Molecular Mechanisms of Cytokine Storm in Multiple Organ Failure: From Pathogenesis to Targeted Therapies
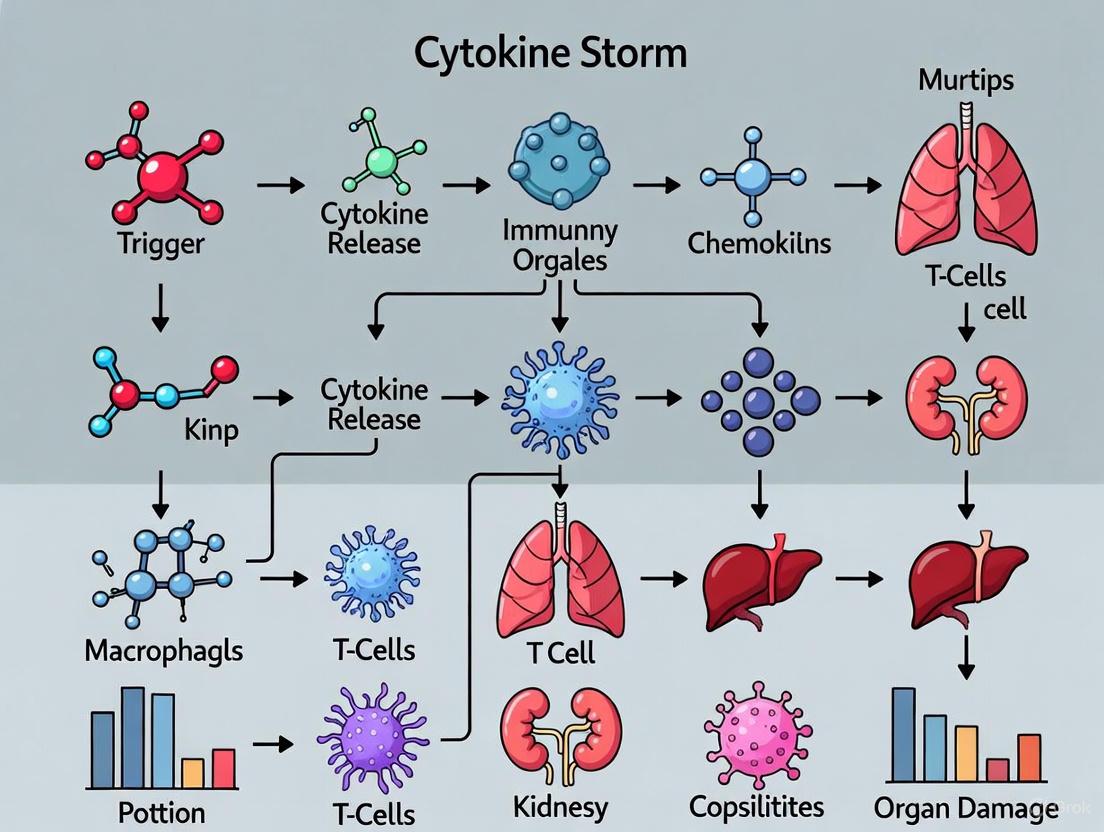
This article provides a comprehensive analysis of the pathophysiology linking cytokine storm (CS) to multiple organ failure (MODS), a life-threatening condition in sepsis, COVID-19, and immunotherapies.
Molecular Mechanisms of Cytokine Storm in Multiple Organ Failure: From Pathogenesis to Targeted Therapies
Abstract
This article provides a comprehensive analysis of the pathophysiology linking cytokine storm (CS) to multiple organ failure (MODS), a life-threatening condition in sepsis, COVID-19, and immunotherapies. We detail the molecular basis of CS, focusing on key signaling pathways like JAK/STAT and Toll-like receptors, and the critical role of inflammatory cell death (PANoptosis). For researchers and drug development professionals, the review explores current and emerging therapeutic strategies, including cytokine antagonists, JAK inhibitors, and extracorporeal therapies. It also covers diagnostic biomarkers, comparative treatment efficacy, and future directions in precision immunomodulation, offering a foundational resource for developing novel interventions.
Unraveling the Molecular Basis of Cytokine Storm and Systemic Inflammation
Cytokine storm (CS) represents a life-threatening systemic inflammatory syndrome characterized by excessive immune cell activation and dramatically elevated circulating cytokine levels. This pathophysiological process is implicated in the development of multi-organ failure across diverse clinical conditions, including severe infections, autoimmune disorders, and novel immunotherapies. This whitepaper provides a comprehensive technical overview of CS-defining clinical syndromes, traces the historical evolution of the concept, delineates underlying molecular mechanisms with a focus on critical signaling pathways, summarizes current experimental models and methodologies, and reviews emerging therapeutic strategies targeting specific components of the dysregulated immune response. The synthesis of current research presented herein aims to facilitate advanced mechanistic research and therapeutic development for this highly lethal condition.
The term "cytokine storm" first appeared in published medical literature in 1993, when James Ferrara used it to describe the engraftment syndrome associated with acute graft-versus-host disease (aGvHD) following allogeneic hematopoietic stem cell transplantation [1] [2]. However, recognition of this hyperinflammatory state predates the terminology, with references to an "influenza-like syndrome" in 1958 describing exaggerated immune responses following systemic viral infections [1]. The conceptual foundation was further established in 1991 when the term "cytokine release syndrome" (CRS) was coined to characterize the inflammatory state and hypercytokinemia following muromonab-CD3 infusion [1].
The cytokine storm concept gained significant traction during the 2005 avian H5N1 influenza pandemic, where it helped explain the severe pathology observed in infected patients [3]. Historical analyses suggest that cytokine storms were likely responsible for the disproportionate number of healthy young adult deaths during the 1918 influenza pandemic, which killed approximately 50 million people worldwide [2]. Similarly, preliminary research from Taiwan indicated cytokine storm as the probable mechanism for many deaths during the SARS epidemic in 2003 [2]. The COVID-19 pandemic further highlighted the clinical significance of cytokine storms, with many fatal cases attributed to this dysregulated immune response [4] [2].
The evolution of CS as a defined pathological entity has been paralleled by developments in targeted therapeutic approaches. One of the earliest targeted therapies was the anti-IL-6 receptor monoclonal antibody tocilizumab, developed in the 1990s for idiopathic multicentric Castleman disease [3]. A pivotal moment in CS management came in 2012 when tocilizumab was successfully used to rescue a 6-year-old patient experiencing a severe cytokine storm following CAR T-cell therapy, leading to its subsequent FDA approval for this indication [4].
Defining Clinical Syndromes and Biomarkers
Clinical Syndromes Associated with Cytokine Storm
Cytokine storm represents a severe systemic inflammatory syndrome characterized by excessive immune cell activation and significantly increased circulating cytokine levels [1] [5]. This pathological process is implicated in numerous life-threatening conditions, which can be broadly categorized into three main groups:
Table 1: Clinical Syndromes Associated with Cytokine Storm
| Syndrome Category | Specific Conditions | Primary Driving Cells | Key Pathogenic Cytokines |
|---|---|---|---|
| Pathogen-Induced | Sepsis (bacterial/viral), COVID-19, Influenza, SARS | Heterogenous immune cells | TNF-α, IFN-γ, IL-6, IL-1β [6] |
| Autoinflammatory/Monogenic | Primary HLH, Secondary HLH, MAS, CAPS, FMF | CD8+ T cells, Myeloid cells | IFN-γ, IL-1β, IL-18 [6] |
| Therapy-Induced | CAR T-cell CRS, ICANS, aGvHD, BiTE therapy | CAR T cells, T cells, Myeloid cells | IL-6, IL-1 [1] [6] |
Cytokine storm syndrome encompasses a diverse set of conditions that can result in this hyperinflammatory state. These include familial hemophagocytic lymphohistiocytosis (HLH), Epstein-Barr virus-associated HLH, systemic juvenile idiopathic arthritis-associated macrophage activation syndrome (MAS), NLRC4 macrophage activation syndrome, cytokine release syndrome (CRS), and sepsis [2]. While the term "cytokine storm" is often used interchangeably with CRS, it more precisely represents a severe episode of CRS or a component of another disease entity such as macrophage activation syndrome [2].
Clinical Manifestations and Biomarkers
The clinical presentation of cytokine storm includes acute systemic inflammatory symptoms, organ dysfunction, and potentially mortality [1]. Constitutional symptoms often include fever, headache, fatigue, and anorexia. Multi-organ system involvement manifests as confusion and delirium (nervous system); nausea, vomiting, and diarrhea (gastrointestinal system); anemia, cytopenia, and coagulopathy (vascular/lymphatic system); hypotension and arrhythmias (cardiac); pneumonitis and acute respiratory distress syndrome (pulmonary); hepatomegaly and liver failure (hepatic); and acute kidney injury (renal) [6].
Multiple biomarkers have been identified that correlate with CS severity and prognosis. A meta-analysis of severe COVID-19 cases identified several key biomarkers: lymphopenia, thrombocytopenia, and elevated levels of interleukin-6, ferritin, D-dimer, aspartate aminotransferase, C-reactive protein, procalcitonin, lactate dehydrogenase, creatinine, neutrophils, and leucocytes [7]. Elevated IL-6 and hyperferritinemia are particularly notable as red flags for systemic inflammation and poor prognosis [7]. More recent studies have identified CXCL13 as a potential biomarker for predicting patient response to siltuximab in Castleman disease [4].
Table 2: Key Biomarkers in Cytokine Storm Syndromes
| Biomarker Category | Specific Biomarkers | Association with CS Severity | Potential Clinical Utility |
|---|---|---|---|
| Cytokines | IL-6, IL-10, TNF-α, IFN-γ | IL-6 > 19.5 pg/mL associated with severe disease [8] | Prognostic stratification, treatment guidance |
| Acute Phase Reactants | Ferritin, C-reactive protein, Procalcitonin | Hyperferritinemia, elevated CRP | Disease monitoring, early diagnosis of SIRS |
| Hematological Parameters | Lymphopenia, Thrombocytopenia, Neutrophilia | Degree of cytopenia correlates with severity | Rapid assessment, risk stratification |
| Organ Function Markers | AST, ALT, LDH, Creatinine, D-dimer | Elevation indicates organ damage | Monitoring multi-organ dysfunction |
Molecular Mechanisms and Signaling Pathways
Key Signaling Pathways in Cytokine Storm
The pathogenesis of cytokine storm involves multiple interconnected signaling pathways that drive excessive cytokine production and inflammatory cell death.
JAK/STAT Pathway
The JAK/STAT pathway represents a highly conserved signaling cascade that plays a significant role in cytokine storm pathogenesis [1]. This pathway consists of three main structural components: transmembrane receptors, receptor-associated JAKs (JAK1, JAK2, JAK3, TYK2), and STATs (STAT1, STAT2, STAT3, STAT4, STAT5A, STAT5B, STAT6) [1]. Multiple cytokines, including ILs, IFNs, and growth factors, participate in JAK/STAT signaling.
IL-6 triggers the JAK/STAT3 pathway through classical cis-signaling, trans-signaling, and trans-presentation mechanisms [1]. IL-6 can interact with both membrane-bound IL-6 receptor (mIL-6R) on immune cells and soluble IL-6R (sIL-6R), forming a complex that activates gp130 and initiates the JAK/STAT3 signaling cascade [1]. This IL-6/IL-6R/JAK/STAT3 activation results in systemic hyperinflammatory response and secretion of various mediators including IL‑1β, IL‑8, CCL2, CCL3, CCL5, GM-CSF, and VEGF [1]. TNF and IFN-γ also activate JAK family kinases, particularly JAK1, leading to phosphorylation and activation of STAT proteins that promote expression of inflammation-related genes [1].
The overactivation of the JAK/STAT pathway has been identified as a key factor in cytokine release and inflammatory disturbances across various diseases, including HLH, aGvHD, CAR-T therapy complications, COVID-19, and fulminant myocarditis [1]. In HLH, elevated levels of various cytokines including IL-1, IL-2, IL-6, IL-10, IL-12, IL-18, TNF, IFN-γ, and GM-CSF primarily activate JAK/STAT pathways, leading to excessive proinflammatory cytokine production [1].
Toll-like Receptors (TLRs) and NF-κB Pathway
Toll-like receptors represent a primitive category of pattern recognition receptors that recognize pathogen-associated molecular patterns [1]. These receptors are present on various immune cells and tissue cells, including monocytes, macrophages, and dendritic cells, serving as detectors of pathogen incursion [1]. TLR activation plays a critical role in the development of infectious diseases and CS progression [1].
Upon recognition of PAMPs, TLRs initiate the release of pro-inflammatory cytokines and orchestrate immune responses to protect cells from harm [1]. TLR activation leads to production of antiviral cytokines such as type I IFNs, IL-1ß, and IL-6, which directly impede viral replication [1]. However, this release of pro-inflammatory factors may also have deleterious effects, contributing to the cytokine storm phenomenon.
Recent research on jellyfish envenomation syndrome has identified NF-κB p65 subunit activation as central to cytokine storm induction [9]. Transcriptomic analyses in a mouse model of delayed jellyfish envenomation syndrome revealed significant perturbation of the NF-κB signaling pathway following envenomation [9]. Knockdown of p65 in macrophages reduced cytokine production and improved cell viability, demonstrating its crucial role in this process [9].
Inflammatory Cell Death (PANoptosis)
Recent studies have elucidated positive feedback loops between cytokine release and cell death pathways, wherein certain cytokines, PAMPs, and DAMPs can activate inflammatory cell death, leading to further cytokine secretion [6]. This synergistic crosstalk between pyroptosis, apoptosis, and necroptosis pathways is referred to as PANoptosis [6].
PANoptosis is regulated by the PANoptosome, a molecular scaffold that enables key molecules from all three cell death pathways to engage contemporaneously [6]. Studies have shown that cytokines are intricately linked to these cell death mechanisms in a positive feedback loop whereby cytokine release causes inflammatory cell death that facilitates further pathogenic cytokine release through membrane pores and cell lysis, culminating in a cytokine storm that drives severe, life-threatening damage to host tissues and organs [6].
Systemic inflammation, tissue damage, multi-organ failure, and mortality in cytokine storm syndromes are prevented by combined treatments with TNF and IFN-γ neutralizing antibodies, which block cytokine-mediated inflammatory cell death in murine models [6]. The identification of cell death-associated molecules, primarily caspase-8, Z-DNA-binding protein 1, transforming growth factor-β-activated kinase, and receptor-interacting serine/threonine protein kinase 1, as master switches of inflammasome activation and PCD pathways has further established the concept of cytokine-mediated inflammatory cell death [6].
Experimental Models and Methodologies
Established Experimental Models for Cytokine Storm Research
Jellyfish Envenomation Syndrome Model
A novel mouse model of delayed jellyfish envenomation syndrome (DJES) has been established to study cytokine storm mechanisms [9]. In this model, mice are injected with tentacle extract from Nemopilema nomurai jellyfish via the tail vein [9]. The venom contains predominantly metalloproteinases and other toxic components such as staphylococcal toxins, coagulation factors, peroxiredoxins, and phospholipases [9].
Experimental Protocol:
- Animals: Laboratory mice (specific strain should be selected based on research objectives)
- Venom Preparation: Tentacle extract obtained from live Nemopilema nomurai jellyfish, purified and standardized
- Administration: Intravenous injection via tail vein at concentrations ranging from 0.7 to 2.29 mg kg−1
- Monitoring: Observation period of 12-48 hours with detailed recording of symptom progression and time to death
- Endpoint Analysis: Histopathological examination of heart, liver, and kidneys; biochemical analysis of organ function markers; cytokine profiling
This model replicates human DJES characterized by acute multi-organ failure and significant upregulation of over 20 pro-inflammatory cytokines (including IL-6, TNF-α, CXCL2, and CCL4) in the heart, liver, and kidneys [9]. The LD50 decreases from 1.9 to 0.7 mg kg−1 when observation time extends from 12 to 48 hours [9].
In Vitro Macrophage Model
To understand how jellyfish envenomation induces inflammatory cytokine storm, RAW 274.6 macrophages are treated with tentacle extract and examined in vitro [9].
Experimental Protocol:
- Cell Line: RAW 274.6 macrophages
- Treatment: Tentacle extract at varying concentrations
- Cytotoxicity Assessment: CCK8 assay to determine IC50 (reported as 17.39 µg mL−1 after 6 hours)
- Binding Studies: Immunofluorescence to confirm TE binding to macrophage membrane
- Transcriptomic Analysis: RNA sequencing to identify differentially expressed genes and pathway enrichment
Transcriptomic analysis of TE-treated macrophages identified 51 differentially expressed genes that overlapped with those found in the heart, liver, and kidneys of TE-treated DJES mice [9]. Similar to the in vivo model, the top enriched pathways in treated macrophages were related to inflammation, with NF-κB signaling emerging as a central pathway [9].
Research Reagent Solutions
Table 3: Essential Research Reagents for Cytokine Storm Investigation
| Reagent Category | Specific Examples | Research Application | Key Functions |
|---|---|---|---|
| Cell Culture Models | RAW 274.6 macrophages, Primary macrophages, Dendritic cells | In vitro cytokine production studies | Response to PAMPs/DAMPs, cytokine secretion profiling [9] |
| Cytokine Detection | ELISA kits (IL-6, TNF-α, IFN-γ), Multiplex immunoassays, LEGENDplex | Cytokine quantification in serum/tissue | Biomarker identification, pathway activation monitoring [7] [9] |
| Pathway Inhibitors | JAK inhibitors (Ruxolitinib), NF-κB inhibitors, Dexamethasone | Mechanistic studies, therapeutic screening | Target validation, pathway interrogation [1] [9] |
| Transcriptomic Tools | RNA sequencing kits, Microarrays, PCR arrays | Gene expression profiling | Pathway identification, biomarker discovery [9] |
| Histological Reagents | H&E staining kits, Immunofluorescence antibodies | Tissue pathology assessment | Organ damage evaluation, cellular infiltration analysis [9] |
Therapeutic Strategies and Research Directions
Targeted Therapeutic Approaches
Current management of cytokine storm typically necessitates a multidisciplinary team strategy encompassing removal of abnormal inflammatory or immune system activation, preservation of vital organ function, treatment of the underlying disease, and provision of life supportive therapy [1]. Several targeted approaches have emerged:
Cytokine-Targeted Therapies:
- IL-6 Inhibition: Tocilizumab (anti-IL-6 receptor monoclonal antibody) was one of the earliest targeted therapies developed for idiopathic multicentric Castleman disease and has since been approved for CRS associated with CAR T-cell therapy [3] [4].
- IL-1 Inhibition: Anakinra (IL-1 receptor antagonist) has demonstrated efficacy in autoinflammatory CS conditions [1].
- IFN-γ Inhibition: Emerging therapies targeting IFN-γ show promise for HLH and other CS conditions [1].
- TNF Inhibition: Anti-TNF agents have been explored for acute graft-versus-host disease and other CS conditions [1].
Intracellular Signaling Inhibitors:
- JAK/STAT Pathway: JAK inhibitors including ruxolitinib have shown promising efficacy in COVID-19, CAR-T associated CRS, and other CS conditions [1]. Inhibition of JAK1 has been shown to reduce CRS associated with CAR-T therapy [1].
- NF-κB Pathway: Dexamethasone, a broad-spectrum anti-inflammatory agent that inhibits NF-κB, effectively suppresses cytokine storm, mitigates multi-organ failure, and improves survival in mouse models of jellyfish envenomation syndrome [9].
Novel Immunomodulatory Approaches:
- Sphingosine Analogues: Targeting sphingosine-1-phosphate receptors have shown potential for controlling virus-induced cytokine storm by downregulating production of IFN-α, CCL2, IL-6, TNF-α, and IFN-γ [3].
- PPAR Agonists: Peroxisome proliferator-activated receptors agonists such as gemfibrozil, pioglitazone, and rosiglitazone downregulate inflammatory response to virus-induced lung inflammation [3].
Future Research Directions
Despite therapeutic advances, the overall mortality rate of cytokine storm resulting from underlying diseases remains high [1]. Several key research directions warrant further investigation:
Biomarker Discovery and Validation: Implementation of biomarker tests to inform personalized treatment approaches is crucial [4]. Proteins such as CXCL13 show promise for predicting patient response to specific therapies like siltuximab [4]. Research should focus on validating these biomarkers across different CS syndromes and developing rapid clinical assays.
Personalized Immunomodulation: A personalized approach to treatment based on biomarkers and comorbidities offers significant potential for improving outcomes [8]. This requires better understanding of individual host responses and proper administration timing of immunomodulatory therapies [3].
Combination Therapies: Given the complexity and redundancy of cytokine networks, combination therapies targeting multiple pathways simultaneously may be necessary. Research should explore optimal combinations that maximize efficacy while minimizing immunosuppressive complications.
Novel Molecular Targets: Continued investigation into the molecular mechanisms of CS, including the role of neutrophil extracellular traps, NLRP3 inflammasome, and other signaling pathways may reveal new therapeutic targets [1]. Better understanding of PANoptosis and its regulation may provide opportunities for novel interventions [6].
Cytokine storm represents a complex, life-threatening systemic inflammatory syndrome with diverse clinical manifestations and etiologies. Understanding its historical context, defining clinical syndromes, elucidating molecular mechanisms through appropriate experimental models, and developing targeted therapeutic strategies are crucial for improving patient outcomes. Continued research into the intricate networks of immune activation, inflammatory cell death, and biomarker discovery will enable more precise diagnostic and therapeutic approaches for this highly lethal condition. As research progresses, personalized immunomodulation strategies based on individual patient biomarkers and underlying pathophysiology offer the greatest potential for advancing the management of cytokine storm syndromes.
Cytokine storm (CS) is a life-threatening systemic inflammatory syndrome characterized by hyperactivation of immune cells and elevated levels of circulating cytokines, driving the pathogenesis of multiple organ failure [1]. This maladaptive immune response represents a critical juncture in the progression of severe infections, autoimmune disorders, and certain treatment modalities, with high mortality rates stemming from associated complications such as acute respiratory distress syndrome (ARDS) and fulminant myocarditis [1] [10]. Understanding the precise initiating stimuli and their downstream consequences is paramount for developing targeted therapeutic strategies. This technical guide provides a comprehensive examination of three principal CS categories—pathogen-induced, autoinflammatory, and therapy-associated—framed within contemporary research on cytokine storm and multi-organ failure mechanisms. We synthesize current knowledge on underlying molecular pathways, diagnostic biomarkers, and experimental approaches, providing researchers and drug development professionals with essential tools for advancing therapeutic innovation in this critical field.
Pathogen-Induced Cytokine Storm
Mechanisms and Key Pathways
Pathogen-induced cytokine storm represents a dysregulated host response to infectious agents, characterized by excessive activation of pattern recognition receptors (PRRs) and subsequent hyperinflammation [11] [10]. The innate immune system detects pathogen-associated molecular patterns (PAMPs) through various receptors, including Toll-like receptors (TLRs), retinoic acid-inducible gene I (RIG-I)-like receptors (RLRs), and nucleotide-binding oligomerization domain (NOD)-like receptors (NLRs) [11]. This recognition triggers downstream signaling cascades, notably NF-κB and AP-1, which upregulate pro-inflammatory gene programs, leading to massive cytokine production [10].
SARS-CoV-2 infection provides a well-characterized model of pathogen-induced CS. The viral spike glycoprotein engages host receptors including ACE2, initiating intracellular signaling that activates multiple PRR pathways [11]. Importantly, SARS-CoV-2 proteins induce mitochondrial damage, resulting in mitochondrial DNA (mitDNA) release that activates the cGAS-STING pathway, contributing to IFN-β expression and vascular damage in severe COVID-19 [11]. Viral evasion strategies, particularly inhibition of IFN-I/III production, further contribute to immune dysregulation [11].
In sepsis, the cytokine storm is driven by uncontrolled systemic inflammation in response to bacterial or other pathogens [10]. PAMPs and damage-associated molecular patterns (DAMPs) activate PRRs on innate immune cells, triggering inflammasome formation and activating caspase-1, which processes pro-IL-1β and pro-IL-18 into their active forms [10]. Inflammatory cell death pathways—pyroptosis, necroptosis, and their integration as panoptosis—create a self-amplifying circuit wherein PAMPs, DAMPs, and pro-inflammatory cytokines perpetuate immune dysfunction and tissue injury [10].
Signalling Pathways in Pathogen-Induced Cytokine Storm
The following diagram illustrates key signalling pathways in pathogen-induced cytokine storm, integrating PRR activation, downstream signalling cascades, and cytokine production.
Quantitative Biomarkers and Clinical Parameters
Table 1: Key Biomarkers in Pathogen-Induced Cytokine Storm
| Biomarker | Physiological Role | Association with CS | Cut-off Values |
|---|---|---|---|
| IL-6 | Pro-inflammatory cytokine; induces acute phase proteins | Primary driver of CRS; correlates with mortality | >19.5 pg/mL predicts severe COVID-19 [8] |
| sCD163 | Scavenger receptor on macrophages; marker of activation | Macrophage activation syndrome; disease severity | Elevated in severe COVID-19 [12] |
| HGF | Tissue repair and anti-inflammatory regulation | Predictor for ICU admission/fatal outcome in COVID-19 | Combined with CXCL13 predicts outcome [12] |
| Pentraxin 3 | Acute phase protein; innate immunity regulation | Predicts COVID-19 disease severity | Elevated in severe cases [12] |
| Serum Amyloid A | Acute phase reactant; modulates innate immunity | Reflects systemic inflammation intensity in sepsis | 1000-fold increase in septic shock [10] |
| Monocyte Distribution Width | Monocyte size heterogeneity | Early sepsis detection in emergency settings | >23.5 optimal cutoff [10] |
Experimental Protocols for Pathogen-Induced CS
Protocol 1: In Vitro Macrophage Activation Assay
- Objective: To quantify macrophage activation and cytokine production in response to pathogen-associated molecular patterns.
- Materials: Human monocyte-derived macrophages (MDMs) or THP-1 cell line; ultrapure LPS (TLR4 agonist); poly(I:C) (TLR3 agonist); cell culture reagents; ELISA kits for TNF-α, IL-6, IL-1β.
- Procedure:
- Differentiate THP-1 cells into macrophages using 100 nM PMA for 48 hours or isolate MDMs from human blood.
- Seed cells in 24-well plates at 2×10^5 cells/well and allow to adhere overnight.
- Stimulate with LPS (100 ng/mL) or poly(I:C) (10 μg/mL) for 6-24 hours.
- Collect culture supernatants and measure cytokine levels via ELISA.
- Analyze cells for surface activation markers (e.g., CD86, HLA-DR) by flow cytometry.
- Applications: Screening of immunomodulatory compounds; mechanistic studies of PRR signaling [11] [10].
Protocol 2: Longitudinal Biomarker Profiling in Clinical Samples
- Objective: To establish temporal cytokine profiles correlating with disease severity.
- Materials: Serial serum/plasma samples from infected patients; multiplex bead-based array (e.g., Luminex) measuring 50+ analytes; clinical severity scoring system (e.g., SCODA score for COVID-19).
- Procedure:
- Collect blood samples at predetermined intervals (e.g., days 1, 3, 7, 14 post-admission).
- Process samples within 1 hour of collection; store at -80°C.
- Measure analyte concentrations using validated multiplex panels.
- Correlate analyte levels with daily clinical severity scores using multivariate statistical models.
- Applications: Identification of prognostic biomarkers; patient stratification for targeted therapy [12].
Autoinflammatory Cytokine Storm
Mechanisms and Key Pathways
Autoinflammatory cytokine storm arises from dysregulated innate immunity in the absence of external pathogens, characterized by uncontrolled activation of the interleukin-1 (IL-1) family cytokines and type I interferon (IFN) responses [13]. This category encompasses systemic autoimmune diseases such as systemic lupus erythematosus (SLE), rheumatoid arthritis (RA), and Sjögren's syndrome (SS), where loss of immune self-tolerance leads to aberrant attacks on host tissues [13]. The pathogenesis involves complex interactions between genetic predisposition, environmental triggers, and breakdown of immune regulatory mechanisms.
The JAK/STAT signaling pathway plays a central role in autoinflammatory CS, transducing signals from multiple cytokine receptors to regulate immune cell differentiation and function [1]. In SLE, enhanced type I IFN signaling creates a positive feedback loop that promotes autoantibody production by B cells and dendritic cell activation [13]. Similarly, in RA, synovial fibroblasts exhibit constitutive activation of STAT3, driving production of pro-inflammatory mediators including IL-6, IL-1β, and TNF-α that perpetuate joint inflammation and destruction [1] [13].
Inflammasome activation represents another critical mechanism in autoinflammatory CS. The NLRP3 inflammasome, activated by various DAMPs, processes pro-IL-1β and pro-IL-18 into their active forms, initiating potent inflammatory responses [1]. Gasdermin D-mediated pyroptosis further amplifies inflammation by releasing additional DAMPs and cytokines, creating a self-perpetuating cycle of tissue damage and immune activation [10].
Signalling Pathways in Autoinflammatory Cytokine Storm
The following diagram illustrates key signalling pathways in autoinflammatory cytokine storm, focusing on JAK/STAT signalling and inflammasome activation.
Quantitative Biomarkers and Clinical Parameters
Table 2: Key Biomarkers in Autoinflammatory Cytokine Storm
| Biomarker | Associated Conditions | Pathogenic Role | Therapeutic Implications |
|---|---|---|---|
| Type I Interferons | SLE, Sjögren's syndrome | Initiate autoimmune activation; enhance antigen presentation | Anti-IFN therapies in development [13] |
| IL-6 | Rheumatoid arthritis, adult-onset Still's disease | Promotes Th17 differentiation; acute phase response | Tocilizumab (IL-6R inhibitor) approved for RA [1] [13] |
| TNF-α | Rheumatoid arthritis, ankylosing spondylitis | Drives synovitis; bone and cartilage destruction | TNF inhibitors established therapy [13] |
| IL-1β | Autoinflammatory syndromes (CAPS), Still's disease | Pyrogenic; activates endothelium; neutrophil recruitment | Anakinra (IL-1Ra) effective in autoinflammatory diseases [1] [13] |
| Autoantibodies | SLE (anti-dsDNA), RA (RF, anti-CCP) | Form immune complexes; activate complement | B-cell depletion therapies [13] |
| CXCL13 | SLE, rheumatoid arthritis | B-cell chemoattractant; lymphoid neogenesis | Marker of disease activity [13] |
Experimental Protocols for Autoinflammatory CS
Protocol 1: JAK/STAT Signaling Inhibition Assay
- Objective: To evaluate the efficacy of JAK inhibitors in suppressing cytokine signaling in autoimmune models.
- Materials: Peripheral blood mononuclear cells (PBMCs) from patients or healthy donors; JAK inhibitors (e.g., ruxolitinib, tofacitinib); recombinant human cytokines (IFN-α, IL-6); phospho-flow cytometry antibodies.
- Procedure:
- Isolate PBMCs using density gradient centrifugation.
- Pre-treat cells with JAK inhibitors (0.1-1000 nM) for 1 hour.
- Stimulate with IFN-α (1000 U/mL) or IL-6 (50 ng/mL) for 15-30 minutes.
- Fix cells with 4% PFA, permeabilize with ice-cold methanol, and stain with anti-pSTAT1 or anti-pSTAT3 antibodies.
- Analyze STAT phosphorylation by flow cytometry.
- Applications: Screening JAK inhibitor potency; personalized medicine approaches for autoimmune diseases [1] [13].
Protocol 2: Inflammasome Activation and Inhibition Assay
- Objective: To measure NLRP3 inflammasome activation and test inhibitory compounds.
- Materials: Human or murine macrophages; NLRP3 activators (ATP, nigericin, uric acid crystals); caspase-1 inhibitor (VX-765); IL-1β ELISA; FLICA caspase-1 assay kit.
- Procedure:
- Prime macrophages with ultrapure LPS (100 ng/mL) for 3 hours.
- Pre-treat with test compounds for 1 hour.
- Activate NLRP3 with ATP (5 mM) or nigericin (10 μM) for 1 hour.
- Measure mature IL-1β in supernatant by ELISA.
- Assess caspase-1 activation using FLICA reagent followed by flow cytometry.
- Applications: Mechanistic studies of autoinflammatory diseases; screening NLRP3 inhibitors [1] [10].
Therapy-Associated Cytokine Storm
Mechanisms and Key Pathways
Therapy-associated cytokine storm represents a significant challenge in modern medical treatments, particularly in immunotherapy. The most characterized form is cytokine release syndrome (CRS) following chimeric antigen receptor T-cell (CAR-T) therapy, with an incidence ranging from 37% to 93% depending on the construct and malignancy [1]. CRS typically manifests within days of infusion, characterized by excessive activation of CAR-T cells and endogenous immune cells, leading to massive cytokine production including IL-6, IFN-γ, and GM-CSF [1].
The JAK/STAT pathway is critically implicated in therapy-associated CS. Appropriate JAK/STAT activation enhances antitumor activity of CAR-T cells, whereas overactivation contributes to CRS [1]. Inhibition of JAK1 has been shown to reduce CRS severity without completely abrogating CAR-T cell function, suggesting a potential therapeutic approach [1]. Additionally, monocytes and macrophages are now recognized as primary producers of key cytokines like IL-6 and IL-1 during CRS, activated by contact with CAR-T cells or through IFN-γ signaling [1].
Another therapy-associated CS occurs in acute graft-versus-host disease (aGVHD) following allogeneic hematopoietic stem cell transplantation, where donor T cells recognize host antigens, triggering inflammatory cascades [1]. The JAK/STAT pathway mediates pro-GVHD effects of natural killer cells, with STAT1 and STAT3 playing essential roles in cytokine production and regulatory T cell fate determination [1].
Signalling Pathways in Therapy-Associated Cytokine Storm
The following diagram illustrates key signalling pathways in therapy-associated cytokine storm, focusing on CAR-T cell and therapeutic antibody responses.
Quantitative Biomarkers and Clinical Parameters
Table 3: Key Biomarkers in Therapy-Associated Cytokine Storm
| Biomarker | Therapeutic Context | Kinetics | Intervention Thresholds |
|---|---|---|---|
| IL-6 | CAR-T therapy, aGVHD, IT | Peaks within 1-2 days post-infusion | Tocilizumab administration at grade ≥2 CRS [1] |
| IFN-γ | CAR-T therapy, immune checkpoint inhibitors | Early rise (within 24 hours) | Predictive marker for severe CRS [1] |
| GM-CSF | CAR-T therapy | Early elevation | Target for prevention (e.g., lenzilumab) [1] |
| sCD163 | CAR-T therapy, aGVHD | Marker of macrophage activation | Correlates with severe neurotoxicity [1] |
| IL-2 | aGVHD, T-cell engaging therapies | Early elevation | Target for inhibition (daclizumab) [1] |
| Angiopoietin-2 | CAR-T therapy | Endothelial activation | Associated with severe CRS and vascular leakage [14] |
Experimental Protocols for Therapy-Associated CS
Protocol 1: In Vitro CRS Model with CAR-T Cells
- Objective: To recapitulate CRS in vitro and test prophylactic or therapeutic interventions.
- Materials: CAR-T cells (CD19-targeting or other specificity); target tumor cell lines; human PBMCs or monocyte-derived macrophages; cytokine measurement platform.
- Procedure:
- Co-culture CAR-T cells with target tumor cells at various effector:target ratios (e.g., 1:1 to 10:1).
- Add PBMCs or macrophages to the system (CAR-T:tumor:PBMC ratio of 1:1:2).
- Collect supernatants at 6, 24, 48, and 72 hours for cytokine analysis (IL-6, IFN-γ, GM-CSF).
- Test JAK inhibitors (ruxolitinib) or monoclonal antibodies (tocilizumab) added at time of co-culture or after cytokine elevation.
- Applications: Preclinical assessment of CRS risk for novel CAR constructs; screening mitigation strategies [1].
Protocol 2: JAK Inhibitor Efficacy in Humanized Mouse Models
- Objective: To evaluate JAK inhibition for managing therapy-associated CS in vivo.
- Materials: NSG mice; human PBMCs (for GVHD model) or CAR-T cells plus tumor cells (for CRS model); ruxolitinib; monitoring equipment.
- Procedure:
- For GVHD: Inject human PBMCs intravenously to create xenogeneic GVHD model.
- For CRS: Establish tumor xenografts followed by CAR-T cell infusion.
- Administer ruxolitinib (30-60 mg/kg twice daily) prophylactically or therapeutically.
- Monitor mice for clinical scores, weight loss, and survival.
- Measure human cytokine levels in serial blood samples using species-specific ELISA.
- Applications: In vivo validation of JAK inhibitors for CS management; dose optimization studies [15].
The Scientist's Toolkit
Table 4: Essential Research Reagent Solutions for Cytokine Storm Investigation
| Reagent Category | Specific Examples | Research Application | Key Function |
|---|---|---|---|
| JAK/STAT Inhibitors | Ruxolitinib (JAK1/2), Tofacitinib (JAK1/3) | Pathogen-induced, autoinflammatory, and therapy-associated CS | Suppresses cytokine signaling; reduces inflammatory gene expression [1] [15] |
| Cytokine Monoclonal Antibodies | Tocilizumab (anti-IL-6R), Anakinra (IL-1Ra) | All CS categories | Neutralizes specific cytokines or blocks their receptors [1] [14] |
| Multiplex Cytokine Arrays | Luminex xMAP Technology, MSD U-PLEX | Biomarker discovery and profiling | Simultaneous quantification of multiple cytokines in limited sample volumes [12] |
| Phospho-Specific Flow Cytometry | Anti-pSTAT1, pSTAT3, pSTAT5 antibodies | Signaling pathway analysis | Measures activation status of intracellular signaling pathways in immune cell subsets [1] |
| Inflammasome Activators | ATP, Nigericin, Monosodium Urate Crystals | Autoinflammatory CS models | Activates NLRP3 inflammasome for mechanistic studies and inhibitor screening [10] |
| Humanized Mouse Models | NSG mice with human immune system | Therapy-associated CS (CAR-T, GVHD) | In vivo modeling of human-specific immune responses and therapeutic efficacy [1] |
Concluding Perspectives
This technical guide has systematically delineated the key initiating stimuli, molecular mechanisms, and research methodologies for investigating cytokine storm across three principal categories. The intricate interplay between pathogen recognition, autoimmune dysregulation, and therapeutic interventions reveals both unique and shared pathways that culminate in uncontrolled systemic inflammation. Critical examination of the JAK/STAT pathway, inflammasome activation, and inflammatory cell death mechanisms across these contexts provides a framework for understanding the fundamental principles governing CS pathogenesis.
The evolving landscape of CS research underscores the importance of precision medicine approaches, leveraging biomarker profiles for early intervention and patient stratification. Future research directions should focus on elucidating the temporal dynamics of cytokine networks, identifying novel checkpoint regulators of immune homeostasis, and developing targeted therapies that mitigate pathological inflammation while preserving protective immunity. Integration of advanced technologies including single-cell multi-omics, computational modeling, and humanized systems immunology will accelerate progress in this critically important field, ultimately reducing the burden of multi-organ failure and mortality associated with cytokine storm syndromes.
Cytokine storm (CS), also referred to as cytokine release syndrome (CRS), is a life-threatening systemic inflammatory syndrome characterized by hyperactivation of immune cells and elevated levels of circulating cytokines. This pathological process is implicated in the development of severe conditions including acute respiratory distress syndrome (ARDS), multi-organ failure (MOF), hemophagocytic lymphohistiocytosis (HLH), and complications from immunotherapies [1]. The uncontrolled and aberrant inflammatory response, rather than the pathogen itself, can result in unintended complications and multi-organ failure [16]. At the core of this dysregulated immune response are key inflammatory mediators, notably Tumor Necrosis Factor-α (TNF-α), Interferon-γ (IFN-γ), Interleukin-1 (IL-1), and Interleukin-6 (IL-6). These cytokines form a complex signaling network that amplifies inflammation, leading to collateral vital organ damage [16] [1]. This review provides an in-depth examination of these four core mediators, their interconnected signaling pathways, and their collective contribution to the pathogenesis of cytokine storm and subsequent multiple organ dysfunction.
Cytokine Profiles and Pathophysiological Roles
The table below summarizes the core structural and functional characteristics of each key inflammatory mediator.
Table 1: Characteristics and Pathogenic Roles of Core Inflammatory Mediators
| Cytokine | Primary Cell Sources | Main Receptors | Key Signaling Pathways | Major Pathogenic Roles in Cytokine Storm |
|---|---|---|---|---|
| TNF-α | Macrophages, Monocytes, Lymphocytes | TNFR1, TNFR2 | NF-κB, MAPK | Endothelial damage, vascular permeability, coagulopathy, fever, apoptosis [16] [17] |
| IFN-γ | NK cells, NKT cells, Th1 CD4+ T cells, CD8+ T cells | IFNGR1, IFNGR2 | JAK-STAT | Macrophage activation, MHC upregulation, promotes Th1 polarization, tissue immunopathology [18] [19] |
| IL-1 (IL-1α/IL-1β) | Macrophages, Monocytes (IL-1β);Non-immune cells (IL-1α) | IL-1R1, IL-1RAcP | MyD88/NF-κB, MAPK | Fever, acute phase response, pyroptosis, "alarmin" function (IL-1α), potent pro-inflammatory effects [20] [21] |
| IL-6 | Macrophages, Dendritic cells, Epithelial cells | IL-6R, gp130 | JAK-STAT | Acute phase response, B/T cell differentiation, fever, inflammation amplifier [1] [22] |
Quantitative Cytokine Levels in Clinical Scenarios
The concentration of these cytokines in circulation can provide critical insights into disease severity and prognosis during a cytokine storm.
Table 2: Cytokine Levels in Human Cytokine Storm Conditions
| Cytokine | Baseline Level (Healthy) | Level in Inflammatory Disease | Association with Clinical Outcomes |
|---|---|---|---|
| IFN-γ | Low or undetectable | - Septic Hyperinflammation: >3 pg/mL defines IFNγ-driven sepsis (IDS) endotype [19].- HLH: Markedly elevated [1]. | High levels with concurrent CXCL9 >2200 pg/mL linked to increased mortality in sepsis [19]. |
| IL-6 | Low (pg/mL range) | - COVID-19 ARDS: Significantly elevated vs. non-ARDS patients [23].- IAV Infection: Correlates with disease severity and poor outcomes [22]. | A predictor of mortality in severe COVID-19; levels increase in non-survivors [23]. |
| TNF-α | Low (pg/mL range) | - COVID-19 ARDS: Elevated in ARDS patients vs. controls [23].- MOF: Transmembrane TNF-α (tmTNF-α) on neutrophils is a potential diagnostic marker for CS [17]. | tmTNF-α expression correlates with liver/kidney damage in MOF mice; better CS diagnostic value than serum TNF-α [17]. |
| IL-1β | Low (pg/mL range) | Elevated in severe inflammatory and autoinflammatory diseases (e.g., CAPS, Still's disease) [20]. | Caspase-1 activity and plasma IL-18 (IL-1 family) correlate with COVID-19 severity [16]. |
Signaling Pathways in Cytokine Storm
The pathogenesis of cytokine storm involves the dysregulation of several key intracellular signaling pathways, which are activated by the core mediators upon binding to their respective receptors.
The JAK-STAT Signaling Pathway
The JAK-STAT pathway is a highly conserved signaling cascade critical for the cellular responses to numerous cytokines, including IFN-γ and IL-6 [1]. The pathway consists of transmembrane receptors, receptor-associated Janus kinases (JAKs), and signal transducers and activators of transcription (STATs) [1].
- IFN-γ Signaling: Binding of IFN-γ to its receptor (IFNGR1/IFNGR2) activates receptor-associated JAK1 and JAK2, which phosphorylate STAT1. Phosphorylated STAT1 forms homodimers (known as gamma-activated factor, GAF), translocates to the nucleus, and drives the expression of interferon-stimulated genes (ISGs) with diverse pro-inflammatory functions [18] [1].
- IL-6 Signaling: IL-6 binds to its membrane-bound IL-6 receptor (mIL-6R) or soluble IL-6R (sIL-6R), leading to gp130 dimerization and activation of JAK1/JAK2. This primarily results in the phosphorylation and dimerization of STAT3, which translocates to the nucleus to promote the expression of a wide portfolio of inflammatory genes, including IL-1β, IL-8, CCL2, and GM-CSF [1]. This IL-6/IL-6R/JAK/STAT3 activation cascade results in a systemic hyperinflammatory response [1].
The IL-1/TLR Signaling Pathway
The IL-1/TLR pathway is fundamental to innate immunity [20]. The cytosolic segment of each IL-1 receptor family member contains the Toll-IL-1-receptor (TIR) domain, which is also present in Toll-like receptors (TLRs) [20] [21].
- Receptor Activation: IL-1 (IL-1α or IL-1β) first binds to the ligand-binding chain (IL-1R1), followed by recruitment of the coreceptor chain (IL-1RAcP). Similarly, TLRs are activated by recognizing pathogen-associated molecular patterns (PAMPs) or damage-associated molecular patterns (DAMPs) [16] [1].
- Downstream Signaling: The formation of the receptor complex brings the intracellular TIR domains together, enabling the recruitment of the adaptor protein MyD88. This initiates a signaling cascade involving IRAK kinases and TRAF6, ultimately leading to the activation of the IKK complex [20] [21]. The IKK complex phosphorylates the inhibitory protein IκB, targeting it for degradation and thus releasing the transcription factor NF-κB. NF-κB translocates to the nucleus and drives the expression of a large portfolio of inflammatory genes, including the cytokines themselves (e.g., IL-6, TNF-α), chemokines, and adhesion molecules [16] [21]. This pathway is a primary driver of the pro-inflammatory gene expression seen in cytokine storm.
The Inflammasome Pathway
The inflammasome pathway is a critical platform for the maturation of key cytokines of the IL-1 family, primarily IL-1β and IL-18 [16] [21].
- Two-Step Process: Activation is typically a two-step process. A priming signal (e.g., from TLRs) induces the expression of pro-IL-1β and pro-IL-18, as well as inflammasome components themselves. A second activation signal (e.g., ATP, viral RNA, ROS) triggers the assembly of the inflammasome complex (e.g., NLRP3) [16].
- Caspase-1 Activation and Pyroptosis: The inflammasome recruits and activates caspase-1. Active caspase-1 then performs two critical functions: 1) It cleaves the pro-forms of IL-1β and IL-18 into their mature, bioactive forms. 2) It cleaves gasdermin D (GSDMD), generating N-terminal fragments that oligomerize and form pores in the plasma membrane [16] [21]. These pores allow the release of the mature cytokines and also lead to a pro-inflammatory form of lytic cell death called pyroptosis, which further amplifies the inflammatory response by releasing cellular contents [16]. SARS-CoV-2 proteins have been shown to promote activation of inflammasomes such as the NLRP3 inflammasome [16].
Experimental Methodologies for Cytokine Research
Key Assays and Techniques
Studying cytokine storm requires a multifaceted experimental approach to quantify cytokines, characterize immune cell responses, and assess resulting organ damage.
Table 3: Key Experimental Protocols for Cytokine Storm Research
| Methodology | Key Application | Technical Description | Example from Literature |
|---|---|---|---|
| Enzyme-Linked Immunosorbent Assay (ELISA) | Quantification of soluble cytokines in serum/plasma. | Uses specific antibodies to capture and detect target cytokines, with colorimetric or chemiluminescent readouts. | Used to measure TNF-α, IL-18, INF-γ, IL-6, IL-4, and CRP in mouse plasma [17] and human serum [23]. |
| Flow Cytometry (FCM) | Analysis of cell surface and intracellular proteins in immune cells. | Uses fluorescently labeled antibodies to detect markers on or in single cells suspended in a fluid stream. | Used to analyze transmembrane TNF-α (tmTNF-α) expression on neutrophils and PBMCs in mouse models of MOF [17]. |
| Histopathology (H&E Staining) | Assessment of tissue damage and immune cell infiltration. | Tissue sections are stained with hematoxylin and eosin to visualize overall structure and nuclei/cytoplasm. | Used to evaluate liver and kidney tissue damage (sinus congestion, necrosis, inflammatory infiltration) in MOF mice [17]. |
| Animal Models of Cytokine Storm | In vivo study of CS pathogenesis and therapeutic interventions. | Models include LPS/D-Galactosamine-induced liver failure/MOF [17] and pathogen-specific infections (e.g., IAV in mice [22]). | The LPS/D-Gal mouse model reproduces key features of human CS, including elevated cytokines and organ dysfunction [17]. |
The Scientist's Toolkit: Essential Research Reagents
Table 4: Essential Research Reagents for Cytokine Storm Investigation
| Reagent / Material | Function/Application | Specific Example |
|---|---|---|
| Recombinant Cytokines | Used as positive controls, to stimulate cells in vitro, or to create animal models of hyperinflammation. | Recombinant IFNγ is used in studies to restore immune function in immunosuppressed sepsis [19]. |
| Cytokine-Specific Antibodies | Core reagents for detection techniques like ELISA, Flow Cytometry, and Immunohistochemistry. | PE-conjugated anti-mouse TNF-α antibody for flow cytometry [17]; antibody pairs for cytokine-specific ELISA kits [17] [23]. |
| Cytokine Neutralizing Antibodies / Inhibitors | To block cytokine activity in vitro and in vivo, establishing mechanistic causality. | Anakinra (IL-1 receptor antagonist) [20] [24]; Bermekimab (anti-IL-1α mAb) [24]; JAK inhibitors (target JAK-STAT pathway) [1]. |
| LPS (Lipopolysaccharide) | A potent PAMP used to trigger innate immune responses and induce experimental inflammation and endotoxemia. | Used in combination with D-Galactosamine to create a mouse model of acute liver failure and MOF [17]. |
| ELISA Kits | Ready-to-use kits for standardized quantification of specific cytokine concentrations in biological fluids. | Commercial kits used to measure TNF-α, IL-18, INF-γ, IL-6, IL-4, and CRP in mouse plasma [17]. |
| Flow Cytometry Staining Reagents | Antibodies, buffers, and viability dyes for immunophenotyping and intracellular cytokine staining. | Stromatolyser-4DL FFD-201A for lysing RBCs; staining buffers and fluorochrome-conjugated antibodies for surface/intracellular markers [17]. |
The core inflammatory mediators TNF-α, IFN-γ, IL-1, and IL-6 function as an integrated network, driving the hyperinflammation characteristic of cytokine storm through interconnected signaling pathways like JAK-STAT, IL-1/TLR, and the inflammasome. Their pathogenic role is underscored by clinical data showing elevated levels in severe conditions like COVID-19 ARDS, sepsis, and MOF. Targeting these cytokines and their pathways (e.g., with JAK inhibitors or IL-1 blockers) has demonstrated therapeutic potential, highlighting their centrality in cytokine storm pathology. Future research should focus on further elucidating the temporal dynamics of these mediators and validating novel biomarkers like tmTNF-α to improve diagnostics and personalize immunomodulatory therapy for life-threatening inflammatory syndromes.
Cytokine storms (CS), or cytokine release syndrome, represent a life-threatening hyperinflammatory condition triggered by infections, immunotherapies, and systemic immune dysregulation. Recent research has identified PANoptosis—a unique, inflammatory programmed cell death pathway that integrates components of pyroptosis, apoptosis, and necroptosis—as a central driver of this pathological cascade. This whitepaper examines the molecular mechanisms by which PANoptosis initiates and amplifies cytokine storms, creating a vicious cycle of inflammation and cell death that culminates in multi-organ dysfunction. Through analysis of current evidence from viral infections and immunotherapy models, we explore how PANoptosome complexes sense inflammatory cues to coordinate simultaneous activation of multiple cell death pathways. Furthermore, we discuss emerging therapeutic strategies that target PANoptosis to disrupt this lethal loop, offering novel approaches for managing cytokine storms in critically ill patients.
PANoptosis represents a transformative concept in cell death biology, first conceptualized by Kanneganti's team in 2019 as an inflammatory programmed cell death pathway that cannot be fully explained by pyroptosis, apoptosis, or necroptosis alone [25]. This pathway is characterized by the simultaneous activation of key molecules from all three death pathways, organized within sophisticated multiprotein complexes called PANoptosomes [26]. The functional outcome of PANoptosis is lytic cell death driven by caspases and receptor-interacting protein kinases (RIPKs), resulting in the massive release of inflammatory mediators [26].
Cytokine storms represent a state of uncontrolled systemic inflammation characterized by excessive release of pro-inflammatory cytokines including IL-1β, IL-18, TNF-α, and IFN-γ [27]. Clinically, this manifests as fever, hypotension, multi-organ dysfunction, and potentially death. Recent evidence positions PANoptosis as a critical nexus in cytokine storm pathogenesis, creating a self-amplifying loop wherein cell death releases inflammatory molecules that in turn trigger further cell death [27] [28]. This deadly cycle is particularly relevant in the contexts of severe infections (including SARS-CoV-2 and influenza) and immunotherapy-induced toxicity [27].
Understanding the molecular architecture of PANoptosis and its regulatory mechanisms provides unprecedented opportunities for therapeutic intervention in cytokine storm pathologies. This whitepaper examines the current state of knowledge regarding PANoptosis-driven cytokine storms within the broader context of multiple organ failure mechanisms research.
Molecular Mechanisms of PANoptosis
PANoptosome Complex Architecture
The core executor of PANoptosis is the PANoptosome, a multiprotein complex that serves as a molecular platform for integrating signals from multiple cell death pathways. PANoptosomes typically contain: (1) sensors for pathogen-associated molecular patterns (PAMPs) or damage-associated molecular patterns (DAMPs); (2) adaptor proteins; and (3) catalytic effectors from pyroptosis, apoptosis, and necroptosis pathways [29]. To date, several distinct PANoptosomes have been characterized, each activated by specific triggers and containing unique sensor components.
Table 1: Characterized PANoptosome Complexes and Their Components
| PANoptosome Type | Key Sensor Molecules | Adaptor Proteins | Catalytic Effectors | Primary Activators |
|---|---|---|---|---|
| ZBP1-PANoptosome | ZBP1, NLRP3 | ASC, FADD | Caspase-1/3/6/8, RIPK1/3, MLKL | Influenza A virus, viral Z-RNA [25] [26] |
| AIM2-PANoptosome | AIM2, Pyrin, ZBP1 | ASC, FADD | Caspase-1/8, RIPK1/3 | Francisella novicida, HSV-1, cytosolic DNA [25] [26] |
| RIPK1-PANoptosome | RIPK1, NLRP3 | ASC, FADD | Caspase-1/8, RIPK3 | TAK1 inhibition, Yersinia infection [25] [26] |
| NLRP12-PANoptosome | NLRP12, NLRP3 | ASC | Caspase-8, RIPK3 | Heme plus PAMPs, TNF [26] [30] |
The assembly of these complexes is governed by domain-specific homotypic and heterotypic interactions between molecular components, allowing for context-specific activation in response to diverse cellular threats [26]. This modular architecture provides the structural basis for the simultaneous engagement of multiple cell death pathways.
Signaling Pathways and Execution Mechanisms
Upon activation, PANoptosomes coordinate a sophisticated execution program that engages multiple cell death effectors simultaneously:
- Pyroptotic Component: Caspase-1 cleaves gasdermin D (GSDMD), generating N-terminal fragments that form membrane pores, and processes pro-IL-1β and pro-IL-18 into their active forms [26] [31].
- Apoptotic Component: Caspase-8 activates executioner caspases (caspase-3/7) and cleaves Bid, connecting extrinsic and intrinsic apoptosis pathways [26] [30].
- Necroptotic Component: RIPK3 phosphorylates MLKL, leading to membrane disruption and lytic cell death [26].
Recent research has identified NINJ1 (ninjurin 1) as a key executioner protein that operates alongside other pore-forming proteins during PANoptosis-mediated plasma membrane rupture [29]. This comprehensive engagement of death effectors ensures robust elimination of compromised cells while triggering substantial inflammatory signaling.
Figure 1: PANoptosis Signaling Pathway in Cytokine Storm Pathogenesis. This diagram illustrates the sequential activation of PANoptosis components and the self-amplifying loop that drives cytokine storm progression.
PANoptosis in Cytokine Storm Pathogenesis
Establishing the Death-Inflammation Loop
PANoptosis drives cytokine storms through several interconnected mechanisms that create a self-reinforcing inflammatory cascade:
Direct Cytokine Release: PANoptosis activation results in the maturation and release of potent inflammatory cytokines, particularly IL-1β and IL-18, through caspase-1-mediated cleavage [25] [31]. These cytokines initiate local and systemic inflammatory responses.
DAMP Amplification: The lytic nature of PANoptosis results in the release of intracellular contents including ATP, HMGB1, and DNA, which function as DAMPs [28]. These molecules engage pattern recognition receptors on neighboring cells, propagating inflammatory signaling and additional rounds of PANoptosis.
Immune Cell Recruitment and Activation: Released cytokines and DAMPs recruit and activate innate immune cells, particularly macrophages and neutrophils, which in turn produce additional inflammatory mediators including TNF-α and IFN-γ [27] [30]. These cytokines can further sensitize cells to PANoptosis, creating a positive feedback loop.
Table 2: Key Molecular Mediators in PANoptosis-Driven Cytokine Storms
| Mediator Category | Specific Molecules | Source | Pathogenic Function |
|---|---|---|---|
| Inflammatory Cytokines | IL-1β, IL-18 | Caspase-1 cleavage in PANoptosis | Fever, endothelial activation, leukocyte recruitment [27] [31] |
| Pore-Forming Proteins | GSDMD, GSDME, MLKL, NINJ1 | PANoptosis execution | Membrane permeabilization, lytic cell death, DAMP release [26] [29] |
| Cell Death Kinases | RIPK1, RIPK3 | PANoptosome core | Necroptosis signaling, inflammasome regulation [25] [30] |
| Transcriptional Regulators | IRF1 | Upstream signaling | Regulates expression of ZBP1, AIM2, NLRP12 [26] |
Evidence from Disease Models
Research across multiple disease models has established the central role of PANoptosis in cytokine storm pathogenesis:
Viral Infections: In influenza A virus infection, ZBP1-PANoptosome activation triggers PANoptosis with concurrent activation of caspase-1 (pyroptosis), caspase-3/8 (apoptosis), and RIPK3/MLKL (necroptosis) [25] [26]. Inhibition of all three pathways is required to block cell death, demonstrating the functional integration within PANoptosis.
Sepsis: PANoptosis contributes significantly to multi-organ dysfunction in sepsis by promoting the release of inflammatory cytokines that disrupt immune cell homeostasis and exacerbate organ damage [28]. Studies demonstrate that PANoptosis inhibition improves survival in septic models.
Immunotherapy Toxicity: In chimeric antigen receptor (CAR)-T cell therapy and other immunotherapies, PANoptosis has been identified as a key contributor to cytokine release syndrome pathology [27]. The extensive tissue damage and immune activation triggered by these therapies creates ideal conditions for PANoptosis initiation.
The feed-forward nature of the PANoptosis-cytokine storm loop explains the rapid clinical deterioration observed in these conditions and underscores the therapeutic potential of targeting this pathway.
Experimental Analysis of PANoptosis
Methodologies for PANoptosis Detection
Comprehensive assessment of PANoptosis requires multiparameter experimental approaches that simultaneously evaluate markers across all three cell death pathways:
Table 3: Essential Methodologies for PANoptosis Detection and Characterization
| Methodology Category | Specific Techniques | Key Readouts | Experimental Considerations |
|---|---|---|---|
| Cell Death Assessment | Time-lapse microscopy, LDH release, propidium iodide uptake | Membrane integrity, lytic cell death | Requires comparison with single pathway inhibitors [26] |
| Protein Activation Analysis | Western blot, immunofluorescence, flow cytometry | Caspase-1/3/8 cleavage, pMLKL, GSDMD cleavage | Multiple markers must be assessed simultaneously [25] [29] |
| Complex Formation Studies | Co-immunoprecipitation, ASC speck formation, proximity ligation | PANoptosome assembly, protein-protein interactions | Cell-type and stimulus specific variations occur [26] |
| Genetic Manipulation | CRISPR/Cas9 knockout, siRNA knockdown, dominant-negative constructs | ZBP1, AIM2, RIPK1, RIPK3, caspase function | Functional redundancy may require multiple knockouts [25] |
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagent Solutions for PANoptosis Investigation
| Reagent Category | Specific Examples | Research Application | Functional Role |
|---|---|---|---|
| PANoptosis Inducers | Influenza A virus, Francisella novicida, HSV-1, heme + PAMPs | Experimental PANoptosis triggering | Activate specific PANoptosomes (ZBP1, AIM2, NLRP12) [25] [26] |
| Gene Targeting Tools | ZBP1 KO cells, RIPK1 kinase-dead mutants, caspase-8 deficient cells | Pathway necessity testing | Establish genetic requirements for PANoptosis [25] [30] |
| Chemical Inhibitors | VX-765 (caspase-1), Z-VAD-FMK (pan-caspase), Necrostatin-1 (RIPK1), GSK'872 (RIPK3) | Pathway dissection | Inhibit specific death pathways; all three required to block PANoptosis [26] [30] |
| Detection Antibodies | Anti-cleaved caspase-3, anti-pMLKL, anti-GSDMD, anti-cleaved caspase-1 | Pathway activation assessment | Detect specific activation markers of each cell death pathway [25] [29] |
Figure 2: Experimental Workflow for PANoptosis Investigation. This diagram outlines the key methodological approaches for inducing, inhibiting, and validating PANoptosis in experimental systems.
Therapeutic Targeting of PANoptosis in Cytokine Storms
Strategic Intervention Points
The molecular characterization of PANoptosis has revealed multiple potential intervention points for disrupting the cell death-inflammation loop in cytokine storms:
PANoptosome Assembly Inhibition: Targeting upstream sensors or adaptor proteins required for PANoptosome formation represents a promising strategic approach. ZBP1, AIM2, and NLRP3 inhibitors could prevent the initiation of the PANoptotic cascade in context-specific manners [25] [31].
Key Effector Molecules: Simultaneous inhibition of multiple cell death effectors may be required to effectively block PANoptosis. Combination therapies targeting caspase-1, caspase-8, and RIPK1/3 have shown promise in preclinical models [30].
Cytokine Neutralization: Existing biologic therapies that target key PANoptosis-associated cytokines, including IL-1β and IL-18 antagonists, may provide clinical benefit by interrupting the inflammatory amplification loop [27] [31].
Logic-Gated Approaches: Innovative strategies such as "logic-gated" activation of PANoptosis modulators that target specific cell populations could maximize therapeutic efficacy while minimizing systemic toxicity [25].
Clinical Translation and Challenges
Despite promising preclinical data, several challenges remain in therapeutically targeting PANoptosis:
Contextual Specificity: PANoptosome composition and regulation varies by cell type, trigger, and disease state, necessitating careful patient stratification and context-appropriate therapeutic selection [25] [30].
Redundancy and Compensation: The inherent redundancy in cell death pathways may allow for compensatory activation when individual components are inhibited, potentially limiting efficacy of single-target approaches [26].
Therapeutic Window: Given the essential role of regulated cell death in host defense and homeostasis, achieving selective inhibition of pathological PANoptosis without disrupting physiological cell death represents a significant challenge.
Ongoing clinical trials evaluating inflammasome-targeting therapies may provide valuable insights into the translatability of PANoptosis modulation for cytokine storm management [31].
PANoptosis represents a critical pathogenic mechanism bridging cell death and inflammation in cytokine storm syndromes. The integrated nature of this cell death pathway explains why historical approaches targeting individual death mechanisms have shown limited success in controlling hyperinflammatory states. Future research directions should focus on:
- Structural Resolution of additional PANoptosome complexes to enable rational drug design.
- Dynamic Mapping of PANoptosis regulatory networks across different pathological contexts.
- Advanced Therapeutic Delivery systems capable of cell-type-specific targeting of PANoptosis components.
- Biomarker Development to identify patients with active PANoptosis who would benefit from targeted therapies.
As our understanding of PANoptosis continues to evolve, so too will our ability to strategically intervene in this lethal process. The concept of targeting PANoptosis offers a promising avenue for developing innovative treatments for cytokine storms and improving outcomes in patients undergoing immunotherapy or battling severe infections.
Hyperinflammation, a state of exaggerated and dysregulated immune activation, is a central driver of severe pathological conditions including cytokine storm syndromes, sepsis, and multiple organ failure. This maladaptive response is characterized by the overproduction of pro-inflammatory cytokines and the massive recruitment of immune cells, leading to collateral tissue damage and organ dysfunction. At the molecular heart of hyperinflammation lie three critically interconnected signaling pathways: the Janus kinase-signal transducer and activator of transcription (JAK-STAT) pathway, the Toll-like receptor (TLR) system, and the inflammasome activation cascade [32] [33] [34]. Individually, each pathway orchestrates specific aspects of the immune response; together, they form a complex network that amplifies inflammatory signaling, often with devastating clinical consequences. Understanding the mechanisms, regulation, and crosstalk between these pathways is not only fundamental to deciphering the biology of cytokine storms but also paramount for developing targeted therapeutic strategies to curb immune-mediated organ damage without compromising host defense. This whitepaper provides an in-depth analysis of these core signaling axes, framed within the context of modern cytokine storm research.
The JAK-STAT Signaling Pathway in Hyperinflammation
Pathway Architecture and Mechanism
The JAK-STAT pathway serves as a crucial conduit for transmitting signals from extracellular cytokines and growth factors directly to the nucleus, thereby regulating gene expression programs governing immune cell activation, proliferation, and differentiation [35]. This signaling cascade is notable for its comparative simplicity, comprising three core components: cell surface cytokine receptors, Janus kinases (JAKs), and signal transducers and activators of transcription (STATs). In humans, four JAK family members (JAK1, JAK2, JAK3, TYK2) and seven STAT proteins (STAT1, STAT2, STAT3, STAT4, STAT5A, STAT5B, STAT6) have been identified, each with non-redundant functions and specific cytokine affiliations [32] [35].
The canonical activation mechanism begins with the binding of a cytokine to its cognate receptor, which induces receptor dimerization or oligomerization. This conformational change brings the associated JAK proteins into close proximity, leading to their trans-phosphorylation and activation. The activated JAKs then phosphorylate specific tyrosine residues on the receptor's cytoplasmic tail, creating docking sites for STAT proteins via their Src homology 2 (SH2) domains. Once recruited, STATs are themselves phosphorylated by JAKs on a conserved tyrosine residue. This phosphorylation triggers STAT dimerization, followed by nuclear translocation where the dimers bind to specific regulatory sequences in target gene promoters, thereby initiating transcription [35]. The pathway is tightly regulated by negative feedback mechanisms, including the suppressor of cytokine signaling (SOCS) proteins, protein inhibitors of activated STATs (PIAS), and protein tyrosine phosphatases [35].
Role in Cytokine Storm and Organ Damage
In the context of hyperinflammation, the JAK-STAT pathway transitions from a carefully regulated communication channel to a primary driver of pathological cytokine production. Many of the cytokines central to cytokine storm syndromes, such as interferons (IFNs), interleukins (IL-6, IL-12, IL-23), and granulocyte-macrophage colony-stimulating factor (GM-CSF), signal predominantly through JAK-STAT cascades [36] [35]. Dysregulation in this pathway can therefore lead to severe immunodeficiencies, autoimmune pathologies, and malignancies.
The role of JAK-STAT signaling extends beyond classical immune cells to include critical functions within the central nervous system (CNS). Despite modest expression levels in the CNS, the pathway is crucial for functions in the cortex, hippocampus, and cerebellum, making it relevant in conditions like Parkinson's disease and other neuroinflammatory disorders [32]. Furthermore, chronic psychological stress and depression are associated with increased pro-inflammatory states within specific brain regions, and JAK-STAT activation influences serotonin receptors and phospholipase C, with implications for stress and mood disorders [32]. In glial cells such as astrocytes and microglia, JAK-STAT activation assumes a pivotal role in regulating the delicate balance between pro-inflammatory and anti-inflammatory cytokines, thereby shaping the neuroinflammatory environment within nervous tissues [32].
Table 1: JAK-STAT Family Members and Their Roles in Hyperinflammation
| Component | Primary Association | Role in Hyperinflammation |
|---|---|---|
| JAK1 | IFN-γ, IL-6 family cytokines | Sustained activation linked to autoimmune pathology; key driver of inflammatory signaling. |
| JAK2 | EPO, TPO, GM-CSF | Gain-of-function mutations (e.g., V617F) cause myeloproliferative neoplasms; crucial in hematopoiesis. |
| JAK3 | γc chain cytokines (IL-2, IL-4, IL-7, etc.) | Mutations cause SCID; targeted for immunosuppression. |
| TYK2 | Type I IFNs, IL-12, IL-23 | Polymorphisms linked to autoimmune diseases (SLE, Crohn's). |
| STAT1 | IFN-α/β, IFN-γ | Promotes anti-viral and pro-inflammatory responses; excessive activation inhibits IL-17. |
| STAT3 | IL-6, IL-10, IL-23 | Central role in Th17 differentiation; key mediator in chronic inflammation and cancer. |
| STAT5 | Prolactin, GM-CSF, IL-2 | Constitutive activation promotes leukemias; regulates immune cell proliferation. |
Experimental Analysis of JAK-STAT Signaling
Investigating the JAK-STAT pathway in the context of hyperinflammation requires a combination of biochemical, cellular, and genomic approaches.
Protocol 1: Assessing STAT Phosphorylation and Nuclear Translocation
- Cell Stimulation: Stimulate immune cells (e.g., primary monocytes, T cells, or macrophage cell lines like THP-1) with a relevant cytokine (e.g., IFN-γ at 10 ng/mL or IL-6 at 50 ng/mL) for time points ranging from 5 minutes to 2 hours.
- Protein Extraction: Lyse cells to obtain total protein extracts. For fractionation, use a cytoplasmic extraction reagent followed by a nuclear extraction reagent to separate nuclear and cytoplasmic fractions.
- Western Blotting: Resolve proteins via SDS-PAGE, transfer to a membrane, and probe with antibodies against phosphorylated STATs (e.g., p-STAT1 Tyr701, p-STAT3 Tyr705) and total STAT proteins. Antibodies against nuclear markers (e.g., Lamin A/C) and cytoplasmic markers (e.g., GAPDH) validate the fractionation efficiency.
- Immunofluorescence: Seed cells on coverslips, stimulate, fix, and permeabilize. Stain with anti-STAT antibodies and a fluorescent secondary antibody, then visualize via confocal microscopy to directly observe nuclear translocation.
Protocol 2: Gene Expression Profiling of JAK-STAT Targets
- Treatment: Treat cells with a JAK inhibitor (e.g., Ruxolitinib, Tofacitinib) prior to cytokine stimulation.
- RNA Isolation and qRT-PCR: Extract total RNA and reverse transcribe to cDNA. Perform quantitative PCR using primers for known JAK-STAT target genes (e.g., SOCS3, IRF1, CXCL10).
- Data Analysis: Normalize expression to housekeeping genes (e.g., ACTB, GAPDH) and analyze using the ΔΔCt method to quantify fold changes in gene expression, thereby assessing the functional impact of pathway activation or inhibition.
Diagram 1: JAK-STAT Pathway Activation. This diagram illustrates the core signaling cascade where cytokine binding induces JAK-mediated STAT phosphorylation, dimerization, and nuclear translocation to drive target gene expression.
Toll-like Receptors (TLRs) as Gatekeepers of Hyperinflammation
TLR Signaling Cascades
Toll-like receptors are a family of pattern recognition receptors (PRRs) that constitute the first line of defense in the innate immune system. They are specialized in recognizing conserved pathogen-associated molecular patterns (PAMPs) from bacteria, viruses, and other microorganisms, as well as endogenous damage-associated molecular patterns (DAMPs) released from stressed or dying cells [37] [34]. In humans, ten functional TLRs (TLR1-TLR10) are identified, which are strategically localized on either the plasma membrane (TLR1, TLR2, TLR4, TLR5, TLR6) to sense extracellular threats or within endosomal membranes (TLR3, TLR7, TLR8, TLR9) to detect nucleic acids from internalized pathogens [34].
TLR activation triggers one of two major signaling cascades: the MyD88-dependent pathway, utilized by all TLRs except TLR3, and the TRIF-dependent pathway (also known as the MyD88-independent pathway), which is primarily engaged by TLR3 and TLR4 [34]. The MyD88-dependent pathway is a rapid-response system. Upon ligand binding, TLRs recruit the adaptor protein MyD88, which then recruits interleukin-1 receptor-associated kinases (IRAKs). This complex, known as the "myddosome," ultimately leads to the activation of the IκB kinase (IKK) complex and mitogen-activated protein kinases (MAPKs). IKK phosphorylates IκB, targeting it for degradation and thereby releasing NF-κB, which translocates to the nucleus to induce the expression of pro-inflammatory cytokines like TNF-α, IL-1β, and IL-6 [34]. The TRIF-dependent pathway, initiated by TLR3 and TLR4, leads to the delayed activation of NF-κB and also activates interferon regulatory factors (IRF3 and IRF7), which are critical for inducing type I interferons (IFN-α/β) [37] [34].
TLRs in Sepsis and Cytokine Storm
In hyperinflammatory syndromes like sepsis and cytokine storm, the precise regulation of TLR signaling is lost. While essential for initial pathogen clearance, excessive or prolonged TLR activation becomes a primary engine of the "cytokine storm" [34]. This hyper-inflammatory state is characterized by an overwhelming release of inflammatory mediators that exacerbate tissue damage and can lead to complications such as acute respiratory distress syndrome (ARDS), acute kidney injury (AKI), and multiple organ dysfunction syndrome (MODS) [34]. For instance, in severe COVID-19, the spike protein of SARS-CoV-2 has been shown to activate TLR4 and TLR2, correlating with excessive NF-κB activation and cytokine release [37]. Furthermore, genetic polymorphisms in TLRs, such as those in TLR3 and TLR7, can influence disease severity by modulating the host's antiviral and inflammatory response [37].
Table 2: Key Toll-like Receptors in Hyperinflammation
| TLR | Localization | Ligands (PAMPs/DAMPs) | Role in Hyperinflammation |
|---|---|---|---|
| TLR2 (with TLR1/6) | Cell Surface | Bacterial lipopeptides, Viral proteins (e.g., SARS-CoV-2) | Contributes to neutrophil extracellular trap (NET) formation; exacerbates inflammatory responses. |
| TLR3 | Endosomal | Viral dsRNA | Rare variants associated with severe COVID-19; generally provides host defense. |
| TLR4 | Cell Surface | LPS (Gram-negative bacteria), SARS-CoV-2 Spike protein | Hyperactivation drives cytokine storm, ARDS, and coagulopathy; key therapeutic target. |
| TLR7/8 | Endosomal | Viral ssRNA | X-chromosome location may contribute to sex-based outcome differences in viral infections. |
| TLR9 | Endosomal | Unmethylated CpG DNA | Activation can contribute to systemic inflammation and autoimmunity. |
Experimental Protocols for TLR Research
Dissecting TLR-specific responses is crucial for understanding their contribution to hyperinflammation.
Protocol 1: TLR-Specific Agonist/Antagonist Studies
- Cell Stimulation: Treat human peripheral blood mononuclear cells (PBMCs) or macrophages with specific TLR agonists: LPS (TLR4, 100 ng/mL), Pam3CSK4 (TLR2/1, 1 µg/mL), R848 (TLR7/8, 1 µM), or Poly(I:C) (TLR3, 10 µg/mL). To inhibit signaling, pre-treat cells with specific antagonists like TAK-242 (for TLR4) or chloroquine (for endosomal TLRs).
- Cytokine Measurement: After 6-24 hours, collect cell culture supernatants. Analyze cytokine levels (e.g., TNF-α, IL-6, IL-1β, IFN-α) using multiplex bead-based immunoassays (e.g., Luminex) or ELISA.
- Pathway Analysis: Lyse cells and perform Western blotting to detect key signaling events, such as phosphorylation of IκBα, p65 (NF-κB), and MAPKs (p38, JNK, ERK).
Protocol 2: Gene Silencing in Primary Immune Cells
- siRNA Transfection: Isolate primary human monocytes or dendritic cells. Transfect with siRNA targeting specific TLRs (e.g., TLR4) or adaptor proteins (e.g., MYD88, TRIF) using non-liposomal transfection reagents optimized for primary cells.
- Efficiency Validation: 48-72 hours post-transfection, assess knockdown efficiency by measuring TLR mRNA levels via qRT-PCR or protein levels by flow cytometry.
- Functional Assay: Challenge the silenced cells with relevant TLR ligands and measure downstream outputs like cytokine production and NF-κB reporter activity to confirm the functional consequence of the knockdown.
Diagram 2: TLR Signaling Pathways. This diagram outlines the two principal signaling branches downstream of TLRs: the MyD88-dependent pathway leading to pro-inflammatory cytokine production, and the TRIF-dependent pathway leading to both NF-κB and type I interferon responses.
Inflammasome Activation: The Inflammatory Executioner
Molecular Basis of Inflammasome Assembly
Inflammasomes are cytosolic multiprotein complexes that act as central signaling hubs in the innate immune response, sensing intracellular PAMPs and DAMPs. They serve as platforms for the activation of caspase-1, which in turn catalyzes the proteolytic maturation and secretion of the highly inflammatory cytokines IL-1β and IL-18, and induces a lytic, pro-inflammatory form of programmed cell death termed pyroptosis [33]. The most extensively studied and clinically significant inflammasome is the NLRP3 inflammasome, which can be activated by a diverse set of stimuli, including microbial toxins, extracellular ATP, crystalline substances, and mitochondrial reactive oxygen species (ROS) [33].
Inflammasome assembly typically involves a sensor protein (e.g., NLRP3, AIM2), the adaptor protein ASC (apoptosis-associated speck-like protein containing a CARD), and the effector enzyme pro-caspase-1. Activation often requires a two-step process: a priming signal (e.g., from TLR activation) that upregulates the expression of NLRP3 and pro-IL-1β, and an activation signal that triggers the oligomerization of the sensor protein. The oligomerized sensor recruits ASC, which through its CARD domain, nucleates the formation of large filamentous structures ("specks") and recruits pro-caspase-1. The clustered pro-caspase-1 undergoes autocleavage into its active form, which then cleaves pro-IL-1β, pro-IL-18, and the pore-forming protein gasdermin D (GSDMD). The N-terminal fragments of cleaved GSDMD oligomerize to form pores in the plasma membrane, leading to pyroptosis and the release of mature cytokines [33].
Role in Sepsis and Organ Failure
In sepsis, excessive inflammasome activation is a key driver of the pathogenic cascade. It contributes to oxidative stress, endothelial dysfunction, immunothrombosis, and immune exhaustion [33]. The release of IL-1β and IL-18 potently amplifies systemic inflammation, while pyroptosis of immune and endothelial cells compromises vascular integrity and releases more DAMPs, creating a self-perpetuating cycle of injury. This maladaptive response is directly linked to the development of multiorgan failure [33]. Furthermore, persistent NLRP3 activation can promote an immunosuppressive state later in sepsis by driving immune cell exhaustion and metabolic reprogramming, increasing susceptibility to secondary infections [33]. Beyond classical infections, endogenous molecules can also trigger inflammasomes; for example, apolipoprotein C3 (ApoC3) has been shown to activate an alternative NLRP3 inflammasome pathway in human monocytes via caspase-8 and dimerization of TLR2 and TLR4, leading to organ damage [38].
Experimental Analysis of Inflammasome Activation
Studying inflammasomes requires careful assessment of both its components and functional outputs.
Protocol 1: Assessing Caspase-1 Activation and IL-1β Secretion
- Cell Priming and Activation: Differentiate THP-1 monocytes into macrophages using PMA (e.g., 100 nM for 48 hours). Prime the cells with a low dose of LPS (e.g., 10-100 ng/mL for 3-4 hours) to induce pro-IL-1β expression. Then, activate the inflammasome with a specific stimulus such as ATP (5 mM for 30 minutes), nigericin (10 µM for 1 hour), or monosodium urate (MSU) crystals (100 µg/mL for 6 hours).
- Caspase-1 Activity: Use a fluorescent caspase-1 activity assay kit (based on the substrate YVAD-AFC) in cell lysates according to the manufacturer's instructions.
- IL-1β Measurement: Collect cell culture supernatants. To detect the mature p17 form of IL-1β, concentrate the supernatants via trichloroacetic acid (TCA) precipitation before performing Western blotting. Alternatively, use ELISA to quantify total secreted IL-1β.
Protocol 2: Detection of ASC Speck Formation and Pyroptosis
- Immunofluorescence for ASC Specks: Seed and stimulate macrophages on glass coverslips. Fix, permeabilize, and stain with an anti-ASC antibody. Visualize under a confocal microscope. Active inflammasomes appear as large, bright, singular perinuclear specks.
- Pyroptosis Assay: Measure pyroptosis by detecting plasma membrane permeability. Perform a lactate dehydrogenase (LDH) release assay on cell culture supernatants using a commercial kit. Simultaneously, use a viability dye (e.g., propidium iodide) and analyze by flow cytometry to quantify the percentage of dying cells.
Table 3: Key Inflammasome Pathways in Hyperinflammation
| Inflammasome Sensor | Activators | Key Outputs | Pathological Role |
|---|---|---|---|
| NLRP3 | ATP, crystals (e.g., MSU), pore-forming toxins, ROS | Caspase-1 activation, IL-1β/IL-18 maturation, Pyroptosis (via GSDMD) | Driver of sepsis, gout, atherosclerosis, and Alzheimer's disease. |
| AIM2 | Cytosolic double-stranded DNA | Caspase-1 activation, Pyroptosis | Protects against intracellular bacteria and viruses; can contribute to autoinflammation. |
| Non-canonical (Caspase-4/5/11) | Intracellular LPS (Gram-negative bacteria) | Pyroptosis (via GSDMD), Pannexin-1 channel opening | Contributes to endotoxic shock; can trigger secondary NLRP3 activation. |
Crosstalk and Integration of Pathways in Organ Injury
The JAK-STAT, TLR, and inflammasome pathways do not operate in isolation; they engage in extensive crosstalk, creating a powerful and often pathological feed-forward loop that amplifies hyperinflammation and drives organ injury.
TLR and Inflammasome Crosstalk: This is one of the most critical interactions. TLR signaling provides the essential priming signal for the NLRP3 inflammasome by inducing the transcription of Nlrp3 and Il1b genes via NF-κB [33]. Furthermore, TLR2/TLR4 dimerization, as induced by endogenous proteins like ApoC3, can directly activate an alternative inflammasome pathway in human monocytes that depends on caspase-8 rather than caspase-1, yet still leads to IL-1β processing and organ damage [38].
JAK-STAT and TLR/Inflammasome Crosstalk: Cytokines that signal through JAK-STAT pathways can also prime or amplify inflammasome responses. For example, IL-6, a classic JAK-STAT cytokine, can enhance inflammatory responses. Conversely, inflammasome-derived cytokines like IL-1β signal through receptors that themselves activate JAK-STAT pathways, further propagating the inflammatory response. This interconnected signaling creates a cytokine network where the output of one pathway serves as the input for another.
The collective activation of these pathways leads to a convergence on damaging effector mechanisms:
- Endothelial Dysfunction: Inflammatory cytokines (e.g., TNF-α, IL-1β) and pyroptotic cell death disrupt endothelial barrier function, increasing vascular permeability and promoting edema.
- Immunothrombosis: Tissue factor expression and phosphatidylserine exposure on apoptotic cells and microvesicles create a procoagulant state, leading to disseminated intravascular coagulation (DIC) and microvascular thrombosis, which compromises organ perfusion [39].
- Necroptosis/Ferroptosis: Inflammasome signaling intersects with other regulated cell death pathways, such as necroptosis and ferroptosis, which further amplify systemic inflammation and tissue injury [33].
The integration of these signals is influenced by host factors, including sex-based differences (e.g., estrogen's modulation of NLRP3 via GPER-1 [33]) and pre-existing conditions like metabolic syndrome, which can create a pre-activated inflammatory state and predispose individuals to more severe outcomes [33].
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Reagents for Investigating Hyperinflammatory Pathways
| Reagent Category | Example Products | Primary Function/Application |
|---|---|---|
| JAK-STAT Inhibitors | Ruxolitinib (JAK1/2), Tofacitinib (JAK1/3), Filgotinib (JAK1), Upadacitinib (JAK1) | Selective pharmacological inhibition to dissect JAK-STAT contribution to cytokine release and cell survival. |
| TLR Agonists/Antagonists | LPS (TLR4), Pam3CSK4 (TLR2/1), Poly(I:C) (TLR3), TAK-242 (TLR4 antagonist), ODN 2088 (TLR9 antagonist) | To specifically activate or block TLR pathways in cellular models of infection and inflammation. |
| Inflammasome Activators/Inhibitors | ATP, Nigericin, MSU Crystals; MCC950 (NLRP3 inhibitor), VX-765 (Caspase-1 inhibitor) | To induce and probe canonical inflammasome activation and assess the efficacy of targeted inhibitors. |
| Cytokine Detection Kits | ELISA or Luminex kits for TNF-α, IL-6, IL-1β, IL-18, IFN-γ | Quantification of key inflammatory mediators in cell culture supernatants, serum, or plasma. |
| Phospho-Specific Antibodies | Anti-p-STAT1/3/5, Anti-p-IκBα, Anti-p-p65, Anti-p-p38/JNK/ERK | Detection of activated signaling intermediates in Western blotting and flow cytometry. |
| Apoptosis/Pyroptosis Assays | Annexin V/PI staining kits, LDH Release Assay Kits, Caspase-1 Activity Assays, Anti-GSDMD antibodies | To distinguish between different modes of cell death (apoptosis vs. pyroptosis) in vitro. |
The JAK-STAT, TLR, and inflammasome pathways represent a tripartite signaling nexus that governs the initiation, amplification, and execution of hyperinflammatory responses. In the context of a cytokine storm, the carefully orchestrated crosstalk between these pathways collapses into a self-reinforcing cycle of cytokine production, immune cell activation, and programmed cell death, culminating in widespread organ damage and failure. The detailed mechanistic understanding of these pathways, as outlined in this whitepaper, provides a robust foundation for ongoing research. The experimental protocols and reagent toolkit offer practical starting points for scientists delving into this complex field. Future therapeutic success will likely hinge on strategies that can selectively disrupt this pathological crosstalk—for instance, through combination therapies using Jakinibs with NLRP3 inhibitors or monoclonal antibodies—while preserving essential host defense mechanisms. As our knowledge deepens, the pursuit of biomarker-guided, personalized immunomodulation represents the most promising path forward for mitigating the devastating consequences of hyperinflammation.
Diagnostic Biomarkers and Emerging Therapeutic Strategies for Clinical Translation
Within the context of cytokine storm and multiple organ failure research, the identification of robust biomarkers for early detection and prognosis is a cornerstone of advancing therapeutic strategies. Dysregulated immune activation, characterized by a massive release of pro-inflammatory cytokines, drives the progression from initial infection or tissue damage to life-threatening organ dysfunction [10]. This mechanistic backdrop underscores the critical need for biomarkers that can not only identify at-risk patients early but also stratify their prognosis and guide targeted interventions. Among the most promising tools are Serum Amyloid A (SAA), Monocyte Distribution Width (MDW), Neutrophil-to-Lymphocyte Ratio (NLR), and detailed cytokine profiling. These biomarkers offer a window into the dynamics of the host immune response, reflecting the intensity of inflammation, the balance between innate and adaptive immunity, and the activity of key inflammatory pathways. This guide provides an in-depth technical examination of these four biomarkers, detailing their prognostic value, standardized measurement protocols, and their integration into a comprehensive framework for basic and clinical research.
Biomarker Performance and Prognostic Value
The prognostic value of SAA, MDW, NLR, and specific cytokines has been validated across numerous clinical settings, including sepsis, cancer, and COVID-19. The tables below summarize key performance metrics and clinical associations.
Table 1: Prognostic Performance of SAA, MDW, and NLR
| Biomarker | Clinical Context | Cut-off Value | Association with Outcome | Statistical Performance |
|---|---|---|---|---|
| SAA | Multiple Cancers [40] | (Variable by cancer type) | Shorter Overall Survival | Pooled 5-year OR: 5.69 (95% CI: 2.66–12.18) |
| SAA | COVID-19 [41] | > 105.95 mg/L | Severe Disease | Sensitivity: 87.5%, Specificity: 100% |
| MDW | Sepsis (ED Triage) [42] | > 21 | Infection | Sensitivity: 73%, Specificity: 82% (AUC: 0.84) |
| MDW | Sepsis (ED Triage) [42] | > 22 | Sepsis/Septic Shock | Sensitivity: 79%, Specificity: 83% |
| MDW | Sepsis Mortality [43] | > 28.4 | Fatal Outcome | Sensitivity: 64.7%, Specificity: 88.2% |
| NLR | Various Cancers [44] | (High vs. Low, study-dependent) | Worse OS & PFS | OS HR: 1.51 (95% CI: 1.39–1.64), PFS HR: 1.26 (95% CI: 1.17–1.36) |
| NLR | Sepsis In-hospital Mortality [45] | > 10.77 (Day 1) | In-hospital Mortality | AUC: 0.880 |
Table 2: Cytokine Profiles as Predictive Biomarkers in Advanced Gastric Cancer (AGC) Immunochemotherapy [46]
| Cytokine | Biological Function | Association with Treatment Outcome |
|---|---|---|
| IL-4 | Anti-inflammatory; Promotes Th2 cell differentiation | High levels correlated with enhanced Progression-Free Survival (PFS) |
| IL-6 | Pro-inflammatory; Acute-phase response, pyrexia | Elevated expression significantly associated with poorer Overall Survival (OS) |
| IL-2 | T-cell proliferation and differentiation | No significant association with PFS observed |
| IL-10 | Anti-inflammatory; inhibits pro-inflammatory cytokine production | No significant association with PFS observed |
| IFN-γ | Pro-inflammatory; Macrophage activation, antiviral defense | No significant association with PFS observed |
Experimental Protocols for Biomarker Analysis
Protocol 1: Measuring SAA and Cytokine Profiles
Objective: To quantify concentrations of Serum Amyloid A (SAA) and specific cytokines (e.g., IL-2, IL-4, IL-6, IL-10, IFN-γ) in human serum or plasma samples.
Materials:
- Research Reagent Solutions:
- Serum Collection Tubes: Gel clot activator tubes for serum separation.
- Immunoassay Kits: Commercial ELISA or electrochemiluminescence (ECLIA) kits for each target analyte (e.g., SAA, IL-6, IL-4).
- Microplate Reader: For colorimetric or chemiluminescent detection.
Methodology:
- Sample Collection and Processing: Draw venous blood into serum separator tubes. Allow blood to clot for 30 minutes at room temperature, then centrifuge at 1000–2000 × g for 10 minutes. Aliquot the supernatant (serum) and store at -80°C until analysis.
- Immunoassay Procedure:
- Follow the manufacturer's instructions for the specific commercial kit.
- Briefly, add standards, controls, and samples to assay plate wells pre-coated with a capture antibody.
- Incubate to allow the target protein to bind, then wash to remove unbound substances.
- Add a biotinylated detection antibody, incubate, and wash.
- Add streptavidin-conjugated enzyme (e.g., Horseradish Peroxidase), incubate, and wash.
- Add a substrate solution that reacts with the enzyme to produce a colorimetric or chemiluminescent signal.
- Stop the reaction (if required) and read the signal intensity.
- Data Analysis: Generate a standard curve from the known concentrations of standards. Interpolate the sample concentrations from the standard curve using a 4- or 5-parameter logistic fit.
Protocol 2: Determining MDW from a Complete Blood Count (CBC)
Objective: To obtain the Monocyte Distribution Width (MDW) as part of a routine complete blood count with differential.
Materials:
- Research Reagent Solutions:
- Blood Collection Tubes: K2 or K3 EDTA vacuum tubes for anticoagulated whole blood.
- Hematology Analyzer: A modern analyzer with volume, conductivity, and scatter (VCS) technology, such as the Beckman Coulter UniCel DxH 900 series.
Methodology:
- Sample Collection: Draw venous blood into a K2/K3 EDTA tube. Invert the tube 8-10 times immediately after collection to ensure proper mixing and anticoagulation.
- Analysis: The same EDTA sample used for the CBC is analyzed. The automated hematology analyzer uses VCS technology:
- Volume (V): Measures cell size using direct current impedance.
- Conductivity (C): Uses high-frequency electromagnetic energy to probe cellular internal composition.
- Scatter (S): Employs laser light scattering to characterize cytoplasmic granularity and nuclear structure.
- MDW Calculation: The instrument analyzes thousands of individual monocyte events. The MDW is computed as the standard deviation (SD) of the monocyte volume distribution, providing a quantitative measure of monocyte morphological heterogeneity. The result is typically reported in fL (femtoliters) as part of the CBC differential report.
Protocol 3: Calculating the Neutrophil-to-Lymphocyte Ratio (NLR)
Objective: To derive the NLR from a standard complete blood count with differential.
Materials:
- Research Reagent Solutions:
- Blood Collection Tubes: K2 or K3 EDTA vacuum tubes.
- Hematology Analyzer: Any standard analyzer capable of providing a validated five-part white blood cell differential.
Methodology:
- Sample Collection and Analysis: Collect blood in an EDTA tube and run it on a hematology analyzer as described in Protocol 3.2.
- Data Extraction: From the CBC report, record the absolute neutrophil count (ANC, cells/µL) and the absolute lymphocyte count (ALC, cells/µL).
- Calculation: Compute the NLR using the following formula: NLR = Absolute Neutrophil Count / Absolute Lymphocyte Count
- Dynamic Monitoring: For prognostic applications, especially in oncology immunotherapy, baseline NLR (NLR1) is calculated before treatment initiation. Subsequent values (NLR2, NLR3) are calculated before the second and third treatment cycles to monitor dynamic changes, which can be more predictive than a single baseline measurement [47].
Signaling Pathways and Biomarker Roles
The following diagrams illustrate the central role of cytokine storm in multiple organ failure and the specific positions of the discussed biomarkers within this pathological network.
Figure 1: This pathway illustrates the central role of a cytokine storm, driven by innate immune hyperactivation, in progressing to multiple organ failure. The biomarkers SAA, MDW, NLR, and Cytokine Profiling (shown in green) serve as measurable indicators at key points in this pathological cascade, reflecting the intensity of the inflammatory response and cellular activation.
Figure 2: The Neutrophil-to-Lymphocyte Ratio (NLR) is a simple but powerful measure of systemic inflammatory status and immune balance. A high NLR reflects an excess of pro-inflammatory, immunosuppressive neutrophils relative to the lymphocytes responsible for adaptive anti-tumor or anti-pathogen immunity, correlating with poor prognosis in cancer and sepsis.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Biomarker Analysis
| Item | Function/Application | Example/Notes |
|---|---|---|
| K2/K3 EDTA Tubes | Anticoagulated whole blood collection for CBC, MDW, and NLR. | Essential for preventing clot formation; ensures accurate cell counts and MDW measurement [43] [42]. |
| Serum Separator Tubes | Serum collection for SAA and cytokine (e.g., IL-6) analysis. | Gel barrier facilitates clean serum separation after centrifugation [46]. |
| Hematology Analyzer with VCS | Automated analysis of CBC with differential and MDW. | Beckman Coulter UniCel DxH 900 series; uses Volume, Conductivity, and Scatter technology to determine MDW [43] [42]. |
| ELISA Kits | Quantifying specific protein biomarkers (SAA, cytokines) in serum/plasma. | Commercial kits provide antibodies, standards, and reagents for precise colorimetric or chemiluminescent quantification [46] [41]. |
| Flow Cytometer | Deep immunophenotyping; validating monocyte activation and lymphocyte subsets. | Can be used to corroborate MDW and NLR data by analyzing surface markers (e.g., CD14, CD16). |
| Cytometric Bead Array (CBA) | Multiplexed quantification of multiple cytokine profiles from a single sample. | Efficient for simultaneously measuring panels of cytokines (e.g., IL-2, IL-4, IL-6, IL-10, IFN-γ) [46]. |
SAA, MDW, NLR, and cytokine profiling represent a powerful ensemble of biomarkers that provide critical, real-time insights into the dynamics of the host immune response within the framework of cytokine storm and multiple organ failure research. Their value is amplified when they are used in combination, offering a more holistic view of the inflammatory landscape than any single marker can provide. The integration of these readily available, cost-effective tools into standardized research protocols, as outlined in this guide, will accelerate the validation of their roles, the establishment of universal cut-off values, and ultimately, their translation into clinical practice for patient stratification and the development of novel immunomodulatory therapies. Future research should focus on longitudinal studies that track these biomarkers in tandem to build predictive algorithms capable of guiding personalized medicine in critical care and oncology.
Cytokine Storm (CS) is a life-threatening systemic inflammatory syndrome characterized by hyperactivation of immune cells and elevated levels of circulating pro-inflammatory cytokines. This pathological process is implicated in the development of critical conditions including fulminant myocarditis, acute respiratory distress syndrome (ARDS), and multiple organ failure (MOF) [1]. The dysregulated release of cytokines such as interleukin-6 (IL-6), tumor necrosis factor-alpha (TNF-α), and interferon-gamma (IFN-γ) creates a positive feedback loop of inflammation that drives progressive organ damage [1] [48].
Direct cytokine antagonism using monoclonal antibodies (mAbs represents a cornerstone therapeutic strategy for disrupting this deleterious cascade. By specifically targeting and neutralizing key mediator cytokines, these biologics aim to restore immune homeostasis and prevent the transition from systemic inflammation to irreversible organ dysfunction. The targeted inhibition of IL-6, TNF-α, and IFN-γ has emerged as a particularly promising approach based on their central roles in CS pathogenesis and promising clinical outcomes across various hyperinflammatory conditions [49] [1].
Pathophysiological Roles of Target Cytokines
Interleukin-6 (IL-6)
IL-6 exhibits pleiotropic activity in CS through multiple signaling mechanisms. The cytokine can engage in classical cis-signaling via membrane-bound IL-6 receptors (mIL-6R), trans-signaling through soluble IL-6 receptors (sIL-6R), and trans-presentation, ultimately activating gp130 and initiating JAK/STAT3 signaling cascades [1]. This activation results in systemic hyperinflammation characterized by increased production of secondary mediators including IL-1β, IL-8, CCL2, CCL3, CCL5, granulocyte-macrophage colony-stimulating factor (GM-CSF), and VEGF [1]. In CS models, IL-6 expression demonstrates temporal and spatial progression, initially peaking in organs such as the liver before disseminating to pulmonary and intestinal tissues, indicating its role as both a mediator and amplifier of systemic inflammation [50]. The JAK/STAT pathway, particularly STAT3 activation downstream of IL-6 signaling, is crucial for the differentiation of Th17 cells, which significantly impact the development and advancement of inflammatory pathologies including myocarditis [1].
Tumor Necrosis Factor-Alpha (TNF-α)
TNF-α serves as a primary initiator cytokine in CS, capable of activating multiple inflammatory pathways including the JAK/STAT cascade [49] [1]. Produced by activated CD4+ T cells, macrophages, and other immune populations, TNF-α synergizes with other pro-inflammatory mediators such as IL-17 to amplify the inflammatory response [49]. In rheumatoid arthritis (RA) models, TNF-α contributes to synovitis, promotes pannus formation, and drives progressive joint destruction [49]. Beyond localized inflammation, TNF-α promotes endothelial dysfunction, increases vascular permeability, and facilitates the recruitment of additional immune cells to sites of inflammation, thereby accelerating the progression toward multi-organ failure [49] [48]. The cytokine also promotes osteoclastogenesis via RANKL upregulation, connecting inflammatory processes with tissue destruction [49].
Interferon-Gamma (IFN-γ)
IFN-γ, primarily produced by Th1 cells and natural killer (NK) cells, plays a pivotal role in coordinating immune responses during CS. This cytokine activates the JAK/STAT pathway, particularly through JAK1 and JAK2, leading to phosphorylation and activation of STAT proteins that promote expression of inflammation-related genes [1]. In conditions such as hemophagocytic lymphohistiocytosis (HLH), elevated IFN-γ levels contribute significantly to the hyperinflammatory state [1]. IFN-γ can upregulate TLR expression, enhance antigen presentation, and activate macrophages, further amplifying the production of additional pro-inflammatory cytokines including TNF-α, IL-1β, and IL-6 [49]. The resulting feed-forward inflammation network sustains the CS state and promotes tissue injury across multiple organ systems.
Table 1: Key Characteristics of Target Cytokines in Cytokine Storm
| Cytokine | Primary Cellular Sources | Major Signaling Pathways | Key Pathological Roles in CS |
|---|---|---|---|
| IL-6 | Macrophages, T cells, Fibroblasts | JAK/STAT3, gp130 | Fever, acute phase response, Th17 differentiation, organ damage initiation |
| TNF-α | Macrophages, T cells, NK cells | JAK/STAT, NF-κB, MAPK | Endothelial activation, vascular permeability, synergistic inflammation with IL-17 |
| IFN-γ | Th1 cells, NK cells, Cytotoxic T cells | JAK/STAT1/2, IRF | Macrophage activation, antigen presentation upregulation, HLA expression |
Monoclonal Antibody Therapeutics: Mechanisms and Applications
IL-6 Pathway Inhibitors
Therapeutic targeting of the IL-6 pathway employs two primary strategies: direct cytokine neutralization and receptor blockade. Secukinumab and ixekizumab represent monoclonal antibodies that directly bind and neutralize IL-17, a key cytokine whose production is influenced by IL-6-mediated Th17 differentiation [49]. Tolizumab (an IL-6 inhibitor) targets the IL-6 receptor, preventing both classical and trans-signaling [50]. Early phase I/II trials of secukinumab (AIN457) demonstrated improved ACR20/50 responses in inflammatory conditions, though subsequent phase II/III trials showed more modest efficacy without superiority over alternative biologics such as abatacept (CTLA-4-Ig) [49]. IL-6 receptor blockade has shown particular promise in the management of CS, with therapeutic interventions potentially most effective when administered prior to 24 hours post-onset, based on temporal expression patterns observed in experimental models [50].
TNF-α Antagonists
TNF-α inhibitors constitute a well-established class of biologic DMARDs (disease-modifying antirheumatic drugs) with demonstrated efficacy in autoimmune conditions such as rheumatoid arthritis [49]. These therapeutics function by binding soluble and membrane-bound TNF-α, preventing receptor engagement and downstream inflammatory signaling. Clinical applications extend beyond rheumatologic conditions to include inflammatory bowel disease and other immune-mediated pathologies characterized by TNF-α dysregulation. The significant improvement in patient outcomes with TNF-α targeting biologics underscores the central role of this cytokine in perpetuating inflammatory cascades [49].
IFN-γ Neutralizing Antibodies
While less extensively documented in the available literature relative to IL-6 and TNF-α antagonists, IFN-γ neutralizing antibodies represent an emerging therapeutic approach for CS management. These agents function by directly binding IFN-γ and preventing its interaction with cognate receptors, thereby interrupting JAK/STAT1-mediated signaling and subsequent inflammatory gene expression [1]. The development of IFN-γ targeted therapies reflects the growing recognition of this cytokine's contribution to pathological immune activation, particularly in conditions such HLH and certain viral-associated hyperinflammatory states [1].
Table 2: Monoclonal Antibody Therapeutics for Cytokine Storm Management
| Therapeutic Category | Representative Agents | Molecular Target | Key Clinical Applications |
|---|---|---|---|
| IL-6/IL-17 Pathway Inhibitors | Secukinumab, Ixekizumab, Tolizumab | IL-17, IL-6R | Rheumatoid arthritis, Cytokine Storm syndrome |
| TNF-α Antagonists | Infliximab, Adalimumab, Etanercept | TNF-α | Rheumatoid arthritis, Inflammatory bowel disease |
| IFN-γ Neutralizing Antibodies | Emerging therapeutics | IFN-γ | Hemophagocytic lymphohistiocytosis (HLH), viral-associated CS |
Experimental Models and Methodologies
Animal Models of Cytokine Storm
Advanced animal models are essential for investigating CS pathogenesis and evaluating therapeutic interventions. While murine systems have been widely utilized, significant limitations exist in their ability to mimic human CS, including poor correlation in gene expression, differences in signaling pathway regulation, and insufficient immune response complexity [50]. Porcine models offer a superior alternative, as the porcine immune system closely resembles that of humans in both structure and function, particularly regarding innate and adaptive immune effectors [50]. The D-galactosamine (D-GalN)-induced minipig model reliably replicates human-like CS progression, characterized by progressive, time-dependent multi-organ injury with initial hepatocellular necrosis followed by pulmonary and intestinal damage [50].
Establishing D-GalN-Induced Cytokine Storm Model
The following protocol outlines the methodology for establishing a porcine CS model:
Animal Preparation: Twenty-four male minipigs (15-25kg) are acclimatized in individual cages for 3 days pre-experiment with fasting 12 hours prior to jugular vein cannulation [50].
Jugular Vein Cannulation:
- Induce anesthesia via intramuscular injection of tiletamine hydrochloride/zolazepam hydrochloride (125mg/20kg)
- Position animal in left lateral position and prepare right neck surgical site
- Perform surgical exposure of common carotid artery and free approximately 3cm vascular segment
- Insert double-lumen anti-infective catheter through vascular incision
- Secure catheter, close surgical site, and apply protective bandaging [50]
CS Induction:
- Prepare D-GalN hydrochloride solution (0.5g/ml in 5% dextrose)
- Filter sterilize using 0.22μm membrane
- Administer intravenously via catheter at 1.5g/kg dosage [50]
Tissue Collection and Analysis:
- Euthanize animals at predetermined intervals (0h, 12h, 24h, 36h post-induction)
- Collect tissues from liver, lungs, intestines, heart, spleen, and kidneys
- Process for hematoxylin-eosin staining and IL-6 immunohistochemistry [50]
In Vivo Therapeutic Efficacy Testing
The MSU crystal-induced peritonitis model provides a robust system for evaluating anti-cytokine therapies:
Model Establishment:
- Administer monosodium urate (MSU) crystals to IL-1RAcP wild-type mice
- Monitor innate immune cell influx into peritoneal cavity, predominantly neutrophils [51]
Therapeutic Intervention:
- Pre-treat with either anti-IL-1RAcP antibody (mCAN10), isotype control antibody, or equimolar IL-1 receptor antagonist (IL-1Ra)
- Quantify peritoneal cavity-infiltrating leukocytes, particularly neutrophils
- Measure cytokine levels (IL-6, G-CSF, eotaxin, IL-5, MCP-1, MIP-1b) [51]
This experimental approach demonstrates the superior efficacy of broad co-receptor blockade compared to single cytokine inhibition, with anti-IL-1RAcP antibody treatment producing more potent reduction of multiple inflammatory mediators than IL-1Ra alone [51].
Signaling Pathways and Molecular Mechanisms
The intricate signaling networks underlying CS pathogenesis involve multiple interconnected pathways that represent potential therapeutic targets. The following diagrams illustrate key mechanistic pathways:
Diagram 1: IL-6 Signaling and Therapeutic Inhibition. IL-6 engages membrane-bound or soluble receptors complexed with gp130, activating JAK kinases that phosphorylate STAT3. STAT3 dimers translocate to the nucleus driving pro-inflammatory gene expression. mAbs target either IL-6 or its receptor to disrupt signaling [1].
Diagram 2: Cytokine Storm Pathogenesis and Therapeutic Intervention. Initiating triggers activate immune cells to release pro-inflammatory cytokines that engage signaling pathways, creating an amplification loop that culminates in endothelial dysfunction and multi-organ failure. mAbs target cytokines or their signaling pathways to interrupt this cascade [1] [48] [50].
Research Reagent Solutions
Table 3: Essential Research Reagents for Cytokine Storm Investigations
| Reagent Category | Specific Examples | Research Applications | Technical Considerations |
|---|---|---|---|
| Animal Models | D-GalN-induced minipig, MSU crystal murine peritonitis | CS pathogenesis, therapeutic efficacy testing | Porcine models better replicate human immune responses than murine [50] [51] |
| Cytokine Detection | IL-6, TNF-α, IFN-γ ELISA kits, Multiplex immunoassays | Cytokine quantification in serum/tissue, kinetics studies | Multi-analyte panels enable comprehensive cytokine profiling [50] |
| Histopathology Reagents | Hematoxylin-eosin stain, IL-6 immunohistochemistry antibodies | Tissue pathology assessment, spatial cytokine localization | Time-dependent tissue collection critical for pathology progression analysis [50] |
| Therapeutic mAbs | Secukinumab (anti-IL-17), Ixekizumab (anti-IL-17), Tolizumab (anti-IL-6R) | Mechanistic studies, dose-response evaluations, combination therapies | Target multiple IL-1 family cytokines simultaneously for enhanced efficacy [49] [51] |
| Signaling Pathway Tools | JAK inhibitors, Phospho-STAT antibodies, Pathway reporter cells | Signaling mechanism elucidation, pharmacodynamic assessments | JAK/STAT pathway central to multiple cytokine signaling cascades [1] |
Direct cytokine antagonism through monoclonal antibodies represents a sophisticated therapeutic approach for disrupting the deleterious cascade of cytokine storm and preventing progression to multiple organ failure. The targeted inhibition of IL-6, TNF-α, and IFN-γ addresses key nodal points in the inflammatory network, with demonstrated efficacy across various experimental models and emerging clinical applications. Future directions in this field include the development of bispecific or multi-specific antibodies capable of simultaneously neutralizing multiple cytokine pathways, enhanced engineering of Fc domains to optimize therapeutic efficacy, and personalized approaches to patient selection based on specific cytokine profiles. As understanding of CS pathogenesis continues to evolve, particularly regarding temporal dynamics of cytokine release and organ-specific vulnerability, increasingly refined therapeutic strategies will emerge to improve outcomes in this life-threatening condition.
The Janus kinase/Signal Transducer and Activator of Transcription (JAK/STAT) pathway represents a critical intracellular signaling cascade that regulates essential cellular processes including hematopoiesis, immune fitness, and inflammation. Dysregulation of this pathway contributes significantly to the pathogenesis of numerous diseases, particularly in contexts involving cytokine storm and multiple organ failure. This whitepaper provides a comprehensive technical analysis of JAK/STAT inhibitors, examining their molecular mechanisms, clinical applications across immune and inflammatory conditions, and emerging roles in managing hyperinflammatory syndromes. We present structured experimental protocols, quantitative clinical data comparisons, and pathway visualizations to support research and drug development efforts targeting this pivotal signaling axis.
The JAK/STAT pathway functions as a central communication node in cellular function, transmitting signals from more than 50 cytokines and growth factors [52]. Discovered more than a quarter-century ago, this pathway constitutes a rapid membrane-to-nucleus signaling module that induces expression of various critical mediators of inflammation and immune responses [52]. The pathway components include transmembrane receptors, receptor-associated Janus kinases (JAKs), and signal transducers and activators of transcription (STATs) that directly regulate gene transcription [53]. As a fulcrum of many vital cellular processes, dysregulation of JAK/STAT signaling is associated with various cancers, autoimmune diseases, and hyperinflammatory conditions [52]. This pathway has emerged as a promising therapeutic target, with multiple small-molecule inhibitors now approved and many more in clinical development [54].
In the context of cytokine storm and multiple organ failure research, the JAK/STAT pathway assumes particular importance due to its role in amplifying inflammatory responses. Cytokine storm is a life-threatening systemic inflammatory syndrome characterized by hyperactivation of immune cells and elevated levels of circulating cytokines, which can progress to multi-organ dysfunction [1]. The significant involvement of the JAK-STAT pathway in this pathological process has been well-established, making it a prime target for therapeutic intervention [1]. This whitepaper examines the scientific foundation, clinical applications, and experimental approaches for targeting this pathway, with particular emphasis on its implications for cytokine storm research.
JAK/STAT Pathway Fundamentals
Molecular Composition and Activation Mechanism
The JAK/STAT signaling pathway consists of three principal components: cytokine receptors, Janus kinases (JAKs), and signal transducers and activators of transcription (STATs). The four JAK family members—JAK1, JAK2, JAK3, and TYK2—are non-receptor tyrosine kinases characterized by seven JAK homology (JH) domains [52]. The JH1 domain functions as the kinase domain, while JH2 represents a pseudokinase domain that regulates kinase activity. The remaining domains (JH3-JH7) facilitate binding to cytokine receptors [52]. The seven STAT family members (STAT1, STAT2, STAT3, STAT4, STAT5a, STAT5b, and STAT6) contain SH2 domains that enable protein-protein interactions and DNA binding domains for transcriptional regulation [52].
Pathway activation initiates when extracellular cytokines bind to their cognate receptors, inducing receptor dimerization and apposition of associated JAKs [53]. This proximity enables trans-phosphorylation and activation of JAKs, which subsequently phosphorylate tyrosine residues on cytokine receptors [53]. STAT proteins are then recruited to these phosphotyrosine motifs via their SH2 domains and undergo JAK-mediated phosphorylation. Following phosphorylation, STATs form homodimers or heterodimers and translocate to the nucleus, where they bind specific DNA sequences to regulate transcription of target genes [53].
Figure 1: JAK/STAT Signaling Pathway and Inhibition Mechanism. The diagram illustrates the sequential activation process from cytokine binding to gene transcription, with JAK inhibitors targeting the kinase activation step.
Regulatory Mechanisms and Pathological Significance
The JAK/STAT pathway is regulated by multiple negative feedback mechanisms to prevent excessive signaling. Key regulators include suppressors of cytokine signaling (SOCS) proteins, which compete with STATs for receptor binding sites and promote ubiquitination and degradation of JAKs and cytokine receptors [55]. Protein inhibitors of activated STATs (PIAS) and protein tyrosine phosphatases provide additional regulatory control [53]. Dysregulation of these regulatory mechanisms can contribute to pathological JAK/STAT activation observed in autoimmune diseases, hematological disorders, and hyperinflammatory conditions [54].
Different JAK family members exhibit distinct expression patterns and biological functions. JAK1, JAK2, and TYK2 demonstrate broad tissue expression, whereas JAK3 expression is primarily restricted to hematopoietic cells, endothelial cells, and vascular smooth muscle cells [52]. This distribution pattern influences both physiological functions and pathological roles of each kinase. JAK3 knockout mice exhibit severe immunodeficiency due to defective lymphocyte development, highlighting this kinase's critical role in immune function [52]. In contrast, JAK2 knockout results in embryonic lethality due to defective erythropoiesis, emphasizing its essential role in hematopoiesis [52].
Clinical Applications and Therapeutic Evidence
Approved JAK Inhibitors and Their Applications
Multiple JAK inhibitors have received regulatory approval for clinical use, with each agent exhibiting distinct selectivity profiles and therapeutic indications. First-generation inhibitors typically target multiple JAK family members, while newer agents demonstrate enhanced selectivity for specific JAK isoforms [54]. These inhibitors function by competitively binding to the ATP-binding site of JAKs, preventing tyrosine phosphorylation and subsequent STAT activation [56].
Table 1: Clinically Approved JAK Inhibitors and Their Characteristics
| Inhibitor | Primary Targets | Key Clinical Indications | Notable Efficacy Findings |
|---|---|---|---|
| Tofacitinib | JAK1, JAK3 | Rheumatoid arthritis, ulcerative colitis | Significant improvement vs placebo in RA phase III trials [56] |
| Baricitinib | JAK1, JAK2 | Rheumatoid arthritis, COVID-19, atopic dermatitis | Superior to adalimumab in methotrexate-resistant RA [56] |
| Ruxolitinib | JAK1, JAK2 | Myelofibrosis, polycythemia vera, acute GVHD | First JAK inhibitor approved for neoplastic diseases [55] |
| Upadacitinib | JAK1 | Rheumatoid arthritis, atopic dermatitis, IBD | Superior to adalimumab in methotrexate-resistant RA [56] |
| Fedratinib | JAK2 | Myelofibrosis | Approved for myeloproliferative neoplasms [55] |
JAK Inhibition in Cytokine Storm and COVID-19
The COVID-19 pandemic highlighted the therapeutic potential of JAK inhibitors in managing cytokine storm syndromes. Severe COVID-19 is characterized by excessive production of proinflammatory cytokines including IL-6, IL-2, IL-7, IL-10, and TNF-α, which employ JAK-STAT signaling and contribute to adverse clinical outcomes [55]. Baricitinib emerged as a particularly promising agent, demonstrating dual mechanisms of action: inhibition of viral receptor-mediated endocytosis via the NAK family and suppression of cytokine signaling through JAK1/2 inhibition [56].
Clinical evidence supporting JAK inhibition in COVID-19-associated cytokine storm includes an expanded access program (NCT04355793) evaluating ruxolitinib in 312 hospitalized patients. In this study, 45.5% of patients achieved ≥1-point improvement in clinical status, with 42.6% experiencing physician-assessed clinical benefit [57]. The most common serious adverse events were acute respiratory failure (12.8%) and respiratory failure (9.6%), while only 2.6% experienced treatment-related serious adverse events [57]. These findings suggest potential benefit in selected patients, though randomized controlled trials are needed to identify optimal candidates.
Table 2: Clinical Outcomes of JAK Inhibitors in Inflammatory and Infectious Conditions
| Condition | Inhibitor | Study Design | Key Efficacy Outcomes | Safety Findings |
|---|---|---|---|---|
| COVID-19 Pneumonia | Baricitinib | Multiple clinical trials | Reduced mortality, ICU admission, and discharge rates [58] | Increased herpes virus infection risk; no other new safety concerns [58] |
| COVID-19 Cytokine Storm | Ruxolitinib | Expanded access program (N=312) | 45.5% with ≥1-point clinical improvement; 42.6% with physician-assessed benefit [57] | 2.6% with treatment-related SAEs; most common SAE: acute respiratory failure (12.8%) [57] |
| Rheumatoid Arthritis | Tofacitinib | Global phase III studies | Significant improvement vs placebo; comparable efficacy to biologics [56] | Black box warnings for cardiovascular events, thrombosis, malignancy, and death [59] |
| RA (Methotrexate-resistant) | Baricitinib/Upadacitinib | Phase III vs adalimumab | Superior efficacy compared to anti-TNF antibody [56] | Similar safety profile to other JAK inhibitors [56] |
Experimental Approaches and Research Methodologies
In Vitro Assessment of JAK/STAT Inhibition
Cell-Based Phosphorylation Assays: Researchers typically employ cytokine-stimulated cell lines (e.g., peripheral blood mononuclear cells, T lymphocyte lines, or monocyte lines) to assess JAK/STAT inhibition efficacy. The experimental protocol involves pre-treating cells with varying concentrations of JAK inhibitors (typically 0.1-1000 nM) for 1-2 hours followed by stimulation with relevant cytokines (e.g., IL-6 for JAK1/STAT3 signaling or IFN-γ for JAK1/JAK2/STAT1 signaling) for 15-30 minutes [52]. Cells are then lysed and analyzed via western blotting using phospho-specific antibodies against JAKs (p-JAK1, p-JAK2) and STATs (p-STAT1, p-STAT3, p-STAT5). Total JAK/STAT protein levels serve as loading controls [52].
STAT Nuclear Translocation Assays: Immunofluorescence microscopy enables visualization of STAT cellular localization. Cells are cultured on chamber slides, treated with inhibitors and cytokines as above, then fixed and stained with anti-STAT antibodies and nuclear markers. Inhibition of cytokine-induced STAT nuclear translocation demonstrates effective pathway blockade [52].
Gene Reporter Assays: Constructs containing STAT-binding elements linked to luciferase reporters allow quantitative assessment of transcriptional activity. Cells are transfected with reporter constructs, treated with JAK inhibitors, and stimulated with cytokines. Luciferase activity is measured after 6-24 hours, with reduced activity indicating successful pathway inhibition [52].
In Vivo Evaluation Models
Autoimmune Disease Models: Experimental autoimmune encephalomyelitis (EAE) in mice serves as a multiple sclerosis model, while collagen-induced arthritis models rheumatoid arthritis. Animals receive JAK inhibitors via oral gavage or dietary administration at various doses based on pharmacokinetic properties. Clinical scoring (e.g., paralysis severity in EAE, joint swelling in arthritis) is performed daily, with histological analysis of target tissues at endpoint [56].
Cytokine Storm Models: LPS-induced endotoxemia and SARS-CoV-2 infection models in transgenic mice expressing human ACE2 receptor evaluate JAK inhibitor efficacy in hyperinflammation. Treatment protocols typically initiate before or shortly after inflammatory challenge. Key endpoints include survival monitoring, serum cytokine profiling (IL-6, TNF-α, IFN-γ), and histological assessment of lung, liver, and spleen tissues [1] [53].
Pharmacodynamic Assessment: Blood collection at predetermined timepoints enables measurement of drug concentrations and p-STAT levels in peripheral blood cells via flow cytometry. This approach validates target engagement and informs dosing regimens for clinical translation [57].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for JAK/STAT Pathway Investigation
| Reagent Category | Specific Examples | Research Applications | Technical Considerations |
|---|---|---|---|
| JAK Inhibitors | Tofacitinib, Ruxolitinib, Baricitinib, Fedratinib | In vitro and in vivo pathway inhibition | Varying selectivity profiles; concentration-dependent effects [54] |
| Phospho-Specific Antibodies | p-JAK1 (Y1034/1035), p-JAK2 (Y1007/1008), p-STAT3 (Y705) | Western blot, flow cytometry, immunohistochemistry | Require careful validation of specificity; phosphorylation status time-dependent [52] |
| Cytokine Stimuli | IL-6, IFN-γ, IL-2, GM-CSF, Type I Interferons | Cell-based activation assays | Concentration and duration critical; cell type-specific responses [53] |
| Reporter Systems | STAT-responsive elements (e.g., GAS, ISRE) linked to luciferase | Transcriptional activity quantification | Enable high-throughput screening; transfection efficiency varies [52] |
| Animal Models | Collagen-induced arthritis, EAE, SARS-CoV-2 infection models | In vivo efficacy assessment | Model-specific pathophysiology; species differences in kinetics [56] |
Safety Considerations and Adverse Event Management
JAK inhibitor therapy presents distinct safety considerations that require careful monitoring. Pharmacovigilance data from large databases have identified several class-related adverse effects, leading to updated safety warnings from regulatory agencies [59]. A comprehensive analysis of 30,051,159 safety reports revealed neurological adverse events in 14.1% of tofacitinib reports, 14.5% of ruxolitinib reports, and 10.2% of baricitinib reports, with memory impairment representing the most frequently reported neurological concern [59].
The U.S. Food and Drug Administration has implemented black box warnings for JAK inhibitors used in inflammatory conditions, highlighting increased risks of serious heart-related events, cancer, blood clots, and death [59]. Post-marketing surveillance studies comparing JAK inhibitors to TNF inhibitors demonstrated elevated cardiovascular risks, resulting in revised treatment recommendations [59]. Infection risk, particularly herpes zoster reactivation, represents another significant concern, though COVID-19 clinical trials noted only slightly increased herpes virus infection risk without other new safety signals [58].
Risk mitigation strategies include thorough patient screening for cardiovascular risk factors, vigilance for neurological symptoms, and appropriate vaccination prior to treatment initiation when feasible. Laboratory monitoring should include complete blood counts, hepatic enzymes, and lipid panels at baseline and periodically during treatment [56]. These safety considerations emphasize the importance of appropriate patient selection and comprehensive monitoring in both clinical practice and research settings.
Future Directions and Research Opportunities
The evolving landscape of JAK/STAT pathway inhibition presents numerous research opportunities. Current investigations focus on developing increasingly selective inhibitors to optimize efficacy while minimizing off-target effects [54]. Further exploration of JAK inhibitor applications in cytokine storm syndromes beyond COVID-19, including CAR-T cell therapy-associated cytokine release syndrome, hemophagocytic lymphohistiocytosis, and fulminant myocarditis, represents a promising research direction [1].
The optimal timing and duration of JAK inhibitor therapy in hyperinflammatory conditions requires further clarification. Evidence suggests that earlier intervention in COVID-19 produces better outcomes, with patients receiving ruxolitinib for 8-14 days demonstrating superior clinical improvement (55.4%) compared to those treated for only 7 days (41.4%) [57]. Similar timing considerations likely apply to other cytokine storm indications.
Combination therapies represent another frontier, with JAK inhibitors potentially synergizing with other immunomodulatory approaches. The simultaneous targeting of multiple cytokine pathways may enhance efficacy in severe hyperinflammation while allowing lower doses of each agent to mitigate toxicity [1]. Research into biomarkers for treatment response will enable personalized approaches, identifying patients most likely to benefit from JAK inhibition while sparing those at high risk for adverse events.
Figure 2: Dual Mechanism of Baricitinib in COVID-19 Therapy. The diagram illustrates how baricitinib simultaneously inhibits viral endocytosis through NAK family inhibition and suppresses cytokine signaling via JAK1/JAK2 blockade, addressing both viral entry and inflammation components.
JAK/STAT pathway inhibitors represent a transformative class of targeted therapeutics with demonstrated efficacy across diverse inflammatory, autoimmune, and hyperinflammatory conditions. Their ability to simultaneously modulate multiple cytokine signals positions them uniquely for managing complex syndromes like cytokine storm, where numerous inflammatory mediators contribute to pathogenesis. The COVID-19 pandemic accelerated our understanding of their therapeutic potential in critical illness while highlighting the importance of appropriate patient selection and timing.
Ongoing research continues to refine the risk-benefit profile of these agents, with next-generation inhibitors offering improved selectivity and novel applications in cytokine-driven pathologies. As our understanding of JAK/STAT biology evolves, so too will our ability to precisely target this pathway in the context of multiple organ failure research. The integration of JAK inhibitors into multidisciplinary treatment approaches for hyperinflammatory syndromes represents a promising frontier in critical care therapeutics, potentially improving outcomes for patients with these life-threatening conditions.
Cytokine Storm (CS), also known as Cytokine Release Syndrome (CRS), is a life-threatening systemic inflammatory syndrome characterized by hyperactivation of immune cells and elevated levels of circulating cytokines [1]. This pathological process is implicated in the development of life-threatening conditions such as fulminant myocarditis, acute respiratory distress syndrome (ARDS), hemophagocytic lymphohistiocytosis, and multi-organ failure [1]. The term "cytokine storm" was first coined in 1993, though recognition of this hyperinflammatory state dates back to earlier literature describing an "influenza-like syndrome" following systemic viral infections [1]. In sepsis and septic shock, which represent critical global health challenges, the "cytokine storm" plays a central role in pathophysiology, leading to multi-organ failure through a complex cascade of inflammatory mediators [60].
The significant involvement of key signaling pathways including JAK-STAT, Toll-like receptors, neutrophil extracellular traps, and NLRP3 inflammasome has been recognized in the pathogenesis of CS [1]. The clinical presentation includes acute systemic inflammatory symptoms, organ dysfunction, and substantial mortality. Cytokines regulate inflammatory responses, immune cell activation, and tissue repair through a complex network, and dysregulation of this network can lead to CS with IFN-γ, IL-1, IL-6, TNF, and IL-18 recognized as major pathogenic mediators [50]. The dysregulated immune response in patients with sepsis ranges from an overzealous hyperinflammatory state with excessive cytokine production to a profound immunosuppressed phenotype known as sepsis-induced immunoparalysis [61].
Extracorporeal cytokine adsorption has emerged as a promising therapeutic strategy to modulate this severe immune dysregulation [60]. By removing pro-inflammatory mediators, endotoxins, and other circulating factors, this approach aims to reduce the inflammatory burden that drives the pathophysiology of cytokine storm conditions [60] [61]. The "peak cytokine hypothesis" suggests that extracorporeal blood purification attenuates the relative excess of pro- and anti-inflammatory mediators in the circulation, potentially mitigating organ damage and mortality [61]. This review provides a comprehensive technical analysis of extracorporeal cytokine removal devices and hemoadsorption technologies, with specific focus on their mechanisms, efficacy, and research applications in the context of cytokine storm and multiple organ failure mechanisms.
Pathophysiological Basis of Cytokine-Mediated Organ Failure
Key Signaling Pathways in Cytokine Storm
The JAK-STAT pathway represents a highly conserved signaling pathway that plays a significant role in cytokine storm pathogenesis [1]. This pathway consists of three main structural components: transmembrane receptors, receptor-associated JAKs (JAK1, JAK2, JAK3, and TYK2), and STATs (STAT1, STAT2, STAT3, STAT4, STAT5A, STAT5B, and STAT6) [1]. Numerous cytokines, including ILs, IFNs, and growth factors, participate in JAK-STAT signaling, contributing to essential physiological processes including immunomodulation. Specifically, IL-6 triggers the JAK-STAT3 pathway through classical cis-signaling, trans-signaling, and trans-presentation mechanisms [1]. IL-6 can interact with both membrane-bound IL-6 receptor (mIL-6R) on immune cells and the soluble form of IL-6 receptor (sIL-6R), forming a complex that triggers activation of gp130 and subsequently initiates the JAK-STAT3 signaling pathway [1]. This activation cascade results in a systemic hyperinflammatory response, leading to secretion of various mediators including IL-1β, IL-8, CCL2, CCL3, CCL5, GM-CSF, and VEGF [1].
Toll-like receptors (TLRs) represent a primitive category of pattern recognition receptors (PRRs) that recognize pathogen-associated molecular patterns (PAMPs) [1]. These receptors are present on various immune cells and tissue cells, including monocytes, macrophages, and dendritic cells, serving as detectors of pathogen incursion. TLR activation plays a critical role in the development of infectious diseases and CS progression [1]. Upon recognition of PAMPs, TLRs initiate the release of pro-inflammatory cytokines and orchestrate immune responses to protect cells from harm. However, the release of pro-inflammatory factors and cytokines by TLRs may also have deleterious effects, contributing to the uncontrolled inflammation characteristic of CS [1].
The NF-κB signaling pathway has been identified as central to cytokine storm induction in multiple models. Research on jellyfish envenomation syndrome demonstrated that NF-κB p65 subunit activation is fundamental to cytokine storm induction, with knockdown of p65 in macrophages reducing cytokine production and improving cell viability [9]. Transcriptomic analyses of hearts, livers, and kidneys in envenomation models revealed significant perturbation of the NF-κB signaling pathway among other inflammatory pathways [9].
Molecular Mechanisms of Multi-Organ Failure
Multi-organ failure in cytokine storm syndromes results from complex interactions between excessive inflammatory mediators and various organ systems. Histopathological studies in animal models reveal progressive, time-dependent multi-organ injury patterns [50]. The liver, lungs, and intestines often show the earliest and most severe damage, including hepatocellular necrosis, alveolar congestion, and intestinal epithelial destruction [50]. Research in porcine models demonstrates that IL-6 expression increases over time during cytokine storm, first peaking in the liver and later spreading to the lungs, intestines, and other organs [50]. At 36 hours in experimental models, IL-6 becomes diffusely expressed in hepatic and pulmonary tissues, indicating an escalating systemic inflammatory response [50].
The observed "liver initiation–lung and intestine diffusion" pattern provides insights into CSS pathogenesis, with the liver identified as a likely initiator of systemic inflammation [50]. This temporal expression of inflammatory mediators suggests a critical therapeutic window prior to 24 hours post-onset for anti-inflammatory interventions [50]. The molecular progression of organ failure involves endothelial activation, increased vascular permeability, recruitment of immune cells to infection sites, disseminated intravascular coagulation, microvascular thrombosis, and mitochondrial dysfunction [60]. While these responses are initially protective, their excessive amplification leads to widespread tissue injury and organ dysfunction [60].
Table 1: Key Cytokines in Cytokine Storm Syndromes and Their Pathophysiological Roles
| Cytokine | Major Cell Sources | Primary Signaling Pathway | Pathophysiological Role in CS |
|---|---|---|---|
| IL-6 | Macrophages, T cells | JAK-STAT3 | Fever, acute phase response, B-cell activation, hematopoiesis |
| TNF-α | Macrophages, monocytes | NF-κB, MAPK | Endothelial activation, vascular permeability, apoptosis |
| IL-1β | Macrophages, monocytes | NF-κB, inflammasome | Fever, lymphocyte activation, fibroblast proliferation |
| IFN-γ | T cells, NK cells | JAK-STAT1 | Macrophage activation, antigen presentation |
| IL-18 | Macrophages | NF-κB, inflammasome | IFN-γ induction, NK and T-cell activation |
| GM-CSF | T cells, macrophages | JAK-STAT5 | Myeloid cell differentiation, inflammatory mediator release |
Extracorporeal Cytokine Removal Devices: Technical Specifications and Mechanisms
Device Classification and Adsorption Principles
Extracorporeal cytokine adsorption devices can be broadly categorized into selective and non-selective adsorption technologies based on their mechanism of action [60] [61]. Selective adsorption devices are designed to target specific molecules or pathogens, such as endotoxins or bacteria, while non-selective devices remove a broad spectrum of inflammatory mediators through various adsorption principles [60]. These devices utilize different materials and mechanisms to target and remove inflammatory mediators and other harmful substances from the blood, operating primarily through hydrophobic interactions, electrostatic (ionic) bonds, and van der Waals forces [62].
The underlying adsorption process depends on the physicochemical properties of the sorbent material, particularly its porosity and surface characteristics [62]. Modern sorbents are derived from polymers that create a porous structure with a high surface-to-volume ratio, classified according to pore density (high or low) and pore size distribution (macropores >500 Å, mesopores 20-500 Å, and micropores <20 Å) [62]. The pore density affects the amount of solute removed by the sorbent, while the pore size distribution affects the spectrum of molecules in the adsorbate [62]. Adsorption capacity is measured by experimental isotherms, specific curves that describe the maximal amount of solute that can be adsorbed by a unit of sorbent [62].
Current sorbents demonstrate effective removal of molecules in the range between 10 and 55 KDa, including cytokines, chemokines, and protein-bound solutes, providing a new perspective on extracorporeal blood purification [62]. The efficiency of toxin removal with conventional systems may be inadequate to fully compensate for the dramatic surge in endogenous pro-inflammatory immune toxins characteristic of cytokine release syndromes, which represents the fundamental rationale for hemoadsorption application as an alternative or additional therapeutic option [62].
Comprehensive Device Specifications
CytoSorb: The CytoSorb adsorber (CytoSorbents Inc., USA) contains polystyrene divinylbenzene copolymer beads coated with polyvinylpyrrolidone to enhance hemocompatibility [60] [61]. This device represents a non-selective adsorption technology designed to remove a broad spectrum of inflammatory mediators, including both pro- and anti-inflammatory cytokines [60]. The cartridge has a surface area of approximately 45,000 m² and is capable of removing molecules in the 10-55 kDa range, with particular efficacy for IL-6, IL-1β, IL-8, IL-10, TNF-α, and MCP-1 [60]. Clinical applications primarily include septic shock, ARDS, and cytokine release syndrome following CAR-T cell therapy or other immunotherapies [60]. The device is typically used in sessions of 6-24 hours, with cartridge replacement recommended every 24 hours due to saturation [60].
Toraymyxin: The Toraymyxin cartridge (Toray Industries, Japan) is a selective adsorption device utilizing polymyxin B-immobilized fiber columns that specifically bind and neutralize endotoxins [60] [61]. This mechanism specifically targets the lipopolysaccharide (LPS) component of gram-negative bacterial endotoxins, with its intended use focused on patients with Gram-negative bacterial septic shock [61]. The device has demonstrated efficacy in lowering endotoxin levels in vitro and in animal models, with clinical studies showing improvement in hemodynamic parameters and vasopressor requirements [61]. The EUPHAS randomized controlled trial demonstrated significant improvements in mean arterial pressure and decreased vasopressor dependency, though larger trials like ABDOMIX and EUPHRATES showed conflicting results [61]. Recent evidence suggests therapeutic efficacy may depend on circulating endotoxin concentrations, with potential benefit limited to patients with intermediate endotoxin activity assay levels (0.60-0.89) [61].
Oxiris: The Oxiris hemofilter (Baxter International Inc., USA) is a multifunctional device that combines high-flux dialysis with adsorption capabilities [60]. It is composed of a polyacrylonitrile-based AN69 membrane surface-treated with polyethyleneimine (PEI), which enhances its ability to bind both endotoxins and cytokines [60]. Additionally, the membrane is heparin-coated to reduce thrombogenicity [60]. Oxiris is designed specifically for use in continuous renal replacement therapy (CRRT) circuits, allowing simultaneous cytokine/endotoxin removal and renal support [60]. This integrated approach makes it particularly suitable for septic patients with concomitant acute kidney injury, providing multiple therapeutic functions within a single extracorporeal circuit [60].
HA330/380 Hemoperfusion Cartridges: These cartridges utilize a neutral macroporous resin (with the HA380 having enhanced surface area and adsorption capacity) designed for non-selective cytokine removal [60]. The spherical sorbent particles provide a large surface area for mediator adsorption, effectively removing a broad range of middle-molecular-weight toxins including cytokines, chemokines, and other inflammatory mediators [60]. Clinical applications include sepsis, SIRS, and acute pancreatitis [60]. The cartridges are typically used in 2-4 hour sessions, with some evidence supporting improved hemodynamic stability and organ function scores following treatment [60].
Seraph 100 Microbind: This novel affinity binder cartridge utilizes ultra-high molecular weight polyethylene beads coated with immobilized heparin to mimic endothelial cell receptors [60]. The mechanism relies on heparin's natural affinity for a broad range of pathogens, including bacteria, viruses, and toxins [60]. By mimicking the human glycocalyx, Seraph 100 acts as a binding site for pathogens and subsequently removes them from the blood [60]. This device represents a unique approach to blood purification by targeting the infectious triggers of cytokine storms rather than the cytokines themselves, potentially addressing the underlying cause of sepsis-related inflammation [60].
PMMA-Based Columns: Polymethyl methacrylate (PMMA) membranes have been developed for cytokine adsorption, particularly in the context of extracorporeal membrane oxygenation (ECMO) and cardiopulmonary bypass (CPB) [63]. These membranes possess a porous structure with nano-sized pores that can adsorb various mediators based primarily on molecular size [63]. Recent research demonstrates that PMMA columns effectively suppress systemic inflammatory reactions during ECMO, with significant reductions in TNF-α and IL-6 levels compared to conventional ECMO, while maintaining IL-10 levels and reducing lung edema incidence [63]. The adsorption properties of PMMA are determined by the size of the porous membrane, as it adsorbs molecules based on their size, largely independent of the environment, ensuring reliable adsorption as long as the size matches the conditions [63].
Table 2: Technical Specifications of Extracorporeal Cytokine Removal Devices
| Device | Sorbent Material | Mechanism of Action | Molecular Targets | Blood Flow Rate | Treatment Duration |
|---|---|---|---|---|---|
| CytoSorb | Polystyrene divinylbenzene copolymer beads | Non-selective adsorption | Broad-spectrum cytokines (10-55 kDa) | 100-300 mL/min | 6-24 hours per session |
| Toraymyxin | Polymyxin B-immobilized fibers | Selective endotoxin adsorption | Endotoxins (LPS) | 80-120 mL/min | 2 hours per session (typically 2 sessions) |
| Oxiris | AN69 membrane with polyethyleneimine | Combined dialysis/adsorption | Endotoxins, cytokines, uremic toxins | 100-200 mL/min | Continuous (CRRT) |
| HA330/380 | Neutral macroporous resin | Non-selective adsorption | Middle molecular weight substances, cytokines | 200-250 mL/min | 2-4 hours per session |
| Seraph 100 | Heparin-coated polyethylene beads | Pathogen affinity binding | Bacteria, viruses, toxins | 150-250 mL/min | 4 hours per session |
| PMMA Column | Polymethyl methacrylate fibers | Size-based cytokine adsorption | TNF-α, IL-6, other cytokines | 4 mL/kg/min (rat model) | 30-60 minutes (experimental) |
Experimental Models and Research Methodologies
Animal Models of Cytokine Storm Syndrome
Porcine CSS Model: A D-galactosamine (D-GalN)-induced miniature pig model has been established to investigate multi-organ pathological changes and inflammatory dynamics in cytokine storm syndrome [50]. This model utilizes twenty-four male minipigs divided into control and D-GalN groups (n=12 each), with the experimental group receiving 1.5 g/kg D-GalN intravenously [50]. The D-GalN binds with uridine triphosphate (UTP) to form UDP-GalN and inhibits UDPG pyrophosphorylase through phosphorylation pathways, leading to significant depletion of UTP and UDPG [50]. This inhibition suppresses the synthesis of nucleic acids, proteins, and glycogen in hepatocytes, disrupts cellular membrane systems, induces intracellular Ca²+ influx, and ultimately causes hepatocellular necrosis [50]. Tissues from the liver, lungs, intestines, heart, spleen, and kidneys are collected at 0 h, 12 h, 24 h, and 36 h post-induction for hematoxylin-eosin (H&E) staining and IL-6 immunohistochemistry [50]. This model replicates human-like disease progression and identifies the liver as a likely initiator of systemic inflammation, with histopathology revealing progressive, time-dependent multi-organ injury where the liver, lungs, and intestines show the earliest and most severe damage [50].
Jellyfish Envenomation Mouse Model: A delayed jellyfish envenomation syndrome (DJES) mouse model has been established to study cytokine storm mechanisms [9]. The model involves injecting various concentrations of tentacle extract (TE) from Nemopilema nomurai jellyfish into the tail vein of mice and monitoring their condition and survival rates [9]. As venom concentration increases from 0 to 2.29 mg kg−1, the animals' average time to death decreases from 48 to 12 hours [9]. Proteomic analysis shows the TE contains predominantly metalloproteinases and other toxic components such as staphylococcal toxins, coagulation factors, peroxiredoxins, and phospholipases, which commonly contribute to sting poisoning [9]. Histopathological studies performed 6 h after envenomation reveal edema and degeneration of myocardial fibers in the heart, loss of lobular structure with extensive hemorrhage and severe hepatocellular necrosis in the liver, and destruction of glomerular capillaries with fibrin microthrombi deposits and severe degenerative changes in the proximal tubules of the kidneys [9]. Transcriptomic analysis of TE-treated macrophages identified 51 differentially expressed genes that overlap with those found in the heart, liver, and kidneys of TE-treated DJES mice, with the NF-κB signaling pathway significantly perturbed [9].
Rat ECMO Model with PMMA Adsorption: A rat model of extracorporeal membrane oxygenation has been developed to investigate inflammatory reduction using novel cytokine adsorption columns [63]. The circuit comprises a membrane oxygenator (surface area: 0.03 m², polypropylene) and a polyvinyl chloride circuit, with a total priming volume of 15 mL [63]. Sprague-Dawley rats (male, 14-16 weeks old, 400-450 g) are divided into three groups: SHAM, ECMO, and ECMO with PMMA (PMMA group) [63]. Experiments comprise 180 min of cannulation only in the SHAM group and 60 min of ECMO followed by 120 min of observation in the ECMO and PMMA groups [63]. PMMA adsorption is conducted from 30 min after ECMO initiation to completion in the PMMA group [63]. Blood parameters and cytokines are measured during experiments, and lung tissues are collected after the experiment for evaluation of tissue edema [63]. The PMMA column used in this experiment for rats comprises 4400 fibers filled with PMMA with a diameter of 116 μm (filling rate, 59% by volume), with a total contact surface area of the adsorbent of 285 cm² and a filling volume of 1.5 mL [63].
Analytical Methodologies for Cytokine Storm Assessment
Transcriptomic Analysis: Comprehensive transcriptomic analysis represents a crucial methodology for investigating cytokine storm mechanisms [9]. In DJES mouse models, transcriptomic analysis of hearts, liver, and kidneys identifies differentially expressed genes, with pathway enrichment analysis revealing inflammation-related pathways including NOD-like receptor and chemokine signaling pathways [9]. Specifically, the NF-κB signaling pathway has been identified as significantly perturbed in cytokine storm models [9]. Transcriptomic analysis of TE-treated macrophages enables identification of overlapping differentially expressed genes with those found in solid organs, facilitating understanding of shared pathogenic mechanisms [9].
Cytokine Measurement Techniques: Multiple methodologies exist for cytokine quantification in experimental models, including enzyme-linked immunosorbent assay (ELISA), electrochemiluminescence assay, and emerging point-of-care technologies [64]. ELISA measurements of serum cytokine levels in DJES mice show significant increases in multiple cytokines, with compliance rates of over 90% with transcriptomic data indicating high reproducibility and consistency of results [9]. Electrochemiluminescence assay (Cobas e 411, Roche Diagnostics GmbH) provides standardized methodology for IL-6 measurements in clinical studies [65]. Emerging point-of-care cytokine detection technologies aim to provide rapid, sensitive, and specific methods for monitoring cytokines in biology and medicine, with potential for clinical translation in disease early diagnosis, management, and prevention [64].
Histopathological Evaluation: Systematic histopathological analysis of multiple organs during CSS development provides crucial evidence for understanding organ injury timing and patterns [50]. Hematoxylin-eosin (H&E) staining enables identification of characteristic pathological changes including hepatocellular necrosis, alveolar congestion, and intestinal epithelial destruction [50]. Immunohistochemistry for IL-6 and other cytokines facilitates tracking of spatial and temporal expression patterns during CSS progression [50]. Lung tissue wet-to-dry ratio measurement provides quantitative assessment of tissue edema as an indicator of inflammatory vascular leakage [63].
Diagram 1: Pathophysiological Pathways in Cytokine Storm Syndrome (CSS). This diagram illustrates the sequential activation from initial triggers through immune cell activation, signaling pathways, cytokine release, and eventual organ damage characteristic of CSS.
Research Reagent Solutions and Methodological Toolkit
Essential Research Reagents
D-galactosamine (D-GalN): Used for establishing porcine CSS models at a dosage of 1.5 g/kg administered intravenously [50]. D-GalN binds with uridine triphosphate (UTP) to form UDP-GalN and inhibits UDPG pyrophosphorylase through phosphorylation pathways, leading to significant depletion of UTP and UDPG [50]. This inhibition suppresses synthesis of nucleic acids, proteins, and glycogen in hepatocytes, disrupts cellular membrane systems, induces intracellular Ca²+ influx, and ultimately causes hepatocellular necrosis, establishing a reproducible liver failure model that progresses to CSS [50].
Jellyfish Tentacle Extract (TE): Prepared from Nemopilema nomurai jellyfish for the DJES mouse model [9]. Proteomic analysis shows TE contains predominantly metalloproteinases and other toxic components including staphylococcal toxins, coagulation factors, peroxiredoxins, and phospholipases [9]. The extract is administered intravenously to mice at concentrations ranging from 0 to 2.29 mg kg−1, with LD50 decreasing from 1.9 to 0.7 mg kg−1 as observation time extends from 12 to 48 hours [9].
Polymethyl Methacrylate (PMMA) Adsorption Columns: Experimental cytokine adsorption columns utilizing PMMA fibers with nano-sized pores for size-based cytokine adsorption [63]. The structure comprises 4400 fibers filled with PMMA with a diameter of 116 μm (filling rate, 59% by volume), with a total contact surface area of 285 cm² and filling volume of 1.5 mL for rat models [63]. PMMA adsorption properties are determined by pore size, adsorbing molecules based primarily on molecular dimensions, largely independent of environment [63].
Cytokine Analysis Kits: Commercial ELISA kits for quantitative measurement of TNF-α, IL-6, IL-10, and other cytokines in serum and tissue samples [9] [63]. Electrochemiluminescence assays (Cobas e 411, Roche Diagnostics GmbH) provide standardized methodology for IL-6 measurements in clinical samples [65]. Emerging point-of-care cytokine detection technologies aim to provide rapid, sensitive, and specific methods for cytokine monitoring [64].
Histopathology Reagents: Standard hematoxylin-eosin staining kits for histological assessment of organ damage [50]. Immunohistochemistry antibodies specific for IL-6, IL-10, and other cytokines for spatial localization of inflammatory mediators in tissue sections [50]. Tissue preservation solutions including formalin for sample fixation following experimental protocols [50].
Experimental Protocols and Technical Parameters
Porcine CSS Model Induction: Animals are prepared with jugular vein cannulation under anesthesia induced by intramuscular injection of tiletamine hydrochloride/zolazepam hydrochloride (Sutex 50, 125mg/20kg) [50]. Following surgical preparation, D-GalN solution (0.5g/ml in 5% dextrose) is administered through the double-lumen catheter at 1.5 g/kg dosage [50]. Tissue samples (liver, lungs, intestines, heart, spleen, kidneys) are collected at predetermined time points (0 h, 12 h, 24 h, 36 h) for histopathological analysis and immunohistochemistry [50].
Rat ECMO with Adsorption Protocol: Animals are anesthetized with isoflurane, orotracheally intubated with a 14 G cannula, and ventilated with a respirator [63]. The left common carotid artery is cannulated using polyethylene tubing for blood delivery, and a 16 G cannula is inserted into the jugular vein for blood drainage to establish ECMO at a flow rate of 60 mL/kg/min [63]. During ECMO, arterial partial pressures of oxygen and carbon dioxide are maintained at 300-400 mmHg and 30-40 mmHg, respectively, with mean arterial pressure above 70 mmHg [63]. Unfractionated heparin is used as anticoagulant, with activated clotting time maintained within 200-250 s [63]. For PMMA groups, blood is perfused through the column parallel to the ECMO circuit at 4 mL/kg/min from 30 to 60 minutes after ECMO initiation [63].
Hemoadsorption Clinical Protocol: CytoSorb integration into CRRT circuits (Prismaflex System/Baxter International Inc.) with cartridge placement in pre-dialyzer position [66]. CRRT performed in continuous hemodiafiltration mode (CVVHDF) at blood flow rates of 100-250 mL/min with systemic unfractionated heparin or regional citrate anticoagulation [66]. Cartridges typically changed every 12 or 24 hours based on clinical response, with treatment discontinuation considered upon clinical improvement (reduced catecholamine requirement, increased PaO2/FiO2 ratio) or lack of improvement after 2 treatment sessions [66].
Diagram 2: Experimental Workflow for Cytokine Storm and Hemoadsorption Research. This diagram outlines the sequential stages of experimental approaches from model development through intervention application, sample analysis, and data integration.
Clinical Evidence and Research Applications
Efficacy Assessment in Clinical Studies
Sepsis and Septic Shock: Extracorporeal cytokine adsorption has demonstrated promising results in reducing cytokine levels, improving organ function, and decreasing vasopressor requirements in sepsis and septic shock [60]. However, evidence regarding mortality reduction remains inconsistent across studies [60]. The EUPHAS prospective randomized controlled trial in 64 patients with severe sepsis or septic shock of abdominal origin showed that Toraymyxin therapy reduced hazard ratios for in-hospital mortality up to 28-day in Cox regression models, though 28-day mortality was not significantly different [61]. The mean arterial pressure increased significantly after initiation of Toraymyxin therapy, accompanied by decreased inotropic requirement and vasopressor dependency index [61]. At 72 hours after start of treatment, the Toraymyxin group showed greater reduction in SOFA score compared with the control group [61]. In contrast, larger prospective RCTs such as the ABDOMIX (n=232) and EUPHRATES (n=450) trials found no improvements in hemodynamic parameters, organ dysfunction, or survival in septic shock patients treated with Toraymyxin compared to those receiving standard care [61].
COVID-19 Associated Cytokine Storm: During the COVID-19 pandemic, hemoadsorption was utilized as adjunctive therapy in critically ill patients with COVID-19 associated pneumonia [66]. A retrospective case series of 13 COVID-19 patients requiring mechanical ventilation and renal replacement therapy showed that hemoadsorption with CytoSorb was well-tolerated, with a tendency toward decreased norepinephrine requirement (from 193.7 [IQR: 34.8-270.4] to 50.2 [6.5-243.5] ug/kg/day) and increased PaO2/FiO2 ratio (from 127.8 [95% CI: 96.0-159.6] to 155.0 [115.3-194.6] mmHg), though these changes did not reach statistical significance [66]. All patients were alive at the end of hemoadsorption therapy, but only 3 survived hospital stay, highlighting the severity of illness in this population [66]. Treatment-related adverse events were not reported, suggesting acceptable safety profile in this critically ill population [66].
Matched Case-Control Studies: A retrospective matched case-control study compared interleukin-6 (IL-6) levels in patients treated with or without cytokine adsorber (CytoSorb) [65]. After matching, 21 patients were included in each group, with similar age, ECMO and renal replacement therapy use, baseline noradrenaline requirement, serum lactate, pH, CRP, and IL-6 levels [65]. The study found no significant differences in the time course of IL-6, lactate, CRP, procalcitonin and noradrenaline requirement between groups [65]. Two-day and ICU mortality and Kaplan-Meier estimated survival were also comparable [65]. These findings highlight the ongoing uncertainty regarding the efficacy of extracorporeal cytokine adsorption and emphasize the need for appropriate patient selection and timing of intervention [65].
Integration with Extracorporeal Support Modalities
Combination with ECMO: Extracorporeal cytokine adsorption has been increasingly used in combination with extracorporeal membrane oxygenation (ECMO) in patients with severe cardiac or respiratory failure complicated by cytokine storm [60] [63]. The interaction between ECMO and inflammatory responses creates a rational basis for combining these therapies, as ECMO circuits themselves can activate inflammatory pathways through blood contact with artificial surfaces [63]. Research in rat ECMO models demonstrates that PMMA-based cytokine adsorption columns effectively suppress systemic inflammatory reactions, with significantly lower levels of TNF-α and IL-6 compared to ECMO alone at 120 minutes after completing ECMO [63]. Lung edema incidence was significantly lower in the PMMA group, suggesting organ-protective effects [63].
Integration with CRRT: The combination of hemoadsorption with continuous renal replacement therapy (HA-CRRT) represents the most common clinical application, indicated in sepsis-associated AKI for simultaneous removal of cytokines and uremic toxins [62]. This technique combines a sorbent cartridge in series with a CRRT filter, with complete saturation of the sorbent typically occurring between 6 and 12 hours [62]. Technical considerations include cartridge positioning (typically in pre-dialyzer position), anticoagulation management, and treatment duration decisions [66]. The integrated approach addresses multiple aspects of critical illness simultaneously, potentially optimizing extracorporeal therapy efficiency in hemodynamically unstable patients [60] [62].
Table 3: Clinical Evidence Summary for Extracorporeal Cytokine Removal Devices
| Device | Clinical Evidence Level | Reported Efficacy | Safety Profile | Key Limitations |
|---|---|---|---|---|
| CytoSorb | Multiple RCTs, case series | Reduced vasopressor need, improved hemodynamics; inconsistent mortality benefit | Well-tolerated; potential drug removal | Patient selection, timing, non-selective adsorption |
| Toraymyxin | Multiple RCTs, meta-analyses | Endotoxin reduction, hemodynamic improvement in subset | Well-tolerated; limited drug adsorption | Efficacy dependent on endotoxin levels |
| Oxiris | Observational studies | Combined cytokine/endotoxin removal with renal support | Similar to standard CRRT | Limited high-quality RCT evidence |
| HA330/380 | Case series, registry data | Cytokine reduction, improved SOFA scores | Acceptable safety profile | Limited controlled trial data |
| Seraph 100 | Early clinical experience | Pathogen reduction in bloodstream infections | Heparin-related considerations | Limited outcome data in CSS |
| PMMA Columns | Preclinical studies | Significant cytokine reduction in animal models | Biocompatibility demonstrated | Limited clinical trial data |
Extracorporeal cytokine removal represents a promising adjunctive therapeutic approach for cytokine storm syndromes, with multiple devices now available employing different adsorption mechanisms and target specificities [60]. The current evidence base demonstrates consistent improvements in intermediate endpoints such as cytokine levels, vasopressor requirements, and hemodynamic parameters, though mortality benefits remain uncertain and inconsistent across studies [60] [65]. This discrepancy highlights the complex pathophysiology of cytokine storm syndromes and suggests that future research should focus on optimizing patient selection, timing of intervention, and device selection based on individual patient characteristics and underlying etiology [61].
The future development of extracorporeal cytokine removal technologies will likely focus on enhanced selectivity, improved biocompatibility, and integration with other extracorporeal support modalities [62]. Novel approaches such as the "IL-6-Sieve" aim to provide more targeted adsorption of specific pathogenic mediators while preserving beneficial molecules [61]. The expanding understanding of cytokine storm endotypes and temporal progression will enable more precise application of these technologies, potentially identifying critical therapeutic windows for intervention [50]. Additionally, combination therapies integrating immunomodulatory medications with extracorporeal cytokine removal may provide synergistic benefits by addressing both circulating cytokines and cellular immune activation [1].
From a research perspective, standardization of experimental models, outcome measures, and analytical methodologies will facilitate more meaningful comparisons across studies and devices [50] [63]. The development of point-of-care cytokine monitoring technologies may enable real-time treatment guidance and dose titration of extracorporeal therapies [64]. As the field advances, the integration of multi-omics approaches, including transcriptomics, proteomics, and metabolomics, with clinical outcomes will provide deeper insights into the mechanisms of action of extracorporeal cytokine removal and its impact on the broader immune landscape in critical illness [9]. Through continued technological innovation and rigorous clinical investigation, extracorporeal cytokine removal has the potential to become an established component of multimodal therapy for cytokine storm syndromes across diverse etiologies.
Combination Therapies and Personalized Immunomodulation Approaches
Cytokine Storm (CS) or Cytokine Release Syndrome (CRS) is a life-threatening systemic inflammatory syndrome characterized by excessive immune cell activation and dangerously elevated circulating cytokine levels. This pathological process is a critical driver of multi-organ failure in severe infectious diseases like COVID-19, sepsis, autoimmune conditions, and complications from immunotherapies such as CAR-T cell therapy [1] [8]. The core pathophysiology involves a self-amplifying loop of pro-inflammatory cytokine production, leading to endothelial damage, increased vascular permeability, coagulopathy, and immune cell infiltration into vital organs, culminating in organ dysfunction and high mortality rates [16]. The profound clinical challenge posed by CS necessitates a therapeutic evolution beyond single-agent approaches toward sophisticated combination therapies and personalized immunomodulation strategies. This paradigm leverages a growing understanding of key signaling pathways, biomarker-based risk stratification, and synergistic drug interactions to improve outcomes for this critical condition.
Pathogenic Mechanisms and Signaling Pathways: Targets for Intervention
The hyperinflammatory state in CS is orchestrated by a complex interplay of several dysregulated signaling pathways. Understanding these mechanisms is foundational to designing effective combination therapies.
The JAK-STAT Signaling Pathway
The JAK-STAT pathway is a central signaling node for numerous cytokines implicated in CS, including IL-6, IFN-γ, and others [1]. Upon cytokine binding, receptor-associated Janus kinases (JAKs) phosphorylate signal transducer and activator of transcription (STAT) proteins. These activated STATs dimerize and translocate to the nucleus, driving the expression of pro-inflammatory genes. In CS, overactivation of this pathway leads to a massive release of cytokines and chemokines (e.g., IL-1β, IL-8, CCL2, GM-CSF) [1]. This pathway's significance is highlighted by its role in HLH, aGVHD, CAR-T associated CRS, and COVID-19, making it a prime therapeutic target [1].
Toll-like Receptors (TLRs) and Inflammasome Activation
Toll-like receptors (TLRs) act as primitive pattern recognition receptors (PRRs) that detect pathogen-associated molecular patterns (PAMPs) from invading microbes or damage-associated molecular patterns (DAMPs) from injured host tissues [1] [16]. Their activation triggers downstream signaling cascades, including NF-κB, which promotes the transcription of pro-inflammatory cytokines like IL-1β, IL-6, and TNF-α [16]. Furthermore, sensors like NLRP3 and AIM2 form inflammasome complexes that activate caspase-1. Active caspase-1 cleaves pro-IL-1β and pro-IL-18 into their active forms and triggers pyroptosis, a highly inflammatory form of cell death, through gasdermin D cleavage [16] [67]. In COVID-19, SARS-CoV-2 proteins (N, ORF3a, E) can directly promote NLRP3 inflammasome activation, fueling the CS [16].
Synergistic Cell Death: Panoptosis
Increasing evidence reveals significant crosstalk between inflammatory cell death pathways. Panoptosis is a unified cell death pathway that integrates molecular components from pyroptosis, apoptosis, and necroptosis [67]. In sepsis and severe COVID-19, cytokines like TNF-α and IFN-γ act synergistically to amplify panoptosis. This process forms a vicious cycle: PAMPs, DAMPs, and cytokines trigger inflammatory cell death, and the contents of dying cells further exacerbate cytokine release, sustaining a state of profound immune dysfunction [67].
The diagram below illustrates the interaction between these key pathways.
Figure 1: Integrated Signaling Pathways in Cytokine Storm. This diagram illustrates how PAMPs/DAMPs trigger parallel pathways (TLR/NF-κB and inflammasome) that converge with JAK-STAT signaling to drive cytokine storm, creating a self-amplifying loop through DAMP release.
Established and Emerging Combination Therapies
Monotherapy often proves insufficient to quell the multifaceted hyperinflammation of CS. Combination strategies target different nodes of the immune network simultaneously, aiming for synergistic efficacy.
Corticosteroids as a Backbone for Combination
Corticosteroids (e.g., dexamethasone) form a foundational element in CS management due to their broad anti-inflammatory effects. In severe COVID-19, dexamethasone significantly reduced mortality in patients requiring respiratory support [68]. Their mechanism involves suppressing a wide spectrum of cytokines and chemokines. However, their non-specific immunosuppression can delay viral clearance. Therefore, they are often used as a platform for combining with more targeted agents to enhance efficacy and potentially allow for lower steroid doses, mitigating side effects [68].
Targeting the IL-6 Axis with Adjunctive Therapies
IL-6 is a cornerstone cytokine in CS pathogenesis, and its blockade with the monoclonal antibody tocilizumab (anti-IL-6R) is a validated strategy. Clinical studies in COVID-19 demonstrate that tocilizumab improves the PaO₂/FiO₂ ratio and reduces inflammatory markers like CRP and fibrinogen [69]. Combining tocilizumab with corticosteroids has shown superior outcomes compared to either agent alone, as steroids broadly dampen inflammation while tocilizumab specifically blocks a key amplification signal [68] [69]. This combination is now standard for severe COVID-19 CRS.
JAK-STAT Inhibition in Combinatorial Regimens
JAK inhibitors, such as baricitinib, offer a strategic approach by targeting signaling downstream of multiple cytokines, including IL-6. The US FDA has approved baricitinib for hospitalized COVID-19 patients [68]. Its combination with corticosteroids and/or remdesivir (an antiviral) has demonstrated significant clinical benefit, illustrating the principle of pairing immunomodulation with antiviral activity and broad anti-inflammatory action [68]. This approach effectively dampens the entire JAK-STAT-dependent cytokine network.
Novel Biologics and Future Combinations
Emerging therapies targeting other key cytokines like IL-1 (e.g., anakinra) and TNF-α are under investigation [1] [8]. The future of combination therapy lies in sequentially or simultaneously targeting multiple specific cytokines based on the patient's dominant cytokine profile. For instance, in CAR-T cell CRS, a combination of anti-IL-6 and JAK inhibition is being explored to manage severe neurotoxicity and systemic inflammation while preserving anti-tumor activity [1].
Table 1: Summary of Key Combination Therapy Components
| Therapeutic Class | Example Agents | Primary Mechanism of Action | Rationale in Combination |
|---|---|---|---|
| Corticosteroids | Dexamethasone, Methylprednisolone | Broad-spectrum suppression of cytokine gene expression | Foundational anti-inflammatory backbone; enhances effects of targeted biologics. |
| Cytokine-Targeting Monoclonal Antibodies | Tocilizumab (anti-IL-6R), Sarilumab (anti-IL-6R), Anakinra (IL-1Ra) | Blocks specific cytokine-receptor interactions | Provides precise inhibition of dominant cytokine drivers; synergizes with broader agents. |
| JAK Inhibitors | Baricitinib, Ruxolitinib | Inhibits intracellular signaling downstream of multiple cytokine receptors | Offers a "network" effect against several cytokines; can be combined with biologics and steroids. |
| Antivirals/Antimicrobials | Remdesivir, Favipiravir | Directly targets and inhibits viral replication | Addresses the underlying infectious trigger, reducing antigenic stimulus for CS. |
The Framework for Personalized Immunomodulation
Personalized immunomodulation moves beyond a one-size-fits-all approach by using biomarkers and clinical data to guide therapy selection, timing, and intensity for individual patients.
Biomarker-Guided Risk Stratification and Diagnosis
Early identification of patients progressing toward severe CS is critical for timely intervention. Several biomarkers have prognostic and diagnostic value.
- Cytokine Levels: Elevated levels of IL-6, IL-10, and TNF-α are strongly associated with the development of ARDS and extrapulmonary organ dysfunction. In COVID-19-associated ARDS, rising levels of IL-6, IL-8, and IL-10 correlate with coagulation abnormalities and disseminated intravascular coagulation (DIC), while IL-6 and TNF-α are linked to acute kidney injury (AKI) [23]. IL-6 levels ≥10 times the upper limit of normal are part of the diagnostic criteria for CRS [69].
- Acute Phase Reactants: C-reactive protein (CRP), ferritin, and Serum Amyloid A (SAA) are routinely used. CRP >4.6 mg/dL and ferritin >250 ng/mL (or >2000 ng/mL in severe cases) support a CRS diagnosis [69]. SAA levels can surge a thousand-fold during sepsis, reflecting inflammatory intensity [67].
- Hematological and Coagulation Parameters: Lymphopenia, an elevated neutrophil-to-lymphocyte ratio (NLR), and increased D-dimer are common findings and correlate with poor prognosis [70] [23]. An increasing Monocyte Distribution Width (MDW) is an emerging early indicator of sepsis [67].
- Gene Expression Profiling: Measuring cytokine gene expression (e.g., of IL-2, IL-6, IFN-γ) via multiplex qRT-PCR early in the disease course can help triage patients at risk for severe disease [70].
Comorbidity and Immune Status Assessment
The patient's baseline immune status and comorbidities significantly influence CS risk and treatment response. Patients with autoimmune rheumatic diseases (AIRDs) on immunosuppressants represent a complex population where the benefit-risk ratio of immunomodulation must be carefully balanced to avoid blunting antiviral defense [68]. Similarly, age >65 years and the presence of diabetes mellitus, hypertension, or multimorbidity are significant risk factors for severe CS [70] [8].
Table 2: Key Biomarkers for Personalizing Cytokine Storm Management
| Biomarker Category | Specific Biomarkers | Association with Cytokine Storm Severity | Potential Clinical Utility |
|---|---|---|---|
| Circulating Cytokines | IL-6, IL-10, TNF-α, IFN-γ | Directly measure the core mediators of CS; levels correlate with organ failure and mortality. | Guiding initiation of targeted biologics (e.g., anti-IL-6 therapy); prognostic stratification. |
| Acute Phase Proteins | CRP, Ferritin, Serum Amyloid A (SAA) | Markers of systemic inflammatory response; high levels are integral to CRS diagnosis. | Rapid, cost-effective screening and monitoring of treatment response. |
| Coagulation Markers | D-dimer, Fibrinogen | Indicators of CS-associated coagulopathy and thrombotic microangiopathy. | Assessing risk of thrombosis/DIC; monitoring efficacy of immunomodulation on coagulation. |
| Cellular Biomarkers | Lymphocyte count, Neutrophil-to-Lymphocyte Ratio (NLR), Monocyte Distribution Width (MDW) | Reflects immune cell activation and consumption. Lymphopenia is a hallmark of severe disease. | Early risk stratification (MDW, NLR); assessing overall immune status. |
Experimental Protocols and Research Methodologies
Research into novel combination and personalized therapies relies on robust in vitro, in vivo, and clinical methodologies.
In Vitro Cytokine Release and Immune Cell Assays
Objective: To screen the efficacy and synergy of immunomodulatory compounds on immune cell activation and cytokine production. Methodology:
- Immune Cell Culture: Isolate human peripheral blood mononuclear cells (PBMCs) from healthy donors or patients. Alternative models include using primary macrophages or dendritic cells.
- Stimulation: Stimulate cells with CS triggers such as lipopolysaccharide (LPS, a TLR4 agonist), SARS-CoV-2 proteins (e.g., S protein), or agents that mimic viral infection (e.g., imiquimod) [16] [71].
- Drug Treatment: Co-incubate stimulated cells with single agents or combinations of investigational drugs (e.g., JAK inhibitors, cytokine-neutralizing antibodies, corticosteroids) across a range of concentrations.
- Outcome Measurement:
- Cytokine Profiling: Quantify a panel of cytokines (e.g., IL-6, TNF-α, IL-1β, IFN-γ) in the supernatant using bead-based multiplex immunoassays (e.g., Luminex) or electrochemiluminescence assays [70] [23].
- Cell Viability: Assess cytotoxicity of treatments using assays like MTT or LDH release.
- Signaling Pathway Analysis: Use western blotting or phospho-flow cytometry to confirm target engagement (e.g., inhibition of STAT phosphorylation by JAK inhibitors) [1].
In Vivo Models of Cytokine Storm
Objective: To evaluate the therapeutic potential and synergistic effects of drug combinations in a whole-organism context. Methodology:
- Animal Model Selection: Common models include:
- SARS-CoV-2 infection models in transgenic mice expressing human ACE2.
- LPS-induced endotoxemia model as a classic model of systemic inflammation [71].
- Mouse models of hemophagocytic lymphohistiocytosis (HLH) or CAR-T cell CRS.
- Treatment Regimen: Animals are randomized to receive vehicle, monotherapies, or combination therapies. Treatment can be prophylactic or therapeutic, initiated after the onset of symptoms.
- Endpoint Analysis:
- Clinical Scoring: Monitor survival, body weight, temperature, and behavior.
- Serum Collection: Measure cytokine levels to assess systemic inflammation.
- Histopathology: Examine organs (lungs, liver, spleen, kidneys) for evidence of immune cell infiltration, damage, and cell death (e.g., pyroptosis/panoptosis) [67].
- Flow Cytometry: Analyze immune cell populations in blood and lymphoid organs for activation status and composition.
Clinical Trial Design for Combination Therapies
Objective: To validate the safety and efficacy of combination immunomodulation in human patients. Methodology:
- Patient Population: Enroll patients with defined CS (e.g., using modified Temple criteria for COVID-19 CRS: worsening respiration, bilateral infiltrates, CRP >4.6 mg/dL, ferritin >250 ng/mL, and IL-6 elevation) [69].
- Study Design: Randomized, controlled trials (RCTs) are the gold standard. Adaptive trial designs are particularly useful for efficiently testing multiple combinations.
- Stratification: Stratify patients at randomization based on key prognostic biomarkers (e.g., baseline IL-6 level, presence of organ dysfunction, comorbidities) to enable personalized analysis.
- Outcome Measures:
The workflow for developing these therapies is systematic, as shown below.
Figure 2: Therapeutic Development Workflow. This chart outlines the translational pipeline from initial biomarker discovery to personalized treatment assignment in clinical trials.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Cytokine Storm Investigation
| Reagent / Tool Category | Specific Examples | Research Function |
|---|---|---|
| Cytokine Detection & Quantification | Multiplex Bead Arrays (Luminex), Electrochemiluminescence Assays (ECLIA), ELISA Kits | Precise measurement of a wide panel of cytokines (e.g., IL-6, TNF-α, IL-1β) in serum, plasma, and cell culture supernatants to characterize CS and monitor interventions. |
| Cell Signaling Assays | Phospho-specific Flow Cytometry, Western Blotting Kits (e.g., for p-STAT3) | Verification of target engagement and mechanism of action for drugs like JAK inhibitors by analyzing phosphorylation status of key signaling proteins. |
| Pathway Agonists/Antagonists | LPS (TLR4 agonist), Recombinant cytokines, JAK inhibitors (e.g., Baricitinib), Neutralizing antibodies (e.g., anti-IL-6R) | Tools to induce CS-like conditions in vitro and in vivo and to probe the function of specific pathways for target validation. |
| Gene Expression Analysis | qRT-PCR Primers for cytokine genes (IL-6, IL-2, IFN-γ), RNA extraction kits, SYBR Green/Probe-based master mixes | Early detection of immune activation and studying transcriptional regulation of cytokines in patient samples or cell models [70]. |
| Animal Models | LPS-induced endotoxemia models, SARS-CoV-2 infected hACE2 transgenic mice, HLH/CRS mouse models | Preclinical in vivo systems for evaluating the efficacy, toxicity, and synergistic potential of combination therapies. |
The management of cytokine storm is rapidly evolving from reactive, broad immunosuppression toward a proactive paradigm of personalized immunomodulation. This approach leverages combination therapies that target multiple pathogenic pathways simultaneously—such as corticosteroids with JAK inhibitors or IL-6 blockers—to achieve synergistic efficacy. The core of this new paradigm is the use of dynamic biomarker profiling (including cytokines, acute phase reactants, and cellular markers) to stratify patients, guide therapy selection, and monitor response in real time.
Future progress hinges on several key areas: the discovery and validation of even more precise predictive biomarkers, the development of advanced in silico and in vitro models for testing drug combinations, and the wider adoption of adaptive clinical trial designs. Furthermore, integrating host immunogenetics and the dynamics of the underlying infection (viral or bacterial) will be crucial for creating truly comprehensive treatment algorithms. By continuing to deconvolute the intricate immunology of the cytokine storm, researchers and clinicians can design increasingly effective, personalized combination regimens that halt pathological inflammation while preserving protective immunity, ultimately improving survival and recovery from this lethal syndrome.
Addressing Clinical Challenges and Optimizing Therapeutic Efficacy
The management of cytokine storm, a life-threatening systemic inflammatory syndrome, presents a critical therapeutic dilemma. Interventions must balance the immediate need to suppress hyperinflammation with the long-term risk of inducing profound immunosuppression. This challenge is particularly acute in sepsis and severe viral infections, where cytokine storm is a primary driver of multiple organ failure (MODS) [48] [10]. Research trends highlight that the molecular and cellular mechanisms in sepsis, including inflammatory cell death pathways and immune dysregulation, are major research hotspots [48]. The pathophysiological progression involves an initial hyperinflammatory phase characterized by excessive release of proinflammatory cytokines such as TNF-α, IL-1β, and IL-6, often followed by a compensatory immunosuppressive phase that increases vulnerability to secondary infections [10]. This review examines the safety concerns and immunosuppression risks associated with current and emerging therapies, providing a framework for developing safer immunomodulatory strategies.
Pathophysiological Basis of Cytokine Storm and Organ Damage
Key Mediators and Signaling Pathways
Cytokine storm pathogenesis involves complex interactions between innate immune hyperactivation, inflammatory cell death pathways, and loss of immune homeostasis. The initial trigger occurs when pathogen-associated molecular patterns (PAMPs) and damage-associated molecular patterns (DAMPs) activate pattern recognition receptors (PRRs), triggering downstream signaling cascades including NF-κB and AP-1 that upregulate pro-inflammatory gene programs [10]. Inflammasome activation leads to caspase-1-mediated cleavage of pro-IL-1β and pro-IL-18 into their active forms, amplifying the inflammatory cascade [10].
Table 1: Major Cytokine Players in Organ Failure Pathogenesis
| Cytokine | Primary Cellular Source | Key Pathogenic Functions | Therapeutic Targeting Approaches |
|---|---|---|---|
| IL-6 | Macrophages, T cells | Fever, acute phase proteins, B-cell differentiation | Monoclonal antibodies (tocilizumab), siRNA |
| TNF-α | Macrophages, NK cells | Endothelial activation, vascular leakage | Monoclonal antibodies (infliximab) |
| IL-1β | Macrophages, monocytes | Pyroptosis induction, endothelial damage | IL-1 receptor antagonist (anakinra) |
| IFN-γ | T cells, NK cells | Macrophage activation, MHC upregulation | Monoclonal antibodies |
| GM-CSF | T cells, macrophages | Monocyte differentiation, inflammatory activation | Monoclonal antibodies (mavrilimumab) |
Inflammatory Cell Death and Organ Damage
Inflammatory forms of programmed cell death are central to cytokine storm pathology. Pyroptosis, mediated through gasdermin family pore formation, and necroptosis, driven by RIPK3-mediated oligomerization of MLKL, create a self-amplifying circuit of inflammation and tissue damage [10]. Under sustained inflammatory stress, these pathways converge in panoptosis, a unified cell death pathway integrating molecular components of pyroptosis, apoptosis, and necroptosis [10]. This synergistic cell death mechanism is particularly destructive in sepsis models, where its inhibition significantly reduces mortality [10]. The resulting organ damage follows a recognizable pattern, with lungs, kidneys, and cardiovascular system being particularly vulnerable due to their extensive endothelial surfaces and high metabolic demands.
Current Therapeutic Limitations and Safety Profiles
Immunosuppressive Agents and Infection Risks
Conventional immunosuppressive approaches carry significant safety concerns, particularly regarding increased susceptibility to secondary infections. Corticosteroids, while reducing inflammation broadly, impair multiple immune functions including neutrophil chemotaxis, antigen presentation, and lymphocyte activation [72]. The non-specific nature of these interventions disrupts homeostatic immune surveillance, creating opportunities for opportunistic pathogens. Clinical data from COVID-19 patients reveals that lymphopenia, a hallmark of severe infection, correlates with increased mortality and may be exacerbated by overly aggressive immunosuppression [72] [73]. This is particularly problematic in sepsis, where early lymphocyte depletion is independently associated with poor outcomes [10].
Cytokine-Targeted Therapies and Limitations
Targeted cytokine blockade represents a more precise approach but faces unique challenges. Anti-cytokine therapies (e.g., IL-6, IL-1 antagonists) risk oversuppressing beneficial inflammation necessary for pathogen clearance [72] [73]. This paradox is evident in patients treated with tocilizumab (anti-IL-6 receptor), who may show improved survival from cytokine storm but experience increased incidence of secondary infections [73]. Additionally, the redundancy in cytokine signaling means that single-target approaches often have limited efficacy, as other cytokines can compensate through overlapping functions.
Table 2: Safety Profiles of Selected Cytokine-Targeted Therapies
| Therapeutic Agent | Target | Efficacy Concerns | Major Safety Risks | Clinical Context |
|---|---|---|---|---|
| Tocilizumab | IL-6 receptor | Delayed administration reduces efficacy | Secondary infections, hepatotoxicity | COVID-19, rheumatoid arthritis |
| Anakinra | IL-1 receptor | Short half-life requires continuous infusion | Neutropenia, increased infection risk | Sepsis, COVID-19 |
| Ruxolitinib | JAK/STAT pathway | Broad immunosuppression | Thrombocytopenia, anemia | COVID-19, myelofibrosis |
| Infliximab | TNF-α | Increased mortality in septic shock | Reactivation of latent tuberculosis | Rheumatoid arthritis, Crohn's |
Quantitative Assessment of Immunosuppression Risks
The transition from hyperinflammatory to immunosuppressive phases in sepsis presents both monitoring and therapeutic challenges. Biomarkers provide critical windows into this immunological progression, enabling more precise therapeutic interventions.
Table 3: Biomarkers for Monitoring Immunosuppression Risk
| Biomarker | Physiological Role | Change During Immunosuppression | Predictive Value |
|---|---|---|---|
| HLA-DR expression on monocytes | Antigen presentation | Reduced expression (>48h low levels) | High for secondary infections |
| Absolute lymphocyte count | Adaptive immune function | Progressive lymphopenia | Mortality correlation |
| IL-6 | Proinflammatory cytokine | Sustained elevation despite therapy | Treatment resistance |
| Monocyte Distribution Width (MDW) | Monocyte activation | Increased heterogeneity | Early sepsis detection |
| Serum amyloid A (SAA) | Acute phase reactant | Rapid decline indicates resolution | Treatment response |
Quantitative analyses reveal that the severity of cytokine storm, measured by elevated levels of interleukin-1B, interferon-γ, interferon-inducible protein 10, and monocyte chemoattractant protein 1, directly correlates with disease severity and subsequent immunosuppression risk [72]. Patients requiring ICU admission demonstrate higher concentrations of granulocyte colony-stimulating factor, IP-10, MCP-1, macrophage inflammatory protein 1A, and TNF-α compared to non-ICU patients [72]. These quantitative relationships enable risk stratification for immunosuppression complications.
Methodologies for Evaluating Therapeutic Safety
In Vitro Immune Competence Assays
Comprehensive safety assessment requires robust methodologies for evaluating immune function. The following protocols provide standardized approaches for quantifying immunosuppression risks:
Protocol 1: Monocyte HLA-DR Expression Quantification
- Principle: Flow cytometric measurement of MHC class II expression indicates antigen presentation capacity
- Procedure:
- Collect peripheral blood samples in EDTA tubes
- Stain with anti-CD14-FITC and anti-HLA-DR-PE antibodies
- Analyze by flow cytometry within 4 hours of collection
- Calculate percentage of HLA-DR positive monocytes and mean fluorescence intensity
- Interpretation: <30% HLA-DR+ monocytes or <5000 MFI indicates significant immunosuppression
- Applications: Stratifying patients for immunoadjuvant therapy, predicting secondary infection risk
Protocol 2: Whole Blood Ex Vivo Cytokine Stimulation
- Principle: Measures reserved immune responsiveness to pathogen challenges
- Procedure:
- Dilute fresh heparinized blood 1:5 with RPMI medium
- Stimulate with LPS (100 ng/mL) for TNF-α response or SEB (1 μg/mL) for IFN-γ response
- Incubate at 37°C for 4-6 hours (TNF-α) or 24-48 hours (IFN-γ)
- Measure cytokine production by ELISA or multiplex assay
- Interpretation: Reduced cytokine production (<50% of healthy controls) indicates functional immunosuppression
- Applications: Identifying candidates for immunostimulatory therapies
Advanced Techniques for Safety Profiling
Emerging methodologies provide deeper insights into therapeutic safety profiles:
Single-Cell RNA Sequencing for Immune Monitoring
- Enables comprehensive characterization of immune cell populations and their functional states
- Identifies novel immunosuppressive cell subsets (e.g., MDSCs, regulatory subsets)
- Reveals changes in immune cell metabolism and signaling pathways
Cellular Metabolism Profiling
- Measures glycolytic and oxidative phosphorylation rates in immune cells
- Immunosuppressed cells typically show metabolic reprogramming
- Can predict functional recovery potential during therapy
Experimental Visualization: Signaling Pathways and Therapeutic Targets
Cytokine Storm Signaling and Therapeutic Intervention Points
Integrated Therapeutic Approaches and Safety Mitigation
Sequential and Combinatorial Strategies
Overcoming current limitations requires integrated approaches that address both hyperinflammation and subsequent immunosuppression:
Phase-Specific Immunomodulation
- Hyperacute Phase (Days 1-3): Targeted cytokine blockade with IL-6 or IL-1 antagonists combined with precision glucocorticoid dosing
- Transition Phase (Days 4-7): Immunomonitoring-guided therapy reduction with surveillance for immunosuppression
- Late Phase (Day 7+): Immunostimulatory interventions (IL-7, IFN-γ, immune checkpoint inhibitors) for persistent immunosuppression
Biomarker-Guided Personalization
- Implement serial immune profiling (HLA-DR, lymphocyte subsets, cytokine levels)
- Use MDW and SAA for early detection and intervention timing
- Apply viral load and clearance rate monitoring to inform immunotherapy duration
Novel Therapeutic Platforms with Improved Safety Profiles
Emerging technologies offer promising approaches for overcoming current limitations:
Nanomedicine-Based Delivery Systems
- Targeted delivery to specific immune cell subsets reduces off-target effects
- Stimuli-responsive release in inflammatory environments enhances precision
- Combination therapy loading enables coordinated intervention on multiple pathways
Bi-Specific and Multi-Functional Biologics
- Engineered molecules that simultaneously target cytokines and immune checkpoints
- Conditionally active biologics that function primarily in hyperinflammatory environments
- Dual-acting compounds that suppress inflammation while promoting microbial clearance
The Scientist's Toolkit: Key Research Reagents
Table 4: Essential Research Tools for Cytokine Storm and Immunosuppression Studies
| Reagent/Category | Specific Examples | Research Application | Safety Assessment Utility |
|---|---|---|---|
| Cytokine ELISA Kits | IL-6, IL-1β, TNF-α, IL-10 | Quantifying cytokine levels in serum/plasma | Monitoring therapy efficacy and inflammation resolution |
| Flow Cytometry Antibodies | CD14, HLA-DR, CD3, CD4, CD8 | Immune phenotyping and functional assessment | Identifying immunosuppressive states (low HLA-DR) |
| Pathway Inhibitors | NF-κB inhibitors, JAK/STAT inhibitors, Caspase-1 inhibitors | Mechanistic studies of signaling pathways | Evaluating targeted therapy specificity and off-target effects |
| Animal Models | CLP sepsis, LPS challenge, SARS-CoV-2 mouse models | In vivo efficacy and safety testing | Modeling hyperinflammation-to-immunosuppression transition |
| Cell Death Assays | Gasdermin D cleavage, LDH release, Annexin V | Quantifying pyroptosis, apoptosis, necroptosis | Assessing tissue damage mechanisms and protective interventions |
| Metabolic Probes | Seahorse XFp Analyzer, 2-NBDG | Immune cell metabolic profiling | Identifying metabolic dysfunction in immunosuppression |
Overcoming the therapeutic limitations in cytokine storm management requires integrated approaches that balance effective inflammation control with preservation of protective immunity. The path forward lies in developing phase-specific interventions, biomarker-guided personalization, and novel therapeutic platforms with inherent safety features. By understanding the intricate dynamics between hyperinflammation and immunosuppression, researchers can design smarter immunomodulatory strategies that maximize efficacy while minimizing risks. The continued development of sophisticated monitoring tools and targeted therapeutics promises to transform the management of cytokine storm and multiple organ failure, ultimately improving outcomes for patients with these life-threatening conditions.
Pathophysiological Transition from Sepsis to PICS
Sepsis initiates a complex immune response characterized by early hyperinflammation, often termed a cytokine storm, which can progress to a state of chronic critical illness known as Persistent Inflammation-Immunosuppression Catabolism Syndrome (PICS). Understanding this transition is crucial for developing targeted therapeutic interventions.
The early phase of sepsis is dominated by innate immune hyperactivation. Pathogen-associated molecular patterns (PAMPs) and damage-associated molecular patterns (DAMPs) are recognized by pattern recognition receptors (PRRs) such as Toll-like receptors (TLRs) on immune cells, triggering intracellular signaling cascades including NF-κB and MAPK pathways [74] [10]. This activation leads to excessive production of pro-inflammatory cytokines including TNF-α, IL-1β, IL-6, IL-12, IFN-α, IFN-β, and IFN-γ [10] [75]. This cytokine storm drives systemic inflammatory response syndrome (SIRS), endothelial dysfunction, and multiple organ dysfunction syndrome (MODS) through several mechanisms: increased vascular permeability, activation of the coagulation cascade, and induction of inflammatory cell death pathways such as pyroptosis and necroptosis [10] [76].
A subset of sepsis patients transitions to PICS, a state of chronic critical illness characterized by concurrent persistent inflammation, immunosuppression, and protein catabolism [77] [10]. This transition involves a shift in immune homeostasis where hyperinflammatory and immunosuppressive responses coexist. Key features of established PICS include sustained elevation of inflammatory markers such as C-reactive protein (CRP), coupled with lymphopenia, hypoalbuminemia, and expansion of myeloid-derived suppressor cells (MDSCs) [77]. The metabolic dysregulation in PICS manifests as muscle wasting, weight loss, and negative nitrogen balance, creating a self-perpetuating cycle of organ failure, recurrent infections, and functional decline [77] [10].
Table 1: Key Characteristics Differentiating Early Sepsis and Established PICS
| Parameter | Early Sepsis (Hyperinflammatory) | Established PICS |
|---|---|---|
| Inflammatory Markers | Sharply elevated TNF-α, IL-1β, IL-6 | Persistently elevated CRP, IL-6 |
| Immune Status | Immune hyperactivation | Concurrent inflammation & immunosuppression |
| Lymphocyte Count | Variable, often decreased | Consistently low (<0.80×10⁹ L⁻¹) |
| Key Cellular Players | Neutrophils, inflammatory macrophages | MDSCs, exhausted T-cells |
| Clinical Course | Acute critical illness | Chronic critical illness (>14 days) |
| Metabolic State | Hypermetabolism | Catabolism, muscle wasting |
Biomarkers and Diagnostic Approaches
Accurate diagnosis and monitoring of sepsis progression to PICS require a multimodal approach incorporating inflammatory, immunosuppressive, and metabolic biomarkers.
Inflammatory Biomarkers
C-reactive protein (CRP) demonstrates significant diagnostic utility, with meta-analysis showing levels approximately 34.4 mg L⁻¹ higher in PICS patients compared to non-PICS patients (95% CI: 12.7–56.2 mg L⁻¹; P<0.01) [77]. Serum amyloid A (SAA), an acute-phase reactant, can surge up to a thousand-fold during septic events and functions as a potent chemoattractant for neutrophils and monocytes [10]. Procalcitonin (PCT) has established value in distinguishing bacterial infections and guiding antimicrobial therapy [75].
Immunosuppression Markers
Lymphopenia is a hallmark feature, with PICS patients showing 0.36×10⁹ L⁻¹ lower lymphocyte counts than non-PICS patients (95% CI: 0.25–0.47×10⁹ L⁻¹; P=0.01) [77]. Reduced HLA-DR expression on monocytes indicates impaired antigen presentation capacity and correlates with increased infection risk [76]. Elevated anti-inflammatory cytokines including IL-10 and IL-37 contribute to immunosuppression by inhibiting T-cell function and promoting regulatory T-cell expansion [76].
Metabolic and Emerging Biomarkers
Serum albumin is significantly lower in PICS patients (mean difference: -4.4 g L⁻¹; 95% CI: 0.5–8.3 g L⁻¹; P<0.01) [77]. Monocyte distribution width (MDW) has emerged as a promising early sepsis biomarker, with values >23.5 demonstrating good discriminatory power in emergency settings [10]. High-density lipoprotein (HDL) undergoes quantitative and qualitative changes during sepsis, with decreased levels and impaired function correlating with disease severity [10].
Table 2: Key Biomarkers for Monitoring Sepsis and PICS Progression
| Biomarker Category | Specific Marker | Significance in Sepsis/PICS | Typical Alteration |
|---|---|---|---|
| Inflammation | CRP | Acute phase reactant, general inflammation | ↑↑ |
| IL-6 | Pro-inflammatory cytokine, prognostic value | ↑↑ | |
| SAA | Acute phase reactant, chemotaxis | ↑↑↑ | |
| Immunosuppression | Lymphocyte count | Indicator of adaptive immune competence | ↓↓ |
| HLA-DR on monocytes | Antigen presentation capacity | ↓ | |
| IL-10 | Anti-inflammatory, immunosuppressive | ↑ | |
| Metabolic/Catabolic | Serum albumin | Nutritional status, inflammation | ↓↓ |
| CD4/CD8 ratio | T-cell exhaustion | ↓ | |
| Emerging | MDW | Monocyte activation | ↑ |
| NLR | Systemic inflammation | ↑ |
Experimental Models and Methodologies
In Vivo Modeling of Sepsis and PICS
The cecal ligation and puncture (CLP) model remains the gold standard for sepsis research due to its clinical relevance in mimicking polymicrobial peritoneal sepsis. Detailed protocol: (1) Anesthetize mice (e.g., C57BL/6, 8-12 weeks) using inhaled isoflurane or injectable ketamine/xylazine; (2) Make a midline laparotomy incision; (3) Expose and ligate 50-75% of the cecum; (4) Perform a single or double through-and-through puncture with specified needle size (e.g., 21-gauge); (5) Express a small amount of fecal material; (6) Return cecum to peritoneal cavity; (7) Close abdomen in layers; (8) Administer subcutaneous fluids and analgesics postoperatively [76]. This model reliably produces hyperinflammatory and immunosuppressive phases, allowing study of the sepsis-to-PICS transition.
The DJES mouse model (Delayed Jellyfish Envenomation Syndrome) demonstrates cytokine storm induction through venom injection. Detailed protocol: (1) Prepare tentacle extract (TE) from Nemopilema nomurai jellyfish; (2) Intravenously inject varying concentrations (LD50: 0.7-1.9 mg kg⁻¹) via tail vein; (3) Monitor survival every 6 hours for 48 hours; (4) Collect tissues (heart, liver, kidneys) for histopathology and cytokine analysis at 6 hours post-injection [9]. This model shows NF-κB p65-dependent cytokine upregulation and multi-organ failure, replicating human delayed envenomation syndrome.
In Vitro Immunological Assays
Macrophage cytotoxicity and cytokine production assays provide mechanistic insights: (1) Culture RAW 274.6 macrophages; (2) Treat with inflammatory stimuli (LPS, jellyfish venom); (3) Measure cytotoxicity using CCK-8 assay (IC50: 17.39 µg mL⁻¹ for jellyfish venom); (4) Quantify cytokine production (IL-6, TNF-α, CXCL2, CCL4) via ELISA or multiplex arrays; (5) Perform transcriptomic analysis to identify differentially expressed genes and pathways [9].
T-cell exhaustion and function assays: (1) Isolate PBMCs from septic patients or model animals; (2) Analyze T-cell subsets (CD4+, CD8+) by flow cytometry; (3) Measure expression of exhaustion markers (PD-1, TIM-3, BTLA); (4) Assess T-cell proliferation via CFSE dilution or ³H-thymidine incorporation; (5) Quantify cytokine production capacity after stimulation [78] [76].
Signaling Pathways and Therapeutic Targets
Key Inflammatory Pathways
Diagram: Inflammatory Signaling in Early Sepsis. This pathway illustrates the initial hyperinflammatory response triggered by PAMPs/DAMPs recognition, leading to cytokine storm through multiple interconnected pathways.
Immunosuppressive Pathways in PICS
Diagram: PICS Immunosuppressive Pathways. This self-perpetuating cycle illustrates how persistent inflammation drives immunosuppression and catabolism in chronic critical illness.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Sepsis and PICS Investigation
| Reagent/Category | Specific Examples | Research Application |
|---|---|---|
| Cytokine Detection | ELISA kits (IL-6, TNF-α, IL-1β, IL-10), Multiplex bead arrays | Quantifying inflammatory and anti-inflammatory mediators in serum/plasma and tissue homogenates |
| Flow Cytometry Antibodies | Anti-CD4, CD8, CD14, HLA-DR, PD-1, TIM-3, BTLA | Immunophenotyping of immune cell populations and exhaustion markers |
| Cell Culture Models | RAW 274.6 macrophages, THP-1 monocytic cells, primary human PBMCs | In vitro mechanistic studies of immune cell function and signaling pathways |
| Pathway Inhibitors JAK inhibitors (tofacitinib), NF-κB inhibitors (BAY-11), Caspase inhibitors | Experimental therapeutic interventions to dissect specific pathway contributions | |
| Animal Models | CLP surgery supplies, LPS, pathogen isolates | In vivo modeling of sepsis progression and therapeutic testing |
| Molecular Biology | RNA extraction kits, qPCR reagents, Western blot antibodies | Analysis of gene expression, protein quantification, and signaling pathway activation |
Emerging Therapeutic Strategies
The management of PICS requires targeting both persistent inflammation and concurrent immunosuppression. Several promising approaches are under investigation:
Immunostimulation strategies aim to reverse sepsis-induced immunosuppression. GM-CSF has shown potential in restoring monocyte function and improving pathogen clearance [74]. Immune checkpoint inhibitors targeting PD-1/PD-L1 and IL-7 are being explored to reverse T-cell exhaustion and improve adaptive immunity [78] [76]. Clinical trials of anti-PD-L1 antibodies in septic patients have demonstrated restored immune function and reduced nosocomial infections [76].
Targeted immunomodulation approaches include JAK/STAT pathway inhibition which has demonstrated efficacy in mitigating cytokine storm across various conditions including COVID-19 and CAR-T cell therapy [1]. IL-6 receptor blockade with tocilizumab and IL-1 inhibition with anakinra have shown promise in selected patient subgroups by modulating specific inflammatory pathways without causing broad immunosuppression [1] [75].
Nutritional and metabolic support is crucial for addressing the catabolic component of PICS. Specific nutritional formulations with high-protein, anti-oxidant, and immunomodulating components (e.g., glutamine, omega-3 fatty acids) may help counteract muscle wasting and support immune reconstitution [77].
The future of PICS management lies in precision immunomodulation based on comprehensive immune monitoring to identify individual patient's dominant pathophysiology and tailor therapies accordingly [74] [10]. This approach requires advanced diagnostic tools to accurately phenotype patients and guide targeted interventions at appropriate timepoints in their clinical course.
The study of cytokine storm (CS) and multiple organ dysfunction syndrome (MODS) represents a critical frontier in critical care medicine and immunology. CS, a life-threatening systemic inflammatory syndrome characterized by hyperactivation of immune cells and elevated levels of circulating cytokines, is implicated in the development of life-threatening conditions including fulminant myocarditis, acute respiratory distress syndrome (ARDS), and hemophagocytic lymphohistiocytosis (HLH) [1]. This uncontrolled immune activation results in cytokine hypersecretion, which becomes an important reason for symptom aggravation and can spread throughout the body leading to systemic multiple organ dysfunction [79]. The clinical presentation includes acute systemic inflammatory symptoms, organ dysfunction, and significant mortality, with severe lung injury often progressing to ARDS [79] [1].
The economic and accessibility challenges surrounding advanced biologic treatments for CS and the physical infrastructure of intensive care units represent interconnected barriers to effective patient management. Biologic drugs have transformed treatment for serious conditions including those mediated by cytokine storms, but their high cost creates insurmountable financial barriers for many patients [80]. Meanwhile, ICU infrastructure limitations directly impact the capacity to manage MODS, where organ dysfunctions are linked in a positive feedback loop through circulating inflammatory mediators [81]. This technical review examines these parallel challenges within the context of ongoing CS and MODS research, addressing both therapeutic access barriers and critical care capacity constraints.
Pathophysiological Mechanisms of Cytokine Storm and Organ Dysfunction
Key Signaling Pathways in Cytokine Storm
The pathogenesis of CS involves multiple interconnected signaling pathways that drive the hyperinflammatory state:
JAK-STAT Pathway: The JAKs (Janus kinases) and STATs (signal transducers and activators of transcription) represent a highly conserved signaling pathway that plays a significant role in CS [1]. This pathway consists of three main structural components: transmembrane receptors, receptor-associated JAKs, and STATs. The JAK family includes four subtypes: JAK1, JAK2, JAK3, and TYK2, while the STAT family consists of seven subtypes [1]. Numerous cytokines, including ILs, IFNs, and growth factors, participate in JAK-STAT signaling. Specifically, IL-6, a multifunctional cytokine, triggers the JAK-STAT3 pathway through classical cis-signaling, trans-signaling, and trans-presentation mechanisms [1]. IL-6 can interact with the membrane-bound IL-6 receptor (mIL-6R) on immune cells, as well as with the soluble form of the IL-6 receptor (sIL-6R), forming a complex that triggers activation of gp130 and subsequently initiates JAK-STAT3 signaling [1]. This activation cascade results in a systemic hyperinflammatory response, leading to secretion of various mediators including IL-1β, IL-8, CCL2, CCL3, CCL5, GM-CSF, and VEGF [1].
Toll-like Receptors (TLRs): TLRs represent a primitive category of pattern recognition receptors (PRRs) that recognize pathogen-associated molecular patterns (PAMPs) [1]. These receptors are present on various immune cells and tissue cells, such as monocytes, macrophages, and dendritic cells (DCs), serving as detectors of pathogen incursion. Activation of TLRs plays a critical role in the development of infectious diseases and CS progression [1]. Upon recognizing PAMPs, TLRs initiate the release of pro-inflammatory cytokines and orchestrate immune responses to safeguard cells from harm. Activation leads to production of antiviral cytokines such as type I IFNs, IL-1β, and IL-6, which directly impede viral replication [1].
NLRP3 Inflammasome: The NLRP3 inflammasome plays a crucial role in the activation of caspase-1, which subsequently processes pro-IL-1β and pro-IL-18 into their active forms [1]. This pathway represents another important mechanism contributing to the cytokine cascade observed in CS.
Table 1: Key Cytokines in Cytokine Storm Pathology
| Cytokine | Primary Source | Major Functions | Role in Organ Injury |
|---|---|---|---|
| IL-6 | Macrophages, T cells | Fever, acute phase response, B-cell activation | Lung injury, ARDS, cardiac dysfunction |
| TNF-α | Macrophages, monocytes | Endothelial activation, fever, cachexia | Vascular leakage, hypotension, renal injury |
| IL-1 | Macrophages, monocytes | T-cell activation, fever, prostaglandin synthesis | Cardiomyocyte dysfunction, vascular instability |
| IFN-γ | T cells, NK cells | Macrophage activation, antigen presentation | Hematopoietic suppression, liver damage |
Mechanisms of Multiple Organ Dysfunction
The pathologic process of MODS comprises two phases [81]. In the early phase, overproduction of numerous inflammatory mediators results in leukocyte/endothelial cell activation, increased endothelial permeability, and polymorphonuclear neutrophil (PMN) adhesion and migration. Inflammatory cells in the spleen, liver, and bloodstream produce the first cytokine storm [81]. When an initial infective or physical insult triggers the release of proinflammatory cytokines including IL-1β, tumor necrosis factor (TNF)-α, and IL-6, a systemic inflammatory response syndrome (SIRS) develops. If this inflammatory response is severe enough, it may lead to the clinical manifestations of MODS [81].
The progression of organ dysfunction follows recognizable patterns, mostly affecting gastrointestinal, lung, liver, kidney, and heart systems in sequence [81]. The difference in constitutive expression and the upregulation of adhesion molecules in vascular beds, plus the density and potency of intrinsic inflammatory cells in different organs, are key factors determining the sequence and severity of organ dysfunction [81]. Through activating intrinsic inflammatory cells in distant organs, organ dysfunctions become linked in a positive feedback loop through circulating inflammatory mediators [81].
Economic Barriers to Biologic Therapies
The High Cost of Biologic Drugs
Biologic drugs used to treat CS-related conditions represent a substantial economic burden on healthcare systems:
- Biologic drugs can cost patients tens of thousands to hundreds of thousands of dollars annually, creating insurmountable financial barriers for many Americans who need these life-saving treatments [80].
- Despite representing only 5% of prescriptions in the U.S., biologics account for 51% of total drug spending as of 2024 [80] [82].
- High prescription costs lead to treatment abandonment, with patients rationing doses, skipping treatments, or going without medication entirely, resulting in disease progression, hospitalizations, and worse health outcomes [80].
The investment required to develop and market a biosimilar is considerably higher than the $1-4 million required in the generic market. It takes 7-8 years to develop a biosimilar, at a cost between $100 million and $250 million [83]. The complexity of monoclonal antibodies makes their development and manufacturing costs much higher than for other biosimilars [83].
Table 2: Biosimilar Development and Economic Impact
| Parameter | Data | Source/Context |
|---|---|---|
| Development Time | 7-8 years | [83] |
| Development Cost | $100-$250 million | [83] |
| FDA-approved biosimilars | 76 | As of 2024 [80] |
| EMA-approved biosimilars | 110 | As of 2024 [80] |
| Average price reduction | 50% vs. reference product | At launch [80] |
| Total healthcare savings | $56 billion since 2015 | U.S. savings [80] |
Biosimilars as a Cost-Saving Solution
Biosimilars are defined as "highly similar" to a branded reference product, with "no clinically meaningful differences between the biological product and the reference product in terms of safety, purity, and potency" [83]. These complex medications treat serious conditions including cancer, autoimmune diseases, and rare disorders that affect millions of Americans [80].
The Biologics Price Competition and Innovation Act (BPCIA) of 2009 provides a pathway for biosimilar competition, analogous to the Hatch-Waxman Act for generics [83]. The BPCIA provides a 12-year market exclusivity and a 4-year data exclusivity period for innovator biologics, beginning when the biologic drug receives FDA marketing approval [83]. A biosimilar cannot be marketed until the 12-year exclusivity expires.
The European experience with biosimilars demonstrates both opportunities and challenges. The first biosimilar was approved in the EU in 2006 [83]. However, the EU market remains relatively small, with only 16 biosimilars approved in 3 classes representing approximately 11% of the total patient volume and approximately 18% of all biologic sales [83]. For the year ending June 2011, biosimilars accounted for approximately 10% of the available market, and make up <1% of the total biologic sales in the EU [83]. Biosimilar prices in the EU have been on average approximately 30% less expensive than their reference products [83].
Regulatory Modernization Efforts
The FDA has recently implemented measures to accelerate biosimilar development:
- Eliminating unnecessary clinical trials - Using improved analytical testing methods instead of requiring expensive human studies when the science shows they're not needed [80] [82]. The FDA's review of accumulated data since 2015 suggests that traditional comparative efficacy trials often provide limited additional insight beyond advanced analytical and functional assays [82].
- Facilitating pharmacy-level substitution - Removing barriers by advancing interchangeability so pharmacists can substitute lower-cost biosimilars, just like they do with generic drugs [80].
- Reducing regulatory barriers - Providing clearer guidance and more efficient processes to speed up approvals and reduce development uncertainty [80].
The FDA no longer generally recommends "switching studies" for biosimilars seeking interchangeability status, bringing biosimilar regulation closer to the generic drug model [82].
ICU Infrastructure and Capacity Challenges
Physical Infrastructure Limitations
ICU infrastructure limitations significantly impact the capacity to manage patients with MODS secondary to CS:
Physical Space Constraints: ICUs are often stressful, noisy, and crowded workplaces [84]. The form and layout, especially concerning the location of the nursing station (centralized, decentralized, or hybrid), significantly impact functionality [84]. During COVID-19, the transformation of non-critical care beds into temporary ICU spaces was a necessary but suboptimal response to capacity limitations [85].
Brazilian Regulatory Framework: Regulation RDC 50/2002 sets requirements for ICUs such as those related to the size of spaces [84]. This regulation specifies that beds should be placed at least 1.0 m away from the lateral walls, and at least 1.2 m from the back wall—dimensions corresponding to an overall patient room of approximately 10 m² [84]. These size requirements differ significantly from those in developed countries; for example, the size of ICU patient rooms in the U.S. should be at least 18 m² [84].
Electricity Supply Infrastructure: Regulation RDC 50/2002 requires an independent, emergency electricity network for three ICU spaces: nursing station, medical prescription room, and patient room [84]. The same regulation defines the maximum tolerable recovery time in case of power outages—equipment for mechanical ventilation must be automatically reactivated by an emergency power source in no more than 15 seconds when there is a drop of 10% or more of the nominal voltage, being available for at least 24 hours [84].
Oxygen Supply Challenges: During the pandemic, oxygen supply infrastructure was severely stressed in multiple countries [84]. Brazilian standard NBR 12,188/2016 posits that, in ICUs, designers should consider that at least 80% of the points of oxygen use will be working concurrently [84]. ICUs must maintain an emergency reserve storage, independent of the central reserve storage for the hospital as a whole [84].
Air Treatment Infrastructure: This is crucial for infection prevention as viruses can be transmitted through aerosols and travel fairly large distances through the air [84]. HVAC utilities of ICUs must be connected to an electrical circuit of emergency, highlighting the relationships between infrastructures [84].
Human Resource Constraints
The availability of trained ICU staff represents a critical limitation in managing CS and MODS:
- Skewed availability of critical care experts: India has only 5000 intensivists or ICU doctors whose presence is more or less saturated across urban centers, leaving most of the population with little to no access [86].
- Need for constant upskilling: Delivery of critical care is challenging and complex, requiring doctors and nurses with skills to rapidly assess and manage complex patients [86].
- Clinician burnout: The overwhelming nature of working in high-pressure ICU situations often leads to burnout of doctors and nurses, further reducing capacity [86].
During the COVID-19 pandemic, redeployment of staff to ICUs and critical care units became a core element of the response in many countries including Ireland [85]. However, redeployed nursing staff experienced significant stress and anxiety, requiring rapid upskill training programs to equip them for ICU deployment [85]. Training varied in length and content, focusing on essential skills such as mechanical ventilation, infection prevention and control, patient monitoring, and proning [85].
Table 3: ICU Infrastructure Slack Resources and Requirements
| Infrastructure Component | Regulatory Requirements | Slack Resources | Implementation Challenges |
|---|---|---|---|
| Physical Space | 10 m² per bed (Brazil), 18 m² per bed (U.S.) | Converted non-ICU spaces, expanded capacity | Suboptimal workflow, visibility issues |
| Electricity Supply | 15s recovery time for mechanical ventilation | Emergency generators, redundant circuits | Fuel supply maintenance, load management |
| Oxygen Supply | 80% concurrent use factor, emergency reserve | Additional tanks/cylinders, portable concentrators | Storage safety, distribution pressure |
| Air Treatment | Emergency circuit for HVAC | HEPA filtration upgrades, pressure monitoring | Airflow management, infection control |
Research Reagents and Methodologies
Essential Research Reagents
The following research reagents are fundamental to CS and MODS investigation:
- Recombinant Cytokines and Antagonists: Essential for establishing in vitro and in vivo CS models. IL-6, TNF-α, IL-1, and IFN-γ are crucial for simulating the cytokine storm environment [79] [1].
- JAK-STAT Pathway Inhibitors: Small molecule inhibitors targeting JAK1, JAK2, JAK3, and TYK2 are critical for evaluating signaling pathway contributions to CS pathogenesis [1].
- TLR Agonists/Antagonists: Tools for modulating pattern recognition receptor activation, which plays a significant role in infection-induced CS [1].
- Neutralizing Antibodies: Anti-IL-6R (tocilizumab), anti-TNF (infliximab), and anti-IL-1 biologics represent both therapeutic agents and research tools [79] [83].
- Flow Cytometry Panels: Multiplexed antibody panels for immune cell phenotyping (macrophages, T cells, neutrophils) and activation status assessment during CS [79].
- Cytokine Detection Assays: ELISA, Luminex, or ELISA-based methods for quantifying circulating cytokine levels in patient serum or experimental models [79] [1].
Experimental Protocols for CS Investigation
In Vitro Immunocyte Activation Assay:
- Isolate PBMCs from healthy donors or patient samples using density gradient centrifugation
- Culture cells in 24-well plates (1×10^6 cells/well) with RPMI-1640 supplemented with 10% FBS
- Stimulate with TLR agonists (LPS, 100 ng/mL) or specific antigenic triggers for 24-48 hours
- Collect supernatant for cytokine profiling via multiplex immunoassay
- Analyze cell surface activation markers (CD69, CD25, HLA-DR) via flow cytometry
- Inhibitor studies: pre-treat cells with JAK inhibitors (1-10 μM) or neutralizing antibodies (10 μg/mL) 1 hour prior to stimulation
In Vivo Cytokine Storm Modeling:
- Utilize transgenic mouse models expressing human ACE2 or immune signaling components
- Administer disease-specific triggers (viral mimics, CAR-T cells, TLR agonists) via appropriate routes
- Monitor clinical symptoms (activity, fur ruffling, weight loss) twice daily
- Collect serial blood samples for cytokine measurement (IL-6, TNF-α, IFN-γ, IL-1β)
- Assess organ function through physiological monitoring (pulse oximetry, blood pressure)
- Terminate experiment at predetermined endpoints for histopathological analysis
Endothelial Barrier Function Assessment:
- Culture endothelial cell monolayers (HUVEC or lung microvascular endothelial cells) on transwell inserts
- Measure transendothelial electrical resistance (TEER) using volt-ohm meter
- Treat with patient serum or recombinant cytokines (IL-6, TNF-α) with/without inhibitors
- Assess permeability using fluorescent dextran tracer (40-70 kD)
- Analyze junctional protein expression (VE-cadherin, ZO-1) via immunofluorescence
Integrated Analysis and Future Directions
The management of CS and MODS requires a multidisciplinary approach that addresses both therapeutic and infrastructural challenges. Targeting key signaling pathways, including JAK-STAT, TLRs, neutrophil extracellular traps, and NLRP3 inflammasome, represents promising therapeutic avenues [1]. Therapies targeting these pathways have been developed or are under investigation, with novel drugs demonstrating promising efficacy in mitigating CS [1].
The regulatory modernization of biosimilar approval processes presents significant opportunities to reduce economic barriers to biologic therapies. By eliminating unnecessary clinical trials, facilitating pharmacy-level substitution, and reducing regulatory barriers, the FDA aims to foster competition and drive down costs without compromising safety or effectiveness [80] [82]. Since 2015, biosimilars have generated an estimated $56 billion in US healthcare savings, including $20 billion in 2024 alone, demonstrating their significant economic impact [80].
For ICU infrastructure, the concept of "slack resources" represents a critical consideration for resilient healthcare system design [84]. Slack is defined as "a cushion of actual or potential resources which allows an organization to adapt successfully to internal pressures for adjustment or to external pressures for change in policy" [84]. These resources can take many forms including financial reserves, extra space, surplus of materials, workers on standby, redundant equipment, and generous time margins [84]. The pandemic dramatically demonstrated the value of investing in slack resources, creating momentum for this discussion in health services [84].
Technology-enabled solutions such as Smart-ICUs show promise for addressing resource constraints. A Smart-ICU setup connects to a central unit with clinicians who manage patients 24/7, utilizing ultra-high definition cameras capable of capturing granular details about patients, their vitals, and other necessary information [86]. This allows remotely located super-specialist trained doctors and nurses to amplify their reach and support patients irrespective of location and time of day [86].
The pathophysiological mechanisms of CS-induced organ injury involve cytokines inducing cell injury and endothelial dysfunction, leading to vascular leakage and nonprogrammed cell death [79]. Through repeated comparison, researchers have found that several cytokines, including IL-1, IL-6, TNF-α, and IFN-γ, always coexist and are critical to CS caused by infection or immunotherapy [79]. When exposure to external stimulus is continuous, positive feedback always exists while negative feedback mechanisms are insufficiently activated, resulting in cascade amplification and continuous positive feedback that brings about immune system overactivation [79].
Future research directions should focus on:
- Advanced biosimilar development for cytokine-targeted therapies to reduce costs
- Resilient ICU design incorporating appropriate slack resources for surge capacity
- Novel CS biomarkers for early detection and intervention before MODS establishment
- Personalized immunomodulation strategies based on individual patient cytokine profiles
- Tele-critical care expansion to extend specialist expertise to underserved areas
Cytokine Storm Signaling Pathways: This diagram illustrates the key pathophysiological mechanisms in cytokine storm development, from initial insult through immune activation, signaling pathway engagement, cytokine release, and eventual organ dysfunction. The dashed lines represent positive feedback loops that perpetuate the inflammatory cascade.
Economic and Access Barrier Relationships: This diagram illustrates the interconnected challenges in biologic therapy access and ICU infrastructure, showing how economic barriers, infrastructure limitations, and patient impacts relate to each other, along with potential solution pathways indicated by dashed lines.
Algorithm Development for Patient Stratification and Therapy Timing
The management of cytokine storm syndrome (CSS), a life-threatening systemic inflammatory condition, presents a significant challenge in critical care and immunotherapy. This whitepaper provides a comprehensive technical framework for developing computational algorithms to stratify patients based on CSS risk and optimize therapeutic timing. By integrating multi-omics data, clinical parameters, and machine learning approaches, we outline methodologies for identifying distinct patient endotypes, predicting disease progression toward multiple organ dysfunction syndrome (MODS), and pinpointing critical intervention windows. Within the broader context of cytokine storm and multiple organ failure mechanisms research, these algorithms enable a paradigm shift from reactive treatment to preemptive precision medicine, potentially improving survival outcomes in conditions such as sepsis, CAR-T cell therapy, and severe COVID-19.
Cytokine storm (CS) is a severe systemic inflammatory syndrome characterized by excessive immune cell activation and dangerously elevated circulating cytokine levels. This dysregulated host response can precipitate life-threatening conditions including fulminant myocarditis, acute respiratory distress syndrome (ARDS), hemophagocytic lymphohistiocytosis (HLH), and multiple organ dysfunction syndrome (MODS) [1]. The significant involvement of specific signaling pathways—particularly JAK-STAT, Toll-like receptors (TLRs), neutrophil extracellular traps (NETs), and the NLRP3 inflammasome—has been recognized in CS pathogenesis [1]. The clinical imperative for advanced algorithms stems from the high mortality rates associated with CS and its heterogenous presentation across patient populations, necessitating stratification tools that can guide targeted therapies against these specific pathways.
The development of predictive algorithms for patient stratification and therapy timing represents a critical frontier in immunology and computational medicine. Such tools are particularly valuable for managing cytokine release syndrome (CRS) associated with emerging immunotherapies like chimeric antigen receptor T-cell (CAR-T) therapy, where early identification of high-grade CRS can guide timely intervention with immunomodulators [87]. Similarly, in sepsis and severe infections, algorithms that stratify patients based on their programmed cell death (PCD) patterns and immune profiles can identify those at highest risk for deterioration, enabling preemptive organ support and personalized immunomodulation [88].
Key Signaling Pathways in Cytokine Storm Pathogenesis
Understanding the core molecular pathways driving cytokine storms is fundamental to identifying therapeutic targets and developing meaningful stratification biomarkers. The following pathways represent prime candidates for integration into algorithmic prediction models.
JAK-STAT Signaling Pathway
The JAK-STAT pathway serves as a central signaling hub for numerous cytokines implicated in CS. This pathway comprises transmembrane receptors, receptor-associated Janus kinases (JAK1, JAK2, JAK3, TYK2), and signal transducers and activators of transcription (STAT1-6) [1]. IL-6, a pivotal cytokine in CS, activates STAT3 through both membrane-bound and soluble IL-6 receptors, initiating a cascade that promotes the secretion of additional mediators including IL-1β, IL-8, CCL2, CCL3, CCL5, GM-CSF, and VEGF [1]. TNF and IFN-γ also activate JAK1, leading to STAT phosphorylation and expression of inflammation-related genes. The overactivation of this pathway has been documented as a key driver in HLH, CAR-T associated CRS, COVID-19, and fulminant myocarditis [1].
Figure 1: JAK-STAT Signaling Pathway in Cytokine Storm
Toll-like Receptor (TLR) Pathway
Toll-like receptors represent a primitive class of pattern recognition receptors that detect pathogen-associated molecular patterns (PAMPs) and damage-associated molecular patterns (DAMPs). Expressed on immune cells like monocytes, macrophages, and dendritic cells, TLR activation initiates the production of pro-inflammatory cytokines and type I IFNs as part of the anti-pathogen response [1]. However, excessive TLR signaling can trigger deleterious effects through uncontrolled cytokine production, contributing to the CS cascade. This pathway is particularly relevant in infection-driven hyperinflammation, such as that observed in severe COVID-19 and bacterial sepsis [1].
Computational Framework for Patient Stratification
Data Acquisition and Preprocessing
Robust algorithm development begins with comprehensive data acquisition from multiple modalities. Key data sources include:
- Transcriptomic Data: Microarray or RNA-seq data from peripheral blood mononuclear cells (PBMCs) or whole blood, focusing on cytokine gene expression patterns (e.g., IL1B, IL-2, IL-6, IFN-γ, TGFβ) and programmed cell death (PCD) signatures [70] [88].
- Clinical Parameters: Vital signs (SpO2, diastolic blood pressure), coagulation profiles (D-dimer, INR), inflammatory markers (CRP, ferritin), and organ function assessments [87] [70].
- Demographic and Comorbidity Data: Age, sex, comorbidities (diabetes, hypertension, multimorbidity), and vaccination status [70].
Data preprocessing should address missing values using robust imputation methods. The non-parametric missForest algorithm, which applies random forest regression for continuous variables and classification trees for categorical variables, has demonstrated effectiveness in CRS prediction studies [87]. Iterative imputation should continue until normalized root mean squared error (NRMSE) stabilizes, ensuring reliable estimates.
Feature Selection and Model Development
Feature selection techniques must identify variables most predictive of CS severity and progression. Effective approaches include:
- Univariate Cox Regression: Identifies prognostic variables significantly associated with disease aggravation, calculating hazard ratios (HRs) with 95% confidence intervals (CIs) to quantify impact [87].
- LASSO (Least Absolute Shrinkage and Selection Operator) Regression: Applies L1 penalty to shrink coefficients, performing variable selection while reducing overfitting [88]. Optimal lambda values can be determined via ten-fold cross-validation.
- Recursive Feature Elimination (RFE): Iteratively constructs models and eliminates the weakest features until optimal feature subset is identified [89].
Multiple machine learning algorithms can be evaluated for stratification performance:
- XGBoost (Extreme Gradient Boosting): Has demonstrated superior performance in predicting high-grade CRS, with identified key predictors including SpO2, D-dimer, diastolic blood pressure, and INR [87].
- Random Forest: Constructs multiple decision trees and aggregates predictions, effective for handling high-dimensional data.
- Support Vector Machines (SVM): Useful for finding optimal separation boundaries in complex feature spaces.
Figure 2: Computational Workflow for Patient Stratification
Stratification Based on Programmed Cell Death Patterns
Comprehensive analysis of programmed cell death (PCD) patterns provides a powerful approach for patient stratification in inflammatory conditions like sepsis. Methodology includes:
- PCD Signature Profiling: Quantify activity scores of 14 PCD patterns (apoptosis, pyroptosis, necroptosis, ferroptosis, netotic cell death, immunogenic cell death, alkaliptosis, mitotic cell death, oxeiptosis, MPT-driven necrosis, parthanatos, cuproptosis, entotic death, and autophagy-dependent death) from transcriptomic data [88].
- Consensus Clustering: Apply ConsensusClusterPlus R package to identify molecular subtypes based on PCD activity scores, determining optimal cluster number using cumulative distribution function (CDF) curves and delta-area plots [88].
- Differential Expression Analysis: Identify differentially expressed genes (DEGs) between clusters using limma package with empirical Bayes moderation, applying Benjamini-Hochberg false discovery rate (FDR < 0.05) for multiple testing correction [88].
- Prognostic Model Development: Construct a PCD-related gene signature (e.g., ELANE, CTSG, MPO, CAMP, TFRC, IL1B, CASP5) using LASSO Cox regression, then validate across independent datasets [88].
Table 1: Key Cytokines in Cytokine Storm Stratification
| Cytokine | Biological Function | Stratification Utility | Detection Methods |
|---|---|---|---|
| IL-6 | Activates JAK-STAT3 pathway, induces acute phase reactants | Primary predictor of severe CRS in CAR-T therapy and COVID-19 | Electrochemiluminescence immunoassay (ECLIA), qRT-PCR gene expression |
| IFN-γ | Potent macrophage activator, enhances antigen presentation | Inverse association with COVID-19 severity when measured via gene expression | Multiplex qRT-PCR, bead-based immunoassay |
| IL-2 | T-cell growth and differentiation factor | Lower gene expression in severe COVID-19 | Multiplex qRT-PCR, ELISpot |
| D-dimer | Fibrin degradation product, marker of coagulation activation | Predictive of high-grade CRS in CAR-T and COVID-19 | Routine autoanalyzer assays |
| IL-1β | Pyroptosis mediator, fever induction | Component of PCD-related prognostic signatures in sepsis | Multiplex qRT-PCR, electrochemiluminescence |
Experimental Protocols for Algorithm Validation
Cytokine Gene Expression Profiling Using Multiplex qRT-PCR
Purpose: To quantify cytokine gene expression levels as early biomarkers for severe disease [70].
Materials:
- EDTA-blood samples collected at defined timepoints (e.g., Day 5 of infection)
- RNA extraction kit (e.g., PAXgene RNA system)
- SYBR-Green master mix
- Real-time thermocycler with multiplex capability
- Fluorophore-tagged primers for target genes (IL-1β, IL-2, IL-6, TGFβ, IFN-γ) and housekeeping gene (β-Actin)
Procedure:
- RNA Extraction and Quantitation: Extract total RNA from EDTA-blood samples following manufacturer protocols. Assess RNA quality and quantity using spectrophotometry.
- Primer Design: Utilize validated primer sequences as detailed in Table 1.
- qRT-PCR Reaction Setup: Prepare reactions with SYBR-Green master mix, specific primers, and RNA template.
- Thermal Cycling: Conduct amplification with the following conditions:
- Enzyme activation: 42°C for 5 minutes
- 40 cycles of:
- Denaturation: 95°C for 10 seconds
- Annealing/extension: 60°C for 20 seconds
- Final extension: 65°C for 15 seconds
- Data Analysis: Calculate cytokine gene expression using the 2^(-ΔΔC_T) method normalized to β-Actin [70].
Machine Learning Model Development and Validation
Purpose: To develop and validate a predictive model for high-grade cytokine release syndrome [87].
Materials:
- Clinical dataset from confirmed CRS patients (n ≥ 400 recommended)
- R or Python programming environment with machine learning libraries (glmnet, randomForest, XGBoost, scikit-learn)
- Computational resources for cross-validation and hyperparameter tuning
Procedure:
- Data Preprocessing:
- Impute missing values using missForest algorithm with 100 trees per forest and maximum of 10 iterations
- Randomly split dataset into training (80%) and testing (20%) sets with stratification by outcome
- Normalize continuous variables using z-score standardization
Feature Selection:
- Perform univariate Cox regression analyses within predefined subgroups
- Calculate hazard ratios (HRs) with 95% confidence intervals
- Retain features with p < 0.05 for multivariate modeling
Model Construction:
- Train multiple algorithms (Lasso regression, Random Forest, XGBoost) using training set
- Optimize hyperparameters using GridSearchCV with cross-validation
- Select best-performing model based on discrimination metrics
Model Interpretation:
- Apply SHapley Additive exPlanations (SHAP) to quantify feature contributions
- Generate receiver operating characteristic (ROC) curves and calculate area under curve (AUC)
- Determine optimal prediction cutoffs using Youden Index
Validation:
- Assess model performance on held-out test set
- Externally validate using independent patient cohort when available
- Evaluate calibration and clinical utility via decision curve analysis
Table 2: Machine Learning Performance in CRS Prediction
| Algorithm | AUC | Key Predictors Identified | Clinical Application |
|---|---|---|---|
| XGBoost | >0.90 | SpO2, D-dimer, diastolic BP, INR | High-grade CRS prediction post-CAR-T therapy |
| Random Forest | 0.85-0.89 | IL-6, ferritin, respiratory rate | Sepsis mortality risk stratification |
| LASSO Regression | 0.82-0.87 | PCD-related genes (ELANE, IL1B, CASP5) | Sepsis subphenotyping and outcome prediction |
| Support Vector Machine | 0.80-0.85 | Age, comorbidities, cytokine levels | General critical illness prognostication |
Table 3: Key Research Reagent Solutions for Cytokine Storm Studies
| Reagent/Resource | Function/Application | Example Specifications |
|---|---|---|
| Multiplex qRT-PCR Primers | Simultaneous detection of multiple cytokine gene expressions | SYBR-Green fluorophore tags; validated primers for IL-1β, IL-6, IL-2, IFN-γ, TGFβ, β-Actin |
| Electrochemiluminescence Immunoassay (ECLIA) | Quantitative measurement of cytokine protein levels | High-sensitivity kits for IL-6, IL-1β, TNF-α; requires specific instrumentation |
| RNA Preservation Systems | Stabilization of blood transcriptome | PAXgene Blood RNA Tubes; maintain cold chain (4°C) during storage and transport |
| ConsensusClusterPlus R Package | Molecular subtyping via consensus clustering | Implements multiple clustering algorithms; generates CDF curves for cluster stability assessment |
| missForest R Package | Non-parametric missing value imputation | Uses random forests; handles mixed data types; outputs NRMSE for imputation accuracy |
| SHAP (SHapley Additive exPlanations) | Model interpretation and feature importance visualization | Quantifies contribution of each feature to individual predictions; compatible with XGBoost |
Application to Therapy Timing and Clinical Decision Support
Algorithmic approaches can significantly enhance therapy timing by identifying critical windows for intervention. Temporal transcriptomic analyses reveal that prognostic genes in sepsis peak in bone marrow and peripheral blood within three days post-onset, suggesting an early therapeutic window for targeted interventions [88]. In CAR-T therapy, monitoring specific clinical parameters (SpO2, D-dimer, diastolic pressure, INR) at days 4, 7, and 10 post-infusion enables prediction of high-grade CRS before clinical deterioration [87].
The integration of these algorithms into clinical workflows provides decision support for:
- Targeted Immunomodulation: Identifying patients with JAK-STAT hyperactivation who may benefit from JAK inhibitors (e.g., in HLH, CAR-T CRS, or COVID-19) [1].
- Personalized Anticipatory Management: Allocating higher-intensity monitoring resources to patients stratified as high-risk based on PCD signatures or clinical biomarker profiles.
- Temporal Optimization of Interventions: Administering therapies during windows of maximal target expression or pathway activity, such as early immunomodulation in sepsis when PCD-related genes show peak expression [88].
Algorithm development for patient stratification and therapy timing represents a transformative approach to managing cytokine storm syndromes and preventing multiple organ failure. By integrating multi-dimensional data from transcriptomics, clinical parameters, and programmed cell death patterns, these computational tools enable precise identification of at-risk patients and optimal intervention timing. The methodologies outlined—from consensus clustering based on PCD patterns to machine learning prediction of CRS severity—provide a robust technical foundation for implementation. As validation in larger prospective cohorts continues, these algorithms hold promise for fundamentally improving outcomes in critical care, immunotherapy, and inflammatory disease management through data-driven precision medicine.
Cytokine storm (CS) represents a life-threatening systemic inflammatory syndrome characterized by immune hyperactivation and significantly elevated circulating cytokines, driving severe organ dysfunction across diverse clinical conditions [1]. Despite differing inciting events—pathogenic infection in sepsis, engineered cellular therapies in Chimeric Antigen Receptor T-cell (CAR-T) Cytokine Release Syndrome (CRS), and viral invasion in COVID-19—these etiologies converge on a common pathophysiological axis of cytokine dysregulation [90] [91] [92]. This dysregulation manifests as a self-amplifying loop of pro-inflammatory mediator release, leading to endothelial injury, coagulopathy, and ultimately, multiple organ failure [67] [93]. Understanding the shared and distinct mechanisms underlying these syndromes is paramount for developing targeted, effective immunomodulatory strategies. This review synthesizes the current evidence on the pathogenesis, quantitative cytokine profiles, and therapeutic approaches for CS across these three critical illnesses, providing a framework for cross-disciplinary application of emerging therapies.
Core Pathogenic Mechanisms and Signaling Pathways
The initiation of CS, while triggered by different stimuli, follows a recognizable sequence of immune recognition, inflammatory amplification, and ultimately, tissue injury.
Initial Immune Recognition and Activation
The CS cascade begins with the recognition of threat signals by pattern recognition receptors (PRRs) on innate immune cells:
- In sepsis, pathogen-associated molecular patterns (PAMPs) from bacteria or fungi and damage-associated molecular patterns (DAMPs) from injured host tissues engage PRRs like Toll-like receptors (TLRs) and NOD-like receptors (NLRs) [90] [93]. This engagement triggers intracellular phosphorylation cascades, primarily via the NF-κB and MAPK pathways, culminating in the transcriptional activation of pro-inflammatory cytokines [90] [67].
- In COVID-19, SARS-CoV-2 infection leads to ACE-2 receptor downregulation, disrupting angiotensin signaling and promoting an initial inflammatory milieu. The subsequent suppression of early interferon (IFN) responses allows for unchecked viral replication and eventual excessive pyroptosis, a pro-inflammatory form of cell death [92].
- In CAR-T CRS, the instigating event is the recognition of tumor antigens by infused CAR-T cells. Their activation and massive proliferation in vivo trigger the release of cytokines like GM-CSF and IL-2, which in turn activate bystander immune cells such as monocytes and macrophages, leading to the dramatic outpouring of additional cytokines [94] [91].
Key Signaling Pathways in Cytokine Storm Amplification
Following initial activation, several key signaling pathways serve as central amplifiers of the inflammatory response.
Diagram 1: Core signaling pathways in cytokine storm. The JAK-STAT and inflammasome pathways are central amplifiers of inflammation. The JAK-STAT pathway transduces signals from extracellular cytokines to drive the transcription of inflammatory genes. Concurrently, inflammasome activation processes key cytokines and induces pyroptotic cell death, releasing more DAMPs and creating a self-amplifying loop.
- JAK-STAT Pathway: This is a primary signaling node for numerous cytokines. Upon cytokine binding (e.g., IL-6), associated JAK proteins are activated and phosphorylate STAT proteins. Phosphorylated STATs dimerize, translocate to the nucleus, and drive the transcription of genes encoding pro-inflammatory mediators, including cytokines themselves, creating a feed-forward loop [1]. This pathway is critically implicated in the CS of CAR-T CRS, COVID-19, and sepsis [1].
- Inflammasome Activation: Intracellular sensors like NLRP3 form inflammasome complexes in response to PAMPs, DAMPs, or cellular stress. These complexes activate caspase-1, which cleaves pro-IL-1β and pro-IL-18 into their active, potent forms. Caspase-1 also cleaves gasdermin D, leading to pyroptosis—an inflammatory cell death that releases more DAMPs, perpetuating the cycle [90] [67]. This mechanism is prominent in COVID-19 and sepsis [67] [92].
- Inflammatory Cell Death Crosstalk: In severe inflammation, crosstalk between pyroptosis, apoptosis, and necroptosis can occur, leading to a synergistic pro-inflammatory cell death pathway termed panoptosis. This is particularly observed in sepsis and contributes to the release of a wide array of DAMPs, further fueling the cytokine storm [67].
Comparative Quantitative Profiling of Cytokine Elevations
A detailed comparison of cytokine levels reveals both shared and distinct patterns, informing targeted therapeutic choices.
Table 1: Comparative Cytokine Profiles Across Sepsis, CAR-T CRS, and Severe COVID-19
| Cytokine / Mediator | Role in Pathogenesis | Sepsis | CAR-T CRS | Severe COVID-19 | Key Comparisons |
|---|---|---|---|---|---|
| IL-6 | Master regulator of acute phase response; activates JAK-STAT3 [1]. | Markedly elevated [67]. | Prominently elevated; key therapeutic target [91]. | Elevated; pooled mean in severe/critical: ~37 pg/mL [95]. | Levels in sepsis and CAR-T CRS are often substantially higher than in COVID-19 [95]. |
| TNF-α | Early pro-inflammatory cytokine; drives endothelial activation [93]. | Key driver of SIRS and tissue injury [67]. | Elevated and implicated in pathogenesis [94]. | Elevated and linked to worse outcomes [96]. | A core early-phase cytokine across all three etiologies. |
| IL-1β | Potent pyrogen; activated by inflammasomes; promotes lymphocyte activation [90]. | Central mediator released via pyroptosis [67]. | Elevated [94]. | Elevated; IL-1β/IFN-α ratio is a proposed severity marker [96]. | Key product of inflammasome activation, prominent in COVID-19 and sepsis. |
| IFN-γ | Polarizes Th1 responses; activates macrophages [1]. | Elevated, contributes to macrophage activation [67]. | Elevated and a key mediator [94]. | Levels not always significantly different from mild cases [96]. | Highly characteristic of CAR-T CRS and HLH-like syndromes. |
| IL-10 | Anti-inflammatory cytokine; induces immunosuppression [90]. | Markedly elevated in CARS phase [90]. | Elevated [91]. | Elevated as a counter-regulatory response [96]. | Signifies the compensatory anti-inflammatory response, often following initial hyperinflammation. |
| IL-8 (CXCL8) | Neutrophil chemoattractant [93]. | Elevated, contributes to neutrophil recruitment and NETosis [93]. | Elevated [91]. | Significantly elevated in critical patients [96]. | Marker of neutrophil activation and recruitment, common to all. |
| IL-2 | T-cell growth factor [1]. | Elevated [96]. | Elevated due to T-cell activation [94]. | Early rise linked to worse outcomes [96]. | Particularly relevant in T-cell driven pathologies like CAR-T CRS. |
| sIL-2R | Marker of T-cell and macrophage activation [1]. | -- | -- | -- | A key biomarker in HLH and severe CRS. |
Table 2: Comparison of Non-Cytokine Biomarkers and Clinical Scores
| Biomarker / Score | Application in Sepsis | Application in CAR-T CRS | Application in COVID-19 | Clinical Utility |
|---|---|---|---|---|
| Ferritin | Extremely high levels in secondary HLH/MAS [67]. | Extremely high levels in severe CRS/HLH [94]. | Elevated to similar/greater extent than in sepsis or ARDS [95]. | Marker of extreme hyperinflammation and HLH-like manifestations. |
| CRP | Standard acute phase reactant [67]. | Elevated [91]. | Elevated to similar/greater extent than in sepsis or ARDS [95]. | General marker of systemic inflammation. |
| D-dimer | Marker of coagulation activation; prognostic in septic shock [93]. | -- | Elevated to similar/greater extent than in sepsis or ARDS [95]. | Indicator of endothelial injury and thrombotic microangiopathy. |
| Monocyte Distribution Width (MDW) | Promising early sepsis biomarker (cutoff ~23.5) [67]. | -- | -- | Early detection of sepsis in emergency settings. |
| SOFA / qSOFA | Diagnostic and prognostic scoring [90]. | -- | Used for assessing organ dysfunction [90]. | Quantifies organ dysfunction severity. |
| HScore / MS Score | -- | Used for CRS/HLH assessment [1]. | Used for CRS/HLH assessment [1]. | Evaluates probability of HLH/cytokine storm. |
| CTCAE Grading | -- | Standard for CRS grading [1]. | -- | Standardizes adverse event reporting for therapies. |
The Scientist's Toolkit: Essential Research Reagents and Models
Advancing the understanding and treatment of cytokine storms relies on a suite of specialized research tools and experimental models.
Table 3: Key Research Reagent Solutions for Cytokine Storm Investigation
| Reagent / Model Category | Specific Examples | Research Application | Key Function |
|---|---|---|---|
| Cytokine Targeting Agents | Tocilizumab (anti-IL-6R), Siltuximab (anti-IL-6), Anakinra (IL-1Ra) [1] [91]. | In vivo and ex vivo testing of cytokine pathway blockade. | Neutralizes specific cytokines or their receptors to dissect their pathogenic role. |
| Small Molecule Inhibitors | JAK inhibitors (e.g., Ruxolitinib), Caspase inhibitors, RIPK inhibitors [1]. | Mechanistic studies of intracellular signaling and cell death pathways. | Inhibits key nodes in JAK-STAT, pyroptosis, and necroptosis pathways. |
| In Vitro Cellular Models | Primary human immune cells (monocytes, T-cells), CAR-T co-culture systems, Endothelial cell cultures [91] [92]. | Study of cell-cell interactions, cytokine release, and endothelial activation. | Models specific cellular interactions driving CRS in a controlled environment. |
| In Vivo Animal Models | LPS-induced endotoxemia, Cecal Ligation and Puncture (CLP) for sepsis, SARS-CoV-2 infected models, CAR-T CRS xenograft models [67]. | Preclinical assessment of pathogenesis and therapeutic efficacy. | Recapitulates the complex, systemic physiology of cytokine storm. |
| Biomarker Assays | Multiplex cytokine arrays (Luminex), ELISA for ferritin/D-dimer, Flow cytometry for immune phenotyping (e.g., HLA-DR) [96] [67]. | Patient stratification, pharmacokinetic/pharmacodynamic studies, and prognostic assessment. | Quantifies cytokine levels and immune cell status for diagnostic and research purposes. |
Detailed Experimental Protocol: In Vitro CAR-T CRS Model
This protocol outlines a standard methodology for investigating CRS mechanisms and screening potential therapeutics [94] [91].
Objective: To model the key immune interactions of CRS by co-culturing CAR-T cells with target tumor cells and monocyte-derived macrophages, and to evaluate the effects of cytokine blockade.
Materials:
- Effector Cells: CAR-T cells (specific for a target antigen, e.g., CD19).
- Target Cells: Antigen-positive tumor cell line (e.g., NALM-6 for CD19).
- Bystander Cells: Primary human monocyte-derived macrophages (MDMs).
- Culture Medium: Appropriate base medium (e.g., RPMI-1640) supplemented with serum and cytokines.
- Therapeutic Agents: Anti-human IL-6R antibody (e.g., Tocilizumab), JAK inhibitor (e.g., Ruxolitinib), and relevant isotype controls.
- Assay Kits: Human multiplex cytokine array (e.g., for IL-6, IFN-γ, IL-10, IL-1β, TNF-α), cell viability assay (e.g., LDH, MTT).
Methodology:
- Cell Preparation:
- Differentiate monocytes from human PBMCs into macrophages using GM-CSF or M-CSF over 5-7 days.
- Expand and activate CAR-T cells ex vivo according to established protocols.
Co-culture Setup:
- Seed target tumor cells in a multi-well plate.
- Add CAR-T cells at a defined Effector:Target ratio (e.g., 1:1 to 5:1).
- Add MDMs as bystander cells.
- Include control wells: tumor cells alone, CAR-T cells alone, MDMs alone, and all cell types together.
- Add therapeutic agents or controls to designated wells at the start of co-culture.
Incubation and Sampling:
- Incubate co-cultures for 24-72 hours at 37°C, 5% CO₂.
- At defined timepoints (e.g., 24h, 48h), collect supernatant and store at -80°C for cytokine analysis.
- Harvest cells for flow cytometric analysis of activation markers (e.g., CD69, CD25) or viability staining.
Downstream Analysis:
- Cytokine Profiling: Quantify cytokine concentrations in supernatant using the multiplex array.
- Viability/Killing: Measure tumor cell killing (e.g., via LDH release or flow cytometry) and overall cell health.
- Immune Phenotyping: Analyze surface marker expression on T-cells and macrophages to assess activation status.
Data Interpretation: A successful CRS model will show significant cytokine elevation (especially IL-6, IFN-γ, TNF-α) in the co-culture condition compared to controls. Effective therapeutic intervention should significantly reduce these cytokine levels and may modulate immune cell activation, without completely abrogating CAR-T cytotoxic function.
Therapeutic Adaptation and Cross-Disease Application
The shared pathophysiology of CS allows for the rational adaptation of therapies across conditions, though with important nuances.
Diagram 2: Adaptation of immunomodulatory therapies across conditions. The application of specific therapies varies based on etiology and evidence strength. IL-6 inhibition is a first-line therapy in CAR-T CRS and is guideline-based in COVID-19, but remains investigational in sepsis. JAK inhibitors and corticosteroids also have established roles in COVID-19, while their use is more limited in other conditions. Organ support is universally essential.
- IL-6 Pathway Blockade: Tocilizumab, an IL-6 receptor antagonist, has the strongest evidence in CAR-T CRS, where it is a first-line therapy [91]. Its success here prompted rapid adoption in severe COVID-19, where it is now a guideline-recommended therapy [95] [1]. In sepsis, despite a strong pathogenic rationale [67], clinical trials have generally not shown consistent mortality benefit, highlighting that the therapeutic window and patient selection are critical and may differ from other CS etiologies [90].
- JAK/STAT Inhibition: JAK inhibitors (e.g., baricitinib, ruxolitinib) target a central signaling hub for multiple cytokines. They have proven effective in COVID-19 [1] [92] and are used investigationally in CAR-T CRS to mitigate severity [94] [1]. Their application in sepsis is more nascent and remains within the preclinical and early clinical trial domain [67].
- Corticosteroids: As broad-spectrum anti-inflammatory agents, corticosteroids are a mainstay in managing severe COVID-19 [92] and are used alongside IL-6 blockade in moderate-severe CAR-T CRS [91]. In sepsis, their use is more controversial, typically reserved for patients with septic shock and evidence of inadequate adrenal response [90].
- Supportive Care and Underlying Cause: Regardless of the etiology, organ support (e.g., mechanical ventilation, vasopressors, renal replacement therapy) is fundamental. Crucially, therapy must address the underlying cause: antibiotics for sepsis, antivirals for COVID-19, and managing the tumor burden and T-cell persistence in CAR-T CRS [90] [91] [92].
The paradigm of cytokine storm provides a powerful framework for understanding and treating a spectrum of severe illnesses. While the triggers for sepsis, CAR-T CRS, and COVID-19 are distinct, the final common pathway of dysregulated immunity and inflammation presents a shared therapeutic target. Future progress hinges on several key approaches: the development of precision immunomodulation strategies that target specific pathways without causing broad immunosuppression; the discovery and validation of robust biomarkers for early patient stratification and therapy guidance; and the use of advanced in vitro and in silico models to better predict therapeutic efficacy and toxicity. By continuing to decipher the intricate mechanisms of CS and leveraging lessons learned across these disciplines, the scientific and medical communities can improve outcomes for patients facing these life-threatening conditions.
Evaluating Clinical Evidence and Comparative Effectiveness of Treatment Modalities
Cytokine storm (CS), a life-threatening systemic inflammatory syndrome characterized by hyperactivation of immune cells and elevated levels of circulating cytokines, represents a common pathological pathway leading to multiple organ failure and mortality across diverse clinical conditions [1]. This hyperinflammatory state is implicated in the pathogenesis of severe COVID-19, acute respiratory distress syndrome (ARDS), graft-versus-host disease (GVHD), and complications from immunotherapies [1] [97]. The dysregulated immune response involves massive release of pro-inflammatory cytokines including IL-6, IL-1, TNF-α, IFN-γ, and GM-CSF, which activate signaling pathways that drive organ damage [1] [97]. This in-depth technical review examines the clinical evidence for three targeted therapeutic approaches—IL-6 receptor inhibition with tocilizumab, JAK-STAT pathway inhibition with ruxolitinib, and viral neutralization with monoclonal antibodies—in managing CS-driven pathologies. We synthesize quantitative efficacy data from recent clinical trials, detail experimental methodologies, and visualize key signaling pathways to provide drug development professionals with a comprehensive evidence base for future research directions.
Pathophysiological Basis of Cytokine Storm and Therapeutic Targets
Key Signaling Pathways in Cytokine Storm
The JAK-STAT pathway represents a crucial signaling cascade in CS pathogenesis, serving as the primary intracellular signaling route for numerous cytokines elevated during hyperinflammatory responses [1]. This pathway consists of transmembrane receptors, receptor-associated Janus kinases (JAK1, JAK2, JAK3, TYK2), and signal transducers and activators of transcription (STAT1-6) [1]. Upon cytokine binding, JAKs phosphorylate STAT proteins, which dimerize and translocate to the nucleus to regulate expression of inflammation-related genes [1]. IL-6, a pivotal cytokine in CS, triggers JAK/STAT3 activation through both membrane-bound and soluble IL-6 receptors, resulting in a systemic hyperinflammatory response and secretion of additional mediators including IL-1β, IL-8, CCL2, CCL3, CCL5, and GM-CSF [1]. The central role of these pathways in CS provides the rational basis for targeted therapeutic intervention.
Cytokine Storm Signaling Pathway: This diagram illustrates the core signaling cascade in cytokine storm, from initial pathogen recognition to systemic hyperinflammation.
Therapeutic Targeting Strategies
Three principal therapeutic strategies have emerged for managing CS:
- IL-6 pathway inhibition: Tocilizumab binds to both membrane-bound and soluble IL-6 receptors, inhibiting IL-6 signal transduction and downstream inflammatory effects [98].
- JAK-STAT pathway inhibition: Ruxolitinib, a selective JAK1/JAK2 inhibitor, attenuates signaling of multiple cytokines implicated in CS, including IL-2, IL-6, IL-7, IL-10, IFN-γ, G-CSF, and GM-CSF [99].
- Viral neutralization: SARS-CoV-2 neutralizing antibodies target the spike protein receptor binding domain, preventing viral entry and subsequent immune activation [100].
Clinical Trial Evidence for Tocilizumab
Mechanism of Action and Experimental Models
Tocilizumab is a humanized monoclonal antibody that binds to both soluble and membrane-bound IL-6 receptors (sIL-6R and mIL-6R), inhibiting IL-6-mediated pro-inflammatory signaling [98]. Single-cell RNA sequencing studies of tocilizumab-treated peripheral blood mononuclear cells (PBMCs) in stimulated conditions demonstrate that the drug reduces expression of inflammatory-mediated genes and biologic pathways, particularly in monocytes [98]. This experimental model provides mechanistic insights into how tocilizumab might mitigate CS in clinical settings.
Table 1: Key Clinical Trials of Tocilizumab for COVID-19 Pneumonia
| Trial Design | Patient Population | Intervention | Primary Outcome | Key Efficacy Results | Reference |
|---|---|---|---|---|---|
| Randomized, controlled, open-label, single-center | 62 hospitalized patients with severe COVID-19 pneumonia and IL-6 >40 pg/mL | SOC vs SOC + single-dose tocilizumab (400mg/<75kg, 600mg/≥75kg) | Death or IMV within 28 days | 12.9% vs 32.3% (p=0.068); RR 0.83 (95% CI: 0.77-0.89) in meta-analysis | [101] |
| Case report with literature review | 48-year-old male with severe COVID-19 and impending respiratory failure | Tocilizumab + hydroxychloroquine/azithromycin/zinc | Prevention of mechanical ventilation | Clinical improvement within days, avoidance of intubation, hospital discharge | [102] |
Efficacy in Cytokine Storm Conditions
The efficacy of tocilizumab appears enhanced when targeted to patients with biochemical evidence of significant inflammation. In a randomized controlled trial focusing on patients with IL-6 levels >40 pg/mL, tocilizumab demonstrated a strong trend toward reducing the composite endpoint of death or invasive mechanical ventilation (12.9% vs 32.3%, p=0.068) [101]. A comprehensive meta-analysis incorporated in this trial revealed a significant risk reduction for death or mechanical ventilation (RR 0.83, 95% CI: 0.77-0.89) in patients receiving tocilizumab compared to standard of care alone [101]. This supports the concept of personalized immunomodulation based on inflammatory biomarkers.
Clinical Trial Evidence for Ruxolitinib
Pharmacological Properties and Preclinical Evidence
Ruxolitinib is an oral inhibitor of Janus Kinase 1 and 2 with potent anti-inflammatory properties [99]. Biochemical assays demonstrate nanomolar half maximal inhibitory concentration (IC50) values for JAK1 (3.3 ± 1.2 nM) and JAK2 (2.8 ± 1.2 nM), with significantly less potency against JAK3 (428 ± 243 nM) and Tyk2 (19 ± 3.2 nM), confirming its selectivity [99]. In preclinical models, ruxolitinib (90 mg/kg twice daily) significantly suppressed elevated IL-6 and normalized TNF-α levels, supporting its potential to mitigate cytokine storm [99].
Table 2: Phase II Trial of Ruxolitinib for Sclerotic Chronic GVHD
| Trial Parameter | Details | Results |
|---|---|---|
| Study Design | Single-arm multicenter phase II trial (n=47) | Primary endpoint met |
| Patient Population | Adults with sclerotic cGVHD refractory to corticosteroids and ≥1 additional line of systemic therapy | Median age: 62 years (range 23-76) |
| Intervention | Ruxolitinib 10 mg twice daily for ≥6 months | Median treatment duration: 11 months |
| Primary Endpoint | Complete or partial response in skin and/or joints at 6 months (2014 NIH cGVHD Criteria) | 49% (95% CI 34-64%) partial response |
| Secondary Endpoints | Overall cGVHD response, treatment failure, FFS, NRM, steroid dose reduction, PROs | Overall cGVHD response: 47% (95% CI 32-61%) |
| Safety Profile | Well tolerated with no new safety signals | 12-month FFS: 77.1% (95% CI 61.3%-87.0%) |
Efficacy in Inflammatory Conditions
In a multicenter phase II trial focusing on sclerotic chronic GVHD—a highly morbid and refractory form of GVHD characterized by progressive tissue fibrosis—ruxolitinib demonstrated substantial clinical efficacy [103]. After a median treatment duration of 11 months, 49% (95% CI 34-64%) of patients achieved partial response in skin and/or joints at 6 months, with specific improvements in joint/fascia (45%) and skin (19%) manifestations [103]. The duration of response was sustained, with 77% (95% CI: 48%-91%) maintaining response at 12 months [103]. These findings support JAK inhibition as an effective strategy for managing steroid-refractory inflammatory conditions driven by dysregulated immune responses.
Clinical Trial Evidence for Neutralizing Antibodies
Mechanism and Preclinical Development
Neutralizing monoclonal antibodies target the receptor binding domain (RBD) of the SARS-CoV-2 spike protein, blocking viral entry into host cells [100]. SCTA01, a human IgG1 monoclonal antibody with a LALA-modified Fc region, was designed to eliminate antibody-dependent cell cytotoxicity (ADCC) and mitigate antibody-dependent enhancement (ADE) [100]. In non-clinical studies, SCTA01 inhibited viral replication in both trachea and lungs, preventing pulmonary damage with no significant adverse events even at ten times the effective dose [100].
Clinical Trial Outcomes
A randomized, double-blinded, placebo-controlled Phase II trial evaluated SCTA01 in high-risk outpatients diagnosed with COVID-19 [100]. The trial assigned 109 patients to receive SCTA01 (750 mg, 1500 mg, or 3000 mg) or placebo, with the primary endpoint being COVID-19-related hospitalization or death by Day 29 [100]. Only two patients experienced COVID-19-related hospitalization (one in 750 mg group, one in 3000 mg group), with no significant differences in viral load reduction (p=0.20) or symptom score reduction (p=0.37) between SCTA01 and placebo groups [100]. The comparable incidence of adverse events between SCTA01 (23.8%) and placebo (24.0%) groups confirmed the antibody's safety profile, though its development was terminated due to emerging Omicron variants resistant to SCTA01 [100].
Experimental Protocols and Methodologies
Protocol for PBMC Stimulation and Tocilizumab Treatment Assessment
Sample Collection and Processing:
- Collect PBMCs from patients via Ficoll-Paque density gradient centrifugation and freeze in FBS with 10% DMSO [98].
- Thaw PBMCs and adjust to 2×10^5 cells/well in 96-well plates; stimulate with soluble anti-CD3 (5 μg/mL) and anti-CD28 antibodies (10 μg/mL) for 24h at 37°C, 5% CO2 [98].
- Include unstimulated PBMCs under identical conditions as controls [98].
Treatment and Analysis:
- Administer tocilizumab (8 mg/kg IV) to treatment group; maintain control group on standard therapy [98].
- For scRNA-seq: Multiplex cell pools, filter through 40μM strainer, and prepare libraries using 10× Chromium Single Cell 3′ Reagent Kits v3 [98].
- Sequence libraries and analyze differential gene expression, particularly focusing on monocyte populations and inflammatory pathways [98].
PBMC Stimulation Protocol: Experimental workflow for assessing tocilizumab effects on immune cells using single-cell RNA sequencing.
Phase II Trial Design for Ruxolitinib in Sclerotic cGVHD
Patient Eligibility Criteria:
- Include adults ≥18 years with sclerotic cGVHD manifesting as superficial/deep skin sclerosis, fasciitis, or joint contractures [103].
- Require prior treatment with systemic corticosteroids for ≥12 months plus ≥1 additional line of systemic therapy, or corticosteroids plus ≥2 additional lines [103].
- Maintain Karnofsky performance status ≥60, ANC >1000/μL, and platelets ≥50,000/μL [103].
Study Design and Endpoints:
- Implement single-arm multicenter design with ruxolitinib 10 mg twice daily continuously for 6 months (extendable to 12 months for responders) [103].
- Assess primary endpoint as complete or partial response in skin and/or joint using 2014 NIH cGVHD Consensus Criteria at 6 months [103].
- Evaluate secondary endpoints including overall cGVHD response, treatment failure, failure-free survival, non-relapse mortality, and patient-reported outcomes (Lee Symptom Scale, SHAQ) [103].
Research Reagent Solutions
Table 3: Essential Research Reagents for Cytokine Storm Therapeutic Development
| Reagent/Category | Specific Examples | Research Application | Key Function |
|---|---|---|---|
| IL-6 Pathway Inhibitors | Tocilizumab | In vitro PBMC stimulation models; clinical trials for COVID-19, GVHD | IL-6 receptor blockade; inhibits trans-signaling |
| JAK-STAT Inhibitors | Ruxolitinib (JAK1/JAK2) | Preclinical cytokine suppression models; cGVHD clinical trials | Pan-JAK inhibition; reduces multiple cytokine signals |
| Neutralizing Antibodies | SCTA01 (anti-SARS-CoV-2) | Viral challenge studies; outpatient clinical trials | Spike protein RBD binding; blocks viral entry |
| Cell Separation Media | Ficoll-Paque PLUS | PBMC isolation from whole blood | Density gradient separation of mononuclear cells |
| Cell Stimulation Reagents | Anti-CD3/CD28 antibodies | T-cell activation in PBMC cultures | Polyclonal T-cell stimulation; mimics immune activation |
| Single-Cell Genomics | 10× Chromium Single Cell 3′ Kits | scRNA-seq of immune cell populations | High-throughput transcriptomic profiling |
| Cytokine Measurement | ELISA/MSD/LEGENDplex | Serum cytokine quantification | Multiplex biomarker assessment for patient stratification |
The strategic targeting of cytokine storm through specific immunomodulatory agents represents a transformative approach in managing hyperinflammatory syndromes. Clinical evidence demonstrates that tocilizumab provides significant benefit in severe COVID-19 patients with elevated IL-6 levels, reducing progression to mechanical ventilation and mortality [101]. Ruxolitinib shows substantial efficacy in refractory sclerotic chronic GVHD, with nearly half of treatment-resistant patients achieving meaningful clinical responses [103]. While neutralizing antibodies like SCTA01 face challenges from viral evolution, their targeted mechanism offers a template for future antiviral approaches [100]. The optimal application of these therapies depends on careful patient stratification using biomarker-guided approaches and appropriate timing within the disease course. Future development should focus on combination strategies that target multiple aspects of the hyperinflammatory cascade while preserving protective immune functions, potentially integrating these targeted immunomodulators with conventional antimicrobial or anticancer therapies.
The management of complex pathophysiological conditions such as cytokine storm syndrome and multiple organ failure presents significant therapeutic challenges. This whitepaper provides a comprehensive technical analysis of three primary therapeutic classes—biologics, small molecules, and device-based therapies—examining their respective mechanisms, applications, and developmental considerations within the context of dysregulated inflammatory responses. As cytokine-mediated pathologies continue to demonstrate multifactorial pathogenesis, understanding the distinct advantages and limitations of each therapeutic modality becomes paramount for researchers and drug development professionals designing targeted intervention strategies. Our analysis synthesizes current structural, mechanistic, and clinical data to inform therapeutic selection and development pipelines for critical inflammatory conditions.
Cytokine storm (CS) or cytokine release syndrome (CRS) represents a life-threatening systemic inflammatory syndrome characterized by immune cell hyperactivation and elevated circulating cytokine levels, frequently culminating in multiple organ dysfunction syndrome (MODS) [79] [1]. This pathophysiological state presents a formidable therapeutic challenge due to its complex, self-amplifying cytokine networks and diverse cellular participants. The development of targeted therapies requires a nuanced understanding of how different drug classes can intervene in specific aspects of this dysregulated immune response.
Within this context, therapeutic interventions can be broadly categorized into biologics, small molecules, and device-based modalities, each possessing distinct characteristics that determine their applicability against specific molecular targets in the inflammatory cascade. This review provides a systematic comparison of these therapeutic classes, with emphasis on their mechanistic actions, development considerations, and potential applications in CS and multi-organ failure research and treatment.
Structural and Mechanistic Characteristics
Fundamental Properties and Target Engagement
Table 1: Fundamental Characteristics of Therapeutic Modalities
| Characteristic | Small Molecules | Biologics | Device-Based Therapies |
|---|---|---|---|
| Molecular Size | <900 Daltons, typically 20-100 atoms [104] [105] [106] | Large, complex molecules (1,000-20,000 atoms) [105] | Physical devices, membranes, or systems |
| Structure | Simple, well-defined chemical structures [106] | Complex 3D structures, often proteins [105] [106] | Varies by application (e.g., filters, cartridges) |
| Production Method | Chemical synthesis [105] [106] | Living cell systems (CHO, E. coli) [105] | Engineering and manufacturing |
| Target Specificity | Lower; potential for off-target effects [105] [106] | High; precise targeting [105] [106] | Physical removal of mediators |
| Administration Route | Oral (most) [104] [105] | Injection/IV infusion [104] [105] | Extracorporeal circuits |
| Stability | Room temperature stable [104] [105] | Typically requires refrigeration [104] [105] | Device-specific shelf life |
Small molecule drugs are chemically synthesized compounds with low molecular weights (<900 Daltons) that enable penetration of cell membranes and access to intracellular targets [104] [106]. Their compact size facilitates oral administration and broad tissue distribution, including crossing the blood-brain barrier, making them particularly valuable for central nervous system applications [104]. However, this promiscuous distribution can also lead to off-target effects and subsequent adverse events [106].
In contrast, biologics are large, complex molecules (typically 200-1000 times larger than small molecules) derived from living organisms [105]. This class includes monoclonal antibodies, therapeutic proteins, antibody-drug conjugates (ADCs), cell therapies (including CAR-T), and nucleic acid-based therapies [104] [106]. Their complex three-dimensional structures enable highly specific target binding, particularly against large, flat protein surfaces involved in protein-protein interactions that are often inaccessible to small molecules [105]. This precision allows biologics to modulate specific immune pathways with reduced off-target effects, though their large size generally restricts them to injectable administration and limits their tissue penetration [105].
Device-based therapies for cytokine storm typically involve extracorporeal blood purification systems designed to remove circulating inflammatory mediators. These systems utilize specialized membranes or adsorption columns to physically remove cytokines and other inflammatory molecules from the bloodstream, functioning independently of specific molecular targets [10].
Molecular Mechanisms in Cytokine Storm Pathology
Diagram: Key Signaling Pathways in Cytokine Storm and Therapeutic Intervention Points
Cytokine storm pathogenesis involves multiple interconnected signaling pathways that represent potential intervention points for different therapeutic classes. The JAK/STAT pathway is particularly significant, with cytokines including IL-6, TNF-α, and IFN-γ activating Janus kinases (JAK1, JAK2, JAK3, TYK2) that subsequently phosphorylate signal transducers and activators of transcription (STATs) [1]. This signaling cascade leads to nuclear translocation of STATs and increased expression of pro-inflammatory genes, creating a self-amplifying inflammatory loop [1].
IL-6 exemplifies a key cytokine mediator with multiple signaling modes: classic signaling (via membrane-bound IL-6R), trans-signaling (via soluble IL-6R), and trans-presentation [79] [1]. The IL-6/JAK/STAT3 axis results in systemic hyperinflammation and secretion of additional mediators including IL-1β, IL-8, CCL2, CCL3, CCL5, and GM-CSF [1]. Additional pathways including Toll-like receptors (TLRs), neutrophil extracellular traps, and NLRP3 inflammasome activation contribute to the cytokine cascade [1].
Biologics primarily target specific cytokines or their receptors. Monoclonal antibodies against IL-6 (tocilizumab), IL-6R, IL-1 (anakinra), and TNF-α (infliximab) can precisely neutralize these mediators [1]. Small molecules typically target intracellular signaling components, with JAK inhibitors (e.g., tofacitinib) blocking downstream signaling of multiple cytokines simultaneously [1]. Device-based therapies employ non-specific physical removal of circulating cytokines through adsorption or filtration mechanisms [10].
Development Considerations and Market Trends
Development Pipelines and Economic Factors
Table 2: Development and Commercialization Comparison
| Parameter | Small Molecules | Biologics | Device-Based Therapies |
|---|---|---|---|
| Development Timeline | 8-10 years [105] | 10-12 years [105] | Varies (typically 5-7 years) |
| Development Cost | $1-2 billion [105] | $2-4 billion [105] | Varies by complexity |
| Manufacturing | Chemical synthesis; cheaper, reproducible [104] | Complex living systems; expensive facilities [104] [105] | Engineering production |
| Success Rates | Lower clinical trial success [105] | Higher clinical trial success [105] | Device-specific |
| Patent Exclusivity | 5 years before generics [104] | 12 years before biosimilars [104] | Varies by jurisdiction |
| Market Share (2023) | 58% of pharma market [104] | 42% of pharma market [104] | Niche segment |
| Market Growth | Slower growth [104] | 3x faster than small molecules [104] | Emerging field |
The development pathways for small molecules and biologics demonstrate significant differences in timeline, cost, and technical requirements. Small molecule development typically requires $1-2 billion over 8-10 years, while biologics development averages $2-4 billion over 10-12 years [105]. This cost differential stems from the complex manufacturing processes for biologics, which require specialized facilities costing upwards of $500 million to construct and stringent controls to avoid product batch variability [104] [105].
Market analysis reflects a shifting landscape, with the global pharma market growing from $828B in 2018 (69% small molecules, 31% biologics) to $1344B in 2023 (58% small molecules, 42% biologics) [104]. Biologics sales are growing three times faster than small molecules, with projections suggesting biologics will surpass small molecule sales by 2027 [104]. This trend is further evidenced by R&D spending shifts, with small molecules consuming 55-60% of the R&D budget in 2014-16, declining to 40-45% by 2024, with corresponding growth in biologics R&D [104].
Approval patterns demonstrate the continuing dominance of small molecules in terms of volume, with FDA's Center for Drug Evaluation and Research (CDER) approving 73% small molecules versus 27% biologics in 2025 through September [107]. However, biologics increasingly target novel mechanisms and command premium pricing, with eight of the top ten best-selling drugs globally being biologics [105].
Clinical Application in Cytokine Storm and Multi-Organ Failure
Table 3: Therapeutic Applications in Inflammatory Pathologies
| Application | Small Molecules | Biologics | Device-Based Therapies |
|---|---|---|---|
| Cytokine Storm Targets | JAK/STAT pathways [1], Inflammasomes [1] | IL-6, IL-1, TNF-α, IFN-γ [1], GM-CSF | Broad-spectrum cytokine removal [10] |
| Specific Conditions | Early hyperinflammation, intracellular targets | Severe CRS, specific cytokine-driven pathology | Refractory cases, broad inflammatory states |
| Oncology CRS | Limited role | Tocilizumab (anti-IL-6R) [1] | Emerging application |
| COVID-19 CRS | JAK inhibitors (baricitinib) [1] | IL-6 inhibitors [108] | Blood purification [10] |
| Sepsis | Investigational JAK/STAT inhibitors [10] | TNF-α inhibitors (investigational) [10] | Blood purification [10] |
| CAR-T CRS | JAK1 inhibitors (reducing severity) [1] | IL-6R antagonists (standard care) [1] | Rescue therapy |
| Administration Setting | Oral; outpatient possible | IV/SC; typically inpatient | Inpatient, ICU settings |
The selection of therapeutic class for cytokine storm management depends on specific clinical considerations, including the predominant cytokines involved, disease stage, and patient-specific factors. Biologics excel in conditions driven by specific, identifiable cytokines. For CAR-T cell associated CRS, IL-6 receptor antagonists like tocilizumab represent standard care [1]. Similarly, in COVID-19 associated CRS, IL-6 inhibitors and JAK inhibitors have demonstrated efficacy in severe cases [1] [108].
Small molecules offer advantages in early intervention and for intracellular targets. JAK inhibitors provide broad cytokine suppression by targeting shared signaling pathways and can be administered orally, facilitating outpatient use [1]. Their ability to cross cell membranes enables targeting of inflammasome components and intracellular signaling cascades upstream of cytokine production [1].
Device-based therapies provide a non-pharmacological approach, typically reserved for severe, refractory cases or when pharmacological interventions are contraindicated. These systems can remove inflammatory mediators without adding immunosuppressive agents to the system, potentially mitigating infection risks in already compromised patients [10].
Experimental Approaches and Research Methodologies
Research Reagent Solutions for Cytokine Storm Investigation
Table 4: Essential Research Tools for Cytokine Storm Therapeutic Development
| Research Tool Category | Specific Examples | Research Applications | Therapeutic Class |
|---|---|---|---|
| Cytokine Detection | ELISA, multiplex immunoassays, ELISpot | Quantifying IL-6, IL-1β, TNF-α, IFN-γ levels in biological samples [79] [1] | All classes |
| Pathway Inhibitors | JAK inhibitors (tofacitinib), STAT inhibitors, NF-κB inhibitors | Pathway validation studies; small molecule therapeutic development [1] | Small molecules |
| Neutralizing Antibodies | Anti-IL-6, anti-IL-6R, anti-TNF-α, anti-IFN-γ antibodies | Target validation; mechanistic studies; biologic therapeutic development [1] | Biologics |
| Cell Culture Models | PBMCs, macrophage cell lines, endothelial cells | In vitro cytokine release assays; cell-specific response profiling [79] | All classes |
| Animal Models | LPS challenge, CLP (cecal ligation puncture), CAR-T mouse models | In vivo efficacy and safety testing [109] | All classes |
| Gene Expression Analysis | RNA-seq, PCR arrays, single-cell RNA-seq | Transcriptional profiling of inflammatory pathways [109] | All classes |
| Adsorption Materials | Polymethylmethacrylate beads, polystyrene fibers | Device efficiency testing; ex vivo blood purification studies [10] | Device-based |
Preclinical Evaluation Workflows
Diagram: Experimental Framework for Evaluating Cytokine Storm Therapies
The experimental evaluation of therapeutic interventions for cytokine storm requires a multidisciplinary approach incorporating in vitro systems, animal models, and specialized analytical techniques. Initial screening typically employs human peripheral blood mononuclear cells (PBMCs) or macrophage cell lines stimulated with LPS or other Toll-like receptor agonists to induce cytokine production [79]. These systems allow rapid assessment of compound efficacy in modulating cytokine release and preliminary mechanism of action studies.
Animal models remain essential for evaluating therapeutic efficacy in complex physiological systems. Common approaches include lipopolysaccharide (LPS) challenge models for acute inflammation, cecal ligation and puncture (CLP) for polymicrobial sepsis, and fecal instillation (FI) models [109]. For CRS associated with specific therapies like CAR-T, specialized mouse models have been developed that reproduce key aspects of the human syndrome [1]. These models enable assessment of not only cytokine modulation but also organ dysfunction, cellular infiltration, and survival outcomes.
Analytical methods focus on quantifying cytokine profiles (using ELISA, multiplex immunoassays), assessing immune cell activation (flow cytometry), and evaluating signaling pathway modulation (western blot, phospho-protein assays) [79] [1]. Transcriptomic approaches including RNA sequencing provide comprehensive views of inflammatory pathway activation and therapeutic effects at the gene expression level [109].
Specialized considerations for each therapeutic class include immunogenicity assessment for biologics [106], off-target profiling for small molecules, and biocompatibility testing for device-based therapies. The successful development of cytokine storm therapeutics requires integration of these diverse methodological approaches to build a comprehensive understanding of therapeutic efficacy and mechanism.
The comparative analysis of biologics, small molecules, and device-based therapies reveals distinct and complementary roles in addressing the complex pathophysiology of cytokine storm and multiple organ failure. Biologics offer high specificity against individual cytokine targets, making them particularly valuable in defined inflammatory conditions such as CAR-T associated CRS. Small molecules provide advantages in targeting intracellular signaling pathways and offer oral administration potential, while device-based therapies present a non-pharmacological approach for broad-spectrum mediator removal.
The evolving therapeutic landscape demonstrates a shifting balance between these modalities, with biologics showing accelerated growth driven by their precision and effectiveness against previously undruggable targets. However, small molecules maintain important roles, particularly for central nervous system applications and conditions requiring broad pathway modulation. Future directions will likely see increased combination approaches, leveraging the unique strengths of each therapeutic class to achieve enhanced efficacy against complex inflammatory syndromes.
For researchers and drug development professionals, selection of therapeutic modality requires careful consideration of the specific cytokine pathways involved, disease stage, and practical clinical considerations including administration route and production feasibility. As our understanding of cytokine storm biology continues to advance, so too will the sophistication of therapeutic interventions across all three classes, ultimately enabling more precise and effective management of these life-threatening inflammatory conditions.
Benchmarking Novel Biomarkers Against Traditional Severity Scores (APACHE II, SOFA)
Risk stratification in the intensive care unit (ICU) is fundamental for prognostication, resource allocation, and guiding therapeutic interventions. For decades, traditional scoring systems such as the Acute Physiology and Chronic Health Evaluation II (APACHE II) and the Sequential Organ Failure Assessment (SOFA) have been the cornerstone of clinical assessment for critically ill patients, including those with cytokine storm-driven multiple organ failure [110] [111]. While effective, these systems have notable limitations, including their complexity, reliance on numerous clinical parameters, and the time required for calculation, which can impede rapid clinical decision-making [110]. This has spurred the investigation of novel, readily available biomarkers that can simplify risk assessment without compromising predictive accuracy.
The context of cytokine storm research adds a layer of biological plausibility to this pursuit. Cytokine storms, life-threatening syndromes characterized by uncontrolled systemic inflammation, innate immune hyperactivation, and excessive cytokine release, are central to the pathogenesis of sepsis and other critical illnesses [112] [1]. This dysregulated immune response directly leads to organ dysfunction and failure. Therefore, biomarkers that reflect key aspects of this pathophysiology—such as endothelial damage, metabolic stress, and immune cell activation—are not only predictive but also mechanistically informative [10] [113]. This technical guide benchmarks emerging biomarkers against traditional scores, providing researchers and drug developers with a rigorous framework for evaluation within the specific context of cytokine storm and multiple organ failure mechanisms.
Performance Comparison: Traditional Scores vs. Novel Biomarkers
Extensive research has compared the predictive power of established scoring systems with novel, simplified biomarkers and models. The following tables summarize key quantitative findings from recent studies.
Table 1: Predictive Performance for In-Hospital Mortality in General ICU Patients
| Scoring System / Biomarker | AUC | Performance Comparison | Study Details |
|---|---|---|---|
| SOFA Score | 0.931 | Reference standard | Retrospective study of 19,720 adult ICU patients [110]. |
| Novel Model 3 (LAR, NPAR, MV, CRRT) | 0.929 | Statistically comparable to SOFA (p=0.052) | Machine learning model using readily available parameters [110]. |
| APACHE II Score | 0.900 | Reference standard | [110]. |
| Novel Model 2 | 0.913 | Comparable to APACHE II (p=0.430) | Enhanced model building on basic biomarkers [110]. |
| Lactate-to-Albumin Ratio (LAR) | 0.830 | -- | Individual biomarker performance [110]. |
| Novel Model 1 (LAR & NPAR only) | 0.898 | Robust performance despite simplicity | Basic two-biomarker model [110]. |
| C-reactive Protein-to-Albumin Ratio (CAR) | 0.749 | -- | Individual biomarker performance [110]. |
| Neutrophil Percent-to-Albumin Ratio (NPAR) | 0.748 | -- | Individual biomarker performance [110]. |
Table 2: Predictive Performance for 28-Day Mortality in Sepsis Patients
| Scoring System | AUC | Study Details |
|---|---|---|
| SAPS II | 0.902 | Prospective study of 165 sepsis patients; no significant difference between scores (p>0.05) [111]. |
| OASIS | 0.879 | Noted as a practical tool requiring no laboratory tests [111]. |
| SOFA Score | 0.873 | [111]. |
| APACHE II | 0.803 | More complex due to abundant parameters [111]. |
Table 3: Emerging Biomarkers in Sepsis and Cytokine Storm
| Biomarker | Function & Pathophysiological Context | Diagnostic/Prognostic Utility |
|---|---|---|
| Monocyte Distribution Width (MDW) | Reflects monocyte activation and morphological changes in early sepsis [10] [113]. | Early detection of sepsis; diagnostic threshold >23.5 [10]. |
| Serum Amyloid A (SAA) | Acute-phase reactant; levels surge (up to 1000-fold) upon microbial insult [10] [113]. | Correlates with systemic inflammation intensity; rules out bacterial infection [10]. |
| High-Density Lipoprotein (HDL) | Vasoprotective, anti-inflammatory; levels and function are severely compromised during sepsis [10]. | Qualitative and quantitative changes offer prognostic value superior to APACHE II/SOFA in septic shock [10]. |
| Neutrophil-to-Lymphocyte Ratio (NLR) | Indicator of systemic inflammation and immune dysregulation [112] [10]. | Potential diagnostic and prognostic value in sepsis [112]. |
| RDW-to-Albumin Ratio (RAR) | Combines a marker of inflammation-induced hematopoiesis dysregulation (RDW) and nutritional/inflammatory status (albumin) [112]. | Emerging prognostic value [112]. |
| Heparin-Binding Protein (HBP) | Released by neutrophils; induces vascular hyperpermeability [113]. | Prognostic indicator for septic deterioration; cut-off 19.8 ng/mL [113]. |
Experimental Protocols for Benchmarking Studies
To ensure the validity and reproducibility of biomarker benchmarking studies, rigorous experimental methodologies must be employed.
Retrospective Cohort Study Design
Objective: To develop and validate simplified prediction models against traditional scores for in-hospital mortality. Population: A large, single-center cohort of adult ICU patients (e.g., n=19,720) [110]. Key Methodological Steps:
- Data Extraction: Utilize a clinical data warehouse to extract demographic data, comorbidities, laboratory results (for biomarker calculation), and clinical parameters for SOFA and APACHE II scoring.
- Variable Definitions:
- Novel Biomarkers: Calculate LAR (lactate [mmol/L] / albumin [g/dL]), NPAR (neutrophil percent [%] / albumin [g/dL]), and others from the worst values in the first 24 hours of ICU admission [110].
- Traditional Scores: Calculate SOFA and APACHE II scores using standard definitions based on the worst values in the first 24 hours [110].
- Data Splitting: Randomly split data into training (70%) and testing (30%) sets, repeating this process multiple times (e.g., 10x) for stability [110].
- Model Development & Validation:
- Use machine learning approaches (e.g., SHapley Additive exPlanations - SHAP - with an XGBoost framework) in the training set to identify the most impactful predictors [110].
- Construct logistic regression models with the selected variables.
- Apply the finalized models to the test sets for validation.
- Statistical Analysis:
- Evaluate model performance using Receiver Operating Characteristic (ROC) curves and calculate the Area Under the Curve (AUC).
- Statistically compare AUCs using the DeLong test.
- Determine optimal cut-offs with Youden's index and compute sensitivity, specificity, PPV, and NPV [110].
Prospective Comparison in Sepsis Populations
Objective: To compare the mortality prediction of APACHE II, SOFA, SAPS II, and OASIS in patients with sepsis/septic shock. Population: Patients admitted to the ICU with a diagnosis of sepsis or septic shock based on established criteria (e.g., Sepsis-3) (e.g., n=165) [111]. Key Methodological Steps:
- Patient Enrollment: Consecutively enroll patients meeting inclusion criteria from the emergency department or inpatient units over a defined period.
- Data Collection: Prospectively collect demographic data, comorbidities, and all physiological and biochemical parameters needed to compute the four scoring systems within the first 24 hours of ICU admission.
- Score Calculation: Calculate APACHE II, SOFA, SAPS II, and OASIS scores according to their standard definitions [111].
- Outcome Measurement: The primary outcome is 28-day mortality.
- Statistical Analysis:
- Use correlation analysis (e.g., Pearson correlation) to assess the relationship between scores and mortality.
- Construct ROC curves and calculate AUCs for each score.
- Compare AUCs using appropriate statistical tests (e.g., DeLong test) [111].
Signaling Pathways in Cytokine Storm and Biomarker Linkage
Cytokine storm pathogenesis involves key signaling pathways that drive the hyperinflammation and organ damage observed in critical illness. The biomarkers discussed often reflect the activity of these pathways.
Cytokine Storm Signaling and Biomarker Correlation
The diagram illustrates the core pathways involved in cytokine storm pathogenesis. The process is initiated by PAMPs/DAMPs binding to Pattern Recognition Receptors (PRRs) like Toll-like Receptors (TLRs), activating downstream signaling such as NF-κB [1] [8]. Concurrently, inflammasome activation occurs, leading to caspase-1 activation and maturation of pro-inflammatory cytokines like IL-1β [112] [1]. These events trigger a massive cytokine release (TNF-α, IL-6, IL-1β). IL-6, a pivotal cytokine, further amplifies the response via the JAK/STAT pathway, creating a positive feedback loop [1]. This hyperinflammation induces inflammatory cell death (pyroptosis/necroptosis) and the formation of Neutrophil Extracellular Traps (NETs), which in turn release more DAMPs, perpetuating a vicious cycle that culminates in multiple organ failure [112] [1]. The novel biomarkers discussed, such as LAR, NPAR, and MDW, are measurable reflections of these underlying pathological processes, linking molecular mechanisms to clinical severity.
The Scientist's Toolkit: Research Reagent Solutions
For researchers investigating these biomarkers and pathways in the context of cytokine storm, the following table outlines essential research reagents and their applications.
Table 4: Key Research Reagents for Biomarker and Pathway Investigation
| Research Reagent / Tool | Function / Application | Research Context |
|---|---|---|
| Cytokine ELISA/Kits (e.g., for IL-6, TNF-α, IL-1β) | Quantify cytokine levels in serum/plasma or cell culture supernatants. | Essential for validating cytokine storm presence and correlating with clinical scores [112] [1]. |
| Phospho-Specific Antibodies (e.g., p-STAT3, p-NF-κB) | Detect activated signaling molecules in Western Blot or IHC to monitor pathway activity. | Crucial for investigating JAK/STAT and TLR pathway activation in patient samples or disease models [1]. |
| JAK Inhibitors (e.g., Tofacitinib, Ruxolitinib) | Small molecule inhibitors to block JAK/STAT signaling. | Used in vitro and in vivo to test the therapeutic potential of pathway inhibition and its effect on biomarker levels [1]. |
| Cytokine Antagonists (e.g., Anti-IL-6R, Anakinra) | Neutralizing antibodies or receptor antagonists targeting specific cytokines. | Key reagents for proof-of-concept studies on mitigating cytokine storm and associated organ damage [112] [8]. |
| Hematology Analyzers (with cell morphology) | Automated analysis of white blood cell counts and morphological parameters like MDW. | Required for validating clinical biomarkers such as MDW and NLR in research cohorts [10] [113]. |
| Enzymatic Colorimetric/Kits (for Lactate, Albumin) | Precisely measure lactate and albumin concentrations in biological fluids. | Fundamental for calculating ratios like LAR and NPAR in patient samples [110]. |
| Recombinant Proteins (e.g., LPS, HMGB1) | Purified PAMPs and DAMPs to stimulate immune cells in vitro. | Used to model cytokine storm initiation and study downstream biomarker release [1]. |
Regulatory Landscapes and Approval Statuses Across Key Regions
Cytokine storm (CS), or cytokine release syndrome (CRS), represents a life-threatening systemic inflammatory syndrome characterized by immune cell hyperactivation and excessive cytokine release, frequently culminating in multiple organ failure [1] [8]. This hyperinflammatory state is a critical driver of mortality in diverse conditions, including severe infections (e.g., sepsis, COVID-19), car-T cell therapy, hemophagocytic lymphohistiocytosis (HLH), and graft-versus-host disease [1] [75]. The significant global morbidity and mortality associated with CS have accelerated research and development of novel therapeutic strategies, creating a complex and evolving global regulatory landscape. For researchers and drug development professionals, navigating the varied approval statuses of CS-targeting therapies and devices across key regions is paramount for guiding clinical development plans, regulatory submissions, and commercial strategy. This whitepaper provides an in-depth analysis of the current regulatory frameworks for CS therapies in the United States (US), European Union (EU), and Japan, synthesizing quantitative approval data and detailing experimental methodologies central to translational research in this field.
Current Regulatory Status Across Key Regions
The regulatory approval of therapies for cytokine storm is stratified by mechanism of action, encompassing immunomodulatory biologics, small molecule inhibitors, and extracorporeal cytokine adsorption devices. The following section and associated tables detail the current status in major regulatory regions.
United States (U.S. Food and Drug Administration - FDA)
The FDA has approved specific therapies for defined CRS indications, primarily in the context of immunotherapy-induced hyperinflammation.
Table 1: FDA-Approved Therapies for Cytokine Release Syndrome (as of 2025)
| Therapeutic Agent | Mechanism of Action | Approved Indication | Approval Year/Notes |
|---|---|---|---|
| Tocilizumab (Actemra) | IL-6 receptor antagonist | Severe or life-threatening CAR T-cell-induced CRS in adults and pediatric patients (≥2 years) | Initially approved; remains benchmark [114] |
| Tocilizumab-anoh (Avtozma) | IL-6 receptor antagonist (biosimilar) | CRS in adults and pediatric patients (≥2 years); aligns with all Actemra IV indications | FDA approval for CRS indication in August 2025 [114] |
| CytoSorb | Extracorporeal cytokine adsorber | Emergency Use Authorization (EUA) for confirmed COVID-19 patients in ICU with confirmed/imminent respiratory failure | Not fully approved; EUA scope limited to specific critically ill COVID-19 population [115] |
European Union (European Medicines Agency - EMA)
The EU maintains a distinct regulatory pathway, often granting broader approvals for devices compared to the US.
Table 2: Key Regulatory Statuses in the European Union
| Therapy/Device | Mechanism of Action | Regulatory Status in EU | Key Indications/Notes |
|---|---|---|---|
| CytoSorb | Extracorporeal cytokine adsorber | Approved in the EU and >75 countries [115] | Elevated cytokines, bilirubin, myoglobin; intraoperative use during cardiopulmonary bypass to remove ticagrelor/rivaroxaban [115] |
| Tocilizumab | IL-6 receptor antagonist | Approved | Approved for multiple inflammatory conditions, including CRS [114] |
| ECOS 300-CY | Ex-vivo perfusion solution adsorber | Approved in EU [115] | Removal of harmful substances from ex-vivo organ perfusion solutions |
Japan (Pharmaceuticals and Medical Devices Agency - PMDA)
Japan's regulatory approach incorporates novel therapies for specific infectious disease-associated cytokine storms.
Table 3: Key Regulatory Statuses in Japan
| Therapy/Device | Mechanism of Action | Regulatory Status in Japan | Key Indications/Notes |
|---|---|---|---|
| Favipiravir | Antiviral (RNA polymerase inhibitor) | Approved by PMDA in 2024 for Severe Fever with Thrombocytopenia Syndrome (SFTS) [116] | SFTS is a viral infection often complicated by cytokine storm and HLH; approval highlights link between antiviral activity and CS management [116] |
Experimental Protocols for Cytokine Storm Research
Translational research into cytokine storm mechanisms and treatments relies on robust in vivo and in vitro models. The following protocols are derived from recent, impactful studies.
Establishing a Mouse Model of Delayed Jellyfish Envenomation Syndrome (DJES)
This protocol outlines the creation of a novel CS model, demonstrating that environmental toxins can trigger a lethal cytokine storm [9].
- Primary Objective: To investigate how minimal jellyfish venom exposure precipitates delayed multi-organ failure via a cytokine storm.
- Materials:
- Animals: Adult wild-type mice. Venom: Tentacle extract (TE) from *Nemopilema nomurai jellyfish.
- Equipment: Syringe pumps, equipment for histopathology and biochemical analysis.
- Reagents: Kits for serum cytokine analysis (ELISA) and RNA sequencing.
- Methodology:
- Venom Preparation: Dissect and homogenize jellyfish tentacles. Use proteomic analysis (e.g., LC-MS/MS) to characterize venom components, confirming the presence of metalloproteinases, phospholipases, and other toxins [9].
- Envenomation: Administer TE intravenously via tail vein at sub-lethal doses (e.g., 0.7 - 2.29 mg kg⁻¹) to model delayed syndrome.
- Monitoring: Record survival rates and time to death. Observe for clinical signs (lethargy, convulsions, respiratory distress).
- Endpoint Analysis:
- Histopathology: At 6 hours post-envenomation, harvest heart, liver, and kidney. Process for H&E staining to assess organ damage (e.g., myocardial fiber edema, hepatocellular necrosis, glomerular destruction).
- Biochemical Analysis: Measure serum markers of organ dysfunction (LDH, CK, ALT, AST, TBIL, BUN, Cr).
- Cytokine Storm Quantification:
- Transcriptomic: Isolve RNA from tissues for RNA-seq. Identify Differentially Expressed Genes (DEGs) and perform pathway enrichment analysis (KEGG, GO).
- Protein Level: Measure serum levels of >20 cytokines (e.g., IL-6, TNF-α, CXCL2, CCL4) via ELISA or multiplex immunoassay.
- Validation: Knockdown of key pathway components (e.g., NF-κB p65) in macrophages to confirm mechanistic involvement. Therapeutic intervention with dexamethasone to suppress cytokine storm and improve survival [9].
In Vitro Assessment of Macrophage-Mediated Cytokine Release
Macrophages are central effector cells in CS; this protocol assesses their direct response to inflammatory stimuli [9].
- Primary Objective: To elucidate the role of macrophages in cytokine production and identify key signaling pathways.
- Materials:
- Cell Line: RAW 264.7 murine macrophages or primary human macrophages.
- Stimuli: Jellyfish venom TE, bacterial Lipopolysaccharide (LPS), or other PAMPs/DAMPs.
- Reagents: Cell culture media, CCK-8 cell viability assay kit, immunofluorescence staining reagents, qPCR reagents, RNA-seq library prep kit.
- Methodology:
- Cytotoxicity Assay: Treat macrophages with a concentration gradient of TE for 6 hours. Perform CCK-8 assay to determine the Half Maximal Inhibitory Concentration (IC₅₀).
- Stimulation & Sampling: Stimulate macrophages with a sub-lethal dose of TE (e.g., 10 µg mL⁻¹) for a defined period (e.g., 4-24 hours). Collect supernatant for cytokine analysis and cell pellet for RNA extraction.
- Pathway Analysis:
- Transcriptomics: Perform RNA-seq on treated vs. control macrophages. Analyze DEGs and overlap with those from the in vivo DJES model. Conduct pathway enrichment analysis to identify central signaling nodes (e.g., NF-κB).
- Immunofluorescence: Stain for NF-κB p65 subunit to visualize its activation and nuclear translocation post-stimulation.
- Mechanistic Inhibition: Pre-treat cells with pathway-specific inhibitors (e.g., dexamethasone for NF-κB) prior to stimulation and measure subsequent cytokine production and cell viability.
Visualization of Key Signaling Pathways
The NF-κB pathway is a central regulator of cytokine storm pathogenesis. The diagram below, generated using Graphviz DOT language, illustrates its activation and potential intervention points.
NF-κB Pathway in Cytokine Storm
The Scientist's Toolkit: Key Research Reagents & Materials
Advancing cytokine storm research requires a specialized toolkit of reagents, models, and technologies.
Table 4: Essential Research Tools for Cytokine Storm Investigation
| Tool/Reagent | Specific Example | Function/Application in CS Research |
|---|---|---|
| Established Animal Models | Delayed Jellyfish Envenomation Syndrome (DJES) Mouse Model [9] | Models delayed, toxin-induced CS and multi-organ failure for pathophysiological and interventional studies. |
| Immune Cell Models | RAW 264.7 Macrophage Cell Line [9] | In vitro system for studying cytokine production, signaling pathways (e.g., NF-κB), and cell-venom/pathogen interactions. |
| Pathway Agonists/Antagonists | Dexamethasone [9] | Broad-spectrum anti-inflammatory agent; used experimentally to inhibit the NF-κB pathway and validate its role in CS. |
| Cytokine Profiling Technologies | Multiplex ELISA, RNA Sequencing [9] | Quantifies protein levels of multiple cytokines simultaneously in serum/tissue; identifies upstream transcriptional drivers of CS. |
| Pathway Analysis Software | KEGG, GO Enrichment Analysis Tools [9] | Bioinformatics tools for analyzing transcriptomic data to identify significantly perturbed signaling pathways (e.g., NF-κB, NOD-like receptor). |
| Extracorporeal Adsorption Devices | CytoSorb, Oxiris, Toraymyxin [60] | Used in clinical-translational research to evaluate the efficacy of non-pharmacological cytokine removal as an adjunct therapy. |
The regulatory landscape for cytokine storm therapies is dynamic and varies significantly across the US, EU, and Japan. The FDA has established a clear pathway for biologics like tocilizumab and its biosimilars for immunotherapy-associated CRS, while the EU has a more advanced framework for approving extracorporeal cytokine adsorption devices like CytoSorb. Japan's recent approval of favipiravir for an infectious disease complicated by CS underscores the expanding therapeutic scope. Driving these regulatory advancements requires robust and standardized experimental models, such as the DJES mouse model and macrophage-based in vitro systems, which are critical for deconvoluting the complex pathophysiology of CS and validating novel therapeutic targets. As research continues to unravel the intricate signaling networks and immune cell interactions underpinning cytokine storms, the regulatory landscape will inevitably evolve, demanding continuous monitoring by researchers and drug developers to successfully translate novel therapies from the bench to the bedside.
Real-World Effectiveness and Post-Market Surveillance Data
Post-market surveillance (PMS) represents a critical phase in the therapeutic lifecycle, providing essential data on the real-world effectiveness and safety of treatments after their regulatory approval. For therapies targeting cytokine storm (CS) and multiple organ dysfunction syndrome (MODS), PMS is particularly vital due to the complex pathophysiology and high mortality associated with these conditions. This systematic collection and analysis of real-world data bridges the gap between controlled clinical trials and actual clinical practice, revealing patterns of adverse drug reactions (ADRs), identifying emerging safety signals, and informing optimized treatment protocols within the broader context of cytokine storm mechanisms research. [117] [118]
Analysis of Post-Market Surveillance Data for CS-Associated Therapies
PMS of CAR-T-Cell Therapies
Chimeric antigen receptor T-cell (CAR-T) therapies represent a breakthrough in oncology but are complicated by high rates of cytokine release syndrome (CRS). Post-marketing analysis of the US Food and Drug Administration Adverse Event Reporting System (FAERS) database from October 2017 to September 2020 provides crucial real-world safety profiles for two CAR-T products: tisagenlecleucel (tisa-cel) and axicabtagene ciloleucel (axi-cel). [117]
Key Findings from CAR-T PMS: [117]
- Among 3,225 reports (1,793 for axi-cel; 1,433 for tisa-cel), CRS was the most frequently reported toxicity (52.2%), followed by febrile disorders (27.7%) and neurotoxicity (27.2%).
- The median time to onset for these events was short, with 75% occurring within the first 10 days after infusion.
- Disproportionality analyses (reporting odds ratio) confirmed known ADRs and detected potential new safety signals: axi-cel was associated with cardiomyopathies (ROR = 2.3; 95% CI 1.2–4.4) and gastrointestinal perforations (ROR = 2.9; 95% CI 1.2–7.3), while tisa-cel was associated with hepatotoxicity (ROR = 2.5; 95% CI 1.1–5.7) and pupil disorders (ROR = 15.3; 95% CI 6–39.1).
- The safety profiles differed between the two products, with analysis suggesting a stronger role for tisa-cel in inducing some immunodeficiency-related events (e.g., hypogammaglobulinemia, infections) and coagulopathies, and for axi-cel in neurotoxicity.
Real-World Data on Cytokine Storm in COVID-19
The SARS-CoV-2 pandemic provided extensive real-world evidence on CS and MODS. The dysregulated immune response in severe COVID-19 exemplifies a pathogen-induced cytokine storm, leading to acute respiratory distress syndrome (ARDS) and multi-organ failure. The significant downregulation of ACE2 receptors following viral entry shifts the renin-angiotensin system balance, activating JAK-STAT and NF-κB pathways and driving pro-inflammatory cytokine production. This cascade results in the collateral organ damage characteristic of MODS. [16]
Table 1: Key Cytokines Elevated in Human Viral Infections Associated with Cytokine Storm [119]
| Cytokine | Primary Function | Infections with Prominent Elevation |
|---|---|---|
| IP-10 (CXCL10) | Chemoattractant for immune cells | SARS-CoV-2, SARS-CoV, MERS-CoV, Influenza H5N1, HIV |
| IL-6 | Pro-inflammatory cytokine; induces acute phase proteins | SARS-CoV-2, SARS-CoV, Influenza H7N9, EBOV |
| IL-8 (CXCL8) | Neutrophil chemotaxis and activation | SARS-CoV-2, MERS-CoV |
| IL-17 | Promotes inflammation; recruits monocytes/neutrophils | MERS-CoV, HIV |
| IFN-γ | Pro-inflammatory; activates macrophages | SARS-CoV, MERS-CoV, HIV, DENV (hemorrhagic fever) |
Analysis of highly pathogenic virus infections has identified IP-10, IL-6, IL-8, and IL-17 as the most consistently and significantly elevated cytokines. Furthermore, research has quantified relationships among cytokine levels, viral load, and clearance rate, formalized in the equation: 1.30 × log₂ (IFN-γ FC) = log₁₀ (viral load) − 2.48 − 2.83 × (clearance rate), where FC is the fold-change relative to healthy controls. This model underscores IFN-γ's central role in the immunopathology of severe viral infections. [119]
Mechanisms Linking Cytokine Storm to Multiple Organ Failure
The progression from cytokine storm to multiple organ failure is a hallmark of severe illnesses, including COVID-19 and MODS in critically ill patients. The sequence and severity of organ dysfunction are not random but are influenced by specific pathophysiological mechanisms. [118] [16]
Pathogenic Mechanisms of Organ Failure: [118] [16]
- Universal Endothelial Injury: In the early phase of MODS, circulating inflammatory cytokines cause widespread damage to the endothelium, the inner lining of blood vessels, across multiple organ systems.
- Parenchymal Injury from Local Inflammation: In later stages, the overexpression of inflammatory mediators within the interstitial spaces of organs becomes a primary mechanism of damage to the functional tissue (parenchyma).
- Organ-Specific Vulnerabilities: The differential expression and upregulation of adhesion molecules in organ vascular beds, combined with the density and potency of resident immune cells (e.g., macrophages in the liver or alveoli), are key determinants of which organs fail first and most severely.
- Positive Feedback Loop: The activation of these intrinsic inflammatory cells in a distant organ creates a self-perpetuating cycle of damage, linked systemically through continuously circulating inflammatory mediators.
Table 2: Real-World Evidence on Organ Failure in Cytokine Storm Conditions
| Condition | Primary Organ(s) Affected | Key Pathophysiological Mechanisms | Supporting Evidence |
|---|---|---|---|
| CAR-T Cell Therapy [117] | Systemic (CRS), Neurological | Direct T-cell activation; elevated IL-6, IFN-γ, TNF. | FAERS database analysis (n=3,225). |
| COVID-19 [16] | Lungs (ARDS), Heart, Kidneys, Liver | Viral entry via ACE2; NLRP3 inflammasome activation; Ang II/AT1R axis & JAK/STAT/NF-κB pathway activation. | Clinical cohort studies; serum cytokine analysis. |
| Multiple Organ Dysfunction Syndrome (MODS) [118] | Sequential failure of lungs, liver, kidneys, heart | Generalized inflammatory response; endothelial damage; interstitial inflammation. | Review of critical care patient outcomes. |
Experimental Models and Methodologies for CS and MODS Investigation
In Vivo Modeling of COVID-19-Associated Cytokine Storm
The zebrafish model has been developed to study the inflammatory processes induced by the SARS-CoV-2 Spike protein and to evaluate potential treatments like photobiomodulation (PBM). [120]
Detailed Experimental Protocol: [120]
- Animal Model: Adult zebrafish (Danio rerio).
- Induction of Cytokine Storm: Intraperitoneal inoculation with recombinant Spike (rSpike) protein.
- Intervention Treatment: Application of red light photobiomodulation (PBM) at specific parameters (wavelength, power density, and exposure time detailed in the source) to rSpike-inoculated subjects.
- Sample Collection: Tissues including brain, intestine, liver, testis, and muscle are collected at 6 and 24 hours post-inoculation.
- Outcome Measures:
- Gene Expression Analysis: Quantitative RT-PCR to measure mRNA levels of pro-inflammatory markers (il1b, il6, tnfa, nfkbiab), oxidative stress modulators (romo1), and energy metabolism markers (slc2a1a, coa1).
- Metabolomic Analysis: LC-MS to profile metabolic changes in response to rSpike and PBM.
- Protein-Protein Interaction Prediction: Bioinformatics tools to predict interactions between SARS-CoV-2 and zebrafish proteins.
- Key Findings: rSpike inoculation significantly increased mRNA levels of all inflammatory and oxidative stress markers across most tissues. PBM treatment effectively downregulated the expression of these markers and improved survival rates, demonstrating its potential as an anti-inflammatory intervention.
Machine Learning for CRS Diagnosis Support
A machine learning (ML) approach has been proposed to address the challenge of swift CRS diagnosis in CAR-T cell therapy patients, where data scarcity is a common limitation. [121]
Detailed Methodology: [121]
- Data Source: Patient cytokine concentration data (e.g., peak IL-6 levels).
- Data Augmentation: A novel method to overcome limited training data by augmenting real patient data with statistical knowledge extracted from the domain literature.
- Model Training: Machine learning algorithms are trained on the augmented dataset to identify patterns indicative of CRS onset.
- Interpretable Outputs: The model is designed to not only predict CRS but also to provide supporting evidence from past clinical studies, making the results more actionable for clinicians.
- Performance: The proposed method achieved more than 90% accuracy in CRS identification and outperformed purely data-driven alternatives in some scenarios.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents and Models for Cytokine Storm Research
| Item / Reagent | Function / Application | Example Use Case |
|---|---|---|
| Recombinant Viral Proteins | To induce specific, pathogen-associated inflammatory responses in vitro and in vivo. | Studying SARS-CoV-2 pathogenesis using rSpike protein in zebrafish models. [120] |
| CAR-T Cells | Autologous T-cells engineered to target tumor antigens; used to study therapy-induced CRS. | Investigating the pathophysiology and treatment of axi-cel or tisa-cel associated CRS. [117] |
| Cytokine-Specific Antibodies | For neutralization studies, immunoassays (ELISA), and immunohistochemistry to quantify and localize cytokines. | Measuring serum levels of IL-6, IFN-γ, IP-10 in patients with viral infections or CRS. [1] [119] |
| JAK-STAT Pathway Inhibitors | Small molecule inhibitors (e.g., JAK1/2 inhibitors) to dissect signaling pathways and as therapeutic candidates. | Testing the efficacy of JAK inhibition to mitigate CRS in CAR-T therapy or COVID-19. [1] [16] |
| Animal Disease Models | In vivo systems (e.g., zebrafish, mouse) to study CS pathophysiology and intervention. | Modeling COVID-19-associated CSS and testing PBM therapy in zebrafish. [120] |
Visualization of Signaling Pathways
The JAK-STAT signaling pathway is a critical mediator of cytokine storm pathogenesis, activated by numerous cytokines including IL-6, IFN-γ, and others. The following diagram illustrates the key components and sequence of events in this pathway, highlighting potential therapeutic targets. [1] [16]
JAK-STAT Pathway in Cytokine Storm
Real-world evidence and post-market surveillance are indispensable for understanding the full clinical spectrum of cytokine storm and its progression to multiple organ failure. Data from sources like the FAERS database reveal therapy-specific safety profiles and emerging risks, while clinical studies of infections like SARS-CoV-2 quantify key cytokine dynamics and organ-specific injury patterns. The integration of advanced experimental models, from zebrafish to machine learning, provides powerful tools for deconstructing the complex pathophysiology of CS and MODS. This comprehensive, evidence-based approach is fundamental for developing targeted, effective treatments to improve outcomes for patients experiencing these life-threatening conditions.
Conclusion
The pathogenesis of cytokine storm-driven multiple organ failure is centrally governed by a self-amplifying loop of inflammatory cell death, particularly PANoptosis, and hyperactivation of key signaling pathways like JAK/STAT. While targeted biologics and signaling inhibitors represent a paradigm shift in management, significant challenges remain in patient stratification, managing late-stage immunosuppression, and cost-effective access. Future research must focus on defining combination therapy protocols, validating novel biomarkers for precision medicine, and developing integrated care algorithms that address the entire disease continuum. For biomedical and clinical research, the priority lies in translating mechanistic insights into next-generation immunomodulators and digital monitoring platforms to ultimately improve survival and functional recovery in this critical condition.
References
- 1. Deep insight into cytokine storm: from pathogenesis to ... [https://www.nature.com/articles/s41392-025-02178-y]
- 2. Cytokine storm [https://en.wikipedia.org/wiki/Cytokine_storm]
- 3. The origins of a cytokine storm [https://www.cellgs.com/blog/the-origins-of-a-cytokine-storm.html]
- 4. A port in the storm [https://www.pennmedicine.org/news/a-port-in-the-storm]
- 5. Deep insight into cytokine storm: from pathogenesis to ... [https://pubmed.ncbi.nlm.nih.gov/40234407/]
- 6. The 'Cytokine Storm': molecular mechanisms and therapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9310545/]
- 7. Biomarkers of cytokine storm as red flags for severe and ... [https://pubmed.ncbi.nlm.nih.gov/34185801/]
- 8. The Impact of Cytokine Storms on Severe Infectious ... [https://jpmsonline.com/article/the-impact-of-cytokine-storms-on-severe-infectious-diseases-progression-a-narrative-review-720/]
- 9. Cytokine Storm Induction Linked to Multi‐Organ Failure in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12499386/]
- 10. Roles of cytokine storm in sepsis progression [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1696366/full]
- 11. The innate immune response in SARS-CoV2 infection [https://pmc.ncbi.nlm.nih.gov/articles/PMC12537681/]
- 12. Longitudinal soluble marker profiles reveal strong ... [https://www.nature.com/articles/s41598-024-63586-8]
- 13. Autoimmune Diseases: Molecular Pathogenesis and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12171081/]
- 14. Recent updates in the clinical trials of therapeutic ... [https://www.sciencedirect.com/science/article/pii/S2405844021002632]
- 15. Ruxolitinib for Emergency Treatment of COVID-19- ... [https://pubmed.ncbi.nlm.nih.gov/40197709/]
- 16. Role of SARS-CoV-2-induced cytokine storm in multi-organ ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9637536/]
- 17. Transmembrane TNF-α as a Novel Biomarker for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9473472/]
- 18. Interferon γ and Its Important Roles in Promoting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6396335/]
- 19. IFNγ in human sepsis: a scoping review [https://annalsofintensivecare.springeropen.com/articles/10.1186/s13613-025-01534-z]
- 20. Interleukin-1 in the pathogenesis and treatment of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3083294/]
- 21. IL-1 family cytokines in inflammation and immunity [https://www.nature.com/articles/s41423-025-01358-8]
- 22. Innate immune role of IL-6 in influenza a virus pathogenesis [https://pmc.ncbi.nlm.nih.gov/articles/PMC12277322/]
- 23. Specific cytokines in the inflammatory cytokine storm of ... [https://virologyj.biomedcentral.com/articles/10.1186/s12985-021-01588-y]
- 24. Interleukin 1α: a comprehensive review on the role of IL ... [https://www.sciencedirect.com/science/article/pii/S1568997221000227]
- 25. PANoptosis in cancer: bridging molecular mechanisms to ... [https://www.nature.com/articles/s41423-025-01329-z]
- 26. Innate Sensors, Inflammasomes, and RIPKs in PANoptosomes [https://pmc.ncbi.nlm.nih.gov/articles/PMC10842719/]
- 27. PANoptosis in Cytokine Release Syndrome: Bridging the ... [https://pubmed.ncbi.nlm.nih.gov/41102952/]
- 28. PANoptosis in Sepsis: A Central Role and Emerging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12085136/]
- 29. PANoptosis in neurological disorders: mechanisms ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1579360/full]
- 30. Wiring and rewiring PANoptosis: Molecular vulnerabilities ... [https://www.sciencedirect.com/science/article/abs/pii/S1359610125001315]
- 31. The role of inflammasomes in human diseases and their ... [https://www.nature.com/articles/s41392-023-01687-y]
- 32. JAK-STAT signaling in inflammation and stress-related diseases [https://pmc.ncbi.nlm.nih.gov/articles/PMC10632324/]
- 33. Inflammasomes and Signaling Pathways: Key Mechanisms in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12191029/]
- 34. Comprehending toll-like receptors: pivotal element in the ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1591011/full]
- 35. The JAK-STAT pathway: from structural biology to cytokine ... [https://www.nature.com/articles/s41392-024-01934-w]
- 36. JAK Inhibitors in Cytokine Storm Syndromes [https://pubmed.ncbi.nlm.nih.gov/39117841/]
- 37. Special Issue “The Role of Toll-Like Receptors (TLRs) in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11396464/]
- 38. Apolipoprotein C3 induces inflammation and organ ... [https://www.nature.com/articles/s41590-019-0548-1]
- 39. Hyperinflammation, apoptosis, and organ damage - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9335505/]
- 40. Serum amyloid A protein in cancer prognosis [https://pmc.ncbi.nlm.nih.gov/articles/PMC8798074/]
- 41. Prognostic value of serum amyloid A protein as ... [https://www.sciencedirect.com/science/article/abs/pii/S0882401024004212]
- 42. Understanding the value of monocyte distribution width ... [https://www.nature.com/articles/s41598-024-65883-8]
- 43. The Role of Monocyte Distribution Width (MDW) in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11858437/]
- 44. Performance of the neutrophil-to-lymphocyte ratio as a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12318771/]
- 45. The early predictive roles of NLR and NE% in in-hospital ... [https://www.sciencedirect.com/science/article/pii/S2405844024025945]
- 46. Cytokine profiles as predictive biomarkers for treatment ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12049293/]
- 47. NLR stability predicts response to immune checkpoint ... [https://www.nature.com/articles/s41598-024-68048-9]
- 48. The Research Trends and Hotspots of Sepsis and Multiple ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12554285/]
- 49. Role of T cells and cytokines in the pathogenesis of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12538455/]
- 50. Multi-organ pathology in a small porcine model of cytokine ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1618665/full]
- 51. Antibodies targeting the shared cytokine receptor IL-1 receptor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11587196/]
- 52. The JAK/STAT signaling pathway: from bench to clinic [https://www.nature.com/articles/s41392-021-00791-1]
- 53. JAK-STAT Pathway Inhibition and their Implications in COVID ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7784782/]
- 54. Small molecule drug discovery targeting the JAK-STAT ... [https://www.sciencedirect.com/science/article/pii/S1043661824001610]
- 55. Targeting JAK-STAT Signaling to Control Cytokine Release ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7298494/]
- 56. A review of Janus kinase inhibitors for the treatment of Covid ... [https://inflammregen.biomedcentral.com/articles/10.1186/s41232-022-00253-3]
- 57. Ruxolitinib for Emergency Treatment of COVID‐19 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11976455/]
- 58. JAK inhibition as a new treatment strategy for patients with ... [https://www.sciencedirect.com/science/article/pii/S0006295222002568]
- 59. Neurological Adverse Events Associated with the Use of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11944788/]
- 60. Extracorporeal Cytokine Adsorption in Sepsis - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12292210/]
- 61. Haemoadsorption to remove inflammatory mediators in sepsis [https://icm-experimental.springeropen.com/articles/10.1186/s40635-025-00740-0]
- 62. Haemoadsorption in Critically Ill Patients: The New Frontier [https://healthmanagement.org/c/icu/issuearticle/haemoadsorption-in-critically-ill-patients-the-new-frontier]
- 63. Investigation of Inflammatory Reduction During ... [https://www.mdpi.com/2077-0383/14/5/1686]
- 64. Point‐of‐care detection of cytokines in cytokine storm ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8242812/]
- 65. A matched case-control study on the effectiveness of ... [https://www.nature.com/articles/s41598-023-40719-z]
- 66. Extracorporeal Cytokine Removal in Critically Ill COVID-19 ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2021.760435/full]
- 67. Roles of cytokine storm in sepsis progression - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12623314/]
- 68. Harnessing immunity: Immunomodulatory therapies in COVID ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11229839/]
- 69. Evaluation of the Efficacy of Tocilizumab in Cytokine Release ... [https://behmedicalbulletin.org/articles/evaluation-of-the-efficacy-of-tocilizumab-in-cytokine-release-syndrome-in-patients-with-covid-19-sars-cov-2-pneumonia-followed-in-the-intensive-care-unit/BMB.galenos.2025.92400]
- 70. Early detection of cytokine storm and IgG levels to predict ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12633999/]
- 71. Inspiration for COVID-19 Treatment: Network Analysis and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8957998/]
- 72. Hazards of the Cytokine Storm and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7428145/]
- 73. The cytokine storm and COVID‐19 - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC7361342/]
- 74. Immune Dysregulation in Sepsis. A Narrative Review for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12561552/]
- 75. The Interleukin Network in Sepsis: From Cytokine Storm to ... [https://www.mdpi.com/2075-4418/15/22/2927]
- 76. -induced Sepsis : immunosuppression , diagnosis and... mechanisms [https://mmrjournal.biomedcentral.com/articles/10.1186/s40779-022-00422-y]
- 77. Risk factors, biomarkers, and mechanisms for persistent ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11347813/]
- 78. Frontiers | Sepsis -induced immunosuppression : mechanisms ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1577105/full]
- 79. Potential Pathophysiological Mechanisms Underlying Multiple ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9007670/]
- 80. Bringing Lower-Cost Biosimilar Drugs to American Patients [https://www.hhs.gov/press-room/fact-sheet-bringing-lower-cost-biosimilar-drugs-to-american-patients.html]
- 81. The cytokine storm and factors determining the sequence ... [https://www.sciencedirect.com/science/article/abs/pii/S0735675707007097]
- 82. FDA Modernizes Biosimilar Approval to Cut Costs and ... [https://www.dermatologytimes.com/view/fda-modernizes-biosimilar-approval-to-cut-costs-and-speed-access]
- 83. The Economics of Biosimilars - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4031732/]
- 84. Slack in the infrastructure of intensive care units: resilience ... [https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-023-09495-4]
- 85. Challenges of Redeployment to ICU: A Qualitative Study ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12181713/]
- 86. Top 5 biggest challenges in a hospital ICU [https://healthcare-digital.com/hospitals/top-5-biggest-challenges-in-a-hospital-icu]
- 87. Machine learning-based predictive model for high [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1692892/full]
- 88. Multi-Dimensional Characterization of Programmed Cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12628821/]
- 89. Early prediction and warning of MODS following major ... [https://www.sciencedirect.com/science/article/pii/S1008127525001075]
- 90. Cytokines in sepsis: a critical review of the literature on ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1682306/full]
- 91. Cytokine release syndrome and CAR T Cell therapy [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1615526/full]
- 92. The key mechanisms underlying severe COVID-19 [https://pubmed.ncbi.nlm.nih.gov/39884914/]
- 93. Mechanism of Sepsis [https://www.mdpi.com/2673-5261/6/3/18]
- 94. Latest updates on pathogenesis mechanisms and ... [https://pubmed.ncbi.nlm.nih.gov/40536724/]
- 95. Cytokine elevation in severe and critical COVID-19 [https://pmc.ncbi.nlm.nih.gov/articles/PMC7567529/]
- 96. Cytokine profiles dynamics in COVID-19 patients [https://www.nature.com/articles/s41598-025-98505-y]
- 97. Pharmaco-immunomodulatory interventions for averting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8769772/]
- 98. Frontiers | Single-Cell RNA Sequencing of Tocilizumab-Treated ... [https://frontiersin.org/articles/10.3389/fgene.2020.610682/full]
- 99. Inhibition of cytokine signaling by ruxolitinib and implications ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7308779/]
- 100. Efficacy and safety of SARS-CoV-2 neutralizing antibody, ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12166818/]
- 101. Efficacy of tocilizumab for hospitalized patients with COVID-19 pneumonia and high IL-6 levels: A randomized controlled trial | Infection [https://link.springer.com/article/10.1007/s15010-025-02506-y]
- 102. Treatment of Severe COVID-19 with Tocilizumab Mitigates Cytokine Storm and Averts Mechanical Ventilation during Acute Respiratory Distress: A Case Report and Literature Review [https://www.mdpi.com/2414-6366/5/3/112]
- 103. A Multicenter Phase II Trial of Ruxolitinib for Treatment ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11568950/]
- 104. From Small Molecules to Biologics, New Modalities in Drug ... [https://chemaxon.com/blog/small-molecules-vs-biologics]
- 105. Biologics vs Small Molecules: A New Era in Drug ... [https://synergbiopharma.com/biologics-vs-small-molecules/]
- 106. Small Molecules vs. Biologics: Key Drug Differences [https://www.allucent.com/resources/blog/points-consider-drug-development-biologics-and-small-molecules]
- 107. What's Trending: New Drug Approvals: Biologics [https://www.dcatvci.org/features/whats-trending-new-drug-approvals-biologics/]
- 108. Delving deeper in the eye of the hurricane - PubMed [https://pubmed.ncbi.nlm.nih.gov/40945384/]
- 109. Special Issue “Molecular Mechanisms and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12524862/]
- 110. Beyond SOFA and APACHE II, Novel Risk Stratification ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12071242/]
- 111. Comparison of Intensive Care Scoring Systems in Predicting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12248853/]
- 112. Roles of cytokine storm in sepsis progression: biomarkers, ... [https://pubmed.ncbi.nlm.nih.gov/41262247/]
- 113. Recent advances in biomarkers for detection and diagnosis of ... [https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-025-03324-6]
- 114. FDA Approves Expanded Indication for Avtozma ... [https://www.drugs.com/newdrugs/fda-approves-expanded-indication-avtozma-tocilizumab-anoh-intravenous-iv-formulation-cytokine-6589.html]
- 115. Regulatory Status Overview CytoSorbents Products [https://cytosorbents.com/regulatory-status/]
- 116. Case Report: Successful treatment of severe fever with ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1566719/full]
- 117. Post-Marketing Surveillance of CAR-T-Cell Therapies [https://pmc.ncbi.nlm.nih.gov/articles/PMC9360149/]
- 118. The cytokine and factors determining the sequence and... storm [https://pubmed.ncbi.nlm.nih.gov/18606328/]
- 119. Quantification of Cytokine Storms During Virus Infections - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8165266/]
- 120. Photobiomodulation Reduces the Cytokine Storm ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10094635/]
- 121. Supporting cytokine storm detection during CAR-T cell ... [https://www.sciencedirect.com/science/article/pii/S1532046423000886]