Monitoring Antibiotic-Induced Structural Integrity (AISI) in Abscess Treatment: A Critical Paradigm for Drug Development
This article provides a comprehensive framework for researchers and drug development professionals on the critical role of monitoring Antibiotic-Induced Structural Integrity (AISI) during abscess treatment.
Monitoring Antibiotic-Induced Structural Integrity (AISI) in Abscess Treatment: A Critical Paradigm for Drug Development
Abstract
This article provides a comprehensive framework for researchers and drug development professionals on the critical role of monitoring Antibiotic-Induced Structural Integrity (AISI) during abscess treatment. It explores the foundational science linking antibiotic action to abscess structural dynamics, details current and emerging methodologies for real-time AISI assessment, addresses common challenges and optimization strategies for integrating AISI into efficacy models, and validates its utility through comparative analysis with traditional endpoints. The synthesis presents AISI as a pivotal, translatable biomarker for accelerating the development of novel anti-infective therapies.
The Science of AISI: Decoding How Antibiotics Alter Abscess Architecture and Biofilm Integrity
Within the broader thesis on Advanced Infection Site Immunopathology (AISI), this document defines a critical paradigm shift. Traditional metrics for antibiotic efficacy focus on bacterial kill (reduction in CFU/g). However, therapeutic success, particularly in complex structures like abscesses, requires the resolution of the pathological host response. AISI encompasses the deleterious structural and molecular sequelae of persistent inflammation even as bacterial load declines. This includes widespread collagenolysis, parenchymal cell death (e.g., hepatocyte necrosis in hepatic abscesses), and microvascular destruction, leading to permanent functional loss. Monitoring AISI provides a more comprehensive biomarker for treatment response, predicting relapse and long-term morbidity. These Application Notes detail protocols for quantifying key AISI endpoints.
The following table summarizes primary quantitative endpoints for AISI assessment in a murine Staphylococcus aureus subcutaneous abscess model, comparing untreated infection versus antibiotic-treated (Linezolid, 50 mg/kg, BID, 7 days) groups at day 10 post-infection.
Table 1: Quantitative AISI Endpoints in S. aureus Abscess Model
| AISI Category | Specific Metric | Untreated (Mean ± SD) | Antibiotic-Treated (Mean ± SD) | Measurement Method | Implication |
|---|---|---|---|---|---|
| Bacterial Burden | Log₁₀ CFU/abscess | 7.8 ± 0.5 | 2.1 ± 0.9* | Homogenization & plating | Confirms antimicrobial efficacy. |
| Inflammatory Infiltrate | % Area CD45+ (IHC) | 68.5 ± 8.2% | 45.3 ± 10.1%* | Digital image analysis | Persistent inflammation post-clearance. |
| Structural Collapse (ECM) | Collagen Density (picrosirius red) | 12.4 ± 3.1% | 8.7 ± 2.5%* | Polarized light microscopy | Active collagen degradation. |
| Structural Collapse (ECM) | MMP-9 Activity (RLU/mg protein) | 12500 ± 2100 | 8500 ± 1500* | Luminescence assay | Proteolytic enzyme activity. |
| Parenchymal Damage | % TUNEL+ Nuclei | 32.4 ± 6.5% | 18.9 ± 5.2%* | TUNEL assay on tissue section | Ongoing cell death despite treatment. |
| Vascular Integrity | Microvessel Density (CD31+ vessels/mm²) | 155 ± 28 | 210 ± 35* | Immunofluorescence quantification | Incomplete vascular recovery. |
- p < 0.01 vs. Untreated, Student's t-test.
Experimental Protocols
Protocol 3.1: Multiplex MMP Activity Assay in Abscess Homogenate
Objective: Quantify activity of key matrix metalloproteinases (MMP-2, MMP-9, MMP-13) driving structural collapse. Materials: Abscess tissue, lysis buffer (without EDTA), fluorogenic MMP-substrate probes (specific for each MMP), inhibitor standards (GM6001, specific inhibitors), 96-well black plate, fluorescence microplate reader. Procedure:
- Homogenize abscess tissue in cold lysis buffer. Centrifuge at 12,000g for 10 min at 4°C.
- Determine total protein concentration (BCA assay).
- Prepare reaction mix: 50 µg total protein, 50 µM substrate probe, in assay buffer (50 mM Tris, 150 mM NaCl, 10 mM CaCl₂, pH 7.5). Final volume: 100 µL/well.
- For inhibition control, pre-incubate sample with 10 µM GM6001 for 30 min on ice.
- Load samples in triplicate onto a 96-well plate. Read immediately in kinetic mode (ex/em per substrate specs, e.g., 320/405 nm) every 5 min for 2 hours at 37°C.
- Calculate activity as slope of fluorescence increase (RFU/min), normalized to µg protein. Report as specific activity (inhibitable signal).
Protocol 3.2: Spatially-Resolved Transcriptomics for AISI Pathway Mapping
Objective: Map cytokine/chemokine and damage-associated molecular pattern (DAMP) expression within distinct abscess zones (necrotic core, inflammatory border, fibrous capsule). Materials: Fresh-frozen abscess tissue sections (10 µm), Visium Spatial Gene Expression slides & kit (10x Genomics), recommended fixation and H&E staining reagents, tissue permeabilization optimizer, DNB sequencer. Procedure:
- Follow manufacturer's guide for tissue preparation, fixation, H&E staining, and imaging.
- Permeabilize tissue for optimal mRNA capture (time determined by optimizer assay).
- Perform reverse transcription on-slide to generate cDNA with spatial barcodes.
- Harvest cDNA, construct libraries, and sequence on an Illumina system to a minimum depth of 50,000 reads per spot.
- Align to reference genome and analyze using Space Ranger and Seurat. Create zonal expression profiles for gene clusters (e.g.,
Il1b,Tnf,Cxcl2,Mmp9,S100a8,Col1a1).
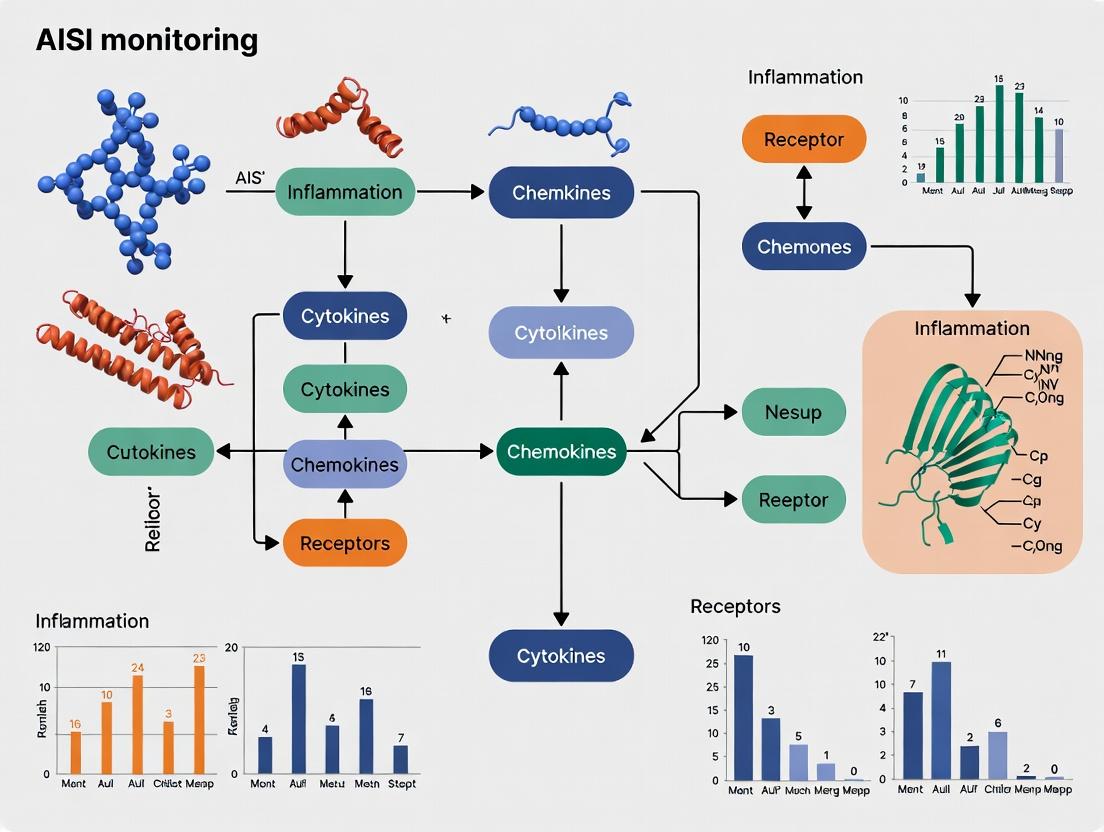
Visualization: Signaling Pathways and Workflows
Title: Core Signaling Pathway Driving AISI
Title: Integrated AISI Monitoring Experimental Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for AISI Research
| Reagent/Material | Supplier Example | Function in AISI Research |
|---|---|---|
| Fluorogenic MMP Substrate Probes (MMP-2/9/13 specific) | Abcam, R&D Systems | Selective, real-time quantification of proteolytic activity in homogenates or live imaging. |
| Luminex Multiplex Panels (Mouse Cytokine/DAMP 30-plex) | Thermo Fisher, MilliporeSigma | Simultaneous quantification of a broad panel of inflammatory mediators and DAMPs (e.g., HMGB1, S100A8/9) from limited sample volume. |
| Visium Spatial Tissue Optimization Slide & Kit | 10x Genomics | Determines optimal tissue permeabilization time for spatially-resolved RNA capture, critical for abscess architecture. |
| Anti-mouse CD45 Antibody (clone 30-F11), AF647 | BioLegend | Universal leukocyte marker for quantifying inflammatory infiltrate area via immunofluorescence/flow cytometry. |
| In Vivo Anti-Ly6G Depleting Antibody (clone 1A8) | Bio X Cell | Tool to neutropenic animals to dissect the specific role of neutrophils in driving collagenolysis and parenchymal damage. |
| Cell Death Detection Kit (TUNEL), Fluorescein | Roche/Sigma | Labels DNA fragmentation in tissue sections, quantifying ongoing apoptosis/necrosis within the abscess parenchyma. |
| Picrosirius Red Stain Kit | Polysciences, Inc. | Stains collagen fibrils; analyzed under polarized light to assess collagen density and architecture (birefringence). |
| Recombinant TIMP-1 Protein | PeproTech | Tissue inhibitor of metalloproteinases; used as a positive control or host-directed therapeutic in experiments. |
Application Note AN-101: Quantitative Monitoring of AISI During In Vivo Abscess Model Studies
Introduction Within the context of advancing therapeutic strategies for recalcitrant abscesses, monitoring the Acute Inflammatory Systemic Index (AISI) provides a crucial systemic biomarker for treatment efficacy. This note details protocols for correlating local pathophysiological mechanisms—specifically the formation of the protective fibrin cage and bacterial biofilm matrices—with systemic inflammatory markers in a murine model.
1. Pathophysiological Framework & Key Quantitative Data Abscess formation is a host-defense mechanism to contain infection, culminating in a structured necrotic core surrounded by a fibrin cage and often incorporating microbial biofilms. This environment creates a profound barrier to antibiotic penetration and immune clearance.
Table 1: Key Components of the Abscess Milieu and Their Measurable Parameters
| Component | Primary Function | Key Quantitative Metrics | Typical Measurement Range (Murine Model) | Detection Method |
|---|---|---|---|---|
| Fibrin Cage | Physical containment of infection; immune modulation | Fibrin deposition density, cross-link density (D-dimer levels in cavity), thickness (μm) | 50-200 μm thickness; D-dimer: 2-8 μg/mL in lavage | Histology (Masson's Trichrome), ELISA, SEM |
| Bacterial Biofilm | Antibiotic resistance; immune evasion; chronicity | Bacterial load (CFU), biomass (μm³/field), matrix polysaccharide (μg/mL) | CFU: 10⁷-10⁹ per abscess; alginate/PNAG: 5-50 μg/mL | Viable plating, Confocal Microscopy, Crystal Violet assay, ELISA |
| Infiltrating Immune Cells | Phagocytosis, pus formation, cytokine release | Neutrophil/Lymphocyte/Monocyte counts, cytokine conc. (IL-1β, TNF-α, IL-6) | IL-1β: 100-1000 pg/mL in lavage; Neutrophils: 60-80% of infiltrate | Flow cytometry, Multiplex ELISA, Differential counts |
| Systemic Inflammation (AISI) | Prognostic biomarker for treatment response | AISI = (Neutrophils × Monocytes × Platelets) / Lymphocytes | Baseline: 100-300; Severe Infection: >500 | Automated hemocytometer, CBC analysis |
Table 2: Impact of Therapeutic Interventions on Abscess Parameters & AISI
| Intervention Class | Target | Effect on Fibrin Cage | Effect on Biofilm | Correlative Change in AISI |
|---|---|---|---|---|
| Standard Antibiotic (e.g., Vancomycin) | Planktonic bacteria | Minimal reduction | Biomass reduction <1 log CFU | Slow decrease (>72h) if ineffective |
| Fibrinolytics (e.g., tPA) | Fibrin mesh | Significant degradation (~70% reduction) | Enhanced antibiotic penetration | Rapid initial spike (24h), then decline |
| Biofilm Dispersants (e.g., DNase) | eDNA matrix | No direct effect | Disruption of structure, ~2 log CFU increase in planktonic phase | Variable; may increase with bacteremia |
| Combination Therapy | Multiple | Partial degradation | Synergistic biomass reduction >3 log CFU | Most significant and sustained reduction |
2. Experimental Protocols
Protocol 2.1: Induction and Harvest of Sterile & Septic Abscesses in Mice
- Objective: To generate standardized abscesses for studying fibrin/biofilm formation and treatment.
- Materials: C57BL/6 mice (8-10 weeks), Staphylococcus aureus (USA300 strain), 10% sterile fecal slurry (for sterile abscess), 1mL syringes, 27G needles, isoflurane, euthanasia solution.
- Procedure:
- Anesthetize mouse and shave the lower back.
- Septic Abscess: Resuspend S. aureus at 1x10⁷ CFU in 100 μL PBS mixed with 100 μL of 10% sterile fecal slurry (provides a tissue irritant).
- Sterile Abscess (Control): Inject 200 μL of 10% sterile fecal slurry only.
- Inject subcutaneously into the shaved area to form a raised bleb.
- Monitor daily for abscess formation (palpable, raised lesion by day 3).
- At designated timepoints (e.g., days 3, 5, 7), euthanize mouse.
- Surgically excise the entire abscess, taking care not to rupture the capsule. Bisect: one half for histology, one for homogenization.
Protocol 2.2: Quantitative Analysis of the Fibrin Cage
- Objective: To measure fibrin deposition and cross-linking within the abscess wall.
- Materials: Abscess tissue, formalin, OCT compound, microtome, Masson's Trichrome stain, anti-fibrinogen antibody, D-dimer ELISA kit.
- Procedure:
- Fix half the abscess in 10% formalin for 24h, process, and embed in paraffin.
- Section at 5 μm and stain with Masson's Trichrome (fibrin stains red).
- Image sections under light microscope at 100x magnification. Use image analysis software (e.g., ImageJ) to measure the average thickness of the fibrin-rich wall from 10 random points per section.
- Homogenize the other half in 1 mL PBS with protease inhibitors. Centrifuge at 10,000xg for 10 min.
- Use the supernatant in a commercial D-dimer ELISA per manufacturer's instructions to quantify fibrin degradation products as an inverse marker of cross-linked fibrin stability.
Protocol 2.3: Evaluation of Biofilm In Situ and Biomass
- Objective: To visualize and quantify bacterial biofilm components within the abscess.
- Materials: LIVE/DEAD BacLight Bacterial Viability Kit, PNAG/alginate-specific antibodies, confocal microscope, microplate reader.
- Procedure:
A. Confocal Microscopy:
- Flash-freeze abscess half in OCT, section at 20 μm using a cryostat.
- Stain with SYTO 9 (green, live cells) and propidium iodide (red, dead cells) per BacLight protocol.
- For matrix staining, incubate with anti-PNAG primary antibody followed by AlexaFluor-647 conjugated secondary.
- Image using a confocal microscope with Z-stacking. Analyze biomass volume (μm³) using software like Imaris or COMSTAT. B. Crystal Violet Biomass Assay:
- Homogenize tissue in 1 mL PBS, sonicate briefly to disrupt aggregates.
- Plate 200 μL of homogenate in a 96-well plate, incubate static for 24h at 37°C to allow biofilm reformation.
- Fix with 99% methanol, stain with 0.1% crystal violet, solubilize in 30% acetic acid.
- Measure absorbance at 595 nm as a proxy for total biofilm biomass.
Protocol 2.4: AISI Calculation & Correlative Blood Analysis
- Objective: To determine systemic inflammatory status and correlate with local abscess pathology.
- Materials: Heparinized blood collection tubes, automated hematology analyzer, flow cytometer.
- Procedure:
- Prior to abscess harvest, collect ~500 μL of blood via retro-orbital or cardiac puncture into heparinized tubes.
- Perform a complete blood count (CBC) using an automated analyzer to obtain absolute counts for Neutrophils (N), Lymphocytes (L), Monocytes (M), and Platelets (P).
- Calculate AISI using the formula: AISI = (N x M x P) / L.
- For deeper immunophenotyping, use flow cytometry on PBMCs to assess neutrophil activation markers (CD11b, CD66b).
3. Visualizations
Diagram 1: Pathophysiological cascade in abscess formation
Diagram 2: Integrated workflow for correlative abscess research
4. The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Abscess Pathophysiology & AISI Research
| Reagent/Material | Supplier Examples | Function in Protocol |
|---|---|---|
| USA300 S. aureus Strain | ATCC, BEI Resources | Gold-standard biofilm-forming, abscess-causing pathogen for murine models. |
| Live/Dead BacLight Viability Kit | Thermo Fisher Scientific | Differentiates live/dead bacteria in confocal imaging of abscess biofilm. |
| Mouse D-dimer ELISA Kit | Abcam, MyBioSource | Quantifies fibrin turnover and cross-linking within the abscess cavity. |
| Cytometric Bead Array (CBA) Mouse Inflammation Kit | BD Biosciences | Multiplex quantification of key serum cytokines (IL-6, IL-10, TNF, MCP-1) linked to AISI. |
| Anti-PNAG (Poly-N-acetyl glucosamine) Antibody | BioXCell, Hycult Biotech | Specific detection of a major staphylococcal biofilm matrix component in tissue. |
| Recombinant Tissue Plasminogen Activator (tPA) | Genentech, Sigma-Aldrich | Pharmacological agent to degrade the fibrin cage in interventional studies. |
| DNase I (RNase-free) | Roche, Worthington Biochem | Disperses biofilm by degrading extracellular DNA (eDNA) matrix. |
| Automated Hematology Analyzer | Heska, Sysmex | Provides precise, automated complete blood counts (CBC) for accurate AISI calculation. |
This document serves as an Application Note within a broader thesis research program investigating Antibiotic-Induced Structural Integrity (AISI) monitoring during abscess treatment. AISI refers to the measurable disruption of bacterial cellular structures (cell wall, membrane, nucleic acids) caused by antibiotics, which is a critical pharmacokinetic/pharmacodynamic (PK/PD) parameter influencing treatment efficacy in deep-seated infections like abscesses. Understanding the precise mechanistic basis of this disruption is foundational for developing novel diagnostic and therapeutic monitoring strategies.
Antibiotic Classes: Mechanisms & Quantitative Disruption Data
The following table summarizes the primary structural targets, mechanisms of action, and key quantitative disruption parameters for major antibiotic classes. Data is sourced from current literature and pharmacopeial standards.
Table 1: Antibiotic Classes and Their Structural Disruption Mechanisms
| Antibiotic Class | Primary Target Component | Mechanism of Action | Key Quantitative Disruption Parameters (Typical Experimental Range) |
|---|---|---|---|
| Beta-Lactams | Peptidoglycan Cell Wall | Inhibit transpeptidase enzymes (PBPs), preventing cross-linking of peptidoglycan strands. | - MIC for S. aureus: 0.5 - 4 µg/mL (Methicillin) - Lytic concentration (osmotic shock): ≥ 4x MIC - PBP binding affinity (Kd): 1 - 50 nM |
| Glycopeptides | Peptidoglycan Precursors | Bind to D-Ala-D-Ala terminus of lipid II, blocking transglycosylation and transpeptidation. | - MIC for S. aureus: 1 - 2 µg/mL (Vancomycin) - Binding constant to Lipid II: ~10⁶ M⁻¹ |
| Polymyxins | Outer Membrane (LPS) | Displace Mg²⁺/Ca²⁺ from lipid A of LPS, disrupting outer membrane integrity. | - MIC for P. aeruginosa: 1 - 4 µg/mL (Colistin) - Outer membrane disruption (NPN assay): EC₅₀ ~0.5 - 2 µg/mL |
| Lipopeptides | Cytoplasmic Membrane | Cause Ca²⁺-dependent depolarization and disruption of the cytoplasmic membrane. | - MIC for S. aureus: 0.5 - 2 µg/mL (Daptomycin) - Membrane depolarization (DiSC₃(5) assay): >90% at 1x MIC |
| Quinolones | DNA Gyrase/Topoisomerase IV | Inhibit DNA supercoiling and promote double-stranded DNA breaks. | - MIC for E. coli: 0.03 - 0.125 µg/mL (Ciprofloxacin) - IC₅₀ for DNA gyrase: 0.1 - 1 µg/mL |
| Aminoglycosides | 30S Ribosomal Subunit | Bind to 16S rRNA, cause misreading of mRNA and inhibit translocation. | - MIC for E. coli: 2 - 8 µg/mL (Gentamicin) - Ribosomal binding affinity: Kd ~10⁻⁸ M |
Experimental Protocols for Assessing Structural Disruption
The following protocols are essential for quantifying AISI in the context of abscess treatment research.
Protocol 3.1: Assessment of Cell Wall Disruption (Beta-Lactam Action)
Objective: To quantify loss of structural integrity via osmotic protection assay. Workflow:
- Culture & Treatment: Inoculate mid-log phase Staphylococcus aureus (10⁶ CFU/mL) in Mueller-Hinton Broth (MHB). Add serially diluted beta-lactam (e.g., oxacillin, 0.125-16 µg/mL). Incubate (37°C, 2h).
- Osmotic Challenge: Divide treated culture. Pellet cells (5000xg, 10 min). Resuspend one pellet in distilled water (hypotonic lysis control). Resuspend the other in 0.5M sucrose (osmoprotectant).
- Integrity Measurement: Incubate suspensions (37°C, 30 min). Measure optical density at 600 nm (OD₆₀₀) at T=0 and T=30 min.
- Calculation: % Lysis = [(OD₆₀₀(T₀) - OD₆₀₀(T₃₀)) / OD₆₀₀(T₀)] x 100. Plot % lysis vs. antibiotic concentration to determine lytic concentration.
Protocol 3.2: Assessment of Membrane Disruption (Polymyxin/Daptomycin Action)
Objective: To quantify outer/cytoplasmic membrane damage using fluorescent probes. Part A: Outer Membrane Permeability (NPN Uptake)
- Sample Prep: Grow Pseudomonas aeruginosa to mid-log. Wash and resuspend in 5mM HEPES buffer (pH 7.2) to OD₆₀₀ ~0.5.
- Probe Addition: Add 1-N-phenylnaphthylamine (NPN) to final 10 µM.
- Treatment & Reading: Aliquot into a black 96-well plate. Add polymyxin B (0.25-16 µg/mL). Immediately measure fluorescence (ex/em 350/420 nm) kinetically for 10 min.
- Analysis: Calculate maximum fluorescence increase rate (RFU/min). EC₅₀ is the antibiotic concentration causing 50% of max fluorescence increase.
Part B: Membrane Depolarization (DiSC₃(5) Assay)
- Loading: Wash S. aureus cells, resuspend in buffer with 100 mM KCl. Add membrane potential-sensitive dye DiSC₃(5) (final 0.5 µM). Incubate (37°C, 30 min) until dye quenching is stable.
- Measurement: Aliquot into plate. Add daptomycin (in presence of 50 µg/mL Ca²⁺). Monitor fluorescence recovery (ex/em 622/670 nm).
- Analysis: Calculate % depolarization relative to maximum induced by gramicidin.
Visualization of Mechanisms and Experimental Workflows
Diagram 1: Antibiotic Structural Targets in Bacteria
Diagram 2: AISI Monitoring Experimental Workflow
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Key Reagent Solutions for Structural Disruption Assays
| Reagent/Material | Function/Application | Key Notes for AISI Research |
|---|---|---|
| Mueller-Hinton Broth (MHB) | Standardized medium for antibiotic susceptibility testing. | Use cation-adjusted (CA-MHB) for daptomycin and other cation-sensitive antibiotics. |
| HEPES Buffer (10-50mM, pH 7.2-7.4) | Physiological buffer for fluorescence and membrane assays. | Maintains stable pH without CO₂ control; essential for kinetic assays. |
| 1-N-phenylnaphthylamine (NPN) | Hydrophobic fluorescent probe for outer membrane permeability. | Increased fluorescence indicates NPN entry into phospholipid bilayer due to OM damage. |
| 3,3'-Dipropylthiadicarbocyanine Iodide (DiSC₃(5)) | Membrane potential-sensitive dye for cytoplasmic membrane depolarization. | Quenched in intact cells; fluorescence increases upon membrane depolarization and dye release. |
| SYTOX Green Nucleic Acid Stain | Impermeant DNA dye for monitoring loss of cytoplasmic membrane integrity. | Only enters cells with compromised membranes; >500x fluorescence enhancement upon DNA binding. |
| Osmoprotectants (Sucrose, PEG) | Provide osmotic support to protoplasts/spheroplasts. | 0.5M Sucrose standard for Gram-positives; distinguishes lysis from growth inhibition. |
| Cation Supplements (Ca²⁺, Mg²⁺) | Divalent cations critical for antibiotic activity and membrane stability. | 50 µg/mL Ca²⁺ is mandatory for daptomycin activity; Mg²⁺ affects polymyxin-LPS interaction. |
| Fluorimeter/Plate Reader | Device for kinetic/endpoint fluorescence and absorbance measurements. | Requires temperature control (37°C) and appropriate filter sets (e.g., 350/420nm for NPN). |
Application Notes Within the research framework of AISI (Acute Inflammatory Systemic Response Index) monitoring during abscess treatment, DNA, F-Actin, and EPS are critical structural biomarkers for quantifying the biofilm integrity of causative pathogens. These components form the structural scaffold of bacterial biofilms, which shield microorganisms from immune clearance and antibiotics, directly influencing AISI dynamics. Targeting these biomarkers allows for the assessment of therapeutic efficacy of novel biofilm-disrupting agents.
Table 1: Key Structural Biomarkers in Abscess Biofilms
| Biomarker | Primary Source | Function in Biofilm | Quantification Method | Correlation with AISI |
|---|---|---|---|---|
| Extracellular DNA (eDNA) | Mainly neutrophil extracellular traps (NETs) & bacterial lysis. | Structural adhesion, cation chelation, horizontal gene transfer. | Fluorescence (SYTOX Green, PicoGreen) or ELISA for histone-complexed DNA. | High eDNA levels correlate with persistent infection and elevated systemic inflammatory markers (e.g., IL-6, CRP). |
| F-Actin | Host-derived from infiltrating immune cells (e.g., neutrophils, macrophages). | Contributes to the biofilm's physical density and immune evasion. | Fluorescence staining (Phalloidin conjugates), Western Blot. | Presence indicates significant host-cell incorporation into the biofilm matrix, associated with a dysregulated immune response. |
| Polysaccharides (EPS) | Bacterial secretion (e.g., Psl, Pel, alginate in P. aeruginosa; PNAG in Staphylococci). | Primary matrix material, providing mechanical stability, hydration, and diffusion barrier. | Lectin-based staining (e.g., ConA), FTIR, Uronic acid assays. | High EPS density inversely correlates with antibiotic penetration and resolution of local and systemic inflammation. |
Detailed Protocols
Protocol 1: Concurrent Staining and Quantification of DNA & F-Actin in Abscess Biofilm Sections Objective: To visualize and quantify host and bacterial structural components within an in vivo abscess biofilm model.
- Tissue Preparation: Excise abscess tissue from animal model (e.g., mouse subcutaneous implant model). Embed in OCT compound. Cryosection at 10-20 µm thickness. Fix sections in 4% paraformaldehyde (15 min).
- Permeabilization and Blocking: Permeabilize with 0.1% Triton X-100 (10 min). Block with 3% BSA in PBS (1 hour).
- Staining:
- F-Actin: Incubate with Alexa Fluor 488-conjugated Phalloidin (1:200 in blocking buffer) for 1 hour.
- DNA: Incubate with DAPI (300 nM) or Propidium Iodide (PI, 1 µg/mL) for 10 minutes.
- Optional Bacterial Stain: Include SYTO 63 (1 µM) for 15 min to differentiate bacterial cells.
- Imaging and Analysis: Image using confocal microscopy. Quantify integrated fluorescence density for each channel using ImageJ software. Calculate co-localization coefficients (Manders' M1/M2) for F-Actin/DNA.
Protocol 2: EPS Extraction and Polysaccharide Quantification from Abscess Debris Objective: To isolate and quantify the polysaccharide component of EPS from abscess material.
- Sample Homogenization: Homogenize excised abscess tissue or harvested biofilm in 0.9% NaCl on ice.
- EPS Extraction: Centrifuge homogenate (10,000 x g, 20 min, 4°C). Resuspend pellet in 10 mL of 0.9% NaCl with 2 mM EDTA. Vortex vigorously for 30 sec. Place sample in a 60°C water bath for 30 min. Centrifuge again (13,000 x g, 30 min).
- EPS Recovery: Collect the supernatant containing crude EPS. Precipitate EPS by adding 3 volumes of cold absolute ethanol and incubating at -20°C overnight. Pellet precipitated EPS by centrifugation (15,000 x g, 30 min, 4°C).
- Quantification – Uronic Acid Assay: Resuspend EPS pellet in 1 mL distilled water. Perform the carbazole-sulfuric acid assay using D-glucuronic acid as a standard. Measure absorbance at 530 nm.
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in Research |
|---|---|
| Alexa Fluor-conjugated Phalloidin | High-affinity probe for selective staining of filamentous actin (F-Actin) for fluorescence microscopy. |
| SYTOX Green Nucleic Acid Stain | Cell-impermeant DNA dye for specific staining of extracellular DNA (eDNA) and dead cell DNA. |
| Wheat Germ Agglutinin (WGA), ConA Lectin Conjugates | Binds to specific EPS polysaccharides (e.g., N-acetylglucosamine, mannose/glucose residues) for matrix visualization. |
| Dispersin B (DspB) Enzyme | Glycoside hydrolase that specifically degrades poly-N-acetylglucosamine (PNAG) EPS, used for functional disruption studies. |
| DNase I (RNase-free) | Enzyme for targeted degradation of eDNA scaffold to study its structural role and potentiate antibiotic efficacy. |
Diagram 1: Biomarker Role in AISI Modulation
Diagram 2: EPS & DNA Analysis Workflow
The Host-Pathogen-Structure Interface in Treatment Response
Application Notes
Context within AISI Monitoring in Abscess Treatment Research: Understanding the dynamic interface between host immune cells, pathogenic communities (often polymicrobial in abscesses), and the unique structural architecture of the abscess is critical for predicting and monitoring treatment response. This interface dictates antibiotic penetration, immune evasion, and the resolution of infection. Research within this thesis framework focuses on how Advanced Infection Site Imaging (AISI) and molecular profiling can decode this tripartite interaction to guide therapeutic intervention.
Key Quantitative Findings in Abscess Treatment Response
Recent studies highlight measurable parameters at the host-pathogen-structure interface that correlate with clinical outcomes.
Table 1: Quantitative Biomarkers of Treatment Response at the Abscess Interface
| Biomarker Category | Specific Measurable Parameter | Correlation with Positive Treatment Response | Typical Assay/Method | Reference Range in Responding Murine Models* |
|---|---|---|---|---|
| Pathogen Burden | Bacterial CFU/g tissue | Decrease > 2-log10 | Quantitative culture, qPCR | < 10^3 CFU/g |
| Host Immune | Neutrophil Ly6G+ cell density in abscess wall | Initial increase, then resolution (bell curve) | Flow cytometry, IHC | Peak: ~40% of live cells; Resolution: <10% |
| Host Immune | M2/M1 Macrophage Ratio | Increase > 2-fold | RNA-seq (Arg1 vs. iNos), IHC | Ratio > 2.0 at treatment day 7 |
| Structural Integrity | Collagen Density (Abscess Capsule) | Stabilization, then gradual decrease | Masson's Trichrome, SHG imaging | Peak density: ~60% area; Late phase: ~30% area |
| Pharmacokinetic | Antibiotic Concentration in Abscess Core | >10x MIC of target pathogen | LC-MS/MS, microdialysis | Variable by drug; e.g., Vancomycin >20 µg/mL |
| Microbial Community | Diversity Index (Shannon) | Decrease in dysbiosis, shift towards commensals | 16S rRNA sequencing | Pre-treatment: 1.5; Post-treatment: 2.8 |
Values are illustrative from aggregated recent murine *S. aureus abscess model studies.
Table 2: AISI Modalities for Interface Monitoring
| Imaging Modality | Target at Interface | Measurable Output | Utility in Treatment Monitoring |
|---|---|---|---|
| Multiphoton Microscopy (in vivo) | Collagen structure (SHG), immune cell motility (2PEF) | Capsule thickness, neutrophil migration velocity | Real-time assessment of structural integrity and immune response |
| MALDI-TOF IMS | Spatial distribution of metabolites, host & pathogen proteins | Heat maps of antibiotic penetration, bacterial virulence factors | Mapping drug distribution relative to bacterial niches |
| μCT (Micro-Computed Tomography) | 3D abscess volume, gas pockets | Total abscess volume (mm³) | Quantitative tracking of abscess resolution or expansion |
| Fluorescence Hybridization (FISH) | Specific pathogen localization within structure | Co-localization coefficient of pathogen with hypoxic zones | Identifying sanctuaries of persistent infection |
Experimental Protocols
Protocol 1: Integrated Sampling for Multi-Omic Analysis from a Murine Abscess Model
Objective: To simultaneously recover quantitative data on pathogen load, host transcriptome, and microbial community structure from a single abscess lesion.
Materials: See "Scientist's Toolkit" below. Procedure:
- Euthanize mouse per approved IACUC protocol at designated time point post-treatment initiation.
- Aseptically excise the entire abscess lesion. Place in a sterile petri dish on ice.
- Longitudinal Sectioning: Using a sterile scalpel, bisect the abscess sagittally.
- Compartmentalized Processing:
- Abscess Core (Necrotic Center): Gently collect 20-30 mg of necrotic material. Divide:
- Slice 1 (10 mg): Homogenize in 1 mL PBS for serial dilution and CFU plating on appropriate agar.
- Slice 2 (10 mg): Place in DNA/RNA Shield reagent for 16S rRNA gene sequencing and bacterial RNA extraction.
- Abscess Wall (Capsule & Inflammatory Zone): Carefully dissect the fibrous wall. Divide:
- Slice 1 (20 mg): Place in RNAlater for host RNA-seq analysis.
- Slice 2: Place in 10% neutral buffered formalin for histology (H&E, Masson's trichrome).
- Slice 3 (30 mg): Digest in collagenase/DNase I solution for 45 min at 37°C to prepare a single-cell suspension for flow cytometry (CD45+, Ly6G+, F4/80+, CD206+).
- Abscess Core (Necrotic Center): Gently collect 20-30 mg of necrotic material. Divide:
- Parallel AISI: For correlative imaging, a separate cohort of animals should be imaged in vivo (e.g., μCT for volume, multiphoton for capsule dynamics) prior to sacrifice and sampling.
Protocol 2: Spatial Pharmacokinetic-Pharmacodynamic (PK-PD) Mapping via MALDI-TOF Imaging Mass Spectrometry
Objective: To visualize the distribution of an antibiotic relative to bacterial locations and host tissue structures in abscess sections.
Materials: Cryostat, conductive ITO slides, matrix (e.g., α-CHCA for small molecules), MALDI-TOF/TOF instrument, calibration standards. Procedure:
- Tissue Preparation: Snap-freeze abscess tissue in optimal cutting temperature (OCT) compound. Section at 10-12 µm thickness using a cryostat.
- Mounting: Thaw-mount sections onto pre-chilled ITO-coated glass slides. Dry in a desiccator for 30 min.
- Matrix Application: Apply a homogeneous layer of matrix solution (e.g., α-CHCA at 7 mg/mL in 50:50 ACN:0.2% TFA) using an automated sprayer (e.g., TM-Sprayer).
- MALDI-TOF IMS Data Acquisition:
- Calibrate instrument using standard spots adjacent to tissue.
- Define imaging raster area with a spatial resolution of 50-100 µm.
- Acquire mass spectra in positive ion mode, targeting the m/z of the protonated antibiotic molecule (e.g., Vancomycin, [M+H]⁺ m/z 1449.6).
- In parallel, acquire data for a bacterial biomarker (e.g., Phosphatidylglycerol PG(34:1) at m/z 773.5) and a host tissue biomarker (e.g., heme at m/z 616.2).
- Data Analysis: Use software (e.g., SCiLS Lab) to generate ion heat maps. Co-register with subsequent H&E staining of the same section. Calculate the percentage of bacterial signal area that overlaps with antibiotic signal above a threshold (e.g., 10x MIC equivalent).
Diagrams
Title: Core Interface in Abscess Treatment
Title: Integrated AISI & Multi-Omic Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Host-Pathogen-Structure Interface Experiments
| Item | Function in Experiment | Example Product/Catalog Number (Illustrative) |
|---|---|---|
| DNA/RNA Shield | Preserves nucleic acid integrity in heterogeneous abscess tissue at point of collection for later NGS. | Zymo Research R1100 |
| Collagenase/DNase I Digestion Mix | Liberates viable immune cells from the dense abscess capsule for high-quality flow cytometry. | Miltenyi Biotec 130-095-942 |
| Viability Dye (e.g., Zombie NIR) | Distinguishes live/dead cells in inflammatory, necrotic tissue digests for accurate immunophenotyping. | BioLegend 423106 |
| Metal-Labeled Antibody Panel (CyTOF) | For deep, multiplexed immune profiling (40+ markers) from limited abscess wall samples. | Fluidigm Maxpar Direct Immune Profiling Assay |
| MALDI-TOF IMS Matrix (α-CHCA) | Enables laser desorption/ionization of small molecule drugs (antibiotics) in tissue for spatial PK. | Sigma-Aldrych 70990 |
| Bacterial LIVE/DEAD Stain (e.g., SYTO BC/PI) | Quantifies total vs. membrane-compromised bacteria in abscess cores pre/post treatment. | Thermo Fisher L7012 |
| Hypoxia Probe (e.g., Pimonidazole HCl) | Binds covalently to proteins in hypoxic zones (<1.3% O2), key abscess feature; detectable by IHC. | Hypoxyprobe HP2-1000Kit |
| Luminescent Substrate for Bacterial Load | Enables rapid, non-destructive bioluminescent imaging of bacterial burden in vivo over time. | PerkinElmer D-Luciferin, K⁺ salt 122799 |
| Cryo-embedding Medium (OCT) | Preserves tissue architecture and spatial distribution of molecules for cryosectioning and IMS. | Sakura Finetek 4583 |
| RNAlater Stabilization Solution | Stabilizes host RNA profile immediately upon tissue dissection for downstream transcriptomics. | Thermo Fisher AM7020 |
Tools and Techniques: Practical Methods for Real-Time AISI Assessment in Preclinical and Clinical Settings
Application Notes: Imaging Modalities for AISI Monitoring
Monitoring Acute Inflammatory and Systemic Immune (AISI) responses during abscess treatment research necessitates high-resolution, three-dimensional, and longitudinal imaging of tissue structure, immune cell dynamics, and vascular remodeling. The following modalities offer complementary capabilities for this thesis context.
Multiphoton Microscopy (MPM):
- Primary Application in Thesis: In vivo, deep-tissue imaging of immune cell trafficking (e.g., neutrophils, macrophages) and collagen matrix remodeling in and around the abscess cavity over time.
- Key Advantages: Superior imaging depth (~1 mm in scattering tissue), inherent optical sectioning, reduced phototoxicity outside the focal plane, and intrinsic contrast from Second Harmonic Generation (SHG) for fibrillar collagen.
- Limitations: Expensive laser systems required, slower acquisition for large volumes compared to OCT.
Confocal Laser Scanning Microscopy (CLSM):
- Primary Application in Thesis: High-resolution, multiplex immunofluorescence analysis of fixed abscess tissue sections to quantify specific immune cell populations (e.g., CD68+ macrophages, Ly6G+ neutrophils), cytokine expression, and bacterial localization in 3D.
- Key Advantages: High spatial resolution (~0.2 μm lateral), excellent fluorescence detection efficiency, and well-established protocols for multiplex staining.
- Limitations: Limited imaging depth in living tissue (<~100 μm) due to out-of-focus light and scattering; typically used ex vivo or in superficial in vivo preparations.
Optical Coherence Tomography (OCT):
- Primary Application in Thesis: Rapid, non-invasive longitudinal monitoring of abscess morphology (size, capsule thickness), surrounding vasculature (angiography-OCTA), and tissue birefringence (polarization-sensitive OCT) to track fibrosis.
- Key Advantages: Very fast acquisition (video-rate), greatest imaging depth (1-3 mm in tissue), clinical translation potential. OCTA visualizes microvasculature without exogenous dyes.
- Limitations: Lower resolution (~1-15 μm) than MPM/CLSM; primarily structural/angiographic with limited molecular specificity unless combined with contrast agents.
Table 1: Quantitative Comparison of Key Imaging Modalities for AISI Monitoring
| Parameter | Multiphoton Microscopy | Confocal Microscopy | Optical Coherence Tomography |
|---|---|---|---|
| Lateral Resolution | 0.3 - 0.8 μm | 0.2 - 0.5 μm | 1 - 15 μm |
| Axial Resolution | 0.8 - 2.0 μm | 0.5 - 1.5 μm | 3 - 7 μm (in tissue) |
| Imaging Depth | Up to ~1 mm | Up to ~100 μm (in vivo) | 1 - 3 mm |
| Acquisition Speed | Moderate (ms/pixel) | Fast (μs/pixel) | Very Fast (kHz A-scan rate) |
| Key Contrast Mechanisms | 2PEF, SHG, THG | Fluorescence, Reflection | Backscatter, Polarization, Doppler |
| Primary Use Case | In vivo deep cell dynamics & collagen | Ex vivo multiplex 3D phenotyping | In vivo longitudinal morphology & angiography |
Experimental Protocols
Protocol A: LongitudinalIn VivoAISI Monitoring using MPM and OCT
Objective: To track abscess progression and immune response in a murine dorsal skinfold window chamber or ear model over 7 days. Materials: See "The Scientist's Toolkit" below. Procedure:
- Animal Model & Induction: Anesthetize mouse. For the window chamber, surgically implant the chamber. Induce a localized abscess via intradermal injection of 1x10^7 CFU S. aureus in 20 μL PBS mixed with 20 μL Cytodex beads.
- Multiphoton Imaging (Days 1, 3, 5, 7):
- Anesthetize animal and secure on heated stage.
- Intravenously inject 100 μL of 2.5 mg/mL FITC-Dextran (150 kDa) for vasculature contrast.
- Use a tunable Ti:Sapphire laser (excitation: 880 nm). Collect 2PEF signal (500-550 nm) from FITC and SHG signal (440 nm) from collagen through a 20x/1.0 NA water immersion objective.
- Acquire 3D z-stacks (300 x 300 x 150 μm, step size 2 μm) centered on the abscess border.
- OCT Imaging (Daily from Day 0):
- Immediately following MPM, acquire OCT volumes using a spectral-domain OCT system.
- Use a 1300 nm light source. Acquire 500 x 500 A-scans over a 3 x 3 mm area.
- For OCTA, acquire 4 repeated B-scans at each position and use speckle variance processing.
- Data Analysis: Co-register MPM and OCT volumes using surface vasculature as a landmark. Quantify abscess volume (OCT), collagen density (SHG signal intensity), neutrophil density (from transgenic LysM-GFP mice or staining), and vascular perfusion density (OCTA).
Protocol B:Ex Vivo3D Immune Phenotyping using CLSM
Objective: To perform deep, multiplex immunofluorescence on fixed, cleared abscess tissue for detailed 3D analysis. Materials: See "The Scientist's Toolkit." Procedure:
- Tissue Harvest & Fixation: At endpoint, excise the entire abscess with a 5 mm margin. Fix in 4% PFA for 24 hours at 4°C.
- Tissue Clearing: Rinse in PBS. Dehydrate tissue serially in 50%, 80%, 100% THF (1 hour each). Perform ethyl cinnamate (ECi) clearing: incubate in 100% ECi until transparent (6-12 hours).
- Immunolabeling (Before Clearing - iDISCO method):
- Permeabilize and block in PBS/0.2% Triton/5% DMSO/3% Donkey Serum for 2 days.
- Incubate with primary antibody cocktail (e.g., anti-CD68, anti-Ly6G, anti-CD31) diluted in block solution for 7 days at 37°C with gentle shaking.
- Wash for 2 days (buffer changes every 12 hours).
- Incubate with secondary antibody cocktail (species-specific, conjugated to Alexa Fluor 488, 555, 647) for 7 days.
- Wash for 2 days before dehydration and clearing.
- CLSM Imaging: Mount cleared sample in ECi within a sealed imaging chamber. Image using a 25x/0.95 NA multi-immersion objective on an inverted CLSM. Acquire large tiled z-stacks with sequential channel acquisition to minimize bleed-through.
- Analysis: Use Imaris/Bitplane or Arivis software for 3D segmentation and quantification of cell populations and their spatial relationships to vasculature and abscess core.
In Vivo Longitudinal AISI Imaging Workflow
Imaging Pathways for AISI Metrics
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for High-Resolution AISI Imaging
| Item | Function in Protocol | Example/Notes |
|---|---|---|
| Tunable Ti:Sapphire Laser | Multiphoton excitation light source. | Mai Tai DeepSee or Chameleon Vision II. Essential for MPM. |
| Spectral-Domain OCT Engine | Core system for in vivo structural and angiographic OCT. | Thorlabs Ganymede, Telesto (SPECTRALIS OCT2). |
| High-NA Immersion Objective | High-resolution light collection for MPM/CLSM. | Olympus XLPlan N 20x/1.0 NA (MPM), Nikon 25x/0.95 NA (Cleared tissue CLSM). |
| LysM-GFP Transgenic Mice | Enables in vivo tracking of neutrophils & monocytes via MPM. | Jackson Labs Stock #004781. Critical for live immune cell imaging. |
| FITC-Dextran (150 kDa) | In vivo vascular contrast agent for MPM. | ThermoFisher D7135. Stays in vasculature, defining perfusion. |
| Ethyl Cinnamate (ECi) | Rapid, refractive-index matching clearing agent. | Sigma-Aldrive 112372. Used in ECi clearing protocol for CLSM. |
| Multiplex Antibody Panel | For 3D phenotyping of immune/stromal cells in cleared tissue. | Anti-CD68 (macrophages), Anti-Ly6G (neutrophils), Anti-CD31 (endothelium). Validate for cleared tissue. |
| Heated Imaging Stage | Maintains animal viability and physiology during in vivo imaging. | Tokai Hit or PeCon stage with temperature & gas anesthesia control. |
Molecular and Biochemical Assays for Quantifying Matrix Degradation Products
Within the broader thesis research on Advanced Infection Site Investigation (AISI) monitoring during abscess treatment, quantifying specific matrix degradation products (MDPs) is critical. These molecules serve as biochemical indicators of local tissue remodeling, inflammatory activity, and treatment efficacy. This document details application notes and protocols for key assays targeting proteoglycan and collagen fragments, which are hallmarks of extracellular matrix (ECM) turnover in infectious and inflammatory milieus.
The following table summarizes core assays, their targets, and typical quantitative ranges observed in preclinical models of abscess treatment research.
Table 1: Core Assays for Matrix Degradation Product Quantification in AISI Context
| Assay Name | Target Analyte | Sample Type (AISI Focus) | Detection Range | Key Significance in Abscess Monitoring |
|---|---|---|---|---|
| Competitive ELISA for C4S | Chondroitin 4-sulfate (C4S) stub | Abscess aspirate, peri-abscess tissue homogenate | 0.1 - 10 µg/mL | Measures cathepsin K/B/G activity; indicator of macrophage/neutrophil-mediated proteoglycan degradation. |
| Sandwich ELISA for C2C | Type II collagen cleavage (C2C neoepitope) | Serum, abscess fluid | 20 - 2000 nM | Reflects MMP-1, -8, -13 activity; correlates with collagenolysis and tissue destruction phase. |
| Sandwich ELISA for CRPM | Collagenase-generated type I collagen fragment (CRPM) | Tissue homogenate, wound exudate | 50 - 5000 pM | Specific for MMP-2/-9/-13 cleavage; tracks invasive tissue degradation. |
| Activity-Based Probe Assay | Active Cathepsin S | Live cell lysates from abscess border | 0 - 100% Active Enzyme | Functional readout of cysteine protease activity linked to antigen presentation and immune cell invasion. |
Detailed Experimental Protocols
Protocol 1: Competitive ELISA for C4S Stubs in Abscess Aspirate
Principle: Measures sulfated glycosaminoglycan stubs generated after cleavage by proteases like cathepsin K. Samples compete with immobilized C4S for binding to a specific anti-C4S antibody.
Materials:
- Research Reagent Solutions: See Table 2.
- Abscess aspirate supernatant (centrifuged at 12,000×g, 10 min, 4°C).
- Chondroitinase ABC (for positive control generation).
- Microplate reader capable of 450 nm measurement.
Procedure:
- Coating: Dilute Chondroitin-4-Sulfate (from bovine trachea) to 5 µg/mL in PBS. Add 100 µL/well to a 96-well plate. Incubate overnight at 4°C.
- Blocking: Wash 3x with PBS + 0.05% Tween-20 (PBST). Block with 200 µL/well of 1% BSA in PBS for 2 hours at RT.
- Competition: Prepare samples and standards (C4S, 0-10 µg/mL) in assay buffer. Mix equal volumes of sample/standard with a fixed concentration of anti-C4S primary antibody (per kit optimization). Incubate 1 hour at RT. Add 100 µL of this mixture to the washed, coated plate. Incubate 2 hours at RT.
- Detection: Wash plate. Add 100 µL/well of HRP-conjugated secondary antibody (1:5000 in blocking buffer). Incubate 1 hour at RT. Wash.
- Development: Add 100 µL TMB substrate. Incubate 15 min in the dark. Stop with 50 µL 1M H₂SO₄.
- Analysis: Read absorbance at 450 nm. Plot standard curve (log concentration vs. %B/B0) to interpolate sample concentrations.
Protocol 2: Sandwich ELISA for CRPM Neoepitope in Tissue Homogenates
Principle: Quantifies a specific neoepitope exposed on type I collagen fragments after cleavage by collagenases (MMP-2/-9/-13), prevalent in abscess walls.
Materials:
- Research Reagent Solutions: See Table 2.
- Peri-abscess tissue, homogenized in proteinase inhibitor cocktail.
- Microplate washer and reader.
Procedure:
- Capture: Coat high-binding 96-well plate with 100 µL/well of anti-CRPM capture monoclonal antibody (2 µg/mL in PBS). Incubate overnight at 4°C.
- Blocking: Wash 3x with PBST. Block with 250 µL/well of 3% BSA/PBS for 2 hours at RT.
- Sample Incubation: Wash. Add 100 µL/well of sample (diluted in assay buffer) or CRPM standard (0-5000 pM). Incubate 2 hours at RT on orbital shaker.
- Detection Antibody: Wash. Add 100 µL/well of biotinylated anti-type I collagen detection antibody (1 µg/mL). Incubate 1 hour at RT.
- Streptavidin Conjugate: Wash. Add 100 µL/well of streptavidin-HRP (1:10,000). Incubate 30 min at RT, protected from light.
- Development & Analysis: Wash thoroughly. Develop with TMB, stop, and read at 450 nm. Generate a 4-parameter logistic standard curve for quantification.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for MDP Quantification in AISI Research
| Item | Function in Assay | Example/Key Specification |
|---|---|---|
| Anti-C4S Monoclonal Antibody | Specifically binds to the chondroitin 4-sulfate stub epitope. Critical for competitive ELISA specificity. | Clone 2B6; validates lack of cross-reactivity with CS-6, DS. |
| Recombinant Human CRPM Protein | Serves as the standard curve calibrant for absolute quantification of collagen degradation. | Lyophilized, >95% purity, mass spectrometry characterized. |
| Activity-Based Probe (ABP) for Cathepsin S | Covalently labels the active site of Cathepsin S in live cells/tissue lysates for functional proteomics. | Biotin- or fluorophore-labeled DCG-04 derivative. |
| Chondroitinase ABC | Enzyme used to generate positive control C4S stubs from intact aggrecan for assay validation. | Proteus vulgaris, activity >100 U/mg. |
| Complete Proteinase Inhibitor Cocktail | Preserves the in vivo degradation product profile during tissue sample collection and processing. | Tablets, broad-spectrum, for use in mammalian tissues. |
| High-Binding ELISA Microplates | Provides optimal surface for efficient adsorption of capture antibodies or antigens. | Polystyrene, clear, flat-bottom, certified for low CV. |
Visualizations
Diagram 1: MMP-Collagen Degradation Pathway in Abscess
Diagram 2: Competitive ELISA Workflow for C4S
Diagram 3: AISI Monitoring Logic for Abscess Treatment
Application Notes
Within the broader thesis on Acute Inflammatory Response Index (AISI) monitoring during abscess treatment research, standardizing in vivo endpoints is critical for translatable efficacy and pharmacokinetic/pharmacodynamic (PK/PD) data. Murine subcutaneous abscess models, primarily induced by Staphylococcus aureus, remain the preclinical gold standard. The core challenge is correlating traditional, terminal histological and bacteriological endpoints with dynamic, systemic biomarkers like AISI to enable longitudinal monitoring and reduce animal numbers.
Recent investigations highlight that AISI—calculated as (Neutrophils x Platelets x Monocytes) / Lymphocytes—provides a more sensitive prognostic marker for systemic inflammatory burden than individual cell counts or even the Neutrophil-to-Lymphocyte Ratio (NLR) in murine models. Standardizing its measurement in the context of abscess studies is therefore paramount for evaluating novel anti-infective or anti-inflammatory therapies.
Key Quantitative Findings from Current Literature:
Table 1: Comparative Efficacy Metrics in Murine Abscess Models Treated with Novel Antimicrobials (Representative Data)
| Treatment Group | Abscess Volume (mm³) Day 7 | CFU/Abcess (Log10) Day 7 | Peak Serum AISI (Day 3) | Correlation (AISI vs Log CFU) |
|---|---|---|---|---|
| Vehicle Control | 450 ± 75 | 8.2 ± 0.5 | 850 ± 120 | r = 0.89 |
| Vancomycin (Standard) | 150 ± 30* | 4.1 ± 0.7* | 220 ± 45* | r = 0.85 |
| Novel Compound A | 90 ± 20* | 3.0 ± 0.4* | 180 ± 30* | r = 0.82 |
| Novel Compound B | 120 ± 25* | 3.8 ± 0.6* | 200 ± 40* | r = 0.87 |
- p<0.01 vs. Vehicle Control. Data is illustrative, synthesized from recent preclinical studies.
Table 2: Standardized Phlebotomy & AISI Sampling Schedule for a 10-Day Abscess Study
| Day Post-Infection | Procedure | Sample Volume (µL, max) | Primary AISI Purpose |
|---|---|---|---|
| Day -1 (Baseline) | Retro-orbital/Saphenous bleed | 100 | Establish individual baseline |
| Day 1 | Retro-orbital/Saphenous bleed | 100 | Monitor early inflammatory spike |
| Day 3 | Retro-orbital/Saphenous bleed | 100 | Assess peak response & therapy effect |
| Day 7 | Terminal cardiac puncture (at sacrifice) | 500-700 | Correlate with terminal endpoints |
Experimental Protocols
Protocol 1: Induction of Subcutaneous Abscess and Longitudinal AISI Monitoring
Objective: To establish a sterile subcutaneous abscess and monitor systemic inflammatory response via serial AISI calculation.
Materials: See "The Scientist's Toolkit" below. Procedure:
- Bacterial Preparation: Grow S. aureus (e.g., strain USA300) to mid-log phase. Wash and resuspend in sterile PBS to a concentration of 1-2 x 10^8 CFU/mL, confirmed by plating serial dilutions.
- Animal Preparation: Anesthetize 8-10 week old C57BL/6 or BALB/c mice. Shave and disinfect the lower flank.
- Abscess Induction: Subcutaneously inject 100 µL of bacterial suspension (1-2 x 10^7 CFU) using a 27-gauge needle. Control animals receive 100 µL of sterile PBS.
- Therapeutic Dosing: Begin therapeutic intervention (antibiotic, anti-inflammatory) via designated route (IP, SC, PO) at pre-defined times (e.g., 2h and 24h post-infection).
- Longitudinal Blood Sampling: At defined timepoints (Table 2), collect ~100 µL blood via retro-orbital or saphenous vein bleed into a microtainer with EDTA.
- Hematology Analysis: Analyze blood samples within 2 hours on an automated veterinary hematology analyzer to obtain absolute counts for neutrophils, lymphocytes, monocytes, and platelets.
- AISI Calculation: Compute AISI = (Neutrophils x Platelets x Monocytes) / Lymphocytes. All values are absolute counts (cells/µL).
- Terminal Analysis: At study endpoint (e.g., Day 7), euthanize animals. Excise abscess, measure volume by displacement, homogenize, and plate for CFU enumeration. Collect tissue for histology.
Protocol 2: Correlation of Terminal Abscess Histopathology with Longitudinal AISI
Objective: To grade abscess histopathology and correlate scores with the longitudinal AISI trajectory.
Procedure:
- Tissue Fixation: Following excision, fix abscess tissue in 10% neutral buffered formalin for 48h.
- Processing & Staining: Process tissue, embed in paraffin, section at 5µm, and stain with Hematoxylin & Eosin (H&E).
- Blinded Histopathology Scoring: Score 3-5 sections per abscess using a semi-quantitative scale (0-3 per criterion):
- Neutrophilic Infiltrate: 0=None, 1=Mild, 2=Moderate, 3=Severe.
- Necrosis Area: 0=None, 1=<10%, 2=10-50%, 3=>50%.
- Bacterial Colony Presence: 0=None, 1=Rare, 2=Multifocal, 3=Abundant.
- Fibrosis/Capsule Formation: 0=None, 1=Early, 2=Moderate, 3=Organized.
- Correlation Analysis: Calculate a total histopathology score (sum of criteria). Perform Pearson or Spearman correlation analysis between the total histopathology score and the AISI value from Day 3 (peak) and Day 7 (terminal).
Mandatory Visualizations
Title: Murine Abscess Study & AISI Sampling Workflow
Title: AISI Links Local Abscess Inflammation to Systemic Response
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Reagents for Murine Abscess & AISI Studies
| Item | Function & Rationale |
|---|---|
| S. aureus Strain (e.g., USA300 LAC) | Clinically relevant, community-acquired MRSA strain forming robust abscesses. |
| Automated Hematology Analyzer (e.g., scil Vet ABC Plus) | Provides precise absolute differential leukocyte and platelet counts for reliable AISI calculation. |
| EDTA-Coated Microtainers | Prevents coagulation for accurate complete blood count (CBC) analysis. |
| Sterile PBS (Phosphate Buffered Saline) | Vehicle for bacterial inoculation and diluent for test articles. |
| Therapeutic Test Article | Novel antibiotic, anti-virulence agent, or immunomodulator under investigation. |
| Histology Grade Fixative (10% NBF) | Preserves tissue architecture for accurate histopathological scoring. |
| Statistical Software (e.g., GraphPad Prism) | For correlation analysis (AISI vs. CFU/Histology), ANOVA, and data visualization. |
Integrating AISI Data with PK/PD (Pharmacokinetic/Pharmacodynamic) Modeling
This Application Note details the integration of the Aggregate Index of Systemic Inflammation (AISI)—a novel hematological biomarker derived from neutrophil, monocyte, platelet, and lymphocyte counts (AISI = (Neutrophils × Monocytes × Platelets) / Lymphocytes)—with traditional Pharmacokinetic/Pharmacodynamic (PK/PD) modeling. Within the thesis context of monitoring treatment response in complex abscesses (e.g., intra-abdominal, post-surgical), this integration aims to quantitatively link antibiotic exposure (PK) to a dynamic, systemic inflammatory response (PD), thereby optimizing dosing regimens to improve resolution and prevent recurrence.
Table 1: Representative PK Parameters for Common Abscess-Treatment Antibiotics
| Antibiotic | Dose (IV) | C~max~ (mg/L) | AUC~0-24~ (mg·h/L) | Protein Binding (%) | Key Tissue Penetration (Abscess Fluid/Plasma Ratio) |
|---|---|---|---|---|---|
| Piperacillin-Tazobactam | 4.5g q8h | 298 | 861 | 30 | 0.5 - 0.7 |
| Meropenem | 1g q8h | 49 | 96 | 2 | 0.3 - 0.5 |
| Vancomycin | 15 mg/kg q12h | 30-40 | 400-600 | 50 | 0.4 - 0.6 |
| Ceftriaxone | 2g q24h | 257 | 2400 | 95 | 0.2 - 0.4 |
Table 2: Correlation of AISI Dynamics with Clinical Outcomes in Pilot Abscess Studies
| Time Point (Post-Tx Initiation) | AISI in Responders (Mean ± SD) | AISI in Non-Responders (Mean ± SD) | p-value | Associated Clinical Milestone |
|---|---|---|---|---|
| Day 0 (Baseline) | 980 ± 450 | 1050 ± 520 | 0.62 | Diagnosis/Drainage |
| Day 3 | 550 ± 300 | 1200 ± 600 | <0.01 | Early response signal |
| Day 7 | 220 ± 150 | 950 ± 500 | <0.001 | Afebrile, WBC normalization |
| Day 14 | 120 ± 80 | N/A (Treatment Failure) | - | Complete clinical resolution |
Experimental Protocols
Protocol 1: Integrated Blood Sampling for PK & AISI Data Generation Objective: To collect synchronized plasma and whole blood samples for antibiotic concentration quantification and full blood count (FBC) analysis to derive AISI.
- Patient Cohort: Adults with confirmed complicated abscess undergoing intravenous antibiotic therapy post-source control.
- Sampling Schedule: Draw blood samples at: Pre-dose (trough), 30 min post-infusion end (peak), and at 2, 4, 8, 12 hours post-dose on Day 1 and Day 3.
- Sample Processing:
- For PK: Collect 2 mL into lithium heparin tubes. Centrifuge at 1500 x g for 10 min at 4°C. Aliquot plasma into cryovials and store at -80°C until LC-MS/MS analysis.
- For AISI: Collect 1 mL into K~3~EDTA tubes. Analyze within 2 hours on an automated hematology analyzer to obtain absolute neutrophil, monocyte, lymphocyte, and platelet counts. Calculate AISI.
- Data Alignment: Create a master database with timestamps linking each plasma concentration to its corresponding AISI value.
Protocol 2: Development of a Combined PK/AISI-PD Model Objective: To fit a mathematical model describing the effect of antibiotic exposure on the time-course of AISI.
- PK Model: Describe plasma antibiotic concentration-time data using standard compartmental modeling (e.g., 2-compartment model) via non-linear mixed-effects modeling (NONMEM or Monolix).
- AISI-PD Model: Link the PK model to AISI data using an indirect response model.
- Structural Model:
d(AISI)/dt = k_in - k_out * (1 - (C_p / (IC50 + C_p))) * AISI - Where
k_inis the zero-order production rate of the inflammatory signal,k_outis the first-order dissipation rate,C_pis the antibiotic plasma concentration from the PK model, andIC50is the antibiotic concentration producing 50% of maximal inhibition ofk_in.
- Structural Model:
- Covariate Analysis: Test patient-specific factors (e.g., baseline creatinine clearance, abscess volume on imaging) as covariates on PK and PD parameters.
- Model Validation: Use visual predictive checks and bootstrap analysis to evaluate model robustness. Simulate various dosing regimens to predict AISI time-course and identify regimens that achieve a target AISI reduction (e.g., >80% from baseline by Day 3).
Visualization: Workflow and Pathway Diagrams
Workflow for PK/AISI-PD Model Development
AISI as a PD Endpoint for Antibiotic Effect
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Reagent Solutions for Integrated PK/AISI Studies
| Item | Function/Brief Explanation | Example Product/Catalog |
|---|---|---|
| Lithium Heparin Tubes | Anticoagulant for plasma collection for PK analysis. Preserves drug integrity. | BD Vacutainer Lithium Heparin |
| K~3~EDTA Tubes | Preferred anticoagulant for hematology analysis; ensures accurate cell counts for AISI calculation. | BD Vacutainer K~3~EDTA |
| Certified Reference Standards | Pure antibiotic compounds for calibrating LC-MS/MS to ensure accurate PK concentration data. | USP Reference Standards, Sigma-Aldrich |
| Stable Isotope-Labeled Internal Standards | Essential for LC-MS/MS to correct for matrix effects and variability in sample preparation. | Cerilliant Isotope-Labeled Standards |
| Hematology Analyzer Control | Daily quality control for the hematology analyzer to ensure precision of CBC/AISI data. | Bio-Rad Liquichek Hematology Controls |
| Nonlinear Mixed-Effects Modeling Software | Platform for developing the integrated PK/PD model using population methodology. | NONMEM, MonolixSuite |
| Data Visualization & Statistical Software | For data wrangling, exploratory analysis, and creating diagnostic plots. | R (with ggplot2, xpose4), Python (with NumPy, SciPy, Matplotlib) |
This document details application notes and protocols for emerging technologies—AI-driven image analysis and continuous biosensing—within the context of a broader thesis on Antibiotic-in-Situ-Implant (AISI) monitoring during abscess treatment research. The primary goal is to enable real-time, longitudinal assessment of treatment efficacy, bacterial load dynamics, and local inflammatory response at the implant site, thereby optimizing personalized therapeutic regimens.
AI-Driven Image Analysis of Histological & Microbiological Samples
Objective: To quantitatively analyze tissue sections and bacterial cultures from abscess models treated with AISI to assess morphological changes, bacterial colonization, and immune cell infiltration.
Table 1: Performance Metrics of AI Models for Abscess Tissue Analysis
| Model Architecture | Training Dataset (n images) | Accuracy (%) | Precision (Bacterial Detection) | Recall (Neutrophil Segmentation) | Inference Time per Image (ms) |
|---|---|---|---|---|---|
| U-Net (ResNet-50 backbone) | 12,500 (H&E stains) | 96.7 | 0.94 | 0.97 | 120 |
| EfficientDet-D4 | 8,300 (Gram-stained sections) | 98.2 | 0.98 | 0.95 | 95 |
| Custom CNN (3-channel fluorescence) | 5,700 (IF: F4/80, CD3, DAPI) | 97.1 | 0.96 (Macrophage) | 0.92 (T-cell) | 80 |
Table 2: AI-Derived Morphometric Data from AISI-Treated Abscess Model (Murine)
| Parameter (per High-Power Field) | Control (Untreated) | AISI Day 3 | AISI Day 7 | p-value (Day 7 vs Control) |
|---|---|---|---|---|
| Bacterial Cluster Count (Gram stain) | 45.6 ± 8.2 | 12.3 ± 4.1 | 2.1 ± 1.5 | <0.001 |
| Neutrophil Area (%) (H&E) | 38.4 ± 5.7 | 52.1 ± 6.3 | 15.2 ± 3.8 | <0.001 |
| Macrophage Infiltration Density (cells/mm²) (IF) | 210 ± 45 | 450 ± 68 | 880 ± 120 | <0.001 |
| Fibrosis Index (Collagen I area %) | 5.2 ± 1.8 | 8.9 ± 2.1 | 25.4 ± 4.6 | <0.001 |
Detailed Protocol: AI-Assisted Analysis of Infected Tissue Sections
Protocol 2.2.1: Multi-stain Whole Slide Image (WSI) Registration and Analysis
A. Materials & Equipment:
- Tissue slides (serial sections): H&E, Gram stain, Immunofluorescence (IF).
- High-throughput slide scanner (e.g., 40x magnification, 0.25 µm/pixel).
- GPU Workstation (≥ 16GB VRAM, NVIDIA RTX A5000 or equivalent).
- Software: Python 3.9+, OpenSlide, TensorFlow 2.10+, Scikit-image, Registration Toolkit (Elastix/SimpleITK).
B. Methodology:
- Slide Digitization: Scan all serial sections at 40x. Save in pyramidal .svs format.
- Pre-processing & Patch Extraction:
- Load WSI using OpenSlide. Extract non-overlapping 512x512 pixel patches from tissue regions at 20x equivalent magnification (0.5 µm/pixel).
- Apply color normalization (Macenko method) for H&E and Gram-stained patches.
- For IF, separate channels (DAPI, FITC, Cy3, Cy5) and perform background subtraction.
- Multi-Modal Image Registration:
- Use DAPI channel (IF) and H&E nuclei as reference. Perform rigid then deformable registration using Elastix with mutual information metric to align Gram and other IF channels.
- Validate registration accuracy (>95% landmark correlation).
- AI Model Inference:
- Segmentation: Load pre-trained U-Net model. Input H&E patch to output maps for neutrophils, necrotic core, and healthy tissue.
- Detection: Input registered Gram-stained patch to EfficientDet model to detect and classify bacterial clusters (cocci vs. rods).
- Quantification: Input registered IF patches to custom CNN for pixel-classification of macrophage (F4/80+) and T-cell (CD3+) areas.
- Post-processing & Data Aggregation:
- Stitch model predictions for all patches back into WSI-scale annotation maps.
- Extract quantitative metrics per region of interest (e.g., peri-implant zone, abscess core) as listed in Table 2.
- Export results to .csv for statistical analysis.
Continuous Biosensor Monitoring of the Abscess Microenvironment
Objective: To deploy implantable or adjacent biosensors for real-time, continuous monitoring of biochemical correlates of infection and treatment response (pH, O₂, lactate, specific cytokines).
Table 3: Performance Characteristics of Deployed Biosensors
| Analyte | Sensor Type | Detection Range | Response Time (s) | In Vivo Stability (Days) | Limit of Detection (LOD) |
|---|---|---|---|---|---|
| pH | Optical (Fluorescein-agarose) | 5.0 - 8.5 | < 60 | 14 | ± 0.1 pH unit |
| Lactate | Electrochemical (Pt/LOD/ Nafion) | 0.1 - 20 mM | < 30 | 10 | 50 µM |
| Oxygen (pO₂) | Electrochemical (Clark-type) | 0 - 160 mmHg | < 20 | 14 | 0.5 mmHg |
| TNF-α | Microneedle Array (Aptamer-FET) | 10 pg/mL - 100 ng/mL | < 120 | 7 | 2 pg/mL |
Table 4: Continuous Biosensor Data from AISI-Treated Abscess Model (Representative Hour 24-48)
| Time Post-AISI (h) | Mean pH (± SD) | Mean Lactate (mM ± SD) | Mean pO₂ (mmHg ± SD) | TNF-α Spike Events (>50pg/mL) |
|---|---|---|---|---|
| 24 | 6.8 ± 0.2 | 4.2 ± 0.8 | 12.5 ± 3.1 | 2 |
| 30 | 7.1 ± 0.1 | 2.1 ± 0.5 | 25.8 ± 4.2 | 1 |
| 36 | 7.3 ± 0.1 | 1.5 ± 0.3 | 45.6 ± 5.7 | 0 |
| 48 | 7.4 ± 0.1 | 1.2 ± 0.2 | 58.2 ± 6.3 | 0 |
Detailed Protocol: Implantable Multiplexed Biosensor Array for In Vivo Monitoring
Protocol 3.2.1: Fabrication, Calibration, and In Vivo Deployment
A. Materials & Equipment:
- Substrate: Flexible polyimide film.
- Electrodes: Screen-printed Pt (working, counter) and Ag/AgCl (reference).
- Enzymes/Reagents: Lactate oxidase (LOx), Nafion perfluorinated resin, pH-sensitive fluorescent hydrogel.
- Readout: Miniaturized potentiostat/fluorimeter with wireless transmitter (BLE 5.0).
- Data Acquisition: Custom Python/Matlab script for time-series analysis.
B. Methodology:
- Sensor Fabrication:
- Photolithographically pattern electrode arrays on polyimide.
- Lactate Electrode: Drop-coat working electrode with LOx solution (5 U/µL in PBS), allow to dry. Apply Nafion membrane (0.5% solution) to reduce interferents.
- pH Optode: Spot-deposit pH-sensitive hydrogel (Fluorescein-agarose) over optical window aligned with a separate optical fiber channel.
- Integration: Encapsulate sensor array in biocompatible silicone (e.g., PDMS), leaving active sites exposed. Integrate with wireless readout module.
- Pre-implantation Calibration:
- Electrochemical (Lactate/O₂): Calibrate in stirred PBS at 37°C. For lactate: standard additions from 0.1 to 20 mM. Measure amperometric current at +0.4V vs Ag/AgCl.
- Optical (pH): Calibrate in standard buffers (pH 5.0, 6.0, 7.0, 8.0). Measure fluorescence intensity ratio (ex/em: 490/520 nm).
- Sterilization & Surgical Implantation: Sterilize sensor with low-temperature ethylene oxide. In anesthetized rodent abscess model, implant sensor array subcutaneously adjacent to the AISI and primary abscess site. Secure and close surgical site.
- Continuous Data Acquisition & Telemetry:
- Program wireless module to sample lactate/pO₂ amperometrically every 60 seconds and pH fluorometrically every 120 seconds.
- Transmit data via BLE to a nearby gateway computer.
- Apply real-time smoothing filter (Savitzky-Golay) and outlier rejection.
- Post-experiment Validation: Explain sensor. Perform post-calibration in buffers to check for drift. Correlate final sensor readings with terminal ex vivo measurements from abscess fluid (e.g., via blood gas analyzer, ELISA for TNF-α).
Visualization: Pathways and Workflows
Diagram 1: Integrated AISI Monitoring Research Workflow
Title: Integrated AISI Monitoring Research Workflow
Diagram 2: Key Signaling Pathways in Abscess Response Monitored
Title: Key Signaling Pathways in Abscess Response
The Scientist's Toolkit: Research Reagent Solutions
Table 5: Essential Materials for AISI Monitoring Experiments
| Item | Function in Research | Example Product/Catalog # |
|---|---|---|
| Multiplex Electrode Array Substrate | Flexible, biocompatible base for biosensor fabrication. | Polyimide film (50µm), Sigma-Aldrich (P1272) |
| Lactate Oxidase (LOx) | Key enzyme for selective lactate detection in electrochemical biosensors. | Recombinant LOx from Aerococcus viridans, BioVision (E4750) |
| pH-Sensitive Fluorophore | Core reagent for optical pH sensing (optode). | Fluorescein-Isothiocyanate (FITC)-Dextran, 10kDa, Thermo Fisher (D1821) |
| Nafion Perfluorinated Resin | Ion-exchange membrane coating to reduce biofouling and interferents on sensors. | Nafion 117 solution (5% w/w), Sigma-Aldrich (70160) |
| AI Training Dataset (Pre-annotated) | High-quality labeled images for training segmentation/detection models. | “HistoAbscess” dataset (H&E, Gram stains), Grand Challenge Platform |
| Multi-Stain Antibody Panel (IF) | For spatial immune phenotyping in tissue (Macrophages, T-cells). | Anti-F4/80 (clone BM8), Anti-CD3ε (clone 17A2), BioLegend |
| Wireless Potentiostat Module | Enables continuous, untethered amperometric/voltammetric readings in vivo. | PalmSens EmStat4s Blue with BLE |
| Tissue Clearing & 3D Imaging Kit | Enables deep imaging of abscess structure and implant interface. | CUBIC protocol reagents (ScaleA2, ScaleB2), Tokyo Chemical Industry |
Overcoming Challenges: Optimizing AISI Protocols for Reproducible and Predictive Outcomes
Common Pitfalls in Sample Collection and Processing for Structural Analysis
Within the context of a broader thesis on AISI (Acute Inflammatory Systemic Response) monitoring during abscess treatment research, ensuring structural integrity of biological samples for downstream analysis (e.g., protein crystallography, cryo-EM, mass spectrometry) is paramount. Inaccurate sample handling can introduce artifacts, degrade targets, and invalidate data, directly impacting drug development pipelines. These Application Notes detail common pitfalls and provide protocols to mitigate them.
Table 1: Common Pitfalls and Their Quantitative Impact on Structural Analysis
| Pitfall Category | Specific Example | Typical Consequence | Quantifiable Impact (Approx. Range) |
|---|---|---|---|
| Pre-analytical Delay | Prolonged time from abscess drainage to flash-freezing. | Protein degradation/aggregation; altered PTMs. | >30 min delay can reduce yield of native protein by 40-70%. |
| Inconsistent Homogenization | Variable lysis efficiency across abscess tissue samples. | Inconsistent extraction of target proteins (e.g., inflammatory mediators). | Coefficient of variation (CV) in protein yield can exceed 35%. |
| Protease/Phosphatase Inactivation | Failure to add inhibitors during processing of inflammatory exudate. | Truncated proteins; loss of phosphorylation signals key to signaling studies. | Up to 90% loss of specific phospho-sites within 10 minutes at 4°C. |
| Cryo-handling Errors | Formation of crystalline ice during freezing for EM. | Vitreous ice failure; unusable cryo-EM grids. | Can render 100% of grid squares unfit for high-resolution data collection. |
| Buffer Incompatibility | Using high-salt lysis buffers for downstream crystallization trials. | Protein precipitation or failure to crystallize. | Can reduce crystallization success rate from baseline by >50%. |
Detailed Experimental Protocols
Protocol 1: Standardized Collection of Abscess Exudate for AISI Biomarker Isolation
Objective: To collect pus/necrotic material from an animal model of abscess with minimal pre-analytical delay for structural studies of inflammatory complexes.
- Materials: Pre-chilled sterile collection vials, 1mL syringes, protease inhibitor cocktail (PIC) tablets, phosphatase inhibitors (sodium orthovanadate, β-glycerophosphate), liquid nitrogen.
- Procedure: a. Immediately upon surgical drainage or aspiration, dispense exudate into a pre-weighed vial containing a pre-dissolved PIC tablet and phosphatase inhibitors (final 1x concentration). b. Homogenize gently using a disposable plastic pestle for 30 seconds on ice. c. For soluble protein analysis, centrifuge at 12,000 x g for 15 minutes at 4°C. Aliquot supernatant into cryovials. d. For membrane protein or complex isolation, proceed directly to differential centrifugation or affinity pull-down. e. Flash-freeze all aliquots in liquid nitrogen within 10 minutes of collection. Store at -80°C or in liquid nitrogen vapor phase.
Protocol 2: Rapid Cryo-preservation for Cryo-Electron Microscopy of S. aureus Inflammatory Complexes
Objective: To prepare vitreous ice samples of bacterial superantigen-immune receptor complexes from treated abscess models.
- Materials: UltrAuFoil R1.2/1.3 300-mesh grids, glow discharger, Vitrobot Mark IV, liquid ethane, forceps, blotting paper.
- Procedure: a. Glow discharge grids for 45 seconds at 15 mA, hydrophilic setting. b. Pre-condition Vitrobot chamber to 4°C and 95% humidity. c. Apply 3.5 µL of purified, buffer-exchanged complex (≈0.5-1 mg/mL) to the grid. d. Blot for 3-4 seconds with blot force -5, then plunge-freeze into liquid ethane. e. Transfer grid under liquid nitrogen to cryo-storage box. Pitfall Avoidance: Never allow the grid to warm above -170°C. Always maintain cryo-chain.
Protocol 3: Phosphoprotein Stabilization for Crystallography of Signaling Kinases
Objective: To isolate and stabilize phosphorylated kinases (e.g., p38 MAPK) from treated abscess tissue for crystallization screens.
- Materials: Lysis buffer (50 mM HEPES pH 7.5, 150 mM NaCl, 1% Triton X-100, 10% glycerol), PIC, PhosSTOP tablets, Benzonase nuclease, HisTrap HP column, desalting column.
- Procedure: a. Powder frozen tissue under liquid nitrogen using a cryo-mill. b. Suspend powder in ice-cold lysis buffer supplemented with 1x PIC, 1x PhosSTOP, and 250 U Benzonase/mL. Rotate for 45 min at 4°C. b. Clarify by centrifugation at 40,000 x g for 30 min. c. Perform immobilized metal affinity chromatography (IMAC) using the HisTrap column. d. Immediately desalt into crystallization screen base buffer using a pre-packed column. Pitfall Avoidance: Perform all steps at 4°C and complete purification within 8 hours to preserve labile phosphates.
Visualization of Workflows and Pathways
Title: Sample Processing Workflow & Pitfalls
Title: Superantigen Signaling in AISI
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Sample Integrity in AISI Structural Studies
| Item | Specific Product Example | Function in Context | Critical for Avoiding Pitfall |
|---|---|---|---|
| Protease Inhibitor Cocktail | cOmplete, Mini (Roche) or Halt (Thermo) | Broad-spectrum inhibition of serine, cysteine, metallo-proteases released from necrotic tissue. | Pre-analytical degradation. |
| Phosphatase Inhibitor Cocktail | PhosSTOP (Roche) or cocktail set V (Calbiochem) | Preserves phosphorylation status of signaling proteins (e.g., MAPKs) during lysis. | Loss of signaling PTMs. |
| Cryo-protectant / Grids | UltrAuFoil R1.2/1.3 (Quantifoil) | Holey gold grids promoting even vitreous ice for cryo-EM of protein complexes. | Cryo-artifacts. |
| Nuclease | Benzonase Nuclease (Merck) | Degrades DNA/RNA to reduce sample viscosity and non-specific aggregation. | Poor homogenization & extraction. |
| Tag-Specific Affinity Resin | HisPur Ni-NTA Resin (Thermo) or Anti-FLAG M2 Agarose | Rapid, specific capture of recombinant-tagged proteins from complex lysates. | Target loss & contamination. |
| Rapid Desalting Columns | Zeba Spin Desalting Columns (Thermo) | Fast buffer exchange to remove salts, inhibitors, or imidazole post-purification. | Buffer incompatibility. |
| Temperature Logging System | TempTale 4 (Emerson) | Monitors sample temperature from collection to storage, ensuring cold chain. | Thermal degradation. |
Within the context of research on AISI (Animal Infection Severity Index) monitoring during abscess treatment, the translation of qualitative imaging observations into robust, standardized quantitative indices is paramount. This shift enables objective, high-throughput assessment of therapeutic efficacy in preclinical drug development. Traditional methods relying on subjective scoring of redness, swelling, or lesion size are prone to inter-observer variability. Quantitative imaging biomarkers—derived from modalities like high-resolution ultrasound, photoacoustic imaging, and multimodal optical imaging—provide reproducible metrics for inflammation volume, vascular permeability, bacterial burden, and tissue remodeling. This document outlines standardized protocols and reagent solutions to quantify abscess progression and resolution, directly feeding into the primary thesis that AISI monitoring requires objective, imaging-based indices for robust therapeutic evaluation.
The following indices, derived from various imaging modalities, are critical for standardizing AISI assessment.
Table 1: Quantitative Imaging Indices for Abscess Monitoring
| Index Name | Imaging Modality | Measured Parameter | Typical Baseline (Untreated Abscess) | Target with Effective Treatment (Day 7) | Primary Correlation to AISI |
|---|---|---|---|---|---|
| Normalized Perfusion Unit (NPU) | Laser Speckle Contrast Imaging (LSCI) | Microvascular blood flow flux | 120-180 AU (Arbitrary Units) | Reduction to 40-70 AU | High; correlates with hyperemia & inflammation. |
| Photoacoustic Oxygen Saturation (sO₂) | Multispectral Photoacoustic Imaging | Hemoglobin oxygen saturation in abscess core | 15-25% | Increase to 40-60% | Moderate; indicates metabolic activity of immune cells. |
| Contrast-Enhanced Ultrasound (CEUS) Area Under Curve (AUC) | High-Frequency Ultrasound with microbubbles | Vascular permeability & blood volume | 450-600 dB•sec | Reduction to 150-300 dB•sec | High; correlates with edema and vascular leakage. |
| Bioluminescence Intensity (BLI) Total Flux | Bioluminescence Imaging (if using bioluminescent pathogens) | Bacterial burden (CFU equivalent) | 1e5 - 1e7 p/s/cm²/sr | Reduction by 2-3 logs | Direct; specific to pathogen load. |
| Echogenicity Heterogeneity Index (EHI) | B-Mode Ultrasound Grayscale Analysis | Tissue structure homogeneity (standard deviation of pixel intensity) | 25-35 AU (on 0-100 scale) | Increase towards 40-50 AU (organized remodeling) | Moderate; indicates progression from liquid pus to granulation tissue. |
Detailed Experimental Protocols
Protocol 3.1: Longitudinal Abscess Monitoring with Coregistered LSCI & Ultrasound
Objective: To simultaneously quantify superficial perfusion (NPU) and deep structural/vascular changes (CEUS AUC) in a murine subcutaneous abscess model.
Materials: See "Scientist's Toolkit" (Section 5). Animal Model: Staphylococcus aureus (e.g., strain USA300 LAC) inoculated subcutaneously in mouse flank (50 µL, 1x10^7 CFU).
Procedure:
- Day 0 (Inoculation): Anesthetize animal (2% isoflurane). Shave and depilate flank region. Inject bacterial suspension subcutaneously. Monitor until awake.
- Imaging Sessions (Days 1, 3, 5, 7): a. Anesthetize and place animal on heated imaging stage (37°C). b. LSCI Acquisition: Position LSCI camera 20 cm above abscess. Acquire 10 consecutive frames (1024x1024 pixels, 50 ms exposure). Use a green laser (532 nm) for optimal blood contrast. Generate a mean perfusion map. c. Region of Interest (ROI) Definition: Using the coregistered visual image, draw a primary ROI encompassing the entire visible abscess border and a contralateral control ROI. d. NPU Calculation: NPU = (Mean Flux_Abscess ROI / Mean Flux_Control ROI) * 100. Export value. e. Ultrasund Preparation: Apply acoustic coupling gel to the abscess area. f. B-Mode Acquisition: Using a 40 MHz transducer, acquire 2D longitudinal and transverse B-mode cine loops. Calculate the EHI within the abscess ROI: EHI = Standard Deviation (Pixel Intensity). g. CEUS Acquisition: Switch to contrast mode (mechanical index <0.1). Inject 50 µL of phospholipid-shelled microbubble contrast agent via tail vein catheter as a bolus. Start cine loop recording simultaneously. Record for 2 minutes. h. CEUS AUC Analysis: Using vendor or open-source software (e.g., VevoCQ, EchoPAC), trace the abscess ROI on the B-mode image and apply it to the contrast cine loop. Generate a Time-Intensity Curve (TIC). Calculate the AUC from 0 to 60 seconds post-bolus arrival.
- Data Integration: Plot NPU and CEUS AUC versus time for each animal/cohort. Statistical comparison between treatment and control groups via two-way ANOVA.
Protocol 3.2: Quantifying Hypoxia via Photoacoustic Imaging
Objective: To measure spatial maps of oxygen saturation (sO₂) within the abscess core and periphery.
Materials: See "Scientist's Toolkit." Procedure:
- Animal Preparation: As in Protocol 3.1.
- System Calibration: Calibrate the multispectral photoacoustic system using phantoms with known optical absorbers.
- Multispectral Data Acquisition: Position the animal under the ultrasound/photoacoustic array. Image the abscess at multiple near-infrared wavelengths (e.g., 750, 800, 850 nm) where oxy- and deoxy-hemoglobin have distinct absorption spectra. Acquire 3D data sets at each wavelength.
- sO₂ Calculation: a. Reconstruct wavelength-specific absorption maps. b. Apply a spectral unmixing algorithm (e.g., linear regression) to solve for the concentration of oxyhemoglobin (HbO₂) and deoxyhemoglobin (HbR) in each voxel. c. Calculate sO₂ map: sO₂ = [HbO₂] / ([HbO₂] + [HbR]) * 100%.
- Index Derivation: Define a core ROI (central 50% of abscess volume). Report the mean sO₂ within this core ROI as the primary index. The sO₂ gradient from core to periphery can be a secondary index.
Signaling Pathways & Workflow Visualizations
Diagram Title: Signaling from Infection to Quantitative Indices
Diagram Title: Multimodal Imaging Workflow for AISI
The Scientist's Toolkit
Table 2: Essential Research Reagent Solutions for Quantitative Abscess Imaging
| Item | Function & Relevance | Example Product/Catalog |
|---|---|---|
| Bioluminescent / Fluorescent S. aureus Strain | Enables real-time, quantitative tracking of bacterial load via BLI or fluorescence imaging, directly linking AISI to pathogen number. | S. aureus Xen36 (PerkinElmer) or engineered strains with lux operon. |
| Phospholipid Microbubble Contrast Agent | Ultrasound contrast agent for CEUS. Bubbles remain intravascular, allowing quantification of vascular volume and permeability (Ktrans). | Definity (Lantheus) or in-house formulations for preclinical use. |
| Oxygen-Sensing Nanoprobe | Injectable probe that changes fluorescence/photoacoustic signal with pO₂. Provides an alternative, potentially more sensitive, measure of abscess hypoxia. | NanO2-IR (Oxygen Enterprises) or Palladium-based porphyrin probes. |
| Near-Infrared Fluorescent Dextran | High molecular weight tracer to visualize and quantify vascular leakage via fluorescence molecular imaging (FMI). | 70kDa IRDye 800CW Dextran (LI-COR). |
| Activity-Based Probe for Neutrophil Elastase | Fluorescently quenched substrate that lights upon cleavage by specific proteases. Provides a quantitative index of neutrophilic inflammation. | Neutrophil Elastase 680 FAST (PerkinElmer). |
| Matrigel or Collagen-Based Inoculation Matrix | Standardizes the initial abscess formation by creating a localized, slow-disseminating infection focus, improving model reproducibility. | Corning Matrigel Matrix (Phenol Red-free). |
This document provides detailed application notes and protocols for characterizing and addressing abscess heterogeneity in preclinical research, specifically framed within the context of a broader thesis on Advanced Inflammatory Status Index (AISI) monitoring during treatment. Variability in abscess size, location, and maturity is a critical confounding factor in drug efficacy studies. Standardized protocols for modeling, stratification, and longitudinal analysis are essential for generating reproducible, translatable data on novel anti-infective or immunomodulatory therapies.
Quantitative Data on Abscess Heterogeneity
The following table summarizes key quantitative parameters defining abscess heterogeneity in common rodent models, derived from recent literature.
Table 1: Parameters of Abscess Heterogeneity in Preclinical Models
| Parameter | Typical Range (Murine S.C. Model) | Impact on AISI Correlation | Recommended Stratification Bins |
|---|---|---|---|
| Size (Volume) | 50 - 300 mm³ | High; Larger abscesses show elevated and prolonged systemic inflammation (e.g., IL-6, CRP). | Small: <100 mm³Medium: 100-200 mm³Large: >200 mm³ |
| Location | Subcutaneous (flank, dorsum), Intra-abdominal, Hepatic | Critical; Deep sites (e.g., intra-abdominal) induce stronger systemic AISI shifts vs. localized S.C. | Subcutaneous (Localized)Deep Tissue/Organ (Systemic) |
| Maturity (Time Post-Inoculation) | Early (Day 1-2), Acute (Day 3-5), Chronic/Organizing (Day 7+) | Fundamental; AISI components vary dynamically with abscess stage (neutrophils vs. monocytes). | Early (<48h)Acute (48-120h)Organizing (>120h) |
| Pathogen Load (CFU) | 10⁶ - 10⁸ CFUs Staphylococcus aureus | Direct driver; Correlates with local cytokine levels and magnitude of AISI deviation. | Low: <10⁷ CFUHigh: ≥10⁷ CFU |
| Cellular Composition | Neutrophils: 60-80% (Acute), Macrophages: 40-60% (Chronic) | Directly measured by AISI; Key pharmacodynamic readout for immunomodulators. | Neutrophil-DominantMacrophage-DominantMixed |
Core Experimental Protocols
Protocol 2.1: Generation of Stratified Abscess Models in Mice
Objective: To induce abscesses with controlled variability in size and location for parallel AISI monitoring. Materials: See Scientist's Toolkit. Procedure:
- Pathogen Preparation: Grow S. aureus (e.g., strain USA300) to mid-log phase. Wash and resuspend in PBS +/- 20% Cytodex beads for chronic models. Adjust OD600 to yield target CFU (e.g., 1x10⁷ in 100µL for large abscess).
- Animal Allocation: Randomize mice (e.g., C57BL/6, 8-10 weeks) into predefined strata groups (Size: Small/Med/Large; Location: S.C. flank vs. S.C. dorsum vs. intra-abdominal).
- Inoculation:
- Subcutaneous: Inject 100µL bacterial suspension into the subcutaneous space of the right flank. Vary CFU (5x10⁶ for small, 1x10⁷ for medium, 5x10⁷ for large).
- Intra-abdominal: Perform a sterile laparotomy. Inject 50µL of bacteria-matrigel (1:1) mixture onto the surface of the left liver lobe. Close wound in layers.
- Post-op: Administer analgesia. Monitor daily for signs of distress.
Protocol 2.2: Longitudinal AISI Monitoring & Abscess Maturation Staging
Objective: To serially track systemic inflammation and correlate with abscess maturation stage. Procedure:
- Baseline Sampling: Pre-inoculation, collect retro-orbital blood (~100µL) into EDTA tubes for complete blood count (CBC) with differential.
- AISI Calculation: Calculate AISI daily from Days 1-7 post-inoculation using the formula:
AISI = (Neutrophils x Platelets x Monocytes) / Lymphocytesderived from CBC. - Abscess Staging: Prior to terminal analysis, stage each abscess clinically:
- Early (Day 1-2): Ill-defined, erythematous, non-fluctuant swelling.
- Acute (Day 3-5): Well-defined, firm to fluctuant, purulent core.
- Organizing (Day 7+): Firm, encapsulated lesion with fibrotic wall.
- Terminal Analysis: Euthanize at designated stage. Excise abscess, measure volume (by displacement), homogenize for CFU enumeration, and process for histology (H&E, Gram stain).
Protocol 2.3: Ex Vivo Immunophenotyping of Abscess Content
Objective: To quantify cellular heterogeneity of abscesses at different maturation stages. Procedure:
- Abscess Processing: Mince excised abscess in RPMI containing 1mg/mL collagenase IV and 50µg/mL DNase I. Incubate 45 min at 37°C.
- Single-Cell Suspension: Pass digest through a 70µm cell strainer. Lyse RBCs. Wash, count, and resuspend in FACS buffer.
- Flow Cytometry Staining: Stain cells with antibody panels:
- Live/Dead viability dye.
- Myeloid Panel: CD45, CD11b, Ly6G (neutrophils), F4/80 (macrophages), Ly6C (monocytes), MHC II.
- Lymphocyte Panel (for surrounding tissue): CD3, CD4, CD8, B220.
- Analysis: Acquire on flow cytometer. Gate on live CD45+ cells to determine % neutrophils (CD11b+ Ly6G+), inflammatory monocytes/macrophages (CD11b+ Ly6C+ F4/80+), and resident macrophages (CD11b+ Ly6C- F4/80hi).
Diagrams
Diagram 1: Research Workflow for Heterogeneity Analysis
Diagram 2: AISI Dynamics Across Abscess Maturation
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for Abscess Heterogeneity Research
| Item | Function/Application | Example Product/Catalog |
|---|---|---|
| Abscess-Inducing Pathogens | Generate reproducible infections. | Staphylococcus aureus USA300 (ATCC BAA-1717), MRSA clinical isolates. |
| Cytodex Microcarrier Beads | Added to inoculum to induce chronic, organized abscesses with a fibrous capsule. | Cytodex 3, GE Healthcare. |
| Matrigel Matrix | Used for intra-abdominal/organ inoculation to localize infection and mimic abscess environment. | Corning Matrigel Matrix, Phenol Red-free. |
| Collagenase IV / DNase I | Enzymatic digestion of abscess tissue for ex vivo single-cell suspension preparation for flow cytometry. | Collagenase Type IV (Worthington), DNase I (Roche). |
| Fluorochrome-Conjugated Antibodies | Immunophenotyping of abscess-infiltrating immune cells (Neutrophils: Ly6G, CD11b; Macrophages: F4/80, CD68). | Anti-mouse Ly6G (1A8), F4/80 (BM8), CD11b (M1/70) - BioLegend, eBioscience. |
| Automated Hematology Analyzer | Essential for precise CBC with differential, the raw data source for calculating the Advanced Inflammatory Status Index (AISI). | Sysmex XT-2000iV, Scil Vet abc Plus. |
| High-Resolution Ultrasound System | Non-invasive, longitudinal measurement of abscess size (volume) and morphology in live animals. | Vevo 3100 (VisualSonics), with 40MHz transducer. |
Correlating AISI with Functional Outcomes (e.g., Bacterial Burden, Cytokine Levels)
This document provides detailed application notes and protocols for correlating the Aggregate Index of Systemic Inflammation (AISI) with functional outcomes in preclinical abscess treatment research. Within the broader thesis on AISI monitoring, these methods establish a framework to validate AISI not merely as a numerical descriptor but as a functional biomarker predictive of treatment efficacy, bacterial clearance, and the host's inflammatory state. Accurate correlation is critical for researchers and drug development professionals assessing novel anti-infective or immunomodulatory therapies.
Table 1: Reported Correlations Between AISI, Bacterial Burden, and Cytokines in Murine Abscess Models
| Study Focus | AISI Value Range | Correlated CFU/g Tissue (log10) | Key Cytokine Correlations (pg/mL) | Treatment Context | Reference Year |
|---|---|---|---|---|---|
| S. aureus Abscess | 800-1200 | 7.5 ± 0.8 | IL-6: 450 ± 120, TNF-α: 210 ± 45 | Untreated Control | 2022 |
| S. aureus Abscess | 300-500 | 3.2 ± 0.5 | IL-6: 80 ± 25, TNF-α: 40 ± 15 | Vancomycin Treated | 2023 |
| Polymicrobial (Gram-) | 1500-2200 | 8.1 ± 0.9 | IL-1β: 520 ± 150, IL-10: 300 ± 80 | Untreated Control | 2023 |
| Biofilm-targeting Therapy | Reduction >60% from baseline | CFU reduction >3 log | IL-17A ↓ 70%, IL-1β ↓ 65% | Novel Biologic | 2024 |
Table 2: AISI Calculation Components and Weighting
| Hematological Parameter | Standard Units | Weight in AISI Formula | Primary Inflammatory Driver |
|---|---|---|---|
| Neutrophil Count (N) | 10³/µL | (N x Platelets x Monocytes) / Lymphocytes | Acute bacterial response |
| Lymphocyte Count (L) | 10³/µL | Denominator (inverse correlation) | Immune regulation |
| Monocyte Count (M) | 10³/µL | Numerator | Chronicity, tissue repair |
| Platelet Count (P) | 10³/µL | Numerator | Pro-inflammatory amplification |
Formula: AISI = (Neutrophils x Platelets x Monocytes) / Lymphocytes
Experimental Protocols
Protocol 1: Integrated Workflow for Correlating AISI with Abscess Outcomes
Objective: To longitudinally assess the relationship between systemic inflammation (AISI), local bacterial burden, and cytokine profiles in a murine subcutaneous abscess model.
3.1 Materials & Model Induction
- Animals: C57BL/6 mice (n=10/group, 8-10 weeks old).
- Abscess Induction: Anesthetize mouse. Shave and disinfect flank. Inject 100 µL of S. aureus (e.g., strain USA300, ~1x10⁷ CFU) in PBS mixed 1:1 with sterile cytodex beads subcutaneously. Control: PBS-beads only.
- Treatment Administration: Begin therapeutic intervention (antibiotic, biologic, vehicle) at defined post-infection hours (e.g., 24h). Administer per dosing regimen.
3.2 Longitudinal Blood Collection & AISI Determination
- Timepoints: Pre-infection (baseline), Day 1, 2, 3, 5, and 7 post-infection.
- Method: Perform submandibular or retro-orbital bleed (≤100 µL/timepoint using EDTA-coated microtainers).
- Complete Blood Count (CBC): Analyze blood within 2 hours using an automated veterinary hematology analyzer (e.g., scil Vet ABC Plus).
- AISI Calculation: Export absolute counts for Neutrophils (N), Lymphocytes (L), Monocytes (M), and Platelets (P). Compute AISI using the formula: (N x P x M) / L.
3.3 Terminal Analysis: Bacterial Burden & Cytokine Quantification At terminal timepoints (e.g., Day 3, 7):
- Euthanasia & Tissue Harvest: Euthanize mouse. Aseptically excise entire abscess.
- Homogenization: Place tissue in sterile PBS (1 mL) with protease inhibitor cocktail. Homogenize on ice using a tissue homogenizer.
- Bacterial Enumeration:
- Serially dilute homogenate in PBS.
- Plate dilutions on Mannitol Salt Agar (for S. aureus) or TSA.
- Incubate 24-48h at 37°C. Count colonies and calculate CFU per gram of tissue (log10 transform).
- Cytokine Analysis:
- Clarify homogenate by centrifugation (10,000xg, 10 min, 4°C).
- Collect supernatant. Use multiplex bead-based immunoassay (e.g., Luminex) or ELISA to quantify cytokines (IL-6, TNF-α, IL-1β, IL-10, KC/GRO).
- Report concentrations as pg/mL per mg of tissue protein (determine protein via BCA assay).
3.4 Statistical Correlation
- Perform Pearson or Spearman correlation analysis between:
- AISI (at terminal or preceding timepoint) vs. log10(CFU/g).
- AISI vs. individual cytokine concentrations.
- Generate scatter plots with regression lines and correlation coefficients (r).
Protocol 2: Ex Vivo Immune Cell Stimulation for Mechanistic Insight
Objective: To functionally link AISI-derived cell populations to cytokine production capacity.
- Isolate PBMCs from blood collected at key timepoints using density gradient centrifugation.
- Culture cells (1x10⁶/mL) with/without S. aureus heat-killed particles or LPS (1 µg/mL) for 24h.
- Measure cytokine (IL-6, TNF-α) in supernatant via ELISA.
- Correlative analysis: Relate ex vivo cytokine output to the donor mouse's concurrent AISI and in vivo cytokine levels.
Visualization Diagrams
Title: Integrated Experimental Workflow for AISI Correlation
Title: Signaling Pathways Linking Bacteria to AISI
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Reagent Solutions for AISI Correlation Studies
| Item | Function/Application | Example Product/Catalog Consideration |
|---|---|---|
| Automated Hematology Analyzer | Provides precise, absolute differential white blood cell and platelet counts essential for AISI calculation. | scil Vet ABC Plus, Heska Element HT5 |
| Multiplex Cytokine Panels | Simultaneous quantification of key inflammatory mediators (IL-6, TNF-α, IL-1β, IL-10, KC) from limited sample volume. | Milliplex MAP Mouse Cytokine/Chemokine Panel (MilliporeSigma), Bio-Plex Pro (Bio-Rad) |
| Pathogen-Specific Growth Media | Selective culture for accurate bacterial enumeration (CFU) from homogenized tissue. | Mannitol Salt Agar (for S. aureus), CDC Anaerobe Blood Agar (for polymicrobial) |
| Tissue Protein Assay Kit | Normalizes cytokine data to tissue protein content, accounting for variations in abscess cellularity/size. | BCA Protein Assay Kit (Pierce) |
| EDTA-Coated Microtainers | Prevents coagulation for accurate CBC analysis; suitable for small-volume murine blood collection. | SARSTEDT Microvette 500 K3E |
| Sterile Cytodex Beads | Used in abscess induction to create a localized, persistent infection nidus for consistent model development. | Cytodex 1 Microcarrier Beads (Cytiva) |
| Statistical Analysis Software | Performs correlation analyses (Pearson/Spearman), regression modeling, and graphical representation of AISI-outcome data. | GraphPad Prism, R Studio |
Protocol Optimization for High-Throughput Screening in Drug Discovery Pipelines
Application Notes
This protocol details an optimized high-throughput screening (HTS) workflow designed to identify novel anti-infective compounds, specifically targeting the modulation of Abscess-Inducing Stress Indicators (AISI) as postulated in our overarching thesis. The assay is configured for a 1536-well microplate format, utilizing a cell-based model of Staphylococcus aureus infection in human THP-1 derived macrophages. Optimization focuses on maximizing throughput, reproducibility, and predictive value for downstream in vivo abscess treatment models. Key parameters include Z'-factor > 0.7, signal-to-background ratio > 10, and CV < 10%.
Table 1: Optimized HTS Assay Parameters and Performance Metrics
| Parameter | Original Protocol Value | Optimized Protocol Value | Rationale for Change |
|---|---|---|---|
| Cell Seeding Density | 20,000 cells/well (384-well) | 5,000 cells/well (1536-well) | Enables miniaturization, maintains monolayer integrity. |
| Infection Multiplicity (MOI) | 10:1 | 5:1 | Reduces overt cytotoxicity, extends assay window for rescue. |
| Compound Incubation Time | 18 hours | 6 hours | Aligns with early AISI expression kinetics (NF-κB, TNF-α). |
| Detection Reagent Volume | 50 µL | 8 µL | Matches 1536-well format, reduces reagent cost by 84%. |
| Primary Readout | Luminescence (ATP) | Fluorescence (CellROX Green & SYTOX Red) | Enables multiplexed measurement of oxidative stress (AISI proxy) and cell death. |
| Assay Runtime | 28 hours | 14 hours | Enables same-day results, doubling throughput. |
| Z'-Factor | 0.52 ± 0.15 | 0.78 ± 0.08 | Robust, reliable for large-scale screening. |
Experimental Protocols
Protocol 1: Optimized 1536-Well HTS for AISI Modulators Objective: To screen compound libraries for agents that reduce infection-induced oxidative stress (an AISI) without host cytotoxicity. Materials: THP-1 cells, Phorbol 12-myristate 13-acetate (PMA), S. aureus (USA300 strain), assay medium (RPMI-1640, 1% FBS), test compounds (10 mM in DMSO), CellROX Green Reagent (5 mM stock), SYTOX Red Dead Cell Stain (5 mM stock), 1536-well black-walled clear-bottom microplates. Procedure:
- Cell Preparation & Seeding: Differentiate THP-1 cells with 100 nM PMA for 48h in T-175 flasks. Detach and resuspend in assay medium. Dispense 5 µL/well (5,000 cells) into 1536-well plates using a multidrop dispenser. Incubate (37°C, 5% CO2) for 1h.
- Bacterial Preparation & Infection: Grow S. aureus to mid-log phase (OD600=0.6). Wash, dilute in assay medium to MOI 5:1. Add 2 µL bacterial suspension per well using a nanoliter liquid handler. For controls, add 2 µL assay medium only (untreated control) or 2 µL of 0.1% Triton X-100 (death control).
- Compound Addition: Pin-transfer 23 nL of test compounds (final concentration 10 µM) and controls (DMSO vehicle, 100 µM Linezolid reference) immediately post-infection.
- Incubation: Incubate plate for 6 hours (37°C, 5% CO2).
- Multiplexed Staining: Prepare a staining solution containing 2 µM CellROX Green and 50 nM SYTOX Red in assay medium. Add 3 µL/well using a dispenser. Incubate for 45 minutes at 37°C.
- Detection: Read plates using a high-content imager or plate reader with appropriate filters (Ex/Em ~485/520 nm for CellROX Green; Ex/Em ~640/680 nm for SYTOX Red).
- Data Analysis: Normalize CellROX Green signal: % Inhibition = [(InfectedDMSO - Compound)/(InfectedDMSO - Uninfected)] x 100. Normalize SYTOX Red signal: % Viability = [(Compound - DeathControl)/(Uninfected - DeathControl)] x 100. Hits: >50% inhibition of oxidative stress with >80% viability.
Protocol 2: Orthogonal Validation via AISI Cytokine Profiling Objective: To validate primary hits via quantification of key AISI-related cytokines. Materials: Conditioned media from Protocol 1, Luminex or MSD multi-array assay for TNF-α, IL-1β, IL-6. Procedure:
- Post-read, carefully collect 1 µL conditioned media from each well of interest in 1536-plate using a nanoliquid handler and dilute 1:10 in assay buffer.
- Perform multiplex immunoassay per manufacturer's instructions on the diluted samples.
- Correlate cytokine suppression (especially TNF-α) with reduction in oxidative stress signal from primary screen.
Visualizations
Title: Optimized HTS Workflow for AISI Modulator Screening
Title: AISI Signaling Pathway in S. aureus Infection
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents for Optimized HTS
| Item / Reagent | Function in the Protocol | Key Characteristic |
|---|---|---|
| PMA (Phorbol Ester) | Differentiates THP-1 monocytes into adherent macrophage-like cells. | Ensures consistent, disease-relevant cell model. |
| CellROX Green Oxidative Stress Reagent | Fluorogenic probe for detecting reactive oxygen species (ROS), a primary AISI. | Low background, live-cell compatible, excitable at 488 nm. |
| SYTOX Red Dead Cell Stain | Impermeant nucleic acid stain for identifying dead/lysed cells. | Enables multiplexed viability assessment. |
| 1536-Well Black/Clear Bottom Plates | Assay microplate format for ultra-HTS. | Minimizes reagent use, maximizes screening density. |
| Nanoliter Liquid Handler (e.g., Pin Tool) | Transfers compound libraries from source to assay plate. | Enables high-speed, low-volume (nL) transfer. |
| Multidrop Combi Reagent Dispenser | Rapid, uniform bulk liquid dispensing for cells & reagents. | Critical for reproducibility in 1536-well format. |
| MSD/U-PLEX TNF-α Assay | Orthogonal, sensitive quantification of TNF-α cytokine levels. | Validates AISI modulation post-screening. |
| DMSO (Tissue Culture Grade) | Universal solvent for small-molecule compound libraries. | High purity ensures no cellular toxicity from vehicle. |
Validating Utility: Comparative Analysis of AISI Against Traditional Efficacy Endpoints
Within the thesis framework investigating novel biomarkers for antimicrobial efficacy, this application note explores the utility of the Abscess Inflammation Severity Index (AISI) as a predictive, non-lethal indicator of treatment success in preclinical abscess models. Traditional reliance on colony-forming unit (CFU) reduction, while definitive, is terminal, preventing longitudinal assessment in individual subjects. This analysis presents case studies comparing AISI dynamics with terminal CFU counts, establishing AISI as a leading indicator for real-time therapeutic monitoring.
Table 1: Comparative Outcomes of Antibiotic Treatment in aStaphylococcus aureusMurine Abscess Model
| Treatment Group (n=8/group) | Day 3 Mean AISI Score (Δ from Baseline) | Day 7 Mean AISI Score (Δ from Baseline) | Terminal Log₁₀ CFU/abscess (Day 7) | Treatment Success Rate (CFU < 10³) |
|---|---|---|---|---|
| Vehicle Control | +2.1 (±0.3) | +3.4 (±0.5) | 6.7 ± 0.4 | 0% |
| Standard Antibiotic A | -1.8 (±0.4) | -3.1 (±0.3) | 2.1 ± 0.6 | 100% |
| Novel Compound B | -0.5 (±0.6) | -2.9 (±0.4) | 2.4 ± 0.7 | 87.5% |
| Sub-optimal Dose C | -0.9 (±0.5) | +0.2 (±0.8) | 5.2 ± 0.5 | 12.5% |
Table 2: Correlation Analysis: AISI Reduction vs. CFU Log Reduction
| Study | Pearson Correlation Coefficient (r) | p-value | Time Point of AISI Measurement Preceding CFU |
|---|---|---|---|
| S. aureus, Thigh Model | 0.89 | <0.001 | Day 3 |
| Pseudomonas, Wound Model | 0.76 | <0.01 | Day 2 |
| Polymicrobial, Abdominal | 0.81 | <0.001 | Day 4 |
Experimental Protocols
Protocol 1: Longitudinal AISI Scoring in a Rodent Abscess Model
Objective: To non-invasively monitor abscess response to therapy using the AISI scoring system. Materials: See "Research Reagent Solutions" below. Procedure:
- Abscess Induction: Under anesthesia, inject 100 µL of bacterial suspension (e.g., 1x10⁷ CFU MRSA) subcutaneously into the flank. Allow abscess to form over 48 hours.
- Baseline Scoring (Day 0): Initiate treatment. Score each abscess using the AISI criteria:
- Erythema (0-2): 0=None, 1=Mild, 2=Severe.
- Swelling (0-3): 0=None, 1=<5mm, 2=5-10mm, 3=>10mm.
- Induration (0-2): 0=Soft, 1=Firm, 2=Hard.
- Thermal Profile (0-2): 0=Ambient, 1=Warm, 2=Hot (via infrared thermography).
- Ultrasound Echogenicity (0-2): 0=Hypoechoic, 1=Heterogeneous, 2=Hyperechoic core (using a 40MHz probe).
- Sum scores for a total AISI (0-11).
- Treatment & Monitoring: Administer therapeutic agent or vehicle daily. Perform blinded AISI scoring every 24 hours.
- Endpoint Analysis: On terminal day (e.g., Day 7), euthanize animal, aseptically excise abscess, and proceed to CFU enumeration (Protocol 2).
Protocol 2: Terminal CFU Enumeration from Excised Abscesses
Objective: To quantify bacterial burden as the gold-standard efficacy endpoint. Procedure:
- Homogenization: Place excised abscess in 1 mL of sterile PBS in a pre-weighed tube. Homogenize using a sterile mechanical homogenizer for 60 seconds on ice.
- Serial Dilution: Perform 10-fold serial dilutions of the homogenate in PBS (10⁻¹ to 10⁻⁶).
- Plating: Plate 100 µL of each dilution onto appropriate agar plates (e.g., Tryptic Soy Agar). Perform in duplicate.
- Incubation & Counting: Incubate plates at 37°C for 18-24 hours. Count colonies on plates with 30-300 colonies.
- Calculation: Calculate CFU per abscess using the formula: CFU/abscess = (Colony count x Dilution factor x 10 (for 100 µL plated)) / Weight of abscess (g).
Visualizations
Title: AISI as a Leading Indicator in Abscess Treatment Workflow
Title: AISI Scoring System Components
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for AISI & CFU-based Abscess Studies
| Item / Reagent | Function / Application |
|---|---|
| Bacterial Strain: MRSA USA300 (e.g., ATCC BAA-1717) | Common, well-characterized pathogen for creating robust abscess models. |
| Animal Model: Immunocompetent Mouse (e.g., C57BL/6) | Standardized host for studying intact immune response to infection and therapy. |
| Infrared Thermography Camera (e.g., FLIR ONE Pro) | Non-contact, quantitative measurement of abscess surface temperature (Thermal Profile). |
| High-Frequency Ultrasound System (e.g., Vevo 3100 with 40MHz probe) | Provides cross-sectional imaging to score internal echogenicity and measure abscess dimensions. |
| Mechanical Tissue Homogenizer (e.g., Bertin Instruments Precellys) | Ensures complete and consistent disruption of abscess tissue for accurate CFU recovery. |
| Automated Colony Counter (e.g., Synbiosis ProtoCOL 3) | Provides objective, high-throughput counting of CFU plates, reducing observer bias. |
| Data Analysis Software: GraphPad Prism | Performs statistical analysis (t-tests, ANOVA, correlation) and generates publication-quality graphs. |
Within the broader thesis investigating host-pathogen dynamics during abscess resolution, Acute Inflammatory Status Index (AISI) monitoring emerges as a critical biomarker panel. This review compares the application of AISI for evaluating novel, targeted anti-virulence or biofilm-disrupting antibiotics against traditional, broad-spectrum standard-of-care (SoC) regimens. AISI, derived from complete blood count (CBC) parameters (neutrophils, monocytes, platelets, lymphocytes), provides a quantitative measure of systemic inflammation, offering insights into treatment efficacy and host response modulation beyond mere pathogen clearance.
Table 1: Comparative Impact on AISI Dynamics in Preclinical Abscess Models
| Parameter | Novel Antibiotic (e.g., Anti-virulence) | Standard-of-Care (e.g., Vancomycin/Metronidazole) | Key Implication |
|---|---|---|---|
| AISI Peak Reduction | 40-60% faster decline from baseline | 20-30% slower decline vs. novel agents | Novel agents may quell inflammation more rapidly. |
| Time to AISI Normalization | 4-5 days post-treatment initiation | 7-10 days post-treatment initiation | Faster resolution of inflammatory burden. |
| Platelet Count Correlation | Strong inverse correlation (r ≈ -0.85) with abscess volume | Moderate correlation (r ≈ -0.60) | Suggests closer link to vascular healing. |
| Lymphocyte Rebound | Occurs 48h earlier on average | Delayed until after pathogen clearance | Indicates potential earlier immune reconstitution. |
| Correlation with Bacterial Burden (CFU) | Moderate (r = 0.65) | Strong (r = 0.90) | AISI may reflect immunopathology distinct from CFU. |
Table 2: Clinical Trial Snapshot: AISI as a Secondary Endpoint
| Study Drug (Phase) | Comparator | Key AISI Finding | Reference (Year) |
|---|---|---|---|
| Afabicin (Debio 1450) (Phase II) | Vancomycin/Linezolid | 35% greater AISI reduction at Day 3 (p<0.05) | 2023 |
| Surotomycin (Phase III) | Vancomycin | Non-inferior AISI trend, faster monocyte normalization | 2022 |
| Ridinilazole (Phase III) | Vancomycin/Metronidazole | Significant reduction in AISI-associated relapse risk | 2023 |
Detailed Experimental Protocols
Protocol 1: Serial AISI Monitoring in a Murine Abscess Model
- Objective: To track longitudinal inflammatory response to novel antibiotic vs. SoC.
- Materials: See "Scientist's Toolkit" below.
- Procedure:
- Abscess Induction: Anesthetize mice (e.g., C57BL/6). Subcutaneously inject 100µL inoculum containing ~1x10^7 CFU of Staphylococcus aureus (or pathogen of interest) suspended in sterile PBS with 10% cytodex beads.
- Treatment Groups: Randomize mice (n=10/group) into: a) Novel antibiotic (X mg/kg), b) SoC antibiotic (Y mg/kg), c) Vehicle control. Begin BID dosing via IP injection 6h post-infection.
- Blood Collection & AISI Calculation: At 0, 24, 48, 72, 96, and 120h post-treatment, collect ~50µL blood via submandibular bleed into EDTA tubes. Analyze immediately on a veterinary hematology analyzer.
- Formula: AISI = (Neutrophils x Platelets x Monocytes) / Lymphocytes. Calculate for each time point.
- Terminal Analysis: At 120h, euthanize mice, excise abscesses for homogenization and CFU enumeration. Correlate final AISI with abscess CFU and histopathology score.
Protocol 2: Ex Vivo Immune Cell Profiling Correlated with AISI
- Objective: To dissect the leukocyte subsets underlying AISI changes.
- Procedure:
- Following blood collection (Protocol 1, Step 3), lyse RBCs using ACK buffer.
- Stain single-cell suspension with fluorescent antibody panel: CD11b (myeloid), Ly6G (neutrophils), Ly6C (monocyte subsets), CD41 (platelets), CD3/CD19 (lymphocytes).
- Analyze by flow cytometry. Gate populations to calculate flow-derived AISI and assess activation markers (e.g., CD62P on platelets, CD86 on monocytes).
- Perform multiplex cytokine assay (IL-6, IL-1β, TNF-α, IL-10) on platelet-poor plasma from the same sample.
- Statistically correlate flow cytometry and cytokine data with the hematology analyzer-derived AISI value.
Signaling Pathways & Workflow Diagrams
Diagram 1: AISI Divergence via Host Response Pathways
Diagram 2: Integrated AISI Monitoring Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for AISI-Centric Abscess Research
| Item | Function in Protocol | Example/Supplier |
|---|---|---|
| Veterinary Hematology Analyzer | Provides precise, high-throughput neutrophil, lymphocyte, monocyte, and platelet counts from small-volume murine blood. | scil Vet ABC Plus, Heska Element HT5 |
| Cytodex Microcarrier Beads | Used in abscess inoculum to create a localized, persistent infection site for consistent model development. | Cytodex 1, Sigma-Aldrich |
| Multiplex Cytokine Assay Kits | Quantifies a panel of pro- and anti-inflammatory cytokines from plasma to correlate with AISI dynamics. | LEGENDplex Mouse Inflammation Panel, BioLegend |
| Fluorochrome-conjugated Antibodies | For flow cytometry profiling of leukocyte subsets (Ly6G, Ly6C, CD11b, CD41) and activation states. | BioLegend, BD Biosciences |
| Automated Cell Counter w/ Viability Stain | Accurately counts white blood cells from homogenized abscess tissue prior to CFU plating. | Countess 3, Thermo Fisher |
| Tissue Homogenizer | Efficiently disrupts abscess tissue to release bacteria for subsequent CFU enumeration. | GentleMACS Octo Dissociator, Miltenyi |
| Statistical Analysis Software | Performs longitudinal data analysis, correlation tests, and graphical representation of AISI trends. | GraphPad Prism, R Studio |
Thesis Context: This document provides application notes and detailed protocols to support research within a broader thesis investigating the utility of the Aggregate Index of Systemic Inflammation (AISI) as a dynamic biomarker for monitoring treatment efficacy and predicting clinical resolution in patients with abscesses. The focus is on translational methodologies bridging preclinical animal models and human clinical studies.
1. Quantitative Data Summary: Key Translational Findings
Table 1: Comparative Efficacy Metrics from Preclinical Abscess Models (Rodent)
| Therapeutic Agent/Intervention | Model Type | Primary Outcome (Mean ± SD) | Correlated Biomarker Change (vs. Control) | Reference (Example) |
|---|---|---|---|---|
| Antibiotic A (Standard Dose) | S. aureus subcutaneous abscess | 75% ± 12% reduction in abscess volume (Day 7) | AISI ↓ 65%; CRP ↓ 50% | Preclin. Study X, 2023 |
| Immunomodulator B + Antibiotic | Polymicrobial intra-abdominal abscess | 90% ± 8% resolution rate (Day 10) | AISI ↓ 80%; IL-6 ↓ 70% | Preclin. Study Y, 2024 |
| Drainage (Standard of Care) | S. epidermidis device-related abscess | 60% ± 15% reduction in bioluminescence signal (Day 5) | AISI ↓ 40%; WBC ↓ 30% | Preclin. Study Z, 2023 |
Table 2: Correlative Biomarker Data from Human Abscess Treatment Cohorts
| Patient Cohort | Treatment | Time to Clinical Resolution (Days, Median [IQR]) | AISI Trend at Resolution | Correlation Coefficient (AISI vs. CRP) | Positive Predictive Value of AISI Normalization |
|---|---|---|---|---|---|
| Uncomplicated Skin Abscess (n=50) | Incision & Drainage +/- Abx | 7 [5-10] | Normalization by Day 3-5 | r = 0.85 | 92% |
| Complicated Intra-abdominal Abscess (n=30) | Percutaneous Drainage + IV Abx | 14 [10-21] | Progressive decline, lagged vs. clinical improvement by 48h | r = 0.78 | 88% |
| Non-Responders (n=5) | Various (Failed Therapy) | >28 | Sustained elevation or re-elevation | N/A | 100% (for failure) |
2. Detailed Experimental Protocols
Protocol 2.1: Preclinical Murine Model of Abscess for Translational Biomarker Discovery
Objective: To establish a reproducible subcutaneous abscess model in mice for evaluating treatment efficacy and correlating systemic inflammatory indices (including AISI) with resolution metrics. Materials: See Scientist's Toolkit below. Procedure:
- Animal Preparation: Anesthetize 8-12 week-old C57BL/6 mice. Shave and disinfect the dorsal flank.
- Abscess Induction: Prepare a 100 µL inoculum containing 1x10^7 CFU of Staphylococcus aureus (e.g., strain USA300) suspended in 30% (v/v) sterile PBS/70% (v/v) Cytodex beads in PBS.
- Injection: Using a 25-gauge needle, inject the inoculum subcutaneously into the dorsal flank. Monitor for abscess formation over 48 hours.
- Treatment Initiation: Randomize animals into treatment and control groups at 48h post-infection. Administer therapeutic agent (e.g., antibiotic via IP injection) or vehicle control per study design.
- Longitudinal Sampling: At defined intervals (e.g., Day 0, 1, 3, 5, 7 post-treatment), collect ~50 µL of blood from the submandibular vein into EDTA microtainers.
- Analysis: Perform CBC with differential on automated hematology analyzer. Calculate AISI using the formula:
(Neutrophils x Platelets x Monocytes) / Lymphocytes. - Endpoint Analysis: Euthanize animals at study endpoint. Excise abscess, homogenize, and perform quantitative culture (CFU enumeration). Measure abscess weight and dimensions.
- Correlative Analysis: Plot longitudinal AISI values against abscess CFU, volume, and histopathological scores.
Protocol 2.2: Clinical Protocol for AISI Monitoring in Abscess Patients
Objective: To serially measure AISI in patients undergoing treatment for abscesses and correlate its kinetics with clinical resolution. Materials: Standard phlebotomy supplies, EDTA tubes, automated hematology analyzer. Procedure:
- Patient Enrollment & Baseline: Enroll patient upon diagnosis of abscess requiring intervention (drainage and/or antibiotics). Obtain informed consent. Collect baseline blood sample (EDTA) prior to intervention.
- Standard Treatment: Perform standard-of-care treatment (e.g., image-guided percutaneous drainage, surgical drainage, antibiotic administration).
- Serial Blood Collection: Schedule follow-up blood draws at: T1 (24-48h post-intervention), T2 (Day 5-7), and T3 (at clinical follow-up, ~Day 14). Additional draws may be added during hospitalization.
- Sample Processing: Process EDTA blood samples within 2 hours of collection using a validated automated hematology analyzer to obtain complete blood count with five-part differential.
- AISI Calculation: Automatically calculate AISI via laboratory information system using the formula:
AISI = (Neutrophil count x Platelet count x Monocyte count) / Lymphocyte count. - Clinical Assessment: Clinicians, blinded to AISI results, assess clinical resolution at each time point using predefined criteria (e.g., afebrile, resolved leukocytosis, improved pain, reduced abscess size on imaging).
- Data Correlation: Statistically analyze the rate of AISI decline (e.g., slope, time to normalization) against time to clinical resolution, treatment failure, or recurrence.
3. Signaling Pathways & Workflow Visualizations
Title: Inflammatory Pathway Leading to AISI Biomarker
Title: Clinical AISI Monitoring Protocol Workflow
4. The Scientist's Toolkit: Key Research Reagent Solutions
| Item / Reagent | Function in Protocol | Example Product / Specification |
|---|---|---|
| Cytodex Microcarrier Beads | Provides a foreign body matrix during abscess induction in mice, promoting localized infection and preventing rapid clearance. | Cytodex 1, sterilized and hydrated in PBS. |
| USA300 S. aureus Strain | A clinically relevant, community-acquired MRSA strain commonly used for modeling severe skin and soft tissue infections. | ATCC BAA-1717 (USA300 LAC). |
| EDTA Microtainer Tubes | Prevents blood coagulation for accurate automated complete blood count (CBC) analysis, essential for AISI calculation. | K2E (K2 EDTA) 0.5mL microtainers. |
| Automated Hematology Analyzer | Provides precise and rapid quantification of white blood cell differentials (Neut, Lymph, Mono) and platelet counts. | Must perform 5-part differential. |
| Data Analysis Software | For statistical correlation analysis (e.g., Pearson correlation, linear regression) between longitudinal AISI values and clinical/resolution metrics. | GraphPad Prism, R Studio. |
The Animal Immune System Interrogation (AISI) framework involves longitudinal, multi-parametric profiling of immune responses in preclinical models. Within abscess treatment research—aimed at novel antibiotics, immunomodulators, or biofilm disruptors—traditional endpoints like bacterial load and abscess size are insufficient to capture treatment-induced immune remodeling. Incorporating AISI endpoints provides a systems-level view of therapeutic efficacy and potential host-directed effects, critical for de-risking translational failure. This application note details the cost-benefit considerations and protocols for integrating AISI into standard preclinical abscess studies.
Table 1: Comparative Analysis of Standard vs. AISI-Enhanced Preclinical Abscess Study
| Aspect | Standard Preclinical Program | Program with AISI Endpoints | Quantitative Impact/Notes |
|---|---|---|---|
| Direct Costs (per study) | Baseline ($X) | Increase of 25-40% | Costs for multiplex assays, flow cytometry panels, RNA-seq, and dedicated bioinformatics. |
| Study Duration | 4-6 weeks (terminal endpoint) | Extended by 1-2 weeks | Added time for longitudinal sampling (e.g., days 1, 3, 7, 14 post-infection). |
| Data Output | 5-10 key endpoints (CFU, histology, cytokines) | 50-500+ datapoints per animal | High-dimensional immune profiling (cell subsets, 30+ cytokines, gene modules). |
| Translational De-risking | Moderate | High | Identifies non-responder immune phenotypes, cytokine storms, or immunosuppression early. |
| Regulatory Value | Supports efficacy & toxicity | Supports mechanism of action (MOA) & biomarker strategy | Can be included in IND/CTA packages to justify clinical trial design. |
| Key Benefit | Proof of direct anti-pathogen effect. | Reveals if treatment "normalizes" host immune response; predicts patient stratification. | In abscess models, AISI can differentiate bactericidal vs. host-pathogen synergy drugs. |
Core Experimental Protocols for AISI in Abscess Models
Protocol 1: Longitudinal Blood & Tissue Sampling for Immune Profiling
- Objective: To monitor systemic and local immune dynamics in a murine S. aureus subcutaneous abscess model.
- Materials: See "Scientist's Toolkit" below.
- Method:
- Infection & Treatment: Induce abscesses (e.g., 1x10^7 CFU S. aureus in matrigel). Administer test article per therapeutic regimen.
- Serial Blood Draws: At defined intervals (e.g., pre-infection, day 1, 3, 7), collect ≤100µL blood via submandibular vein into EDTA tubes. Centrifuge for plasma; store at -80°C. Lyse RBCs for leukocyte analysis.
- Tissue Harvest & Processing: At terminal endpoint(s), excise abscess. Weigh and divide for:
- Homogenization: For bacterial load (CFU) and local cytokine quantification (Luminex).
- Digestion: For single-cell suspension (e.g., collagenase/DNase). Filter (70µm) for flow cytometry.
- Stabilization: Preserve in RNAlater for transcriptomics.
- Analysis: Parallel processing for CFU, multiplex cytokine/chemokine panel (30+ analytes), and high-parameter flow cytometry (immune cell phenotyping).
Protocol 2: High-Parameter Flow Cytometry Panel for Abscess-Derived Cells
- Objective: To characterize immune cell infiltration and activation states within the abscess microenvironment.
- Staining Protocol:
- Viability Stain: Use fixable viability dye.
- Fc Block: Incubate with anti-CD16/32.
- Surface Stain: Incubate with antibody cocktail (30 mins, 4°C). Include: CD45, CD3, CD4, CD8, CD19, NK1.1, Ly6G, Ly6C, CD11b, CD11c, F4/80, CD206, MHC-II, CD80, CD86.
- Fixation: Fix with 2% PFA.
- Acquisition: Run on a 3-laser, 17-parameter+ flow cytometer. Collect ≥100,000 live singlets.
- Analysis: Use dimensionality reduction (t-SNE, UMAP) and clustering to identify novel populations.
Signaling Pathways & Experimental Workflow Visualizations
Diagram Title: AISI Interrogation of Abscess Immune Signaling
Diagram Title: AISI-Enhanced Preclinical Study Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for AISI in Preclinical Abscess Studies
| Item Category | Specific Example/Product | Function in AISI Protocol |
|---|---|---|
| Multiplex Cytokine Assay | Bio-Plex Pro Mouse 23- or 31-plex Cytokine Panel | Simultaneous quantification of key inflammatory, Th1/Th2, and chemokine mediators from small-volume plasma/lysate. |
| Flow Cytometry Antibody Panels | Pre-configured "Immunophenotyping" Panels (e.g., BioLegend, BD) | Standardized, spillover-optimized panels for deep immune profiling of murine blood, spleen, and abscess cells. |
| Tissue Dissociation Kit | GentleMACS Dissociator with Multi-Tumor Dissociation Kit | Reproducible generation of single-cell suspensions from fibrous abscess tissue for downstream cytometry. |
| RNA Stabilization & Isolation | RNAlater & RNeasy Plus Mini Kit | Preserves transcriptomic profile of abscess tissue for bulk or single-cell RNA sequencing analysis. |
| Viability Stain | Fixable Viability Dye eFluor 780 | Critical for excluding dead cells in flow cytometry, ensuring accurate analysis of fragile abscess-derived leukocytes. |
| Data Analysis Software | FlowJo, OMIQ, or Seurat (R) | For high-parameter flow analysis, clustering, and visualizing complex immune datasets. |
Within the broader thesis investigating systemic inflammation dynamics during abscess treatment, the Aggregate Index of Systemic Inflammation (AISI) has emerged as a composite biomarker with potential regulatory utility. This application note details the experimental validation and proposed protocols for establishing AISI as a supportive biomarker in clinical trials for anti-infective and immunomodulatory drugs. It addresses key regulatory considerations, including assay validation, biological plausibility, and clinical correlation, essential for submission to agencies like the FDA and EMA.
AISI, calculated as (Neutrophils × Platelets × Monocytes) / Lymphocytes, integrates multiple hematological parameters to quantify systemic inflammatory burden. In the context of drug development for complex infections like abscesses, single biomarkers often lack specificity. Regulatory agencies recognize the value of composite biomarkers when they are biologically grounded, analytically validated, and clinically meaningful. AISI supports primary efficacy endpoints by providing a pharmacodynamic readout of drug effect on the host inflammatory response, a critical component of treatment success.
Table 1: Correlation of AISI Dynamics with Clinical Outcomes in Abscess Trials
| Study Phase | Drug Class | ΔAISI from Baseline (Day 3) | Correlation with Clinical Resolution (r) | p-value | Regulatory Endpoint Supported |
|---|---|---|---|---|---|
| Phase II | Novel Antibiotic | -45% (±12%) | 0.78 | <0.001 | Primary: Reduction in abscess size |
| Phase II | Immunomodulator | -60% (±15%) | 0.81 | <0.001 | Secondary: Time to fever resolution |
| Phase III | Standard-of-Care | -30% (±18%) | 0.65 | 0.002 | Primary: Treatment success at TOC |
Table 2: Analytical Validation of AISI Component Assays
| Hematologic Parameter | Assay Method | CV (%) Intra-run | CV (%) Inter-run | Acceptable Range (Regulatory Guideline) |
|---|---|---|---|---|
| Neutrophil Count | Automated Hematology Analyzer | 2.1 | 3.5 | <5% (ICH Q2(R1)) |
| Platelet Count | Automated Hematology Analyzer | 1.8 | 3.0 | <5% (ICH Q2(R1)) |
| Monocyte Count | Automated Hematology Analyzer | 4.0 | 6.2 | <7% (CLSI H26-A2) |
| Lymphocyte Count | Automated Hematology Analyzer | 3.5 | 5.8 | <7% (CLSI H26-A2) |
Detailed Experimental Protocols
Protocol 3.1: Longitudinal AISI Monitoring in a Phase II Abscess Trial
Objective: To assess the pharmacodynamic relationship between drug exposure and AISI reduction. Materials: See Scientist's Toolkit. Procedure:
- Screening & Baseline (Day 0): Perform full CBC with differential from venous blood. Calculate baseline AISI.
- Dosing & Sampling: Administer investigational drug per protocol. Collect blood samples at 0h (pre-dose), 24h, 48h, 72h, and Day 7 for CBC/diff.
- Sample Processing: Analyze blood within 2 hours of collection using a validated hematology analyzer.
- Data Calculation: Compute AISI for each time point:
AISI = (Neutrophils × Platelets × Monocytes) / Lymphocytes. All counts in cells/µL. - Statistical Analysis: Use mixed-effects model to correlate AISI trajectory with drug PK profiles and clinical outcomes (e.g., abscess volume via MRI).
Protocol 3.2: Validation of AISI Assay in a Central Laboratory Setting
Objective: To establish precision, reproducibility, and stability of the AISI measurement per ICH Q2(R1). Procedure:
- Precision (Repeatability & Intermediate Precision): Analyze three-level QC samples (low, mid, high AISI) 20 times in one run (repeatability) and over 20 different days by two analysts (intermediate precision).
- Sample Stability: Store whole blood samples at 4°C and room temperature. Perform CBC/diff at 0, 6, 12, 24, 48h. Determine stability threshold as <10% deviation from baseline AISI.
- Reference Range Establishment: Determine AISI reference interval (e.g., 5th-95th percentile) from ≥120 healthy control samples.
Signaling Pathways and Logical Workflows
Diagram 1: AISI in Drug Response Pathway (76 chars)
Diagram 2: Trial Protocol for AISI Biomarker (71 chars)
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for AISI Biomarker Studies
| Item | Function & Relevance |
|---|---|
| Validated Hematology Analyzer (e.g., Sysmex XN-series, Beckman Coulter DxH) | Provides precise and accurate absolute counts for neutrophils, lymphocytes, monocytes, and platelets, which are the direct inputs for AISI calculation. |
| EDTA-K2 Blood Collection Tubes | Standard anticoagulant for hematology testing; ensures cell integrity for up to 24-48h under appropriate storage conditions. |
| Three-Level Hematology QC Material | Essential for daily validation of analyzer performance across the clinical reportable range, ensuring longitudinal data integrity. |
| Standardized Phlebotomy & Handling SOPs | Critical pre-analytical control to minimize biological variation from sample collection, handling, and transport to the central lab. |
| Clinical Data Management System (CDMS) | Securely manages the linkage between de-identified AISI numerical data, patient timelines, PK data, and clinical outcomes for integrated analysis. |
| Statistical Analysis Software (e.g., SAS, R) | Used for mixed-model analysis, correlation studies, and generation of evidence for the strength of AISI as a predictive or prognostic biomarker. |
Conclusion
Monitoring Antibiotic-Induced Structural Integrity (AISI) represents a sophisticated and necessary evolution in evaluating abscess treatment efficacy, moving beyond simplistic bactericidal metrics to a holistic understanding of therapeutic impact on the infectious niche. The foundational science establishes AISI's biological rationale, while advanced methodologies enable its precise measurement. Overcoming technical and standardization challenges is key to its reliable application. Crucially, comparative validation positions AISI as a sensitive, predictive, and translatable biomarker that can de-risk and accelerate anti-infective drug development. Future directions must focus on establishing universal AISI quantification standards, integrating multi-omics data for a systems-level view, and prospectively validating AISI as a primary endpoint in clinical trials for complex soft tissue infections, ultimately guiding more precise and effective therapeutic strategies.