JAK-STAT Signaling in Inflammation: From Molecular Mechanisms to Therapeutic Targeting
This article provides a comprehensive analysis of the JAK-STAT pathway's pivotal role in inflammatory signaling, tailored for researchers and drug development professionals.
JAK-STAT Signaling in Inflammation: From Molecular Mechanisms to Therapeutic Targeting
Abstract
This article provides a comprehensive analysis of the JAK-STAT pathway's pivotal role in inflammatory signaling, tailored for researchers and drug development professionals. It explores the foundational biology and structure-function relationships of JAK and STAT proteins, detailing the canonical and non-canonical activation mechanisms. The scope extends to methodological approaches for investigating the pathway, including the development and application of small-molecule JAK inhibitors (Jakinibs) in autoimmune and inflammatory diseases. It further addresses key challenges in therapeutic targeting, such as selectivity and safety optimization, and concludes with a comparative evaluation of clinical efficacy and safety data for current and emerging therapies, validating their place in the treatment landscape.
The JAK-STAT Pathway: Core Architecture and Its Role in Inflammatory Signaling
The Janus kinase/Signal Transducer and Activator of Transcription (JAK-STAT) signaling pathway represents a fundamental membrane-to-nucleus communication module that enables cells to rapidly respond to extracellular cytokine cues. Discovered more than a quarter-century ago, this evolutionarily conserved pathway has emerged as a central signaling node governing critical processes including immune fitness, hematopoiesis, inflammation, and cell survival [1]. This technical review comprehensively examines the JAK-STAT pathway's architecture, quantitative signaling parameters, experimental methodologies, and its integral position within cytokine communication networks, with particular emphasis on its implications for inflammatory signaling research and therapeutic intervention.
Pathway Architecture and Core Components
The JAK-STAT pathway operates through a relatively straightforward structural framework that efficiently transmits signals from the cell surface to the nucleus. This pathway consists of three principal elements: cytokine receptors, Janus kinases (JAKs), and Signal Transducers and Activators of Transcription (STATs) [2] [3].
Receptor Complexes
Cytokine receptors function as the pathway's signal reception system. These transmembrane proteins typically lack intrinsic enzymatic activity and instead rely on associated JAK kinases for signal transduction. These receptors exist as two primary classes: Type I cytokine receptors (which include four conserved cysteines and a WSXWS motif in their extracellular domain) and Type II cytokine receptors (characterized by cysteine pairs at both N- and C-termini) [4]. The intracellular membrane-proximal region contains conserved box1 and box2 motifs that serve as docking sites for JAK proteins [1] [4].
Janus Kinase (JAK) Family
JAKs constitute the pathway's catalytic engine. Four JAK family members—JAK1, JAK2, JAK3, and TYK2—share a conserved seven-domain JH architecture [1] [3]:
- JH1 domain: C-terminal tyrosine kinase domain responsible for phosphorylating substrates
- JH2 domain: Pseudokinase domain that regulates JH1 kinase activity
- JH3-JH7 domains: Include SH2-like and FERM domains that mediate receptor binding [1] [4]
Each JAK exhibits distinct expression patterns and functional specializations, as detailed in Table 1.
Signal Transducer and Activator of Transcription (STAT) Family
STAT proteins serve as the pathway's nuclear messengers. The seven mammalian STAT family members (STAT1, STAT2, STAT3, STAT4, STAT5a, STAT5b, and STAT6) share conserved functional domains [3]:
- N-terminal domain: Facilitates protein-protein interactions
- Coiled-coil domain: Participates in protein interactions and nuclear import
- DNA-binding domain: Mediates specific DNA sequence recognition
- SH2 domain: Binds phosphorylated tyrosine residues (critical for receptor docking and STAT dimerization)
- C-terminal transactivation domain: Contains conserved tyrosine phosphorylation site and modulates transcriptional activity [3]
Table 1: JAK Family Members and Their Functional Specializations
| JAK Family Member | Primary Expression | Key Activating Cytokines | Biological Functions | Phenotype of Knockout Models |
|---|---|---|---|---|
| JAK1 | Ubiquitous | IFN-α/β, IFN-γ, IL-2, IL-4, IL-6, IL-10, IL-13, G-CSF | Hematopoiesis, immune function, lymphocyte development | Perinatal lethality; neurological defects; severe lymphocyte deficiency [1] |
| JAK2 | Ubiquitous | EPO, GH, TPO, GM-CSF, IL-3, IL-5, IFN-γ | Hematopoiesis, erythropoiesis, growth hormone signaling | Embryonic lethality (~E12.5) due to defective erythropoiesis [1] |
| JAK3 | Hematopoietic system, endothelial cells | IL-2, IL-4, IL-7, IL-9, IL-15, IL-21 | Lymphocyte development, function, and homeostasis | Severe combined immunodeficiency; defective lymphocyte production [1] |
| TYK2 | Ubiquitous | IFN-α/β, IL-6, IL-10, IL-12, IL-13, IL-23 | Type I interferon signaling, immune regulation | Viable; impaired response to low IFN-α; defective IL-12 signaling [1] |
Core Signaling Mechanism
The JAK-STAT pathway operates through a sequential activation cascade that transmits extracellular signals directly to the nucleus.
Pathway Activation and Nuclear Translocation
The canonical JAK-STAT signaling mechanism follows these key steps [1] [2] [3]:
Cytokine binding and receptor dimerization: Ligand binding induces receptor oligomerization, bringing associated JAK proteins into proximity
JAK transphosphorylation and activation: Reciprocal phosphorylation of activation loop tyrosine residues (Y1038/Y1039 in JAK1, Y1007/Y1008 in JAK2) enhances kinase activity
Receptor phosphorylation: Activated JAKs phosphorylate tyrosine residues on cytokine receptors, creating docking sites for STAT proteins via their SH2 domains
STAT recruitment and phosphorylation: STATs bind to phosphorylated receptors and undergo JAK-mediated phosphorylation on conserved C-terminal tyrosine residues
STAT dimerization and nuclear translocation: Phosphorylated STATs form homo- or heterodimers that translocate to the nucleus through nuclear pore complexes via importin proteins (e.g., STAT1/2 with importin α5, STAT3 with importin α3/α6)
Gene transcription: STAT dimers bind specific promoter elements (e.g., GAS elements for most STATs, ISRE for STAT1/2/IRF9 complex) to regulate target gene expression
Regulatory Mechanisms
JAK-STAT signaling is tightly regulated through multiple mechanisms [3] [5]:
- Post-translational modifications: Acetylation, methylation, and serine phosphorylation fine-tune STAT activity, stability, and DNA binding
- Negative regulators:
- SOCS proteins: Compete for STAT binding sites and target signaling components for proteasomal degradation
- PIAS proteins: Inhibit STAT-DNA binding and promote SUMOylation
- Protein tyrosine phosphatases: Directly dephosphorylate signaling components
Alternative Signaling Modes
Beyond the canonical pathway, JAK-STAT components participate in non-canonical signaling [3]:
- Cross-talk with other pathways: Integration with MAPK/ERK and PI3K/AKT/mTOR pathways through shared docking sites on activated receptors
- Kinase-independent STAT functions: Roles in mitochondrial metabolism, chromatin organization, and transcriptional regulation independent of tyrosine phosphorylation
Quantitative Analysis of Cytokine-JAK-STAT Relationships
Understanding the quantitative relationships between cytokines and their associated JAK-STAT components provides critical insights for both basic research and therapeutic development.
Table 2: Cytokine-JAK-STAT Signaling Specificity and Key Parameters
| Cytokine/Ligand | Receptor Components | JAK Kinases | STAT Effectors | ECâ‚…â‚€ / Potency | Primary Cellular Functions |
|---|---|---|---|---|---|
| IL-2 | IL-2Rα + IL-2Rβ + γc | Jak1, Jak2, Jak3 | Stat3, Stat5 | 3.2–16.0 pM [6] | T-cell proliferation, Treg function, immune tolerance [7] |
| IL-4 | IL-4Rα + γc or IL-4Rα + IL-13Rα1 | Jak1, Jak3 | Stat6 | 3.3–26.7 pM [6] | B-cell activation, Th2 differentiation, IgE class switching [7] |
| IL-6 | IL-6Rα + gp130 | Jak1, Jak2, Tyk2 | Stat1, Stat3 | 0.38–38.00 pM [6] | Acute phase response, B-cell differentiation, inflammation [7] |
| IL-10 | IL-10Rα + IL-10Rβ | Jak1, Tyk2 | Stat1, Stat3, Stat5 | 8.06–53.80 pM [6] | Anti-inflammatory signaling, macrophage regulation [7] |
| IL-12 | IL-12Rβ1 + IL-12Rβ2 | Jak2, Tyk2 | Stat4 | 0.14–2.90 pM [6] | Th1 differentiation, IFN-γ production, cell-mediated immunity [7] |
| IL-23 | IL-12Rβ1 + IL-23R | Jak2, Tyk2 | Stat3, Stat4 | 0.9–5.4 pM [6] | Th17 maintenance, inflammatory pathology [7] |
| IFN-α/β | IFNAR1 + IFNAR2 | Jak1, Tyk2 | Stat1, Stat2 (primarily) | ~40 pM (IFNα) [6] | Antiviral response, MHC class I expression [7] |
| IFN-γ | IFN-γR1 + IFN-γR2 | Jak1, Jak2 | Stat1 | 2.9–44.0 pM [6] | Macrophage activation, MHC class II expression, antimicrobial defense [7] |
| G-CSF | G-CSFR | Jak2, Tyk2 | Stat3 | 0.53–3.00 pM [6] | Neutrophil production, differentiation [7] |
| GM-CSF | GM-CSFR + βc | Jak2 | Stat3, Stat5 | 0.43–2.10 pM [6] | Granulocyte, monocyte production and function [7] |
| EPO | EpoR | Jak2 | Stat5 (mainly Stat5a) | Not specified | Erythropoiesis, red blood cell production [7] |
Experimental Approaches and Methodologies
Advanced Technique: Cytokine Adaptor Engineering
Recent innovative methodologies enable precise manipulation of JAK-STAT signaling. The cytokine adaptor approach represents a cutting-edge technology for redirecting endogenous cytokine signals [8].
Experimental Objective: Engineer molecular switches that transform one cytokine signal into an alternative signaling output with different functional consequences [8].
Detailed Protocol: TGF-β→IL-2 Adaptor System [8]
Adaptor Design and Construction:
- Component selection: Utilize single-chain variable fragments (scFv) against input cytokine (e.g., GC1008 for TGF-β) and variable heavy chain-only antibody fragments (VHH) against output receptors (e.g., IL-2RβNb6 for IL-2Rβ, γcNb6 for γc)
- Construct assembly: Generate two-component system (separate molecules) or single-chain adaptor with optimized linker length (e.g., 20 amino acids for TGF-β→IL-2 adaptor T.3)
Signaling Validation:
- Cell systems: Employ cytokine-responsive cell lines (e.g., YT-1 human NK cells for IL-2 signaling) and primary human T cells
- Stimulation conditions: Treat cells with adaptor molecules in presence or absence of input cytokine (TGF-β)
- Readout measurement: Quantify phosphorylated STAT5 (pSTAT5) via flow cytometry or Western blotting; compare to IL-2 positive control
Functional Assessment:
- Proliferation assays: Measure reversal of TGF-β-mediated suppression of T-cell proliferation over 6 days
- Cytokine production: Quantify TNF-α and IFN-γ production via intracellular staining or ELISA
- Specificity controls: Verify absence of signaling with adaptor alone or cytokine alone
Core Signaling Assessment Methods
Standard experimental approaches for JAK-STAT pathway analysis include:
- Phospho-flow cytometry: Enables single-cell resolution of STAT phosphorylation dynamics in heterogeneous cell populations
- Electrophoretic mobility shift assays (EMSAs): Detect STAT-DNA binding interactions
- Chromatin immunoprecipitation (ChIP): Identify genome-wide STAT binding sites
- Gene expression profiling: Monitor transcriptional responses to JAK-STAT activation
- Co-immunoprecipitation: Investigate protein-protein interactions in JAK-STAT complexes
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for JAK-STAT Pathway Investigation
| Reagent Category | Specific Examples | Research Applications | Technical Considerations |
|---|---|---|---|
| Recombinant Cytokines | IL-2, IL-6, IL-10, IFN-γ, EPO, G-CSF [4] | Pathway stimulation, dose-response studies, functional assays | Verify species specificity; consider carrier proteins and storage conditions |
| Recombinant Receptors | Soluble EPOR-Fc, IL-3RA-hFc, IFNGR1-Fc [4] | Binding studies, receptor blocking experiments, biosensor development | Fc-fusion proteins enable easy detection and immobilization |
| JAK/STAT Proteins | Recombinant STAT3, JAK2 kinase domains [4] | Biochemical assays, structural studies, inhibitor screening | Active kinases require proper phosphorylation state; pseudokinase domains regulate activity |
| Phospho-Specific Antibodies | Anti-pSTAT1 (Y701), anti-pSTAT3 (Y705), anti-pSTAT5 (Y694) | Signaling activation assessment, phospho-flow cytometry, Western blotting | Optimize fixation/permeabilization for flow cytometry; validate specificity |
| Inhibitors | JAK inhibitors (ruxolitinib, tofacitinib), STAT3 inhibitors | Pathway blockade, mechanistic studies, therapeutic assessment | Consider selectivity profiles (JAK1 vs JAK2 vs JAK3); assess off-target effects |
| Cell Lines | Engineered reporter cells (STAT-responsive luciferase), cytokine-responsive lines (YT-1) | High-throughput screening, signaling dynamics, functional validation | Authenticate regularly; monitor cytokine responsiveness over passages |
| Luseogliflozin | Luseogliflozin, CAS:898537-18-3, MF:C23H30O6S, MW:434.5 g/mol | Chemical Reagent | Bench Chemicals |
| Lycoramine hydrobromide | Lycoramine hydrobromide, CAS:89505-76-0, MF:C17H24BrNO3, MW:370.3 g/mol | Chemical Reagent | Bench Chemicals |
Integration with Inflammatory Signaling Networks
The JAK-STAT pathway functions as a central integrator within broader inflammatory signaling networks, with particular relevance to disease pathogenesis and therapeutic development.
Cross-Pathway Communication
JAK-STAT signaling exhibits extensive cross-talk with other critical pathways [3] [5]:
- PI3K/AKT/mTOR pathway: Activated via direct PI3K recruitment to phosphorylated receptor-JAK complexes
- MAPK/ERK pathway: Engaged through Grb2 binding to phospho-receptors; MAPK-mediated serine phosphorylation modulates STAT activity
- NF-κB pathway: STAT3 directly interacts with NF-κB components, promoting constitutive inflammatory activation
Therapeutic Implications
Dysregulated JAK-STAT signaling contributes to numerous inflammatory and autoimmune conditions [1] [5]:
- Rheumatoid arthritis: Inflammatory cytokine signaling (IL-6, IFN-γ) drives pathogenesis through JAK-STAT activation
- Inflammatory bowel disease: IL-23/STAT3 and IL-12/STAT4 axes promote Th17 and Th1-mediated inflammation
- Psoriasis: IL-23/STAT3 signaling central to disease pathology
- Cancer-associated inflammation: STAT3 activation creates pro-tumorigenic inflammatory microenvironment
The development of JAK inhibitors (tofacitinib, ruxolitinib, baricitinib) demonstrates successful therapeutic targeting of this pathway, though optimal selectivity profiles remain an area of active investigation [1].
Future Directions and Research Opportunities
Emerging research areas continue to expand our understanding of JAK-STAT biology:
- Context-dependent signaling tools: Advanced cytokine adaptors enabling precise manipulation of immune responses in specific microenvironments [8]
- Structural biology advances: Cryo-EM studies of full-length receptor-JAK-STAT complexes
- Single-cell analysis: Resolution of cell-to-cell variability in JAK-STAT responses within complex tissues
- Metabolic integration: Elucidation of connections between JAK-STAT signaling and cellular metabolism
- Epigenetic regulation: Understanding how STAT proteins orchestrate long-term transcriptional programs through epigenetic modifications
The JAK-STAT pathway continues to serve as a paradigm for understanding how extracellular signals are rapidly communicated to the nucleus, maintaining its position as a central hub for cytokine communication and a fertile ground for basic research and therapeutic innovation.
The Janus kinase–signal transducer and activator of transcription (JAK-STAT) pathway serves as a paradigm for signal transduction from the extracellular environment to the nucleus, playing a pivotal role in physiological functions such as hematopoiesis, immune balance, tissue homeostasis, and surveillance against tumors [9]. Advances in the structural biology of this pathway have enabled critical insights into how the signaling cascade operates at the molecular level, laying the groundwork for therapeutic development [9]. This review details the structural basis governing key nodes in this pathway, offering a comprehensive overview of the signal transduction process framed within the context of inflammatory signaling research [9].
Domain Architecture of JAK and STAT Proteins
JAK Family Homology Domains
The Janus kinase (JAK) family of non-receptor tyrosine kinases includes four members in mammals: JAK1, JAK2, JAK3, and TYK2 [10] [1]. These large proteins, comprising over 1000 amino acids with molecular weights ranging from 120 to 140 kDa, share a characteristic seven JAK homology (JH) domain structure, numbered JH1 to JH7 from the C-terminus to the N-terminus [10] [1].
Table 1: JAK Protein Homology Domains and Their Functions
| Domain | Alternative Name | Location | Primary Function |
|---|---|---|---|
| JH1 | Kinase domain | C-terminus | Catalytic tyrosine kinase activity; contains activation loop with conserved tyrosine residues |
| JH2 | Pseudokinase domain | Central | Regulatory function; autoinhibits JH1 activity despite lacking catalytic function |
| JH3-JH4 | SH2-like domain | Central | Protein-protein interactions; binds phosphotyrosine residues |
| JH4-JH7 | FERM domain | N-terminus | Mediates interaction with cytokine receptors via membrane-proximal box1/2 regions |
The JH1 domain represents the catalytically active tyrosine kinase domain, containing a conserved activation loop with characteristic tyrosine residues (Y1038/Y1039 in JAK1, Y1007/Y1008 in JAK2, Y980/Y981 in JAK3, and Y1054/Y1055 in TYK2) whose phosphorylation is essential for kinase activation [1]. The JH2 pseudokinase domain, despite its structural similarity to JH1, lacks catalytic activity due to substitutions in conserved motifs and primarily serves a regulatory role, controlling the activity of the JH1 domain [10]. The FERM domain (band 4.1, ezrin, radixin, moesin), formed by JH4-JH7, is crucial for JAK association with cytokine receptors, while the SH2-like domain (JH3-JH4) facilitates protein-protein interactions [11] [10].
STAT Family Functional Domains
The signal transducer and activator of transcription (STAT) family comprises seven members: STAT1, STAT2, STAT3, STAT4, STAT5a, STAT5b, and STAT6 [10]. These proteins range from 750 to 900 amino acids in length and contain several functionally specialized domains arranged linearly from N- to C-terminus.
Table 2: STAT Protein Functional Domains and Characteristics
| Domain | Position | Function | Structural Features |
|---|---|---|---|
| N-terminal domain | ~100 amino acids | Facilitates STAT dimerization, nuclear translocation, and cooperativity in DNA binding | Conserved across family members; interacts with transcriptional co-activators |
| Coiled-coil domain | Central | Protein-protein interactions; nuclear import and export | Four-helix bundle; interacts with regulatory proteins (StIP, c-Jun, Nmi, IRF9) |
| DNA-binding domain | Central | Sequence-specific DNA recognition | S-type immunoglobulin fold; recognizes TTCN3-4GAAA promoter sequences |
| Linker domain | Central | Connects DNA-binding and SH2 domains; contributes to transcriptional regulation | Critical for STAT1 transcriptional regulation |
| SH2 domain | C-terminal region | Binds phosphotyrosine residues; mediates STAT dimerization | Highly conserved; recognizes pY residues on receptors and mediates STAT dimerization |
| Transactivation domain (TAD) | C-terminus | Transcriptional activation; contains conserved tyrosine phosphorylation site | Variable length; serine phosphorylation sites enhance transcriptional activity |
The SH2 domain is particularly critical for STAT function as it mediates both receptor docking through recognition of specific phosphorylated tyrosine residues and STAT dimerization through reciprocal phosphotyrosine-SH2 interactions [12] [11]. The C-terminal transactivation domain contains a conserved tyrosine residue that serves as the phosphorylation target for JAKs, alongside serine residues whose phosphorylation can further modulate transcriptional activity [11].
Structural Mechanisms of JAK-STAT Pathway Activation
The JAK-STAT pathway operates through a sequential activation mechanism that transmits signals from the cell surface to the nucleus. The pathway is initiated when extracellular cytokines bind to their cognate transmembrane receptors, inducing receptor dimerization or oligomerization [9] [12]. This conformational change brings receptor-associated JAKs into close proximity, allowing their trans-phosphorylation and activation [12]. Activated JAKs then phosphorylate specific tyrosine residues on the intracellular domains of cytokine receptors, creating docking sites for STAT proteins via their SH2 domains [12] [11]. Once recruited, STATs become substrates for JAK-mediated phosphorylation at their conserved C-terminal tyrosine residue [12].
Following tyrosine phosphorylation, STATs undergo dimerization through reciprocal SH2-phosphotyrosine interactions, forming parallel complexes that translocate to the nucleus [12] [11]. These STAT dimers bind to specific palindromic sequences within promoter regions of target genes, thereby initiating transcriptional programs that regulate critical cellular processes including proliferation, differentiation, and apoptosis [9] [12].
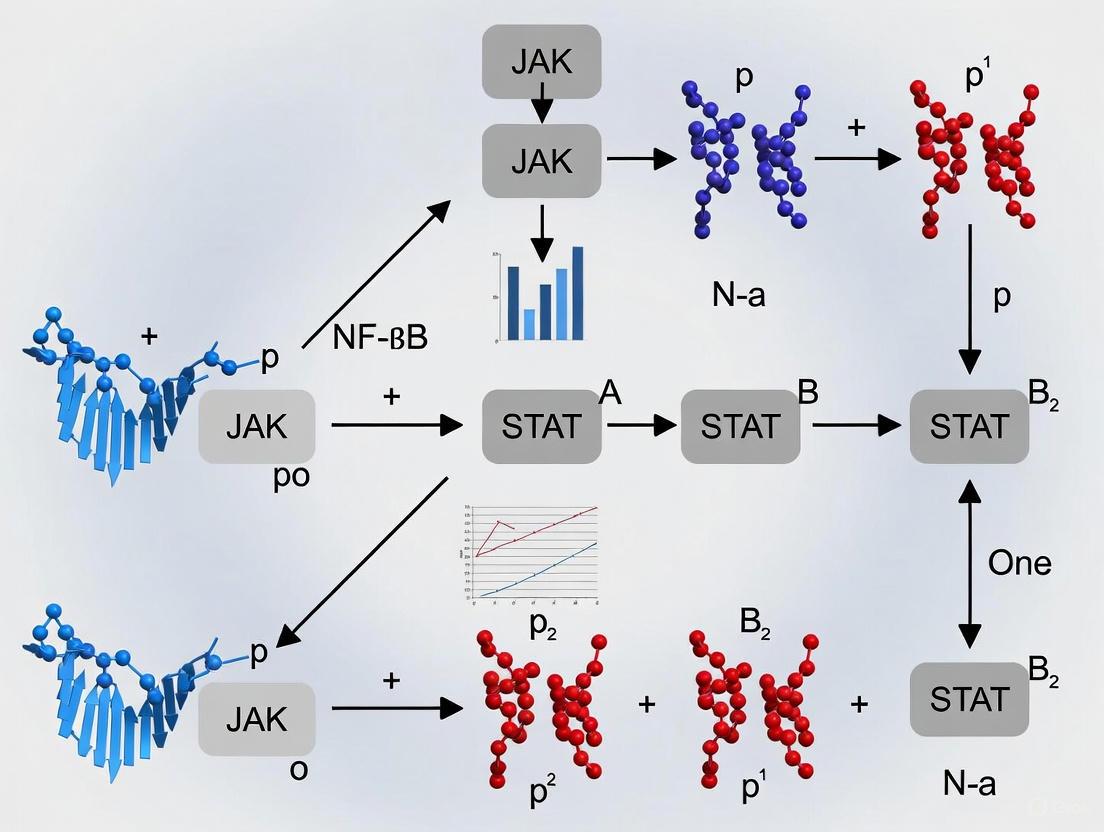
Figure 1: JAK-STAT Pathway Activation Cascade. This diagram illustrates the sequential process from cytokine binding to gene expression regulation.
Experimental Approaches for Studying JAK-STAT Structure and Function
Phosphorylation Analysis via Western Blot
The activation status of JAK-STAT pathway components is routinely assessed through phosphorylation-specific Western blotting, a fundamental technique in pathway analysis [13]. This method enables researchers to detect and quantify the activated (phosphorylated) forms of JAK and STAT proteins, providing critical insights into pathway dynamics under various experimental conditions.
Detailed Protocol:
- Sample Preparation: Homogenize tissue or cell samples in lysis buffer (e.g., 50 mM Tris, 150 mM NaCl, 5 mM EDTA) supplemented with protease and phosphatase inhibitors [13]. Centrifuge at 10,000 × g for 10 minutes and determine protein concentration using a standardized assay (e.g., Bio-Rad DC protein assay) [13].
- Gel Electrophoresis: Mix protein extracts with loading buffer, heat to 95°C for 5 minutes, and separate 20 μg of total protein on 4-12% Bis-Tris Plus gels at 120 V for 85 minutes [13].
- Protein Transfer: Transfer separated proteins to PVDF membranes at 15 V for 90 minutes [13].
- Blocking and Antibody Incubation: Treat membranes with Western blot enhancer, block with 5% BSA, and incubate with primary antibodies against phosphorylated JAKs or STATs overnight at 4°C [13]. Use phospho-specific antibodies validated for JAK-STAT components with appropriate positive controls.
- Detection: Incubate with HRP-conjugated secondary antibodies for 1 hour at room temperature and visualize using enhanced chemiluminescence substrate on an imaging system [13].
- Membrane Stripping and Reprobing: Strip membranes with commercial stripping buffer for 10 minutes at room temperature to remove antibodies, then re-probe for total protein levels or housekeeping proteins (e.g., β-actin) for normalization [13].
- Quantitative Analysis: Perform densitometric analysis using software such as ImageJ to calculate phosphorylation levels normalized to total protein or loading controls [13].
Structural Elucidation Techniques
High-resolution structural studies of JAK and STAT proteins have been revolutionized by advances in cryo-electron microscopy (cryo-EM), which enables visualization of large protein complexes that are challenging to study using NMR spectroscopy or crystallography [9]. These technological breakthroughs allow researchers to examine intricate details of signaling complexes at near-atomic resolution, providing invaluable insights into the functional mechanisms of key signaling molecules [9].
Key Structural Biology Methods:
- Cryo-EM Single Particle Analysis: Rapidly freeze purified protein complexes in vitreous ice and image using electron microscopy, followed by computational reconstruction to generate 3D density maps [9]. Particularly valuable for studying cytokine receptor-JAK complexes and STAT-DNA complexes.
- X-ray Crystallography: Generate high-quality crystals of isolated JAK or STAT domains (e.g., SH2 domains, kinase domains) for atomic-resolution structure determination. Has provided fundamental insights into STAT DNA-binding mechanisms and JAK kinase domains.
- Nuclear Magnetic Resonance (NMR) Spectroscopy: Study solution-state dynamics and interactions of smaller JAK and STAT domains, particularly useful for characterizing flexible regions and transient interactions.
Research Reagent Solutions for JAK-STAT Investigations
Table 3: Essential Research Reagents for JAK-STAT Pathway Analysis
| Reagent Category | Specific Examples | Research Application | Technical Notes |
|---|---|---|---|
| Phospho-Specific Antibodies | Anti-p-JAK1 (Y1034/1035), Anti-p-STAT3 (Y705) | Detection of activated pathway components by Western blot, immunofluorescence | Validate using kinase-inactive JAK mutants or STAT phosphorylation site mutants |
| JAK Inhibitors | Tofacitinib (JAK1/3), Ruxolitinib (JAK1/2) | Functional interrogation of pathway dependence; therapeutic modeling | Vary selectivity profiles; use multiple inhibitors to confirm specificity |
| Cytokine Stimuli | IFN-α (STAT1/2), IL-6 (STAT3), IL-4 (STAT6) | Pathway activation under controlled conditions | Concentration and time course optimization required for specific responses |
| Cell Line Models | JAK-or STAT-deficient cell lines (e.g., U4A-JAK1-) | Genetic validation of protein functions | Complementation with wild-type or mutant constructs for structure-function studies |
| Protease/Phosphatase Inhibitors | Complete EDTA-free, PhosSTOP | Preservation of phosphorylation states during sample preparation | Essential for accurate assessment of pathway activation status |
| Lysis Buffers | Tris-based (50 mM Tris, 150 mM NaCl, 5 mM EDTA) | Protein extraction while maintaining protein interactions and modifications | Supplement with fresh inhibitors immediately before use |
Functional Implications of Structural Domains in Inflammatory Signaling
The precise domain architecture of JAK and STAT proteins directly dictates their functional specialization in inflammatory signaling. Understanding these structure-function relationships is essential for elucidating the pathway's role in inflammation and for developing targeted therapeutic interventions.
JAK Regulatory Mechanisms in Inflammation
The JH2 pseudokinase domain, once considered a catalytically inactive relic, is now recognized as a critical regulatory module with profound implications for inflammatory disease. Mutations in the JH2 domain of JAK2 (e.g., V617F) are associated with constitutive pathway activation and myeloproliferative neoplasms [9]. Structural studies have revealed that JH2 domains exert autoinhibitory control over their adjacent JH1 kinase domains, and mutations disrupting this interaction lead to hyperactive signaling that drives inflammatory responses [9].
The FERM domain mediates specific JAK-receptor interactions that determine cytokine responsiveness. For instance, JAK3's FERM domain specifically interacts with the common gamma chain (γc) of cytokine receptors, explaining its non-redundant role in lymphocyte development and function [1]. Mutations disrupting JAK3-γc binding result in severe combined immunodeficiency (SCID), highlighting the critical importance of this specific protein-protein interaction module in immune system function [12].
STAT DNA Recognition and Transcriptional Regulation
The DNA-binding domain of STAT proteins contains an S-type immunoglobulin fold that recognizes specific DNA sequences with high specificity [11]. Structural analyses have revealed that different STAT family members recognize variations of the palindromic TTCN3-4GAAA sequence, providing a structural basis for their differential gene targeting in inflammatory responses [11].
STAT SH2 domains facilitate both receptor docking and STAT dimerization through phosphotyrosine recognition. The precise geometry of SH2-phosphotyrosine interaction determines the specificity of STAT activation by different cytokines; for example, STAT1's SH2 domain preferentially recognizes phosphorylated motifs in the IFN-γ receptor, while STAT6's SH2 domain specifically binds phosphorylated IL-4 receptor sequences [11]. This underlies the specific STAT activation patterns observed in different inflammatory contexts.
The N-terminal domain of STAT proteins facilitates cooperative DNA binding through interactions between STAT dimers bound to adjacent DNA sites, enabling transcriptional amplification of inflammatory response genes [11]. This domain also participates in nuclear import and export, shuttling STATs between cytoplasmic and nuclear compartments to dynamically regulate inflammatory gene expression.
The structural biology of JAK and STAT proteins provides a molecular framework for understanding their critical roles in inflammatory signaling. The precise domain architecture of these signaling molecules dictates their activation mechanisms, protein-protein interactions, and DNA recognition properties. Advances in structural elucidation techniques, particularly cryo-EM, continue to reveal novel insights into the complex regulation of this pathway. This structural knowledge provides the foundation for rational drug design targeting specific JAK or STAT domains in inflammatory diseases, enabling the development of therapeutics with enhanced specificity and reduced off-target effects. Future research integrating structural biology with cellular signaling studies will further illuminate the intricate mechanisms controlling JAK-STAT pathway activation in inflammation.
The Janus kinase/Signal Transducer and Activator of Transcription (JAK-STAT) pathway represents a fundamental signaling module that enables rapid transmission of information from extracellular cytokines directly to the nucleus. This canonical pathway, operating as a concise membrane-to-nucleus signaling cascade, governs critical cellular processes including proliferation, differentiation, and immune responses. Dysregulation of this meticulously orchestrated mechanism underpins numerous pathological conditions, from autoimmune diseases to cancer, making it a pivotal therapeutic target. This technical guide delineates the precise molecular events comprising canonical JAK-STAT activation, details established methodologies for its investigation, and provides essential resources for ongoing research and therapeutic development aimed at this pathway.
Discovered more than a quarter-century ago through investigations into interferon signaling, the JAK-STAT pathway has emerged as a central communication node in cellular function [1]. The pathway is activated by more than 50 cytokines and growth factors—including interferons (IFN), interleukins (ILs), and colony-stimulating factors—that transduce signals through this system [1] [14]. The pathway's moniker derives from its two core components: the Janus kinases (JAKs), non-receptor tyrosine kinases, and the Signal Transducers and Activators of Transcription (STATs), transcription factors that directly link signal transduction to gene expression [1]. This direct coupling creates a remarkably efficient signaling circuit, allowing extracellular cues to rapidly modulate nuclear gene transcription without secondary messengers. The critical nature of this pathway is evidenced by the severe immunological phenotypes observed in both humans and mice bearing loss- or gain-of-function mutations in JAK-STAT components [14]. In inflammatory signaling research, understanding the precise mechanics of canonical JAK-STAT activation provides the foundational knowledge required to develop targeted interventions for immune-mediated diseases.
Molecular Components of the Pathway
The Janus Kinase (JAK) Family
The JAK family comprises four members in mammals: JAK1, JAK2, JAK3, and TYK2 [1] [15]. These intracellular tyrosine kinases share a conserved structure featuring seven JAK homology (JH) domains, JH1-JH7 [1] [16]. The C-terminal JH1 domain is the catalytically active kinase domain responsible for phosphorylating downstream substrates [1] [17]. Adjacent to JH1 lies the JH2 pseudokinase domain, which structurally resembles a kinase domain but lacks catalytic activity; instead, it plays a crucial regulatory role by inhibiting the basal activity of JH1 [1] [17]. The N-terminal region (JH3-JH7) includes SH2-like domains (JH3-JH4) and a FERM domain (JH5-JH7), which mediates interaction with cytokine receptors [1] [16]. With the exception of JAK3, which displays more restricted expression primarily in hematopoietic and lymphatic systems, JAK family members are ubiquitously expressed across tissues [1] [16].
Table 1: JAK Family Members and Their Characteristics
| JAK Member | Conserved Tyrosine Sites | Primary Expression | Key Functions |
|---|---|---|---|
| JAK1 | Y1038/Y1039 | Ubiquitous | Phosphorylates all STATs; essential for γc, gp130, and class II cytokine receptor signaling [1] |
| JAK2 | Y1007/Y1008 | Ubiquitous | Critical for hematopoiesis; signals through single-chain receptors (EPO, GH, TPO) [1] |
| JAK3 | Y980/Y981 | Hematopoietic, bone marrow, lymphatic system | Exclusive partner for γc receptor subunit; vital for lymphocyte development [1] |
| TYK2 | Y1054/Y1055 | Ubiquitous | Involved in IFN-α/β, IL-12, and IL-23 signaling [1] |
The STAT Transcription Factor Family
The STAT family consists of seven members: STAT1, STAT2, STAT3, STAT4, STAT5a, STAT5b, and STAT6 [1] [14]. All STAT proteins share characteristic structural domains: an N-terminal domain that facilitates protein-protein interactions, a coiled-coil domain involved in protein interactions and nuclear import, a central DNA-binding domain (DBD), a linker domain, a Src homology 2 (SH2) domain critical for receptor docking and STAT dimerization, and a C-terminal transcriptional activation domain (TAD) [14] [17]. The SH2 domain is particularly crucial for the canonical activation mechanism, as it recognizes specific phosphotyrosine motifs on activated cytokine receptors and mediates reciprocal STAT dimerization following phosphorylation [17]. While STATs can be activated by overlapping sets of cytokines, they exert non-redundant biological effects, with specific STATs often recruited to particular cytokine receptors [1].
Table 2: STAT Family Members and Their Primary Associations
| STAT Member | Primary Cytokine Associations | Key Functions |
|---|---|---|
| STAT1 | IFNs, IL-6 family, IL-27, IL-28/29 | Antiviral defense, tumor suppression [16] |
| STAT2 | IFNs (type I) | Forms ISGF3 complex with STAT1 and IRF9 [1] |
| STAT3 | IL-6 family, IL-10, IL-21, IL-23 | Cell proliferation, survival, immune regulation; often oncogenic [16] |
| STAT4 | IL-12, IL-23 | Drives Th1 immune responses [16] |
| STAT5a/b | IL-2, IL-3, IL-5, IL-7, IL-15, GM-CSF, GH, Prolactin | Mammary gland development, Treg function, hematopoiesis [14] |
| STAT6 | IL-4, IL-13 | Regulates Th2 responses and allergic inflammation [16] |
The Canonical Activation Mechanism
Step 1: Cytokine Binding and Receptor Oligomerization
The canonical JAK-STAT activation cascade initiates when an extracellular cytokine binds to its specific transmembrane receptor. Cytokine receptors utilizing the JAK-STAT pathway are primarily type I/II cytokine receptors, which lack intrinsic kinase activity [17]. These receptors exist as multi-subunit complexes, often sharing common receptor chains. Upon ligand binding, receptor subunits undergo obligatory oligomerization—typically dimerization or higher-order clustering [14] [17]. This ligand-induced conformational change brings the intracellular domains of the receptor subunits into proximity, subsequently activating the receptor-associated JAK kinases.
Step 2: JAK Trans-activation and Phosphorylation
The spatial reorganization of receptor subunits following oligomerization positions the associated JAKs within catalytic proximity, enabling their trans-activation [1] [15]. Specifically, the JAKs phosphorylate each other on specific tyrosine residues within their activation loops (e.g., Y1007/Y1008 in JAK2), dramatically enhancing their kinase activity [1]. The activated JAKs then phosphorylate specific tyrosine residues on the intracellular domains of the cytokine receptors, creating docking sites for STAT proteins [1] [14] [15]. These phosphotyrosine motifs on the receptor serve as molecular beacons that recruit STATs via their SH2 domains.
Step 3: STAT Recruitment, Phosphorylation, and Dimerization
Cytosolic STAT monomers are recruited to the receptor-JAK complex through interactions between their SH2 domains and the receptor phosphotyrosine motifs [1] [17]. Once positioned near the activated JAKs, STATs undergo tyrosine phosphorylation at a conserved C-terminal tyrosine residue [14]. This phosphorylation induces a dramatic conformational change in the STAT protein, enabling it to form stable dimers through reciprocal SH2-phosphotyrosine interactions between two STAT monomers [17]. The resulting STAT dimer represents the transcriptionally active form of the protein, capable of nuclear translocation and DNA binding.
Step 4: Nuclear Translocation and DNA Binding
Following dimerization, the active STAT dimers are transported into the nucleus through the nuclear pore complex via a importin-dependent mechanism [1]. Once in the nucleus, STAT dimers bind to specific DNA sequences known as gamma-activated sites (GAS) in the promoter/enhancer regions of target genes [15]. The consensus GAS motif is TTN5-6AA, though precise sequences vary among different STAT family members [14]. An exception is the STAT1-STAT2 heterodimer, which forms a complex with IRF9 (Interferon Regulatory Factor 9) to create the ISGF3 (Interferon-Stimulated Gene Factor 3) complex; this trimeric complex binds to Interferon-Stimulated Response Elements (ISRE) instead of GAS sites [1] [15]. DNA binding by STATs recruits additional transcriptional co-activators—including CBP/p300, which mediates histone acetylation—leading to chromatin remodeling and transcriptional activation of target genes [14].
Table 3: Key Molecular Events in Canonical JAK-STAT Activation
| Activation Step | Key Molecular Event | Regulatory Checkpoints |
|---|---|---|
| Receptor Engagement | Cytokine-induced receptor oligomerization | Receptor subunit availability and affinity |
| JAK Activation | Trans-phosphorylation of JAK activation loops | JH2 pseudokinase domain-mediated autoinhibition |
| STAT Recruitment | SH2 domain recognition of receptor pTyr motifs | STAT expression levels and cellular localization |
| STAT Activation | JAK-mediated tyrosine phosphorylation | Protein tyrosine phosphatase activity |
| Dimerization | Reciprocal SH2-pTyr interaction between STATs | Dimer stability and specificity |
| Nuclear Translocation | Importin-mediated nuclear import | Nuclear pore complex accessibility |
| DNA Binding | Recognition of GAS/ISRE elements | Chromatin accessibility and epigenetic status |
| Transcriptional Regulation | Recruitment of co-activators (CBP/p300) | Presence of transcriptional repressors |
Experimental Methodologies for Investigating JAK-STAT Activation
Protocol 1: Monitoring STAT Phosphorylation and Dimerization
Purpose: To detect and quantify STAT phosphorylation and dimer formation, key events in JAK-STAT pathway activation.
Method Details:
- Cell Stimulation and Lysis: Serum-starve cells for 4-6 hours, then stimulate with target cytokine (e.g., IFN-γ at 10 ng/mL for 15-30 minutes). Lyse cells using RIPA buffer supplemented with phosphatase and protease inhibitors [14].
- Immunoprecipitation/Western Blot: For total STAT phosphorylation, resolve cell lysates by SDS-PAGE and immunoblot with anti-phospho-STAT antibodies (e.g., pY701-STAT1, pY705-STAT3). For dimerization analysis, use non-denaturing (native) PAGE to preserve protein complexes, followed by Western blotting with STAT-specific antibodies [14].
- Alternative Approach: For STAT-receptor interaction studies, perform immunoprecipitation with anti-receptor antibodies, followed by Western blotting with anti-STAT antibodies.
Technical Considerations: Include JAK inhibitor controls (e.g., 1 μM ruxolitinib or tofacitinib) to confirm JAK-dependence. Time-course experiments (0-120 minutes) capture activation dynamics.
Protocol 2: Chromatin Immunoprecipitation (ChIP) for STAT-DNA Binding
Purpose: To identify genome-wide STAT binding sites and assess in vivo DNA binding activity.
Method Details:
- Crosslinking and Sonication: Treat cells with 1% formaldehyde for 10 minutes at room temperature for crosslinking. Quench with glycine, harvest cells, and sonicate chromatin to 200-500 bp fragments [14].
- Immunoprecipitation: Incubate chromatin with STAT-specific antibodies (e.g., anti-STAT1, anti-STAT3) or species-matched IgG control overnight at 4°C. Use protein A/G beads for precipitation.
- Library Preparation and Sequencing: Reverse crosslinks, purify DNA, and prepare libraries for ChIP-seq following standard protocols. Sequence on an appropriate NGS platform [14].
- Data Analysis: Align sequences to reference genome, call peaks with tools like MACS2, and integrate with RNA-seq data to identify direct transcriptional targets.
Technical Considerations: For validation, use quantitative PCR (qPCR) for known STAT target genes (e.g., SOCS1, IRF1 for STAT1). Include input DNA controls for normalization.
Protocol 3: Localization Studies Using Immunofluorescence and Live-Cell Imaging
Purpose: To visualize and quantify STAT nuclear translocation in response to cytokine stimulation.
Method Details:
- Immunofluorescence: Seed cells on glass coverslips, stimulate with cytokine, fix with 4% paraformaldehyde, and permeabilize with 0.1% Triton X-100. Incubate with STAT-specific primary antibodies followed by fluorophore-conjugated secondary antibodies. Mount and image by confocal microscopy [14].
- Live-Cell Imaging: Transfert cells with STAT-GFP fusion constructs. After cytokine stimulation, image cells over time using live-cell microscopy with environmental control. Quantify nuclear/cytoplasmic fluorescence ratio using image analysis software (e.g., ImageJ).
- FRAP Analysis: Perform Fluorescence Recovery After Photobleaching in the nucleus to assess STAT dynamics and shuttling.
Technical Considerations: Include leptomycin B (nuclear export inhibitor) to confirm active nuclear import. Use automated image analysis for high-throughput quantification.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagent Solutions for JAK-STAT Investigation
| Reagent Category | Specific Examples | Research Application | Mechanism of Action |
|---|---|---|---|
| JAK Inhibitors (Jakinibs) | Ruxolitinib (JAK1/2), Tofacitinib (JAK1/3), Oclacitinib, Filgotinib, Upadacitinib [14] [17] | Pathway inhibition studies, therapeutic validation | Competitive ATP-binding site inhibitors in JAK kinase domain (JH1) [17] |
| Phospho-Specific Antibodies | Anti-pY701-STAT1, Anti-pY705-STAT3, Anti-pY694-STAT5, Pan-phospho-STAT | Detection of activated STATs, Western blot, immunofluorescence | Recognize phosphorylated tyrosine residues in STAT transactivation domains |
| STAT DNA-Binding Probes | GAS consensus oligonucleotides (TTN5-6AA), ISRE probes | EMSA, reporter assays | Provide binding sites for STAT dimers to measure DNA-binding activity |
| Cytokine Reagents | Recombinant IFNs, IL-6, IL-4, IL-12, specific cytokine antagonists | Pathway activation, receptor studies | Activate or block specific cytokine receptors to initiate or inhibit JAK-STAT signaling |
| SOCS Expression Constructs | SOCS1, SOCS3, CIS overexpression vectors | Negative regulation studies | Endogenous feedback inhibitors that target JAKs and receptors for degradation [15] |
| STAT Knockout Cells/Animals | STAT1-/- mice, STAT3 conditional knockouts, CRISPR-Cas9 edited cells | Loss-of-function studies | Enable determination of STAT-specific functions in physiological contexts |
| Lysicamine | Lysicamine, CAS:15444-20-9, MF:C18H13NO3, MW:291.3 g/mol | Chemical Reagent | Bench Chemicals |
| Lysolipin I | Lysolipin I, CAS:59113-57-4, MF:C29H24ClNO11, MW:598.0 g/mol | Chemical Reagent | Bench Chemicals |
The canonical JAK-STAT activation mechanism—from receptor binding to nuclear translocation—represents an elegantly direct signaling pathway that enables rapid transcriptional responses to extracellular cues. The precise molecular choreography of receptor oligomerization, JAK trans-activation, STAT phosphorylation, nuclear translocation, and DNA binding provides multiple regulatory nodes that maintain signaling fidelity. Continued refinement of experimental approaches to study this pathway, including advanced genomic techniques and high-resolution imaging, yields increasingly sophisticated understanding of its operation in both health and disease. For inflammatory signaling research and drug development, targeting specific components of this canonical pathway—particularly with the advent of selective Jakinibs—offers promising therapeutic strategies for a spectrum of immune-mediated diseases. The integration of basic mechanistic knowledge with translational applications ensures that JAK-STAT research remains at the forefront of biomedical science.
Type I/II Cytokines and Their Specific Receptor-JAK-STAT Partnerships
The Janus kinase-signal transducer and activator of transcription (JAK-STAT) pathway serves as a fundamental signaling module for a vast array of cytokines, transmitting extracellular signals directly to the nucleus to regulate gene transcription. This canonical pathway is critically employed by over 50 type I and type II cytokines, which share structural similarities but utilize distinct receptor complexes. The specificity of cytokine signaling is achieved through precise, non-redundant partnerships between cytokine receptors, JAK kinases (JAK1, JAK2, JAK3, TYK2), and STAT transcription factors (STAT1-6). Dysregulation of these specific partnerships is implicated in numerous immune disorders, hematologic diseases, and cancers, making them compelling targets for therapeutic intervention. This whitepaper delineates the precise receptor-JAK-STAT partnerships for type I and type II cytokines, provides methodologies for their experimental investigation, and visualizes the core signaling cascades, thereby offering a framework for understanding their role in inflammatory signaling and targeted drug development.
The JAK-STAT pathway represents an elegantly simple membrane-to-nucleus signaling module, initially discovered through research into interferon (IFN) signaling [1] [9]. This pathway operates through a minimal set of components: extracellular cytokines, cell surface receptors, intracellular Janus kinases (JAKs), and signal transducers and activators of transcription (STATs) [18] [3]. More than 50 cytokines, including interleukins, interferons, colony-stimulating factors, and hormones, utilize this pathway to regulate critical processes such as hematopoiesis, immune responses, inflammation, and apoptosis [1] [18] [19].
The canonical signaling mechanism begins with cytokine binding to its cognate transmembrane receptor, inducing receptor dimerization or multimerization. This conformational change brings receptor-associated JAKs into close proximity, enabling their trans-activation through cross-phosphorylation on tyrosine residues [18] [3] [11]. The activated JAKs then phosphorylate specific tyrosine motifs on the receptor cytoplasmic tails, creating docking sites for latent cytoplasmic STAT proteins via their Src homology 2 (SH2) domains. Once recruited, STATs are themselves phosphorylated by JAKs on a conserved C-terminal tyrosine residue, prompting their dissociation from the receptor, dimerization (homo- or hetero-), and subsequent nuclear translocation. Within the nucleus, STAT dimers bind to specific promoter sequences to regulate the transcription of target genes [1] [18] [11].
Structural and Functional Classification of Cytokines and Receptors
Type I vs. Type II Cytokines: Structural and Receptor Paradigms
Cytokines signaling through the JAK-STAT pathway are broadly categorized as type I or type II based on their structural features and receptor complexes [19] [20].
Type I Cytokines (or hematopoietins) constitute the largest family and are characterized by a conserved structural fold comprising a bundle of four α-helices [21]. Their receptors are classified as type I cytokine receptors, which typically consist of multimeric complexes often featuring shared signaling subunits. Prominent subgroups within this family include:
- γc-family cytokines (IL-2, IL-4, IL-7, IL-9, IL-15, IL-21): Utilize the common gamma chain (γc, CD132) as a critical receptor component [1] [19].
- gp130-family cytokines (IL-6, IL-11, IL-27, IL-31, LIF, CNTF, OSM): Signal through the shared gp130 receptor subunit [1] [18].
- βc-family cytokines (IL-3, IL-5, GM-CSF): Employ the common beta chain (βc) [18].
- Homodimeric receptor cytokines (EPO, TPO, GH, Prolactin): Signal via homodimerization of their specific receptors [21] [18].
Type II Cytokines primarily include interferons (IFNs) and IL-10 related cytokines (IL-10, IL-19, IL-20, IL-22, IL-24, IL-26, IL-28, IL-29) [18] [19] [20]. These cytokines possess a slightly different helical bundle structure and engage type II cytokine receptors, which are structurally distinct from type I receptors but similarly lack intrinsic kinase activity [20].
A fundamental principle underlying the signaling of both cytokine classes is receptor oligomerization. The paradigm, established by structural studies of growth hormone signaling, involves cytokine engagement leading to receptor dimerization or reorganization of pre-formed receptor dimers, which is the critical event that triggers JAK activation and initiation of the signaling cascade [21].
Comprehensive Partnership Mapping: Cytokines, Receptors, JAKs, and STATs
The specificity of cellular responses to cytokines is largely determined by selective usage of JAK and STAT family members. This specificity arises from several factors: the restricted expression of certain receptor subunits (e.g., JAK3 with γc), the unique docking motifs presented on different activated receptors, and the expression patterns and SH2 domain specificities of different STATs [1] [22] [11].
Table 1: JAK-STAT Signaling Partnerships for Major Type I and Type II Cytokines
| Cytokine | Receptor Components | JAK Kinases | STAT Transcription Factors |
|---|---|---|---|
| IL-2, IL-15 | IL-2Rα/IL-15Rα + IL-2Rβ + γc | JAK1, JAK3 [1] [22] | STAT3, STAT5 [22] [19] |
| IL-4 | IL-4Rα + γc or IL-4Rα + IL-13Rα1 | JAK1, JAK3 [1] [22] [19] | STAT6 [22] [19] |
| IL-6, IL-11 | IL-6Rα/IL-11Rα + gp130 | JAK1, JAK2, TYK2 [1] [22] | STAT1, STAT3 (Primary for IL-11) [22] |
| IL-7 | IL-7R + γc | JAK1, JAK3 [1] [22] | STAT3, STAT5 [22] [19] |
| IL-12 | IL-12Rβ1 + IL-12Rβ2 | JAK2, TYK2 [1] [22] | STAT4 [22] [19] |
| IL-13 | IL-13Rα1 + IL-4Rα | JAK1, JAK2, TYK2 [22] [19] | STAT6 [22] [19] |
| IL-21 | IL-21R + γc | JAK1, JAK3 [1] [22] | STAT1, STAT3, STAT5 [22] [19] |
| IL-23 | IL-12Rβ1 + IL-23R | JAK2, TYK2 [1] [22] | STAT3, STAT4 [22] [19] |
| IL-27 | gp130 + WSX-1 | JAK1, JAK2, TYK2 [22] | STAT1, STAT2, STAT3, STAT4, STAT5 [22] |
| IFN-α/β (Type I) | IFNAR1 + IFNAR2 | JAK1, TYK2 [1] [22] [20] | STAT1, STAT2 (Primary), STAT3,4,5,6 (Secondary) [22] [20] |
| IFN-γ (Type II) | IFN-γR1 + IFN-γR2 | JAK1, JAK2 [1] [22] [20] | STAT1 [22] [19] [20] |
| IL-10 | IL-10Rα + IL-10Rβ | JAK1, TYK2 [1] [22] | STAT1, STAT3, STAT5 [22] |
| GM-CSF, IL-3, IL-5 | α-chain + βc | JAK2 [1] [22] [19] | STAT3, STAT5, STAT6 (for IL-3, IL-5) [22] [19] |
| EPO, TPO, Prolactin | Homodimeric Receptors | JAK2 [1] [22] | STAT5 (Mainly STAT5a for EPO/Pro) [22] [19] |
| G-CSF | G-CSFR | JAK2, TYK2 (Lyn) [22] | STAT3 [22] |
Table 2: Functional Consequences of JAK or STAT Deficiency
| Component | Phenotype of Knockout/Deficiency | Implication |
|---|---|---|
| JAK1 | Perinatal lethality; severe lymphocyte defects, neurological issues [1]. | Critical for γc, gp130, and class II cytokine receptor signaling [1]. |
| JAK2 | Embryonic lethality at ~E12.5 due to defective erythropoiesis [1]. | Essential for EPO, TPO, GH, and IL-3 receptor family signaling [1]. |
| JAK3 | Defective lymphocyte development; Severe Combined Immunodeficiency (SCID)-like phenotype [1]. | Non-redundant role in signaling from γc-chain receptors [1]. |
| TYK2 | Partial defects in IFN-α/β and IL-12 signaling; susceptible to infections [1]. | Modulates signaling for multiple cytokines (IFNs, IL-12, IL-23) but is not always absolutely required [1]. |
| STAT1 | High susceptibility to viral and microbial infections [9]. | Master regulator of IFN signaling and antiviral defense [9] [20]. |
| STAT3 | Embryonic lethality; critical for IL-6 family cytokine signaling [9]. | Key for acute-phase response, Th17 differentiation, and is often constitutively active in cancers [9] [11]. |
| STAT4 | Impaired Th1 differentiation and IFN-γ production [11]. | Mediates responses to IL-12 and type I IFNs [11]. |
| STAT6 | Impaired Th2 differentiation and allergic responses [11]. | Primary transducer of IL-4 and IL-13 signaling [11]. |
Experimental Analysis of JAK-STAT Partnerships
Elucidating the specific JAK-STAT components engaged by a cytokine is fundamental to research in immunology and signal transduction. Below are core methodologies employed in the field.
Protocol 1: Assessing STAT Phosphorylation and Activation
Objective: To determine which STAT protein(s) are activated by a cytokine of interest in a specific cell type.
Principle: Cytokine-induced activation of STATs is marked by their tyrosine phosphorylation. This can be detected by immunoblotting whole-cell lysates with phospho-specific antibodies.
Materials:
- Research Reagent Solutions: Cell line expressing the relevant cytokine receptor; recombinant target cytokine; phospho-STAT specific antibodies (e.g., pSTAT1, pSTAT3, pSTAT5, pSTAT6); total STAT antibodies for normalization; cell culture lysis buffer (e.g., RIPA buffer) supplemented with protease and phosphatase inhibitors; SDS-PAGE and immunoblotting equipment.
Methodology:
- Serum Starvation: Culture cells to 70-80% confluence and serum-starve them for 4-6 hours to reduce basal signaling.
- Cytokine Stimulation: Stimulate cells with the target cytokine (e.g., 10-50 ng/mL) for a time-course (e.g., 0, 5, 15, 30, 60 minutes). Include an unstimulated control.
- Cell Lysis: Rapidly aspirate media and lyse cells in ice-cold lysis buffer.
- Immunoblotting: Resolve equal amounts of protein by SDS-PAGE, transfer to a membrane, and probe with phospho- specific STAT antibodies.
- Membrane Stripping and Reprobing: Strip the membrane and re-probe with total STAT antibodies to confirm equal loading and calculate the phosphorylation ratio.
Protocol 2: Co-Immunoprecipitation (Co-IP) to Identify Receptor-JAK Associations
Objective: To verify the physical interaction between a cytokine receptor and specific JAK kinases.
Principle: JAKs are constitutively associated with cytokine receptors. An antibody against the receptor can be used to immunoprecipitate the receptor-JAK complex, which can then be detected by immunoblotting.
Materials:
- Research Reagent Solutions: Antibody against the extracellular domain of the target cytokine receptor; species-matched control IgG; Protein A/G agarose beads; mild, non-denaturing lysis buffer (e.g., with 1% NP-40 or Triton X-100) to preserve protein complexes; antibodies for JAK1, JAK2, JAK3, TYK2.
Methodology:
- Cell Lysis: Lyse cells in mild, non-denaturing lysis buffer.
- Pre-clearing: Incubate lysates with protein A/G beads alone to reduce non-specific binding.
- Immunoprecipitation: Incubate pre-cleared lysates with the receptor-specific antibody or control IgG overnight at 4°C. Add protein A/G beads the next day for 2-4 hours to capture the immune complexes.
- Washing and Elution: Wash beads extensively with lysis buffer to remove non-specifically bound proteins. Elute bound proteins by boiling in SDS-PAGE sample buffer.
- Analysis: Perform immunoblotting on the eluted proteins using antibodies against different JAKs to identify which one(s) co-precipitate with the receptor.
Protocol 3: Electrophoretic Mobility Shift Assay (EMSA) for STAT-DNA Binding
Objective: To confirm the functional outcome of STAT activation by demonstrating its specific binding to DNA consensus sequences.
Principle: Activated, dimerized STATs bind to specific DNA sequences. This binding reduces the electrophoretic mobility of the DNA probe in a native gel.
Materials:
- Research Reagent Solutions: Biotin- or radioactively-labeled double-stranded DNA probe containing a consensus STAT binding site (e.g., GAS for STAT1/3/5 or ISRE for ISGF3); nuclear extraction kit; native polyacrylamide gel electrophoresis system; shift buffer.
Methodology:
- Nuclear Extraction: Prepare cytoplasmic and nuclear extracts from cytokine-stimulated and unstimulated cells.
- Binding Reaction: Incubate nuclear extracts with the labeled DNA probe in a binding buffer.
- Competition Assays: (For specificity) Include a 100-fold molar excess of unlabeled identical probe (specific competitor) or an unrelated probe (non-specific competitor) in separate reactions.
- Supershift Assay: (For STAT identification) Pre-incubate the nuclear extract with an antibody against a specific STAT protein. The antibody-STAT-DNA complex will migrate even more slowly ("supershift").
- Gel Electrophoresis and Detection: Resolve the reaction mixtures on a non-denaturing polyacrylamide gel. Transfer to a membrane if using biotin-labeled probes and detect using streptavidin-HRP and chemiluminescence.
Pathway Visualization and Regulatory Networks
The core JAK-STAT signaling mechanism and its key regulatory checkpoints are summarized in the following diagram.
Diagram 1: Canonical JAK-STAT Signaling Cascade. This diagram illustrates the core sequence of events: cytokine-receptor binding, JAK activation, STAT phosphorylation and dimerization, and nuclear translocation to drive gene expression.
The activity of the JAK-STAT pathway is tightly controlled by several families of negative regulators, forming a critical negative feedback loop.
Table 3: Key Negative Regulators of the JAK-STAT Pathway
| Regulator Family | Examples | Mechanism of Action |
|---|---|---|
| SOCS (Suppressor of Cytokine Signaling) | SOCS1, SOCS3, CIS | 1. Bind phosphorylated JAKs or receptors via SH2 domain to inhibit kinase activity. 2. Target JAK/receptor complexes for ubiquitination and proteasomal degradation. 3. SOCS genes are STAT targets, forming a classic negative feedback loop [18] [11]. |
| PTPs (Protein Tyrosine Phosphatases) | SHP1, SHP2, CD45, PTP1B | Dephosphorylate activated JAKs and/or receptors, thereby terminating signaling [18] [11]. |
| PIAS (Protein Inhibitors of Activated STATs) | PIAS1, PIAS3, PIASx, PIASy | 1. Bind to phosphorylated STAT dimers and inhibit their DNA-binding activity. 2. Promote SUMOylation of STATs and other transcription factors [11]. |
The Scientist's Toolkit: Essential Research Reagents
A curated selection of critical reagents for investigating cytokine-JAK-STAT partnerships is provided below.
Table 4: Essential Research Reagents for JAK-STAT Pathway Investigation
| Reagent Category | Specific Examples | Primary Function in Research |
|---|---|---|
| Phospho-Specific Antibodies | Anti-pSTAT1 (Tyr701), Anti-pSTAT3 (Tyr705), Anti-pSTAT5 (Tyr694), Anti-pJAK2 (Tyr1007/1008) | Detect activation-specific phosphorylation of JAKs and STATs by Western blot, flow cytometry, or immunofluorescence. |
| JAK Inhibitors (Jakinibs) | Tofacitinib (pan-JAK), Ruxolitinib (JAK1/2), Tofacitinib (JAK3-preferential) | Pharmacological tools to inhibit JAK kinase activity and validate the dependency of a cytokine response on specific JAKs. |
| Recombinant Cytokines | Human/Mouse IFN-γ, IL-6, IL-4, IL-2, etc. | Defined ligands to specifically activate their cognate receptors and downstream JAK-STAT pathways in vitro. |
| STAT DNA-Binding Probes | Biotin-labeled GAS (Gamma-Activated Sequence) or ISRE (IFN-Stimulated Response Element) probes | Detect active, DNA-binding STAT transcription factor complexes via EMSA. |
| siRNA/shRNA Libraries | siRNA pools targeting JAK1, JAK2, JAK3, TYK2, STAT1-6 | Knockdown gene expression to determine the necessity of specific pathway components for functional responses. |
| Lys-psi(CH2NH)-Trp(Nps)-OMe | Lys-psi(CH2NH)-Trp(Nps)-OMe, CAS:141365-20-0, MF:C24H31N5O4S, MW:485.6 g/mol | Chemical Reagent |
| H-Lys-Trp-Lys-OH | H-Lys-Trp-Lys-OH is a small peptide with researched antibacterial and antiviral activity. This product is for research use only and not for human use. |
Concluding Perspectives
The precise partnerships between type I/II cytokines, their receptors, and specific JAK-STAT components form a sophisticated communication network that dictates cellular fate in immunity and inflammation. The structural basis of cytokine-receptor engagement dictates which JAKs are activated, which in turn shapes the STAT dimer repertoire that enters the nucleus to define the transcriptional program. The quantitative tables and experimental frameworks provided in this whitepaper offer a roadmap for researchers to decode the functional outcomes of these interactions in specific pathological contexts.
The critical role of this pathway in disease is underscored by the clinical success of JAK inhibitors (Jakinibs) in conditions like rheumatoid arthritis and myeloproliferative neoplasms [9] [19]. Future research will continue to leverage detailed structural insights [21] [9] to engineer novel cytokines with tailored properties and develop next-generation therapeutics with improved specificity, moving beyond JAK inhibition to target specific STATs or pathological STAT complexes. A deep understanding of these specific partnerships is therefore not only fundamental to biology but also paramount for pioneering new therapeutic strategies in inflammatory disease and cancer.
The Janus kinase-signal transducer and activator of transcription (JAK-STAT) pathway serves as a critical communication node, transmitting signals from over 50 cytokines and growth factors to regulate fundamental processes including hematopoiesis, immune fitness, and inflammation [9] [1]. This direct membrane-to-nucleus signaling module, while architecturally simple, must be tightly controlled, as its dysregulation is implicated in a spectrum of pathologies ranging from autoimmune diseases to cancer [10]. The transient nature of cytokine responses indicates the existence of powerful molecular switches that terminate signaling [23]. The duration and intensity of a cell's response to cytokine are determined by the net effect of several sophisticated regulatory mechanisms that prevent sustained or excessive pathway activation [23] [24]. This in-depth technical guide examines the three principal families of negative regulators that ensure pathway homeostasis: the Suppressors of Cytokine Signaling (SOCS), Protein Inhibitors of Activated STATs (PIAS), and protein tyrosine phosphatases (PTPs). Understanding these regulatory systems is paramount for developing targeted therapeutic strategies for inflammatory diseases where JAK-STAT signaling is aberrantly active.
Molecular Mechanisms of Key Negative Regulators
The Suppressor of Cytokine Signaling (SOCS) Family
The SOCS family represents the primary inducible negative feedback system for the JAK-STAT pathway. This family comprises eight intracellular proteins (CIS and SOCS1-7), each featuring a central Src homology 2 (SH2) domain, a variable N-terminal domain, and a C-terminal SOCS box module [24]. Among these, CIS, SOCS1, SOCS2, and SOCS3 are the best characterized. Their mechanisms of action combine direct kinase inhibition with the generic targeting of associated proteins for proteasomal degradation.
- Mechanisms of Inhibition: SOCS proteins employ diverse strategies to suppress signaling. CIS and SOCS2 primarily function by competing with STATs for binding to phosphorylated tyrosine residues on activated cytokine receptors, thus sterically hindering STAT recruitment and activation [24]. In contrast, SOCS1 and SOCS3 directly inhibit JAK tyrosine kinase activity. Their key structural feature is a kinase inhibitory region (KIR) within the N-terminal domain, which acts as a pseudosubstrate for JAKs [24]. While SOCS1 binds directly to the activation loop of JAKs via its SH2 domain, SOCS3 typically binds to phosphorylated tyrosine residues on the cytokine receptor (e.g., Tyr757 on gp130, Tyr985 on the leptin receptor), thereby positioning its KIR to inhibit the associated JAK [24].
- Role of the SOCS Box: The SOCS box serves as a universal recruitment module for the ubiquitin-transferase system. It interacts with Elongins B and C, Cullin-5 or Cullin-2, and Rbx-1 to form an E3 ubiquitin ligase complex [24]. This complex mediates the ubiquitination of proteins bound to the N-terminal regions of SOCS proteins, targeting them for proteasomal degradation. This mechanism is crucial for the suppression of oncogenic signaling, as evidenced by the necessity of the SOCS box in SOCS1 for suppressing TEL-JAK2 and degrading activated JAK2 [24]. The SOCS box also contributes to the stability and turnover of the SOCS proteins themselves [24].
Table 1: Key Members of the SOCS Family and Their Functions
| Protein | Primary Mechanism of Action | Key Target Interactions | Physiological/Role from KO Mouse Models |
|---|---|---|---|
| CIS | Competes with STAT5 for receptor binding [24] | Phosphorylated EPO, IL-2, IL-3, prolactin receptors [24] | Negative regulator of STAT5; transgenic mice show growth retardation, impaired mammary gland development [24]. |
| SOCS1 | Binds JAKs via SH2 domain; KIR acts as pseudosubstrate [24] | JAK1, JAK2, TYK2; also targets Vav, IRS-1/2 for degradation [24] | Critical regulator of IFN-γ signaling; KO mice die neonatally with lymphopenia, liver necrosis, macrophage infiltration [24]. |
| SOCS2 | Competes with STATs for receptor binding [24] | Growth hormone (GH) receptor [24] | Negative regulator of GH-STAT5b; KO mice exhibit 30-40% increased body weight, organ hypertrophy [24]. |
| SOCS3 | Binds phosphorylated receptor; KIR inhibits associated JAK [24] | gp130 (Tyr757), leptin receptor (Tyr985), EPO receptor [24] | Key regulator of IL-6, leptin, and G-CSF signaling; embryonic lethality in KO mice [24]. |
The following diagram illustrates the multi-faceted inhibitory mechanisms employed by SOCS proteins:
Protein Inhibitors of Activated STATs (PIAS)
The PIAS family constitutes a second tier of regulation that operates at the level of activated STAT dimers within the nucleus. Initially discovered as inhibitors that bind to activated STATs, PIAS proteins suppress STAT-mediated transcription through several distinct mechanisms [25].
- Mechanisms of Inhibition: The primary action of PIAS proteins involves direct physical interaction with activated STAT dimers. This binding can block the DNA-binding activity of STATs, thereby preventing them from associating with their target gene promoters [24] [25]. Furthermore, PIAS proteins function as E3 SUMO ligases. They facilitate the SUMOylation of STATs and other transcription factors, which modulates their activity, stability, and subcellular localization [25]. Through these actions, PIAS proteins effectively dampen the transcriptional output of the JAK-STAT pathway, adding another layer of control following STAT nuclear translocation.
Protein Tyrosine Phosphatases (PTPs)
A third fundamental mechanism for attenuating JAK-STAT signaling involves the dephosphorylation of key phosphotyrosine residues by constitutively expressed protein tyrosine phosphatases. This process is essential for resetting the pathway to its basal state.
- Targets and Specific PTPs: PTPs act on multiple components of the activated signaling cascade. They can dephosphorylate the tyrosine kinases JAKs, directly turning off their catalytic activity [23] [25]. They also target phosphorylated tyrosine residues on cytokine receptors, eliminating docking sites for STAT proteins [23]. Finally, they can dephosphorylate activated STATs themselves in both the cytoplasm and nucleus, leading to STAT deactivation, dimer dissociation, and export from the nucleus [23]. Specific phosphatases implicated in this process include SH2-containing phosphatase (SHP-1), SHP-2, protein tyrosine phosphatase 1B (PTP1B), CD45, and T cell protein tyrosine phosphatase (TCPTP) [24] [25]. The coordinated action of these PTPs ensures a rapid termination signal, making dephosphorylation a critical first line of defense against sustained JAK-STAT activation.
Table 2: Overview of the Three Major Negative Regulatory Systems
| Regulator Family | Main Members | Site of Action | Primary Mechanism | Inducible/Constitutive |
|---|---|---|---|---|
| SOCS | CIS, SOCS1-7 [24] | Cytoplasm / Receptor complex | 1. Pseudokinase competition (KIR) [24]2. Receptor competition [24]3. Ubiquitin-mediated degradation [24] | Inducible (Feedback) |
| PIAS | PIAS1, PIAS3, PIASx, PIASy [25] | Nucleus | 1. Block STAT DNA-binding [25]2. Promote SUMOylation [25] | Constitutive / Inducible |
| PTPs | SHP-1, SHP-2, PTP1B, CD45, TCPTP [24] [25] | Cytoplasm / Nucleus | Dephosphorylation of JAKs, Receptors, and STATs [23] [25] | Constitutive |
The integrated relationship of these regulatory systems within the JAK-STAT pathway is summarized below:
Experimental Analysis in Inflammatory Disease Context
The critical role of negative regulation is profoundly evident in the context of inflammatory diseases, where its failure or insufficiency can drive pathology. Profiling the activation state of the JAK-STAT pathway and its regulators in patient tissues provides invaluable insights for targeted therapy.
Quantifying Pathway Activation: An Ulcerative Colitis Case Study
A 2025 prospective observational study on ulcerative colitis (UC) provides a template for experimentally assessing JAK-STAT activation in inflamed human tissue [26] [13]. The researchers employed a methodology centered on Western blot analysis to quantify the phosphorylation levels of key JAK-STAT components, revealing a distinct activation signature and important sex-based differences.
- Experimental Workflow and Key Findings:
- Patient Cohort and Sample Collection: The study enrolled 61 adult UC patients with endoscopic activity. Paired biopsies were collected from each patient during colonoscopy: from inflamed colonic mucosa (Mayo Endoscopic Score > 0) and non-inflamed mucosa (MES = 0) [13].
- Sample Processing: Tissue samples underwent mechanical digestion and sonication in a lysis buffer supplemented with protease and phosphatase inhibitors to preserve post-translational modifications. Protein concentration was determined using a colorimetric assay (Bio-Rad DC protein assay) [13].
- Western Blot Analysis: Activation (phosphorylation) of JAK1, JAK2, JAK3, TYK2, STAT1, STAT3, and STAT4 was quantified by Western blot. Proteins were separated on Bis-Tris gels, transferred to PVDF membranes, and probed with specific phospho-antibodies. β-actin was used as a loading control. A key technical aspect was the sequential stripping and re-probing of membranes to analyze multiple phospho-proteins from the same sample, ensuring direct comparability [13].
- Data Analysis: Band intensity was quantified using ImageJ software. Phosphorylation levels in inflamed tissue were compared to the patient's own non-inflamed tissue, which served as an internal control [13].
Table 3: Key Findings from UC JAK-STAT Activation Study
| Protein | Phosphorylation Status in Inflamed vs. Non-Inflamed Tissue | Key Correlations and Notes |
|---|---|---|
| JAK1 | No significant difference [26] [13] | Suggests a non-pivotal role in UC inflammation. |
| JAK2 | Significantly increased [26] [13] | Coordinated activation with JAK3, TYK2, STAT3. Higher in males [26] [13]. |
| JAK3 | Significantly increased [26] [13] | Part of a coordinated activation cluster [26]. |
| TYK2 | Significantly increased [26] [13] | Part of a coordinated activation cluster [26]. |
| STAT1 | Significantly increased [26] [13] | -- |
| STAT3 | Significantly increased [26] [13] | Coordinated activation with JAK2, JAK3, TYK2. Higher in males [26] [13]. |
| STAT4 | Significantly increased [26] [13] | -- |
The experimental workflow from this study is detailed below:
The Scientist's Toolkit: Key Research Reagents and Methods
The following table compiles essential reagents and methodologies utilized in the cited UC study and relevant for general research into JAK-STAT pathway negative regulation.
Table 4: Research Reagent Solutions for JAK-STAT Pathway Analysis
| Reagent / Method | Specific Example / Kit | Function in Experimental Design |
|---|---|---|
| Phospho-Specific Antibodies | Commercial antibodies for p-JAK1, p-JAK2, p-JAK3, p-TYK2, p-STAT1, p-STAT3, p-STAT4 [13] | Semiquantitative detection of activated (phosphorylated) pathway components via Western blot. |
| Protein Extraction & Stabilization | Lysis Buffer (Tris, NaCl, EDTA) with Complete EDTA-free Protease Inhibitor and PhosSTOP [13] | Preserves native protein state and prevents dephosphorylation/degradation during sample preparation. |
| Protein Quantification Assay | Bio-Rad DC Protein Assay [13] | Colorimetric determination of total protein concentration for equal loading across gels. |
| Western Blot Substrates | Pierce ECL Western Blotting Substrate [13] | Chemiluminescent detection of HRP-conjugated antibodies for protein band visualization. |
| Membrane Stripping Buffer | Restore Western Blot Stripping Buffer [13] | Allows sequential probing of multiple targets on a single membrane, conserving sample and ensuring internal comparison. |
| SOCS/Signaling Studies | SOCS-family KO mouse models [24] | In vivo validation of regulator function; e.g., SOCS1-/- mice model IFN-γ-dependent inflammation. |
| m-3M3FBS | m-3M3FBS, CAS:200933-14-8, MF:C16H16F3NO2S, MW:343.4 g/mol | Chemical Reagent |
| Madrasin | Madrasin, MF:C16H17N5O2, MW:311.34 g/mol | Chemical Reagent |
Discussion and Therapeutic Implications
The sophisticated interplay between JAK-STAT activation and its negative regulators is a decisive factor in inflammatory disease pathogenesis and treatment. The documented heterogeneity in JAK-STAT activation patterns in UC, including the pronounced JAK2/STAT3 activation in males, underscores the limitations of a one-size-fits-all therapeutic approach and highlights the potential of personalized medicine [26] [13]. The success of small-molecule JAK inhibitors (JAKinibs) in treating immune-mediated diseases like rheumatoid arthritis and ulcerative colitis validates the pathway as a drug target [9] [27]. However, a deeper understanding of negative regulators opens new avenues for therapeutic innovation.
Targeting negative regulators offers a promising alternative or complementary strategy to direct JAK inhibition. For instance, augmenting SOCS function could be a viable approach to suppress pathological signaling. Strategies could include developing SOCS-mimetic peptides that replicate the KIR function of SOCS1/SOCS3, or gene therapy approaches to enhance SOCS expression in specific tissues [28]. Similarly, modulating PIAS activity could fine-tune the transcriptional output of STATs, offering a more targeted intervention compared to broad JAK inhibition. Furthermore, the activity of PTPs could potentially be enhanced pharmacologically to accelerate signal termination. The ongoing research into the structural biology of these regulators, fueled by advances in cryo-electron microscopy, is critical for rational drug design [9].
In conclusion, the negative regulators SOCS, PIAS, and PTPs are not mere off-switches; they are integral components of a dynamic homeostatic system that shapes the intensity, duration, and specificity of JAK-STAT signaling. Their critical role is vividly demonstrated in disease states where their function is compromised. Integrating the profiling of pathway activation and regulator expression into clinical research is therefore essential for developing the next generation of targeted, effective, and personalized anti-inflammatory therapies.
The Janus kinase–signal transducer and activator of transcription (JAK-STAT) pathway is a cornerstone of cellular signaling, traditionally recognized for its role in immune regulation and cytokine-mediated responses [29] [1]. However, emerging evidence reveals its critical involvement in neuroinflammation, stress-related disorders, and central nervous system (CNS) homeostasis [29] [30]. Dysregulation of this pathway contributes to pathologies ranging from neurodegenerative diseases (e.g., Alzheimer’s and Parkinson’s) to psychiatric conditions (e.g., depression) [29] [31]. This review synthesizes current knowledge on the non-immune functions of the JAK-STAT pathway, emphasizing experimental methodologies, quantitative data, and therapeutic implications for researchers and drug developers.
Pathway Composition and Activation Mechanisms
The JAK-STAT cascade comprises four JAK kinases (JAK1, JAK2, JAK3, TYK2) and seven STAT transcription factors (STAT1–STAT6, including STAT5A/B) [1]. Activation occurs via cytokine binding (e.g., interleukins, interferons) to transmembrane receptors, inducing JAK transphosphorylation. STATs are subsequently recruited, phosphorylated, and dimerize before translocating to the nucleus to regulate gene expression [1] [32]. Key domains include:
- JH1: Catalytic kinase domain.
- JH2: Pseudokinase domain regulating activity.
- SH2 and FERM: Facilitate receptor binding and STAT recruitment [1].
Table 1: JAK Family Members and Their Roles
| JAK Isoform | Associated Receptors | Primary Functions | Knockout Phenotypes |
|---|---|---|---|
| JAK1 | γc receptor subunit, gp130, IFN receptors | Immune modulation, neuroinflammation | Perinatal lethality; neuronal and lymphoid defects |
| JAK2 | EPO, GH, prolactin receptors | Hematopoiesis, neuroendocrine signaling | Embryonic lethality due to defective erythropoiesis |
| JAK3 | γc receptor subunit (IL-2, IL-4, etc.) | Lymphocyte development | Severe combined immunodeficiency (SCID) |
| TYK2 | IL-12, IL-23, IFN-α/β receptors | Antiviral responses, Th17 differentiation | Partial cytokine signaling defects |
JAK-STAT in CNS Homeostasis and Neuroinflammation
Homeostatic Maintenance
Despite modest expression in the CNS, the JAK-STAT pathway is critical for cortical, hippocampal, and cerebellar function [29]. It regulates:
- Neurotransmitter signaling (e.g., serotonin receptor cross-talk) [29].
- Glia-driven homeostasis: Astrocytes and microglia use JAK-STAT to balance pro-/anti-inflammatory cytokines [29] [31].
- Neural repair: STAT3 activation promotes axon regeneration and remyelination post-injury [30].
Neuroinflammatory and Neurodegenerative Pathologies
Chronic JAK-STAT activation drives neuroinflammation via microglial/astrocyte hyperactivation, linking it to:
- Alzheimer’s disease (AD): STAT hyperphosphorylation correlates with Aβ plaque burden and tau hyperphosphorylation [31].
- Parkinson’s disease: α-synuclein aggregates activate JAK-STAT, amplifying dopaminergic neuron loss [29] [30].
- Stress-induced disorders: Psychoemotional stress elevates pro-inflammatory cytokines (e.g., IL-6), activating JAK-STAT in limbic regions to foster anxiety/depression [29].
Table 2: JAK-STAT Dysregulation in Neurological Disorders
| Disease | Key STATs Involved | Upstream Activators | Pathogenic Consequences |
|---|---|---|---|
| Alzheimer’s Disease | STAT1, STAT3 | IL-6, IFN-γ, Aβ plaques | Microglial activation, synaptic loss, cognitive decline |
| Parkinson’s Disease | STAT1, STAT3 | α-synuclein, IL-1β | Dopaminergic neuron apoptosis, neuroinflammation |
| Depression | STAT3, STAT5 | IL-6, cortisol, chronic stress | HPA axis dysregulation, hippocampal atrophy |
| Multiple Sclerosis | STAT1, STAT4 | IFN-γ, IL-12/23 | T-cell infiltration, demyelination |
Stress Responses and Crosstalk with Neuroendocrine Pathways
Chronic stress triggers maladaptive neuroinflammation by activating JAK-STAT in glial cells, leading to:
- HPA axis dysregulation: Glucocorticoid resistance and heightened IL-6/JAK-STAT signaling [29].
- Cellular pro-inflammatory stress: Oxidative stress and metabolic demands in neurons exacerbate JAK-STAT activity [29].
- Limbic system alterations: Hippocampal STAT3 activation impairs neurogenesis, reinforcing depressive-like behaviors [29] [33].
Experimental Insight: In murine endometriosis models, JAK-STAT inhibition reduced pain sensitization and hippocampal inflammation, highlighting its role in stress-pain circuitry [33] [34].
Experimental Methodologies for JAK-STAT Research
In Vitro and Cellular Assays
Phosphorylation Analysis:
- Protocol: Stimulate cells (e.g., primary microglia, SH-SY5Y) with IL-6 (10–50 ng/mL) for 15–30 min. Lyse cells, immunoprecipitate STATs, and detect p-STAT/STAT ratios via Western blot (antibodies: anti-pSTAT3 [Tyr705], anti-STAT3) [1] [31].
- Validation: JAK inhibition (e.g., 1 μM tofacitinib) should abolish phosphorylation.
Gene Reporter Assays:
- Protocol: Transfect cells with a STAT-responsive luciferase construct (e.g., pSTAT3-TA-luc). After cytokine exposure, measure luminescence to quantify transcriptional activity [32].
In Vivo Models
- Neuroinflammatory Studies:
- Model: LPS-induced neuroinflammation in C57BL/6 mice (5 mg/kg i.p.).
- Endpoint: JAK-STAT activation in cortical lysates via ELISA/JAK2/STAT3 phosphorylation [31].
- Behavioral Assessments:
- Forced Swim Test (FST): Measure immobility time in JAK inhibitor-treated vs. control rodents to assess antidepressant effects [29].
Imaging and Molecular Techniques
- Immunofluorescence: Localize p-STAT3 in brain sections (e.g., hippocampus) using Alexa Fluor-conjugated antibodies [33].
- RNA-Seq: Profile STAT-regulated genes in laser-captured microglia from post-mortem AD brains [31].
Visualization of JAK-STAT Signaling in Neuroinflammation
Below is a DOT script modeling JAK-STAT activation in CNS disorders:
Title: JAK-STAT Activation in CNS Pathologies
Therapeutic Targeting and Research Tools
JAK Inhibitors (Jakinibs)
First-generation (e.g., tofacitinib) and isoform-selective inhibitors (e.g., filgotinib [JAK1], upadacitinib [JAK1]) show efficacy in autoimmune and neuroinflammatory models [29] [32]. Combination therapies with monoclonal antibodies enhance specificity [29].
Table 3: Research Reagent Solutions for JAK-STAT Studies
| Reagent/Tool | Function | Example Application |
|---|---|---|
| Tofacitinib (CP-690550) | Pan-JAK inhibitor | Suppresses STAT3 phosphorylation in microglia; 1–10 μM in vitro |
| AG490 | JAK2/STAT3 inhibitor | Reduces infarct volume in cerebral ischemia models; 5 mg/kg i.p. in mice |
| Anti-pSTAT3 (Tyr705) Antibody | Phospho-STAT detection | Immunofluorescence/Western blot for nuclear pSTAT3 quantification |
| STAT-responsive Luciferase Reporters | Transcriptional activity | High-throughput screening of JAK inhibitors in transfected cells |
| JAK3-KO Mice | Genetic loss-of-function | Study lymphocyte and neural defects in SCID models |
Natural Products as JAK Inhibitors
Natural compounds (e.g., naringenin [JAK1], myricetin [JAK1/STAT3]) offer novel scaffolds for inhibitor design [32]. For instance:
- Ellagic acid: Inhibits JAK1/STAT1 and NOX4 in renal ischemia-reperfusion models [32].
- Isobavachalcone: Dual PI3K-AKT and JAK1-STAT3 inhibition in rheumatoid arthritis [32].
The JAK-STAT pathway extends far beyond immunity, acting as a key integrator of stress, CNS homeostasis, and neuroinflammatory signaling. Future work should:
- Develop CNS-penetrant isoform-specific inhibitors to minimize off-target effects.
- Explore crosstalk with Nrf2, mTOR, and BACE-1 pathways in neurodegeneration [30] [31].
- Leverage single-cell omics to map JAK-STAT cell-type-specific roles in human brains.
By bridging basic science and clinical applications, targeting JAK-STAT signaling offers transformative potential for treating neurological and stress-related disorders.
Research Tools and Therapeutic Translation: Targeting the JAK-STAT Pathway
Preclinical Models for Studying JAK-STAT Dysregulation in Inflammation
The Janus kinase-signal transducer and activator of transcription (JAK-STAT) pathway serves as a crucial intracellular signaling cascade, transmitting signals from over 50 cytokines and growth factors involved in immune regulation, hematopoiesis, and tissue homeostasis [1] [35]. This evolutionarily conserved pathway represents a paradigm for signal transduction from the extracellular environment to the nucleus, functioning as a central communication node in cellular processes [9]. Dysregulation of JAK-STAT signaling has been firmly established as a cornerstone in the pathogenesis of diverse inflammatory and autoimmune diseases, including rheumatoid arthritis, psoriasis, inflammatory bowel disease, and atopic dermatitis [17] [36] [10]. The pathway's significance in inflammatory signaling research stems from its position as a fulcrum connecting extracellular cytokine signals to transcriptional programs that drive immune cell activation, differentiation, and inflammatory mediator production.
The JAK-STAT pathway operates through a deceptively simple architectural framework comprising three principal components: cytokine receptors, JAK kinases, and STAT transcription factors [5]. This direct membrane-to-nucleus signaling module enables rapid transcriptional responses to environmental stimuli without secondary messengers. The JAK family consists of four cytoplasmic tyrosine kinases—JAK1, JAK2, JAK3, and TYK2—while the STAT family includes seven transcription factors—STAT1, STAT2, STAT3, STAT4, STAT5A, STAT5B, and STAT6 [1] [36]. The specificity of signaling is achieved through distinct receptor-chain associations and combinatorial activation of STAT proteins, creating a sophisticated regulatory network that governs inflammatory responses [17].
Table 1: Core Components of the JAK-STAT Signaling Pathway
| Component Type | Family Members | Key Functions in Inflammation |
|---|---|---|
| JAK Kinases | JAK1, JAK2, JAK3, TYK2 | Cytokine receptor association; tyrosine phosphorylation; signal initiation |
| STAT Transcription Factors | STAT1-6 (including STAT5A/B) | DNA binding; transcriptional regulation; target gene activation |
| Receptor Families | Type I/II cytokine receptors | Cytokine recognition; receptor dimerization; JAK recruitment |
| Negative Regulators | SOCS, PIAS, PTPs | Signal termination; feedback inhibition; pathway modulation |
JAK-STAT Pathway Architecture and Activation Mechanisms
Structural Basis of JAK-STAT Signaling
The molecular architecture of JAK-STAT pathway components reveals critical insights into their function and regulation. JAKs contain seven JAK homology (JH) domains, with JH1 representing the catalytically active kinase domain and JH2 functioning as a pseudokinase domain that regulates kinase activity [17] [1]. The JH3-JH7 domains form the FERM and SH2-like regions that mediate receptor binding [36]. STAT proteins share a conserved domain structure featuring an N-terminal domain that facilitates protein-protein interactions, a coiled-coil domain, a DNA-binding domain, a linker region, an SH2 domain that mediates phosphotyrosine binding and STAT dimerization, and a C-terminal transactivation domain [17] [10]. These structural features enable the precise molecular interactions that govern pathway activation and nuclear translocation.
The canonical JAK-STAT activation cascade initiates when extracellular cytokines bind to their cognate transmembrane receptors, inducing receptor dimerization or oligomerization [17] [27]. This conformational change brings receptor-associated JAKs into proximity, leading to their trans-phosphorylation and activation. The activated JAKs then phosphorylate specific tyrosine residues on the receptor cytoplasmic tails, creating docking sites for STAT proteins via their SH2 domains [27] [5]. Once recruited, STATs undergo JAK-mediated phosphorylation at conserved C-terminal tyrosine residues, triggering their dissociation from the receptor and facilitating STAT dimerization through reciprocal SH2-phosphotyrosine interactions [9]. These STAT dimers then translocate to the nucleus, where they bind specific promoter elements and regulate the transcription of target genes involved in inflammatory processes [9] [10].
Figure 1: Canonical JAK-STAT Pathway Activation. Cytokine binding induces receptor activation and JAK phosphorylation, leading to STAT recruitment, phosphorylation, dimerization, nuclear translocation, and target gene regulation.
Negative Regulation and Feedback Mechanisms
The JAK-STAT pathway incorporates sophisticated negative feedback mechanisms to ensure precise control of signaling duration and intensity, preventing excessive inflammatory responses. Three major classes of negative regulators fine-tune pathway activity: suppressors of cytokine signaling (SOCS), protein inhibitors of activated STATs (PIAS), and protein tyrosine phosphatases (PTPs) [36] [37]. SOCS proteins function as inducible feedback inhibitors that compete with STATs for receptor docking sites, directly inhibit JAK catalytic activity, or target pathway components for proteasomal degradation via E3 ubiquitin ligase activity [37]. The PIAS family proteins interact with STAT dimers to block DNA binding or recruit transcriptional corepressors, while PTPs such as SHP1, SHP2, and CD45 dephosphorylate JAKs, receptors, and STATs to terminate signaling [36] [37]. This multi-layered regulatory network ensures precise control of JAK-STAT-mediated inflammatory responses and presents additional targets for therapeutic intervention.
Preclinical Model Systems for JAK-STAT Dysregulation
In Vitro Model Systems
Cell-based models provide reductionist systems for dissecting specific aspects of JAK-STAT signaling in inflammation. Immortalized cell lines offer reproducible, scalable platforms for initial pathway characterization and therapeutic screening. Macrophage-like cell lines (RAW264.7, THP-1), T-cell lines (Jurkat), and epithelial cell lines respond to inflammatory cytokines and demonstrate JAK-STAT activation under controlled conditions [17]. Primary cells isolated from human donors or animal tissues, including peripheral blood mononuclear cells (PBMCs), synovial fibroblasts, and intestinal epithelial cells, maintain physiological relevance while enabling investigation of cell-type-specific JAK-STAT responses in inflammatory contexts [27].
Advanced in vitro systems have emerged to better model the complexity of inflammatory environments. Primary human cell co-cultures recapitulate cell-cell interactions central to inflammation, such as T cell-macrophage or epithelial cell-immune cell cross-talk [27]. Patient-derived primary cells from diseased tissues (e.g., synovial fluid from rheumatoid arthritis patients, skin biopsies from psoriasis patients) preserve the pathological signaling signatures of human disease, including characteristic JAK-STAT activation patterns [17]. Three-dimensional organoid systems developed from intestinal, synovial, or skin tissues incorporate multiple cell types and more accurately mimic tissue architecture and inflammatory microenvironmental cues than traditional monolayer cultures [9].
Table 2: Preclinical Models for Studying JAK-STAT Dysregulation in Inflammation
| Model Category | Specific Examples | Applications in JAK-STAT Research | Key Advantages | Limitations |
|---|---|---|---|---|
| In Vitro Systems | Immortalized cell lines (RAW264.7, THP-1, Jurkat); Primary cells (PBMCs, synovial fibroblasts); Co-culture systems; 3D organoids | Pathway mechanism studies; High-throughput drug screening; Cell-type specific signaling analysis | High reproducibility; Genetic manipulation ease; Scalability for screening; Cost-effectiveness | Limited microenvironmental complexity; Absence of systemic regulation |
| In Vivo Animal Models | Collagen-induced arthritis (CIA); Imiquimod-induced psoriasis; DSS-induced colitis; Genetic models (JAK/STAT mutations) | Disease pathogenesis studies; Therapeutic efficacy evaluation; Systemic effect assessment; Toxicity profiling | Intact organismal context; Complex immune interactions; Pharmacokinetic assessment; Clinical translation potential | Species-specific differences; High cost and time requirements; Ethical considerations |
| Humanized Models | Human PBMC-engrafted mice; Human cytokine-expressing transgenic mice; Patient-derived xenografts (PDX) | Human-specific therapeutic evaluation; Human cytokine signaling analysis; Personalized medicine approaches | Direct human target relevance; Clinical prediction improvement; Patient-specific response modeling | Technical complexity; High cost; Limited availability |
In Vivo Animal Models
Rodent models of inflammatory disease provide indispensable platforms for studying JAK-STAT dysregulation in physiologically relevant contexts. Induced inflammation models, including collagen-induced arthritis (rheumatoid arthritis), imiquimod-induced skin inflammation (psoriasis), and dextran sulfate sodium (DSS)-induced colitis (inflammatory bowel disease), recapitulate key aspects of human inflammatory pathologies and demonstrate characteristic JAK-STAT activation [17] [27]. These models respond to JAK inhibition, validating their utility for preclinical therapeutic development [17].
Genetic mouse models with targeted manipulations of JAK-STAT components elucidate the specific contributions of pathway elements to inflammatory processes. Global and conditional knockout mice (JAK1^-/^-, JAK3^-/^-, STAT1^-/^-, STAT3^-/^-) reveal non-redundant functions of JAK-STAT members in immune cell development and inflammation [1] [36]. Constitutively active STAT transgenic mice model diseases driven by persistent JAK-STAT signaling, while humanized mice expressing human cytokine receptors or JAK proteins facilitate evaluation of human-specific therapeutics [36]. These genetic models have established that complete JAK1, JAK2, or STAT3 deficiencies result in perinatal lethality, underscoring their essential roles in development, while partial or tissue-specific deletions produce viable animals with specific immune and inflammatory phenotypes [1] [9].
Experimental Autoimmune Disease Models
Disease-specific autoimmune models enable detailed investigation of JAK-STAT dysregulation in particular inflammatory contexts. For rheumatoid arthritis research, the collagen-induced arthritis (CIA) model in mice and rats demonstrates synovial inflammation, cartilage degradation, and bone erosion accompanied by elevated JAK1/STAT3 activation, effectively modeling the human disease [17]. For psoriasis studies, the imiquimod-induced model exhibits epidermal hyperplasia, immune cell infiltration, and elevated Th17 cytokines dependent on JAK-STAT signaling, particularly STAT3 activation [36]. In inflammatory bowel disease research, the DSS colitis model displays intestinal epithelial damage, immune activation, and JAK-STAT dysregulation that responds therapeutically to JAK inhibition [17]. These validated models serve as critical bridges between basic pathway characterization and clinical translation.
Methodologies for Assessing JAK-STAT Dysregulation
Pathway Activation and Signaling Analysis
Comprehensive assessment of JAK-STAT dysregulation requires multi-level methodologies that quantify pathway components and activity. Phospho-flow cytometry enables high-throughput measurement of phosphorylated STAT proteins (pSTAT1, pSTAT3, pSTAT5, pSTAT6) at single-cell resolution in heterogenous cell populations, revealing cell-type-specific signaling patterns in complex inflammatory environments [17]. Western blotting remains the gold standard for validating STAT phosphorylation states and protein expression levels, while enzyme-linked immunosorbent assays (ELISAs) quantitatively measure cytokine concentrations in biological fluids and culture supernatants [27]. Immunofluorescence and immunohistochemistry provide spatial resolution of STAT localization and activation within tissues, revealing nuclear translocation in specific cellular compartments during inflammatory responses [27].
Genomic and transcriptional approaches elucidate the functional consequences of JAK-STAT activation. Chromatin immunoprecipitation (ChIP) assays, particularly STAT-specific ChIP, identify direct transcriptional targets by mapping STAT binding to genomic regulatory elements [36]. RNA sequencing comprehensively profiles transcriptomic changes downstream of JAK-STAT activation, revealing inflammatory gene signatures and pathway interactions [9]. Reverse transcription quantitative polymerase chain reaction (RT-qPCR) validates expression of key JAK-STAT target genes (e.g., SOCS3, IRF1, CISH) in response to inflammatory stimuli or inhibitory interventions [27]. These complementary approaches provide a comprehensive view of JAK-STAT pathway activity from signal initiation to functional outcomes.
Figure 2: Experimental Workflow for JAK-STAT Dysregulation Analysis. Integrated approach combining inflammatory stimulation with protein and gene expression analyses to comprehensively assess pathway activity.
Functional Assays for Inflammatory Responses
Functional assays contextualize JAK-STAT signaling measurements within biologically relevant inflammatory processes. Immune cell migration assays evaluate chemotactic responses dependent on JAK-STAT activation, while cell proliferation and viability assays measure growth regulation by cytokine-JAK-STAT axes [27]. Cytokine secretion profiling using multiplex bead arrays or ELISpot assays characterizes inflammatory mediator production downstream of JAK-STAT signaling [17]. For tissue-level analyses, histopathological scoring of inflammation, immune cell infiltration, and tissue architecture in target organs (joints, skin, intestine) correlates JAK-STAT activation with disease severity [27]. These functional readouts establish the physiological consequences of JAK-STAT dysregulation and provide critical validation for pathway-directed therapeutic interventions.
Table 3: Key Methodologies for Assessing JAK-STAT Dysregulation
| Method Category | Specific Techniques | Measured Parameters | Applications in Inflammation Research |
|---|---|---|---|
| Pathway Activation | Phospho-flow cytometry; Western blot; ELISA; Immunofluorescence | STAT phosphorylation; Nuclear translocation; JAK activation; Cytokine levels | Single-cell signaling analysis; Pathway kinetics; Spatial localization; Activation quantification |
| Genomic & Transcriptional | RNA-seq; RT-qPCR; ChIP-seq; Microarrays | Target gene expression; STAT DNA binding; Transcriptional networks | Inflammatory signature identification; Direct target validation; Pathway crosstalk mapping |
| Functional Assays | Cell migration; Proliferation; Cytokine secretion; Histopathology | Immune cell recruitment; Cellular expansion; Inflammatory mediator production; Tissue damage | Functional consequence assessment; Therapeutic efficacy evaluation; Disease severity correlation |
| Pharmacological Modulation | JAK inhibitor treatment; SOCS overexpression; siRNA knockdown | Pathway inhibition; Target validation; Specificity profiling | Mechanistic studies; Target validation; Therapeutic screening |
The Scientist's Toolkit: Research Reagent Solutions
Essential Reagents and Methodological Approaches
Advanced research tools enable precise dissection of JAK-STAT dysregulation in inflammatory contexts. Pharmacological JAK inhibitors ("jakinibs") represent cornerstone reagents for pathway modulation, with pan-JAK inhibitors (tofacitinib, ruxolitinib) and isoform-selective compounds (filgotinib-JAK1, upadacitinib-JAK1) providing tools to probe the contributions of specific JAK family members to inflammatory processes [17] [35]. Cytokine stimulation reagents (IFN-γ, IL-6, IL-4, IL-12, IL-23) activate distinct JAK-STAT signaling branches, while neutralizing antibodies against specific cytokines or their receptors enable targeted pathway interruption [27].
Genetic manipulation approaches offer precise, long-term pathway modulation. siRNA and shRNA-mediated knockdown of specific JAK or STAT isoforms reveals their non-redundant functions in inflammatory signaling cascades [36]. CRISPR-Cas9 gene editing enables complete JAK or STAT knockout in cell lines or primary cells, while conditional knockout mouse models (Cre-loxP system) facilitate tissue-specific and inducible JAK-STAT ablation in vivo [36]. Reporter cell lines (STAT-GFP, STAT-luciferase) provide real-time monitoring of pathway activity in living cells, and recombinant SOCS proteins serve as natural pathway inhibitors to dissect feedback mechanisms [37]. These complementary reagents form a comprehensive toolkit for interrogating JAK-STAT dysregulation across multiple experimental contexts.
Preclinical models for studying JAK-STAT dysregulation in inflammation span from reductionist cell systems to complex animal models, each offering unique insights into pathway pathophysiology. The integration of findings across these models, coupled with advanced methodological approaches for pathway assessment, continues to elucidate the central role of JAK-STAT signaling in inflammatory diseases. As our understanding of JAK-STAT biology deepens, preclinical models are evolving to better recapitulate human disease complexity, particularly through humanized systems and patient-derived samples. These advanced models, combined with increasingly selective pharmacological tools, promise to accelerate the development of novel JAK-targeted therapeutics with improved efficacy and safety profiles for inflammatory disorders. The continued refinement of preclinical models remains essential for translating basic JAK-STAT research into meaningful clinical interventions for patients suffering from chronic inflammatory conditions.
The Janus kinase-signal transducer and activator of transcription (JAK-STAT) pathway serves as a fundamental signaling cascade that transduces extracellular cytokine signals into transcriptional responses within the nucleus [9]. This pathway regulates critical cellular processes including proliferation, differentiation, apoptosis, and immune responses [38]. The architectural simplicity of the pathway—comprising cytokines, receptors, JAKs, and STATs—belies its functional complexity and broad influence on human physiology and disease [9].
Four JAK family members exist in mammalian cells: JAK1, JAK2, JAK3, and tyrosine kinase 2 (TYK2). These enzymes associate with the intracellular domains of type I and type II cytokine receptors [38]. Upon cytokine binding, receptor-associated JAKs undergo transphosphorylation, subsequently phosphorylating STAT proteins. Phosphorylated STATs then dimerize, translocate to the nucleus, and regulate gene transcription [38] [9]. Dysregulation of this pathway through excessive cytokine signaling or gain-of-function mutations drives numerous pathological conditions, particularly in immune-mediated diseases and hematological malignancies [9] [39]. This established the JAK-STAT pathway as a compelling target for therapeutic intervention, spurring the development of Janus kinase inhibitors (jakinibs) [40].
Structural Biology of the JAK-STAT Pathway
Molecular Architecture and Activation Mechanism
The structural organization of JAK proteins reveals conserved domains critical for their function. Each JAK contains a C-terminal tyrosine kinase domain (JH1) responsible for catalytic activity, preceded by a pseudokinase domain (JH2) that regulates kinase activity [39]. The N-terminal region consists of FERM and SH2 domains, which mediate constitutive association with cytokine receptors [38]. Signal initiation occurs through cytokine-induced receptor dimerization or multimerization, which brings associated JAKs into proximity for transphosphorylation and activation [9].
Table: JAK Family Members and Their Associated Cytokine Signaling Pathways
| JAK Family Member | Key Cytokine Signaling Pathways | Primary Biological Functions |
|---|---|---|
| JAK1 | Common γ-chain cytokines (IL-2, IL-4, IL-7, IL-9, IL-15, IL-21), IL-6 family cytokines (IL-6, IL-11), type II interferon (IFNγ) [38] | Broad immune function, neural development [39] |
| JAK2 | Common β-chain cytokines (IL-3, IL-5, GM-CSF), EPO, TPO, G-CSF, IFNγ [38] | Hematopoiesis, growth [39] |
| JAK3 | Common γ-chain cytokines (IL-2, IL-4, IL-7, IL-9, IL-15, IL-21) [38] | Immune response regulation [39] |
| TYK2 | Type I interferons (IFNα, IFNβ), IL-12, IL-23 [38] | Immune response regulation [39] |
| Maesopsin | Maesopsin, CAS:5989-16-2, MF:C15H12O6, MW:288.25 g/mol | Chemical Reagent |
| Mafenide | Mafenide, CAS:138-39-6, MF:C7H10N2O2S, MW:186.23 g/mol | Chemical Reagent |
The high degree of conservation in the ATP-binding cleft among JAK family members presented a significant challenge for developing selective inhibitors [39]. Advances in structural biology, particularly cryo-electron microscopy (cryo-EM), have enabled visualization of large protein complexes at near-atomic resolution, providing invaluable insights for structure-based drug design [9].
Figure 1: JAK-STAT Pathway Activation Cascade. This diagram illustrates the core signaling mechanism: cytokine binding induces receptor activation and JAK transphosphorylation, leading to STAT phosphorylation, dimerization, nuclear translocation, and regulation of gene transcription.
Evolution of JAK Inhibitors: Generations and Selectivity
First-Generation JAK Inhibitors
The first generation of jakinibs consisted of orthosteric ATP-competitive inhibitors that targeted multiple JAK family members with limited selectivity [41]. These pioneering compounds established the clinical utility of JAK inhibition across diverse therapeutic areas. Ruxolitinib, a JAK1/JAK2 inhibitor, was the first jakinib approved for myeloproliferative neoplasms (MPNs) often driven by JAK2 V617F gain-of-function mutations [40] [39]. Tofacitinib, inhibiting JAK1/JAK2/JAK3, became the first jakinib approved for rheumatoid arthritis (RA) and later for psoriatic arthritis (PsA) and ulcerative colitis (UC) [40]. These pan-jakinibs demonstrated that simultaneously blocking multiple cytokine pathways could yield potent anti-inflammatory effects but also produced characteristic side effects including anemia, thrombocytopenia, and increased infection risk [39].
Second-Generation Selective Inhibitors
To improve safety profiles, second-generation jakinibs were developed with enhanced selectivity for specific JAK family members [41]. These compounds remain orthosteric ATP competitors but were engineered for preferential binding to particular JAK isoforms. Upadacitinib and filgotinib were designed as JAK1-selective inhibitors, aiming to block pro-inflammatory cytokines while sparing JAK2-mediated hematopoiesis and JAK3-dependent immune cell functions [40]. Baricitinib, a JAK1/JAK2 inhibitor, demonstrated efficacy in RA, atopic dermatitis (AD), and emergency authorization for COVID-19 [40]. Deucravacitinib, a TYK2 inhibitor, represents a distinct approach by targeting the pseudokinase domain through allosteric inhibition, offering a novel mechanism with high specificity [42].
Table: Approved JAK Inhibitors and Their Selectivity Profiles
| Drug Name | Primary Molecular Targets | Key Approved Indications | Generation |
|---|---|---|---|
| Ruxolitinib | JAK1/JAK2 [40] [39] | Myeloproliferative neoplasms, acute GVHD [40] | First |
| Tofacitinib | JAK1/JAK2/JAK3 [40] [39] | RA, PsA, ulcerative colitis, polyarticular JIA [40] | First |
| Baricitinib | JAK1/JAK2 [40] [39] | RA, COVID-19 (EUA), AD [40] | Second |
| Upadacitinib | JAK1 [40] | RA [40] | Second |
| Filgotinib | JAK1 [40] | RA (EU, Japan) [40] | Second |
| Peficitinib | Multiple JAKs [40] | RA (Japan, Korea) [40] | First |
| Deucravacitinib | TYK2 [42] | Plaque psoriasis [42] | Second |
Third-Generation Allosteric Inhibitors
The most recent advance involves third-generation jakinibs that exploit structural insights to achieve unprecedented specificity. These agents function as allosteric inhibitors, binding to regulatory regions outside the conserved ATP-binding pocket [41]. Specifically, they target the pseudokinase domain (JH2), which naturally regulates the catalytic activity of the kinase domain (JH1) [41]. This approach circumvents the challenge of achieving selectivity within highly conserved ATP-binding sites and may offer improved safety profiles by preserving off-target kinase functions.
Figure 2: Evolution of JAK Inhibitor Generations. This timeline shows the progression from broad-spectrum first-generation inhibitors to increasingly selective second-generation agents and novel allosteric third-generation compounds.
Experimental Approaches in JAK Inhibitor Development
Structural-Based Virtual Screening
The discovery of selective JAK inhibitors has been accelerated by computational approaches. Structure-based virtual screening involves docking compounds from chemical libraries into target protein structures and selecting candidates based on binding scores and pharmacological interactions [39]. For JAK2 inhibitor identification, researchers have analyzed key pharmacological interactions in the JAK2 binding site using known inhibitors as templates, then performed virtual screening of databases such as the National Cancer Institute (NCI) compound collection [39]. Filtering compounds based on docking scores and interactions with key residues (particularly hinge region residues) improves hit rates for potential kinase inhibitors [39].
Protocol: Structure-Based Virtual Screening for JAK Inhibitors
- Target Preparation: Obtain the crystal structure of the target JAK kinase domain from the Protein Data Bank (e.g., PDB ID: 3JY9 for JAK2). Prepare the protein by adding hydrogen atoms, assigning protonation states, and removing water molecules.
- Compound Library Preparation: Curate a database of small molecule structures in appropriate formats. Apply chemical filters to remove non-druglike compounds and generate three-dimensional conformations.
- Molecular Docking: Use docking software (e.g., LeadIT, Sybyl, CDOCKER) to position each compound into the ATP-binding site of the target kinase. Score poses based on predicted binding affinity and interaction energy.
- Interaction Analysis: Filter docked compounds based on formation of key pharmacological interactions with hinge region residues (e.g., Glu930 and Leu932 in JAK2) and other conserved motifs.
- Hit Selection: Select top-ranking compounds for experimental validation based on docking scores, interaction profiles, and chemical novelty.
Assessment of JAK-STAT Pathway Activation in Disease
Understanding tissue-specific JAK-STAT pathway activation informs targeted therapeutic applications. A standardized protocol for quantifying phosphorylation levels of JAK-STAT components in patient tissue samples enables precision medicine approaches [13].
Protocol: Western Blot Analysis of JAK-STAT Phosphorylation in Tissue Biopsies
- Sample Preparation: Homogenize tissue biopsies in lysis buffer (e.g., 50 mM Tris, 150 mM NaCl, 5 mM EDTA) supplemented with protease and phosphatase inhibitors. Centrifuge at 10,000 × g for 10 minutes and quantify protein concentration using a standardized assay (e.g., Bio-Rad DC protein assay) [13].
- Gel Electrophoresis: Load 20 μg of total protein per lane onto 4-12% Bis-Tris Plus gels. Separate proteins at 120 V for 85 minutes using SDS-PAGE [13].
- Protein Transfer: Transfer proteins to PVDF membranes at 15 V for 90 minutes [13].
- Immunoblotting: Block membranes with 5% BSA, then incubate overnight at 4°C with phospho-specific primary antibodies against JAK1, JAK2, JAK3, TYK2, STAT1, STAT3, and STAT4. Use β-actin as a loading control. Incubate with HRP-conjugated secondary antibodies for 1 hour at room temperature [13].
- Detection and Quantification: Develop blots using enhanced chemiluminescence substrate. Capture images on a digital imaging system and perform quantitative band analysis using ImageJ software. Normalize phosphoprotein signals to loading controls [13].
The Scientist's Toolkit: Essential Research Reagents
Table: Key Research Reagents for JAK-STAT Pathway Investigation
| Reagent/Category | Specific Examples | Research Application | Experimental Function |
|---|---|---|---|
| Phospho-Specific Antibodies | Anti-pJAK1, pJAK2, pJAK3, pTYK2, pSTAT1, pSTAT3, pSTAT4 [13] | Western blot, immunohistochemistry | Detection of activated JAK-STAT pathway components |
| Selective JAK Inhibitors | Tofacitinib (pan-JAK), Ruxolitinib (JAK1/2), Upadacitinib (JAK1), Deucravacitinib (TYK2) [40] [42] | Functional validation, pathway modulation | Tool compounds for pharmacological inhibition studies |
| Cell-Based Reporter Assays | STAT-responsive luciferase constructs (e.g., STAT1, STAT3, STAT5) | High-throughput screening | Measurement of STAT transcriptional activity |
| Kinase Activity Assays | Recombinant JAK kinases (JAK1, JAK2, JAK3, TYK2) | Enzymatic profiling | Determination of inhibitor IC50 values and selectivity |
| Cytokine Stimulation Reagents | IFNγ, IL-6, IL-4, IL-12, IL-23 [38] | Pathway activation | Induction of JAK-STAT signaling in cellular models |
| Mafenide Hydrochloride | Mafenide Hydrochloride, CAS:138-37-4, MF:C7H11ClN2O2S, MW:222.69 g/mol | Chemical Reagent | Bench Chemicals |
| Malotilate | Malotilate, CAS:59937-28-9, MF:C12H16O4S2, MW:288.4 g/mol | Chemical Reagent | Bench Chemicals |
Clinical Translation and Therapeutic Applications
Efficacy Across Inflammatory Diseases
Jakinibs have demonstrated significant clinical efficacy across immune-mediated diseases. In rheumatoid arthritis, tofacitinib, baricitinib, upadacitinib, and filgotinib have shown superiority to methotrexate in clinical trials, with more rapid clinical effects observed as early as the first week of therapy [40]. For atopic dermatitis, real-world evidence confirms the effectiveness of JAK inhibitors, with Eczema Area and Severity Index (EASI)-75 response rates reaching 59% at 12 weeks and 86% at 52 weeks [43]. In ulcerative colitis, research reveals heterogeneous activation of JAK-STAT components, with inflamed tissue showing significantly increased phosphorylation of JAK2, JAK3, TYK2, STAT1, STAT3, and STAT4 compared to non-inflamed mucosa [13]. This pattern suggests the value of targeting specific JAK-STAT components based on individual patient pathology.
Safety Considerations and Pharmacovigilance
The safety profile of jakinibs reflects their target selectivity and pharmacological properties. First-generation pan-JAK inhibitors are associated with class-effect adverse events including opportunistic infections, anemia, neutropenia, and thrombocytopenia [39]. Real-world safety data from the FDA Adverse Event Reporting System (FAERS) database for psoriasis and psoriatic arthritis patients reveals that skin and subcutaneous tissue disorders, infections, and gastrointestinal disorders are frequently reported for JAK inhibitors [42]. Musculoskeletal and connective tissue disorders are prominent with upadacitinib and tofacitinib [42]. Sex-specific differences in adverse event profiles have been observed, with female subjects showing higher likelihood of developing skin and subcutaneous tissue disorders after tofacitinib treatment [42].
Emerging Frontiers and Future Directions
Natural products represent a promising resource for discovering novel JAK inhibitors with unique chemotypes. Recent research has identified 88 natural products with JAK inhibitory activity, classified by structural characteristics into flavonoids, alkaloids, and terpenoids [32]. Specific examples include Igalan (a sesquiterpene lactone from Inula helenium) that ameliorates epidermal barrier dysfunction through JAK1 inhibition, and cycloastragenol (a triterpenoid) that inhibits constitutive STAT3 activation through JAK1 suppression [32]. The structural diversity of natural products offers opportunities for developing next-generation JAK inhibitors with improved therapeutic profiles.
Personalized Medicine Approaches
Research increasingly supports personalized approaches to JAK inhibitor therapy based on individual patient characteristics and disease mechanisms. Studies in ulcerative colitis have revealed sex-dependent activation of JAK-STAT pathways, with male patients exhibiting significantly higher activation of JAK2 and STAT3 than female patients [13]. Correlation analyses show coordinated activation among JAK2, JAK3, TYK2, and STAT3 in inflamed tissues, suggesting interdependent roles that might be simultaneously targeted [13]. These findings highlight the potential for profiling JAK-STAT activation patterns in individual patients to guide selection of specific jakinibs for precision therapy.
The development of jakinibs has evolved substantially from first-generation pan-JAK inhibitors to increasingly selective agents that optimize efficacy and safety. Structural biology insights have been instrumental in this progression, enabling structure-based drug design and allosteric inhibition strategies. While approved jakinibs have demonstrated significant clinical benefits across inflammatory diseases, autoimmune conditions, and hematological malignancies, research continues to address challenges including opportunistic infections and other class-effect adverse events. Future directions include exploiting natural product diversity, developing enhanced selectivity through allosteric mechanisms, and implementing personalized treatment approaches based on individual patient pathway activation profiles. As our understanding of JAK-STAT biology and inhibitor selectivity advances, the next decade promises further refinement in targeting this critical signaling pathway for therapeutic benefit.
The Janus kinase-signal transducer and activator of transcription (JAK-STAT) pathway represents a fundamental signaling cascade that transmits information from extracellular cytokines directly to the nucleus, thereby regulating gene expression for critical cellular processes including proliferation, differentiation, and immune activation [1] [9]. As a fulcrum of inflammatory signaling, dysregulation of this pathway underpins numerous autoimmune, inflammatory, and neoplastic diseases, making it a compelling therapeutic target [1] [10]. The development of JAK inhibitors (jakinibs) constitutes a landmark advancement in targeted therapy, offering oral bioavailability and a novel mechanism of action distinct from biologic agents [44]. This whitepaper provides a comprehensive technical overview of approved JAK inhibitors, detailing their clinical applications, mechanistic profiles, and experimental methodologies essential for research and drug development professionals.
The JAK-STAT Signaling Pathway: Molecular Architecture
Pathway Components and Activation Mechanism
The JAK-STAT pathway is evolutionarily conserved and consists of three core components: cytokine receptors, Janus kinases (JAKs), and signal transducers and activators of transcription (STATs) [1] [10]. The four JAK family members—JAK1, JAK2, JAK3, and TYK2—are non-receptor tyrosine kinases characterized by seven JAK homology (JH) domains [1]. The C-terminal JH1 domain contains the functional kinase activity, while the adjacent JH2 (pseudokinase) domain regulates kinase activity [1] [10]. The N-terminal FERM domain facilitates binding to cytokine receptors [10]. The seven STAT family members (STAT1, STAT2, STAT3, STAT4, STAT5a, STAT5b, STAT6) contain several functional domains: an N-terminal domain that promotes dimerization, a coiled-coil domain for protein interactions, a DNA-binding domain, a linker domain, an SH2 domain that recognizes phosphotyrosine motifs, and a C-terminal transactivation domain [10].
Pathway activation initiates when extracellular cytokines bind to their cognate receptors, inducing receptor dimerization and consequent trans-phosphorylation of associated JAKs [44] [1]. The activated JAKs then phosphorylate tyrosine residues on the cytokine receptors, creating docking sites for STAT proteins via their SH2 domains [1]. Following recruitment to the receptor complex, JAKs phosphorylate STATs on conserved tyrosine residues, prompting STAT dimerization through reciprocal SH2-phosphotyrosine interactions [1] [9]. These STAT dimers translocate to the nucleus, where they bind specific promoter sequences and regulate transcription of target genes [1].
JAK-STAT Pathway Diagram
The following diagram illustrates the sequential activation of the JAK-STAT signaling pathway, from cytokine binding to gene transcription.
Cytokine Signaling Specificity and JAK Pairings
Different cytokine families activate specific combinations of JAKs, which determines downstream signaling consequences [44] [1]. JAK1 partners with JAK3 for γ-chain cytokine signaling (IL-2, IL-4, IL-7, IL-9, IL-15, IL-21) and with JAK2 or TYK2 for interferon and IL-6 family signaling [1]. JAK2 primarily forms homodimers activated by hematopoietic cytokines (erythropoietin, thrombopoietin, GM-CSF) [44]. JAK3 exclusively pairs with JAK1 following engagement of cytokines that use the common gamma chain (γc) receptor [1]. TYK2 participates in signaling for type I interferons, IL-12, and IL-23 [1]. This selective pairing enables precise therapeutic targeting of specific cytokine pathways implicated in different diseases.
Approved JAK Inhibitors: Clinical Indications and Selectivity Profiles
Systemic JAK Inhibitors
Since the first JAK inhibitor approval in 2011, numerous agents have received regulatory approval for various indications. The table below summarizes the key characteristics of currently approved systemic JAK inhibitors.
Table 1: FDA-Approved Systemic JAK Inhibitors and Their Clinical Applications
| Inhibitor | Molecular Targets | Approved Indications | Key Clinical Trial Data |
|---|---|---|---|
| Baricitinib (Olumiant) | JAK1/JAK2 [45] [46] | Rheumatoid Arthritis, Alopecia Areata [47] [45] | 32-35% of alopecia patients achieved ≥80% scalp hair regrowth at 4mg/36 weeks; 90% after 104 weeks [47] |
| Tofacitinib (Xeljanz) | JAK1/2/3 > TYK2 [46] | Rheumatoid Arthritis, Psoriatic Arthritis, Ulcerative Colitis [47] [48] | First JAK inhibitor demonstrating efficacy in alopecia areata (2014 case report) [47] |
| Upadacitinib (Rinvoq) | JAK1 [45] [46] | Atopic Dermatitis, Rheumatoid Arthritis, Psoriatic Arthritis, Axial Spondyloarthritis, Crohn's Disease, Ulcerative Colitis, Giant Cell Arteritis [48] | 46% of GCA patients achieved sustained remission at 15mg/day vs 29% with placebo [48] |
| Abrocitinib | JAK1 [45] | Atopic Dermatitis [45] | Superior efficacy versus placebo in improving AD symptoms [45] |
| Ritlecitinib (Litfulo) | JAK3/TEC [46] | Alopecia Areata (adults and adolescents ≥12) [47] [45] | First FDA-approved treatment for patients aged 12+ with severe alopecia areata [47] |
| Deuruxolitinib (Leqselvi) | JAK1/JAK2 [45] | Alopecia Areata [47] | ~33% of patients achieved ≥80% scalp hair regrowth at 8mg BID/24 weeks vs <1% placebo [47] |
| Deucravacitinib | TYK2 [45] [46] | Plaque Psoriasis [45] | Superior efficacy in psoriasis with unique allosteric inhibition mechanism [45] [46] |
Topical JAK Inhibitors
Topical formulations offer localized therapy with reduced systemic exposure, particularly beneficial for dermatologic conditions.
Table 2: Approved Topical JAK Inhibitors
| Inhibitor | Molecular Targets | Approved Indications | Key Characteristics |
|---|---|---|---|
| Ruxolitinib Cream | JAK1/JAK2 [45] [46] | Atopic Dermatitis, Vitiligo [45] | Minimal systemic absorption; favorable safety profile [45] |
| Delgocitinib Ointment | Pan-JAK [45] | Atopic Dermatitis, Chronic Hand Eczema (EU) [45] | Negligible systemic absorption; primarily application-site reactions [45] |
Mechanism of Action and Inhibitor Selectivity
JAK inhibitors function by competitively binding to the ATP-binding pocket in the JH1 kinase domain of JAK enzymes, preventing phosphorylation and subsequent activation of the signaling cascade [44]. However, they differ significantly in their selectivity profiles for the four JAK family members, which influences both their efficacy and safety patterns.
The selectivity spectrum ranges from non-selective agents (tofacitinib) that inhibit multiple JAK enzymes to highly selective inhibitors targeting specific family members (upadacitinib for JAK1; deucravacitinib for TYK2) [44] [46]. This selectivity is not absolute but rather preferential, as most inhibitors demonstrate some activity across JAK family members, particularly at higher concentrations [44]. The diagram below illustrates the distinct binding mechanisms of different JAK inhibitor classes.
TYK2 inhibitors like deucravacitinib employ a unique allosteric mechanism, binding to the regulatory JH2 pseudokinase domain rather than the catalytic JH1 domain, which may contribute to their distinct safety profile [46]. JAK3-selective inhibitors such as ritlecitinib achieve enhanced specificity through irreversible covalent binding to a cysteine residue (Cys-909) unique to JAK3 [46]. The clinical efficacy of JAK3 inhibition is particularly notable in alopecia areata, where targeting this kinase appears sufficient to reverse disease pathology [46].
Experimental Methodology for JAK Inhibitor Profiling
Standardized Assays for JAK Inhibitor Evaluation
Comprehensive profiling of JAK inhibitors requires multidisciplinary approaches spanning biochemical, cellular, and functional assays.
Table 3: Essential Experimental Protocols for JAK Inhibitor Characterization
| Method Category | Specific Assays | Key Output Parameters | Research Applications |
|---|---|---|---|
| Biochemical Profiling | • Kinase activity assays (FRET, radioactive)• ATP competition studies• Cellular thermal shift assays (CETSA) | • IC50 values• Selectivity ratios (JAK1:2:3:TYK2)• Binding affinity (Kd) | Quantifying inhibitor potency and selectivity across JAK family [44] |
| Cellular Signaling Analysis | • Phospho-STAT flow cytometry• Western blotting for pSTAT• JAK-STAT reporter gene assays | • STAT phosphorylation inhibition• Pathway-specific IC50• Temporal inhibition patterns | Assessing cellular pathway inhibition and functional selectivity [44] |
| Functional Immune Assays | • T cell proliferation assays• Cytokine production measurements (ELISA/MSD)• Mixed lymphocyte reactions | • Inhibition of immune cell activation• Cytokine suppression profiles• Immunomodulatory potency | Evaluating functional immunomodulatory effects [44] [49] |
| In Vivo Models | • Mouse models of inflammation (arthritis, dermatitis)• Xenograft models for oncology• Pharmacodynamic assessment | • Disease activity reduction• Target engagement markers• PK/PD relationships | Translational efficacy assessment and biomarker identification [50] |
Research Reagent Solutions for JAK-STAT Investigations
Table 4: Essential Research Tools for JAK-STAT Pathway Studies
| Reagent/Category | Specific Examples | Research Applications |
|---|---|---|
| Cell-Based Reporter Systems | • STAT-responsive luciferase constructs (STAT1, STAT3, STAT5, STAT6)• Engineered cell lines with JAK-STAT pathway components | High-throughput screening of JAK inhibitor compounds and pathway activity quantification [44] |
| Recombinant Proteins | • Purified JAK kinase domains (JH1)• Full-length STAT proteins• Cytokine extracellular domains | Biochemical assays, structural studies, and in vitro kinase activity measurements [44] |
| Phospho-Specific Antibodies | • Anti-pSTAT1 (Y701), pSTAT3 (Y705), pSTAT5 (Y694)• Anti-pJAK2 (Y1007/1008) | Flow cytometry, Western blotting, and immunohistochemistry for pathway activation assessment [44] |
| Validated Inhibitors | • Selective tool compounds (JAK1: filgotinib; JAK2: fedratinib; JAK3: tofacitinib)• Pan-JAK inhibitors (delgocitinib) | Experimental controls, pathway dissection, and mechanism-of-action studies [45] [46] |
JAK inhibitors represent a transformative class of targeted therapies that have expanded treatment options across numerous immune-mediated diseases. Their oral bioavailability and rapid onset of action offer distinct advantages over biologic agents, though their unique safety considerations necessitate appropriate patient selection and monitoring. The continued evolution of JAK inhibitor therapeutics includes developing enhanced selectivity profiles, innovative administration approaches like topical formulations, and combining JAK inhibition with other therapeutic modalities. As research elucidates more precise roles of specific JAK-STAT pathway components in disease pathogenesis, the next generation of inhibitors will likely demonstrate improved therapeutic indices and expanded clinical applications across autoimmune diseases, inflammatory disorders, and hematologic malignancies.
The Janus kinase/signal transducer and activator of transcription (JAK-STAT) pathway is a critical membrane-to-nucleus signaling module that regulates fundamental cellular processes, including hematopoiesis, immune fitness, and inflammation [1]. More than 50 cytokines and growth factors signal through this pathway [1]. While therapeutic targeting has historically focused on the kinase components (JAK1, JAK2, JAK3, TYK2), growing evidence indicates that direct STAT inhibition represents a promising new frontier, particularly for overcoming the limitations of current JAK inhibitors, such as waning response durability and compensatory pathway activation [51] [52].
The STAT family comprises seven members (STAT1, STAT2, STAT3, STAT4, STAT5a, STAT5b, and STAT6) that function as transcription factors upon phosphorylation and nuclear translocation [1]. Among these, STAT3 and STAT5 have emerged as particularly compelling therapeutic targets due to their established roles in promoting cell proliferation and preventing apoptosis in various malignancies and inflammatory conditions [53] [52]. This whitepaper provides a comprehensive technical overview of emerging strategies for direct STAT inhibition, detailing the pipeline compounds, experimental validation, and research methodologies driving this innovative field.
The STAT Inhibitor Pipeline: From Preclinical to Clinical Assets
The STAT inhibitor landscape has expanded significantly, with over 18 companies and 22 drugs in various stages of development [53]. These agents employ diverse mechanisms to target the traditionally challenging STAT proteins, ranging from small molecule degraders to direct domain inhibitors.
Table 1: Emerging STAT Inhibitors in Development
| Compound | Developer | Stage | Target | Key Indications |
|---|---|---|---|---|
| TTI-101 | Tvardi Therapeutics | Phase II | STAT3 Inhibitor | Breast Cancer, Idiopathic Pulmonary Fibrosis, Liver Cancer [53] |
| KT-621 | Kymera Therapeutics | Preclinical/Phase I | STAT6 Degrader | Atopic Dermatitis [53] |
| VVD-850 | Vividion Therapeutics | Phase I | STAT3 Inhibitor | Tumors [53] |
| JPX-1244 | Academic Research | Preclinical | STAT3/STAT5 Dual Degrader | T-PLL, other leukemias [52] |
| Undisclosed | Recludix | Discovery | STAT3/STAT5 | Inflammatory Conditions [53] |
A key insight driving current development is the therapeutic advantage of dual STAT3/STAT5 inhibition. In T-prolymphocytic leukemia (T-PLL), for instance, single STAT5 inhibition has shown limited efficacy due to compensatory STAT3 activation via a SOCS2-mediated feedback loop [52]. This redundancy has prompted the development of dual inhibitors, such as compounds from the JPX-series, which simultaneously target both STAT3 and STAT5 to prevent bypass mechanisms and enhance cytotoxic effects [52].
Experimental Validation: Assessing STAT Inhibition Efficacy
Establishing Pathogenic JAK/STAT Activation
Initial experiments must confirm constitutive JAK/STAT pathway activation as a disease driver. A meta-analysis of 335 T-PLL cases revealed that over 52% carried at least one mutation in a JAK or STAT gene, with JAK3 and STAT5B mutations being most common (16.3% each) [52]. The experimental workflow involves:
- Genomic Analysis: DNA or RNA sequencing to identify gain-of-function mutations, particularly in the pseudokinase domain of JAK1 (e.g., V658F) and JAK3 (e.g., M511I), or in STAT5B [52].
- Phosphoprotein Assessment: Western blot quantification of phosphorylation levels for key STAT proteins (e.g., STAT3, STAT5) in patient-derived samples compared to healthy controls. Inflamed tissues from ulcerative colitis patients, for example, showed significantly increased phosphorylation of JAK2, JAK3, TYK2, STAT1, STAT3, and STAT4 compared to non-inflamed mucosa [26].
- Transcriptomic Profiling: RNA-sequencing to identify upregulated STAT target genes, confirming functional pathway activity [52].
Compound Screening and Validation
Following target validation, a standard protocol for evaluating STAT inhibitors involves a multi-tiered approach:
- Primary Viability Screening: Treat primary patient samples or representative cell lines with compound dilutions. Assess cell viability using luminescent assays (e.g., CellTiter-Glo) after 48-72 hours to determine ICâ‚…â‚€ values [52].
- Mechanistic Confirmation:
- Immunoblotting: Confirmation of reduced STAT phosphorylation (pSTAT3, pSTAT5) and total protein levels following treatment with degraders [52].
- Flow Cytometry: Quantification of cell death via Annexin V/7AAD staining to determine LDâ‚…â‚€ [52].
- RNA-seq: Transcriptional analysis to validate downregulation of STAT-dependent target genes (e.g., downstream effectors of STAT5) after 8-24 hours of treatment [52].
- Combination Screening: Test STAT inhibitors with standard-of-care agents (e.g., cladribine, venetoclax, azacytidine) to identify synergistic interactions using Bliss independence or similar models [52].
Diagram 1: STAT Inhibition Mechanism. STAT inhibitors directly bind transcription factors, blocking cancer-promoting gene expression.
The Scientist's Toolkit: Essential Research Reagents
Research into STAT inhibition requires a specialized set of reagents and tools for rigorous experimental validation.
Table 2: Essential Research Reagents for STAT Inhibition Studies
| Reagent / Tool | Function / Application | Example Use Case |
|---|---|---|
| Phospho-Specific STAT Antibodies | Detect activated (phosphorylated) STAT proteins via Western blot, flow cytometry, or IHC. | Quantifying pSTAT3 (Tyr705) and pSTAT5 (Tyr694) levels pre- and post-inhibitor treatment [52]. |
| Primary Patient-Derived Cells | Ex-vivo testing of compound efficacy in biologically relevant models. | Maintaining T-PLL cells from patient blood samples for drug sensitivity assays [52]. |
| Cell Viability Assays | Measure metabolic activity or ATP levels as a proxy for cell viability. | Using CellTiter-Glo to determine ICâ‚…â‚€ values for JPX-series compounds [52]. |
| Apoptosis Detection Kits | Quantify early and late-stage apoptotic cells. | Using Annexin V-APC/7AAD staining and flow cytometry to determine LDâ‚…â‚€ [52]. |
| RNA-sequencing Reagents | Profile global transcriptional changes following STAT inhibition. | Validating downregulation of direct STAT target genes (e.g., BCL-xL, PIM1) after JPX-1244 treatment [52]. |
| JAK/STAT Mutant Constructs | Model gain-of-function mutations found in patients. | Expressing JAK3 M511I or STAT5B mutants in cell lines to study inhibitor resistance [52]. |
| Mancozeb | Mancozeb, CAS:8018-01-7, MF:C4H6N2S4Mn . C4H6N2S4Zn, MW:541.1 g/mol | Chemical Reagent |
The strategic shift from JAK to direct STAT inhibition represents a significant evolution in targeting the JAK-STAT pathway. The growing pipeline of selective and dual STAT inhibitors, combined with sophisticated diagnostic methods to identify patients with hyperactive STAT signaling, promises a new generation of more effective and potentially safer therapeutics. Future success will depend on comprehensively understanding STAT biology, including the functional redundancies and compensatory mechanisms between different STAT family members. Furthermore, the clinical translation of these agents will require robust biomarker strategies to select patients most likely to benefit, such as those with STAT mutations or evidence of constitutive pathway activation. As these innovative compounds progress through clinical development, they hold substantial potential to improve outcomes for patients with STAT-driven cancers and inflammatory disorders.
The Janus kinase-signal transducer and activator of transcription (JAK-STAT) pathway, once primarily targeted in rheumatology, has emerged as a critical therapeutic pathway across multiple medical specialties. This whitepaper examines the expanding applications of JAK-STAT pathway inhibitors into dermatology and neurology, underpinned by mechanistic insights into inflammatory signaling. We explore the molecular basis for this therapeutic expansion, summarize clinical and preclinical evidence across indications, and provide detailed experimental methodologies for investigating pathway activation. The diversification of JAK-STAT therapeutics represents a paradigm shift in managing complex inflammatory diseases through targeted intracellular signaling modulation, offering new avenues for drug development across disciplinary boundaries.
The JAK-STAT signaling pathway serves as a fundamental intracellular communication network that transduces signals from over 60 cytokines, interferons, interleukins, and growth factors from the cell surface to the nucleus [10] [9]. This pathway regulates essential cellular processes including proliferation, differentiation, apoptosis, and immune responses [10]. The pathway consists of three main components: tyrosine kinase-associated receptors, Janus kinases (JAKs), and signal transducer and activator of transcription (STAT) proteins [10]. Four JAK family members (JAK1, JAK2, JAK3, and TYK2) and seven STAT proteins (STAT1, 2, 3, 4, 5A, 5B, and 6) comprise the core signaling machinery [54].
Upon cytokine binding, receptor-associated JAKs undergo transphosphorylation, subsequently phosphorylating STAT proteins [55]. Phosphorylated STATs then dimerize and translocate to the nucleus, where they regulate transcription of target genes involved in immune homeostasis and inflammation [55]. Dysregulation of this carefully orchestrated pathway contributes significantly to the pathogenesis of various inflammatory, autoimmune, and neoplastic conditions [10] [9]. The central role of JAK-STAT signaling in immune modulation established it as a compelling therapeutic target, first successfully exploited in rheumatology with the approval of tofacitinib for rheumatoid arthritis in 2012.
Structural and Molecular Basis of JAK-STAT Signaling
Molecular Architecture of Pathway Components
JAK proteins are non-receptor tyrosine kinases ranging from 120-140 kDa, each containing seven conserved JAK homology (JH) domains [10]. The C-terminal JH1 domain represents the catalytically active kinase domain, while the adjacent JH2 domain functions as a pseudokinase that regulates JH1 activity [10]. The JH3-JH4 segments form an SH2-like domain, and the N-terminal JH4-JH7 domains constitute a FERM domain that mediates receptor interaction [10]. STAT proteins (79-113 kDa) contain multiple functional domains including an N-terminal domain that facilitates protein-protein interactions, a coiled-coil domain involved in regulatory protein interactions, a central DNA-binding domain, a linker domain, an SH2 domain that mediates STAT dimerization, and a C-terminal transactivation domain [10].
Signaling Cascade Mechanism
The canonical JAK-STAT activation cascade initiates when extracellular cytokines bind to their cognate transmembrane receptors, inducing receptor dimerization or oligomerization [9]. This conformational change brings associated JAK proteins into proximity, enabling their transphosphorylation and activation [9]. Activated JAKs then phosphorylate specific tyrosine residues on cytokine receptors, creating docking sites for STAT proteins via their SH2 domains [10]. Once recruited, STATs are phosphorylated by JAKs on conserved tyrosine residues, prompting STAT dimerization either as homodimers or heterodimers [10]. These activated STAT dimers translocate to the nucleus, bind specific promoter sequences, and regulate transcription of target genes [10].
Figure 1: Canonical JAK-STAT Signaling Cascade. This diagram illustrates the core JAK-STAT pathway activation mechanism, from cytokine binding through STAT phosphorylation, dimerization, nuclear translocation, and gene transcription regulation.
Expansion into Dermatology: From Pathogenesis to Targeted Therapy
Dermatological Conditions with JAK-STAT Involvement
The JAK-STAT pathway has been implicated in the pathogenesis of numerous inflammatory dermatoses, creating opportunities for targeted therapeutic intervention. Key conditions with established JAK-STAT involvement include:
Psoriasis and Psoriatic Arthritis: STAT3 activation drives keratinocyte hyperproliferation and promotes Th17 differentiation, while TYK2 and JAK2 mediate IL-12/IL-23 signaling critical for Th1 and Th17 responses [55]. Keratinocyte-specific STAT3 overexpression alone can induce psoriasis-like lesions in murine models [55].
Atopic Dermatitis: Multiple cytokines involved in AD pathogenesis (IL-4, IL-13, IL-31) signal through JAK-STAT pathways, making JAK inhibition an effective strategy for moderate-to-severe cases [56] [54].
Alopecia Areata: JAK-STAT signaling disruption has shown remarkable efficacy in hair regrowth, with JAK3 inhibitors particularly demonstrating significant clinical benefit [56].
Vitiligo: IFN-γ signaling through JAK-STAT pathways drives CD8+ T-cell mediated melanocyte destruction, providing a rationale for JAK inhibition in repigmentation strategies [56] [54].
Chronic Hand Eczema: Delgocitinib recently became the first FDA-approved topical JAK inhibitor for moderate-to-severe CHE, demonstrating substantial improvements in skin clearance and symptom relief [57].
Approved JAK Inhibitors in Dermatology
Table 1: Selected JAK Inhibitors with Dermatological Applications
| Drug Name | JAK Selectivity Profile | Approved Dermatologic Indications | Administration Route | Key Clinical Trials |
|---|---|---|---|---|
| Delgocitinib | Pan-JAK inhibitor | Moderate-to-severe chronic hand eczema | Topical cream | Phase 3 trials showed significant improvement in Hand Eczema Severity Index [57] |
| Ruxolitinib | JAK1/JAK2 inhibitor | Atopic dermatitis (topical) | Topical cream | TRuE-AD program demonstrated efficacy in mild-to-moderate atopic dermatitis [54] |
| Upadacitinib | JAK1 selective | Atopic dermatitis | Oral | Measure Up 1 & 2, AD Up showed significant EASI-75 response vs placebo [54] |
| Tofacitinib | JAK1/JAK3 inhibitor | Psoriatic arthritis (off-label dermatologic use) | Oral | OPAL Broaden, OPAL Beyond demonstrated efficacy in psoriatic arthritis [55] |
| Baricitinib | JAK1/JAK2 inhibitor | Atopic dermatitis | Oral | BREEZE-AD program showed significant improvement in EASI scores [54] |
Molecular Mechanisms in Dermatologic Disease
In psoriasis, the IL-23/IL-17 axis activates JAK-STAT signaling through multiple mechanisms. IL-23 stimulates TYK2 and JAK2, promoting Th17 differentiation and IL-22 production, which subsequently activates STAT3 in keratinocytes [55]. STAT3 then induces keratinocyte proliferation and impaired differentiation, forming psoriatic plaques [55]. Additionally, IL-17A promotes inflammatory gene expression, while IL-22 induces keratinocyte proliferation through matrix metalloproteinase upregulation and anti-apoptotic protein induction [55]. IL-9 stimulates keratinocyte proliferation and enhances production of hyperproliferative keratinocyte cytokines and VEGF [55]. These interconnected pathways create a self-amplifying inflammatory loop that can be disrupted at multiple points by JAK inhibitors.
Neurological Applications: Targeting Neuroinflammation and Pain
Endometriosis-Associated Pain Mechanisms
Chronic pain in endometriosis exemplifies the intersection of inflammation and neurology mediated by JAK-STAT signaling. Endometriotic lesions generate a pro-inflammatory microenvironment rich in cytokines (IL-1β, IL-6, TNF-α), neurotrophic factors (NGF, BDNF), and other mediators that promote neurogenesis and peripheral nerve sensitization [50] [33]. These factors activate JAK-STAT signaling in both immune cells and neurons, driving pain sensitization through multiple mechanisms:
Peripheral Sensitization: Inflammatory mediators activate JAK-STAT pathways in dorsal root ganglion (DRG) neurons, increasing expression of pain-related ion channels (TRPV1, TRPA1) and promoting excessive axonal sprouting and hyperinnervation of endometriotic lesions [33].
Central Sensitization: Endometriosis-induced neuroinflammation triggers maladaptive neural plasticity, including remodeling of synaptic connections and disrupted neurogenic processes in pain-processing brain regions [33]. Patients exhibit altered brain chemistry with elevated glutamate/glutamine concentrations in the anterior insula and increased connectivity between pain-processing regions [33].
Mast Cell Activation: Mast cells colocalize with nerve fibers in endometriotic lesions and release additional inflammatory mediators that amplify JAK-STAT signaling, creating a neuroimmune feedback loop that sustains pain [50] [33].
Preclinical Evidence for JAK Inhibition in Neurological Conditions
Emerging research supports JAK-STAT pathway involvement in other neurological conditions:
Neuropathic Pain Models: Preclinical studies demonstrate that JAK inhibitors attenuate pain hypersensitivity in rodent models of endometriosis, potentially through disruption of the IL-6/JAK/STAT3 axis that mediates cross-talk between immune cells and sensory neurons [50].
Central Nervous System Changes: Murine endometriosis models show differential gene expression in pain-processing brain regions (insula, amygdala, hippocampus, cerebral cortex) and increased microglial activation, suggesting central nervous system involvement in chronic pain maintenance [33].
Figure 2: Neuroimmune Interactions in Endometriosis Pain. This diagram illustrates how endometriotic lesions initiate JAK-STAT-mediated neuroinflammation, engaging mast cells (MC) and neurons in a feedforward cycle that maintains chronic pain states.
Experimental Approaches for JAK-STAT Pathway Investigation
Phosphoprotein Analysis in Human Tissue
A recent study investigating JAK-STAT activation in ulcerative colitis provides a robust methodological framework applicable to dermatologic and neurologic research [13]:
Protocol: Western Blot Analysis of JAK-STAT Phosphorylation
Sample Collection and Preparation: Collect tissue biopsies from both affected and unaffected regions. Process samples through mechanical digestion and sonication in lysis buffer (50 mM Tris, 150 mM NaCl, 5 mM EDTA) supplemented with protease and phosphatase inhibitors. Centrifuge at 10,000 × g for 10 minutes and determine protein concentration using DC assay.
Gel Electrophoresis and Transfer: Mix 20 μg total protein with LDS sample buffer, heat to 95°C for 5 minutes, and separate on 4-12% Bis-Tris Plus gels at 120V for 85 minutes. Transfer to PVDF membranes at 15V for 90 minutes.
Membrane Processing: Treat membranes with Western Blot Enhancer, block with 5% BSA, and incubate with primary antibodies overnight at 4°C. Use phospho-specific antibodies for JAK1, JAK2, JAK3, TYK2, STAT1, STAT3, and STAT4 with appropriate validation.
Detection and Analysis: Incubate with HRP-conjugated secondary antibodies, develop with ECL substrate, and visualize using imaging systems. Use β-actin as loading control. Perform sequential stripping and reprobing for multiple targets. Quantify bands using ImageJ software, calculating integrated density normalized to non-inflamed controls.
Table 2: Key Research Reagents for JAK-STAT Pathway Investigation
| Reagent Category | Specific Examples | Research Application | Technical Considerations |
|---|---|---|---|
| Phospho-Specific Antibodies | p-JAK1 (Y1034/1035), p-JAK2 (Y1007/1008), p-STAT3 (Y705) | Western blot, immunohistochemistry, flow cytometry | Validate using recommended cell lysates; confirm specificity with molecular weight verification [13] |
| JAK Inhibitors | Tofacitinib (pan-JAK), Ruxolitinib (JAK1/2), Upadacitinib (JAK1 selective) | Functional studies, mechanism of action | Consider selectivity profiles; use concentration ranges based on IC50 values (nM-μM) [54] |
| Cell-Based Assay Systems | Reporter gene assays (STAT-responsive elements), Phospho-STAT flow cytometry | High-throughput screening, signaling dynamics | Optimize cytokine stimulation timing (minutes-hours); include pathway-specific controls [10] |
| Animal Models | Keratinocyte-specific STAT3 overexpression (psoriasis), Endometriosis rodent models | Pathophysiology studies, drug efficacy testing | Monitor species-specific JAK-STAT pathway differences; validate disease-relevant readouts [33] [55] |
Natural products represent promising sources for novel JAK inhibitors with potentially improved safety profiles. Current research has identified numerous compounds with JAK inhibitory activity:
Flavonoids: Myricetin demonstrates high-affinity binding to JAK1 and STAT3, inhibiting EGF-induced malignant transformation [32]. Galangin selectively inhibits JAK1 phosphorylation in LPS-stimulated macrophages [32].
Terpenes: Cycloastragenol inhibits constitutive STAT3 activation through JAK1 and Src kinase suppression, showing synergistic cytotoxicity with paclitaxel in gastric cancer models [32].
Chalcones: Isobavachalcone demonstrates dual modulation of PI3K-AKT and JAK1-STAT3 pathways, providing therapeutic effects in rheumatoid arthritis models [32].
These natural compounds offer structural diversity for developing next-generation JAK inhibitors with enhanced therapeutic profiles and reduced adverse effects compared to current synthetic inhibitors.
The expansion of JAK-STAT therapeutics from rheumatology to dermatology and neurology exemplifies how understanding fundamental signaling pathways can drive therapeutic innovation across disciplinary boundaries. The mechanistic role of JAK-STAT signaling in neuroinflammation and chronic pain establishes a strong rationale for investigating JAK inhibitors in neurological conditions, particularly those with significant inflammatory components. Future research directions should include:
- Development of tissue-specific JAK inhibitors to maximize efficacy while minimizing systemic adverse effects
- Exploration of combination therapies targeting JAK-STAT alongside complementary pathways
- Investigation of sex-specific differences in JAK-STAT pathway activation to inform personalized treatment approaches
- Natural product discovery for novel JAK inhibitors with improved safety profiles
As our understanding of JAK-STAT biology continues to evolve, so too will therapeutic opportunities across the dermatology and neurology spectrum, ultimately advancing care for patients with inflammatory conditions mediated by this fundamental signaling pathway.
Overcoming Hurdles: Selectivity, Safety, and Resistance in JAK Inhibition
The Janus kinase-signal transducer and activator of transcription (JAK-STAT) pathway represents a fundamental signaling cascade that transmits information from extracellular cytokines directly to the nucleus, regulating gene expression for critical processes including immune response, cell proliferation, and differentiation [9] [10]. This pathway's central role in inflammatory signaling has made it an attractive therapeutic target for a spectrum of immune-mediated inflammatory diseases (IMIDs) and cancers. However, the structural conservation across JAK family members (JAK1, JAK2, JAK3, and TYK2) presents a significant pharmacological challenge: achieving sufficient potency against pathogenic signaling while minimizing off-target effects on physiologically important pathways [58].
The "selectivity challenge" embodies the delicate balance between therapeutic efficacy and mechanism-based toxicity. First-generation JAK inhibitors, designed as ATP-competitive compounds that target the conserved kinase domain, often exhibit limited selectivity, leading to broad immunosuppression and undesirable side effects [59] [55]. This review examines the current landscape of strategies aimed at overcoming the selectivity challenge, focusing on structural insights, innovative therapeutic modalities, and advanced experimental approaches for evaluating next-generation JAK-targeted therapies within inflammatory signaling research.
Structural Basis of JAK-STAT Signaling and Inhibition
Pathway Architecture and Activation Mechanism
The JAK-STAT pathway operates through a precisely orchestrated sequence of molecular events. In its basal state, JAK kinases are non-covalently associated with cytokine receptors via their FERM domains [10]. Upon cytokine binding-induced receptor dimerization, JAKs undergo trans-phosphorylation, creating docking sites for STAT proteins via their SH2 domains. Subsequently, JAKs phosphorylate STATs, prompting their dimerization and nuclear translocation to regulate target gene expression [9] [10].
The following diagram illustrates this fundamental signaling cascade:
Structural Conservation and Selectivity Challenges
The high degree of structural homology within the JAK kinase domain, particularly the ATP-binding pocket targeted by conventional inhibitors, constitutes the fundamental basis of the selectivity challenge. Although JAKs share this conserved catalytic region, their non-catalytic domains—including the pseudokinase domain (JH2) that regulates kinase activity—exhibit greater diversity, offering potential avenues for developing more selective inhibitors [58] [10].
The therapeutic consequences of limited selectivity are significant. For example, simultaneous inhibition of JAK1, JAK2, and JAK3 can lead to pan-JAK suppression, resulting in increased infection risk, anemia, thrombocytopenia, and other dose-limiting toxicities [59]. Therefore, understanding the structural nuances that differentiate JAK family members is paramount for rational drug design aimed at improving selectivity profiles.
Emerging Strategies for Enhanced Selectivity
Isoform-Selective ATP-Competitive Inhibitors
Advances in structural biology have enabled the design of inhibitors that exploit subtle differences in the ATP-binding pockets of JAK isoforms. TYK2-specific inhibitors represent a promising approach in this category. By utilizing a unique regulatory mechanism rather than direct kinase domain targeting, these inhibitors achieve functional selectivity, preserving JAK1- and JAK2-dependent signaling while effectively blocking IL-12, IL-23, and type I interferon pathways relevant to autoimmune diseases [58]. This strategy demonstrates that high selectivity can potentially mitigate the risk of adverse effects associated with broader JAK inhibition, such as infections and hematological abnormalities [59].
Allosteric and Pseudokinase-Targeted Inhibition
Targeting the pseudokinase domain (JH2) represents a structurally distinct approach to achieving selectivity. Unlike the highly conserved kinase domain, the JH2 domain exhibits greater sequence variation among JAK family members, providing a promising target for allosteric inhibitors. These compounds modulate JAK activity indirectly by stabilizing the autoinhibitory conformation of the protein, potentially offering improved specificity and reduced off-target effects [58].
Dual-Target Inhibitors and PROTAC-Based Degraders
Strategic dual-target inhibition represents an alternative approach to the selectivity challenge. Lestaurtinib exemplifies this strategy by concurrently targeting JAK2 and serine/threonine kinases (JNK, ERK), resulting in more complete suppression of STAT phosphorylation at both tyrosine (Y701/705) and serine (S727) residues [60]. This comprehensive pathway suppression demonstrates superior antineoplastic activity compared to selective JAK inhibitors like ruxolitinib in ovarian cancer models, particularly in therapy-resistant settings [60].
Proteolysis-Targeting Chimeras (PROTACs) offer a completely different mechanism by inducing targeted protein degradation rather than enzymatic inhibition. TYK2 degraders can achieve prolonged pathway suppression and potentially overcome resistance mechanisms associated with traditional occupancy-driven inhibitors, representing a promising frontier in JAK-STAT therapeutics [58].
Table 1: Selectivity Profiles and Therapeutic Implications of JAK-Targeting Modalities
| Therapeutic Modality | Mechanism of Action | Selectivity Advantages | Therapeutic Context | Key Limitations |
|---|---|---|---|---|
| First-Generation JAKi (e.g., Ruxolitinib) | ATP-competitive inhibition of JAK1/JAK2 | Broad immunosuppression | Myeloproliferative neoplasms, rheumatoid arthritis | Increased risk of infections, hematological toxicity [59] |
| TYK2-Selective Inhibitors | Functional selectivity via regulatory domain | Preserves JAK1/JAK2-dependent cytokine signaling | Plaque psoriasis, psoriatic arthritis [55] | Potential for pathway-specific escape mechanisms [58] |
| Dual-Target Inhibitors (e.g., Lestaurtinib) | Concurrent inhibition of JAK2 & JNK/ERK | More complete STAT suppression (Y705 + S727) | Therapy-resistant ovarian cancer [60] | Complex safety profile requiring careful evaluation |
| PROTAC Degraders | Targeted protein degradation | Catalytic, event-driven activity | Preclinical development for autoimmune indications [58] | Optimizing pharmacokinetics and tissue specificity |
Quantitative Assessment of Selectivity and Safety Profiles
Recent large-scale meta-analyses provide crucial quantitative data on the comparative safety profiles of JAK inhibitors versus other biologic therapies. The following table summarizes incidence rates of key adverse events from a comprehensive analysis of head-to-head comparative effectiveness studies including over 813,000 patients with immune-mediated inflammatory diseases [59]:
Table 2: Comparative Safety Profiles: JAK Inhibitors vs. TNF Antagonists in Immune-Mediated Inflammatory Diseases
| Safety Outcome | JAK Inhibitors Incidence Rate (per 100 person-years) | TNF Antagonists Incidence Rate (per 100 person-years) | Pooled Hazard Ratio (95% CI) | Heterogeneity (I²) |
|---|---|---|---|---|
| Serious Infections | 3.79 (2.85-5.05) | 3.03 (2.32-3.95) | 1.05 (0.97-1.13) | Minimal to moderate |
| Malignant Neoplasms | 1.00 (0.77-1.31) | 0.94 (0.72-1.22) | 1.02 (0.90-1.16) | Minimal to moderate |
| Major Adverse Cardiovascular Events (MACE) | 0.72 (0.56-0.92) | 0.66 (0.49-0.89) | 0.91 (0.80-1.04) | Minimal to moderate |
| Venous Thromboembolism (VTE) | 0.57 (0.40-0.82) | 0.52 (0.37-0.73) | 1.26 (1.03-1.54) | Minimal to moderate |
This analysis reveals that while most serious adverse event risks are comparable between JAK inhibitors and TNF antagonists, there remains a slightly elevated risk of venous thromboembolism with JAK inhibitor use (HR 1.26, 95% CI 1.03-1.54) [59]. These findings underscore the importance of patient selection and risk stratification when prescribing JAK-targeted therapies, particularly for individuals with pre-existing cardiovascular risk factors.
Experimental Framework for Evaluating Selectivity and Efficacy
Comprehensive Selectivity Profiling Workflow
Rigorous preclinical assessment is essential for characterizing the selectivity of novel JAK inhibitors. The following experimental workflow outlines a comprehensive approach to selectivity and efficacy evaluation:
Detailed Experimental Protocols
In Vitro Kinase Selectivity Profiling
Purpose: Quantitatively assess inhibitor specificity across kinome [60]. Methodology:
- Utilize competitive binding assays against recombinant JAK kinases (JAK1, JAK2, JAK3, TYK2)
- Extend profiling to 100+ non-JAK kinases to identify off-target interactions
- Determine ICâ‚…â‚€ values for each kinase using ATP-concentration at Km
- Calculate selectivity scores (S(10) and S(35)) based on the number of kinases inhibited at 10x and 35x ICâ‚…â‚€ for primary target
Key Reagents:
- Recombinant human JAK proteins (catalytic domains)
- ATP, ADP-Glo Kinase Assay System
- Test compounds dissolved in DMSO (<1% final concentration)
Cellular Phospho-STAT Analysis
Purpose: Evaluate pathway inhibition in physiologically relevant cellular contexts [60] [61]. Methodology:
- Stimulate cytokine-responsive cells (e.g., THP-1, peripheral blood mononuclear cells) with appropriate cytokines (IFN-γ, IL-6, IL-4)
- Pre-treat with inhibitor compounds (15-60 minutes) before cytokine stimulation
- Fix cells, permeabilize, and stain with phospho-specific antibodies (pSTAT1, pSTAT3, pSTAT5, pSTAT6)
- Analyze by flow cytometry or capillary electrophoresis
- Determine cellular ICâ‚…â‚€ values and compare to biochemical potency
Key Reagents:
- Phospho-STAT antibodies (Y701-STAT1, Y705-STAT3, Y694-STAT5, Y641-STAT6)
- Cell stimulation cocktails (e.g., IFN-γ 50 ng/mL, IL-6 100 ng/mL)
- Cell fixation/permeabilization buffers
Transcriptomic Analysis of Pathway Modulation
Purpose: Comprehensively assess downstream consequences of JAK inhibition [60] [61]. Methodology:
- Treat disease-relevant cell lines (e.g., ovarian cancer models, immune cells) with selective vs. non-selective inhibitors
- Extract RNA after 6-24 hours of treatment
- Perform bulk RNA-sequencing (Illumina platform, 30-50 million reads/sample)
- Conduct differential gene expression analysis (DESeq2, edgeR)
- Perform pathway enrichment analysis (GSEA, IPA) on JAK-STAT hallmark gene sets
Key Reagents:
- RNA extraction kits (e.g., RNeasy)
- RNA sequencing library preparation kits
- Bioinformatics software packages for pathway analysis
In Vivo Efficacy and Safety Assessment
Purpose: Evaluate therapeutic efficacy and mechanism-based toxicities in physiological systems [60] [61]. Methodology:
- Utilize patient-derived xenograft (PDX) models of relevant diseases (e.g., ovarian cancer, autoimmune models)
- Administer test compounds at clinically relevant exposures (based on prior PK studies)
- Monitor tumor growth inhibition or disease severity metrics
- Assess mechanism-based toxicities: complete blood counts (JAK2-related anemia/thrombocytopenia), immune cell profiling (JAK1/3-related immunosuppression)
- Analyze tissue samples for phospho-STAT suppression and target engagement
Key Reagents:
- Immunodeficient mice (NSG, NOG) for PDX models
- Clinical chemistry and hematology analyzers
- Multiplex cytokine/phosphoprotein assays
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for JAK-STAT Selectivity and Efficacy Studies
| Reagent Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| Recombinant Kinases | JAK1, JAK2, JAK3, TYK2 catalytic domains | In vitro kinase assays | Source purity (>90%), maintenance of native conformation |
| Phospho-Specific Antibodies | pSTAT1 (Y701), pSTAT3 (Y705), pSTAT5 (Y694), pSTAT6 (Y641) | Cellular signaling assessment by flow cytometry/Western blot | Specificity validation, application-appropriate conjugate |
| Cytokine Stimulation Reagents | IFN-γ, IL-6, IL-4, IL-2, IL-12, IL-23 | Pathway activation in cellular models | Cell type-specific response optimization |
| Cell Line Models | JAK2V617F-mutated SET2 cells, STAT1-knockout cells | Genetic context-dependent inhibitor evaluation | Authentication, mycoplasma testing |
| Animal Models | Patient-derived xenografts (PDXs), CIA (collagen-induced arthritis) | In vivo efficacy and safety profiling | Model translatability to human disease |
The pursuit of selective JAK-STAT pathway modulation continues to evolve beyond conventional ATP-competitive inhibition. Emerging strategies including allosteric inhibitors, bifunctional degraders, and context-dependent therapeutics represent promising approaches to overcome the selectivity challenge. The integration of structural biology insights with functional cellular profiling enables rational design of next-generation inhibitors with improved therapeutic indices.
As these novel modalities progress through preclinical development, rigorous assessment using the comprehensive experimental framework outlined herein will be essential to validate their selectivity claims. The ultimate goal remains the development of JAK-targeted therapies that achieve precise pathological signaling inhibition while preserving physiological immune function and hematopoietic homeostasis—a critical balance for maximizing therapeutic benefit across diverse inflammatory and oncological indications.
The Janus kinase-signal transducer and activator of transcription (JAK-STAT) pathway serves as a fundamental signaling cascade, transmitting information from extracellular cytokines directly to the nucleus to regulate gene transcription. This pathway plays a pivotal role in numerous physiological processes, including hematopoiesis, immune cell development, and immune homeostasis [9]. However, dysregulation of JAK-STAT signaling is a key contributor to the pathogenesis of inflammatory and autoimmune diseases, as well as hematologic malignancies. Consequently, therapeutic inhibition of the JAK-STAT pathway has emerged as a powerful strategy for managing a range of immune-related conditions. The clinical use of JAK inhibitors, while beneficial, requires meticulous management of associated adverse events, particularly an increased risk of infections and alterations in hematologic profiles. This in-depth technical guide examines the underlying mechanisms, profiles the specific risks, and outlines essential monitoring and research methodologies for these critical adverse events within the context of inflammatory signaling research.
JAK-STAT Pathway Fundamentals and Pharmacologic Inhibition
Pathway Architecture and Mechanism
The JAK-STAT pathway is characterized by its relatively simple architecture, consisting of three core components: cytokine receptors, Janus kinases (JAKs), and signal transducers and activators of transcription (STATs). The signaling cascade initiates when a cytokine binds to its corresponding transmembrane receptor, inducing receptor dimerization or multimerization. This conformational change brings associated JAKs into close proximity, leading to their trans-activation via phosphorylation. The activated JAKs then phosphorylate tyrosine residues on the receptor cytoplasmic tails, creating docking sites for STAT proteins. Upon recruitment, STATs are themselves phosphorylated by JAKs, prompting their dimerization, nuclear translocation, and binding to specific promoter sequences to regulate target gene expression [9]. The family of JAKs includes JAK1, JAK2, JAK3, and TYK2, each with distinct but overlapping roles in cytokine signaling.
JAK Inhibitors as Therapeutic Agents
JAK inhibitors (JAKi) are small molecules that target the ATP-binding site of JAKs, preventing the phosphorylation and activation of downstream STATs. Approved JAKi exhibit varying selectivities for different JAK family members:
- Tofacitinib: Primarily inhibits JAK1 and JAK3.
- Baricitinib and Ruxolitinib: Selectively target JAK1 and JAK2 [62]. Ruxolitinib was first approved for myelofibrosis and polycythemia vera, while tofacitinib and baricitinib are used for inflammatory conditions like rheumatoid arthritis. Their mechanism of action provides a powerful means to dampen dysregulated immune responses, but it also inherently disrupts protective immune and hematopoietic functions, leading to characteristic adverse events.
Visualizing the JAK-STAT Signaling Cascade and Inhibitor Action
The following diagram illustrates the core JAK-STAT signaling pathway and the site of action for JAK inhibitors.
Figure 1: JAK-STAT Pathway and Inhibitor Mechanism.
Quantitative Profiling of Infection Risks with JAK Inhibitors
Evidence from Large-Scale Pharmacovigilance
A comprehensive analysis of the World Health Organization's pharmacovigilance database (VigiBase), encompassing 126,815 Individual Case Safety Reports (ICSRs), quantified the association between JAK inhibitors and infectious adverse events. The study found a significant disproportionate reporting of infections and infestations for ruxolitinib, tofacitinib, and baricitinib combined (Information Component, IC₀₂₅ = 1.7) [62]. This indicates a substantially higher reporting rate of infections with these drugs compared to all other drugs in the database.
Table 1: Spectrum of Infectious Adverse Events Associated with JAK Inhibitors [62]
| Infection Category | Specific Infection Type | Reporting Signal (IC₀₂₅)* | Notes on JAKi-Specific Risk |
|---|---|---|---|
| Viral Infections | Herpes viral infections | 2.9 | Highest for baricitinib, then tofacitinib |
| Influenza viral infections | 2.4 | Highest for tofacitinib, then baricitinib | |
| Fungal Infections | Pneumocystis infections | 1.9 | Over-reporting for baricitinib |
| Cryptococcal & Coccidioides infections | 1.9 | Significant for all three JAKi | |
| Mycobacterial Infections | Tuberculous infections | 1.9 | Over-reported for ruxolitinib vs. tofacitinib |
| Atypical mycobacterial infections | 1.7 | Significant signal observed | |
| Bacterial/Other Infections | Upper respiratory tract infections | 1.9 | Highest for baricitinib |
| Urinary tract infections | 1.9 | Highest for baricitinib | |
| Lower respiratory tract & lung infections | 1.9 | Highest for baricitinib |
*IC₀₂₅: Lower end of the 95% credibility interval of the Information Component. A positive value indicates a significant signal.
Risk in Vulnerable Populations: Hematologic Malignancies
Patients with hematologic malignancies possess multiple risk factors for severe infections, including baseline immunodeficiencies from their disease and myelosuppressive therapies. A large population-based study using the SEER database found that these patients had a 3.34-fold higher risk of death from infectious diseases compared to the general US population [63]. The risk was most pronounced within the first two months after diagnosis. Factors independently associated with infectious disease mortality included older age, acute graft-versus-host disease (aGvHD) ≥ grade 2, and the use of corticosteroids or T-cell depleting agents [63]. A separate systematic review and meta-analysis further identified previous allogeneic hematopoietic stem cell transplant (HSCT), especially with a haploidentical donor, as a key risk factor for invasive fungal infections (IFI) in this population [64]. These findings underscore the critical need for vigilant monitoring and prophylaxis in hematology patients, particularly those initiating JAKi therapy.
Hematologic Profiles and Comorbidities
Hematologic Adverse Events and Malignancy Risk
JAK inhibitors are associated with distinct hematologic abnormalities and malignancy risks, influenced by their pharmacologic targets. JAK2 is particularly critical for signaling by erythropoietin, thrombopoietin, and granulocyte-macrophage colony-stimulating factor, making its inhibition a primary driver of cytopenias [9]. Furthermore, gain-of-function mutations in JAK2 (e.g., V617F) are directly implicated in myeloproliferative neoplasms [9].
Table 2: Hematologic and Oncologic Adverse Events Associated with JAK Inhibitors [62]
| Event Category | Specific Event | Reporting Signal (IC₀₂₅)* | Comments and Pathophysiology |
|---|---|---|---|
| Cytopenias | (Reported under 'Investigations' SOC) | 0.9 | Linked to JAK2 inhibition affecting hematopoiesis. |
| Malignancies | All Neoplasms | 0.8 | General increased reporting observed. |
| Hematopoietic neoplasms | 3.7 | Excluding leukemias and lymphomas. | |
| Malignant skin neoplasms | >0 | Significant increased reporting, particularly non-melanoma skin cancer with ruxolitinib. | |
| Thromboembolism | Embolism and thrombosis | 0.4 | Notable for tofacitinib and baricitinib, leading to FDA/EMA warnings. |
*IC₀₂₅: Lower end of the 95% credibility interval of the Information Component. A positive value indicates a significant signal.
Experimental Protocols for Assessing Infection Risk and Immune Function
In Vivo Model of Acute Bacterial Infection
A 2025 study on shrimp provides a paradigm for investigating the role of excessive JAK-STAT activation in acute infection and mortality, offering a streamlined model for preclinical research [65].
Objective: To determine the role of overactivated JAK-STAT signaling in the pathogenesis of acute Vibrio parahaemolyticus infection. Materials:
- Animal Model: Pacific white shrimp (Penaeus vannamei).
- Pathogen: V. parahaemolyticus strain with pirAvp and pirBvp virulence genes.
- Key Reagents: dsRNA for JAK, STAT, SOCS2 (experimental); dsRNA for GFP (control); specific primers for qRT-PCR; rabbit anti-shrimp STAT, Dorsal, Relish antibodies; anticoagulant buffer.
Methodology:
- Gene Silencing via RNAi: Shrimp are injected with gene-specific dsRNA (JAK, STAT, SOCS2) or control GFP-dsRNA. Hemocytes and gill tissues are sampled 48 hours post-injection to confirm knockdown efficiency via qRT-PCR [65].
- Immune Challenge: Shrimp are divided into groups and intramuscularly injected with a high dose of V. parahaemolyticus or a PBS control.
- Post-Infection Monitoring:
- Mortality: Recorded every 2 hours.
- Bacterial Load: Quantified in gill tissues at 8 and 16 hours post-infection using qPCR targeting the pirAvp toxin gene.
- Pathological Analysis: Muscle tissue from injection sites is paraffin-sectioned and stained with hematoxylin-eosin (H&E) for observation of inflammation-like pathological changes.
- Immune Activation: Analyze STAT activation (phosphorylation and dimerization) via Western blot using nuclear extracts from hemocytes. Reactive oxygen species (ROS) levels, apoptosis rates, and phagocytic activities of hemocytes are assessed by flow cytometry [65].
Key Finding: Weakening JAK-STAT signaling via RNAi attenuated the inflammatory response and reduced mortality, whereas enhancing signaling accelerated death, demonstrating that immune overactivation is a direct cause of mortality in acute infection [65].
Workflow for In Vivo Infection and Pathway Analysis
The experimental workflow for the described protocol is outlined below.
Figure 2: In Vivo Workflow for JAK-STAT Pathway Analysis in Infection.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Investigating JAK-STAT Pathway in Infection and Immunity
| Reagent / Material | Function / Application | Specific Examples / Notes |
|---|---|---|
| Gene-Specific dsRNA | Targeted gene silencing in experimental models to establish causal relationships. | dsRNA targeting JAK, STAT, or negative regulators like SOCS2 [65]. |
| Pathogen Stocks | For immune challenge experiments to model infection in a controlled setting. | Vibrio parahaemolyticus with defined virulence genes (e.g., pirAvp, pirBvp) [65]. |
| Phospho-Specific Antibodies | Detection of pathway activation by Western blot or immunofluorescence. | Rabbit anti-STAT, anti-Dorsal, anti-Relish; anti-phospho-STAT antibodies [65]. |
| qRT-PCR Assays | Quantifying gene expression of pathway components, cytokines, and antimicrobial effectors. | Primers for JAK, STAT, SOCS, EF-1α (internal control), pathogen load (e.g., pirAvp) [65]. |
| Flow Cytometry Reagents | Profiling immune cell populations, apoptosis, ROS production, and phagocytic activity. | Assays for ROS, apoptosis (Annexin V), phagocytosis (fluorescent beads/bacteria) [65]. |
| JAK Inhibitors | Pharmacologic tools to inhibit the pathway in cellular or animal models. | Ruxolitinib (JAK1/2), Tofacitinib (JAK1/3), Baricitinib (JAK1/2) [62]. |
Understanding and Overcoming Drug Resistance Mechanisms
The Janus kinase-signal transducer and activator of transcription (JAK-STAT) pathway serves as a critical communication node in cellular function, transducing signals from over 50 cytokines, growth factors, and hormones [1] [66] [67]. This evolutionarily conserved pathway regulates vital processes including hematopoiesis, immune fitness, inflammation, and apoptosis [1]. The pathway's core components include four JAK family members (JAK1, JAK2, JAK3, TYK2) and seven STAT transcription factors (STAT1, STAT2, STAT3, STAT4, STAT5A, STAT5B, STAT6) [1] [27]. Upon cytokine binding, receptor-associated JAKs undergo trans-phosphorylation, subsequently phosphorylating STAT proteins, which then dimerize and translocate to the nucleus to modulate gene expression [1] [27].
Dysregulated JAK-STAT signaling underpins various pathologies, particularly myeloproliferative neoplasms (MPNs), autoimmune diseases, and cancers [1] [68] [67]. The landmark discovery of the JAK2V617F gain-of-function mutation in most patients with polycythemia vera and approximately half with essential thrombocythemia or primary myelofibrosis revolutionized MPN treatment and spurred development of JAK inhibitors [68] [69]. These small molecule therapeutics, beginning with ruxolitinib approved in 2011, target the ATP-binding site of JAK kinases to suppress constitutive pathway activation [68] [70]. However, their clinical success is increasingly compromised by acquired drug resistance, presenting a formidable challenge in therapeutic management [70].
Established Mechanisms of Drug Resistance
Mutation-Driven Resistance
The most characterized resistance mechanism involves acquired mutations in the kinase domain of JAK proteins that impair inhibitor binding while preserving catalytic activity. These mutations frequently parallel resistance mechanisms observed in other kinase-driven malignancies.
Gatekeeper Mutations: Analogous to T315I in BCR-ABL, gatekeeper mutations in JAKs represent a key resistance mechanism. The gatekeeper residue controls access to a hydrophobic pocket in the ATP-binding site [70]. Substitutions like JAK2V617F/T875N and other structurally analogous positions reduce drug affinity through steric hindrance and altered interaction networks while maintaining kinase functionality [70].
ATP-Binding Pocket Mutations: Additional mutations within the ATP-binding pocket, such as those affecting the phosphate-binding loop (P-loop) and activation loop (A-loop), can allosterically modify the drug-binding site conformation, reducing inhibitor affinity without compromising ATP binding and catalytic activity [70].
Bypass Signaling and Pathway Reactivation
Tumor cells evade JAK inhibition through compensatory signaling pathways that maintain downstream STAT activation and survival signals.
STAT-Independent JAK2 Signaling: Nuclear JAK2 phosphorylates histone H3 at tyrosine 41 (H3Y41), displacing HP1α and modifying chromatin architecture to promote expression of oncogenes like MYC [68]. This epigenetic mechanism persists despite JAK kinase inhibition, maintaining oncogenic transcription.
Alternative Kinase Activation: Resistance emerges through upregulation of parallel signaling cascades, including PI3K/Akt/mTOR, MAPK, and Src-family kinases [68]. These pathways compensate for inhibited JAK-STAT signaling, sustaining cellular proliferation and survival.
Cytokine Feedback Loops: Therapeutic JAK inhibition disrupts negative feedback mechanisms, leading to elevated circulating cytokines that reactivate pathway signaling through wild-type JAK proteins or alternative JAK isoforms not targeted by the specific inhibitor [68].
Heterodimerization and JAK Isoform Switching
JAKs function as homodimers or heterodimers upon cytokine receptor activation [70]. Resistance can emerge through altered dimerization partnerships or isoform compensation, where inhibited JAK isoforms are replaced by non-targeted family members. For instance, JAK1 inhibition may be bypassed by increased JAK3 or TYK2 activity in specific cytokine signaling contexts [70].
Table 1: Key Resistance Mutations in JAK-STAT Pathway Components
| Mutation | Location | Functional Consequence | Therapeutic Impact |
|---|---|---|---|
| JAK2T875N | Gatekeeper | Steric hindrance of inhibitor binding | Reduces efficacy of multiple ATP-competitive inhibitors |
| JAK2V617F | Pseudokinase domain (JH2) | Constitutive kinase activation | Primary driver mutation; alters sensitivity to JAK2 inhibitors |
| JAK1 Mutations | Kinase domain | Altered ATP-binding pocket conformation | Resistance to JAK1-selective inhibitors |
| MPLW515L/K | Transmembrane domain | Ligand-independent activation | JAK2-independent pathway activation |
Experimental Approaches for Resistance Mechanism Investigation
Real-Time Monitoring of STAT Activation
Conventional methods for detecting STAT activation (e.g., phospho-STAT antibodies) require cell fixation, preventing dynamic monitoring of pathway activity. Recently developed STATeLight biosensors enable real-time tracking of STAT conformational changes in live cells using fluorescence lifetime imaging microscopy-Förster resonance energy transfer (FLIM-FRET) [71].
Protocol: STATeLight Biosensor Implementation
Biosensor Design: Fuse mNeonGreen (donor) and mScarlet-I (acceptor) fluorescent proteins to STAT C-termini adjacent to SH2 domains. This positioning maximizes FRET efficiency changes during cytokine-induced STAT conformational shifts from antiparallel to parallel dimers [71].
Cell Line Development: Transfect biosensor constructs into relevant cell models (e.g., HEK-Blue IL-2 cells for STAT5 studies). Validate biosensor functionality against traditional phospho-STAT measurements [71].
FLIM-FRET Imaging:
- Culture STATeLight-expressing cells in imaging-optimized media
- Acquire baseline fluorescence lifetime measurements
- Treat with JAK inhibitors and/or cytokines
- Monitor fluorescence lifetime changes over time (1-60 minutes)
- Calculate FRET efficiency from lifetime reductions [71]
Data Analysis: Quantify STAT activation kinetics and inhibitor efficacy through FRET efficiency curves and dose-response relationships [71].
Resistance Mutation Screening
Comprehensive genomic profiling of resistant disease identifies acquired mutations driving therapeutic escape.
Protocol: Longitudinal Mutation Monitoring
Sample Collection: Obtain paired pre-treatment and progression samples (bone marrow, peripheral blood, or tissue biopsies).
Genetic Analysis:
- Targeted sequencing: Focus on JAK-STAT pathway genes (JAK1, JAK2, JAK3, TYK2, STATs, SOCS)
- Whole exome sequencing: Identify novel resistance mutations outside canonical pathway
- Digital droplet PCR: Sensitively quantify allele burden of known resistance mutations
Functional Validation:
- Clone identified mutations into cytokine-dependent cell lines (e.g., Ba/F3)
- Assess cytokine-independent growth and inhibitor sensitivity (IC50 shifts)
- Evaluate STAT phosphorylation and downstream signaling in presence of inhibitor
Structural Biology Approaches
Understanding resistance mutations at atomic resolution informs next-generation inhibitor design.
Protocol: Structural Analysis of JAK-Inhibitor Complexes
Protein Expression: Express and purify wild-type and mutant JAK kinase domains.
Crystallization: Co-crystallize JAK proteins with clinical inhibitors using vapor diffusion methods.
Structure Determination: Solve crystal structures through X-ray crystallography (typically 1.8-2.8Ã… resolution).
Molecular Dynamics: Simulate protein-inhibitor interactions to understand conformational flexibility and binding energetics.
Table 2: Essential Research Reagents for Resistance Studies
| Reagent/Category | Specific Examples | Research Application |
|---|---|---|
| JAK Inhibitors | Ruxolitinib, Tofacitinib, Baricitinib | Reference compounds for resistance profiling |
| Biosensors | STATeLight constructs (STAT5A variants) | Real-time STAT activation monitoring in live cells |
| Cell Lines | HEL, SET-2, Ba/F3, HEK-Blue IL-2 | Models for mutation expression and signaling studies |
| Antibodies | Phospho-STATs (Y694/699), Total STATs, pJAK2 | Traditional Western blot and flow cytometry analysis |
| Mutation Plasmids | JAK2V617F, JAK2T875N, other resistance mutants | Functional validation of resistance mechanisms |
Emerging Strategies to Overcome Resistance
Next-Generation JAK Inhibitors
Novel inhibitors are designed to maintain efficacy against resistance mutations through distinct binding modes.
Type II Inhibitors: These compounds bind to the inactive "DFG-out" JAK conformation, accessing deep hydrophobic pockets less susceptible to gatekeeper mutations. Type II inhibitors demonstrate activity against various resistance mutations in biochemical and cellular assays [70].
Covalent JAK Inhibitors: Irreversible inhibitors forming covalent bonds with non-catalytic cysteine residues near the ATP-binding pocket. This mechanism provides sustained target engagement and potential efficacy against resistance mutations that reduce drug affinity through allosteric mechanisms [70].
JAK Dimerization Disruption
The recent elucidation of full-length murine JAK1 structure revealed a unique dimerization interface involving FERM-SH2 domains [70]. Targeting this protein-protein interaction represents a novel strategy to overcome catalytic site mutations.
Approach: Develop peptide mimetics or small molecules that disrupt JAK-JAK or JAK-receptor interactions, preventing pathway activation upstream of kinase activity. This strategy may remain effective against kinase domain mutations [70].
Rational Combination Therapies
Leveraging JAK inhibitors with complementary agents targets multiple resistance mechanisms simultaneously.
HDAC Inhibitors: Overcome JAK2-mediated epigenetic modifications by normalizing histone acetylation patterns.
PI3K/mTOR Inhibitors: Counteract bypass signaling pathway activation that maintains cell survival despite JAK inhibition.
BCL-2/xL Inhibitors: Target mitochondrial dependencies in resistant cells, potentially eradicating persistent progenitor populations.
Drug resistance in JAK-STAT targeted therapy represents a multifaceted challenge requiring integrated basic, translational, and clinical research approaches. The convergence of real-time biosensor technology, structural biology, and comprehensive genomic profiling enables unprecedented dissection of resistance mechanisms. Future efforts should prioritize identifying and targeting persistent JAK2V617F-positive stem cells, developing selective inhibitors with activity against common resistance mutations, and validating rational combination strategies in clinical trials. As structural insights into full-length JAK complexes advance, new therapeutic opportunities beyond ATP-competitive inhibition will emerge, ultimately improving outcomes for patients with JAK-STAT-driven diseases.
Optimizing Dosing Regimens for Efficacy and Safety
The Janus kinase-signal transducer and activator of transcription (JAK-STAT) signaling pathway serves as a central communication node in cellular function, transmitting signals from over 50 cytokines, interleukins, and growth factors [1] [36]. This evolutionarily conserved pathway regulates crucial processes including immune response, hematopoiesis, inflammation, and cell differentiation [1] [72]. Upon extracellular ligand binding to transmembrane receptors, receptor-associated JAKs (JAK1, JAK2, JAK3, and TYK2) undergo trans-phosphorylation, subsequently phosphorylating STAT transcription factors (STAT1-6) [36] [72]. Phosphorylated STATs dimerize and translocate to the nucleus, where they direct the transcription of target genes governing inflammatory and immune responses [1] [36].
Dysregulated JAK-STAT signaling constitutes a fundamental driver of numerous immune-mediated diseases, including rheumatoid arthritis (RA), psoriasis, psoriatic arthritis (PsA), atopic dermatitis (AD), and inflammatory bowel disease (IBD) [73] [36] [55]. This central role in immunopathology has established JAK proteins as promising therapeutic targets, leading to the development of JAK inhibitors (jakinibs) [35] [73]. First-generation jakinibs like tofacitinib, baricitinib, and ruxolitinib have demonstrated significant clinical efficacy across multiple inflammatory conditions [73] [36]. However, their clinical application presents a fundamental challenge: balancing therapeutic efficacy against potential adverse effects, including opportunistic infections, thromboembolic complications, and other dose-dependent toxicities [49] [73]. This whitepaper examines current strategies for optimizing JAK inhibitor dosing regimens to maximize clinical efficacy while maintaining acceptable safety profiles for researchers and drug development professionals.
Quantitative Analysis of JAK Inhibitor Activity and Dosing
Pharmacological Profiles of JAK Inhibitors
Table 1: Comparative ICâ‚…â‚€ Values and Selectivity Profiles of JAK Inhibitors
| Inhibitor Name | JAK1 ICâ‚…â‚€ (nM) | JAK2 ICâ‚…â‚€ (nM) | JAK3 ICâ‚…â‚€ (nM) | TYK2 ICâ‚…â‚€ (nM) | Primary Clinical Indications | Key Safety Considerations |
|---|---|---|---|---|---|---|
| Tofacitinib [73] | 112 (preferentially inhibits JAK1/JAK3 over JAK2) | - | - | - | Rheumatoid Arthritis, Psoriatic Arthritis | Opportunistic infections, thromboembolism |
| Ruxolitinib [73] | - | - | - | - | Myeloproliferative Neoplasms, Myelofibrosis | Hematological toxicity, infection risk |
| Baricitinib [36] | 5.9 | 5.7 | >400 | 53 | Rheumatoid Arthritis, Atopic Dermatitis | Thrombosis, increased cholesterol |
| Igalan (Natural Product) [49] | <5,000 nM | - | - | - | Preclinical (Atopic Dermatitis) | - |
| Cycloastragenol (Natural Product) [49] | <50,000 nM | - | - | - | Preclinical (Gastric Cancer) | - |
| Homoharringtonine (Natural Product) [49] | <1,000 nM | - | - | - | Preclinical (NSCLC) | - |
Clinically Established Dosing Regimens
Table 2: Approved Dosing Regimens for JAK Inhibitors in Inflammatory Conditions
| JAK Inhibitor | Disease Indication | Standard Dose | Dose Adjustment Criteria | Efficacy Endpoints | Key Trial Findings |
|---|---|---|---|---|---|
| Tofacitinib [73] | Rheumatoid Arthritis | 5 mg BID (immediate-release) 11 mg QD (extended-release) | Renal/hepatic impairment, drug interactions, lymphopenia | ACR20/50/70 response, HAQ-DI improvement, radiographic progression inhibition | Superior to methotrexate in methotrexate-naïve patients; non-inferior to adalimumab |
| Tofacitinib [73] | Psoriatic Arthritis | 5 mg BID | Similar to RA dosing | ACR20 response, skin clearance (PASI) | Effective in refractory disease |
| Baricitinib [36] | Rheumatoid Arthritis | 4 mg QD (2 mg QD with renal impairment) | Renal impairment, lymphopenia, anemia | ACR20 response, radiographic progression inhibition | Effective as monotherapy or with methotrexate |
| Ruxolitinib [73] | Myelofibrosis | 15-20 mg BID (based on platelet count) | Thrombocytopenia, anemia | Spleen volume reduction, symptom improvement | Approved based on COMFORT-I and II trials |
Experimental Approaches for Dosing Optimization
In Vitro Profiling of JAK Inhibitor Potency and Selectivity
Protocol 1: Determination of ICâ‚…â‚€ Values Using Phospho-STAT Inhibition Assays
Purpose: To quantitatively measure the potency and selectivity of JAK inhibitors against different JAK isoforms in cellular systems.
Methodology:
- Cell Line Selection: Utilize cytokine-responsive cell lines expressing specific JAK-dependent receptors (e.g., T cells for JAK3, erythroid progenitors for JAK2).
- Compound Treatment: Incubate cells with serial dilutions of JAK inhibitors (typically spanning 0.1 nM to 10,000 nM) for 1-2 hours.
- Pathway Stimulation: Activate specific JAK-STAT pathways using isoform-selective cytokines:
- Cell Lysis and Analysis: Lyse cells after 15-30 minutes of cytokine stimulation and quantify phosphorylated STAT levels via:
- Western blotting with phospho-specific STAT antibodies
- Phospho-flow cytometry
- ELISA-based phospho-STAT detection assays
- Data Analysis: Calculate ICâ‚…â‚€ values using non-linear regression of inhibitor concentration versus percentage phosphorylation inhibition relative to cytokine-stimulated controls.
Applications: This methodology enabled the characterization of natural products like Igalan (IC₅₀ <5 μM for JAK1) and Homoharringtonine (IC₅₀ <1 μM for JAK1) [49], establishing their potential as JAK inhibitors.
In Vivo Efficacy and Safety Profiling
Protocol 2: Preclinical Dosing Optimization in Disease Models
Purpose: To establish therapeutic windows and identify optimal dosing regimens in biologically relevant systems.
Methodology:
- Animal Model Selection:
- Dosing Regimen Testing:
- Multiple daily dosing (BID) versus single daily dosing (QD)
- Dose escalation studies (low, medium, high doses based on in vitro ICâ‚…â‚€ values)
- Route of administration optimization (oral gavage, subcutaneous, intraperitoneal)
- Efficacy Assessment:
- Clinical scoring of disease severity (e.g., arthritis index, skin inflammation)
- Histopathological analysis of target tissues
- Cytokine profiling in serum and tissues (e.g., IL-6, IL-17, IFN-γ)
- Phospho-STAT analysis in target tissues via immunohistochemistry
- Safety and Tolerability Assessment:
- Complete blood counts (monitoring for anemia, lymphopenia, thrombocytopenia)
- Liver and kidney function tests
- Assessment of opportunistic infections
- Thrombotic events evaluation in susceptible models
Applications: Preclinical studies with tofacitinib in arthritis models demonstrated efficacy with dose-dependent suppression of STAT phosphorylation, informing initial clinical trial designs [73].
Clinical Dose-Finding Strategies
Protocol 3: Phase 2 Dose-Ranging Study Design
Purpose: To identify the optimal therapeutic dose for Phase 3 confirmatory trials.
Methodology:
- Study Population: Patients with active disease despite standard therapy.
- Trial Design: Randomized, double-blind, placebo-controlled, parallel-group.
- Dosing Arms: Multiple active doses (e.g., 1 mg, 2.5 mg, 5 mg, 10 mg, 15 mg BID) plus placebo.
- Primary Endpoints: Disease-specific efficacy measures:
- Safety Monitoring:
- Comprehensive laboratory assessments (hematology, chemistry)
- Adverse event recording with special attention to infections
- Cardiovascular and thromboembolic event monitoring
- Malignancy assessment
- Pharmacodynamic Assessments:
- Biomarker evaluation (e.g., CRP, SAA)
- STAT phosphorylation inhibition in circulating immune cells
- Gene expression profiling of JAK-STAT pathway genes
Applications: The tofacitinib RA development program included six Phase 3 trials encompassing over 6,000 subjects followed for up to 8 years, establishing the 5 mg BID dose as optimal for efficacy-safety balance [73].
Visualization of JAK-STAT Signaling and Therapeutic Targeting
JAK-STAT Signaling Pathway and Inhibitor Mechanism
JAK-STAT Pathway and Inhibition Mechanism
Dosing Optimization Strategy Workflow
Dosing Optimization Workflow
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for JAK-STAT Pathway Investigation
| Reagent Category | Specific Examples | Research Applications | Technical Considerations |
|---|---|---|---|
| JAK Inhibitors | Tofacitinib, Ruxolitinib, Baricitinib, Decernotinib (JAK3-selective) | Pathway inhibition studies, dose-response experiments, combination therapies | Varying selectivity profiles; consider off-target effects at high concentrations |
| Cytokines for Pathway Activation | IFN-α/γ (JAK1/TYK2), IL-6 (JAK1/JAK2), IL-2/4/7/9/15/21 (JAK1/JAK3), EPO/TPO (JAK2) | Selective JAK-STAT pathway stimulation, phospho-STAT analysis | Concentration and timing critical for specific pathway activation |
| Phospho-Specific Antibodies | Anti-pSTAT1 (Y701), pSTAT3 (Y705), pSTAT5 (Y694), pSTAT6 (Y641) | Western blotting, flow cytometry, immunohistochemistry for pathway activation assessment | Requires proper cell fixation/permeabilization; short stimulation times (15-30 min) |
| JAK-STAT Reporter Cell Lines | STAT-responsive luciferase constructs (e.g., STAT1: ISRE, STAT3: APRE, STAT5: GAS, STAT6: IL-4RE) | High-throughput inhibitor screening, functional pathway assessment | Context-dependent responses; validate with endogenous targets |
| Natural Product JAK Inhibitors | Igalan, Isobavachalcone, Homoharringtonine, Myricetin [49] | Novel inhibitor discovery, structure-activity relationship studies | Often less potent than synthetic inhibitors; potential multi-target effects |
| Genetic Tools | JAK knockout cells, siRNA/shRNA, CRISPR-Cas9 gene editing | Target validation, mechanistic studies, synthetic lethality screens | Compensation by other JAK family members; cell viability concerns |
The optimization of JAK inhibitor dosing regimens represents an ongoing challenge at the intersection of clinical efficacy and safety management. Current strategies employing fixed dosing based on extensive clinical trials have proven effective for conditions like rheumatoid arthritis and psoriatic arthritis [73]. However, the future of JAK inhibitor therapy lies in more personalized approaches that account for individual patient characteristics, disease states, and pharmacogenetic profiles. Emerging strategies include therapeutic drug monitoring to maintain target concentrations, biomarker-driven dose adjustments, and the development of more selective next-generation inhibitors with improved therapeutic windows [35] [36]. Natural products from traditional medicine systems continue to provide novel chemical scaffolds for developing JAK inhibitors with potentially distinct safety and efficacy profiles [49]. As our understanding of JAK-STAT biology evolves, so too will our approaches to dosing optimization, ultimately enabling more precise, effective, and safer targeting of this critical signaling pathway in inflammatory diseases.
The Role of Pharmacogenomics in Tailoring Jakinib Therapy
The Janus kinase-signal transducer and activator of transcription (JAK-STAT) pathway is a cornerstone of inflammatory signaling, and its inhibition with "jakinibs" has revolutionized the treatment of immune-mediated inflammatory diseases (IMIDs) [74]. However, individual patient responses to these therapies are highly variable. This whitepaper explores the emerging role of pharmacogenomics in deciphering this variability, detailing how genetic profiling of the JAK-STAT pathway can guide the selection of JAK inhibitors (JAKi), optimize dosing, predict adverse effects, and ultimately pave the way for personalized treatment strategies that maximize efficacy and safety for patients with rheumatoid arthritis (RA) and other IMIDs.
JAK inhibitors, including tofacitinib, baricitinib, upadacitinib, and filgotinib, are established therapies for numerous IMIDs [75]. They function as small-molecule antagonists of the JAK-STAT pathway, a critical hub for transmitting signals from over 50 cytokines [66]. Despite proven clinical efficacy, a significant proportion of patients exhibit inadequate response or experience adverse events. This heterogeneity stems from the complex pathophysiology of IMIDs, where the specific cytokine profiles and the degree of JAK-STAT activation can differ substantially between individuals [76] [74].
Evidence suggests that beyond peripheral inflammation, JAK-STAT signaling is integral to central pain processing and neuroimmune interactions, explaining why some patients experience pain relief dissociated from inflammatory control [76]. This multifactorial pathophysiology, combined with genetic differences in drug metabolism and JAK-STAT component function, creates a compelling case for a pharmacogenomic approach to tailor therapy. The integration of genomic data aims to move beyond the current "trial-and-error" paradigm, enabling a precision medicine framework where the most appropriate JAKi and dose are selected based on a patient's unique genetic signature.
JAK-STAT Pathway Architecture and Jakinib Mechanisms
A thorough understanding of the JAK-STAT pathway is fundamental to appreciating the pharmacogenomic targets within it.
Canonical Pathway Activation
The canonical JAK-STAT signaling cascade is initiated when a cytokine binds to its corresponding cell surface receptor, typically leading to receptor dimerization [27]. This event brings the receptor-associated JAK kinases (JAK1, JAK2, JAK3, and TYK2) into close proximity, facilitating their trans-phosphorylation and activation. The activated JAKs then phosphorylate tyrosine residues on the receptor cytoplasmic tails, creating docking sites for STAT proteins. Upon recruitment, STATs are themselves phosphorylated by JAKs, prompting their dimerization and translocation to the nucleus. Inside the nucleus, STAT dimers act as transcription factors, binding to specific regulatory sequences to control the expression of target genes involved in inflammation, cell proliferation, and differentiation [27] [9].
The following diagram illustrates this core signaling mechanism:
Mechanism of JAK Inhibition
Jakinibs are ATP-competitive small molecules that bind to the catalytic site of JAK kinases, preventing the phosphorylation and subsequent activation of STAT proteins [74]. This blockade inhibits the downstream transcription of pro-inflammatory genes. A critical differentiator among available JAKi is their selectivity for specific JAK isoforms, which directly influences their efficacy and safety profiles [74]. For instance, JAK1 inhibition is largely responsible for anti-inflammatory effects, while inhibition of JAK2 is linked to hematological adverse effects like anemia and thrombocytopenia due to its role in erythropoietin and thrombopoietin signaling [74].
Table 1: Selectivity and Approved Doses of Common JAK Inhibitors [76]
| JAK Inhibitor | Selectivity Profile | Recommended Dose |
|---|---|---|
| Tofacitinib | JAK1 and JAK3 (strong); JAK2 (minor) | 2 × 5 mg |
| Baricitinib | JAK1 and JAK2 (strong); TYK2 (moderate) | 2 mg / 4 mg |
| Upadacitinib | JAK1 (strong) | 15 mg |
| Filgotinib | JAK1 (strong) | 100 mg / 200 mg |
Key Pharmacogenomic Determinants of JAKi Response
Interindividual variability in JAKi response is influenced by polymorphisms in genes encoding drug transporters, metabolizing enzymes, and components of the JAK-STAT pathway itself.
Pharmacokinetic Variability: Absorption, Distribution, Metabolism, and Excretion (ADME)
Genetic variations in proteins governing the ADME of JAKi can significantly alter drug exposure.
- Drug Transporters: Polymorphisms in genes encoding efflux transporters like P-glycoprotein (ABCB1) can influence gastrointestinal absorption and tissue distribution of JAKi, which are predominantly oral small molecules [77].
- Drug-Metabolizing Enzymes: JAKi are primarily metabolized by cytochrome P450 (CYP) enzymes, particularly CYP3A4. Genetic polymorphisms leading to increased or decreased CYP3A4 activity can result in subtherapeutic or toxic drug levels, respectively [74]. For example, filgotinib undergoes intestinal metabolization, which may characterize its distinct benefit/risk ratio [74].
Pharmacodynamic Variability: The JAK-STAT Pathway and Drug Targets
Genetic variation within the JAK-STAT pathway itself can alter the target's structure, expression, or function, thereby modulating drug response.
- JAK and STAT Polymorphisms: Single nucleotide polymorphisms (SNPs) in JAK2 have been associated with Behçet’s disease, while SNPs in TYK2 are strongly linked to systemic lupus erythematosus (SLE) and rheumatoid arthritis (RA) [9]. These same polymorphisms could theoretically affect JAKi binding affinity or downstream signaling efficacy.
- Cytokine and Receptor Genetics: Variants in genes for specific cytokines (e.g., IL-6, IFN-γ) or their receptors can alter the inflammatory milieu and the degree of pathway activation, influencing which JAK isoform is most critical for signaling in a given patient [76] [27]. For instance, an "IL-6-high" patient might respond optimally to a JAK1-selective inhibitor.
Table 2: Key Genetic Variants with Potential Impact on JAKi Therapy
| Gene | Variant | Functional Implication | Potential Clinical Impact on JAKi |
|---|---|---|---|
| CYP3A4/CYP3A5 | Multiple SNPs | Altered enzyme activity (Poor/Intermediate/Extensive Metabolizer) | Modified drug clearance and exposure, requiring dose adjustment. |
| ABCB1 | rs1045642 (C3435T) | Altered P-gp transporter activity | Potential impact on oral bioavailability and tissue penetration. |
| TYK2 | rs34536443 | Loss-of-function; associated with autoimmunity [9] | May predict enhanced response to TYK2-targeting therapies. |
| JAK2 | V617F (somatic) | Gain-of-function; driver of myeloproliferative neoplasms [9] | Determines efficacy of JAK2-inhibitors like ruxolitinib in oncology [66]. |
| STAT4 | rs7574865 | Risk variant for RA and SLE [9] | May identify patients with distinct pathway activation amenable to JAK inhibition. |
Experimental Methodologies for Pharmacogenomic Research
Robust experimental protocols are essential to validate pharmacogenomic associations and translate them into clinical tools.
Genome-Wide Association Studies (GWAS)
Objective: To identify novel genetic variants across the entire genome associated with JAKi treatment response or toxicity without a prior hypothesis. Protocol:
- Cohort Selection: Recruit a large cohort of patients with a well-defined IMID (e.g., RA) treated with a specific JAKi. Precisely phenotype patients as "responders," "non-responders," or those with specific adverse events (e.g., herpes zoster, cytopenias).
- Genotyping: Extract genomic DNA from peripheral blood mononuclear cells (PBMCs). genotype using high-density SNP microarrays (e.g., Illumina Infinium Global Screening Array).
- Quality Control: Filter out SNPs with low call rates (<95%), significant deviation from Hardy-Weinberg equilibrium (p < 1 × 10â»â¶), or low minor allele frequency (<1%). Exclude samples with high genotype failure rates or unexpected relatedness.
- Imputation: Use reference panels (e.g., 1000 Genomes Project) to infer ungenotyped SNPs, increasing genomic coverage.
- Association Analysis: Perform a logistic regression analysis between SNP genotypes and response phenotype, adjusting for covariates like age, sex, and disease duration. A p-value < 5 × 10â»â¸ is typically considered genome-wide significant.
Targeted Next-Generation Sequencing (NGS)
Objective: To deeply sequence all exons and regulatory regions of candidate genes involved in JAK-STAT signaling and JAKi ADME. Protocol:
- Panel Design: Design a custom oligonucleotide probe library to capture genomic regions of interest (e.g., JAK1, JAK2, JAK3, TYK2, STAT1-6, CYP3A4, ABCB1).
- Library Preparation & Sequencing: Fragment genomic DNA, ligate adapters, and hybridize with the custom probe library. Capture the target regions, amplify the library, and sequence on a high-throughput platform (e.g., Illumina NovaSeq).
- Bioinformatic Analysis: Align sequence reads to a reference genome (GRCh38). Call variants (SNPs, insertions/deletions) and annotate them for functional impact (e.g., missense, nonsense, splice-site) using databases like ClinVar and gnomAD.
- Association Testing: Statistically correlate identified rare and common variants with clinical outcomes.
Functional Validation of Genetic VariantsIn Vitro
Objective: To establish a causal link between an identified genetic variant and an altered cellular response to JAKi. Protocol:
- Cell Line Engineering: Use CRISPR/Cas9 gene editing to introduce a candidate gain-of-function (GOF) or loss-of-function (LOF) variant into a human cell line (e.g., HEK293T or a macrophage cell line). An isogenic control line with the wild-type sequence is generated in parallel.
- Stimulatory Assay: Stimulate the engineered cells with a relevant cytokine (e.g., IL-6 for JAK1/2, IFN-α for JAK1/TYK2) in the presence of a titrated dose of a JAKi.
- Downstream Readouts:
- Western Blot: Harvest cell lysates and probe with antibodies against phosphorylated STAT proteins (e.g., pSTAT3, pSTAT1) and total STATs to assess pathway inhibition by the drug.
- Quantitative PCR (qPCR): Extract RNA, reverse transcribe to cDNA, and measure the expression of downstream inflammatory genes (e.g., SOCS3, MX1) to quantify functional pathway blockade.
- Cell Proliferation/Viability Assay: Use assays like MTT or CellTiter-Glo to assess if the variant confers altered sensitivity to JAKi-induced cytostasis.
The following diagram outlines this functional validation workflow:
The Scientist's Toolkit: Key Reagents for JAK-STAT Pharmacogenomics
Table 3: Essential Research Reagents for Investigating JAK-STAT Pharmacogenomics
| Reagent / Solution | Function in Research |
|---|---|
| Phospho-Specific STAT Antibodies | Essential for Western Blot or flow cytometry to directly measure JAK-STAT pathway activation and its inhibition by JAKi in patient-derived cells or engineered lines. |
| Recombinant Human Cytokines (e.g., IL-6, IFN-γ, GM-CSF) | Used to ex vivo stimulate PBMCs or cell lines to activate specific JAK-STAT signaling modules and test the potency of JAKi. |
| JAK Inhibitors (Selective and Pan-Inhibitors) | Tool compounds for in vitro studies to dissect the contribution of specific JAK isoforms to signaling and gene expression in genetically defined contexts. |
| CRISPR/Cas9 Gene Editing System | Enables the introduction or correction of specific genetic variants in cell lines to establish causality and study their functional impact on JAKi response. |
| DNA/RNA Extraction Kits (from Whole Blood/PAXgene tubes) | For obtaining high-quality genetic material for genotyping, sequencing, and transcriptomic analyses from patient cohorts. |
| CYP Inhibition & Phenotyping Kits | To characterize the metabolic stability of JAKi and assess the functional consequences of genetic polymorphisms in CYP enzymes on drug metabolism. |
Pharmacogenomics holds immense promise for refining the use of JAK inhibitors in clinical practice. By integrating genetic data on drug metabolism and JAK-STAT pathway biology, it is becoming increasingly possible to predict which patients will derive the greatest benefit from a specific, selective JAKi while minimizing the risk of adverse events. The future of this field lies in the development of comprehensive pre-treatment genetic profiling panels that incorporate both ADME and pathway-specific variants. Furthermore, as the JAK inhibitor market expands—projected to reach $47.1 billion by 2029 with a robust pipeline of over 55 drugs in development—the need for such personalized approaches becomes ever more critical [77] [78]. Continued research, leveraging large-scale biobanks and advanced functional genomics, will be essential to fully realize the goal of precision immunomodulation, ensuring that the right JAKi is delivered to the right patient at the right dose.
The Janus kinase-signal transducer and activator of transcription (JAK-STAT) pathway represents an evolutionarily conserved signaling mechanism that enables rapid transduction of extracellular signals from the cell membrane to the nucleus, regulating fundamental processes including immune response, cellular proliferation, differentiation, and apoptosis [36] [1]. Since its discovery more than three decades ago, research on the JAK-STAT pathway has revolutionized our understanding of cytokine signaling and its implications in human disease [79]. The initial discovery that this pathway is employed by more than 50 cytokines, interferons, interleukins, and growth factors established its central role in immunoregulation and provided the foundation for therapeutic targeting [36] [1].
First-generation JAK inhibitors, often termed "jakinibs," including tofacitinib, baricitinib, and ruxolitinib, demonstrated the clinical viability of targeting this pathway but revealed significant limitations related to selectivity and safety [44]. These early agents typically inhibited multiple JAK family members simultaneously, leading to broad immunosuppressive effects and mechanism-based toxicities [44] [80]. The current development landscape is now focused on next-generation inhibitors with enhanced selectivity profiles, novel therapeutic modalities beyond conventional small molecules, and innovative approaches to overcome the limitations of first-generation agents [81] [36]. This review examines the emerging therapeutic strategies that constitute the future of JAK-STAT pathway modulation, with particular emphasis on their application in inflammatory signaling research and drug development.
The clinical pipeline for JAK inhibitors remains robust, with over 50 pharmaceutical companies actively developing more than 55 therapeutic candidates across various stages of clinical development [81] [77]. This expansive pipeline reflects the continued interest in targeting the JAK-STAT pathway for a diverse array of autoimmune, inflammatory, and oncologic indications. The current pipeline encompasses molecules with varying selectivity profiles, novel chemical structures, and optimized therapeutic indices compared to first-generation agents.
Table 1: Selected Next-Generation JAK Inhibitors in Clinical Development
| Drug Name | Company | Phase | Key Indications | Selectivity Profile | Notable Characteristics |
|---|---|---|---|---|---|
| Povorcitinib (INCB054707) | Incyte Corporation | Phase III | Hidradenitis Suppurativa, Prurigo Nodularis, Vitiligo | JAK1-selective | Oral small-molecule; demonstrates high selectivity for JAK1 [81] [77] |
| Zasocitinib | Takeda | Phase III | Plaque Psoriasis, Erythrodermic Psoriasis, Pustular Psoriasis | Not specified | Oral administration; targets multiple psoriasis subtypes [81] |
| Ritlecitinib | Pfizer | Phase III | Ulcerative Colitis, Vitiligo | JAK3/TYK2 inhibitor | Strong inhibition of JAK3 and TYK2 with minimal effect on JAK1/JAK2 [81] [80] |
| CPL409116 | Celon Pharma | Phase II | Rheumatoid Arthritis | Dual JAK/ROCK inhibitor | First-in-class dual inhibitor; generates anti-inflammatory and anti-fibrotic effects [77] |
| ATI-2138 | Aclaris Therapeutics | Phase II | Atopic Dermatitis, T-cell mediated diseases | Covalent ITK/JAK3 inhibitor | Investigational oral covalent inhibitor; potential across T cell-mediated diseases [77] |
| INCB-160058 | Incyte Corporation | Phase I | Myeloproliferative Disorders | Not specified | Oral administration; targets hematologic malignancies [81] |
| SDC-1802 | Sareum | Preclinical | Cancer (T-ALL, B-cell lymphoma) | TYK2/JAK1 inhibitor | High selectivity for TYK2 and JAK1 over JAK2 and JAK3; potential for once-daily oral dosing [77] |
The diversity of mechanisms represented in the pipeline highlights several key trends in next-generation JAK inhibitor development. First, there is a pronounced emphasis on enhanced selectivity, with compounds designed to inhibit specific JAK isoforms to improve safety profiles while maintaining efficacy [44]. Second, the development of dual-specificity inhibitors that target JAKs along with complementary pathways represents an innovative approach to address complex disease pathophysiology [77]. Finally, the expansion into novel therapeutic areas beyond classical autoimmune conditions underscores the growing understanding of JAK-STAT signaling in diverse pathological processes.
Novel Therapeutic Modalities and Targeting Strategies
Enhanced Selectivity Profiles and Rational Drug Design
The evolution of JAK inhibitor design has progressively moved from first-generation pan-JAK inhibitors to increasingly selective agents that target specific JAK isoforms or combinations. This strategic shift is predicated on the understanding that each JAK family member (JAK1, JAK2, JAK3, and TYK2) mediates distinct biological functions through association with different cytokine receptors [44] [36].
JAK1 is predominantly involved in inflammatory cytokine signaling (e.g., IL-6, IFN-γ), making it a prime target for autoimmune and inflammatory conditions. JAK2 is principally associated with hematopoiesis (e.g., EPO, TPO signaling), and its inhibition is linked to hematological adverse effects including anemia, thrombocytopenia, and neutropenia. JAK3, which partners exclusively with the common gamma chain (γc) receptor subunit, is primarily expressed in hematopoietic cells and mediates signaling for IL-2, IL-4, IL-7, IL-9, IL-15, and IL-21. TYK2 regulates signaling for IL-12, IL-23, and type I interferons, positioning it as a promising target for autoimmune conditions with potentially improved safety profiles [44] [36] [27].
The structural basis for enhanced selectivity lies in the subtle differences in the ATP-binding pockets of the JAK kinases. While the ATP-binding sites are structurally similar across the JAK family, variations in amino acid sequences and conformational dynamics enable the design of inhibitors with preferential binding to specific JAK isoforms [44]. Contemporary drug design approaches utilize high-resolution crystallographic data of JAK kinase domains in complex with inhibitors to optimize interactions with these unique structural elements [36].
Diagram 1: The evolving spectrum of JAK inhibitor selectivity, from first-generation pan-JAK inhibitors to next-generation agents with enhanced specificity and novel mechanisms.
Dual-Specificity Inhibitors and Polypharmacology
Beyond isoform-selective inhibition, another innovative approach involves the development of dual-specificity inhibitors that simultaneously target JAKs and complementary signaling pathways. This strategy of "polypharmacology" aims to enhance efficacy through coordinated modulation of multiple pathogenic mechanisms while potentially mitigating resistance development [77].
CPL409116 represents a pioneering example of this approach as a first-in-class dual JAK/ROCK inhibitor currently in Phase II development for rheumatoid arthritis, particularly in patients with coexisting interstitial lung disease [77]. By combining JAK inhibition with ROCK (Rho-associated coiled-coil containing protein kinase) inhibition, this compound generates both anti-inflammatory and anti-fibrotic effects, addressing two key pathological processes in rheumatoid lung disease. The ROCK pathway is implicated in fibroblast activation, extracellular matrix deposition, and tissue fibrosis – processes not directly modulated by JAK inhibition alone.
Similarly, SDC-1802, a TYK2/JAK1 inhibitor in preclinical development, demonstrates high selectivity for TYK2 and JAK1 kinases over JAK2 and JAK3 [77]. This selectivity profile potentially offers a favorable balance of efficacy in autoimmune and inflammatory conditions while minimizing hematological adverse effects associated with JAK2 inhibition. The compound shows compelling efficacy in blocking cancer cell proliferation in cellular and disease models of T-cell acute lymphoblastic leukaemia (T-ALL) and B-cell lymphoma, suggesting potential applications in oncology beyond traditional inflammatory indications.
Covalent Inhibition Strategies
Covalent JAK inhibitors represent another innovative modality in the therapeutic landscape. ATI-2138 is an investigational oral covalent ITK/JAK3 inhibitor being developed for various T-cell-mediated diseases [77]. As a covalent inhibitor, ATI-2138 forms irreversible bonds with its target kinases, potentially offering extended target engagement, reduced dosing frequency, and improved selectivity through specific interaction with unique cysteine residues in the target kinases.
ITK (IL-2-inducible T-cell kinase) is a T-cell receptor-activated kinase involved in driving T-cell effector functions, while JAK3 is responsible for signal transduction of common gamma chain cytokines including IL-2, IL-4, IL-7, IL-9, IL-15, and IL-21. By simultaneously blocking both T-cell receptor function and cytokine signaling, ATI-2138 has potential utility across a spectrum of T-cell-driven autoimmune diseases [77].
Natural products derived from traditional medicinal plants are emerging as valuable sources for novel JAK inhibitors with unique structural motifs and potentially favorable safety profiles [49]. Recent comprehensive analyses have identified 88 natural products demonstrating JAK inhibitory activity across multiple pathological conditions, classified according to structural characteristics including flavonoids, alkaloids, and terpenoids [49].
Table 2: Selected Natural Products with JAK Inhibitory Activity
| Compound | Natural Source | Structural Class | Molecular Target | Potential Applications |
|---|---|---|---|---|
| Igalan | Inula helenium L. | Sesquiterpene | JAK1-STAT3 | Atopic dermatitis [49] |
| Spilanthol | Acmella oleracea (L.) R.K.Jansen | Diterpene | JAK1/2-STAT3 | Gastric cancer [49] |
| Isobavachalcone | Cullen corylifolium (L.) Medik | Isoflavonoid | JAK1-STAT3 | Rheumatoid arthritis [49] |
| Nitidine chloride | Zanthoxylum nitidum (Roxb.) DC | Alkaloid | JAK1-STAT3 | Hepatocellular carcinoma [49] |
| Homoharringtonine | Cephalotaxus harringtonia var. fastigiata | Alkaloid | JAK1-STAT3 | Non-small cell lung cancer [49] |
| Myricetin | Myrica rubra (Lour.) Siebold & Zucc | Isoflavonoid | JAK1-STAT3 | Inflammatory responses, Cancer [49] |
| Ellagic Acid | Rubus cochinchinensis Tratt. | Polyphenol | JAK1/JAK2-STAT1-NOX4 | Renal ischemic-reperfusion injury [49] |
These natural compounds offer diverse chemical scaffolds distinct from synthetic JAK inhibitors, potentially enabling the development of agents with novel binding modes and improved safety profiles. The structural diversity of natural products may facilitate optimization of selectivity patterns that differ from conventional ATP-competitive inhibitors, possibly through allosteric mechanisms or stabilization of unique kinase conformations [49].
Experimental Approaches and Methodologies
Target Validation and Selectivity Profiling
Rigorous assessment of target engagement and selectivity is paramount in the development of next-generation JAK inhibitors. The following experimental approaches represent state-of-the-art methodologies for characterizing novel JAK inhibitors:
Kinase Selectivity Profiling: Comprehensive screening against panels of recombinant human kinases (typically >300 kinases) is essential to establish selectivity profiles. This is performed using biochemical assays that measure the inhibition of kinase activity through various detection methods, including radioactivity, fluorescence polarization, time-resolved fluorescence resonance energy transfer (TR-FRET), or mobility shift assays. The resulting selectivity scores (such as S(10) or S(35) values) quantify the number of kinases inhibited with less than 10-fold or 35-fold selectivity compared to the primary target [44].
Cellular Target Engagement: Assessment of target engagement in physiologically relevant cellular systems is conducted through phospho-flow cytometry or Western blot analysis of STAT phosphorylation following cytokine stimulation. For example, IL-6-induced STAT3 phosphorylation evaluates JAK1 inhibition, while EPO-induced STAT5 phosphorylation assesses JAK2 inhibition. The differential effects on these signaling pathways establish the functional selectivity of inhibitors in cellular contexts [44] [36].
Crystallographic Studies: X-ray crystallography of JAK-inhibitor complexes provides atomic-level resolution of binding interactions and informs structure-based drug design efforts. Recent determination of the full-length JAK1 structure complexed with the intracellular domain of a cytokine receptor has revealed extended structural units that facilitate dimerization of the cytokine receptor/JAK complex, offering new insights for allosteric inhibitor development [79].
In Vitro and In Vivo Disease Modeling
Advanced disease models are essential for evaluating the therapeutic potential of next-generation JAK inhibitors in pathophysiologically relevant contexts:
Immune Cell Functional Assays: Primary human immune cell cultures (T cells, B cells, monocytes, dendritic cells) stimulated with specific cytokines (IL-6, IL-12, IL-23, IFNs) are used to assess the functional consequences of JAK inhibition on immune cell activation, proliferation, and differentiation. For example, Th17 cell differentiation assays measure the effect of JAK inhibitors on IL-23-driven expansion of this pathogenic T-cell subset [27].
3D Skin Equivalents and Tissue Models: Reconstituted human skin models incorporating keratinocytes, fibroblasts, and immune cells provide physiologically relevant systems for evaluating JAK inhibitors in dermatological indications such as atopic dermatitis, psoriasis, and alopecia areata. These models recapitulate key aspects of disease pathophysiology, including epidermal barrier dysfunction, cytokine production, and immune cell infiltration [80] [49].
Xenograft Models of Autoimmunity: The AA mouse model, involving grafting of lesional skin from human alopecia areata patients onto mouse hosts, has been instrumental in validating JAK inhibition as a therapeutic strategy for this condition [80]. Treatment with JAK inhibitors in this model prevented the upregulation of CD8+ NKG2D+ T cells and onset of AA, providing preclinical proof-of-concept that supported subsequent clinical development [80].
Diagram 2: Integrated workflow for the development and validation of next-generation JAK inhibitors, encompassing target identification, compound optimization, and preclinical validation stages.
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Table 3: Key Research Reagent Solutions for JAK-STAT Pathway Investigation
| Reagent/Method | Function/Application | Key Considerations |
|---|---|---|
| Recombinant JAK Kinases | Biochemical kinase assays for inhibitor screening and selectivity profiling | Available from multiple vendors (e.g., Invitrogen, MilliporeSigma); essential for establishing initial potency and selectivity [44] |
| Phospho-Specific STAT Antibodies | Detection of STAT phosphorylation in cellular systems by Western blot, flow cytometry, or immunofluorescence | Critical for assessing functional target engagement; antibodies available for all STAT family members [36] [1] |
| Cytokine-Specific Cellular Assays | Evaluation of inhibitor effects on specific cytokine signaling pathways | IL-6 for JAK1/2; IL-4 for JAK1/3; IL-12 for TYK2/JAK2; GM-CSF for JAK2 [44] [27] |
| JAK-Reporter Cell Lines | High-throughput screening of JAK inhibitor compounds | Engineered cells with STAT-responsive elements driving luciferase or fluorescent reporters [36] |
| Primary Immune Cell Cultures | Assessment of inhibitor effects in physiologically relevant human cell systems | Peripheral blood mononuclear cells (PBMCs), T cells, B cells, monocytes; maintain native signaling context [27] |
| 3D Tissue Models | Evaluation of JAK inhibitors in tissue-relevant contexts | Reconstituted human skin models, synovial tissue models; recapitulate cell-cell interactions [80] [49] |
The field of JAK-STAT pathway modulation is evolving rapidly toward next-generation inhibitors with enhanced selectivity, novel mechanisms of action, and improved therapeutic indices. The expanding pipeline of clinical candidates reflects multiple innovative approaches, including isoform-selective inhibition, dual-specificity targeting, covalent inhibition, and natural product-derived compounds. These advancements are complemented by sophisticated experimental methodologies for target validation and compound optimization.
Future directions in JAK inhibitor development will likely focus on several key areas: First, the continued refinement of selectivity profiles to precisely target disease-relevant signaling nodes while sparing homeostatic functions. Second, the development of tissue-specific targeting strategies to enhance local efficacy while minimizing systemic exposure. Third, the exploration of allosteric and non-ATP-competitive inhibition mechanisms to overcome limitations of conventional active-site inhibitors. Finally, the integration of JAK inhibitors with complementary therapeutic modalities to address complex disease pathophysiology through rational combination approaches.
As our understanding of JAK-STAT biology continues to evolve, particularly regarding pathway regulation, non-canonical signaling, and context-dependent functions, new opportunities for therapeutic intervention will undoubtedly emerge. The next generation of JAK-targeted therapies holds significant promise for improving outcomes across a spectrum of immune-mediated diseases while addressing the limitations of current standard-of-care treatments.
Clinical Evidence and Comparative Analysis of JAK-Targeted Therapies
The Janus kinase-signal transducer and activator of transcription (JAK-STAT) pathway serves as a fundamental signaling cascade that transmits information from extracellular cytokines directly to the nucleus, regulating gene expression for critical processes including immune cell differentiation, proliferation, and inflammatory responses [9]. This pathway, comprising cytokines, receptors, JAK enzymes (JAK1, JAK2, JAK3, TYK2), and STAT transcription factors, represents a paradigm for signal transduction from the extracellular environment to the genetic regulatory machinery [9]. In autoimmune pathologies such as rheumatoid arthritis (RA) and ulcerative colitis (UC), dysregulation of the JAK-STAT pathway drives sustained inflammation and tissue damage through excessive cytokine signaling [26] [13]. This molecular understanding has positioned the JAK-STAT pathway as a compelling target for therapeutic intervention, leading to the development and clinical implementation of Janus kinase inhibitors (JAKinibs).
JAKinibs represent a class of small molecule therapeutics that target the intracellular kinase domain of JAK enzymes, thereby modulating the signaling of numerous cytokines implicated in autoimmune pathogenesis [9]. Their oral bioavailability and targeted mechanism offer distinct advantages over biologic therapies, though their relative efficacy and safety profiles require meticulous comparison to inform clinical decision-making [82]. Network meta-analysis (NMA) has emerged as a powerful statistical methodology for comparing multiple interventions simultaneously, even in the absence of head-to-head randomized controlled trials (RCTs) [83]. This technical guide explores the application of NMA methodologies to evaluate the comparative efficacy and safety of JAKinibs across autoimmune diseases, providing researchers and drug development professionals with advanced tools for evidence synthesis.
JAK-STAT Pathway Architecture and Relevance to Autoimmune Diseases
Molecular Architecture and Signaling Mechanism
The JAK-STAT pathway operates through a precisely orchestrated sequence of molecular events. Cytokine binding induces receptor dimerization, bringing associated JAK proteins into proximity for trans-phosphorylation and activation. These activated JAKs then phosphorylate tyrosine residues on cytokine receptors, creating docking sites for STAT proteins. Upon recruitment, STATs are phosphorylated by JAKs, form dimers, and translocate to the nucleus where they regulate transcription of target genes [9]. The specificity of signaling is achieved through selective pairing of JAK isoforms (JAK1, JAK2, JAK3, TYK2) with different cytokine receptors and preferential activation of particular STAT family members (STAT1-6), creating a sophisticated regulatory network for immune homeostasis [9].
Pathway Dysregulation in Autoimmune Pathology
In autoimmune conditions, chronic inflammation is perpetuated by persistent activation of the JAK-STAT pathway. Research in ulcerative colitis has demonstrated significantly increased phosphorylation of JAK2, JAK3, TYK2, STAT1, STAT3, and STAT4 in inflamed colonic mucosa compared to non-inflamed tissue [26] [13]. Notably, coordinated activation patterns among JAK2, JAK3, TYK2, and STAT3 suggest interdependent roles in driving intestinal inflammation [13]. Furthermore, sex-dependent differences in pathway activation have been observed, with male UC patients exhibiting significantly higher activation of JAK2 and STAT3 than females, highlighting the importance of personalized therapeutic approaches [13]. Similar pathway dysregulation occurs in rheumatoid arthritis, where multiple cytokines implicated in disease pathogenesis (including IL-6, IFNs, and common gamma-chain cytokines) signal through JAK-STAT mechanisms [82] [83].
Diagram: JAK-STAT Signaling Pathway and JAKinib Therapeutic Inhibition. The illustration depicts cytokine-mediated activation of JAK-STAT signaling and the site of therapeutic intervention by JAK inhibitors, which target intracellular JAK proteins to modulate downstream inflammatory gene expression.
Network Meta-Analysis Methodology for JAKinib Comparisons
Fundamental Principles of Network Meta-Analysis
Network meta-analysis extends conventional pairwise meta-analysis by simultaneously synthesizing evidence from multiple treatment comparisons across a network of randomized controlled trials [83]. This methodology enables both direct comparisons (within trials) and indirect comparisons (across trials connected through common comparators), providing a comprehensive framework for ranking multiple interventions [82] [83]. For JAKinib evaluations, NMA is particularly valuable given the multitude of approved agents (tofacitinib, baricitinib, upadacitinib, filgotinib, peficitinib) and the scarcity of head-to-head clinical trials directly comparing all agents [83].
The statistical foundation of NMA relies on the consistency assumption, which posits that direct and indirect evidence are in agreement, allowing for valid mixed treatment comparisons [82]. Frequentist approaches implement NMA using multivariate meta-analysis models that account for the correlation structure induced by multiple treatments comparisons within trials [82]. The netmeta package in R is commonly employed for frequentist NMA, providing comprehensive tools for network visualization, effect estimation, and inconsistency assessment [82] [84].
Component Network Meta-Analysis for Complex Interventions
Component network meta-analysis (CNMA) represents an advanced extension of standard NMA particularly relevant for evaluating complex interventions like JAKinib therapy combinations [85]. Unlike conventional NMA that treats each unique treatment combination as a distinct node, CNMA models the individual components (e.g., specific JAKinibs, background therapies) and their additive or interactive effects [85]. This approach offers several advantages: increased precision through sharing information across treatment combinations, ability to predict effects of untested combinations, and identification of components driving efficacy [85].
CNMA models range from simple additive models (where combination effects equal the sum of component effects) to complex interaction models accounting for synergistic or antagonistic effects between components [85]. For JAKinib analyses, CNMA can elucidate whether specific JAKinibs demonstrate enhanced efficacy when combined with conventional synthetic disease-modifying antirheumatic drugs (csDMARDs) compared to monotherapy [83].
Data Collection and Quality Assessment
Comprehensive literature searches across multiple databases (e.g., PubMed, EMBASE, Cochrane Library, ClinicalTrials.gov) form the foundation of robust NMA [82] [83]. Search strategies should incorporate all approved JAKinibs (tofacitinib, baricitinib, upadacitinib, filgotinib, peficitinib) and their common brand names and research codes [83]. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines provide a structured framework for conducting and reporting systematic reviews that underpin NMA [86].
Quality assessment of included studies typically employs the Cochrane Risk of Bias tool for randomized trials, evaluating domains such as random sequence generation, allocation concealment, blinding, incomplete outcome data, and selective reporting [82]. For observational studies included in safety analyses, the Newcastle-Ottawa Scale provides a validated quality assessment instrument [86].
Diagram: Network Meta-Analysis Workflow for JAKinib Comparisons. The flowchart outlines the sequential phases of conducting an NMA, from systematic literature review through statistical analysis to result interpretation and reporting.
Comparative Efficacy of JAKinibs in Rheumatoid Arthritis
Efficacy Outcomes and Measurement Instruments
The efficacy of JAKinibs in rheumatoid arthritis is predominantly assessed using the American College of Rheumatology response criteria (ACR20, ACR50, ACR70), which measure the percentage of patients achieving 20%, 50%, or 70% improvement in both tender and swollen joint counts plus improvement in at least three of five other core set measures [83]. The Disease Activity Score using 28 joints with C-reactive protein (DAS28-CRP) provides a continuous measure of disease activity, with remission defined as DAS28-CRP < 2.6 [83]. These validated instruments enable standardized efficacy comparisons across clinical trials and facilitate NMA.
NMA Findings on JAKinib Efficacy
Recent network meta-analyses have synthesized evidence from numerous randomized controlled trials to compare the efficacy of approved JAKinibs. The table below summarizes key efficacy findings from comprehensive NMAs in moderate-to-severe rheumatoid arthritis:
Table 1: Comparative Efficacy of JAKinibs in Rheumatoid Arthritis from Network Meta-Analyses
| Treatment Regimen | ACR50 at 12-24 weeks (RR vs placebo) | ACR70 at 12-24 weeks (RR vs placebo) | DAS28-CRP <2.6 at 12-24 weeks (RR vs placebo) | SUCRA Ranking (Efficacy) |
|---|---|---|---|---|
| Upadacitinib 30 mg + csDMARD | 7.47 (95% CI: 2.02-18.13) [83] | 18.13 (95% CI: 2.68-122.68) [83] | 7.09 (95% CI: 2.70-18.62) [83] | Highest [83] |
| Upadacitinib 15 mg + csDMARD | 6.85 (95% CI: 4.80-9.78) [83] | 14.21 (95% CI: 7.94-25.43) [83] | 6.45 (95% CI: 4.32-9.63) [83] | High [83] |
| Baricitinib 4 mg + csDMARD | 5.92 (95% CI: 4.39-7.98) [83] | 11.32 (95% CI: 6.83-18.76) [83] | 5.12 (95% CI: 3.58-7.32) [83] | High [83] |
| Decernotinib 300 mg | 7.55 (95% CI: 3.48-16.39) [82] | Not reported | Not reported | High (ACR50) [82] |
| Filgotinib 200 mg + csDMARD | 4.68 (95% CI: 3.32-6.60) [83] | 8.12 (95% CI: 4.61-14.31) [83] | 4.35 (95% CI: 2.89-6.55) [83] | Moderate [83] |
| Tofacitinib 5 mg + csDMARD | 4.25 (95% CI: 3.22-5.61) [83] | 7.01 (95% CI: 4.37-11.24) [83] | 3.89 (95% CI: 2.78-5.44) [83] | Moderate [83] |
| Peficitinib 150 mg + csDMARD | 3.75 (95% CI: 2.45-5.74) [83] | 5.89 (95% CI: 3.13-11.09) [83] | 3.42 (95% CI: 2.07-5.66) [83] | Moderate [83] |
RR: Risk Ratio; CI: Confidence Interval; SUCRA: Surface Under the Cumulative Ranking Curve
NMAs consistently demonstrate that all JAKinibs show superior efficacy to placebo across multiple outcome measures [82] [83]. Upadacitinib regimens (particularly 30 mg and 15 mg) and baricitinib 4 mg consistently rank highest for efficacy outcomes, with upadacitinib 15 mg + csDMARD and baricitinib 4 mg + csDMARD showing robust performance at 24-week assessments [83]. The surface under the cumulative ranking curve (SUCRA) values provide a numerical representation of relative ranking, with higher values (closer to 1) indicating better performance [82] [83].
Combination therapy with csDMARDs (typically methotrexate) generally enhances JAKinib efficacy compared to monotherapy regimens, supporting current treatment guidelines that recommend combination approaches for optimal disease control [83]. This observation aligns with the multifactorial pathogenesis of RA, where targeting multiple inflammatory pathways simultaneously may yield superior clinical outcomes.
Safety Considerations in JAKinib Therapy
Comparative Safety Profiles of JAKinibs
Safety represents a critical consideration in JAKinib therapy, particularly following regulatory concerns based on the ORAL Surveillance trial, which identified increased cardiovascular and malignancy risks with tofacitinib in high-risk RA patients [86]. Subsequent NMAs have provided broader perspectives on JAKinib safety across diverse patient populations. The table below summarizes key safety findings from recent comparative analyses:
Table 2: Comparative Safety Profiles of JAKinibs from Network Meta-Analyses
| Safety Outcome | JAKinibs with Favorable Profile | JAKinibs with Increased Risk | Comparative Findings vs TNF Antagonists |
|---|---|---|---|
| Serious Infections | Filgotinib 100 mg (RR = 0.40, 95% CI: 0.21-0.79) [82] | Not significantly different among most JAKinibs [82] | No meaningful difference (HR = 1.05, 95% CI: 0.97-1.13) [86] |
| Herpes Zoster | Tofacitinib 1 mg BID (RR = 0.80, 95% CI: 0.65-0.99) [82] | Baricitinib 4 mg (RR = 4.79, 95% CI: 1.03-22.21) [82] | Not specifically reported in comparative meta-analysis [86] |
| Venous Thromboembolism | Not specifically identified | JAKinib class (HR = 1.26, 95% CI: 1.03-1.54 vs TNF antagonists) [86] | Slightly higher with JAK inhibitors (IR = 0.57 vs 0.52 per 100 person-years) [86] |
| Major Adverse Cardiovascular Events | No significant differences among JAKinibs [83] | No significant differences among JAKinibs [83] | No meaningful difference (HR = 0.91, 95% CI: 0.80-1.04) [86] |
| Malignant Neoplasms | No significant differences among JAKinibs [83] | No significant differences among JAKinibs [83] | No meaningful difference (HR = 1.02, 95% CI: 0.90-1.16) [86] |
| Adverse Drug Reactions | Tofacitinib 1 mg BID (RR = 0.80, 95% CI: 0.65-0.99) [82] | Not specifically identified | Not specifically reported |
HR: Hazard Ratio; IR: Incidence Rate
Recent comprehensive meta-analyses of head-to-head comparative effectiveness studies have challenged strict regulatory guidance that restricted JAKinib use after TNF antagonist failure, finding no meaningful differences in risk of serious infections, malignant neoplasms, or major adverse cardiovascular events between JAK inhibitors and TNF antagonists across immune-mediated inflammatory diseases [86]. The overall incidence of serious adverse events remains low for both treatment classes [86].
Dose-Dependent Safety Considerations
Safety profiles demonstrate dose dependence for several JAKinibs. Lower doses (e.g., tofacitinib 1 mg twice daily) show favorable adverse event profiles, while higher doses (e.g., baricitinib 4 mg) associate with increased herpes zoster reactivation risk [82]. This dose-response relationship underscores the importance of individualized dosing strategies that balance efficacy and safety, particularly in patients with specific risk factors.
Experimental Approaches for JAK-STAT Pathway Analysis
Methodologies for Assessing Pathway Activation
Comprehensive evaluation of JAK-STAT pathway activation employs multiple technical approaches to quantify protein phosphorylation and functional activity. Recent research in ulcerative colitis provides a representative methodological framework applicable across autoimmune diseases [26] [13]. The experimental workflow typically involves tissue collection from both inflamed and non-inflamed regions, protein extraction under conditions that preserve phosphorylation states, and quantitative assessment of pathway components through Western blotting with phospho-specific antibodies [13].
Standardized sample processing is critical for reliable phosphoprotein analysis. Mechanical digestion in lysis buffer supplemented with protease and phosphatase inhibitors preserves phosphorylation patterns, while protein concentration normalization ensures comparable loading across samples [13]. Western blot methodologies employing sequential stripping and reprobing enable comprehensive analysis of multiple phosphorylated proteins from limited tissue samples, maximizing data yield from precious clinical specimens [13].
Research Reagent Solutions for JAK-STAT Analysis
Table 3: Essential Research Reagents for JAK-STAT Pathway Analysis
| Reagent Category | Specific Examples | Research Application | Technical Considerations |
|---|---|---|---|
| Phospho-Specific Antibodies | Anti-phospho-JAK2, anti-phospho-STAT3 [13] | Detection of activated pathway components | Validation using defined positive controls; specificity confirmation through molecular weight verification [13] |
| Protein Extraction Reagents | Tris-based lysis buffer with protease/phosphatase inhibitors [13] | Preservation of native phosphorylation states | Mechanical digestion with sonication; immediate stabilization at -80°C [13] |
| Detection Systems | HRP-linked secondary antibodies with ECL substrate [13] | Signal amplification and visualization | Linear range determination; appropriate exposure times to prevent saturation [13] |
| Normalization Controls | β-actin [13] | Protein loading normalization | Validation of consistent expression across experimental conditions [13] |
| Cell Line Controls | Cytokine-stimulated cell lines [13] | Antibody validation and experimental controls | Generation of defined phosphorylation signals for method optimization [13] |
These methodological approaches enable robust quantification of JAK-STAT pathway activation in patient-derived samples, facilitating correlation between pathway activity and clinical responses to JAKinib therapy. The identification of sex-dependent activation patterns for JAK2 and STAT3 highlights the importance of considering biological variables in experimental design and data interpretation [13].
Advanced Visualization Techniques for Network Meta-Analysis
Innovative Approaches for Complex Evidence Structures
Visualization represents a critical component of NMA, enabling researchers to comprehend complex evidence networks and communicate findings effectively. Traditional network diagrams illustrate treatment comparisons but become limited with numerous interventions and complex connections [85]. Innovative visualization approaches address these limitations:
CNMA-UpSet Plots efficiently display intervention combinations in networks with large numbers of components, clearly illustrating which component sets have been evaluated in clinical trials [85]. These plots enhance understanding of evidence structure for component NMAs, identifying evidence gaps and informing model selection.
CNMA Heat Maps visualize the distribution of component combinations across trials, facilitating decisions about which pairwise interactions to include in CNMA models [85]. Heat maps can reveal clustering patterns and identify components that always co-occur, which may present identifiability challenges in additive effects models.
CNMA-Circle Plots illustrate component combinations that differ between trial arms, offering flexibility for presenting additional information such as patient numbers or outcome events [85]. These plots enhance comprehension of the experimental designs employed across the evidence base.
Interactive Visualization Tools
Interactive platforms such as Shiny apps transform static NMA visualizations into dynamic exploration tools, allowing researchers to adjust parameters and instantly visualize effects on model results [87]. These tools enable real-time exploration of heterogeneity, subgroup effects, and network geometry, facilitating deeper understanding of complex evidence structures [87].
MetaInsight, a freely accessible web application, provides comprehensive NMA implementation without requiring advanced programming expertise, supporting both frequentist and Bayesian analytical approaches [84]. The platform incorporates advanced visualization capabilities including network diagrams, forest plots, and rankograms, enhancing accessibility of sophisticated NMA methodologies to broader research communities [84].
Network meta-analysis provides a powerful methodological framework for comparing the efficacy and safety of JAKinibs across autoimmune diseases, overcoming limitations posed by the scarcity of head-to-head clinical trials. Synthetic evidence from NMAs demonstrates consistent superiority of JAKinibs over placebo, with differentiation in efficacy rankings favoring upadacitinib and baricitinib regimens, particularly when combined with csDMARDs [82] [83]. Safety profiles exhibit both class effects and agent-specific characteristics, informing risk-benefit assessments tailored to individual patient characteristics [82] [86].
Future methodological advancements will likely include the integration of component network meta-analysis to deconstruct complex treatment regimens, enhanced visualization approaches for communicating multidimensional evidence structures, and the incorporation of real-world evidence to complement RCT findings [85]. As understanding of JAK-STAT biology deepens, particularly regarding tissue-specific and sex-dependent activation patterns, NMAs will increasingly inform personalized therapeutic selection optimized for individual patient pathophysiology [13]. The ongoing evolution of JAKinib therapeutics and analytical methodologies ensures that network meta-analysis will remain an indispensable tool for evidence-based drug development and clinical decision-making in autoimmune diseases.
The Janus kinase-signal transducers and activators of transcription (JAK-STAT) pathway serves as a pivotal signaling cascade in the regulation of immune homeostasis and inflammatory responses. This pathway functions as the primary intracellular mechanism for over 50 cytokines, growth factors, and hormones, positioning it at the nexus of numerous inflammatory signaling networks. Inflammatory triggers such as interleukins (IL-4, IL-13, IL-31) bind to cell surface receptors that lack intrinsic enzymatic activity, instead relying on associated JAK enzymes (JAK1, JAK2, JAK3, TYK2) for intracellular signal propagation. Subsequent tyrosine phosphorylation of STAT proteins enables their dimerization and nuclear translocation, where they directly regulate gene expression of key inflammatory mediators [88].
The central role of JAK-STAT signaling in immunoinflammatory cascades has made it an attractive therapeutic target for immune-mediated inflammatory diseases (IMIDs). JAK inhibitors are small molecules that competitively bind to the adenosine triphosphate (ATP)-binding domain of JAK enzymes, thereby preventing tyrosine phosphorylation and subsequent STAT activation [88]. This mechanism fundamentally differs from biologic therapies such as tumor necrosis factor-alpha (TNF-α) inhibitors, which target extracellular cytokines. The intracellular targeting approach of JAK inhibitors allows for broader modulation of multiple cytokine pathways while maintaining administration flexibility through oral formulations.
Recent clinical evidence and regulatory decisions have highlighted the necessity for comprehensive safety evaluations of JAK inhibitors relative to established biologic therapies. This technical analysis systematically examines the comparative safety profiles of JAK inhibitors versus TNF antagonists across diverse IMID populations, with particular emphasis on head-to-head comparative effectiveness studies and their implications for targeted therapeutic intervention in inflammatory signaling pathways.
Methodological Framework for Comparative Safety Assessment
Systematic Literature Search and Study Selection Criteria
The evidence synthesis presented in this whitepaper derives from a rigorous methodological framework adapted from recent high-quality systematic reviews and meta-analyses. The foundational search strategy encompassed major biomedical databases including Ovid Medline, Ovid EMBASE, and Web of Science from inception through June 2025 [86]. Additional specialized searches focused on real-world evidence from clinical registries and pharmacovigilance studies were incorporated to complement randomized trial data.
The study selection process employed PICOS criteria (Participants, Interventions, Comparators, Outcomes, Study design) with the following specifications:
- Participants: Adults (≥18 years) with diagnosed IMIDs including rheumatoid arthritis (RA), inflammatory bowel disease (IBD), psoriasis or psoriatic arthritis (PsO/PsA), and spondyloarthropathy
- Interventions: JAK inhibitors (tofacitinib, baricitinib, upadacitinib, filgotinib) at therapeutic doses
- Comparators: TNF antagonists (infliximab, adalimumab, etanercept, certolizumab, golimumab)
- Outcomes: Primary safety endpoints included serious infections, malignant neoplasms, major adverse cardiovascular events (MACE), and venous thromboembolism (VTE)
- Study designs: Head-to-head comparative effectiveness studies with adjusted analyses, excluding randomized clinical trials, noncomparative observational studies, and studies with sample sizes <500 [86]
Data Extraction and Quality Assessment Protocol
Standardized data extraction forms captured study characteristics, patient demographics, treatment regimens, outcome definitions, and statistical adjustments. Four investigators independently abstracted data in duplicate pairs to ensure accuracy [86]. The Newcastle-Ottawa Scale was applied for quality assessment of observational studies, evaluating selection, comparability, and outcome ascertainment [86].
For quantitative synthesis, adjusted hazard ratios (HRs) with 95% confidence intervals (CIs) were prioritized. When adjusted HRs were unavailable, unadjusted incidence rate ratios (IRRs) were calculated from reported event rates. Statistical heterogeneity was quantified using the I² statistic, with values <30%, 30%-60%, and >60% representing minimal, moderate, and substantial heterogeneity, respectively [86]. Random-effects models accounting for between-study variance were employed for all meta-analyses.
Statistical Analysis Plan for Safety Outcomes
The analytic approach employed inverse-variance weighted random-effects meta-analysis to calculate pooled hazard ratios for safety outcomes comparing JAK inhibitors versus TNF antagonists. Incidence rates (IRs) per 100 person-years were calculated for each treatment group to facilitate absolute risk interpretation [86]. Pre-specified subgroup analyses examined effect modification by:
- IMID type (RA, IBD, PsO/PsA, SpA)
- Specific JAK inhibitor molecule
- Geographic region
- Age stratification
- Concomitant immunosuppressive use
- Study period relative to regulatory safety warnings
Meta-regression techniques explored the influence of study-level covariates including median age, sex distribution, comorbidity burden, and calendar time. Sensitivity analyses assessed robustness by excluding studies without adequate adjustment for key confounders. All analyses were conducted using R statistical software (version 4.2.0) with the metafor package for effect size aggregation [86].
Comparative Safety Profiles: Quantitative Analysis
Major Adverse Cardiovascular Events (MACE) and Venous Thromboembolism (VTE)
The cardiovascular safety profile of JAK inhibitors has been extensively evaluated following signals from the ORAL Surveillance trial, which found increased cardiovascular risk with tofacitinib versus TNF inhibitors in high-risk RA patients [86]. Contemporary meta-analyses of head-to-head comparative studies provide more nuanced insights across broader IMID populations.
Table 1: Cardiovascular and Thromboembolic Safety Profiles of JAK Inhibitors vs. TNF Antagonists
| Safety Outcome | JAK Inhibitor Incidence (per 100 person-years) | TNF Antagonist Incidence (per 100 person-years) | Pooled Hazard Ratio [95% CI] | Heterogeneity (I²) |
|---|---|---|---|---|
| MACE | 0.72 [0.56-0.92] | 0.66 [0.49-0.89] | 0.91 [0.80-1.04] | Minimal to Moderate |
| Myocardial Infarction | - | - | 0.89 [0.63-1.25]* | - |
| Venous Thromboembolism | 0.57 [0.40-0.82] | 0.52 [0.37-0.73] | 1.26 [1.03-1.54] | Minimal to Moderate |
| Stroke | - | - | No significant difference | - |
*Data from JAK-pot collaboration [89]
A comprehensive meta-analysis of 42 studies encompassing 813,881 patients with IMIDs demonstrated no significant difference in MACE risk between JAK inhibitors and TNF antagonists (HR 0.91, 95% CI 0.80-1.04) [86]. The incidence rates were low in both treatment groups (0.72 vs. 0.66 per 100 person-years) [86]. Real-world evidence from the JAK-pot collaboration, which included 51,233 patients across 15 registries, similarly found comparable MACE rates between JAK inhibitors and TNF inhibitors (incidence rate ratio [IRR] 0.89, 95% CI 0.63-1.25) [89].
In contrast, VTE risk was modestly elevated with JAK inhibitors compared to TNF antagonists (HR 1.26, 95% CI 1.03-1.54), though absolute incidence rates remained low (0.57 vs. 0.52 per 100 person-years) [86]. This represents a 26% relative risk increase with narrow confidence intervals crossing unity, suggesting the need for careful consideration in patients with pre-existing thromboembolic risk factors.
Malignancy and Serious Infection Risks
The oncological safety of immunomodulatory therapies remains a paramount concern in treatment selection for chronic IMIDs. The quantitative synthesis of malignancy and infection risks provides critical insights for benefit-risk assessment.
Table 2: Malignancy and Infection Risks: JAK Inhibitors vs. TNF Antagonists
| Safety Outcome | JAK Inhibitor Incidence (per 100 person-years) | TNF Antagonist Incidence (per 100 person-years) | Pooled Hazard Ratio [95% CI] | Heterogeneity (I²) |
|---|---|---|---|---|
| Malignant Neoplasms | 1.00 [0.77-1.31] | 0.94 [0.72-1.22] | 1.02 [0.90-1.16] | Minimal to Moderate |
| Serious Infections | 3.79 [2.85-5.05] | 3.03 [2.32-3.95] | 1.05 [0.97-1.13] | Minimal to Moderate |
| Herpes Zoster | - | - | Significantly increased^ | - |
^Based on real-world studies [88] [90]
The meta-analysis of head-to-head studies demonstrated comparable risks for malignant neoplasms between JAK inhibitors and TNF antagonists (HR 1.02, 95% CI 0.90-1.16) with nearly identical incidence rates (1.00 vs. 0.94 per 100 person-years) [86]. Similarly, serious infection risk was not significantly different between treatment classes (HR 1.05, 95% CI 0.97-1.13), though absolute incidence was notably higher for both endpoints (3.79 vs. 3.03 per 100 person-years) [86].
Real-world evidence from a multicenter retrospective cohort study of 685 patients receiving JAK inhibitors revealed herpes zoster as a particularly notable risk, with other adverse events of special interest (AESI) occurring in 18% of patients over 1,137 patient-years of observation [90]. Importantly, this study documented only one stroke and three deaths (all infection-related) in this cohort, suggesting an overall favorable safety profile in unselected clinical populations [90].
Safety in Specific Inflammatory Dermatoses
The application of JAK inhibitors in inflammatory dermatoses warrants specialized consideration of both systemic and cutaneous safety profiles. A systematic review and meta-analysis of real-world evidence in atopic dermatitis encompassing 50 studies demonstrated favorable effectiveness, with Eczema Area and Severity Index (EASI)-75 response rates reaching 59% at 12 weeks and 86% at 52 weeks [43].
The safety profile in dermatologic applications demonstrated characteristic patterns, with the most frequent adverse events being acne (16%), increased creatine phosphokinase (13%), and elevated lipids (12%) [43]. These findings highlight both class-effects and molecule-specific considerations for JAK inhibitor use in dermatologic practice, particularly regarding laboratory monitoring requirements and anticipatory management of cutaneous adverse events.
Molecular Mechanisms and Signaling Pathway Implications
JAK-STAT Signaling Architecture and Inhibitor Specificity
The JAK-STAT pathway represents a sophisticated intracellular communication system that translates extracellular cytokine signals into targeted gene expression programs. Understanding the structural basis of JAK inhibitor specificity is essential for interpreting their differential safety profiles.
JAK inhibitors function through competitive inhibition of the ATP-binding cavity within the kinase domain of JAK enzymes [88]. This mechanism prevents the phosphorylation and activation of downstream STAT transcription factors. The specificity profiles of different JAK inhibitors create distinct therapeutic and safety implications:
- Upadacitinib: Selective JAK1 inhibitor with minimal JAK2 interaction, potentially explaining its favorable hematological safety profile [88]
- Baricitinib: JAK1/JAK2 inhibitor with implications for interferon signaling and hematopoietic parameters [88]
- Tofacitinib: Pan-JAK inhibitor affecting JAK1, JAK2, and JAK3, associated with broader immunomodulatory effects [88]
- Deucravacitinib: Selective TYK2 inhibitor with a unique allosteric binding mechanism, potentially explaining its distinct safety profile [88]
The varying selectivity profiles across the JAK inhibitor class translate into differentiated effects on specific cytokine signaling pathways, potentially explaining the heterogeneous safety signals observed across molecules and indications.
Mechanistic Insights into Thrombotic Risk
The modestly elevated VTE risk observed with JAK inhibitors compared to TNF antagonists may derive from differential effects on coagulation homeostasis and endothelial function. Preclinical evidence suggests that JAK2 inhibition may influence platelet activation thresholds through modulation of thrombopoietin signaling, which operates predominantly through JAK2-STAT5 pathways [86]. Additionally, JAK1-dependent cytokines including IL-6 and IL-11 participate in the regulation of endothelial function and coagulation cascade activation.
The 26% relative risk increase for VTE with JAK inhibitors versus TNF antagonists must be interpreted in context of absolute risk, which remains low (0.57 vs. 0.52 events per 100 person-years) [86]. This translates to a number needed to harm (NNH) of approximately 2,000 patient-years for one additional VTE event with JAK inhibitors compared to TNF antagonists. This risk-benefit calculus favors individualized treatment decisions based on specific patient risk factors and anticipated therapeutic benefits.
Research Reagent Solutions for JAK-STAT Investigation
Table 3: Essential Research Tools for JAK-STAT Pathway and Inhibitor Profiling
| Research Reagent | Primary Application | Technical Specification | Research Utility |
|---|---|---|---|
| Phospho-STAT Flow Cytometry | STAT phosphorylation quantification | Antibodies against pSTAT1, pSTAT3, pSTAT5, pSTAT6 | Cellular signaling pathway activation assessment |
| JAK Inhibitor Profiling Panels | Kinase selectivity screening | Radioactive/fluorescence-based kinase assays | Determination of inhibitor specificity across kinome |
| Cytokine Stimulation Assays | Pathway activation potential | IL-4, IL-6, IL-13, IFN-γ at physiologic concentrations | Evaluation of JAK inhibitor potency in cellular contexts |
| ATP-Competitive Binding Assays | Mechanism of action confirmation | Fluorescence polarization or TR-FRET technologies | Direct assessment of JAK enzyme engagement |
| Multiplex Cytokine Profiling | Systemic immune monitoring | Luminex or electrochemiluminescence platforms | Comprehensive cytokine network analysis pre/post-treatment |
The experimental toolkit for JAK-STAT pathway analysis continues to evolve with technological advancements in molecular profiling. Critical methodologies for comprehensive safety assessment include:
Phospho-STAT flow cytometry enables single-cell resolution analysis of pathway activation across diverse immune cell populations. This technique employs phospho-specific antibodies against activated STAT proteins (pSTAT1, pSTAT3, pSTAT5, pSTAT6) to quantify signaling dynamics in response to cytokine stimulation with and without JAK inhibitor treatment [88].
Selectivity profiling panels utilize high-throughput kinase assays encompassing diverse members of the kinome to establish the specificity landscape of JAK inhibitors. These panels typically employ radioactive ATP-transfer or fluorescence resonance energy transfer (FRET) methodologies to quantify inhibitory potency (IC50 values) across hundreds of human kinases, establishing selectivity indices that predict off-target effects [88].
Functional immune cell assays measure downstream consequences of JAK inhibition on immune cell functions including T-cell proliferation, B-cell antibody production, and monocyte inflammatory cytokine secretion. These systems employ primary human cells or cell line models stimulated with relevant cytokines (IL-4, IL-6, IL-23, IFN-γ) to establish the functional immunomodulatory profile of each inhibitor [88].
Discussion: Implications for Targeted Therapy and Future Directions
Integration with Current Regulatory Frameworks
The accumulating evidence from head-to-head comparative effectiveness studies suggests a need to revisit regulatory guidance that restricts JAK inhibitor use across all indications. The current FDA labeling mandates JAK inhibitor use only after TNF antagonist failure or contraindication, reflecting safety concerns originating from the ORAL Surveillance trial [86]. However, contemporary meta-analyses demonstrate comparable safety profiles between these drug classes across most serious adverse event categories, with the exception of modestly elevated VTE risk with JAK inhibitors [86] [91].
The divergence between trial findings and real-world evidence may reflect fundamental differences in study populations. The ORAL Surveillance trial specifically enrolled older RA patients (≥50 years) with at least one additional cardiovascular risk factor [86]. In contrast, the broader IMID populations represented in recent meta-analyses and real-world studies include younger, healthier patients, potentially explaining the more favorable safety observations. This highlights the critical importance of population context in safety signal interpretation and clinical decision-making.
Future Research Priorities and Unanswered Questions
Several important research questions remain unresolved in the comparative safety profile of JAK inhibitors:
Long-term safety characterization beyond 2-5 years of follow-up remains limited for most JAK inhibitors, particularly in non-RA indications. Extended observational studies with appropriate comparator groups are needed to fully elucidate the temporal patterns of risk accumulation [86].
Molecule-specific differentiation within the JAK inhibitor class requires additional investigation. Current evidence is insufficient to definitively establish differentiated safety profiles among various JAK inhibitors, though mechanistic considerations suggest this likelihood [90]. Larger head-to-head studies or network meta-analyses could help clarify these potential differences.
Biomarker-driven risk stratification represents a promising frontier for personalized safety optimization. Potential biomarkers including baseline lipid profiles, inflammatory markers, and genetic polymorphisms in drug metabolism or thrombotic pathways may enable identification of patient subgroups with preferentially favorable benefit-risk profiles for JAK inhibitor versus TNF antagonist therapy [92].
The evolving landscape of JAK inhibitor safety evidence underscores the dynamic nature of therapeutic risk-benefit assessment in immunomodulatory therapy. Continued pharmacovigilance, thoughtful clinical trial design, and mechanistic research will further refine our understanding of how to optimally position these targeted therapies within the armamentarium for immune-mediated inflammatory diseases.
This systematic evaluation of JAK inhibitor safety profiles in comparison to TNF antagonists demonstrates generally comparable safety across most serious adverse event categories, with nuanced differentiation in specific risk domains. The evidence from head-to-head comparative effectiveness studies does not support broad-based safety restrictions across all JAK inhibitors and all patient populations. Rather, these findings advocate for individualized therapeutic decision-making that considers specific molecule characteristics, disease context, and patient-specific risk factors.
The modestly elevated VTE risk with JAK inhibitors warrants thoughtful patient selection and potential prophylaxis in high-risk scenarios, while the absence of significant differentiation in MACE, malignancy, and serious infection risks should reassure clinicians regarding the overall safety profile of this drug class. As the JAK-STAT signaling field continues to evolve, next-generation inhibitors with refined selectivity profiles and novel mechanisms of action will likely further optimize the therapeutic index of this important drug class for inflammatory disorders.
The Janus kinase/Signal Transducer and Activator of Transcription (JAK-STAT) pathway represents a critical signaling node in the pathogenesis of immune-mediated inflammatory diseases, including psoriatic arthritis (PsA). This ubiquitous pathway transduces signals from over 50 cytokines, growth factors, and hormones, ultimately regulating gene transcription and diverse cellular processes including proliferation, differentiation, and immune activation [13]. In PsA, dysregulation of this pathway leads to the production of pro-inflammatory cytokines and mediators that drive synovitis, enthesitis, dactylitis, and skin manifestations. The development of JAK inhibitors (JAKi) has introduced a targeted oral treatment strategy for PsA, modulating cytokine signaling at the intracellular level. This case study provides a comprehensive technical analysis of the efficacy and safety profiles of three JAK inhibitors—filgotinib, upadacitinib, and tofacitinib—within the framework of JAK-STAT pathway activation in inflammatory signaling research.
JAK-STAT Pathway Activation in Inflammatory Disease
Molecular Architecture and Signaling Dynamics
The JAK-STAT pathway comprises four JAK proteins (JAK1, JAK2, JAK3, TYK2) and seven STAT transcription factors (STAT1, STAT2, STAT3, STAT4, STAT5A, STAT5B, STAT6). In canonical signaling, cytokine binding induces receptor dimerization, bringing associated JAK proteins into proximity for trans-phosphorylation and activation. These activated JAKs then phosphorylate tyrosine residues on the receptor cytoplasmic tails, creating docking sites for STAT proteins via their Src homology 2 (SH2) domains. Once recruited, STATs are phosphorylated by JAKs on a single tyrosine residue, inducing dimerization through reciprocal SH2-phosphotyrosine interactions. These STAT dimers translocate to the nucleus where they bind specific DNA response elements to regulate target gene expression [13].
Recent research has elucidated non-canonical signaling modes, including STAT activation by non-tyrosine kinase receptors, unphosphorylated STAT functions, and STAT-independent JAK signaling. The specific combinatorial activation of JAK-STAT components creates signaling diversity, with different cytokine receptors preferentially activating distinct JAK and STAT combinations. For instance, cytokines signal predominantly through JAK1/JAK3 pairs, while JAK2 homodimers mediate signaling, and JAK1/TYK2 or JAK2/TYK2 combinations transduce and cytokine family signals [13].
Pathway Dysregulation in Psoriatic Arthritis
In PsA, sustained JAK-STAT activation creates a pro-inflammatory feedback loop. Inflamed tissues from patients with inflammatory conditions show significantly increased phosphorylation of JAK2, JAK3, TYK2, STAT1, STAT3, and STAT4 compared to non-inflamed mucosa, while JAK1 levels may not differ significantly [26] [13]. Correlation analyses reveal coordinated activation among JAK2, JAK3, TYK2, and STAT3, suggesting functionally interdependent roles in the inflammatory response [13].
Notably, male patients exhibit significantly higher activation of JAK2 and STAT3 than female patients, indicating sex-specific differences in pathway activation that may inform personalized therapeutic approaches [13]. This heterogeneous activation pattern underscores the complexity of targeting this pathway while highlighting opportunities for precision medicine.
The diagram below illustrates the core JAK-STAT signaling mechanism and its therapeutic inhibition:
Figure 1: JAK-STAT Signaling Pathway and Inhibition Mechanism. The diagram illustrates cytokine-mediated JAK-STAT activation and targeted inhibition by JAK inhibitors currently used in psoriatic arthritis treatment.
Comparative Efficacy Analysis of JAK Inhibitors in PsA
Network Meta-Analysis of Relative Efficacy
A recent network meta-analysis conducted in accordance with PRISMA-NMA and Cochrane methods provides direct comparisons between JAK inhibitors for PsA. This analysis included five randomized controlled trials encompassing 2,757 patients and evaluated multiple efficacy endpoints [93].
Table 1: Comparative Efficacy of JAK Inhibitors from Network Meta-Analysis
| Treatment Regimen | ACR20 Response vs Tofacitinib | Statistical Significance | Safety Profile |
|---|---|---|---|
| Filgotinib 200 mg OD | OR = 3.17 (95% CrI: 1.07-9.88) | Significantly higher | Most favorable safety profile |
| Upadacitinib 30 mg OD | OR = 2.34 (95% CrI: 1.13-4.78) | Significantly higher | Highest risk of adverse events |
| Upadacitinib 15 mg OD | Not superior | Comparable | Comparable to other regimens |
| Tofacitinib 5 mg BID | Reference | - | Intermediate risk |
OR: Odds Ratio; CrI: Credible Interval; OD: Once Daily; BID: Twice Daily [93]
The pairwise meta-analysis revealed that JAK inhibitors significantly increased American College of Rheumatology 20 (ACR20) score responses and Psoriasis Area and Severity Index 75 (PASI75) responses compared to placebo. The network meta-analysis further delineated the hierarchy between specific agents, demonstrating that filgotinib 200 mg once daily and upadacitinib 30 mg once daily had superior ACR20 responses compared to tofacitinib 5 mg twice daily [93].
Long-Term Efficacy Across Treatment Modalities
Upadacitinib has demonstrated sustained efficacy in long-term studies. The SELECT-PsA 1 trial, now with 5-year data (260 weeks), shows maintenance of clinical responses across multiple domains of PsA. At week 260, the proportions of patients achieving ACR20/50/70 responses or minimal disease activity (MDA) with upadacitinib 15 mg treatment were comparable to adalimumab, with less than 10% difference between groups [94]. Real-world evidence from the UPJOINT study confirms these findings, showing rapid treatment effects with MDA achievement as early as week 4 in both oligoarticular and polyarticular PsA subtypes. By week 24, 41.5% of patients overall achieved MDA (55.8% with oligoarticular PsA and 32.0% with polyarticular PsA), increasing to 47.5% and 35.1% respectively at week 48 [95] [96].
Tofacitinib demonstrates sustained efficacy to month 42 regardless of prior biologic DMARD treatment, though numerical differences favor biologic-naïve patients. Minimal disease activity and Psoriatic Arthritis Disease Activity Score response rates were numerically lower in TNF inhibitor-inadequate responders versus biologic-naïve patients, but rates of achieving a Health Assessment Questionnaire Disability Index score ≤0.5 and enthesitis/dactylitis resolution were similar between subgroups [97]. A separate analysis of patients directly switching from adalimumab to tofacitinib demonstrated maintained efficacy without a washout period, with similar ACR20/50/70 response rates between patients who switched versus those continuing tofacitinib [98].
Filgotinib showed robust efficacy in the Phase 2 EQUATOR trial, with 80% of patients on filgotinib 200mg once-daily achieving ACR20 at week 16 compared with 33% on placebo. The study also demonstrated significantly greater improvements in minimal disease activity (23% vs 9%) and individual disease components including skin psoriasis, enthesitis, and dactylitis [99]. Subgroup analyses showed consistent efficacy across baseline characteristics including sex, body mass index, disease duration, and prior TNF inhibitor exposure [100].
Table 2: Long-Term Efficacy Outcomes in Psoriatic Arthritis Clinical Trials
| Treatment | Study Duration | ACR20/50/70 | MDA Response | DAPSA Remission | Study Population |
|---|---|---|---|---|---|
| Upadacitinib 15 mg | 260 weeks (5 years) | Maintained from year 1 | Comparable to adalimumab | ~24% (oligoarticular) ~15% (polyarticular) | Inadequate response to ≥1 nbDMARD [94] [96] |
| Tofacitinib 5 mg BID | 42 months | Sustained in bDMARD-naïve and TNFi-IR | Numerically higher in bDMARD-naïve | Similar between subgroups | bDMARD-naïve and TNFi-IR [97] |
| Filgotinib 200 mg OD | 16 weeks (Phase 2) | 80% ACR20, 48% ACR50, 23% ACR70 | 23% vs 9% (placebo) | Not reported | Inadequate response to ≥1 cDMARD [99] |
Safety Profile Comparison
Adverse Event Spectra Across JAK Inhibitors
Safety considerations are paramount in JAK inhibitor therapy, with distinct risk profiles emerging across the class:
Upadacitinib safety data through 5 years of treatment show a generally consistent profile compared to adalimumab, though with some distinct characteristics. Rates of major adverse cardiovascular events (MACE), malignancy excluding non-melanoma skin cancer (NMSC), and venous thromboembolism (VTE) were low compared to historical comparators and generally similar across treatment groups. However, rates of serious infection, herpes zoster, anemia, lymphopenia, creatine phosphokinase elevation, and NMSC remained higher with upadacitinib versus adalimumab. The 30 mg dose was associated with higher rates of serious infection, herpes zoster, anemia, neutropenia, and CPK elevation compared to the 15 mg dose [94]. The network meta-analysis identified upadacitinib 30 mg as carrying the highest risk of adverse events among JAK inhibitors (OR = 1.80 vs placebo) [93].
Tofacitinib safety analyses reveal differential risk based on prior treatment exposure. In TNF inhibitor-inadequate responders versus biologic-naïve patients, treatment-emergent adverse event incidence rates were higher, and serious adverse events, serious infections, and herpes zoster incidence rates were numerically higher (though confidence intervals overlapped) [97]. The benefit-risk profile appears more favorable in biologic-naïve patients, likely reflecting their generally lower burden of comorbidities and shorter disease duration.
Filgotinib has demonstrated a favorable safety profile in clinical trials. In the EQUATOR trial, safety-related outcomes were similar between filgotinib and placebo arms, including rates of treatment-emergent adverse events (57% and 59%, respectively) and infections (22% and 21%). No deep venous thrombosis, pulmonary embolism, malignancies, gastrointestinal perforations, opportunistic infections/active tuberculosis, or cases of herpes zoster were reported in the core study period [99]. The network meta-analysis identified filgotinib as having the most favorable safety profile among JAK inhibitors [93].
Laboratory Monitoring Parameters
Treatment with JAK inhibitors requires monitoring of specific laboratory parameters:
- Hematological parameters: Lymphocyte, neutrophil, and hemoglobin counts should be monitored regularly due to potential decreases
- Hepatic enzymes: AST, ALT, and gamma glutamyl transferase should be tracked for potential elevations
- Lipid profiles: Increases in LDL cholesterol, HDL cholesterol, total cholesterol, and triglycerides may occur, typically within the first 6-12 weeks of treatment
- Creatine phosphokinase: Elevations have been observed, particularly with upadacitinib [94] [98]
Experimental Protocols for JAK-STAT Research
Assessment of Pathway Activation in Human Tissue
Research investigating JAK-STAT pathway activation in inflammatory diseases employs sophisticated molecular techniques:
Sample Collection and Processing: In a recent study of ulcerative colitis, paired biopsies were collected from inflamed and non-inflamed colonic mucosa during routine colonoscopy. Tissues underwent mechanical digestion and sonication in lysis buffer containing Tris, NaCl, EDTA, and supplemented with protease and phosphatase inhibitors. Post-digestion, samples were centrifuged and protein concentration was determined using the RD DC protein assay kit [13].
Western Blot Analysis: Protein extracts (20 µg total protein) were mixed with LDS sample buffer, heated to 95°C for 5 minutes, separated on 4-12% Bis-Tris Plus gels at 120V for 85 minutes, and transferred to PVDF membranes. Membranes were treated with Western Blot Enhancer, blocked in 5% BSA, and incubated overnight at 4°C with phospho-specific primary antibodies against JAK1, JAK2, JAK3, TYK2, STAT1, STAT3, and STAT4. After washing, membranes were incubated with HRP-linked secondary antibodies and detected using ECL substrate [13].
Quantitative Analysis: Band intensity was quantified using ImageJ software to calculate integrated volume (average optical density per mm²). The integrated intensity of each phosphorylated protein in non-inflamed areas was normalized, enabling comparison of pathway activation between diseased and control tissues [13].
Clinical Trial Endpoints and Assessment Methods
Modern PsA clinical trials employ comprehensive efficacy assessment:
Primary Efficacy Endpoints:
- ACR20/50/70: Composite measures incorporating tender and swollen joint counts, patient and physician global assessments, pain, disability, and acute phase reactants
- Minimal Disease Activity (MDA): Defined as meeting 5 of 7 criteria: tender joint count ≤1, swollen joint count ≤1, PASI ≤1 or BSA ≤3%, patient pain VAS ≤15, patient global disease activity VAS ≤20, HAQ-DI ≤0.5, tender entheseal points ≤1
Secondary Efficacy Endpoints:
- Psoriasis Area and Severity Index (PASI75/90/100)
- Disease Activity in Psoriatic Arthritis (DAPSA) remission
- Very Low Disease Activity (VLDA)
- Enthesitis and dactylitis resolution
- Radiographic progression via modified van der Heijde-Sharp score
Safety Assessments:
- Treatment-emergent adverse events collection using MedDRA coding
- Serious adverse events monitoring
- Laboratory parameter monitoring
- Vital signs and physical examinations [95] [94] [96]
Research Reagent Solutions
Table 3: Essential Research Tools for JAK-STAT Pathway Investigation
| Reagent/Category | Specific Examples | Research Application | Technical Notes |
|---|---|---|---|
| Phospho-Specific Antibodies | Anti-pJAK1, pJAK2, pJAK3, pTYK2, pSTAT1, pSTAT3, pSTAT4 | Western blot, immunohistochemistry | Validate using recommended cell line lysates; use phospho-protocols [13] |
| Protein Analysis Reagents | RIPA lysis buffer, protease inhibitors (Complete EDTA-free), phosphatase inhibitors (PhosSTOP) | Protein extraction and stabilization | Maintain samples at -80°C; include phosphatase inhibitors for phospho-proteins [13] |
| Detection Systems | HRP-conjugated secondary antibodies, ECL substrate, PVDF membranes, iBright imaging system | Protein detection and visualization | Optimize exposure times; use stripping buffer for sequential probing [13] |
| Clinical Assessment Tools | ACR response criteria, MDA criteria, DAPSA, PASI, HAQ-DI | Clinical trial endpoint assessment | Train assessors; standardize assessment timing [95] [94] |
| Cell Signaling Models | Cytokine-stimulated cell lines (peripheral blood mononuclear cells), patient-derived tissue cultures | Pathway activation studies | Use paired non-inflamed controls; correlate phospho-signals with clinical measures [13] |
Discussion and Future Directions
The comparative efficacy and safety profiles of JAK inhibitors in PsA reflect their distinct targeting of JAK-STAT pathway components. The superior efficacy of filgotinib and upadacitinib 30 mg over tofacitinib in network meta-analysis may relate to their enhanced selectivity profiles, potentially minimizing compensatory signaling through alternative JAK isoforms [93]. The more favorable safety profile of filgotinib suggests that preferential JAK1 inhibition may maintain efficacy while reducing class-associated toxicities.
The observed sex-dependent activation of JAK2/STAT3 in inflammatory conditions highlights the importance of personalized approaches to JAK inhibitor therapy [13]. Future research should focus on biomarker development to match specific JAK-STAT activation patterns with optimal JAK inhibitor selection.
Long-term extension studies demonstrate maintained efficacy of both upadacitinib and tofacitinib over several years, supporting their durability as treatment options [97] [94]. Real-world evidence confirms the effectiveness of upadacitinib across PsA subtypes, including both oligoarticular and polyarticular phenotypes [95] [96].
As JAK inhibitor research evolves, attention is turning to combination approaches, sequencing strategies, and positioning within treatment algorithms. The similar efficacy observed between upadacitinib 15 mg and adalimumab at 5 years supports JAK inhibitors as viable alternatives to TNF inhibition [94], while the maintained efficacy when switching directly from adalimumab to tofacitinib provides evidence for sequential therapy without washout periods [98].
In conclusion, the JAK-STAT pathway represents a critical therapeutic target in PsA, with distinct JAK inhibitors offering varied efficacy-safety profiles. Understanding the molecular nuances of pathway activation and inhibition enables more precise therapeutic targeting and personalized treatment approaches for patients with psoriatic arthritis.
The Janus kinase-signal transducer and activator of transcription (JAK-STAT) pathway serves as a fundamental signaling nexus that transduces extracellular cytokine signals into intracellular transcriptional responses. This evolutionarily conserved pathway regulates critical processes including immune cell differentiation, proliferation, and inflammatory mediator production [9]. In healthy states, JAK-STAT signaling is tightly regulated; however, constitutive pathway activation contributes to the pathogenesis of numerous immune-mediated inflammatory diseases (IMIDs) [9] [55]. Recent research has illuminated the complex activation patterns of this pathway in specific disease contexts, revealing heterogeneous involvement of individual JAK-STAT components that informs targeted therapeutic development [26] [13].
The emergence of Janus kinase inhibitors (Jakinibs) represents a paradigm shift in the management of IMIDs, offering a small-molecule alternative to biologic therapies that target specific cytokine receptors or ligands [101]. Unlike monoclonal antibodies that act on extracellular targets, Jakinibs modulate intracellular signaling pathways, potentially yielding broader immunomodulatory effects. This comprehensive review examines the positioning of Jakinibs relative to biologic therapies in treatment algorithms, with particular emphasis on mechanistic distinctions, efficacy profiles, safety considerations, and personalized medicine approaches grounded in contemporary JAK-STAT pathway research.
Molecular Mechanisms: Distinct Therapeutic Approaches to Pathway Modulation
JAK-STAT Pathway Architecture and Dysregulation
The JAK-STAT pathway comprises four JAK family members (JAK1, JAK2, JAK3, TYK2) and seven STAT proteins (STAT1, STAT2, STAT3, STAT4, STAT5A, STAT5B, STAT6) that orchestrate signaling for numerous cytokines, interleukins, and growth factors [9]. Upon cytokine-receptor engagement, receptor-associated JAKs undergo trans-phosphorylation, creating docking sites for STAT proteins which are subsequently phosphorylated. These activated STATs dimerize and translocate to the nucleus, regulating transcription of target genes involved in immune and inflammatory responses [9] [55].
Dysregulated JAK-STAT signaling manifests differently across IMIDs. In ulcerative colitis (UC), inflamed mucosa demonstrates significantly increased phosphorylation of JAK2, JAK3, TYK2, STAT1, STAT3, and STAT4 compared to non-inflamed tissue, with coordinated activation patterns suggesting functional interdependence [26] [13]. Notably, recent research has identified sex-dependent differences in pathway activation, with male UC patients exhibiting significantly higher JAK2 and STAT3 phosphorylation [26] [13]. In psoriasis and psoriatic arthritis, the JAK-STAT pathway (particularly STAT3) drives keratinocyte hyperproliferation and synovial inflammation, with IL-23-mediated TYK2 activation promoting Th17 responses [55].
Figure 1: JAK-STAT Signaling Pathway. This diagram illustrates the core JAK-STAT signaling cascade, from cytokine-receptor engagement to STAT phosphorylation, nuclear translocation, and regulation of target gene transcription.
Mechanism of Action: Jakinibs vs. Biologics
Jakinibs are small-molecule inhibitors that target the intracellular kinase domain of JAK proteins, preventing STAT phosphorylation and downstream signaling. They exhibit diverse selectivity profiles:
- Tofacitinib: Pan-JAK inhibitor (JAK1/JAK3 > JAK2)
- Upadacitinib: JAK1-selective inhibitor
- Filgotinib: JAK1-selective inhibitor
- Selective TYK2 inhibitors: Target TYK2 pseudokinase domain [101] [55]
Biologic therapies are large-protein drugs that target extracellular inflammatory components:
- Cytokine antagonists (e.g., anti-TNF, anti-IL-12/23, anti-IL-17)
- Lymphocyte trafficking modifiers (e.g., anti-integrins)
- B-cell depleting agents (e.g., anti-CD20) [102] [101]
The fundamental distinction lies in their sites of action: biologics target specific, extracellular components with high specificity, while Jakinibs modulate broader intracellular signaling networks with potential impacts across multiple cytokine pathways.
Clinical Efficacy and Response Dynamics
Induction and Maintenance of Clinical Response
Clinical trial data and real-world evidence demonstrate distinctive efficacy profiles for Jakinibs versus biologics across various IMIDs. In ulcerative colitis, tofacitinib induction therapy (10 mg twice daily) achieved clinical remission in 18.5% and 16.6% of patients in OCTAVE Induction 1 and 2 trials, respectively, versus 8.2% and 3.6% with placebo [101]. Maintenance therapy with tofacitinib (5 mg or 10 mg twice daily) sustained remission in 34.3% and 40.6% of respondents, respectively [101]. Similarly, upadacitinib and filgotinib have demonstrated significant efficacy in UC clinical trials [101].
Real-world comparative studies in atopic dermatitis reveal differential response dynamics: Jakinibs produce faster early responses, while biologics achieve greater absolute improvements between weeks 16 and 52, along with longer treatment persistence [102]. This pattern suggests complementary roles in treatment algorithms, with Jakinibs potentially offering rapid symptom control and biologics providing sustained long-term remission.
Table 1: Comparative Efficacy of JAK Inhibitors in Ulcerative colitis Clinical Trials
| JAK Inhibitor | Trial Phase | Dosage | Remission Rate | Placebo Rate | Study Duration |
|---|---|---|---|---|---|
| Tofacitinib | OCTAVE Induction 1 | 10 mg BID | 18.5% | 8.2% | 8 weeks |
| Tofacitinib | OCTAVE Induction 2 | 10 mg BID | 16.6% | 3.6% | 8 weeks |
| Tofacitinib | OCTAVE Sustain | 5 mg BID | 34.3% | 11.1% | 52 weeks |
| Tofacitinib | OCTAVE Sustain | 10 mg BID | 40.6% | 11.1% | 52 weeks |
| Filgotinib | SELECTION (Biologic-naïve) | 200 mg daily | 26.1% | 15.3% | 10 weeks |
Novel Applications and Combination Approaches
Emerging evidence supports Jakinib use in challenging clinical scenarios. For acute severe ulcerative colitis (ASUC), tofacitinib shows promise as rescue therapy. A prospective randomized trial found 83% of patients receiving tofacitinib (10 mg three times daily) achieved clinical response at day 7 versus 59% receiving standard care alone [101]. Similar trends are observed in other IMIDs, including refractory noninfectious uveitis, where Jakinibs maintained disease control in patients failing conventional immunomodulators [103].
The potential for combination therapy remains an area of active investigation. While concurrent use of Jakinibs with biologics is generally restricted in clinical practice, rational combination approaches based on complementary mechanisms may offer enhanced efficacy in treatment-resistant disease.
Safety and Tolerability Profiles
Class-Specific Adverse Events
Systematic literature reviews reveal consistent safety profiles across Jakinibs, with some class-wide adverse events of special interest (AESI) [104]. These include:
- Increased infection risk (especially herpes zoster)
- Laboratory abnormalities (transaminitis, cytopenias, lipid elevations)
- Malignancy risk (particularly with higher doses in at-risk populations)
- Thromboembolic events (more prevalent with JAK2-selective inhibition)
- Cardiovascular events [104] [101]
Comparative real-world studies in atopic dermatitis demonstrate distinct adverse event patterns: infections and acne occur more frequently with Jakinibs, while ocular symptoms are more common with biologics [102]. These differential safety profiles inform risk-stratified treatment selection, particularly in patients with comorbidities or specific risk factors.
Risk Mitigation and Patient Selection
Safety considerations have prompted refined risk-benefit assessments and risk mitigation strategies. Regulatory agencies now emphasize careful patient selection, considering:
- Age and cardiovascular risk factors
- Smoking status
- Cancer history
- Thromboembolic risk
- Chronic infection risk [104] [101]
Laboratory monitoring (complete blood count, comprehensive metabolic panel, lipid profile) before and during treatment facilitates early detection of abnormalities. Dose adjustment or treatment discontinuation may be necessary for certain laboratory changes or clinical adverse events.
Biomarkers and Personalized Treatment Selection
Pathway Activation Signatures
Recent research highlights the potential for biomarker-driven treatment selection. In ulcerative colitis, heterogeneous activation of JAK-STAT components suggests that pathway profiling could predict treatment response [26] [13]. The coordinated activation of JAK2, JAK3, TYK2, and STAT3 in inflamed mucosa indicates these proteins may represent strategic therapeutic targets [13].
Sex-dependent differences in pathway activation further refine personalized approaches. The significantly higher JAK2 and STAT3 phosphorylation observed in male UC patients suggests potentially enhanced responsiveness to JAK2/STAT3-targeted therapies [26] [13]. Such molecular stratification represents the frontier of precision medicine in IMIDs.
Treatment Response Monitoring
Beyond baseline biomarkers, dynamic monitoring of pathway activity during treatment may guide therapy optimization. Phosphorylation levels of JAK-STAT components could potentially serve as pharmacodynamic biomarkers, reflecting target engagement and pathway suppression [26]. Integration of these molecular measures with conventional clinical, endoscopic, and radiographic assessments provides a comprehensive view of treatment response.
Table 2: Research Reagent Solutions for JAK-STAT Pathway Analysis
| Research Tool | Specific Application | Key Features | Experimental Utility |
|---|---|---|---|
| Phospho-Specific Antibodies | Western blot detection of phosphorylated JAK/STAT proteins | Target-specific; validated with control lysates | Quantification of pathway activation in tissue samples [13] |
| JAK Inhibitor Compounds | Pathway inhibition studies | Varied selectivity profiles (pan vs. selective) | Mechanistic studies; dose-response relationships [101] [32] |
| Cytokine Stimulation Assays | Pathway activation experiments | Controlled JAK-STAT pathway stimulation | Assessment of signaling dynamics and inhibitory potency [13] |
| Protein Extraction Reagents | Tissue protein isolation | Protease/phosphatase inhibitor compatibility | Preservation of phosphorylation states during sample processing [13] |
Experimental Approaches for JAK-STAT Pathway Analysis
Assessment of Pathway Activation in Human Tissue
Cutting-edge research elucidating JAK-STAT activation patterns employs sophisticated methodological approaches. A recent prospective observational study of UC patients utilized paired biopsies from inflamed and non-inflamed colonic mucosa obtained during routine colonoscopy [13]. Detailed methodology included:
- Sample Processing: Mechanical digestion and sonication in lysis buffer supplemented with protease and phosphatase inhibitors
- Protein Quantification: RD DC protein assay for precise protein concentration determination
- Western Blot Analysis:
- Protein separation using Bolt 4-12% Bis-Tris Plus gels
- Transfer to PVDF membranes
- Sequential probing with phospho-specific antibodies for JAK1, JAK2, JAK3, TYK2, STAT1, STAT3, and STAT4
- Enhanced detection using SuperSignal Western Blot Enhancer
- Stripping and reprobing membranes for multiple targets
- Quantification: Densitometric analysis using ImageJ software normalized to β-actin loading controls [13]
This rigorous approach enables comprehensive phosphorylation profiling across multiple JAK-STAT components, revealing activation patterns relevant to disease pathophysiology and treatment response.
Comparative Effectiveness Study Designs
Real-world comparative studies require meticulous methodology to ensure valid conclusions. Recent investigations comparing Jakinibs and biologics employ:
- Ambispective Designs: Combining retrospective data collection with prospective follow-up
- Adequate Sample Sizing: Powered to detect clinically relevant differences in outcomes
- Balanced Treatment Groups: Assessing baseline demographic and clinical characteristics to ensure comparability
- Comprehensive Outcome Assessment: Including clinical severity scores, treatment persistence, super-responder rates, and adverse events
- Appropriate Statistical Analyses: Accounting for confounding variables and treatment switches [102]
These methodological considerations strengthen the validity of real-world evidence informing treatment algorithms.
Figure 2: Treatment Algorithm Decision Pathway. This diagram outlines a personalized approach to selecting between JAK inhibitors and biologic therapies based on patient-specific factors and treatment goals.
Evolving Treatment Paradigms
The positioning of Jakinibs within treatment algorithms continues to evolve with emerging evidence. Key areas of development include:
- Novel Selective Inhibitors: Next-generation Jakinibs with enhanced selectivity for specific JAK isoforms may improve therapeutic indices
- Biomarker-Driven Selection: Validation of predictive biomarkers for treatment response will enable precision medicine approaches
- Combination Strategies: Rational combination with biologics may benefit patients with refractory disease
- Treatment Sequencing: Optimal ordering of Jakinibs and biologics requires further prospective study [105] [101]
Bibliometric analyses reveal shifting research priorities, with early studies focused on efficacy validation now giving way to investigations of long-term safety, comparative effectiveness, and personalized treatment strategies [105].
Integrated Treatment Algorithm
An evidence-based treatment algorithm must incorporate multiple patient- and disease-specific factors:
- Disease Severity and Urgency: Jakinibs may be preferred when rapid symptom control is prioritized
- Prior Treatment History: Jakinibs show efficacy in patients failing multiple biologic classes
- Comorbidity Profile: Safety considerations may favor one class over another in specific risk populations
- Pathway Activation Patterns: Molecular profiling may eventually guide targeted selection
- Patient Preferences: Route of administration, monitoring requirements, and cost influence shared decision-making
In conclusion, Jakinibs and biologics represent complementary therapeutic approaches with distinct mechanistic foundations, efficacy profiles, and safety considerations. Contemporary treatment algorithms should integrate these modalities in a rational, personalized approach that optimizes outcomes for patients with immune-mediated inflammatory diseases. Future advances in JAK-STAT pathway biology and predictive biomarkers will further refine this positioning, ultimately enhancing precision medicine in clinical practice.
The Janus kinase-signal transducer and activator of transcription (JAK-STAT) pathway serves as a central signaling nexus that coordinates rapid transduction of extracellular signals from membrane receptors to nuclear effectors, regulating diverse cellular processes encompassing proliferation, apoptosis, inflammation, and differentiation [49]. This pathway comprises four structurally homologous JAK family members (JAK1, JAK2, JAK3, TYK2) and various STAT transcription factors. Dysregulation of JAK-STAT signaling has been implicated in the pathogenesis of multiple immune-mediated inflammatory diseases (IMIDs), including atopic dermatitis, rheumatoid arthritis, alopecia areata, and inflammatory bowel disease [49] [106]. The recognition of this pathway's crucial role in inflammatory signaling has catalyzed the development of targeted therapeutic agents designed to selectively inhibit specific JAK isoforms while minimizing off-target effects.
First-generation JAK inhibitors demonstrated potent anti-inflammatory effects but exhibited relatively broad inhibition profiles across multiple JAK isoforms. Advances in structural biology and molecular modeling have enabled the development of second-generation inhibitors with enhanced selectivity for specific JAK family members [106]. This evolution toward precision targeting represents a paradigm shift in therapeutic development for inflammatory conditions, potentially offering improved efficacy and safety profiles. The clinical validation of these selective inhibitors requires rigorous assessment through controlled trials and biomarker analyses to establish their place in the therapeutic landscape and optimize their application through precision medicine approaches.
Methodological Framework for Evaluating Selective JAK Inhibitors
Clinical Trial Design Considerations
The evaluation of selective JAK inhibitors employs methodologically rigorous clinical trial designs incorporating objective efficacy endpoints, comprehensive safety monitoring, and biomarker assessments. Pivotal Phase 2 and 3 trials typically utilize randomized, double-blind, placebo-controlled designs with active comparator arms when appropriate. Trial duration generally ranges from 12-24 weeks for initial efficacy assessment, with extension phases evaluating long-term outcomes up to 152 weeks [80] [107].
Disease-specific validated instruments serve as primary efficacy endpoints. In dermatologic conditions such as atopic dermatitis (AD), the Eczema Area and Severity Index (EASI) quantifies disease severity, with EASI75 (≥75% improvement from baseline) representing a clinically meaningful threshold [108]. The Peak Pruritus Numerical Rating Scale (PP-NRS) measures itch intensity, while the Severity of Alopecia Tool (SALT) score objectively quantifies hair loss in alopecia areata trials [80] [106]. These standardized metrics enable cross-trial comparisons and regulatory evaluation.
Safety assessment follows standardized protocols with continuous monitoring of adverse events (AEs), serious AEs (SAEs), and specific laboratory parameters including complete blood count, hepatic and renal function, lipid profiles, and creatine phosphokinase (CPK) levels [109] [107]. Prospective adjudication of major adverse cardiovascular events (MACE), venous thromboembolism (VTE), and malignancies ensures consistent classification across studies.
Biomarker Assessment Methodologies
Biomarker evaluation incorporates both serum-based and tissue-based approaches to elucidate mechanism of action and identify potential predictors of treatment response. Serum biomarkers including thymus and activation-regulated chemokine (TARC/CCL17), eosinophil count, total immunoglobulin E (IgE), dipeptidyl peptidase-4 (DPP-4), and periostin are quantified using standardized immunoassays at baseline and predetermined intervals during treatment [108] [110]. These measurements provide insights into effects on specific inflammatory pathways.
Transcriptomic profiling of skin biopsies using RNA sequencing assesses gene expression changes in key inflammatory pathways (Th2, Th1, Th17, Th22) following treatment [110]. Non-invasive tape stripping methodologies enable collection of stratum corneum proteins for proteomic analysis, providing molecular data without requiring invasive procedures [110]. These complementary approaches facilitate comprehensive characterization of drug effects on inflammatory pathways and correlation with clinical outcomes.
Table 1: Core Methodological Assessments in JAK Inhibitor Clinical Trials
| Assessment Category | Specific Measures | Timing | Application |
|---|---|---|---|
| Efficacy Endpoints | EASI75, SALT ≤20, PP-NRS improvement | Weeks 12, 24, 52 | Primary efficacy determination |
| Safety Monitoring | AE/SAE incidence, laboratory parameters, MACE, VTE, malignancies | Continuous with scheduled reviews | Risk-benefit assessment |
| Biomarker Analysis | TARC, eosinophils, IgE, DPP-4, periostin | Baseline, Weeks 4, 12, 24 | Mechanism of action, response prediction |
| Pharmacokinetics | Drug concentration, metabolic profiles | Pre-dose, multiple post-dose timepoints | Exposure-response relationships |
| Quality of Life | DLQI, PRISM, ADerm-SS | Baseline, Week 12, 24 | Patient-reported outcomes |
Statistical Analytical Approaches
Statistical analysis of trial data employs intention-to-treat principles with appropriate handling of missing data, typically using multiple imputation or mixed-effects models for repeated measures. For efficacy endpoints, logistic regression models adjusted for key baseline covariates evaluate differences between treatment groups, reporting odds ratios (OR) with 95% confidence intervals (CI) [108]. Safety analyses employ incidence rates (IR) per 100 person-years with hazard ratios (HR) from Cox proportional hazards models for time-to-event outcomes [86]. Meta-analytic approaches incorporate random-effects models to pool data across multiple studies when appropriate, quantifying heterogeneity using I² statistics [86] [107].
Clinical Trial Outcomes for Selective JAK Inhibitors
JAK1-Selective Inhibitors
JAK1-selective inhibitors represent a significant advancement in targeted therapy, designed to mitigate safety concerns associated with broader JAK inhibition while maintaining efficacy.
Upadacitinib, a highly selective JAK1 inhibitor, has demonstrated robust efficacy across multiple inflammatory conditions. In atopic dermatitis, upadacitinib treatment resulted in significant improvement in EASI75 scores and superior antipruritic effects compared to IL-13 targeted therapy, with 100% of patients showing PP-NRS improvement at 3 months versus 60% with IL-13 inhibition (OR=34.61 for PP-NRS 0/1 achievement) [108]. A systematic review and meta-analysis of safety data from 9,547 patients across 18 randomized controlled trials revealed that upadacitinib was associated with increased risks of hepatic disorder, neutropenia, acne, herpes zoster, and elevated creatine phosphokinase levels, with hepatic disorder, neutropenia, and acne exhibiting dose-dependent relationships [107]. Importantly, no significant association was observed with renal dysfunction, non-melanoma skin cancer, MACE, or VTE, supporting its generally favorable safety profile [107].
Abrocitinib, another JAK1-selective inhibitor, has shown dose-dependent efficacy in moderate-to-severe AD, with higher doses (200mg) demonstrating more rapid improvement than lower doses (100mg) [108]. Abrocitinib treatment significantly reduced Th22-associated genes (S100A8/9/12) in a dose-dependent manner, beginning as early as week 2 and continuing through week 12 [110]. Real-world studies confirmed significant eosinophil count reduction after 4 weeks of abrocitinib treatment in 47 patients, suggesting this parameter may serve as a responsive biomarker [110].
JAK3-Selective Inhibition
Ritlecitinib, a selective JAK3 inhibitor, received FDA approval in 2023 for patients aged ≥12 years with severe alopecia areata [80]. In the pivotal ALLEGRO phase 3 trial, 23% of patients achieved SALT ≤20 at week 24, with response rates increasing to 45% at 1 year and 61% at 2 years, demonstrating cumulative benefit with extended treatment [80]. This sustained efficacy supports the role of JAK3 inhibition in modifying the underlying autoimmune process in alopecia areata.
Dual JAK1/JAK2 Inhibitors
Baricitinib, a JAK1/JAK2 inhibitor, was the first JAK inhibitor approved for severe alopecia areata in June 2022 based on pivotal trials (BRAVE-AA1 and BRAVE-AA2) demonstrating significant hair regrowth [80]. At 36 weeks, 35-40% of patients achieved SALT scores ≤20 (representing ≥80% scalp hair coverage), with efficacy sustained through 152 weeks [80]. In a retrospective longitudinal cohort study of patients aged <12 years, baricitinib treatment resulted in a mean SALT score reduction of 68% after at least 24 weeks of treatment [106]. Common adverse events included infection, headache, acne, and elevated blood creatine phosphokinase, with a generally favorable risk-benefit ratio compared to conventional systemic immunosuppressants [106].
Deuruxolitinib, another JAK1/JAK2 inhibitor, obtained FDA approval in July 2024 for alopecia areata [80]. In the THRIVE-AA1 and AA2 trials, 41% of patients achieved SALT ≤20 by week 24, with continued improvement observed through 68 weeks of treatment [80].
Table 2: Efficacy Outcomes of JAK Inhibitors in Pivotal Clinical Trials
| JAK Inhibitor | Selectivity Profile | Indication | Key Trial | Efficacy Outcome | Duration |
|---|---|---|---|---|---|
| Upadacitinib | JAK1 | Atopic Dermatitis | Measure Up 1 & 2 | EASI75: ~70-80% | Week 16 |
| Baricitinib | JAK1/JAK2 | Alopecia Areata | BRAVE-AA1 & AA2 | SALT≤20: 35-40% | Week 36 |
| Ritlecitinib | JAK3/TYK2 | Alopecia Areata | ALLEGRO | SALT≤20: 23% (24wk), 45% (1yr) | Week 24-52 |
| Deuruxolitinib | JAK1/JAK2 | Alopecia Areata | THRIVE-AA1 & AA2 | SALT≤20: 41% | Week 24 |
| Abrocitinib | JAK1 | Atopic Dermatitis | JADE-MONO | EASI75: ~60-70% | Week 12 |
Biomarker Insights and Precision Medicine Applications
Predictive Biomarkers of Treatment Response
Biomarker studies have revealed distinct patterns associated with response to different JAK inhibitor classes, informing potential precision medicine approaches. For JAK1 inhibitors, eosinophil count reduction has emerged as a consistently observed biomarker, correlating with EASI improvement in patients treated with upadacitinib (univariate: R=0.525, p=0.0009; adjusted: β=0.567, p=0.0004) [108]. This likely reflects inhibition of IL-5 signaling, a key eosinophil regulator. Additional JAK1-inhibitor associated biomarkers include reduction of IL5RA and CCL23, both upregulated in the eosinophil-high endotype [110].
In contrast, TARC (thymus and activation-regulated chemokine) reduction demonstrates the strongest correlation with treatment response to IL-13 antibodies (univariate: R=0.677, p<0.0001; adjusted: β=0.661, p<0.0001) but shows less consistent association with JAK inhibitor response [108]. This differential biomarker association reflects the distinct mechanisms of action between these targeted therapies.
For specific cytokine-targeted therapies, DPP-4 and periostin have been identified as potential biomarkers for predicting response to tralokinumab (anti-IL-13), with patients exhibiting higher baseline concentrations of these IL-13 activity markers showing greater EASI improvement [110]. Additionally, baseline IL-22 expression may predict response to therapies targeting this pathway, including fezakinumab and potentially JAK inhibitors that modulate Th22 signaling [110].
Pathway-Specific Biomarker Signatures
Comprehensive transcriptomic analyses have elucidated the multifaceted effects of JAK inhibitors on inflammatory pathways. Upadacitinib treatment downregulates key AD genes associated with multiple pathways including Th2 (CCL17), Th1 (CXCL10), and Th22 (S100A9/12, PI3) [110]. Similarly, abrocitinib downregulates genes associated with inflammation, epidermal hyperplasia, and Th2/Th22 immune responses in moderate-to-severe AD skin [110]. This broad modulation of multiple inflammatory axes contrasts with the more restricted pathway inhibition of cytokine-specific biologics and may explain the potent clinical efficacy observed with JAK inhibitors.
Cluster analyses have identified distinct AD endotypes characterized by unique serum biomarker profiles, suggesting potential for patient stratification. Two clusters characterized by Th2-dominated biomarker profiles (Th1/Th2/Th17-dominant and Th2/Th22/PARC-dominant) with elevated Th2-related cytokines may represent ideal candidates for Th2-blocking therapies, while other inflammatory patterns might respond more favorably to JAK inhibition [110].
Comparative Safety Profiles and Risk Mitigation
Class-Wide Safety Considerations
JAK inhibitors carry a FDA boxed warning for serious infections, malignancy, MACE, thrombosis, and mortality, primarily based on the ORAL Surveillance trial of tofacitinib in rheumatoid arthritis patients aged ≥50 years with cardiovascular risk factors [86]. However, subsequent comparative effectiveness studies across broader IMID populations have provided important context for these risks.
A comprehensive systematic review and meta-analysis of 42 head-to-head comparative effectiveness studies including 813,881 patients with IMIDs found no meaningful differences in risk of serious infections (HR 1.05, 95% CI 0.97-1.13), malignant neoplasms (HR 1.02, 95% CI 0.90-1.16), or MACEs (HR 0.91, 95% CI 0.80-1.04) between JAK inhibitors and TNF antagonists [86]. JAK inhibitor use was associated with a slightly higher risk of VTE compared with TNF antagonist use (HR 1.26, 95% CI 1.03-1.54), though absolute incidence rates remained low (0.57 vs. 0.52 per 100 person-years) [86].
Risk Stratification and Management Strategies
Current evidence indicates the existence of a subpopulation at increased risk of JAK inhibitor adverse events, including patients over 65 years of age, those with cardiovascular and malignancy risk factors, and smokers [109]. These findings have informed risk mitigation strategies incorporating careful patient selection, pretreatment screening, and ongoing monitoring.
Recommended safety assessments prior to initiating JAK inhibitor therapy include complete blood count, comprehensive metabolic panel, lipid profile, viral serologies (hepatitis B/C), and tuberculosis screening [109]. Vaccination status should be reviewed and updated as needed, with particular attention to herpes zoster vaccination given the increased risk of herpes zoster reactivation observed with JAK inhibitors [109] [107]. During treatment, ongoing monitoring for infections, cardiovascular symptoms, laboratory abnormalities, and potential malignancies facilitates early detection and management of adverse events.
Table 3: Safety Profiles of Selective JAK Inhibitors
| JAK Inhibitor | Most Frequent AEs | Laboratory Abnormalities | Black Box Warnings | Risk Mitigation Strategies |
|---|---|---|---|---|
| Upadacitinib | Acne, herpes zoster, hepatic disorder | Increased CPK, neutropenia | Serious infections, malignancy, thrombosis, mortality | CBC, LFT monitoring; zoster vaccination |
| Baricitinib | Upper respiratory infections, headache, acne | Increased CPK, LDL cholesterol | Same as above | TB screening; lipid monitoring; infection vigilance |
| Ritlecitinib | Headache, diarrhea, acne | Increased CPK | Same as above | Similar to above with dose adjustment considerations |
| Abrocitinib | Nausea, headache, acne | Increased CPK, LDL cholesterol | Same as above | Antiemetics for nausea; lipid management |
Research Reagent Solutions for JAK-STAT Pathway Investigation
Table 4: Essential Research Tools for JAK-STAT Pathway and Inhibitor Studies
| Research Tool Category | Specific Examples | Research Application | Technical Considerations |
|---|---|---|---|
| JAK Selectivity Assays | Cell-free kinase assays, Ba/F3 proliferation assays | Inhibitor selectivity profiling | Pan-JAK screening panels assess isoform specificity |
| Phospho-STAT Detection | Phospho-flow cytometry, Western blot, MSD immunoassays | Target engagement verification | Multiplex approaches enable pathway mapping |
| Cytokine Profiling | LEGENDplex arrays, Ella automated immunoassays | Inflammatory pathway modulation | Focus on JAK-STAT relevant cytokines (IFN-γ, IL-4, IL-13, IL-31) |
| Transcriptomic Analysis | RNA sequencing, Nanostring nCounter panels | Pathway analysis and endotyping | Custom codesets for JAK-STAT pathway genes |
| Animal Models | MC903-induced dermatitis, AA mouse models | In vivo efficacy assessment | Humanized mice enable translational studies |
| Biomarker Assays | TARC/CCL17, DPP-4, periostin ELISAs | Treatment response monitoring | Standardized sampling timing critical for comparison |
The clinical validation of selective JAK inhibitors represents a significant advancement in targeted immunomodulation, demonstrating robust efficacy across multiple inflammatory conditions while offering improved safety profiles through enhanced selectivity. The comprehensive trial data summarized herein supports their role as valuable therapeutic options, particularly for patients with inadequate response to conventional therapies or cytokine-specific biologics.
Future development in this field will likely focus on further refinement of selectivity profiles, optimization of dosing strategies to balance efficacy and safety and advancement of precision medicine approaches through validated biomarker-driven patient selection. Additionally, long-term extension studies and real-world evidence will continue to clarify the safety profiles of these agents in diverse patient populations. As understanding of JAK-STAT biology evolves, the integration of biomarker assessments and patient stratification strategies will enable increasingly targeted application of these potent therapeutic agents, ultimately optimizing outcomes for patients with immune-mediated inflammatory diseases.
Long-Term Data and Real-World Evidence on Jakinib Performance
The Janus kinase-signal transducer and activator of transcription (JAK-STAT) pathway represents a crucial signaling cascade that transmits information from extracellular cytokines to the nucleus, regulating gene expression in fundamental cellular processes including immunity, hematopoiesis, and inflammation [9]. Dysregulation of this pathway contributes significantly to the pathogenesis of various immune-mediated inflammatory diseases (IMIDs), positioning JAK inhibitors (JAKi) as a transformative therapeutic class [9] [111]. While randomized controlled trials (RCTs) establish the efficacy of JAKi, real-world evidence (RWE) is indispensable for understanding their long-term performance in clinically complex, diverse patient populations encountered in routine practice [112] [113]. This whitepaper synthesizes long-term data and RWE on Jakinib performance, providing researchers and drug development professionals with a critical analysis of their effectiveness, safety, and practical utility across IMIDs, framed within the context of JAK-STAT pathway activation.
The JAK-STAT Pathway: Mechanism and Therapeutic Target
Pathway Architecture and Signaling Dynamics
The JAK-STAT pathway functions as a primary conduit for cytokine signaling. Its architecture comprises three key components: cell surface cytokine receptors, associated JAK kinases (JAK1, JAK2, JAK3, TYK2), and STAT transcription factors (STAT1-6) [9] [55]. Upon cytokine binding, receptor dimerization triggers trans-phosphorylation and activation of JAKs, which in turn phosphorylate STAT proteins. Phosphorylated STATs dimerize, translocate to the nucleus, and initiate transcription of target genes governing immune cell activation, proliferation, and survival [9] [55]. The specificity of responses is achieved through distinct cytokine-receptor pairings and selective activation of JAK and STAT family members.
Recent structural biology advances, particularly using cryo-electron microscopy, have elucidated the molecular mechanisms governing cytokine-receptor recognition, JAK activation, and STAT phosphorylation [9]. This structural insight is foundational for engineering targeted therapies and understanding the mechanistic basis of JAK inhibitor action.
Pathogenic Dysregulation in Immune-Mediated Diseases
Dysregulation of the JAK-STAT pathway, through excessive or sustained activation, is a hallmark of numerous IMIDs. Genetic variations in pathway components are risk factors for autoimmune conditions [9]. Disease-specific patterns of JAK-STAT activation are increasingly recognized:
- Rheumatoid Arthritis (RA): Multiple cytokines implicated in RA pathogenesis (e.g., IL-6, IFNs, GM-CSF) signal through JAKs, driving inflammation and joint damage [112].
- Ulcerative Colitis (UC): Inflamed colonic mucosa shows significantly increased phosphorylation of JAK2, JAK3, TYK2, STAT1, STAT3, and STAT4 compared to non-inflamed tissue, indicating localized pathway hyperactivation [26] [13].
- Psoriasis and Psoriatic Arthritis (PsA): The pathway, particularly STAT3 activation by IL-23 and IL-17, drives keratinocyte hyperproliferation, immune cell infiltration, and synovial inflammation [55].
- Alopecia Areata (AA): Aberrant JAK-STAT signaling, fueled by cytokines like IFN-γ, underlies the collapse of immune privilege in hair follicles [114].
Table 1: JAK-STAT Pathway Components and Their Roles in Inflammation
| Pathway Component | Key Functions | Association with IMIDs |
|---|---|---|
| JAK1 | Cytokine signaling (IFN, γ-chain cytokines) | Rheumatoid Arthritis, Inflammatory Bowel Disease |
| JAK2 | Hematopoiesis (EPO, TPO signaling) | Ulcerative Colitis (sex-dependent activation) [26] [13] |
| JAK3 | Immune function (γ-chain cytokines) | Immunodeficiencies, Autoimmune Inflammation |
| TYK2 | IL-12, IL-23 signaling | Psoriasis, Psoriatic Arthritis, Lupus [9] [55] |
| STAT3 | Th17 differentiation, Acute phase response | Ulcerative Colitis, Psoriasis, RA [26] [13] [55] |
Figure 1: JAK-STAT Pathway Activation Cascade. This diagram illustrates the core signaling mechanism where cytokine binding triggers JAK kinase activation, leading to STAT protein phosphorylation, dimerization, nuclear translocation, and subsequent regulation of target gene transcription.
Real-World Effectiveness of JAK Inhibitors Across Diseases
Rheumatoid Arthritis
Systematic analyses of US real-world studies demonstrate the effectiveness of JAKi in RA across adherence, persistence, clinical, and patient-reported outcomes [112] [113]. Key performance metrics from 35 observational studies are summarized below.
Table 2: Real-World Effectiveness of JAK Inhibitors in Rheumatoid Arthritis
| Effectiveness Domain | Metric | Real-World Findings | Data Source |
|---|---|---|---|
| Treatment Patterns | Adherence (PDC) | 0.53 - 0.83 (11 studies) [112] | Administrative Claims |
| Persistence (Median) | 121 - 516 days (14 studies) [112] | Administrative Claims | |
| Effectiveness Algorithm* | 14.8% - 26% of patients (6 studies) [112] | Administrative Claims | |
| Clinical Response | Mean CDAI Change (6 months) | -4.7 to 5.1 (10 studies) [112] | Registry, EMR |
| Patient-Reported Outcomes | Mean Pain Change | -9.3 to 8.9 (12 studies) [112] | Registry, EMR |
Claims-based algorithm criteria: high adherence, no switch/addition of bDMARDs/JAKi or csDMARDs, no dose increase, no more than one glucocorticoid injection, no new/increased oral glucocorticoids [112].
A single-center study directly comparing baricitinib and tofacitinib found no significant difference in effectiveness, including in first-line use, after bDMARD failure, or in monotherapy versus combination therapy [115]. The Clinical Disease Activity Index (CDAI) was the most common measure of clinical response in registry-based studies [112].
Alopecia Areata
A single-center retrospective cohort study of 72 patients with severe AA revealed that 61% achieved substantial regrowth at a median time of 7 months, with cumulative regrowth rates increasing over time: 11.1% at 3 months, 40.2% at 6 months, 55.6% at 9 months, and 59.7% at 12 months [114]. This underscores that extended treatment durations are often necessary for optimal outcomes. Notably, among patients who did not respond to an initial JAKi, 75% achieved substantial regrowth after switching to a different JAKi, highlighting a viable therapeutic strategy for non-responders [114].
Comparative Performance Across IMIDs
Two comprehensive systematic reviews published in 2024 evaluated the efficacy and safety of 21 JAK inhibitors across 51 IMIDs [111]. The efficacy review, analyzing 102 RCTs, confirmed the broad effectiveness of JAKi therapies across diseases including RA, psoriatic arthritis, and ulcerative colitis [111]. The reviews also advanced the understanding of JAK selectivity, exploring how differential inhibition of JAK subtypes influences clinical profiles and provides a framework for more tailored treatment strategies [111].
Safety Profile from Real-World and Long-Term Data
A systematic literature review on the safety of JAKi in IMIDs, incorporating data from 209 studies including RCTs, long-term extensions, and real-world cohort studies, found that safety profiles are generally consistent across compounds and indications [104] [111]. However, the analysis identified important modifying factors:
- Patient profiles, treatment dosing, and background medications can influence drug safety [104].
- Differentially selective JAKi exhibit distinct effects on specific adverse events of special interest (AESI) and laboratory outcomes [104].
Key safety concerns addressed in the review include cardiovascular events, serious infections, and malignancy risks [111]. This extensive body of evidence supports informed risk-benefit assessments and underscores the necessity for personalized patient management strategies, particularly for populations at increased risk for adverse events.
Methodological Frameworks for Real-World Evidence Generation
Real-world studies on JAKi utilize diverse data sources, each with strengths and limitations:
- Administrative Claims Databases (65.7% of US RA studies): Primarily used for analyzing treatment patterns (adherence, persistence, effectiveness algorithms) in large populations [112].
- Electronic Medical Record (EMR) Data: Facilitates linkage of clinical metrics (e.g., CDAI) with treatment history [112].
- Patient Registry Databases: Rich sources for longitudinal clinical and patient-reported outcome data [112].
- Single-Center Retrospective Cohorts: Enable detailed characterization of specialized patient populations and treatment sequencing [114] [115].
Experimental Protocol: Quantifying JAK-STAT Pathway Activation
The following protocol, adapted from a prospective observational study in ulcerative colitis, details the methodology for quantifying JAK-STAT pathway activation in human tissue biopsies [26] [13].
Objective: To quantify and compare the phosphorylation levels of JAK-STAT pathway components in inflamed versus non-inflamed colonic mucosa from UC patients.
Materials and Reagents:
- Lysis Buffer: 50 mM Tris, 150 mM NaCl, 5 mM EDTA, supplemented with protease and phosphatase inhibitors.
- Primary Antibodies: Specific, validated phospho-specific antibodies against p-JAK1, p-JAK2, p-JAK3, p-TYK2, p-STAT1, p-STAT3, p-STAT4.
- Secondary Antibody: HRP-linked anti-rabbit antibody.
- Detection: Enhanced chemiluminescence (ECL) substrate.
- Loading Control: HRP-conjugated anti-β-actin antibody.
Procedure:
- Sample Collection: Obtain paired biopsies from endoscopically inflamed (Mayo Endoscopic Score > 0) and non-inflamed (MES = 0) colonic mucosa during routine colonoscopy. Pseudo-anonymize and store at -80°C.
- Protein Extraction:
- Mechanically digest and sonicate tissue samples in lysis buffer.
- Centrifuge lysates at 10,000 x g for 10 minutes.
- Collect supernatant and determine protein concentration using a standardized assay (e.g., DC protein assay).
- Western Blotting:
- Separate 20 µg of total protein per sample by SDS-PAGE (e.g., 4-12% Bis-Tris Plus gels).
- Transfer proteins to a PVDF membrane.
- Block membrane with 5% BSA.
- Incubate with primary antibody overnight at 4°C.
- Wash membrane and incubate with HRP-linked secondary antibody for 1 hour at room temperature.
- Detect protein bands using ECL substrate and image on a system like iBright CL1500.
- Strip membrane and re-probe for β-actin as a loading control.
- Repeat stripping and incubation for each phospho-protein target.
- Data Analysis:
- Perform quantitative band density analysis using ImageJ software.
- Normalize the integrated density of each phospho-protein band to the corresponding β-actin band.
- Compare normalized phosphorylation levels between inflamed and non-inflamed tissue using paired statistical tests (e.g., Wilcoxon signed-rank test). A p-value < 0.05 is considered significant.
Figure 2: Experimental Workflow for JAK-STAT Activation Analysis. This diagram outlines the key steps in the protocol, from tissue collection and protein extraction through Western blotting with sequential probing, to final densitometric and statistical analysis.
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for JAK-STAT Pathway Research
| Research Reagent | Specific Example | Function in Experimental Protocol |
|---|---|---|
| Phospho-Specific Antibodies | Anti-p-JAK2, Anti-p-STAT3 | Semiquantitative detection of activated (phosphorylated) pathway components by Western blot. Critical for assessing pathway status [26] [13]. |
| Protease & Phosphatase Inhibitors | Complete EDTA-free, PhosSTOP | Preserve the native phosphorylation state of proteins and prevent degradation during tissue lysis and protein extraction [26] [13]. |
| Protein Quantification Assay | DC Protein Assay | Accurately determine total protein concentration from tissue lysates to ensure equal loading across Western blot gels [26] [13]. |
| Enhanced Chemiluminescence Substrate | Pierce ECL Substrate | Enable sensitive detection of HRP-conjugated antibodies for visualization of protein bands on Western blots [26] [13]. |
| Loading Control Antibody | HRP-conjugated anti-β-actin | Verify consistent protein loading and transfer across lanes, serving as a reference for normalizing target protein expression levels [26] [13]. |
Long-term and real-world evidence solidifies the role of JAK inhibitors as effective therapeutic options across a spectrum of immune-mediated inflammatory diseases. Data from real-world practice confirm that JAKi improve clinical and patient-reported outcomes in RA, AA, and other IMIDs, while also providing insights into treatment patterns, persistence, and the value of switching strategies [112] [114] [113]. The safety profile of JAKi is well-characterized, enabling risk-aware clinical decision-making [104] [111]. Crucially, the integration of RWE with foundational science—such as the detailed profiling of JAK-STAT activation in ulcerative colitis revealing sex-dependent JAK2/STAT3 activation—paves the way for personalized therapeutic approaches [26] [13]. For researchers and drug developers, continued investigation into JAK selectivity, patient stratification biomarkers, and long-term outcomes in diverse populations remains essential to fully optimize the therapeutic potential of JAK inhibition.
Conclusion
The JAK-STAT pathway is unequivocally established as a master regulator of inflammation and a validated therapeutic target for a growing spectrum of diseases. The evolution from first-generation to more selective Jakinibs marks significant progress in improving the therapeutic window, though challenges regarding long-term safety and optimal patient selection remain. Future directions will be shaped by a deeper understanding of pathway complexity in different tissue contexts, the development of STAT-specific inhibitors, and the strategic use of Jakinibs in combination therapies. For researchers and drug developers, the continued unraveling of JAK-STAT biology promises a pipeline of increasingly precise and effective immunomodulatory drugs.
References
- 1. The JAK/STAT signaling pathway: from bench to clinic | Signal Transduction and Targeted Therapy [https://www.nature.com/articles/s41392-021-00791-1]
- 2. JAK-STAT Signaling Pathway - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/jak-stat-signaling-pathway]
- 3. JAK-STAT signaling pathway [https://en.wikipedia.org/wiki/JAK-STAT_signaling_pathway]
- 4. JAK-STAT Signal Pathway - Creative BioMart [https://www.creativebiomart.net/resource/signal-pathway-jak-stat-signal-pathway-389.htm]
- 5. JAK/STAT pathway: Extracellular signals, diseases, immunity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9995824/]
- 6. Cytokine-mediated communications: a quantitative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8126146/]
- 7. Jak/Stat Utilization Table [https://www.cellsignal.com/learn-and-support/reference-tables/jak-stat-utilization-table?srsltid=AfmBOorBTIZBMIqfwFXC1mcUc6ZG7yyvSLvdebndFFEqu1Rl8Ihe8t4b]
- 8. Redirecting immune signaling with cytokine adaptors [https://www.nature.com/articles/s41467-025-57681-1]
- 9. The JAK-STAT pathway: from structural biology to cytokine ... [https://www.nature.com/articles/s41392-024-01934-w]
- 10. JAK-STAT Signaling in Autoimmunity and Cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12080488/]
- 11. The role of JAK-STAT signaling pathway and its regulators in ... [https://biosignaling.biomedcentral.com/articles/10.1186/s12964-017-0177-y]
- 12. Biology and significance of the JAK/STAT signalling pathways [https://pmc.ncbi.nlm.nih.gov/articles/PMC3762697/]
- 13. Exploration of JAK/STAT pathway activation in ulcerative ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1609740/full]
- 14. Mechanisms and consequences of Jak-STAT signaling in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11565648/]
- 15. JAK/STAT Activation: A General Mechanism for Bone ... [https://www.mdpi.com/1422-0067/21/23/9004]
- 16. Modulating the JAK/STAT pathway with natural products [https://pmc.ncbi.nlm.nih.gov/articles/PMC12018655/]
- 17. JAK–STAT Signaling as a Target for Inflammatory and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7102286/]
- 18. The molecular details of cytokine signaling via the JAK/STAT ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6237706/]
- 19. Type I/II cytokines, JAKs, and new strategies for treating ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4688091/]
- 20. Mechanisms of type-I- and type-II-interferon-mediated ... [https://www.nature.com/articles/nri1604]
- 21. Insights into Cytokine–Receptor Interactions ... - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC4445396/]
- 22. Jak/Stat Utilization Table [https://www.cellsignal.com/learn-and-support/reference-tables/jak-stat-utilization-table?srsltid=AfmBOopCl5Ug6sw2JnCg6iW8J161yPit3Fpfdnz699GPzK2KQRX8qmmx]
- 23. Negative regulation of the JAK/STAT pathway [https://pubmed.ncbi.nlm.nih.gov/10070253/]
- 24. Negative regulation of cytokine signaling and immune ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1174965/]
- 25. Negative Regulators of the Jak/STAT Pathway [https://www.rndsystems.com/research-area/negative-regulators-of-the-jak-stat-pathway]
- 26. Exploration of JAK/STAT pathway activation in ulcerative ... [https://pubmed.ncbi.nlm.nih.gov/40761789/]
- 27. JAK-STAT pathway, type I/II cytokines, and new potential ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1563286/full]
- 28. SOCS modulates JAK-STAT pathway as a novel target to ... [https://www.sciencedirect.com/science/article/pii/S0361923024001217]
- 29. JAK-STAT signaling in inflammation and stress-related diseases [https://pmc.ncbi.nlm.nih.gov/articles/PMC10632324/]
- 30. Navigating the complexities of neuronal signaling and ... [https://www.sciencedirect.com/science/article/abs/pii/S0014299925001712]
- 31. The Role of the JAK/STAT Signaling Pathway in ... [https://www.mdpi.com/1422-0067/24/1/864]
- 32. An exhaustive examination of the research progress in ... [https://cmjournal.biomedcentral.com/articles/10.1186/s13020-025-01176-0]
- 33. targeting the JAK-STAT pathway and mast cell activation [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1621178/full]
- 34. Neuroinflammation is responsible for pain in endometriosis [https://pmc.ncbi.nlm.nih.gov/articles/PMC12425711/]
- 35. Small molecule drug discovery targeting the JAK-STAT ... [https://pubmed.ncbi.nlm.nih.gov/38777110/]
- 36. Evolving cognition of the JAK-STAT signaling pathway [https://www.nature.com/articles/s41392-023-01468-7]
- 37. Dysregulation of JAK-STAT pathway in hematological ... [https://biomarkerres.biomedcentral.com/articles/10.1186/2050-7771-1-5]
- 38. Selectivity, efficacy and safety of JAKinibs: new evidence for a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10850682/]
- 39. A Novel Selective JAK2 Inhibitor Identified Using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6288363/]
- 40. A Decade of Jakinibs: what have we learned and what may ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8671145/]
- 41. JAK inhibitors: Is specificity at all relevant? [https://www.sciencedirect.com/science/article/abs/pii/S0049017223001695]
- 42. Comprehensive disproportionality analysis of individual ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1629886/full]
- 43. Real-World Effectiveness and Safety of JAK Inhibitors in ... [https://pubmed.ncbi.nlm.nih.gov/40751489/]
- 44. Basic Mechanisms of JAK Inhibition - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC7361186/]
- 45. Topical Ruxolitinib and Delgocitinib Versus Systemic JAK ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12607478/]
- 46. Understanding the Mechanism of Action in JAK Inhibitors [https://www.dermatologytimes.com/view/understanding-the-mechanism-of-action-in-jak-inhibitors]
- 47. FDA-Approved JAK Inhibitors [https://www.naaf.org/navigation-toolkit/fda-approved-jak-inhibitors/]
- 48. JAK Inhibitors 101 [https://www.the-rheumatologist.org/article/jak-inhibitors-101/?singlepage=1]
- 49. An exhaustive examination of the research progress in ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12369162/]
- 50. targeting the JAK-STAT pathway and mast cell activation [https://pubmed.ncbi.nlm.nih.gov/40948761/]
- 51. Emerging Therapies in Myelofibrosis Could Extend Beyond ... [https://www.onclive.com/view/emerging-therapies-in-myelofibrosis-could-extend-beyond-jak-inhibitors]
- 52. Dual STAT3/STAT5 inhibition as a novel treatment strategy in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12133589/]
- 53. STAT Inhibitors Pipeline Market Landscape Report 2025 [https://finance.yahoo.com/news/stat-inhibitors-pipeline-market-landscape-100100382.html]
- 54. JAK-STAT pathway inhibitors in dermatology [https://www.anaisdedermatologia.org.br/en-jak-stat-pathway-inhibitors-in-dermatology-articulo-S0365059623001149]
- 55. JAK/STAT Pathway in Psoriasis and Psoriatic Arthritis [https://www.jdermis.com/full-text/jak-stat-pathway-in-psoriasis-and-psoriatic-arthritis-insights-into-inflammation-and-tissue-remodeling]
- 56. Label and off-label treatment of dermatological diseases ... [https://pubmed.ncbi.nlm.nih.gov/41178404/]
- 57. Newly Approved Specialty Drugs Advance Care for ... [https://www.pharmacytimes.com/view/newly-approved-specialty-drugs-advance-care-for-inflammatory-and-autoimmune-diseases]
- 58. Breakthroughs in autoimmune disease and cancer therapy [https://pubmed.ncbi.nlm.nih.gov/40782408/]
- 59. Comparative Safety of JAK Inhibitors vs TNF Antagonists in ... [https://pubmed.ncbi.nlm.nih.gov/40928778/]
- 60. Lestaurtinib's antineoplastic activity converges on JAK ... [https://www.nature.com/articles/s41698-025-00947-0]
- 61. Overcoming platinum-resistant ovarian cancer targeting the ... [https://www.nature.com/articles/s42003-025-08771-9]
- 62. Adverse events associated with JAK inhibitors in ... [https://www.nature.com/articles/s41598-022-10777-w]
- 63. A Populationâ€Based Study of Infectious Diseases Mortality ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11959415/]
- 64. Risk factors for invasive fungal infections in adult patients ... [https://www.nature.com/articles/s41598-025-16066-6]
- 65. Excessive activation of JAK-STAT signaling contributes to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11749392/]
- 66. Small molecule drug discovery targeting the JAK-STAT ... [https://www.sciencedirect.com/science/article/pii/S1043661824001610]
- 67. The JAK-STAT pathway: from structural biology to cytokine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11339341/]
- 68. JAK/STAT PATHWAY: MUTATIONS, INHIBITORS ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5021219/]
- 69. Comparative analysis of the JAK/STAT signaling through ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2648785/]
- 70. Molecular dissection of Janus kinases as drug targets for ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2022.1075192/full]
- 71. Real-time visualization of STAT activation in live cells using ... [https://www.nature.com/articles/s41589-025-02012-0]
- 72. JAK/STAT Signaling: Molecular Targets, Therapeutic ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2022.821344/full]
- 73. JAK inhibition as a therapeutic strategy for immune and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6168198/]
- 74. JAK inhibitors: an evidence-based choice of the most ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11570808/]
- 75. JAK inhibitors (JAKi): Mechanisms of action and ... [https://www.sciencedirect.com/science/article/pii/S0248866324012517]
- 76. Effects of Janus Kinase Inhibitors on Rheumatoid Arthritis Pain [https://pmc.ncbi.nlm.nih.gov/articles/PMC12562154/]
- 77. JAK Inhibitor Treatment Landscape 2025: Pipeline Drugs ... [https://www.barchart.com/story/news/35106445/jak-inhibitor-treatment-landscape-2025-pipeline-drugs-clinical-trials-insights-therapeutic-innovations-and-active-companies]
- 78. Key Trends Influencing the Growth of the Janus Kinase (JAK) [https://www.openpr.com/news/4182333/key-trends-influencing-the-growth-of-the-janus-kinase-jak]
- 79. JAK-STAT pathway at 30: much learned, much more to do - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9815833/]
- 80. Evaluating Current and Emergent JAK Inhibitors for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12454744/]
- 81. Clinical Trial Pipeline Appears Robust With 50+ Key... JAK Inhibitors [https://finance.yahoo.com/news/jak-inhibitors-clinical-trial-pipeline-180000168.html]
- 82. Comparative Efficacy and Safety of JAK Inhibitors in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11859343/]
- 83. Comparative efficacy of five approved Janus kinase ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2024.1387585/full]
- 84. MetaInsight v6.4.0 [https://crsu-metainsight.le.ac.uk/MetaInsight/]
- 85. Data visualisation approaches for component network meta ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-023-02026-z]
- 86. Comparative Safety of JAK Inhibitors vs TNF Antagonists in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12423869/]
- 87. Visualizing-meta-analysis-advanced-plots-and-interactive- ... [https://www.enago.com/academy/visualizing-meta-analysis-advanced-plots-and-interactive-tools/]
- 88. Systemic Janus kinase inhibitors in inflammatory dermatoses [https://www1.racgp.org.au/ajgp/2025/november/systemic-janus-kinase-inhibitors-in-inflammatory-d]
- 89. Cardiovascular Risks Similar for JAK Inhibitors & bDMARDs [https://www.the-rheumatologist.org/article/cardiovascular-risks-similar-for-jak-inhibitors-bdmards/]
- 90. Safety of JAK inhibitors: a real-life multicenter retrospective ... [https://www.jrheum.org/content/early/2023/07/25/jrheum.2023-0145]
- 91. Equal Safety of JAK Inhibitors and TNF Inhibitors [https://rheumnow.com/news/equal-safety-jak-inhibitors-and-tnf-inhibitors]
- 92. Pharmacogenomics of TNF inhibitors [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1521794/full]
- 93. Comparative Efficacy and Safety of Different Regimens ... [https://pubmed.ncbi.nlm.nih.gov/40184480/]
- 94. 5-YEAR RESULTS FROM THE PHASE 3 SELECT-PsA 1 ... [https://www.sciencedirect.com/science/article/abs/pii/S0003496725022435]
- 95. Effectiveness and Safety of Upadacitinib in Treating ... [https://pubmed.ncbi.nlm.nih.gov/41191276/]
- 96. Effectiveness and Safety of Upadacitinib in Treating ... [https://link.springer.com/article/10.1007/s40744-025-00802-5]
- 97. Long-term tofacitinib efficacy and safety in psoriatic arthritis ... [https://pubmed.ncbi.nlm.nih.gov/40241921/]
- 98. Efficacy and safety of tofacitinib in an open-label, long-term ... [https://arthritis-research.biomedcentral.com/articles/10.1186/s13075-024-03442-2]
- 99. Positive Trial Results with Filgotinib in Psoriatic Arthritis ... [https://www.gilead.com/news/news-details/2018/positive-trial-results-with-filgotinib-in-psoriatic-arthritis-and-ankylosing-spondylitis-both-published-in-the-lancet]
- 100. FRI0343 EFFICACY AND SAFETY OF FILGOTINIB, A ... [https://www.sciencedirect.com/science/article/abs/pii/S0003496724679185]
- 101. Small Molecules, Big Results: How JAK Inhibitors Have ... [https://link.springer.com/article/10.1007/s10620-024-08792-0]
- 102. Comparative real-world effectiveness and safety of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12592040/]
- 103. The use of Janus kinase inhibitors to treat noninfectious ... [https://www.nature.com/articles/s41433-025-04065-w]
- 104. Safety of Janus kinase inhibitors in immune-mediated ... [https://www.sciencedirect.com/science/article/pii/S0003496725000809]
- 105. Research Trends and Hotspots in JAK Inhibitors for Ulcerative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12539411/]
- 106. Janus kinase inhibitors for alopecia areata: a review of ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1577115/full]
- 107. Safety profile and dose-dependent adverse events of ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1598972/full]
- 108. Comparative short-term efficacy of Janus kinase 1 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12375639/]
- 109. Safety profile of JAK inhibitors in inflammatory or ... [https://www.sciencedirect.com/science/article/pii/S0248866325006514]
- 110. Enabling precision medicine with biomarkers of response ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1574697/full]
- 111. New Insights on Janus Kinase Inhibitors (JAKi) in Immune ... [https://innere-med-3.meduniwien.ac.at/en/our-departments/rheumatologie/news/14052025-new-insights-on-janus-kinase-inhibitors-jaki-in-immune-mediated-inflammatory-diseases/]
- 112. Evaluation of Real-World Evidence to Assess Effectiveness ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11724667/]
- 113. Real-World Evidence Confirms the Benefits of JAK ... [https://www.ajmc.com/view/real-world-evidence-confirms-the-benefits-of-jak-inhibitors-in-patients-with-rheumatoid-arthritis]
- 114. Real-world Effectiveness and Safety of Janus Kinase ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11995430/]
- 115. Real-world Effectiveness and Safety of JAK Inhibitors in ... [https://reumatologiaclinica.org/en-real-world-effectiveness-safety-jak-inhibitors-articulo-S1699258X21001893]