Macrophage Polarization in Chronic Inflammation: Molecular Mechanisms, Therapeutic Targeting, and Clinical Implications
This article provides a comprehensive analysis of the mechanisms governing macrophage polarization and its pivotal role in chronic inflammatory diseases.
Macrophage Polarization in Chronic Inflammation: Molecular Mechanisms, Therapeutic Targeting, and Clinical Implications
Abstract
This article provides a comprehensive analysis of the mechanisms governing macrophage polarization and its pivotal role in chronic inflammatory diseases. Targeting researchers, scientists, and drug development professionals, it synthesizes foundational knowledge on the M1/M2 spectrum, key signaling pathways (JAK/STAT, NF-κB, PI3K/Akt), and immunometabolic reprogramming. The content explores cutting-edge methodological approaches for modulating polarization, including natural compounds, nanomaterials, and repurposed drugs, with applications in oncology, autoimmune disorders, and metabolic diseases. It further addresses challenges in therapeutic targeting and offers comparative validation of strategies across disease contexts, concluding with a forward-looking perspective on translating mechanistic insights into novel clinical interventions for restoring immune homeostasis.
Decoding the Macrophage Polarization Spectrum: From Basic Biology to Inflammatory Dysregulation
Macrophages, pivotal cells of the innate immune system, exhibit remarkable functional plasticity, allowing them to respond dynamically to microenvironmental cues [1]. This plasticity is exemplified by their ability to polarize into distinct functional phenotypes, a process critical for orchestrating immune responses in health and disease [2]. The M1/M2 paradigm provides a foundational framework for understanding these polarization states, mirroring the Th1/Th2 nomenclature of T helper cells [3]. Classically activated M1 macrophages typically initiate and sustain pro-inflammatory responses, while alternatively activated M2 macrophages promote immunoregulation, tissue repair, and resolution of inflammation [4] [1]. Although this classification represents a simplified continuum of activation states rather than discrete entities, it remains an essential utilitarian shorthand for discussing the pro-inflammatory and anti-inflammatory extremes of macrophage function [4]. In chronic inflammatory diseases such as osteoarthritis, rheumatoid arthritis, and tumor microenvironments, the balance between M1 and M2 polarization significantly influences disease progression, making understanding of this paradigm therapeutically relevant [5] [2].
Historical Foundation and Conceptual Evolution
The conceptual foundation of macrophage polarization emerged from parallel investigations in immunology during the late 20th century. In 1986, Mosmann and colleagues established the Th1/Th2 dichotomy for T helper cells, which provided the conceptual groundwork for analogous macrophage categorization [3]. The term "macrophage activation" was introduced earlier by Mackaness in the 1960s within infection contexts, describing antigen-dependent enhancement of microbicidal activity against intracellular pathogens [3]. Subsequent research revealed that Th1-derived interferon-gamma (IFN-γ) promoted this classical activation, while Th2 cytokines like IL-4 and IL-13 induced a different activation pattern characterized by high endocytic activity and reduced pro-inflammatory cytokine secretion, termed "alternative activation" by Stein, Doyle, and colleagues [3].
The specific M1/M2 terminology originated from investigations of macrophage arginine metabolism by Mills and colleagues, who observed that macrophages from mouse strains with Th1 and Th2 backgrounds metabolized arginine through divergent pathways—M1 macrophages produced toxic nitric oxide (NO), while M2 macrophages produced trophic polyamines [3]. Mantovani and colleagues later expanded this classification, grouping polarization stimuli into a continuum between two polarized states: M1 (induced by IFN-γ combined with LPS or TNF) and M2 (with subgroups M2a induced by IL-4, M2b induced by immune complexes, and M2c induced by IL-10 or glucocorticoids) [3]. This categorization acknowledged the diversity of macrophage activation while providing a structured framework for investigation.
Table 1: Historical Milestones in M1/M2 Paradigm Development
| Year | Key Discovery | Researchers | Significance |
|---|---|---|---|
| 1960s | Concept of "macrophage activation" | Mackaness | Described enhanced microbicidal activity against intracellular pathogens |
| 1986 | Th1/Th2 dichotomy | Mosmann et al. | Established functional T helper cell subsets providing conceptual basis for macrophage polarization |
| 1990s | Alternative activation | Stein, Doyle et al. | Defined IL-4/IL-13-induced activation state with distinct receptor expression and cytokine profile |
| 2000 | M1/M2 terminology | Mills et al. | Introduced M1/M2 classification based on arginine metabolism pathways in different mouse strains |
| Early 2000s | Expanded polarization states | Mantovani et al. | Categorized M2 subgroups (M2a, M2b, M2c) based on different inducing stimuli |
Signaling Pathways and Molecular Regulation
M1 Polarization Signaling Cascades
Classical M1 macrophage polarization is primarily triggered by IFN-γ alone or in combination with microbial products such as lipopolysaccharide (LPS) [1]. The binding of IFN-γ to its receptor (IFNGR) activates Janus kinase (JAK) adapters, leading to phosphorylation and activation of signal transducer and transcription activator 1 (STAT1) [1]. Activated STAT1 dimerizes and translocates to the nucleus, where it induces expression of pro-inflammatory genes including major histocompatibility complex (MHC) II, IL-12, and NOS2 [1].
Simultaneously, LPS recognition by Toll-like receptor 4 (TLR4) activates two distinct signaling adapters: TIR-domain-containing adapter-inducing interferon-β (TRIF) and myeloid differentiation response 88 (MyD88) [1]. The TRIF-dependent pathway activates interferon-responsive factor 3 (IRF3), driving type I interferon production, while MyD88 signaling activates nuclear factor kappa-B (NF-κB) and activator protein 1 (AP-1) via MAPK pathways [1]. These transcription factors collectively promote expression of pro-inflammatory cytokines (TNF, IL-1β, IL-12), chemokines (CXCL10, CXCL11), co-stimulatory molecules, and antigen-processing proteins that characterize the M1 phenotype [1].
M2 Polarization Signaling Cascades
Alternative M2 macrophage polarization is primarily induced by IL-4 and IL-13, which signal through the IL-4 receptor alpha (IL-4Rα) chain [1]. Receptor engagement activates JAK1 and JAK3, leading to phosphorylation and activation of STAT6 [1]. Activated STAT6 translocates to the nucleus and cooperates with other transcription factors including IRF4 and peroxisome proliferator-activated receptor gamma (PPARγ) to drive expression of characteristic M2 markers [6] [1]. These include arginase 1 (Arg1), chitinase-like proteins (Ym1), resistin-like-α (Fizz1), CCL17, and the macrophage mannose receptor (CD206) [1].
IL-10 represents another potent M2-inducing cytokine that signals through its receptor (IL10R), leading to activation of STAT3 [1]. STAT3 induces expression of suppressor of cytokine signaling 3 (SOCS3), which inhibits pro-inflammatory cytokine signaling pathways, thereby reinforcing the anti-inflammatory M2 phenotype [1]. Glucocorticoids also promote M2 polarization through binding to glucocorticoid receptors (GR), which translocate to the nucleus and either directly bind DNA to transcribe anti-inflammatory genes like IL-10 or interact with transcription factors like NF-κB to inhibit inflammatory gene expression [1].
Table 2: Key Transcription Factors in Macrophage Polarization
| Transcription Factor | Primary Inducers | Target Genes | Polarization Role |
|---|---|---|---|
| STAT1 | IFN-γ, IFN-α/β | MHC II, IL-12, NOS2, SOCS1 | Master regulator of M1 polarization |
| NF-κB | LPS (via TLR4/MyD88), TNF-α | TNF, IL-1β, IL-6, IL-12, CXCL chemokines | Drives pro-inflammatory gene expression |
| STAT6 | IL-4, IL-13 (via IL-4Rα) | Arg1, Ym1, Fizz1, CCL17, CD206 | Master regulator of IL-4-induced M2 polarization |
| PPARγ | IL-4, fatty acids | Arg1, CD36, FABP4 | Enhances M2 gene expression and metabolic reprogramming |
| STAT3 | IL-10 | SOCS3, IL-10, IL1-R2 | Promotes anti-inflammatory M2 polarization |
| IRF4 | IL-4, IL-13 | CCL17, CCL22, CD206 | Cooperates with STAT6 for M2 gene expression |
Metabolic Reprogramming in Polarized Macrophages
Distinct Metabolic Signatures
M1 and M2 macrophages exhibit fundamentally different metabolic programs that support their divergent functions [6]. M1 polarization is characterized by a shift toward glycolysis, the pentose phosphate pathway, and fatty acid synthesis, even under normoxic conditions [6] [7]. This metabolic reprogramming is driven by stabilization of hypoxia-inducible factor 1-alpha (HIF1α), which promotes expression of glycolytic enzymes and pro-inflammatory genes [7]. The glycolytic shift provides rapid ATP generation and generates metabolic intermediates that support inflammatory functions, while also producing lactate which can itself exert immunomodulatory effects [6].
In contrast, M2 macrophages primarily utilize oxidative phosphorylation (OXPHOS) and fatty acid oxidation (FAO) for energy production [6] [7]. This metabolic phenotype supports the longevity and tissue remodeling functions of M2 macrophages. IL-4 signaling promotes mitochondrial biogenesis and enhances electron transport chain activity, making M2 macrophages dependent on intact tricarboxylic acid (TCA) cycle function [7]. Additionally, M2 polarization increases dependence on fatty acid synthesis and oxidation, with PPARγ playing a key role in regulating these metabolic pathways [6].
Advanced Metabolic Imaging Techniques
Recent advances in metabolic imaging have enabled non-invasive classification of macrophage polarization states. Fluorescence lifetime imaging microscopy (FLIM) of the intrinsic fluorophores NAD(P)H and FAD+ provides quantitative metrics of cellular metabolic states [7]. NAD(P)H fluorescence lifetime parameters differ between M1 and M2 macrophages due to their distinct metabolic programs: M1 macrophages exhibit FLIM signatures consistent with enhanced glycolysis, while M2 macrophages show parameters indicative of active oxidative phosphorylation [7].
When combined with machine learning algorithms such as random forests, 2P-FLIM can classify human macrophage polarization with excellent accuracy (ROC-AUC value of 0.944) based on metabolic parameters [7]. This non-destructive methodology enables temporal monitoring of polarization states and responses to therapeutic interventions without requiring fixation or staining, making it particularly valuable for dynamic studies of macrophage plasticity in chronic inflammation [7].
Experimental Models and Methodologies
Established Polarization Protocols
In vitro polarization of human macrophages typically begins with isolation of monocytes from peripheral blood or utilization of monocytic cell lines like THP-1 [6] [7]. THP-1 cells are differentiated into macrophages (M0) using phorbol myristate acetate (PMA) for 24 hours, followed by polarization induction [6]. For M1 polarization, cells are treated with IFN-γ (typically 20-100 ng/mL) combined with LPS (10-100 ng/mL) for 24 hours to 4 days to achieve full polarization [6]. For M2 polarization, IL-4 (10-20 ng/mL) is administered for the same duration [6]. Similar protocols apply to primary human monocyte-derived macrophages, which are generated by culturing CD14+ monocytes with macrophage colony-stimulating factor (M-CSF) for 5-7 days before polarization induction.
Table 3: Research Reagent Solutions for Macrophage Polarization Studies
| Reagent Category | Specific Examples | Function | Typical Concentrations |
|---|---|---|---|
| M1 Inducers | IFN-γ, LPS (from E. coli or Salmonella), TNF-α | Activate classical M1 polarization signaling pathways | IFN-γ: 20-100 ng/mL; LPS: 10-100 ng/mL |
| M2 Inducers | IL-4, IL-13, IL-10, M-CSF, glucocorticoids | Promote alternative M2 polarization | IL-4: 10-20 ng/mL; IL-13: 10-20 ng/mL; IL-10: 10-50 ng/mL |
| Signaling Inhibitors | MEK inhibitors (e.g., U0126, trametinib), HDAC inhibitors, PI3K inhibitors | Block specific polarization pathways for mechanistic studies | Varies by inhibitor potency and specificity |
| Metabolic Probes | 2-NBDG (glucose analog), MitoTracker, NAAD(P)H FLIM | Assess metabolic reprogramming during polarization | Manufacturer recommended concentrations |
| Polarization Markers | Antibodies against CD86, CD80, MHC II (M1); CD206, CD163, Arg1 (M2) | Identify and validate polarization states by flow cytometry or immunofluorescence | Manufacturer recommended dilutions |
Validation and Characterization Methods
Comprehensive characterization of polarized macrophages requires multimodal assessment of surface markers, cytokine secretion, gene expression, and metabolic profiles. Well-established M1 markers include surface proteins CD80, CD86, and MHC II; cytokines IL-12, TNF-α, and IL-1β; and enzymes iNOS (NOS2) [6] [1]. Prototypical M2 markers include surface receptors CD206 (mannose receptor), CD163, and CD209; cytokines IL-10, TGF-β, and CCL17; and enzymes Arg1, Ym1/2, and Fizz1 [6] [1].
Global quantitative proteomic analyses have identified approximately 7,900 proteins differentially expressed between M1 and M2 macrophages, with M2 macrophages showing upregulated MRC1, TGM2, FABP4, CCL24, and CCL26, while M1 macrophages express high levels of IDO1, FAM26F, CXCL9, and CXCL10 [6]. Time-course phosphoproteomic analyses during the first 24 hours of polarization have revealed dynamic phosphorylation events and kinase activation patterns that differ between M1 and M2 polarization, with MEK/ERK signaling identified as particularly important for M2 polarization [6].
Beyond the Dichotomy: Limitations and Refinements
While the M1/M2 paradigm provides a valuable conceptual framework, it represents a simplified view of macrophage biology that requires refinement in several aspects [3] [4]. The classification's primary limitation is its inability to fully capture the heterogeneity and plasticity of macrophage activation states observed in vivo [4]. Single-cell RNA sequencing studies have revealed multiple distinct macrophage subpopulations in tissues and tumors that don't align neatly with the M1/M2 dichotomy [8]. For example, tumor-associated macrophages (TAMs) include subsets such as C1Q+ macrophages in hepatocellular carcinomas and FN1+ TAMs in gliomas that exhibit unique transcriptional programs beyond traditional M1/M2 classification [8].
The polarization process exists along a spectrum rather than representing discrete endpoints, with macrophages often exhibiting mixed or intermediate phenotypes [4]. This continuum is influenced by complex combinations of signals in specific tissue microenvironments overlaid with temporal fluctuations [4]. Furthermore, the M1/M2 system may be inappropriate for describing the behavior of certain tissue-resident macrophage populations, such as alveolar macrophages, which minimally express many canonical M1 markers even in pro-inflammatory conditions [4].
Despite these limitations, the M1/M2 paradigm remains a useful heuristic tool for describing the pro-inflammatory and anti-inflammatory extremes of macrophage function, particularly in the context of chronic inflammatory diseases where shifts along this spectrum have therapeutic implications [5] [4]. Ongoing research aims to develop more comprehensive classification systems that incorporate spatial, temporal, and functional heterogeneity while acknowledging the contextual nature of macrophage activation.
Therapeutic Implications and Targeting Strategies
The M1/M2 balance has significant implications for chronic disease pathogenesis and treatment [5] [2]. In osteoarthritis, synovial macrophages polarized toward the M1 phenotype promote chronic inflammation and tissue destruction, while M2 macrophages facilitate tissue repair and resolution of inflammation [5] [2]. Similarly, in tumor microenvironments, M1-like TAMs generally exert antitumor effects, while M2-like TAMs promote angiogenesis, immunosuppression, and metastasis [8].
Therapeutic strategies targeting macrophage polarization include:
Inhibition of protumorigenic M2-like TAMs using CSF-1R inhibitors, CCL2 antagonists, or CD47-blocking antibodies to disrupt recruitment or survival pathways [8].
Reprogramming TAMs from M2 to M1 phenotype using nanoparticle-mediated delivery of IFN-γ or TLR agonists to stimulate antitumor immunity [8].
Targeting metabolic pathways such as MEK/ERK signaling or PPARγ-induced retinoic acid signaling that are critical for specific polarization states [6].
Epigenetic modulation using histone deacetylase (HDAC) inhibitors that can selectively block M2 polarization without inhibiting M1 polarization [6].
These therapeutic approaches highlight the translational potential of targeting macrophage polarization in chronic inflammatory diseases and cancer, though challenges remain due to macrophage plasticity and heterogeneity across disease contexts [2] [8].
The M1/M2 paradigm of macrophage activation provides a foundational framework for understanding the remarkable functional plasticity of these immune cells. While representing a simplification of in vivo complexity, the classification remains valuable for conceptualizing the pro-inflammatory and anti-inflammatory extremes of macrophage function in health and disease. The continuing refinement of this paradigm through single-cell technologies, spatial transcriptomics, and advanced metabolic imaging will enhance our understanding of macrophage biology in chronic inflammation and support the development of novel therapeutic strategies that target macrophage polarization states.
Macrophage polarization is a dynamic process whereby macrophages adopt distinct functional phenotypes in response to signals within their microenvironment [9]. This process is crucial for their diverse roles in immunity, tissue homeostasis, and repair [10]. The historical classification of macrophages into classically activated (M1) and alternatively activated (M2) types represents an oversimplification of a much more complex biological reality [11] [10]. Emerging research reveals that macrophage phenotypes exist along a continuous spectrum of activation states, with the M2 category encompassing several functionally distinct subtypes—M2a, M2b, M2c, and M2d—each playing unique roles in chronic inflammatory processes [12] [13] [14].
Understanding this continuum is paramount for chronic inflammation research, as the imbalance and plasticity of these macrophage populations contribute significantly to disease pathogenesis [11] [14]. This whitepaper provides an in-depth analysis of the macrophage polarization spectrum, with a detailed focus on the characteristics, regulatory mechanisms, and functions of M2 subtypes, providing researchers with the conceptual framework and methodological tools needed to advance therapeutic development.
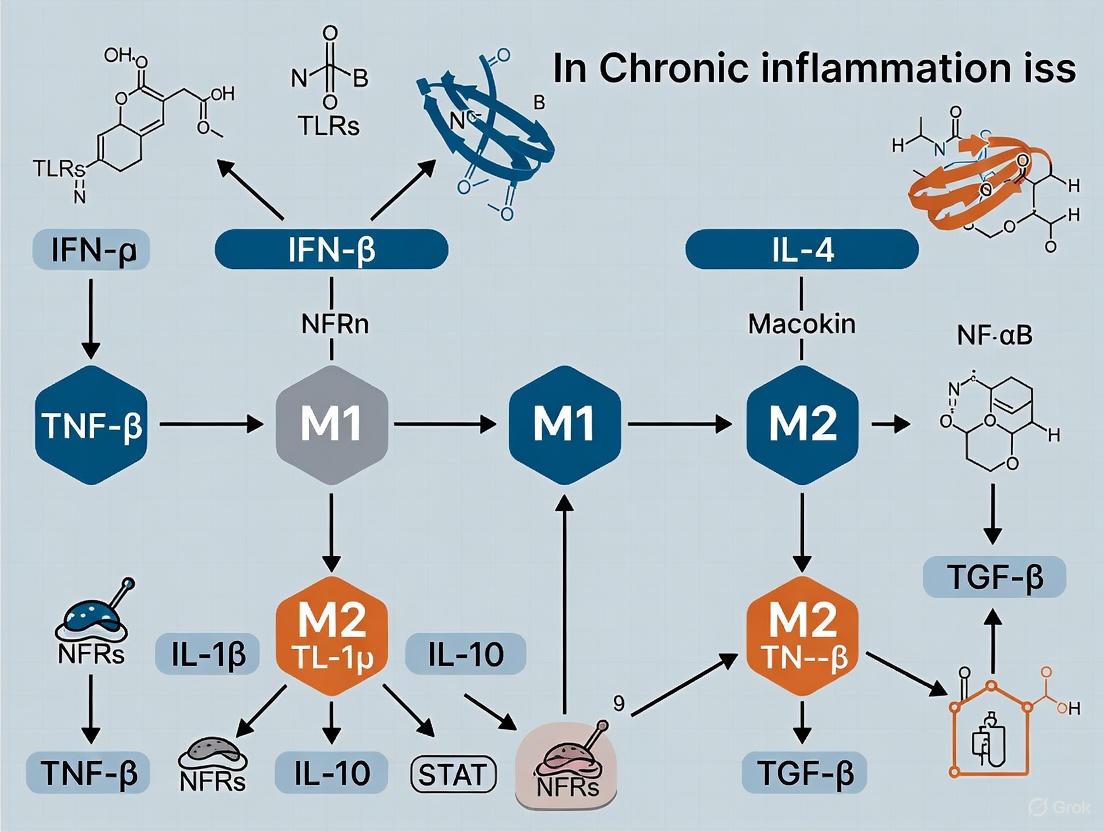
Beyond M1 and M2: The Continuum of Macrophage Activation
The M1/M2 dichotomy, originating from in vitro studies, has provided a valuable but limited framework for understanding macrophage biology [10]. In vivo, macrophages display a spectrum of phenotypic states that do not conform to this binary model [9]. Transcriptomic and epigenetic analyses have uncovered at least nine distinct directions of human macrophage activation, with numerous intermediate phenotypes existing between the M1 and M2 extremes [9]. This continuum is characterized by several key principles, as illustrated in the diagram below.
- Plasticity and Reversibility: Macrophage polarization states are not "terminally differentiated" but can change or reverse in response to evolving microenvironmental cues [9]. This plasticity is a critical feature in the transition from inflammation to resolution.
- Tissue-Specific Profiles: Tissue-resident macrophages exhibit unique transcriptional profiles shaped by their microenvironment, creating a diverse ecosystem of macrophage identities and functions throughout the body [11] [9].
- Coexistence of Phenotypes: Multiple macrophage phenotypes frequently coexist in tissues, with unique or hybrid phenotypes emerging in response to complex signal combinations [9] [10].
The M2 Subtypes: Detailed Characterization and Functional Profiles
The M2 category encompasses at least four distinct subtypes (M2a, M2b, M2c, M2d), each induced by specific stimuli and exhibiting unique marker expression and functional profiles [12] [13] [14].
M2 Subtypes: Inducing Factors, Key Markers, and Primary Functions
Table 1: Comprehensive Profile of M2 Macrophage Subtypes
| Subtype | Inducing Factors | Key Surface Markers | Secreted Cytokines & Mediators | Primary Functions |
|---|---|---|---|---|
| M2a | IL-4, IL-13 [12] [14] | CD206, MHCII, Arg1, Dectin-1, DC-SIGN (CD209) [11] [12] | IL-10, TGF-β, IGF, Fibronectin, CCL17, CCL22 [12] [14] | Wound healing, tissue repair and fibrosis, allergy and anti-parasitic responses [12] [10] |
| M2b | Immune Complexes + TLR agonists or IL-1R agonists [12] [14] | CD86, MHCII, MR (CD206) [12] [14] | High IL-10, TNF-α, IL-1β, IL-6, CCL1 [12] [14] | Immunoregulation, regulation of inflammation, promotion of Th2 activation [12] |
| M2c | IL-10, TGF-β, Glucocorticoids [12] [14] | CD163, MR (CD206), MerTK [12] [14] | IL-10, TGF-β, CCL16, CCL18, MMPs [12] [13] [14] | Acquired deactivation, phagocytosis of apoptotic cells, immunosuppression, tissue remodeling [12] [10] |
| M2d | TLR antagonists + A2R agonists, IL-6 [12] [14] | (Similar to TAMs) [12] | High IL-10, VEGF, TGF-β, low IL-12 [12] | Angiogenesis, tumor progression (often referred to as TAMs) [12] [13] |
M2 Subtype-Specific Cytokine and Chemokine Profiles
Table 2: Quantitative Secretion Profiles of M2 Macrophage Subtypes
| Secreted Factor | M2a | M2b | M2c | M2d |
|---|---|---|---|---|
| IL-10 | Moderate [12] | High [12] | High [12] | High [12] |
| IL-12 | Low [12] | Low [12] | Low [12] | Low [12] |
| TNF-α | Low | High [12] | Low | Low |
| IL-1β | Low | High | Low | Low |
| IL-6 | Low | High [12] | Low | Low |
| TGF-β | High [12] | Low | High [12] | High [12] |
| VEGF | Low | Low | Low | High [12] |
| CCL1 | Low | High [12] | Low | Low |
| CCL17/22 | High [12] | Low | Low | Low |
| CCL18 | Low | Low | High [13] [14] | Low |
Signaling Pathways Governing M2 Subtype Polarization
The differentiation of macrophages into specific M2 subtypes is controlled by distinct signaling pathways and transcription factors, as shown in the diagram below.
Experimental Protocols for M2 Subtype Analysis
In Vitro Generation of Human M2 Macrophage Subtypes
Protocol Objective: To generate and characterize human M2 macrophage subtypes from monocyte-derived macrophages.
Materials and Reagents:
- Human peripheral blood mononuclear cells (PBMCs) or isolated CD14+ monocytes
- Macrophage colony-stimulating factor (M-CSF) (50 ng/mL)
- M2a Polarization Cocktail: IL-4 (20 ng/mL) + IL-13 (20 ng/mL) for 48 hours [12]
- M2b Polarization Cocktail: Immune complexes (IgG/ovalbumin) + LPS (10 ng/mL) or IL-1R agonists for 48 hours [12]
- M2c Polarization Cocktail: IL-10 (20 ng/mL) for 48 hours [12]
- M2d Polarization Cocktail: IL-6 (20 ng/mL) + adenosine A2A receptor agonist for 48 hours [12]
Procedure:
- Monocyte Isolation: Isolate CD14+ monocytes from PBMCs using magnetic-activated cell sorting (MACS).
- Macrophage Differentiation: Culture monocytes with M-CSF (50 ng/mL) for 6 days to generate M0 macrophages.
- M2 Polarization: On day 6, stimulate M0 macrophages with the appropriate polarization cocktail for 48 hours.
- Validation: Harvest cells for flow cytometry analysis of surface markers (see Table 1) and collect supernatant for cytokine analysis by ELISA.
Technical Notes: For M2b polarization under low serum conditions (as described in [15]), reduce serum concentration to 1% during polarization to enhance immunosuppressive characteristics, including increased expression of B7-H1, FasL, and TRAIL.
Flow Cytometry Analysis of M2 Subtypes
Panel Design:
- M2a Identification: CD206+ (high), CD86- (low), IL-10+ (moderate)
- M2b Identification: CD86+ (high), CD206+ (moderate), IL-10+ (high), TNF-α+
- M2c Identification: CD163+ (high), CD206+ (moderate), IL-10+ (high)
- M2d Identification: VEGF+ (high), IL-10+ (high), CD206+ (variable)
Instrument Setup: Configure flow cytometer (e.g., BD FACSCanto II, BD LSRFortessa) using BD FACSDiva Software with application settings for consistent resolution of macrophage populations [16]. Perform daily quality control with CS&T Research Beads to ensure optimal performance.
Table 3: Key Research Reagents for M2 Macrophage Studies
| Reagent / Resource | Function / Application | Example Use Case |
|---|---|---|
| Recombinant Cytokines (IL-4, IL-13, IL-10, M-CSF) | Direct polarization of M2 subtypes in vitro | M-CSF for monocyte to macrophage differentiation; IL-4/IL-13 for M2a polarization [12] |
| Immune Complexes (IgG/OVA) | Induction of M2b phenotype | Combined with low-dose LPS for M2b polarization [12] |
| Flow Cytometry Antibodies (anti-CD206, CD163, CD86, CD80) | Identification and quantification of M2 subtypes | Multicolor flow panel to distinguish M2a (CD206+ CD86-) from M2b (CD206+ CD86+) [16] [14] |
| ELISA Kits (IL-10, TGF-β, TNF-α, VEGF) | Quantification of subtype-specific cytokine secretion | Confirm M2b phenotype via high IL-10/TNF-α secretion; M2d via VEGF detection [12] |
| BD FACSDiva Software | Flow cytometer setup, acquisition, and analysis | Automated performance tracking and index sorting for single-cell analysis [16] |
| TLR Agonists/Antagonists (LPS, A2AR agonists) | Modulation of polarization pathways | M2d generation using TLR antagonists with A2AR activation [12] |
Research Implications and Therapeutic Targeting
The precise characterization of M2 subtypes opens promising avenues for therapeutic intervention in chronic inflammatory diseases and cancer. Potential strategies include:
- Metabolic Reprogramming: Targeting metabolic pathways (e.g., arginine metabolism) that differentially regulate M1/M2 polarization [9].
- Epigenetic Modulation: Using inhibitors of DNA methyltransferases (DNMTs) or histone modifiers to shift macrophage polarization states [11].
- Nanoparticle Targeting: Designing nanocarriers that specifically deliver therapeutic agents to distinct macrophage subsets based on their surface markers and physiological environments [17].
- Signaling Pathway Manipulation: Developing drugs that target key signaling nodes (STAT6, IRF4, PPARγ) to promote beneficial M2 functions or inhibit pathological ones [1] [9].
In chronic diseases like rheumatoid arthritis, where an increased M1/M2 ratio drives pathology, promoting a shift toward M2b or M2c phenotypes could ameliorate inflammation [14]. Conversely, in tumor environments, reprogramming M2d-like tumor-associated macrophages toward an M1 phenotype could enhance anti-tumor immunity [10].
The macrophage activation spectrum extends far beyond the traditional M1/M2 dichotomy, encompassing a continuum of phenotypes with the M2 category containing at least four functionally distinct subtypes. Understanding the specific inducing signals, marker profiles, and functional capabilities of M2a, M2b, M2c, and M2d macrophages provides a critical foundation for developing targeted therapies for chronic inflammatory diseases and cancer. As single-cell technologies and spatial transcriptomics continue to reveal the complexity of macrophage biology in vivo, researchers and drug development professionals must adopt this nuanced spectrum model to advance the next generation of immunomodulatory treatments.
In the realm of immunology and chronic inflammation research, macrophages emerge as master regulators of tissue homeostasis, defense, and repair. Their remarkable functional plasticity, particularly their ability to polarize into distinct functional phenotypes, is orchestrated by a complex interplay of intracellular signaling pathways. Among these, three pathway families stand out as critical molecular switches: the Janus kinase/Signal Transducer and Activator of Transcription (JAK/STAT) pathway, the Nuclear Factor kappa-B (NF-κB) pathway, and the Phosphoinositide 3-Kinase/Protein Kinase B (PI3K/Akt) pathway. These signaling cascades transduce extracellular signals into nuanced transcriptional programs that ultimately determine macrophage polarization states and functional outcomes in health and disease.
The significance of these pathways extends beyond fundamental biology to therapeutic applications, as their dysregulation underpins numerous chronic inflammatory diseases, autoimmune conditions, and cancer [18] [19] [20]. This technical guide provides an in-depth examination of these pivotal signaling pathways, framed within the context of macrophage polarization in chronic inflammation research. We explore their molecular architectures, activation mechanisms, crosstalk, and experimental approaches for their investigation, offering researchers a comprehensive resource for advancing our understanding of immune regulation and developing targeted therapeutic interventions.
The JAK-STAT Signaling Pathway
Architectural Framework and Activation Dynamics
The JAK-STAT pathway serves as a paradigm for signal transduction from the cell surface to the nucleus, operating with remarkable architectural simplicity despite its diverse biological functions [18]. This pathway comprises three core components: cytokines and their cognate receptors, Janus kinases (JAKs), and Signal Transducers and Activators of Transcription (STATs). The JAK family of non-receptor tyrosine kinases includes four members: JAK1, JAK2, JAK3, and TYK2, which are differentially expressed across various cell types and play distinct roles in cytokine signaling [19]. The STAT family consists of seven transcription factors (STAT1-4, STAT5A, STAT5B, and STAT6) that serve as both signal transducers and transcription factors [20].
Pathway activation initiates when extracellular cytokines bind to their corresponding transmembrane receptors, inducing receptor dimerization or multimerization. This conformational change brings associated JAKs into proximity, enabling their trans-phosphorylation and activation. The activated JAKs then phosphorylate tyrosine residues on the receptor cytoplasmic tails, creating docking sites for STAT proteins via their Src homology 2 (SH2) domains. Once recruited, STATs are phosphorylated by JAKs on conserved tyrosine residues, leading to their dimerization, nuclear translocation, and DNA binding to regulate gene transcription [18].
Role in Macrophage Polarization and Inflammation
The JAK-STAT pathway is a critical determinant of macrophage polarization, primarily through its responsiveness to key cytokines in the microenvironment. STAT1 activation, triggered by IFN-γ and IL-12 signaling, drives polarization toward the pro-inflammatory M1 phenotype [20]. These macrophages produce high levels of inflammatory mediators such as TNF-α, IL-1β, IL-6, and nitric oxide synthase (iNOS), and exhibit enhanced microbicidal and tumoricidal activity [21] [20].
Conversely, STAT6 and STAT3 activation promotes the alternative M2 activation program. IL-4 and IL-13 stimulation activates STAT6, while IL-6 signaling primarily activates STAT3, both leading to expression of anti-inflammatory and tissue-reparative genes including IL-10, TGF-β, and arginase 1 (Arg1) [20]. This M2 polarization supports Th2 responses, tissue remodeling, and inflammation resolution [21].
Table 1: JAK-STAT Pathway Components in Macrophage Polarization
| Pathway Component | Role in M1 Polarization | Role in M2 Polarization |
|---|---|---|
| STAT1 | Master regulator; induced by IFN-γ/IL-12 | Generally suppressed |
| STAT3 | Can be activated but context-dependent | Primary driver; activated by IL-6, IL-10 |
| STAT6 | Not involved | Primary driver; activated by IL-4, IL-13 |
| JAK1/JAK2 | Mediates IFN-γ signaling | Mediates IL-4/IL-13 signaling |
| TYK2 | Participates in IL-12 signaling | Limited role |
The JAK-STAT pathway's involvement in inflammatory and stress-related diseases extends to neuroinflammatory disorders, with pathway activation detected in brain regions such as the cortex, hippocampus, and cerebellum in conditions like Parkinson's disease [19]. The effectiveness of JAK inhibitors (Jakinibs) in chronic inflammatory conditions such as rheumatoid arthritis has expanded the therapeutic applications of targeting this pathway [19].
Experimental Analysis of JAK-STAT Signaling
Investigating JAK-STAT signaling in macrophage polarization requires a multi-faceted approach. Essential methodologies include:
- Phospho-flow Cytometry: Enables quantification of phosphorylated STAT proteins at single-cell resolution, allowing researchers to correlate STAT activation with surface markers of macrophage polarization.
- Electrophoretic Mobility Shift Assay (EMSA): Assesses STAT DNA-binding activity using nuclear extracts and radiolabeled oligonucleotides containing STAT-binding sequences.
- Chromatin Immunoprecipitation (ChIP): Determines STAT occupancy at specific genomic loci in polarized macrophages, providing insights into transcriptional regulation.
- Luciferase Reporter Assays: Utilize STAT-responsive promoters to monitor pathway activity in response to polarizing stimuli or pharmacological inhibition.
Table 2: Key Research Reagents for JAK-STAT Pathway Analysis
| Reagent Category | Specific Examples | Research Application |
|---|---|---|
| JAK Inhibitors | Tofacitinib (JAK1/3), Ruxolitinib (JAK1/2), Filgotinib (JAK1-selective) | Functional pathway blockade; therapeutic assessment |
| STAT Phosphorylation Antibodies | Anti-pSTAT1 (Y701), Anti-pSTAT3 (Y705), Anti-pSTAT6 (Y641) | Western blot, flow cytometry for activation monitoring |
| Cytokines for Polarization | IFN-γ (M1), IL-4/IL-13 (M2) | Macrophage polarization induction |
| STAT Knockdown Tools | siRNA, shRNA constructs | Loss-of-function studies |
Diagram 1: JAK-STAT Signaling Pathway in Macrophage Polarization. This diagram illustrates the core JAK-STAT activation mechanism and its role in directing macrophage polarization toward M1 (pro-inflammatory) or M2 (anti-inflammatory) phenotypes.
The NF-κB Signaling Pathway
Canonical and Non-Canonical Activation Cascades
NF-κB transcription factors serve as pivotal regulators of immunity, inflammation, and cell survival. The mammalian NF-κB family comprises five members: NF-κB1 (p105/p50), NF-κB2 (p100/p52), RelA (p65), RelB, and c-Rel, which form various homo- and heterodimers with distinct transcriptional functions [22] [23]. These dimers are sequestered in the cytoplasm by inhibitory IκB proteins in unstimulated cells [23].
The canonical NF-κB pathway is typically activated by proinflammatory stimuli such as TNF-α, IL-1β, and pathogen-associated molecular patterns (PAMPs) through Toll-like receptors (TLRs) [23] [24]. This pathway involves the IκB kinase (IKK) complex, consisting of catalytic subunits IKKα and IKKβ and the regulatory subunit NEMO (IKKγ) [22]. Upon activation, IKKβ phosphorylates IκBα, leading to its K48-linked ubiquitination and proteasomal degradation. This process liberates predominantly RelA:p50 dimers for nuclear translocation and transcriptional activation of target genes [23] [24].
The non-canonical pathway is activated by a more limited set of receptors, including CD40, lymphotoxin beta receptor, and B-cell activating factor (BAFF) receptor [24]. This pathway depends on NF-κB-inducing kinase (NIK)-mediated activation of IKKα, which phosphorylates p100, leading to its partial proteolytic processing to p52. The resulting RelB:p52 dimers translocate to the nucleus to regulate genes involved in lymphoid organ development and adaptive immunity [23] [24].
Inflammatory Gene Regulation and Macrophage Polarization
NF-κB is often described as a "master switch" for pro-inflammatory gene expression, playing an indispensable role in M1 macrophage polarization [20]. TLR engagement on macrophages by ligands such as lipopolysaccharide (LPS) activates the canonical NF-κB pathway through either the MyD88-dependent or TRIF-dependent pathways, resulting in nuclear translocation of NF-κB p65/p50 complexes [20]. These dimers bind to κB enhancer elements in promoters of pro-inflammatory genes, including IL-1β, IL-6, TNF-α, and COX-2, thereby amplifying inflammatory signals and reinforcing the M1 polarization state [23] [20].
The relationship between NF-κB and other polarization pathways is complex and involves significant crosstalk. STAT1 has been shown to activate NF-κB transcriptional activity, while STAT3 and NF-κB engage in mutual regulation to maintain M1/M2 homeostasis [20]. This intricate interplay creates a sophisticated regulatory network that fine-tunes macrophage responses to environmental cues.
Table 3: NF-κB Family Members and Their Roles in Signaling
| NF-κB Member | Structural Features | Primary Dimerization Partners | Role in Macrophage Biology |
|---|---|---|---|
| RelA (p65) | Contains TAD | p50, c-Rel | Master driver of M1 polarization; pro-inflammatory gene transcription |
| p50/p105 | Lacks TAD; processed precursor | RelA, c-Rel, p50 | Transcriptional activator with TAD partners; repressor as homodimer |
| c-Rel | Contains TAD | p50, p65 | Enhances pro-inflammatory gene expression |
| RelB | Contains TAD | p52, p50 | Predominantly non-canonical pathway; lymphoid development |
| p52/p100 | Lacks TAD; processed precursor | RelB | Non-canonical pathway; B-cell maturation |
Experimental Approaches for NF-κB Pathway Analysis
Key methodologies for investigating NF-κB signaling in macrophage polarization include:
- IKK Kinase Assays: Measure IKK activity through in vitro kinase reactions using IκBα as substrate, often combined with immunoprecipitation of the IKK complex.
- Nuclear-Cytoplasmic Fractionation: Followed by Western blotting for NF-κB subunits to monitor nuclear translocation.
- EMSA with κB Probes: Assesses NF-κB DNA-binding activity in nuclear extracts.
- NF-κB Reporter Cell Lines: Lentiviral transduction with κB-driven luciferase constructs enables dynamic monitoring of pathway activity in living macrophages.
- ChIP-Seq: Provides genome-wide mapping of NF-κB binding sites under different polarization conditions.
Diagram 2: NF-κB Canonical and Non-canonical Signaling Pathways. This diagram illustrates both the canonical (left) and non-canonical (right) NF-κB activation pathways, highlighting their distinct triggers, signaling components, and biological outcomes.
The PI3K/Akt Signaling Pathway
Metabolic Regulation and Signal Transduction
The PI3K/Akt pathway serves as a central regulator of cellular metabolism, growth, survival, and proliferation, integrating signals from extracellular growth factors, cytokines, and nutrients [25] [26]. This pathway begins with activation of phosphoinositide 3-kinases (PI3Ks), which are classified into three categories (I, II, and III) based on structure and substrate specificity [26]. Class I PI3Ks, particularly relevant in macrophage signaling, consist of a catalytic subunit (p110α, p110β, p110γ, or p110δ) and a regulatory subunit (e.g., p85) [26].
Upon activation by receptor tyrosine kinases or G protein-coupled receptors, PI3K phosphorylates the membrane lipid phosphatidylinositol (4,5)-bisphosphate (PIP2) to generate phosphatidylinositol (3,4,5)-trisphosphate (PIP3). This lipid second messenger recruits Akt (also known as PKB) and phosphoinositide-dependent kinase 1 (PDK1) to the plasma membrane through their pleckstrin homology (PH) domains. PDK1 phosphorylates Akt at Threonine 308, while mammalian target of rapamycin complex 2 (mTORC2) phosphorylates Akt at Serine 473, resulting in full Akt activation [26]. The pathway is negatively regulated by phosphatase and tensin homolog (PTEN), which dephosphorylates PIP3 back to PIP2, and by protein phosphatase 2A (PP2A), which dephosphorylates Akt [26].
Role in Macrophage Polarization and Immunometabolism
The PI3K/Akt pathway exerts complex, context-dependent effects on macrophage polarization, influencing both M1 and M2 phenotypes through regulation of metabolic pathways and transcription factors. Akt activation generally promotes an M2-like polarization state through several mechanisms:
- mTORC1 Activation: Akt inhibits the tuberous sclerosis complex (TSC1/2), leading to activation of mTORC1, which promotes translation of M2-associated genes and regulates cellular metabolism toward glycolytic and biosynthetic pathways supportive of M2 functions [26].
- FOXO Inhibition: Akt phosphorylates Forkhead box O (FOXO) transcription factors, promoting their cytoplasmic sequestration and degradation, thereby relieving FOXO-mediated suppression of M2 gene expression [26].
- GSK3β Inhibition: Akt-mediated phosphorylation inhibits glycogen synthase kinase 3β (GSK3β), which normally suppresses M2 polarization, thus permitting alternative activation [26].
Despite this general pro-M2 bias, the PI3K/Akt pathway also contributes to specific aspects of M1 polarization, particularly in regulating inflammatory cytokine production and metabolic reprogramming to aerobic glycolysis. This apparent paradox highlights the pathway's complex, context-dependent functionality in macrophage biology.
Table 4: PI3K/Akt Pathway Components and Their Functions
| Pathway Component | Subtypes/Forms | Function in Pathway | Role in Macrophage Polarization |
|---|---|---|---|
| PI3K Catalytic Subunits | p110α, p110β, p110γ, p110δ | Phosphorylates PIP2 to PIP3 | p110α/β most relevant; initiates Akt signaling |
| Akt | Akt1, Akt2, Akt3 | Serine/threonine kinase; main effector | Generally promotes M2 polarization |
| PTEN | - | PIP3 phosphatase; pathway brake | Suppresses M2 polarization when active |
| PDK1 | - | Phosphorylates Akt at T308 | Required for partial Akt activation |
| mTORC2 | - | Phosphorylates Akt at S473 | Required for full Akt activation |
Experimental Methodologies for PI3K/Akt Pathway Investigation
Comprehensive analysis of PI3K/Akt signaling in macrophage polarization requires integrated experimental approaches:
- Lipid Blotting and Mass Spectrometry: Quantify PIP3 levels and other phosphoinositides in response to polarizing stimuli.
- Akt Activity Assays: Measure Akt kinase activity using immunoprecipitated Akt and recombinant substrates like GSK3 fusion proteins.
- Metabolic Profiling: Assess glycolytic flux, oxidative phosphorylation, and nutrient utilization using Seahorse extracellular flux analyzers and metabolic tracer studies.
- Pharmacological Inhibition: Utilize isoform-specific PI3K inhibitors (e.g., BYL719 for p110α, TGX221 for p110β), pan-PI3K inhibitors (e.g., LY294002, wortmannin), and Akt inhibitors (e.g., MK-2206) to dissect pathway requirements.
- Genetic Approaches: Employ conditional knockout mice (e.g., myeloid-specific PTEN deletion) or CRISPR/Cas9-mediated gene editing to manipulate pathway components in primary macrophages.
Diagram 3: PI3K/Akt Signaling Pathway in Macrophage Polarization. This diagram illustrates PI3K/Akt activation and its downstream effectors, showing the pathway's predominant role in promoting M2 macrophage polarization while contributing to selected M1 functions.
Pathway Crosstalk in Macrophage Polarization
Integrated Signaling Networks
The signaling pathways governing macrophage polarization do not operate in isolation but rather form an intricate network of synergistic, antagonistic, and compensatory interactions. Understanding this crosstalk is essential for comprehending the robustness and plasticity of macrophage responses in chronic inflammation.
JAK-STAT and NF-κB Crosstalk: Multiple points of integration exist between these pathways. STAT1 can activate NF-κB transcriptional activity, creating positive feedback that amplifies M1 polarization [20]. Simultaneously, STAT3 and NF-κB engage in mutual regulation to maintain M1/M2 homeostasis, with STAT3 often counterbalancing NF-κB-driven inflammation [20]. Additionally, NF-κB induces expression of various cytokines that signal through JAK-STAT pathways, creating autocrine and paracrine reinforcement loops.
PI3K/Akt and NF-κB Interactions: Akt can directly phosphorylate IKKα, enhancing NF-κB activation and potentially reinforcing M1 polarization despite Akt's general pro-M2 bias [26]. This exemplifies the context-dependent nature of pathway crosstalk, where the same molecule can contribute to apparently opposing functional outcomes depending on timing, subcellular localization, and interaction partners.
PI3K/Akt and JAK-STAT Interplay: Akt-mediated regulation of FOXO transcription factors influences STAT signaling, as FOXOs can modulate expression of STAT-dependent genes [26]. Additionally, mTORC1, a key Akt effector, regulates translation of STAT transcripts and proteins, creating another layer of integration between these pathways.
Experimental Framework for Analyzing Pathway Crosstalk
Investigating these complex interactions requires sophisticated experimental designs:
- Multiplex Phosphoprotein Analysis: Simultaneous measurement of phosphorylation states across multiple pathways using phospho-flow cytometry or Luminex arrays.
- Pathway Co-inhibition Studies: Combined pharmacological targeting of two or more pathways to identify synergistic or antagonistic interactions.
- Time-Resolved Activation Mapping: Sequential analysis of pathway activation following polarizing stimuli to establish hierarchical relationships.
- Computational Modeling: Integration of experimental data into mathematical models to predict system behavior under different perturbation conditions.
- Multi-Omics Integration: Correlation of phosphoproteomic data with transcriptomic and epigenomic profiles to connect signaling events with functional outcomes.
Table 5: Pathway Crosstalk in Macrophage Polarization
| Pathway Interaction | Molecular Mechanism | Functional Outcome |
|---|---|---|
| STAT1 → NF-κB | STAT1 enhances NF-κB transcriptional activity | Enhanced M1 polarization; amplified inflammation |
| STAT3 NF-κB | Mutual regulation; balance maintenance | M1/M2 homeostasis; prevention of excessive polarization |
| Akt → IKK/NF-κB | Akt phosphorylates IKKα | Context-dependent enhancement of NF-κB signaling |
| Akt → FOXO → STAT | Akt inhibits FOXO, modulating STAT-dependent genes | Fine-tuning of M2 polarization programs |
| mTORC1 → STAT | mTORC1 regulates STAT translation | Control of STAT protein levels and activity |
Therapeutic Targeting and Research Applications
Translational Implications for Chronic Inflammation
The pivotal role of JAK-STAT, NF-κB, and PI3K/Akt pathways in macrophage polarization and chronic inflammation has made them attractive therapeutic targets. Several targeting strategies have emerged:
JAK-STAT Targeting: JAK inhibitors (Jakinibs) have demonstrated clinical efficacy in rheumatoid arthritis and other inflammatory diseases [19]. Next-generation inhibitors with improved selectivity, such as filgotinib (JAK1-selective) and upadacitinib, offer enhanced therapeutic profiles with reduced off-target effects [19]. Combination therapies pairing Jakinibs with biological agents represent a promising frontier for enhancing specificity and efficacy.
NF-κB Pathway Modulation: Therapeutic strategies include IKK inhibitors, proteasome inhibitors (preventing IκB degradation), nuclear translocation inhibitors, and compounds interfering with NF-κB DNA binding [22] [23]. The challenge lies in achieving sufficient pathway suppression for therapeutic benefit while avoiding unacceptable immunosuppression, given NF-κB's fundamental role in host defense.
PI3K/Akt Pathway Inhibition: Isoform-specific PI3K inhibitors such as alpelisib (targeting p110α) are FDA-approved for PIK3CA-mutated cancers and are being investigated for inflammatory applications [25] [27]. Dual PI3K/mTOR inhibitors and Akt-specific inhibitors are in clinical development, with combination therapies showing promise in overcoming resistance mechanisms [27].
Research Toolkit for Investigating Pathway Roles in Macrophage Polarization
A comprehensive approach to studying these pathways requires well-defined experimental systems and reagents:
Table 6: Essential Research Tools for Signaling Pathway Investigation
| Tool Category | Specific Examples | Application Notes |
|---|---|---|
| Cell Models | Primary human monocyte-derived macrophages, murine bone marrow-derived macrophages, THP-1 human monocytic cell line | Primary cells most physiologically relevant; cell lines offer reproducibility |
| Polarization Inducers | LPS + IFN-γ (M1), IL-4/IL-13 (M2), IL-10 + TGF-β (M2c) | Standardized polarization protocols enable cross-study comparisons |
| Pathway Reporters | Lentiviral STAT-, NF-κB-, or Akt-responsive luciferase constructs | Enable real-time monitoring of pathway activity in live cells |
| Pharmacological Inhibitors | JAKi: Tofacitinib; IKKi: BMS-345541; PI3Ki: LY294002; Akti: MK-2206 | Use at validated concentrations; assess selectivity limitations |
| Genetic Tools | CRISPR/Cas9 for gene editing, siRNA/shRNA for knockdown, Conditional knockout mice | Enable specific pathway component manipulation |
| Lemildipine | Lemildipine | High-purity Lemildipine for research applications. This calcium channel blocker is for laboratory analysis. For Research Use Only. Not for human or veterinary use. |
| Lersivirine | Lersivirine, CAS:473921-12-9, MF:C17H18N4O2, MW:310.35 g/mol | Chemical Reagent |
The JAK-STAT, NF-κB, and PI3K/Akt signaling pathways represent fundamental molecular switches that orchestrate macrophage polarization and function in chronic inflammation. While each pathway possesses distinct activation mechanisms and downstream effectors, their extensive crosstalk creates a sophisticated regulatory network that enables precise control of immune responses. Continued elucidation of these signaling circuits, particularly in the context of human diseases, will undoubtedly yield new therapeutic opportunities for managing chronic inflammatory conditions, autoimmune diseases, and cancer. The experimental frameworks and technical approaches outlined in this review provide a foundation for advancing our understanding of these critical molecular switches and their integrated control of immune cell function.
Macrophages, as versatile components of the innate immune system, exhibit remarkable plasticity in response to microenvironmental signals. Their activation state, or polarization, is fundamentally linked to specific metabolic reprogramming that dictates their function in health and disease [28]. In the context of chronic inflammation, such as persistent infections or degenerative diseases, this metabolic switching plays a critical role in either perpetuating or resolving inflammatory responses [29] [30]. The classic dichotomy of macrophage polarization describes pro-inflammatory M1 macrophages and anti-inflammatory M2 macrophages, each relying on distinct metabolic pathways to fuel their functions [28] [31]. M1 macrophages predominantly utilize glycolysis for rapid energy production, even under aerobic conditions, while M2 macrophages rely primarily on oxidative phosphorylation (OXPHOS) for efficient ATP generation [31] [32]. This metabolic reprogramming is not merely a consequence of activation but an essential regulatory mechanism that controls macrophage phenotype and function through metabolic intermediates that act as signaling molecules [33] [34]. Understanding the intricate relationship between macrophage polarization and metabolic reprogramming provides crucial insights into the pathogenesis of chronic inflammatory conditions and reveals potential therapeutic targets for modulating immune responses.
Metabolic Pathways in Macrophage Polarization
Macrophages utilize five primary metabolic pathways to generate energy and biosynthetic precursors: glycolysis, the tricarboxylic acid (TCA) cycle, the pentose phosphate pathway (PPP), fatty acid metabolism (including both fatty acid oxidation and synthesis), and amino acid metabolism [29] [30]. The configuration and flux through these pathways vary dramatically between different polarization states, creating a metabolic signature that supports specific immune functions.
Glycolysis occurs in the cytoplasm and involves the breakdown of glucose to pyruvate, with a net gain of two ATP molecules per glucose molecule [33]. Under aerobic conditions, pyruvate typically enters the mitochondria for oxidation in the TCA cycle, but in M1 macrophages, this process is disrupted, and pyruvate is preferentially converted to lactate [29]. The TCA cycle, located in the mitochondrial matrix, normally generates reducing equivalents (NADH and FADH2) that feed into the electron transport chain to support OXPHOS [29] [35]. The PPP branches from glycolysis and produces NADPH for biosynthetic reactions and antioxidant defense, along with pentose sugars for nucleotide synthesis [31]. Fatty acid metabolism encompasses both catabolic (β-oxidation) and anabolic (synthesis) processes, while amino acid metabolism, particularly glutamine metabolism, provides carbon and nitrogen sources for biomass production and TCA cycle intermediates [29].
M1 Macrophages: Glycolytic Metabolism
M1 macrophages, activated by stimuli such as lipopolysaccharide (LPS) and interferon-gamma (IFN-γ), undergo a metabolic shift toward glycolysis, similar to the Warburg effect observed in cancer cells [32] [34]. This metabolic reprogramming supports their pro-inflammatory functions and antimicrobial activity through several interconnected mechanisms.
Enhanced Glycolytic Flux: M1 macrophages increase their expression of glucose transporters (GLUT1 and GLUT6) and glycolytic enzymes, including hexokinase (HK1, HK2), phosphofructokinase-1 (PFK-1), and the isoform M2 of pyruvate kinase (PKM2) [29] [31]. This increased glycolytic capacity provides rapid ATP generation to meet the energy demands of inflammation and produces metabolic intermediates that support biosynthetic processes. The transcription factor hypoxia-inducible factor-1α (HIF-1α) plays a central role in driving this glycol switch, upregulating glycolytic genes even under normoxic conditions [32].
Disrupted TCA Cycle: In M1 macrophages, the TCA cycle is broken at several points, leading to accumulation of intermediates that serve signaling functions [29] [32]. Citrate is exported from mitochondria and used for fatty acid synthesis and the production of prostaglandins and nitric oxide (NO) [32]. Succinate accumulates and stabilizes HIF-1α by inhibiting prolyl hydroxylases, further promoting glycolysis and IL-1β production [32]. Itaconate, derived from the TCA cycle intermediate cis-aconitate, has antimicrobial effects and regulates inflammatory responses [31].
Pentose Phosphate Pathway Activation: The PPP is upregulated in M1 macrophages, generating NADPH that fuels the oxidative burst via NADPH oxidase (NOX2) and supports inducible nitric oxide synthase (iNOS) activity [31]. This pathway also provides ribose-5-phosphate for nucleotide synthesis, which is necessary for the production of inflammatory mediators.
Table 1: Key Metabolic Enzymes and Their Roles in M1 Macrophages
| Enzyme | Function | Role in M1 Polarization |
|---|---|---|
| HIF-1α | Master regulator of glycolysis | Upregulates glycolytic genes, promotes inflammatory responses [32] |
| PKM2 | Glycolytic enzyme; pyruvate kinase isoform | Regulates inflammasome activation; promotes IL-1β production [31] |
| iNOS | Produces nitric oxide from arginine | Inhibits mitochondrial respiration; promotes bacterial killing [32] |
| PFKFB3 | Synthesis of fructose-2,6-bisphosphate | Allosterically activates PFK-1; drives glycolytic flux [31] |
M2 Macrophages: Oxidative Phosphorylation
In contrast to M1 macrophages, M2 macrophages (activated by IL-4 or IL-13) rely primarily on oxidative metabolism to support their functions in tissue repair, immunoregulation, and parasite clearance [28] [31]. This metabolic phenotype is characterized by intact mitochondrial pathways and efficient energy production.
Oxidative Phosphorylation: M2 macrophages maintain high rates of OXPHOS, generating ATP through the complete oxidation of glucose [31]. This process begins with glycolysis, but unlike in M1 cells, the pyruvate produced enters the mitochondria and is converted to acetyl-CoA by pyruvate dehydrogenase. Acetyl-CoA then feeds into the TCA cycle, producing NADH and FADH2 that drive the electron transport chain to produce substantial ATP yields [35].
Fatty Acid Oxidation: A hallmark of M2 polarization is the increased reliance on fatty acid oxidation (FAO) [29] [30]. Fatty acids are broken down through β-oxidation in the mitochondria, generating acetyl-CoA that fuels the TCA cycle and producing NADH and FADH2 for the electron transport chain. This metabolic pathway supports the longevity and tissue repair functions of M2 macrophages. The transcription factor PPAR-γ and its coactivator PGC-1β are key regulators of FAO in M2 macrophages [28].
Complete TCA Cycle Function: Unlike the broken TCA cycle in M1 macrophages, M2 macrophages maintain an intact cycle that efficiently generates energy and precursors [29]. Glutamine metabolism is particularly important in M2 cells, providing α-ketoglutarate that enters the TCA cycle and supports ATP production [29]. Additionally, α-ketoglutarate derived from glutamine catabolism can inhibit M1 polarization by suppressing the NF-κB pathway, thereby reinforcing the M2 phenotype [29].
Table 2: Key Metabolic Enzymes and Their Roles in M2 Macrophages
| Enzyme/Pathway | Function | Role in M2 Polarization |
|---|---|---|
| Fatty Acid Oxidation | Mitochondrial β-oxidation of fatty acids | Supports OXPHOS; provides acetyl-CoA for TCA cycle [29] |
| PPAR-γ | Nuclear receptor transcription factor | Upregulates genes for fatty acid uptake and oxidation [28] |
| Arginase-1 | Hydrolyzes arginine to ornithine and urea | Promotes polyamine and proline synthesis for tissue repair [28] |
| Glutamine Metabolism | Provides carbon and nitrogen sources | Sustains TCA cycle via α-ketoglutarate [29] |
Signaling Pathways Regulating Metabolic Reprogramming
HIF-1α Signaling in M1 Macrophages
The hypoxia-inducible factor 1α (HIF-1α) pathway serves as a master regulator of the metabolic switch to glycolysis in M1 macrophages, acting as a central node integrating inflammatory and metabolic signals [32].
Figure 1: HIF-1α Signaling in M1 Macrophage Metabolic Reprogramming. This diagram illustrates how LPS and IFN-γ signaling converge on HIF-1α activation to promote glycolysis and inflammation.
PPAR-γ and PGC-1β Signaling in M2 Macrophages
The peroxisome proliferator-activated receptor gamma (PPAR-γ) and its coactivator PGC-1β form a key signaling axis that promotes oxidative metabolism in M2 macrophages [28].
Figure 2: PPAR-γ/PGC-1β Signaling in M2 Macrophage Oxidative Metabolism. This diagram shows the signaling pathway through which IL-4 and IL-13 promote oxidative metabolism in M2 macrophages.
Experimental Protocols for Studying Macrophage Metabolism
Inducing and Validating Macrophage Polarization
M1 Polarization Protocol:
- Isolate human mononuclear cells from peripheral blood or use murine bone marrow-derived progenitors
- Differentiate monocytes into macrophages using 50 ng/mL M-CSF for 6-7 days
- Polarize macrophages toward M1 phenotype using 100 ng/mL LPS + 20 ng/mL IFN-γ for 18-24 hours [28] [32]
- Validate polarization by measuring surface markers (CD80, CD86) via flow cytometry and cytokine production (IL-1β, IL-6, IL-12, TNF-α) via ELISA [28]
M2 Polarization Protocol:
- Differentiate monocytes as described above
- Polarize macrophages toward M2 phenotype using 20 ng/mL IL-4 or IL-13 for 18-24 hours [28]
- Validate polarization by measuring surface markers (CD206, CD163) via flow cytometry and cytokine production (IL-10, TGF-β) via ELISA [28]
Metabolic Flux Analysis
Extracellular Flux Analysis:
- Seed polarized macrophages in XF96 or XF24 cell culture microplates (40,000-100,000 cells/well)
- Replace culture medium with unbuffered assay medium (XF Base Medium supplemented with 1-10 mM glucose, 1-2 mM glutamine, and 1 mM pyruvate)
- Measure glycolytic rate using the Glycolysis Stress Test:
- Measure oxidative phosphorylation using the Mito Stress Test:
- Baseline measurement of oxygen consumption rate (OCR)
- Inject 1-2 μM oligomycin to measure ATP-linked respiration
- Inject 0.5-1 μM FCCP to measure maximum respiratory capacity
- Inject 0.5 μM rotenone/antimycin A to measure non-mitochondrial respiration [31]
Metabolomic Profiling:
- Quench metabolism rapidly using cold methanol/acetonitrile/water solutions
- Extract intracellular metabolites
- Analyze metabolites using:
Research Reagent Solutions for Macrophage Metabolism Studies
Table 3: Essential Research Reagents for Studying Macrophage Metabolic Reprogramming
| Reagent Category | Specific Examples | Function/Application |
|---|---|---|
| Polarization Inducers | LPS (100 ng/mL), IFN-γ (20 ng/mL), IL-4 (20 ng/mL), IL-13 (20 ng/mL) | Induce M1 or M2 macrophage polarization [28] [32] |
| Metabolic Inhibitors | 2-Deoxyglucose (2-DG, 50 mM), Oligomycin (1 μM), FCCP (0.5-1 μM), Rotenone (0.5 μM), Antimycin A (0.5 μM) | Inhibit specific metabolic pathways for flux analysis and functional studies [31] [32] |
| Metabolic Probes | 2-NBDG (fluorescent glucose analog), MitoTracker dyes, TMRE (mitochondrial membrane potential dye) | Visualize and quantify nutrient uptake and mitochondrial function [32] |
| Antibodies for Validation | Anti-CD86, Anti-CD206, Anti-iNOS, Anti-Arg1 | Confirm macrophage polarization status via flow cytometry or Western blot [28] |
| Cytokine Assays | ELISA kits for IL-1β, IL-6, TNF-α, IL-10, TGF-β | Quantify inflammatory and anti-inflammatory cytokine secretion [28] |
Metabolic Reprogramming in Chronic Inflammation
In chronic infections and inflammatory diseases, the dynamic interplay between M1 and M2 macrophage populations and their metabolic programs plays a crucial role in disease progression and resolution [29] [30]. During early infection, M1 macrophages dominate the immune response, utilizing glycolysis to rapidly produce ATP and inflammatory mediators to combat pathogens [29]. However, as infections persist, many pathogens have evolved mechanisms to manipulate macrophage metabolism to facilitate immune evasion and ensure their long-term survival [29] [30].
In tuberculosis, caused by Mycobacterium tuberculosis, the pathogen induces metabolic reprogramming that shuts down glycolysis in infected macrophages, creating a favorable environment for bacterial persistence [31]. Similarly, in obesity-associated chronic inflammation, alterations in macrophage substrate availability (increased fatty acids and glucose) drive polarization toward pro-inflammatory phenotypes, contributing to insulin resistance and metabolic dysfunction [36]. The transition from M1 to M2 metabolism during the resolution phase of inflammation is characterized by a metabolic rebalancing, with restoration of the TCA cycle, increased OXPHOS, and enhanced fatty acid oxidation [29]. Failure of this metabolic transition can result in persistent inflammation or fibrosis, highlighting the importance of understanding these processes for therapeutic development.
The metabolic reprogramming of macrophages between glycolytic and oxidative states represents a fundamental mechanism underlying their polarization and function in chronic inflammation. The distinct metabolic signatures of M1 and M2 macrophages not only reflect their activation states but actively regulate their pro-inflammatory versus tissue-repair functions through metabolic intermediates that serve as signaling molecules. The intricate relationship between metabolism and macrophage function reveals numerous potential therapeutic targets for modulating immune responses in chronic inflammatory diseases, including metabolic enzymes, signaling pathways, and substrate availability. Future research focusing on spatiotemporal control of macrophage metabolism and the development of targeted delivery systems for metabolic modulators holds promise for innovative treatments that can precisely manipulate macrophage polarization to resolve chronic inflammation while preserving essential immune functions.
Macrophages, as crucial sentinels of the innate immune system, exhibit remarkable plasticity, allowing them to respond to microenvironmental cues by polarizing into distinct functional phenotypes. This process is central to both the initiation and resolution of inflammation in chronic inflammatory diseases. Beyond their traditional roles as structural components and energy sources, lipids and their bioactive metabolites have emerged as key regulators of macrophage polarization, shaping immune responses and inflammatory outcomes [37]. The application of lipidomics—a subset of metabolomics focused on the systematic identification and quantification of lipids—has begun to unveil the profound complexity of the lipidome and its intricate relationship with macrophage fate [38]. This technical guide explores the role of bioactive lipids and lipidomics in understanding macrophage polarization, framed within the context of chronic inflammation research. By integrating quantitative lipid profiling, detailed experimental protocols, and pathway visualizations, this review provides researchers and drug development professionals with a comprehensive framework for investigating lipid-mediated mechanisms in immunometabolic diseases.
Macrophage Polarization: A Spectrum of Functional States
Macrophages exist on a continuum of activation states, broadly categorized into classically activated (M1) and alternatively activated (M2) phenotypes, each with distinct functional roles and metabolic characteristics.
- M1 Macrophages (Pro-inflammatory): M1 polarization is typically induced by stimuli such as interferon-gamma (IFNγ) and bacterial lipopolysaccharide (LPS) [39] [40]. These cells express surface markers like CD80, CD86, and MHC-II, and secrete pro-inflammatory cytokines including IL-1, IL-6, and TNF-α [39]. A key metabolic hallmark is their reliance on aerobic glycolysis, with disruptions in the tricarboxylic acid (TCA) cycle leading to accumulation of citrate and succinate. They also produce high levels of nitric oxide (NO) via inducible nitric oxide synthase (iNOS), which confers microbicidal properties [37] [41].
- M2 Macrophages (Anti-inflammatory/reparative): M2 polarization is driven by cytokines such as IL-4 and IL-13 [37] [39]. These cells express markers like CD206, CD163, and arginase-1 (Arg1) [39]. They primarily depend on oxidative phosphorylation (OXPHOS) and feature an intact TCA cycle. Their metabolic program supports roles in immune regulation, tissue repair, and wound healing [37] [41].
Table 1: Characteristics of Macrophage Polarization States
| Feature | M1 (Classically Activated) | M2 (Alternatively Activated) |
|---|---|---|
| Activating Stimuli | IFNγ, LPS [39] [40] | IL-4, IL-13, IL-10 [37] [40] |
| Key Markers | CD80, CD86, MHC-II, iNOS [39] | CD206, CD163, Arg1, FIZZ1 [39] |
| Secreted Factors | IL-1, IL-6, TNF-α, NO, ROS [39] | IL-10, TGF-β, Arg1 [39] |
| Primary Metabolism | Aerobic Glycolysis [37] | Oxidative Phosphorylation, Fatty Acid Oxidation [37] |
| Primary Functions | Host defense, Pro-inflammation, Antimicrobial [39] | Tissue repair, Immunoregulation, Anti-inflammatory [39] |
Lipid Metabolism in Macrophage Polarization
Lipid metabolism is a central regulator of macrophage polarization, influencing membrane composition, energy production, and the generation of signaling molecules.
Metabolic Reprogramming of Lipids
- M1 Macrophages: Pro-inflammatory activation is associated with increased fatty acid synthesis (FAS). Citrate, exported from the mitochondria, is converted to acetyl-CoA by ATP-citrate lyase (ACLY) in the cytosol. Acetyl-CoA carboxylase (ACC) and fatty acid synthase (FAS) then catalyze the de novo synthesis of saturated fatty acids like palmitate [37]. This metabolic shift supports membrane remodeling for phagosome formation and provides precursors for lipid signaling molecules.
- M2 Macrophages: The anti-inflammatory phenotype relies on fatty acid oxidation (FAO) to fuel OXPHOS. M2 macrophages show increased uptake of exogenous fatty acids via receptors like CD36 and utilize the catabolic FAO pathway to generate energy, which supports their long-term tissue repair functions [37] [41].
Bioactive Lipid Signaling
Bioactive lipids, particularly eicosanoids derived from arachidonic acid (AA), are potent mediators that shape macrophage function.
- M1-Associated Signaling: In M1 macrophages, cytosolic phospholipase A2 (cPLA2) releases AA from membrane phospholipids. Free AA is subsequently metabolized by cyclooxygenase-2 (COX-2) to produce pro-inflammatory prostaglandins (e.g., PGE2) or by 5-lipoxygenase (5-LOX) to generate leukotrienes (e.g., LTB4), which amplify the inflammatory response [37].
- M2-Associated Signaling: The role of lipid mediators in M2 polarization is an area of active investigation. However, certain lysophospholipids, such as those generated by secreted phospholipase A2 (sPLA2), have been implicated in processes like phagocytosis [37]. Furthermore, the anti-inflammatory and pro-resolving lipid mediators (e.g., resolvins, protectins) often derived from polyunsaturated fatty acids like EPA and DHA, are crucial for inflammation resolution, a process in which M2-like macrophages play a key role.
Diagram 1: Lipid signaling pathways in macrophage polarization. M1 and M2 stimuli trigger distinct metabolic programs and enzymatic activities, leading to the production of specialized lipid mediators that dictate functional outcomes.
Lipidomics: Decoding the Macrophage Lipidome
Lipidomics provides a powerful set of analytical techniques for the comprehensive study of lipids in biological systems, enabling the characterization of macrophage polarization states beyond conventional gene and protein markers [42] [38].
Core Lipidomics Workflows
A typical lipidomics analysis involves multiple critical steps, from sample preparation to data analysis, as outlined below.
Diagram 2: Standard lipidomics workflow. The process involves lipid extraction from biological samples, chromatographic separation (or direct infusion), detection by mass spectrometry, and subsequent data analysis for lipid identification and quantification.
Key Methodologies and Instrumentation
Mass spectrometry (MS) is the cornerstone of modern lipidomics. The choice of MS platform depends on the research goals, whether for untargeted discovery or targeted, quantitative analysis.
Table 2: Comparison of Mass Spectrometry Technologies for Lipidomics
| Method | Key Advantages | Key Limitations | Common Application in Macrophage Studies |
|---|---|---|---|
| LC-Triple Quadrupole (LC-QqQ) | High sensitivity and specificity in MRM mode; ideal for targeted quantification of known lipids [42]. | Lower mass resolution than QTOF or Orbitrap; less effective for untargeted discovery [42]. | Targeted profiling of eicosanoids and specific phospholipid classes [43]. |
| LC-Quadrupole Time-of-Flight (LC-QTOF) | High mass accuracy and resolution; suitable for untargeted profiling and identification of unknown lipids [42]. | Lower sensitivity than MRM in QqQ; longer run times; higher instrument cost [42]. | Global, untargeted lipidomics to discover novel lipid markers of polarization [38]. |
| Shotgun Lipidomics | High-throughput; no chromatography; reduced analysis time; suitable for limited sample material [38]. | Cannot distinguish isobaric lipids; ion suppression effects in complex mixtures [38]. | High-throughput screening of major lipid classes in macrophage subpopulations [38]. |
| LC-Orbitrap | Very high mass resolution and accuracy; excellent for structural elucidation and complex mixtures [42]. | High cost; longer run times; requires expert operation [42]. | Deep characterization of lipidomes and identification of low-abundance lipid species. |
Quantitative Lipid Profiling in Polarized Macrophages
Lipidomics studies have revealed specific alterations in the lipidome during macrophage polarization. The following table summarizes key quantitative changes observed in human and murine macrophages.
Table 3: Select Lipidomic Changes in Polarized Macrophages from Experimental Studies
| Lipid Class | Observed Change | Experimental Model | Potential Functional Implication |
|---|---|---|---|
| Glycerophospholipids (PC, PE, PS, PI) | Shift from saturated/monounsaturated to polyunsaturated species in M1 and M2 vs. monocytes/M0 [43]. | Human THP-1 monocyte cell line. | Increased membrane fluidity and provision of substrates for lipid mediator synthesis. |
| Lysophosphatidylinositol (lysoPI) | Significantly increased in M2 vs. M1 macrophages [43]. | Human THP-1 and mouse RAW264.7 cell lines. | Potential role in M2 polarization and anti-inflammatory processes [43]. |
| Phosphatidylglycerol (PG) | Upregulated in M1 macrophages [43]. | Human THP-1 monocyte cell line. | Association with pro-inflammatory activation. |
| Lysophosphatidylserine (lysoPS) | Decreased in M2 vs. M1 macrophages [43]. | Human THP-1 monocyte cell line. | Potential marker for distinguishing M1 from M2 phenotypes. |
| Arachidonic Acid (AA) in Phospholipids | Increased mobilization in M1 macrophages [40]. | Human monocyte-derived macrophages (MDM). | Provides substrate for pro-inflammatory eicosanoid production. |
| Thromboxane Aâ‚‚ (TXAâ‚‚) | Identified as a specific marker of M1 polarization [40]. | Human monocyte-derived macrophages (MDM). | Contributes to pro-inflammatory and pro-thrombotic state. |
Detailed Experimental Protocol: Lipidomics of Polarized Human Macrophages
The following protocol, adapted from published methodologies [40] [43], details the process for generating and analyzing polarized human macrophages.
Monocyte Isolation and Macrophage Differentiation
- Source Cells: Use human peripheral blood mononuclear cells (PBMCs) isolated from healthy donors via density gradient centrifugation (e.g., Ficoll-Paque). Isolate monocytes from PBMCs by negative selection using a commercial kit (e.g., Miltenyi Monocyte Isolation Kit II) [40].
- Exclusion Criteria: Consider donor health status. Typical exclusions include fever >101°F in preceding 48 hours, current antibiotic or immunosuppressive therapy, chronic viral infection, or active cancer [40].
- Differentiation: Culture isolated monocytes (e.g., 1.35 x 10ⶠcells/well in a 6-well plate) for 7 days in RPMI 1640 medium supplemented with 10% FBS and 100 ng/mL recombinant human M-CSF to differentiate them into monocyte-derived macrophages (MDMs) or M0 macrophages [40]. Allow cells to rest for 24 hours in M-CSF-free medium before polarization.
Macrophage Polarization
Treat differentiated MDMs for 24 hours with specific polarizing stimuli in RPMI medium with 5% FBS [40]:
- M1 Polarization: 20 ng/mL IFNγ + 100 ng/mL ultrapure LPS from E. coli K12.
- M2a Polarization: 20 ng/mL IL-4.
- M2c Polarization: 20 ng/mL IL-10.
- M0 (Resting): Vehicle control.
Lipid Extraction and Sample Preparation
- Extraction Method: Use a modified Folch method for biphasic lipid extraction [40] [38].
- Wash polarized macrophage cells and scrape cell pellets.
- Add 500 μL of 5% HCl and 750 μL of Folch solution (chloroform:methanol, 2:1 v/v, containing an antioxidant like 17 mg/L butylated hydroxytoluene) to the pellet.
- Vortex vigorously and centrifuge briefly (e.g., 15,000 rpm).
- Carefully recover the lower organic phase, which contains the lipids.
- Sample Storage: Dry the organic extracts under a gentle stream of nitrogen or using a vacuum concentrator. Store dried lipid extracts at -80°C until MS analysis [40].
Lipidomic Analysis by Mass Spectrometry
- Instrumentation: Employ liquid chromatography coupled to a triple quadrupole mass spectrometer (LC-QqQ) operating in multiple reaction monitoring (MRM) mode for targeted, quantitative analysis [43]. Alternatively, use LC-QTOF for untargeted profiling.
- Chromatography: Utilize reverse-phase liquid chromatography (RPLC) with a C18 column for separation based on lipid hydrophobicity. A typical mobile phase system is a gradient of water and methanol or acetonitrile, often with additives like 10 mM ammonium formate to enhance ionization [40] [43].
- Quantification: Use internal standards for precise quantification. A commercial SPLASH Lipidomix standard cocktail, containing stable isotope-labeled or unnatural lipid species representing major lipid classes, is added to each sample prior to extraction. Quantify individual lipid species by comparing their peak areas to the area of the corresponding internal standard [38].
Data Analysis and Validation
- Bioinformatics: Use specialized software (e.g., LipidSearch, MarkerView, or open-source platforms) for peak picking, alignment, and lipid identification based on precursor mass, fragmentation patterns, and retention time [38].
- Statistical Analysis: Perform multivariate statistical analysis, such as Principal Component Analysis (PCA) and clustering analysis, to identify lipid signatures that distinguish polarization states. Follow with univariate analysis (e.g., t-tests, ANOVA) to determine significant changes in individual lipid species (fold change >1.5 or <0.67 with p < 0.05 is often used as a threshold) [43].
- Phenotype Validation: Validate macrophage polarization states in parallel cultures using established molecular markers. Isolate RNA and perform qRT-PCR to measure the expression of M1 markers (e.g., CCL3, TNFα) and M2 markers (e.g., CCL22, CCL17) [43].
Table 4: Key Research Reagent Solutions for Macrophage Lipidomics
| Reagent / Resource | Function / Purpose | Example Product / Specification |
|---|---|---|
| Cell Culture Cytokines | To induce and maintain macrophage differentiation and polarization. | Recombinant Human M-CSF, IFNγ, IL-4, IL-10 (PeproTech, R&D Systems) [40]. |
| Polarization Inducer | To trigger robust M1 polarization via TLR4 activation. | Ultrapure LPS from E. coli K12 (Invivogen) [40]. |
| Lipid Internal Standards | For accurate quantification of lipids; corrects for extraction efficiency and ionization variability. | SPLASH Lipidomix Mass Spec Standard (Avanti Polar Lipids) [38]. |
| Lipid Extraction Solvents | To isolate lipids from cells and remove proteins/nucleic acids. | Chloroform, Methanol (HPLC or MS-grade) for Folch (2:1) or Bligh & Dyer (1:2) methods [38]. |
| LC-MS Column | To separate complex lipid mixtures prior to MS detection. | Reverse-Phase C18 column (e.g., 1.7μm, 3.0 x 100 mm) [40]. |
| Mass Spectrometer | For identification and quantification of lipid species. | LC-Triple Quadrupole (e.g., for MRM) or LC-QTOF systems (e.g., Waters Synapt G2-S) [40] [42]. |
Implications for Chronic Inflammation and Therapeutic Development
The interaction between lipid metabolism and macrophage polarization is critically involved in the pathogenesis of chronic inflammatory diseases. In conditions like atherosclerosis, dysfunctional lipid metabolism leads to the accumulation of modified lipoproteins (e.g., oxidized LDL) in the arterial wall, which can be taken up by macrophages via scavenger receptors, promoting a pro-inflammatory, M1-like state and fueling a chronic inflammatory cycle [44] [41]. Similarly, in obese adipose tissue, increased lipolysis leads to elevated free fatty acids that can activate macrophages, contributing to a state of meta-inflammation and insulin resistance [41].
Lipidomics holds significant promise for therapeutic development. It facilitates the discovery of multiparameter lipid biomarkers for diagnosing disease stages and monitoring therapeutic efficacy in preclinical and clinical trials [42] [45]. Furthermore, understanding the specific lipid pathways that drive macrophage polarization provides a basis for developing novel therapeutics. Strategies may include small molecules that modulate key lipid-metabolizing enzymes (e.g., cPLA2, COX-2) or dietary interventions with specialized pro-resolving lipid mediators to promote an anti-inflammatory, M2-like macrophage phenotype and facilitate inflammation resolution [37] [42]. As lipidomics technologies and standardization continue to advance, they are poised to play an increasingly vital role in dissecting disease pathophysiology and guiding targeted immunomodulatory therapies.
Therapeutic Modulation of Macrophage Phenotype: From Natural Compounds to Advanced Nanotechnologies
Macrophage polarization plays a pivotal role in immune homeostasis and disease progression across inflammatory, neoplastic, and metabolic disorders. The dynamic process whereby macrophages adopt distinct functional phenotypes—pro-inflammatory M1 or anti-inflammatory M2—in response to environmental signals represents a crucial therapeutic target for managing chronic inflammation. Natural compounds, particularly saponins and polyphenols, have emerged as promising therapeutic regulators of macrophage polarization due to their multi-target mechanisms and favorable safety profiles. This technical guide provides an in-depth analysis of the mechanistic insights, experimental methodologies, and therapeutic applications of ginsenosides, astragaloside IV, and pomegranate peel polyphenols in modulating macrophage polarization, offering researchers and drug development professionals a comprehensive resource for advancing this promising field.
Molecular Mechanisms of Macrophage Polarization
Macrophages exhibit exceptional plasticity, dynamically shifting between phenotypes regulated by cytokines, growth factors, and microbial signals that influence gene expression via distinct intracellular pathways. The traditional classification distinguishes between classically activated M1 macrophages and alternatively activated M2 macrophages, though this represents a spectrum rather than a strict dichotomy [46].
- M1 Macrophages: Characterized by surface markers including MHC II, CD40, CD80, and CD86, M1 macrophages differentiate under stimulation with lipopolysaccharide (LPS), interferon-gamma (IFN-γ), or tumor necrosis factor-alpha (TNF-α) [46]. They express receptors including TLR4, MARCO, CD25, and CD80, and secrete high levels of pro-inflammatory cytokines such as TNF-α, interleukin-6 (IL-6), IFN-γ, nitric oxide (NO), and reactive oxygen species (ROS) [46]. These macrophages enhance immune surveillance and directly kill pathogens through strong cytotoxic effects.
- M2 Macrophages: Associated with anti-inflammatory and regenerative functions, M2 macrophages polarize upon stimulation by anti-inflammatory cytokines such as interleukin-4 (IL-4), interleukin-10 (IL-10), IL-13, or transforming growth factor-beta (TGF-β) [46]. They express markers including CD163, CD204, and CD206, and recognize receptors such as the mannose receptor (MR), scavenger receptor A (SR-A), CD163, and CD209 [46]. These macrophages secrete bioactive molecules including resistin-like Fizz1, arginase-1 (Arg1), chitinase-3-like-protein-1 (CHI3L1), IL-10, and MR C-type 1 (Mrc1, also known as CD206) that play critical roles in tissue repair, wound healing, and immune modulation [46].
The M2 phenotype exhibits notable diversity across inflammatory and pathological conditions and is further subdivided into M2a, M2b, M2c, and M2d subtypes, each with distinct activation stimuli, markers, and functional roles [46].
Table 1: Macrophage Polarization Phenotypes and Characteristics
| Polarization Type | Activation Stimuli | Surface Markers | Secreted Cytokines/Factors | Primary Functions |
|---|---|---|---|---|
| M1 | LPS, IFN-γ, TNF-α | CD86, CD197, MHC II | TNF-α, IL-6, IL-12, IL-23, NO, ROS | Pro-inflammatory response, pathogen clearance, anti-tumor activity |
| M2a | IL-4, IL-13 | CD206, ARG1 | IL-10, TGF-α, IGF | Tissue repair, anti-inflammatory, fibrosis promotion |
| M2b | IL-1β, immune complexes | CD86 | IL-10, IL-1, IL-6, TNF-α | Immunoregulation, Th2 activation |
| M2c | IL-10, TGF-β, glucocorticoids | CD163 | IL-10, TGF-β | Phagocytosis, matrix deposition, tissue remodeling |
| M2d | TLR ligands, adenosine | CD206, CD163, TIE2 | IL-10, VEGF | Angiogenesis, tumor progression |
Mechanistic Insights into Natural Compound Action
Saponin-Mediated Macrophage Polarization
Saponins, characterized by steroidal or triterpenoid aglycone structures linked to sugar moieties, demonstrate significant therapeutic potential through immunomodulatory, anti-inflammatory, and anti-tumor activities. Key saponins including ginsenosides, astragaloside IV, dioscin, platycodin D, pulsatilla saponins, and panax notoginseng saponins modulate macrophage polarization through multiple signaling pathways [46] [47].
Ginsenosides: These triterpenoid saponins from Panax ginseng exhibit remarkable effects on macrophage polarization. Comparative studies of six ginsenosides (Rg1, Rg3, Rd, Re, Rb1, and Rf) revealed that Rg1, Rg3, and Rf were most effective in reducing LPS-induced inflammation in RAW264.7 macrophages, with Rg1 demonstrating superior efficacy in restoring the M1/M2 balance by decreasing CD86+ M1 macrophages and promoting polarization toward CD206+ M2 phenotypes [48]. Ginsenosides have been shown to activate the STAT6 pathway, driving macrophages toward the M2 phenotype, thereby enhancing anti-inflammatory responses and supporting tissue repair [46].
Astragaloside IV (AS-IV) and Cycloastragenol (CAG): Derived from Astragalus membranaceus, these triterpenoid saponins modulate critical signaling pathways including TLR4/NF-κB, PI3K-AKT, AMPK, and PPARγ [49]. AS-IV mitigates sepsis by inhibiting macrophage activation and polarization, while CAG alleviates neuroinflammation in Parkinson's disease by promoting microglial autophagy and suppressing ROS-induced NLRP3 inflammasome activation [49]. In atherosclerosis, AS-IV mitigates foam cell formation by targeting the TGF-β-activated kinase (TAK1) signaling pathway, reducing macrophage adhesion and migration [49]. Additionally, CAG improves imiquimod-induced psoriasis-like inflammation in mice by selectively inhibiting NLRP3 inflammasome-mediated pyroptosis [49].
Table 2: Saponin Effects on Macrophage Polarization and Signaling Pathways
| Saponin Compound | Source | Macrophage Effects | Key Signaling Pathways | Therapeutic Applications |
|---|---|---|---|---|
| Ginsenoside Rg1 | Panax ginseng | ↓ M1 (CD86+), ↑ M2 (CD206+), ↓ IL-6, TNF-α, ↑ IL-10 | STAT6, NF-κB | Inflammatory bowel disease, colitis [48] |
| Astragaloside IV | Astragalus membranaceus | ↓ M1, ↑ M2, ↓ NLRP3 inflammasome | TLR4/NF-κB, PI3K-AKT, AMPK, PPARγ, TAK1 | Sepsis, atherosclerosis, fibrosis [49] |
| Cycloastragenol | Astragalus membranaceus | ↑ Autophagy, ↓ NLRP3, ↓ ROS | NLRP3 inflammasome, AMPK | Neuroinflammation, psoriasis [49] |
| Total Saponins of Panax japonicus | Panax japonicus | ↓ M1/M2a ratio, ↓ glycolysis | HIF-1α, GLUT1, HK2, LDHA | Rheumatoid arthritis [50] |
Polyphenol-Mediated Macrophage Polarization
Pomegranate Peel Polyphenols (PPPs): Pomegranate peel, a by-product comprising approximately 50% of the fruit mass, is rich in bioactive metabolites including ellagitannins (ellagic acid, punicalagin, punicalin), phenolic acids, and flavonoids [51]. These compounds demonstrate significant effects on macrophage polarization through modulation of critical signaling pathways.
PPPs exhibit therapeutic effects in acne vulgaris by inhibiting the Notch/NF-κB signaling pathway. In both in vivo (SD rats injected with Cutibacterium acnes) and in vitro (LPS-induced RAW264.7 cells) models, PPPs significantly reduced pro-inflammatory cytokine levels (IL-1α, TNF-α, IL-6, IL-8, IL-12) and decreased macrophage infiltration in skin lesions [52]. The mechanism involves inhibition of Notch, NF-κB, IL-1α, IL-6, and TNF-α protein and mRNA expression, along with reduced NF-κB phosphorylation [52].
Individual components of PPPs demonstrate specific activities. Punicalagin, the primary contributor to antioxidant properties in pomegranate products, significantly inhibits TNF-induced expression of pro-inflammatory factors (IL-1β, IL-6) in human placenta and adipose tissue [51]. Pedunculagin alleviates lupus nephritis in mice by inhibiting the protease-activated receptor 2 pathway, while corilagin inhibits reverse transcriptase activity of RNA tumor viruses, demonstrating anticancer effects [51].
Experimental Models and Methodologies
In Vitro Models and Protocols
RAW264.7 Macrophage Culture and Treatment:
- Cell Culture: RAW264.7 murine macrophage cells are grown in high-glucose Dulbecco's Modified Eagle Medium (DMEM) supplemented with 10% fetal bovine serum and 1% penicillin/streptomycin at 37°C in a 5% CO₂ incubator [48].
- Viability Assessment: Cell viability is tested using Cell Counting Kit-8 (CCK-8) assay. Cells are plated in 96-well plates at 2×10ⴠcells/well with 6 replicates per treatment. After adherence, cells are treated with various concentrations of compounds (0-100 μM) for 24h. Supernatant is replaced with medium containing 10% CCK-8 solution for 2h, and absorbance is measured at 450nm [48].
- Inflammation Induction: For polarization studies, cells are treated with compounds at concentrations of 25μM (low) or 50μM (high) followed by LPS (1μg/mL) for 12h to induce M1 polarization [48].
- Flow Cytometry Analysis: Macrophage polarization is assessed using flow cytometry with the following antibodies: PE/Cyanine7 anti-mouse CD86 (M1 marker), Alexa Fluor 647 anti-mouse CD206 (M2 marker), FITC anti-mouse/human CD11b, and PE anti-mouse F4/80 [48].
- Gene Expression Analysis: mRNA expression of inflammatory cytokines is quantified by qPCR. Cells are lysed with Trizol reagent, RNA is extracted, and cDNA is synthesized using reverse transcriptase. Gene expression is analyzed using SYBR Green-based qPCR with specific primers [48].
In Vivo Models and Protocols
Dextran Sulfate Sodium (DSS)-Induced Colitis Model:
- Induction Protocol: Mouse colitis is induced by administering sterile water containing 2-3% DSS for 7 days [48].
- Compound Administration: Test compounds are administered orally or intraperitoneally during or after DSS induction.
- Disease Assessment: Disease activity index (DAI) is calculated based on body weight loss, stool consistency, and fecal blood. Colon length is measured as an indicator of inflammation severity [48].
- Cytokine Measurement: Serum inflammatory cytokines are quantified by ELISA according to manufacturer protocols [48].
- Metabolomic Analysis: Intestinal metabolites are analyzed by LC-MS/MS. Approximately 50mg of colon content or tissue is homogenized in methanol:water (4:1) solution, centrifuged, and supernatant is analyzed [48].
Cutibacterium acnes-Induced Acne Model:
- Model Establishment: SD rats are injected intracutaneously with C. acnes solution (6×10ⷠCFU/mL) into both sides of the auricle once daily for 3 days, followed by intraperitoneal injection of the same solution (1mL) once daily for 7 consecutive days [52].
- Treatment Protocol: PPPs cream is applied topically at doses of 0.28, 0.14, and 0.07 g/kg twice daily for 7 days [52].
- Assessment: Inflammatory cytokine levels (IL-1α, TNF-α, IL-6, IL-8, IL-12) in serum and skin lesions are measured by ELISA. Skin histopathology is evaluated by H&E staining [52].
Adjuvant-Induced Arthritis (AIA) Model:
- Induction and Treatment: AIA is induced in rats, which are then treated with total saponins from Panax japonicus (TSPJ) [50].
- Analysis: Joint swelling is measured, serum inflammatory cytokines are quantified by ELISA, and joint bone erosion is evaluated by micro-CT [50].
- Glycolytic Regulators: Protein expressions of HIF-1α, GLUT1, HK2, and LDHA in ankle joints are analyzed by immunohistochemistry and western blotting [50].
- Microbiome Analysis: Colonic contents and mucosa are analyzed by 16S rRNA sequencing to assess microbiota diversity and community structure [50].
Signaling Pathway Visualization
Diagram 1: Mechanism of Natural Compounds in Macrophage Polarization Regulation. This diagram illustrates how saponins and polyphenols target multiple signaling pathways to modulate macrophage polarization, resulting in diverse therapeutic effects.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for Macrophage Polarization Studies
| Reagent/Category | Specific Examples | Research Application | Experimental Function |
|---|---|---|---|
| Cell Lines | RAW264.7 murine macrophages, THP-1 human monocytes | In vitro polarization studies | Provide reproducible cellular models for mechanistic studies and compound screening [52] [48] |
| Polarization Inducers | LPS, IFN-γ, IL-4, IL-13 | M1/M2 polarization induction | Standardized stimuli to induce specific macrophage phenotypes for experimental manipulation [48] [53] |
| Cytokine Detection | ELISA kits for TNF-α, IL-6, IL-1β, IL-10, IL-12 | Inflammatory profiling | Quantify secreted cytokines to assess inflammatory status and compound efficacy [52] [48] |
| Flow Cytometry Antibodies | Anti-CD86 (M1), anti-CD206 (M2), anti-CD11b, anti-F4/80 | Phenotype characterization | Identify and quantify macrophage polarization states using surface marker expression [48] |
| Molecular Biology Kits | qPCR reagents, western blot kits, RNA extraction kits | Mechanistic studies | Analyze gene and protein expression in signaling pathways modulated by compounds [52] [48] |
| Animal Models | DSS-induced colitis, AIA rats, C. acnes-induced acne | In vivo validation | Assess therapeutic efficacy of compounds in disease-relevant contexts [52] [50] [48] |
| Letrazuril | Letrazuril | Letrazuril is a small molecule triazine compound for anticoccidial research. This product is for Research Use Only (RUO). Not for human or veterinary use. | Bench Chemicals |
| L-Leucinol | L-Leucinol, CAS:7533-40-6, MF:C6H15NO, MW:117.19 g/mol | Chemical Reagent | Bench Chemicals |
Therapeutic Applications and Clinical Translation
The therapeutic potential of saponins and polyphenols in macrophage polarization extends across diverse disease contexts, offering promising approaches for conditions characterized by inflammatory dysregulation.
Inflammatory Bowel Disease (IBD): Ginsenoside Rg1 demonstrates exceptional efficacy in colitis models, significantly decreasing M1-related pro-inflammatory cytokines while increasing M2-related anti-inflammatory cytokines [48]. It promotes polarization toward CD206+ M2 macrophages and restores gut metabolite composition, reversing key metabolic alterations associated with colitis [48].
Rheumatoid Arthritis (RA): Total saponins from Panax japonicus (TSPJ) alleviate adjuvant-induced arthritis by inhibiting the glycolysis pathway in M1 macrophages, reducing inflammatory cytokines, lactate, and LPS levels [50]. TSPJ downregulates glycolytic regulators HIF-1α, GLUT1, HK2, and LDHA in ankle joints and restores microbiota diversity, enriching probiotic abundances like Eubacterium_coprostanoligenes_group and Christensenella [50].
Atherosclerosis: Astragaloside IV mitigates atherosclerosis development by targeting the TAK1 signaling pathway, reducing macrophage adhesion and migration, and preventing foam cell formation [49]. The compound shifts the balance from pro-inflammatory M1 macrophages dominant in early plaques toward M2 macrophages that stabilize plaques through IL-10, TGF-β, and collagen synthesis [46].
Acne Vulgaris: Pomegranate peel polyphenols ameliorate C. acnes-induced inflammation by inhibiting the Notch/NF-κB signaling pathway, reducing pro-inflammatory cytokine production and macrophage infiltration in skin lesions [52].
Cancer: Saponins demonstrate anti-tumor activity by suppressing M2-like tumor-associated macrophages (TAMs) that promote tumor progression through metabolic reprogramming including upregulation of fatty acid oxidation and CD36-mediated lipid uptake via PPAR-γ-dependent pathways [46]. Astragaloside IV shows anti-tumor activity in gastric, colon, and liver cancer by affecting key molecular signaling pathways including miRNA regulation, mitochondrial apoptosis, and immune checkpoint suppression [54].
Challenges and Future Perspectives
Despite the significant therapeutic potential of natural compounds in regulating macrophage polarization, several challenges hinder clinical translation. Poor bioavailability of compounds like astragaloside IV (only 3.66% in rats) and complex multi-target mechanisms present substantial obstacles [46] [54].
Innovative delivery strategies are essential to overcome these limitations. Nanotechnology approaches including nanoemulsions, engineered exosomes, and nanodrug carriers have emerged as transformative solutions to enhance pharmacokinetics and therapeutic index [46] [49]. For pomegranate peel extract, applications in biomedical materials such as nanodrug carriers, hydrogels, and tissue engineering scaffolds show promise for improving delivery and efficacy [51].
Future research should prioritize:
- Elucidating precise molecular mechanisms underlying natural compound-mediated macrophage polarization
- Developing targeted delivery systems to enhance bioavailability and tissue specificity
- Exploring combination therapies with conventional treatments
- Incorporating gene-editing technologies and computer-aided drug design to optimize therapeutic potential
- Conducting rigorous clinical trials to validate preclinical findings
The integration of advanced technologies with traditional natural compounds represents a promising frontier for developing novel therapeutic strategies that target macrophage polarization in chronic inflammatory diseases, cancer, and metabolic disorders.
Macrophages are highly plastic cells of the innate immune system that play critical roles in maintaining tissue homeostasis, defending against pathogens, and resolving inflammation [1]. Their functional diversity is largely governed by a process called polarization, where they adopt distinct phenotypic states in response to microenvironmental cues. The classical M1 (pro-inflammatory) and alternative M2 (anti-inflammatory/resolutive) polarization states represent extremes along a functional spectrum, each characterized by unique transcriptional programs, metabolic profiles, and secretory outputs [20]. In chronic inflammatory diseases, including atherosclerosis, rheumatoid arthritis, and metabolic dysfunction-associated fatty liver disease (MASLD), a persistent imbalance in macrophage polarization—often favoring the M1 phenotype—drives disease progression by sustaining inflammatory responses, promoting tissue damage, and impairing resolution mechanisms [55] [20].
Targeting macrophage polarization has emerged as a promising therapeutic strategy for recalibrating the immune response in chronic inflammation. While novel drug development faces considerable time and cost barriers, drug repurposing offers a strategic alternative. Screening existing FDA-approved compounds for macrophage-modulating effects can rapidly identify candidates with established safety profiles for new therapeutic applications [55] [56]. This whitepaper synthesizes recent advances in this field, highlighting repurposed drugs, their mechanisms of action, and practical experimental approaches for evaluating macrophage modulation.
Key Signaling Pathways Regulating Macrophage Polarization
Macrophage polarization is directed by intricate signaling networks that translate extracellular signals into distinct transcriptional and metabolic programs. The major pathways involved are summarized below.
JAK-STAT Signaling Pathway
The JAK-STAT pathway is a principal mediator of cytokine-driven polarization [20]. STAT1 activation downstream of IFN-γ and LPS promotes M1 polarization by inducing pro-inflammatory genes like iNOS. Conversely, STAT6 activation by IL-4/IL-13 and STAT3 activation by IL-10 drive M2 polarization, upregulating genes such as Arg1, CD206, and CD163 [1] [20].
NF-κB Signaling Pathway
Acting as a "master switch" for inflammation, the NF-κB pathway is activated by TLR ligands like LPS via MyD88-dependent or TRIF-dependent signaling [1] [20]. This leads to nuclear translocation of NF-κB subunits (e.g., p65/p50), stimulating transcription of key M1 markers and pro-inflammatory cytokines (TNF-α, IL-1β, IL-6).
PPARγ and Retinoic Acid Signaling
The nuclear receptor PPARγ is a critical regulator of M2 polarization [6] [57]. Activation of PPARγ promotes fatty acid oxidation and induces genes involved in resolution. Recent work shows that the MEK/ERK signaling axis can promote M2 polarization by inducing PPARγ and subsequent retinoic acid signaling [6]. Furthermore, the antipsychotic thiothixene was found to promote efferocytosis in macrophages by upregulating the retinol-binding protein receptor Stra6L, thereby enhancing production of the M2-associated enzyme Arginase 1 [55].
FDA-Approved Drugs with Macrophage-Modulating Effects
High-throughput screening of FDA-approved drug libraries has identified several promising candidates for repurposing as macrophage-polarizing agents. The table below summarizes key compounds, their original indications, and their newly identified effects on macrophage biology.
Table 1: FDA-Approved Drugs with Macrophage-Modulating Effects
| Drug Name | Original Indication | Macrophage Effect | Primary Mechanism | Key Experimental Findings |
|---|---|---|---|---|
| Thiothixene [55] | Antipsychotic | Pro-efferocytic; Enhances continual clearance of apoptotic cells | Dopamine receptor antagonism; ↑ Stra6L → ↑ Arginase 1 | • 100% increase in efferocytosis of apoptotic cells [55]• Enhanced clearance of lipid-laden foam cells [55] |
| Fluoxetine [56] | Antidepressant (SSRI) | Inhibits CCL17 production; Ameliorates arthritic pain | Inhibits GM-CSF-induced STAT5 phosphorylation & IRF4 expression | • 75% inhibition of CCL17 in human monocytes [56]• Significant pain reduction in zymosan-induced arthritis [56] |
| Ponesimod [56] | Multiple Sclerosis | Inhibits CCL17 production; Ameliorates arthritic pain | Inhibits GM-CSF-induced STAT5 phosphorylation & IRF4 expression | • Selective CCL17 inhibition without affecting CCL22 [56]• Reduced pain in inflammatory arthritis model [56] |
| Terbutaline [56] | Asthma (β-agonist) | Inhibits CCL17 production; Ameliorates arthritic pain | Inhibits GM-CSF-induced STAT5 phosphorylation & IRF4 expression | • Maintained CCL22 expression while inhibiting CCL17 [56]• Therapeutic efficacy in inflammatory arthritis [56] |
| Ractopamine [56] | Veterinary (lean meat promotion) | Inhibits CCL17 production; Ameliorates arthritic pain | Inhibits GM-CSF-induced STAT5 phosphorylation & IRF4 expression | • Potent inhibition of CCL17 in human and mouse cells [56]• Reduced arthritic pain in vivo [56] |
| MEK Inhibitors (e.g., Mirdametinib) [6] [58] | Neurofibromatosis | Selective blockade of M2 polarization | Inhibits MEK/ERK → PPARγ → Retinoic Acid signaling | • Selective inhibition of M2 but not M1 polarization [6]• Blocked M2-driven angiogenesis in disease models [6] |
| HDAC Inhibitors [6] | Various (e.g., oncology) | Selective blockade of M2 polarization | Epigenetic modulation of polarization genes | • Selective inhibition of M2 polarization [6]• Suppressed pathologic angiogenesis [6] |
| Gamifant (Emapalumab-lzsg) [59] [60] | HLH/Macrophage Activation Syndrome | Blocks IFNγ-driven hyperinflammation | Monoclonal antibody neutralizing IFNγ | • 54% complete response rate in MAS at Week 8 [60]• 82% achieved clinical MAS remission [60] |
Quantitative Assessment of Drug Effects
Rigorous in vitro and in vivo models are essential for quantifying the macrophage-modulating effects of repurposed drugs. The following table presents key quantitative findings from recent studies.
Table 2: Quantitative Effects of Macrophage-Modulating Drugs
| Drug Name | Experimental Model | Key Metric | Result | Citation |
|---|---|---|---|---|
| Thiothixene | RAW macrophage-apoptotic cell co-culture | Efferocytosis increase | >100% vs. vehicle control | [55] |
| Thiothixene | Mouse BMDMs, human PBMCs | Continual efferocytosis | Enhanced via Stra6L-Arginase 1 axis | [55] |
| Fluoxetine | Human monocytes (GM-CSF stimulated) | CCL17 inhibition | 75% reduction at 10µM | [56] |
| Fluoxetine | Zymosan-induced arthritis (mouse) | Pain amelioration | Significant reduction vs. control (Days 2-7) | [56] |
| Ponesimod | Human monocytes (GM-CSF stimulated) | CCL17/CCL22 selectivity | Inhibited CCL17 only | [56] |
| MEK Inhibitors | IL-4 polarized macrophages | M2 marker reduction | Selective inhibition of M2 genes | [6] |
| Gamifant | MAS/Still's disease (clinical trial) | Complete response rate | 54% (21/39) at Week 8 | [60] |
| Gamifant | MAS/Still's disease (clinical trial) | Clinical remission | 82% (32/39) at Week 8 | [60] |
Experimental Approaches for Evaluating Macrophage Modulation
High-Throughput Screening Platforms
Screening FDA-approved compound libraries requires robust, quantitative assays capable of handling thousands of compounds. The most common approaches include:
- Flow Cytometry-Based Efferocytosis Assays: Co-culture systems where phagocytes (e.g., RAW macrophages) are labeled with CellTracker Red and apoptotic target cells (e.g., staurosporine-treated) with CellTracker Green. Double-positive cells indicate successful efferocytosis, quantified via high-throughput flow cytometry [55].
- Live-Cell Imaging Phagocytosis Systems: Using pH-sensitive fluorescent dyes in target cells that fluoresce upon internalization into phagolysosomes, enabling real-time kinetic monitoring of efferocytosis (e.g., IncuCyte system) [55].
- Cytokine/Chemokine Secretion Profiling: ELISA-based screening of culture supernatants from drug-treated macrophages stimulated with polarizing cytokines (e.g., GM-CSF for CCL17/CCL22 production) [56].
Validation in Primary Cells and Disease Models
Initial hits from cell-line screens require validation in physiologically relevant systems:
- Primary Macrophage Cultures: Testing candidate drugs in bone marrow-derived macrophages (BMDMs) from mice and human peripheral blood mononuclear cell (PBMC)-derived macrophages confirms effects across species and in non-immortalized cells [55] [56].
- Viability and Apoptosis Assays: Critical counter-screens to ensure pro-phagocytic effects aren't secondary to increased target cell apoptosis. Annexin V staining and MTT assays at various timepoints (e.g., 4h, 12h) and doses exclude cytotoxic artifacts [55].
- Disease-Specific Models: In vivo validation in models such as zymosan-induced arthritis (for inflammatory pain), murine models of atherosclerosis (for foam cell clearance), or laser-induced choroidal neovascularization (for M2-driven pathology) [6] [56].
Mechanism of Action Studies
Elucidating the molecular pathways underlying drug effects involves:
- Phosphoproteomics and Kinase Enrichment Analysis: Global quantitative time-course phosphoproteomics can identify kinase activation patterns unique to M1 vs. M2 polarization and reveal drug targets [6].
- Western Blotting for Signaling Intermediates: Validating effects on specific pathways (e.g., STAT5 phosphorylation, IRF4 expression for CCL17 inhibitors; Stra6L induction for thiothixene) [55] [56].
- Metabolic Profiling: Assessing shifts in metabolic pathways (e.g., oxidative phosphorylation vs. glycolysis) using Seahorse analyzers or metabolomics, given the tight link between metabolism and polarization [6].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Macrophage Polarization and Efferocytosis Studies
| Reagent/Cell Type | Function/Application | Specific Examples |
|---|---|---|
| Polarizing Cytokines | Directing macrophage polarization in vitro | IFN-γ + LPS (M1); IL-4/IL-13 (M2) [6] [20] |
| Immortalized Macrophage Lines | High-throughput screening | RAW 264.7 cells (mouse); THP-1-derived macrophages (human) [55] [6] |
| Primary Macrophages | Physiologically relevant validation | Bone marrow-derived macrophages (BMDMs); Human PBMC-derived macrophages [55] [56] |
| Apoptotic Target Cells | Efferocytosis assays | Staurosporine-treated RAW cells; OxLDL-loaded macrophages [55] |
| Fluorescent Cell Trackers | Phagocyte/target discrimination in co-culture | CellTracker Red CMTPX (phagocytes); CellTracker Green CMFDA (targets) [55] |
| pH-Sensitive Dyes | Live-cell imaging of phagocytosis | Dyes that fluoresce upon phagolysosome acidification (IncuCyte system) [55] |
| Polarization Marker Antibodies | Phenotype validation via flow cytometry/IF | iNOS, CD80, CD86 (M1); Arg1, CD206, CD163 (M2) [1] [20] |
| Leucomycin A5 | Leucomycin A5, CAS:18361-45-0, MF:C39H65NO14, MW:771.9 g/mol | Chemical Reagent |
| Leucomyosuppressin | Leucomyosuppressin, CAS:106884-19-9, MF:C59H84N16O15, MW:1257.4 g/mol | Chemical Reagent |
Repurposing FDA-approved drugs for macrophage modulation presents a promising strategy for rapidly developing new therapies for chronic inflammatory diseases. The compounds highlighted herein—including thiothixene for enhancing efferocytosis, fluoxetine and related drugs for selective chemokine inhibition, and MEK/HDAC inhibitors for altering polarization balance—demonstrate the feasibility of this approach. Their known human safety profiles potentially accelerate translational pathways.
Future efforts should focus on developing more targeted delivery systems to minimize off-target effects, exploring combination therapies that simultaneously address multiple facets of macrophage dysregulation, and validating repurposing candidates in advanced human disease models. As our understanding of macrophage biology deepens, particularly through omics technologies, the rational repurposing of existing drugs will continue to offer efficient pathways to novel immunomodulatory therapies.
Gene Therapy and Biomaterial-Based Strategies for Precise Phenotype Control
The precise control of macrophage polarization represents a frontier in the treatment of chronic inflammatory diseases. Macrophages, as highly plastic immune cells, can adopt a spectrum of functional phenotypes, broadly categorized as pro-inflammatory (M1) or anti-inflammatory (M2) [11]. In chronic inflammatory conditions—including rheumatoid arthritis, atherosclerosis, intervertebral disc degeneration, and impaired bone healing—a persistent dominance of M1 macrophages perpetuates inflammation and tissue destruction, while preventing the M2-mediated resolution phase essential for tissue repair [61] [53] [14]. This imbalance has spurred the development of advanced therapeutic strategies aimed at reprogramming macrophage phenotypes. The convergence of gene editing technologies, particularly CRISPR/Cas9, with sophisticated biomaterial delivery systems now enables unprecedented precision in modulating the underlying genetic programs that govern macrophage polarization, offering new hope for treating previously intractable chronic diseases [62] [63].
Macrophage Polarization in Chronic Inflammation
The Polarization Spectrum and Its Regulatory Mechanisms
Macrophages exist on a continuum of activation states, classically divided into M1 and M2 phenotypes, each with distinct functions and secretory profiles. M1 macrophages, activated by stimuli such as IFN-γ and LPS, are characterized by high production of pro-inflammatory cytokines (e.g., TNF-α, IL-1β, IL-6, IL-12) and expression of surface markers like CD80, CD86, and iNOS. They are potent effectors in pathogen clearance and exhibit anti-tumor activity [11] [53] [14]. In contrast, M2 macrophages, induced by IL-4, IL-13, or IL-10, display an anti-inflammatory, pro-reparative profile, secreting factors like IL-10, TGF-β, and VEGF, and expressing markers such as CD206, CD163, and Arginase-1 [64] [53] [14]. The M2 category encompasses several subtypes (M2a, M2b, M2c, M2d) with nuanced functions in tissue repair, immunoregulation, and angiogenesis [53] [14].
The polarization process is governed by intricate signaling networks and molecular regulators. Key pathways include JAK-STAT, NF-κB, and IRF signaling [11]. For instance, STAT1 activation promotes M1 polarization, while STAT3 and STAT6 activation drives M2 polarization [11]. Furthermore, epigenetic modifications, transcription factors, and microRNAs (e.g., miR-155 promoting M1 and let-7c favoring M2) fine-tune the polarization process [11].
Table 1: Macrophage Polarization Phenotypes, Markers, and Functions
| Phenotype | Inducing Stimuli | Key Surface Markers | Secreted Factors | Primary Functions |
|---|---|---|---|---|
| M1 | IFN-γ, LPS | CD80, CD86, iNOS | TNF-α, IL-1β, IL-6, IL-12, IL-23 | Pro-inflammatory response, pathogen clearance, anti-tumor activity [53] [14] |
| M2a | IL-4, IL-13 | CD206, ARG1 | IL-10, TGF-α | Tissue repair, anti-inflammation, fibrosis [53] [14] |
| M2b | Immune complexes, TLR ligands | CD86 | IL-1, IL-6, IL-10 | Immunoregulation [53] [14] |
| M2c | IL-10, Glucocorticoids | CD163 | IL-10, TGF-β | Phagocytosis, immunoregulation, matrix remodeling [53] [14] |
| M2d | Adenosine, TLR ligands | CD206, CD163, TIE2 | IL-10, VEGF | Angiogenesis, tumor progression [53] [14] |
Consequences of Polarization Imbalance in Disease
In chronic inflammatory diseases, the failure to transition from an M1-dominant to an M2-dominant state underlies pathological progression. In rheumatoid arthritis, a high M1/M2 ratio in synovial tissue perpetuates inflammation through the production of TNF-α and IL-6, leading to joint destruction [14]. Similarly, in chronic bone infections like osteomyelitis, persistent M1 polarization prevents the transition to M2 macrophages required for successful bone regeneration, creating a state of impaired healing and bone resorption [61]. In intervertebral disc degeneration, M1 macrophages exacerbate tissue breakdown by amplifying inflammatory cytokines that promote cellular senescence and extracellular matrix degradation [53]. The common theme across these conditions is that the chronic inflammatory microenvironment is locked in a pathological state, necessitating therapeutic intervention to reprogram the local immune response.
Biomaterial Platforms for Immunomodulation
Biomaterials, particularly hydrogels, have emerged as powerful tools for creating a favorable immunomodulatory microenvironment. They can be engineered to deliver bioactive factors in a spatiotemporally controlled manner, directly influencing macrophage polarization [61] [65].
Design Principles and Physical Cues
The physical properties of biomaterials themselves can significantly modulate macrophage phenotype. Stiffness, topography, pore architecture, and hydrophilicity are key design parameters [65]. For example, hydrogels with bone-mimetic stiffness have been shown to promote a more M2-like phenotype, supporting regenerative outcomes [65]. Biomaterials can also be designed as "instructive" scaffolds that not only deliver cargo but also actively engage with and reshape the host immune response through their intrinsic physical and chemical characteristics [61] [65].
Delivery of Bioactive Cargo
Immunomodulatory hydrogels are engineered to incorporate and release a variety of bioactive molecules to steer macrophage polarization:
- Cytokines and Small Molecules: Sustained local release of IL-4 or IL-10 can promote M2 polarization, while inhibitors of pro-inflammatory signaling pathways can suppress M1 phenotypes [61] [53].
- Antimicrobial Agents: In infected environments, such as osteomyelitis, hydrogels can co-deliver antibiotics or antimicrobial nanoparticles to eliminate pathogens, thereby removing the M1-polarizing stimulus and facilitating the switch to M2 [61].
- Sequential Release Systems: Advanced hydrogel designs incorporate sequential release profiles, first delivering antimicrobials to control infection and then releasing pro-regenerative cytokines to promote M2 polarization and tissue repair [61].
Table 2: Biomaterial Strategies for Controlling Macrophage Polarization
| Strategy | Mechanism of Action | Example Applications | Key Advantages |
|---|---|---|---|
| Cytokine Delivery | Sustained local release of IL-4, IL-13, or IL-10 to drive M2 polarization [61] [53] | Bone regeneration, IVDD, wound healing | Direct phenotypic control, high bioactivity |
| Physical Cue Engineering | Tuning scaffold stiffness, topography, and porosity to guide macrophage polarization [65] | Bone tissue engineering, implant integration | Passive, non-pharmacologic modulation, synergistic with tissue engineering |
| Sequential Drug Release | Initial release of antimicrobials, followed by pro-regenerative immunomodulators [61] | Osteomyelitis, infected wound healing | Addresses multiple disease phases (infection control then regeneration) |
| ROS-Scavenging Mechanisms | Incorporation of antioxidants to neutralize reactive oxygen species and reduce M1 inflammation [61] | Chronic inflammatory conditions (RA, atherosclerosis) | Breaks cycle of oxidative stress-driven inflammation |
| Cell Delivery Platforms | Delivery of M2-polarized macrophages or progenitor cells [61] | Tissue regeneration, immunomodulation | Living system with potential for adaptive response |
Gene Editing Strategies for Phenotype Control
CRISPR/Cas9 technology offers a precise and permanent method for altering the genetic programs that control macrophage polarization, moving beyond transient pharmacological modulation.
CRISPR/Cas9 System Fundamentals
The CRISPR/Cas9 system consists of two core components: the Cas9 enzyme, which acts as a "molecular scissor" to create double-strand breaks in DNA, and a guide RNA (gRNA) that directs Cas9 to a specific genomic sequence [62]. Once the DNA is cut, the cell's repair mechanisms—either Non-Homologous End Joining (NHEJ) or Homology-Directed Repair (HDR)—can be harnessed to knock out genes or insert new genetic material [62]. This allows researchers to directly target key transcription factors, signaling molecules, or epigenetic regulators involved in macrophage polarization.
Delivery Technologies for Macrophages
Efficient and safe delivery of CRISPR/Cas9 components to target cells is a critical challenge. The main delivery strategies are compared below:
Table 3: CRISPR/Cas9 Delivery Technologies for Macrophage Targeting
| Delivery Method | Mechanism | Therapeutic Payload | Advantages | Limitations |
|---|---|---|---|---|
| Viral Vectors | Engineered viruses (e.g., lentiviruses, AAV) infect cells and deliver genetic material encoding Cas9 and gRNA [62] [66] | Plasmid DNA | High transduction efficiency, stable expression | Immunogenicity, limited packaging capacity, potential insertional mutagenesis [62] |
| Non-Viral Vectors | Synthetic nanoparticles (e.g., lipid nanoparticles, polymers) encapsulate and protect CRISPR components for cellular uptake [62] [66] | Cas9 protein, mRNA, or ribonucleoprotein (RNP) | Improved safety, large payload capacity, tunable surface chemistry [62] | Generally lower efficiency than viral vectors, potential cytotoxicity |
| Biomaterial-Mediated Delivery | Biomaterial scaffolds (e.g., hydrogels) provide localized, sustained release of CRISPR components at the target site [62] | Cas9 RNP, mRNA | Localized delivery reduces off-target effects, provides a supportive niche for tissue regeneration [61] [62] | Primarily for localized diseases, complex fabrication |
Therapeutic Gene Targets for Polarization Control
Gene editing strategies can be designed to promote M2 polarization or suppress M1 polarization by targeting key nodes in polarization pathways:
- Knock-out of M1-Associated Genes: Targeting genes like NF-κB or STAT1 can reduce the macrophage's capacity for M1 polarization, diminishing the pro-inflammatory response [11] [14].
- Knock-in of M2-Associated Genes: Using HDR with a donor template, genes encoding for M2-promoting factors like IL-10 or Arginae-1 can be inserted into safe genomic harbors, enabling sustained expression of anti-inflammatory mediators [53].
- Epigenetic Modulators: Editing genes encoding epigenetic enzymes like DNMT1, which is involved in silencing M2-associated genes, can create a more permissive state for M2 polarization [11].
Experimental Protocols for Preclinical Research
Protocol 1: Polarizing and Validating Human iPSC-Derived Macrophages
This protocol, adapted from quantitative proteomics studies, provides a reproducible platform for generating human macrophages for polarization studies [67].
Differentiation of iPSCs to Macrophages (iPSDM):
- Culture human iPSCs (e.g., Wibj2 line) in mTESR medium.
- Form embryoid bodies (EBs) by seeding 1x10^4 cells/well in a 96-well V-bottom plate in mTESR supplemented with SCF (20 ng/mL), VEGF (50 ng/mL), BMP4 (50 ng/mL), and Y-27632 (10 µM). Centrifuge at 300× g for 5 min.
- On day 4, harvest EBs and seed onto 0.1% gelatin-coated plates in X-VIVO15 medium containing IL-3 (25 ng/mL) and M-CSF (100 ng/mL). Refresh medium every 3-4 days.
- From day 21 onwards, harvest suspension monocyte-like cells from the supernatant every 3-4 days.
- Differentiate the monocytes into macrophages (iPSDM) by culture in X-VIVO15 with M-CSF (100 ng/mL) for 7 days in non-tissue culture treated plates [67].
Macrophage Polarization:
- M1 Polarization: Stimulate iPSDM (1x10^6 cells/well) with IFN-γ (50 ng/mL) + LPS (10 ng/mL) for 24-48 hours.
- M2 Polarization: Stimulate iPSDM with IL-4 (20 ng/mL) for 24-48 hours [67].
Phenotypic Validation by Flow Cytometry:
- Harvest cells using PBS containing 2 mM EDTA.
- Stain with viability dye (e.g., Zombie Aqua) for 30 min at 4°C.
- Block Fc receptors using human Fc block.
- Stain with antibody panels for 30 min at 4°C.
- M1 Marker Panel: CD80, CD86, CD197 (CCR7).
- M2 Marker Panel: CD206, CD163, CD209.
- Analyze using a flow cytometer (e.g., BD FACSCanto II) and software (e.g., FlowJo) [67] [64].
Protocol 2: Assessing Macrophage-Mediated Effects on Target Cells
To model the impact of polarized macrophages on tissue health, co-culture systems or conditioned media experiments are used.
Conditioned Media (CM) Collection:
- Polarize iPSDM or primary human monocyte-derived macrophages as described above.
- After polarization, wash cells twice with PBS and replace media with serum-free basal medium (e.g., RPMI without phenol red) for 14-24 hours.
- Collect supernatant, centrifuge, and filter through a 0.45 µm filter to remove cell debris. Concentrate if necessary using centrifugal filters. This is the conditioned media (M1-CM or M2-CM) [67] [53].
Treatment of Target Cells:
- Culture target cells relevant to the disease model (e.g., Nucleus Pulposus Cells for IVDD, osteoblasts for bone regeneration, annulus fibrosus cells) in standard conditions.
- Treat target cells with the collected CM (e.g., 50% CM mixed with 50% fresh medium) for 24-72 hours.
- Include a control group treated with CM from unstimulated (M0) macrophages [53].
Downstream Analysis:
- Cell Senescence/Apoptosis: Assess using β-galactosidase staining or caspase-3/7 activity assays.
- Gene Expression: Analyze expression of pro-inflammatory genes (IL-6, IL-8, COX-2) and matrix-degrading enzymes (MMPs, ADAMTS) in target cells via qRT-PCR.
- Extracellular Matrix (ECM) Production: Measure levels of key ECM components (e.g., collagen type II, aggrecan) using immunofluorescence or ELISA [53].
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Reagents for Macrophage Polarization and Analysis
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Polarization Cytokines | Recombinant Human IFN-γ, LPS, IL-4, IL-13, IL-10 | To induce and study classical (M1) and alternative (M2) macrophage polarization in vitro [67] [53] |
| Flow Cytometry Antibodies | Anti-human CD80, CD86, CD206 (MRC1), CD163, CD14, CCR7 | Identification and quantification of macrophage surface polarization markers [67] [64] |
| Cell Culture Media & Supplements | X-VIVO15 Serum-Free Medium, M-CSF, Penicillin-Streptomycin, GlutaMAX | Maintenance and differentiation of monocytes into macrophages [67] |
| Key Assay Kits | NO (Nitric Oxide) Detection Kit, Arginae Activity Assay Kit, ELISA kits for TNF-α, IL-1β, IL-6, IL-10, IL-12 | Functional assessment of polarized macrophage activity and cytokine secretion profiles [53] [14] |
| CRISPR/Cas9 Components | Cas9 Nuclease (protein/mRNA), sgRNAs targeting NFKB1, STAT1, STAT6 | Genetic manipulation of polarization pathways via gene knockout or knock-in [62] [66] |
| Leupeptin | Leupeptin | Leupeptin is a reversible, broad-spectrum inhibitor of serine, cysteine, and threonine proteases. For Research Use Only. Not for human or animal use. |
| Levamlodipine | Levamlodipine, CAS:103129-82-4, MF:C20H25ClN2O5, MW:408.9 g/mol | Chemical Reagent |
Signaling Pathways and Experimental Workflows
Signaling Pathways in Macrophage Polarization
The following diagram summarizes the core signaling pathways and molecular regulators involved in macrophage polarization, illustrating potential targets for gene therapy.
Diagram Title: Core Macrophage Polarization Signaling Pathways
Biomaterial-Mediated Gene Delivery Workflow
This workflow outlines the key steps in developing and testing a biomaterial-based strategy for delivering gene therapies to control macrophage phenotype.
Diagram Title: Biomaterial-Based Therapy Development Workflow
The integration of advanced biomaterial platforms with precise gene editing technologies represents a paradigm shift in our ability to control macrophage polarization for therapeutic purposes. By moving beyond broad-acting anti-inflammatory drugs to targeted interventions that reshape the local immune microenvironment, these strategies hold immense potential for treating a wide range of chronic inflammatory diseases. The future of this field lies in developing ever more sophisticated delivery systems that can respond to dynamic changes in the disease state, providing sequential and conditional release of therapeutic agents. Furthermore, combining macrophage-targeted therapies with other treatment modalities will likely yield synergistic effects, ultimately enabling the restoration of tissue homeostasis and functional regeneration in conditions where current treatments fall short.
Macrophages are innate immune cells of remarkable plasticity, capable of dynamically polarizing into distinct functional phenotypes in response to microenvironmental cues. This polarization represents a critical mechanism in the pathogenesis and progression of chronic inflammatory diseases [68]. At the extremes of the polarization spectrum are the pro-inflammatory, classically activated (M1) macrophages and the anti-inflammatory, alternatively activated (M2) macrophages, though in vivo states represent a continuum with significant heterogeneity [9]. The balance between these polarization states is governed by complex signaling networks and transcriptional regulators that determine macrophage function in tissue homeostasis, immune defense, and disease pathology [68]. This technical guide examines the mechanisms of macrophage polarization within three major disease contexts, providing researchers with quantitative data, experimental methodologies, and visualization tools to advance therapeutic development.
Macrophage Polarization in Cancer Immunotherapy
Polarization States and Their Roles in the Tumor Microenvironment
Within the tumor microenvironment (TME), tumor-associated macrophages (TAMs) constitute a major component and play paradoxical roles based on their polarization state. M1 macrophages typically exert anti-tumoral effects through pro-inflammatory cytokine production and direct tumor cell killing, while M2-like TAMs generally promote tumor progression, angiogenesis, immunosuppression, and metastasis [69] [68]. This functional dichotomy makes macrophage polarization a promising therapeutic target.
Table 1: Characteristics of Macrophage Polarization States in Cancer
| Parameter | M1 (Anti-tumoral) | M2 (Pro-tumoral) |
|---|---|---|
| Primary Inducers | IFN-γ, LPS, GM-CSF [9] | IL-4, IL-13, IL-10, IL-33, TGF-β [9] |
| Key Surface Markers | CD80, CD86, TLR2, TLR4, MHC II [9] | CD206, CD163, CD209 [9] |
| Characteristic Cytokines/Chemokines | IL-12, IL-1β, IL-6, TNF-α, CCL2, CCL5 [9] | IL-10, TGF-β, CCL17, CCL18, CCL22, CCL24 [68] [9] |
| Metabolic Profile | Glycolysis [68] | Oxidative Phosphorylation [68] |
| Transcription Factors | STAT1, STAT5, IRF3, IRF5, NF-κB [9] | STAT6, IRF4, JMJD3, PPARδ, PPARγ [9] |
| Therapeutic Targeting Approach | Promote M1 polarization via PKM2 inhibition [70] | Inhibit M2 polarization; CAR-M therapies [69] |
Key Signaling Pathways and Molecular Targets
The pyruvate kinase M2 (PKM2) isoform has emerged as a critical regulator of macrophage polarization in cancer. PKM2 translocates to the nucleus and interacts with hypoxia-inducible factor-1α (HIF-1α) to promote glycolysis and M1 polarization [70]. In hepatocellular carcinoma, Follistatin-like 1 (FSTL1) binding to PKM2 promotes M1 polarization, attenuating liver inflammation and fibrosis [68]. The JAK-STAT signaling pathway represents another fundamental regulatory axis, with STAT1 driving M1 polarization while STAT6 promotes M2 polarization [9].
Figure 1: Signaling Pathways in Macrophage Polarization
Experimental Protocol: In Vitro Polarization of Human iPSC-Derived Macrophages
Objective: Generate and characterize M1 and M2 polarized macrophages from human induced pluripotent stem cells (iPSCs) for cancer immunotherapy research [67].
Materials and Methods:
iPSC Culture and Embryoid Body Formation: Maintain Wibj2 iPSC line in mTESR medium. On day 0, seed 1×10^4 cells per well in a 96-well Ultralow attachment V-bottom plate in mTESR medium supplemented with SCF (20 ng/mL), VEGF (50 ng/mL), BMP4 (50 ng/mL), and Y-27632 (10 µM). Centrifuge plate at 300× g for 5 min at room temperature to form embryoid bodies (EBs) [67].
Monocyte Lineage Differentiation: On day 4, harvest EBs and seed at 10-15 EBs per well in 0.1% gelatin-coated 6-well plates. Culture in X-VIVO15 medium supplemented with IL-3 (25 ng/mL) and M-CSF (100 ng/mL). Change medium every 3-4 days. After 21 days, harvest monocyte-like suspension cells from the supernatant every 3-4 days [67].
Macrophage Differentiation: Differentiate harvested monocytes into macrophages (iPSDM) in X-VIVO15 medium supplemented with M-CSF (100 ng/mL) for 7 days in non-tissue culture treated plates [67].
Polarization Protocol: Polarize iPSDM (1×10^6 cells per well) for 24-48 hours with:
- M1 polarization: IFN-γ (50 ng/mL) + LPS (10 ng/mL)
- M2 polarization: IL-4 (20 ng/mL) [67]
Validation and Analysis:
- Flow Cytometry: Analyze surface markers using antibodies against CD80, CD86, CD206, CD163.
- Proteomic Analysis: Process cell lysates using SP3 protocol. Lyse cells in buffer containing 4% SDS, 10 mM TCEP, and 50 mM TEAB. Determine protein concentrations using MicroBCA assay [67].
- Secretome Analysis: Culture polarized macrophages in serum-free RPMI without phenol red for 14 hours. Collect supernatants, pass through 0.45 µm filters, and concentrate 10x using Amicon centrifugal filters [67].
- Phagocytosis Assay: Incubate macrophages with FITC-conjugated Zymosan A particles (5 particles per cell) at 37°C for 1 hour. Analyze uptake by flow cytometry after adding trypan blue to quench extracellular fluorescence [67].
Macrophage Polarization in Autoimmune Diseases
Dysregulated Polarization in Systemic Autoimmunity
In autoimmune diseases including systemic lupus erythematosus (SLE), rheumatoid arthritis (RA), and systemic sclerosis (SSc), aberrant macrophage polarization contributes to loss of self-tolerance and chronic inflammation. M1 macrophages dominate inflammatory lesions, producing pro-inflammatory cytokines that drive tissue damage, while impaired M2 functions disrupt resolution phases and tissue repair [71].
Table 2: Macrophage Dysregulation in Autoimmune Diseases
| Disease | Macrophage Abnormalities | Key Mechanisms | Clinical Consequences |
|---|---|---|---|
| Systemic Lupus Erythematosus (SLE) | Increased glomerular macrophages; Defective efferocytosis [71] | Accumulation of uncleared apoptotic cells; Increased type I IFNs; FcγR-mediated uptake of immune complexes [71] | Glomerulonephritis; Autoantigen exposure; Chronic inflammation |
| Rheumatoid Arthritis (RA) | M1 polarization in synovium; Osteoclast differentiation [71] | TLR activation by DAMPs; RANKL-mediated signaling; Pro-inflammatory cytokine production [71] | Joint destruction; Pannus formation; Bone erosion |
| Systemic Sclerosis (SSc) | Monocyte recruitment; M2a profibrotic polarization [71] | CCL2 and CCL24-mediated recruitment; IL-4/IL-13 STAT6 signaling; TGF-β production [71] | Tissue fibrosis; Vascular damage; Organ dysfunction |
| Type 1 Diabetes (T1D) | Islet-infiltrating macrophages; Altered antigen presentation [71] | β-cell antigen presentation to T cells; ROS and cytokine production [71] | β-cell destruction; Insulin deficiency |
Experimental Protocol: Assessing Phagocytic Function in Autoimmunity
Objective: Evaluate efferocytosis (apoptotic cell clearance) dysfunction in autoimmune models, a key feature of SLE pathogenesis [71].
Methods:
Induction of Apoptosis: Induce apoptosis in Jurkat T-cells or thymocytes using UV irradiation (254 nm, 100-200 mJ/cm²) or staurosporine (1 µM, 4-6 hours). Confirm apoptosis by Annexin V/PI staining with >70% Annexin V+ cells required.
Macrophage-Monocyte Co-culture: Isolate CD14+ monocytes from human PBMCs using magnetic bead separation. Differentiate to macrophages with M-CSF (100 ng/mL, 7 days). Plate macrophages in 24-well plates (2×10^5 cells/well).
Efferocytosis Assay: Label apoptotic cells with pHrodo Green or Red dye (1 µM, 30 min). Add labeled apoptotic cells to macrophages at 5:1 ratio. Incubate for 1-2 hours at 37°C.
Quantification:
- Flow Cytometry: Analyze macrophage fluorescence. Calculate efferocytosis index as (% pHrodo+ macrophages) × (mean fluorescence intensity).
- Immunofluorescence: Fix cells, stain with DAPI and phalloidin. Count ingested apoptotic cells per macrophage microscopically.
Inhibition Studies: Pre-treat macrophages with inhibitors targeting potential therapeutic pathways: TLR inhibitors (TAK-242 for TLR4), ROS scavengers (N-acetylcysteine), or LXR/PPARγ agonists to enhance efferocytosis.
Figure 2: Macrophage Dysregulation in Autoimmunity
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Macrophage Polarization Research
| Reagent Category | Specific Examples | Research Application | Technical Notes |
|---|---|---|---|
| Polarization Cytokines | IFN-γ (50 ng/mL), LPS (10 ng/mL), IL-4 (20 ng/mL), IL-13 (20 ng/mL) [67] [9] | Directing macrophage polarization in vitro | Use endotoxin-free preparations; Optimize concentrations for specific cell systems |
| Cell Culture Media | X-VIVO15 Serum-free Medium, RPMI 1640 [67] | iPSC-derived macrophage differentiation and polarization | Serum-free conditions preferred for secretome studies |
| Growth Factors | M-CSF (100 ng/mL), GM-CSF (varies) [67] | Monocyte to macrophage differentiation | M-CSF generates more M2-like baselines; GM-CSF promotes M1-like baselines |
| Flow Cytometry Antibodies | CD80, CD86, MHC II (M1); CD206, CD163, CD209 (M2) [67] [9] | Phenotypic validation of polarization states | Include appropriate isotype controls; Use Fc receptor block before staining |
| Metabolic Probes | 2-NBDG (glucose uptake), MitoTracker (mitochondrial mass), Seahorse Assay Kits [68] | Assessing metabolic reprogramming | Glycolysis vs. oxidative phosphorylation distinguishes M1 vs. M2 |
| Signaling Inhibitors | STAT1 inhibitors (Fludarabine); STAT6 inhibitors (AS1517499); PKM2 inhibitors | Mechanistic studies of polarization pathways | Validate specificity with phospho-flow cytometry |
| iPSC Differentiation Reagents | BMP4, VEGF, SCF, IL-3, Y-27632 (ROCK inhibitor) [67] | Generating genetically defined human macrophages | Protocol adapted from Wilgenburg et al. and Lopez-Yrigoyen et al. [67] |
| Levamlodipine hydrobromide | Levamlodipine hydrobromide, CAS:865430-78-0, MF:C20H26BrClN2O5, MW:489.8 g/mol | Chemical Reagent | Bench Chemicals |
| Liproxstatin-1 | Liproxstatin-1, MF:C19H21ClN4, MW:340.8 g/mol | Chemical Reagent | Bench Chemicals |
Targeting Macrophage Polarization in Disease
Therapeutic strategies leveraging macrophage polarization are advancing rapidly, particularly in cancer immunotherapy. Chimeric antigen receptor macrophages (CAR-M) represent a breakthrough approach, engineering macrophages to recognize and phagocytose tumor cells [69]. Similarly, targeting phagocytosis checkpoints like the CD47-SIRPα axis can enhance macrophage-mediated tumor cell clearance [69]. In autoimmune diseases, strategies to inhibit monocyte recruitment via CCL2/CCL24 blockade show promise in limiting macrophage-mediated tissue damage [71]. Metabolic reprogramming through PKM2 modulation offers another avenue for controlling macrophage polarization across disease contexts [70] [68].
Future Directions and Integrative Analysis
The complexity of macrophage biology necessitates sophisticated research approaches that account for tissue-specific heterogeneity, plasticity, and origin differences between tissue-resident and monocyte-derived macrophages [68] [9]. Single-cell technologies and fate-mapping models are revealing unprecedented diversity within macrophage populations, moving beyond the traditional M1/M2 dichotomy [68] [9]. Future therapeutic development will require precision targeting of specific disease-relevant macrophage subsets while preserving homeostatic functions. The integrated analysis of signaling networks, metabolic programs, and polarization states across cancer, autoimmunity, and metabolic diseases provides a robust foundation for macrophage-targeted therapies that can be tailored to specific disease contexts and patient profiles.
Navigating Challenges in Macrophage Polarization Research: Technical Hurdles and Therapeutic Roadblocks
The therapeutic targeting of macrophage polarization represents a paradigm shift in managing chronic inflammatory diseases and cancer. However, the clinical translation of promising therapeutic compounds is severely hampered by inherent pharmacological challenges, including poor aqueous solubility, low permeability, chemical instability, and rapid systemic clearance, which collectively diminish bioavailability and therapeutic efficacy [72]. These limitations are particularly problematic for modulating macrophage function, as it requires precise delivery to specific tissue microenvironments and intracellular targets.
Emerging nanoscale platforms provide innovative solutions to these persistent delivery problems. Nanoformulations and engineered exosomes have demonstrated remarkable capabilities to protect bioactive cargo from degradation, enhance absorption across biological barriers, and facilitate targeted delivery to macrophages through inherent tropism and surface modifications [73] [74] [72]. This technical review examines these advanced delivery systems within the context of macrophage polarization biology, providing researchers with experimental frameworks and practical resources for developing next-generation immunomodulatory therapies.
Macrophage Polarization: Signaling Pathways and Metabolic Reprogramming
Binary Polarization States and Functional Roles
Macrophages display remarkable functional plasticity in response to microenvironmental cues, dynamically polarizing into distinct phenotypes traditionally categorized as pro-inflammatory M1 or anti-inflammatory M2 states [68] [1]. This binary classification, while simplified, provides a valuable framework for understanding macrophage contributions to chronic inflammation:
- M1 Macrophages: Polarized by Th1 cytokines (IFN-γ, TNF-α) and microbial products (LPS) through signaling pathways including NF-κB, JAK-STAT1, and MAPK [68] [1]. They exhibit a glycolytic metabolic phenotype [29], produce pro-inflammatory cytokines (IL-1β, IL-6, IL-12, TNF-α), generate reactive oxygen and nitrogen species, and contribute to pathogen clearance and tissue destruction [68] [75].
- M2 Macrophages: Activated by Th2 cytokines (IL-4, IL-13, IL-10) primarily through the JAK-STAT6 pathway with contributions from IRF4 and PPARγ [68] [1]. They primarily utilize oxidative phosphorylation [68] and perform immunoregulatory functions including tissue repair, angiogenesis, and resolution of inflammation [68] [75]. The M2 category encompasses functionally distinct subtypes (M2a, M2b, M2c, M2d) with specialized roles [75].
The imbalance between M1 and M2 populations drives pathogenesis across numerous chronic diseases, including rheumatoid arthritis, atherosclerosis, obesity-related metabolic dysfunction, and cancer [75]. This understanding has positioned macrophage polarization as a compelling therapeutic target.
Signaling Pathway Visualization
The following diagram illustrates the core signaling pathways and metabolic reprogramming associated with M1 and M2 macrophage polarization, integrating key receptors, intracellular signaling cascades, and resulting functional outputs:
Figure 1: Core Signaling Pathways in Macrophage Polarization. M1 polarization (yellow) is triggered by IFN-γ and LPS, activating STAT1, NF-κB, and IRF3 pathways that drive pro-inflammatory gene expression and glycolytic metabolism. M2 polarization (green) is induced by IL-4, IL-13, and IL-10, signaling through STAT6, STAT3, PPARγ, and IRF4 to promote anti-inflammatory gene expression and oxidative metabolism. [68] [1] [29]
Nanoformulation Strategies for Enhanced Bioavailability
Nanocarrier Platforms and Applications
Nanoformulations overcome bioavailability challenges through various mechanisms, including protection of labile compounds, enhanced permeability, and sustained release profiles [72]. The table below summarizes major nanocarrier platforms, their structural components, and applications relevant to macrophage targeting:
Table 1: Nanoformulation Platforms for Bioavailability Enhancement
| Platform | Composition | Key Advantages | Relevant Cargos | Macrophage Targeting Potential |
|---|---|---|---|---|
| Liposomes | Phospholipid bilayers enclosing aqueous core [72] | Biocompatible, encapsulate hydrophilic/hydrophobic drugs, surface modifiable | Polyphenols, anti-inflammatory drugs [72] | Innate phagocytosis; mannose receptor targeting via surface modification |
| Polymeric Nanoparticles | PLGA, chitosan, gelatin [72] | Controlled release, high stability, functionalizable surface | Proteins, nucleic acids, small molecules [72] | Tunable size for phagocytosis; ligand decoration for active targeting |
| Solid Lipid Nanoparticles (SLNs) | Solid lipid matrix [72] | Improved physical stability, avoidance of organic solvents, scale-up feasibility | Lipophilic compounds [72] | Lymphatic uptake following oral administration |
| Niosomes | Non-ionic surfactants [72] | Enhanced chemical stability, lower cost than liposomes | Antioxidants, anti-inflammatories [72] | Similar uptake mechanisms to liposomes |
| Nanoemulsions | Oil-in-water or water-in-oil dispersions [72] | Enhanced solubility and absorption of lipophilic compounds | Curcumin, resveratrol [72] | Mucoadhesive formulations for gut-associated lymphoid tissue uptake |
| Metal Nanoparticles | Gold, silver, iron oxide [72] | Unique optical/magnetic properties, surface plasmon resonance | Diagnostics combined with therapeutics [72] | Innate phagocytosis; magnetic targeting capabilities |
Quantitative Comparison of Nanoformulation Performance
Research studies have quantitatively demonstrated the bioavailability enhancement achieved through nanoformulation. The following table compiles key experimental findings:
Table 2: Experimental Efficacy of Selected Nanoformulations
| Formulation | Cargo | Experimental Model | Key Outcomes | Reference |
|---|---|---|---|---|
| Liposomal Curcumin | Curcumin | In vitro antioxidant assays | Significantly enhanced radical scavenging activity compared to free curcumin | [72] |
| Polyphenol-Loaded Nanoemulsions | Plant polyphenols | Simulated GI digestion | Protection of polyphenols from degradation, sustained release profile | [72] |
| FA-AgNPS | Silver nanoparticles | Rheumatoid arthritis model | Targeted delivery to inflammatory sites, promotion of M1-to-M2 transition | [75] |
| Polymer-based Nanoparticles | Nucleic acids | Cell culture studies | Improved cellular uptake and endosomal escape for intracellular delivery | [72] |
Experimental Protocol: Preparation and Characterization of Liposomal Nanoformulations
Objective: To prepare, characterize, and evaluate liposomal formulations for encapsulation of hydrophobic compounds targeting macrophage polarization.
Materials:
- Lipids: Hydrogenated soybean phosphatidylcholine (HSPC), cholesterol, DSPE-PEG(2000) [72]
- Cargo: Hydrophobic compound of interest (e.g., curcumin, resveratrol) [72]
- Solvents: Chloroform, methanol, ethanol
- Equipment: Rotary evaporator, extruder with polycarbonate membranes, dynamic light scattering instrument, HPLC system
Methodology:
Lipid Film Formation:
- Dissolve HSPC, cholesterol, and DSPE-PEG (70:25:5 molar ratio) in chloroform:methanol (2:1 v/v) in round-bottom flask [72].
- Remove organic solvents using rotary evaporator (40°C, 30 min) to form thin lipid film.
- Maintain under vacuum overnight to ensure complete solvent removal.
Hydration and Encapsulation:
- Hydrate lipid film with PBS (pH 7.4) containing cargo compound (above its aqueous solubility limit) at 60°C for 1 hour with gentle agitation.
- Alternatively, dissolve cargo in organic phase with lipids for higher encapsulation efficiency.
Size Reduction and Homogenization:
- Subject multilamellar vesicles to 5 freeze-thaw cycles (liquid nitrogen/60°C water bath).
- Extrude through polycarbonate membranes (400 nm, 200 nm, 100 nm sequentially) using high-pressure extruder [72].
Purification:
- Separate unencapsulated cargo using Sephadex G-50 size exclusion chromatography or dialysis (MWCO 10 kDa) against PBS for 24 hours.
Characterization:
- Size and Zeta Potential: Analyze by dynamic light scattering (DLS); target size: 100-150 nm for enhanced permeability and retention effect [72].
- Encapsulation Efficiency: Determine by HPLC after disruption of liposomes with 0.1% Triton X-100.
- Morphology: Confirm using transmission electron microscopy with negative staining.
- In Vitro Release: Use dialysis method in PBS (pH 7.4 and 5.5) with sink conditions; sample at predetermined intervals.
Cellular Uptake and Polarization Studies:
- Differentiate THP-1 monocytes to macrophages with PMA (100 nM, 48 hours).
- Treat macrophages with liposomal formulations and assess uptake via flow cytometry.
- Evaluate polarization by measuring M1/M2 surface markers (CD80/CD206) and cytokine secretion profiles.
Engineered Exosomes for Targeted Macrophage Modulation
Native and Engineered Exosome Properties
Exosomes, natural extracellular vesicles (30-150 nm) secreted by most cell types, have emerged as sophisticated drug delivery vehicles due to their inherent biocompatibility, low immunogenicity, and natural targeting capabilities [73] [74]. Their native composition includes transmembrane proteins that facilitate membrane fusion and tissue homing, making them particularly suitable for macrophage-targeted therapy.
Engineering approaches further enhance exosome capabilities:
- Cargo Loading: Passive incubation, electroporation, sonication, extrusion, freeze-thaw cycles for incorporating therapeutic nucleic acids, proteins, or small molecules [73].
- Surface Modification: Genetic engineering of parent cells, chemical conjugation, or membrane fusion to display targeting ligands (peptides, antibodies, aptamers) for precise macrophage receptor targeting [73] [74].
- Hybrid Systems: Combination of synthetic nanoparticles with exosomal membranes to create biomimetic vehicles with enhanced functionality [74].
Experimental Protocol: Engineering Exosomes for Targeted miRNA Delivery
Objective: To engineer exosomes for targeted delivery of polarization-modulating miRNAs to macrophages.
Materials:
- Cell Lines: HEK-293T cells (for exosome production), macrophage cell lines (THP-1, RAW264.7)
- Plasmids: Lamp2b-RVG (rabies virus glycoprotein) fusion construct for neuronal targeting; alternative: Lamp2b-MG1 (macrophage galactose-type lectin targeting peptide) for macrophage-specific targeting [73]
- Reagents: miRNA mimic/inhibitor, transfection reagent, total exosome isolation reagent, PKH67 dye, anti-CD63/CD81 antibodies
Methodology:
Exosome Production:
- Culture HEK-293T cells in exosome-depleted FBS medium.
- Co-transfect with Lamp2b-RVG (or Lamp2b-MG1) plasmid and miRNA mimic/inhibitor using PEI transfection reagent.
- Collect conditioned media after 48 hours.
Exosome Isolation and Purification:
- Centrifuge media at 2,000 × g for 30 minutes to remove cells and debris.
- Concentrate supernatant using 100 kDa molecular weight cut-off filters.
- Purify using size-exclusion chromatography (qEV columns) or density gradient centrifugation [73].
- Validate exosome markers (CD63, CD81, TSG101) by western blot.
Engineered Exosome Characterization:
- Determine particle size and concentration using nanoparticle tracking analysis.
- Confirm surface expression of targeting ligand by flow cytometry.
- Quantify miRNA loading efficiency using RT-qPCR.
Functional Validation:
- Differentiate THP-1 monocytes to macrophages.
- Treat with PKH67-labeled engineered exosomes and assess uptake by confocal microscopy and flow cytometry.
- Evaluate polarization modulation by measuring signature markers:
- M1: CD80, CD86, iNOS, IL-1β, IL-6, TNF-α
- M2: CD206, CD163, Arg1, Ym1, Fizz1, IL-10
The following diagram illustrates the experimental workflow for engineering and evaluating targeted exosomes:
Figure 2: Experimental Workflow for Engineering Targeted Exosomes. The process involves selecting therapeutic miRNAs, genetically engineering parent cells to express targeting ligands, loading miRNAs into exosomes, and comprehensive characterization before functional validation in macrophage polarization assays. [73] [74]
Table 3: Key Research Reagents for Macrophage Polarization and Nanoformulation Studies
| Category | Reagent/Resource | Specifications | Application and Function |
|---|---|---|---|
| Polarization Inducers | Lipopolysaccharide (LPS) | Ultrapure, TLR4 agonist | M1 polarization (100 ng/mL) [1] |
| Recombinant IFN-γ | Carrier-free, cell culture grade | M1 polarization (20-50 ng/mL) with LPS [1] | |
| Recombinant IL-4 | Carrier-free, cell culture grade | M2a polarization (20-50 ng/mL) [1] [75] | |
| Recombinant IL-13 | Carrier-free, cell culture grade | M2a polarization (20-50 ng/mL) [1] [75] | |
| Recombinant IL-10 | Carrier-free, cell culture grade | M2c polarization (20-50 ng/mL) [1] [75] | |
| Characterization Antibodies | Anti-CD80 (APC) | Clone 16-10A1, mouse | M1 surface marker detection [75] |
| Anti-CD206 (FITC) | Clone 15-2, mouse | M2 surface marker detection [75] | |
| Anti-CD163 (PE) | Clone GHI/61, human | M2 surface marker detection [75] | |
| Anti-iNOS (Western) | Rabbit monoclonal | M1 functional marker [1] | |
| Anti-Arg1 (Western) | Rabbit monoclonal | M2 functional marker [1] | |
| Nanoformulation Materials | DSPC, Cholesterol, DSPE-PEG2000 | >99% purity, pharmaceutical grade | Liposome/niosome formulation [72] |
| PLGA (50:50) | MW 10-20 kDa, acid-terminated | Polymeric nanoparticle matrix [72] | |
| Chitosan | Medium MW, >75% deacetylated | Mucoadhesive nanoparticles [72] | |
| Analytical Tools | Zetasizer Nano ZS | DLS capability | Size and zeta potential measurement [72] |
| Nanoparticle Tracking Analyzer | LM10/14 system | Particle concentration and size distribution [73] | |
| ExoQuick-TC | PCR-based | Exosome isolation and purification [73] |
The strategic integration of nanoformulations and engineered exosomes represents a transformative approach to overcoming bioavailability and delivery challenges in macrophage-targeted therapies. By leveraging these advanced delivery platforms, researchers can now develop more precise interventions for modulating macrophage polarization in chronic inflammatory diseases and cancer. The experimental frameworks and technical resources provided in this review offer practical guidance for advancing this promising field toward clinical translation and therapeutic realization. As these technologies continue to evolve, they hold exceptional promise for achieving unprecedented specificity and efficacy in immunomodulatory therapies.
Addressing Phenotype Stability and Plasticity in the Dynamic Inflammatory Microenvironment
Macrophages are fundamental components of the innate immune system, demonstrating remarkable plasticity by dynamically shifting their functional phenotypes in response to changing microenvironmental cues [76]. This plasticity, defined as their ability to polarize into distinct functional states, is crucial for orchestrating appropriate immune responses, maintaining tissue homeostasis, and facilitating repair processes [77] [1]. The polarization of macrophages exists along a broad spectrum, classically categorized into pro-inflammatory M1-like and anti-inflammatory M2-like phenotypes, though modern single-cell technologies reveal this represents a simplification of a more complex continuum of activation states [77].
In chronic inflammatory diseases, the precise regulation of macrophage phenotype stability and plasticity becomes disrupted. The dynamic inflammatory microenvironment, characterized by persistent signaling cues, metabolic alterations, and epigenetic modifications, can lock macrophages into pathological phenotypes that perpetuate disease processes [78] [79]. In aging-related chronic inflammation or "inflammaging," specialized macrophage subsets decline while pro-inflammatory populations emerge, driving tissue dysfunction [80] [79]. Similarly, in the tumor microenvironment, macrophages typically adopt an immunosuppressive M2-like phenotype that promotes angiogenesis, immune evasion, and tumor progression [77].
Understanding the molecular mechanisms governing macrophage phenotype stability and plasticity provides critical insights for developing targeted therapeutic strategies for chronic inflammatory diseases, cancer, and age-related pathologies. This technical guide examines the sophisticated regulatory networks controlling macrophage polarization and presents experimental approaches for investigating phenotype dynamics within inflammatory microenvironments, framed within the context of advancing macrophage polarization research in chronic inflammation.
Molecular Mechanisms Regulating Macrophage Phenotype Dynamics
Signaling Pathways and Transcriptional Control
Macrophage polarization is regulated by complex signaling networks that translate microenvironmental cues into distinct transcriptional programs. The JAK-STAT signaling pathway serves as a primary regulator: STAT1 activation drives M1 polarization through IFN-γ signaling, while STAT6 and STAT3 activation promotes M2 polarization through IL-4/IL-13 and IL-10 signaling, respectively [1]. The NF-κB pathway, activated by TLR ligands such as LPS, functions as a master regulator of M1 polarization by inducing pro-inflammatory gene expression [1]. Meanwhile, the PI3K-AKT pathway integrates metabolic and inflammatory signals, with AKT activation promoting M2 polarization through mechanisms including TIPE2-mediated pathway activation [77]. The PPARγ transcription factor, activated by fatty acid receptors and STAT6, coordinates M2-associated gene expression including arginase 1 (Arg1) and resistin-like-α [1].
Table 1: Key Signaling Pathways in Macrophage Polarization
| Pathway | Primary Inducers | Key Transcription Factors | Phenotype | Target Genes |
|---|---|---|---|---|
| JAK-STAT1 | IFN-γ, LPS | STAT1, IRF5 | M1 | iNOS, IL-12, CXCL10 |
| TLR-NF-κB | LPS, DAMPs/PAMPs | NF-κB (p65/p50), AP-1 | M1 | TNF-α, IL-1β, IL-6, IL-12 |
| JAK-STAT6 | IL-4, IL-13 | STAT6, IRF4, PPARγ | M2 | Arg1, Ym1, Fizz1, CCL17 |
| PI3K-AKT | IL-4, IL-13 | CREB, mTORC1 | M2 | Arg1, Mrc1 |
| IL-10-STAT3 | IL-10, glucocorticoids | STAT3, GR | M2 (regulatory) | IL-10, IL1-R2, SOCS3 |
Metabolic Reprogramming
Macrophage polarization is intrinsically linked to metabolic reprogramming, where distinct phenotypes utilize different metabolic pathways to fulfill their energy and biosynthetic requirements. M1 macrophages predominantly rely on glycolysis, even under oxygen-rich conditions, to rapidly generate ATP and support their antimicrobial functions [81] [77]. This glycolytic shift is stabilized by hypoxia-inducible factors (HIFs) and supports the production of nitric oxide (NO) and reactive oxygen species (ROS) through inducible nitric oxide synthase (iNOS) and NADPH oxidase, respectively [77].
In contrast, M2 macrophages primarily depend on oxidative phosphorylation (OXPHOS) and fatty acid oxidation (FAO) to support their anti-inflammatory and tissue-reparative functions [81] [77]. The metabolic enzyme ATP-citrate lyase (ACLY) helps bridge glucose metabolism to inflammatory processes by generating acetyl-CoA for histone acetylation and cytokine production [77]. This metabolic reprogramming is not merely a consequence of polarization but actively regulates it through metabolites that influence epigenetic modifications and signaling pathways [82].
Epigenetic and Post-Translational Regulation
Epigenetic mechanisms, including DNA methylation, histone modifications, and microRNA expression, establish stable polarization states by modulating chromatin accessibility and gene expression patterns [78]. MicroRNAs function as fine-tuning regulators of polarization; for instance, miR-210 promotes the anti-inflammatory M2 phenotype by regulating metabolic adaptation and inflammatory responses during tissue repair processes [81]. Deletion of miR-210 skews resting macrophages toward a pro-inflammatory transcriptional state and impairs IL-4-induced M2 polarization, highlighting its critical role in phenotype stability [81].
Ubiquitination, a reversible post-translational modification, has emerged as a central mechanism controlling macrophage immunometabolism and phenotype transitions [82]. E3 ubiquitin ligases and deubiquitinating enzymes (DUBs) dynamically regulate key inflammatory and metabolic pathways by modifying the stability, localization, or interactions of target proteins. For instance, the E3 ligase Cbl-b dampens inflammatory signaling by ubiquitinating MyD88 and TRIF after CD11b–Src–Syk signaling, thereby terminating TLR signaling [82]. Conversely, the deubiquitinase BRCC3 promotes NLRP3 inflammasome activation by removing inhibitory ubiquitin chains, facilitating IL-1β maturation [82]. The ubiquitin-editing enzyme A20 provides negative feedback regulation by removing activating ubiquitin chains from NF-κB pathway components and adding degradative chains to key adaptors [82].
Macrophage Polarization Regulatory Network
Phenotype Stability and Plasticity in Disease Contexts
Aging and Chronic Inflammation
In aging tissues, the homeostasis of macrophage populations is disrupted, leading to a predominance of pro-inflammatory phenotypes that drive chronic low-grade inflammation, or "inflammaging" [79]. Yale researchers have identified that nerve-associated macrophages (NAMs), which regulate fat metabolism and control age-related inflammation, decline during aging [80]. Concurrently, a novel subset of age-associated macrophages (AAMs) emerges that expresses high levels of inflammatory markers and contributes to tissue dysfunction [80]. This age-related shift in macrophage subsets is particularly evident in cardiovascular tissues, where the proportion of monocyte-derived macrophages increases with age, promoting vascular damage and accelerating cardiovascular disease progression [79]. These senescent macrophages exhibit a senescence-associated secretory phenotype (SASP) characterized by high production of pro-inflammatory cytokines (IL-6, IL-1β, TNF-α), chemokines, matrix metalloproteinases, and reactive oxygen species [79].
Tumor Microenvironment
Within the tumor microenvironment (TME), macrophages typically undergo polarization toward M2-like tumor-associated macrophages (TAMs) that support tumor progression through multiple mechanisms [77]. TAMs promote angiogenesis by secreting vascular endothelial growth factor (VEGF), facilitate immune evasion by suppressing T cell function, and enhance metastasis by remodeling the extracellular matrix [77]. This polarization is driven by factors in the TME including IL-4, IL-10, TGF-β, and metabolic byproducts such as lactate [77]. The metabolic reprogramming of TAMs is a core mechanism for their functional shift, with interventions targeting metabolic pathways holding promise for reprogramming TAMs to inhibit tumor progression [77]. Single-cell transcriptomics has revealed that macrophage phenotypes in vivo exist along a dynamic continuum rather than discrete categories, exhibiting remarkable plasticity shaped by local microenvironmental cues, developmental origins, and disease-specific pathological contexts [77].
Limitations of the M1/M2 Dichotomy
While the M1/M2 classification provides a valuable framework for studying macrophage functions, it represents an oversimplification of macrophage biology [77]. Advanced single-cell transcriptomics and spatial multi-omics technologies have demonstrated that macrophage phenotypes exist along a dynamic continuum rather than as discrete categories [77]. Certain macrophage populations can co-express both classical M1 and M2 markers, demonstrating unprecedented capacity for rapid functional switching between antimicrobial defense and tissue repair processes [77]. This remarkable plasticity fundamentally challenges the explanatory power of traditional classification systems and underscores the need for multi-dimensional profiling approaches to fully decipher macrophage functional states [77].
Experimental Approaches for Investigating Phenotype Dynamics
In Vitro Polarization Protocols
Table 2: Standardized Macrophage Polarization Protocols
| Phenotype | Induction Method | Key Markers | Metabolic Profile | Functional Assays |
|---|---|---|---|---|
| M1 | 20 ng/mL IFN-γ + 100 ng/mL LPS for 24h | CD86, iNOS, IL-12, TNF-α, CXCL10 | Glycolysis, HIF-1α stabilization | Phagocytosis, Bactericidal activity, T cell activation |
| M2 | 20 ng/mL IL-4 for 72h | CD206, Arg1, Ym1, Fizz1, CCL17 | OXPHOS, Fatty acid oxidation | Phagocytosis of apoptotic cells, Tissue remodeling, Angiogenesis |
| M2a | IL-4 or IL-13 | CD206, Arg1 | OXPHOS | Immune suppression |
| M2b | Immune complexes + TLR or IL-1R agonists | CD206, IL-10 | Mixed metabolism | Immunoregulation |
| M2c | IL-10, TGF-β, glucocorticoids | CD163, TGF-β, MER TK | OXPHOS | Matrix deposition, Tissue repair |
Bone marrow-derived macrophages (BMDMs) serve as a primary model for polarization studies. For M1 polarization, cells are treated with 20 ng/mL IFN-γ combined with 100 ng/mL LPS for 24 hours [1]. For M2 polarization, 20 ng/mL IL-4 stimulation for 72 hours effectively induces alternative activation [81] [1]. The metabolic and functional consequences of polarization can be assessed through Seahorse extracellular flux analysis to measure glycolytic rates and oxidative phosphorylation, qPCR and Western blotting for marker expression, and cytokine profiling via ELISA or multiplex arrays [81].
Genetic Manipulation Approaches
Genetic manipulation provides powerful tools for investigating molecular mechanisms governing phenotype stability. miR-210 knockout models demonstrate that deletion of this hypoxia-inducible microRNA skews resting macrophages toward a pro-inflammatory state and impairs IL-4-driven M2 polarization [81]. miR-210 KO macrophages exhibit reduced glycolytic activity, diminished metabolic flexibility, and increased phagocytosis as a potential compensatory mechanism [81]. Transcriptomic analysis of these cells reveals distinct clustering between M0 and M2 states, with miR-210 KO cells showing an increased pro-inflammatory state and incomplete M2 polarization, potentially due to reduced activation of mitotic regulators and slower cell cycle progression [81].
CRISPR-Cas9-mediated gene editing enables targeted investigation of specific regulators. For instance, knockout of E3 ubiquitin ligases (e.g., Cbl-b, Itch) or deubiquitinases (e.g., A20, CYLD) reveals their critical roles in maintaining polarization balance [82]. A20-deficient macrophages exhibit prolonged activation and excessive cytokine production, while CYLD deficiency leads to hyperinflammatory signaling and increased susceptibility to inflammation-associated pathology [82].
Experimental Workflow for Macrophage Studies
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Macrophage Polarization Studies
| Reagent Category | Specific Examples | Function/Application | Key Experimental Uses |
|---|---|---|---|
| Polarization Cytokines | Recombinant mouse/ human IFN-γ, IL-4, IL-13, IL-10, LPS | Induce specific polarization states | M1 (IFN-γ + LPS), M2 (IL-4/IL-13) polarization protocols |
| Metabolic Inhibitors | 2-DG, Oligomycin, Etomoxir, Metformin | Inhibit specific metabolic pathways | Glycolysis (2-DG), OXPHOS (Oligomycin), FAO (Etomoxir) inhibition studies |
| Signaling Modulators | JAK inhibitors (Ruxolitinib), NF-κB inhibitors (BAY-11), PI3K inhibitors (LY294002) | Target specific signaling pathways | Dissecting signaling requirements for polarization |
| Genetic Tools | miR-210 KO models, CRISPR-Cas9 systems for E3 ligases/DUBs, siRNA/shRNA | Genetic manipulation of polarization regulators | Investigating molecular mechanisms of phenotype stability |
| Detection Antibodies | Anti-CD86, anti-CD206, anti-iNOS, anti-Arg1, cytokine antibodies | Identify polarization markers | Flow cytometry, Western blot, immunofluorescence |
| Metabolic Assay Kits | Seahorse XF Glycolysis/OXPHOS kits, ATP assays, Glucose/Uptake kits | Measure metabolic parameters | Metabolic phenotyping of polarized macrophages |
| Lirimilast | Lirimilast, CAS:329306-27-6, MF:C17H12Cl2N2O6S, MW:443.3 g/mol | Chemical Reagent | Bench Chemicals |
| Liroldine | Liroldine, CAS:105102-20-3, MF:C20H20F2N4, MW:354.4 g/mol | Chemical Reagent | Bench Chemicals |
Therapeutic Targeting of Macrophage Plasticity
Emerging therapeutic strategies aim to modulate macrophage plasticity for clinical benefit. Natural products like astragaloside IV (AS-IV) and cycloastragenol (CAG) demonstrate multi-target regulation of macrophage polarization by suppressing pro-inflammatory M1 phenotypes and promoting anti-inflammatory M2 phenotypes through modulation of TLR4/NF-κB, PI3K-AKT, AMPK, and PPARγ pathways [49]. Nanotechnology approaches enhance the bioavailability and targeted delivery of these compounds, expanding their clinical applicability [49].
Ubiquitination machinery represents another promising therapeutic target for controlling macrophage polarization. Small molecule inhibitors targeting specific E3 ligases or deubiquitinases could rebalance dysregulated macrophage responses in chronic inflammation, cancer, and autoimmune diseases [82]. For instance, targeting the deubiquitinase BRCC3 might inhibit NLRP3 inflammasome activation and reduce IL-1β-mediated inflammation [82].
In aging-related chronic inflammation, strategies to preserve nerve-associated macrophages (NAMs) and prevent the emergence of pro-inflammatory age-associated macrophages (AAMs) could potentially reduce inflammaging and its associated tissue dysfunction [80]. Similarly, in cancer immunotherapy, reprogramming tumor-associated macrophages from M2-like to M1-like phenotypes represents a promising approach to enhance antitumor immunity [77]. This can be achieved through CSF-1R inhibitors to block monocyte recruitment, CD40 agonists to promote M1-like activation, or metabolic interventions that shift macrophage metabolism from OXPHOS to glycolysis [77].
The integration of single-cell multi-omics with spatial profiling technologies will enable higher-resolution characterization of macrophage subsets, ultimately facilitating the development of more precise macrophage-targeted therapies that account for the remarkable plasticity and context-dependent functions of these versatile immune cells [77].
Macrophage polarization stands as a pivotal mechanism in the resolution of inflammation and the maintenance of tissue homeostasis. Within the context of chronic inflammation, the alternative activation of macrophages toward an M2 phenotype presents a complex dualism: these cells are indispensable for wound healing and tissue repair, yet their sustained or dysregulated activity is a driving force in the pathogenesis of fibrosis and tumor progression. This whitepaper delineates the precise molecular mechanisms, including key signaling pathways and metabolic reprogramming, that underpin the functional plasticity of M2 macrophages. Furthermore, it provides a critical evaluation of experimental methodologies for investigating these cells and explores emerging therapeutic strategies aimed at mitigating their detrimental roles while preserving their beneficial functions, thereby offering a roadmap for researchers and drug development professionals in this field.
Macrophages, as key regulators of the immune response, exhibit remarkable plasticity, allowing them to adopt a spectrum of activation states in response to signals within their microenvironment [83] [29]. The classification of M1 (classically activated) and M2 (alternatively activated) macrophages, while a useful framework, represents a simplification of a continuous phenotypic diversity [8] [77]. Within the context of chronic inflammation—a common incubator for fibrotic diseases and cancer—the M2 polarization state is of particular interest due to its context-dependent functional duality.
M2 macrophages are traditionally associated with immunoregulatory functions and the resolution of inflammation. Following tissue injury, they are recruited and polarized to suppress damaging immune responses, clear apoptotic cells, and initiate the processes of tissue repair and regeneration [83]. This role is mediated through the secretion of anti-inflammatory cytokines such as IL-10 and TGF-β, and growth factors that promote angiogenesis and matrix deposition [8] [84]. However, when these reparative processes become dysregulated, the same mechanisms can drive pathological outcomes. In fibrotic diseases, such as Idiopathic Pulmonary Fibrosis (IPF), M2 macrophages contribute to excessive scarring by producing pro-fibrotic factors like TGF-β and PDGF, which stimulate collagen production and fibroblast activation [85]. Similarly, in the tumor microenvironment (TME), M2-polarized Tumor-Associated Macrophages (TAMs) facilitate tumor progression by promoting angiogenesis, immunosuppression, and metastasis [8] [77]. Understanding the mechanisms that govern this fine balance is essential for developing targeted therapies that can selectively inhibit the harmful functions of M2 macrophages without compromising their vital role in tissue homeostasis.
Molecular Mechanisms of M2 Polarization and Function
The polarization of macrophages to the M2 phenotype is orchestrated by a complex network of extracellular cues, intracellular signaling pathways, and metabolic reprogramming.
Signaling Pathways and Transcriptional Regulation
M2 polarization is primarily induced by cytokines such as IL-4 and IL-13, which activate the JAK-STAT6 signaling pathway [77] [86]. STAT6, in conjunction with the transcription factor IRF4, drives the expression of characteristic M2 genes, including those encoding for arginase-1 (Arg1), the mannose receptor (CD206), and various chitinase-like proteins [77]. Other stimuli, including IL-10, TGF-β, and glucocorticoids, can also promote M2-like phenotypes through distinct but often overlapping pathways, such as the activation of STAT3 [84]. Furthermore, signaling through the PI3K/AKT pathway is critically involved in M2 polarization, enhancing cell survival and contributing to the metabolic shifts associated with this phenotype [77] [86]. The TREM2 receptor has also been identified as a key regulator of a pro-fibrotic macrophage subpopulation in liver fibrosis, highlighting the diversity of regulatory inputs [83].
Metabolic Reprogramming
A fundamental aspect of M2 polarization is the rewiring of cellular metabolism. Unlike pro-inflammatory M1 macrophages, which rely predominantly on glycolysis, M2 macrophages preferentially utilize oxidative phosphorylation (OXPHOS) and fatty acid oxidation (FAO) to meet their energy demands [8] [29]. This metabolic profile supports their long-term tissue-remodeling functions. Key aspects of M2 metabolic reprogramming include:
- Enhanced Fatty Acid Oxidation: The transcription factors PPARγ and PPARδ are activated and promote the catabolism of fatty acids, fueling the TCA cycle and mitochondrial respiration [77].
- Urea Cycle and Polyamine Synthesis: The enzyme arginase-1 (Arg1) is a hallmark of M2 macrophages. It competes with inducible nitric oxide synthase (iNOS) for the substrate arginine. While iNOS produces nitric oxide (NO) in M1 cells, Arg1 in M2 cells converts arginine to ornithine, which is further metabolized to produce polyamines and proline, essential components for cell proliferation and collagen synthesis, respectively [8] [77].
- Amino Acid Metabolism: Glutamine metabolism is another crucial pathway, generating α-ketoglutarate to replenish the TCA cycle (anaplerosis) and support OXPHOS [29].
The pyruvate kinase isoform PKM2 has been identified as a critical node integrating metabolic and inflammatory signaling in macrophages. PKM2 can regulate the M1/M2 balance through both its enzymatic activity in glycolysis and its role as a protein kinase and transcriptional co-activator, making it a potential therapeutic target [70] [87].
Effector Functions in Repair, Fibrosis, and Cancer
The functional output of M2 macrophages is mediated by their secretome:
- Tissue Repair: They secrete growth factors like VEGF and IGF-1 to promote angiogenesis and epithelial cell proliferation [83].
- Fibrosis: The sustained production of TGF-β and PDGF by M2 macrophages is a primary driver of fibrosis. TGF-β activates resident fibroblasts, inducing their differentiation into collagen-producing myofibroblasts, while PDGF stimulates fibroblast proliferation [83] [85]. They also produce matrix metalloproteinases (MMPs) and their inhibitors (TIMPs) to remodel the extracellular matrix (ECM) [85].
- Tumor Progression: In the TME, M2 TAMs suppress cytotoxic T lymphocyte (CTL) function through multiple mechanisms, including the expression of PD-L1, secretion of IL-10 and TGF-β, and depletion of arginine via Arg1 [8]. They also produce VEGF and other factors to stimulate tumor angiogenesis and facilitate metastasis by promoting ECM remodeling and epithelial-mesenchymal transition (EMT) [8] [77].
The diagram below summarizes the core signaling and metabolic pathways driving M2 macrophage polarization and function.
Quantitative Data on M2 Macrophage Functions
The dual role of M2 macrophages is evidenced by quantitative data on their recruitment, marker expression, and functional outputs across different pathological contexts. The following tables summarize key quantitative findings from experimental and clinical studies.
Table 1: M2 Macrophage Markers and Functional Secretome
| Marker / Factor | Function | Expression/Level in M2 | Pathological Context |
|---|---|---|---|
| CD206 (Mannose Receptor) | Endocytosis, phagocytosis | Highly upregulated [8] [84] | Fibrosis, Cancer |
| CD163 (Scavenger Receptor) | Hemoglobin-haptoglobin complex clearance | Highly upregulated [8] [29] | Cancer, Chronic Inflammation |
| Arginase-1 (Arg1) | Arginine metabolism to ornithine | Highly upregulated [8] [77] | Fibrosis, Cancer (Immunosuppression) |
| IL-10 | Anti-inflammatory cytokine | High secretion [8] [83] | Fibrosis, Cancer (Immunosuppression) |
| TGF-β | Fibroblast activation, collagen production | High secretion [8] [85] | Fibrosis, Tumor progression |
| VEGF | Angiogenesis | High secretion [8] [77] | Tumor progression, Wound healing |
| PDGF | Fibroblast proliferation & recruitment | High secretion [85] | Idiopathic Pulmonary Fibrosis |
Table 2: M2 Macrophage Quantification and Association with Disease Outcomes
| Parameter | Observation / Measurement | Disease Context | Clinical/Experimental Correlation |
|---|---|---|---|
| Tissue Infiltration | ~10x increase in lamina propria macrophages in active UC vs. healthy [88] | Ulcerative Colitis (UC) | Drives disease pathogenesis |
| Spatial Distribution | M2-like TAMs infiltrate hypoxic and stromal regions [8] | Solid Tumors | Promotes angiogenesis, immune suppression, ECM remodeling |
| Prognostic Value | High infiltration of TAMs (often M2) correlates with poor survival [8] [84] | Breast, Lung Cancers | Marker of poor prognosis |
| Prognostic Value | Paradoxical association with improved prognosis in some cases [8] | Colorectal Cancer | Highlights context-dependence |
| Therapeutic Depletion | Optimal control strategy reduced M2 levels in a mathematical model, preventing fibrosis [85] | Idiopathic Pulmonary Fibrosis (Model) | Suggests therapeutic potential of M2 targeting |
Experimental Protocols for M2 Macrophage Research
Robust experimental models are crucial for dissecting the mechanisms of M2 polarization and function. Below are detailed methodologies for key experiments in this field.
In Vitro Polarization and Functional Assay
This protocol describes the generation and validation of human M2 macrophages from monocyte precursors.
Workflow: M2 Macrophage Polarization and Analysis
Key Research Reagent Solutions:
- CD14+ MicroBeads: For positive selection of human monocytes from Peripheral Blood Mononuclear Cells (PBMCs) using magnetic-activated cell sorting (MACS).
- Recombinant Human M-CSF (Macrophage Colony-Stimulating Factor): Essential for the differentiation of monocytes into naive (M0) macrophages in culture over 5-7 days.
- Recombinant Human IL-4 and IL-13: The canonical cytokines used to polarize M0 macrophages toward the M2 phenotype. Typical working concentrations range from 20 to 50 ng/mL for 24 to 48 hours.
- Anti-CD206 (e.g., APC-conjugated) & Anti-Arginase-1 Antibodies: Antibodies for flow cytometry or immunofluorescence to confirm successful M2 polarization by detecting surface and intracellular markers.
- ELISA Kits for IL-10 and TGF-β: Used to quantify the secretion of characteristic anti-inflammatory cytokines from M2 macrophage culture supernatants.
Procedure:
- Monocyte Isolation: Isolate PBMCs from human whole blood using density gradient centrifugation (e.g., Ficoll-Paque). Subsequently, isolate CD14+ monocytes using CD14 MicroBeads and a magnetic separation column according to the manufacturer's protocol.
- M0 Macrophage Differentiation: Culture the purified CD14+ monocytes (e.g., in RPMI-1640 medium supplemented with 10% FBS and 1% Penicillin/Streptomycin) in the presence of 50 ng/mL recombinant human M-CSF for 5-7 days. Refresh the medium and cytokines every 2-3 days. The resulting adherent cells are naive M0 macrophages.
- M2 Polarization: Stimulate the M0 macrophages with 20-50 ng/mL recombinant human IL-4 and IL-13 for 24-48 hours.
- Phenotypic Validation:
- Flow Cytometry: Harvest polarized macrophages and stain with fluorochrome-conjugated antibodies against M2 surface markers (e.g., CD206, CD163). Use an isotype control for gating. Analyze on a flow cytometer. Successful polarization is indicated by high expression of these markers.
- qPCR: Isolve total RNA and perform cDNA synthesis. Use qPCR to measure the relative mRNA expression of M2 genes (e.g., ARG1, MRC1 (CD206), CD163) compared to M0 and M1 controls. Calculate fold change using the 2^(-ΔΔCt) method.
- Functional Assay (Cytokine Secretion): Collect cell culture supernatants from M2 macrophages. Use commercial ELISA kits to quantify the concentrations of secreted IL-10 and TGF-β, following the manufacturer's instructions.
In Vivo Model of Macrophage-Driven Fibrosis
This protocol uses carbon tetrachloride (CClâ‚„) to induce liver fibrosis in mice, a well-established model for studying the role of macrophages in this process.
Procedure:
- Animal Model: Administer CClâ‚„ (e.g., 0.5-1 mL/kg body weight, diluted in olive oil) to mice via intraperitoneal injection twice weekly for 4-8 weeks. A control group should receive olive oil only.
- Macrophage Depletion/Modulation: To investigate the specific role of M2 macrophages, utilize transgenic models (e.g., CD11b-DTR mice) or administer therapeutic agents (e.g., a CSF-1R inhibitor) at specific time points during or after the injury phase. For example, depleting CD11b+ cells during active injury reduces inflammation, while depletion during the recovery phase impairs matrix degradation and tissue repair, highlighting the dual role of macrophages [83].
- Tissue Analysis:
- Histology: Harvest liver tissue at endpoint. Fix in formalin, embed in paraffin, and section. Perform staining:
- Masson's Trichrome or Picrosirius Red: To visualize and quantify collagen deposition (fibrosis).
- Immunofluorescence/Immunohistochemistry: Stain sections with antibodies against F4/80 (pan-macrophage marker) and CD206 or Arg1 (M2 markers) to identify and localize M2 macrophages within fibrotic areas.
- Hydroxyproline Assay: Use a colorimetric hydroxyproline assay on liver tissue hydrolysates as a quantitative biochemical measure of total collagen content.
- Histology: Harvest liver tissue at endpoint. Fix in formalin, embed in paraffin, and section. Perform staining:
Therapeutic Strategies for Targeting M2 Macrophages
Therapeutically, the goal is to reprogram or inhibit the pro-fibrotic and pro-tumorigenic functions of M2 macrophages. Several strategies are under preclinical and clinical investigation.
- Targeting Recruitment and Survival: Inhibition of the CSF-1/CSF-1R axis or the CCL2/CCR2 chemokine pathway can block the recruitment and survival of monocytes/macrophages in tissues. CSF-1R inhibitors have shown promise in modulating TAMs in cancer and are being evaluated in clinical trials [8].
- Repolarization Strategies: Agents that can shift M2 macrophages back to an M1-like, anti-tumorigenic state are highly sought after. This can be achieved using nanoparticle-encapsulated drugs delivering IFN-γ or TLR agonists, or by targeting metabolic checkpoints like PKM2 [8] [70] [87].
- Inhibition of Protumorigenic Effector Functions: Blocking key M2-derived factors, such as TGF-β or VEGF, with neutralizing antibodies or receptor inhibitors is another viable approach. Pirfenidone and nintedanib, approved for IPF, have anti-fibrotic effects that may partially involve the modulation of macrophage functions, though they do not target M2 cells directly [85].
- Mathematical Modeling for Therapeutic Control: As exemplified in IPF research, optimal control theory can be applied to design dosing strategies for "anti-M1" agents (which indirectly regulate M2 dynamics) to minimize fibrosis formation over time, offering a novel model-based therapeutic framework [85].
M2 macrophages represent a double-edged sword in chronic inflammation, capable of driving both essential tissue repair and devastating pathological fibrosis and tumor progression. This duality is governed by precise signaling pathways and profound metabolic reprogramming. While the M1/M2 dichotomy provides a useful framework, it is an oversimplification. Future research must leverage single-cell multi-omics technologies to deconvolute the full spectrum of macrophage heterogeneity and identify novel, functionally relevant subpopulations [8] [77].
The translational potential of targeting M2 macrophages is immense. Future directions should focus on developing context-specific therapies that consider the temporal and spatial dynamics of macrophage functions. This includes:
- Designing smart delivery systems that target therapeutics specifically to disease-associated macrophage subsets.
- Exploring combination therapies that simultaneously target M2 macrophages and other components of the fibrotic or tumor microenvironment (e.g., cancer-associated fibroblasts).
- Validating M2-related biomarkers (e.g., CD206, CD163) for patient stratification and monitoring treatment response.
By deepening our understanding of the mechanistic switches that tilt the balance of M2 macrophage function from protective to pathogenic, we can develop more precise and effective interventions for a wide range of chronic inflammatory diseases, fibrotic disorders, and cancers.
Macrophages, central players in the innate immune system, exhibit remarkable functional plasticity in response to microenvironmental signals [1]. This plasticity is most commonly described through the paradigm of macrophage polarization, where macrophages adopt a spectrum of activation states, from the pro-inflammatory, classically activated M1 phenotype to the anti-inflammatory, alternatively activated M2 phenotype [89] [14]. The dynamic and often reversible transition between these states is a critical regulatory mechanism in inflammatory diseases [2]. In chronic inflammation, a persistent imbalance favoring M1 macrophages drives tissue damage and pathology, whereas a shift toward M2 dominance can facilitate tissue repair and resolution of inflammation [14] [20]. Consequently, the M1/M2 ratio has emerged as a crucial indicator of immune status and a promising therapeutic target [14]. This whitepaper provides an in-depth technical guide on the mechanisms underlying macrophage polarization and explores strategic approaches for therapeutically modulating the M1/M2 balance in chronic inflammatory diseases, framed within the context of advanced research and drug development.
Foundational Mechanisms of Macrophage Polarization
Phenotype Definition and Functional Roles
Macrophage polarization is not a binary switch but a continuum of functional states, broadly categorized into M1 and M2 phenotypes, each with distinct triggers, markers, and effector functions [89] [14].
- M1 Macrophages (Pro-inflammatory): M1 polarization is classically induced by interferon-gamma (IFN-γ) alone or in combination with microbial ligands such as lipopolysaccharide (LPS) [1] [20]. These macrophages are characterized by high secretion of pro-inflammatory cytokines, including tumor necrosis factor-alpha (TNF-α), interleukin-1 beta (IL-1β), and IL-6 [89] [14]. They also express high levels of inducible nitric oxide synthase (iNOS), which generates nitric oxide (NO), contributing to their potent microbicidal and antitumor activities [1] [90]. Key surface markers for M1 identification include CD80, CD86, and TLR-4 [14].
- M2 Macrophages (Anti-inflammatory/Reparative): The M2 phenotype is alternatively activated by cytokines such as IL-4 and IL-13 [89] [1]. M2 macrophages secrete anti-inflammatory factors like IL-10 and transforming growth factor-beta (TGF-β), which help limit inflammation and promote tissue repair, angiogenesis, and wound healing [89] [14]. They express markers including CD163, CD206, and arginase-1 (Arg1), the latter of which competes with iNOS for arginine metabolism, further dampening inflammation [14] [20]. The M2 category is often subdivided into M2a, M2b, M2c, and M2d, each with nuanced functions, though all generally fall under an "anti-inflammatory" umbrella [29] [14].
Core Signaling Pathways Regulating Polarization
The polarization process is coordinately regulated by a network of intricate signaling pathways. Understanding these pathways is fundamental to developing targeted therapies.
Table 1: Core Signaling Pathways in Macrophage Polarization
| Pathway | Primary Inducers | Key Signaling Molecules | Transcriptional Regulators | Polarization Outcome |
|---|---|---|---|---|
| JAK/STAT [89] [20] | IFN-γ, IL-4, IL-13 | JAK1, JAK2, JAK3 | STAT1 (M1), STAT6 (M2) | IFN-γ/STAT1 drives M1; IL-4,IL-13/STAT6 drives M2 |
| NF-κB [2] [20] | LPS, TNF-α | TLR4, MyD88, IKK complex | NF-κB p65/p50 | Promotes transcription of M1-related pro-inflammatory genes |
| PI3K/Akt [2] [20] | Growth factors, cytokines | PI3K, Akt (PKB), mTOR | Not a primary transcription factor, modulates others | Context-dependent; generally associated with M2 polarization |
| MAPK [2] | LPS, stress | ERK, JNK, p38 | AP-1 | Involved in both M1 and M2 polarization dynamics |
The following diagram illustrates the logical relationships and cross-talk between these key signaling pathways in determining macrophage fate.
Quantitative Data in Disease Contexts
The M1/M2 imbalance is a hallmark of numerous chronic diseases. The table below summarizes key quantitative findings from recent research, highlighting the central role of this ratio in disease pathogenesis and its potential as a biomarker.
Table 2: M1/M2 Ratio in Chronic Inflammatory and Autoimmune Diseases
| Disease Model | Key Findings on M1/M2 Balance | Associated Mediators/Factors | Experimental Evidence |
|---|---|---|---|
| Osteoarthritis (OA) [2] | Synovial macrophages predominantly M1; M1/M2 ratio correlates with synovitis & cartilage degradation. | ↑ IL-1β, TNF-α, IL-6, MMP-13; Signaling via PI3K/Akt, NF-κB, MAPK | Clinical imaging (SPECT-CT), synovial tissue analysis, murine models. |
| Rheumatoid Arthritis (RA) [14] | High M1/M2 ratio in synovial tissue & peripheral blood; RA remission associated with increased M2. | ↑ TNF-α, IL-6 (M1); ↑ IL-10 (M2); Pathways: NF-κB, JAK/STAT, SAPK/MAPK | Flow cytometry of patient samples, in vitro stimulation. |
| Autoimmune Hepatitis (AIH) [14] | Increased M1/M2 ratio contributes to autoimmune damage. | M1-derived reactive oxygen species (ROS). | Animal models, human tissue studies. |
| Glioblastoma (GBM) [91] | Tumor microenvironment skewed towards M2; high M2 TAMs associated with tumor progression. | ↑ IL-10, TGF-β, VEGF; M2 genes: CD163, CD206, ARG1 | Single-cell RNA sequencing (scRNA-seq), bioinformatic analysis of patient data. |
| Inflammatory Bowel Disease (IBD) [14] | Mucosal inflammation characterized by increased M1/M2 ratio. | ↑ M1 pro-inflammatory cytokines. | Human intestinal mucosal studies, murine colitis models. |
| Allergic Asthma [14] | Imbalance towards M2-driven Th2 response. | ↑ IL-4, IL-13, IL-10; IgE production. | Bronchoalveolar lavage (BAL) fluid analysis, murine asthma models. |
| Atherosclerosis [14] | M1 macrophages dominate in unstable atherosclerotic plaques. | ↑ iNOS, pro-inflammatory cytokines. | Histology of human plaques, murine atherosclerosis models. |
Experimental Protocols for Polarization Research
This section outlines standard in vitro methodologies for inducing, analyzing, and modulating macrophage polarization, providing a core workflow for preclinical research.
Standard In Vitro Polarization Protocol
A typical workflow for generating and validating M1 and M2 macrophages in vitro is described below [89] [1] [20].
Macrophage Derivation:
- Isolate primary monocytes from human peripheral blood or mouse bone marrow using density gradient centrifugation (e.g., Ficoll-Paque).
- Differentiate monocytes into naive, undifferentiated macrophages (M0) by culturing for 5-7 days in media supplemented with Macrophage Colony-Stimulating Factor (M-CSF or CSF-1) at 20-50 ng/mL.
Polarization Induction:
Phenotypic Validation:
- Gene Expression Analysis: Quantify mRNA levels of M1 markers (e.g., TNF, IL6, IL12, iNOS) and M2 markers (e.g., CD206, ARG1, YM1, FIZZ1) via qRT-PCR.
- Surface Marker Analysis: Use flow cytometry to detect protein expression of M1 surface markers (CD80, CD86) and M2 surface markers (CD163, CD206).
- Cytokine Secretion: Measure secreted cytokines in the culture supernatant using enzyme-linked immunosorbent assay (ELISA) or multiplex bead-based arrays (e.g., Luminex). Key analytes include TNF-α, IL-12p70 (M1) and IL-10, CCL17 (M2).
- Functional Assays: Assess metabolic profile (e.g., Seahorse Analyzer for glycolysis vs. oxidative phosphorylation) or phagocytic capacity.
The following diagram visualizes this standard experimental workflow.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Macrophage Polarization Research
| Reagent Category | Specific Examples | Function in Research |
|---|---|---|
| Polarizing Cytokines | Recombinant Human/Mouse: IFN-γ, LPS (from E.coli), IL-4, IL-13 | To induce and control M1 or M2 polarization in vitro and in vivo. |
| Differentiation Factors | M-CSF (CSF-1), GM-CSF | To differentiate monocytes or bone marrow progenitors into macrophages. |
| Flow Cytometry Antibodies | Anti-human/mouse: CD80, CD86, CD64, MHC-II (M1); CD163, CD206, CD209 (M2) | To identify and sort macrophage populations based on surface protein expression. |
| ELISA Kits | Kits for TNF-α, IL-6, IL-12p70, IL-1β (M1); IL-10, TGF-β, CCL17, CCL18 (M2) | To quantitatively measure cytokine secretion profiles of polarized macrophages. |
| qPCR Assays | TaqMan assays or SYBR Green primers for iNOS, TNF, IL6 (M1); ARG1, MRC1, FIZZ1, YM1 (M2) | To analyze gene expression patterns characteristic of M1/M2 states. |
| Signal Pathway Modulators | Small molecule inhibitors for JAK (e.g., Tofacitinib), PI3K (e.g., LY294002), NF-κB (e.g., BAY 11-7082); Agonists for PPARγ (e.g., Rosiglitazone) | To dissect the contribution of specific signaling pathways to polarization. |
Therapeutic Strategies for Modulating the M1/M2 Balance
Therapeutic targeting of the M1/M2 ratio involves two primary strategic goals: inhibiting detrimental polarization (e.g., M1 in RA) or promoting beneficial polarization (e.g., M2 in tissue repair). Emerging approaches include:
Cytokine and Receptor Blockade: Using monoclonal antibodies or receptor antagonists to block pro-inflammatory cytokines like IL-1β, IL-6, or TNF-α can effectively reduce M1-driven inflammation, as demonstrated in RA treatment [14]. Conversely, administering IL-4 or IL-13 could theoretically promote M2 polarization, though clinical delivery remains challenging.
Small Molecule Inhibitors: Targeting intracellular signaling hubs is a powerful approach. Inhibitors of the JAK/STAT pathway (e.g., Tofacitinib) are already in clinical use for autoimmune diseases and can modulate the M1/M2 balance by interfering with polarization signals [14] [20]. Similarly, developing specific inhibitors for key nodes in the NF-κB or MAPK pathways can suppress M1 polarization.
Metabolic Reprogramming: M1 and M2 macrophages rely on distinct metabolic pathways—M1 on glycolysis and M2 on oxidative phosphorylation [89] [29]. Pharmacologically shifting macrophage metabolism is a promising strategy. For instance, the mitochondrial metabolite itaconate can inhibit succinate dehydrogenase and suppress M1 inflammation [89].
Engineered Cell Therapies: Advanced bioengineering has led to the development of Chimeric Antigen Receptor Macrophages (CAR-M). These cells are engineered to recognize specific tumor antigens and can be designed to adopt a pro-inflammatory (M1) phenotype, thereby directly repolarizing the tumor microenvironment in cancers like melanoma and enhancing T cell recruitment [90].
Nanoparticle-Based Drug Delivery: Macrophages' inherent phagocytic capacity makes them ideal targets for nanoparticle (NP)-mediated drug delivery. NPs can be loaded with polarizing agents (e.g., STAT6 agonists for M2, or NF-κB inhibitors for M1) and surface-functionalized to target specific macrophage subsets, enabling precise modulation of the local M1/M2 ratio within diseased tissues [90].
The M1/M2 macrophage balance is a dynamic and pivotal regulator of immune homeostasis whose dysregulation is a pathological cornerstone of chronic inflammation, autoimmunity, and cancer. Targeting this balance represents a paradigm shift from broad immunosuppression to precise immunomodulation. Future research must focus on deepening our understanding of the human-specific plasticity of macrophages in vivo, developing more sophisticated delivery systems for polarizing agents, and identifying novel, disease-specific molecular targets within the polarization network. The integration of single-cell omics, advanced bioengineering, and targeted nanotherapeutics will undoubtedly unlock the next generation of therapies aimed at optimizing the disease-specific polarization balance for therapeutic benefit.
Strategies for Enhancing Specificity and Reducing Off-Target Effects in Polarization Therapies
Within the broader thesis on mechanisms of macrophage polarization in chronic inflammation research, a critical challenge emerges: achieving precise control over macrophage phenotypes while minimizing off-target effects. Macrophages, ubiquitous innate immune cells, exist along a dynamic continuum of activation states, broadly categorized into pro-inflammatory (M1) and anti-inflammatory (M2) extremes [4]. The polarization process involves transcriptional reprogramming of over 1,000 genes, governed by core regulators like STAT1 for M1 and STAT6 for M2 states [4]. However, this complexity creates significant challenges for therapeutic interventions. In diseases like ulcerative colitis, a skewed balance where M1 macrophages drive inflammation while M2 macrophages promote resolution underscores the therapeutic imperative [92]. Similarly, in oncology, tumor-associated macrophages (TAMs) often exhibit M2-like properties that support tumor progression and can even protect cancer cells from novel therapies like cold atmospheric plasma [93]. This whitepaper details advanced strategies to enhance the specificity of polarization therapies, leveraging cutting-edge targeting technologies, multimodal approaches, and sophisticated experimental methodologies to overcome the limitations of current paradigms and pave the way for precision immunomodulation.
Advanced Targeting Strategies for Precision Polarization
Molecular and Nanomaterial-Based Targeting
Table 1: Advanced Targeting Strategies for Macrophage Polarization Therapies
| Targeting Strategy | Mechanism of Action | Therapeutic Application | Specificity Advantage |
|---|---|---|---|
| Targeting Peptides [94] | Binds specifically to surface markers overexpressed on target macrophages | Tumor microenvironment (TME) targeting; Delivery of polarizing agents | Reduces normal tissue exposure and systemic side effects |
| Receptor Targeting (e.g., Folate Receptor) [94] | Utilizes ligand-receptor interaction for cellular uptake | Inflammatory disease; Cancer | Exploits differential receptor expression on specific macrophage subsets |
| Mitochondrial Targeting [94] | Directs therapeutics to mitochondria to alter metabolic programming | Shifting metabolic phenotype from M1 to M2 or vice versa | Leverages the central role of metabolism in macrophage polarization |
| Nucleic Acid Aptamers [94] | High-affinity binding to specific cell-surface proteins | Specific blockade of pro-inflammatory or pro-fibrotic signals | High specificity and lower immunogenicity than antibodies |
| Tissue Compliance Modulation [4] | Alters macrophage phenotype via mechanotransduction signals | Fibrotic diseases; Inflammatory conditions | Targets physical rather than chemical aspects of the microenvironment |
Innovative targeting strategies are crucial for enhancing specificity. Beyond the molecular approaches summarized in Table 1, nanomaterial-based delivery systems significantly improve precision. Platforms such as exosomes, liposomes, and nano-metal-organic frameworks enhance the delivery efficiency of polarizing agents to specific macrophage subpopulations [94]. For instance, exosomes can be engineered with homing peptides to deliver M1-polarizing miRNAs specifically to TAMs, repolarizing them to an anti-tumor phenotype without broadly activating systemic inflammation. Furthermore, the emerging understanding of biomechanical signaling reveals that substrate stiffness influences macrophage polarization [4]. Softer substrates favor a host-defense phenotype, suggesting that modulating tissue compliance could represent a novel physical targeting strategy to steer macrophage function in fibrotic diseases.
Signal Transduction and Transcriptional Targeting
Targeting the intricate intracellular signaling networks that govern polarization requires equal precision. The CBP/p300-interacting transactivator (CITED) family of transcriptional co-regulators, particularly CITED2, functions as a master controller of the M1 program by competing with transcription factors like STAT1, IRF, and NF-κB for binding to the CBP/p300 coactivator [4]. Inhibiting CITED2 could potentially enhance M1 polarization with high specificity. Conversely, post-transcriptional regulators like the long non-coding RNA MALAT1 bias macrophages toward the M1 state by antagonizing miR-30 family members that support M2 gene expression [4]. Targeting such RNA networks offers a layer of specificity distinct from direct transcriptional inhibition. In the context of chronic inflammation like ulcerative colitis, targeting NEU-derived proteases (e.g., MMP-9) and NET formation can indirectly influence macrophage polarization by resolving the initial inflammatory triggers that drive M1 activation [92].
Experimental Protocols for Validating Specificity
Establishing a Co-Culture Model to Study TAM-Mediated Therapy Resistance
Objective: To investigate how M2-polarized macrophages in the tumor microenvironment protect cancer cells from cytotoxic therapies, as observed with Cold Atmospheric Plasma (CAP) [93].
Materials:
- Cell Lines: THP-1 human monocytic cells; Human lung cancer cells (e.g., Calu-1, H1299).
- Polarizing Agents: Phorbol 12-myristate 13-acetate (PMA) for THP-1 differentiation; IL-4 + IL-13 for M2 polarization; LPS + IFN-γ for M1 polarization.
- Antibodies: Anti-CD206 (M2 marker), Anti-CD80 (M1 marker) for flow cytometry.
- Inhibitors: STAT1 inhibitor (Fludarabine), STAT3 inhibitor (Stattic), IL-10 neutralizing antibodies.
- Equipment: Cold Atmospheric Plasma device, CO2 incubator, flow cytometer, Western blot apparatus.
Methodology:
- Macrophage Differentiation and Polarization:
- Differentiate THP-1 monocytes into M0 macrophages by treating with 100 nM PMA for 48 hours.
- Polarize M0 macrophages to M2 phenotype by incubating with IL-4 (20 ng/mL) and IL-13 (20 ng/mL) for 48 hours. Validate polarization via flow cytometry for CD206 expression [93].
Co-Culture System Establishment:
- Seed M2-polarized macrophages and Calu-1 lung cancer cells in transwell co-culture plates, allowing for the exchange of soluble factors without direct cell contact.
- Include control groups of Calu-1 cells cultured alone.
Therapeutic Intervention and Analysis:
- Treat the co-culture system and monoculture controls with CAP (e.g., 30-second exposure).
- Viability Assessment: At 24 hours post-treatment, measure cancer cell viability using CCK-8 assay and cell death via Propidium Iodide (PI) staining.
- Mechanistic Analysis:
- Collect co-culture supernatants to measure IL-10 secretion by ELISA.
- Analyze Calu-1 cells for phosphorylation of STAT1/STAT3 and markers of Endoplasmic Rticulum (ER) stress (e.g., CHOP, BIP) via Western blot.
- To confirm the role of IL-10, pre-treat Calu-1 cells with an IL-10R1-specific siRNA before co-culture and CAP exposure.
Protocol for Assessing Transcriptional Specificity
Objective: To evaluate whether a candidate M2-polarizing agent specifically upregulates M2-associated genes without inadvertently activating pro-inflammatory M1 genes.
Methodology:
- Cell Treatment: Isolate primary bone marrow-derived macrophages (BMDMs) or use a relevant macrophage cell line. Treat with the candidate polarizing agent (e.g., IL-4) and a control M1-inducing agent (LPS).
- RNA Extraction and qRT-PCR: Extract total RNA and perform quantitative RT-PCR using a panel of primers for hallmark genes.
- M1 Markers: iNOS, TNF-α, IL-6, IL-1β.
- M2 Markers: Arg1, Ym1, Fizz1, CD206.
- Data Interpretation: Specific M2 polarization is confirmed by a significant upregulation of M2 markers with no concurrent increase in M1 markers. A mixed profile suggests potential off-target effects.
Visualization of Key Signaling Pathways
The diagram illustrates the mechanism by which M2 macrophages, induced by Cold Atmospheric Plasma (CAP), protect lung cancer cells. CAP triggers M2 polarization, leading to IL-10 release. IL-10 binding to its receptor on cancer cells activates JAK1, resulting in the phosphorylation of both STAT1 and STAT3. This activated STAT1/STAT3 complex alleviates CAP-induced Endoplasmic Reticulum stress, ultimately attenuating tumor cell death and promoting survival [93].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagents for Macrophage Polarization Studies
| Reagent / Tool | Category | Function / Application | Example Use Case |
|---|---|---|---|
| PMA (Phorbol 12-myristate 13-acetate) [93] | Differentiation Agent | Differentiates monocytic cell lines (e.g., THP-1) into adherent M0 macrophages. | In vitro model establishment. |
| IL-4 + IL-13 [93] | Cytokines | Classic combination for inducing alternative M2 macrophage polarization. | Studying M2 functions in tissue repair or pro-tumorigenesis. |
| LPS + IFN-γ [93] | Cytokines / PAMP | Classic combination for inducing classical M1 macrophage polarization. | Modeling pro-inflammatory responses in infection or autoimmunity. |
| Anti-CD206 & Anti-CD80 Antibodies [93] | Flow Cytometry Reagents | Surface markers for identifying M2 (CD206) and M1 (CD80) macrophage populations. | Phenotypic validation after polarization treatments. |
| Fludarabine & Stattic [93] | Small Molecule Inhibitors | Fludarabine inhibits STAT1 transcription; Stattic inhibits STAT3 phosphorylation. | Mechanistic studies to validate STAT pathway involvement. |
| siRNA against IL-10R1 [93] | Molecular Biology Tool | Knocks down expression of the IL-10 receptor subunit 1. | Confirming the specific role of IL-10 signaling in a pathway. |
| AIPH Radical Initiator [94] | Thermodynamic Therapy Agent | Heat-labile compound that generates oxygen-free radicals upon thermal activation. | Studying oxygen-independent anti-tumor macrophage activation. |
| MT-MOF TNS [94] | Piezoelectric Nanomaterial | Generates reactive oxygen species under ultrasound excitation for sonodynamic therapy. | Activating specific immune responses in deep tissues. |
Enhancing the specificity of macrophage polarization therapies requires a multi-faceted approach that integrates advanced targeting technologies, a deep understanding of signaling pathways, and robust experimental validation. The strategies outlined—from molecular and nanomaterial targeting to the exploitation of transcriptional and post-transcriptional regulators—provide a roadmap for developing next-generation therapies with reduced off-target effects. The critical role of the microenvironment, as exemplified by M2 macrophages protecting tumors from CAP, underscores that effective therapeutic strategies must consider and overcome endogenous resistance mechanisms [93]. Future efforts should focus on optimizing sensitizer design, improving pathological microenvironments (e.g., hypoxia), and developing multifunctional nanoplatforms that combine precise targeting with multimodal treatments to achieve synergistic and specific polarization of macrophages for a wide range of chronic inflammatory diseases and cancers [94].
Bench-to-Bedside Translation: Validating Polarization Strategies Across Disease Models and Human Studies
In the realm of chronic inflammation research, macrophage polarization represents a critical focal point for understanding disease pathogenesis and developing novel therapeutic strategies. Macrophages, as pivotal regulators of immunity, exhibit remarkable plasticity, dynamically shifting between classically activated pro-inflammatory (M1) and alternatively activated anti-inflammatory (M2) phenotypes in response to microenvironmental cues [1]. The precise identification of these phenotypic states is fundamental to decoding their functional roles in chronic inflammatory conditions such as rheumatoid arthritis, inflammatory bowel disease, atherosclerosis, and diabetic complications [92] [14] [95].
This technical guide provides an in-depth examination of the core biomarkers—surface markers (CD80, CD86, CD206, CD163) and cytokine profiles—essential for accurate macrophage phenotype identification. Within the context of chronic inflammation, where the M1/M2 balance is frequently disrupted, these biomarkers serve as crucial indicators of disease progression, therapeutic response, and underlying molecular mechanisms [11] [14]. We present a comprehensive framework integrating quantitative biomarker data, detailed experimental methodologies, and signaling pathway visualizations to equip researchers with robust tools for advancing macrophage-centric research in chronic inflammatory diseases.
Macrophage Polarization in Chronic Inflammation
The Spectrum of Macrophage Activation
Macrophages exist along a continuum of activation states, with the M1/M2 paradigm representing polarized extremities of this functional spectrum [11]. In chronic inflammation, this polarization is not binary but rather a dynamic process where macrophages can adopt diverse functional phenotypes influenced by tissue-specific microenvironments [1]. The M1 phenotype, driven by interferon-γ (IFN-γ) and microbial products like lipopolysaccharide (LPS), promotes inflammation through the production of pro-inflammatory cytokines and reactive oxygen species [1] [20]. Conversely, the M2 phenotype, induced by IL-4, IL-13, IL-10, or glucocorticoids, contributes to inflammation resolution, tissue repair, and immunoregulation [1] [20].
Chronic inflammatory diseases typically exhibit an imbalance in macrophage polarization, with a predominant M1 response driving tissue damage and pathology [14]. In rheumatoid arthritis, for instance, increased M1 macrophages in synovial tissue produce TNF-α and IL-6 that perpetuate inflammation and joint destruction [14]. Similarly, in ulcerative colitis, infiltrating macrophages exacerbate mucosal injury through pro-inflammatory mediators [92]. Understanding and quantifying these polarization states through specific biomarkers is therefore essential for both basic research and therapeutic development.
Core Biomarkers for Phenotype Identification
Surface Markers: Expression and Significance
Cell surface markers provide definitive signatures for distinguishing macrophage polarization states. These markers can be quantitatively assessed using flow cytometry or immunohistochemistry, enabling precise phenotypic characterization in both in vitro and in vivo settings.
Table 1: Surface Markers for Macrophage Phenotype Identification
| Surface Marker | Macrophage Phenotype | Expression Level | Function and Significance |
|---|---|---|---|
| CD80 | M1 | High | Co-stimulatory molecule that promotes T-cell activation; indicates pro-inflammatory state [14] [20] |
| CD86 | M1 | High | Co-stimulatory molecule that binds CD28 on T-cells; enhances inflammatory responses [14] [20] |
| CD206 (Mannose Receptor) | M2 | High | Phagocytic receptor for glycoproteins; mediates endocytosis; marker of alternative activation [14] [20] |
| CD163 | M2 | High | Scavenger receptor for hemoglobin-haptoglobin complexes; associated with anti-inflammatory functions [14] [20] |
The utility of these markers extends beyond simple classification, as their expression patterns often correlate with disease activity and treatment response. For example, in head and neck squamous cell carcinomas, high infiltration of CD163+ M2 macrophages is associated with poor overall survival [96]. Similarly, in diabetic cardiomyopathy, M1 macrophage polarization marked by CD80/CD86 expression promotes inflammation and disease progression [95].
Cytokine Secretion Profiles
Beyond surface markers, macrophages exhibit distinct cytokine secretion patterns that define their functional capabilities. These soluble mediators not only reflect polarization status but also actively shape the inflammatory microenvironment.
Table 2: Characteristic Cytokine Profiles of Polarized Macrophages
| Cytokine/Chemokine | M1 Macrophages | M2 Macrophages | Primary Function |
|---|---|---|---|
| TNF-α | High secretion | Low secretion | Pro-inflammatory mediator; activates endothelial cells [92] [1] |
| IL-6 | High secretion | Low secretion | Promotes acute phase response; contributes to chronic inflammation [92] [14] |
| IL-1β | High secretion | Low secretion | Pyrogenic cytokine; amplifies inflammatory cascades [92] [1] |
| IL-12 | High secretion | Low secretion | Drives Th1 differentiation; links innate and adaptive immunity [96] [1] |
| IL-10 | Low secretion | High secretion | Potent anti-inflammatory cytokine; suppresses M1 functions [92] [14] |
| TGF-β | Low secretion | High secretion | Immunosuppressive; promotes tissue repair and fibrosis [92] [14] |
| CCL17 | Low secretion | High secretion | Chemoattractant for Th2 cells; recruits alternative activation partners [1] |
The balance between these pro- and anti-inflammatory mediators dictates the overall impact of macrophages in chronic inflammation. In conditions like ulcerative colitis, the persistent production of M1-associated cytokines (TNF-α, IL-1β, IL-6) perpetuates mucosal damage and barrier dysfunction [92]. Therapeutic strategies that shift this balance toward M2-associated cytokines (IL-10, TGF-β) represent promising approaches for resolving chronic inflammation [92] [14].
Experimental Protocols for Phenotype Identification
Flow Cytometry for Surface Marker Analysis
Flow cytometry represents the gold standard for quantitative assessment of macrophage surface markers, allowing simultaneous evaluation of multiple targets at the single-cell level.
Sample Preparation and Staining Protocol
Cell Harvesting and Washing:
- Harvest macrophages using gentle cell scraping or enzymatic dissociation (e.g., Accutase or non-enzymatic cell dissociation buffers).
- Wash cells twice with cold flow cytometry buffer (PBS + 1% BSA + 0.1% sodium azide).
- Count cells and adjust concentration to 1-5×10^6 cells/mL [97].
Fc Receptor Blocking:
- Resuspend cell pellet in flow cytometry buffer containing Fc block (e.g., anti-CD16/32 for mouse cells or human Fc receptor binding inhibitor).
- Incubate for 10-15 minutes on ice to prevent non-specific antibody binding [97].
Surface Antigen Staining:
- Add fluorochrome-conjugated antibodies against target markers (CD80, CD86, CD206, CD163) at predetermined optimal concentrations.
- Include appropriate isotype controls for each antibody to establish background staining levels.
- Vortex gently and incubate for 30 minutes in the dark at 4°C [97].
Washing and Fixation:
- Wash cells twice with cold flow cytometry buffer to remove unbound antibody.
- Resuspend in fixation buffer (1-4% paraformaldehyde in PBS) for intracellular staining or analysis delay.
- For immediate analysis, resuspend in flow cytometry buffer with viability dye if needed [97].
Data Acquisition and Analysis:
- Acquire data using a flow cytometer equipped with appropriate lasers and filters.
- Use forward and side scatter to gate on single, viable cells.
- Analyze fluorescence using histogram overlays and contour plots comparing isotype controls and stained samples.
- Report results as geometric mean fluorescence intensity (MFI) or percentage of positive cells [97].
Multicolor Panel Design Considerations
When designing multicolor panels for macrophage phenotyping:
- Include CD45 to confirm hematopoietic origin
- Incorporate viability dyes to exclude dead cells
- Balance fluorochrome brightness with antigen density
- Validate panel with compensation controls to address spectral overlap
- Consider including additional markers (MHC II, CD64, CD11b) for more comprehensive immunophenotyping [97]
Cytokine Profiling Methods
Enzyme-Linked Immunosorbent Assay (ELISA)
ELISA provides sensitive, quantitative measurement of specific cytokines in cell culture supernatants, tissue homogenates, or biological fluids.
Sample Collection and Preparation:
- Collect cell culture supernatants by centrifugation (500×g for 5 minutes) to remove cells and debris.
- Aliquot and store samples at -80°C if not testing immediately.
- Avoid repeated freeze-thaw cycles to preserve cytokine integrity [98].
Assay Procedure:
- Add samples and standards to pre-coated 96-well plates in duplicate or triplicate.
- Incubate according to manufacturer's instructions (typically 2 hours at room temperature).
- Wash plates thoroughly between each incubation step to remove unbound proteins.
- Add detection antibody, followed by enzyme conjugate (e.g., streptavidin-HRP).
- Develop with substrate solution (e.g., TMB) and measure absorbance using a plate reader [98].
Data Analysis:
- Generate standard curves using recombinant cytokines with known concentrations.
- Calculate sample concentrations by interpolating from the standard curve.
- Normalize to total protein content or cell number as appropriate [98].
Multiplex Immunoassays
For comprehensive cytokine profiling, multiplex assays enable simultaneous quantification of multiple analytes from a single sample.
ProcartaPlex Multiplex Immunoassays:
- Utilize magnetic beads conjugated with capture antibodies for multiple targets.
- Incubate with samples, followed by detection antibodies and streptavidin-PE.
- Analyze using a Luminex instrument with distinct fluorescent signatures for each bead region [98].
ProQuantum High-Sensitivity Assays:
- Employ proximity-based amplification technology for enhanced sensitivity.
- Combine antigen-antibody binding with qPCR signal amplification.
- Require minimal sample volume while providing broad dynamic range [98].
Signaling Pathways Regulating Macrophage Polarization
The polarization of macrophages is governed by intricate signaling networks that translate microenvironmental cues into distinct phenotypic programs. Understanding these pathways is essential for contextualizing biomarker expression within the broader framework of chronic inflammation.
Diagram 1: Signaling Pathways in Macrophage Polarization. M1 polarization is driven by IFN-γ and LPS through STAT1 and NF-κB activation, resulting in pro-inflammatory cytokine production. M2 polarization is induced by IL-4/IL-13 and IL-10 via STAT6, STAT3, and PPARγ pathways, leading to anti-inflammatory mediator expression [1] [20].
The JAK/STAT pathway represents a central signaling axis in macrophage polarization. STAT1 activation promotes M1 polarization, while STAT3 and STAT6 drive M2 differentiation [20]. Concurrently, the NF-κB pathway serves as a "master switch" for M1-associated pro-inflammatory gene expression, with TLR4 recognition of LPS triggering downstream signaling through both MyD88-dependent and TRIF-dependent pathways [1] [20]. The PI3K/Akt pathway further modulates macrophage polarization, integrating metabolic and inflammatory signals to fine-tune phenotypic outcomes [20].
In chronic inflammation, these signaling pathways are frequently dysregulated, creating self-reinforcing loops that maintain pathological macrophage activation states. Therapeutic targeting of these pathways represents a promising strategy for resetting macrophage polarization in diseases such as rheumatoid arthritis, where shifting the balance from M1 to M2 phenotypes can ameliorate disease pathology [14].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Macrophage Phenotype Studies
| Reagent Category | Specific Examples | Research Application |
|---|---|---|
| Polarization Inducers | IFN-γ, LPS, IL-4, IL-13, IL-10 | Directing macrophage differentiation toward specific phenotypes in vitro [96] [1] |
| Flow Cytometry Antibodies | Anti-CD80, CD86, CD206, CD163 | Surface marker detection and quantification by flow cytometry [96] [14] |
| ELISA Kits | TNF-α, IL-6, IL-1β, IL-10, TGF-β | Quantitative measurement of cytokine secretion profiles [98] |
| Multiplex Assay Panels | ProcartaPlex Inflammation Panels | Simultaneous quantification of multiple cytokines from limited samples [98] |
| Cell Culture Media | RPMI-1640, DMEM with M-CSF | Monocyte differentiation and macrophage maintenance [96] |
| Signal Pathway Inhibitors | STAT inhibitors, NF-κB inhibitors, PI3K/Akt inhibitors | Mechanistic studies of polarization pathways [14] [20] |
Advanced Methodologies and Workflow Integration
To comprehensively characterize macrophage polarization in chronic inflammation research, we recommend an integrated workflow that combines multiple methodological approaches.
Diagram 2: Integrated Workflow for Macrophage Phenotype Analysis. A comprehensive approach combining surface marker detection, cytokine profiling, and functional validation provides robust phenotypic characterization in chronic inflammation research.
This integrated workflow enables researchers to:
- Correlate surface marker expression with functional outputs through parallel assessment of receptor expression and cytokine secretion
- Validate phenotypic classifications through functional assays including phagocytosis, metabolic profiling, and signaling pathway activity
- Contextualize findings within disease-specific mechanisms by examining polarization states in relevant chronic inflammation models
The precise identification of macrophage phenotypes through surface markers (CD80, CD86, CD206, CD163) and cytokine profiles represents an essential methodology in chronic inflammation research. As our understanding of macrophage plasticity deepens, these biomarkers provide critical insights into disease mechanisms, progression, and therapeutic responses. The integrated experimental approaches outlined in this technical guide—encompassing flow cytometry, cytokine detection, and signaling pathway analysis—offer researchers robust tools for elucidating the complex roles of macrophages in chronic inflammatory diseases. Through the continued refinement of these methodologies and their application in both basic and translational contexts, we advance toward more targeted interventions capable of modulating macrophage polarization for therapeutic benefit.
Comparative Analysis of Polarization Profiles in Rheumatoid Arthritis, Atherosclerosis, Obesity, and Osteoarthritis
Macrophage polarization represents a critical mechanism in the pathogenesis of chronic inflammatory diseases. The dynamic plasticity of macrophages, allowing them to adopt pro-inflammatory (M1) or anti-inflammatory/pro-resolving (M2) phenotypes, underpins their dual roles in both driving and resolving inflammation across various pathological contexts [68]. This review provides a comprehensive comparative analysis of macrophage polarization profiles in four prevalent chronic inflammatory conditions: rheumatoid arthritis (RA), atherosclerosis, obesity, and osteoarthritis (OA). By examining the distinct and shared polarization mechanisms across these diseases, we aim to illuminate core pathophysiological principles and highlight emerging therapeutic targets within the framework of macrophage biology. Understanding these nuanced polarization profiles provides a foundation for developing precision therapies that modulate macrophage function to restore immune homeostasis.
The balance between M1 and M2 macrophage polarization varies significantly across chronic inflammatory conditions, contributing to disease-specific pathological trajectories. The table below summarizes the characteristic polarization profiles and their functional consequences in RA, atherosclerosis, obesity, and OA.
Table 1: Comparative Analysis of Macrophage Polarization in Chronic Inflammatory Diseases
| Disease | Predominant Polarization | Key Polarizing Signals | Major Functional Outcomes | References |
|---|---|---|---|---|
| Rheumatoid Arthritis (RA) | M1 Dominance | TNF-α, IFN-γ, LPS, exosomal circRNAs | Synovitis, cartilage/bone erosion, pro-inflammatory cytokine release (IL-1β, TNF-α, IL-6) | [99] [100] [101] |
| Atherosclerosis | Spatial Dynamics (M1 in unstable plaques) | oxLDL, IFN-γ, IL-4, m6A modification | Plaque instability (M1), foam cell formation, tissue repair & plaque stabilization (M2) | [102] [103] [44] |
| Obesity | Adipose Tissue M1 Skewing | Saturated fatty acids, LPS, metabolic intermediates (e.g., lactate) | Adipose tissue inflammation, insulin resistance, impaired thermogenesis | [36] |
| Osteoarthritis (OA) | Synovial M1/M2 Imbalance | DAMPs, TNF-α, IL-1β, TGF-β | Synovitis, cartilage catabolism, oxidative stress, failed tissue repair | [104] [105] |
Disease-Specific Molecular Mechanisms and Signaling Pathways
Rheumatoid Arthritis: Transcriptional and Epigenetic Regulation
In RA, the pronounced M1 polarization is driven by a complex interplay of signaling pathways and novel epigenetic mechanisms. The JAK-STAT and NF-κB pathways are activated by cytokines like IFN-γ and TNF-α, promoting transcription of pro-inflammatory M1 genes [68]. Recent research has identified critical regulatory nodes, such as the transcription factor KLF11, which is significantly downregulated in RA synovium. KLF11 exerts a protective effect by binding to the YAP1 promoter and suppressing its expression, thereby inhibiting the ERK signaling pathway and subsequent M1 polarization [101]. Furthermore, post-transcriptional regulation via m6A modification of non-coding RNAs is a emerging mechanism. In fibroblast-like synoviocytes (FLSs), the protein WTAP binds to circular RNA circ-CBLB, enhancing its m6A modification and degradation. This reduction in exosomal circ-CBLB promotes macrophage polarization toward the pro-inflammatory M1 phenotype, creating a vicious cycle of inflammation [100].
Atherosclerosis: Metabolic Integration and Plaque Microenvironment
Atherosclerosis exemplifies the intricate coupling of metabolic dysregulation and inflammation in macrophage polarization. M1 macrophages are predominantly found in unstable shoulder regions of plaques, where they secrete pro-inflammatory cytokines (IL-1, IL-6, TNF-α) and matrix metalloproteinases (MMPs), contributing to plaque rupture [102] [103]. In contrast, M2 macrophages, often located in stable plaque areas or the adventitia, promote tissue repair and plaque stability via IL-10 and TGF-β [103]. The uptake of oxidized low-density lipoprotein (oxLDL) by macrophages is a seminal event, leading to foam cell formation and creating a pro-inflammatory lipid milieu that skews polarization toward M1 [102] [44]. The m6A RNA modification has been identified as a key regulator, influencing the polarization process by modulating the transcriptome of macrophages within the atherosclerotic plaque [103].
Obesity: Metabolic Reprogramming of Adipose Tissue Macrophages
In obesity, adipose tissue macrophages undergo metabolic reprogramming that underlies their functional polarization. A central feature is a shift from oxidative phosphorylation (OXPHOS), characteristic of M2 macrophages, toward aerobic glycolysis in pro-inflammatory M1 macrophages [36]. This metabolic switch is driven by microenvironmental cues such as saturated fatty acids and DAMPs, which activate TLR and NLRP3 inflammasome signaling, reinforcing the M1 phenotype [36] [68]. The resulting M1-skewed population secretes cytokines like TNF-α that impair insulin signaling in adipocytes, establishing a feed-forward loop of metabolic dysfunction and chronic, low-grade inflammation [36].
Osteoarthritis: Synovial Inflammation and Chondrocyte Crosstalk
In OA, synovial macrophages are key drivers of disease progression through their interaction with chondrocytes. M1 macrophages in the synovium release catabolic mediators, including IL-1β, TNF-α, MMPs, and ADAMTS-5, which directly contribute to cartilage degradation [104] [105]. This inflammatory milieu pushes chondrocytes toward a catabolic phenotype, further amplifying the breakdown of the extracellular matrix [104]. The imbalance toward M1 dominance disrupts joint homeostasis, while the anti-inflammatory and anabolic activities of M2 macrophages are insufficient to counteract this process. The ratio of M1 to M2 macrophages in the synovium is therefore a critical determinant of OA severity, making modulation of this balance a promising therapeutic strategy [105].
Experimental Models and Methodologies for Studying Polarization
In Vitro Models of Human Macrophage Polarization
Standardized in vitro protocols are essential for investigating the molecular mechanisms of human macrophage polarization. A common approach involves using the human THP-1 monocytic cell line.
Protocol: Induction and Validation of M1/M2 Macrophages from THP-1 Cells
Differentiation into Macrophages (M0):
Polarization to Specific Phenotypes:
- M1 Polarization: Differentiated M0 macrophages are stimulated for 24-48 hours with a cocktail of 100 ng/mL Lipopolysaccharide (LPS) and 20-50 ng/mL Interferon-gamma (IFN-γ) [101].
- M2 Polarization: M0 macrophages are stimulated for 24-48 hours with 20 ng/mL Interleukin-4 (IL-4) or IL-13.
Phenotype Validation:
- Surface Markers (Flow Cytometry): M1 macrophages are characterized by high expression of CD86 and CD16/32. M2 macrophages (specifically M2a) show high expression of CD206 [103] [101].
- Gene/Protein Expression (qPCR, Western Blot, Immunofluorescence):
- Cytokine Secretion (ELISA): Confirmation via measurement of M1-associated cytokines (TNF-α, IL-6, IL-12) or M2-associated cytokines (IL-10, TGF-β) in the cell culture supernatant [101].
In Vivo Models and Functional Assessment
Animal models are indispensable for studying the role of macrophage polarization in disease contexts and evaluating therapeutic interventions.
- Rheumatoid Arthritis: The Collagen-Induced Arthritis (CIA) model in DBA/1 mice is a gold standard. Mice are immunized with type II collagen emulsified in Complete Freund's Adjuvant. Disease severity is scored clinically (0-4 per paw, maximum 16 per mouse), and joint destruction is assessed histologically by Hematoxylin & Eosin (H&E) and Safranin O staining [101].
- Atherosclerosis: The ApoE-/- or Ldlr-/- mouse models on a high-fat diet are widely used. Plaque burden and composition are analyzed through histology (Oil Red O for lipids, trichrome for collagen), and macrophage phenotypes within plaques are characterized by immunofluorescence for markers like iNOS (M1) and CD206 (M2) [102] [103].
- Osteoarthritis: The destabilization of the medial meniscus (DMM) model in mice is a common post-traumatic OA model. Synovitis and cartilage degradation are scored using the OARSI system, and macrophage infiltration in the synovium is assessed via immunohistochemistry for F4/80 (pan-macrophage) and phenotype-specific markers [104].
Visualization of Key Signaling Pathways
The following diagrams, generated using Graphviz DOT language, illustrate core signaling pathways that regulate macrophage polarization in these chronic inflammatory diseases.
Core M1/M2 Macrophage Polarization Signaling
Figure 1: Core signaling pathways driving M1 and M2 macrophage polarization. M1 polarization is triggered by LPS, IFN-γ, and TNF-α, activating TLR/NF-κB and JAK/STAT1 pathways. M2 polarization is induced by IL-4/IL-13, signaling primarily through the IL-4R/JAK/STAT6/PPAR-γ axis [103] [68].
Molecular Regulation of Polarization in Rheumatoid Arthritis
Figure 2: Novel molecular mechanisms regulating M1 macrophage polarization in RA. The WTAP-mediated m6A modification degrades exosomal circ-CBLB, promoting M1 polarization [100]. Separately, low KLF11 expression fails to repress YAP1, leading to ERK pathway activation and enhanced M1 polarization [101].
The Scientist's Toolkit: Essential Research Reagents
The following table catalogues critical reagents and tools for investigating macrophage polarization in the context of these chronic inflammatory diseases.
Table 2: Essential Research Reagents for Studying Macrophage Polarization
| Reagent / Tool | Specific Example(s) | Primary Function in Research | Application Context |
|---|---|---|---|
| Polarization Inducers | LPS, IFN-γ, PMA, IL-4, IL-13 | Differentiate and polarize monocytes/macrophages into M1 or M2 phenotypes in vitro. | Universal for in vitro polarization studies [100] [101]. |
| Cell Lines | THP-1 (human monocytic) | Provide a consistent, renewable source of human monocytes for in vitro polarization assays. | Standard in vitro model for human macrophage biology [100] [101]. |
| Cytokine ELISA Kits | TNF-α, IL-1β, IL-6, IL-10 | Quantify secreted cytokine levels to validate macrophage phenotype and inflammatory status. | Phenotype validation in vitro and in vivo (serum, tissue homogenates) [101]. |
| Flow Cytometry Antibodies | Anti-human: CD86, CD80, iNOS (M1); CD206, CD163 (M2) | Identify and sort macrophage subpopulations based on surface and intracellular markers. | Phenotypic quantification from in vitro cultures or digested tissues [103] [101]. |
| Animal Models | CIA (DBA/1 mice), ApoE-/- mice, DMM model | Model human chronic inflammatory diseases in a complex in vivo system for pathophysiological and therapeutic studies. | RA, Atherosclerosis, OA research [102] [101]. |
| Gene Manipulation Tools | siRNA/shRNA (e.g., against KLF11, WTAP), overexpression plasmids (e.g., KLF11, YAP1) | Functionally interrogate the role of specific genes in regulating macrophage polarization. | Mechanistic studies (in vitro and in vivo) [100] [101]. |
| Histology Stains & Antibodies | H&E, Safranin O, Anti-F4/80, Anti-iNOS, Anti-CD206 | Visualize tissue pathology, macrophage infiltration, and phenotype in situ. | Analysis of joint, plaque, or adipose tissue sections from animal models or human samples [102] [101]. |
Macrophages, central mediators of innate immunity, exhibit remarkable functional plasticity by dynamically polarizing into distinct functional states in response to microenvironmental cues [68]. This polarization spans a spectrum with pro-inflammatory (M1) and anti-inflammatory (M2) macrophages representing polar opposites that play critical yet opposing roles in chronic inflammation [1]. The M1/M2 balance significantly influences disease progression, making the targeted regulation of macrophage polarization a promising therapeutic strategy for chronic inflammatory diseases, autoimmune disorders, and cancer [106]. Assessing therapeutic efficacy requires a multidisciplinary approach that begins with in vitro macrophage culture systems and progresses through predictive in vitro bioactivity assays before final validation in complex pre-clinical animal models. This technical guide provides a comprehensive framework for this tiered assessment strategy, emphasizing the critical methodological considerations at each stage to ensure reliable, reproducible, and clinically translatable results.
Fundamentals of Macrophage Polarization
Macrophage Subsets and Polarization States
Macrophages originate from two primary lineages: tissue-resident macrophages (TRMs) derived from embryonic precursors, and monocyte-derived macrophages (MoMFs) that differentiate from circulating monocytes [68]. When exposed to specific microenvironmental signals, these macrophages undergo polarization into specialized functional phenotypes:
M1 Macrophages: Polarized by Th1 cytokines (IFN-γ, TNF-α) or microbial products (LPS) [68] [1]. They exhibit a pro-inflammatory profile characterized by high production of IL-1β, IL-6, IL-12, TNF-α, and iNOS (NOS2) [29] [6]. M1 macrophages inhibit tumor growth and promote chronic inflammation through metabolic reprogramming toward glycolysis, the pentose phosphate pathway, and fatty acid synthesis [6].
M2 Macrophages: Activated by Th2 cytokines (IL-4, IL-13, IL-10) [68] [1]. They display an anti-inflammatory profile associated with tissue repair, angiogenesis, and pro-tumor functions [68]. The M2 category encompasses several subtypes:
- M2a: Induced by IL-4 or IL-13, characterized by high CD206 expression and profibrotic activity [68]
- M2b: Activated by immune complexes and TLR ligands, producing both pro- and anti-inflammatory cytokines [68] [29]
- M2c: Stimulated by glucocorticoids or IL-10, primarily immunosuppressive [29]
- M2d/TAMs: Tumor-associated macrophages that promote angiogenesis and metastasis [29]
Table 1: Characteristic Markers of Macrophage Polarization States
| Polarization State | Inducing Signals | Surface Markers | Cytokine/Chemokine Secretion | Metabolic Pathway |
|---|---|---|---|---|
| M1 | IFN-γ, LPS, TNF-α | CD80, CD86 | High: IL-1β, IL-6, IL-12, TNF-α, CXCL9, CXCL10 | Glycolysis, PPP, FAS |
| M2a | IL-4, IL-13 | CD206 | High: CCL17, CCL18, CCL22, IL-10, TGF-β | OXPHOS, FAO |
| M2b | Immune complexes + TLR ligands | CD86 | High: IL-10, IL-1β, TNF-α | OXPHOS, FAO |
| M2c | IL-10, glucocorticoids | CD163, CD206 | High: IL-10, TGF-β | OXPHOS, FAO |
| M2d/TAMs | TLR ligands + A2AR agonists | VEGF, IL-10 | High: IL-10, VEGF, TGF-β | Glycolysis, OXPHOS |
Signaling Pathways Regulating Macrophage Polarization
Macrophage polarization is governed by intricate signaling networks that translate extracellular cues into distinct transcriptional and metabolic programs:
M1-Polarizing Pathways: IFN-γ binding to IFNGR activates JAK-STAT1 signaling [1]. LPS recognition by TLR4 triggers both MyD88-dependent activation of NF-κB and MAPK pathways, and TRIF-dependent IRF3 activation [1]. These pathways collectively drive expression of pro-inflammatory genes.
M2-Polarizing Pathways: IL-4/IL-13 binding to IL-4Rα activates JAK-STAT6 signaling, often cooperating with IRF4 and PPARγ [68] [6] [1]. IL-10 engagement of IL-10R initiates STAT3 activation, promoting anti-inflammatory gene expression [1]. Glucocorticoid receptor signaling also contributes to M2 polarization [1].
The following diagram illustrates the core signaling pathways driving macrophage polarization:
In Vitro Macrophage Culture Systems
Establishing Representative Macrophage Cultures
In vitro macrophage culture systems provide controlled environments for initial therapeutic screening and mechanistic studies. Several established models are available:
Cell Line-Based Models: The RAW 264.7 murine macrophage cell line offers reproducibility and convenience for high-throughput screening [107]. THP-1 human monocytic cells can be differentiated into macrophages using phorbol esters (PMA) and subsequently polarized [6]. These systems provide uniform, scalable platforms but may not fully recapitulate primary macrophage biology.
Primary Macrophage Cultures: Bone marrow-derived macrophages (BMDMs) from mice offer greater physiological relevance and are preferred for translational studies [6]. Human monocyte-derived macrophages from peripheral blood provide species-specific data but show donor-dependent variability.
Critical Considerations for Culture Conditions
Culture media composition significantly impacts macrophage viability, phenotype, and responsiveness to polarization cues [108]. Key considerations include:
Serum Requirements: Macrophages require serum for survival, with viability markedly decreased in serum-free skin differentiation media [108]. However, high serum concentrations can interfere with keratinocyte differentiation in co-culture systems [108].
Media Additives: Calcium concentrations above 1 mM promote keratinocyte differentiation in skin co-culture models [108]. Growth factors (KGF), vitamin C, and specific amino acids (L-carnitine, L-serine) support skin maturation but may affect immune cell function [108].
Metabolic Considerations: Media formulations should accommodate the distinct metabolic requirements of polarized macrophages - M1 macrophages rely heavily on glycolysis, while M2 macrophages preferentially utilize oxidative phosphorylation [29] [6].
Table 2: Research Reagent Solutions for Macrophage Culture and Polarization
| Reagent Category | Specific Examples | Function/Application | Considerations |
|---|---|---|---|
| Polarizing Cytokines | IFN-γ, LPS (M1); IL-4, IL-13, IL-10 (M2) | Induce specific macrophage polarization states | Concentration optimization required; LPS source affects potency |
| Cell Culture Media | RPMI, DMEM, specialized macrophage media | Support macrophage viability and function | Serum concentration critical; affects polarization capacity [108] |
| Differentiation Agents | PMA (for THP-1 cells), M-CSF (for BMDMs) | Differentiate monocytes into macrophages | Concentration and duration affect maturation state |
| Polarization Markers | Anti-CD86, anti-CD206, anti-CD80, anti-CD163 | Identify polarization states via flow cytometry | Validate antibody specificity for species used |
| Metabolic Probes | 2-NBDG (glucose uptake), MitoTracker | Assess metabolic reprogramming | Correlate with functional assays |
| Signaling Inhibitors | MEK inhibitors, HDAC inhibitors, STAT inhibitors | Mechanistic studies and therapeutic targeting | Confirm specificity; assess viability effects |
Assessing Polarization and Therapeutic Efficacy In Vitro
Standardized Macrophage Polarization Assays
A well-standardized in vitro macrophage assay enables reliable ranking of therapeutic efficacy across different preparations [107]. The following workflow outlines a robust approach for assessing anti-inflammatory activity:
Methodological Protocol: In Vitro Macrophage Anti-inflammatory Assay
Objective: To assess the efficacy of therapeutic compounds (e.g., anti-inflammatory exosomes, small molecule inhibitors) in suppressing M1 macrophage polarization [107].
Materials:
- RAW 264.7 macrophages or primary bone marrow-derived macrophages
- Complete culture media (RPMI 1640 with 10% FBS for RAW 264.7)
- LPS (E. coli O111:B4, 1-10 ng/mL working concentration)
- Therapeutic test compounds (e.g., MSC-derived exosomes, kinase inhibitors)
- Dexamethasone (10-100 nM as positive control)
- ELISA kits for IL-6 and TNF-α
- RNA extraction kit and qPCR reagents
- Cell culture plates (96-well for ELISA, 12-well for RNA)
Procedure:
- Cell Preparation: Thaw and culture RAW 264.7 macrophages, maintaining cells in logarithmic growth phase. Create a cell bank for reproducible assays [107].
- Plating: Seed cells at standardized density (optimized for 50-70% confluency at time of stimulation) in complete medium.
- Treatment: Pre-treat cells with therapeutic compounds for 1-2 hours before LPS stimulation.
- Polarization: Stimulate macrophages with LPS at optimized concentration (1-10 ng/mL) to induce M1 polarization. Avoid excessive LPS concentrations (>10 ng/mL) that may overwhelm therapeutic effects [107].
- Incubation: Culture for 4 hours for IL-6 protein measurement by ELISA, or 6 hours for cytokine mRNA quantification by qPCR [107].
- Analysis:
- ELISA: Collect culture supernatants and measure IL-6 and TNF-α levels according to manufacturer protocols.
- qPCR: Extract RNA, synthesize cDNA, and quantify expression of M1 markers (TNF-α, IL-1β, IL-6, iNOS) and M2 markers (Arg1, Ym1, Fizz1) for comprehensive polarization assessment.
- Viability: Assess cell viability using MTT or similar assays to exclude cytotoxic effects.
Validation: Include dexamethasone as positive control for anti-inflammatory activity, expected to suppress IL-6 production by approximately 60% at 4 hours [107].
Comprehensive Polarization Assessment
Beyond cytokine measurement, thorough polarization assessment should include:
- Surface Marker Analysis: Flow cytometry for M1 (CD80, CD86) and M2 (CD206, CD163) markers [68] [29]
- Metabolic Profiling: Extracellular flux analysis to measure glycolytic rates and oxidative phosphorylation [29] [6]
- Global Omics Approaches: Proteomic and phosphoproteomic analyses provide unbiased insights into polarization states and therapeutic mechanisms [6]
Metabolic Reprogramming in Macrophage Polarization
Metabolic Signatures of Polarized Macrophages
Macrophage polarization is intrinsically linked to metabolic reprogramming, which both enables and sustains their functional states:
M1 Metabolism: Characterized by a shift toward aerobic glycolysis (Warburg effect) even under normoxic conditions [29] [6]. Key features include:
- Increased glucose uptake via GLUT1 and GLUT6
- Enhanced pentose phosphate pathway activity generating NADPH
- Disrupted TCA cycle with accumulation of citrate, succinate, and itaconate
- Fatty acid synthesis supporting membrane biogenesis and inflammatory mediator production
- HIF-1α stabilization promoting inflammatory gene expression
M2 Metabolism: Dominated by oxidative phosphorylation and mitochondrial metabolism:
- Intact TCA cycle coupled to electron transport chain
- Enhanced fatty acid oxidation supporting energy production
- Increased glutamine metabolism replenishing TCA intermediates
- UCP2-mediated mitochondrial uncoupling reducing ROS production
Table 3: Metabolic Pathways in Macrophage Polarization
| Metabolic Pathway | M1 Macrophages | M2 Macrophages |
|---|---|---|
| Glycolysis | Enhanced | Basal |
| Oxidative Phosphorylation | Suppressed | Enhanced |
| Pentose Phosphate Pathway | Activated | Basal |
| Fatty Acid Synthesis | Enhanced | Suppressed |
| Fatty Acid Oxidation | Suppressed | Enhanced |
| TCA Cycle | Broken (succinate, citrate accumulation) | Intact |
| Glutamine Metabolism | Anaplerotic | Major energy source |
| ATP Production | Glycolysis-dependent | OXPHOS-dependent |
Assessing Metabolic Reprogramming
Methodologies for evaluating macrophage metabolic states:
- Extracellular Flux Analysis: Real-time measurement of glycolytic rates (ECAR) and mitochondrial respiration (OCR) using Seahorse or similar platforms
- Metabolomic Profiling: LC-MS based quantification of intracellular metabolites and pathway intermediates
- Glucose Uptake Assays: Fluorescent glucose analogs (2-NBDG) to measure glucose transporter activity
- Enzyme Activity Assays: Measure key metabolic enzyme activities (PKM2, HIF-1α, ACLY) [70]
Transitioning to Pre-Clinical Animal Models
Model Selection Considerations
Pre-clinical animal models provide essential assessment of therapeutic efficacy in complex physiological environments. Selection criteria should include:
- Species Considerations: Mouse models offer genetic tractability and established methodologies; humanized models may be needed for species-specific therapeutics
- Disease Relevance: Models should recapitulate key aspects of human chronic inflammatory conditions
- Macrophage Compartment: Consider model-specific differences in macrophage biology between mice and humans
- Practical Constraints: Resource availability, technical expertise, and ethical considerations
Improving Predictive Value and Translation
Systematic reviews reveal significant limitations in current pre-clinical models, with poor prediction of clinical outcomes [109] [110]. Key strategies to enhance translational value:
- Model Diversity: Utilize multiple complementary models rather than relying on a single system
- Reporting Standards: Adhere to ARRIVE guidelines for comprehensive methodology reporting [110]
- Experimental Design: Implement randomization, blinding, and appropriate statistical powering [110]
- Clinical Relevance: Consider route of administration, dosing schedules, and therapeutic windows relevant to human applications
The tiered assessment of therapeutic efficacy from in vitro macrophage cultures to pre-climental animal models provides a robust framework for evaluating compounds that modulate macrophage polarization. Success requires careful attention to methodological standardization at each stage, particularly in culture conditions, polarization validation, and metabolic assessments. As the field advances, integrating more sophisticated humanized models and improving pre-clinical reporting standards will enhance the translational potential of macrophage-targeted therapies for chronic inflammatory diseases.
Within the broader research on mechanisms of macrophage polarization in chronic inflammation, a critical translational objective is to establish clear, evidence-based correlations between specific macrophage phenotypes and clinical disease outcomes. Macrophages, central to innate immunity, demonstrate remarkable plasticity, polarizing into distinct functional phenotypes—classically activated pro-inflammatory M1 or alternatively activated anti-inflammatory M2—in response to microenvironmental cues [75] [1]. The imbalance between these phenotypes is a hallmark of chronic inflammatory diseases [75]. This guide synthesizes clinical evidence from recent patient cohort studies, providing researchers and drug development professionals with a structured analysis of how specific macrophage polarization patterns directly correlate with disease severity, progression, and exacerbation across multiple pathologies. By integrating quantitative clinical data with detailed experimental methodologies, this review aims to furnish the scientific community with a robust framework for evaluating macrophage phenotypes as biomarkers and therapeutic targets.
Macrophage Polarization: Phenotypes and Clinical Significance
Macrophage polarization represents a functional spectrum. The pro-inflammatory M1 phenotype, induced by stimuli like IFN-γ and LPS, is characterized by high production of cytokines such as TNF-α, IL-1β, and IL-6, and expression of iNOS, contributing to host defense and tissue damage [75] [111]. Conversely, the M2 phenotype, induced by IL-4, IL-13, or IL-10, upregulates arginase-1 (Arg1), CD206, and CD163, promoting tissue repair, immunoregulation, and resolution of inflammation [75] [1]. The M2 phenotype can be further subdivided into M2a, M2b, and M2c subsets, each with unique functional roles in disease contexts [75] [112].
Critically, the shift from a balanced state to a dominant M1 or M2 phenotype is intricately linked to disease pathogenesis. The following sections and tables summarize the clinical evidence establishing these correlations in patient cohorts.
Quantitative Clinical Evidence from Patient Cohorts
Evidence from clinical studies across diverse diseases consistently demonstrates that specific shifts in macrophage polarization are quantifiable indicators of disease state.
Key Clinical Correlations
Table 1: Correlations between Macrophage Phenotypes and Disease Severity in Clinical Cohorts
| Disease | Patient Cohort | Phenotype Correlation | Measured Outcome | Citation |
|---|---|---|---|---|
| Childhood Asthma | 51 asthmatic children vs. 27 normal controls [112] | ↑ M2a, M2b, M2c; ↓ M1 in moderate vs. mild | Severity (GINA criteria); Hospitalization | [112] |
| Childhood Asthma | Subgroups by severity [112] | ↓ M1; ↑ M2c in moderate asthma | Disease Severity | [112] |
| Childhood Asthma | Subgroups by exacerbation [112] | ↓ PM-2K+CD14+ cells & M1; ↑ M2c | Requirement for Hospitalization | [112] |
| Rheumatoid Arthritis (RA) | RA patients [75] | ↑ M1/M2 Ratio | Synovial inflammation, joint damage | [75] |
| Chronic Rhinosinusitis with Nasal Polyps (CRSwNP) | 75 CRSwNP patients vs. 28 controls [113] | ↑ M2 Macrophages | Polyp formation, disease recurrence | [113] |
| Type 2 Diabetes (T2D) Vascular Complications | T2D patients [111] | ↑ M1 in vascular tissues | Endothelial dysfunction, vascular injury | [111] |
Analysis of Clinical Data
The data in Table 1 reveals several key trends. In allergic and Th2-associated diseases like asthma and CRSwNP, the M2 phenotype, particularly the M2c subset, is strongly associated with disease severity and poor clinical outcomes such as hospitalization [113] [112]. In contrast, in autoimmune diseases like RA, the pro-inflammatory M1 phenotype and a high M1/M2 ratio drive pathology [75]. In metabolic diseases such as T2D, a persistent M1 polarization in vascular tissues is a key mediator of chronic complications [111]. These patterns underscore that disease severity is not simply a function of too much or too little inflammation, but rather a consequence of specific and maladaptive macrophage polarization states.
Detailed Experimental Protocols for Human Cohort Studies
To ensure the reproducibility and rigorous evaluation of clinical evidence, this section outlines standard operating procedures for key methodologies used in the cited studies.
Flow Cytometry for Circulating Macrophage Phenotyping
This protocol is foundational for quantifying macrophage subsets in peripheral blood mononuclear cells (PBMCs) from patient cohorts, as utilized in the childhood asthma study [112].
- 1. Patient Cohort Definition and Sample Collection: Define patient and control groups using established clinical diagnostic criteria (e.g., GINA guidelines for asthma). Obtain informed consent and ethical approval. Collect peripheral blood samples in anticoagulant tubes.
- 2. PBMC Isolation: Isolate PBMCs from whole blood via density-gradient centrifugation using Ficoll-Paque. Briefly, layer diluted blood over Ficoll and centrifuge. Harvest the opaque PBMC interface ring and wash cells with PBS.
- 3. Cell Staining for Surface Markers: Resuspend PBMCs in FBS-containing buffer. Incubate with an Fc receptor binding inhibitor to reduce non-specific antibody binding. Stain cells with a pre-optimized antibody cocktail for macrophage subsets. A representative panel includes:
- Pan-macrophage marker: Anti-PM-2K antibody
- Monocyte/Macrophage marker: Anti-CD14
- M1 markers: Anti-CCR7, Anti-CD86
- M2 subset markers: Anti-CXCR1 (M2a), Anti-CD86 (M2b), Anti-CCR2 (M2c)
- Include appropriate viability dye and isotype controls.
- 4. Flow Cytometry Acquisition and Analysis: Acquire data on a flow cytometer (e.g., BD LSRII). First, gate on live, single cells. Identify macrophages as PM-2K+ cells. Subsequently, subset based on CD14 expression and further delineate M1 and M2 subsets using the marker combinations above. Analyze data using software such as FlowJo [112].
Transcriptomic Analysis for Macrophage-Associated Biomarker Discovery
This workflow, used in the CRSwNP study, identifies macrophage polarization and metabolism-related genes from public transcriptomic data [113].
- 1. Data Acquisition: Download relevant transcriptomic datasets (e.g., from GEO database, such as GSE136825 for CRSwNP). Define sample groups (e.g., nasal polyp tissue vs. healthy control tissue).
- 2. Differential Expression Analysis: Process raw data. Perform normalization and differential expression analysis using a package like DESeq2 in R. Identify Differentially Expressed Genes (DEGs) with a threshold of |log2Fold Change| > 1 and an adjusted p-value (FDR) < 0.05.
- 3. Functional Module Identification: Perform Weighted Gene Co-expression Network Analysis (WGCNA) to identify clusters (modules) of highly correlated genes. Correlate these modules with a pre-defined Macrophage Polarization-Related Gene (MP-RG) score to identify key modules of interest.
- 4. Biomarker Screening and Validation:
- Intersect DEGs, genes from key WGCNA modules, and a curated list of metabolism-related genes (MRGs) to identify candidate genes.
- Apply machine learning algorithms (e.g., LASSO regression and Random Forest) to refine the candidate gene list to a few robust biomarkers.
- Validate the diagnostic power of the biomarkers by constructing Receiver Operating Characteristic (ROC) curves and calculating the Area Under the Curve (AUC) in both training and validation datasets.
- Confirm gene expression levels in independent patient samples using RT-qPCR [113].
Visualization of Research Workflows and Signaling Pathways
The following diagrams, generated with Graphviz, illustrate the core experimental and analytical pathways described in this guide.
Macrophage Phenotyping Workflow
Key Signaling Pathways in Macrophage Polarization
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful research in this field relies on a suite of well-validated reagents and tools. The following table details essential solutions for studying macrophage phenotypes in clinical cohorts.
Table 2: Research Reagent Solutions for Macrophage Phenotyping
| Reagent / Material | Function / Application | Specific Examples & Notes |
|---|---|---|
| Flow Cytometry Antibody Panels | Identification and quantification of macrophage subsets in PBMCs or tissue digests. | PM-2K (pan-macrophage), CD14 (monocyte), CCR7/CD86 (M1), CXCR1/CCR2/CD86 (M2 subsets). Critical to include isotype and fluorescence-minus-one (FMO) controls [112]. |
| Transcriptomic Databases | Source of public data for bioinformatic analysis of macrophage-related genes. | Gene Expression Omnibus (GEO), ArrayExpress. Used for identifying DEGs and building co-expression networks [113]. |
| Bioinformatic Analysis Tools | Statistical and functional analysis of high-throughput data. | R/Bioconductor packages: DESeq2 (DEG analysis), WGCNA (co-expression networks), clusterProfiler (pathway enrichment) [113]. |
| Cell Isolation Kits | Isolation of specific cell populations from patient samples. | Ficoll-Paque (PBMC isolation), MACS or FACS kits for isolating CD14+ monocytes for in vitro polarization assays. |
| In Vitro Polarizing Cytokines | Directing naive macrophages (M0) to specific phenotypes for functional validation. | M1: IFN-γ + LPS; M2a: IL-4 + IL-13; M2c: IL-10. Used to create reference profiles and test therapeutic compounds [75] [111]. |
The consolidation of clinical evidence from patient cohorts irrefutably links specific macrophage polarization states to measurable disease severity, progression, and exacerbation. The methodologies outlined—from high-dimensional flow cytometry to integrated bioinformatics—provide a robust toolkit for quantifying these phenotypes and uncovering their molecular underpinnings. As the field progresses, the focus will shift towards leveraging these correlations for therapeutic intervention, using agents that can precisely modulate macrophage polarization to restore immune homeostasis and improve patient outcomes. The ongoing challenge and opportunity lie in translating these mechanistic insights into targeted therapies for chronic inflammatory diseases.
Head-to-Head Comparisons of Small Molecules, Biologics, and Nanotherapies for Polarization Control
Macrophage polarization represents a fundamental process in the regulation of chronic inflammation, where these highly plastic immune cells differentiate into distinct functional phenotypes in response to microenvironmental cues [114] [1]. The classical activation state (M1) and alternative activation state (M2) constitute the extremes of a functional spectrum, with M1 macrophages promoting pro-inflammatory responses through the production of cytokines such as TNF-α, IL-1β, and IL-6, while M2 macrophages facilitate inflammation resolution and tissue repair via IL-10, TGF-β, and vascular endothelial growth factor (VEGF) [114] [115]. In chronic inflammatory diseases—including diabetes, atherosclerosis, rheumatoid arthritis, and fibrotic lung diseases—a persistent imbalance toward the M1 phenotype drives pathological progression [114] [75] [116]. This imbalance has established macrophage polarization as a compelling therapeutic target, spurring the development of diverse intervention strategies ranging from small molecules to advanced nanotherapies [1] [117]. The complexity of polarization control necessitates a thorough understanding of the distinct advantages, limitations, and appropriate applications for each therapeutic modality within the researcher's toolkit.
Signaling Pathways Governing Macrophage Polarization
The polarization of macrophages is precisely regulated by an intricate network of intracellular signaling pathways that translate microenvironmental signals into distinct functional phenotypes. Understanding these pathways is prerequisite for developing targeted therapeutic interventions.
M1-Polarizing Signaling Pathways: Pro-inflammatory stimuli, including interferon-gamma (IFN-γ) and lipopolysaccharide (LPS), drive M1 polarization primarily through the JAK/STAT1 and NF-κB pathways [1] [20]. IFN-γ binding to its receptor activates JAK kinases, which phosphorylate STAT1. Phosphorylated STAT1 dimerizes and translocates to the nucleus to induce expression of pro-inflammatory genes [1]. Simultaneously, LPS engagement of Toll-like receptor 4 (TLR4) activates the adaptor protein MyD88, triggering the IKK complex and leading to NF-κB nuclear translocation [1] [20]. NF-κB then activates transcription of key M1 markers including iNOS, TNF-α, IL-1β, and IL-6 [20]. These pathways exhibit metabolic coordination, with M1 macrophages relying predominantly on glycolytic metabolism and experiencing a broken TCA cycle that leads to accumulation of succinate and citrate, further stabilizing HIF-1α and enhancing IL-1β production [29].
M2-Polarizing Signaling Pathways: Alternatively, anti-inflammatory cytokines IL-4 and IL-13 promote M2 polarization through activation of the STAT6 pathway [1] [115]. IL-4 binding to the IL-4Rα receptor recruits JAK kinases that phosphorylate STAT6, which then dimerizes and translocates to the nucleus to drive expression of characteristic M2 markers such as arginase-1 (Arg1), Ym1, and Fizz1 [1]. Additional transcription factors including IRF4 and PPARγ further reinforce the M2 transcriptional program [1] [115]. Metabolically, M2 polarization depends on oxidative phosphorylation and fatty acid oxidation, with intact TCA cycle function and enhanced mitochondrial biogenesis [29] [115]. The IL-10/STAT3 axis represents another important M2-promoting pathway, particularly for the M2c subtype, through suppression of pro-inflammatory cytokine production [1].
Diagram 1: Core signaling pathways regulating macrophage polarization. M1 pathways (yellow stimuli) activate STAT1 and NF-κB, driving pro-inflammatory gene expression. M2 pathways (yellow stimuli) activate STAT6, STAT3, IRF4, and PPARγ, promoting anti-inflammatory gene expression.
Comparative Analysis of Therapeutic Modalities
Small Molecule Approaches
Small molecules represent the most extensively characterized class of polarization-modulating agents, typically acting through direct targeting of intracellular signaling proteins and metabolic enzymes. Their low molecular weight (<900 Daltons) enables favorable tissue penetration and intracellular access, though this can sometimes lead to off-target effects [118].
Natural Compounds: Resveratrol, a naturally occurring polyphenol, demonstrates concentration-dependent polarization effects, with higher concentrations promoting M2 polarization through inhibition of NF-κB signaling, while moderate concentrations may enhance M1 responses [118]. This concentration dependency underscores the importance of precise dosing in experimental and therapeutic applications. Additional natural compounds including curcumin and epigallocatechin-3-gallate (EGCG) have shown polarization-modulating capacity, though their mechanisms are less thoroughly characterized.
Synthetic Enzyme Inhibitors: Targeted kinase inhibitors against JAK, STAT, and PI3K/Akt pathway components represent a growing class of synthetic small molecules for polarization control [20]. These compounds offer high specificity but may disrupt physiological signaling in non-target cell types. Metabolic enzyme inhibitors targeting PKM2, a key glycolytic enzyme upregulated in M1 macrophages, have shown promise in preclinical models of inflammatory disease and cancer [70].
Table 1: Characterization of Small Molecule Polarization Modulators
| Compound | Molecular Target | Polarization Effect | Key Signaling Pathways | Therapeutic Context | Key Advantages | Major Limitations |
|---|---|---|---|---|---|---|
| Resveratrol | Multiple (NF-κB, STAT3, S1P) | M2 promotion (high concentration); M1 promotion (moderate concentration) | NF-κB, PI3K/Akt, AMPK, STAT3 | Cancer, diabetes, cardiovascular diseases | Favorable safety profile, pleiotropic effects | Concentration-dependent effects complicate dosing |
| JAK Inhibitors | JAK kinases | M1 inhibition | JAK/STAT | Rheumatoid arthritis, autoimmune diseases | High specificity, clinical experience | Immunosuppression risk |
| PKM2 Inhibitors | Pyruvate kinase M2 | M1 inhibition | Glycolysis, STAT3 | Cancer, inflammatory diseases | Metabolic specificity | Potential disruption of normal cellular metabolism |
| PPARγ Agonists | PPARγ nuclear receptor | M2 promotion | PPARγ, STAT6 | Metabolic disease, diabetes | Established drug class | Side effects including weight gain |
Biological Approaches
Biologics encompass large-molecule therapeutics including monoclonal antibodies, recombinant proteins, and cytokine-based agents that typically target extracellular signaling components with high specificity.
Cytokine and Receptor Targeting: Antibodies against pro-inflammatory cytokines such as TNF-α (infliximab, adalimumab) and IL-1β (canakinumab) represent the most clinically validated biological approach to M1 macrophage modulation, with demonstrated efficacy in rheumatoid arthritis and other autoimmune conditions [75] [20]. These agents effectively reduce inflammation but may increase infection risk due to broad immunosuppression. CTLA-4 Ig (abatacept) has shown capacity to shift macrophages from M1 to M2 phenotypes in vitro, representing a more sophisticated immunomodulatory approach [75].
Cell-Directed Therapies: Emerging biological strategies employ engineered macrophages themselves as therapeutic agents. While still primarily in preclinical development, approaches involving ex vivo polarization and reinfusion of M2 macrophages show promise for promoting tissue repair and inflammation resolution in conditions including acute kidney injury and fibrosis [115].
Table 2: Characterization of Biological Polarization Modulators
| Biological Agent | Target/Mechanism | Polarization Effect | Therapeutic Context | Development Status | Key Advantages | Major Limitations |
|---|---|---|---|---|---|---|
| Anti-TNF-α mAbs (e.g., Infliximab) | TNF-α neutralization | M1 inhibition | Rheumatoid arthritis, autoimmune diseases | Clinical use | High specificity, proven efficacy | Systemic immunosuppression, cost |
| CTLA-4 Ig (Abatacept) | T-cell co-stimulation modulation | M1 to M2 conversion | Rheumatoid arthritis | Clinical use | Indirect polarization via T-cell modulation | Complex mechanism of action |
| IL-4/IL-13 cytokine therapy | IL-4 receptor activation | M2 promotion | Fibrotic diseases, tissue repair | Preclinical | Direct polarization control | Potential pro-fibrotic effects |
| Engineered M2 macrophages | Cell-based therapy | M2 promotion | Tissue repair, regenerative medicine | Preclinical | Potent tissue repair capacity | Manufacturing complexity, delivery challenges |
Nanotherapeutic Approaches
Nanotherapies represent the most advanced technological approach to polarization control, offering unique capabilities for targeted delivery, combination therapy, and spatiotemporal control of immunomodulation.
Targeted Nanocarriers: Liposomal, polymeric, and inorganic nanoparticles can be engineered with surface ligands (peptides, antibodies, aptamers) to specifically target macrophage subpopulations through surface markers such as CD163 (M2), CD206 (M2), or CD86 (M1) [117]. This targeting enhances therapeutic specificity while reducing off-target effects. For example, folic acid-modified silver nanoparticles (FA-AgNPS) have demonstrated targeted anti-inflammatory effects in rheumatoid arthritis models [75].
Stimuli-Responsive Systems: "Smart" nanotherapies designed to respond to microenvironmental cues (pH, reactive oxygen species, enzymes) prevalent in inflammatory sites enable precise spatial control of therapeutic activity [117]. These systems remain inert until encountering the pathological microenvironment, thereby maximizing therapeutic index. ROS-responsive nanoparticles that release anti-inflammatory payloads specifically in M1-skewed environments represent a promising example of this approach.
Combination Therapy Platforms: Nanocarriers facilitate codelivery of multiple therapeutic agents with distinct polarization effects, enabling synergistic modulation of macrophage function [117]. Sequential release profiles can be engineered to mirror the natural progression of inflammation resolution—first inhibiting M1 signaling, then promoting M2 polarization.
Table 3: Characterization of Nanotherapeutic Approaches for Polarization Control
| Nanoplatform | Composition | Targeting Approach | Polarization Effect | Therapeutic Context | Key Advantages | Major Limitations |
|---|---|---|---|---|---|---|
| FA-AgNPS | Silver nanoparticles with folic acid coating | Folic acid receptor targeting | M1 inhibition | Rheumatoid arthritis | Targeted delivery, combinatorial material properties | Potential nanoparticle toxicity |
| Liposomal corticosteroids | Lipid bilayers encapsulating steroids | Passive targeting to inflamed tissues | M2 promotion | Inflammatory diseases | Enhanced therapeutic index, reduced steroid side effects | Stability challenges |
| ROS-responsive NPs | Polymers with ROS-cleavable linkers | Microenvironmental activation in inflammatory sites | M1 to M2 shift | Chronic inflammation, atherosclerosis | Spatiotemporal control, minimized off-target effects | Complex manufacturing |
| Sequential-release scaffolds | Biodegradable polymers with multiple cargoes | Temporal release programming | Sequential M1 inhibition then M2 promotion | Tissue engineering, implants | Mimics natural healing progression | Elaborate formulation requirements |
Experimental Methodology for Polarization Assessment
In Vitro Macrophage Polarization Protocols
Primary Macrophage Isolation and Culture:
- Cell Source: Isolate primary human monocytes from peripheral blood mononuclear cells (PBMCs) using Ficoll density gradient centrifugation followed by CD14+ magnetic-activated cell sorting (MACS) to achieve >95% monocyte purity.
- Differentiation: Culture monocytes in RPMI-1640 medium supplemented with 10% fetal bovine serum (FBS) and 50 ng/mL macrophage colony-stimulating factor (M-CSF) for 6 days to generate M0 macrophages, with medium refreshment on day 3.
- Polarization: Induce polarization by treating M0 macrophages with either:
Compound Screening Protocol:
- Pretreatment: Incubate M0 macrophages with test compounds at varying concentrations (typically 1-100 μM for small molecules) for 1-2 hours prior to polarization induction.
- Co-treatment: Maintain compounds throughout polarization period.
- Validation: Include appropriate controls—untreated M0, M1 polarized (LPS+IFN-γ), and M2 polarized (IL-4+IL-13) macrophages without compound treatment.
Phenotypic Characterization Techniques
Surface Marker Analysis by Flow Cytometry:
- M1 Markers: Stain for CD80, CD86, MHC-II, TLR-4 using fluorochrome-conjugated antibodies
- M2 Markers: Stain for CD163, CD206, CD209
- Procedure: Harvest macrophages, incubate with antibodies for 30 minutes at 4°C, wash, and analyze using flow cytometry with appropriate isotype controls [75] [20]
Gene Expression Profiling:
- RNA Extraction: Use TRIzol reagent or commercial RNA extraction kits
- qRT-PCR Analysis: Measure expression of:
- Normalization: Use housekeeping genes (GAPDH, β-actin) for quantification
Cytokine Secretion Analysis:
- ELISA: Quantify secreted proteins in culture supernatants for TNF-α, IL-1β, IL-6 (M1) and IL-10, TGF-β (M2)
- Multiplex immunoassays: Simultaneously measure multiple cytokines from small sample volumes
Metabolic Profiling:
- Extracellular Flux Analysis: Measure glycolytic rate and oxygen consumption rate using Seahorse Analyzer to confirm metabolic reprogramming
- M1 metabolism: Elevated glycolysis, suppressed oxidative phosphorylation
- M2 metabolism: Enhanced oxidative phosphorylation, fatty acid oxidation [29] [115]
Diagram 2: Experimental workflow for evaluating macrophage polarization modulators. The standardized protocol progresses from macrophage differentiation through polarization induction, therapeutic intervention, and multi-modal phenotypic characterization.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Essential Research Reagents for Macrophage Polarization Studies
| Reagent Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| Polarization Inducers | LPS (E. coli 055:B5), recombinant IFN-γ, IL-4, IL-13 | Induction of M1/M2 polarization | Verify endotoxin levels in cytokines; use consistent sources |
| Cell Culture Media | RPMI-1640, DMEM, Macrophage-SFM | Primary macrophage culture | Serum-free options available; batch test FBS for polarization support |
| Surface Marker Antibodies | Anti-human CD80, CD86, CD163, CD206, MHC-II | Flow cytometry phenotyping | Validate clones for specific applications; include isotype controls |
| Cytokine Detection | ELISA kits for TNF-α, IL-1β, IL-6, IL-10, TGF-β | Secreted protein quantification | Consider multiplex platforms for comprehensive profiling |
| Gene Expression Assays | TaqMan assays for iNOS, Arg1, TNF-α, IL-10 | qRT-PCR analysis | Normalize to multiple housekeeping genes |
| Metabolic Probes | 2-NBDG (glucose uptake), MitoTracker (mitochondrial mass) | Metabolic profiling | Combine with extracellular flux analysis for complete assessment |
| Small Molecule Modulators | Resveratrol, JAK inhibitors (ruxolitinib), STAT inhibitors | Pathway-specific polarization control | Optimize DMSO concentrations; include vehicle controls |
| Nanoparticle Systems | PLGA nanoparticles, liposomal formulations, gold nanoparticles | Advanced delivery systems | Characterize size, zeta potential, and stability in culture media |
The strategic modulation of macrophage polarization represents a promising therapeutic approach for chronic inflammatory diseases, with each class of therapeutic modality—small molecules, biologics, and nanotherapies—offering distinct advantages and limitations. Small molecules provide excellent tissue penetration and established manufacturing protocols but often lack cellular specificity. Biologics offer exceptional target specificity but face delivery challenges and high production costs. Nanotherapies enable sophisticated delivery strategies and combination approaches but require complex characterization and raise unique regulatory considerations.
Future advances in polarization control will likely emphasize temporal precision approaches that mirror the natural progression of inflammation resolution, spatial targeting strategies that limit activity to pathological microenvironments, and personalized approaches based on individual patient macrophage profiles. The integration of multi-omics technologies—including single-cell RNA sequencing, proteomic profiling, and metabolic flux analysis—will enable unprecedented resolution in understanding polarization states and therapeutic responses. As these technologies mature, the next generation of macrophage-targeted therapies will increasingly move beyond simplistic M1/M2 dichotomies to embrace the continuous spectrum of macrophage functional states, ultimately enabling more precise and effective control of chronic inflammation.
Conclusion
The intricate mechanisms of macrophage polarization represent a central regulatory node in chronic inflammation, with significant implications for understanding disease pathogenesis and developing novel therapeutics. The balance between pro-inflammatory M1 and anti-inflammatory/reparative M2 phenotypes, governed by specific signaling pathways and metabolic programs, is disrupted in a wide array of chronic conditions, from autoimmune diseases and diabetes to cancer and atherosclerosis. Future research must prioritize the development of sophisticated delivery platforms that ensure precise spatiotemporal control over polarization, the identification of robust biomarkers for patient stratification, and the execution of well-designed clinical trials to validate the therapeutic potential of macrophage-focused strategies. Successfully harnessing macrophage plasticity will undoubtedly unlock new frontiers in personalized immunomodulation and regenerative medicine, offering hope for managing some of the most challenging chronic inflammatory diseases.
References
- 1. Macrophages in immunoregulation and therapeutics [https://www.nature.com/articles/s41392-023-01452-1]
- 2. Macrophages: pivotal orchestrators and emerging therapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12604222/]
- 3. The M1 and M2 paradigm of macrophage activation [https://pmc.ncbi.nlm.nih.gov/articles/PMC3944738/]
- 4. Editorial: Exploring the molecular mechanisms that regulate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12041800/]
- 5. Advances in research on M1/M2 macrophage polarization ... [https://www.sciencedirect.com/science/article/pii/S2405844025012629]
- 6. Global characterization of macrophage polarization ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8783961/]
- 7. Non-invasive classification of macrophage polarisation by ... [https://elifesciences.org/articles/77373]
- 8. Dual roles and therapeutic targeting of tumor-associated ... [https://www.nature.com/articles/s41392-025-02325-5]
- 9. Macrophage Polarization - an overview [https://www.sciencedirect.com/topics/medicine-and-dentistry/macrophage-polarization]
- 10. - Wikipedia Macrophage polarization [https://en.wikipedia.org/wiki/Macrophage_polarization]
- 11. Macrophage Polarization in Chronic Inflammatory Diseases [https://pmc.ncbi.nlm.nih.gov/articles/PMC5821995/]
- 12. M2b macrophage polarization and its roles in diseases - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7379745/]
- 13. Unraveling Macrophage Polarization: Functions ... [https://www.mdpi.com/1422-0067/25/22/12078]
- 14. Macrophage polarization: an important role in inflammatory ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1352946/full]
- 15. The Phenotypic Features of Human... and Functional [https://pubmed.ncbi.nlm.nih.gov/26678544/]
- 16. BD FACSDivaâ„¢ Software [https://www.bdbiosciences.com/en-us/products/software/instrument-software/bd-facsdiva-software]
- 17. Advancements in Macrophage-Targeted Drug Delivery for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10680479/]
- 18. The JAK-STAT pathway: from structural biology to cytokine ... [https://www.nature.com/articles/s41392-024-01934-w]
- 19. JAK-STAT signaling in inflammation and stress-related diseases [https://pmc.ncbi.nlm.nih.gov/articles/PMC10632324/]
- 20. Advances in the study of macrophage polarization in ... [https://journal-inflammation.biomedcentral.com/articles/10.1186/s12950-023-00360-z]
- 21. The Multifaceted Role of Macrophages in Biology and Diseases [https://pmc.ncbi.nlm.nih.gov/articles/PMC11900619/]
- 22. NF-κB in biology and targeted therapy: new insights and ... [https://www.nature.com/articles/s41392-024-01757-9]
- 23. NF-κB: master regulator of cellular responses in health and ... [https://link.springer.com/article/10.1007/s44466-025-00014-0]
- 24. The NF-κB activation pathways, emerging molecular targets ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3043547/]
- 25. Network centric identification of PI3K/Akt hub proteins as ... [https://www.nature.com/articles/s41598-025-24625-0]
- 26. Important Roles of PI3K/AKT Signaling Pathway and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11529649/]
- 27. Strategic advancements in targeting the PI3K/AKT/mTOR ... [https://www.sciencedirect.com/science/article/pii/S0006295225001121]
- 28. Effects of Metabolism on Macrophage Polarization Under ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9331907/]
- 29. Macrophages in chronic infections: regulation and ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1594988/full]
- 30. Macrophages in chronic infections: regulation and remodeling [https://pmc.ncbi.nlm.nih.gov/articles/PMC12310494/]
- 31. Glucose Metabolic Reprogramming of Macrophages Against ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12584850/]
- 32. Metabolic reprogramming in macrophages and dendritic ... [https://www.nature.com/articles/cr201568]
- 33. Glycolysis: A multifaceted metabolic pathway and signaling hub [https://pmc.ncbi.nlm.nih.gov/articles/PMC11605472/]
- 34. The ERK and JNK pathways in the regulation of metabolic ... [https://www.nature.com/articles/s41388-018-0582-8]
- 35. regulation and role in cellular and tissue metabolism - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5709332/]
- 36. Review The Evolving Role of Macrophage Metabolic ... [https://www.sciencedirect.com/science/article/pii/S0828282X25003204]
- 37. Bioactive lipid signaling and lipidomics in macrophage ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1550500/full]
- 38. Lipidomics unveils the complexity of the lipidome in metabolic ... [https://clintransmed.springeropen.com/articles/10.1186/s40169-018-0182-9]
- 39. Signaling pathways in macrophages: molecular mechanisms ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10495745/]
- 40. Lipid Profiling of Polarized Human Monocyte-derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6053630/]
- 41. Metabolic and Molecular Mechanisms of Macrophage ... [https://www.mdpi.com/1422-0067/21/16/5731]
- 42. Lipidomics in Understanding Pathophysiology and ... [https://www.mdpi.com/2218-1989/12/4/333]
- 43. Quantitative profiling of glycerophospholipids during ... [https://www.nature.com/articles/s41598-017-00341-2]
- 44. Interaction between lipid metabolism and macrophage ... [https://www.sciencedirect.com/science/article/pii/S2589004225004298]
- 45. Lipidomics in drug and biomarker development [https://pubmed.ncbi.nlm.nih.gov/23495996/]
- 46. Natural saponins and macrophage polarization [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1584035/full]
- 47. Natural saponins and macrophage polarization [https://pubmed.ncbi.nlm.nih.gov/40417220/]
- 48. Evaluation of Anti-Inflammatory Effects of Six Ginsenosides ... [https://www.mdpi.com/2076-3921/14/3/283]
- 49. Macrophage polarization in disease therapy: insights from ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1598022/full]
- 50. Total saponins of Panax japonicus alleviate adjuvant ... [https://www.sciencedirect.com/science/article/pii/S1226845325000971]
- 51. Bioactivity and biomedical applications of pomegranate ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1569141/full]
- 52. The Pomegranate Peel Polyphenols Protects Acne ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12520010/]
- 53. Mechanisms and Therapeutic Strategies of Macrophage ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12077540/]
- 54. In Vivo Insights into the Role of Astragaloside IV ... [https://www.mdpi.com/1422-0067/26/9/4250]
- 55. The antipsychotic drug thiothixene stimulates macrophages to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12068545/]
- 56. Screening of the FDA-approved drug library identifies ... [https://www.nature.com/articles/s41598-025-12191-4]
- 57. Swertianin Suppresses M1 Macrophage Polarization and ... [https://www.mdpi.com/2073-4425/16/6/693]
- 58. Novel Drug Approvals for 2025 [https://www.fda.gov/drugs/novel-drug-approvals-fda/novel-drug-approvals-2025]
- 59. FDA Approved Medications For June 2025 [https://www.guidelinecentral.com/insights/fda-med-approvals-june-2025/]
- 60. FDA Approves Gamifant (emapalumab-lzsg) as First-Ever ... [https://www.drugs.com/newdrugs/fda-approves-gamifant-emapalumab-lzsg-first-ever-adults-children-macrophage-activation-syndrome-6559.html]
- 61. From macrophage polarization to clinical translation [https://pmc.ncbi.nlm.nih.gov/articles/PMC12504304/]
- 62. Biomaterials-mediated CRISPR/Cas9 delivery - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC10568484/]
- 63. Macrophage-related therapeutic strategies: Regulation of ... [https://www.sciencedirect.com/science/article/pii/S104366182300378X]
- 64. Flow Cytometric Analysis of Macrophages and Cytokines ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10650702/]
- 65. Physical cues in biomaterials modulate macrophage ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1640560/full]
- 66. CRISPR/Cas9 systems: Delivery technologies and ... [https://www.sciencedirect.com/science/article/pii/S1818087623000818]
- 67. Quantitative Proteomics of Polarised Macrophages Derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8869710/]
- 68. Macrophage Signaling Pathways in Health and Disease [https://pmc.ncbi.nlm.nih.gov/articles/PMC12171086/]
- 69. Targeting macrophages in cancer immunotherapy [https://www.sciencedirect.com/science/article/pii/S2090123224006222]
- 70. Role of macrophage PKM2 in inflammation and tumor ... [https://www.sciencedirect.com/science/article/abs/pii/S0304419X25002203]
- 71. Macrophage: Key player in the pathogenesis of autoimmune ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9974150/]
- 72. Nanoformulations to Enhance the Bioavailability and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7587200/]
- 73. Native and engineered exosomes for inflammatory disease [https://pmc.ncbi.nlm.nih.gov/articles/PMC9793369/]
- 74. Engineered Extracellular Vesicles for Treatment of ... [https://link.springer.com/article/10.1007/s12033-025-01528-z]
- 75. Macrophage polarization: an important role in inflammatory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11039887/]
- 76. Macrophages: Subtypes, Distribution, Polarization, ... [https://pubmed.ncbi.nlm.nih.gov/40717900/]
- 77. Advances in the regulation of macrophage polarization by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12328869/]
- 78. A bibliometric analysis of macrophages associated with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12603411/]
- 79. Senescent Polarization of Macrophages and Inflammatory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12428708/]
- 80. Scientists Pinpoint Macrophages that Fight Chronic Inflammation [https://medicine.yale.edu/news-article/scientists-pinpoint-macrophages-that-fight-chronic-inflammation/]
- 81. miR-210 promotes the anti-inflammatory phenotype and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12361208/]
- 82. Ubiquitination in macrophage plasticity: from inflammatory ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1621328/full]
- 83. Macrophages in tissue repair, regeneration, and fibrosis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4794754/]
- 84. M1 macrophages – unexpected contribution to tumor ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1638102/full]
- 85. Reducing M2 macrophage in lung fibrosis by controlling ... [https://www.nature.com/articles/s41598-024-76561-0]
- 86. Macrophage polarization in cancer and beyond: from ... [https://www.sciencedirect.com/science/article/abs/pii/S0304383525003386]
- 87. Role of macrophage PKM2 in inflammation and tumor ... [https://pubmed.ncbi.nlm.nih.gov/41101510/]
- 88. Mechanisms and therapeutic strategies of macrophages ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12425758/]
- 89. Regulatory Mechanism of M1/M2 Macrophage Polarization in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10270764/]
- 90. Engineering macrophages for targeted immunotherapy and ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06687-w]
- 91. Exploration of M2 macrophage-related biomarkers and a ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1587258/full]
- 92. Mechanisms and therapeutic strategies of macrophages ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1615340/full]
- 93. M2 polarization of macrophage protects the lung cancer ... [https://www.nature.com/articles/s41420-025-02775-4]
- 94. Nanodynamic therapy for cancer: mechanistic innovations ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-07277-6]
- 95. Identification of biomarkers associated with macrophage polarization in diabetic cardiomyopathy based on bioinformatics and machine learning approaches - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0024320525000761]
- 96. Dealing with Macrophage Plasticity to Address Therapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9224268/]
- 97. Flow Cytometry Protocols [https://www.bdbiosciences.com/en-us/resources/protocols/flow-cytometry]
- 98. Inflammation and Cytokine Storm ELISA Kits and Multiplex ... [https://www.thermofisher.com/us/en/home/life-science/antibodies/immunoassays/immunoassay-research-areas/inflammation-cytokine-storm-immunoassays.html]
- 99. Modulating M1/M2 macrophage polarization with plant ... [https://pubmed.ncbi.nlm.nih.gov/41181606/]
- 100. WTAP modulates macrophage polarization in rheumatoid ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1601259/full]
- 101. KLF11 alleviates rheumatoid arthritis by regulating M1 ... [https://arthritis-research.biomedcentral.com/articles/10.1186/s13075-025-03634-4]
- 102. Progress in macrophage immune regulation of ... [https://pubmed.ncbi.nlm.nih.gov/40535630/]
- 103. m6A modification: a novel mechanism that regulates ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1607932/full]
- 104. Global research trends on macrophage polarization in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12575332/]
- 105. Mechanisms of synovial macrophage polarization in ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1637731/full]
- 106. Recent advancement on development of drug-induced ... [https://pubmed.ncbi.nlm.nih.gov/34453949/]
- 107. In Vitro Macrophage Assay Predicts the In Vivo Anti ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6350420/]
- 108. In vitro skin culture media influence the viability and ... [https://www.nature.com/articles/s41598-021-86486-7]
- 109. Predictive value of preclinical models for CAR-T cell ... [https://pubmed.ncbi.nlm.nih.gov/40514065/]
- 110. Preclinical pancreatic cancer mouse models for treatment ... [https://www.nature.com/articles/s41598-025-25191-1]
- 111. in diabetic vascular complications... Macrophage polarization [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-07075-0]
- 112. Altered Pattern of Macrophage as a Polarization for... Biomarker [https://pmc.ncbi.nlm.nih.gov/articles/PMC8608023/]
- 113. Frontiers | Discovering biomarkers for chronic sinusitis with nasal... [https://www.frontiersin.org/journals/bioinformatics/articles/10.3389/fbinf.2025.1613136/full]
- 114. Macrophage polarization in diabetic vascular complications [https://pmc.ncbi.nlm.nih.gov/articles/PMC12495728/]
- 115. Macrophage Polarization and Reprogramming in Acute ... [https://www.mdpi.com/2076-3921/11/7/1394]
- 116. Macrophage Polarization in Lung Diseases [https://pubmed.ncbi.nlm.nih.gov/40213814/]
- 117. Delivery strategies to control inflammatory response [https://pmc.ncbi.nlm.nih.gov/articles/PMC4945478/]
- 118. Resveratrol-driven macrophage polarization: unveiling ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2024.1516609/full]