in serum regardless of the anticoagulant used for plasma. |
| Variable or Context-Dependent | IL-6, CXCL-8 (IL-8) | One study found IL-6 lower in serum [69], while another found IL-8 higher in serum [68]. |
| More Sensitive Detection in Plasma | Low-abundance cytokines (e.g., IL-10, IL-13) [10] | Disease-related decreases in low-abundance cytokines were sometimes detectable in plasma but not in serum, attributed to lower background [10]. |
A separate study using Olink's PEA technology across 1,463 proteins developed linear models to transform data between serum and plasma, identifying 551 proteins with reproducible transformation factors. This underscores that while relationships exist, a simple conversion factor is not universally applicable and requires rigorous validation [70].
The Influence of Anticoagulants in Plasma
The type of anticoagulant used for plasma collection introduces another layer of variation. Sodium heparin, citrate, and EDTA chelate calcium via different mechanisms, which can affect analyte stability and detection.
| Anticoagulant | Key Findings from Multiplex Studies |
|---|---|
| Sodium Heparin | Often recommended as a good default choice; one study concluded it allowed the best measurements overall for the cytokines assessed [69]. Some analytes (e.g., eotaxin, MCP-1, VEGF) show higher concentrations in heparinized plasma [68]. |
| EDTA | Showed significant differences from heparin for a limited number of cytokines (e.g., IP-10) [68]. |
| Sodium Citrate | Similar to EDTA, with most cytokines showing comparable levels to heparin plasma, but with specific exceptions [68]. |
Detailed Experimental Protocols for Matrix Comparison
To ensure the reliability of cytokine data, researchers must employ standardized and well-optimized experimental protocols. The following sections detail key methodologies cited in the comparative studies.
Sample Collection and Processing Protocols
Standardized processing is vital to minimize pre-analytical variability.
- Serum Processing: Collect blood into red-top (no additive) or serum separator tubes. Incubate at room temperature for at least 30 minutes to allow complete clotting. Centrifuge at 1,200-2,000 RCF for 10 minutes. Aliquot the supernatant (serum) into cryovials and freeze at -80°C [10] [69].
- Plasma Processing: Collect blood into tubes containing an anticoagulant (e.g., sodium heparin, EDTA, citrate). Invert tubes immediately to mix. Centrifuge at a lower force (e.g., 200 RCF for 10 minutes) to remove cells, followed by a higher-speed centrifugation (e.g., 1,000-2,000 RCF for 10 minutes) to pellet any remaining platelets or debris. Aliquot the supernatant (plasma) and freeze at -80°C [10] [69].
Multiplex Immunoassay Protocol (Luminex)
The described protocol is adapted from studies that compared serum and plasma matrices [10].
- Bead Incubation: Mix samples, controls, or standards with antibody-linked magnetic or polystyrene beads in a 96-well filter plate. Incubate for 2 hours at room temperature with shaking, or overnight at 4°C for increased sensitivity.
- Washing: Vacuum filter the plate and wash wells twice with wash buffer to remove unbound proteins.
- Detection Antibody Incubation: Add biotinylated detection antibodies to the beads. Incubate for 1-2 hours at room temperature with shaking.
- Washing: Vacuum filter and wash the plate twice as before.
- Signal Amplification: Add streptavidin-conjugated phycoerythrin (SA-PE) to the beads. Incubate for 30-60 minutes at room temperature with shaking. SA-PE binds to the biotin on the detection antibodies.
- Final Washing and Reading: Perform a final wash, resuspend the beads in a reading buffer, and analyze the plate on a Luminex instrument. The instrument measures the fluorescence of the SA-PE, which is proportional to the amount of captured cytokine [10].
Assay Validation: Spike and Recovery
This critical experiment evaluates matrix-specific interference and is essential for validating any cytokine assay [10] [5].
- Preparation: Create a known concentration of recombinant cytokine standard in a neutral buffer. Prepare a dilution series.
- Spiking: Spike the recombinant cytokine into separate aliquots of the sample matrix (e.g., serum from several donors, heparin plasma, EDTA plasma). Also, prepare the same concentrations of the standard in the assay's dilution buffer to create a "reference" curve.
- Analysis: Run all samples (spiked matrices and reference) in the same assay.
- Calculation: Calculate the percent recovery for each matrix:
- Recovery (%) = (Measured Concentration in Spiked Matrix / Expected Concentration) × 100
- The expected concentration is derived from the reference curve prepared in the buffer.
- Interpretation: Ideally, recovery should be between 80-120%. Consistent recovery outside this range indicates a matrix effect that inhibits or enhances detection, necessitating the use of a matrix-specific standard curve or sample dilution to overcome the interference [10].
The Scientist's Toolkit: Key Research Reagent Solutions
The table below lists essential materials and reagents required for conducting serum and plasma cytokine comparisons, based on the cited methodologies.
| Item | Function & Application | Example from Literature |
|---|---|---|
| Sodium Heparin Tubes | Prevents coagulation for plasma preparation; considered a robust default choice for many cytokine panels [68] [69]. | BD Vacutainer Sodium Heparin tubes (Green top) [10]. |
| Serum Tubes | Contains clot activator for serum preparation. | BD Vacutainer Serum Tubes (Red top) [10]. |
| Multiplex Immunoassay Kits | Enable simultaneous quantification of multiple cytokines from a single, small-volume sample. | Affymetrix 51-plex, EMD Millipore 42-plex, MSD Human Cytokine 30-Plex V-PLEX Kit [10] [71]. |
| Matched Antibody Pairs | Essential for developing in-house (sandwich) ELISAs; consist of a capture and a biotinylated detection antibody [5]. | Monoclonal capture with polyclonal biotinylated detection antibody [5]. |
| Recombinant Cytokine Standards | Used to generate standard curves for quantification and for spike-recovery experiments to assess matrix effects [10] [5]. | Purified recombinant proteins for cytokine standards [5]. |
| Assay Diluent | Buffer used to dilute samples and standards; its composition can partially reverse matrix inhibition [10]. | Commercial diluents from vendors (e.g., Pierce Standard Diluent) [10] [5]. |
Decision Framework and Best Practices
Integrating the experimental data and methodological considerations leads to the following actionable guidance.
Key Recommendations for Researchers
- For Maximizing Sensitivity: Choose plasma, particularly for detecting low-abundance cytokines. Its lower non-specific background makes it a more sensitive matrix for revealing subtle, disease-related changes [10].
- For Specific Analytes: If your targets include platelet-derived factors like VEGF, be aware that serum levels are artificially elevated. Plasma provides a more accurate reflection of in vivo circulating levels [66]. Conversely, for cytokines consumed in clots, serum might be more relevant.
- For Consistency and Biomarker Discovery: Plasma is often preferred for proteomic and biomarker studies due to more controlled processing and a more complete representation of the native blood proteome, as recommended by consortia like the HUPO Plasma Proteome Project [66].
- For Longitudinal and Multi-Site Studies: Standardize the matrix and processing protocol across all collection sites. Never switch matrices mid-study. If comparing across studies that used different matrices, use published transformation factors with caution and validate them for your specific assay [70].
- For Assay Validation: Always perform spike-recovery and linearity-of-dilution experiments in your specific sample matrix (e.g., human heparin plasma) to quantify and account for matrix effects. Do not assume dilution is linear [10] [5].
The accurate quantification of cytokines is fundamental to advancing research in immunology, drug development, and personalized medicine. However, the reliability of these measurements is critically dependent on pre-analytical conditions, particularly the effects of long-term sample storage and repeated freeze-thaw cycles. These factors can induce protein degradation or modification, leading to inaccurate concentration readings that may ultimately compromise research conclusions and clinical decisions. Within the broader context of comparing the sensitivity of cytokine detection methods, understanding and controlling for these sample integrity variables is not merely a procedural detail but a core component of methodological rigor. This guide objectively compares the stability of various cytokines and common clinical chemistry analytes under different storage conditions, providing researchers with a consolidated evidence base to inform their experimental planning and sample handling protocols.
Comparative Stability of Biomarkers
The stability of biomarkers varies significantly depending on the specific analyte, the biological matrix, and the storage conditions. The data below summarize findings from multiple studies on the impact of freeze-thaw cycles and long-term storage.
Table 1: Impact of Multiple Freeze-Thaw Cycles on Biomarker Stability
| Analyte Category | Specific Analyte | Maximum Stable Cycles | Key Findings | Source |
|---|---|---|---|---|
| Clinical Chemistry | ALT, AST, CK, GGT, Direct Bilirubin, Glucose, Creatinine, Cholesterol, Triglycerides, HDL | 10 cycles | Stable after ten freeze-thaw cycles at -20°C. | [72] |
| Clinical Chemistry | Lactate Dehydrogenase (LD), Blood Urea Nitrogen (BUN), Uric Acid, Total Protein, Albumin, Total Bilirubin, Calcium | <10 cycles | Showed statistically and clinically significant changes. | [72] |
| Cytokines (Serum) | 36 of 45 Inflammation Markers (e.g., various interleukins, chemokines) | 2 cycles | Measurements between 1 (T1) and 2 (T2) thaws were largely similar. 36 markers showed significant change after a 3rd (T3) thaw. | [73] |
| Cytokines (Ocular Fluid) | 27 Cytokines (including IL-2, IL-10, IL-12, PDGF-BB) | 3 cycles | Up to three freeze-thaw cycles did not significantly impact concentrations in aqueous humour or vitreous. | [74] |
| Equine Cytokines | IL-1Ra, IL-10, IL-1β, TNF-α | 4 cycles | IL-1Ra concentration decreased significantly after the 5th freeze-thaw cycle. No effect at 3 or 4 cycles. | [75] |
| Urinary Metabolites | 11-dehydro-Thromboxane-B2, Creatinine | 10 cycles | Stable across all ten cycles. | [76] |
| Urinary Metabolites | 8-iso-Prostaglandin F2α | <6 cycles | Significantly increased by cycle 6 (151% of baseline at cycle 10); effect mitigated by antioxidant. | [76] |
Table 2: Impact of Long-Term Storage on Biomarker Stability
| Analyte Category | Specific Analyte | Storage Temperature | Stability Duration | Key Findings | Source |
|---|---|---|---|---|---|
| Clinical Chemistry | ALT, AST, CK, GGT, Direct Bilirubin, Glucose, Creatinine, Cholesterol, Triglycerides, HDL | -20°C | 3 months | Showed adequate stability. | [72] |
| Clinical Chemistry | LD, BUN, Uric Acid, Total Protein, Albumin, Total Bilirubin, Calcium | -20°C | 3 months | Changed significantly over 3 months. | [72] |
| Cytokines (Plasma/Serum) | IL-1α, IL-1β, IL-10, IL-15, CXCL8 | -80°C | 2 years | Stable for up to 2 years. Degraded to ≤75% of baseline after 4 years. | [77] |
| Cytokines (Ocular Fluid) | IL-2, IL-10, IL-12, PDGF-BB | -80°C | 3 months | Concentrations significantly decreased as early as 3 months post-collection (9-37% decline by 15 months). | [74] |
| Cytokines (Serum) | Osteoprotegerin (OPG) | -80°C | 44 months | Significant decay (-33% per year). Not stable for long-term storage. | [78] |
| Cytokines (Serum) | Osteopontin (OPN), VEGF-A | -80°C | 44 months | Stable during long-term storage (-0.3% and -6.3% per year, respectively). | [78] |
| Urinary Metabolites | 11-dehydro-TxB2, 8-iso-PGF2α, Creatinine | -40°C | 10 years | Highly correlated measurements between first and second analysis after 10 years (all rho = 0.99). | [76] |
Detailed Experimental Protocols
To ensure the reproducibility of stability studies, the experimental methodologies from key cited works are detailed below.
Protocol for Evaluating Freeze-Thaw Cycles in Serum
This protocol is adapted from a study investigating the stability of 45 inflammation markers in human serum [73].
- Sample Collection and Preparation: Blood samples are collected from participants using standard venipuncture. Serum is prepared by allowing blood to clot in a serum separator tube for 20-30 minutes at room temperature, followed by centrifugation (e.g., 1200 x g for 15 minutes). The serum is then aliquoted into sterile cryovials.
- Baseline Measurement (T1): One aliquot is thawed, centrifuged to remove debris (e.g., 671 x g for 5 minutes), and analyzed immediately to establish baseline cytokine concentrations.
- Generation of Multiple Freeze-Thaw Cycles (T2, T3):
- T2 Samples: A second set of aliquots is thawed overnight in a refrigerator (2-8°C), centrifuged, and the supernatant is transferred to a new tube to simulate the process of creating aliquots for an assay. The samples are then immediately refrozen at -80°C.
- T3 Samples: The T2 samples are later thawed again under the same conditions, centrifuged, and transferred to new tubes, creating samples that have undergone three freeze-thaw cycles before final analysis.
- Analysis: All samples (T1, T2, T3) from the same subject are assayed together in the same batch, preferably in duplicate, using a multiplex bead-based assay (e.g., Luminex). The plate layout should position T1, T2, and T3 specimens adjacently to minimize inter-well variation.
- Data Analysis: The absolute difference and percent difference in marker concentrations between T1-T2 and T2-T3 are calculated. Statistical significance is evaluated using tests like the Wilcoxon signed-rank test. Spearman rank correlation coefficients are computed to assess the preservation of subject rank ordering.
Protocol for Evaluating Long-Term Storage Stability
This protocol is based on studies assessing the stability of cytokines and other analytes over periods of months to years [72] [78].
- Sample Pooling and Aliquoting: Residual plasma or serum samples from multiple donors or patients are pooled to create a homogeneous sample matrix. This pooled sample is then divided into a large number of identical, small-volume aliquots in sterile cryovials.
- Storage Conditions: All aliquots are stored at a consistent and monitored temperature, typically -80°C, to minimize enzymatic and chemical degradation.
- Serial Analysis: At predetermined time points (e.g., 1 week, 3 months, 9 months, 15 months, and annually thereafter), a set of aliquots is removed from storage. For each time point, multiple aliquots (e.g., n=5) are thawed and analyzed in the same batch to account for intra-assay variability.
- Control for Assay Variation: To distinguish sample degradation from changes in assay performance over time, a stable internal control sample (e.g., a pooled supernatant from stimulated PBMCs or a commercial quality control material) is included in every assay batch [77].
- Data Analysis: The concentration of each analyte at different time points is compared to the baseline measurement (the first time point). A mixed effects linear model or ANOVA is often used to assess the significance of concentration changes over time, with a correction for multiple comparisons (e.g., Bonferroni correction).
Stability-Informed Research Workflow
The following diagram illustrates a recommended workflow for handling samples intended for cytokine analysis, integrating stability findings to minimize pre-analytical variability.
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table lists key reagents and materials critical for conducting robust sample stability studies and cytokine measurements.
Table 3: Key Reagent Solutions for Stability and Cytokine Detection Research
| Reagent/Material | Function and Importance in Research |
|---|---|
| Cryogenic Vials | For consistent, small-volume aliquoting to avoid repeated freezing and thawing of stock samples. |
| Controlled-Temperature Freezers (-80°C) | Essential for long-term storage to preserve biomarker integrity; stability is highly temperature-dependent [77] [78]. |
| Multiplex Bead-Based Assay Kits | Enable simultaneous measurement of dozens of cytokines from a single, small-volume sample, conserving precious biobank samples [73] [74]. |
| Internal Control Samples | Pooled, aliquoted samples from stimulated cell cultures or patient pools used in every assay batch to monitor inter-assay variation and analyte stability over time [77]. |
| Protein Stabilizing Cocktails/Antioxidants | Additives that can inhibit protease activity and prevent oxidative degradation (e.g., of 8-iso-PGF2α), thereby improving analyte stability during storage and freeze-thaw cycles [76]. |
| Luminex xMAP or FCM-based Platforms | Core instrumentation for reading multiplex bead assays, offering high-throughput and sensitivity for cytokine profiling [73] [79]. |
The data unequivocally demonstrate that there is no universal rule for sample stability; it is intrinsically analyte- and matrix-specific. While common clinical chemistry analytes and certain cytokines like OPN and VEGF-A demonstrate robust stability, others, including OPG and several interleukins, are highly susceptible to degradation during storage or freeze-thaw cycles. The choice of detection method, whether multiplex immunoassay or ELISA, must be coupled with a rigorous, stability-informed pre-analytical protocol. For research aimed at comparing the sensitivity of cytokine detection methods, failing to control for these variables introduces a significant and often unquantified source of error. Therefore, the implementation of standardized protocols for sample handling, the use of internal controls, and meticulous matching of freeze-thaw histories in case-control studies are not just best practices but necessities for generating reliable, reproducible, and clinically translatable data.
Addressing Matrix Effects and Interfering Substances in Complex Samples
In the pursuit of accurate cytokine profiling for research and drug development, matrix effects present a formidable challenge. These effects, caused by interfering substances in complex biological samples, can suppress or enhance detection signals, leading to compromised data and erroneous conclusions. This guide objectively compares the performance of various cytokine detection platforms, detailing how each technology manages matrix interference, supported by experimental data and methodologies.
Understanding Matrix Interference
Matrix effects refer to the unintended alteration of an analytical measurement caused by all other components of the sample besides the target analyte [80]. In biological samples like serum, plasma, or urine, these interfering substances can include proteins (e.g., albumin, lysozymes), lipids, carbohydrates, salts, and complement proteins [80]. Their interference can manifest as:
- False Positives: Due to non-specific binding or signal enhancement.
- False Negatives: Due to analyte binding to matrix components or signal suppression [80].
The spike-and-recovery assay is a standard method for evaluating matrix effects. A known concentration of the recombinant analyte is added ("spiked") into the sample matrix, and the measured concentration is compared to the expected value. Recovery rates between 80% and 120% are generally considered acceptable, indicating minimal interference [80].
Platform Comparison: Sensitivity and Matrix Tolerance
The following table summarizes key performance metrics for leading cytokine detection platforms, highlighting their advertised strengths and documented performance in the face of matrix effects.
Table 1: Comparison of Cytokine Detection Platform Performance
| Platform | Reported Sensitivity | Dynamic Range | Key Advantages for Matrix Management | Cited Limitations |
|---|---|---|---|---|
| Meso Scale Discovery (MSD) | Highest sensitivity in low detection limit [13] | Broadest dynamic range [13] | Electroluminescence technology reduces background noise [13]. | Not specified in search results. |
| Cytometric Bead Array (CBA) / Flow Cytometry | Superior performance in sensitivity [13] | Superior performance in dynamic range [13] | One-step, lyophilized assays can simplify procedure and reduce cold storage needs [21]. | Dedicated flow cytometer required [21]. |
| Simoa | Ultra-high sensitivity [81] | Not specified | Designed for high-sensitivity quantification in complex samples; extensive validation for matrix effects recommended [81]. | Not specified in search results. |
| Luminex | Superior performance in sensitivity [13] | Superior performance in dynamic range [13] | Multiplexing capability [13]. | Requires dedicated instrumentation; upfront costs can be high [21]. |
| ELISA | Varies by kit and target | Varies by kit and target | Well-established; multiple documented strategies to manage matrix (e.g., dilution, calibration) [80] [82]. | Susceptible to matrix interference; accuracy can be compromised in complex samples [83] [80]. |
Experimental Protocols for Addressing Matrix Effects
Sample Dilution and Matrix-Matched Calibration
Sample dilution is one of the simplest and most effective methods to minimize matrix interference.
Protocol (Minimum Required Dilution - MRD):
- Prepare a series of dilutions of your sample using the same buffer as the kit standards (e.g., 1:2, 1:5, 1:10) [80].
- Assay the diluted samples alongside the standard curve.
- Determine the Minimum Required Dilution (MRD), which is the lowest dilution at which the measured analyte concentration falls within the linear range of the assay and shows acceptable spike-and-recovery (80-120%) [80].
- The final concentration is calculated by multiplying the readout from the assay by the dilution factor.
Protocol (Matrix-Matched Calibration):
- Prepare standard curves in a matrix that closely matches the sample (e.g., normal serum for serum samples) [80].
- This approach compensates for any uniform effects the matrix has on the assay, as both standards and samples are subjected to the same interference.
- A limitation is the requirement for a representative, analyte-free blank matrix, which can be difficult to obtain [80].
The Standard Addition Method
This quantitative procedure is particularly useful for compensating for matrix effects in complex, variable samples where a blank matrix is unavailable [82].
- Protocol:
- Prepare Test Solutions: Aliquot equal volumes of the sample with an unknown analyte concentration (Cx) into several tubes. To these, add increasing, known volumes (Vs) of a standard solution with a known, high concentration (Cs) [82].
- Measure Instrument Response: Analyze all spiked samples and the original unspiked sample. The sensor's response (e.g., optical density, fluorescence) is recorded for each [82].
- Calculate Unknown Concentration: Plot the measured signal against the volume or concentration of the added standard. Perform linear regression and extrapolate the line to where it crosses the x-axis (signal = 0). The absolute value of the x-intercept corresponds to the original concentration of the analyte in the sample [82].
The workflow for this method is outlined below.
Solid-Phase Extraction for Sample Cleanup
For techniques like UPLC-MS/MS, advanced cleanup methods can be employed to remove interfering substances physically.
- Protocol (Magnetic Dispersive Solid-Phase Extraction - MDSPE):
- Extraction: Samples are homogenized with an organic solvent (e.g., 1% ammonia-acetonitrile) to extract the target analytes [84].
- Purification: Synthesized magnetic nanoparticles (e.g., Fe3O4@SiO2-PSA) are added to the extract. These nanoparticles adsorb and remove matrix interferences like proteins and lipids [84].
- Separation: A magnet is applied to the tube to separate the nanoparticles with bound interferences from the purified extract [84].
- Analysis: The purified extract is then injected into the UPLC-MS/MS system for analysis. This method has demonstrated recoveries of 74.9–109% for diazepam in complex aquatic product matrices [84].
The Scientist's Toolkit: Key Reagents and Materials
Table 2: Essential Research Reagents and Solutions for Managing Matrix Effects
| Item | Function / Application |
|---|---|
| Assay-Specific Diluent | A proprietary buffer designed to be compatible with the sample type (e.g., serum, plasma, cell culture supernatant) and the antibodies in the kit, helping to neutralize matrix interference [80]. |
| Magnetic Nanoparticles (e.g., Fe3O4@SiO2-PSA) | Used in MDSPE for rapid, efficient cleanup of complex samples prior to analysis by removing interfering proteins and lipids [84]. |
| Stable Isotopically Labeled Internal Standards (SIL-IS) | Used primarily in MS, these are chemically identical to the analyte but with a different mass. They compensate for analyte loss during preparation and signal suppression/enhancement during ionization by co-eluting with the target [85]. |
| Lyophilized Reagent Beads | Pre-mixed, freeze-dried capture beads and detection antibodies simplify assays into a single step, reduce storage requirements, and can standardize performance, minimizing operational variability [21]. |
| Blank Matrix | A representative sample (e.g., serum, plasma) that is confirmed to be free of the target analyte. It is essential for preparing matrix-matched calibration curves to account for matrix effects [80]. |
A Strategic Workflow for Method Validation
To ensure reliable cytokine quantification, a systematic approach to evaluate and mitigate matrix effects is crucial. The following diagram illustrates a recommended validation workflow.
No single cytokine detection platform holds a universal advantage; the choice involves a strategic trade-off between sensitivity, multiplexing capability, and robustness to matrix effects. Technologies like MSD and Simoa offer exceptional sensitivity, while flow cytometry-based methods provide robust multiplexing. The reliability of any platform, however, is contingent upon rigorous validation and the application of appropriate sample preparation techniques, such as optimal dilution, standard addition, or advanced cleanup methods, to mitigate the confounding influence of complex sample matrices.
In the sensitivity comparison of cytokine detection methods, the precise handling of values reported below the assay's detection limit (DL) is a critical methodological challenge with direct implications for statistical error control. When analytical instruments fail to detect analytes present at low concentrations, researchers must make informed decisions about how to treat these non-detects in their datasets. The approach selected creates a fundamental trade-off between Type I errors (false positives, where a true null hypothesis is incorrectly rejected) and Type II errors (false negatives, where a false null hypothesis is not rejected) [86] [87]. In cytokine detection research, this might manifest as either falsely concluding a cytokine is present when it is not (Type I) or failing to detect a biologically relevant cytokine that is present below the detection limit (Type II) [88].
The statistical handling of non-detects becomes particularly crucial in drug development contexts, where cytokine profiles may serve as biomarkers for therapeutic efficacy or toxicity. Suboptimal handling of data near detection limits can systematically bias results, leading to inaccurate conclusions about drug mechanisms or patient responses [25]. This article examines established methodologies for values below detection limits within cytokine detection research, evaluates their impact on Type I and II error rates, and provides guidance for selecting appropriate approaches based on research objectives and error tolerance.
Statistical Foundations: Type I and Type II Errors in Diagnostic Testing
Fundamental Definitions
In statistical hypothesis testing for cytokine detection, two mutually exclusive propositions are considered: the null hypothesis (Hâ‚€) typically states that a cytokine is not present at detectable levels or that there is no difference between experimental groups, while the alternative hypothesis (Hâ‚) states that the cytokine is present or that a significant difference exists [86]. The relationship between decision outcomes and ground truth is summarized below:
Table: Decision Outcomes in Statistical Hypothesis Testing
| Statistical Decision | Reality: Hâ‚€ True | Reality: Hâ‚ True |
|---|---|---|
| Reject Hâ‚€ | Type I Error (False Positive) | Correct Inference (True Positive) |
| Fail to Reject Hâ‚€ | Correct Inference (True Negative) | Type II Error (False Negative) |
Error Trade-offs and Consequences in Cytokine Research
The probability of committing a Type I error is denoted by α (significance level), while the probability of a Type II error is denoted by β [87]. The power of a statistical test (1-β) is its ability to correctly reject a false null hypothesis [88]. In cytokine detection research, these errors have distinct practical implications:
Type I Error Consequences: Falsely reporting cytokine presence or group differences can lead to incorrect biological conclusions, wasted resources following false leads, and potential publication of erroneous findings [87]. In drug development, this might translate to pursuing ineffective therapeutic pathways based on spurious cytokine signals.
Type II Error Consequences: Failing to detect clinically relevant cytokines can result in missed therapeutic targets, overlooked safety signals, or incorrect conclusions about biological mechanisms [88]. This is particularly problematic in biomarker discovery where low-abundance cytokines may have diagnostic significance.
The trade-off between these errors is influenced by methodological choices in handling data below detection limits, with more conservative approaches reducing Type I errors but potentially increasing Type II errors, and vice versa [87].
Methodologies for Handling Values Below Detection Limits
Established Statistical Approaches
Several statistical approaches have been developed for handling values below detection limits, each with distinct implications for Type I and II error rates:
Table: Statistical Methods for Handling Values Below Detection Limits
| Method | Description | Impact on Type I Error | Impact on Type II Error | Best Application in Cytokine Research |
|---|---|---|---|---|
| Substitution with DL/2 | Replaces non-detects with half the detection limit [89] | Moderate control | Moderate control | Default approach when cytokines may be present; balanced error trade-off |
| Simple Substitution (DL) | Replaces non-detects with the full detection limit [89] | Increases risk | Decreases risk | Highly conservative safety assessment; minimizes false negatives |
| Simple Substitution (Zero) | Treats non-detects as zero concentration [89] | Decreases risk | Increases risk | When confident cytokine is absent; minimizes false positives |
| Statistical Estimation | Uses distributional methods to estimate values [89] | Optimized control | Optimized control | Large datasets with >50% detects; advanced statistical capability required |
| Multiple Imputation | Generates multiple possible values based on observed data | Optimized control | Optimized control | Complex studies with patterned missingness; advanced implementation needed |
The U.S. Environmental Protection Agency's guidance on handling chemical concentration data near detection limits provides a structured decision path for selecting appropriate methods, which can be adapted to cytokine detection research [89]. This decision process considers whether: (1) the compound is present at hazardous concentrations in any sample; (2) the sample was taken down-gradient from a detectable concentration; (3) physical-chemical characteristics permit the compound to be present; and (4) the treatment of non-detects significantly impacts risk estimates [89].
Impact on Cytokine Detection Sensitivity Comparisons
The choice of method for handling values below detection limits directly influences reported sensitivity metrics in method comparison studies. For instance, when comparing traditional ELISA with multiplex platforms like Luminex or Meso Scale Discovery, inconsistent handling of non-detects across platforms can systematically bias sensitivity comparisons [25]. Methods that aggressively substitute non-detects with zero may artificially improve apparent sensitivity by reducing background signals, while conservative approaches using full DL substitution may make sensitivity appear worse by increasing background measurements.
Statistical power considerations are particularly important when designing cytokine detection studies. Power, defined as the probability of correctly rejecting a false null hypothesis (1-β), depends on significance level (α), sample size, and effect size [88]. Studies with insufficient power due to small sample sizes or problematic handling of non-detects may fail to detect biologically relevant cytokine differences (Type II errors), potentially missing important therapeutic insights [88].
Cytokine Detection Technologies and Their Technical Specifications
Method Comparison and Performance Characteristics
Different cytokine detection platforms exhibit varying sensitivities, dynamic ranges, and multiplexing capabilities, which directly influence how frequently researchers encounter values below detection limits and must apply statistical correction methods:
Table: Technical Comparison of Major Cytokine Detection Methods
| Method | Sensitivity Range | Dynamic Range | Multiplexing Capacity | Sample Volume | Impact on Non-Detect Frequency |
|---|---|---|---|---|---|
| ELISA | Low picogram/mL [25] | 2-3 logs [25] | Single-plex [25] | 100-200 μL [25] | Higher for low-abundance cytokines |
| Luminex xMAP | Low picogram/mL to femtogram/mL [25] | 3-5 logs [25] | Up to 500 analytes [25] | 25-50 μL [25] | Lower due to enhanced sensitivity |
| Meso Scale Discovery (MSD) | Sub-picogram/mL [25] | 3-5 logs [25] | Moderate to high multiplexing [25] | 25-50 μL [25] | Lower, especially for low-abundance cytokines |
| Flow Cytometry-Based | Comparable to Luminex [21] | Similar to conventional methods [21] | 12-plex and higher [21] | Varies by protocol | Moderate, protocol-dependent |
Method Selection Considerations for Error Control
Researchers can minimize statistical error propensity through strategic method selection based on their specific research context:
For exploratory studies where cytokine signatures are unknown, high-plex methods with broad dynamic range (e.g., Luminex) reduce Type II errors by detecting more cytokines simultaneously, though potentially increasing Type I errors without proper multiple comparison corrections [25].
For targeted validation studies of specific cytokines, high-sensitivity single-plex methods (e.g., optimized ELISA) provide more reliable quantification with better-controlled Type I error rates for the specific targets of interest [25].
For studies with limited sample volume (e.g., pediatric research or animal models), multiplex methods requiring smaller volumes (25-50 μL) prevent sample dilution that can push low-concentration cytokines below detection limits, thus reducing Type II errors [25].
The "hook effect" observed in some immunoassays at extremely high cytokine concentrations (e.g., sepsis models) represents a special case where high analyte levels paradoxically reduce signal, potentially creating false negatives (Type II errors) if not properly addressed through sample dilution or method selection with appropriate dynamic range [25].
Experimental Protocols for Method Validation
Protocol for Determining Method Detection Limits
Establishing precise detection limits is fundamental to proper statistical handling of non-detects. The EPA guidance outlines several distinct detection limits that can be adapted to cytokine detection assays [89]:
Instrument Detection Limit (IDL): Determine by running seven replicate analyses of a laboratory standard at the lowest concentration that is statistically different from a blank (calculated as three times the standard deviation of the replicates) [89].
Method Detection Limit (MDL): Process seven replicate spiked samples through the entire analytical procedure as environmental samples (calculated as three times the standard deviation of these replicates) [89].
Sample Quantitation Limit (SQL): Calculate by correcting the MDL for sample-specific adjustments, including dilution factors and sample matrix effects [89].
For cytokine detection specifically, the conventional flow cytometry-based multiplex assay protocol involves: (1) combining 50 μL of sample or standard with 50 μL of capture microspheres in a 96-well plate and incubating with shaking at room temperature for 2 hours; (2) washing to remove unbound material; (3) adding biotinylated secondary antibody and incubating for 30 minutes; (4) washing and adding streptavidin-PE conjugate with incubation for 30 minutes; and (5) final wash before reading on a flow cytometer [21].
Protocol for One-Step Lyophilized Assay
Recent methodological advances include simplified one-step approaches that can reduce variability and potential errors:
- Prepare lyophilized reagent beads using optimized buffer formulations (e.g., PBS with 0.1% BSA, 5% mannitol, and 3% trehalose) [21].
- Rapidly dispense 250 μL aliquots into liquid nitrogen for crystallization (approximately 10 seconds) [21].
- Transfer frozen beads to a pre-cooled vacuum freeze-dryer for lyophilization for 12 hours [21].
- For detection, add 100 μL of sample to a 96-well plate containing lyophilized reagent beads [21].
- Incubate with shaking at room temperature for 1.5 hours [21].
- Wash to remove unbound components, add reading buffer, and analyze using a flow cytometer [21].
This simplified approach reduces operational steps and potential handling errors that might contribute to statistical errors in final measurements.
Visualizing Statistical Relationships and Experimental Workflows
Relationship Between Statistical Errors and Detection Limits
Decision Pathway for Handling Non-Detects in Cytokine Research
Experimental Workflow for Cytokine Detection Method Validation
The Scientist's Toolkit: Essential Research Reagent Solutions
Table: Essential Research Reagents for Cytokine Detection Studies
| Reagent/Category | Function | Example Specifications | Error Control Considerations |
|---|---|---|---|
| Capture Antibodies | Bind specific cytokines to solid phase | High specificity, minimal cross-reactivity [25] | Reduces false positives (Type I) by ensuring specific detection |
| Detection Antibodies | Generate measurable signal for bound cytokines | Phycoerythrin-labeled, high affinity [21] | Enhances sensitivity, reducing false negatives (Type II) |
| Fluorescently Encoded Microspheres | Enable multiplex detection | Carboxylated beads, distinct fluorescence signatures [21] | Allows simultaneous measurement, controlling multiple comparison errors |
| Cytokine Standards | Calibration and quantification | Recombinant proteins, known concentrations [21] | Enables accurate quantification, minimizing both Type I and II errors |
| Assay Buffers | Maintain optimal reaction conditions | PBS with stabilizers (BSA, trehalose, mannitol) [21] | Reduces technical variability that contributes to both error types |
| Lyophilization Reagents | Stabilize assay components for storage | Trehalose, mannitol for cryoprotection [21] | Improves reproducibility between experiments, reducing systematic errors |
The statistical handling of values below detection limits represents a critical methodological consideration in cytokine detection research with direct implications for Type I and II error control. No single approach is universally optimal; rather, the selection should be guided by research objectives, sample characteristics, and the relative consequences of different error types in the specific research context. Methodologies ranging from simple substitution to advanced statistical estimation offer different trade-offs between false positive and false negative risks.
Strategic method selection, appropriate experimental design with adequate statistical power, and transparent reporting of detection limits and handling methods collectively contribute to improved validity and reproducibility in cytokine research. As detection technologies continue advancing toward greater sensitivity and multiplexing capability, the frequency of values near detection limits may decrease, but the fundamental statistical principles for their proper handling will remain essential for robust scientific inference in drug development and basic research.
Head-to-Head Technology Comparison: Sensitivity, Multiplexing, and Practical Applications
Accurately measuring cytokine levels is fundamental to biomedical research, clinical diagnostics, and drug development. Cytokines, as critical immune system messengers, often exist at low concentrations in biological samples, making the sensitivity of detection platforms a paramount consideration. The limit of detection (LOD) serves as a crucial benchmark for comparing platform performance, directly impacting the ability to detect biologically significant concentrations of biomarkers. This guide provides a direct, data-driven comparison of major cytokine detection platforms, evaluating their analytical sensitivity to inform method selection for research and development applications.
The choice of detection technology can significantly influence reported cytokine concentrations and study outcomes. Cross-platform comparisons have revealed substantial variability in performance, with differences in sensitivity, precision, and frequency of endogenous analyte detection [18]. This variability underscores the importance of objective, data-backed platform assessments to ensure research reproducibility and reliability.
Key Cytokine Detection Platforms and Technologies
Multiple technology platforms have been developed for cytokine detection, each with distinct operating principles and performance characteristics.
Enzyme-Linked Immunosorbent Assay (ELISA) represents one of the most established methods, using enzyme-mediated colorimetric detection in a sandwich assay format. While simple and well-established, it typically offers lower sensitivity compared to newer technologies and is inherently single-plex [25].
Luminex xMAP Technology utilizes color-coded magnetic microspheres to enable multiplex detection of up to 500 analytes simultaneously. This bead-based immunoassay platform provides excellent throughput with minimal sample volume requirements [25].
Electrochemiluminescence (ECL) Platforms such as Meso Scale Discovery (MSD) use electricity and light to create a highly sensitive detection signal. These platforms combine multiplexing capability with a broad dynamic range [25] [18].
Single Molecule Array (Simoa) Technology represents the current pinnacle of sensitivity, employing digital ELISA technology to detect individual protein molecules. This platform can achieve detection limits in the femtomolar range, significantly surpassing conventional methods [18].
Direct Sensitivity Comparison: Limits of Detection
Quantitative Comparison of Platform Sensitivity
Table 1: Direct Comparison of Limits of Detection (LOD) Across Major Cytokine Detection Platforms
| Detection Platform | Technology Principle | Reported Sensitivity Range | Multiplexing Capacity | Sample Volume Required |
|---|---|---|---|---|
| Simoa | Digital ELISA | Femtomolar (fg/mL) range [18] | Low to moderate | Not specified |
| MSD (Meso Scale Discovery) | Electrochemiluminescence | Low pg/mL range [25] [18] | High (customizable panels) | 25-50 μL [25] |
| Luminex xMAP | Bead-based fluorescence | Low pg/mL to fg/mL [25] [18] | Very high (up to 500-plex) | 25-50 μL [25] |
| Traditional ELISA | Colorimetric detection | Low pg/mL range [25] | Single-plex (can be run in parallel) | 100-200 μL [25] |
Cross-Platform Performance Assessment
A comprehensive cross-platform evaluation compared five leading technologies for detecting cytokines implicated in neuroinflammatory disorders. The assessment revealed stark differences in analytical performance:
- The Simoa platform demonstrated the highest sensitivity in detecting endogenous analytes across all tested cytokines (IL-1β, IL-6, TNF-α, and IFN-γ) and clinical populations, as reflected by the highest frequency of endogenous analyte detection (FEAD) [18].
- Variable performance was observed for MESO V-plex, R&D Luminex, and Quantikine ELISA assays, while Myriad's Luminex xMAP exhibited low FEAD across all analytes and samples [18].
- For IL-6 detection, most platforms (except Myriad's Luminex xMAP) showed strong correlations with one another (r range = 0.59-0.86). However, for IL-1β, TNF-α, and IFN-γ, there was low to no correlation across platforms, indicating significant measurement variability between technologies [18].
- The Simoa platform also demonstrated high precision, with <20% coefficient of variance (%CV) across replicate runs for samples from healthy controls, PTSD patients, and PD patients [18].
Experimental Protocols for Sensitivity Determination
Standard ELISA Protocol
The indirect sandwich ELISA remains a fundamental methodology for cytokine detection, with sensitivity optimization achieved through specific procedural refinements [5]:
Day 1: Plate Coating
- Dilute capture antibody in PBS to concentrations determined by checkerboard titration (typically 1-10 μg/mL).
- Add 50 μL/well to a 96-well high-binding microplate.
- Tap plate gently to ensure complete coverage of well bottom.
- Incubate overnight at 4°C.
Day 2: Assay Procedure
- Wash plate five times with 250 μL/wash of PBS containing 0.05% Tween-20 using an automatic plate washer.
- Block plates with 150 μL/well of blocking buffer (e.g., 2% BSA, Blotto, or Casein in PBS) for 1 hour at ambient temperature on an orbital shaker.
- Prepare cytokine standards in dilution buffer across a 3-log concentration range.
- Wash plate and add 50 μL/well of standards or samples. Incubate for 2 hours.
- Prepare detection antibody dilutions in dilution buffer. Wash plate and add 50 μL/well of detection antibody. Incubate for 2 hours.
- Prepare streptavidin-HRP conjugate (typically 1:20,000 dilution in PBS with 0.1% BSA and 0.005% Tween-20). Wash plate and add 50 μL/well. Incubate for 30 minutes.
- Wash plate and add 100 μL/well of TMB substrate solution. Incubate in dark without shaking for 20-30 minutes.
- Stop reaction with 1.5 N sulfuric acid and read optical density at 450-590 nm.
Sensitivity Optimization Considerations:
- Checkerboard titrations of both capture and detection antibodies are essential for optimizing signal-to-noise ratio.
- Blocking buffer selection (BSA, Blotto, or Casein) requires empirical testing for each antibody pair.
- Signal development time must be controlled to ensure measurements fall within the linear range of detection [5].
Multiplex Immunoassay Protocol
Multiplex platforms share similarities with ELISA but require additional considerations for cross-reactivity and signal interference:
Sample Preparation:
- Process samples (serum, plasma, or other biofluids) to remove particulates by centrifugation.
- Aliquot samples to minimize freeze-thaw cycles, which can degrade cytokine stability.
Assay Procedure:
- For bead-based assays (Luminex), pre-mix capture antibody-coupled beads.
- Add samples or standards to wells containing mixed beads.
- Incubate to allow antigen-antibody binding, typically 2 hours with shaking.
- Wash to remove unbound material.
- Add biotinylated detection antibody mixture and incubate.
- Wash and add streptavidin-fluorophore or streptavidin-enzyme conjugate.
- Measure signal using platform-specific reader.
Critical Validation Steps:
- Assess cross-reactivity between different antibody pairs in the multiplex panel.
- Determine parallelism using serial dilutions of samples to confirm consistent detection across expected concentrations.
- Perform spike-recovery experiments to verify accuracy in the specific sample matrix [5] [18].
Visual Guide to Platform Selection and Performance
Cytokine Detection Platform Selection Workflow
Platform Sensitivity Comparison
Research Reagent Solutions
Table 2: Essential Research Reagents for Cytokine Detection Assays
| Reagent Category | Specific Examples | Function and Importance |
|---|---|---|
| Matched Antibody Pairs | Monoclonal capture with biotinylated detection antibodies | Form the core recognition system; quality directly impacts specificity and sensitivity [5] |
| Blocking Buffers | BSA (2%), Blotto, Casein, Superblock | Prevent non-specific binding; optimal buffer varies by antibody pair and must be determined empirically [5] |
| Detection Reagents | Streptavidin-HRP, Streptavidin-IR dyes | Signal generation; enzyme conjugates provide amplification for sensitivity [5] |
| Substrates | TMB (3,3',5,5'-tetramethylbenzidine) | Enzyme substrate that generates measurable colorimetric, chemiluminescent, or fluorescent signal [5] |
| Wash Buffers | PBS with Tween-20 (0.05%) | Remove unbound reagents while maintaining assay integrity; surfactant concentration critical [5] |
| Cytokine Standards | Recombinant proteins | Quantification reference; must be highly pure and accurately quantified for reliable standard curves [5] |
This direct sensitivity comparison reveals significant differences in limits of detection across major cytokine detection platforms. The Simoa platform demonstrates superior sensitivity for detecting low-abundance cytokines, while Luminex xMAP technology offers an optimal balance of sensitivity and multiplexing capacity for comprehensive cytokine profiling. MSD platforms provide robust sensitivity with flexible multiplexing options, whereas traditional ELISA remains viable for single-analyte studies with sufficient sample volume.
Platform selection should be guided by specific research requirements, including required sensitivity level, multiplexing needs, sample volume constraints, and throughput considerations. The substantial variability in cross-platform performance underscores the importance of method standardization, particularly for longitudinal studies or multi-site collaborations. As cytokine detection technologies continue to evolve, ongoing comparative assessments will remain essential for ensuring measurement reliability and research reproducibility.
In the study of immune responses, cytokines serve as crucial signaling molecules, and their profiling is essential for understanding disease pathogenesis, from HIV to COVID-19 [14] [90]. The ability to accurately measure multiple cytokines simultaneously from a single small sample volume—a capability known as multiplexing—has transformed immunology research and drug development. This guide objectively compares current multiplexing platforms, examining the critical trade-offs between expanding the number of analytes measured and maintaining data quality, with particular focus on sensitivity, reproducibility, and specificity. As research moves toward systems-level biology, the demand for comprehensive cytokine profiling has intensified, making the balancing act between panel size and data quality a central concern in experimental design [91] [63].
Technology Platform Comparison
Established Multiplexing Platforms
Luminex xMAP Technology: This bead-based flow cytometry platform allows simultaneous detection of up to 100 analytes in a single well, though many commercially available panels are typically smaller (e.g., 10-13 plex for cytokine measurements) [14]. The technology uses color-coded microspheres as the solid phase for immunoassays, with a fluorescent reporter system for quantification. While it offers good sensitivity for many cytokines, studies have revealed significant variability between laboratories and kit lots, potentially limiting its utility for long-term multisite studies requiring absolute quantification [14].
Meso Scale Discovery (MSD): MSD employs electrochemiluminescence detection on carbon electrode arrays, providing a broad dynamic range and excellent sensitivity, particularly for low-abundance cytokines [13]. Comparative studies have demonstrated that MSD generally achieves lower limits of detection compared to Luminex-based platforms, with one direct comparison highlighting MSD as the most sensitive technology among those tested [13]. The platform typically supports panels of up to 10-20 analytes while maintaining robust performance.
Olink Proximity Extension Assay (PEA): This innovative technology uses antibody pairs labeled with DNA oligonucleotides that only form amplifiable DNA sequences when both antibodies bind their target. The platform achieves high specificity through dual recognition and PCR amplification, enabling highly multiplexed panels (up to 96-plex or more) while minimizing cross-reactivity [91] [90]. However, it converts protein signals to DNA sequences, which may limit detection of protein complexes or post-translational modifications.
Emerging Platforms and Technologies
nELISA: Recently described in Nature Methods (2025), nELISA represents a significant technological advancement addressing reagent-driven cross-reactivity (rCR), the primary barrier to high-plex immunoassays [91]. The platform combines CLAMP (colocalized-by-linkment assays on microparticles) with advanced multicolor bead barcoding (emFRET). nELISA preassembles antibody pairs on target-specific barcoded beads, ensuring spatial separation between noncognate assays, and uses a novel detection-by-displacement mechanism via toehold-mediated strand displacement. This approach has demonstrated capability for 191-plex inflammation panels while maintaining sub-picogram-per-milliliter sensitivity across seven orders of magnitude [91].
NULISAseq: Another emerging platform, NULISAseq, employs a modified proximity ligation assay that has shown promising performance in comparative studies. When evaluated against Luminex and Olink for analyzing COVID-19 patient samples, NULISAseq demonstrated the highest proportion of detectable targets and identified the largest number of significant changes in longitudinal samples [90].
Table 1: Performance Comparison of Major Multiplex Platforms
| Platform | Maximum Plexity | Sensitivity | Dynamic Range | Reproducibility | Key Limitations |
|---|---|---|---|---|---|
| Luminex | ~100-plex (theoretical) | Variable by analyte; some cytokines poorly detected [14] | Good for most analytes | Significant lot-to-lot and inter-lab variability [14] | rCR limits effective plexity; standardization challenges |
| MSD | ~10-20 plex | Excellent, particularly for low-abundance targets [13] | Broadest among compared platforms [13] | Good intra-platform consistency | Lower multiplexing capacity |
| Olink | 92-plex (commercial panels) | Excellent for most targets | Good | Good correlation with NULISAseq [90] | Converts protein signal to DNA; limited PTM detection |
| nELISA | 191-plex (demonstrated) [91] | Sub-pg/mL sensitivity | 7 orders of magnitude [91] | High (rCR-free design) | New technology with limited track record |
| NULISAseq | Not specified | Highest detectability in COVID-19 study [90] | Good | Good correlation with Olink [90] | Emerging technology |
Experimental Data and Performance Metrics
Sensitivity and Detectability Comparisons
Direct platform comparisons reveal substantial differences in cytokine detectability. A multisite evaluation of high-sensitivity multiplex assays found that while IL-6, IL-8, IL-10, and TNF-α were detectable with at least three different platforms, other cytokines like IL-1β were clearly detected with only one kit [14]. No single multiplex panel reliably detected all cytokines across platforms, highlighting the importance of matching platform capabilities to specific analyte requirements.
In a comparative analysis of COVID-19 patient samples, NULISAseq showed the highest proportion of detectable targets, followed by Olink, with Luminex demonstrating lower detectability for many targets [90]. This pattern underscores the sensitivity advantages of newer detection methodologies, particularly for low-abundance cytokines in complex matrices like serum.
Reproducibility and Cross-Laboratory Consistency
Reproducibility remains a significant challenge for multiplex assays. A comprehensive multisite comparison found "highly significant differences (P < 0.001) between laboratories and/or lots with all kits" [14]. This variability suggests that current multiplex assays "may not be sufficiently reproducible for repeated determinations over a long-term study or in multiple laboratories but may be useful for longitudinal studies in which relative, rather than absolute, changes in cytokines are important" [14].
The same study noted that despite absolute concentration differences between platforms, the kits "generally detected similar patterns of cytokine perturbation during primary HIV viremia," indicating that relative comparisons within studies remain valid [14]. This distinction between absolute and relative quantification is crucial for researchers designing longitudinal or multi-site studies.
Table 2: Quantitative Performance Metrics from Comparative Studies
| Performance Measure | Luminex | MSD | Olink | nELISA |
|---|---|---|---|---|
| Lower Limit of Detection | Variable by analyte and kit; IL-1β particularly challenging [14] | Best sensitivity in comparative study [13] | Excellent for most targets | Sub-picogram/milliliter [91] |
| Dynamic Range | Good for most analytes | Broadest among platforms [13] | Good | 7 orders of magnitude [91] |
| Inter-laboratory Variability | Highly significant differences [14] | Less variable than Luminex | Good correlation between platforms [90] | Expected low variability (design principle) |
| Sample Volume Requirements | 35-50μL/well [14] | Similar to Luminex | Low (sample-sparing) [92] | Not specified |
| Multiplexing Ceiling | ~50-plex practical limit due to rCR [91] | ~20-plex | 92-plex+ | 191-plex demonstrated [91] |
Methodologies and Experimental Protocols
Standardized Testing Protocols for Platform Comparison
To ensure valid comparisons between platforms, researchers should implement standardized sample processing protocols. The multisite comparison study provides a helpful methodology: all participating laboratories received identical 1-ml aliquots of serum and plasma samples, which were thawed upon receipt, centrifuged (for plasma samples), and prepared as 70-125μl aliquots that were refrozen at -80°C until testing [14]. This approach standardized freeze-thaw history across all testing sites.
For the actual assays, each platform should be operated according to the manufacturer's protocol for the specific sample matrix (serum or plasma), utilizing recommended sample dilutions and standard curve concentrations, with all samples and standards assayed in duplicate [14]. Instrument calibration using validation kits within 2 weeks of each assay run is essential for generating reliable, comparable data.
Addressing Technical Challenges
Reagent-Driven Cross-Reactivity (rCR): Traditional multiplex immunoassays face increasing rCR as panel size expands, which occurs when noncognate antibodies mix and incubate together, enabling combinatorial interactions that form mismatched sandwich complexes [91]. This fundamental limitation has historically restricted robust multiplexing to approximately 25-plex, with many commercial kits limited to 10-plex [91].
Lot-to-Lot Variability: The significant differences observed between kit lots highlight the importance of using the same lot throughout a longitudinal study and carefully documenting lot numbers for all experiments [14]. For critical applications, purchasing sufficient reagents from a single lot to complete an entire study is recommended.
Diagram 1: Balancing multiplexing factors. The optimal balance between panel size and data quality requires addressing competing demands through technological innovation.
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful multiplex cytokine detection requires careful selection and quality control of research reagents. The following table outlines essential materials and their functions for implementing multiplex cytokine detection assays.
Table 3: Essential Research Reagents for Multiplex Cytokine Detection
| Reagent/Material | Function | Key Considerations | Example Vendors |
|---|---|---|---|
| Capture Antibodies | Immobilize target cytokines on solid phase | High specificity and affinity critical; lot-to-lot consistency | Thermo Fisher, R&D Systems, Bio-Rad |
| Detection Antibodies | Generate measurable signal upon binding | Minimal cross-reactivity; compatible with detection system | Thermo Fisher, R&D Systems, Bio-Rad |
| Cytokine Standards | Quantification reference | Matrix-matched; cover expected concentration range | NIBSC, kit manufacturers |
| Assay Diluents | Maintain antibody and cytokine stability | Minimize nonspecific binding; matrix appropriate | Kit-specific recommended solutions |
| Signal Detection Reagents | Generate measurable output (fluorescence, luminescence) | Compatible with platform; stable signal | Platform-specific reagents |
| Quality Controls | Monitor assay performance | Representative of study samples; multiple concentration levels | Commercial QC material or in-house preparations |
Leading vendors in the cytokine detection reagents space include Thermo Fisher Scientific, Agilent, R&D Systems, Promega, ACROBiosystems, and Bio-Rad [93]. When selecting reagents, researchers should prioritize lot consistency and provide validation data demonstrating performance characteristics relevant to their specific applications.
Emerging Trends and Innovation Pathways
The multiplex cytokine detection landscape is evolving rapidly, with several promising trends shaping future capabilities. The integration of artificial intelligence and machine learning for data analysis is improving interpretation accuracy and identifying subtle patterns in complex cytokine networks [63] [94]. Point-of-care testing developments aim to translate multiplex capabilities to clinical settings, though this application faces significant technical hurdles [63] [93]. Single-cell cytokine analysis represents another frontier, enabling resolution of cellular heterogeneity in immune responses that bulk measurements inevitably obscure [93].
The market trajectory reflects these technological advances, with the multiplex sepsis biomarker panels market alone projected to grow from $162.6 million in 2025 to $326.0 million by 2035, demonstrating the increasing adoption and commercial validation of these platforms [95]. Similarly, the broader cytokine detection services market is experiencing robust growth, further incentivizing technological innovation [63].
Diagram 2: Multiplex cytokine detection workflow. The process from sample collection to data interpretation involves critical decision points at each stage that impact data quality.
The optimal balance between multiplexing capability and data quality depends heavily on specific research requirements. For studies requiring absolute quantification across multiple sites or over extended periods, platforms with demonstrated reproducibility like MSD may be preferable, despite their lower plexity [14] [13]. When comprehensive profiling from limited samples is the priority, higher-plex technologies like nELISA, Olink, or NULISAseq offer compelling advantages, particularly as their reproducibility continues to be validated [91] [90].
The fundamental trade-off between panel size and data quality remains technologically constrained by reagent-driven cross-reactivity, though innovative approaches like spatial separation of immunoassays (CLAMP) and DNA-based signal amplification are progressively relaxing these constraints [91]. Researchers must carefully consider whether their applications require absolute quantification (favoring lower-plex, highly reproducible platforms) or relative comparison (where higher-plex platforms excel), while also weighing practical considerations including sample volume, throughput requirements, and available instrumentation. As technological innovation continues, the optimal balance point will undoubtedly shift toward increasingly comprehensive profiling without compromising data quality.
In biomedical research, accurately quantifying cytokines—key regulators of immune responses—is fundamental to understanding disease mechanisms, from cancer and autoimmune disorders to infectious diseases like COVID-19 [96]. Cytokine concentrations in biological samples can vary dramatically, spanning several orders of magnitude. This presents a significant analytical challenge: an ideal detection method must identify low-abundance signaling molecules at picogram or even femtogram per milliliter levels while simultaneously quantifying highly concentrated inflammatory mediators without requiring sample dilution [15] [25]. This capability defines an assay's dynamic range.
The dynamic range of an immunoassay is the span between the lowest and highest concentrations of an analyte that can be reliably measured [25]. A broad dynamic range is crucial for capturing the complete biological picture in complex physiological states such as cytokine release syndrome (CRS), where some cytokine levels may be massively elevated while others remain modest [96]. Methods with a narrow dynamic range risk losing data at the extremes—either failing to detect critical low-abundance biomarkers or saturating at high concentrations, leading to the "hook effect" and inaccurate measurements [25]. This comparative guide objectively analyzes the dynamic range performance of major cytokine detection platforms, providing researchers with the data needed to select the optimal technology for their specific application.
Multiple technology platforms are available for cytokine detection, each with distinct principles and performance characteristics. The evolution from traditional single-plex assays to sophisticated multiplex systems has been driven by the need to understand complex cytokine networks more efficiently and with limited sample material [15].
- ELISA (Enzyme-Linked Immunosorbent Assay): As the long-standing gold standard, ELISA is a single-plex, sandwich-style immunoassay that uses enzyme-linked antibodies for chromogenic or chemiluminescent detection [15]. While known for high specificity and reproducibility, its dynamic range is typically limited to 2-3 logs, which can be a constraint when measuring cytokines with widely varying concentrations [25].
- Luminex xMAP (Multi-Analyte Profiling): This bead-based multiplex flow cytometry method uses color-coded microspheres. Each bead set is coated with a capture antibody for a specific cytokine, allowing simultaneous detection of up to 500 analytes from a single sample [15] [25]. It offers a broader dynamic range of 3–5 logs [25].
- MSD (Meso Scale Discovery): MSD employs electrochemiluminescence detection. Capture antibodies are spotted onto carbon electrode-coated plates, and detection antibodies are labeled with a sulfo-tag that emits light upon electrical stimulation [13] [28]. This technology provides a very wide dynamic range and exceptional sensitivity for low-abundance cytokines [13] [28].
- Olink PEA (Proximity Extension Assay): A newer, high-plex technology, Olink uses pairs of antibodies tagged with unique DNA oligonucleotides. When both bind to the target protein, the DNA strands hybridize and are extended, creating a quantifiable DNA barcode via qPCR or NGS [28]. This method combines high specificity with a broad dynamic range from minimal sample volume (≈1 µL) [28].
- CBA (Cytometric Bead Array): Similar to Luminex, CBA is a bead-based flow cytometry system that allows for multiplexed cytokine measurement and is noted for its superior performance in sensitivity and dynamic range [13].
The table below summarizes the core characteristics of these major platforms.
Table 1: Core Characteristics of Major Cytokine Detection Platforms
| Method | Detection Principle | Multiplexing Capacity | Sample Volume per Panel | Key Feature |
|---|---|---|---|---|
| ELISA | Colorimetric/Chemiluminescent enzymatic reaction | Single-plex | 100–200 µL [25] | Well-established gold standard; high specificity per analyte [15] |
| Luminex | Bead-based flow cytometry | High-plex (up to 500 analytes) [25] | ~25-50 µL [25] | High-throughput; good for profiling many cytokines [28] |
| MSD | Electrochemiluminescence | Moderate-plex (e.g., 10-plex) [28] | ~20-40 µL [28] | Exceptional sensitivity and broadest dynamic range [13] |
| Olink PEA | Proximity Extension Assay with DNA readout | High-plex | ~1 µL [28] | High specificity & low sample requirement [28] |
| CBA | Bead-based flow cytometry | Multiplex | Varies | Superior performance in sensitivity and dynamic range [13] |
Experimental Data on Dynamic Range and Sensitivity
Direct comparative studies reveal critical differences in the performance of these technologies, particularly regarding dynamic range and sensitivity—two interrelated yet distinct parameters. Sensitivity determines the lowest detectable cytokine concentration, while dynamic range defines the span over which quantification remains accurate.
A comprehensive comparative analysis of several common technologies for measuring IL-1β, IL-6, and TNF-α found that MSD demonstrated the best sensitivity in the low detection limit and the broadest dynamic range [13]. The same study noted that CBA and Luminex also showed superior performance in both sensitivity and dynamic range [13]. In a targeted white paper comparison focusing on 20 overlapping cytokines, the Olink platform showed robust linearity and performance across its dynamic range, requiring a fraction of the sample volume (1 µL) compared to Luminex (12.5 µL) and MSD (20-40 µL) [28].
These findings are consolidated in the table below, which summarizes key performance metrics from experimental comparisons.
Table 2: Experimental Performance Metrics from Platform Comparisons
| Method | Reported Sensitivity | Reported Dynamic Range | Key Findings from Experimental Comparisons |
|---|---|---|---|
| ELISA | Low picogram/mL range [25] | 2-3 logs [25] | Good for single-plex, but narrow range may require sample dilution [15]. |
| Luminex | Low pg/mL to fg/mL for some assays [25] | 3–5 logs [25] | Demonstrates superior sensitivity and dynamic range; good for high-throughput multiplex profiling [13] [25]. |
| MSD | Very sensitive, broadest dynamic range [13] | >4 logs | Best sensitivity in low detection limit and broadest dynamic range in a multi-platform study [13]. |
| Olink PEA | Low-pg/mL possible [28] | Broad | Shows robust linearity and performance in dilution series; similar or better sensitivity than Luminex for many analytes [28]. |
| CBA | High sensitivity [13] | Broad | Demonstrates superior performance in sensitivity and dynamic range [13]. |
The following diagram illustrates the fundamental workflow common to sandwich-style immunoassays like ELISA, MSD, and Luminex, highlighting the step where dynamic range is determined.
Diagram 1: Core Immunoassay Workflow. The signal generation step is critical for determining the assay's dynamic range.
Detailed Experimental Protocols
To ensure reproducible and reliable dynamic range analysis, adherence to standardized protocols is essential. Below are detailed methodologies for key experiments cited in the performance comparisons.
Protocol: Multi-Platform Comparison for IL-1β, IL-6, and TNF-α
This protocol is adapted from a study that directly compared ELISA, Luminex, MSD, TR-FRET, CBA, AlphaLISA, and FirePlex technologies [13].
- Sample Preparation: Use the same set of pre-characterized samples (e.g., cell culture supernatants or patient serum/plasma) across all platforms to enable direct comparison. Include a dilution series of recombinant cytokine standards in a biologically relevant matrix to assess linearity and dynamic range experimentally.
- Assay Execution: Run each technology according to its manufacturer's instructions, strictly adhering to recommended incubation times, temperatures, and wash steps. For bead-based assays (Luminex, CBA), verify bead count and detector settings on the flow cytometer or analyzer.
- Data Collection and Analysis: Generate a standard curve for each analyte on every platform. The dynamic range is defined by the Lower Limit of Quantification (LLOQ) and Upper Limit of Quantification (ULOQ), typically where the coefficient of variation (CV) exceeds 20% or the recovery falls outside 80-120%. Calculate the percent recovery for each point in the dilution series and plot log concentration versus signal response to visualize the linear range.
Protocol: Assessing Dynamic Range via Dilution Parallelism
This method tests whether an assay maintains a linear response as sample concentration changes, a key indicator of a robust dynamic range [28] [25].
- Sample Dilution Series: Prepare a series of logarithmic dilutions (e.g., 1:2, 1:10, 1:100) of a sample with known high cytokine concentration (e.g., stimulated PBMC supernatant) using the assay's recommended diluent.
- Linearity Assessment: Run the diluted samples in the same assay. The measured concentration, when corrected for the dilution factor, should remain constant across the dilutions that fall within the assay's dynamic range. Significant deviations indicate the limits of the range have been reached.
- Data Interpretation: Plot the observed concentration against the expected concentration. A linear fit with an R² value >0.95 is generally considered evidence of acceptable linearity and a well-defined dynamic range.
Analysis of Platform Performance in Dynamic Range
The experimental data consistently positions MSD as the leader in dynamic range breadth [13]. The underlying electrochemiluminescence technology is a key differentiator; unlike the enzymatic amplification in ELISA, the electrochemical stimulation creates a highly amplified, low-background signal. This allows MSD assays to detect low-abundance cytokines without sacrificing the ability to measure high-abundance ones, resulting in a wider effective dynamic range [13] [28].
Luminex and CBA technologies also offer broad dynamic ranges (3-5 logs), making them suitable for comprehensive cytokine profiling in complex samples like serum [13] [25]. However, they can be more susceptible to matrix effects in plasma or serum compared to culture supernatants, which can sometimes compress the effective dynamic range or reduce concordance with ELISA [15].
The Olink PEA platform presents a unique case where the dynamic range is coupled with exceptional specificity and minimal sample consumption. The DNA-based readout is less susceptible to protein-based interference in complex matrices, helping to maintain a consistent dynamic range across different sample types [28].
A critical challenge for all multiplex assays is managing the varying dynamic ranges of different analytes within a single panel. The concentration of a high-abundance cytokine like CXCL10 (IP-10) can be thousands of times greater than a low-abundance cytokine like IL-2 in the same sample [97]. This can force a compromise in assay settings, potentially saturating the signal for some analytes while others remain near the detection limit.
The Scientist's Toolkit: Key Reagent Solutions
Successful dynamic range analysis relies on high-quality, specific reagents. The following table outlines essential materials and their functions.
Table 3: Essential Research Reagents for Cytokine Detection Assays
| Item | Function | Considerations for Dynamic Range |
|---|---|---|
| Matched Antibody Pairs (Capture & Detection) | Provide specificity for the target cytokine. | Antibody affinity and specificity directly impact the sensitivity and the upper limit of detection before saturation occurs. [98] |
| Cytokine Standards | Used to generate the standard curve for quantification. | Recombinant protein quality and accurate dilution series are fundamental for defining the dynamic range of the assay. [98] |
| Assay Diluent | Matrix for diluting standards and samples. | Must mimic the sample matrix to ensure parallel recovery; critical for accurate dilution parallelism studies. [97] |
| Signal Generation Reagents (Enzyme substrates, ECL co-reactants, etc.) | Produce the measurable signal. | The quality and linearity of the signal amplification determine the width of the dynamic range. MSD's ECL, for example, provides a wider range than colorimetric ELISA. [13] [28] |
| Quality Controls (High, Low, Negative) | Monitor inter-assay precision and accuracy. | Essential for verifying that the dynamic range and sensitivity of the assay remain consistent over time and across lots. [98] |
The choice of cytokine detection platform profoundly influences the depth and accuracy of research findings. Based on the comparative dynamic range analysis:
- For studies requiring the broadest possible dynamic range and highest sensitivity, particularly for challenging low-abundance targets, MSD is the most capable platform [13].
- For high-throughput screening of a well-defined cytokine panel where multiplexing capability is paramount, Luminex and CBA offer an excellent balance of performance, dynamic range, and efficiency [13] [25].
- In scenarios with extremely limited sample volume (e.g., pediatric studies or serial sampling), Olink PEA provides a compelling solution with a wide dynamic range and high specificity from just 1 µL of sample [28].
- Traditional ELISA remains a powerful, cost-effective tool for validating a limited number of targets where maximum specificity per analyte is required, acknowledging its narrower dynamic range [15].
Future directions in cytokine detection are leaning toward the integration of artificial intelligence (AI) and machine learning with novel biosensing technologies. These emerging platforms aim to enhance the analytical performance, interpretability, and clinical utility of cytokine diagnostics, further pushing the boundaries of sensitivity and dynamic range at the point-of-care [4]. Researchers should base their platform selection on a careful consideration of their specific research objectives, sample constraints, and the required balance between multiplexing breadth and quantitative performance across the full spectrum of cytokine concentrations.
In biomedical research, cytokines serve as critical messengers regulating immunity, inflammation, and cell communication. Their accurate measurement is fundamental to understanding disease mechanisms, discovering biomarkers, and developing new therapies. However, the field faces a significant reproducibility challenge, where studies indicate that a substantial percentage of published research results cannot be successfully replicated by independent laboratories. These reproducibility issues stem from multiple sources including protocol variations, equipment differences, operator variability, and inadequate documentation of experimental conditions. The complexity of modern cytokine profiling experiments exacerbates these challenges, as studies often involve dozens of variables that must be precisely controlled to ensure consistent outcomes. Small variations in temperature, pH, timing, reagent quality, or equipment calibration can dramatically impact experimental results, yet traditional documentation methods often fail to capture these critical details with sufficient precision.
Inter-laboratory variability represents a particularly significant challenge, as different research organizations may interpret protocols differently, use different equipment brands, or employ different standard operating procedures. These variations can lead to conflicting results that slow scientific progress and create uncertainty about the validity of research findings. This article provides a comprehensive comparison of cytokine detection methodologies through the lens of inter-laboratory validation studies, offering researchers evidence-based guidance for selecting appropriate platforms and implementing practices that enhance reproducibility across diverse laboratory environments.
Comparative Analysis of Cytokine Detection Platforms
Multiple technologies are currently employed for cytokine detection, each with distinct advantages and limitations. The enzyme-linked immunosorbent assay (ELISA) represents one of the most widely used techniques due to its simplicity, well-established protocols, and high specificity. As a single-plex method, ELISA can only detect one cytokine per well, but multiplexing can be achieved by running multiple tests in parallel, albeit with increased time, sample consumption, and costs. ELISA offers good sensitivity for many cytokines, typically in the low picogram per milliliter (pg/mL) range, though it is generally less sensitive than some newer technologies.
Luminex xMAP technology utilizes color-coded microspheres that allow for the simultaneous detection of multiple cytokines. One of Luminex's greatest advantages is its exceptional multiplexing capacity, measuring up to 500 analytes in a single sample depending on the panel. This technology provides excellent sensitivity, capable of detecting cytokine concentrations in the low pg/mL range, with some assays reaching femtogram per milliliter (fg/mL) sensitivity. The electrochemiluminescence-based Meso Scale Discovery (MSD) platform represents another advanced option, with studies indicating it demonstrates the best sensitivity in low detection limits and the broadest dynamic range among available technologies.
Inter-laboratory Performance Validation
A critical multisite comparison of high-sensitivity multiplex cytokine assays revealed substantial variability across platforms and laboratories. Four different high-sensitivity cytokine multiplex assays on Luminex or MSD platforms were evaluated for their ability to detect circulating concentrations of 13 cytokines across six laboratories. The findings demonstrated that in a majority of serum samples, interleukin-6 (IL-6), IL-8, IL-10, and tumor necrosis factor alpha (TNF-α) were detectable with at least three kits, while IL-1β was clearly detected with only one kit. Importantly, no single multiplex panel detected all cytokines effectively, and there were highly significant differences (P < 0.001) between laboratories and/or lots with all kits.
Nevertheless, the kits generally detected similar patterns of cytokine perturbation during primary HIV viremia, suggesting that while absolute concentrations may vary, relative changes in cytokine levels remain consistent across platforms. This multisite comparison suggests that current multiplex assays vary in their ability to measure serum and/or plasma concentrations of cytokines and may not be sufficiently reproducible for repeated determinations over a long-term study or in multiple laboratories, but may be useful for longitudinal studies in which relative, rather than absolute, changes in cytokines are important.
Table 1: Performance Comparison of Major Cytokine Detection Platforms
| Platform | Sensitivity | Dynamic Range | Multiplexing Capacity | Sample Volume | Inter-lab CV |
|---|---|---|---|---|---|
| ELISA | Low pg/mL | 2-3 logs | Single-plex | 100-200 μL | Not reported |
| Luminex | Low pg/mL to fg/mL | 3-5 logs | High (up to 500-plex) | 25-50 μL | Significant variations reported |
| MSD | Best sensitivity in low detection limit | Broadest dynamic range | Moderate to High | 25-50 μL | Significant variations reported |
| TR-FRET | Moderate | Moderate | Low to Moderate | Not specified | Limited data |
| CBA | Superior performance in sensitivity | Comparable to Luminex | Moderate | Not specified | Limited data |
Experimental Protocols for Robust Cytokine Detection
Standardized ELISA Protocol
The indirect sandwich ELISA represents a fundamental approach for cytokine detection with remarkable sensitivity (pg/mL or ~0.5 pM for a 15 kDa protein). The procedure involves four essential steps: (1) capturing analyte from sample with capture antibody; (2) detecting captured analyte with biotin-labeled detection antibody; (3) detection amplification with streptavidin conjugated with horseradish peroxidase (HRP); and (4) substrate addition and signal measurement via optical density with a microplate reader. After each incubation step throughout the assay, unbound reactants are washed away. Due to the binding properties of the microplates used, the plates must be blocked with an inert protein after coating with capture antibody to prevent non-specific binding.
Critical to assay performance is the optimization of antibody concentrations through checkerboard titration. The process begins with coating a 96-well high-binding microplate with four dilutions of capture antibody (typically using the manufacturer's suggested dilution as a starting point) and incubating overnight at 4°C. After washing, the plate is blocked with an appropriate buffer for 1 hour at ambient temperature. Using dilution buffer, suitable volumes of high, medium, low, and zero standards are prepared (a three-log range between high and low is usually sufficient). After the plate has been blocked and washed, standards are added and incubated for 2 hours. Subsequently, three dilutions of biotinylated detection antibody are added following another wash step, followed by another 2-hour incubation. Streptavidin-HRP is then added, incubated for 30 minutes, followed by addition of TMB substrate and incubation in the dark without shaking for 20-30 minutes. The reaction is stopped with acid, and the plate is read at the appropriate wavelengths.
Multiplex Assay Implementation
For multiplex assays such as Luminex or MSD, strict adherence to manufacturer protocols is essential for inter-laboratory consistency. Each assay must be performed strictly according to the manufacturer's protocol for serum or plasma samples, utilizing recommended sample dilutions and standard curve concentrations, with all samples and standards assayed in duplicate. Instruments should be validated using appropriate validation kits within 2 weeks of each assay and calibrated on assay days. Sample handling procedures must be standardized across laboratories; this includes consistent thawing procedures, centrifugation protocols for plasma samples, and preparation of aliquots that are refrozen at -80°C until testing to ensure identical freeze-thaw history at the time of testing in each laboratory.
A key consideration in multiplex assays is managing cross-reactivity between detection antibodies. The quality of capture and detection antibodies directly impacts specificity, and poorly optimized antibodies can result in false positives or inaccurate readings. In single-plex assays, specificity is typically high, but in multiplex assays, managing cross-reactivity between cytokines is more challenging. Cross-reactivity can occur when an antibody binds to a similar, unintended target, which is a particular concern in multiplex assays where multiple cytokines are measured simultaneously. Using well-validated, high-quality panels and referring to manufacturer-provided data on cross-reactivity helps minimize this risk.
Key Findings from Inter-laboratory Validation Studies
Inter-laboratory studies have identified multiple sources of variability that significantly impact the reproducibility of cytokine measurements. A multisite comparison revealed that there were highly significant differences (P < 0.001) between laboratories and/or lots with all kits tested. These variations persisted despite standardized protocols, indicating that subtle differences in implementation, reagent batches, or equipment calibration contribute substantially to measurement variability. Similar challenges have been observed in other methodological areas, as demonstrated by an inter-laboratory study for medical device extraction testing, which found that laboratories consistently reported analytes that were explicitly disclosed, but significant variability in quantitation was observed across different laboratories.
The same study established that both intra-laboratory (repeatability) and inter-laboratory (reproducibility) variation significantly impact measurement consistency in analytical chemistry, mirroring challenges seen in cytokine detection. These findings highlight that quantitation variability is a universal challenge in biomedical measurement systems that must be addressed through rigorous validation and standardization protocols. Another interlaboratory validation study focusing on α-amylase activity measurements found that through protocol optimization, reproducibility was greatly improved with interlaboratory coefficients of variation (CVs) ranging from 16 to 21% - up to four times lower than with the original method. This demonstrates that systematic protocol optimization can substantially enhance inter-laboratory consistency.
Strategies for Enhancing Reproducibility
Several evidence-based strategies emerge from inter-laboratory validation studies for improving reproducibility in cytokine measurement. First, protocol optimization and standardization are critical factors in reducing inter-laboratory variability. The experience from the α-amylase activity validation study demonstrates that carefully optimized protocols incorporating multiple time-point measurements at physiologically relevant temperatures (37°C versus 20°C) significantly improved reproducibility. Similarly, in histological staining, the JFRL staining method demonstrated consistent patterns across different manufacturers and facilities when proper procedures were followed, with dehydration steps being particularly crucial for optimal results.
Second, continuous, automated monitoring systems can minimize human-introduced variability. Studies of preclinical research models have found that digital home cage monitoring technologies enable continuous, non-invasive observation, minimizing human interference and capturing rich behavioral and physiological data through automated, unbiased measurement. The integration of such automated systems in cytokine measurement could similarly reduce operator-dependent variability. Third, robustness testing during method validation provides a systematic approach to identifying critical parameters that affect assay performance. As defined by the International Conference on Harmonization (ICH), "The robustness/ruggedness of an analytical procedure is a measure of its capacity to remain unaffected by small but deliberate variations in method parameters and provides an indication of its reliability during normal usage."
Table 2: Essential Research Reagent Solutions for Cytokine Detection
| Reagent/Material | Function | Implementation Considerations |
|---|---|---|
| Matched Antibody Pairs | Capture and detect specific cytokines | Monoclonal for capture; mono- or polyclonal biotinylated for detection; require checkerboard titration optimization |
| Cytokine Standards | Quantification reference | Recombinant proteins; require three-log range between high and low standards |
| Blocking Buffers | Prevent non-specific binding | Multiple options available (BSA, Blotto, Casein, Superblock); optimal buffer determined experimentally |
| Streptavidin-Conjugated HRP | Detection amplification | Typically diluted 1:20,000; alternative: streptavidin-conjugated IR dye for multiplex systems |
| TMB Substrate | Signal generation | 1% TMB in DMSO diluted in acetate buffer with Hâ‚‚Oâ‚‚; light-sensitive and carcinogenic |
| Wash Buffer | Remove unbound reactants | PBS with 0.05% Tween-20, pH 7.4; critical after each incubation step |
Visualization of Inter-laboratory Validation Workflow
The following diagram illustrates the systematic workflow for conducting inter-laboratory validation of cytokine detection methods, highlighting critical decision points and standardization requirements:
The evidence from multiple inter-laboratory validation studies clearly demonstrates that reproducibility challenges in cytokine detection stem from multiple sources, including protocol variations, equipment differences, reagent lot variability, and operator technique. While no single platform emerges as perfect for all applications, understanding the performance characteristics of each technology enables researchers to select the most appropriate method based on their specific needs. For studies requiring absolute quantification across multiple laboratories, careful standardization and validation procedures are essential. For longitudinal studies where relative changes are more important than absolute values, multiplex platforms offer significant practical advantages despite their inter-laboratory variability.
Future improvements in cytokine detection reproducibility will likely come from several directions. First, the adoption of digital technologies and artificial intelligence for protocol standardization, experimental optimization, and quality control shows promise for ensuring consistent results across different laboratory environments. Generative AI systems can create standardized experimental protocols that capture critical details often overlooked in traditional documentation approaches. Second, advanced robustness testing during method development can identify critical parameters that require tight control to maintain reproducibility. Finally, international standardization initiatives that establish reference methods and materials for cytokine detection could substantially improve inter-laboratory comparability, much as has been achieved in other areas of clinical chemistry.
As cytokine measurements continue to play an increasingly important role in both basic research and clinical applications, addressing these reproducibility challenges becomes ever more critical. By implementing the validated protocols, robustness testing frameworks, and standardization practices outlined in this review, researchers can enhance the reliability and translational potential of their cytokine profiling studies.
For researchers and drug development professionals selecting cytokine detection methods, the decision involves critical trade-offs between throughput, sample consumption, and operational complexity. This guide provides an objective comparison of major technologies—from traditional ELISA to advanced multiplex and homogeneous platforms—using published experimental data to highlight how each method balances these competing factors. The analysis reveals that while multiplex immunoassays dramatically increase data density from limited samples, and homogeneous assays eliminate washing steps to streamline workflow, the optimal choice fundamentally depends on specific project requirements for data breadth, sensitivity, and compatibility with high-throughput automation.
Quantitative Comparison of Key Performance Metrics
The following table synthesizes experimental data from published studies and technical literature to compare the operational characteristics of major cytokine detection platforms.
Table 1: Performance and Operational Comparison of Cytokine Detection Methods
| Detection Method | Sample Consumption per Analyte (μL) | Multiplexing Capacity | Approximate Assay Duration | Throughput Potential | Key Operational Considerations |
|---|---|---|---|---|---|
| ELISA | 100-200 [25] | Single-plex [25] | Several hours [25] [11] | Moderate (96-well format) [25] | Multiple wash and incubation steps; low automation compatibility [11] |
| Luminex xMAP | 25-50 (for multiple analytes) [25] | High (30-500 analytes) [25] | 2.5 - 4 hours [99] | High (96- or 384-well, automated systems) [25] | Bead-based assay requires vacuum wash systems; complex data analysis [25] |
| MSD (ECL) | Similar to Luminex [25] | High (customizable panels) [25] | Not explicitly stated | High [13] | Broad dynamic range; cited as one of the most sensitive technologies [13] |
| Flow Cytometry (CBA) | ~50 [13] | Moderate | ~4 hours including staining | Cell throughput high; sample throughput moderate | Requires expensive equipment and technical expertise [11] |
| Lumit Immunoassay | Minimal (homogeneous format) [11] | Low to Moderate (depends on panel) | ~70 minutes [11] | Very High (384-well format, no-wash) [11] | No-wash, homogeneous protocol; easy automation; requires luminometer [11] |
| Intracellular Staining | Requires millions of cells [100] | High (11+ colors) [100] | Multi-day protocol [100] | Low to Moderate | Complex workflow with cell stimulation, fixation, and permeabilization [100] |
Detailed Experimental Protocols and Methodologies
Multiplex Immunoassay (Luminex/xMAP Technology)
The bead-based multiplex immunoassay protocol allows simultaneous quantification of dozens of cytokines from a single small sample volume, making it particularly valuable for limited clinical specimens [77] [25].
Key Protocol Steps [77]:
- Sample Preparation: Serum or plasma samples are centrifuged through a 0.22 μm filter to remove debris. Interfering heterophilic antibodies are removed by pre-absorption with protein-L coated plates without depleting cytokines.
- Assay Procedure:
- A mixture of magnetic or polystyrene microspheres, each coupled with a unique capture antibody, is added to a filter plate.
- Samples or standards are added and incubated for 1 hour.
- After washing, a cocktail of biotinylated detection antibodies is added and incubated for 1 hour.
- Streptavidin conjugated to R-phycoerythrin is added, and after a final wash, the beads are resuspended.
- The plate is analyzed using a dedicated analyzer (e.g., Bio-Plex/Luminex) which identifies each bead set and quantifies the bound fluorescence.
- Critical Pre-Analytical Considerations: Cytokine stability varies significantly. While cytokines are stable for up to 2 years at -80°C, degradation of up to 75% was observed for some cytokines (e.g., IL-1α, IL-1β, IL-10) after 4 years. Most cytokines degrade with repeated freeze-thaw cycles [77].
Homogeneous Bioluminescent Immunoassay (Lumit Technology)
This no-wash protocol is designed for maximum throughput and minimal hands-on time, ideal for drug screening [11].
Key Protocol Steps [11]:
- Antibody Labeling: Primary antibodies specific to the target cytokine are chemically labeled with two subunits of a luciferase enzyme: SmBiT and LgBiT.
- Assay Procedure:
- Labeled antibodies are added directly to the sample in a microplate well.
- The plate is incubated for 1 hour. If the target cytokine is present, it brings the SmBiT and LgBiT subunits into proximity, forming a functional enzyme.
- A luminescent substrate is added, and the signal is read immediately on a standard luminometer. The signal generated is proportional to the cytokine concentration.
- Throughput and Performance Data: This technology has been successfully automated in a 384-well format. In a validation study measuring IL-2 release from stimulated PBMCs, the assay demonstrated excellent performance for high-throughput screening (HTS), with Z' factors ≥ 0.68 and a broad linear range spanning over three logs of cytokine concentration [11].
Intracellular Cytokine Staining with Flow Cytometry
This protocol enables detection of cytokine production at the single-cell level, identifying specific immune cell subsets.
Key Protocol Steps [100]:
- Cell Activation: Isolated peripheral blood mononuclear cells (PBMCs) are stimulated for ~24 hours with agents like immobilized anti-CD3 and soluble anti-CD28 to induce cytokine production.
- Protein Transport Inhibition: Brefeldin A is added for approximately 4 hours before harvesting to block cytokine secretion, retaining proteins within the cell.
- Cell Staining:
- Cells are first stained with fluorescently-labeled antibodies against cell surface markers (e.g., CD3, CD4).
- Cells are then fixed and permeabilized using specialized buffers to make intracellular proteins accessible.
- Cells are stained with fluorescent antibodies against intracellular cytokines (e.g., IFN-γ, IL-4, IL-17A) or transcription factors (e.g., FoxP3).
- Data Acquisition and Analysis: Cells are analyzed by multi-color flow cytometry. The resulting data allows for the identification of specific T-helper cell subsets (Th1, Th2, Th17, Treg) based on their cytokine and marker profiles [100].
Operational Workflows and Decision Pathways
The following diagrams illustrate the core operational workflows for the key assay types and a logical pathway for selecting the appropriate method.
Comparative Assay Workflows
Diagram 1: Core operational workflows for three classes of cytokine detection methods, highlighting the significant difference in step complexity and hands-on time.
Method Selection Decision Pathway
Diagram 2: A decision pathway to guide the selection of a cytokine detection method based on key experimental requirements.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful cytokine detection requires carefully selected reagents and materials. The following table details essential components for setting up these assays.
Table 2: Key Research Reagent Solutions for Cytokine Detection
| Reagent / Material | Function | Key Considerations |
|---|---|---|
| Matched Antibody Pairs (Capture & Detection) | Specifically bind the target cytokine in sandwich immunoassays (ELISA, Luminex, MSD). | Antibody quality directly impacts specificity and sensitivity. Check for cross-reactivity, especially in multiplex panels [5] [25]. |
| Brefeldin A | Inhibits protein transport, allowing intracellular accumulation of cytokines for flow cytometry detection [100]. | Critical for detecting cytokine-producing cells. Typically added for the last 4-6 hours of cell stimulation. |
| Luminex Microspheres | Color-coded beads that serve as the solid phase for capture antibodies in multiplex assays [77] [25]. | Beads with distinct spectral signatures are coupled to different antibodies, enabling multiplexing. |
| Blocking Buffers (e.g., BSA, Blotto, Casein) | Reduce non-specific binding by occupying unused protein-binding sites on surfaces [5]. | The optimal buffer (e.g., BSA, Blotto, Casein) must be determined empirically to minimize background [5]. |
| Stimulation Cocktail (e.g., anti-CD3/CD28, PMA/Ionomycin) | Activates T-cells ex vivo to induce cytokine production for intracellular detection [100]. | Required for intracellular cytokine staining. The specific stimulant can influence the cytokine profile produced. |
| Streptavidin-Phycoerythrin / Streptavidin-HRP | Signal generation system. Binds to biotinylated detection antibodies and produces a fluorescent (PE) or colorimetric (HRP) signal [77] [5]. | PE is common for bead-based and flow assays. HRP is used with colorimetric (TMB) substrates in ELISA. |
| NanoBiT Subunits (SmBiT/LgBiT) | Enzyme fragments used in Lumit assays. They complement to form a functional luciferase when brought together by a target cytokine [11]. | Enable homogeneous, no-wash assay formats. Antibodies must be specifically labeled with these subunits. |
| Fixation/Permeabilization Buffers | Preserve cell structure and permeabilize the cell membrane to allow intracellular antibody access for flow cytometry [100]. | Essential for intracellular staining. Commercial kits are available to ensure optimal results. |
Critical Considerations for Data Integrity
- Assay Standardization: Significant differences in absolute cytokine concentrations can be measured using different commercial kits, even when targeting the same analyte [99]. For longitudinal or multi-center studies, using the same validated kit and platform throughout is critical. Where possible, reference to World Health Organization (WHO) international standards is recommended [99].
- Sample Handling: Pre-analytical variables are a major source of variability. The stability of cytokines in plasma and serum is highly variable, with some cytokines degrading significantly after multiple freeze-thaw cycles or during long-term storage, even at -80°C [77]. Consistent sample collection, processing, and storage protocols are non-negotiable for reliable results.
- Platform Validation: No single platform is universally superior. A comparative analysis noted that MSD demonstrated exceptional sensitivity, while CBA (a flow cytometry-based bead assay) was highlighted as a strong candidate for high-throughput screening with multiplexing capability [13]. Researchers should validate their chosen platform for their specific set of target cytokines and sample matrices.
Cytokines are pivotal signaling proteins that regulate immunity, inflammation, and hematopoiesis, making their accurate quantification essential for both basic research and clinical decision-making [101] [4]. The selection of appropriate cytokine detection technologies significantly influences research outcomes, diagnostic accuracy, and therapeutic development across diverse fields including immuno-oncology, infectious diseases, and autoimmune disorders [28] [79]. This guide provides a comprehensive comparison of current cytokine detection platforms, focusing on their distinct applications in discovery research versus clinical validation contexts. Discovery research often prioritizes multiplexing breadth and novel biomarker identification, whereas clinical validation demands high sensitivity, robust reproducibility, and regulatory compliance [102] [103]. Understanding these divergent requirements enables researchers to select optimal technologies for each stage of the development pipeline, ultimately accelerating the translation of biomarker discoveries into clinically actionable diagnostic tools.
The evolving landscape of cytokine detection reflects broader trends in precision medicine, where technological advances are enabling increasingly sensitive, multiplexed, and computationally enhanced analyses [4] [103]. Conventional methods like ELISA are now complemented by ultra-sensitive platforms capable of detecting cytokines at femtogram-per-milliliter concentrations, revealing previously unquantifiable biological processes [8]. Simultaneously, artificial intelligence (AI) and machine learning are transforming data analysis approaches, allowing researchers to extract meaningful patterns from complex cytokine profiles [101] [79]. This guide examines these technological innovations through the dual lenses of discovery research and clinical application, providing researchers with practical frameworks for technology selection based on specific project requirements, sample constraints, and intended applications.
Technology Comparison: Performance Metrics Across Platforms
Analytical Performance Specifications
Table 1: Comparative analytical performance of major cytokine detection platforms
| Technology | Sensitivity Range | Dynamic Range | Sample Volume | Multiplexing Capacity | Key Strengths |
|---|---|---|---|---|---|
| ELISA | Moderate (pg/mL) | Moderate (2-3 logs) | 50-100 μL | Single-plex | High specificity, well-established, gold standard [103] |
| Luminex | Moderate (pg/mL) | Wide (3-4 logs) | 25-50 μL | Medium (up to 50-80 analytes) | Good profiling capacity, flexible panels [28] |
| MSD | High (sub-pg/mL) | Wide (3-4 logs) | 20-40 μL | Medium (up to 10-plex per well) | Broad dynamic range, low background [28] [103] |
| Olink PEA | High (low pg/mL) | Wide | ~1 μL | High (up to 96-plex) | Excellent specificity, minimal sample requirement [28] |
| Simoa | Ultra-sensitive (fg/mL) | Wide (3-4 logs) | 50 μL | Low to medium | Single-molecule detection, exceptional sensitivity [8] |
| Flow Cytometry | Moderate (pg/mL) | Moderate | 50-100 μL | Medium (up to 12-plex) | Instrument accessibility, rapid results [79] |
Operational and Economic Considerations
Table 2: Operational characteristics and application suitability
| Platform | Hands-on Time | Time to Results | Cost per Sample | Best-Suited Applications |
|---|---|---|---|---|
| ELISA | Moderate | 4-6 hours | $$ | Targeted analysis, clinical validation [103] |
| Luminex | Moderate | 3-4 hours | $$ | Biomarker discovery, exploratory research [28] |
| MSD | Moderate | 3-4 hours | $$ | Clinical trials, translational studies [103] |
| Olink PEA | Low | 1-2 days | $$$ | Discovery with limited samples, precision medicine [28] |
| Simoa | Low to moderate | 2-3 hours | $$$ | Low-abundance cytokines, therapy monitoring [8] |
| Flow Cytometry | Low (with one-step) | 1.5 hours | $ | Rapid profiling, clinical diagnostics [79] |
Case Study 1: Discovery Research Applications
AI-Driven Cytokine Inference for Novel Biomarker Identification
Discovery research increasingly leverages computational approaches to overcome limitations in cytokine measurement. The TSCytoPred framework exemplifies this trend by employing deep learning to infer cytokine expression trajectories from gene expression data, effectively addressing the challenge of limited cytokine profiling in temporal studies [101]. This approach is particularly valuable in discovery settings where comprehensive time-series cytokine data may be unavailable due to cost constraints or sample volume limitations. The model identifies genes relevant for predicting target cytokines through interaction relationships and high correlation, subsequently utilizing these genes in a neural network with interpolation capabilities to estimate cytokine expression between observed time points [101].
Performance evaluations demonstrate that TSCytoPred significantly outperforms baseline regression methods, achieving superior coefficient of determination (R²) and lower mean absolute error (MAE) [101]. This computational framework enables researchers to extract additional value from existing gene expression datasets, potentially revealing novel cytokine-disease associations without requiring additional wet-lab experiments. The model's ability to handle datasets with limited time points and irregular temporal gaps makes it particularly suitable for real-world discovery research, where sample collection often occurs at inconsistent intervals [101].
Multiplexed Profiling for Disease Subtyping
Discovery research frequently employs highly multiplexed platforms to identify cytokine signatures associated with disease states and treatment responses. In one application, researchers utilized a 12-plex flow cytometry-based assay to profile cytokine patterns in COVID-19 and HBV patients, subsequently applying machine learning algorithms to predict disease severity and viral load [79]. This approach exemplifies the discovery research paradigm, where broad profiling generates hypothesis-free data for subsequent computational analysis.
The technical workflow incorporated both supervised machine learning algorithms (logistic regression, random forest, and support vector machine) and unsupervised approaches (t-SNE clustering) to extract meaningful biological insights from complex cytokine data [79]. The integration of multiple cytokines, along with ALT and AST features, enabled more accurate prediction of HBV viral load than any single biomarker could provide, demonstrating the value of multiplexed approaches in discovery research [79]. Methodological innovations included lyophilization of assay reagents and single-step detection, significantly simplifying procedures while maintaining performance comparable to conventional approaches [79].
Diagram 1: Discovery research workflow emphasizing high-plex profiling and computational analysis
Case Study 2: Clinical Validation Applications
Ultra-Sensitive Detection for Patient Stratification
Clinical validation requires technologies capable of reliably quantifying low-abundance cytokines with high precision and reproducibility. Simoa (Single Molecule Array) technology addresses this need through digital immunoassay technology that enables single-molecule detection, achieving sensitivity in the femtogram-per-milliliter range—orders of magnitude better than conventional ELISA [8]. This exceptional sensitivity is particularly crucial in clinical applications where low-abundance cytokines may serve as early indicators of treatment response or adverse effects.
In a validation study conducted by Frontage Laboratories, the Simoa platform demonstrated exceptional performance characteristics essential for clinical applications: intra- and inter-assay coefficients of variation (CVs) under 10%, minimal matrix effects in serum, and excellent recovery in spike-and-recovery and dilution linearity assessments [8]. These metrics meet the rigorous standards required for clinical biomarker validation, supporting the platform's use in therapeutic areas including immuno-oncology, autoimmune conditions, and infectious disease profiling [8]. The ability to detect cytokine changes earlier in longitudinal studies provides clinicians with timely information for treatment decisions, potentially improving patient outcomes through more personalized therapeutic interventions.
Regulatory-Compliant Assays for Clinical Trials
Clinical validation necessitates technologies that comply with evolving regulatory standards for biomarker qualification. Meso Scale Discovery (MSD) platforms exemplify this category, offering electrochemiluminescence-based detection that provides up to 100 times greater sensitivity than traditional ELISA while supporting multiplexed analysis [103]. This combination of sensitivity and multiplexing capability enables comprehensive biomarker assessment while conserving valuable clinical samples—a critical consideration in trials with limited specimen volumes.
The regulatory landscape for biomarker validation increasingly emphasizes fit-for-purpose approaches, where validation rigor corresponds to the biomarker's intended clinical use [103]. Advanced technologies like MSD and LC-MS/MS are gaining favor with regulatory agencies due to their superior precision, sensitivity, and freedom from matrix effects [103]. Evidence of this regulatory acceptance includes the FDA's exploration of AI/ML-based regulatory frameworks and the EMA's emphasis on biomarker qualification in its Regulatory Science Strategy to 2025 [104] [103]. The economic advantage of multiplexed platforms further supports their clinical adoption, with one analysis demonstrating that measuring four inflammatory biomarkers (IL-1β, IL-6, TNF-α, and IFN-γ) using MSD multiplex assays reduced costs by approximately $42 per sample compared to individual ELISAs [103].
Diagram 2: Clinical validation workflow emphasizing regulatory compliance and analytical rigor
Comparative Analysis: Discovery versus Clinical Applications
Methodological Priorities Across Development Stages
The technological requirements for cytokine detection diverge significantly between discovery research and clinical validation contexts, reflecting their distinct objectives and constraints. Discovery research prioritizes multiplexing capacity, novel biomarker identification, and hypothesis generation, often utilizing platforms like Olink PEA and Luminex that can simultaneously quantify dozens to hundreds of analytes from minimal sample volumes [28]. These platforms enable researchers to cast a wide net, identifying potential cytokine signatures associated with disease states or treatment responses without prior knowledge of specific involved cytokines. In contrast, clinical validation emphasizes analytical robustness, regulatory compliance, and clinical utility, favoring technologies with demonstrated precision, reproducibility, and regulatory acceptance such as MSD and validated ELISA methods [103].
The transition from discovery to clinical application presents substantial challenges, with only approximately 0.1% of potentially clinically relevant cancer biomarkers described in literature progressing to routine clinical use [103]. This high attrition rate reflects both biological complexity and methodological limitations in translating discovery findings to clinically applicable tests. Platforms that successfully bridge this gap typically offer multiplexing capabilities sufficient for verification studies while maintaining the analytical rigor required for clinical applications. MSD's U-PLEX platform exemplifies this balanced approach, allowing researchers to design custom biomarker panels that maintain analytical performance across discovery and verification stages [103].
Practical Implementation Considerations
Table 3: Technology selection guide based on research phase and requirements
| Research Context | Recommended Platforms | Key Selection Criteria | Implementation Timeline |
|---|---|---|---|
| Early Discovery | Olink, Luminex, Flow Cytometry | Maximum plex, minimal sample, cost efficiency | Short (days to weeks) |
| Biomarker Verification | MSD, Custom Panels | Balance of plex and precision, fit-for-purpose | Medium (weeks to months) |
| Clinical Validation | Simoa, Validated ELISA, MSD | Regulatory readiness, robustness, sensitivity | Long (months to years) |
| Point-of-Care | Emerging Biosensors | Speed, ease of use, connectivity | Variable |
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 4: Key research reagents and materials for cytokine detection
| Reagent/Material | Function | Example Applications | Technical Notes |
|---|---|---|---|
| Capture Antibody-Modified Microspheres | Analyte-specific binding in multiplex assays | Luminex, flow cytometry-based multiplexing | Spectral encoding enables multiplexing; coupling efficiency critical [79] |
| PE-Labeled Detection Antibodies | Signal generation in immunoassays | Flow cytometry, MSD, Luminex | Reporter intensity proportional to analyte concentration [79] |
| Lyophilization Stabilizers | Reagent preservation without cold chain | One-step FCM assays, point-of-care applications | Trehalose/mannitol formulations maintain stability [79] |
| Electrochemiluminescent Tags | Signal generation in MSD platforms | MSD immunoassays | Sulfo-tag labels emit light upon voltage application [28] [103] |
| DNA Oligonucleotide Tags | Proximity extension in PEA assays | Olink platform | Dual antibody binding required for DNA hybridization/extension [28] |
| Quality Controls | Assay performance monitoring | All clinical validation studies | Essential for demonstrating assay reproducibility [103] [8] |
Emerging Trends and Future Directions
AI-Enhanced Cytokine Analytics
Artificial intelligence is progressively transforming cytokine research through enhanced analytical capabilities and novel computational approaches. Machine learning algorithms are being integrated with multiplexed cytokine data to improve disease classification, predict treatment responses, and identify biologically relevant biomarker signatures [79]. These approaches leverage pattern recognition capabilities that often exceed traditional statistical methods, particularly when analyzing high-dimensional datasets with complex interactions between multiple cytokines and clinical variables.
The TSCytoPred framework represents a particularly advanced application of AI in cytokine research, enabling temporal inference of cytokine expression from more readily available gene expression data [101]. This approach addresses a fundamental challenge in longitudinal clinical studies—the difficulty of collecting frequent, comprehensive cytokine measurements—by computationally inferring cytokine trajectories from more feasible gene expression profiling. Performance validation in COVID-19 datasets demonstrated that cytokine data inferred by TSCytoPred enhanced severity risk predictions, confirming the clinical utility of this approach [101]. As AI methodologies continue evolving, their integration with cytokine detection platforms will likely expand, potentially enabling more predictive biomarker signatures and personalized treatment approaches.
Technological Convergence: Multiplexing, Sensitivity, and Accessibility
The future of cytokine detection reflects a convergence of technological capabilities, with emerging platforms simultaneously improving multiplexing capacity, analytical sensitivity, and operational accessibility. Point-of-care biosensing technologies exemplify this trend, achieving limits of detection as low as 0.01-100 pg/mL with dynamic ranges spanning 3-4 orders of magnitude while using only 1-50 μL of sample and delivering results within 5-30 minutes [4]. These platforms increasingly incorporate AI-enabled signal processing and calibration, enhancing their analytical performance and reliability while maintaining the rapid turnaround times essential for clinical decision-making.
This technological convergence is particularly evident in the emergence of simplified workflow solutions like the one-step flow cytometry-based assay, which incorporates lyophilized reagents to eliminate cold chain requirements and reduces hands-on time while maintaining analytical performance comparable to conventional approaches [79]. Similarly, platforms like Simoa's Cytokine Advantage PLUS line offer both single-plex and multiplex assays on a single instrument system, supporting flexible experimental designs from initial discovery to clinical validation [8]. These innovations reflect a broader trend toward integrated solutions that maintain the rigorous analytical performance required for clinical applications while offering the practicality and accessibility needed for widespread implementation across diverse research and healthcare settings.
Conclusion
Selecting the optimal cytokine detection method requires careful consideration of sensitivity requirements, multiplexing needs, sample limitations, and research objectives. Traditional ELISA offers reliability for single-analyte studies, while multiplex platforms like Luminex and MSD provide comprehensive profiling capabilities with MSD demonstrating superior sensitivity and dynamic range. For ultra-sensitive detection of low-abundance cytokines, digital immunoassays like Simoa represent a breakthrough with femtogram-per-milliliter sensitivity. Future directions point toward increased multiplexing capabilities, standardized validation protocols, real-time monitoring technologies, and point-of-care applications. By aligning methodological strengths with specific research goals, scientists can generate more reliable, reproducible cytokine data to advance both basic immunology research and clinical translation in drug development.
References
- 1. Performance evaluation of FlowCytomix assays to quantify ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4659018/]
- 2. Dictionary of immune responses to cytokines at single-cell ... [https://www.nature.com/articles/s41586-023-06816-9]
- 3. Systematic investigation of cytokine signaling activity at the ... [https://www.nature.com/articles/s41592-021-01274-5]
- 4. AI, multiplexing, and point-of-care biosensing technologies [https://pubmed.ncbi.nlm.nih.gov/41175281/]
- 5. Detection and Quantification of Cytokines and Other ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5659280/]
- 6. Mouse-Specific Single cell cytokine activity prediction and ... [https://journals.plos.org/ploscompbiol/article?id=10.1371/journal.pcbi.1013475]
- 7. Comparative effects of three SARS-CoV-2 inactivation ... [https://www.sciencedirect.com/science/article/pii/S0166093425001375]
- 8. Unlocking Ultra-Sensitive Cytokine : Insights... | Quanterix Detection [https://www.quanterix.com/blog-unlocking-ultra-sensitive-cytokine-detection-insights-from-the-frontage-amp-quanterix-webinar/]
- 9. Enhanced Label-Free Nanoplasmonic Cytokine Detection in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9627400/]
- 10. Effects of serum and plasma matrices on multiplex immunoassays... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4332596/]
- 11. High-Throughput Cytokine Detection with Lumit® Technology [https://www.promega.com/resources/pubhub/2024/high-throughput-cytokine-detection-with-lumit-technology/]
- 12. Label-free electrochemical biosensor for direct detection of ... [https://www.sciencedirect.com/science/article/abs/pii/S003991402400105X]
- 13. Comparative Analysis of Multiple Immunoassays for ... [https://www.sciencedirect.com/science/article/pii/S2472555222066473]
- 14. Multisite Comparison of High-Sensitivity Multiplex Cytokine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3147360/]
- 15. ELISA AND MULTIPLEX TECHNOLOGIES FOR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2562869/]
- 16. Mouse-Specific Single cell cytokine activity prediction and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12469201/]
- 17. Cross-platform comparison of highly-sensitive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10948291/]
- 18. Cross-platform comparison of highly sensitive ... [https://www.sciencedirect.com/science/article/pii/S2590153220300070]
- 19. Evaluation Of Highly Sensitive Immunoassay Technologies ... [https://www.quanterix.com/posters/evaluation-highly-sensitive-immunoassay-technologies-quantitative/]
- 20. Comparison of Rapid Cytokine Immunoassays for ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2022.940030/full]
- 21. Simplified flow cytometry-based assay for rapid multi-cytokine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12245854/]
- 22. Comparing machine learning screening approaches using ... [https://www.nature.com/articles/s41598-024-63707-3]
- 23. Comparison of ELISA and flow cytometry for measurement ... [https://www.degruyterbrill.com/document/doi/10.1515/tjb-2017-0164/html?lang=en&srsltid=AfmBOorh468tqGNv65cfzT7WSl_2V4zzWHr_V13DkNrf51QDoH9R1tut]
- 24. Quantitative Validation and Comparison of Multiplex ... [https://www.sciencedirect.com/science/article/pii/S2472555222079229]
- 25. How to Choose the Right Cytokine Detection Method for ... [https://cytokine.creative-proteomics.com/choosing-right-cytokine-detection-method-research-success.htm]
- 26. Accurate Cancer Diagnosis and Treatment Monitoring ... [https://pubmed.ncbi.nlm.nih.gov/40340378/]
- 27. Digital biomarkers for precision diagnosis and monitoring ... [https://www.nature.com/articles/s41746-024-01217-2]
- 28. Olink Cytokine Panel vs Other Cytokine Detection Methods [https://olinkpanel.creative-proteomics.com/knowledge/olink-cytokine-panel-vs-other-methods.html]
- 29. ELISA vs. Multiplex Assays: Which Is Better for Cytokine ... [https://synapse.patsnap.com/article/elisa-vs-multiplex-assays-which-is-better-for-cytokine-detection]
- 30. Comparison of ELISA and flow cytometry for measurement ... [https://www.degruyterbrill.com/document/doi/10.1515/tjb-2017-0164/html?lang=en&srsltid=AfmBOooFtUKjoGewO36eRn43iAV_uAAiyhdTqyks4UVDIDrQVlR9e0c5]
- 31. ELISA versus ELISpot: Which assay is right for your ... [https://www.mabtech.com/knowledge-hub/elisa-versus-elispot-which-assay-right-your-research]
- 32. The Ultimate Guide To Using Elisa Kits For Cytokine ... [https://www.biomatik.com/blog/ultimate-guide-using-elisa-kits-for-cytokine-detection/]
- 33. A Simple, Highly Sensitive, and Highly Specific Dot-Blot- ... [https://www.mdpi.com/2414-6366/10/10/279]
- 34. The difference between sensitivity and detection range in ... [https://www.bosterbio.com/blog/post/the-difference-between-sensitivity-and-the-minimum-level-of-assay-range-in-elisa-testing?srsltid=AfmBOorZKqGg-9kkXUhsX0KXu35YS3Y_OBgSKz_30t9aJequZcP1r7vZ]
- 35. ELISPOT protocol [https://www.abcam.com/en-us/technical-resources/protocols/elispot]
- 36. ELISA vs. ELISpot: Which assay is right for your research? [https://www.bio-connect.nl/news/elisa-vs-elispot-which-assay-is-right-for-your-research/]
- 37. A comparison of ELISpot and FluoroSpot with flow ... [https://www.mabtech.com/knowledge-hub/comparison-elispot-and-fluorospot-flow-cytometry-methods]
- 38. Validation of an IFN-gamma ELISpot assay to measure ... [https://www.nature.com/articles/s41434-020-00214-w]
- 39. Comparison between enzymeâ€linked immunospot assay and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9449588/]
- 40. ELISPOT Assays in 384-Well Format: Up to 30 Data Points ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4381210/]
- 41. High resolution as a key feature to perform accurate ... [https://pubmed.ncbi.nlm.nih.gov/15937349/]
- 42. Multiplex Bead Array Assays: Performance Evaluation and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1534009/]
- 43. Comparing Luminex and ELISA Methods [https://cytokine.creative-proteomics.com/maximizing-accuracy-in-cytokine-analysis-comparing-luminex-and-elisa-methods.htm]
- 44. Luminex® Multiplexing Platforms Comparison [https://www.sigmaaldrich.com/US/en/technical-documents/product-supporting/milliplex/luminex-multiplexing-platforms-comparison?srsltid=AfmBOorQGX6VaYwijIDCq3r__Y1T92ZH_JNJguQbKmiTpx8tZDZkPmkW]
- 45. Comparative Overview of Luminex and MSD Platforms For ... [https://kcasbio.com/blogs/comparative-overview-of-luminex-and-msd-platforms-for-biomarker-analysis/]
- 46. Sources of variability in Luminex bead-based cytokine ... [https://www.sciencedirect.com/science/article/abs/pii/S002217592400084X]
- 47. Optimization and evaluation of Luminex performance with ... [https://bmcimmunol.biomedcentral.com/articles/10.1186/s12865-016-0182-8]
- 48. Comparative evaluation of Luminex based assays for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10091782/]
- 49. Comparison of Bead-Based Fluorescence Versus Planar ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2020.572634/full]
- 50. Why Electrochemiluminescence [https://www.mesoscale.com/en/technical_resources/our_technology/ecl]
- 51. Development of a Sensitive and Reliable Meso Scale ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11675039/]
- 52. A highly sensitive electrochemiluminescence ... [https://www.sciencedirect.com/science/article/abs/pii/S0165572810000093]
- 53. Meso Scale Discovery - MSD [https://cellcarta.com/meso-scale-discovery-platform/]
- 54. A novel high-sensitivity electrochemiluminescence (ECL ... [https://pubmed.ncbi.nlm.nih.gov/22890005/]
- 55. Single-molecule immunoassay technology: Recent advances [https://www.sciencedirect.com/science/article/abs/pii/S0039914023006549]
- 56. Single Molecule Protein Detection With Attomolar ... [https://www.quanterix.com/posters/single-molecule-protein-detection-attomolar-sensitivity-using/]
- 57. Comparative Analysis of SiMoA and Ella Immunoassay ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12134389/]
- 58. Ultrasensitive IFN-α Detection with Simoa® Technology [https://www.quanterix.com/blog-the-evolution-of-ifn-a-measurement-how-simoa-is-driving-new-breakthroughs/]
- 59. Ultrasensitive interferons quantification reveals different ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1529582/full]
- 60. A Comparison of Biofluid Cytokine Markers across Platform ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6289877/]
- 61. A cytometric bead array for the measurement of plasma ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11928653/]
- 62. Ultrasensitive digital quantification of cytokines and ... [https://www.nature.com/articles/s41467-020-16124-9]
- 63. Exploring Cytokine Detection Service Trends 2025-2033 [https://www.marketreportanalytics.com/reports/cytokine-detection-service-52457]
- 64. Optimization of analytical and pre-analytical variables ... [https://www.sciencedirect.com/science/article/abs/pii/S0731708505006680]
- 65. Pre-analytical sample handling effects on blood cytokine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8359910/]
- 66. Blood Proteomics: Serum or Plasma – Which Should You ... [https://www.metwarebio.com/blood-proteomics-serum-vs-plasma/]
- 67. Comparison of serum and plasma as a source of blood ... [https://www.merckmillipore.com/HN/es/tech-docs/paper/1566750]
- 68. Effect of anticoagulants on multiplexed measurement ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3449030/]
- 69. Measuring Cytokine Levels in Serum or Plasma [https://sanguinebio.com/pbmc-basics/considerations-for-measuring-cytokine-levels-in-serum-or-plasma/?srsltid=AfmBOorvCNa-AZOpnOiA8BseYl9GaK0i4wDwBWYbopIoLEIbOIU9ox7X]
- 70. A Method for Comparing Proteins Measured in Serum and ... [https://www.sciencedirect.com/science/article/pii/S1535947625000994]
- 71. The Importance of Cytokine Detection and Analysis [https://www.bioagilytix.com/blog/the-importance-of-cytokine-detection-and-analysis/]
- 72. The effect of storage time and freeze-thaw cycles on the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3900085/]
- 73. Impact of Freeze-Thaw Cycles on Circulating Inflammation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6411278/]
- 74. Evaluating the long-term biological stability of cytokine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10729172/]
- 75. Effects of Production Method and Repeated Freeze Thaw ... [https://www.frontiersin.org/journals/veterinary-science/articles/10.3389/fvets.2021.759828/full]
- 76. Effect of very long-term storage and multiple freeze and ... [https://www.nature.com/articles/s41598-024-55720-3]
- 77. Prerequisites for cytokine measurements in clinical trials with ... [https://bmcimmunol.biomedcentral.com/articles/10.1186/1471-2172-10-52]
- 78. Reliability, stability during long-term storage, and intra ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10873926/]
- 79. Simplified flow cytometry-based assay for rapid multi- ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1594141/full]
- 80. Matrix Interference in Sandwich ELISA Kits [https://assaybiotechnology.com/site/matrix-interference]
- 81. Discover How to Achieve High Sensitivity Cytokine ... [https://www.quanterix.com/webinars/discover-how-to-achieve-high-sensitivity-cytokine-biomarker-quantification-in-complex-samples-using-simoa-assays/]
- 82. Standard Addition Procedure in Analytical Chemistry [https://alpha-measure.com/standard-addition-method/]
- 83. Matrix Interference of Vegetable on Enzyme-Linked ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12524109/]
- 84. Matrix Interference Removal Using Fe3O4@SiO2-PSA-Based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12294301/]
- 85. The effect of sample preparation and data processing [https://www.sciencedirect.com/science/article/abs/pii/S0039914024010373]
- 86. Type I and type II errors [https://en.wikipedia.org/wiki/Type_I_and_type_II_errors]
- 87. Type I & Type II Errors | Differences, Examples, Visualizations [https://www.scribbr.com/statistics/type-i-and-type-ii-errors/]
- 88. Type I and Type II Errors and Statistical Power - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK557530/]
- 89. Regional Guidance on Handling Chemical Concentration ... [https://www.epa.gov/risk/regional-guidance-handling-chemical-concentration-data-near-detection-limit-risk-assessments]
- 90. Comparison of multiplexed platforms for serum cytokine ... [https://alamarbio.com/comparison-of-multiplexed-platforms-for-serum-cytokine-detection-in-covid-19-patients-2/]
- 91. nELISA: a high-throughput, high-plex platform enables ... [https://www.nature.com/articles/s41592-025-02861-6]
- 92. Multiplex sample-sparing assay for detecting type-specific ... [https://pubmed.ncbi.nlm.nih.gov/39730005/]
- 93. Cytokine Detection Reagents 2025 Trends and Forecasts ... [https://www.datainsightsmarket.com/reports/cytokine-detection-reagents-544119]
- 94. Multiplex PCR Assay Market CAGR, Segments and ... [https://www.towardshealthcare.com/insights/multiplex-pcr-assay-market-sizing]
- 95. Multiplex Sepsis Biomarker Panels Market [https://www.futuremarketinsights.com/reports/multiplex-sepsis-biomarker-panels-market]
- 96. Inflammation and Cytokine Storm ELISA Kits and Multiplex ... [https://www.thermofisher.com/us/en/home/life-science/antibodies/immunoassays/immunoassay-research-areas/inflammation-cytokine-storm-immunoassays.html]
- 97. Comparison of Low-Abundance Biomarker Levels in Capillary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3668804/]
- 98. Cytokine Immunoassay Kits [https://www.rndsystems.com/research-area/cytokines-and-receptors/cytokine-immunoassay-kits]
- 99. Comparison of the Calibration Standards of Three Commercially Available Multiplex Kits for Human Cytokine Measurement to WHO Standards Reveals Striking Differences - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2688352/]
- 100. Intracellular cytokine detection by flow cytometry in surface ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5547893/]
- 101. TSCytoPred: a deep learning framework for inferring cytokine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12614104/]
- 102. Preclinical vs. Clinical Biomarkers: Understanding Their ... [https://blog.crownbio.com/preclinical-vs-clinical-biomarkers-understanding-their-distinct-roles-in-drug-development]
- 103. Beyond ELISA: the future of biomarker validation [https://www.drugtargetreview.com/article/154316/beyond-elisa-the-future-of-biomarker-validation/]
- 104. Artificial Intelligence in Cancer Drug Discovery in 2025 [https://oncodaily.com/oncolibrary/artificial-intelligence-in-cancer-drug-discovery]