Longitudinal In Vivo Bioluminescence Imaging of Inflammation: Techniques, Applications, and Optimization for Preclinical Research
Longitudinal in vivo bioluminescence imaging (BLI) has emerged as a powerful non-invasive technology for monitoring inflammatory processes in real-time within living organisms.
Longitudinal In Vivo Bioluminescence Imaging of Inflammation: Techniques, Applications, and Optimization for Preclinical Research
Abstract
Longitudinal in vivo bioluminescence imaging (BLI) has emerged as a powerful non-invasive technology for monitoring inflammatory processes in real-time within living organisms. This comprehensive review explores the foundational principles, methodological applications, optimization strategies, and validation approaches for BLI in inflammation research. We examine how BLI enables researchers to track spatial and temporal dynamics of immune responses, distinguish between acute and chronic inflammation phases, and evaluate therapeutic efficacy in disease models ranging from infectious diseases to cancer and autoimmune disorders. By synthesizing current methodologies and addressing common technical challenges, this article provides researchers and drug development professionals with practical insights for implementing robust BLI protocols in preclinical studies, ultimately facilitating more efficient therapeutic development and reducing animal usage through longitudinal study designs.
Understanding Bioluminescence Imaging: Core Principles and Biological Basis of Inflammation Monitoring
Bioluminescence imaging (BLI) has become an indispensable tool for longitudinal in vivo studies of inflammatory processes, enabling non-invasive monitoring of biological phenomena in live animal models. This technology relies on the enzymatic reaction between luciferase enzymes and their substrates (luciferins) to produce light without the need for external excitation. Unlike fluorescence imaging, BLI offers near-zero background, superior signal-to-noise ratio, and high sensitivity for deep-tissue imaging, making it particularly valuable for tracking inflammation over time [1] [2]. The fundamental principle involves luciferase-catalyzed oxidation of luciferin, requiring oxygen and sometimes co-factors like ATP, resulting in an excited-state intermediate that emits light upon returning to its ground state [3] [1]. This application note details the core mechanisms, optimized protocols, and practical implementation of BLI for inflammation research, providing scientists with the foundational knowledge needed to design robust longitudinal studies.
Fundamental Reaction Mechanisms and Systems
Core Biochemical Reaction
The bioluminescence reaction is a biochemical process where luciferase catalyzes the oxidation of a luciferin substrate, leading to photon emission. The general reaction requires three key components: the enzyme luciferase, the substrate luciferin, and molecular oxygen (O₂). Some systems additionally require cofactors such as adenosine triphosphate (ATP) and Mg²⺠ions [3] [1] [4]. The reaction mechanism proceeds through several key steps:
- Activation: Luciferin is adenylated by ATP in the active site of luciferase, forming luciferyl-adenylate.
- Oxidation: The adenylated intermediate reacts with molecular oxygen, forming a high-energy, cyclic dioxetanoine intermediate.
- Light Emission: The decomposition of this intermediate produces excited-state oxyluciferin, which emits light as it returns to its ground state [3] [5].
The color of the emitted light is determined by the structure of the oxyluciferin and the specific luciferase enzyme, with emission spectra ranging from blue to red [5].
Major Bioluminescence Systems and Their Characteristics
While numerous bioluminescent systems exist in nature, a few have been optimized and are widely used in biomedical research. The table below summarizes the key features of the primary systems applied in inflammation imaging.
Table 1: Characteristics of Major Bioluminescence Systems
| System | Luciferase Source | Luciferin | Cofactors Required | Peak Emission Wavelength | Key Features & Applications |
|---|---|---|---|---|---|
| Firefly (Fluc) | Photinus pyralis (Firefly) | D-Luciferin | ATP, Mg²âº, Oâ‚‚ | 550-620 nm (pH-dependent) [3] [1] | High quantum yield; glow-type kinetics; ideal for deep-tissue imaging due to yellow-red light [3] [1]. |
| Click Beetle | Pyrophorus plagiophthalamus | D-Luciferin | ATP, Mg²âº, Oâ‚‚ | 537-593 nm [3] | Tolerant to broad pH range; engineered variants emit different colors for multiplexing [3]. |
| Renilla (Rluc) | Renilla reniformis (Sea pansy) | Coelenterazine | Oâ‚‚ | ~480 nm [3] [1] | Small, cytosolic enzyme; flash-type kinetics; does not require ATP [3] [1]. |
| Gaussia (Gluc) | Gaussia princeps (Copepod) | Coelenterazine | Oâ‚‚ | ~480 nm [3] [1] | Naturally secreted; very bright; high thermostability; flash-type kinetics [3] [1]. |
| NanoLuc (Nluc) | Oplophorus gracilirostris (Shrimp) | Furimazine (engineered coelenterazine) | Oâ‚‚ | ~460 nm [3] | Small size (19 kDa); exceptionally bright; high stability; useful for protein-protein interaction studies [3]. |
Diagram 1: Core luciferase-luciferin reaction pathway leading to light emission.
Quantitative Data and Kinetics for Experimental Design
Understanding the kinetic properties of different luciferase systems is critical for designing sensitive and reproducible experiments, especially for quantifying inflammatory responses over time.
Table 2: Kinetic Parameters and Operational Characteristics for Experimental Planning
| Luciferase | Reaction Kinetics | Optimal Substrate Administration for In Vivo Imaging | Signal Peak & Duration | Key Considerations |
|---|---|---|---|---|
| Firefly (Fluc) | Glow-type [1] | Intraperitoneal (IP) injection of D-luciferin (150 mg/kg) [1] | Peaks at ~10 min; stable for ~30 min [1] | Signal is ATP-dependent; light output can be used to monitor cellular metabolic activity [3]. |
| Renilla (Rluc) / Gaussia (Gluc) | Flash-type [1] | Intravenous (IV) injection of coelenterazine [1] | Peaks within seconds; rapid decay [1] | Imaging must be performed immediately after substrate injection. Coelenterazine has poor aqueous solubility [1]. |
| NanoLuc (Nluc) | Not specified in results | Not specified in results | Not specified in results | Very high brightness and stability; uses a synthetic furimazine substrate [3]. |
The firefly luciferase reaction follows Michaelis-Menten kinetics. The reaction rate and final light output are dependent on the concentrations of enzyme, substrate (D-luciferin), and essential co-factors (ATP, Mg²âº, Oâ‚‚) [4] [6]. It is important to note that the firefly luciferase reaction can be subject to product inhibition, where the accumulation of oxyluciferin or other byproducts can reduce light output over time [4]. Furthermore, ionizing radiation has been shown to affect the reaction rate, primarily by eliminating dissolved oxygen, with a dose constant for oxygen removal of approximately 70 Gy [4].
Application Protocol: Imaging Caspase-8 in Programmable Cell Death
Inflammation research often involves monitoring programmed cell death (e.g., apoptosis, pyroptosis). This protocol details the use of a Caspase-8-activated bioluminescence probe for sensitive in vivo imaging of this key inflammatory process [2].
Principle
The probe, Ac-IETD-Amluc, is designed to be "off" until it encounters activated Caspase-8, a key regulator of apoptosis and pyroptosis. The probe consists of:
- A tetrapeptide substrate (Ac-IETD) recognized and cleaved specifically by Caspase-8.
- A D-Aminoluciferin (Amluc) motif, which is a substrate for firefly luciferase (fLuc) but is caged and non-emissive in the intact probe.
Upon cleavage by Caspase-8, the Amluc motif is released. In cells expressing fLuc, the free Amluc is oxidized, producing a bioluminescence signal that reports the location and activity of Caspase-8 [2].
Reagents and Materials
Table 3: Key Reagents for Caspase-8 Activation Imaging
| Reagent / Material | Function / Description |
|---|---|
| Ac-IETD-Amluc Probe | Caspase-8-activated bioluminescent probe; the core diagnostic agent. |
| Firefly Luciferase (fLuc) | Reporting enzyme; can be expressed in cells via stable or transient transfection. |
| Cisplatin or other apoptogens | Chemical inducer of apoptosis (positive control). |
| D-Luciferin | Native substrate for firefly luciferase; used for background signal comparison. |
| In Vivo Imager | System equipped with a sensitive CCD camera for detecting low-light bioluminescence. |
Step-by-Step Procedure
- Cell Line Preparation: Use a cell line (e.g., 4T1 murine mammary carcinoma cells) stably expressing firefly luciferase (fLuc-4T1) [2].
- Apoptosis Induction: Treat fLuc-4T1 cells with cisplatin (e.g., 20 µM for 12 hours) to trigger Caspase-8-mediated apoptosis [2].
- In Vitro Validation:
- Incubate the Ac-IETD-Amluc probe (200 µM) with recombinant Caspase-8 (5 µg/mL) in reaction buffer (25 mM HEPES, 10 mM DTT, 0.1% CHAPS, pH 7.5) at 37°C for 1-2 hours [2].
- Confirm cleavage and light emission using a luminometer or imager.
- In Vivo Imaging:
- Establish tumors in animal models by injecting fLuc-4T1 cells.
- Induce apoptosis in vivo via systemic administration of cisplatin.
- Inject the Ac-IETD-Amluc probe intravenously into the subject.
- Acquire bioluminescence images using an in vivo imaging system. The signal generated is specific to the sites of Caspase-8 activation.
Data Interpretation and Analysis
The bioluminescence signal from the Ac-IETD-Amluc probe shows a linear relationship with Caspase-8 concentration (Y = 1.163 + 2.107X, R² = 0.96), with a calculated detection limit of 0.082 µg/L for Caspase-8 [2]. This quantitative relationship allows for longitudinal monitoring of changes in programmed cell death activity in response to therapeutic interventions.
Diagram 2: Caspase-8 probe activation pathway for imaging cell death.
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of bioluminescence imaging relies on a suite of reliable reagents and tools. The following table catalogs essential solutions for the field.
Table 4: Key Research Reagent Solutions for Bioluminescence Imaging
| Reagent / Kit | Function / Application |
|---|---|
| D-Luciferin (synthetic) [7] | Substrate for firefly and click beetle luciferases; essential for in vivo imaging with Fluc. |
| Coelenterazine (native & analogs) [1] | Substrate for Renilla, Gaussia, and NanoLuc luciferases. Analogs like Viviren and Enduren offer higher stability or sensitivity. |
| Caspase-8 Activated Probe (e.g., Ac-IETD-Amluc) [2] | Smart probe for specific detection of apoptosis/pyroptosis in vivo. |
| Recombinant Luciferases (Fluc, Rluc, Gluc, Nluc) [3] | Enzymes for in vitro assay development, probe validation, and standardization. |
| Stable Luciferase-Expressing Cell Lines | Ready-to-use cellular models for studying inflammation, cancer progression, and drug efficacy in vivo. |
| Bioluminescence-Compatible Matrigel | Medium for housing cells during subcutaneous tumor implantation, ensuring reliable bioluminescence signal development. |
| Methscopolamine bromide | Methscopolamine bromide, CAS:155-41-9, MF:C18H24BrNO4, MW:398.3 g/mol |
| Methylthiouracil | Methylthiouracil|Antithyroid Agent|CAS 56-04-2 |
The fundamental mechanisms of luciferase-luciferin reactions provide a powerful foundation for sensitive optical imaging in live animal models of inflammation. The D-luciferin-dependent firefly system remains a cornerstone for deep-tissue imaging due to its favorable emission wavelength and glow-type kinetics, while coelenterazine-dependent systems like NanoLuc offer exceptional brightness for highly sensitive applications. The development of activatable probes, such as the Caspase-8-sensitive Ac-IETD-Amluc, exemplifies how these fundamental principles can be leveraged to create specific molecular tools for monitoring key inflammatory processes like programmed cell death. By adhering to optimized protocols and understanding the kinetic properties of these systems, researchers can robustly apply bioluminescence imaging to longitudinally track disease progression and therapeutic responses in vivo, thereby accelerating drug development for inflammatory diseases.
Nuclear Factor-kappa B (NF-κB) represents a pivotal coordinator of innate and adaptive immune responses, functioning as a master regulator of inflammation and a critical molecular target in cancer biology. Initially identified in B lymphocytes, NF-κB is activated by a diverse range of stimuli including proinflammatory cytokines, bacterial and viral products, and cellular stresses [8] [9]. The reciprocal activation between NF-κB and inflammatory cytokines creates a fundamental signaling loop that drives inflammation-associated cancer development [8]. In cancer biology, NF-κB activation promotes cell survival, proliferation, and resistance to anticancer therapies, making it a promising target for therapeutic intervention [8] [9]. This application note details advanced methodologies for investigating NF-κB activation pathways and tracking immune responses, with particular emphasis on longitudinal in vivo bioluminescence imaging techniques that enable real-time monitoring of inflammatory processes in live animal models.
Molecular Composition and Activation Pathways of NF-κB
NF-κB Protein Family and Regulatory Components
The NF-κB signaling system consists of a sophisticated network of proteins and regulatory elements that collectively control its transcriptional activity:
NF-κB Transcription Factor Family: Five members form this family: p65 (RelA), RelB, c-Rel, p50/p105 (NF-κB1), and p52 (NF-κB2). These proteins contain a Rel homology domain (RHD) responsible for dimerization, DNA binding, and association with inhibitory IκB proteins. The p65, RelB, and c-Rel subunits possess C-terminal transactivation domains (TAD) that interact with transcriptional machinery, while p50 and p52 homodimers lacking TADs can function as transcriptional repressors [8] [9].
IκB Inhibitor Family: Seven known members (IκBα, IκBβ, IκBγ, IκBε, BCL-3, and precursor proteins p105 and p100) sequester NF-κB dimers in the cytoplasm through ankyrin repeat domains that mask nuclear localization signals. IκB proteins undergo signal-induced phosphorylation and degradation to activate NF-κB signaling [8] [9].
IKK Kinase Complex: The IκB kinase complex contains two catalytic subunits (IKKα/IKK1 and IKKβ/IKK2) and a regulatory subunit (IKKγ/NEMO). IKKβ serves as the primary catalytic subunit for the canonical pathway, while IKKα mediates the non-canonical pathway [8] [9].
NF-κB Activation Pathways
NF-κB activation occurs through distinct signaling pathways that respond to different extracellular stimuli:
Figure 1: NF-κB Activation Pathways. The diagram illustrates the canonical, non-canonical, and atypical NF-κB activation mechanisms in response to various stimuli.
Canonical (Classical) Pathway: This major activation route involves IKKβ-catalyzed phosphorylation of IκB proteins, particularly in response to proinflammatory cytokines (TNF-α, IL-1β) and cellular stresses. TNF-α binding to its receptor recruits IKK to the TNFR1 signaling complex through TRAF2 and RIP1. K63 ubiquitination of RIP by E3 ubiquitin ligases cIAP-1 and cIAP-2 creates a platform for IKK recruitment and activation via MEKK3 or TAK1-mediated phosphorylation. Activated IKKβ phosphorylates IκB at serine residues 32 and 36, triggering polyubiquitination and proteasomal degradation. This process exposes nuclear localization signals on p65 and p50, enabling nuclear translocation and activation of target genes [8] [9].
Non-canonical Pathway: Activated by specific TNF receptor family members (CD40, LTβ, BAF) and viral proteins such as Epstein-Barr virus LMP-1, this pathway depends on NF-κB-inducing kinase (NIK)-mediated activation of IKKα. Activated IKKα triggers phosphorylation and processing of p100 to p52, which then forms a transcriptionally active complex with RelB that translocates to the nucleus. Interestingly, cIAP proteins that promote the canonical pathway negatively regulate the non-canonical pathway by triggering NIK ubiquitination and degradation [8].
Atypical Pathways: Certain stimuli activate NF-κB through IKK-independent mechanisms. Short-wavelength UV light induces casein kinase 2 (CK2)-mediated phosphorylation and calpain-dependent IκB degradation, while hydrogen peroxide activates NF-κB through tyrosine phosphorylation of IκB at Tyr42 via c-Src or Syk kinases [8].
Quantitative Assessment of NF-κB Pathway Activity
Signal Transduction Pathway Activity Profiling
Recent technological advances enable quantitative measurement of NF-κB signaling activity in immune cells. The Simultaneous Transcriptome-based Activity Profiling of Signal Transduction Pathways (STAP-STP) technology simultaneously measures activity of nine relevant signal transduction pathways (including NF-κB) in immune cells based on mRNA analysis of target genes [10].
Table 1: Signal Transduction Pathway Activity in Resting vs. Activated Immune Cells
| Immune Cell Type | Activation State | NF-κB Pathway Activity | PI3K-FOXO Activity | JAK-STAT3 Activity | Key Activators |
|---|---|---|---|---|---|
| CD4+ T cells | Resting | Low | Low | Low | - |
| CD4+ T cells | Activated (Th1) | High | High | High | Anti-CD3/CD28, IL-12 |
| CD8+ T cells | Resting | Low | Low | Low | - |
| CD8+ T cells | Activated | Moderate | High | Moderate | Antigen-specific activation |
| B cells | Resting | Low | Low | Low | - |
| B cells | Activated | High | High | Moderate | Anti-IgM |
| Monocytes | Resting | Low | Low | Low | - |
| Monocytes | Activated | High | Moderate | High | TNF-α, IFN-α2a, IFN-γ |
| Macrophages | Resting | Low | Low | Low | - |
| Macrophages | Activated | High | Moderate | High | LPS (100 ng/mL) |
| Natural Killer cells | Resting | Low | Low | Low | - |
| Natural Killer cells | Activated | Moderate | High | High | IFN-α (1-100 ng/mL) |
| Dendritic cells | Resting | Low | Low | Low | - |
| Dendritic cells | Activated | High | Moderate | High | Newcastle Disease Virus |
This methodology reveals that each immune cell type displays a characteristic signal transduction pathway activity profile (SAP) that reflects both cell lineage and activation status. Analysis of rheumatoid arthritis patients using this technology demonstrated increased TGFβ pathway activity in whole blood samples, highlighting its clinical utility for monitoring immune dysfunction in inflammatory diseases [10].
Bioluminescence Imaging for NF-κB Activity Monitoring
Bioluminescence imaging (BLI) provides a noninvasive approach for longitudinal monitoring of NF-κB activation in live animal models. This technology utilizes transgenic mice carrying luciferase reporter genes under the control of NF-κB-responsive elements, enabling real-time assessment of inflammatory responses through in vivo imaging systems [11] [12].
Table 2: Bioluminescence Signal Intensity in Mouse Models of Inflammation
| Disease Model | Baseline Bioluminescence (photons/sec) | Peak Inflammation Bioluminescence (photons/sec) | Fold Increase | P-value | Imaging Time Post-Induction |
|---|---|---|---|---|---|
| Primed Mycobacterial Uveitis (PMU) | 1.47×10ⴠ| 1.46×10ⵠ| 9.9 | 0.01 | Day 2 |
| Endotoxin-Induced Uveitis (EIU) | 1.09×10ⴠ| 3.18×10ⴠ| 2.9 | 0.04 | 18 hours |
| Experimental Autoimmune Uveitis (EAU) | Not significant | Not significant | - | NS | Days 15-21 |
| Autoimmune Disease Model | Variable baseline | Significant increase in diseased organs | - | <0.05 | Preclinical phase |
The sensitivity of NF-κB bioluminescence imaging enables detection of subclinical disease activity before onset of clinical symptoms and autoantibody production. In autoimmune models, bioluminescence signals emerge from secondary lymphoid organs, inflamed intestines, skin lesions, and arthritic joints, correlating with disease progression and permitting evaluation of anti-inflammatory interventions [11].
Experimental Protocols for NF-κB Imaging and Immune Cell Tracking
Protocol: Longitudinal NF-κB Bioluminescence Imaging in Transgenic Mice
Purpose: To monitor NF-κB activation in real-time using transgenic mice with NF-κB-responsive luciferase reporters.
Materials:
- NF-κB-luciferase transgenic mice (FVB background)
- D-luciferin potassium salt (15 mg/mL in PBS)
- In Vivo Imaging System (IVIS Spectrum, PerkinElmer)
- Isoflurane anesthesia system
- Heating pad or IVIS warming stage
- Depilatory cream for hair removal
Procedure:
- Animal Preparation: Anesthetize mice using isoflurane (2.5-3% induction, 1.5-2% maintenance). Apply ophthalmic ointment to prevent corneal drying. Remove hair from imaging area using depilatory cream to minimize light absorption.
- Substrate Administration: Inject D-luciferin intraperitoneally (150 mg/kg body weight) using sterile technique. Alternatively, intravenous injection via tail vein provides brighter initial signal with more rapid decay.
- Image Acquisition: Place animals in IVIS chamber maintained at 37°C. Position animals to ensure optimal orientation for region of interest. Acquire images 10-15 minutes post-injection for peak signal intensity using field of view "A," subject height 1.5 cm, with medium binning for 5-minute exposure periods.
- Image Analysis: Quantify bioluminescence signal using Living Image software or similar platform. Draw regions of interest (ROI) around signal areas and calculate total flux (photons/second). Normalize values to baseline measurements.
- Longitudinal Timing: Perform imaging at consistent time points post-intervention. For acute inflammation models (EIU, PMU), image at 18-48 hours. For chronic models (EAU), monitor weekly for 3-4 weeks.
Technical Considerations:
- Intraperitoneal luciferin injection provides more stable signal than IV with peak at 10-15 minutes post-injection.
- Consistent positioning is critical for reproducible ROI analysis.
- Background subtraction using control regions ensures accurate quantification [13] [11] [14].
Protocol: Immune Cell Migration and Tracking Analysis
Purpose: To quantify immune cell migration dynamics using advanced computational tracking methods.
Materials:
- Time-lapse microscopy system with environmental control
- celltrackR R package (available on CRAN and GitHub)
- Immune cells of interest (T cells, dendritic cells, macrophages)
- Appropriate culture media and migration chambers
- Fluorescent labeling reagents (optional)
Procedure:
- Experimental Setup: Prepare immune cells in appropriate migration assay system (Boyden chamber, collagen matrix, or similar). Maintain constant temperature (37°C) and CO₂ (5%) throughout imaging.
- Image Acquisition: Capture time-lapse images at 30-60 second intervals for 2-4 hours using 10-20× objectives. Ensure adequate resolution for single-cell tracking while minimizing phototoxicity.
- Cell Tracking: Import image sequences into celltrackR package. Pre-process images to correct for drift and background noise. Use automated tracking algorithms to generate cell trajectories.
- Quality Control: Implement package quality control measures to identify and exclude tracking artifacts. Filter tracks based on duration and displacement thresholds.
- Migration Analysis: Calculate migration parameters including mean velocity, persistence, turning angle distribution, and confinement ratio. Compare experimental conditions using statistical methods provided in package.
- Data Visualization: Generate rose plots, displacement graphs, and track overlays to visualize migration patterns. Perform cluster analysis to identify distinct migration phenotypes.
Technical Considerations:
- celltrackR supports both 2D and 3D migration analysis
- The package includes simulation tools for modeling cell migration
- Method corrects for common imaging artifacts and biases [15]
Protocol: Assessment of Host-Biomaterial Interactions via NF-κB Imaging
Purpose: To evaluate inflammatory responses to implanted biomaterials using NF-κB bioluminescence imaging.
Materials:
- NF-κB-luciferase transgenic mice
- Biomaterial of interest (e.g., genipin-cross-linked gelatin conduit)
- Sterile surgical instruments
- D-luciferin substrate
- IVIS imaging system
Procedure:
- Biomaterial Preparation: Sterilize biomaterial implants according to established protocols. For infection modeling, immerse materials in LPS solution (100 ng/mL) for endotoxin exposure.
- Surgical Implantation: Anesthetize mice and perform aseptic implantation of biomaterials in subcutaneous dorsal pockets. Close incisions with sterile sutures or wound clips.
- Longitudinal Imaging: Image mice pre-implantation for baseline and at regular intervals post-implantation (days 1, 3, 7, 14). Follow standard bioluminescence imaging protocol with D-luciferin injection.
- Histological Correlation: Following final imaging time point, euthanize animals and harvest implant sites for histological analysis. Process tissues for H&E staining and immunohistochemistry using antibodies against luciferase and inflammatory markers.
- Data Correlation: Compare bioluminescence signals with histological evidence of inflammation (immune cell infiltration, tissue damage). Statistical analysis should correlate imaging data with conventional inflammation metrics.
Applications: This protocol enables real-time assessment of host-biomaterial interactions, evaluation of biocompatibility, and screening of anti-inflammatory biomaterial coatings [12].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents for NF-κB and Immune Cell Imaging
| Reagent/Material | Function/Application | Example Products/Specifications | Technical Considerations |
|---|---|---|---|
| Firefly Luciferase (FLuc) | Primary bioluminescent reporter for in vivo imaging | VivoGlo Luciferin, In Vivo Grade | ATP-dependent; peak emission 562 nm; ideal for tumor models |
| NanoLuc (NLuc) | Small, bright ATP-independent reporter | Nano-Glo Fluorofurimazine In Vivo Substrate (FFz) | 19kDa size; blue light (460 nm); better for surface imaging |
| Akaluc/AkaLumine | Red-shifted variant for enhanced tissue penetration | Akaluc/AkaLumine system | Improved tissue penetration; higher signal intensity |
| Renilla Luciferase (RLuc) | Multiplexing with other reporters | ViviRen In Vivo Renilla Luciferase Substrate | Coelenterazine substrate; blue light (480 nm); minimal cross-reactivity |
| NF-κB Transgenic Mice | In vivo model for inflammation imaging | NF-κB-RE-luciferase transgenic mice | FVB background; responsive to inflammatory stimuli |
| IVIS Imaging System | In vivo bioluminescence detection | PerkinElmer IVIS Spectrum | Cooled CCD camera; sensitive photon detection |
| celltrackR Software | Immune cell migration analysis | celltrackR R package | Open-source; 2D/3D track analysis; quality control features |
| LPS | Toll-like receptor agonist for inflammation induction | Lipopolysaccharide from E. coli | Typical concentration 100 ng/mL for in vitro studies |
| Recombinant Cytokines | Immune cell activation | TNF-α, IL-1β, IFN-γ | Concentration-dependent NF-κB activation |
| Methicillin | Methicillin, CAS:61-32-5, MF:C17H20N2O6S, MW:380.4 g/mol | Chemical Reagent | Bench Chemicals |
| Metioprim | Metioprim, CAS:68902-57-8, MF:C14H18N4O2S, MW:306.39 g/mol | Chemical Reagent | Bench Chemicals |
Advanced Applications and Future Directions
Emerging Imaging Technologies for Immunology Research
The field of immune imaging continues to evolve with several emerging technologies showing particular promise:
Multiplexed Bioluminescence Imaging: Simultaneous tracking of multiple biological processes using spectrally distinct luciferase reporters (e.g., FLuc and NLuc combination) enables more comprehensive understanding of immune responses. The key advantage lies in absent substrate cross-reactivity between these systems. Applications include monitoring CAR-T cell activity while simultaneously tracking tumor response, providing integrated assessment of immunotherapeutic efficacy [14].
Nanoparticle-Enhanced Imaging: Novel nanoparticle approaches are being developed to improve immune cell tracking precision. These systems facilitate monitoring of how immune cells target and attack cancer cells, particularly when combined with dendritic cell therapies that train the immune system to recognize cancer-specific antigens. Clinical trials are currently evaluating these approaches for boosting cancer immunotherapy [16].
Advanced Computational Analysis: New computational tools beyond celltrackR are emerging for deeper analysis of immune cell behavior. These include machine learning approaches for classifying cell migration patterns and predicting immune cell functions based on dynamic behavior. Integration with transcriptomic data (such as STAP-STP profiles) provides multidimensional insights into immune cell states [10] [17] [15].
Therapeutic Implications and Translational Applications
The methodologies described herein have significant implications for drug development and therapeutic assessment:
Cancer Therapeutics: NF-κB imaging enables evaluation of chemotherapeutic efficacy and resistance mechanisms. Since constitutive NF-κB activation blunts anticancer therapy effectiveness, these imaging approaches permit real-time assessment of NF-κB inhibitory compounds as potential chemosensitizers [8] [9].
Autoimmune Disease Monitoring: The capability to detect NF-κB activation before clinical symptom onset provides valuable opportunities for early therapeutic intervention in autoimmune conditions. This approach facilitates evaluation of anti-inflammatory drugs in preclinical models with enhanced translational potential [11].
Biomaterial Compatibility Screening: The noninvasive nature of NF-κB bioluminescence imaging allows efficient screening of biomaterial biocompatibility, accelerating development of medical implants and tissue engineering scaffolds with reduced inflammatory potential [12].
These advanced imaging and analysis protocols provide researchers with powerful tools for investigating inflammatory pathways, immune cell dynamics, and therapeutic interventions in longitudinal study designs that reduce animal usage while increasing data quality - aligning with the 3Rs principles of ethical animal research [13] [14].
In vivo bioluminescence imaging (BLI) is a powerful optical imaging technique that has become indispensable for modern biological research, enabling the non-invasive interrogation of living animals using light emitted from luciferase-expressing bioreporter cells [18]. This technology has been applied to study a wide range of biomolecular functions including gene expression, drug discovery and development, cellular trafficking, protein-protein interactions, tumorigenesis, cancer treatment, and disease progression [18]. Unlike conventional methods that require euthanizing groups of animals at multiple time points, BLI allows investigators to perform longitudinal studies by repeatedly imaging the same cohort of animals over time [19]. This review will focus on the significant advantages of longitudinal BLI for inflammation research, with particular emphasis on how this approach reduces animal numbers while enabling powerful within-subject study designs that account for individual variation and provide more comprehensive data throughout the disease course.
The Principle of Longitudinal Bioluminescence Imaging
Longitudinal BLI involves the repeated monitoring of biological processes in the same living animal over time through the detection of light emitted from luciferase-expressing cells or tissues. The fundamental components of this technology include luciferase enzymes and their respective substrates. When luciferase-expressing cells are introduced into an animal model, either through injection of engineered cells or by using animals carrying a luciferase transgene, subsequent administration of the appropriate substrate enables the visual tracking of biological activities in real time [14].
A key advantage of BLI over fluorescence imaging is that it does not require an external light source for excitation, which results in minimal background autofluorescence and a much higher signal-to-noise ratio [14]. This characteristic is particularly valuable for longitudinal studies as it enables sensitive detection of biological processes even in deep tissues, though signal penetration remains challenging for blue-emitting luciferases [18] [1].
The longitudinal imaging process typically involves several key steps: animal preparation (including anesthesia and potentially fur removal), substrate administration (usually via intraperitoneal or intravenous injection), image acquisition using a sensitive charge-coupled device (CCD) camera, and quantitative analysis of the bioluminescent signal [13] [14]. This workflow can be repeated multiple times in the same animal, allowing researchers to track dynamic biological processes without the need to sacrifice multiple animal cohorts at different time points.
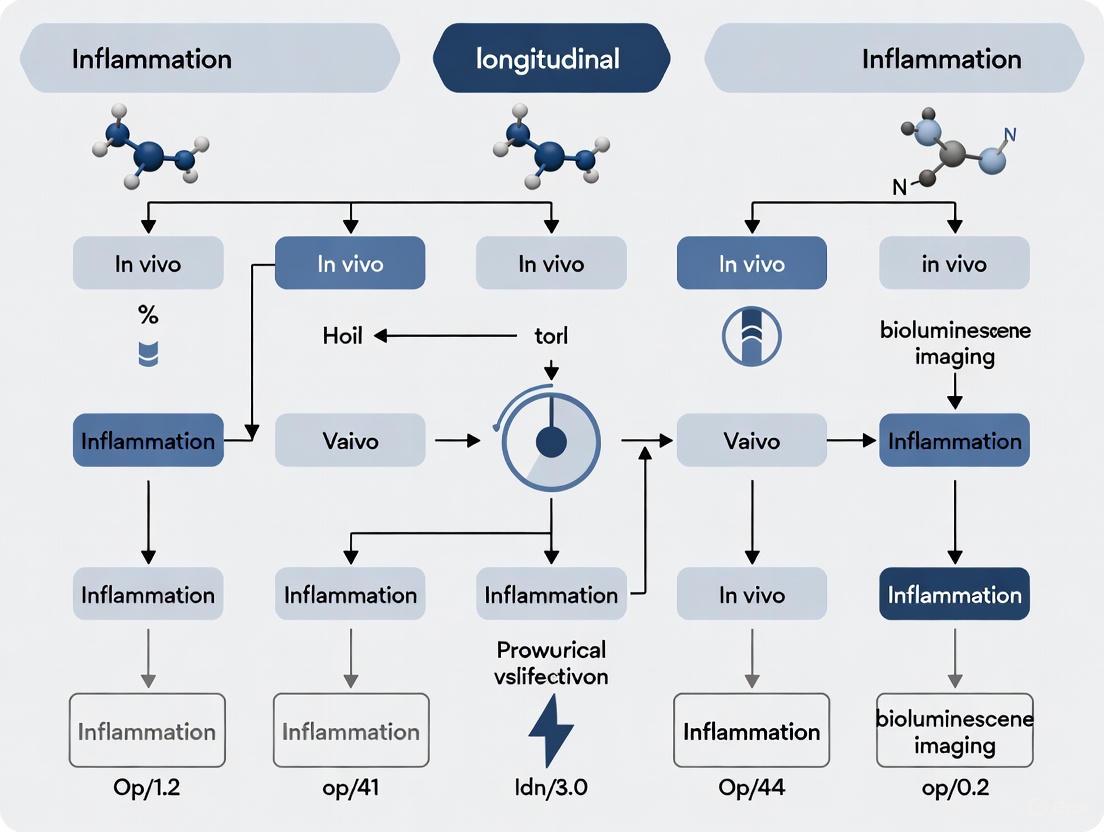
Figure 1: Workflow for longitudinal bioluminescence imaging studies. The same animals proceed through repeated imaging cycles, enabling within-subject monitoring of biological processes over time. IP = intraperitoneal; IV = intravenous; CCD = charge-coupled device.
Key Advantages of Longitudinal Imaging Designs
Reduction in Animal Numbers
Longitudinal BLI significantly reduces the number of animals required for well-powered experiments by enabling each subject to serve as its own control throughout the study duration. Traditional experimental designs necessitate separate animal cohorts for each time point, resulting in exponentially increasing animal requirements as more time points are added to the study [19]. In contrast, longitudinal imaging allows investigators to follow disease progression and therapeutic response in the same animals from baseline through peak response and resolution phases.
This approach directly aligns with the "3Rs" principle of animal research - Replacement, Reduction, and Refinement [14]. By reducing variability through within-subject comparisons and decreasing the total number of animals required, longitudinal BLI enhances both the ethical standards and statistical power of preclinical studies. The ability to monitor biological processes without euthanizing animals at intermediate time points has been particularly valuable in studies of dynamic processes such as inflammatory responses, where the timing of peak response may vary between individuals [13] [20].
Monitoring Dynamic Biological Processes
Longitudinal BLI provides unique insights into the temporal dynamics of disease progression and treatment response that would be impossible to capture with terminal endpoints. This capability is especially valuable in inflammation research, where immune responses evolve over time with distinct phases of activation, peak inflammation, and resolution.
In studies of uveitis, an inflammatory eye disease, researchers have successfully used longitudinal BLI to monitor intraocular inflammation in animal models over time. For example, one study demonstrated that bioluminescence signals in endotoxin-induced uveitis (EIU) peaked at 18 hours post-induction and returned to near baseline levels by 48 hours, providing a quantitative measure of inflammatory dynamics that correlated with clinical observations [13]. Similarly, in primed mycobacterial uveitis (PMU) models, bioluminescence imaging detected significant increases in photon flux at peak inflammation (1.46 × 10^5 photons/second) compared to baseline (1.47 × 10^4 photons/second, P = 0.01) [13].
The ability to track these dynamic processes in individual animals allows researchers to identify unexpected patterns of disease progression or treatment response that might be missed when analyzing separate cohorts at predetermined time points [19]. This feature is particularly important for understanding complex inflammatory conditions where response timing may vary substantially between individuals.
Enhanced Data Quality Through Within-Subject Controls
Longitudinal imaging designs enhance data quality by using each animal as its own control, thereby reducing inter-animal variability and increasing statistical power. Traditional between-subject designs are confounded by inherent biological variation between individuals, requiring larger sample sizes to detect significant effects. In contrast, within-subject comparisons minimize this variability by tracking changes relative to baseline measurements in the same animal [18].
This advantage was demonstrated in a study of cell-type-specific inflammation in uveitis, where researchers generated transgenic mouse lines expressing luciferase in specific immune cell populations (myeloid cells, T cells, and B cells) [20]. By performing serial bioluminescence imaging for 35 days following uveitis induction, they were able to document distinct temporal patterns of immune cell infiltration: acute inflammation (day 2) was predominantly neutrophilic, followed by a T cell-dominated phase (day 7), and later B cell involvement (day 28 onward) [20]. This sophisticated characterization of immune dynamics would have been extremely challenging with terminal endpoints, requiring substantially more animals to achieve the same temporal resolution.
Quantitative Data from Longitudinal BLI Studies
Table 1: Representative quantitative data from longitudinal BLI studies in inflammation research
| Disease Model | Measurement Time Points | Baseline Signal (photons/sec) | Peak Signal (photons/sec) | Signal Return to Baseline | Reference |
|---|---|---|---|---|---|
| Primed Mycobacterial Uveitis (PMU) | Day 0, Day 2 | 1.47 × 10^4 | 1.46 × 10^5 (Day 2) | Not reported | [13] |
| Endotoxin-Induced Uveitis (EIU) | 0, 18, 48 hours | 1.09 × 10^4 | 3.18 × 10^4 (18 hours) | 48 hours | [13] |
| Experimental Autoimmune Uveitis (EAU) | Days 0, 15, 21 | Not reported | Nonsignificant increase | Not applicable | [13] |
| Myeloid Cell Inflammation (PMU model) | Weekly for 35 days | Baseline levels established on Day 0 | Significant increase on Day 2 | Return to baseline by Day 7 | [20] |
| T Cell Inflammation (PMU model) | Weekly for 35 days | Baseline levels established on Day 0 | Significant increase on Day 7 | Sustained through Day 35 | [20] |
| B Cell Inflammation (PMU model) | Weekly for 35 days | Baseline levels established on Day 0 | Significant increase starting Day 28 | Sustained through Day 35 | [20] |
Table 2: Comparison of bioluminescent reporters for longitudinal imaging
| Luciferase Reporter | Origin | Emission Peak | Substrate | Cofactors | Kinetics | Advantages for Longitudinal Studies |
|---|---|---|---|---|---|---|
| Firefly Luciferase (FLuc) | Photinus pyralis | 562 nm | D-luciferin | ATP, Mg²âº, Oâ‚‚ | Glow | Stable signal, optimal for longitudinal tracking [18] [21] |
| NanoLuc (NLuc) | Engineered | 460 nm | Furimazine | None | Glow | Small size, brightness, ATP-independent [14] |
| Renilla Luciferase (RLuc) | Renilla reniformis | 480 nm | Coelenterazine | Oâ‚‚ | Flash | Compatible with multiplexing [18] [14] |
| Gaussia Luciferase (GLuc) | Gaussia princeps | 480 nm | Coelenterazine | None | Flash | Secreted nature allows detection in blood [22] [21] |
| Bacterial Luciferase (Lux) | Vibrio species | 490 nm | None (autonomous) | NADPH, Oâ‚‚ | Glow | No substrate injection required [18] |
Detailed Experimental Protocol for Longitudinal BLI in Inflammation Research
Animal Preparation and Uveitis Induction
This protocol is adapted from established models of uveitis [13] [20] and provides a framework for longitudinal BLI studies of ocular inflammation.
- Animals: C57BL/6 albino mice (6-8 weeks old, female)
- Uveitis Models:
- Primed Mycobacterial Uveitis (PMU): Subcutaneous injection of 100 μg killed Mycobacterium tuberculosis H37Ra antigen in incomplete Freund's adjuvant, followed 7 days later by intravitreal injection of 3.5-5 μg Mycobacterium tuberculosis antigen in 1 μL PBS into the right eye.
- Endotoxin-Induced Uveitis (EIU): Intravitreal injection of 1 μL of 125 ng/μL lipopolysaccharide (LPS) in PBS into the right eye.
- Experimental Autoimmune Uveitis (EAU): Subcutaneous injection of 500 μg interphotoreceptor retinoid binding protein peptide (IRBP1-20) in complete Freund's adjuvant on day 0, plus intraperitoneal pertussis toxin (0.15 μg) on days 0 and 2.
Bioluminescence Imaging Procedure
- Imaging System: PerkinElmer In Vivo Imaging System (IVIS) Spectrum or equivalent
- Substrate Administration:
- Anesthesia: 2-3% isoflurane in oxygen throughout imaging procedure
- Image Acquisition:
- Field of view: "A"
- Subject height: 1.5 cm
- Binning: Medium
- Acquisition time: 1-5 minutes (optimize based on signal strength)
- Imaging time points: Baseline (before uveitis induction), then regularly throughout disease course (e.g., days 1, 2, 7, 14, 21, 28, 35)
- Image Analysis:
- Use Living Image software or equivalent
- Define regions of interest (ROIs) over inflamed eyes and background regions
- Quantify total flux (photons/second) for each ROI
- Subtract background signal from measured values
- Normalize to baseline measurements where appropriate
Validation Methods
- Clinical Scoring: Anterior chamber and posterior chamber inflammation scores according to established criteria [20]
- Optical Coherence Tomography: For objective assessment of ocular structural changes
- Histology: Post-mortem validation of inflammatory cell infiltration
- Flow Cytometry: Characterization of immune cell populations in inflamed tissues [20]
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential research reagents for longitudinal BLI studies
| Reagent Category | Specific Examples | Function/Application | Key Considerations |
|---|---|---|---|
| Luciferase Reporters | Firefly luciferase (FLuc), NanoLuc (NLuc), Renilla luciferase (RLuc) | Engineered into cells or animals to enable bioluminescence detection | Consider emission wavelength, kinetics, and substrate requirements for longitudinal studies [18] [14] |
| Luciferase Substrates | D-luciferin, Furimazine, Coelenterazine | Chemical reactants that generate light when processed by luciferase enzymes | Administration route (IP vs. IV) affects signal kinetics and intensity [14] [1] |
| Imaging Systems | IVIS Spectrum (PerkinElmer), other CCD-based systems | Detect and quantify bioluminescent signals from living animals | Cooled CCD cameras reduce thermal noise for sensitive detection [18] [13] |
| Animal Models | Transgenic reporter mice, cell line xenografts | Provide context for studying biological processes | Cell-type-specific reporters enable monitoring of specific immune populations [20] [19] |
| Anesthesia Equipment | Isoflurane delivery systems with nose cones | Maintain animal immobilization during imaging | Proper anesthesia is essential for image quality and animal welfare [13] |
| Analysis Software | Living Image Software, other quantification tools | Process and quantify bioluminescence image data | Enable background subtraction and signal quantification in defined ROIs [13] |
| Metoprine | Metoprine, CAS:7761-45-7, MF:C11H10Cl2N4, MW:269.13 g/mol | Chemical Reagent | Bench Chemicals |
| Metribuzin | Metribuzin Herbicide|Research Grade | Bench Chemicals |
Longitudinal bioluminescence imaging represents a transformative approach for inflammation research that simultaneously advances both scientific rigor and ethical standards in preclinical studies. By enabling researchers to track dynamic biological processes in the same animals over time, this technology reduces inter-animal variability, decreases the number of animals required for statistically powerful experiments, and provides unique insights into disease progression and treatment response that would be impossible to obtain through traditional terminal endpoints. As BLI technology continues to evolve with improvements in luciferase reporters, imaging equipment, and analytical methods, its application in longitudinal study designs will undoubtedly expand, further enhancing our understanding of inflammatory processes and accelerating the development of novel therapeutic strategies.
Bioluminescence imaging (BLI) has emerged as a preeminent, non-invasive modality for longitudinal monitoring of biological processes in live animal models of disease and therapy development [1] [23]. This technology leverages the enzymatic reaction between luciferase enzymes and their substrates (luciferins) to produce visible light, enabling real-time visualization of everything from bacterial infection and inflammatory responses to the progression of chronic metabolic diseases [14] [24]. A core advantage of BLI is its capacity for longitudinal study design, allowing researchers to track disease pathogenesis or therapeutic response in the same cohort of animals over time, which enhances statistical power, reduces animal usage, and provides critical insights into dynamic biological timelines [13] [25]. This application note details key biological uses of BLI, supported by specific protocols and quantitative data, framed within the context of inflammation research.
Key Applications of In Vivo Bioluminescence Imaging
Monitoring Inflammatory Responses in Uveitis Models
BLI enables direct, longitudinal quantification of intraocular inflammation, as demonstrated in studies of experimental autoimmune uveitis (EAU), endotoxin-induced uveitis (EIU), and primed mycobacterial uveitis (PMU) [13]. In these models, inflammation is detected via luminol, a substrate that emits light (λmax = 425 nm) upon oxidation by hypochlorous acid, a product of myeloperoxidase activity within activated neutrophils infiltrating the site [13]. This application provides a non-lethal, quantifiable alternative to terminal endpoints like histology.
Table 1: Bioluminescence Signal at Peak Inflammation in Mouse Uveitis Models
| Disease Model | Peak Bioluminescence (photons/second) | Baseline Bioluminescence (photons/second) | P-value |
|---|---|---|---|
| Primed Mycobacterial Uveitis (PMU) | 1.46 x 10âµ | 1.47 x 10â´ | P = 0.01 |
| Endotoxin-Induced Uveitis (EIU) | 3.18 x 10â´ | 1.09 x 10â´ | P = 0.04 |
| Experimental Autoimmune Uveitis (EAU) | Non-significant increase | - | - |
Source: Data adapted from [13].
Key findings from these studies show that acute models with robust anterior inflammation (PMU and EIU) demonstrate significant changes in bioluminescence corresponding with peak inflammation, while the more indolent posterior uveitis of the EAU model generates a more modest signal [13]. The bioluminescence signal in EIU returned to near-baseline levels by 48 hours, highlighting the utility of BLI for tracking kinetic profiles [13].
Tracking Bacterial Infections and Antibiotic Efficacy
BLI is indispensable for studying bacterial pathogenesis and evaluating novel antimicrobial therapies in vivo. Research commonly employs engineered, bioluminescent bacteria (e.g., E. coli) to establish infections, allowing for real-time monitoring of bacterial load and spatial distribution without sacrificing the animal [25]. This approach was validated in a urinary tract infection (UTI) model, where the bioluminescent signal was strongly correlated with the bacterial burden determined by the traditional serial-plating method (colony-forming units, or CFU) [25].
Table 2: Correlation Between BLI Signal and Bacterial Burden
| Imaging Metric | Correlation with CFU | Application in Drug Development |
|---|---|---|
| Surface Light Intensity | Semi-quantitative; affected by depth and tissue properties | Screening for antibiotic efficacy |
| 3D Tomographic Reconstruction (BLt) | Quantitative; enables calculation of CFU mmâ»Â³ in specific organs | Determining in vivo bacterial organ load and pharmacokinetic/pharmacodynamic studies |
Source: Data adapted from [25].
Advanced tools like InVivoPLOT, which combines a body-conforming animal mold (BCAM) with bioluminescence tomography (BLt) and an organ probability map, now allow for fully automated, operator-independent quantification of bacterial density within deep-set organs like the kidneys [25].
Modeling Metabolic Syndrome and Diabetes
In metabolic research, BLI is used to monitor dynamic processes such as pancreatic β-cell mass and function in models of Type 2 diabetes [24]. Transgenic mice, such as the MIP-Luc model, express firefly luciferase under the control of the mouse insulin promoter (MIP), restricting expression to pancreatic β-cells [24]. The bioluminescence signal intensity from the pancreatic region shows a strong positive correlation with β-cell mass, enabling non-invasive tracking of its expansion in response to a high-fat diet or its decline following streptozotocin (STZ)-induced ablation [24].
Interrogating Gene Regulation and Signaling Pathways
Reporter systems where luciferase expression is driven by specific promoter elements (e.g., NF-κB response elements) allow for the in vivo study of signal transduction and gene regulation [26] [1]. For instance, the effect of Gram-negative bacterial lipopolysaccharide (LPS, endotoxin) on HIV-1 LTR-driven transcription was visualized in transgenic reporter mice, revealing organ-specific induction of the NF-κB pathway [26]. Similarly, the activity of specific promoters can be imaged to study processes like stem cell differentiation or the activity of cell signaling pathways in cancer [1].
Detailed Experimental Protocols
Protocol 1: Longitudinal Monitoring of Ocular Inflammation
This protocol is adapted from a study investigating uveitis in mouse models [13].
Research Reagent Solutions
| Item | Function | Example/Specification |
|---|---|---|
| Luminol Sodium Salt | Chemiluminescent substrate for myeloperoxidase | Sigma Life Science; 200 mg/kg in PBS [13] |
| C57BL/6 Albino Mice | Animal model; absence of melanin reduces light absorption | Jackson Laboratories [13] |
| IVIS Spectrum Imager | Captures and quantifies bioluminescent signal | PerkinElmer [13] |
| Living Image Software | Analyzes total flux (photons/second) | PerkinElmer [13] |
| Inhaled Isoflurane | Anesthesia for animal immobilization during imaging | Veterinary grade [13] |
Methodology:
- Animal Preparation: Induce uveitis in C57BL/6 albino mice (e.g., for EIU, via intravitreal injection of 125 ng LPS). Use albino strains to minimize light absorption by pigment [13].
- Substrate Administration: Ten minutes before imaging, administer an intraperitoneal (IP) injection of luminol sodium salt at a dose of 200 mg/kg [13].
- Anesthesia and Positioning: Anesthetize the animal with inhaled isoflurane. Dilate eyes with topical phenylephrine (2.5%) and apply a lubricating ophthalmic gel to prevent corneal drying. Position the animal in lateral decubitus with the ocular surface directly facing the camera sensor [13].
- Image Acquisition: Capture images using an IVIS Spectrum system with field of view "A," subject height of 1.5 cm, and medium binning. Acquire a sequence of 5-minute images starting 10 minutes post-luminol injection [13].
- Data Analysis: Using Living Image software, define a region of interest (ROI) around the eye. Quantify the signal as total flux (photons/second) and subtract background signal from a reference ROI. Compare longitudinal data to baseline (day 0) measurements [13].
Protocol 2: Firefly Luciferase-Based Tumor Cell Imaging
This is a standard protocol for monitoring tumor growth and metastasis using firefly luciferase-expressing cells [23] [14] [27].
Research Reagent Solutions
| Item | Function | Example/Specification |
|---|---|---|
| D-Luciferin, K⺠Salt | Substrate for Firefly luciferase | Promega VivoGlo; 150 mg/kg in PBS [14] [27] |
| Firefly Luciferase (FLuc) Cells | Reporter cells for tumor burden | Stable expression via lentiviral transduction [23] |
| CCD Camera System | Detects low-light bioluminescence | Cooled CCD camera (e.g., IVIS) [23] [14] |
| Insulin Syringe | For precise substrate injection | Lo-dose B-D 1/2 cc 28G1/2 [23] |
Methodology:
- Cell Implantation: Implant firefly luciferase-expressing tumor cells (e.g., via subcutaneous or orthotopic injection) into immunocompromised or syngeneic mice [23].
- Substrate Administration: Inject D-luciferin intraperitoneally at a standard dose of 150 mg/kg. The IP route is preferred for its ease and signal stability, with peak emission occurring approximately 10 minutes post-injection [14] [27].
- Image Acquisition: Anesthetize mice with isoflurane. Acquire images 10-15 minutes after D-luciferin injection. Use auto-exposure settings or a series of exposures (e.g., 5 seconds to 5 minutes) to ensure signals are within the camera's linear range without saturation [27].
- Data Analysis: Quantify the tumor burden by measuring the total flux (photons/second) within an ROI drawn over the tumor signal. For longitudinal studies, image animals from the same position and at a consistent time after substrate injection to ensure comparability [23] [27].
Visualizing Experimental Workflows and Pathways
Endotoxin-Induced NF-κB Activation Pathway
Diagram Title: Endotoxin-Induced NF-κB Activation Pathway
Longitudinal BLI Experimental Workflow
Diagram Title: Longitudinal BLI Experimental Workflow
In the field of longitudinal in vivo imaging for inflammation research, selecting the appropriate optical imaging technique is paramount for data accuracy and experimental success. This application note provides a detailed comparison between fluorescence imaging and bioluminescence imaging (BLI), focusing on two critical parameters: signal-to-noise ratio (SNR) and tissue penetration depth. For researchers tracking inflammatory processes over time, understanding these fundamental differences ensures reliable data collection and interpretation in studies involving animal models of disease, drug efficacy testing, and mechanistic investigations.
Technical Comparison: SNR and Penetration Depth
Fundamental Mechanisms and Their Implications
The core distinction between these modalities lies in their physical mechanisms for light generation, which directly influences their performance.
Fluorescence Imaging requires an external light source to excite fluorescent molecules (fluorophores). The emitted light is then detected to form an image. A significant challenge is that the excitation light can be scattered and absorbed by tissues, and it can also cause autofluorescence from endogenous molecules, generating a substantial background signal that reduces the SNR [28] [14]. Furthermore, the excitation light itself is subject to tissue absorption and scattering, which limits the effective penetration depth [29].
Bioluminescence Imaging (BLI) is an auto-illuminating process. It relies on luciferase enzymes (e.g., firefly luciferase) oxidizing a substrate (e.g., D-luciferin). This biochemical reaction produces visible light without the need for external excitation. The absence of exciting light virtually eliminates issues related to autofluorescence and light scattering, resulting in a very high SNR [14]. This makes BLI exceptionally sensitive for detecting low numbers of cells or weak biological signals deep within an animal.
The table below synthesizes key performance characteristics based on current literature and reagent specifications.
Table 1: Comparative Performance of Fluorescence and Bioluminescence Imaging
| Feature | Fluorescence Imaging | Bioluminescence Imaging |
|---|---|---|
| Background Signal | High (due to tissue autofluorescence under external light) [28] | Extremely low (no external excitation, minimal tissue autofluorescence) [14] |
| Typical SNR | Lower; can be enhanced by advanced algorithms (e.g., ~8% increase with lock-in processing) [30] | Inherently very high |
| Penetration Depth | Limited by scattering/absorption of excitation and emission light | Superior for deep-tissue imaging; limited primarily by emission light absorption |
| Key Reporter | Green Fluorescent Protein (GFP), FITC, others | Firefly Luciferase (FLuc), NanoLuc (NLuc) |
| Emission Peak | Varies by fluorophore (e.g., ~515 nm for FITC) [28] | FLuc: ~562 nm [14]; NLuc: ~460 nm [14] |
| Optimal Wavelength | >600 nm for better penetration | >600 nm for better penetration [14] |
| Substrate/Kinetics | N/A | D-luciferin (for FLuc); time-to-peak and signal duration depend on dose and route [31] |
Table 2: Bioluminescence Reporter Systems
| Reporter | Substrate | Emission Peak | Key Characteristics | Best For |
|---|---|---|---|---|
| Firefly Luciferase (FLuc) | D-luciferin | 562 nm [14] | ATP-dependent, yellow-green light, many pre-engineered cell lines [14] | Tracking tumor progression, ATP-dependent processes [14] |
| NanoLuc (NLuc) | Furimazine (FFz) | 460 nm [14] | Small size (19 kDa), very bright, ATP-independent, short exposure times [14] | Viral reporters, protein fusions, tracking exosomes [14] |
| Akaluc/AkaLumine | AkaLumine | Red-shifted [14] | Engineered FLuc variant for better tissue penetration and higher signal [14] | Deep-tissue imaging where signal intensity is critical [14] |
| Click Beetle Luciferase | D-luciferin | Red (~615 nm) [29] | Naturally red-shifted emission | Enhanced tissue penetration [29] |
Diagram 1: Decision workflow for selecting between fluorescence and bioluminescence imaging for longitudinal inflammation studies.
Optimized Protocol for Longitudinal BLI of Inflammation
This protocol is optimized for sensitivity and reproducibility in monitoring inflammatory processes in the brain, based on the work by Aswendt et al. [31], and can be adapted for other tissues.
Reagent and Material Preparation
Research Reagent Solutions
| Item | Specification | Function/Purpose |
|---|---|---|
| D-Luciferin | Potassium salt, in vivo grade (e.g., VivoGlo) [14] | Substrate for firefly luciferase (FLuc); oxidized to produce light. |
| Luciferase-Expressing Cells | Stable transfection or transgenic animal (e.g., DCX-Luc mice) [31] | Biological source of the luciferase reporter enzyme. |
| Anesthetic | Isoflurane (e.g., 3% for induction, 1.5-2% for maintenance) [31] | Ensures animal immobility during image acquisition. |
| Sterile PBS | Phosphate-buffered saline, pH 7.4 | Vehicle for dissolving D-Luciferin substrate. |
| Depilatory Cream | Commercial hair removal cream | Removes fur from the imaging area to minimize light absorption and scattering. |
Step-by-Step Procedure
Substrate Injection:
- Prepare a stock solution of D-Luciferin at a concentration of 30 mg/mL in sterile PBS.
- Inject D-Luciferin intraperitoneally (IP) at a dose of 300 mg/kg body weight [31]. Note: Intravenous (IV) injection provides a faster and brighter initial signal but decays rapidly and is more technically challenging [14] [31].
- The higher dose of 300 mg/kg has been shown to provide a significant signal gain (~200%) compared to the standard 150 mg/kg dose for brain imaging, without reaching saturation [31].
Anesthesia Induction:
- Wait for 5 minutes post-injection. This is a critical step, as injecting the substrate before anesthesia induction leads to significantly higher and more stable bioluminescence signals [31].
- After the 5-minute wait, induce anesthesia with 3% Isoflurane in an induction chamber.
Animal Preparation:
- Transfer the animal to the imaging chamber, maintaining anesthesia with 1.5-2% Isoflurane delivered via a nose cone.
- Apply depilatory cream to the skin over the region of interest (e.g., the head for brain imaging). Leave it on for about 1 minute, then gently wipe it off and clean the area with a damp paper towel to ensure no residue remains. This step drastically improves light transmission.
Image Acquisition:
- Position the animal in the bioluminescence imager (equipped with a cooled CCD camera) in a supine or lateral position, depending on the target tissue.
- Begin image acquisition 10-15 minutes after the D-Luciferin injection, as this is typically when the signal peaks for IP administration [31]. Acquire a series of images with exposure times ranging from 1 second to 5 minutes to ensure the signal is within the dynamic range of the camera and not saturated.
- Maintain a constant temperature on the imaging stage (e.g., 37°C) to ensure animal welfare and stable physiological conditions.
Diagram 2: Step-by-step workflow for the optimized in vivo BLI protocol.
Data Analysis and SNR Calculation
- Regions of Interest (ROI): Draw an ROI around the signal source (e.g., the brain) and an identical ROI over a background region (e.g., the shoulder or an area with no expected signal).
- Quantification: Use the imaging software to calculate the total flux (photons/second) or average radiance (p/s/cm²/sr) within each ROI.
- SNR Calculation: Calculate the Signal-to-Noise Ratio using the formula: ( SNR = \frac{\text{Mean Signal}{\text{ROI}} - \text{Mean Background}{\text{ROI}}}{\text{Standard Deviation}_{\text{Background}}} ) This optimized protocol has been demonstrated to lower the detection limit from 6,000 to 3,000 luciferase-expressing cells grafted in the mouse brain, directly due to a gain in the SNR [31].
Advanced SNR Enhancement Techniques for Fluorescence Imaging
For experimental scenarios where fluorescence imaging is necessary (e.g., for high temporal resolution or multiplexing), several advanced techniques can be employed to mitigate its inherent SNR limitations.
- Digital Lock-In Algorithm: This method modulates the light sources (e.g., white and near-infrared) at specific frequencies. The acquired images are then demodulated to separate the signal from the background noise. This technique has been shown to increase the SNR of white light and fluorescent images by 8.2% and 6.7%, respectively, in a fluorescence endoscope system [30].
- Total Internal Reflection Fluorescence (TIRF) and Substrate Optimization: Using microfluidic chips fabricated on silicon-on-insulator (SOI) substrates instead of conventional silicon wafers creates an ultra-flat surface. This minimizes light scattering and angle-dependent filter issues, reducing the fluorescent background signal by ~5 times and improving the SNR for single-molecule detection by more than 18 times [28].
- Fluorescence Lifetime Imaging (FLIM): FLIM uses the characteristic time a fluorophore remains in its excited state (lifetime) to generate contrast, rather than relying solely on intensity. This lifetime is independent of fluorophore concentration and probe intensity, making it highly sensitive to the molecular microenvironment (e.g., pH, ion concentration) and immune to many artifacts that plague intensity-based measurements. It is particularly powerful when combined with Förster Resonance Energy Transfer (FRET) to study protein-protein interactions [32] [33] [34].
The choice between bioluminescence and fluorescence imaging for longitudinal inflammation studies involves a direct trade-off between sensitivity and versatility.
- Bioluminescence Imaging is the superior choice for quantitative, high-sensitivity tracking of specific cell populations or molecular pathways over time in live animals, especially when targets are located in deep tissues. Its inherently low background provides an excellent SNR, which is critical for reliable longitudinal monitoring.
- Fluorescence Imaging is indispensable for studies requiring real-time kinetics, high spatial resolution, or the simultaneous monitoring of multiple targets (multiplexing). While its SNR is generally lower, advanced techniques like FLIM and lock-in processing can significantly enhance its performance.
The optimized BLI protocol outlined here, featuring a higher D-Luciferin dose (300 mg/kg) and pre-anesthesia injection, provides a robust methodological framework for maximizing data quality in preclinical inflammation research and drug development.
Practical Implementation: BLI Protocols for Specific Inflammatory Conditions and Disease Models
Non-invasive bioluminescence imaging (BLI) enables longitudinal assessment of inflammation in live animal models. This application note details the use of two chemiluminescent probes—luminol and lucigenin—to distinguish between acute and chronic inflammatory phases by detecting distinct oxidative burst activities in neutrophils and macrophages. Luminol bioluminescence specifically detects myeloperoxidase (MPO) activity during neutrophil-mediated acute inflammation, whereas lucigenin bioluminescence relies on phagocyte NADPH oxidase (Phox) activity in macrophages during chronic phases. We provide validated protocols, quantitative data, and mechanistic insights to support the application of these probes in preclinical research.
Inflammation is a fundamental biological response involved in a wide range of pathological conditions, including microbial infection, wound healing, diabetes, cancer, and autoimmune diseases [35]. The inflammatory process requires coordinated recruitment and activation of various immune cells, primarily neutrophils in the acute phase and macrophages in the chronic phase [36] [35]. Non-invasive imaging methods that can distinguish between these cellular phases provide powerful tools for quantitative longitudinal assessment of disease progression and therapeutic intervention.
Bioluminescence imaging (BLI) with chemiluminescent substrates enables real-time, non-invasive visualization of specific biological processes in live animals. Luminol (5-amino-2,3-dihydro-1,4-phthalazinedione) and lucigenin (bis-N-methylacridinium nitrate) are two well-characterized probes that react with distinct reactive oxygen species (ROS) produced by different phagocyte populations [36] [35]. This technical note details the underlying mechanisms, optimized protocols, and applications of these probes for distinguishing neutrophil-dominated acute inflammation from macrophage-dominated chronic inflammation in vivo.
Background and Mechanisms
The Phagocytic Oxidative Burst in Inflammation
Phagocyte NADPH oxidase (Phox) is the primary source of superoxide production in both neutrophils and macrophages [35]. During phagocytosis, neutrophils assemble the Phox holoenzyme at phagosomal membranes, where it consumes oxygen to produce superoxide anion in a rapid burst known as the "respiratory burst" [35]. The biochemical environment and subsequent reactive oxygen species differ significantly between neutrophil and macrophage phagocytes:
- Neutrophils: Contain high levels of myeloperoxidase (MPO), which constitutes approximately 5% of neutrophil dry weight [37]. MPO catalyzes the conversion of hydrogen peroxide to highly bactericidal hypochlorous acid (HOCl) [37] [35].
- Macrophages: Have lower MPO expression and assemble Phox primarily at the plasma membrane rather than in phagosomes, producing superoxide at lower levels for regulatory functions [35].
Probe Specificity and Mechanisms
Table 1: Comparison of Luminol and Lucigenin Specificity
| Parameter | Luminol | Lucigenin |
|---|---|---|
| Primary Cellular Target | Neutrophils | Macrophages |
| Key Enzymatic Requirement | Myeloperoxidase (MPO) | Phagocyte NADPH Oxidase (Phox) |
| Reactive Species Detected | Hypochlorous acid (HOCl), other MPO-derived oxidants | Superoxide anion (O₂•â») |
| Specificity Evidence | Abolished in MPO-deficient mice despite neutrophil infiltration [37] | Dependent on Phox activity; independent of MPO [36] |
| Optimal Imaging Window | 5-25 minutes post-injection [37] [13] | 1-15 minutes post-injection [35] |
Figure 1: Mechanism of Luminol and Lucigenin Specificity for Neutrophils and Macrophages
Research Reagent Solutions
Table 2: Essential Research Reagents for Inflammation Imaging
| Reagent | Composition/Preparation | Storage | Function |
|---|---|---|---|
| Luminol Sodium Salt | 10 mg/ml in sterile normal saline (0.9% NaCl) [35] | -20°C | MPO-dependent detection of neutrophil activity |
| Lucigenin | 2.5 mg/ml in sterile normal saline [35] | -20°C | Phox-dependent detection of macrophage activity |
| PMA (Phorbol 12-myristate 13-acetate) | 5 mg/ml in DMSO, dilute to 1 mg/ml in PBS before use [35] | -20°C | Potent protein kinase C activator for phagocyte stimulation |
| LPS (Lipopolysaccharide) | 1 mg/ml in sterile PBS [35] | -20°C | Toll-like receptor agonist for inflammation induction |
| 4-ABAH (4-aminobenzoic acid hydrazide) | 0-500 μM in appropriate buffer [37] | -20°C | Selective MPO inhibitor for specificity controls |
Signal Characteristics and Detection Parameters
Table 3: Quantitative Imaging Parameters for Inflammation Probes
| Parameter | Luminol | Lucigenin |
|---|---|---|
| Optimal Dosage | 100-200 mg/kg [13] [35] | 10-25 mg/kg [35] |
| Signal Peak Time | 20-25 minutes post-stimulation [37] | Within 15 minutes post-injection [35] |
| Signal Intensity Range | 30-40-fold over background [37] | Model-dependent |
| Sensitivity | <5 × 10³ phagocytes in 1 μl whole blood [37] | Model-dependent |
| Inhibition IC₅₀ | 4-ABAH: 1.0 ± 0.7 μM (purified MPO), 50 ± 15 μM (whole blood) [37] | Phox inhibitor-dependent |
Application Across Disease Models
Table 4: Probe Performance in Preclinical Inflammation Models
| Disease Model | Luminol Signal | Lucigenin Signal | Key Findings |
|---|---|---|---|
| Acute Dermatitis | Significant increase at peak inflammation [37] | Not reported | Luminol bioluminescence colocalized with histological inflammation sites [37] |
| Focal Arthritis | Significant increase at peak inflammation [37] | Not reported | MPO-dependent signal abolished in Mpo−/− mice [37] |
| Endotoxin-induced Uveitis (EIU) | 3.18 × 10ⴠp/s at peak vs 1.09 × 10ⴠp/s baseline (P = 0.04) [13] | Not reported | Signal returned to baseline by 48 hours [13] |
| Subcutaneous PMA | Robust acute signal [35] | Limited acute signal [35] | Distinction between acute (luminol) and chronic (lucigenin) phases |
| Subcutaneous LPS | Early acute signal [35] | Sustained chronic signal [35] | Temporal transition from neutrophil to macrophage dominance |
Experimental Protocols
Subcutaneous Inflammation Models
PMA-Induced Inflammation
Figure 2: PMA-Induced Inflammation Model Workflow
PMA Solution Preparation: Prepare stock solution at 5 mg/ml in DMSO. Store at -20°C. Before inoculation, thaw and dilute to 1 mg/ml in PBS [35].
Animal Preparation: Anesthetize mice in an induction chamber with 1-2% isoflurane. Confirm general anesthesia by loss of movement and constant respiratory rate [35].
Injection Procedure:
- Clean and disinfect injection site on left flank with isopropyl alcohol wipe
- Using sterile technique, inject 50 μl of PMA inoculation solution (containing 50 μg of PMA) into subcutaneous space
- Remove excess fluid with isopropyl alcohol pad
- Avoid analgesia as it may affect inflammatory responses [35]
Post-Injection Care:
- Return animal to housing cage and monitor recovery from anesthesia
- Use heating pad to maintain body temperature during recovery [35]
LPS-Induced Inflammation
LPS Solution Preparation: Dissolve lipopolysaccharide (LPS from Salmonella enterica serotype enteritidis) in sterile PBS at 1 mg/ml prior to subcutaneous inoculation [35].
Footpad Injection:
- Anesthetize C57BL/6J mice with 1-2% isoflurane
- Clean injection site on left footpad with isopropyl alcohol wipe
- Inject 50 μl of LPS solution (containing 50 μg of LPS) into left footpad
- Remove excess fluid from injection site [35]
Bioluminescence Imaging Protocol
Substrate Administration:
- Anesthetize animal with 1-2% isoflurane
- Intraperitoneally inject either:
- Luminol solution (10 mg/ml, final dosage 100 mg/kg) for acute inflammation imaging, OR
- Lucigenin solution (2.5 mg/ml, final dosage 25 mg/kg) for chronic inflammation imaging [35]
- Note: C57BL/6J strain has lower lucigenin tolerability; consider lower dose (10-15 mg/kg) to avoid toxicity [35]
Imaging Parameters:
- Transfer animal to imaging chamber of bioluminescence imaging system
- Perform sequential imaging at 1 min intervals
- Each imaging step: 1 min acquisition time, f/stop = 1, binning = 16, 0 sec delay
- Program 15 one-minute steps to determine maximal luminescence output [35]
Post-Processing and Analysis:
- Use imaging software to calculate peak total bioluminescent signal through standardized regions of interest (ROI)
- Present images as radiance in photons/sec/cm²/sr with minimal and maximal threshold indicated
- Quantitative data presented as total flux in photons per second per ROI [35]
Specificity Controls and Validation
MPO Inhibition:
- Use 4-aminobenzoic acid hydrazide (4-ABAH) at concentrations of 0-500 μM to inhibit MPO activity [37]
- Confirm MPO-dependence with significant signal reduction
Genetic Controls:
- Utilize Mpo−/− mice to verify luminol specificity [37]
- Compare wild-type and knockout responses to confirm MPO-dependent signaling
Cellular Infiltration Validation:
Applications in Disease Models
The luminol/lucigenin imaging approach has been successfully applied across multiple disease models, demonstrating its versatility for inflammatory process assessment:
Ocular Inflammation Models
In endotoxin-induced uveitis (EIU), luminol bioluminescence significantly increased at peak inflammation (3.18 × 10ⴠp/s) compared to baseline (1.09 × 10ⴠp/s, P = 0.04), returning to near baseline levels by 48 hours [13]. This rapid kinetics aligns with neutrophil infiltration patterns in acute ocular inflammation.
Longitudinal Monitoring of Inflammation Phases
The combination of luminol and lucigenin enables non-invasive tracking of inflammatory phase transitions. In subcutaneous inflammation models, luminol detects early neutrophil activity (0-48 hours), while lucigenin identifies subsequent macrophage activity (48+ hours), allowing complete longitudinal assessment without sacrificing animals [36] [35].
Troubleshooting and Technical Considerations
- Low Signal-to-Noise Ratio: Optimize substrate dosage and imaging timing. Luminol typically peaks 20-25 minutes post-stimulation [37]
- Probe Toxicity: Monitor animals for respiratory distress, particularly with lucigenin in C57BL/6J mice [35]
- Signal Specificity: Always include appropriate controls (MPO inhibitors, genetic controls) to verify signal specificity [37]
- Background Signal: Distinguish true inflammatory signal from background by careful ROI selection and background subtraction [13] [20]
The combination of luminol and lucigenin bioluminescence imaging provides researchers with a powerful methodology for non-invasive distinction between acute neutrophil-dominated and chronic macrophage-dominated inflammation. The specific protocols and quantitative data presented herein enable robust application across preclinical models, facilitating longitudinal assessment of inflammatory progression and therapeutic efficacy in live animals.
NF-κB Activation Monitoring in Pulmonary Inflammation Models Using Transgenic Reporter Mice
Nuclear factor-κB (NF-κB) is a pivotal transcription factor that regulates inflammatory responses and is a major pathogenic feature of various inflammatory diseases, including acute lung injury (ALI) and acute respiratory distress syndrome (ARDS) [38] [39]. Monitoring the spatiotemporal dynamics of NF-κB activation in live animal models is crucial for understanding inflammatory pathogenesis and evaluating anti-inflammatory therapies. Transgenic reporter mice enable non-invasive, longitudinal monitoring of NF-κB activity, providing insights into complex inflammatory processes in pulmonary inflammation models that traditional endpoint measurements cannot capture [38] [40].
This application note details the use of cutting-edge transgenic reporter mice and optimized protocols for monitoring NF-κB activation in preclinical models of pulmonary inflammation, with a focus on LPS-induced lung injury.
Reporter Mouse Models for NF-κB Imaging
The selection of an appropriate reporter mouse model is fundamental to the success of in vivo NF-κB imaging studies. The table below compares the key reporter systems available.
Table 1: Key Features of NF-κB Reporter Mouse Models
| Reporter Model | Detection Method | Key Features | Advantages | Limitations |
|---|---|---|---|---|
| NF-κB-Luc (Bioluminescence) [38] | Bioluminescence Imaging (BLI) | Expresses luciferase under NF-κB response elements. | Non-invasive, suitable for longitudinal whole-body imaging, high signal-to-noise ratio. | Limited spatial resolution; substrate pharmacokinetics can influence signal. |
| Fluorescent Knockin (e.g., mEGFP-RelA, mScarlet-c-Rel) [40] | Fluorescence Imaging (Flow Cytometry, Microscopy) | Endogenous loci of RelA or c-Rel tagged with fluorescent proteins (e.g., mEGFP, mScarlet). | Single-cell resolution, accurate endogenous expression, enables dynamic live-cell imaging, no substrate needed. | Requires tissue extraction for high-resolution analysis (except intravital imaging). |
| KappaBle (ROSA26 Knock-in) [41] | Fluorescence Imaging (Flow Cytometry) | Knock-in of destabilized EGFP at the ROSA26 locus for sensitive NF-κB activity reporting. | Sensitive, dynamic monitoring at single-cell level, low background. | Fluorescence limitations for deep-tissue in vivo imaging. |
Experimental Protocols for Pulmonary Inflammation Models
LPS-Induced Acute Lung Injury Model
Principle: Intratracheal administration of lipopolysaccharide (LPS) mimics bacterial infection by activating Toll-like receptor 4 (TLR4), leading to robust NF-κB-driven inflammation and lung injury [39].
Materials:
- Animals: NF-κB-Luc reporter mice or similar (C57BL/6 background, 8-12 weeks old).
- Reagents: LPS (e.g., from E. coli O111:B4), sterile phosphate-buffered saline (PBS), isoflurane, anesthetic equipment.
Procedure:
- Anesthetize mice using isoflurane (e.g., 3-4% for induction, 1-2% for maintenance).
- Suspend LPS in sterile PBS. A typical dose for inducing ALI is 2.5 mg/kg [39].
- Administer LPS via intratracheal instillation.
- Position the anesthetized mouse on an intubation stand.
- Gently extract the tongue and visualize the glottis.
- Using a calibrated micropipette with a sterile tip, instill the LPS solution (e.g., 50 µL) directly into the trachea.
- Return mice to their cages with free access to food and water. Monitor animals closely post-procedure.
In Vivo Bioluminescence Imaging of NF-κB Activation
Materials:
- Substrate: D-luciferin, 15 mg/mL in PBS [38].
- Equipment: In vivo bioluminescence imaging system (e.g., Ami X, VISQUE InVivo ART100), isoflurane anesthesia system.
Procedure:
- Administer Substrate: At the desired time points post-LPS challenge (e.g., 2h, 6h, 24h), inject D-luciferin intraperitoneally (i.p.) at a standard dose of 150 mg/kg (e.g., 100 µL of 15 mg/mL solution for a 20g mouse) [38].
- Anesthetize mice using isoflurane and place them in the imaging chamber.
- Acquire Image: Initiate image acquisition 5-10 minutes after luciferin injection. A typical exposure time is 1-60 seconds, depending on signal strength [38].
- Analyze Data: Quantify the bioluminescence signal intensity from the thoracic region using the region of interest (ROI) tools in the imaging software. Express data as total flux (photons/second) or average radiance (p/s/cm²/sr).
Cell-Type-Specific NF-κB Analysis using NF-κB-Luc:[Cre] Mice
Principle: Crossing NF-κB-Luc reporter mice with cell-type-specific Cre recombinase mice (e.g., Lyz2-Cre for macrophages) allows for precise monitoring of NF-κB activity in specific immune cell populations [38].
Procedure:
- Generate NF-κB-Luc:[Cre] mice by crossing NF-κB-Luc mice with Cre-driver lines (e.g., Lyz2-Cre for myeloid cells).
- Induce pulmonary inflammation as described in Section 3.1.
- Perform bioluminescence imaging as in Section 3.2 to track NF-κB activation specifically within the targeted cell lineage.
Signaling Pathway and Workflow
The following diagram illustrates the core signaling pathway in LPS-induced NF-κB activation and the corresponding experimental workflow for its monitoring.
Diagram 1: NF-κB Signaling Pathway and Experimental Workflow for Monitoring LPS-Induced Pulmonary Inflammation.
The Scientist's Toolkit: Essential Research Reagents
The table below lists key reagents and their applications for monitoring NF-κB in pulmonary inflammation models.
Table 2: Essential Research Reagents for NF-κB Imaging in Lung Inflammation
| Reagent / Tool | Function / Target | Example Application in Research |
|---|---|---|
| NF-κB-Luc Reporter Mice [38] | Reports integrated NF-κB pathway activity via bioluminescence. | Longitudinal, non-invasive monitoring of global NF-κB activation in LPS-induced lung injury. |
| mEGFP-RelA / mScarlet-c-Rel Knockin Mice [40] | Labels endogenous NF-κB subunits for fluorescence-based tracking. | High-resolution, single-cell analysis of RelA and c-Rel dynamics in specific lung cell populations. |
| LPS (Lipopolysaccharide) [39] | TLR4 agonist; induces potent inflammatory response and NF-κB activation. | Gold standard for modeling bacterial infection-induced acute lung injury and inflammation. |
| D-Luciferin [38] | Substrate for firefly luciferase in BLI. | Administered i.p. to generate bioluminescence signal in NF-κB-Luc mice. |
| Sparstolonin B (SsnB) nano-formulation [39] | TLR4 antagonist; inhibits upstream NF-κB signaling. | Therapeutic intervention to attenuate LPS-induced NF-κB activation and lung injury. |
| Click Beetle Green Luciferase (CBG) [42] | Alternative luciferase with minimal immunogenicity. | Reduces risk of immune rejection in longitudinal studies in immunocompetent mice. |
| Mevastatin | Mevastatin, CAS:73573-88-3, MF:C23H34O5, MW:390.5 g/mol | Chemical Reagent |
| Lovastatin Acid | Lovastatin Acid|Potent HMG-CoA Reductase Inhibitor | Lovastatin acid, the active metabolite of Lovastatin, is a potent, competitive HMG-CoA reductase inhibitor (Ki=0.6 nM). This product is for Research Use Only and not for human consumption. |
Transgenic NF-κB reporter mice provide a powerful platform for non-invasive, longitudinal investigation of pulmonary inflammation. The protocols outlined herein for LPS-induced lung injury, combined with the appropriate selection of reporter models and reagents, enable precise quantification of NF-κB dynamics. This approach is invaluable for deciphering inflammatory mechanisms and evaluating the efficacy of novel anti-inflammatory therapeutics.
Chagas disease, caused by the protozoan parasite Trypanosoma cruzi, remains a serious public health issue affecting approximately 7 million people worldwide, with high morbidity and mortality rates [43]. The disease presents significant challenges for treatment and monitoring, particularly in its chronic phase where parasite burden is extremely low and infections are highly focal at a tissue level [44]. Traditional methods for assessing parasite load, such as microscopy and PCR, suffer from limitations in sensitivity and spatial resolution, constraining both basic research and clinical trials of potential new treatments [45] [44].
In vivo bioluminescence imaging (BLI) has emerged as a powerful technology that addresses these limitations by enabling highly sensitive, longitudinal monitoring of parasite burden in real-time within living animal models [45]. This application note details the implementation of BLI for monitoring T. cruzi infection, providing researchers with comprehensive protocols, technical considerations, and practical insights to advance drug discovery and pathogenesis studies for Chagas disease.
Bioluminescence imaging relies on the detection of light produced by luciferase enzymes catalyzing the oxidation of a substrate (luciferin) [46]. For in vivo applications, the most commonly used system is the red-shifted firefly luciferase (Photinus pyralis) with D-luciferin as substrate, as its emission spectrum (peak ≈560-650 nm) penetrates biological tissues more effectively than blue or green light [46] [45]. The recent development of even brighter luciferase systems, such as NanoLuc and AkaBLI, has further enhanced sensitivity and tissue penetration capabilities [46].
The principal advantage of BLI for monitoring infection is its exceptional signal-to-noise ratio due to the near absence of background autoluminescence in mammalian tissues [46]. This enables direct, quantitative measurement of pathogen load in vivo. Furthermore, BLI allows repeated assessment of the same animals over time, reducing inter-individual variability and the number of animals required while providing comprehensive data on infection dynamics and treatment response [45].
Application-Specific Methodology
Parasite Strain and Genetic Modification
The foundational requirement for BLI monitoring of T. cruzi is a genetically modified parasite strain that constitutively expresses luciferase. The T. cruzi CL Brener Luc::Neon lineage has been successfully implemented and validated for drug efficacy studies [45]. This strain expresses a red-shifted firefly luciferase variant, providing optimal tissue penetration for in vivo imaging [45].
Key validation parameters for the reporter strain include:
- Unaltered growth kinetics and differentiation capacity compared to wild-type parasites
- Stable luciferase expression throughout the parasite life cycle
- Maintained infectivity in vitro and in vivo
- Linear correlation between bioluminescence signal and parasite number [47] [45]
Experimental Infection Model
Host: Immunocompetent or immunodeficient mice (e.g., BALB/c, C57BL/6) Infection route: Intraperitoneal injection is commonly used, though other routes may better model specific transmission pathways Infectious dose: 1×10^4 - 1×10^5 metacyclic trypomastigotes, depending on research objectives [45]
Detailed Imaging Protocol
The following protocol outlines the standardized procedure for longitudinal monitoring of parasite burden in a Chagas disease mouse model:
Preparation of Imaging Substrate:
- Prepare a sterile solution of D-luciferin in phosphate-buffered saline (PBS) at 15 mg/mL
- Filter-sterilize using a 0.22 μm filter and store protected from light at 4°C
- Warm to 37°C before administration [45]
Animal Preparation:
- Anesthetize mice using isoflurane (2-3% in oxygen)
- Administer D-luciferin intraperitoneally at 150 mg/kg body weight (10 μL/g of 15 mg/mL solution)
- Place animals in a sterile cage and maintain under anesthesia for 10-15 minutes to allow luciferin distribution and substrate-enzyme reaction [45]
Image Acquisition:
- Position animals in the imaging chamber in a supine position
- Acquire images with exposure times ranging from 5 seconds to 5 minutes, depending on signal intensity
- Use medium binning and f/stop = 1 to optimize signal detection
- Maintain anesthesia throughout the imaging procedure [45]
Data Analysis:
- Define regions of interest (ROIs) corresponding to specific anatomical locations or the entire animal
- Quantify signal intensity as total flux (photons/second) within each ROI
- Normalize data to baseline or pre-treatment values for longitudinal studies [45]
Table 1: Key Parameters for BLI Data Acquisition in Chagas Disease Models
| Parameter | Recommended Setting | Notes |
|---|---|---|
| Luciferin dose | 150 mg/kg | IP administration provides consistent signal |
| Incubation time | 10-15 min | Optimal for substrate distribution and reaction |
| Image exposure | 5 sec - 5 min | Adjust based on signal intensity; avoid saturation |
| Binning | Medium | Balances resolution and sensitivity |
| Anesthesia | 2-3% isoflurane | Maintain throughout imaging procedure |
| Imaging frequency | 1-3 times/week | Minimize stress while capturing disease dynamics |
Experimental Workflow Visualization
Data Interpretation and Validation
Quantitative Analysis: Bioluminescence signal intensity shows a linear correlation with parasite number, enabling quantitative assessment of parasite burden [45]. The sensitivity of BLI allows detection of as few as 10 parasites in a mammalian cell infection, far exceeding the sensitivity of traditional microscopy-based parasitemia assessment [47].
Spatial Distribution: BLI provides valuable information on the tissue distribution and tropism of T. cruzi. Research has demonstrated the particular importance of adipose tissue as a reservoir for the parasite in the chronic phase of infection [43]. Quantitative PCR and bioluminescence imaging systems have shown that T. cruzi displays tropism for the gastrointestinal tract and adipose tissue, among other tissues, which may act as reservoirs during the chronic phase [43].
Validation with Complementary Methods: While BLI provides exceptional sensitivity for longitudinal monitoring, correlation with established methods strengthens experimental findings:
- qPCR: For quantification of parasite burden in specific tissues post-mortem
- Serological assays: Multi-Cruzi immunoassay platform for detecting antibody responses [44]
- Histopathology: Assessment of tissue inflammation and damage
Table 2: Comparison of Parasite Detection Methods in Chagas Disease Models
| Method | Sensitivity | Spatial Information | Longitudinal Capability | Key Applications |
|---|---|---|---|---|
| In vivo BLI | High (≈10 parasites) | Whole-body, 2D | Excellent | Longitudinal treatment efficacy, parasite distribution |
| qPCR | Very high (single parasite) | Tissue-specific, destructive | No (terminal procedure) | Validation of cure in specific tissues |
| Microscopy | Low (≥1×10^5 parasites/mL) | Blood smear, limited | Moderate (repeated bleeding) | Acute phase parasitemia monitoring |
| Immunoassay | Indirect measure | None | Yes (serial bleeding) | Serological response, biomarker identification |
Research Reagent Solutions
Table 3: Essential Research Reagents for BLI in Chagas Disease Models
| Reagent/Material | Function | Application Notes |
|---|---|---|
| T. cruzi CL Brener Luc::Neon | Bioluminescent parasite strain | Constitutively expresses red-shifted firefly luciferase; maintain with 150 μg/mL hygromycin [45] |
| D-Luciferin | Luciferase substrate | 15 mg/mL in PBS; filter sterilize; IP injection at 150 mg/kg [45] |
| Benznidazole | Reference compound | 100 mg/kg once daily for 10 days for curative treatment; dissolve in DMSO then HPMC-SV [45] |
| HPMC-SV Vehicle | Compound suspension | 0.5% HPMC, 0.4% Tween 80, 0.5% benzyl alcohol; store at 4°C [45] |
| Grace's Insect Medium | Metacyclogenesis induction | For differentiation of epimastigotes to metacyclic trypomastigotes; 7-10 days incubation [45] |
| LIT Media | Epimastigote culture | Supplement with 10% FBS, penicillin/streptomycin, and hygromycin [45] |
| Giemsa Stain | Differentiation assessment | Evaluate metacyclogenesis rate by microscopy [45] |
Technical Considerations and Troubleshooting
Optimizing Signal Detection
Substrate Administration: Intraperitoneal injection of D-luciferin provides more consistent signals compared to subcutaneous administration in rodent models. The optimal time between substrate administration and image acquisition may vary slightly depending on the specific parasite strain and infection stage, with 10-15 minutes generally providing peak signal intensity [45].
Image Acquisition Parameters: Appropriate exposure time is critical for quantitative analysis. Overexposed images (saturated pixels) cannot be used for accurate quantification, while underexposed images may miss low-level signals. It is recommended to acquire a series of images with varying exposure times when establishing the model [45].
Limitations and Mitigation Strategies
Spatial Resolution: Conventional 2D BLI provides limited depth resolution, making it difficult to precisely localize signals from deep tissues. This can be mitigated through:
- 3D tomographic reconstruction when available
- Correlation with post-mortem analyses of specific tissues
- Use of multi-modal imaging approaches [45]
Signal Attenuation: Bioluminescence signal is attenuated by overlaying tissues, potentially leading to underestimation of parasite burden in deep organs. The use of red-shifted luciferase reporters minimizes this effect [46].
Advanced Applications in Drug Discovery
BLI has become the standard approach for in vivo drug efficacy studies against T. cruzi, enabling unprecedented sensitivity in detecting residual infection after treatment [45]. The technology has been instrumental in identifying compounds with trypanocidal activity and has supported the drug discovery efforts coordinated by organizations such as the Drugs for Neglected Diseases initiative (DNDi) [45] [44].
The exceptional sensitivity of BLI allows detection of parasite foci in visceral organs even after drug treatment that appears curative by traditional parasitemia monitoring methods [45]. This capability is particularly valuable for assessing drug efficacy against the chronic stage of infection, where parasite burden is extremely low and tissue-specific [44].
Furthermore, the combination of highly sensitive BLI with antibody multiplex assay systems enables identification of serological markers of infection and confirmation of parasitological cure, addressing a critical need in clinical trial design for Chagas disease [44].
Bioluminescence imaging represents a powerful methodology for monitoring parasite burden in Chagas disease models, offering significant advantages in sensitivity, longitudinal assessment, and whole-body evaluation of infection dynamics. The detailed protocols and technical considerations outlined in this application note provide researchers with a framework for implementing this technology to advance our understanding of T. cruzi pathogenesis and accelerate the development of new therapeutic interventions for this neglected tropical disease.
The tumor immune microenvironment (TIME) is a complex ecosystem where immune cells constantly interact with cancer cells. Tumor-associated inflammation is not merely a bystander effect but a critical driver of cancer progression and therapy resistance. It is characterized by the infiltration of various immune cells, including cytotoxic T lymphocytes (CTLs), and the release of specific molecular mediators. Among these, granzyme B, a serine protease released by activated CTLs, has been identified as a primary effector enzyme responsible for inducing target cell apoptosis and is a key marker of successful immune activation following immunotherapy [48].
Molecular imaging technologies have revolutionized cancer research by enabling the non-invasive visualization and quantification of biological processes within living organisms. Bioluminescence imaging (BLI), in particular, provides a powerful tool for longitudinal monitoring of immune activity due to its high sensitivity, specificity, and the capacity for repetitive measurements without autofluorescence background or the need for external excitation light [48] [49]. This Application Note details protocols for using activatable bioluminescence probes to track granzyme B activity, a direct functional readout of cytotoxic T-cell activity within tumors, facilitating the assessment of therapeutic efficacy in preclinical models.
The Role of Granzyme B in Cancer Immunotherapy
Granzyme B as a Key Effector of Cytotoxic Immunity
The efficacy of cancer immunotherapy, particularly immune checkpoint inhibitors (ICIs) that target pathways like PD-1/PD-L1 and CTLA-4, relies on reactivating the cytotoxic function of T cells [50]. Upon recognizing a tumor cell, activated CTLs release cytotoxic granules containing granzyme B into the immunological synapse. Once inside the target cell, granzyme B initiates a cascade of caspase activation, leading to programmed cell death (apoptosis) [48]. Consequently, the detection of granzyme B activity provides a direct and functional measure of successful T-cell-mediated killing of tumor cells, making it a highly relevant biomarker for evaluating immunotherapy response.
Challenges in Monitoring Immunotherapy Response
Traditional methods for assessing therapy response, such as tumor size measurement, can be misleading in the context of immunotherapy. A phenomenon known as "pseudoprogression"—where an apparent increase in tumor size is due to beneficial immune cell infiltration rather than tumor growth—can occur, complicating early treatment evaluation [48]. While biopsy can offer a snapshot of the TIME, it is invasive, subject to sampling error, and impractical for repetitive, longitudinal monitoring [48]. Therefore, non-invasive imaging tools that can probe the dynamic functional state of the immune system are instrumental for improving the efficacy of cancer immunotherapies [48] [49].
Probe Design and Mechanism of Action
GBLI-2: A Granzyme B-Activated Bioluminescence Probe
The core technology described in this protocol is GBLI-2, a bioluminescence probe designed for the specific, non-invasive imaging of granzyme B activity in vivo [48].
- Design Principle: GBLI-2 is constructed by conjugating a granzyme B-specific tetrapeptide substrate (IEFD for mouse granzyme B) to D-luciferin (the substrate for firefly luciferase) via a self-immolative linker [48].
- Activation Mechanism: In its native state, the peptide cage sterically hinders the interaction between D-luciferin and luciferase, resulting in a low signal. Upon cleavage by active granzyme B in the tumor microenvironment, the linker self-immolates, releasing free D-luciferin. This free D-luciferin can then participate in the luciferase-catalyzed bioluminescent reaction, producing a light signal proportional to granzyme B activity [48].
The following diagram illustrates the logical workflow from probe administration to signal interpretation:
Biochemical Validation of GBLI-2
Prior to in vivo application, GBLI-2 was rigorously validated in vitro.
- Specificity: GBLI-2 demonstrated a 284-fold increase in bioluminescence signal upon incubation with recombinant mouse granzyme B. In contrast, incubation with other proteases, including granzyme A, caspase-1, -3, -8, and cathepsin C, produced signals similar to the blank control, confirming high specificity for granzyme B [48].
- Inhibition: The cleavage of GBLI-2 by granzyme B could be effectively blocked by the specific inhibitor Ac-IEPD-CHO, resulting in a 74% reduction in the bioluminescence signal, further verifying the enzymatic mechanism [48].
- Kinetics: The enzymatic Michaelis-Menten constant (K~m~) for the hydrolysis of GBLI-2 by granzyme B was determined to be 97 µM, indicating efficient enzyme-substrate interaction [48].
Table 1: Key Performance Metrics of GBLI-2 Probe from In Vitro Characterization
| Parameter | Result | Interpretation |
|---|---|---|
| Signal Increase (vs. blank) | 284-fold | High activation ratio and specificity for granzyme B. |
| Inhibition by Ac-IEPD-CHO | 74% signal reduction | Confirms mechanism is dependent on granzyme B's proteolytic activity. |
| Michaelis Constant (K~m~) | 97 µM | Indicates favorable enzyme-substrate binding affinity. |
| Selectivity | No significant activation by granzyme A, caspases, or cathepsin C | Minimal off-target activation ensures signal fidelity in complex biological environments. |
Experimental Protocols
Longitudinal Imaging of Immunotherapy Response
This protocol describes the application of GBLI-2 for monitoring the response to immune checkpoint blockade in a syngeneic mouse model of colorectal carcinoma.
Materials and Reagents
Table 2: Research Reagent Solutions for GBLI-2 Imaging
| Item | Function/Description | Source / Example |
|---|---|---|
| GBLI-2 Probe | Granzyme B-activated bioluminescent probe. Synthesized from IEFD peptide and D-luciferin. | Custom synthesis per [48] |
| D-Luciferin | Native substrate for firefly luciferase; used for control imaging. | Commercially available (e.g., GoldBio, PerkinElmer) |
| CT26-luc Cells | Murine colorectal carcinoma cells stably expressing firefly luciferase. | ATCC, modified in-house |
| Anti-PD-1 / Anti-CTLA-4 Antibodies | Immune checkpoint inhibitors for therapeutic intervention. | BioXCell, commercial suppliers |
| In Vivo Imaging System (IVIS) | Platform for sensitive detection and quantification of bioluminescent signals. | PerkinElmer IVIS Spectrum |
Procedure
- Tumor Model Establishment: Inoculate immunocompetent mice (e.g., BALB/c) subcutaneously with CT26-luc cells (e.g., 0.5 - 1 x 10^6^ cells per mouse). Allow tumors to establish to a predefined volume (e.g., 50-100 mm³).
- Treatment Administration: Randomize mice into treatment and control groups. Administer immune checkpoint inhibitors (e.g., anti-PD-1 antibody, 200 µg per mouse, intraperitoneally) or isotype control antibodies according to the desired schedule (e.g., every 2-3 days).
- Bioluminescence Imaging with GBLI-2:
- At selected time points post-treatment (e.g., days 0, 3, 7, 10), inject mice with GBLI-2 probe (e.g., 100 µL of a 5 mg/mL solution in PBS, intravenously or intraperitoneally).
- Anesthetize mice using an isoflurane/oxygen mixture.
- Acquire bioluminescence images using the IVIS system 10-20 minutes after probe injection. Standard acquisition parameters (e.g., medium binning, f/stop 1, 1-5 minute exposure) should be determined and kept consistent.
- Control Imaging for Tumor Burden: To monitor tumor volume independently of immune activity, inject mice with D-luciferin (150 mg/kg, intraperitoneally) and image 10-15 minutes post-injection. This step should be performed on a separate day or with a sufficient washout period to avoid signal interference.
- Data Analysis: Quantify the total flux (photons/second) within a consistent region of interest (ROI) drawn over the tumor for both GBLI-2 and D-luciferin images. The GBLI-2 signal should be normalized to the baseline measurement or to the tumor burden signal from D-luciferin.
Advanced Protocol: Imaging Immunological Memory
GBLI-2 can also be used to visualize the cytotoxic response in a tumor rechallenge model, which demonstrates the establishment of immunological memory.
- After the primary tumors have regressed following successful immunotherapy, allow mice to enter a drug-free resting period for several weeks.
- Rechallenge the mice by injecting CT26-luc cells into the opposite flank.
- Image the rechallenged tumor site using the GBLI-2 protocol described above. A strong, rapid granzyme B signal upon rechallenge indicates a potent memory T-cell response, whereas a weak signal suggests the absence of protective immunity [48].
The following diagram summarizes the core experimental workflow:
Data Interpretation and Quantification
Correlation with Immunological Parameters
The bioluminescence signal generated by GBLI-2 is functionally relevant. Studies have shown a direct correlation between the in vivo GBLI-2 signal and the population of PD-1 and granzyme B co-expressing CD8+ T cells within the tumor as quantified by post-mortem flow cytometry [48]. This validation confirms that the probe accurately reports the activity of a key, therapeutically activated immune cell population.
- Responding Tumors: Exhibit a significant and sustained increase in the GBLI-2 signal following ICI treatment.
- Non-Responding Tumors: Show a flat or decreasing GBLI-2 signal profile over time.
Quantitative Analysis and Standardization
For robust and reproducible data, moving from relative to absolute optical signal quantification is critical.
- Absolute Quantification: Bioluminescence signals are typically measured in relative light units (RLU), which are device-dependent. For cross-study comparisons, absolute quantification of the total photon flux (photons/second) is recommended. This can be achieved by calibrating the imaging system with a traceable optical reference light source, such as a luminescent solution with a known absolute value measured by an integrating sphere spectrometer [51].
- Automated Analysis: Tools like InVivoPLOT that utilize a body-conforming animal mold (BCAM) and statistical mouse atlases can provide data congruency across animals of different sizes and poses. This enables automated, operator-independent quantification of bioluminescent source distributions and improves reproducibility in longitudinal studies [25].
Advanced Applications and Future Directions
Emerging Bioluminescence Technologies
The field of bioluminescence imaging is rapidly advancing, with new technologies offering enhanced performance.
- NIR-II Bioluminescence: Conventional BLI emits in the visible spectrum (400-700 nm), where tissue scattering and absorption are high. Novel probes that emit in the second near-infrared window (NIR-II, 1000-1700 nm) have been developed. These probes, often based on bioluminescence resonance energy transfer (BRET) to specially designed cyanine dyes, enable higher contrast imaging with significantly improved signal-to-noise ratios and spatial resolution due to reduced tissue scattering [52]. This technology is particularly promising for imaging deep-seated tumors.
Integration with Other Modalities
BLI is one component of a growing molecular imaging toolkit for immuno-oncology. Other key modalities include:
- Positron Emission Tomography (PET): Useful for whole-body imaging and quantifying the expression of immune checkpoint proteins like PD-L1 or for tracking specific immune cells (e.g., CD8+ T cells) using radiolabeled antibodies or ligands [49].
- Magnetic Resonance Imaging (MRI): Provides high-resolution anatomical information and can be used to characterize the tumor microenvironment through techniques like diffusion-weighted imaging (DWI) and dynamic contrast-enhanced (DCE) MRI [49].
The combination of functional BLI data with anatomical and other functional data from MRI or PET provides a comprehensive view of the tumor-immune interplay.
A paramount challenge in regenerative medicine is the low rate of stem cell survival and engraftment following transplantation; typically, less than 3% of administered cells successfully engraft in the hostile ischemic microenvironment of the target tissue [53]. This significant cell loss, primarily due to apoptosis, inflammation, and anoikis (detachment-induced cell death), severely limits the therapeutic efficacy of stem cell-based treatments [53]. Therefore, non-invasive, quantitative methods to monitor cell fate in real-time are not merely beneficial but essential for evaluating treatment success and optimizing protocols.
Longitudinal in vivo bioluminescence imaging (BLI) has emerged as a powerful tool for addressing this need. Unlike fluorescence imaging, BLI does not require external excitation light, thereby avoiding issues of phototoxicity and autofluorescence. Its self-illuminating nature, driven by enzymatic reactions, provides exceptional signal-to-noise ratio and high sensitivity for deep-tissue imaging in live subjects [2]. This application note details protocols for using BLI to visualize stem cell survival and engraftment, with a specific focus on imaging inflammation and programmed cell death within the context of longitudinal research studies.
Key Monitoring Strategies and Instrumentation
Research Reagent Solutions for Bioluminescence Imaging
The following table catalogues essential reagents and their functions for successful bioluminescence imaging in stem cell therapy research.
Table 1: Key Research Reagents for Bioluminescence Imaging
| Reagent / Tool | Function / Application | Key Characteristics |
|---|---|---|
| NanoLuc Luciferase [54] | Engineered reporter enzyme for BLI. | Small size, extreme brightness, ATP-independent functionality allows for imaging of both intra- and extracellular events. |
| Nano-Glo Fluorofurimazine (FFz) Substrate [54] | In vivo substrate for NanoLuc Luciferase. | Aqueous solubility, enhanced bioavailability, and specificity for NanoLuc, enabling bright signals in vivo. |
| Nano-Glo Cephalofurimazine (CFz9) Substrate [54] | In vivo substrate for brain imaging. | Specifically engineered to cross the blood-brain barrier, enabling non-invasive exploration of the central nervous system. |
| Caspase-8 Probe (Ac-IETD-Amluc) [2] | Activated bioluminescence probe for imaging apoptosis/pyroptosis. | Consists of a Caspase-8-specific cleavable peptide (Ac-IETD) linked to a D-Aminoluciferin (Amluc) motif. Becomes luminescent upon cleavage by Caspase-8. |
| Luminol Sodium Salt [13] | Chemiluminescent substrate for imaging inflammation. | Emits light (λmax = 425 nm) when oxidized by reactive oxygen species (e.g., hypochlorous acid) produced by activated neutrophils during inflammation. |
Imaging Modalities at a Glance
While BLI is a focus, it is one of several non-invasive imaging techniques used in stem cell therapy development. The table below compares key modalities.
Table 2: Comparison of Non-Invasive Imaging Modalities for Stem Cell Therapy Monitoring
| Imaging Modality | Key Principle | Applications in Stem Cell Therapy | Key Considerations |
|---|---|---|---|
| Bioluminescence Imaging (BLI) | Light emission from enzymatic reactions (e.g., luciferase-luciferin) [2]. | Longitudinal tracking of cell survival, location, and specific biological processes (e.g., apoptosis) [2] [13]. | High sensitivity, low background. Requires genetic modification of cells to express reporter genes. |
| Magnetic Resonance Imaging (MRI) | Detection of labeled cells based on magnetic properties. | Anatomical localization and tracking of iron oxide-labeled stem cells; assessment of structural and functional outcomes [55]. | Excellent anatomical resolution. Lower sensitivity for cell detection (~10^5 cells); potential label dilution with cell division [55]. |
| Fluorescence Imaging (FLI) | Light emission from fluorophores after external excitation [2]. | Tracking of labeled cells and histological validation. | Can be used for high-resolution ex vivo analysis. In vivo use can be limited by tissue autofluorescence and light scattering [2]. |
| Positron Emission Tomography (PET) | Detection of gamma rays from radioactive tracers. | Tracking of radiolabeled cells; metabolic imaging. | Very high sensitivity. Lower spatial resolution than MRI; use of radioactive compounds [53]. |
Detailed Experimental Protocols
Protocol 1: Monitoring Stem Cell Survival and Engraftment Using Reporter Gene Imaging
This protocol utilizes cells engineered to stably express a luciferase reporter gene (e.g., NanoLuc) for longitudinal tracking of cell location and viability.
Cell Line Engineering:
- Transduce your stem cell line of interest (e.g., Mesenchymal Stem Cells) with a lentiviral vector encoding the NanoLuc Luciferase gene [54].
- Apply antibiotic selection to create a stable polyclonal cell line and confirm high expression levels via in vitro bioluminescence assay.
Animal Preparation and Cell Transplantation:
- Induce the relevant disease model (e.g., myocardial infarction, ischemic stroke) in immunocompromised or immunocompetent (with immunosuppression) mice [56].
- At the desired time post-injury, harvest the engineered stem cells and administer them via the chosen route (e.g., intravenous, intra-arterial, or direct intramyocardial injection) [57] [53].
In Vivo Bioluminescence Imaging:
- At designated time points post-transplantation (e.g., 1 day, 1 week, 2 weeks), anesthetize the animal using inhaled isoflurane.
- Administer the Nano-Glo Fluorofurimazine (FFz) substrate via intraperitoneal injection at 200 mg/kg [54]. For brain imaging, use the Nano-Glo Cephalofurimazine (CFz9) substrate [54].
- Place the animal in an imaging chamber (e.g., PerkinElmer IVIS Spectrum) and acquire images for 5-20 minutes post-injection [13].
- Use living image software to quantify the total flux (photons/second) within a defined region of interest (ROI) over the target area.
Data Analysis:
- Plot the total bioluminescence flux over time. A stable or increasing signal indicates successful engraftment and proliferation, while a decreasing signal suggests cell death or clearance [13].
Protocol 2: Visualizing Caspase-8-Mediated Programmed Cell Death in Inflammatory Environments
This protocol uses a novel activatable bioluminescence probe to directly image apoptosis and pyroptosis, key inflammatory cell death pathways, in real-time.
Probe Synthesis:
- Synthesize the Caspase-8-activated bioluminescence probe, Ac-IETD-Amluc, as described by Yuan et al. [2]. The probe consists of a Caspase-8-specific tetrapeptide substrate (Ac-IETD) conjugated to a D-Aminoluciferin (Amluc) motif.
- Confirm probe structure and purity using electrospray ionization mass spectrometry (ESI-MS) and NMR [2].
In Vitro Validation:
- Induce apoptosis in a firefly luciferase (fLuc)-expressing cell line (e.g., fLuc-4T1 cells) using a chemotherapeutic agent like cisplatin [2].
- Incubate cells with the Ac-IETD-Amluc probe (e.g., 200 μM) and measure bioluminescence. Validate cell death and Caspase-8 activation via parallel assays (e.g., flow cytometry for Annexin V/PI).
In Vivo Imaging of Cell Death:
- Establish a tumor model or an inflammatory stem cell transplantation model in mice.
- Administer the Ac-IETD-Amluc probe intravenously to the animal.
- Image the animal using an IVIS system. The probe is in an "off" state until cleaved by active Caspase-8 at the site of cell death, releasing the Amluc motif and generating a bioluminescent signal ("on" state) [2].
Quantification and Correlation:
- The bioluminescence intensity shows a linear relationship with Caspase-8 concentration (reported equation: Y = 1.163 + 2.107X, R² = 0.96), allowing for semi-quantitative assessment of cell death levels [2].
- Correlate BLI signals with post-mortem histological analysis of the target tissue.
Integrating longitudinal bioluminescence imaging into stem cell therapy research provides invaluable, real-time insights into two critical aspects: the survival and location of the administered cells and the inflammatory cell death processes in the host tissue. The protocols outlined herein, leveraging both reporter genes and activatable probes, empower researchers to move beyond endpoint analyses. This enables a dynamic understanding of therapy kinetics, facilitates the optimization of delivery methods and timing, and ultimately helps de-risk the translation of stem cell-based therapies from the bench to the bedside.
Engineered Bacterial Biosensors for Gastrointestinal Inflammation Detection
The management of gastrointestinal (GI) inflammatory diseases, such as Inflammatory Bowel Disease (IBD), relies on the accurate and timely detection of inflammation flares. Conventional methods like endoscopy are invasive, costly, and poorly suited for frequent monitoring, often leading to delays in diagnosis and treatment [58] [59]. Engineered bacterial biosensors represent a transformative approach, offering a non-invasive, real-time solution for detecting inflammation biomarkers within the GI tract. Framed within longitudinal in vivo bioluminescence imaging research, these biosensors enable the continuous tracking of disease progression and therapeutic response in live animal models, providing unprecedented insights into inflammatory dynamics.
Application Notes: Principles and Recent Advances
Bacterial biosensors are typically composed of an input module (sensing unit), a signal transduction module (processing unit), and an output module (response unit) [60]. For GI inflammation, sensors are engineered to detect specific biomarkers, such as heme (a component of blood) or calprotectin (a protein released by neutrophils during inflammation) [58] [59]. Upon biomarker detection, synthetic genetic circuits trigger the production of a quantifiable signal, most commonly bioluminescence or fluorescence, allowing for non-invasive readouts using imaging systems like IVIS (In Vivo Imaging System) [13] [60].
Recent innovations have focused on enhancing the functionality and practicality of these systems. The MagGel-BS platform encapsulates heme-sensing bacteria and magnetic particles within a protective hydrogel shell, enabling oral delivery, enhanced bacterial survival in the GI tract, and easy retrieval from feces using a magnet [58]. This system demonstrated rapid detection of gastrointestinal bleeding in a mouse colitis model within 20 minutes of administration. In parallel, advanced biosensors have been developed for the clinically validated biomarker calprotectin. One such sensor utilizes the zinc uptake regulator (Zur)-controlled promoter Pykg from Escherichia coli Nissle (EcN), which is highly upregulated during zinc limitation induced by calprotectin [59]. This biosensor was further engineered with a genetic memory circuit, enabling it to record transient inflammatory events, and was coupled with the production of the anti-inflammatory cytokine IL-10, demonstrating both diagnostic and therapeutic capabilities in vivo [59].
Table 1: Key Biomarkers for GI Inflammation Detection Using Bacterial Biosensors
| Biomarker | Significance | Biosensor Mechanism | Reported Detection Limit |
|---|---|---|---|
| Heme | Indicator of gastrointestinal bleeding [58] | Bacterial sensor triggers bioluminescence [58] | Rapid detection in mouse models within 20 minutes [58] |
| Calprotectin | Clinical gold-standard biomarker for gut inflammation [59] | Zur transcription factor responds to zinc sequestration; activates reporter gene [59] | As low as 10 µg mLâ»Â¹ in optimized sensors [59] |
| Tetrathionate | Chemical produced during inflammation [59] | Native bacterial metabolic pathways | Information missing |
Experimental Protocols
Protocol 1: Longitudinal Imaging of Inflammation Using the MagGel-BS Platform
This protocol details the use of magnetic, hydrogel-encapsulated bacterial biosensors for the speedy detection of gut disease in mouse models [58].
Materials
- MagGel-BS Microspheres: Magnetic hydrogel microspheres (e.g., sodium alginate-based) encapsulating engineered heme-sensing bacteria (e.g., E. coli with a heme-responsive promoter driving luciferase expression) and magnetic particles [58].
- Animal Model: Mice with chemically-induced colitis (e.g., using DSS or TNBS).
- Imaging Equipment: In Vivo Imaging System (IVIS) or equivalent with bioluminescence detection capability.
- Magnet: A strong permanent or electromagnetic separator for microsphere retrieval.
Procedure
- Sensor Administration: Orally administer a defined dose (e.g., 200 µL) of MagGel-BS microspheres to mice using a gavage needle [58].
- In Vivo Imaging:
- At desired time points post-administration (e.g., 4, 8, 12, 24 hours), anesthetize mice using isoflurane.
- Acquire bioluminescence images using the IVIS system. Typical acquisition settings include a field of view of "A," subject height of 1.5 cm, medium binning, and an exposure time of 1-5 minutes [13].
- Sensor Retrieval and Ex Vivo Analysis:
- Collect fecal samples at experimental endpoints.
- Suspend feces in phosphate-buffered saline (PBS) and isolate the microspheres using a magnet.
- Wash the retrieved microspheres and perform ex vivo bioluminescence imaging to quantify the signal intensity, which correlates with the level of GI bleeding [58].
- Data Analysis: Quantify the total flux (photons/second) from regions of interest (ROIs) over the abdominal area or from retrieved microspheres. Compare signal intensity across different disease stages or treatment groups.
Protocol 2: Assessing Inflammation with a Calprotectin-Responsive Biosensor
This protocol describes the use of EcN engineered with a Zur-based calprotectin sensor for detecting and recording inflammation [59].
Materials
- Bacterial Strain: EcN harboring the optimized calprotectin biosensor plasmid (e.g., pBSI2 with J23109-zur and Pykg-sfgfp). For memory function, use the BSIM strain with the two-plasmid integrase system [59].
- Induction Agent: Purified human calprotectin (or the zinc chelator TPEN for in vitro optimization).
- Animal Model: Mouse models of colitis (e.g., DSS-induced or Helicobacter hepaticus-induced models).
- Flow Cytometer or Fluorescence Microscope: For analyzing sfGFP expression.
Procedure
- In Vitro Sensor Characterization:
- Grow the biosensor strain to mid-log phase in minimal media (e.g., M9).
- Treat cultures with a range of calprotectin concentrations (e.g., 0 - 500 µg mLâ»Â¹) or TPEN for a set duration (e.g., 4-6 hours).
- Measure fluorescence (sfGFP) using a flow cytometer or microplate reader to establish a dose-response curve and determine the sensor's dynamic range [59].
- In Vivo Administration and Sampling:
- Orally gavage mice with ~10â¹ CFU of the biosensor strain suspended in PBS.
- For longitudinal monitoring, collect fecal samples at various time points over several days.
- Signal Detection and Analysis:
- Homogenize fecal samples and resuspend bacteria in PBS.
- For immediate response sensors (BSI), analyze sfGFP fluorescence directly via flow cytometry.
- For memory sensors (BSIM), the fluorescence signal will persist even after the inflammatory trigger has subsided due to the genetic memory circuit. Analyze the percentage of GFP-positive cells to determine the history of inflammation exposure [59].
- Therapeutic Coupling: To assess therapeutic potential, administer a strain that couples the calprotectin sensor to the secretion of an anti-inflammatory molecule like IL-10 and monitor disease activity indices and histology [59].
Table 2: Research Reagent Solutions for Bacterial Biosensor Development
| Reagent / Material | Function / Application | Example Use Case |
|---|---|---|
| E. coli Nissle (EcN) | Engineered chassis organism; probiotic with good gut colonization [59] | Base for building calprotectin-sensing circuits [59] |
| Zur/Pykg Genetic Circuit | Sensing module for calprotectin via zinc sequestration [59] | Detects inflammation in mouse colitis models [59] |
| Sodium Alginate Hydrogel | Protective encapsulation material for oral delivery [58] | Forms the core of the MagGel-BS platform [58] |
| Magnetic Particles | Enables retrieval of biosensors from feces [58] | Integrated into MagGel-BS microspheres for isolation [58] |
| Luminol | Chemiluminescent substrate for myeloperoxidase activity [13] | Used in IVIS to detect innate immune activity in uveitis models [13] |
| IVIS Imaging System | Platform for longitudinal, non-invasive bioluminescence imaging [13] | Tracks spatial and temporal dynamics of inflammation in live animals [58] [13] |
Pathway and Workflow Visualizations
Diagram 1: Calprotectin Sensing & Memory Pathway
Diagram 2: In Vivo Experimental Workflow
Ex vivo organ culture systems have emerged as a transformative experimental bridge, offering a more physiologically relevant environment than two-dimensional cell cultures while avoiding the full complexity and ethical constraints of whole-animal studies. Within the specific context of inflammation research, these systems enable the longitudinal monitoring of biological processes in a controlled setting. The integration of bioluminescence imaging (BLI) technologies with ex vivo cultures provides a powerful, non-invasive method for real-time tracking of cellular behaviors, immune cell recruitment, and inflammatory progression over time. This approach is particularly valuable for studying complex, dynamic processes like neutrophil trafficking in acute inflammation or the development of chronic inflammatory diseases, allowing researchers to dissect molecular mechanisms with high spatial and temporal resolution [61]. Furthermore, ex vivo systems facilitate the use of human tissues, thereby enhancing the clinical translatability of preclinical findings. By offering a platform for continuous, quantitative observation, ex vivo organ culture bridges a critical methodological gap, accelerating the development and testing of novel anti-inflammatory therapeutics.
Key Applications and Quantitative Comparisons
Ex vivo BLI has been successfully adapted for a diverse range of applications, from tracking stem cells for regenerative medicine to monitoring metastatic spread in cancer research. The table below summarizes key quantitative findings from different ex vivo model systems, highlighting the versatility and measurable outcomes of this approach.
Table 1: Quantitative Findings from Ex Vivo Organ Culture Systems Integrating Bioluminescence Imaging
| Organ/Tissue System | Cell Type/Agent Imaged | Key Quantitative Findings | Research Context |
|---|---|---|---|
| Goat Intervertebral Disc [22] | Adipose-derived stem cells (gADSCs) | Gaussia luciferase (Gluc) proved more suitable than Firefly luciferase (Fluc) for longitudinal monitoring over at least 7 days of culture. | Regenerative Medicine |
| Mouse Bone & Lung [62] | Prostate cancer cells (PC-3) | Correlation between ex vivo BLI and other methods for metastasis quantification was strong for lungs (r ~0.8) but weaker for bone (r ~0.4). | Cancer Metastasis |
| Human Skin [63] | Native skin cells and structures | Microneedle-based culture enabled viable long-term live imaging for up to 11 days, with significantly reduced LDH and inflammatory cytokine (IL-6, IL-10, TNF) levels compared to conventional culture. | Dermatological Research & Toxicology |
| Mini-pig Skin [64] | Recombinant Fluc (rFluc) Protein | A custom imaging buffer (IB) was essential for sustaining rFluc luminescence ex vivo, enabling signal detection from biopsy samples post-euthanasia. | Drug Delivery & Bio-Distribution |
The data demonstrates that the success of ex vivo BLI is highly dependent on the choice of luciferase reporter, the specific organ being studied, and the culture conditions engineered to maintain tissue viability and reporter function.
Experimental Protocols for Key Experiment Types
Protocol: Monitoring Stem Cell Survival in a Large Mammal Ex Vivo Organ Culture
This protocol, adapted from studies using goat intervertebral discs, details the process of lentiviral transduction of stem cells for longitudinal viability tracking via BLI [22].
Step 1: Luciferase Reporter Transduction of Stem Cells
- Isolate and expand primary cells of interest (e.g., goat adipose-derived stem cells, gADSCs) in standard culture medium.
- Produce lentivirus particles for the desired luciferase reporter (e.g., Gluc-CFP or Fluc-mCherry) using a third-generation packaging system in HEK293T cells.
- Transduce gADSCs at ~60% confluence using lentivirus-conditioned medium for 4 hours. Verify transduction efficiency via fluorescence microscopy of the co-expressed fluorescent protein (CFP or mCherry).
Step 2: Preparation of Ex Vivo Organ Culture
- Isolate the target organ (e.g., intervertebral disc) under sterile conditions, preserving its structural integrity.
- Inject a standardized number of luciferase-expressing cells (e.g., 1x10^5 gADSC-GC or gADSC-FM) into the organ parenchyma using a micro-syringe.
- Place the cell-injected organ into a specialized bioreactor or culture system that maintains physiological conditions (e.g., temperature, humidity, and mechanical load, if applicable).
Step 3: Longitudinal Bioluminescence Imaging
- For Gaussia luciferase (Gluc) imaging: Collect small aliquots (e.g., 50 µL) of the culture medium at designated time points. Mix the medium with a freshly prepared Gluc substrate (e.g., coelenterazine) and measure luminescence immediately using a luminometer or CCD camera [22].
- For Firefly luciferase (Fluc) imaging: At each time point, transfer the entire organ to a culture dish. Submerge the tissue in a buffer containing D-luciferin (e.g., 150 µg/mL) and incubate for 5-10 minutes to allow for substrate penetration. Image the organ using an IVIS imaging system with an auto-exposure setting or a standardized exposure time (e.g., 1-5 minutes) [62] [22].
Protocol: Refined Ex Vivo Culture of Human Skin for Live Imaging
This protocol describes a novel microneedle-based culture technique designed to overcome diffusion limitations, enabling long-term, high-resolution live imaging of human skin tissue [63].
Step 1: Tissue Acquisition and Preparation
- Obtain human skin tissue (e.g., from cosmetic surgery surplus) with subcutaneous fat intact.
- Using a biopsy punch, prepare tissue samples of a manageable size (e.g., 8 mm diameter).
Step 2: Microneedle-Based Culture Setup
- Prepare a culture medium reservoir connected to a micro-infusion pump.
- Instead of relying solely on basal medium diffusion, use fine-gauge microneedles to infuse culture medium directly and continuously into the core of the dermis and subcutaneous tissue.
- Place the tissue sample in a custom chamber or a transwell insert that allows for gas exchange and submersion in a controlled atmosphere.
Step 3: Staining and Live Imaging
- Introduce fluorescent probes for cellular structures (e.g., membranes, mitochondria, ROS) into the culture medium or via microneedle injection.
- Mount the culture chamber on a confocal or multiphoton microscope equipped with an environmental chamber maintained at 37°C and 5% CO2.
- Acquire time-lapse images over several days. Use multiphoton microscopy to leverage tissue autofluorescence for visualizing collagen and elastin fibers without additional staining [63].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of ex vivo organ culture and imaging relies on a set of core reagents and technologies. The following table outlines key solutions for this field.
Table 2: Key Research Reagent Solutions for Ex Vivo Culture and Bioluminescence Imaging
| Reagent/Material | Function/Application | Examples & Notes |
|---|---|---|
| Luciferase Reporters | Engineered light-producing enzymes for tracking cells or biological processes. | Firefly Luc (FLuc): ATP-dependent, uses D-luciferin. Ideal for viability [14].NanoLuc (NLuc): Small, bright, ATP-independent, uses furimazine. Good for fusions [14].Gaussia Luc (GLuc): Small, secreted, uses coelenterazine. Suitable for medium assays [22]. |
| Luciferase Substrates | Chemical compounds oxidized by luciferase to produce light. | D-luciferin: For Firefly luciferase. IP injection is common for in vivo/ex vivo work [14].Coelenterazine: For Renilla and Gaussia luciferases [14].Fluorofurimazine (FFz): In vivo-grade substrate for NanoLuc [14]. |
| Specialized Culture Media | Maintain tissue viability and function outside the body. | Chemically Defined Media: Eliminates batch-to-batch variability of serum, improves reproducibility [65].Custom Imaging Buffers (IB): Can contain HEPES, ATP, MgSO4, and luciferin to sustain luciferase activity ex vivo, especially in post-euthanasia tissues [64]. |
| Microfluidic Chips & Bioreactors | Devices that provide precise environmental control and nutrient delivery to tissues. | Inflammation-on-a-Chip: Microfluidic devices with embedded endothelial layers to study neutrophil trafficking and transendothelial migration (TEM) [61].Loaded Disc Culture System (LDCS): Bioreactors that apply controlled mechanical load to organs like intervertebral discs [22]. |
| Microneedle Arrays | Minimally invasive tools for delivering nutrients and reagents deep into tissue explants. | Used to prevent central necrosis in thick human skin explants, enabling long-term culture (≥11 days) and high-resolution live imaging by ensuring core perfusion [63]. |
| MF-438 | MF-438, CAS:921605-87-0, MF:C19H18F3N5OS, MW:421.4 g/mol | Chemical Reagent |
| MF-592 | MF-592, CAS:1064195-48-7, MF:C34H33Cl2N3O6S, MW:682.6 g/mol | Chemical Reagent |
Workflow and Signaling Diagrams
Ex Vivo BLI Workflow for Inflammation Studies
The following diagram illustrates the generalized, multi-stage workflow for conducting longitudinal bioluminescence imaging in an ex vivo organ culture system, typical for studies on inflammation or cancer metastasis.
Neutrophil Signaling and Trafficking in On-Chip Inflammation Models
Inflammation-on-a-chip models have been instrumental in revealing sophisticated neutrophil behaviors. This diagram synthesizes key signaling pathways and cellular processes involved in neutrophil trafficking during acute inflammation, as probed in microfluidic devices [61].
Overcoming Technical Challenges: Optimization Strategies for Enhanced Sensitivity and Reliability
Longitudinal in vivo bioluminescence imaging (BLI) has become an indispensable tool for monitoring inflammatory processes in real-time, enabling researchers to track disease progression, cell migration, and therapeutic responses in live animal models. However, the sensitivity and reproducibility of BLI are profoundly influenced by technical factors, particularly the route of substrate administration and dosage optimization. This application note provides a comprehensive framework for optimizing these critical parameters, with specific focus on inflammation research. We present systematically collected quantitative data, detailed protocols, and visualization tools to enhance signal detection while minimizing experimental variability in longitudinal studies of inflammatory conditions.
Bioluminescence imaging enables sensitive detection of visible light produced during enzyme (luciferase)-mediated oxidation of molecular substrates expressed in vivo as reporters. The technology is particularly valuable for inflammation research because it allows noninvasive, serial quantification of biological processes throughout disease progression, significantly reducing inter-animal variability that plagues traditional histological approaches [29]. However, the reliability of BLI data is heavily dependent on substrate bioavailability, which varies based on administration parameters.
In inflammation studies, researchers commonly use transgenic reporter mice with NF-κB-responsive promoters driving luciferase expression to monitor inflammatory activation in real-time [29]. The sensitivity of detecting these internal light sources depends on multiple factors: luciferase expression levels, depth of labeled cells within the body, detection system sensitivity, and critically - the efficient delivery of substrate to the target tissue [29]. Optimizing substrate dosing and administration route is therefore essential for accurate interpretation of inflammatory processes in longitudinal studies.
Quantitative Comparison of Substrate Administration Parameters
D-Luciferin Dosage Optimization
Systematic evaluation of D-Luciferin concentrations reveals a clear dose-response relationship without saturation effects at higher doses, though with delayed time-to-peak at increasing concentrations.
Table 1: Impact of D-Luciferin Dose on BLI Signal Characteristics
| Dose (mg/kg) | Maximal Photon Emission | Time-to-Peak | Signal-to-Noise Ratio | Recommended Applications |
|---|---|---|---|---|
| 15 | Low | Short | Moderate | Preliminary screening |
| 150 | Moderate | Intermediate | Good | Standard inflammation models |
| 300 | High | Delayed | Excellent | Low-cell-number detection |
| 750 | Very High | Significantly Delayed | Excellent | Deep tissue inflammation |
Data adapted from Plössl et al. (2013) [66]
The optimal dose of 300 mg/kg provides an approximately 200% signal gain compared to the commonly used 150 mg/kg dose, significantly lowering the detection limit from 6,000 to 3,000 cells in brain inflammation models [66]. This enhanced sensitivity is particularly valuable for detecting early inflammatory responses or subtle treatment effects in longitudinal studies.
Administration Route Comparison
The route of substrate administration significantly impacts pharmacokinetic profiles, affecting the timing and intensity of bioluminescence signals.
Table 2: Characteristics of Different D-Luciferin Administration Routes
| Route | Time-to-Peak | Signal Intensity | Practical Considerations | Best Applications |
|---|---|---|---|---|
| Intravenous (IV) | Fastest (≈2 min) | Highest | Technically challenging | Acute inflammation kinetics |
| Intraperitoneal (IP) | Intermediate (10-20 min) | High | Technically simple | Most inflammation studies |
| Subcutaneous (SC) | Slowest (≈30 min) | Sustained plateau | Excellent reproducibility | Longitudinal time courses |
Data synthesized from Plössl et al. (2013) and Inoue et al. (2009) [66]
The comparison of intravenous, subcutaneous, and intraperitoneal substrate injection reflects expected pharmacokinetics with fastest and highest photon emission for intravenous administration [66]. However, intraperitoneal injection offers a favorable balance of technical simplicity and signal intensity for most inflammation studies, while subcutaneous administration provides the most sustained signal for longitudinal monitoring.
Experimental Protocols for Optimized BLI in Inflammation Research
Optimized Protocol for Inflammation-Specific BLI
This protocol has been specifically adapted for inflammation research using NF-κB reporter mice or similar models:
Materials Required:
- D-Luciferin potassium salt (15-300 mg/kg)
- Isoflurane anesthesia system
- Pre-warmed heating pad (37°C)
- In vivo imaging system with cooled CCD camera
- NF-κB reporter mice (e.g., HLL transgenic mice) [29]
Procedure:
- Prepare D-Luciferin solution at 30 mg/mL in sterile phosphate-buffered saline (PBS)
- Weigh animal and calculate required volume for 300 mg/kg dose
- Administer D-Luciferin via intraperitoneal injection (for optimal balance of signal intensity and technical feasibility)
- Immediately after injection, anesthetize animal with 2-3% isoflurane
- Place animal in imaging chamber maintained at 37°C with continued 1-2% isoflurane
- Begin image acquisition 10 minutes post-injection for inflammatory models
- Continue sequential imaging every 2-5 minutes for 30-40 minutes to capture peak signal
- Maintain consistent imaging parameters (exposure time, binning, f-stop) across all sessions in longitudinal studies
Critical Considerations for Inflammation Studies:
- Administer substrate PRE Isoflurane anesthesia for signal gain of approximately 200% compared to post-anesthesia injection [66]
- For systemic inflammation models, optimal imaging window is 10-20 minutes post-IP injection
- For localized inflammation (e.g., arthritis, brain inflammation), extend imaging window to 20-30 minutes to ensure adequate substrate distribution
- In NF-κB reporter models, baseline imaging before inflammatory stimulus provides crucial reference values [29]
Anesthesia Optimization Protocol
Anesthesia type significantly impacts bioluminescence signals, particularly in inflammation models:
Isoflurane Protocol:
- Induction: 3-4% in oxygen
- Maintenance: 1-2% via nose cone
- Inject D-Luciferin PRE-anesthesia for maximal signal [66]
Ketamine/Xylazine Protocol:
- Induction: 100/10 mg/kg IP
- Maintenance: Supplemental doses as needed
- No significant beneficial effect on maximal photon emission compared to optimized isoflurane protocol [66]
Longitudinal Study Design for Inflammation Monitoring
For serial imaging of inflammatory processes:
- Establish baseline imaging before inflammatory stimulus
- Perform subsequent imaging sessions at consistent time points post-stimulus
- Maintain identical substrate dosing, administration route, and imaging parameters throughout study
- Include control groups to account for potential inflammatory effects of repeated anesthesia/substrate administration
- For NF-κB activation studies, image at 4, 8, 24, and 48 hours post-stimulus to capture activation kinetics [29]
Visualization of Experimental Workflows
Substrate Administration Decision Pathway
Inflammation-Specific BLI Workflow
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for Optimized Inflammation BLI
| Reagent/Equipment | Specifications | Function in Inflammation BLI |
|---|---|---|
| D-Luciferin potassium salt | >98% purity, sterile | Luciferase substrate for light production |
| NF-κB reporter mice | HLL transgenic strain [29] | Monitor NF-κB activation in inflammation |
| Isoflurane anesthesia system | Precision vaporizer | Consistent anesthesia across imaging sessions |
| Cooled CCD camera | -90°C to -100°C cooling | High-sensitivity photon detection |
| LPS (Lipopolysaccharide) | E. coli serotypes | Induce inflammatory response for validation |
| Dexamethasone | Water-soluble formulations | Anti-inflammatory control compound [29] |
| MG-115 | MG-115, CAS:133407-86-0, MF:C25H39N3O5, MW:461.6 g/mol | Chemical Reagent |
| Midecamycin | Midecamycin CAS 35457-80-8 - Macrolide Antibiotic |
Optimal substrate administration is fundamental to reliable bioluminescence imaging in inflammation research. The recommended protocol of 300 mg/kg D-Luciferin administered intraperitoneally pre-Isoflurane anesthesia provides significantly enhanced sensitivity for detecting inflammatory processes in longitudinal studies. By implementing these standardized approaches, researchers can improve data quality, reduce animal numbers, and obtain more reliable insights into inflammatory disease mechanisms and therapeutic interventions.
In the field of longitudinal in vivo bioluminescence imaging (BLI) of inflammation, achieving accurate and reproducible quantitative data is paramount for preclinical research and drug development. A primary challenge in this endeavor is the significant absorption and scattering of light by mammalian tissues, which constrains signal detection, particularly from deep-seated inflammatory sites. The emitted light, especially at shorter wavelengths, is strongly absorbed by chromophores such as hemoglobin and melanin [1]. This physical limitation directly impacts the sensitivity and accuracy of longitudinal studies aimed at monitoring neuroinflammatory processes, such as those occurring after cerebral ischemia [67]. This Application Note addresses two core strategies to overcome these constraints: the strategic selection of luciferase enzymes with favorable emission wavelengths and the implementation of robust signal quantification correction methodologies. By integrating these approaches, researchers can obtain more reliable quantitative data on inflammatory burden and dynamics in live animal models.
Luciferase Selection for Optimal Depth Penetration
The choice of luciferase is a critical determinant for the success of deep-tissue bioluminescence imaging. The fundamental optical property to consider is the emission wavelength, as longer wavelengths in the red and near-infrared spectrum (≥ 600 nm) experience less absorption and scattering in biological tissues, leading to superior detection sensitivity from deep structures [68] [1].
Table 1: Key Luciferases for Deep-Tissue Bioluminescence Imaging
| Luciferase | Organism | Emission Peak (nm) | Key Features for In Vivo Imaging | Primary Substrate |
|---|---|---|---|---|
| Firefly (Fluc) | Photinus pyralis | 562 nm [1] | The benchmark for in vivo imaging; glow kinetics [68] [1] | D-luciferin [68] |
| Red Firefly | Photinus pyralis (engineered) | Shifted to red [69] | Improved depth penetration; can be multiplexed with blue-emitting luciferases [69] | D-luciferin [69] |
| Click Beetle | Pyrophorus plagiophthalamus | Red-emitting variants exist [1] | Enhanced sensitivity in deep tissues [1] | D-luciferin |
| Railroad Worm | Phrixothrix hirtus | ~620 nm (Red) [1] | Naturally emits red light; superior tissue penetration [1] | D-luciferin |
| Renilla (Rluc) | Renilla reniformis | 480 nm [1] | Strong light absorption by tissues limits deep-tissue use [1] | Coelenterazine [68] |
| Gaussia (Gluc) | Gaussia princeps | 480 nm [1] | Naturally secreted; blue light is highly absorbed in vivo [1] | Coelenterazine [68] |
The following diagram illustrates the decision-making workflow for selecting an appropriate luciferase based on experimental goals, particularly for inflammation imaging.
Diagram 1: Luciferase selection workflow for inflammation imaging. The process emphasizes emission wavelength as the primary criterion for deep-tissue studies.
Beyond emission wavelength, other practical considerations are vital:
- Reaction Kinetics: Firefly luciferase exhibits "glow" kinetics, producing a stable light signal for up to 60 minutes, which is convenient for in vivo imaging. In contrast, Renilla and Gaussia luciferases exhibit "flash" kinetics, where the signal decays rapidly, requiring immediate measurement after substrate injection [68] [1].
- Substrate Administration: For firefly luciferase imaging with D-luciferin, intraperitoneal (IP) injection is common. The signal typically peaks around 10 minutes post-injection and remains stable for about 30 minutes. For Renilla/Gaussia imaging with coelenterazine, intravenous (IV) injection is standard, with a signal peak occurring within seconds [1].
Signal Quantification and Correction Methodologies
Raw bioluminescence signal intensity measured at the surface of an animal is not a direct or absolute measure of the underlying biological source strength due to profound tissue effects. Implementing correction methods is therefore essential for accurate quantitation in longitudinal studies of inflammation.
Spectral Filtering for Tissue Absorption Correction
The degree of spectral shifting caused by tissue absorption can be used to calculate a correction factor. One established method involves using two optical filters that bracket the 620 nm wavelength, where hemoglobin absorption decreases significantly [70].
- Procedure: Two sequential images of the same animal are acquired using different bandpass filters (e.g., a 600 nm filter and a 620 nm filter).
- Analysis: The ratio of the signals obtained with the two filters is calculated. This ratio is correlated with the percentage of transmitted light through the tissues.
- Application: A significant correlation (R² = 0.97) has been demonstrated between this spectral ratio and light transmission, allowing for a more accurate quantitation of tumor proliferation in disseminated models [70].
Bioluminescence Tomography (BLT) and Automated Tools
Bioluminescence Tomography is a more advanced technique that moves beyond surface measurements to reconstruct the 3D spatial distribution and photon emission density (photons sâ»Â¹ mmâ»Â³) of the luminescent source within the animal [25].
- Principle: BLT uses an iterative algorithm that compares measured light intensities at the tissue surface to predictions generated from a model of light propagation through tissue. The model requires knowledge of the animal's surface geometry and optical tissue properties [25].
- Automated System (InVivoPLOT): The InVivoPLOT system integrates several innovations to automate and standardize quantification:
- Body-Conforming Animal Mold (BCAM): A shuttle that holds the mouse in a fixed, confined pose, providing a known and consistent geometry for light propagation modeling and enabling data congruency across animals of different sizes [25].
- Organ Probability Map (OPM): A statistical mouse atlas that is aligned with the BCAM, allowing for automated organ-specific region-of-interest (ROI) analysis without manual operator input [25].
- Output: This system can transform raw multispectral BLI images into 3D maps of bioluminescence source density, which can be linearly translated into quantitative measures, such as bacterial colony-forming units (CFU mmâ»Â³) [25].
Absolute Quantification Using Calibrated Reference
For the highest level of reproducibility, particularly across different instruments and laboratories, the absolute value of the BL signal can be measured as total photon flux (photons sâ»Â¹).
- Method: This involves calibrating the imaging system or luminometer using a reference light source with a known, absolute output traceable to a national metrology institute.
- Procedure: An optical reference light source (e.g., a homogeneous bioluminescence reaction solution) is prepared. Its absolute total photon flux is measured using an integrating sphere spectrometer. The same sample is then measured in the device to be calibrated, establishing the device's absolute responsivity (counts photonâ»Â¹) [71].
- Benefit: This allows the BL signal from biological samples to be reported in absolute units (photons sâ»Â¹), enabling direct comparison of data obtained from different experiments, days, and equipment [71].
The logical relationship between the quantification challenge and the appropriate corrective methodology is outlined below.
Diagram 2: Relationship between quantification challenges and advanced correction methodologies.
Protocol: Longitudinal Imaging of Neuroinflammation Post-Cerebral Ischemia
The following detailed protocol integrates the principles of luciferase selection and signal quantification for a specific application in neuroinflammation research, using a transient Middle Cerebral Artery Occlusion (MCAO) model in rats as an example [67].
Animal Model and Luciferase-Expressing Cell Preparation
- Animal Model: Adult male Sprague-Dawley rats (approx. 300-320 g) are subjected to a 90-minute transient MCAO under isoflurane anesthesia, followed by reperfusion [67].
- Cell Line and Transduction:
- Cell Culture: Maintain relevant cell lines (e.g., microglial or macrophage cells) in appropriate culture medium.
- Lentiviral Transduction: To ensure stable and proportional bioluminescent signal, transduce cells using a lentiviral vector (e.g., pTM915) carrying the firefly luciferase gene and a selectable marker (e.g., Hygromycin B resistance) under a constitutive promoter [72].
- Selection: Culture transduced cells under antibiotic selection (e.g., Hygromycin B) for at least one week to generate a stable, polyclonal population. This avoids the fragility and potential immunogenicity associated with single-cell clones, especially in immunocompetent models, and ensures signal stability over time [72].
- Validation: Validate the luciferase expression and function in vitro using a luciferase assay system before in vivo use.
In Vivo Imaging Procedure
- Substrate Administration: At each imaging time point (e.g., Day 1, 3, 7, 14, 21, 28 post-ischemia), inject D-luciferin intraperitoneally at a standard dose (e.g., 150 mg/kg body weight) [1].
- Image Acquisition:
- Anesthetize the animal and place it in the imaging chamber.
- Acquire a series of images using multiple spectral filters (e.g., 580 nm, 600 nm, 620 nm, 640 nm) 10-15 minutes after luciferin injection, during the signal plateau [70] [1].
- If using a BCAM system, place the animal in the weight-appropriate mold prior to imaging to ensure geometric consistency [25].
- Acquire a background image without the animal for noise subtraction.
Image Analysis and Data Correction
- Spectral Analysis for Quantitation:
- ROI Definition: Draw regions of interest (ROIs) over the brain region.
- Signal Extraction: Extract the total photon counts (or relative light units) from the images captured with each filter.
- Correction Factor Calculation: Calculate the signal ratio between a long-wavelength filter (e.g., 640 nm) and a short-wavelength filter (e.g., 580 nm). Apply a pre-determined correction factor (based on prior validation with tissue phantoms or BLT) to the raw signal to estimate the actual source strength [70].
- Bioluminescence Tomography (Optional): For studies requiring 3D localization, use the multispectral images as input for a BLT reconstruction algorithm. Coregister the resulting 3D source map with an anatomical reference, such as an MR image or a digital mouse atlas, to assign the signal to specific brain regions [67] [25].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Reagents and Materials for Quantitative Bioluminescence Imaging
| Item | Function/Description | Example/Catalog |
|---|---|---|
| Red-Emitting Luciferase | Engineered firefly or other luciferase with emission >600 nm for superior tissue penetration [69]. | Thermo Scientific Red Firefly Luciferase [69] |
| D-Luciferin | Substrate for firefly and red firefly luciferases; administered intraperitoneally for in vivo imaging [68]. | Promega Luciferin [73] |
| Luciferase Assay System | Reagents for in vitro validation of luciferase activity in cell lysates [73]. | Promega Luciferase Assay System (Cat.# E1500) [73] |
| Cell Culture Lysis Reagent | Component of assay systems for preparing cell lysates for in vitro luciferase measurement [73]. | Promega Cell Culture Lysis Reagent (CCLR) [73] |
| Lentiviral Vector | For stable integration of the luciferase gene into the genome of target cells [72]. | pTM915 (or similar construct) [72] |
| Selection Antibiotic | For selecting stably transduced polyclonal cell populations post-transduction [72]. | Hygromycin B [72] |
| Body-Conforming Animal Mold (BCAM) | Provides a fixed, known geometry for automated and reproducible image analysis and BLT [25]. | InVivoPLOT BCAM [25] |
| Optical Filters | Set of bandpass filters for multispectral imaging and spectral correction analysis [70]. | 580 nm, 600 nm, 620 nm, 640 nm filters |
| Calibrated Light Source | Reference source for absolute calibration of imaging system responsivity [71]. | Traceable to national metrology institute [71] |
| Mifobate | Mifobate, CAS:76541-72-5, MF:C11H17ClO7P2, MW:358.65 g/mol | Chemical Reagent |
| Migalastat | Migalastat (Galafold) | Migalastat is a pharmacological chaperone for Fabry disease research. It stabilizes amenable mutant α-galactosidase A. For Research Use Only. Not for human use. |
In longitudinal in vivo bioluminescence imaging of inflammation, the choice and management of anesthetic agents are critical methodological considerations. Anesthetics are not physiologically inert; they exert significant, agent-specific effects on vascular dynamics and immune responses that can confound experimental results. These confounders are particularly problematic in longitudinal studies where consistent measurements are essential for tracking inflammatory progression or resolution. This application note provides a structured framework for selecting and administering anesthetic regimens to minimize these confounders, thereby enhancing the reliability and reproducibility of data in preclinical inflammation research.
Anesthetic-Induced Confounders in Research
Effects on Vascular Dynamics
Anesthetics directly influence cerebral blood flow (CBF) and systemic circulation through multiple mechanisms, potentially altering the distribution of inflammatory cells and biomarkers at the imaging site.
- Cerebral Autoregulation and Reactivity: Anesthetics like sevoflurane and isoflurane cause cerebral vasodilation, which can modify local CBF and potentially affect the delivery and concentration of bioluminescent probes or cells in neurological inflammation models. In contrast, ketamine-dexmedetomidine combinations induce cerebral vasoconstriction under physiological conditions [74].
- Endothelial Function: The endothelium, a key regulator of vascular homeostasis, is a target for anesthetic agents. Some anesthetics can increase the production of reactive oxygen species (ROS), leading to oxidative stress and reduced nitric oxide (NO) bioavailability, resulting in endothelial dysfunction. This may influence vascular permeability and leukocyte adhesion, critical steps in the inflammatory response [75].
Immunomodulatory Effects
A wide body of evidence demonstrates that anesthetics have profound, agent-specific effects on both innate and adaptive immunity, which can directly impact the bioluminescent signal in inflammation models.
Innate Immunity Suppression: Volatile anesthetics (e.g., sevoflurane, isoflurane) and intravenous agents (e.g., propofol, midazolam) can suppress the function of key innate immune cells.
- Neutrophils: Impaired adhesion, chemotaxis, and reactive oxygen species (ROS) production have been observed with isoflurane and sevoflurane exposure [76].
- Natural Killer (NK) Cells: Cytotoxicity is decreased by sevoflurane, isoflurane, and halothane, which is a significant consideration in oncology-related inflammation models [76].
- Macrophages/Monocytes: Suppressed phagocytosis and decreased pro-inflammatory cytokine release (e.g., IL-1β, TNF-α) are documented effects [76].
Adaptive Immunity and Cellular Shifts: The depth and type of anesthesia can influence lymphocyte populations.
- Deep anesthesia (BIS < 45) has been shown to cause a significant drop in NK-cell and regulatory T-cell numbers, creating a state of generalized immune suppression [77].
- The balance between T-helper cells can be altered; for instance, isoflurane can change the Th1/Th2 ratio, potentially skewing the immune response [76].
Table 1: Quantitative Effects of Common Anesthetics on Immune Parameters
| Anesthetic Agent | Immune Cell/Parameter | Reported Effect | Experimental Context |
|---|---|---|---|
| Sevoflurane | Neutrophil Adhesion | Decreased [76] | In vitro & animal models |
| NK-cell Cytotoxicity | Decreased [76] | In vitro | |
| Pro-inflammatory Cytokines (IL-1β, TNF-α) | Decreased release from PBMCs [76] | In vitro | |
| Isoflurane | Neutrophil Migration | Decreased to inflammation site [76] | In vivo (mouse) |
| Microglial Cytokine Release | Decreased [76] | In vitro | |
| Propofol | Inflammatory Response (IL-6, TNF-α) | Attenuated increase post-surgery [78] | Human clinical study |
| Midazolam | Inflammatory Response (IL-6, TNF-α) | Attenuated increase post-surgery [78] | Human clinical study |
| Deep Anesthesia (BIS < 45) | NK-cell & T-reg Count | Dropped to almost half of plasma level [77] | Human clinical study |
Experimental Protocols for Anesthesia in Longitudinal Imaging
Pre-study Anesthesia Regimen Optimization
Before initiating a longitudinal study, characterize the specific effects of candidate anesthetic regimens on your model system.
Protocol: Baseline Immune and Vascular Phenotyping
- Subject Grouping: Randomize experimental animals into at least three groups: a test group for your model, an anesthetic-control group (anesthesia without model induction), and a naive-control group (no anesthesia, no model).
- Anesthesia Administration: Apply the proposed anesthetic regimen (e.g., 1.5-2% isoflurane in Oâ‚‚ or intraperitoneal ketamine/xylazine) to the test and anesthetic-control groups for a duration matching the planned imaging sessions.
- Blood Collection: Collect blood samples via venipuncture at baseline (pre-anesthesia), immediately post-anesthesia, and at 2, 6, and 24 hours post-procedure.
- Serum Analysis: Process samples and use ELISA to quantify key pro-inflammatory (IL-6, TNF-α) and anti-inflammatory (IL-10) cytokines [78].
- Flow Cytometry: Analyze blood or tissue samples to profile major immune cell populations (neutrophils, monocytes, NK cells, T and B lymphocytes) [20].
- Data Interpretation: Compare the kinetic profiles of cytokine levels and cell counts between groups. An ideal anesthetic regimen for the test group should show minimal deviation from the naive-control baseline, indicating low immunomodulatory confound.
Standardized In Vivo Imaging Procedure
Consistency is paramount for longitudinal studies. The following workflow details a standardized protocol for anesthetic administration during bioluminescence image acquisition.
Protocol: Consistent Anesthesia for Image Acquisition
- Preparation: Calibrate the vaporizer and ensure a sealed induction chamber. Use a bispectral index (BIS) monitor or similar if available to standardize depth [77].
- Induction: Place the animal in the induction chamber. Deliver 3-4% isoflurane in 100% oxygen at a 2 L/min flow rate until the loss of righting reflex is observed (typically 2-3 minutes) [13].
- Maintenance: Transfer the animal to the imaging stage and maintain anesthesia with 1.5-2% isoflurane delivered via a nose cone. Ensure the platform is heated to maintain body temperature at 37°C.
- Monitoring & Stabilization: Continuously monitor respiration rate (target: 50-80 breaths per minute). Allow a 5-minute stabilization period after transfer before substrate administration to establish hemodynamic and anesthetic equilibrium.
- Substrate Injection & Imaging: Administer D-luciferin (150 mg/kg) via intraperitoneal injection. Initiate the imaging sequence at the predetermined peak signal time (e.g., 10-15 minutes post-injection) using standardized IVIS settings (e.g., medium binning, 5-minute acquisition) [13] [20].
- Recovery: After imaging, disconnect the anesthetic and place the animal in a warm, clean cage. Monitor until fully ambulatory before returning to housing.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Anesthesia in Imaging Studies
| Reagent / Equipment | Function / Application | Key Considerations |
|---|---|---|
| Isoflurane (Volatile Anesthetic) | General anesthesia for induction and maintenance. | Fast onset/offset; allows fine-tuning of depth; known immunomodulatory effects must be characterized [76]. |
| Medical Oxygen (Oâ‚‚) | Carrier gas for volatile anesthetics; prevents hypoxia. | Use 100% Oâ‚‚ for induction; consider physiological concentrations (e.g., 30%) for maintenance in long studies. |
| Precision Vaporizer | Delivers a precise and calibrated concentration of volatile anesthetic. | Critical for dose consistency and animal safety. Must be regularly calibrated. |
| D-Luciferin | Substrate for firefly luciferase in bioluminescence imaging. | Dose (150 mg/kg), route (i.p.), and timing relative to image acquisition must be rigorously standardized [20]. |
| In Vivo Imaging System (IVIS) | CCD camera system for quantifying bioluminescence. | Use consistent settings (binning, FOV, acquisition time) across all sessions and animals [13]. |
| Heated Imaging Stage | Maintains core body temperature of anesthetized animals. | Prevents hypothermia, which can independently alter physiology and immune function. |
| Bispectral Index (BIS) Monitor | Measures depth of anesthesia via EEG. | Optional but valuable for objectively standardizing anesthetic depth across subjects and sessions [77]. |
| Mitonafide | Mitonafide, CAS:54824-17-8, MF:C16H15N3O4, MW:313.31 g/mol | Chemical Reagent |
| MK-4101 | MK-4101, MF:C24H24F5N5O, MW:493.5 g/mol | Chemical Reagent |
Decision Framework for Anesthetic Selection
Choosing the right anesthetic requires balancing experimental goals, known pharmacological effects, and practical constraints. The following pathway aids in this decision.
Data Normalization and Reporting Standards
To ensure rigor and reproducibility, explicitly account for anesthesia in data analysis and reporting.
- Internal Controls: Always include a baseline (pre-anesthesia) imaging time point within the longitudinal series. This allows each animal to serve as its own control for calculating fold-changes in signal, correcting for some of the inter-individual variation in anesthetic response.
- Reporting Standards: In publications and internal documents, meticulously document:
- Anesthetic Agent(s): Full name, supplier, and catalog number.
- Dosage/Concentration: For volatile anesthetics, report % v/v in carrier gas. For injectables, report dose (mg/kg), route, and volume.
- Duration: Total time under anesthesia for each session.
- Physiological Parameters: Record and report average body temperature and respiration rate.
- Methodological Justification: Justify the chosen anesthetic regimen based on its known effects relative to your research question.
Anesthesia is a potent experimental variable in longitudinal bioluminescence imaging. By systematically selecting anesthetic regimens based on their known vascular and immune effects, standardizing administration protocols, and transparently reporting methodology, researchers can significantly reduce data confounders. The frameworks and protocols provided herein offer a path toward achieving more reliable, reproducible, and interpretable data in preclinical inflammation research.
The Tumor Microenvironment (TME) is a complex ecosystem that differs significantly from the normal tissue environment (NTE) in aspects such as chronic inflammation, level of oxygen and pH, nutritional state of the cells, and tissue architecture [79]. These differences create a pro-tumorigenic niche that promotes cancer growth, immune evasion, and treatment resistance. A critical strategy in modern oncology involves normalization of the TME—reverting these abnormal conditions toward a state that more closely resembles normal tissue. This approach can inhibit cancer growth, outcompete malignant cells, and significantly improve the efficacy of conventional therapies [79]. For researchers utilizing longitudinal in vivo bioluminescence imaging to monitor inflammation and therapeutic response, accounting for tumor necrosis and metabolic variations is paramount. These confounding factors can significantly skew imaging data interpretation, making normalization approaches essential for accurate experimental outcomes.
This Application Note provides detailed methodologies for implementing TME normalization strategies, with particular emphasis on their impact on longitudinal bioluminescence imaging studies. We focus specifically on addressing the challenges posed by tumor necrosis and the profound metabolic reprogramming characteristic of cancer cells, providing structured protocols and analytical frameworks to enhance the validity and reproducibility of preclinical therapeutic research.
Metabolic Context: Necrosis, Metabolism, and Imaging Challenges
Tumor necrosis arises from severe hypoxia and nutrient deprivation within poorly vascularized regions of solid tumors [79]. This necrotic core presents a substantial challenge for bioluminescence imaging, as it represents areas with drastically altered cell viability and metabolic activity. Furthermore, the process of necrosis releases intracellular contents that can potentiate inflammation, indirectly influencing bioluminescence signals generated by probes sensitive to the inflammatory milieu [79].
Concurrently, cancer cells undergo extensive metabolic reprogramming to support rapid growth and proliferation. A hallmark of this reprogramming is the Warburg Effect, where cells preferentially rely on aerobic glycolysis, converting glucose to lactate even in the presence of oxygen [80]. This shift results in:
- High Glucose Consumption: Cancer cells exhibit up to 10-fold greater glucose uptake compared to normal tissue, a principle exploited clinically in FDG-PET imaging [80].
- Lactate Production and Acidosis: The export of lactate via monocarboxylate transporters (MCTs), particularly MCT1 and MCT4, creates an acidic TME (pH ~6.7-7.1) that is adverse to normal cells and can induce apoptosis [79] [80].
- Metabolic Coupling: Stromal cells, such as cancer-associated fibroblasts (CAFs), can undergo aerobic glycolysis to produce lactate, which is then utilized by adjacent cancer cells for oxidative metabolism—a process known as the Reverse Warburg Effect [80].
These metabolic adaptations are not uniform across the tumor mass, creating intratumor heterogeneity that can manifest as spatial and temporal variations in bioluminescence signal intensity during longitudinal studies. The following diagram illustrates the core metabolic relationships and their impact on the TME.
Diagram 1: Metabolic Pathways Influencing the TME and Bioluminescence Imaging. This diagram illustrates how dysregulated glucose metabolism in cancer cells leads to lactate production and acidosis. The resulting acidic TME promotes immune evasion, polarizes macrophages toward a tumor-promoting M2 phenotype, and contributes to tumor necrosis. These pathological processes can directly confound the interpretation of bioluminescence imaging signals in longitudinal studies.
Normalization Strategies: From Theory to Practice
Normalization of the TME targets the specific aberrant features that promote tumor progression. The table below summarizes key therapeutic targets and agents, with a specific focus on those addressing metabolic dysregulation and cell death processes relevant to imaging studies.
Table 1: Strategies for Tumor Microenvironment Normalization
| Normalization Approach | Specific Target | Exemplar Agent/Method | Primary Effect on TME | Relevance to Imaging |
|---|---|---|---|---|
| Anti-inflammation | Cyclooxygenase, Platelets | Aspirin, NSAIDs [79] | Reduces chronic inflammation & immunosuppression | Lowers background inflammatory signal |
| Targeting TAMs | Depletion/Repolarization of TAMs | RG7155, BLZ945, low-dose radiation [79] | Shifts from M2 to tumoricidal M1 phenotype | Reduces macrophage-derived signal |
| Stromal Normalization | Carcinoma-Associated Fibroblasts (CAFs) | Vitamin D, Vitamin A, Pirfenidone [79] | Reduces desmoplasia, improves drug delivery | Improves probe distribution & uniformity |
| Tumor Vessel Normalization | VEGF/VEGFR | Bevacizumab, Cediranib [79] | Improves pericyte coverage, reduces hypoxia | Reduces necrosis, normalizes perfusion |
| pH-Centric Therapy | NHE1, CA IX, MCTs | Amiloride, Acetazolamide, AZD3965 [79] | Increases extracellular pH, disrupts metabolic symbiosis | Mitigates acidosis-induced necrosis |
| Imaging Cell Death | Caspase-8 Activity | Ac-IETD-Amluc Probe [2] | Detects apoptosis/pyroptosis via BLI | Quantifies therapeutic efficacy |
Targeting Acidosis and Metabolic Symbiosis
The acidic TME is a key driver of tumor progression and necrosis. Normalization strategies aimed at disrupting this pH imbalance include:
- Targeting Proton Export: Inhibition of sodium-hydrogen exchangers (e.g., NHE1 with Amiloride or Cariporide) reduces the export of protons from cancer cells, thereby raising the extracellular pH [79].
- Inhibiting Carbonic Anhydrase: Agents like Acetazolamide target carbonic anhydrase IX (CA IX), an enzyme overexpressed in hypoxic tumor regions that facilitates acidification [79].
- Blocking Lactate Transport: Inhibiting monocarboxylate transporters (MCTs), particularly MCT1 and MCT4, with drugs like AZD3965 disrupts the lactate shuttle between stromal and cancer cells, a key element of metabolic symbiosis [79] [80].
These interventions work to neutralize the TME, which can inhibit the growth of acid-resistant cancer cells, reduce necrosis, and mitigate the confounding effects of acidosis on bioluminescence probes.
Monitoring Programmed Cell Death with Caspase-8 Probes
The accurate detection of specific cell death forms is crucial for assessing treatment efficacy. Traditional endpoint assays preclude longitudinal monitoring. The development of a Caspase-8-activated bioluminescence probe, Ac-IETD-Amluc, enables real-time, non-invasive imaging of apoptosis and pyroptosis in live subjects [2].
This probe consists of a tetrapeptide substrate (Ac-IETD) specific for Caspase-8, conjugated to a D-Aminoluciferin (Amluc) motif. Upon cleavage by activated Caspase-8, the free Amluc is oxidized by firefly luciferase in the presence of ATP and Oâ‚‚, generating a bioluminescent signal. This allows for sensitive quantification of programmed cell death, helping researchers distinguish therapeutic-induced apoptosis from nonspecific necrosis [2]. The workflow for using this probe is integrated into the comprehensive experimental protocol below.
Integrated Experimental Protocol for Normalization and Imaging
This section provides a detailed methodology for conducting a longitudinal therapy study that combines TME normalization with bioluminescence imaging to monitor cell death and inflammatory response.
Pre-study Preparation: Reagent Solutions and Animal Models
Table 2: Research Reagent Solutions and Essential Materials
| Item Name | Specification / Example Catalog Number | Primary Function in Protocol |
|---|---|---|
| Caspase-8 BLI Probe | Ac-IETD-Amluc [2] | Activated by Caspase-8 to enable specific detection of apoptosis/pyroptosis via bioluminescence. |
| Luminol Sodium Salt | L-012, Sigma-Aldrich [13] | Chemiluminescent substrate that emits light upon oxidation by MPO in activated neutrophils; general inflammation imaging. |
| pH Normalization Agent | Amiloride (e.g., A7410, Sigma) | NHE1 inhibitor for targeting tumor acidosis [79]. |
| Metabolism-Targeting Agent | AZD3965 (e.g., S8442, Selleckchem) | MCT1 inhibitor to disrupt lactate shuttle [79]. |
| IVIS Imaging System | PerkinElmer IVIS Spectrum [13] | High-sensitivity CCD camera for quantifying bioluminescence signals in live animals. |
| Firefly Luciferase-Expressing Cells | fLuc-4T1 (for murine models) [2] | Engineered cancer cells that enable bioluminescence imaging with D-luciferin or specialized probes. |
| Isoflurane Anesthesia System | VetFlo, Kent Scientific | Provides stable inhalation anesthesia during imaging procedures. |
| Living Image Software | PerkinElmer [13] | Standard software for quantifying total flux (photons/second) in defined Regions of Interest (ROIs). |
- Cell Line and Animal Model: Utilize firefly luciferase (fLuc)-expressing tumor cells (e.g., fLuc-4T1)[ccitation:2]. Establish subcutaneous or orthotopic tumors in immunocompromised or immunocompetent mice as required by the research question.
- Therapeutic Agents: Prepare stock solutions of normalization agents (e.g., Amiloride, AZD3965) and chemotherapeutic agents (e.g., Cisplatin) in accordance with manufacturer instructions and sterile filter if required for in vivo administration.
Step-by-Step Experimental Workflow
The following diagram outlines the integrated workflow for a longitudinal study combining normalization therapy and bioluminescence imaging.
Diagram 2: Integrated Workflow for Longitudinal Therapy and Imaging Study. This protocol outlines the key steps for evaluating TME normalization therapies, from tumor establishment and treatment randomization to longitudinal bioluminescence imaging and final data analysis.
Week 1-2: Tumor Inoculation and Baseline Imaging
- Inoculate mice with fLuc-expressing tumor cells.
- Monitor tumor growth until they reach a predefined volume (e.g., 50-100 mm³).
- On day 0, prior to therapy initiation, perform baseline bioluminescence imaging as described in the "Image Acquisition" section below.
Week 2-6: Therapeutic Intervention and Longitudinal Monitoring
- Randomize animals into cohorts (e.g., Control, Chemotherapy alone, Chemotherapy + Normalization Agent).
- Administer Therapies: Treat mice according to the established schedule for each agent (e.g., oral gavage for normalization drugs, intraperitoneal injection for chemotherapeutics).
- Longitudinal Imaging: On a weekly basis, image mice using the following procedure:
- Anesthetize mice using an isoflurane-oxygen mixture (typically 2-3% for induction, 1-2% for maintenance).
- Inject Probe: Administer the Caspase-8 BLI probe (Ac-IETD-Amluc, ~200 μL per dose via intraperitoneal or intravenous route) or other relevant bioluminescent agent [2].
- Image Acquisition: Place mice in the IVIS Spectrum imaging chamber with the tumor region directly facing the CCD camera. Acquire a series of images over 20-30 minutes post-injection using the following parameters [13]:
- Field of View: Appropriate to encompass all animals (e.g., Field A, B, or C).
- Binning: Medium (for optimal signal-to-noise ratio).
- Exposure Time: Auto or fixed (typically 1-300 seconds, ensuring no pixel saturation).
- Data Storage: Save images in the native IVIS file format for subsequent quantification.
Endpoint Analysis
- After the final imaging time point, euthanize animals and harvest tumor tissues.
- Process tumors for histological analysis (H&E staining) to quantify the extent of necrosis and correlate with in vivo imaging data.
Data Quantification and Normalization
Image Analysis:
- Open image sequences in Living Image software.
- Draw consistent Regions of Interest (ROIs) around the tumor boundary for each animal and at each time point.
- Use the software's tool to quantify the total flux (photons/second) within each ROI.
- For longitudinal tracking, normalize bioluminescence signal within each animal to its own baseline signal (from Day 0).
Accounting for Necrosis:
- In the final tumor sections, calculate the percentage of necrotic area relative to the total tumor area using histomorphometry.
- Statistically correlate the necrotic area with the terminal bioluminescence signal to identify and correct for potential confounding. A strong positive correlation may indicate that the signal is dominated by nonspecific inflammation associated with necrosis rather than therapy-induced cell death.
Integrating TME normalization strategies with advanced bioluminescence imaging protocols provides a more robust framework for evaluating anticancer therapies in preclinical models. By systematically targeting metabolic aberrations such as acidosis and by employing specific probes like Ac-IETD-Amluc to monitor programmed cell death, researchers can significantly enhance the specificity and interpretability of longitudinal imaging data. The protocols and reagents detailed herein offer a practical roadmap for scientists in drug development to dissect therapeutic mechanisms and improve the predictive power of their animal studies, ultimately facilitating the translation of more effective cancer treatments.
In the field of longitudinal in vivo bioluminescence imaging of inflammation, understanding and controlling the pharmacokinetics of your substrate is paramount. The route of administration is a critical experimental variable that directly dictates the biodistribution profile, influencing signal intensity, localization, and interpretation of results. Intravenous (IV) and intraperitoneal (IP) injections represent two fundamental delivery methods, each with distinct advantages and limitations for inflammation research. This application note provides a structured comparison of IP versus IV administration, summarizing key quantitative data, detailing standardized protocols for biodistribution studies, and offering a strategic framework for selecting the optimal route to enhance the reliability and relevance of your imaging data.
Quantitative Comparison of Biodistribution and Efficacy
The choice between IP and IV administration can lead to significantly different outcomes in terms of organ-level accumulation and overall therapeutic or imaging efficacy. The following tables synthesize findings from recent preclinical studies across various substrates, from nanoparticles to viral vectors.
Table 1: Biodistribution Profile Comparison (IP vs IV)
| Organ/Tissue | Intraperitoneal (IP) Administration | Intravenous (IV) Administration | Key Findings & Context |
|---|---|---|---|
| Peritoneal Tumors | High and targeted accumulation [81] | Lower, systemic distribution [81] | In pancreatic cancer models, IP injection significantly increased nanoparticle accumulation in orthotopic tumors compared to IV [81]. |
| Liver | Lower initial exposure [82] [83] | Primary site of accumulation [84] [83] | mRNA-LNPs and some nanoparticles show predominant hepatic uptake after IV, while IP can redirect distribution [84] [83]. |
| Spleen | Moderate exposure [82] | Significant uptake [84] | A key organ for immune response in inflammation studies. |
| Lungs | Reduced frequency of detection [82] | Frequent and persistent localization [84] [82] | Gold nanoparticles and oncolytic viruses show higher lung presence after IV injection [84] [82]. |
| Kidneys | Reduced frequency of detection [82] | Significant uptake and clearance pathway [84] [82] | Quantum dot nanocarbons persist in kidneys after IV administration [84]. |
| Heart | Reduced frequency of detection [82] | Variable (substrate-dependent) [84] [82] | Nanodiamonds can accumulate in the heart after IV injection [84]. |
| Systemic Circulation | Slower, more gradual absorption | Immediate and complete bioavailability | IV provides direct access, while IP requires absorption from the peritoneal cavity. |
Table 2: Efficacy and Toxicity Outcomes (IP vs IV)
| Parameter | Intraperitoneal (IP) Administration | Intravenous (IV) Administration | Key Findings & Context |
|---|---|---|---|
| Therapeutic Efficacy | Superior for peritoneal diseases [82] [81] | Superior for systemic or deep-seated targets [83] | IP administration of oncolytic virus doubled median survival in a peritoneal metastasis model versus IV [82]. |
| Localized vs Systemic Expression | Higher localized expression (e.g., skin, lymph nodes) [83] | Predominantly systemic (e.g., liver) [83] | After SC and IV mRNA-LNP administration, protein expression patterns differ significantly [83]. |
| Toxicity & Tolerability | Higher LD(_{50}) (reduced toxicity) [82] | Lower LD(_{50}) [82] | The restricted biodistribution of IP delivery is associated with a better tolerability profile [82]. |
| Inflammatory Response | Can be tailored and localized | Can trigger systemic inflammatory response [84] | IV-administered gold nanoparticles elicited significant IL-6 and T cell activation [84]. |
Experimental Protocols for Biodistribution Analysis
Accurately determining the biodistribution of an administered substrate is crucial for validating imaging data and understanding its biological fate. The following protocol, adapted from standardized guidelines for radiotracers, can be tailored for bioluminescence substrates and other imaging agents [85].
Ex VivoBiodistribution Study Protocol
Objective: To quantitatively determine the concentration of a substrate in various tissues at specific time points post IV or IP administration.
Materials:
- Test substrate (e.g., bioluminescence probe, nanoparticle, therapeutic agent)
- Experimental animal model (e.g., murine inflammation model)
- Syringes (e.g., 0.3 mL insulin syringe for IP, 1 mL for IV)
- Analytical balance (accuracy ≥ 0.0001 g)
- Dissection tools
- Pre-weighed tissue collection tubes
- Liquid nitrogen or other freezing apparatus for tissue preservation
- Appropriate analytical equipment (e.g., gamma counter for radiotracers, plate reader for fluorescence, LC-MS for small molecules)
Procedure:
- Study Design and Dose Preparation:
- Define time points based on the substrate's pharmacokinetics (e.g., 5 min, 1 h, 4 h, 24 h post-injection).
- Randomize animals into experimental groups.
- Precisely prepare the dosing solution. For quantitative analysis, a weighed standard dose should be prepared for calibrating the injected amount per animal [85].
Administration:
- Intraperitoneal (IP) Injection:
- Restrain the animal in a head-down position.
- Identify the lower left quadrant of the abdomen to avoid the cecum and midline organs.
- Insert the needle (25-27 gauge) at a 30-degree angle. Aspirate slightly to check for bodily fluids; if none, inject slowly.
- Intravenous (IV) Injection:
- Use a rodent restrainer. Gently warm the tail to dilate the veins.
- Identify one of the lateral tail veins. Insert the needle (27-30 gauge) parallel to the vein.
- Aspirate to confirm blood flashback, then inject slowly. A successful injection will show no resistance or swelling.
- Intraperitoneal (IP) Injection:
Tissue Collection:
- At each time point, euthanize animals according to approved ethical guidelines.
- Rapidly collect tissues of interest (e.g., liver, spleen, lungs, kidneys, heart, brain, lymph nodes, blood, and target inflammatory sites).
- Gently rinse tissues in saline, blot dry on absorbent paper, and place them in pre-weighed tubes. Record the precise weight of each tissue sample.
Sample Analysis:
- Process tissues according to the detection method (e.g., homogenization, digestion).
- Quantify the substrate concentration in each tissue using the appropriate analytical technique.
- Calculate the percentage of injected dose per gram of tissue (%ID/g) or other relevant pharmacokinetic parameters.
Data Processing:
- Use the following fundamental formula for %ID/g:
%ID/g = (Measured activity or mass in tissue / Weight of tissue (g)) / (Total injected dose) * 100
- Utilize standardized data processing tools, such as open-source biodistribution calculators, to ensure consistency and perform error propagation [85].
Strategic Workflow for Route Selection
The decision to use IP or IV administration should be guided by the specific research question, the nature of the inflammatory model, and the properties of the substrate. The following workflow diagram outlines the key decision points.
The Scientist's Toolkit: Research Reagent Solutions
Successful execution of biodistribution studies in inflammation imaging requires careful selection of materials and reagents.
Table 3: Essential Research Reagents and Materials
| Item | Function/Application | Example & Notes |
|---|---|---|
| Near-IR Fluorescent Dyes | In vivo and ex vivo imaging and biodistribution tracking. | Flamma Fluor 749: Conjugated to nanoparticles for sensitive detection of distribution in orthotopic tumor models [81]. |
| Radiolabeled Probes | Highly sensitive and quantitative biodistribution studies. | Iodine-125 (¹²âµI): A gamma-emitting isotope used for precise quantification of monoclonal antibody concentrations in tissues over time [86]. |
| Ionizable Lipids | Key component of Lipid Nanoparticles (LNPs) for mRNA delivery; impacts PK/BD. | SM-102, ALC-0315: The choice of ionizable lipid significantly affects mRNA-LNP biodistribution after both SC and IV injection [83]. |
| PEGylated Coatings | Surface functionalization to improve stability and circulation time. | PEG-Ale (Alendronate-PEG): Used to coat upconversion nanoparticles, providing colloidal stability and biocompatibility [81]. |
| Size Exclusion Chromatography (SEC) | Purification of nanoparticles or extracellular vesicles from protein aggregates. | Used to obtain pure, intact extracellular vesicle preparations with better integrity than ultracentrifugation [87]. |
| Gamma Counter | Essential instrument for quantifying radioactivity in tissue samples from radiolabeled biodistribution studies [85]. | Must be calibrated for the specific radioisotope's energy window and capable of decay correction. |
The decision between intraperitoneal and intravenous administration is fundamental to the experimental design of longitudinal in vivo imaging studies. IP delivery offers a strategic advantage for targeting peritoneal inflammation and localized diseases, often resulting in enhanced local efficacy and reduced systemic toxicity. In contrast, IV administration provides immediate and complete systemic exposure, which is necessary for targeting deep-seated organs or achieving rapid whole-body distribution. By integrating the quantitative comparisons, standardized protocols, and strategic workflow outlined in this application note, researchers can make an informed, rational choice of administration route, thereby enhancing the quality, reproducibility, and biological relevance of their data in inflammation research.
In longitudinal in vivo bioluminescence imaging of inflammation, researchers often face the challenge of signal saturation when tracking high concentrations of biological targets. Similar challenges exist in ultrasound localization microscopy (ULM) where accurate microbubble (MB) counting and localization are essential for reconstructing super-resolved microvasculature. Signal saturation occurs when high concentrations of emitting sources—whether bioluminescent cells or MBs—overlap, leading to inaccurate quantification and loss of critical spatial information. This article addresses these challenges by providing application notes and protocols for handling high-concentration conditions, drawing parallels between bioluminescence imaging and ULM methodologies to enhance quantitative accuracy in longitudinal inflammation studies.
Technical Background and Fundamental Concepts
The Signal Saturation Problem in Imaging
In both bioluminescence and ultrasound localization microscopy, signal saturation arises when emitter density exceeds the detection system's ability to resolve individual point sources. In bioluminescence imaging, conventional probes operating in the visible spectrum (400-700 nm) suffer from strong tissue absorption and scattering, limiting their dynamic range in deep tissues [52]. Similarly, in ULM, high MB concentrations cause overlapping point spread functions (PSFs), resulting in inaccurate localization and compromised image reconstruction [88] [89]. This saturation effect hampers quantitative analysis in longitudinal inflammation studies where precise tracking of immune cell populations or vascular changes is crucial.
The fundamental limitation stems from the diffraction barrier, which dictates that two emitters must be separated by at least half the wavelength of the detected signal to be resolved as distinct entities. In practice, saturation effects begin at much lower densities due to background noise, system imperfections, and PSF variability. Understanding these physical constraints is essential for developing effective strategies to overcome saturation limitations.
Advanced Probes and Technologies
Table 1: Advanced Imaging Probes and Their Characteristics
| Probe Type | Emission Peak | Key Advantages | Applications in Inflammation Research |
|---|---|---|---|
| NIR-II Bioluminescence Probes [52] | 1029 nm | ~5× higher SNR; ~1.5× higher spatial resolution; minimal tissue scattering | Deep-tissue inflammation monitoring; metastasis tracking with T/N ratio of 83.4 |
| LOCA-ULM [89] | N/A (Ultrasound) | 97.8% detection accuracy; 23.8% missing rate under high MB concentrations | Cerebrovascular imaging; functional ULM for hemodynamic response detection |
| Luminol [13] | 425 nm | Detects MPO activity from activated neutrophils | Acute inflammation models (EIU, PMU) |
| Cell-Type Specific Luciferase Reporters [20] | 560 nm (Firefly) | Cell population-specific monitoring | Longitudinal tracking of myeloid cells, T cells, and B cells in uveitis |
Materials and Reagents
Research Reagent Solutions
Table 2: Essential Research Reagents and Materials
| Item | Function/Application | Key Characteristics | Example Sources/Formulations |
|---|---|---|---|
| NIR-II-BPs [52] | Deep-tissue bioluminescence imaging | Emission at 1029 nm; BRET-FRET-FRET energy transfer; ATP-responsive | FD-1029 cyanine dye with DSPE-PEG2000 micelles |
| Microbubble Formulations [90] | Ultrasound contrast agents | Lipid shell (DSPC, HSPC) with perfluorocarbon core; 1-10 μm diameter | OFP gas core with lipid compositions (DSPC, mPEG2000-DSPE) |
| Luminol Sodium Salt [13] | Myeloperoxidase detection | Chemiluminescent substrate for neutrophil activity | 200 mg/kg IP injection; λmax = 425 nm |
| Cell-Type Specific Cre:LUC Models [20] | Immune cell population tracking | Myeloid (LyzM-cre), T-cell (Lck-cre), B-cell (Cd19-cre) specific | ROSA26-Luciferase with floxed stop sequence |
| LOCA-ULM Training Data [89] | Deep learning localization | LSGAN-generated MB templates; in vivo signal characteristics | Field-II simulations with system noise modeling |
Methodologies and Experimental Protocols
LOCA-ULM for High-Concentration Microbubble Localization
Protocol: Deep Learning-Enhanced Microbubble Localization
Sample Preparation
- Prepare lipid-shelled microbubbles with perfluorocarbon gas core using established formulations [90].
- Dilute MB samples to appropriate concentrations (typically 1:10-1:100 in PBS) for initial characterization.
- Characterize MB size distribution using optical methods with BubblesizerJ-2.0 ImageJ macro [90].
Data Acquisition
- Acquire in vivo ultrasound data using clinical or preclinical ultrasound systems.
- Set imaging parameters to maximize MB signal detection:
- Frequency: 1-10 MHz (depending on depth)
- Mechanical Index: 0.1-0.3 (for stable cavitation)
- Frame rate: 10-50 Hz (depending on flow velocity)
- Acquire data for 1-5 minutes depending on MB concentration and flow characteristics.
Data Processing with LOCA-ULM
- Generate realistic MB templates using Least-Squares Generative Adversarial Network (LSGAN) trained on in vivo MB signals [89].
- Train DECODE neural network with joint count loss and localization loss using simulated data with known ground truth positions.
- Apply trained network to experimental data for MB detection and localization.
- Post-process localization data to reconstruct super-resolved vascular maps.
Validation
- Compare localization performance with conventional methods (normalized cross-correlation) under varying MB concentrations.
- Quantify metrics including detection accuracy, missing rate, and localization error.
- Validate against known vascular phantoms or histological references when possible.
Figure 1: LOCA-ULM processing workflow for high-concentration microbubble localization.
NIR-II Bioluminescence for Inflammation Monitoring
Protocol: NIR-II Bioluminescence Imaging of Inflammation
Probe Preparation
- Synthesize NIR-II bioluminescence probes (NIR-II-BPs) through BRET-FRET-FRET cascade [52]:
- Prepare FD-1029 cyanine dye (absorption: 977 nm; emission: 1029 nm)
- Form micelles using DSPE-PEG2000 amphiphilic polymers
- Load with Cy5 and Cy7.5 as bridge fluorophores
- Conjugate with firefly luciferase (∼5 enzymes per micelle)
- Characterize probe properties: size distribution, energy transfer efficiency, and bioluminescence stability.
Animal Model Preparation
- Generate transgenic mouse lines expressing luciferase in specific immune cell populations [20]:
- Myeloid cells: LyzM-cre × ROSA26-LUC
- T cells: Lck-cre × ROSA26-LUC
- B cells: Cd19-cre × ROSA26-LUC
- Induce uveitis models: Primed Mycobacterial Uveitis (PMU), Endotoxin-Induced Uveitis (EIU), or Experimental Autoimmune Uveitis (EAU) [13] [20].
Image Acquisition
- Administer imaging substrate:
- For NIR-II-BPs: D-luciferin (150 mg/kg, intraperitoneal)
- For luminol imaging: Luminol sodium salt (200 mg/kg, intraperitoneal) [13]
- Anesthetize animals with isoflurane and position in imaging system.
- Acquire images using appropriate filters:
- NIR-II window: >1000 nm filter
- Standard bioluminescence: 500-600 nm range
- Capture multiple time points for longitudinal assessment (e.g., days 0, 2, 7, 14, 21, 28, 35).
Image Analysis
- Define regions of interest (ROIs) for inflamed eyes, control eyes, and background.
- Quantify total flux (photons/second) for each ROI.
- Calculate signal-to-noise ratios and compare across time points.
- For cell-type-specific imaging, correlate bioluminescence signals with flow cytometry data from matched time points.
Figure 2: NIR-II bioluminescence workflow for inflammation monitoring.
Quantitative Metrics and Performance Analysis
Performance Comparison Under Saturation Conditions
Table 3: Localization Performance Metrics Under High Emitter Concentrations
| Method | Detection Accuracy | Missing Rate | Localization Error | Optimal Concentration Range |
|---|---|---|---|---|
| Conventional ULM [88] | 80-85% | ~60% | ~1.5 μm | Low MB concentration (<300 MBs/mm²) |
| LOCA-ULM [89] | 97.8% | 23.8% | <1.0 μm | High MB concentration (>1000 MBs/mm²) |
| Deep-ULM [89] | ~85% | ~45% | ~1.2 μm | Moderate MB concentration |
| NIR-II Bioluminescence [52] | N/A | N/A | <1 mm spatial resolution | Not concentration-dependent |
Longitudinal Monitoring Capabilities
Table 4: Temporal Resolution and Longitudinal Monitoring Performance
| Imaging Modality | Temporal Resolution | Longitudinal Stability | Key Metrics for Inflammation Studies |
|---|---|---|---|
| Conventional BLI (Luminol) [13] | 5-minute acquisition windows | Signal returns to baseline by 48 hours in EIU | Peak bioluminescence: 1.46×10ⵠp/s (PMU); 3.18×10ⴠp/s (EIU) |
| Cell-Type Specific BLI [20] | Daily imaging feasible | 35-day monitoring demonstrated | Myeloid peak: Day 2; T-cell peak: Day 7; B-cell increase: Day 28+ |
| LOCA-ULM [89] | 1-2 minute acquisitions | Limited by MB circulation time | Vessel MB saturation time reduced by >50% |
| NIR-II BLI [52] | 5-minute acquisitions | >80% signal stability at 320 minutes | T/N ratio: 83.4 for metastasis detection |
Implementation Considerations
Optimization Strategies for Signal Saturation
When implementing these protocols for longitudinal inflammation studies, several optimization strategies can enhance performance under saturation conditions:
For microbubble imaging, carefully titrate MB concentrations to balance between rapid vascular filling and localization accuracy. LOCA-ULM enables higher concentration usage (≥1000 MBs/mm²) while maintaining localization precision [89]. Implement motion correction algorithms to compensate for respiratory and physiological movements during extended acquisitions.
For bioluminescence imaging, select appropriate luciferase-luciferin pairs based on the inflammatory model. Acute inflammation models with robust neutrophil infiltration benefit from luminol-based detection [13], while chronic models with adaptive immune responses require cell-type-specific luciferase reporters [20]. NIR-II probes provide superior penetration and spatial resolution for deep-tissue inflammation monitoring [52].
Validation and Quality Control
Rigorous validation is essential for reliable longitudinal quantification. For ULM, validate against histological sections or optical microscopy when possible. For bioluminescence imaging, correlate signals with flow cytometry data from matched time points to verify cell population changes [20]. Implement phantom studies and control experiments to establish baseline performance metrics and detect system drift over extended longitudinal studies.
Quality control measures should include regular calibration of imaging systems, standardization of substrate administration protocols, and implementation of background subtraction routines. For quantitative comparisons across time points, maintain consistent positioning, anesthesia protocols, and ROI definitions.
The protocols and application notes presented here provide researchers with robust methodologies for handling signal saturation in both microbubble imaging and bioluminescence applications. The advanced localization techniques like LOCA-ULM and NIR-II bioluminescence imaging significantly enhance quantitative capabilities under high emitter concentrations, enabling more accurate longitudinal assessment of inflammatory processes. By implementing these standardized protocols with appropriate quality control measures, researchers can achieve improved dynamic range and quantification accuracy in their inflammation studies, ultimately supporting more reliable therapeutic assessment and mechanistic understanding of inflammatory diseases.
Longitudinal in vivo bioluminescence imaging (BLI) is a powerful tool for monitoring biological processes such as inflammation over time in live animal models. A critical factor determining the validity and reproducibility of data generated in these studies is longitudinal consistency – the maintenance of precise imaging plane alignment across multiple experimental sessions. This application note details standardized protocols and analytical methods for achieving this consistency, framed within the context of preclinical inflammation research. We provide methodologies for animal positioning, imaging system configuration, and data normalization that enable researchers to minimize technical variability and enhance the detection of true biological signals in longitudinal studies of uveitis, encephalomyelitis, and other inflammatory conditions.
Longitudinal in vivo bioluminescence imaging enables researchers to track the progression of inflammation repeatedly in the same animal, significantly reducing the number of animals required for well-powered experiments compared to terminal endpoints [13] [20]. This approach is particularly valuable in preclinical drug development, where it allows for direct assessment of therapeutic efficacy over time.
However, a significant technical challenge in longitudinal BLI is maintaining consistent imaging plane alignment across sessions. Variations in animal positioning, camera angle, distance to sensor, and imaging parameters can introduce substantial measurement variability that may obscure true biological changes. In inflammation research, where bioluminescence signals can vary over several orders of magnitude throughout disease progression, these technical artifacts can compromise data interpretation and lead to erroneous conclusions [13] [91].
This protocol addresses these challenges by providing a standardized framework for achieving longitudinal consistency in BLI studies of inflammatory models. The methods have been validated across multiple inflammation models, including experimental autoimmune uveitis (EAU), primed mycobacterial uveitis (PMU), and autoimmune encephalomyelitis (EAE) [13] [20] [91].
Experimental Protocols for Longitudinal Imaging
Animal Preparation and Positioning Standardization
Materials:
- Anesthesia system (isoflurane recommended)
- Heating pad or IVIS warming stage
- Eye dilation agents (e.g., 2.5% phenylephrine)
- Ocular lubricant (e.g., Genteal)
- Custom positioning apparatus (e.g., Costar 50 ml reagent reservoir with one end removed)
Procedure:
- Anesthesia and Physiological Maintenance:
- Induce anesthesia with 3% isoflurane and maintain with 1.5-2% during imaging.
- Place animal on warming stage maintained at 37°C to prevent hypothermia.
- Apply ocular lubricant to prevent corneal drying during prolonged imaging.
Standardized Positioning:
- Utilize a custom positioning apparatus to maintain consistent animal orientation. For ocular imaging, position mice in lateral decubitus with the ocular surface directly facing the camera sensor [13].
- For brain and spinal cord imaging, position animals supine with head fixed in a standardized orientation using tooth bar and ear pins [91].
- Mark positioning landmarks on the imaging stage for reproducible placement across sessions.
Substrate Administration:
- Administer luminol sodium salt (200 mg/kg, intraperitoneal) for myeloperoxidase-dependent imaging of myeloid cells [13] [92].
- For luciferase-based systems, administer D-luciferin (150 mg/kg, intraperitoneal) 10 minutes before imaging [20] [91].
- Maintain consistent timing between substrate administration and image acquisition across all sessions.
Imaging System Configuration and Calibration
Materials:
- IVIS Spectrum Imaging System (PerkinElmer) or equivalent CCD camera system
- Living Image software or equivalent
- Light-tight imaging chamber
Procedure:
- System Calibration:
- Perform daily system calibration using internal standards.
- Verify camera sensitivity and background counts before each imaging session.
Parameter Standardization:
- Set field of view to "A" for mouse imaging.
- Use consistent subject height (typically 1.5 cm).
- Apply medium binning for optimal signal-to-noise ratio.
- Set exposure time to auto-expose within linear range or use fixed duration (typically 1-5 minutes) [13].
- Maintain identical f/stop and pixel binning settings across all sessions.
Background Control:
- Capture background image with no animal present at each session.
- Image non-expressing control animals periodically to establish background bioluminescence levels.
Image Acquisition and Analysis
Procedure:
- Image Capture:
Region of Interest (ROI) Analysis:
- Define standardized ROIs for each anatomical region (eyes, brain, spinal cord).
- Maintain consistent ROI size and positioning across sessions using anatomical landmarks.
- Measure total flux (photons/second) for each ROI after background subtraction.
- For inflammation studies, include a background ROI (e.g., top of head) to establish baseline [20].
Data Normalization:
- Normalize signals to baseline (pre-inflammation) measurements for each animal.
- Express data as fold-change over baseline or absolute flux with background subtraction.
Table 1: Quantitative Bioluminescence Signals in Inflammation Models
| Disease Model | Peak Signal (photons/second) | Baseline Signal (photons/second) | Fold Increase | Temporal Profile |
|---|---|---|---|---|
| PMU (Uveitis) | 1.46 × 10ⵠ| 1.47 × 10ⴠ| 9.9 | Acute (peak day 2) |
| EIU (Uveitis) | 3.18 × 10ⴠ| 1.09 × 10ⴠ| 2.9 | Acute (peak 18h) |
| EAU (Uveitis) | Non-significant increase | - | - | Chronic (indolent) |
| EAE (CNS) | 5-10 fold over baseline | Baseline levels | 5-10 | Peak at 14 dpi |
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagents for Longitudinal Bioluminescence Imaging
| Reagent/Category | Specific Examples | Function in Imaging |
|---|---|---|
| Bioluminescence Substrates | Luminol sodium salt | Detects MPO activity in neutrophils during acute inflammation [13] [92] |
| D-luciferin | Substrate for firefly luciferase in transgenic reporter systems [20] [91] | |
| Animal Models of Inflammation | Primed Mycobacterial Uveitis (PMU) | Acute anterior uveitis model with robust neutrophilic infiltration [13] |
| Experimental Autoimmune Encephalomyelitis (EAE) | CNS inflammation model for multiple sclerosis research [91] | |
| Cell-type-specific reporter mice (LyzM-cre, Lck-cre, Cd19-cre) | Enable monitoring of specific immune cell populations [20] | |
| Imaging Equipment | IVIS Spectrum System | Commercial CCD-based bioluminescence imaging system [13] |
| Custom positioning apparatus | Ensures reproducible animal placement across sessions [13] | |
| Validation Tools | Flow cytometry | Gold standard for validating immune cell infiltration [20] |
| Histopathology | Provides spatial context for bioluminescence signals [91] |
Workflow Visualization
Figure 1: Experimental workflow for longitudinal bioluminescence imaging.
Data Interpretation and Technical Validation
Correlation with Gold Standard Measures
Longitudinal BLI data must be validated against terminal endpoints to establish biological relevance:
Flow Cytometry Correlation:
- In PMU models, bioluminescence signals strongly correlate with flow cytometry quantification of infiltrating immune cells [20].
- Acute phase (day 2): 78% neutrophils, 12% T-cells of CD45+ cells.
- Chronic phase (day 35): 5% neutrophils, 50% T-cells, 4% B-cells of CD45+ population.
Histopathological Validation:
- In EAE models, GFAP-luc bioluminescence correlates with astrogliosis (GFAP immunoreactivity) and microgliosis (CD68 immunoreactivity) [91].
- Bioluminescence signals precede clinical symptoms by several days, enabling early disease detection.
Troubleshooting Alignment Issues
Signal Variability Between Sessions:
- If signal variability exceeds 15-20% between technical replicates, verify positioning consistency.
- Confirm substrate injection technique and timing.
Background Contamination:
- High background may indicate substrate contamination or insufficient background subtraction.
- Image non-inflamed control animals to establish acceptable background levels.
Anatomical Localization Challenges:
- Use overlay with white light images for anatomical reference.
- For deep tissues, consider complementary imaging modalities (e.g., MRI) for initial localization.
Maintaining imaging plane alignment across multiple sessions is essential for generating reliable longitudinal bioluminescence data in inflammation research. The protocols outlined herein provide a standardized approach for achieving this consistency, enabling researchers to distinguish true biological signals from technical artifacts. By implementing these methods for animal preparation, system configuration, and data analysis, researchers can enhance the reproducibility and translational potential of their preclinical studies in inflammatory disease models.
The integration of these alignment strategies with cell-type-specific reporter systems and validation endpoints creates a robust framework for monitoring immune responses throughout disease progression and therapeutic intervention. As BLI technology continues to evolve, these foundational principles of longitudinal consistency will remain critical for extracting meaningful biological insights from live animal imaging studies.
Validation Approaches and Multimodal Integration: Correlating BLI with Conventional Metrics
In the field of longitudinal in vivo bioluminescence imaging (BLI) of inflammation, validating the cellular and molecular signals detected by this sensitive optical method remains a critical challenge. BLI enables real-time tracking of inflammatory processes and specific immune cell populations in live animals by leveraging the expression of luciferase reporter genes [21] [20]. However, the technique has inherent limitations, including limited spatial resolution and an inability to provide specific cellular or molecular phenotypes based on photon emission alone [93] [94]. Consequently, correlation with established ex vivo gold standards is essential for definitive biological interpretation.
This Application Note details the methodology for correlating BLI data with the gold standard of bronchoalveolar lavage (BAL) cytology and cytokine profiling, with a specific focus on models of pulmonary inflammation. BAL provides a direct window into the pulmonary microenvironment by allowing for quantitative cellular analysis and soluble factor measurement within the epithelial lining fluid [95] [96]. We present standardized protocols for BAL fluid processing, analytical techniques, and the integration of this validated data with longitudinal BLI datasets to enhance the rigor and interpretability of in vivo imaging studies.
Bronchoalveolar Lavage as a Diagnostic Gold Standard
Bronchoalveolar lavage is a well-established clinical and research procedure that allows for sampling of the lower respiratory tract. The technique involves instilling sterile saline into a specific bronchopulmonary segment via a bronchoscope and then aspirating the fluid for analysis [95]. The recovered BAL fluid (BALF) contains cells and soluble mediators directly from the alveolar space, providing a representative snapshot of the pulmonary immune status [95].
BAL Cellular Analysis
Cellular analysis of BALF is fundamental for characterizing inflammatory responses. In healthy subjects, BALF is typically macrophage-predominant (approximately 85%), with lymphocytes comprising about 10%, neutrophils approximately 5%, and eosinophils and basophils each less than 1% [95]. Deviations from this profile provide critical diagnostic information, as shown in Table 1.
Table 1: BAL Cellular Patterns in Inflammatory Lung Conditions
| Condition | Predominant BAL Cell Type | Key Characteristics |
|---|---|---|
| Healthy (Non-smoker) | Macrophages (~85%) | Low lymphocytes (~10%), neutrophils (~2%) [95] |
| Acute Eosinophilic Pneumonia | Eosinophils | Significant eosinophilia supports diagnosis [95] |
| Sarcoidosis/HP | Lymphocytes | Lymphocytic predominance with compatible clinical history [95] |
| Cystic Fibrosis | Neutrophils | Neutrophil-predominant even between exacerbations [95] |
| COVID-19 (Severe) | Neutrophils | High neutrophil/lymphocyte ratio associates with poor outcome [96] |
| Invasive Pulmonary Aspergillosis | Neutrophils/Inflammatory | IL-8 ≥904 pg/mL in BALF predicts infection [97] |
BAL Cytokine Profiling
Analysis of soluble cytokines and chemokines in BALF provides a quantitative measure of the local immune environment. This profiling is particularly valuable for identifying specific inflammatory pathways activated in disease states. For instance, in invasive pulmonary aspergillosis (IPA), a distinct cytokine signature emerges, with IL-1β, IL-6, IL-8, IL-17A, IL-23, and TNFα significantly elevated in BALF from infected patients [97]. Among these, IL-8 has demonstrated particularly strong diagnostic performance, with alveolar levels ≥904 pg/mL predicting IPA with 90% sensitivity and 73% specificity [97].
Similarly, in critically ill COVID-19 patients, a decompartimentalized immune response—characterized by lower BALF-to-blood ratios of IL-6, IL-10, and IFN-γ—is associated with poor 28-day outcomes [96]. In lung transplant recipients, a BAL protein signature including CXCL10, IL6, and S100A8 can predict the subsequent development of chronic lung allograft dysfunction or death [98]. These findings underscore the prognostic and diagnostic utility of BAL cytokine profiling.
Correlation of BLI with BAL Parameters
The correlation between non-invasive BLI signals and gold-standard BAL parameters validates the imaging approach and enhances its biological relevance. This multi-modal strategy is exemplified in a syngeneic mouse model of lung metastasis, where BLI and μCT provided complementary biomarkers describing different aspects of disease progression [94].
Cell-Type-Specific BLI Validation
Cell-type-specific BLI can be powerfully validated through BAL cytology. In the Primed Mycobacterial Uveitis (PMU) model, despite being an ocular inflammation model, the principle applies directly to pulmonary research: flow cytometry of infiltrating cells at serial timepoints confirmed that bioluminescence signals from myeloid-specific (LyzM-cre), neutrophil-specific (S100A8-cre), T-cell-specific (Lck-cre), and B-cell-specific (Cd19-cre) reporter lines accurately reflected changes in the respective immune cell populations [20]. For example, the acute inflammatory phase (day 2) was predominantly neutrophilic (78% of CD45+ cells), which correlated with a significant increase in bioluminescence from the S100A8-cre reporter line [20].
Table 2: Correlation of BAL Cytology with BLI and Other Modalities
| Analysis Method | Key Parameters | Correlation Value with BLI | Applications in Validation |
|---|---|---|---|
| BAL Cytology & Flow Cytometry | Cell differential (%, absolute count); Lymphocyte phenotyping | Direct cellular validation | Confirms immune cell populations causing BLI signal [20] [96] |
| BAL Cytokine Profiling | Concentrations of IL-8, IL-6, IFN-γ, etc. (pg/mL) | Pathway/mechanism validation | Links BLI intensity to specific inflammatory pathways [97] |
| Micro-Computed Tomography (μCT) | Lung tissue volume, aerated lung volume, mean density | Anatomical/morphological correlation | Provides anatomical context for BLI signal location [94] |
| Histopathology | Tissue structure, cellular infiltration, injury | Terminal gold standard | Definitive structural and cellular analysis post-imaging [94] |
Inflammatory Pathway Correlation
Beyond cellular correlation, BAL cytokine profiling can link BLI signals to specific molecular pathways. A study investigating invasive pulmonary aspergillosis used random forest analysis to identify the most important cytokines discriminating infection from controls, finding that IL-8 was the dominant discriminator [97]. In a BLI study of inflammation, a strong correlation between increasing photon flux and elevated BALF concentrations of IL-8, IL-1β, and IL-6 would strongly suggest that the BLI signal reflects a neutrophilic and pro-inflammatory environment, thereby validating the biological significance of the optical imaging data.
Experimental Protocols
Protocol 1: Bronchoalveolar Lavage in Rodents
Objective: To obtain representative cellular and soluble material from the lower respiratory tract for correlation with BLI data.
Materials:
- Anesthetized mouse or rat
- Sterile saline (0.9%)
- Tracheal catheter or cannula
- Syringe (1-3 mL)
- Microcentrifuge tubes
- Refrigerated centrifuge
Procedure:
- Anesthesia and Preparation: Ensure the animal is under deep surgical anesthesia. Secure the animal in a supine position. Perform a midline neck incision to expose the trachea.
- Tracheal Cannulation: Carefully insert a sterile catheter or cannula into the trachea and secure it with a suture to prevent dislodgement.
- Lavage Instillation and Aspiration:
- Attach a syringe containing the calculated volume of sterile, warm saline (e.g., 1 mL for a mouse, 3 mL for a rat) to the catheter.
- Slowly instill the saline into the lungs. Gently aspirate the fluid back into the same syringe. The recovery rate is typically 50-80%.
- Place the collected BALF on ice immediately.
- Sample Processing:
- Centrifuge the BALF (4°C, 400-500 x g, 10 minutes) to separate cells from supernatant.
- Cell Pellet: Re-suspend in PBS for total cell count using a hemocytometer. Prepare cytospin slides for differential cell count (e.g., May-Grunwald-Giemsa stain). Analyze by flow cytometry for immune cell subsets.
- Cell-Free Supernatant: Aliquot and store at -80°C for subsequent cytokine/chemokine analysis.
Protocol 2: Cytokine Profiling of BAL Fluid
Objective: To quantify the concentration of inflammatory mediators in BALF using a multiplex immunoassay.
Materials:
- BALF cell-free supernatant
- Multiplex cytokine assay kit (e.g., ProcartaPlex, Quanterix CorPlex)
- Magnetic plate washer
- Luminex platform or digital ELISA analyzer
- Microcentrifuge tubes
Procedure:
- Sample Preparation: Thaw BALF samples on ice. Centrifuge briefly to pellet any precipitates.
- Assay Setup: Following the manufacturer's instructions for the multiplex panel, prepare standards, controls, and samples in the assay plate.
- Incubation: Add the BALF samples and standards to the plate containing antibody-conjugated magnetic beads. Seal the plate and incubate with shaking. Wash the plate as directed.
- Detection: Add the detection antibody mixture, incubate, wash, and then add the streptavidin-PE reporter. After a final wash, re-susend the beads in reading buffer.
- Data Acquisition and Analysis: Run the plate on the Luminex instrument or digital ELISA analyzer. Use the standard curve to interpolate cytokine concentrations in the samples (pg/mL). Normalize data to total protein concentration or BALF volume.
Protocol 3: Correlative Timepoint Analysis for Longitudinal BLI
Objective: To validate longitudinal BLI data with terminal BAL analysis at strategic timepoints.
Procedure:
- Experimental Groups: Divide subjects into cohorts for longitudinal BLI and terminal analysis.
- BLI Acquisition: Acquire BLI signals at predetermined intervals (e.g., baseline, day 1, 3, 7, 14) following inflammatory stimulus or cell administration. Administer the relevant substrate (e.g., D-luciferin for firefly luciferase) and image using a cooled CCD camera system. Quantify the total flux (photons/second) from defined regions of interest.
- Terminal BAL Collection: At each key timepoint (e.g., peak BLI signal, signal resolution), euthanize a cohort of animals and perform BAL as described in Protocol 1.
- Data Integration: Correlate the magnitude of the BLI signal with the corresponding BAL parameters (e.g., neutrophil count, IL-6 concentration) from the same timepoint. Use statistical analysis (e.g., Pearson correlation) to establish the strength of the relationship.
Signaling Pathways and Inflammatory Biomarkers
The inflammatory response in the lung is a coordinated event driven by specific signaling pathways that recruit immune cells and promote the release of cytokines. BAL analysis directly measures the output of these pathways, providing a mechanistic context for BLI signals.
Diagram 1: Inflammatory Signaling Cascade Linking BLI and BAL Biomarkers. This pathway illustrates how an initial stimulus triggers cytokine release (detectable in BAL) and immune cell recruitment (quantifiable by BAL cytology and specific BLI reporter lines).
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Correlative BLI and BAL Studies
| Reagent / Assay | Function / Application | Specific Example |
|---|---|---|
| Firefly Luciferase (FLuc) Reporters | Engineered into cells or animals for BLI; requires D-luciferin substrate [21]. | Red-shifted Luciola italica luciferase for improved tissue penetration [93]. |
| Cell-Type-Specific Cre Drivers | Enables targeted luciferase expression in specific immune lineages for BLI [20]. | LyzM-cre (myeloid), Lck-cre (T cells), Cd19-cre (B cells), S100A8-cre (neutrophils) [20]. |
| D-Luciferin | Substrate for firefly luciferase; administered intraperitoneally for in vivo BLI [21]. | Potassium salt formulation, typically 126-150 mg/kg dose in mice [20] [94]. |
| Multiplex Cytokine Assays | Simultaneously quantify multiple cytokines/chemokines from small volume BALF samples [97] [96]. | ProcartaPlex panels, Quanterix CorPlex, or digital ELISA (Simoa) [99] [96]. |
| Flow Cytometry Antibodies | Characterize and quantify immune cell populations in BALF cell pellets. | Antibodies against CD45 (pan-leukocyte), CD11b (myeloid), CD3 (T cells), etc. [20] [96]. |
| Exosome Isolation Kits | Isolate exosomes from BALF or serum for analysis of encapsulated cytokines [99]. | Ultracentrifugation (highest purity) or commercial polymer-based precipitation kits (high yield) [99]. |
| Micro-CT Imaging | Provides high-resolution anatomical context for BLI signals in lung imaging studies [94]. | Respiratory-gated μCT scans to quantify lung volume, density, and tumor load [94]. |
Integrating bronchoalveolar lavage cytology and cytokine profiling with longitudinal bioluminescence imaging creates a powerful framework for validating and interpreting in vivo data in models of pulmonary inflammation. While BLI offers unparalleled sensitivity for tracking biological processes over time, BAL provides the essential cellular and molecular resolution that transforms photon flux into biologically meaningful insights. The standardized protocols and correlation strategies outlined in this Application Note will enable researchers to design more robust experiments, leading to greater confidence in their conclusions regarding immune cell dynamics, therapeutic efficacy, and disease progression. This multi-modal approach ensures that the compelling visual data generated by BLI are firmly grounded in established pathological and immunological gold standards.
Within the framework of longitudinal in vivo bioluminescence imaging (BLI) for inflammation research, ex vivo validation serves as a critical bridge, confirming that the optical signals detected in living animals accurately represent underlying molecular and pathological events. While in vivo BLI enables non-invasive, real-time tracking of processes such as neuroinflammation or immune cell recruitment in experimental autoimmune encephalomyelitis (EAE) models [100], the technique faces limitations, including signal attenuation by overlying tissues and an inability to provide precise spatial localization of the signal source. Ex vivo luciferase activity assays on excised tissues address these limitations by offering higher sensitivity, direct correlation with histopathology, and the ability to detect minute foci of activity, such as micro-metastases in cancer models or isolated inflammatory lesions [62] [100]. This protocol details the methodologies for quantifying luciferase activity in excised tissues, ensuring that longitudinal imaging data are validated with robust, endpoint analyses.
Quantitative Correlation Between Ex Vivo BLI and Pathological Markers
Ex vivo bioluminescence imaging (BLI) signals from tissues can be rigorously quantified and have demonstrated strong correlations with established measures of disease burden, including histopathology and DNA-based detection methods. The strength of this correlation, however, is highly dependent on the tissue type.
Table 1: Correlation of Ex Vivo BLI with Orthogonal Validation Methods
| Tissue Type | Validation Method | Correlation Coefficient (r) / Key Finding | Reference |
|---|---|---|---|
| Lung | Histology & Alu-qPCR | ~0.8 (Strong Correlation) | [62] |
| Bone | Histology & Alu-qPCR | ~0.4 (Considerable Discrepancy) | [62] |
| Brain & Spinal Cord (EAE model) | Clinical Score | 0.715 (Brain), 0.868 (Spinal Cord) | [100] |
| Brain & Spinal Cord (EAE model) | Astrogliosis (GFAP) | 0.801 (Brain), 0.858 (Spinal Cord) | [100] |
| Brain & Spinal Cord (EAE model) | Microgliosis (CD68) | 0.844 (Brain), 0.828 (Spinal Cord) | [100] |
| Brain & Spinal Cord (EAE model) | T-cell Infiltration (CD4) | 0.831 (Brain), 0.855 (Spinal Cord) | [100] |
The data underscore a critical consideration: ex vivo BLI is a reliable surrogate for pathological changes in soft tissues like lung and brain, but its accuracy diminishes in complex, mineralized tissues like bone. Consequently, for comprehensive validation, combining ex vivo BLI with a secondary method such as histology or PCR is strongly recommended, especially for bone metastasis studies [62].
Detailed Experimental Protocol for Ex Vivo BLI
This protocol is adapted from established procedures for quantifying metastatic burden and neuroinflammation in rodent models [62] [100].
Materials and Reagents
Table 2: Research Reagent Solutions for Ex Vivo Luciferase Assay
| Reagent / Material | Function | Example & Specification |
|---|---|---|
| D-Luciferin | Substrate for firefly luciferase (Fluc); oxidized by luciferase to produce light. | Potassium or sodium salt; 15 mg/mL stock in molecular biology grade Hâ‚‚O [101]. |
| Luciferase Lysis Buffer | Lyses cells while preserving luciferase enzyme activity for sensitive detection. | Compatible with firefly luciferase assays; avoids interference with bioluminescent reagents [101]. |
| Phenol Red-Free Culture Medium | Medium for explant culture; phenol red can interfere with optical imaging. | e.g., Phenol red-free DMEM, supplemented with B27 and luciferin [102]. |
| Passive Lysis Buffer (PLB) | Gently lyses cells for assays with secreted luciferases (e.g., Renilla, Gaussia). | Used for Renilla luciferase reporter assays [101]. |
| Coelenterazine | Substrate for Renilla (Rluc) and Gaussia (Gluc) luciferases. | Dissolved in acidified methanol; 1 mg/mL stock [101]. |
Step-by-Step Procedure
Animal Preparation and Substrate Administration:
- At the experimental endpoint, anesthetize the animal according to approved institutional guidelines.
- Administer the appropriate luciferase substrate intraperitoneally. For firefly luciferase, inject 150 mg/kg body weight of D-luciferin [62] [100].
- Allow 10 minutes for systemic distribution and uptake before sacrifice [100].
Tissue Harvest and Preparation:
- Sacrifice the animal humanely via a method such as cervical dislocation [62].
- Rapidly dissect and excise the tissues of interest (e.g., brain, spinal cord, lungs, limbs).
- For limbs or other hard tissues, carefully remove all surrounding muscle tissue using a scalpel, scissors, and cellulose cloths to minimize background signal [62].
- Place the cleaned tissues in a Petri dish or an imaging plate for immediate analysis.
Ex Vivo Imaging and Signal Acquisition:
- Transfer the tissues to the imaging chamber of a cooled CCD camera system (e.g., IVIS series, Perkin Elmer).
- Acquire the bioluminescence signal using auto-exposure or a predetermined integration time (e.g., 1-5 minutes) [62] [100].
- Quantify the signal intensity as total flux (photons per second, p/s) or average radiance (p/s/cm²/sr) using dedicated software (e.g., Living Image) [62] [100].
Post-Imaging Sample Processing for Downstream Analysis:
- For DNA-based quantification (e.g., Alu-qPCR): Tissues designated for PCR (e.g., the lung or the limb with lower BLI signal) should be processed accordingly. Bones can be cut transversely, and the marrow pelleted by centrifugation. Tissues are then homogenized, and DNA is isolated using a commercial kit [62].
- For histology: The contralateral tissue (e.g., the lung or the limb with higher BLI signal) is fixed in 4% paraformaldehyde, cryoprotected in sucrose, and sectioned for immunohistochemical staining with antibodies against markers like GFAP, CD68, or CD4 [62] [100].
Data Normalization and Statistical Analysis
- Normalization: For luciferase reporter assays from tissue lysates, the ratiometric method (Firefly/Renilla) is common but can be biased with low transfection efficiency. Regression-based methods, particularly Robust Errors-in-Variables (REIV) regression, are superior for normalizing data from samples with high variability [103].
- Statistical Analysis: Correlation between BLI signal and pathological scores is typically analyzed using Pearson correlation analysis. For comparing groups, an unpaired two-sample t-test is appropriate, while ANOVA is used for comparing more than two groups [104] [100].
Diagram 1: Experimental workflow for ex vivo luciferase activity validation, showing parallel processing for imaging and molecular analysis.
Advanced Applications: Imaging Programmed Cell Death
Beyond tracking cells, luciferase assays can be engineered to report on specific signaling pathway activities. For inflammation research, where programmed cell death (e.g., apoptosis, pyroptosis) plays a key role, Caspase-8-activated bioluminescence probes represent a cutting-edge application.
These probes, such as Ac-IETD-Amluc, consist of a Caspase-8-specific cleavage peptide (Ac-IETD) linked to a modified luciferin (Aminoluciferin). In the presence of active Caspase-8 during apoptosis or pyroptosis, the peptide is cleaved, releasing the luciferin motif. This free luciferin is then available for the firefly luciferase enzyme, producing a bioluminescent signal that reports directly on cell death activity in tumors or inflamed tissues [2].
Diagram 2: Caspase-8-activated bioluminescence probe mechanism for imaging programmed cell death.
Technical Considerations and Troubleshooting
- Tissue Depth and Signal Attenuation: Bioluminescence signals from deeper tissue layers are weaker due to absorption and scattering by the tissue itself. Using luciferases that emit red-shifted light can improve sensitivity [1].
- Substrate Kinetics: The timing of image acquisition is critical. For firefly luciferase with IP injection of D-luciferin, the signal typically peaks around 10 minutes and remains stable for ~30 minutes. Imaging should be performed within this window [1].
- Signal Saturation and Linearity: Ensure the camera acquisition settings are within the linear range. Very bright signals from large tumors can saturate the CCD camera, leading to inaccurate quantification. Reducing the acquisition time or aperture can mitigate this [1].
- Optical Enhancement: For very weak signals, such as those from single cells in tissue explants, optical telecompression using a high numerical aperture objective with a magnification-reducing relay lens can significantly increase light collection efficiency without increasing background noise [102].
In the context of longitudinal in vivo bioluminescence imaging (BLI) of inflammation, understanding how this non-invasive technology compares with traditional histological endpoints is crucial for research and drug development. BLI enables real-time monitoring of biological processes in living animals, while histopathology and immunohistochemistry (IHC) provide detailed, terminal analyses of tissue morphology and protein expression at specific time points.
This application note details a structured methodology for the direct comparison of ex vivo BLI with histopathology and IHC for quantifying metastases, enabling researchers to validate and contextualize BLI findings within established pathological frameworks.
## Experimental Protocol: Correlative Analysis of Metastatic Burden
### Background and Principle
The spontaneous metastasis xenograft model is a cornerstone of cancer research, replicating the complex process of cancer dissemination from a primary tumor to distant sites. A study of 93 immunodeficient mice subcutaneously injected with luciferase-labeled human prostate cancer PC-3 cells demonstrated a protocol for quantifying spontaneous bone and lung metastases using three independent methods: ex vivo BLI, DNA-based Alu-qPCR, and histology [62].
The core principle is to leverage the strengths of each technique: BLI for rapid, sensitive screening of whole organs; histology for morphological validation and precise localization; and Alu-qPCR for quantitative, human-specific DNA detection. This multi-faceted approach overcomes the individual limitations of each method, providing a comprehensive assessment of metastatic burden [62].
### Materials and Reagents
- Animals: 8-12 week-old immunodeficient NSG mice (NOD.Cg-Prkdcscid Il2rgtm1Wjl/SzJ) [62].
- Cell Line: Human prostate cancer PC-3 cells, transduced with a lentiviral Luc2-containing RGB vector for stable luciferase expression [62].
- BLI Substrate: D-Luciferin (150 mg/kg body weight, administered intraperitoneally) [62].
- Imaging System: IVIS 200 Imaging System (PerkinElmer) or equivalent [62].
- Analysis Software: Living Image Software (PerkinElmer) for BLI signal quantification in photons/second (p/s) [62].
- Tissue Processing: Supplies for histology (formalin, paraffin, embedding molds) and Alu-qPCR (DNA isolation kits, human-specific Alu primers) [62].
### Step-by-Step Procedure
Primary Tumor Implantation and Resection:
- Subcutaneously inject
1 × 10^6PC-3-Luc2 cells above the scapula of each mouse. - Allow the primary tumor to grow until it reaches ~0.75 cm³.
- Surgically remove the primary tumor [62].
- Subcutaneously inject
Metastasis Outgrowth:
- Monitor mice for approximately 3 weeks post-resection to allow for the development of spontaneous metastases [62].
Terminal Analysis and Sample Collection:
- At the experimental endpoint, anesthetize mice and administer D-Luciferin via intraperitoneal injection.
- Ten minutes post-injection, perform an initial in vivo BLI scan to detect systemic metastatic burden.
- Sacrifice the animal and immediately isolate the lungs and hind limbs.
- Remove all surrounding muscle tissue from the hind limbs carefully.
- Perform ex vivo BLI on the isolated organs to detect micro-metastases. Record the bioluminescence signal as total flux (p/s) for each organ [62].
Sample Allocation for Correlative Analysis:
- For Paired Organs (e.g., Hind Limbs): The limb with the higher BLI signal (BLIHi bone) is processed for histology. The contralateral limb with the lower signal (BLILo bone) is processed for Alu-qPCR [62].
- For Lungs: The left lung lobes are typically processed for Alu-qPCR, while the right lungs are prepared for histology [62].
Parallel Processing with Traditional Methods:
- Histology and IHC: Fix BLIHi bones and right lungs in formalin, decalcify bones, embed in paraffin, and section. Perform standard H&E staining. Confirm the human origin of metastatic deposits using IHC with antibodies against firefly luciferase or human-specific markers [62].
- Alu-qPCR: Homogenize lung samples. For bone marrow, centrifuge transversely cut femora and tibiae to pellet the marrow. Isolate DNA from the pellets and homogenates. Perform qPCR with human-specific Alu primers to quantify the human tumor cell load [62].
### Data Analysis and Correlation
Correlate the quantitative data from all three methods. The 2024 study revealed that the correlation between these methods is organ-dependent [62].
- For Lung Metastases: A strong correlation was observed between ex vivo BLI, Alu-qPCR, and histology (correlation coefficient, r ~ 0.8) [62].
- For Bone Metastases: A considerable discrepancy was noted, with a much weaker correlation between methods (r ~ 0.4). This highlights the challenges of quantifying tumor burden in bone and underscores the necessity of a multi-method approach for accurate assessment [62].
Table 1: Summary of Metastasis Detection by Different Methods in a PC-3 Xenograft Model [62]
| Method | Organ | Metastasis Detection Rate | Quantitative Range |
|---|---|---|---|
| Alu-qPCR | Lung | 100% (n=93/93) | N/A |
| Histology | Lung | 100% (n=13/13) | N/A |
| BLI | Lung | 100% (n=91/91) | 5.72 × 10^6 to 4.82 × 10^10 p/s |
| Alu-qPCR | Bone | 71.6% (n=53/74) | N/A |
| Histology | Bone | 18.7% (n=14/75) | N/A |
| BLI | Bone (BLIHi) | 100% (n=75/75) | 1.69 × 10^5 to 2.02 × 10^10 p/s |
| BLI | Bone (BLILo) | 100% (n=75/75) | 8.61 × 10^4 to 8.61 × 10^6 p/s |
## The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagent Solutions for BLI and Correlative Histology
| Item | Function/Application | Key Considerations |
|---|---|---|
| Firefly Luciferase (Fluc) | Primary reporter enzyme for BLI. Catalyzes light emission from D-luciferin [1] [21]. | Requires ATP, emits glow-type kinetics (562 nm peak). Ideal for longitudinal monitoring [1]. |
| D-Luciferin | Substrate for Fluc. Crosses cell membranes freely [21]. | For IP injection, signal peaks ~10 min and remains stable for ~30 min [1]. |
| IVIS Imaging System | High-sensitivity CCD camera system for detecting bioluminescent signal [105]. | Enables quantification of photon flux (p/s) from regions of interest (ROIs) [62] [105]. |
| Lentiviral RGB Vectors | For stable, high-efficiency transduction of luciferase gene into target cells [62]. | Ensures consistent and heritable luciferase expression in transplanted cells and their progeny. |
| Human-Specific Antibodies | IHC validation of human tumor cells in mouse tissue (e.g., anti-luciferase Abs) [62]. | Critical for confirming the human origin of micro-metastases and single disseminated cells. |
| Alu-qPCR Primers | Quantitative detection of human-specific Alu sequences in mouse tissue [62]. | Provides a highly sensitive and objective measure of human tumor cell load, independent of luciferase activity. |
## Comparative Workflow and Data Interpretation
The following diagram illustrates the integrated workflow for comparing BLI with traditional endpoints, highlighting the divergent paths for sample processing and the final correlative analysis.
Diagram Title: Workflow for Correlative BLI and Traditional Analysis.
### Critical Considerations for Data Interpretation
- Promoter Choice: The promoter driving luciferase expression (e.g., CMV) can be non-specifically regulated by cellular stimuli (e.g., NF-κB activation by some cancer treatments), leading to false conclusions about cell viability [1].
- Tumor Size and Substrate Access: Larger tumors may have higher substrate uptake, potentially leading to an overestimation of tumor burden. Necrotic areas within tumors can result in an underestimation [1].
- Signal Saturation: The high sensitivity of BLI can lead to signal saturation by CCD cameras, necessitating a reduction in acquisition time to maintain a linear range [1].
- Tissue Attenuation: Light is absorbed and scattered by mammalian tissues, with blue-green light (e.g., from Renilla luciferase) being more affected than red light. The use of red-shifted luciferases is recommended for imaging deep tissues [1].
Ex vivo BLI serves as a powerful, high-throughput screening tool for detecting metastatic burden, particularly for micro-metastases in organs like bone. However, the observed discrepancies in bone metastasis quantification emphasize that BLI should not be used as a standalone method for definitive quantification in all tissues. Instead, the most robust experimental designs incorporate ex vivo BLI as a primary screen, followed by confirmation and precise quantification using histology/IHC and/or DNA-based methods like Alu-qPCR. This integrated protocol provides a validated framework for researchers to confidently utilize BLI in longitudinal studies while grounding their findings in the concrete, spatially resolved data provided by traditional pathological endpoints.
This application note details a protocol for the integration of Bioluminescence Imaging (BLI) and Ultrasound Localization Microscopy (ULM), two powerful modalities that, when combined, provide a comprehensive platform for the longitudinal assessment of inflammatory diseases. Individually, each technique offers unique insights: BLI enables sensitive, cell-type-specific tracking of inflammatory processes, while ULM delivers super-resolution maps of the underlying microvascular structure and hemodynamics. Their integration is particularly powerful within the context of a broader thesis on longitudinal in vivo imaging, as it allows researchers to directly correlate the cellular events of inflammation, visualized by BLI, with consequent functional and morphological changes in the microcirculation, quantified by ULM. This multimodal approach provides a non-invasive, quantitative method for monitoring disease progression and treatment efficacy in live animal models, thereby enhancing the depth and reliability of preclinical research [106] [13] [20].
The core of this synergy lies in addressing a key limitation of standalone imaging. BLI provides excellent functional data on immune cell location and activity but offers limited anatomical context, especially for deep-tissue microvascular changes. Conversely, ULM excels at visualizing microvasculature but does not directly report on specific inflammatory cell populations. By combining them, a researcher can, for instance, observe a rising BLI signal from infiltrating neutrophils in an organ and simultaneously use ULM to detect the resulting reduction in capillary density or altered blood flow velocity, creating a complete pathophysiological picture [106] [20].
Workflow and Signaling Integration
The following diagram illustrates the integrated experimental workflow, from animal preparation to final correlated multimodal analysis.
Figure 1. Integrated workflow for combined BLI and ULM imaging. The process begins with the preparation of an animal disease model, which leverages cell-type-specific reporter lines for BLI. The two imaging modalities can be conducted in the same imaging session or longitudinally. Data streams are finally coregistered to produce a correlated quantitative output.
Experimental Protocols
Protocol A: Cell-Type-Specific Bioluminescence Imaging
This protocol is designed for the longitudinal monitoring of specific immune cell populations (e.g., myeloid cells, T cells) in murine models of inflammation, such as uveitis [13] [20].
Table 1: Key Steps for Bioluminescence Imaging Protocol
| Step | Parameter | Specification | Purpose & Notes |
|---|---|---|---|
| 1. Animal Prep | Reporter Lines | S100A8-Cre (neutrophils), LyzM-Cre (myeloid), Lck-Cre (T cells), Cd19-Cre (B cells) [20] | Enables cell-type-specific luciferase expression via Cre-lox system. |
| Disease Induction | Model-dependent (e.g., intravitreal antigen for uveitis [13]) | Induces controlled inflammation in target tissue. | |
| 2. Substrate Admin. | Reagent | D-luciferin (firefly) or Luminol (for myeloperoxidase) [13] [51] | Luminol is specific for myeloid cells; D-luciferin for general reporter genes. |
| Dosage & Route | 150-200 mg/kg, Intraperitoneal (IP) injection [13] [20] | Standard dosage for systemic distribution. | |
| 3. Image Acquisition | Instrument | IVIS Spectrum or equivalent CCD camera system [13] [25] | |
| Timing | 10-15 minutes post-injection for peak signal [13] | Requires empirical determination for optimal S/N. | |
| Exposure | 1-5 minutes, medium binning [13] | Prevents signal saturation. | |
| 4. Data Analysis | ROI Definition | Manually draw over target tissue (e.g., eye) and background [20] | |
| Quantification | Total flux (photons/sec) from background-subtracted ROI [13] [20] | Primary quantitative metric for longitudinal tracking. |
Protocol B: Ultrasound Localization Microscopy
This protocol details the acquisition of super-resolution microvascular images using ULM, which can be applied to abdominal organs, brain, and tumors to visualize vascular changes concomitant with inflammation [106] [107].
Table 2: Key Steps for Ultrasound Localization Microscopy Protocol
| Step | Parameter | Specification | Purpose & Notes |
|---|---|---|---|
| 1. Contrast Agent | Type | Gas-filled Microbubbles (MB) [106] | Acts as tracer; highly compressible for nonlinear scattering. |
| Administration | Intravenous (IV), cluster injection or slow drip infusion [106] | Lower concentrations reduce overlap, improving localization [106]. | |
| 2. Data Acquisition | Imaging Mode | Plane-wave ultrasound transmission [106] | Enables very high frame rates. |
| Frame Rate | Ultra-fast (hundreds to thousands of fps) [106] | Essential for tracking individual MB trajectories. | |
| 3. Image Processing | Motion Correction | Phase correlation or Kalman filtering [106] | Compensates for breathing/heartbeat. |
| MB Detection | Spatiotemporal filtering (SVD) or deep learning [106] | Separates MB signals from tissue background. | |
| Localization | Gaussian fitting or centroid methods [106] | Determines MB position with sub-wavelength precision. | |
| Tracking | Hungarian algorithm or Kalman filter [106] | Links positions across frames to form trajectories. | |
| 4. Visualization | Parameters | Vessel density, flow velocity, direction, complexity [106] | Quantitative metrics of vascular structure and function. |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents and Materials for Integrated BLI-ULM Studies
| Item | Function | Specification & Notes |
|---|---|---|
| Cell-Specific Reporter Mice | Enables targeting of luciferase expression to specific immune cell lineages for BLI. | Examples: LyzM-Cre (myeloid), Lck-Cre (T cells) crossed with ROSA26-Luciferase line [20]. |
| Luciferin | Substrate for firefly luciferase; produces photons upon reaction. | D-luciferin, typically administered at 150 mg/kg via IP injection [20] [51]. |
| Luminol | Chemiluminescent substrate for myeloperoxidase activity in innate immune cells. | Sodium salt, 200 mg/kg IP; specific for neutrophils and other myeloid cells [13]. |
| Microbubbles (MB) | Ultrasound contrast agent; serves as tracer for blood flow in ULM. | Inert gas core (e.g., perfluorocarbon) with lipid/protein shell; safe for renal excretion [106]. |
| Ultra-High Frequency US System | Hardware for ULM data acquisition. | Capable of plane-wave imaging and frame rates >500 Hz for MB tracking [106]. |
| In Vivo Imaging System (IVIS) | Hardware for BLI data acquisition. | CCD camera cooled to -90°C for low-light detection; includes gas anesthesia system [13] [25]. |
| Motion Stabilization Platform | Minimizes movement artifacts during ULM. | Critical for achieving precise MB localization over long acquisition times [106]. |
Quantitative Data Outputs and Correlation
The power of this multimodal approach lies in the quantitative correlation of parameters derived from both techniques. The tables below summarize key quantifiable outputs.
Table 4: Quantitative BLI Parameters for Inflammation Monitoring
| Parameter | Definition | Application in Inflammation Research |
|---|---|---|
| Total Flux | Total photon emission rate from a defined ROI (photons/second) [13]. | Primary measure of inflammatory cell burden; tracks disease progression/response [20]. |
| Signal-to-Noise Ratio (SNR) | Ratio of BLI signal intensity to background fluctuation. | Determines detectability threshold for low-grade inflammation. |
| Temporal Profile | Change in total flux over time (longitudinal tracking). | Identifies acute vs. chronic phases of inflammation and relapse events [13] [20]. |
Table 5: Quantitative ULM Parameters for Microvascular Assessment
| Parameter | Definition | Application in Inflammation Research |
|---|---|---|
| Vessel Density | Total length or area of perfused microvessels per unit volume [106]. | Reductions can indicate vascular rarefaction; increases can indicate angiogenesis. |
| Blood Flow Velocity | Speed of MBs within vessels, from <1 mm/s to several cm/s [106]. | Inflammation can cause flow abnormalities (e.g., slowing, shunting). |
| Vessel Complexity | Metric of vascular network branching and tortuosity. | Altered in pathologies like cancer and chronic inflammation [106] [107]. |
| Perfusion Index | Measure of tissue blood volume flow over time. | Critical functional readout of tissue health and inflammatory status. |
The following diagram conceptualizes how signals from innate and adaptive immune cells, detected by BLI, drive physiological changes in the microvasculature that are quantified by ULM.
Figure 2. Logical relationship between inflammatory cell activity and microvascular changes. The innate immune response, detectable via luminol-based BLI, drives acute microvascular dysfunction quantified by ULM as reduced flow velocity. The subsequent adaptive immune response, tracked by firefly luciferase-based BLI in T-cell/B-cell reporters, drives chronic vascular remodeling measured by ULM as changes in vessel density and network complexity. LPS, lipopolysaccharide.
Cross-species validation represents a critical pathway in translational research, ensuring that biological discoveries made in rodent models maintain their relevance when applied to more complex physiological systems. Within inflammation research, longitudinal in vivo bioluminescence imaging (BLI) has emerged as a powerful technology for noninvasive monitoring of cellular processes in living animals, providing insights into disease progression and treatment efficacy across species. The integration of ex vivo model systems from large mammals bridges the translational gap, offering human-relevant tissue contexts while maintaining controlled experimental conditions. This application note details standardized methodologies and validation frameworks that leverage BLI technology to enhance the reliability of cross-species extrapolation in inflammatory disease research and drug development.
BLI enables real-time, noninvasive visualization of biological processes in living animal models through light emission from luciferase-expressing bioreporter cells. Unlike fluorescence imaging, BLI does not require excitation light, thereby eliminating autofluorescence and providing exceptionally high signal-to-noise ratios for sensitive detection of inflammatory processes [108]. The core principle involves the enzymatic reaction between luciferase enzymes and their substrates, generating light that can be detected externally using sensitive CCD cameras.
The most commonly utilized luciferase systems include:
- Firefly luciferase (FLuc): Catalyzes oxidation of D-luciferin with ATP cofactor, emitting yellow-green light (peak ~562 nm) with high quantum efficiency (~40%) [108]
- Renilla luciferase (RLuc): Utilizes coelenterazine substrate to produce blue-green light (peak ~480 nm), often employed in dual-reporter systems [108]
- Bacterial luciferase (Lux): Autonomous light production through luxCDABE operon without exogenous substrate requirement [108]
Advanced multi-color BLI systems now enable simultaneous tracking of multiple inflammatory pathways through dual-acceptor bioluminescence resonance energy transfer (BRET) approaches, with recent developments expanding the color palette to 20 distinct hues for multiplexed target observation [109].
Table 1: Comparison of Common Luciferase Systems for Inflammation Imaging
| Luciferase Type | Substrate | Emission Peak | Advantages | Limitations |
|---|---|---|---|---|
| Firefly Luciferase (FLuc) | D-luciferin + ATP | 562 nm | High signal intensity, optimized kits available | Requires substrate injection, ATP-dependent |
| Renilla Luciferase (RLuc) | Coelenterazine | 480 nm | Smaller size, no ATP requirement | Lower quantum yield, faster signal decay |
| NanoLuc | Furimazine | 460 nm | Bright signal, small size | Blue-shifted light with poorer tissue penetration |
| Bacterial Lux | Endogenous | 490 nm | No substrate needed, autonomous | Bacterial applications primarily |
Quantitative Validation Data Across Model Systems
Cross-species validation requires systematic correlation of imaging data with established endpoint measurements. The following data tables summarize key validation metrics across rodent and ex vivo systems.
Table 2: Correlation of BLI Signal Intensity with Orthotopic Tumor Volume Across Imaging Modalities [110]
| Model System | Imaging Modality | Correlation with BLI (R²) | Detection Sensitivity | Spatial Resolution |
|---|---|---|---|---|
| Orthotopic Pancreatic Murine | BLI vs. MRI | 0.21 | High (early detection) | Low |
| Orthotopic Pancreatic Murine | Robotic US vs. MRI | 0.94 | Moderate | High (100μm) |
| Orthotopic Pancreatic Murine | Combined BLI-US vs. MRI | 0.97 | Very High | High |
Table 3: Cross-Species NPC1 Receptor Utilization Efficiency for Viral Entry [111]
| Species | NPC1 Receptor Efficiency (%) | Relative to Human | Application Relevance |
|---|---|---|---|
| Human | 100 ± 8.2 | 1.00 | Gold standard |
| Bat | 98.5 ± 7.6 | 0.99 | Reservoir species studies |
| Mouse | 95.3 ± 9.1 | 0.95 | Transgenic model development |
| Pig | 102.4 ± 6.8 | 1.02 | Large mammal ex vivo systems |
| Ferret | 94.2 ± 8.7 | 0.94 | Respiratory inflammation models |
| Non-human Primate | 101.2 ± 5.9 | 1.01 | Preclinical validation |
Experimental Protocols
Protocol: Longitudinal BLI in Rodent Inflammation Models
Purpose: To establish standardized methodology for noninvasive monitoring of inflammatory processes in rodent models using BLI.
Materials:
- Luciferase-expressing inflammatory cells or pathogen strains
- Isoflurane anesthesia system
- D-luciferin potassium salt (15 mg/mL in PBS)
- Pre-cooled CCD camera system (IVIS Spectrum or equivalent)
- Heated imaging stage maintained at 37°C
- Hair removal cream (for furred animals)
Procedure:
- Animal Preparation: Anesthetize mice using 1.5-3% isoflurane. For furred animals, remove hair from imaging area using electric clippers followed by depilatory cream to minimize signal attenuation [112].
- Substrate Administration: Administer D-luciferin intraperitoneally at 150mg/kg body weight. Uniform injection volume and site are critical for reproducibility.
- Image Acquisition: Place animals in light-tight imaging chamber. Acquire data at 15, 20, and 25 minutes post-injection to capture peak signal. Use auto-exposure settings initially, then standardize to 1-60 second exposures based on signal intensity [112].
- Data Analysis: Define regions of interest (ROIs) using standardized templates. Quantify signal as total flux (photons/sec) rather than radiance to account for three-dimensional distribution.
- Longitudinal Consistency: Image at consistent timepoints, maintaining identical animal positioning, anesthesia depth, and camera settings throughout study.
Validation Notes: Signal intensity correlates with cell viability and inflammatory activity. For orthotopic models, combine with ultrasound for anatomical correlation [110].
Protocol: Ex Vivo Precision-Cut Intestinal Slice (PCIS) Modeling
Purpose: To validate inflammatory mechanisms identified in rodent models using human-relevant ex vivo tissue systems.
Materials:
- Fresh intestinal tissue from surgical resections (IBD patients or controls)
- Kreb's-Henseleit buffer with 25mM glucose
- Tissue slicer (Krumdieck or Compressord)
- DMEM/F12 culture medium with antibiotics
- 95% Oâ‚‚/5% COâ‚‚ gas mixture
- LPS (1μg/mL) or ConA (10μg/mL) for stimulation
Procedure:
- Tissue Preparation: Immediately place surgical specimens in oxygenated ice-cold buffer. Remove mucosal layers if required.
- Slice Preparation: Embed tissue in 3% low-melting-point agarose. Generate 300μm slices using precision tissue slicer.
- Culture Conditions: Maintain slices in 12-well plates on orbital shakers (90 rpm) at 37°C with 95% O₂/5% CO₂.
- Stimulation: Apply inflammatory stimuli (LPS/ConA) for 24-48 hours. Include calcineurin inhibitors (e.g., pimecrolimus) for pharmacological validation.
- Endpoint Analysis: Collect conditioned media for cytokine analysis (IL-17, IL-21, IFN-γ). Assess tissue viability via ATP content and LDH release [113].
Validation Notes: PCIS maintains native tissue architecture and cellular heterogeneity for 72-96 hours. This system successfully modeled disease-specific immune activity and drug responses ex vivo [113].
Protocol: Cross-Species Receptor Tropism Validation
Purpose: To validate conserved receptor usage across species boundaries using pseudovirus systems.
Materials:
- HIV-based pseudovirus expressing target glycoprotein
- HEK293T cells
- NPC1-knockout HEK293T cells
- Plasmids encoding NPC1 receptors from multiple species
- Luciferase reporter system
Procedure:
- Pseudovirus Production: Co-transfect HEK293T cells with HIV backbone and DEHV glycoprotein plasmids using PEI transfection reagent.
- Receptor Expression: Transfect NPC1-knockout cells with plasmids encoding NPC1 from human, bat, mouse, or pig.
- Infection Assay: Incubate pseudovirus with receptor-expressing cells for 48 hours.
- Quantification: Measure luciferase activity as indicator of successful entry.
- Neutralization: Incubate with species-specific antisera to validate receptor specificity [111].
Validation Notes: This approach confirmed NPC1 as the conserved entry receptor for Dehong virus across seven mammalian species, demonstrating its potential for cross-species transmission [111].
Visualizing Signaling Pathways and Experimental Workflows
Diagram 1: Cross-species validation workflow integrating rodent and ex vivo systems.
Diagram 2: Conserved NPC1 receptor pathway for viral entry across species.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Reagents for Cross-Species Validation Studies
| Reagent/Category | Specific Examples | Function/Application | Cross-Species Considerations |
|---|---|---|---|
| Luciferase Reporters | Firefly Luc (FLuc), NanoLuc | Bioluminescence source for imaging | Species-specific codon optimization may be required |
| Luciferin Substrates | D-luciferin, Coelenterazine | Enzyme substrates for light generation | Pharmacokinetics may vary between species |
| Cell Culture Media | DMEM/F12, RPMI-1640 | Ex vivo tissue maintenance | May require species-specific supplementation |
| Cytokine Kits | IL-17, IL-21, IFN-γ assays | Inflammation biomarker quantification | Verify antibody cross-reactivity across species |
| Pseudovirus Systems | HIV-based, VSV-G pseudotyped | Safe study of pathogenic viruses | Glycoprotein compatibility with target cells |
| Primary Cells | Human/murine macrophages, epithelial cells | Species-specific cellular responses | Donor variability requires multiple replicates |
The integration of longitudinal BLI in rodent models with large mammal ex vivo systems creates a powerful validation pipeline for inflammation research. This approach addresses a critical limitation in translational science by enabling direct mechanistic comparison across species boundaries while maintaining physiological relevance. The standardized protocols presented here facilitate systematic assessment of inflammatory pathways, cellular trafficking, and therapeutic interventions.
Key advantages of this integrated approach include:
- Enhanced Predictive Value: Ex vivo human tissue models bridge the species gap, providing human-relevant data before advancing to clinical trials [113] [114].
- Reduced Experimental Variability: Controlled ex vivo systems minimize confounding factors present in in vivo environments [115].
- Mechanistic Insight: Combined imaging and molecular analysis uncovers conserved biological pathways across species [111].
- Ethical Optimization: Ex vivo models reduce animal usage while providing human-translatable data [115].
As BLI technology advances with multi-color capabilities and improved detection sensitivity [109], and ex vivo systems incorporate more complex tissue interactions, this validation framework will become increasingly vital for successful translation of inflammatory disease therapeutics from bench to bedside.
Longitudinal in vivo bioluminescence imaging (BLI) has become an indispensable tool for monitoring inflammatory processes in live animal models, enabling non-invasive assessment of disease progression, immune cell trafficking, and therapeutic efficacy in real-time [20] [116] [19]. However, the quantitative reproducibility of BLI data across different laboratories and experimental setups remains a significant challenge, potentially limiting the translational impact of preclinical findings. Technical variations in instrumentation, substrate administration, animal positioning, and data analysis methodologies can introduce substantial inter-laboratory variability, confounding direct comparisons between studies [1] [25]. This application note establishes a comprehensive framework for standardizing BLI protocols and implementing rigorous quality control measures specifically for inflammation research, with the goal of enhancing data reliability and reproducibility across different research settings.
The fundamental principle of BLI relies on the detection of photons emitted from luciferase enzymes in the presence of specific substrates (e.g., D-luciferin or coelenterazine) and co-factors [1]. In inflammation research, this technology has been successfully applied to monitor neuroinflammation in experimental autoimmune encephalomyelitis (EAE) [91], quantify intraocular inflammation in uveitis models [20] [116], and track immune cell populations in various disease contexts [20] [19]. Despite its widespread adoption, the field lacks unified standards for acquisition parameters, calibration procedures, and validation metrics, creating an urgent need for the systematic approach outlined in this document.
Quantitative Evidence: Assessing Current Reproducibility Challenges
Correlation Between BLI and Established Inflammation Metrics
Table 1: Correlation Analysis of BLI with Pathological and Clinical Inflammation Metrics in EAE
| Measurement Metric | Correlation with Brain BLI (Pearson r) | Correlation with Spinal Cord BLI (Pearson r) | Statistical Significance (p-value) |
|---|---|---|---|
| Clinical Score | 0.87 | 0.85 | < 0.001 |
| Weight Loss | 0.84 | 0.81 | < 0.001 |
| Astrogliosis (GFAP) | 0.92 | 0.90 | < 0.001 |
| Microgliosis (CD68) | 0.89 | 0.86 | < 0.001 |
| CD4+ T Cell Infiltration | 0.79 | 0.75 | < 0.01 |
Data adapted from Nissen et al., Journal of Neuroinflammation (2008) demonstrates strong correlations between GFAP-luciferase bioluminescence and established pathological markers of neuroinflammation in experimental autoimmune encephalomyelitis [91]. The high correlation coefficients validate BLI as a quantitative method for monitoring inflammatory processes, while simultaneously highlighting the robust relationships that can be achieved with standardized imaging approaches.
Temporal Dynamics of Immune Cell Infiltration in Uveitis
Table 2: Longitudinal Immune Cell Population Dynamics in Experimental Uveitis
| Time Point | Neutrophils (% of CD45+ cells) | T Cells (% of CD45+ cells) | B Cells (% of CD45+ cells) | Corresponding BLI Signal |
|---|---|---|---|---|
| Day 2 | 78% | 12% | 0.2% | Myeloid reporter peak |
| Day 7 | 25% | 47% | 1% | T cell reporter peak |
| Day 21 | 12% | 52% | 3% | T cell dominance |
| Day 35 | 5% | 50% | 4% | B cell reporter increase |
Data from Scientific Reports (2020) shows the dynamic changes in intraocular immune cell populations during experimental uveitis and their correlation with cell-type-specific bioluminescence signals [20]. This longitudinal quantification demonstrates how BLI can accurately reflect underlying cellular changes during inflammatory responses, providing a non-invasive method for monitoring disease progression and immune mechanisms.
Standardized Experimental Protocols
Protocol for Cell-Type-Specific Inflammation Monitoring
This protocol adapts methodology from Cao et al. (2020) for longitudinal monitoring of specific immune cell populations in inflammatory models using Cre-lox reporter systems [20].
Materials Required:
- Cell-type-specific Cre driver mice (e.g., LyzM-cre for myeloid cells, Lck-cre for T cells, CD19-cre for B cells)
- ROSA26-loxP-stop-loxP-luciferase (ROSA-LUC) reporter mice
- Appropriate animal model of inflammation (e.g., primed mycobacterial uveitis, EAE)
- D-luciferin substrate (15 mg/mL in PBS)
- In vivo imaging system (IVIS) with cooled CCD camera
- Isoflurane anesthesia system
- Living Image software or equivalent for data analysis
Procedure:
- Animal Model Generation: Cross Cre driver mice with ROSA-LUC reporter mice to generate cell-type-specific luciferase expression.
- Model Induction: Induce inflammatory disease in experimental animals while maintaining appropriate controls.
- Substrate Administration: Inject D-luciferin intraperitoneally at 150 mg/kg body weight 10-15 minutes before imaging [20] [91].
- Anesthesia: Maintain animals under isoflurane anesthesia (2-3% in oxygen) during imaging procedure.
- Image Acquisition:
- Place animals in the imaging chamber in a consistent, predetermined position
- Set acquisition parameters: medium binning, f/stop 1, 3-5 minute exposure time
- Acquire images daily during acute phase, then weekly during chronic phase
- Data Analysis:
- Define consistent regions of interest (ROIs) for experimental and control tissues
- Measure bioluminescence as total flux (photons/second)
- Normalize signals to baseline pre-inflammation values
- Compare with terminal validation assays (flow cytometry, histology)
Validation: Verify cell-type-specific luciferase expression by flow cytometry or magnetic sorting of splenocytes followed by in vitro bioluminescence measurement [20].
Protocol for Instrument Standardization and Cross-Lab Calibration
Standardized instrument calibration is essential for comparing BLI data across different laboratories and imaging systems [25].
Materials Required:
- Light-tight imaging chamber
- Certified luminance standards or stable light-emitting sources
- Uniform phantom simulating tissue optical properties
- Body-conforming animal molds (BCAM) for consistent positioning [25]
Procedure:
- System Linear Range Determination:
- Image a series of light standards with known emission intensities
- Determine the range over which measured signal increases linearly with exposure time
- Establish maximum non-saturating exposure times for common applications
Sensitivity Threshold Assessment:
- Image dilution series of luciferase-expressing cells in tissue phantoms
- Determine minimum detectable cell number for each system
- Document limit of detection for common experimental models
Spatial Uniformity Calibration:
- Image a uniformly illuminated phantom across the entire field of view
- Quantify positional variations in signal intensity
- Generate correction matrices for spatial inhomogeneity
Inter-instrument Alignment:
- Image identical biological samples on multiple instruments
- Compare absolute measurements and establish correlation factors
- Document inter-system variability for cross-study comparisons
Quality Control Metrics:
- Perform calibration monthly or following any system maintenance
- Maintain log of all calibration results and corrective actions
- Establish tolerance limits for key performance parameters
Quality Control Framework and Standardization Measures
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Reproducible BLI
| Reagent/Material | Function | Standardization Consideration | Example Application |
|---|---|---|---|
| Cell-type-specific Cre mice | Targets luciferase expression to specific immune lineages | Validate recombination efficiency; backcross to common genetic background | Myeloid vs. lymphocyte imaging in inflammation [20] |
| ROSA26-LUC reporter mice | Provides ubiquitously accessible luciferase cassette | Confirm single integration site; maintain as separate strain until crossing | Conditional luciferase expression in multiple cell types [20] |
| D-luciferin | Substrate for firefly luciferase | Use consistent lot; standardize concentration (150 mg/kg) and injection route (IP) | Longitudinal monitoring of inflammatory processes [116] [91] |
| Body-conforming animal molds (BCAM) | Standardizes animal positioning and geometry | Use weight-adjusted molds (17-38g range); ensure optical transparency | Automated image analysis; cross-study comparability [25] |
| Akaluc luciferase | Engineered luciferase with enhanced brightness | Use matched substrate (Akalumine); optimal for stem cell tracking | Hematopoietic reconstitution imaging [117] |
Implementing Internal Quality Control Practices
Adapting clinical laboratory quality control frameworks to BLI provides a systematic approach to monitoring analytical performance [118].
Defining Acceptability Criteria:
- Establish baseline bioluminescence values for control animals
- Set acceptable coefficients of variation for replicate measurements
- Define thresholds for investigating unexpected signal variations
Statistical Control Rules:
- Implement Westgard rules or similar statistical monitoring
- Track control measurements over time to detect trends or shifts
- Establish action limits for corrective measures
Frequency of Quality Control Assessment:
- Perform daily system checks with reference standards
- Include biological controls with each experimental series
- Conduct comprehensive quarterly performance reviews
Post-QC Impact Assessment:
- Document all deviations from expected QC results
- Assess impact on experimental data validity
- Implement corrective actions and verify effectiveness
Visualization Framework for Standardized Workflows
Experimental Workflow for Reproducible Inflammation Monitoring
Figure 1: Comprehensive Workflow for Standardized BLI in Inflammation Research. This diagram outlines the key steps in implementing reproducible bioluminescence imaging, highlighting critical standardization points (yellow) and essential research reagents (red) that must be controlled to ensure inter-laboratory reproducibility.
Quality Control Implementation Pathway
Figure 2: Systematic Quality Control Implementation Pathway. This visualization outlines the sequential steps for establishing robust quality control practices in BLI, with specific technical components (red) that must be implemented at each stage to ensure ongoing monitoring and maintenance of data quality.
The standardization framework and quality control measures outlined in this document provide a comprehensive approach to enhancing reproducibility in longitudinal BLI of inflammation. By implementing standardized protocols, controlling critical experimental variables, and establishing systematic quality monitoring, researchers can significantly improve the reliability and cross-study comparability of BLI data. The integration of automated analysis tools like InVivoPLOT [25] and the adoption of standardized reference materials will further advance the field toward truly quantitative in vivo imaging. As BLI continues to evolve as a critical tool in preclinical drug development and basic inflammation research, these harmonization efforts will be essential for generating robust, translatable findings that can accelerate therapeutic innovation.
Longitudinal in vivo bioluminescence imaging (BLI) has become a cornerstone technique in preclinical research, enabling the real-time, non-invasive monitoring of biological processes such as inflammation in live animal models. Its high sensitivity, low background noise, and quantitative nature make it an powerful tool for understanding disease mechanisms and evaluating therapeutic efficacy [119]. However, the traditional reliance on transgenic luciferase-expressing organisms has historically been a significant barrier to its clinical translation. This application note details recent technological breakthroughs that are overcoming these limitations, thereby bridging the gap between preclinical findings and human applications. We frame these advances within the context of inflammation research, providing detailed protocols and a scientific toolkit to facilitate the adoption of these next-generation BLI methodologies.
Technological Advances Enhancing Clinical Translation
Several key innovations are expanding the potential of BLI from a purely preclinical tool to one with a clearer pathway toward human application.
Portable Bioluminescent (PBL) Platform for Non-Transgenic Subjects
The Portable Bioluminescent (PBL) platform represents a paradigm shift by enabling functional BLI in non-transgenic animals, including large species [120]. This system circumvents the need for genetic modification by employing an injectable, biocompatible "plug" or cell-encapsulating device that contains the luciferase enzyme. When used in conjunction with caged luciferin probes that are activated by specific biological processes (e.g., enzyme activity), the system generates a bioluminescent signal proportional to the process's activity level.
- Clinical Relevance: This technology has been successfully demonstrated in mice, dogs, and even human cadavers, paving the way for its use in non-invasive clinical diagnostics and monitoring of drug effects in larger animal models during drug development [120].
- Instrumentation: The platform utilizes a compact, portable light detector resembling a stethoscope, which is directly affixed over the luciferase plug. This design eliminates the need for expensive, stationary "black box" imaging systems and prolonged anesthesia, making it suitable for clinical settings [120].
Automated and Quantitative Analysis Tools
Traditional BLI analysis is often semiquantitative and operator-dependent. The development of InVivoPLOT, an automated data analysis tool, addresses this by providing operator-independent, quantitative determination of bioluminescent reporter distributions [25]. Its core innovation is a Body-Conforming Animal Mold (BCAM) that standardizes animal posture and size, enabling data congruency across different subjects and time points. This system, combined with a statistical mouse atlas, allows for automated biodistribution analysis and precise calculation of metrics like bacterial organ burden, moving BLI from qualitative visualization to rigorous quantification [25].
Expansion of the Bioluminescent Color Palette
The development of a color-tunable bioluminescence imaging portfolio has expanded the spectrum of bioluminescent light from blue to far-red [121]. By synthesizing novel coelenterazine (CTZ) analogues and pairing them with specific marine luciferases (e.g., RLuc8, ALuc16), researchers can now generate a full palette of colors. The ability to produce red-shifted bioluminescence (exceeding 600 nm) is particularly critical for clinical translation, as longer wavelengths experience less scattering and absorption by hemoglobin, allowing for superior tissue penetration and signal detection from deeper structures within the body [121].
Standardization of Absolute Optical Signals
A significant challenge in translating any optical imaging technique is the lack of standardized, absolute quantification. Recent research has focused on moving beyond relative light units (RLU) to measuring absolute optical values, such as total photon flux (photons sâ»Â¹) [51]. This is achieved by calibrating imaging devices with traceable reference light sources. Such standardization is essential for reproducing results across different laboratories and instruments, a prerequisite for any clinically adopted methodology [51].
Table 1: Key Technological Advances and Their Impact on Clinical Translation
| Technology | Key Innovation | Addressed Limitation | Potential Clinical Application |
|---|---|---|---|
| Portable BL Platform [120] | Injectable luciferase "plug"; portable detector | Requires transgenic models; non-portable instrumentation | Functional monitoring in non-transgenic large animals and humans |
| Automated Analysis (InVivoPLOT) [25] | Body-Conforming Animal Mold (BCAM); statistical atlas | Operator-dependent, semi-quantitative analysis | Standardized, quantitative biodistribution studies |
| Color-Tunable Portfolio [121] | Novel CTZ analogues for red-shifted spectra | Poor tissue penetration of blue/green light | Deep-tissue imaging and multiplexed sensing |
| Absolute Quantification [51] | Calibrated reference light sources | Relative signal reporting (RLU) | Reproducible, standardized measurements across sites |
Application Note: Longitudinal Imaging of Inflammation
Inflammation is a core component of numerous diseases, and its longitudinal monitoring is vital for understanding pathology and treatment response.
Detailed Protocol: Myeloperoxidase Imaging at Injury Site
The following protocol is adapted for monitoring inflammation in a mouse ankle injury model using a chemiluminescent probe for myeloperoxidase (MPO), a key inflammatory enzyme [122].
I. Materials and Reagents
- Animal Model: Mice with induced ankle injury.
- Probe: RediJect Inflammation Probe (e.g., from PerkinElmer).
- Imaging System: IVIS Spectrum Imaging System (PerkinElmer) or equivalent.
- Software: Living Image Software or similar.
- Anesthesia System: Isoflurane vaporizer and induction chamber.
II. Experimental Workflow
- Animal Preparation: Anesthetize the mouse using an isoflurane/oxygen mixture (typically 2-3% for induction, 1-2% for maintenance).
- Probe Administration: Administer the RediJect Inflammation Probe via intraperitoneal (i.p.) injection at a dose of 150 μl per mouse (or 200 mg/kg) [122].
- Image Acquisition:
- Place the anesthetized animal in the imaging chamber.
- Acquire bioluminescence images for 5 minutes using the following parameters: F/stop = 1, Binning Factor = 8 [122].
- Maintain a consistent delay between probe injection and image acquisition across all subjects.
- Data Analysis:
- Display planar bioluminescent images in units of photon/sec/cm²/sr.
- Define a standardized region of interest (ROI) over the injury site using Living Image software.
- Quantify the peak total bioluminescent signal within the ROI. Report data as total flux in photons per second per ROI [122].
The logical workflow and signaling pathway for this application are summarized in the diagram below.
Protocol Integration with Advanced Platforms
The inflammation monitoring protocol can be significantly enhanced by integrating it with the technologies described in Section 2.
- For Non-Transgenic Models: The PBL platform can be adapted. Instead of a transgenic animal, a mouse implanted with a luciferase plug would be used. A caged luciferin probe designed to be activated by MPO would be injected. The released luciferin would then generate light at the plug site, detectable by the portable detector [120].
- For Automated Quantification: Mice can be imaged within the BCAM shuttle of the InVivoPLOT system to ensure perfect registration and automated ROI analysis across longitudinal time points, removing operator bias and improving reproducibility [25].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Research Reagent Solutions for Translational BLI
| Item | Function/Description | Example Application |
|---|---|---|
| RediJect Inflammation Probe | Chemiluminescent probe for myeloperoxidase (MPO) activity | Specific detection of neutrophil-mediated inflammation at injury sites [122]. |
| Caged Luciferin Probes | Functionally activated luciferin substrates (e.g., for DPP-4, CYP450) | Sensing specific enzymatic activities in vivo with the PBL platform [120]. |
| Body-Conforming Animal Mold (BCAM) | Standardized animal shuttle for posture and size normalization | Enables automated, quantitative analysis and data congruency in longitudinal studies [25]. |
| Color-Tunable CTZ Analogues | Novel coelenterazines (e.g., 1d, 2d) that emit red-shifted light | Improved tissue penetration for deep-tissue imaging and multiplexed assays [121]. |
| Portable PBL Detector | Handheld, high-sensitivity photodiode-based light detector | Enables bioluminescence monitoring in large, non-transgenic animals and clinical settings [120]. |
| Absolute Light Standard | Calibrated reference light source (traceable to national standards) | Standardizes BLI measurements across instruments and laboratories, enabling absolute quantification [51]. |
The landscape of in vivo bioluminescence imaging is evolving rapidly from a tool confined to transgenic rodent models to one with a tangible pathway to human application. Technologies such as the portable bioluminescent platform, automated quantitative analysis, red-shifted probes, and standardized absolute quantification are collectively overcoming the major hurdles of model dependency, poor tissue penetration, and analytical variability. For researchers and drug development professionals focused on inflammation, integrating these advanced protocols and tools into their workflow will not only enhance the quality and reproducibility of preclinical data but also accelerate the translation of therapeutic findings from bench to bedside. Future efforts will likely focus on refining the biocompatibility and longevity of implantable reporter systems and expanding the library of caged probes to target a wider array of human disease biomarkers.
Conclusion
Longitudinal in vivo bioluminescence imaging represents a transformative approach for inflammation research, enabling non-invasive, real-time monitoring of disease progression and therapeutic response within the same subjects. The technology's ability to distinguish between acute and chronic inflammatory phases, track specific immune cell populations, and reduce animal usage through within-subject designs positions it as an essential tool in preclinical drug development. Future directions should focus on developing more sensitive luciferase-luciferin systems with improved tissue penetration, creating standardized protocols for cross-study comparisons, and advancing multimodal imaging platforms that combine BLI with complementary techniques like ultrasound and MRI. As synthetic biology continues to produce enhanced reporter systems and computational methods improve signal quantification, BLI is poised to become increasingly central to personalized medicine approaches and the development of targeted anti-inflammatory therapies. The integration of engineered bacterial biosensors and ex vivo organ culture systems further expands BLI's potential, creating a robust framework for understanding inflammatory processes across multiple biological contexts.
References
- 1. BIOLUMINESCENCE IMAGING: PROGRESS AND ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4314955/]
- 2. Caspase 8-activated bioluminescence probe for in vivo ... [https://www.sciencedirect.com/science/article/abs/pii/S0956566325008802]
- 3. A Comprehensive Exploration of Bioluminescence Systems ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10861286/]
- 4. An Investigation of the Reaction Kinetics of Luciferase and ... [https://pubmed.ncbi.nlm.nih.gov/19093108/]
- 5. Molecular Design of d-Luciferin-Based Bioluminescence ... [https://www.mdpi.com/1420-3049/26/6/1618]
- 6. Model | Cambridge - iGEM 2025 [https://2025.igem.wiki/cambridge/model]
- 7. A practical, biomimetic, one-pot synthesis of firefly luciferin [https://www.nature.com/articles/s41598-024-82996-2]
- 8. The NF-κB activation pathways, emerging molecular targets ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3043547/]
- 9. NF-κB in biology and targeted therapy: new insights and ... [https://www.nature.com/articles/s41392-024-01757-9]
- 10. Quantitative characterization of immune cells by measuring ... [https://www.nature.com/articles/s41598-024-75666-w]
- 11. Tracking Early Autoimmune Disease by Bioluminescent ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2671367/]
- 12. Noninvasive nuclear factor-κB bioluminescence imaging ... [https://www.sciencedirect.com/science/article/abs/pii/S0142961207005285]
- 13. In Vivo Bioluminescence Imaging for Longitudinal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5361579/]
- 14. Navigating In Vivo Bioluminescence Imaging [https://www.promega.com/resources/pubhub/2024/navigating-in-vivo-bioluminescence-imaging/]
- 15. An R package for fast and flexible analysis of immune cell ... [https://www.sciencedirect.com/science/article/pii/S2667119021000033]
- 16. New imaging method helps immune cells zero in on cancer [https://bme.ufl.edu/2025/11/04/new-imaging-method-helps-immune-cells-zero-in-on-cancer/]
- 17. Four game-changing immunology tools to watch [https://www.nature.com/articles/d41586-025-03335-7]
- 18. In Vivo Bioluminescent Imaging (BLI) - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC3274065/]
- 19. Bioluminescence imaging of reporter mice for studies ... [https://www.sciencedirect.com/science/article/abs/pii/S0166354210000318]
- 20. Bioluminescence for in vivo detection of cell-type-specific ... [https://www.nature.com/articles/s41598-020-68227-4]
- 21. In Vivo Cell Tracking with Bioluminescence Imaging - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4354780/]
- 22. Bioluminescence-mediated longitudinal monitoring of ... [https://www.nature.com/articles/srep13960]
- 23. High throughput quantitative bioluminescence imaging for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3027220/]
- 24. Application and trend of bioluminescence imaging in ... [https://www.frontiersin.org/journals/chemistry/articles/10.3389/fchem.2022.1113546/full]
- 25. Automated quantification of bioluminescence images [https://www.nature.com/articles/s41467-018-06288-w]
- 26. Bioluminescent detection of endotoxin effects on HIV-1 LTR ... [https://pubmed.ncbi.nlm.nih.gov/12754285/]
- 27. In Vivo Imaging Core Facility Methods and Protocols [https://www.bumc.bu.edu/camed/research-impact/cores/ivis-imaging-core/ivis-methods-and-protocols/]
- 28. Improvement of the signal to noise ratio for fluorescent ... [https://www.nature.com/articles/s41598-022-23426-z]
- 29. Bioluminescence Imaging - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2713342/]
- 30. Enhancement of signal-to-noise ratio for fluorescence ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8074948/]
- 31. An Optimized Protocol for Brain Studies | PLOS One [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0055662]
- 32. Fluorescence lifetime imaging microscopy: fundamentals ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7219965/]
- 33. A Guide to Fluorescence Lifetime Imaging Microscopy (FLIM) [https://www.leica-microsystems.com/science-lab/life-science/a-guide-to-fluorescence-lifetime-imaging-microscopy-flim/]
- 34. Fluorescence lifetime and polarization-resolved imaging in ... [https://www.sciencedirect.com/science/article/abs/pii/S0958166909000044]
- 35. In vivo Imaging Method to Distinguish Acute and Chronic ... [https://www.jove.com/t/50690/in-vivo-imaging-method-to-distinguish-acute-and-chronic-inflammation]
- 36. In vivo imaging method to distinguish acute and chronic ... [https://pubmed.ncbi.nlm.nih.gov/23978851/]
- 37. Bioluminescence imaging of myeloperoxidase activity in vivo [https://pmc.ncbi.nlm.nih.gov/articles/PMC2831476/]
- 38. Novel NF-κB reporter mouse for the non-invasive ... - Nature [https://www.nature.com/articles/s41598-023-29689-4]
- 39. Sparstolonin B nano-formulation attenuates LPS-induced ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12011759/]
- 40. Double knockin mice show NF-κB trajectories in immune ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9764224/]
- 41. KappaBle fluorescent reporter mice enable low- ... [https://www.sciencedirect.com/science/article/pii/S1933021922000903]
- 42. Immune Response to Bioluminescence Imaging Reporters ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12162783/]
- 43. Adipose Tissue in Chagas Disease: A Neglected Component ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12030347/]
- 44. Comparing in vivo bioluminescence imaging and the Multi ... [https://dndi.org/scientific-articles/2022/comparing-invivo-bioluminescence-imaging-and-multi-cruzi-immunoassay-platform-improved-chagas-diagnostic-procedures-biomarkers/]
- 45. Demystifying In Vivo Bioluminescence Imaging of a ... [https://www.jove.com/t/66740/demystifying-vivo-bioluminescence-imaging-chagas-disease-mouse-model]
- 46. Bioluminescence as a functional tool for visualizing and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10861157/]
- 47. Development of bioluminescent reporter Trypanosoma ... [https://www.frontiersin.org/journals/chemical-biology/articles/10.3389/fchbi.2024.1423430/full]
- 48. In Vivo Bioluminescence Imaging of Granzyme B Activity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9588750/]
- 49. Current status and future prospects of molecular imaging in ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1518555/full]
- 50. Therapeutic targets and biomarkers of tumor immunotherapy [https://www.nature.com/articles/s41392-022-01136-2]
- 51. Quantitative Analysis of Bioluminescence Optical Signal [https://pmc.ncbi.nlm.nih.gov/articles/PMC9953788/]
- 52. NIR-II bioluminescence for in vivo high contrast imaging ... [https://www.nature.com/articles/s41467-020-18051-1]
- 53. Insight on stem cell preconditioning and instructive ... [https://www.sciencedirect.com/science/article/abs/pii/S0142961216300412]
- 54. Bioluminescence Imaging [https://www.promega.com/resources/technologies/nanoluc-luciferase-enzyme/bioluminescence-imaging/]
- 55. Stem Cell Therapy: MRI Guidance and Monitoring - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3075622/]
- 56. Achieving stable human stem cell engraftment and survival in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3403688/]
- 57. Clinical trials and advanced MRI techniques with stem cell ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-07054-5]
- 58. Orally Administered Bacterial Biosensors Detect ... [https://www.genengnews.com/topics/translational-medicine/orally-administered-bacterial-biosensors-detect-gastrointestinal-disease-in-mice]
- 59. Microbial Biosensor for Sensing and Treatment of Intestinal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12279244/]
- 60. Innovative applications and research advances of bacterial ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1507491/full]
- 61. Inflammation-on-a-chip: probing the immune system ex vivo [https://pmc.ncbi.nlm.nih.gov/articles/PMC6098972/]
- 62. Comparison of ex vivo bioluminescence imaging, Alu-qPCR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10972982/]
- 63. Development of a novel technology for long-term culture ... [https://www.nature.com/articles/s41598-025-94022-0]
- 64. Ex vivo culture conditions for bioluminescence imaging of ... [https://www.jbtr.or.kr/archive/view_article?pid=jbtr-25-1-1]
- 65. Culturing Potential: advances in ex vivo cell culture systems ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12284713/]
- 66. an optimized protocol for brain studies [https://pubmed.ncbi.nlm.nih.gov/23405190/]
- 67. Longitudinal imaging evaluation of the inflammatory role ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12417452/]
- 68. Luciferase Reporters | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/luciferase-reporters.html]
- 69. Luciferase Assay Selection Guide [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-assays-analysis/reporter-gene-assays/luciferase-assays/luciferase-product-selection-guide.html]
- 70. Quantitation in Bioluminescence Imaging by Correction of ... [https://pubmed.ncbi.nlm.nih.gov/20686859/]
- 71. Quantitative Analysis of Bioluminescence Optical Signal [https://www.mdpi.com/2079-6374/13/2/223]
- 72. Luciferase transduction and selection protocol for reliable ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11259842/]
- 73. Luciferase Assay System Protocol [https://www.promega.com/resources/protocols/technical-bulletins/0/luciferase-assay-system-protocol/]
- 74. Anesthetics in pathological cerebrovascular conditions - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11563546/]
- 75. The Influence of Anesthetics on the Functions ... [https://www.mdpi.com/2227-9059/13/10/2357]
- 76. Immune Modulation by Volatile Anesthetics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5074538/]
- 77. Suppressive effects of deep balanced anesthesia on cellular immunity ... [https://bmcanesthesiol.biomedcentral.com/articles/10.1186/s12871-025-02980-9]
- 78. The perioperative effect of anesthetic drugs on the immune ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9289698/]
- 79. Toward Normalization of the Tumor Microenvironment for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6614947/]
- 80. Metabolic Adaptations in Cancer Progression: Optimization ... [https://www.mdpi.com/2072-6694/17/14/2341]
- 81. Intraperitoneal versus intravenous administration of Flamma [https://pubs.rsc.org/en/content/articlehtml/2025/na/d4na00764f]
- 82. of Comparison administration of... intravenous versus intraperitoneal [https://pmc.ncbi.nlm.nih.gov/articles/PMC2657185/]
- 83. Impact of ionizable lipid type on the pharmacokinetics and ... [https://pubmed.ncbi.nlm.nih.gov/40505892/]
- 84. Toxicity and biodistribution comparison of functionalized ... [https://www.frontiersin.org/journals/nanotechnology/articles/10.3389/fnano.2025.1512622/full]
- 85. A Guide to Ex Vivo Biodistribution Studies with ... [https://link.springer.com/article/10.1007/s11307-025-02055-8]
- 86. Pharmacokinetic and biodistribution analysis of monoclonal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12622353/]
- 87. of therapeutic extracellular vesicles Biodistribution [https://www.oaepublish.com/articles/evcna.2023.12]
- 88. Deep Learning-Based Microbubble Localization for ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9116497/]
- 89. Context-aware deep learning enables high-efficacy ... [https://www.nature.com/articles/s41467-024-47154-2]
- 90. Methods for Rapid Characterization of Tunable ... [https://www.mdpi.com/2306-5354/11/12/1224]
- 91. Bioluminescence in vivo imaging of autoimmune ... [https://jneuroinflammation.biomedcentral.com/articles/10.1186/1742-2094-5-6]
- 92. In Vivo Imaging of Inflammatory Phagocytes [https://www.sciencedirect.com/science/article/pii/S1074552112002839]
- 93. A Comparison of the Sensitivity and Cellular Detection ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11598277/]
- 94. added value to bioluminescence imaging [https://www.nature.com/articles/labinvest2016114]
- 95. Bronchoalveolar lavage as a diagnostic procedure [https://pmc.ncbi.nlm.nih.gov/articles/PMC7578496/]
- 96. Identification of bronchoalveolar and blood immune ... [https://www.nature.com/articles/s41598-022-13179-0]
- 97. Evaluation of Bronchoalveolar Lavage Fluid Cytokines as ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2017.02362/full]
- 98. Bronchoalveolar lavage cytokine-based risk stratification of ... [https://www.sciencedirect.com/science/article/pii/S1053249824019673]
- 99. Cytokine profiling in serum-derived exosomes isolated by ... [https://www.nature.com/articles/s41598-020-70584-z]
- 100. Bioluminescence in vivo imaging of autoimmune ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2267451/]
- 101. A Deep Dive Into the Luciferase Assay: What It is ... [https://www.goldbio.com/blogs/articles/a-deep-dive-into-the-luciferase-assay-what-it-is-how-it-works-and-more?srsltid=AfmBOorhrwsNmxx3w1iNg77g038qsdejzleLGuN85hLExxYJwVbQyIGR]
- 102. Enhancing Bioluminescence Imaging of Cultured Tissue ... [https://www.mdpi.com/1424-8220/24/18/6041]
- 103. Robust Normalization of Luciferase Reporter Data - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6789503/]
- 104. Statistical analysis of Luciferase Assays [https://www.moritzs.de/biology/statistics/analysis-luciferase-assay/]
- 105. Bioluminescence imaging: In vivo monitoring of tumor ... [https://oncology.labcorp.com/bioluminescence-imaging-vivo-monitoring-tumor-development-disease-dissemination-and-treatment]
- 106. Progresses and clinical application of super-resolution ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12170475/]
- 107. Applications of Ultrasound Localization Microscopy in ... [https://www.sciopen.com/article/10.26599/AUDT.2025.250097]
- 108. In Vivo Bioluminescent Imaging (BLI) [https://www.mdpi.com/1424-8220/11/1/180]
- 109. Creating coveted bioluminescence colors for simultaneous ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11753369/]
- 110. Validation of a combined ultrasound and bioluminescence ... [https://www.nature.com/articles/s41598-021-03684-z]
- 111. Development of a neutralization assay and bioluminescent ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12054171/]
- 112. Guidance - Preclinical Imaging & Testing - MIT [https://preclinical-imaging.mit.edu/preclinical-imaging/guidance/]
- 113. Ex Vivo Modeling and Pharmacological Modulation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12288778/]
- 114. Translational Biomarkers and Ex Vivo Models of Joint ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6174937/]
- 115. Ex vivo models | Translational pharmacology [https://www.oncodesign-services.com/discovery-services/ex-vivo-assays/]
- 116. In Vivo Bioluminescence Imaging for Longitudinal Monitoring ... [https://pubmed.ncbi.nlm.nih.gov/28278321/]
- 117. Protocol for noninvasive imaging of hematopoietic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12491520/]
- 118. Ensuring internal quality control practices in medical ... [https://www.sciencedirect.com/science/article/abs/pii/S0009898125001196]
- 119. Bioluminescence from the bright and dark sides [https://www.frontiersin.org/journals/chemical-biology/articles/10.3389/fchbi.2024.1459397/full]
- 120. Portable bioluminescent platform for in vivo monitoring of ... [https://www.nature.com/articles/s41467-021-22892-9]
- 121. Color-tunable bioluminescence imaging portfolio for cell ... [https://www.nature.com/articles/s41598-021-81430-1]
- 122. In vivo bioluminescent imaging of inflammation [https://bio-protocol.org/exchange/minidetail?id=5855276&type=30]