Mouse Peritonitis Models: A Comprehensive Guide for Evaluating Inflammatory Responses in Preclinical Research
This article provides a systematic overview of mouse peritonitis models, essential tools for studying inflammatory responses, sepsis, and evaluating novel therapeutics.
Mouse Peritonitis Models: A Comprehensive Guide for Evaluating Inflammatory Responses in Preclinical Research
Abstract
This article provides a systematic overview of mouse peritonitis models, essential tools for studying inflammatory responses, sepsis, and evaluating novel therapeutics. Tailored for researchers and drug development professionals, it covers the foundational pathophysiology of peritonitis, details established and novel methodologies like fecal-induced peritonitis (FIP) and cecal ligation and puncture (CLP), and addresses critical troubleshooting for model standardization. It further explores validation techniques, including robust sepsis scoring systems and comparative analyses of model translatability, offering a complete framework for designing, executing, and interpreting preclinical studies in inflammatory diseases.
Understanding Peritonitis Pathophysiology and Model Selection Criteria
The Clinical Significance of Peritonitis in Human Disease
Peritonitis is a serious medical condition characterized by inflammation of the peritoneum, the thin layer of tissue that lines the inner wall of the abdomen and covers the abdominal organs [1] [2]. This condition typically arises from bacterial or fungal infections but can also be triggered by chemical irritation from fluids that leak into the peritoneal cavity from damaged organs [2]. Peritonitis represents a medical emergency that requires immediate intervention, as it can rapidly progress to life-threatening systemic infection (sepsis), organ failure, and death if left untreated [1] [2].
The clinical significance of peritonitis extends across multiple medical specialties, including emergency medicine, surgery, gastroenterology, and nephrology. For researchers and drug development professionals, understanding the pathophysiology of peritonitis is crucial for developing novel therapeutic strategies. Mouse models of peritonitis have become indispensable tools for investigating the inflammatory responses, immune mechanisms, and potential treatments for this condition [3] [4] [5].
Classification and Etiology
Peritonitis is clinically classified into different types based on its underlying cause and mechanism. The table below summarizes the main classifications and their characteristics.
Table 1: Classification and Causes of Peritonitis
| Type | Underlying Causes | Key Characteristics |
|---|---|---|
| Spontaneous Bacterial Peritonitis (SBP) [1] [2] | Liver cirrhosis, kidney disease, ascites from congestive heart failure or cancer [1] [2] | Primary infection without an obvious source of contamination; common in patients with advanced liver disease and ascitic fluid buildup. |
| Secondary Peritonitis [1] [2] | Perforated appendix, stomach ulcer, diverticulitis, inflammatory bowel disease, traumatic injury, pancreatitis, surgical complications [1] [2] | Caused by a hole/rupture in an abdominal organ or direct contamination; most common form. |
| Peritoneal Dialysis-Associated [1] | Contamination during dialysis procedures (poor hygiene, tainted equipment) [1] | Infection related to peritoneal dialysis catheters; a major complication of this treatment modality. |
| Chemical Peritonitis [2] | Leakage of sterile fluids (bile, stomach acid, pancreatic enzymes) [2] | Inflammation triggered by non-infectious irritants before potential secondary bacterial infection. |
Pathophysiology and Inflammatory Mechanisms
The pathophysiology of peritonitis involves a complex cascade of immune responses initiated when pathogens or irritants breach the peritoneal cavity. Macrophages play a pivotal role as the first line of defense, recognizing pathogens and releasing pro-inflammatory cytokines such as IL-1β, IL-6, and TNF-α [4]. This cytokine storm recruits neutrophils and other immune cells to the site of infection, leading to the hallmark inflammation of the peritoneum [4].
Recent research has uncovered novel molecular mechanisms driving this excessive inflammation. The transcription factor IKZF1 has been identified as a key regulator that exacerbates the inflammatory response in macrophages during acute peritonitis [3] [4]. Mechanistically, IKZF1 directly represses Succinate Dehydrogenase Complex Iron Sulfur Subunit B (SDHB) by recruiting histone deacetylase 3 (HDAC3) to deacetylate SDHB. This epigenetic silencing disrupts mitochondrial function, leading to reactive oxygen species (ROS) accumulation, reduced ATP production, and succinate buildup, which in turn amplifies pro-inflammatory signaling [3] [4]. This IKZF1/HDAC3-SDHB-succinate axis represents a promising therapeutic target for modulating the inflammatory response in peritonitis.
Figure 1: Inflammatory Signaling Pathway in Peritonitis. The diagram illustrates the key molecular and cellular events triggered by bacterial infection or chemical irritation, culminating in systemic inflammation.
Concurrently, transcriptomic analyses of blood from murine peritonitis models have revealed systemic changes in gene expression. Studies using LPS-induced peritonitis have identified 290 differentially expressed genes (DEGs), with 242 upregulated and 48 downregulated [5]. Activated pathways include NOD-like receptor signaling, Toll-like receptor signaling, apoptosis, and phagocytosis, while pathways involved in adaptive immunity, such as Th1/Th2 cell differentiation and T-cell receptor signaling, are suppressed [5]. This systemic immunosuppressive state often follows the initial hyperinflammatory phase and contributes to the vulnerability to secondary infections.
Established Mouse Models of Peritonitis
Mouse models are fundamental for studying the inflammatory responses in peritonitis. The table below summarizes the key quantitative findings from recent studies utilizing different models.
Table 2: Quantitative Outcomes from Mouse Peritonitis Models
| Model Type | Key Experimental Outcomes | Reference |
|---|---|---|
| Cecal Ligation and Puncture (CLP) | IKZF1 expression significantly upregulated in macrophages; Lenalidomide treatment attenuated inflammatory responses and lung injury. [3] [4] | Liu et al., 2025 |
| LPS-Induced | 290 differentially expressed genes (DEGs) identified in blood: 242 up-regulated, 48 down-regulated. [5] | Li et al., 2025 |
| MSSA Lethal Peritonitis | 6-times lavage with PD solution significantly reduced 24-h mortality and prevented rough fur, intraabdominal adhesion, and pus formation. [6] | PMC, 2025 |
| IL-1β-Induced | Peritoneal cells harvested 3 hours post intraperitoneal injection of 25 ng IL-1β in 200 µL PBS. [7] | Grieshaber-Bouyer et al. |
Cecal Ligation and Puncture (CLP) Model
The Cecal Ligation and Puncture (CLP) model is a widely used and clinically relevant polymicrobial model that mimics human perforated appendicitis or diverticulitis [3] [4].
Protocol:
- Anesthesia: Induce anesthesia in mice (e.g., 8-week-old male WT) via isoflurane inhalation [4].
- Laparotomy: Perform a midline abdominal incision to exteriorize the cecum.
- Ligation: Ligate the cecum below the ileocecal valve without causing intestinal obstruction.
- Puncture: Puncture the ligated cecum once with a 22-gauge needle to extrude a small amount of feces [4].
- Closure: Return the cecum to the abdominal cavity and close the abdominal wall in layers.
- Resuscitation: Administer subcutaneous saline (e.g., 0.3 mL) for fluid resuscitation immediately after surgery [4].
- Sham Control: For sham-operated controls, perform the same surgical procedure without ligation and puncture.
LPS-Induced Peritonitis Model
The intraperitoneal injection of Lipopolysaccharide (LPS), a component of the Gram-negative bacterial cell wall, provides a model for studying the initial systemic inflammatory response [5].
Protocol:
- Animals: Use male C57BL/6 mice (6-8 weeks old) [5].
- Preparation: Prepare an LPS solution in sterile phosphate-buffered saline (PBS).
- Injection: Administer LPS (e.g., 10 mg/kg) via intraperitoneal injection [5].
- Control Group: Inject control mice with an equal volume of sterile PBS.
- Sample Collection: Euthanize mice at the desired time point (e.g., 3-24 hours post-injection) to collect blood, peritoneal lavage fluid, or tissues for analysis.
IL-1β-Induced Peritonitis Model
This model involves direct injection of the pro-inflammatory cytokine IL-1β to study specific aspects of the cytokine-driven inflammatory response [7].
Protocol:
- Injection: Inject mice (e.g., male WT, 8 weeks old) intraperitoneally with 25 ng of IL-1β in 200 µL of PBS [7].
- Harvesting: Euthanize the mice 3 hours post-injection.
- Cell Collection: Harvest peritoneal cells from the peritoneum by lavage with 5 mL of cold PBS [7].
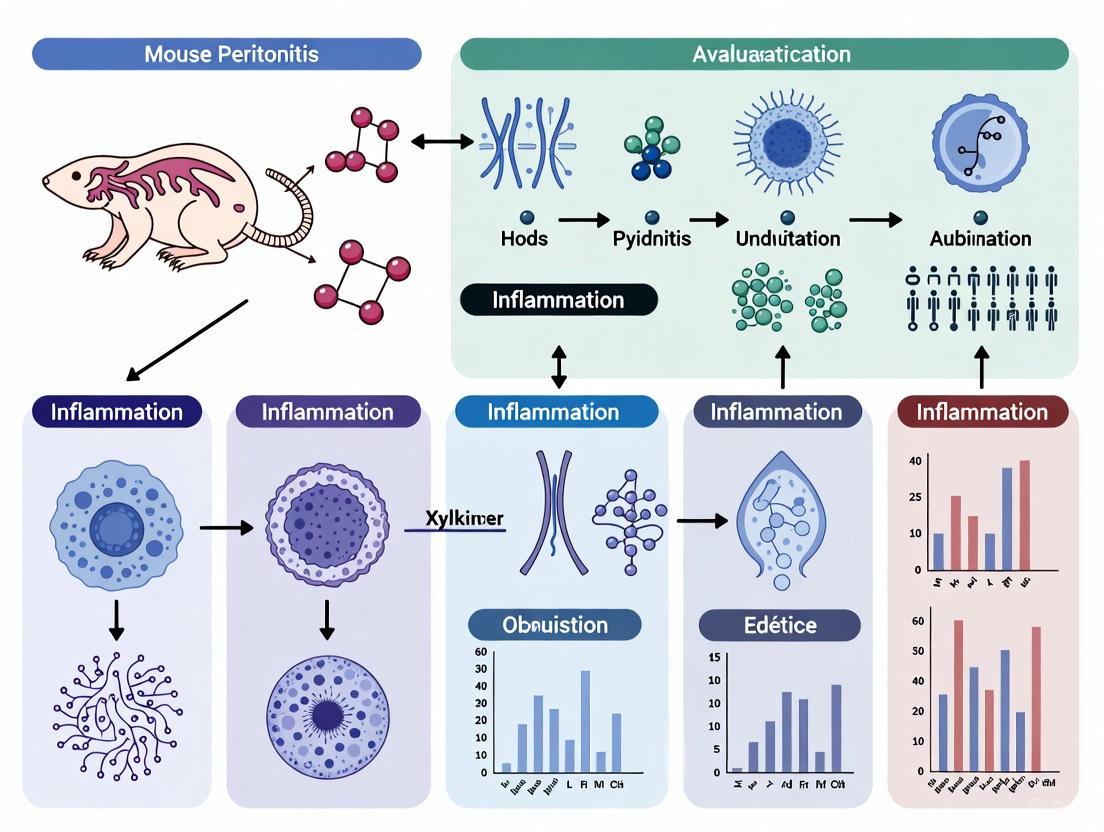
Figure 2: Mouse Peritonitis Model Workflow. The diagram outlines the primary experimental models used in peritonitis research and their main applications.
Research Reagent Solutions
The following table details essential reagents and materials used in peritonitis research, facilitating experimental reproducibility for scientists and drug developers.
Table 3: Essential Research Reagents for Peritonitis Models
| Reagent/Material | Function/Application | Example Specification |
|---|---|---|
| Lenalidomide [3] [4] | IKZF1 inhibitor used to attenuate macrophage-mediated inflammation and mitigate lung injury. | Administered to assess effects on inflammatory response. |
| Thioglycollate Broth [4] | Elicitant for recruiting macrophages to the peritoneal cavity prior to isolation. | 3% (w/v), injected intraperitoneally 3 days before cell harvest. |
| Low GDP Neutral pH PD Solution [6] | Biocompatible solution for peritoneal lavage; used to study efficacy of lavage monotherapy. | e.g., Midpeliq 135. |
| LPS (Lipopolysaccharide) [5] | Endotoxin used to induce sterile, Gram-negative bacterial-like inflammatory response. | 10 mg/kg, administered intraperitoneally. |
| Recombinant IL-1β [7] | Pro-inflammatory cytokine used to induce specific acute inflammatory response. | 25 ng in 200 µL PBS, injected intraperitoneally. |
| MSSA JCM 2413 [6] | Bacterial strain for creating lethal peritonitis models to test therapeutic interventions. | Methicillin-Susceptible S. aureus, e.g., 1x10^10 CFU for LD100 in rats. |
| Antibodies for ELISA [4] | Quantification of cytokine levels (e.g., TNF-α, IL-6, IL-1β) in lavage fluid or serum. | e.g., LEGEND MAX Mouse ELISA Kits. |
Therapeutic Insights and Future Directions
Current treatment for peritonitis in humans primarily involves broad-spectrum antibiotics and supportive care with IV fluids to prevent shock and correct fluid imbalances [2]. Surgical intervention is often required to address the underlying cause, such as repairing a perforated organ [1] [2]. For patients on peritoneal dialysis, strict hygiene protocols are critical for prevention [1].
Research from animal models is driving the development of novel therapeutic strategies. The identification of the IKZF1/HDAC3-SDHB axis suggests that targeting IKZF1 with drugs like lenalidomide or enhancing acetylation with agents like acetate could represent promising adjunct therapies to control excessive inflammation [3] [4]. Furthermore, studies demonstrating that peritoneal lavage with biocompatible PD solution significantly reduces mortality and severity in a lethal peritonitis model, even without antibiotics, challenge current clinical guidelines and suggest a potential role for mechanical cleansing in severe cases [6].
The translation of findings from mouse models to human applications is strengthened by integrated approaches. Validation of hub genes identified in mouse blood transcriptomics (e.g., LDLR, ZAP70) against single-cell RNA-sequencing datasets from human sepsis patients confirms conserved expression patterns and enhances the clinical relevance of these targets [5]. This multi-scale research strategy, combining animal models, omics technologies, and computational biology, provides a powerful framework for uncovering the complex mechanisms of peritonitis and developing more effective, targeted treatments.
Peritonitis, an inflammatory condition of the peritoneal lining, represents a life-threatening clinical challenge with mortality rates remaining as high as 20-35% despite advances in management protocols [8]. This condition arises from diverse etiologies including gastrointestinal perforation, chemical irritation, bacterial contamination, and catheter-related infections [4] [8]. The peritoneal membrane consists of a single layer of mesothelial cells overlying a vascular, lymph-rich sub-mesothelial matrix, functioning as both a physical barrier and an active immune sentinel [8]. Upon insult, resident macrophages and mesothelial cells initiate a robust inflammatory response, releasing cytokines and chemokines that recruit additional immune cells to the infection site [4] [8].
In experimental settings, mouse models of peritonitis have proven invaluable for dissecting the underlying molecular mechanisms. The most commonly employed models include lipopolysaccharide (LPS)-induced peritonitis, cecal ligation and puncture (CLP), and more recently, meconium slurry-induced peritonitis [5] [3] [9]. These models replicate key aspects of human disease and have identified three central inflammatory pathways that drive disease progression: cytokine signaling, Toll-like receptor (TLR)/NF-κB activation, and NLRP3 inflammasome assembly. Understanding the interplay between these pathways provides crucial insights for developing targeted therapeutic strategies for this devastating condition.
Key Inflammatory Pathways in Peritonitis
Cytokine Signaling Network
Cytokines serve as crucial molecular messengers that coordinate the immune response during peritonitis. Upon peritoneal injury or infection, resident macrophages and mesothelial cells rapidly release pro-inflammatory cytokines including tumor necrosis factor-alpha (TNF-α), interleukin-6 (IL-6), and interleukin-1 beta (IL-1β) [4] [8]. These cytokines function in an orchestrated cascade to amplify the inflammatory response, inducing fever, pain, vasodilation, and endothelial activation that facilitates immune cell infiltration [10] [11]. IL-1β induces the expression of genes that control fever, pain threshold, vasodilatation, and hypotension, while IL-6 serves as a potent inducer of acute phase proteins including C-reactive protein (CRP) [10] [8]. Clinical studies have demonstrated that IL-6 and IL-8 are massively elevated in the ascites of infants with meconium peritonitis, suggesting their potential utility as therapeutic targets [9].
The cytokine network exhibits both synergistic and regulatory interactions during peritonitis progression. For instance, TNF-α can stimulate the production of other cytokines including IL-1β and IL-6, creating an inflammatory amplification loop [11]. Simultaneously, anti-inflammatory cytokines such as IL-10 are upregulated to counterbalance this pro-inflammatory response and prevent excessive tissue damage [4]. The dynamic equilibrium between pro-inflammatory and anti-inflammatory cytokines ultimately determines disease severity and clinical outcomes, with persistent elevation of pro-inflammatory cytokines correlating with progression to sepsis and multiple organ dysfunction [4].
TLR/NF-κB Signaling Pathway
The Toll-like receptor (TLR) and nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB) pathway represents the primary signaling cascade that initiates the inflammatory response in peritonitis. TLRs are pattern recognition receptors (PRRs) that detect conserved microbial components known as pathogen-associated molecular patterns (PAMPs), such as lipopolysaccharide (LPS) from Gram-negative bacteria, as well as damage-associated molecular patterns (DAMPs) released from injured host cells [12] [10]. In peritonitis, LPS binding to TLR4 activates downstream signaling adaptors including myeloid differentiation primary response protein (MyD88) and interleukin-1 receptor-associated kinase (IRAK), ultimately leading to the nuclear translocation of NF-κB [12] [11].
Once in the nucleus, NF-κB functions as a master transcriptional regulator that upregulates the expression of numerous pro-inflammatory mediators, including cytokines (TNF-α, IL-1β, IL-6), chemokines, and adhesion molecules [10] [11]. Additionally, the TLR/NF-κB pathway provides the essential "priming signal" (Signal 1) for NLRP3 inflammasome activation by inducing the transcription of NLRP3 and pro-IL-1β [12] [10] [11]. Transcriptomic analyses of blood from LPS-induced peritonitis models have confirmed significant activation of TLR signaling pathways, along with simultaneous suppression of adaptive immunity pathways such as Th1/Th2 cell differentiation and T-cell receptor signaling [5].
NLRP3 Inflammasome Activation
The NLRP3 inflammasome is a multiprotein complex that serves as a critical platform for caspase-1 activation and subsequent maturation of IL-1β and IL-18 in response to microbial infection and cellular damage [12] [10]. The NLRP3 protein contains three domains: an N-terminal pyrin domain (PYD), a central NACHT domain that mediates oligomerization, and a C-terminal leucine-rich repeat (LRR) domain [12] [13]. In peritonitis, the NLRP3 inflammasome is activated through a meticulously regulated two-step process: priming (Signal 1) and activation (Signal 2) [12] [10] [11].
The priming step typically occurs through TLR/NF-κB signaling, which upregulates the transcription of NLRP3, pro-IL-1β, and pro-IL-18 [10] [11]. This step also involves post-translational modifications of NLRP3 that license it for subsequent activation [11] [13]. The activation step is triggered by diverse stimuli including extracellular ATP, particulate matter, bacterial toxins, and ionic fluxes, which induce NLRP3 oligomerization and recruitment of the adapter protein ASC and procaspase-1 [12] [10]. This complex formation leads to caspase-1 activation, which cleaves pro-IL-1β and pro-IL-18 into their mature, biologically active forms [12] [13]. Additionally, activated caspase-1 cleaves gasdermin D (GSDMD), whose N-terminal domain oligomerizes to form plasma membrane pores that facilitate cytokine release and trigger an inflammatory form of cell death termed pyroptosis [12] [10].
Table 1: Key Molecular Components of Major Inflammatory Pathways in Peritonitis
| Pathway | Molecular Components | Function in Peritonitis |
|---|---|---|
| Cytokine Signaling | TNF-α, IL-1β, IL-6, IL-8, IL-18 | Pro-inflammatory mediators that recruit immune cells, induce fever, pain, and acute phase response |
| TLR/NF-κB | TLR4, MyD88, IRAK, NF-κB | Pattern recognition and initiation of inflammatory gene transcription; provides "Signal 1" for inflammasome priming |
| NLRP3 Inflammasome | NLRP3, ASC, Caspase-1, NEK7 | Caspase-1 activation, IL-1β/IL-18 maturation, pyroptosis execution |
| Downstream Effectors | GSDMD, IL-1β, IL-18 | Pore formation in plasma membrane, pro-inflammatory cytokine activity, pyroptosis |
Recent research has identified the critical involvement of the NIMA-related kinase 7 (NEK7) in NLRP3 inflammasome assembly [12] [13]. NEK7 binds to NLRP3 following activation signals and facilitates the structural rearrangement that exposes PYD domains, allowing for NACHT domain oligomerization and subsequent ASC recruitment [12]. The assembled ASC filaments form a macromolecular structure termed the "ASC speck," which serves as the platform for caspase-1 activation [13]. This intricate assembly process ensures that the potent inflammatory mediators IL-1β and IL-18 are released only when appropriate signals are present, preventing excessive inflammation while effectively combating infection.
Experimental Models and Methodologies
Established Mouse Models of Peritonitis
Several well-characterized mouse models of peritonitis have been developed to study the inflammatory pathways involved in disease pathogenesis. The LPS-induced peritonitis model involves intraperitoneal administration of lipopolysaccharide, typically at a dose of 10 mg/kg, which triggers a robust but transient inflammatory response characterized by neutrophil infiltration and cytokine production [5]. This model is particularly useful for studying the early innate immune response and TLR4 signaling pathways. The cecal ligation and puncture (CLP) model more closely replicates human polymicrobial sepsis secondary to peritonitis [3] [4]. In this surgical model, the cecum is ligated below the ileocecal valve and punctured with a needle to allow leakage of fecal material into the peritoneal cavity, resulting in a progressive and polymicrobial infection [4].
More recently, a neonatal mouse model of meconium peritonitis has been developed using intraperitoneal administration of human meconium slurry (MS) [9]. This model closely reflects the pathology of human neonatal meconium peritonitis, a non-infectious chemical peritonitis that occurs following fetal intestinal perforation. The model has demonstrated dose-dependent mortality, with an LD40 established at 200 µL per pup, and is characterized by substantial hematological and hepatorenal abnormalities along with increased inflammatory gene expression [9]. Importantly, this model has revealed that the pathogenic agent in meconium is primarily digestive enzymes rather than bacterial components, as antibiotic treatment was ineffective while enzymatic inactivation improved survival rates [9].
Table 2: Comparison of Mouse Models of Peritonitis
| Model Type | Induction Method | Key Features | Applications |
|---|---|---|---|
| LPS-Induced | Intraperitoneal injection of LPS (10 mg/kg) | Rapid inflammation, neutrophil infiltration, cytokine release | Study of early innate immune responses, TLR4 signaling, neutrophil recruitment |
| Cecal Ligation and Puncture (CLP) | Surgical ligation and puncture of cecum | Polymicrobial infection, progressive sepsis, systemic inflammation | Modeling human sepsis, antibiotic efficacy studies, long-term outcomes |
| Meconium Slurry | Intraperitoneal administration of human meconium slurry | Chemical peritonitis, sterile inflammation, digestive enzyme-mediated damage | Neonatal meconium peritonitis pathophysiology, sterile inflammatory processes |
Protocol: LPS-Induced Peritonitis in Mice
Purpose: To establish a reproducible model of acute sterile inflammation for studying innate immune responses and early cytokine production.
Materials:
- Male C57BL/6 mice (6-8 weeks old)
- Lipopolysaccharide (LPS from E. coli, serotype O111:B4)
- Sterile phosphate-buffered saline (PBS)
- 1 mL syringes with 25-gauge needles
- Isoflurane anesthesia system
- Microtainer tubes for blood collection
Procedure:
- Prepare LPS solution by dissolving in sterile PBS to a concentration of 1 mg/mL.
- Anesthetize mice using isoflurane (3% induction, 1.5-2% maintenance in oxygen).
- Administer LPS (10 mg/kg) by intraperitoneal injection using a 25-gauge needle with a total volume of 100-200 µL.
- Return mice to cages with free access to food and water.
- Monitor mice every 2 hours for the first 8 hours, then every 6 hours for 48 hours for signs of distress (pilorection, hunched posture, decreased mobility).
- At desired time points (typically 6, 12, 24 hours), euthanize mice by CO2 asphyxiation followed by cervical dislocation.
- Collect blood via cardiac puncture for serum cytokine analysis.
- Perform peritoneal lavage with 3 mL of ice-cold PBS containing 3 mM EDTA for cellular infiltration analysis.
- Process lavage fluid by centrifugation (500 × g for 5 min at 4°C) and collect supernatant for cytokine measurement.
- Analyze immune cell populations in lavage fluid by flow cytometry or cytospin preparation.
Notes: This model produces robust neutrophil infiltration within 6 hours, peaking at 12-18 hours, with parallel increases in TNF-α, IL-6, and IL-1β levels [5]. The inflammatory response typically resolves within 48-72 hours.
Protocol: Cecal Ligation and Puncture (CLP) Model
Purpose: To establish a clinically relevant model of polymicrobial sepsis secondary to peritonitis for studying systemic inflammatory response and organ dysfunction.
Materials:
- Male C57BL/6 mice (8-12 weeks old, 20-25 g)
- Ketamine/xylazine anesthetic (100/10 mg/kg)
- Ophthalmic ointment
- Heating pad
- Sterile surgical instruments (forceps, scissors, needle holder)
- 5-0 silk suture
- 22-gauge needle
- Normal saline for fluid resuscitation
Procedure:
- Anesthetize mice with ketamine/xylazine (100/10 mg/kg) via intraperitoneal injection.
- Apply ophthalmic ointment to prevent corneal drying.
- Shave and disinfect the abdominal area with alternating betadine and 70% ethanol scrubs.
- Make a 1-1.5 cm midline abdominal incision.
- Exteriorize the cecum carefully using sterile forceps.
- Ligate the cecum below the ileocecal valve with 5-0 silk suture without causing bowel obstruction.
- Puncture the cecum once through-and-through with a 22-gauge needle.
- Gently extrude a small amount of feces (approximately 1 mm) through the puncture site.
- Return the cecum to the abdominal cavity.
- Close the abdominal wall in two layers with 5-0 suture.
- Administer 1 mL of warm normal saline subcutaneously for fluid resuscitation.
- Place mice on a heating pad until fully recovered from anesthesia.
- Administer buprenorphine (0.1 mg/kg) every 12 hours for postoperative analgesia.
Notes: The severity of sepsis can be modulated by varying the needle size (larger for more severe) or the percentage of cecum ligated [3] [4]. This model produces a progressive inflammatory response with significant cytokine production, immune cell infiltration, and organ dysfunction that mimics human sepsis.
Signaling Pathway Visualization
NLRP3 Inflammasome Activation Pathway: This diagram illustrates the two-signal mechanism of NLRP3 inflammasome activation. Signal 1 (priming) through TLR/NF-κB signaling upregulates NLRP3 and pro-IL-1β transcription. Signal 2 (activation) via diverse stimuli triggers NLRP3 oligomerization and NEK7 binding, leading to inflammasome assembly, caspase-1 activation, and subsequent IL-1β/IL-18 maturation and pyroptosis [12] [10] [11].
Research Reagent Solutions
Table 3: Essential Research Reagents for Peritonitis Studies
| Reagent Category | Specific Examples | Research Application | Key Findings Using Reagent |
|---|---|---|---|
| NLRP3 Inhibitors | MCC950, CY-09, Lenalidomide | Specific inhibition of NLRP3 inflammasome assembly | Lenalidomide (IKZF1 inhibitor) attenuates inflammatory responses and mitigates lung injury in CLP [3] |
| Cytokine Antibodies | Anti-IL-1β, Anti-TNF-α, Anti-IL-6 | Neutralization of specific cytokines | IL-1 antagonists reverse inflammation in cryopyrin-associated periodic syndromes [14] |
| TLR4 Signaling Inhibitors | TAK-242, LPS-RS, CLI-095 | Blockade of TLR4 signaling pathway | Inhibition prevents priming signal for NLRP3 inflammasome [11] |
| Caspase-1 Inhibitors | VX-765, Z-YVAD-FMK | Inhibition of caspase-1 activity | Blocks maturation of IL-1β and IL-18 [10] [13] |
| ROS Scavengers | Mito-TEMPO, N-acetylcysteine | Reduction of mitochondrial ROS | Attenuates NLRP3 activation signal [10] [11] |
| Ion Channel Modulators | Glybenclamide, Nigericin | Modulation of K+ efflux | Glybenclamide inhibits NLRP3 activation; Nigericin activates via K+ efflux [10] [13] |
| Transcriptional Profiling | RNA-seq kits, PCR arrays (e.g., Mouse Inflammatory Cytokines & Receptors) | Gene expression analysis | Identified 290 DEGs (242 up-regulated, 48 down-regulated) in LPS-induced peritonitis [5] |
Discussion and Research Implications
The intricate interplay between cytokine networks, TLR/NF-κB signaling, and NLRP3 inflammasome activation creates a complex inflammatory milieu that drives disease progression in peritonitis. Recent research has revealed novel regulatory mechanisms, including the role of IKZF1 in exacerbating macrophage inflammation through epigenetic modulation of mitochondrial function in CLP-induced peritonitis [3] [4]. IKZF1 expression is significantly upregulated in macrophages during peritonitis, where it directly represses SDHB expression by recruiting HDAC3 to deacetylate SDHB, leading to mitochondrial dysfunction and amplified inflammation [4]. This finding establishes an IKZF1/HDAC3-SDHB-succinate axis driving macrophage hyperactivation and identifies IKZF1 as a potential biomarker and therapeutic target [3].
From a translational perspective, targeting these inflammatory pathways holds significant promise for clinical intervention. The NLRP3 inflammasome, in particular, represents an attractive therapeutic target given its central role in processing and releasing mature IL-1β and IL-18 [12] [13]. Several small molecule inhibitors targeting different stages of NLRP3 inflammasome activation have shown efficacy in preclinical models of inflammatory diseases [13]. These include compounds that inhibit NEK7-NLRP3 interaction, disrupt ASC speck formation, or block caspase-1 activity [12] [13]. Additionally, the discovery that disassembly of the trans-Golgi network serves as a common cellular event triggering NLRP3 activation in response to diverse stimuli provides new opportunities for therapeutic intervention [12].
Future research directions should focus on elucidating the cell type-specific roles of NLRP3 in peritonitis pathogenesis. While the NLRP3 inflammasome is well-established in myeloid cells, its expression and functionality in non-immune cells, including mesothelial cells, remains controversial [14]. Unbiased transcriptome data sets often report the absence of NLRP3 inflammasome-related transcripts in non-myeloid cells, despite numerous experimental studies reporting NLRP3 expression and activity in these cells [14]. Resolving this discrepancy will require sophisticated cell type-specific knockout models and single-cell transcriptomic analyses of peritoneal tissues during inflammation. Additionally, further investigation is needed to understand the inflammasome-independent functions of NLRP3, such as its role in regulating TGF-β signaling and fibrosis, which may contribute to long-term complications of peritonitis including adhesion formation [14].
In conclusion, the inflammatory pathways in peritonitis represent a complex but orchestrated response to peritoneal injury and infection. A comprehensive understanding of these pathways, particularly the two-signal mechanism of NLRP3 inflammasome activation, provides valuable insights for developing targeted therapeutic strategies. The integration of biomarker profiling with mechanistic studies promises a new era of precision medicine in secondary peritonitis, enabling risk-adapted interventions and improved patient outcomes.
Peritonitis, the inflammation of the peritoneal membrane, initiates a complex cellular response crucial for host defense and tissue repair. The pathophysiology involves a tightly coordinated interaction between immune cells and stromal components, primarily driven by macrophages, neutrophils, and fibroblasts [15] [16]. In mouse models of peritonitis, understanding the roles and interactions of these cells is fundamental for evaluating inflammatory responses and screening potential therapeutic interventions. Macrophages act as central orchestrators of the immune response, neutrophils are the first responders that infiltrate the site of injury, and fibroblasts are the key effectors of tissue remodeling and fibrosis [15] [16] [17]. The dysregulation of these cellular processes can lead to persistent inflammation and peritoneal fibrosis, a serious complication that can cause ultrafiltration failure and necessitate the discontinuation of peritoneal dialysis (PD) [15]. This application note details the mechanisms, protocols, and analytical tools for studying these cellular players in the context of a mouse peritonitis model.
Detailed Cellular Roles and Mechanisms
Macrophages: Orchestrators of Inflammation and Fibrosis
Macrophages exhibit remarkable plasticity, allowing them to adopt different functional phenotypes—or polarization states—in response to microenvironmental signals. This plasticity is central to their role in peritonitis and its outcomes [15].
Activation and Polarization: Macrophages are broadly categorized into classically activated (M1) and alternatively activated (M2) phenotypes.
- M1 Macrophages are induced by Th1 cytokines like interferon-gamma (IFN-γ) and microbial products such as lipopolysaccharide (LPS). They express Toll-like receptors (TLR) 2 and 4, CD80, CD86, and inducible nitric oxide synthase (iNOS). They secrete pro-inflammatory cytokines including TNF-α, IL-6, IL-12, and IL-23, and produce nitric oxide (NO) to combat pathogens [15]. The LPS/TLR4 signaling pathway is a crucial trigger for M1 polarization, leading to the activation of NF-κB and IRF3 and driving the production of pro-inflammatory cytokines [15].
- M2 Macrophages are induced by IL-4, IL-10, IL-13, and TGF-β. They are identified by markers like the mannose receptor (CD206) and CD163 and are further subdivided into M2a, M2b, M2c, and M2d subtypes based on the inducing stimuli and specific functions. M2 macrophages are generally involved in tissue repair, angiogenesis, and immunoregulation through the production of IL-10, TGF-β, and various chemokines [15].
Role in Fibrosis: In prolonged peritoneal dialysis, macrophage infiltration and polarization are key contributors to pathology. They show a strong correlation with the epithelial-to-mesenchymal transition (EMT) of mesothelial cells and directly drive the fibrotic process [15]. M2 macrophages, particularly, are implicated in the production of pro-fibrotic factors that stimulate fibroblasts and lead to excessive extracellular matrix (ECM) deposition [15] [16].
Neutrophils: First Responders and Their Dynamics
Neutrophils are the most abundant leukocytes in human blood and are among the first immune cells to be recruited to the site of inflammation during peritonitis [17] [5].
- Infiltration and Recruitment: Neutrophil infiltration is a hallmark of peritonitis. This can be experimentally induced by intraperitoneal (i.p.) injection of inflammatory agents like CXCL1 or TNF-α [17]. Upon stimulation, neutrophils are rapidly recruited from the bone marrow into the circulation and then to the peritoneal cavity.
- Circulating Dynamics: Recent advancements using in vivo flow cytometry (IVFC) have allowed for the non-invasive, real-time monitoring of circulating neutrophils (LysM-EGFP+ cells) in mouse models. Studies show a significant increase in circulating neutrophils within 20 minutes of TNF-α challenge, accompanied by their concurrent recruitment to the peritoneum and emigration from the bone marrow [17].
- Adhesion and Migration: The adhesion molecule CD18 is critical for neutrophil recruitment from the vasculature into the inflamed peritoneum. Blockade of CD18 was shown to double the number of circulating neutrophils, indicating its essential role in neutrophil extravasation during peritonitis [17].
Fibroblasts and Myofibroblasts: Effectors of Tissue Remodeling
The generation and activity of myofibroblasts are central events in the induction of peritoneal fibrosis [16].
- Origin and Activation: Myofibroblasts in the peritoneum can originate from various sources, including resident fibroblasts and mesothelial cells that undergo EMT. These cells are instructed by a network of signals from both stromal resident cells and recirculating immune cells [16].
- ECM Production: Activated myofibroblasts are the primary cells responsible for the abnormal production and remodeling of extracellular matrix (ECM) proteins, such as collagen. This leads to the progressive thickening and scarring of the submesothelial compact zone, a characteristic feature of peritoneal fibrosis [16].
- Cross-talk with Immune Cells: The persistence of myofibroblasts and the progression of fibrosis are fueled by a cross-talk with macrophages. For instance, M2 macrophages secrete TGF-β, a potent pro-fibrotic cytokine that activates fibroblasts and promotes EMT, creating a feed-forward loop that perpetuates fibrosis [15] [16].
The following tables consolidate key quantitative findings from recent research on cellular mechanisms in mouse peritonitis models.
Table 1: Transcriptomic Profile in LPS-Induced Peritonitis Mouse Model
| Parameter | Measurement | Details/Methodology |
|---|---|---|
| Differentially Expressed Genes (DEGs) | 290 Total | 242 upregulated, 48 downregulated [5] |
| Activated Pathways | NOD-like receptor, Toll-like receptor, Apoptosis, Phagocytosis | Bioinformatics analysis of RNA-seq data [5] |
| Inhibited Pathways | Th1/Th2 cell differentiation, T cell receptor signaling | Bioinformatics analysis of RNA-seq data [5] |
| Identified Hub Proteins | 8 Proteins | LDLR, FNBP1L, SNX18, FAM20C, INPP5F, PACSIN1, ZAP70, SYNJ2; structural stability confirmed via 300 ns molecular dynamics [5] |
Table 2: Neutrophil Dynamics in TNF-α-Induced Mouse Peritonitis Model
| Parameter | Measurement | Details/Methodology |
|---|---|---|
| Circulating Neutrophil Increase | Significant increase | Peaked at ~20 min post i.p. TNF-α injection, monitored by In Vivo Flow Cytometry (IVFC) [17] |
| CD64 Expression on Neutrophils | Significant increase | Measured via flow cytometry and in vivo IVFC with fluorescent antibodies [17] |
| Effect of CD18 Blockade | Doubled circulating neutrophil count | Suggests critical role for CD18 in neutrophil recruitment from vasculature [17] |
Table 3: Macrophage Polarization States and Functions
| Phenotype | Inducing Stimuli | Key Markers | Primary Functions & Secreted Factors |
|---|---|---|---|
| M1 | IFN-γ, TNF-α, LPS | TLR2/4, CD80/86, iNOS, MHCII | Pro-inflammatory; host defense; secretes TNF-α, IL-6, IL-12, IL-23, NO [15] |
| M2a | IL-4, IL-13 | CD206, CD163, Arg1 | Tissue repair; secretion of CCL17, CCL18, CCL24 [15] |
| M2b | Immune complexes, TLR agonists | CD86, MHC-II | Immunoregulation; secretes IL-1β, IL-6, IL-10, TNF-α [15] |
| M2c | IL-10, TGF-β, glucocorticoids | CD206, CD163, MERTK | Anti-inflammatory, tissue remodeling; secretes IL-10, TGF-β [15] |
| M2d | IL-6, M-CSF, TLR agonists | CD80, CD86, MHC-II | Angiogenesis, immunosuppression; secretes IL-10, TGF-β, CXCL10 [15] |
Experimental Protocols
Protocol 1: Monitoring Circulating Myeloid Cell Dynamics via IVFC
This protocol details the use of in vivo flow cytometry (IVFC) to monitor LysM-EGFP-labeled circulating myeloid cells (primarily neutrophils) in a TNF-α-induced mouse peritonitis model [17].
- Mouse Model: LysM-EGFP transgenic mice (12-16 weeks old, both sexes).
- Key Reagents:
- Recombinant TNF-α (0.5 µg in 200 µL PBS for i.p. injection).
- Rhodamine B-labeled dextran (70,000 MW) or PE-conjugated anti-mouse CD64 mAb for in vivo labeling.
- Anesthetics: Ketamine (125 mg/kg) and Xylazine (12.5 mg/kg).
- Procedure:
- Anesthetize the mouse with an i.p. injection of ketamine/xylazine.
- Perform a retro-orbital injection of 20 µL of Rhodamine B-dextran (10 mg/mL) to outline the microvasculature. For CD64 measurement, inject 100 µL of PE-anti-CD64 mAb (50 µg/mL) instead.
- For CD18 blockade experiments, co-inject 100 µg of CD18 blocking mAb with the dye.
- Fix the mouse on the stage of a multi-photon microscope. Use a 20x water immersion objective to image the microvasculature in the mouse ear.
- Perform line scanning on vessels with a diameter of 20-45 µm at ~650-850 Hz for 120 seconds to record traversing LysM-EGFP+ cells. This serves as the baseline (0 min) measurement.
- Administer TNF-α (0.5 µg in 200 µL PBS) or vehicle control via i.p. injection.
- Repeat the IVFC measurement at 10, 20, 30, 60, 90, 120, 150, and 180 minutes post-injection.
- Data Analysis:
- Analyze line scanning images with FIJI-ImageJ or custom Python code to determine cell diameter, traversing time, and vessel diameter.
- Count the number of fluorescent cells in each recording.
- Confirm cell identity and phenotype using conventional flow cytometry on blood, peritoneal lavage, and bone marrow samples collected at endpoint.
Protocol 2: Induction of Meconium Peritonitis in Neonatal Mice
This protocol describes a non-surgical model of sterile chemical peritonitis using human meconium, which is distinct from infectious sepsis models [18].
- Mouse Model: 4-day-old mouse pups (immunologically equivalent to human preterm infants).
- Key Reagents:
- Human Meconium Slurry (MS): Prepared from sterile meconium from healthy term newborns, suspended in PBS (500 mg/mL), and stored at -80°C.
- Procedure:
- Thaw an aliquot of stock MS and vortex before injection.
- Administer MS intraperitoneally to 4-day-old pups. The LD40 (dose causing 40% lethality) is established at 200 µL per pup. Doses between 100-300 µL can be used for dose-dependent studies.
- Monitor pups daily for health and survival for up to 7 days. Record body weights of survivors daily.
- For validation, subject MS to heat inactivation (70°C or 100°C for 15 min) prior to injection to denature digestive enzymes, which are the primary pathogenic agents.
- Endpoint Analyses:
- Hematology and Biochemistry: At 24 hours post-induction, collect blood via decapitation for complete blood counts (CBC) and analysis of hepatorenal function.
- Immunomodulatory Gene Expression: At 6 hours post-induction, harvest liver tissue, extract RNA, and perform PCR arrays to profile the expression of 84 genes related to innate and adaptive immune responses.
Signaling Pathways and Experimental Workflows
Diagram 1: Key Signaling Pathways in Mouse Peritonitis. This diagram illustrates the primary signaling cascades driving macrophage polarization and neutrophil recruitment in response to inflammatory stimuli like LPS and TNF-α, and their subsequent role in tissue repair and fibrosis [15] [17].
Diagram 2: IVFC Workflow for Neutrophil Dynamics. This workflow outlines the key steps for non-invasive monitoring of circulating myeloid cells in a live mouse model of peritonitis using intravital flow cytometry (IVFC) [17].
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents for Mouse Peritonitis Studies
| Reagent | Function/Application | Example Usage in Protocol |
|---|---|---|
| Lipopolysaccharide (LPS) | Induces robust immune response by binding to TLR4; used to establish inflammatory peritonitis. | i.p. injection at 10 mg/kg to induce systemic inflammation and transcriptomic changes in blood [5]. |
| Recombinant TNF-α | Pro-inflammatory cytokine; used to induce neutrophil recruitment and sterile inflammation. | i.p. injection of 0.5 µg in 200 µL PBS to model TNF-α-driven peritonitis and neutrophil dynamics [17]. |
| LysM-EGFP Transgenic Mice | Genetically modified model where myeloid cells (neutrophils, macrophages) express EGFP for tracking. | Enables real-time IVFC monitoring and flow cytometric identification of circulating and infiltrating myeloid cells [17]. |
| CD18 Blocking Antibody | Inhibits neutrophil adhesion and extravasation; used to study recruitment mechanisms. | Retro-orbital injection of 100 µg to demonstrate the role of CD18 in neutrophil migration to the peritoneum [17]. |
| Human Meconium Slurry (MS) | Sterile, enzyme-rich slurry; induces chemical peritonitis distinct from live bacterial infection. | i.p. administration in neonatal mice (LD40 = 200 µL/pup) to model meconium peritonitis pathology [18]. |
| Fluorescent Conjugated Antibodies | Cell surface and intracellular staining for phenotyping via flow cytometry. | e.g., Anti-Ly6G (neutrophils), Anti-CD64 (activation), Anti-CD206 (M2 macrophages) [17]. |
| Rhodamine B-Dextran | High molecular weight fluorescent tracer; outlines blood vessels for IVFC. | Retro-orbital injection to visualize vasculature during line-scanning IVFC measurements [17]. |
Mouse peritonitis models are indispensable tools in biomedical research, serving as critical early in vivo screening systems for evaluating inflammatory responses and therapeutic efficacy of novel compounds [19] [20]. These models simulate the complex pathophysiology of peritoneal inflammation, enabling researchers to investigate innate immune mechanisms, leukocyte trafficking, and systemic inflammatory cascades. The historical significance of these models is profound, as the mouse peritonitis model was the first experimental animal system used in antibiotic research, demonstrating the efficacy of Prontosil and derivative sulphonamides against Streptococcus pyogenes in 1935 [19]. Since then, these models have evolved to encompass a diverse array of induction methods, each tailored to address specific research questions within immunology, infectious diseases, and drug development.
The utility of mouse peritonitis models stems from several practical advantages: they utilize small, cost-effective animals that are easy to maintain; they produce highly reproducible infections; and they offer straightforward experimental endpoints such as survival monitoring and bacterial quantification [20]. Furthermore, the ability to customize these models through various induction methods, mouse strains, and adjunctive agents makes them exceptionally versatile for studying different facets of inflammatory responses. This application note provides a comprehensive classification and methodological overview of the major mouse peritonitis models, detailing their applications, standardized protocols, and associated analytical approaches to guide researchers in selecting and implementing the most appropriate system for their investigative needs.
Model Classifications and Comparative Analysis
Mouse peritonitis models can be broadly categorized based on the method of inflammatory induction. The table below summarizes the primary model classifications, their induction agents, key characteristics, and major research applications.
Table 1: Classification of Major Mouse Peritonitis Models
| Model Type | Inducing Agent | Key Characteristics | Primary Applications | Example Strains |
|---|---|---|---|---|
| Chemical Induction [21] [22] [5] | Zymosan, Thioglycollate, LPS | - Non-infectious, sterile inflammation- Highly reproducible & tunable- Peaks within hours | - Study of leukocyte recruitment & migration- Analysis of soluble mediator networks- Screening anti-inflammatory drugs | BALB/c, C57BL/6 |
| Bacterial Induction (Non-Resistant) [23] [24] | Live bacteria (e.g., E. coli, MRSA) | - Mimics natural infection- Allows bacterial load enumeration- Can progress to sepsis | - Evaluation of antimicrobial drug efficacy- Host-pathogen interaction studies- Vaccine research | Kunming, BALB/c |
| Bacterial Induction (Drug-Resistant) [25] [26] | Carbapenem-resistant Gram-negative bacteria, MRSA | - Models difficult-to-treat infections- Often requires virulence enhancers (e.g., mucin)- High mortality rate | - Testing novel antibiotics against MDR pathogens- PK/PD studies for last-resort drugs | BALB/c, ICR |
| Lethal Bacteremia Model [19] [20] | High virulence bacteria (e.g., S. pneumoniae) | - Naturally virulent in mice- Death/survival as primary endpoint- Does not require immunocompromised hosts | - Early-stage in vivo antibiotic screening- Determination of protective/curative doses | Various |
Analysis of Model Selection Criteria
The choice of a specific peritonitis model is dictated by the research objectives. For dissecting fundamental mechanisms of innate immunity and leukocyte biology, chemical induction models are ideal due to their sterility and reproducibility [21] [22]. The zymosan-induced model, for instance, is characterized by a rapid inflammatory response that peaks within a few hours and can be resolved, allowing for the study of both inflammation initiation and resolution phases [21].
When the goal is to evaluate the in vivo efficacy of therapeutic agents, bacterial induction models are more appropriate. For standard pathogens, standard models suffice [23], but for the critical pre-clinical testing of new antimicrobials against multidrug-resistant (MDR) organisms, specialized models that incorporate clinical isolates of carbapenem-resistant Gram-negative bacilli or MRSA are essential [25] [24]. A key technical consideration for these models is the frequent use of virulence-enhancing agents. The addition of hog gastric mucin (typically at 3-4% concentration) is a well-established method to overcome the natural resistance of mice to many human pathogens, ensuring consistent and lethal infection necessary for robust therapeutic testing [25] [26] [24].
Detailed Experimental Protocols
Protocol 1: Zymosan-Induced Sterile Peritonitis
This protocol induces a sterile, acute inflammatory response, ideal for studying basic immunology and pharmacodynamics of anti-inflammatory compounds [21].
- Animals: Mice (e.g., C57BL/6), 6-8 weeks old.
- Reagents: Zymosan suspension in sterile saline (common doses: 1 mg or 10 mg per mouse) [21].
- Procedure:
- Preparation: Suspend zymosan in sterile, pyrogen-free saline. The concentration should be adjusted so the desired dose (e.g., 1 mg) is delivered in a volume of 200-500 µL.
- Induction: Anesthetize the mouse briefly using inhaled isoflurane. Using a 26-gauge needle, inject the zymosan suspension intraperitoneally (i.p.) in one of the lower abdominal quadrants to avoid internal organs.
- Monitoring: Monitor mice until fully recovered from anesthesia. The inflammatory response peaks within a few hours post-injection.
- Sample Collection: At the desired time point (e.g., 4-24h), euthanize the animal. Inject 5 mL of cold lavage buffer (e.g., HBSS containing 1-5% FBS or EDTA to prevent cell adherence) into the peritoneal cavity. Gently massage the abdomen and then aspirate the peritoneal wash fluid (PWF).
- Analysis: Centrifuge the PWF. The supernatant can be analyzed for cytokines (e.g., IL-1β, TNF-α, MIP-1a) by ELISA, and the cell pellet can be resuspended for leukocyte counting and differentiation by flow cytometry (e.g., identifying PMNs as CD115-Gr-1+ cells and macrophages as CD115+Gr-1- cells) [21].
Protocol 2: Bacterial Peritonitis with Hog Gastric Mucin
This protocol is designed for establishing a lethal infection with drug-resistant clinical isolates, crucial for antimicrobial efficacy testing [25] [26].
- Animals: 6-week-old female BALB/c or ICR mice [25].
- Reagents:
- Procedure:
- Bacterial Preparation: Grow the bacterial strain to logarithmic phase in broth. Centrifuge and adjust the bacterial pellet to a concentration of ~1x10⁸ CFU/mL in PBS using spectrophotometry, verifying the count by plating.
- Mucin Preparation: Dissolve hog gastric mucin in PBS to make a 6% (w/v) solution. Sterilize appropriately (e.g., autoclaving).
- Inoculum Preparation: Immediately before injection, mix equal volumes of the adjusted bacterial suspension and the 6% mucin solution. The final challenge dose will be ~10⁷ CFU in 0.2 mL containing 3% mucin [25].
- Infection: Anesthetize mice with isoflurane. Inject the 0.2 mL inoculum intraperitoneally.
- Therapeutic Intervention: Administer the test compound or vehicle control at a predefined time post-infection (e.g., 1 hour) via an appropriate route (intravenous, subcutaneous, etc.).
- Endpoint Analysis: Monitor survival for up to 24-48 hours, checking every 12 hours. For bacterial burden assessment, collect blood via cardiac puncture or peritoneal lavage fluid at set times, serially dilute, and plate on agar to enumerate CFUs [23].
The following diagram illustrates the workflow for establishing and analyzing a bacterial peritonitis model.
Protocol 3: LPS-Induced Peritonitis for Transcriptomic Studies
This model is used to study systemic gene expression changes in response to localized inflammation [5].
- Animals: Male C57BL/6 mice, 6-8 weeks old.
- Reagents: Lipopolysaccharide (LPS from E. coli).
- Procedure:
- Induction: Administer LPS (e.g., 10 mg/kg) via intraperitoneal injection. Control mice receive sterile PBS.
- Sample Collection: At the designated time point (e.g., 1-4 hours), anesthetize mice and collect blood via retro-orbital bleeding or cardiac puncture into tubes containing anticoagulant.
- Transcriptomic Analysis: Isolate total RNA from whole blood or peripheral blood mononuclear cells (PBMCs). Perform bulk RNA sequencing. Subsequent bioinformatics analysis can identify differentially expressed genes (DEGs) and enriched pathways (e.g., NOD-like receptor, Toll-like receptor signaling) [5].
The Scientist's Toolkit: Essential Research Reagents
Successful execution of peritonitis studies requires a standardized set of core reagents and materials. The following table lists critical components for model establishment and analysis.
Table 2: Essential Reagents and Materials for Mouse Peritonitis Models
| Category/Item | Specific Examples | Function & Application |
|---|---|---|
| Inflammatory Inducers | Zymosan (from yeast) [21], Thioglycollate [22], Ultrapure LPS [5] | Induces sterile inflammation for studying leukocyte migration and mediator release. |
| Virulence Enhancer | Hog Gastric Mucin (Type III) [25] [26] [24] | Impairs host clearance mechanisms, enabling lethal infection with clinical bacterial isolates. |
| Bacterial Strains | Carbapenem-resistant E. coli, K. pneumoniae [25], MRSA (e.g., NRS71) [24] | Clinical isolates used to model difficult-to-treat human infections for antibiotic testing. |
| Assay Kits | ELISA Kits (for TNF-α, IL-1β, IL-6, etc.) [21] | Quantifies cytokine and chemokine levels in peritoneal wash fluid or serum. |
| Flow Cytometry Antibodies | Anti-mouse Ly6G (neutrophils), CD115, Gr-1, CCR3, Siglec-F [21] [17] | Identifies and quantifies infiltrating leukocyte populations (e.g., PMNs, macrophages, eosinophils). |
| Lavage & Culture Media | Hank's Balanced Salt Solution (HBSS) [22], Phosphate-Buffered Saline (PBS) [25], Mueller-Hinton Broth [25] | Used for peritoneal lavage, bacterial culture, and as a vehicle/diluent for injections. |
Analytical Methods and Data Interpretation
A key strength of mouse peritonitis models is the breadth of analytical endpoints that can be measured to quantify the inflammatory response and therapeutic effects.
Cellular and Molecular Analysis
- Leukocyte Quantification: Peritoneal lavage fluid is the primary sample for analysis. Total and differential leukocyte counts are performed using automated hematology analyzers or, more precisely, by flow cytometry. Specific cell populations are identified using surface markers: PMNs as CD115-Gr-1+, macrophages as CD115+Gr-1-, and eosinophils as CCR3+Siglec-F+ [21]. Time-course studies show that total leukocyte infiltration peaks within hours of zymosan injection and declines thereafter [21].
- Cytokine and Chemokine Profiling: The supernatant from peritoneal wash fluid (PWF) or serum is analyzed using ELISA or multiplex immunoassays to measure the concentrations of key inflammatory mediators such as IL-1β, TNF-α, IFN-γ, and MIP-1α [21]. These molecules drive the pathophysiology of peritonitis and are critical biomarkers for assessing the anti-inflammatory activity of test compounds.
- Transcriptomic Analysis: Bulk RNA sequencing of blood or peritoneal cells from LPS-induced models can reveal global changes in gene expression. Studies have identified hundreds of differentially expressed genes (DEGs), with upregulated pathways including NOD-like and Toll-like receptor signaling, and suppressed pathways involving T-cell receptor signaling and Th1/Th2 differentiation [5]. Advanced techniques like in vivo flow cytometry (IVFC) can non-invasively monitor the dynamics of circulating immune cells, such as LysM-EGFP+ neutrophils, in real-time during TNFα-induced peritonitis [17].
Outcome-Based Analysis
- Bacterial Enumeration: In infection models, the efficacy of an antimicrobial agent is directly assessed by quantifying the bacterial load. Samples of blood and peritoneal fluid are collected, serially diluted, plated on agar, and incubated to count the number of colony-forming units (CFU) [23] [24]. A successful treatment will show a significant reduction in CFU/mL compared to untreated controls.
- Survival Studies: For lethal models, the survival rate over a defined period (e.g., 24-48 hours) is a primary, unambiguous endpoint. Data are often presented using Kaplan-Meier survival curves, and statistical comparisons (e.g., Log-rank test) determine the significance of a treatment's protective effect [25] [24]. The 50% effective dose (ED₅₀) of a drug can be calculated from such studies [19].
The signaling pathways activated in peritonitis are complex. The following diagram summarizes the key pathways and cellular responses identified through transcriptomic and molecular analyses.
Mouse models of peritonitis are indispensable tools for investigating the pathophysiology of inflammatory responses and evaluating potential therapeutic interventions. The choice of a specific model is crucial, as it must accurately reflect the research objectives, whether related to infectious peritonitis, sterile chemical inflammation, or the complex interplay between metabolism and immunity. This application note provides a structured comparison of established murine peritonitis models, detailed protocols for their implementation, and guidance for matching scientific questions to the appropriate experimental system.
Selecting the correct peritonitis model is the first critical step in designing a scientifically sound experiment. The table below summarizes the key characteristics of four commonly used models to aid in this selection process.
Table 1: Characteristics of Different Mouse Peritonitis Models
| Model Name | Primary Induction Method | Type of Inflammation | Key Research Applications | Key Inflammatory Readouts |
|---|---|---|---|---|
| Cecal Slurry (CS) Model [9] | Intraperitoneal injection of cecal content suspension | Polymicrobial Sepsis, Infectious | Sepsis pathophysiology, antibiotic efficacy testing, immune responses to live bacteria | Survival rates, bacterial load (CFU), plasma cytokines (IL-6, TNF-α), hematological parameters [9] |
| Meconium Slurry (MS) Model [9] | Intraperitoneal injection of human meconium | Sterile, Chemical Peritonitis | Neonatal meconium peritonitis, sterile inflammatory cascades, digestive enzyme-mediated pathology | Survival rates, histopathology of peritoneal organs, serum biochemistry (liver/kidney function), inflammatory gene expression (PCR array) [9] |
| Cecal Ligation and Puncture (CLP) [27] | Surgical ligation and puncture of the cecum | Polymicrobial Sepsis, Infectious | Gold-standard for sepsis and septic shock, drug efficacy, immune cell recruitment and function | Cytokine levels in lavage fluid (ELISA), lung injury (histology), immune cell phenotyping, organ failure assessment [27] |
| Hog Gastric Mucin Model [26] | Intraperitoneal co-injection of bacteria with mucin | Monomicrobial, Infectious | Pathogenesis studies of specific clinical isolates (e.g., carbapenem-resistant bacteria), virulence studies | Survival rates, bacterial load (CFU), efficacy of antimicrobial agents [26] |
Detailed Experimental Protocols
Protocol: Meconium-Induced Sterile Peritonitis Model
This protocol generates a neonatal mouse model that closely reflects the pathology of human meconium peritonitis, a life-threatening condition in the perinatal period [9].
A. Reagent Preparation
- Human Meconium Slurry (MS) Stock Solution:
- Collection: Aseptically collect fresh meconium from healthy term human newborns with parental consent.
- Preparation: Add 1.0 mL of phosphate-buffered saline (PBS) per 500 mg of meconium (500 mg/mL concentration).
- Homogenization: Stir the mixture vigorously and aspirate through a 23-gauge needle.
- Storage: Aliquot into cryovials and store at -80°C.
- Sterility Check: Before use, thaw an aliquot and plate 50 µL on brain/heart infusion (BHI) agar. Incubate at 37°C for 24 hours. Use only stocks with no bacterial growth [9].
B. Animal Model Induction
- Animals: Use 4-day-old mouse pups (e.g., FVB/NJcl strain), which are immunologically equivalent to human preterm infants.
- Injection: Administer the MS stock solution intraperitoneally at a defined dose (e.g., an LD40 of 200 µL per pup).
- Monitoring: Monitor pups daily for health and survival for up to 7 days. Record body weights of survivors daily beginning 24 hours post-injection [9].
C. Data Collection and Analysis
- Survival Analysis: Monitor and record survival rates for 7 days.
- Sample Collection: At desired endpoint (e.g., 24 hours post-induction), sacrifice pups and collect blood via decapitation.
- Hematology & Biochemistry: Perform complete blood counts (CBC) and analyze serum for hepatorenal function markers.
- Molecular Analysis: Extract RNA from tissues (e.g., liver) for PCR array analysis of immunomodulatory gene expression [9].
The following diagram illustrates the workflow for establishing and analyzing the meconium peritonitis model.
Protocol: Cecal Ligation and Puncture (CLP) Model
The CLP model is a widely accepted gold standard for studying polymicrobial sepsis and subsequent inflammatory responses [27].
A. Pre-Surgical Preparation
- Animals: Anesthetize mice (e.g., 8-12 week old) via isoflurane inhalation.
- Asepsis: Shave and disinfect the abdominal area.
B. Surgical Procedure
- Incision: Make a midline abdominal incision (approximately 1.5 cm).
- Exteriorization: Gently exteriorize the cecum.
- Ligation: Ligate the cecum below the ileocecal valve without causing intestinal obstruction.
- Puncture: Puncture the ligated cecum once with a 22-gauge needle.
- Replacement: Gently squeeze a small amount of feces through the puncture to ensure patency, then replace the cecum into the abdominal cavity.
- Closure: Close the abdominal wall in layers [27].
C. Post-Operative Care
- Resuscitation: Administer 0.3 mL of saline subcutaneously immediately after surgery.
- Monitoring: Return mice to their cages with free access to food and water; monitor closely.
D. Sample Collection and Analysis
- Peritoneal Macrophage Isolation:
- Elicit macrophages by injecting 3 mL of 3% thioglycollate broth intraperitoneally 3-4 days prior.
- Harvest cells by lavaging the peritoneal cavity with DMEM.
- Plate adherent cells for in vitro assays [27].
- Cytokine Measurement: Collect peritoneal lavage fluid and analyze cytokine levels (e.g., TNF-α, IL-6, IL-1β) by ELISA [27].
- Histopathology: Inflate and fix lungs with 4% paraformaldehyde for H&E staining to assess injury [27].
The Scientist's Toolkit: Key Research Reagent Solutions
The table below lists essential reagents used in peritonitis research, along with their specific functions and application contexts.
Table 2: Essential Reagents for Peritonitis Research
| Reagent | Function/Application | Example Usage in Protocols |
|---|---|---|
| Hog Gastric Mucin | Virulence-enhancing factor; inhibits bacterial clearance | Used at 3% concentration mixed with bacterial inoculum to establish monomicrobial infection with clinical isolates [26]. |
| Thioglycollate Broth | Inflammatory eliciting agent | Injected intraperitoneally (3%, w/v) to recruit macrophages for harvesting and subsequent in vitro studies [27]. |
| Lenalidomide | IKZF1 transcription factor inhibitor | Used in CLP models to investigate mechanisms of macrophage-mediated inflammation, e.g., administered to attenuate inflammatory response [27]. |
| Phosphate-Buffered Saline (PBS) | Isotonic solution for dilutions and lavage | Used as a diluent for meconium slurry preparation and for peritoneal lavage to collect immune cells [9] [27]. |
| Collagenase I | Enzyme for tissue digestion | Used to enzymatically digest the omentum to create single-cell suspensions for single-cell RNA sequencing analysis [28]. |
Signaling Pathways in Peritonitis
Understanding the molecular pathways driving inflammation is key to developing targeted therapies. Recent research highlights the role of the IKZF1/HDAC3-SDHB-succinate axis in macrophage hyperactivation during CLP-induced peritonitis [27].
The following diagram illustrates this key signaling pathway identified in macrophage hyperactivation during peritonitis.
Pathway Description: In macrophages during CLP-induced peritonitis, inflammatory stimuli (e.g., LPS) lead to upregulation of the transcription factor IKZF1. IKZF1 recruits histone deacetylase 3 (HDAC3) to the promoter of SDHB, a key subunit of mitochondrial complex II. This recruitment results in SDHB deacetylation and subsequent repression of its expression. The loss of SDHB disrupts the mitochondrial electron transport chain, causing succinate accumulation, elevated ROS, and reduced ATP. This metabolic dysfunction amplifies the pro-inflammatory response, leading to increased production of IL-1β, IL-6, and TNF-α, and ultimately exacerbating tissue injury, such as in the lungs [27].
Establishing Robust Protocols: From Infectious Agents to Non-Infectious Inducers
Mouse models of peritonitis are indispensable tools for studying the pathophysiology of sepsis and systemic inflammatory responses. Among these, Fecal-Induced Peritonitis (FIP) and Cecal Ligation and Puncture (CLP) represent two widely utilized polymicrobial sepsis models that closely mimic human intra-abdominal infections. These models facilitate the investigation of complex immune pathways, organ dysfunction, and potential therapeutic interventions in a controlled laboratory setting. The FIP model involves the direct intraperitoneal injection of a standardized fecal slurry, creating a reproducible polymicrobial challenge [29]. In contrast, the CLP model combines tissue ischemia and bacterial leakage through surgical ligation and puncture of the cecum, generating a more gradual onset of peritonitis [30] [31]. Both models trigger a systemic inflammatory response characterized by cytokine release, immune cell activation, and eventual organ failure, providing critical platforms for evaluating inflammatory mechanisms and treatment strategies. This protocol outlines standardized methodologies for both approaches, emphasizing practical implementation within the context of preclinical sepsis research.
Model Comparison and Selection
The choice between FIP and CLP depends on the specific research objectives, technical expertise, and desired disease progression characteristics. The table below provides a systematic comparison of these models to guide appropriate experimental selection.
Table 1: Comparative Analysis of FIP and CLP Murine Sepsis Models
| Feature | Fecal-Induced Peritonitis (FIP) | Cecal Ligation and Puncture (CLP) |
|---|---|---|
| Core Principle | Intraperitoneal injection of prepared fecal slurry [29] | Surgical ligation and puncture of the cecum [30] [31] |
| Inflammatory Drivers | Polymicrobial infection without significant tissue necrosis [29] | Polymicrobial infection combined with ischemic/necrotic tissue [30] |
| Key Advantages | High reproducibility; less operator-dependent; minimal surgical trauma; easily standardized for multi-laboratory studies [29] | Clinically relevant progression; includes an ischemic tissue component; established as a gold standard for polymicrobial sepsis [30] [31] |
| Technical Complexity | Moderate (requires slurry preparation) | High (requires survival surgery and aseptic technique) |
| Disease Onset | Rapid, acute | More gradual, subacute |
| Severity Control | Modulating fecal slurry dose (e.g., 0.5-2.5 mg/g) [29] [32] | Modulating ligation length (>1 cm for high severity) and needle gauge (e.g., 19G-27G) [30] [31] |
| Typical Mortality | Adjustable with dose (e.g., 60-89% with 0.75 mg/g) [29] [32] | Adjustable with technique (e.g., 55-100% with 19G needle and long ligation) [31] |
| Recommended Applications | High-throughput therapeutic screening, immunology studies, multi-center trials [29] | Studies of sepsis with ischemic component, long-term survival, and therapeutic timing [30] |
Critical parameters from published studies utilizing these models are consolidated below to inform experimental design and expectation of outcomes.
Table 2: Quantitative Experimental Data from Preclinical Studies
| Study Focus | Model & Parameters | Key Quantitative Findings | Citation |
|---|---|---|---|
| Model Development & Multi-lab Variation | FIP (Fecal Slurry: 0.75 mg/g) | • Mortality: 60% (Site 1) vs. 88% (Site 2)• Early Antibiotics (4h): 100% survival• Late Antibiotics (12h): Significant mortality | [29] |
| Aging and Sepsis Susceptibility | FIP (0.75 mg/g in young vs. aged mice) | • Mortality: 42% (Young) vs. 89% (Aged)• Aged mice exhibited increased inflammation and lung injury | [32] |
| Technical Severity Modulation in CLP | CLP (Ligation length and needle size) | • Ligation >1 cm: ~100% mortality in <3 days• Needle 19G (2 punctures): 55-60% survival• Needle 22G: 100% survival | [31] |
| Scoring and Prediction | FIP (90 mg/mL slurry concentration) | • MSS ≥ 3: 100% specificity for predicting death within 24h• Mortality: 75% at 24 hours | [33] |
Experimental Protocols
Fecal-Induced Peritonitis (FIP) Model
Fecal Slurry Preparation
- Source Material: Collect fresh cecal contents from donor animals (e.g., rats or mice) immediately after euthanasia [29] [33].
- Homogenization: Weigh the cecal contents and homogenize in phosphate buffer (e.g., 6 mL/g of content) [29]. Alternatively, normal saline can be used to achieve concentrations of 45-180 mg/mL [33].
- Filtration and Centrifugation: Filter the homogenate through a 70-100 μm cell strainer to remove large particulate matter [29] [33]. Centrifuge the filtered solution at 3000 × g for 25 minutes at 4°C [29].
- Aliquoting and Storage: Resuspend the pellet in a 5% dextrose solution with 10% glycerol to a final concentration of 100 mg/mL. Aliquot (e.g., 1 mL per tube) and store at -80°C [29].
Induction of Sepsis
- Animals: Use 8-13 week old C57BL/6 mice. Acclimatize for at least one week prior to experimentation [29] [32].
- Injection: Thaw an aliquot of slurry and warm to room temperature. Under light isoflurane anesthesia, administer the slurry via intraperitoneal (IP) injection into the lower abdominal quadrant using a 25-gauge needle [29]. The dose should be calculated based on body weight (e.g., 0.75 mg/g for a mid-range mortality model) [29] [32].
- Controls: Inject control mice with the vehicle solution (5% dextrose with 10% glycerol) only [29].
Post-Procedural Care
- Supportive Care: Provide fluid resuscitation with subcutaneous Ringer's lactate (e.g., 200 μL) [29]. Place heating blankets or pads beneath half the cage to allow thermoregulation [29] [32].
- Analgesia: Administer subcutaneous buprenorphine (e.g., 0.01 mg/kg) at 4 hours post-procedure and every 8-12 hours thereafter [29].
- Antibiotics: To mimic clinical practice, administer antibiotics (e.g., piperacillin-tazobactam or imipenem) subcutaneously or IP, typically starting at 12 hours post-FIP induction [29] [32].
Cecal Ligation and Puncture (CLP) Model
Surgical Procedure
- Anesthesia: Induce surgical anesthesia with inhaled isoflurane (3.5-4.5%) or an injectable cocktail like ketamine/xylazine (75/15 mg/kg, IP) [30] [31].
- Preparation: Shave and aseptically prepare the abdominal skin with alternating betadine and 70% alcohol scrubs [30] [31].
- Laparotomy: Perform a 1-2 cm midline incision through the skin and abdominal wall to expose the cecum [30] [31].
- Ligation: Gently exteriorize the cecum. Identify the ileocecal valve and ligate 50-75% of the cecum (approximately 1 cm from the cecal tip) using a 4-0 or 5-0 silk suture, ensuring not to cause intestinal obstruction [30] [31].
- Puncture: Puncture the ligated cecum once with a 19-27 gauge needle. Gently squeeze the cecum to extrude a small amount of fecal material (approximately 1 mm bead) through the puncture site [30] [31].
- Closure: Return the cecum to the peritoneal cavity. Close the abdominal muscle layer with absorbable sutures (e.g., Vicryl) and the skin with wound clips or non-absorbable sutures [30] [31].
- Sham Control: For sham-operated controls, perform the identical procedure including exteriorization of the cecum, but omit the ligation and puncture [30].
Post-Operative Care
- Resuscitation: Immediately after surgery, administer 1 mL of pre-warmed sterile saline subcutaneously [31].
- Analgesia: Provide post-operative analgesia with subcutaneous buprenorphine (0.05-0.2 mg/kg) every 8-12 hours for at least 24 hours [30] [31].
- Supportive Care: Place animals on a heating pad or under a heat lamp until fully recovered from anesthesia. Provide hydrogel and standard chow ad libitum on the cage floor [31].
The following workflow diagram summarizes the key decision points and procedures for both the FIP and CLP models.
Figure 1: Experimental workflow for FIP and CLP models, highlighting key procedural steps and post-operative care.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents and Materials for FIP and CLP Models
| Category | Item | Specification / Example | Critical Function |
|---|---|---|---|
| Animal Model | Mouse Strain | C57BL/6 (8-12 weeks old) [29] [33] | Standardized genetic background for reproducible immune responses. |
| Anesthesia & Analgesia | Isoflurane | 3.5-4.5% for induction, 1.5-2% for maintenance [30] | Provides stable and reversible surgical anesthesia. |
| Buprenorphine | 0.05-0.2 mg/kg, subcutaneously, q12h [30] [31] | Opioid analgesic for post-operative pain management. | |
| Surgical Materials (CLP) | Suture | 4-0 or 5-0 Silk for cecal ligation [30] [31] | Provides secure ligation of the cecum. |
| Needles | 19-27 gauge for cecal puncture [30] [31] | Controls severity of peritonitis; larger gauge increases lethality. | |
| Wound Clips | 7mm auto-clips [31] | For rapid and consistent skin closure. | |
| Supportive Care | Fluids | Sterile 0.9% Saline or Ringer's Lactate [29] [31] | Fluid resuscitation to counter hypovolemia. |
| Antibiotics | Piperacillin-Tazobactam or Imipenem [29] | Mimics clinical standard of care; timing affects outcomes. | |
| Assessment Tools | Murine Sepsis Score (MSS) | 7-parameter clinical score [33] | Standardized metric for monitoring sepsis severity and predicting outcomes. |
Assessment and Analytical Methods
Clinical Scoring: Murine Sepsis Score (MSS)
The Murine Sepsis Score is a validated clinical assessment tool for monitoring disease progression, with high specificity for predicting mortality [33]. The system evaluates seven parameters: spontaneous activity, response to touch, response to auditory stimulus, posture, respiration rate, respiration quality, and appearance (piloerection). Each parameter is scored from 0 (normal/healthy) to 4 (severely compromised), generating a cumulative score. An MSS ≥ 3 has 100% specificity for predicting death within 24 hours, providing a robust, ethically sound endpoint for intervention or euthanasia [33].
Sample Collection and Analysis
- Blood Collection: Terminal blood collection via cardiac puncture under anesthesia is standard. Plasma/serum can be analyzed for:
- Peritoneal Lavage: Collect by injecting and retrieving sterile PBS from the peritoneal cavity. Analyze for immune cell populations (flow cytometry), cytokine levels, and bacterial load [29] [4].
- Tissue Harvest: Harvest organs (e.g., liver, lungs, spleen, kidney) for:
- Histopathology: Fix in formalin for H&E staining to assess inflammation and damage [4] [33].
- Bacterial Load: Homogenize tissues and plate serial dilutions on agar to quantify Colony Forming Units (CFU) [29] [33].
- Myeloperoxidase (MPO) Assay: Quantifies neutrophil infiltration in tissues [31].
- Gene/Protein Expression: RNA/protein extraction for PCR, western blot, or other molecular analyses [4].
The FIP and CLP models are robust and complementary systems for investigating peritonitis and systemic inflammation. The FIP model offers superior standardization and is ideal for high-throughput studies of immune responses and therapeutic efficacy, while the CLP model provides high clinical relevance with its combination of infection and ischemia. Adherence to the detailed protocols for model induction, post-procedural care, and objective assessment using tools like the MSS is paramount for generating valid, reproducible, and ethically conducted preclinical data. Mastery of these models provides a powerful foundation for advancing our understanding of sepsis and evaluating novel anti-inflammatory strategies.
Within the broader investigation of inflammatory responses, mouse peritonitis models represent a cornerstone methodology for dissecting the complex cellular and molecular pathways of innate immunity. These models are indispensable for evaluating novel therapeutic agents and understanding the fundamental biology of inflammation. Among the various approaches, non-infectious models—specifically those induced by Lipopolysaccharide (LPS), Zymosan, and Mechanical Scraping—provide controlled, reproducible, and highly informative systems for research and drug development. This article details the application and protocols for these three key models, providing a structured resource for scientists to select and implement the most appropriate system for their investigative needs.
The choice of peritonitis model is critical and depends on the specific research questions, whether they pertain to acute neutrophil-driven inflammation, sterile fungal-mimetic responses, or injury-induced fibrosis. The following table provides a direct comparison of the three featured models to guide researchers in their selection.
Table 1: Comparative Overview of Non-Infectious Mouse Peritonitis Models
| Feature | LPS-Induced Model | Zymosan-Induced Model | Mechanical Scraping Model |
|---|---|---|---|
| Inducing Agent | Lipopolysaccharide (LPS), a component of Gram-negative bacterial outer membrane [34] [35] | Zymosan A, a yeast cell wall derivative [36] [37] [38] | Physical scraping of the parietal peritoneum [39] |
| Primary Inflammation Type | Innate immune activation via TLR4 signaling pathway [35] | Sterile, fungal-mimetic inflammation; complement activation [39] [40] | Sterile injury with robust wound-healing response [39] |
| Key Characteristics | Rapid, strong cytokine release (TNF-α, IL-6, IL-1β); high neutrophil influx [35] | Self-resolving acute inflammation; sequential recruitment of neutrophils and monocytes/macrophages [39] [37] | Direct tissue damage leading to fibrosis and neoangiogenesis; models chronic peritoneal injury [39] |
| Typical Time Course | Peak inflammation at 4-6 hours post-injection [34] [35] | Peak neutrophil influx at 4 hours; resolution phase studied over days [36] [39] | Neutrophil infiltration at 6-24h; fibrosis and angiogenesis evident from days 7-14 [39] |
| Ideal For | Studying cytokine storms, TLR4 signaling, acute innate immunity, and septic shock [35] | Investigating resolution of inflammation, leukocyte recruitment, macrophage function, and phagocytosis [37] [40] | Research into peritoneal fibrosis, ultrafiltration failure, and long-term structural remodeling [39] |
LPS-Induced Peritonitis Model
Model Applications and Rationale
The LPS-induced peritonitis model is a quintessential system for studying acute sterile inflammation driven by the Toll-like Receptor 4 (TLR4) pathway. LPS, a potent pathogen-associated molecular pattern (PAMP), reliably elicits a robust innate immune response characterized by the rapid production of pro-inflammatory cytokines and a significant influx of neutrophils into the peritoneal cavity [35]. This model is extensively used to screen anti-inflammatory compounds, investigate the pathogenesis of sepsis, and delineate the TLR4 signaling cascade and its downstream effects. The ability to induce a highly reproducible and synchronized inflammatory burst makes this model a staple in immunology and pharmacology research.
Detailed Experimental Protocol
Materials:
- Animals: C57BL/6 mice (8-12 weeks old).
- Reagent: LPS from Escherichia coli (e.g., Sigma-Aldrich).
- Vehicle: Sterile, pyrogen-free phosphate-buffered saline (PBS).
- Equipment: Syringes (1 mL), 25-30G needles, anesthetic equipment (if applicable), materials for peritoneal lavage.
Procedure:
- Preparation: Dissolve LPS in sterile PBS to a working concentration. A common dose for robust inflammation is 10 mg/kg body weight [35], though lower doses (e.g., 10 μg/kg) are also used for specific protocols [34].
- Induction: Restrain the mouse and administer the LPS solution via intraperitoneal (i.p.) injection. A typical injection volume is 0.5 mL [35]. A vehicle control group should receive an equal volume of PBS alone.
- Monitoring: Closely monitor mice for signs of inflammation, including piloerection, lethargy, and hunched posture, for a predetermined period (e.g., 4-6 hours).
- Sample Collection: At the experimental endpoint, euthanize the mouse humanely. Perform peritoneal lavage by injecting a known volume (e.g., 3-5 mL) of sterile ice-cold PBS into the peritoneal cavity. Gently massage the abdomen and then aspirate the lavage fluid.
- Analysis: The lavage fluid (peritoneal exudate) can be analyzed for:
- Cellular Infiltrate: Total and differential leukocyte counts (using a hemocytometer and Turk solution or flow cytometry) [34].
- Soluble Mediators: Levels of cytokines (TNF-α, IL-6, IL-1β, IFN-γ) and nitric oxide (NO) by ELISA and Griess assay, respectively [35].
- Peritoneal Tissue: The peritoneal wall can be excised for transcriptomic (RNA-seq) or histological analysis [35].
Signaling Pathway
The inflammatory response in this model is primarily mediated by the TLR4 pathway. The diagram below illustrates the core signaling cascade.
Figure 1: LPS-Induced TLR4 Signaling Pathway. LPS binding to TLR4 recruits the adaptor protein MyD88, leading to the activation of NF-κB and subsequent transcription of pro-inflammatory cytokines (TNF-α, IL-6, IL-1β). These cytokines are released into the peritoneum, driving the recruitment of neutrophils. The TLR4-specific inhibitor TAK-242 can block this signaling cascade [35].
Zymosan-Induced Peritonitis Model
Model Applications and Rationale
The zymosan-induced peritonitis model is a well-established system for studying sterile, fungal-mimetic inflammation and the physiological process of inflammatory resolution. Zymosan, derived from yeast cell walls, activates the complement system and engages various pattern recognition receptors on immune cells, including decin-1 and TLR2 [39] [38] [40]. This triggers a self-resolving inflammatory cascade characterized by a defined sequence of leukocyte recruitment: an initial wave of neutrophils is followed by monocytes and macrophages [37]. This model is particularly valuable for researching the mechanisms of leukocyte trafficking, macrophage phagocytosis, and the pro-resolving actions of novel therapeutic compounds [37] [40].
Detailed Experimental Protocol
Materials:
- Animals: C57BL/6 mice (8-12 weeks old).
- Reagent: Zymosan A from Saccharomyces cerevisiae (e.g., Sigma-Aldrich).
- Vehicle: Sterile PBS without Ca²⁺/Mg²⁺.
- Equipment: As in the LPS protocol.
Procedure:
- Preparation: Prepare a fresh suspension of zymosan in PBS. A standard dose is 1 mg in 0.5 mL of PBS per mouse [37] [41]. The suspension may require sonication or vortexing to ensure homogeneity.
- Induction: Administer the zymosan suspension via i.p. injection.
- Monitoring & Dosing Paradigms: The model allows for flexible dosing of test compounds. Therapeutic agents can be administered subcutaneously (s.c.), orally (p.o.), intravenously (i.v.), or i.p., starting 30 minutes prior to zymosan injection and continuing until necropsy [37].
- Sample Collection: Euthanize the mouse and perform peritoneal lavage as described in the LPS protocol. Time points for analysis are critical and can be chosen based on the research focus: 4-6 hours for peak neutrophil influx, or 12-24 hours for studying macrophage-dominated phases [36] [37].
- Analysis: Lavage fluid is analyzed for:
Key Pathway and Workflow
Zymosan triggers a complex inflammatory response, with the NF-κB pathway playing a central role in the production of key mediators.
Figure 2: Zymosan-Induced Inflammatory and Resolution Pathway. Zymosan engagement of PRRs leads to NF-κB activation and the production of cytokines and chemokines, which drive neutrophil recruitment. The inflammation naturally resolves through neutrophil apoptosis and subsequent clearance by macrophages. Compounds like Forsythoside A (FTA) can accelerate resolution by inhibiting NF-κB activation [36].
Mechanical Scraping Model
Model Applications and Rationale
The mechanical scraping model is a unique non-infectious system designed to mimic the peritoneal injury, fibrosis, and neoangiogenesis associated with long-term peritoneal dialysis (PD) and repeated episodes of peritonitis [39]. Unlike the transient inflammation seen with LPS or zymosan, this model induces a sustained wound-healing response that leads to permanent structural changes in the peritoneal membrane. It is therefore an indispensable tool for investigating the pathogenesis of peritoneal fibrosis, encapsulating peritoneal sclerosis (EPS), and for evaluating therapeutic interventions aimed at preventing or reversing maladaptive tissue remodeling [39].
Detailed Experimental Protocol
Materials:
- Animals: Rats or mice (e.g., C57BL/6).
- Equipment: Surgical tools (scissors, forceps), anesthetic (e.g., isoflurane), suture clips, and a sterile scraping instrument (e.g., the edge of a 15-mL centrifuge tube cap for rats, or an injection needle cap for mice) [39].
Procedure:
- Anesthesia and Preparation: Induce deep surgical anesthesia in the mouse. Shave and disinfect the abdominal skin.
- Laparotomy: Perform a midline laparotomy (approximately 1.5-2 cm) to expose the peritoneal cavity.
- Scraping Injury: Gently scrape the right parietal peritoneum for a defined duration (e.g., 90 seconds in mice) using the sterile scraping instrument. Take care to apply consistent pressure to standardize the injury [39].
- Closure: Carefully return the intestines to the abdominal cavity and close the abdominal wall and skin with suture clips.
- Post-operative Care: Provide analgesic care and monitor animals until fully recovered.
- Time Course and Analysis: Euthanize animals at various time points to capture the dynamic pathological changes:
- 6-24 hours: Analysis of acute neutrophil infiltration and fibrin exudation.
- Day 3: Peak of mononuclear cell infiltration; loss of mesothelial layer.
- Days 7-14: Analysis of established fibrosis, α-SMA-positive fibroblast accumulation, and neoangiogenesis [39].
- Tissue Collection: The scraped peritoneal tissue is excised for histology (e.g., H&E, Masson's trichrome for collagen, immunohistochemistry for α-SMA, CD31) and molecular analysis (e.g., mRNA expression of TGF-β, PAI-1, MCP-1) [39].
Pathological Progression Workflow
The scraping model follows a defined sequence of histological events, from acute injury to chronic fibrosis.
Figure 3: Time Course of Pathological Changes in the Scraping Model. The model progresses from acute neutrophil infiltration to a macrophage-dominated phase, culminating in submesothelial fibrosis and the formation of new blood vessels, closely mimicking the chronic changes seen in long-term PD patients [39].
The Scientist's Toolkit: Essential Research Reagents
Successful execution of peritonitis models relies on key reagents. The following table lists critical materials and their applications in the featured protocols.
Table 2: Key Research Reagents for Peritonitis Models
| Reagent | Function/Application | Example Usage in Protocols |
|---|---|---|
| LPS (E. coli) | TLR4 agonist; induces potent acute inflammation and cytokine storm [34] [35] | i.p. injection at 10 mg/kg to model septic shock [35] |
| Zymosan A | Yeast wall particle; induces sterile, self-resolving inflammation and leukocyte recruitment [36] [37] | i.p. injection of 1 mg/mouse to study neutrophil and macrophage dynamics [37] [41] |
| TAK-242 (Resatorvid) | Selective TLR4 signaling inhibitor; tool for pathway validation [35] | Pre- or co-treatment to block LPS-induced cytokine production [35] |
| Forsythoside A (FTA) | Natural product with anti-inflammatory activity; inhibits NF-κB pathway [36] | Treatment (e.g., 40 mg/kg) to accelerate resolution in zymosan-induced peritonitis [36] |
| Recombinant AIM/CD5L | Enhances clearance of necrotic debris; promotes resolution [40] | Administration to ameliorate persistent inflammation and necrosis in zymosan-treated mice [40] |
| Spironolactone | Mineralocorticoid receptor (MR) blocker; attenuates fibrosis [39] | Oral administration to suppress fibrosis and neoangiogenesis in the scraping model [39] |
Feline Infectious Peritonitis (FIP) is a systemic inflammatory syndrome caused by a mutated feline coronavirus (FCoV) [42] [43]. Until recently, FIP was considered fatal; however, the discovery of effective antiviral compounds like GS-441524 and molnupiravir has transformed it into a treatable condition, with recovery rates now exceeding 85-90% in cats [42]. Research into FIP and the efficacy of these antivirals relies on robust animal models that accurately replicate the disease's inflammatory pathology. This protocol provides a detailed framework for establishing a mouse model of peritonitis, a system that provides critical insights into the inflammatory responses and host-pathogen interactions relevant to FIP research [27] [44]. The Cecal Ligation and Puncture (CLP) model described herein is a gold standard for inducing polymicrobial sepsis and peritonitis, allowing for the evaluation of novel therapeutic agents and the underlying mechanisms of inflammatory disease [27].
Materials and Reagents
Research Reagent Solutions
The following reagents are essential for the successful execution of the peritonitis model and subsequent analyses.
Table 1: Key Research Reagent Solutions
| Reagent/Solution | Function/Explanation in the Protocol |
|---|---|
| Lipopolysaccharide (LPS) | A bacterial endotoxin used to induce a robust and standardized inflammatory response; administered intraperitoneally to simulate bacterial infection [45]. |
| Escherichia coli (tdTomato strain) | Fluorescently tagged bacteria used to establish a bacterial peritonitis model; enables quantitative tracking of bacterial load and phagocytic activity via fluorescence [44]. |
| Retinoic Acid (RA) | A vitamin A metabolite used to modulate macrophage function and population dynamics within the peritoneal cavity; often administered via loaded nanoparticles (e.g., ZIF-8) to prolong effect [44]. |
| Lenalidomide (Len) | A compound identified as an IKZF1 inhibitor; used in mechanistic studies to attenuate inflammatory responses by targeting specific transcription factors in macrophages [27]. |
| Enzyme-Linked Immunosorbent Assay (ELISA) Kits | Used for the quantitative measurement of key pro-inflammatory cytokines (e.g., TNF-α, IL-6, IL-1β) in plasma, serum, or peritoneal lavage fluid to assess the inflammatory status [27]. |
| Flow Cytometry Antibodies | Fluorescently conjugated antibodies against cell surface markers (e.g., CD11b, F4/80, MHC-II) for identifying and sorting immune cell populations, such as large and small peritoneal macrophages [44]. |
| Thioglycollate Broth | An eliciting agent injected intraperitoneally to recruit macrophages into the peritoneal cavity for subsequent isolation and ex vivo studies [27]. |
Experimental Methods and Workflows
Animal Models of Peritonitis
Two primary methods are utilized for inducing peritonitis in mice, each with distinct applications.
Cecal Ligation and Puncture (CLP) Model
The CLP procedure is the most clinically relevant model for polymicrobial sepsis and secondary peritonitis [27].
- Anesthesia: Induce anesthesia in the mouse using isoflurane inhalation.
- Midline Incision: Make a small midline abdominal incision to exteriorize the cecum.
- Ligation: Ligate the cecum below the ileocecal valve without causing intestinal obstruction.
- Puncture: Puncture the ligated cecum once with a 22-gauge needle to extrude a small amount of fecal content.
- Closure: Return the cecum to the abdominal cavity and suture the muscle and skin layers.
- Resuscitation: Administer 0.3 mL of sterile saline subcutaneously for fluid resuscitation immediately post-surgery [27].
- Sham Control: For sham-operated controls, perform the identical procedure, including exteriorizing the cecum, but omit the ligation and puncture.
Bacterial Challenge Model
This model uses a defined bacterial load to study early immune responses.
- Bacterial Preparation: Culture E. coli ER2272 expressing tdTomato fluorescence marker overnight. Resuspend in PBS to a concentration of 1 × 10^7 CFU in a 0.2 mL volume [44].
- Administration: Inject the bacterial suspension intraperitoneally.
- Sample Collection: Collect samples (e.g., peritoneal cells, lavage fluid) at predetermined time points (e.g., 30 min, 60 min, 4 h) post-injection to analyze bacterial clearance and immune cell recruitment [44].
Peritoneal Macrophage Isolation and Culture
This protocol is critical for obtaining primary cells for ex vivo experiments.
- Elicitation: Intraperitoneally inject 3 mL of 3% (w/v) thioglycollate broth to recruit macrophages [27].
- Harvesting: After 3 days, lavage the peritoneal cavity with 3-5 mL of cold DMEM or RPMI 1640 medium. Gently massage the abdomen and collect the peritoneal exudate using a sterile pipette.
- Centrifugation: Centrifuge the collected cells at 1000 rpm for 5 minutes to pellet.
- Plating and Adherence: Resuspend the cell pellet and seed 1×10^6 cells into culture plates. Incubate for 2 hours to allow macrophage adherence.
- Washing: Wash the plates three times with DPBS to remove non-adherent cells. The remaining adherent cells are highly enriched for peritoneal macrophages and can be cultured for further experiments [27].
Drug Administration and Dosing
The following dosing guidelines are derived from effective protocols used in feline FIP treatment and can be adapted for preclinical efficacy studies in mice. Dosing should be adjusted based on the mouse's weight and the specific research compound.
Table 2: Antiviral Dosing Protocol for FIP Research
| Condition / Form | Antiviral Agent | Dosage Regimen & Administration | Treatment Duration |
|---|---|---|---|
| Standard (Non-Ocular/Neurological) | GS-441524 (Oral) | 15 mg/kg per day [46] | Minimum 84 days [43] [46] |
| GS-441524 (Subcutaneous) | 6-7.5 mg/kg per day [46] | Minimum 84 days [43] [46] | |
| Molnupiravir (Oral) | 10-15 mg/kg, twice daily (BID) [46] | Minimum 84 days [46] | |
| Ocular FIP | GS-441524 (Oral) | 15-20 mg/kg per day [46] | Minimum 84 days [46] |
| GS-441524 (Subcutaneous) | 8-10 mg/kg per day (minimum) [46] | Minimum 84 days [46] | |
| Molnupiravir (Oral) | 15 mg/kg, twice daily (BID) [46] | Minimum 84 days [46] | |
| Neurological FIP | GS-441524 (Oral) | Minimum of 10 mg/kg, twice daily (BID) [46] | Minimum 84 days [46] |
| GS-441524 (Subcutaneous) | 10 mg/kg per day (minimum) [46] | Minimum 84 days [46] | |
| Molnupiravir (Oral) | 15-20 mg/kg, twice daily (BID) [46] | Minimum 84 days [46] | |
| Rescue Therapy | Paxlovid (Nirmatrelvir + Ritonavir) | 75 mg nirmatrelvir + 25 mg ritonavir, combined with GS-441524 or molnupiravir [46] | As required for combo therapy |
Sample Collection and Analysis
- Peritoneal Lavage: Flush the peritoneal cavity with ice-cold saline post-euthanasia to collect immune cells and fluid for cytokine analysis [27] [44].
- Histopathology: Inflate and fix tissues (e.g., lung) with 4% paraformaldehyde. Process, embed in paraffin, section, and stain with Hematoxylin and Eosin (H&E) or Masson's Trichrome to assess inflammation and tissue damage [27].
- Cytokine Measurement: Quantify cytokine levels (TNF-α, IL-6, IL-1β, IL-10) in lavage fluid or serum using commercial ELISA kits according to the manufacturer's protocols [45] [27].
- Western Blot: Analyze protein expression (e.g., IKZF1, SDHB) from cell lysates using SDS-PAGE and specific primary antibodies [27].
- RNA Extraction and qPCR: Isolate RNA from cells or tissues and perform quantitative PCR to analyze gene expression of inflammatory markers [27] [44].
Signaling Pathways and Inflammatory Mechanisms
Understanding the molecular pathways activated during peritonitis is crucial for target identification. Recent research highlights the role of the IKZF1/HDAC3-SDHB-succinate axis in driving macrophage hyperactivation [27].
Figure 1: IKZF1-mediated inflammatory pathway in macrophages. Lipopolysaccharide (LPS) stimulation upregulates the transcription factor IKZF1, which recruits HDAC3 to deacetylate and repress SDHB, a key component of the mitochondrial complex II. This repression leads to mitochondrial dysfunction, characterized by succinate accumulation and reactive oxygen species (ROS) production, ultimately amplifying the pro-inflammatory response [27].
Data Analysis and Modeling
Key Biomarkers of Inflammation
Monitoring specific biomarkers is essential for quantifying the inflammatory response and evaluating therapeutic efficacy.
Table 3: Key Inflammatory Biomarkers in Peritonitis
| Biomarker Category | Specific Marker | Relevance in Peritonitis & Notes |
|---|---|---|
| Pro-inflammatory Cytokines | IL-6 | Key driver of acute phase response; correlates with sepsis severity and prognosis [45] [8]. |
| TNF-α | Early pro-inflammatory mediator; initiates cytokine cascade [45] [8]. | |
| IL-1β | Pyrogenic cytokine; contributes to fever and systemic inflammation [45] [8]. | |
| Anti-inflammatory Cytokine | IL-10 | Provides negative feedback; inhibits pro-inflammatory cytokine production [45]. |
| Clinical Biomarkers | Procalcitonin (PCT) | Highly specific biomarker for bacterial infections; useful for guiding antibiotic therapy [8]. |
| C-Reactive Protein (CRP) | Classic acute phase protein; rises rapidly in response to inflammation [8]. | |
| Cellular Biomarkers | Neutrophil-to-Lymphocyte Ratio (NLR) | Accessible systemic inflammation marker; elevated in sepsis [8]. |
| Mitochondrial Metabolite | Succinate | Accumulates due to mitochondrial dysfunction; acts as a pro-inflammatory signal in macrophages [27]. |
Mathematical Modeling of Inflammation
Computational models provide a systems-level understanding of the inflammatory response. A multiscale Ordinary Differential Equation (ODE) model can simulate the dynamics from cellular activation to systemic vital signs [45]. Such a model typically includes:
- Cellular Activation: LPS activates resting immune cells (e.g., macrophages).
- Cytokine Cascade: Activated cells express mRNA and release cytokines (TNF, IL-6, IL-1β, IL-10).
- Regulatory Feedback: IL-10 inhibits pro-inflammatory cytokine production.
- Systemic Effects: Cytokines like IL-6 and IL-1β induce fever, which increases heart rate. Tissue damage from inflammation can lead to decreased blood pressure [45].
This framework allows for the simulation of different challenge scenarios, such as acute LPS bolus or prolonged infusion, providing insights into the temporal dynamics of sepsis.
Figure 2: Workflow of inflammatory response modeling. An inflammatory stimulus triggers a cascade from cellular activation to the release of pro-inflammatory cytokines, resulting in clinical signs and potential tissue damage. Simultaneously, anti-inflammatory pathways are activated, providing crucial negative feedback to modulate the response [45].
Sepsis and peritonitis research relies heavily on animal models that accurately mimic the human clinical condition. The cecal ligation and puncture (CLP) model has long been considered the gold standard for modeling polymicrobial sepsis but suffers from significant variability due to inconsistent surgical technique and microbial composition [47] [4]. This variability compromises experimental reproducibility and comparability across different laboratories. Recent advancements have introduced the enriched cecal slurry (CS) model as a superior alternative that offers unprecedented standardization capabilities while maintaining the pathophysiological relevance of polymicrobial sepsis [47] [48].
The enriched CS technique addresses a critical need in inflammatory response research by providing a defined, consistent microbial challenge that can be quantitatively administered across experimental groups. This protocol details the methodology for creating, standardizing, and implementing enriched cecal slurry bacterial cultures for inducing peritonitis in mouse models, specifically designed for researchers investigating inflammatory pathways, immune responses, and therapeutic interventions.
Principle and Advantages
The enriched cecal slurry model operates on the principle of intraperitoneal administration of a standardized polymicrobial inoculum derived from murine cecal contents. Unlike traditional CS methods that use fresh, uncharacterized cecal material for each experiment, the enriched approach involves bacterial culture expansion in liquid media, followed by preservation in glycerol stocks at -80°C [47]. This process provides several significant advantages:
- Standardization: Bacterial cultures are expanded and quantified, ensuring consistent microbial composition and concentration across all experiments [47]
- Reproducibility: Frozen glycerol stocks allow different laboratories to use identical microbial preparations, enabling direct comparison of results [47] [48]
- Ethical Reduction: Avoids unnecessary euthanasia of donor animals for each experiment by utilizing preserved stocks [47]
- Flexibility: Enables generation of defined Gram-negative and Gram-positive specific cultures using selective antibiotics [47]
- Quantitative Dosing: Permits precise control over the microbial load administered to each animal [47]
Materials and Reagents
Research Reagent Solutions
Table 1: Essential Materials for Enriched Cecal Slurry Preparation
| Item | Function/Application |
|---|---|
| Cecal Slurry Donor Mice | Source of polymicrobial inoculum [47] |
| Glycerol Stocks | Long-term preservation of bacterial cultures at -80°C [47] |
| LB Media | Bacterial culture expansion and enrichment [47] |
| Aztreonam | Selective enrichment for Gram-negative bacteria [47] |
| Vancomycin | Selective enrichment for Gram-positive bacteria [47] |
| Phosphate Buffered Saline (PBS) | Diluent and injection vehicle [47] |
| Anaerobic Culture System | Mimics physiological gut environment during culture |
Protocol
Preparation of Enriched Cecal Slurry Stock
- Cecal Content Collection: Euthanize donor mice (Swiss albino or C57BL/6, 4-5 months old) and aseptically collect cecal contents into pre-weighed sterile tubes [47]
- Initial Suspension: Homogenize cecal contents in PBS (e.g., 1:5 w/v ratio) under anaerobic conditions
- Culture Enrichment: Inoculate LB media with the cecal suspension and culture for 12-24 hours at 37°C with shaking (anaerobic conditions preferred) [47]
- Glycerol Stock Preparation: Mix the enriched culture with sterile glycerol to a final concentration of 15-20%, then aliquot and store at -80°C [47]
- Quality Control: Determine colony-forming units (CFU) per milliliter for each stock batch using standard plating techniques
Defined Culture Preparation
- Selective Enrichment: Supplement LB media with either:
- Inoculation and Culture: Inoculate selective media with base cecal slurry and culture as described in section 4.1
- Verification: Confirm microbial selection through Gram staining and culture-based methods
Sepsis/Peritonitis Induction
- Animal Preparation: Use age and sex-matched mice (e.g., 4-5 month-old Swiss albino). Acclimate for at least 7 days with free access to food and water [47]
- Inoculum Preparation: Thaw glycerol stock and dilute to desired concentration in sterile PBS. Keep on ice until administration
- Dosing Administration: Inject the bacterial suspension intraperitoneally using appropriate needle gauge (e.g., 25-27G) [47]. The following dosing regimen has been validated:
Table 2: Bacterial Concentration-Dependent Survival Outcomes
| Group | Bacterial Concentration (CFU/mL) | Survival Rate (at 48 hours) | Clinical Severity |
|---|---|---|---|
| A | 2 × 10⁹ | Lowest | Most severe |
| B | 1 × 10⁹ | Low | Severe |
| C | 0.5 × 10⁹ | Moderate | Moderate |
| D | 0.1 × 10⁹ | High | Mild |
| E (Control) | Saline only | 100% | None [47] |
- Post-Procedure Care: Administer subcutaneous saline (0.3 mL) for fluid resuscitation and monitor closely according to ethical guidelines [47]
Validation and Assessment
Survival Monitoring
- Monitor survival every 6-8 hours for at least 48 hours post-injection [47]
- Record time to mortality and calculate survival percentages for each experimental group
Histopathological Analysis
- Tissue Collection: Euthanize mice at desired endpoint (e.g., 10 hours post-injection for early inflammatory response) and collect tissues (liver, kidney, lung) [47]
- H&E Staining: Process tissues for hematoxylin and eosin staining using standard protocols [47] [4]
- Assessment: Evaluate sections for immune cell infiltration, necrosis, and tissue damage [47]
Serum Marker Analysis
- Collect blood samples via cardiac puncture at time of euthanasia
- Analyze serum for inflammatory markers (e.g., TNF-α, IL-6, IL-1β) and organ damage markers (e.g., ALT, AST, creatinine) [4]
Peritoneal Macrophage Isolation and Analysis
- Lavage: Inject 3-5 mL of cold PBS intraperitoneally, massage abdomen, and collect peritoneal fluid [4] [49]
- Macrophage Enrichment: Plate cells and allow adherence (2 hours at 37°C), then remove non-adherent cells [4]
- Functional Assays: Analyze macrophage activation markers, cytokine production, and metabolic responses [4]
Expected Results
The enriched cecal slurry model produces dose-dependent sepsis severity with high reproducibility [47]. Animals receiving higher bacterial loads (≥1 × 10⁹ CFU/mL) typically exhibit:
- Significant reduction in survival rates [47]
- Increased immune cell infiltration in vital organs [47]
- Elevated serum markers of inflammation and organ dysfunction [47]
- Histopathological evidence of liver and kidney damage [47]
The defined Gram-negative and Gram-positive cultures enable investigation of pathogen-specific immune responses, while the mixed polymicrobial inoculum more closely mimics clinical sepsis.
Troubleshooting
- Unexpected Survival: Verify CFU counts and bacterial viability from glycerol stocks
- Inconsistent Response: Ensure consistent injection technique and confirm proper storage of bacterial stocks
- Low Inflammatory Response: Confirm culture viability and consider optimizing culture conditions
- Excessive Mortality: Titrate bacterial concentration to achieve desired mortality rate for specific research objectives
Applications in Inflammatory Response Research
This standardized model is particularly valuable for:
- Evaluating novel anti-inflammatory and antimicrobial therapies [47]
- Investigating specific inflammatory pathways, such as the IKZF1/HDAC3-SDHB-succinate axis in macrophage hyperactivation [4]
- Studying time-dependent inflammatory and immunosuppressive phases of sepsis
- Generating reproducible data for pre-clinical drug development
Experimental Workflow for Enriched Cecal Slurry Model
Inflammatory Signaling Pathway in Peritonitis
The mouse peritonitis model is a well-established and versatile in vivo system for evaluating inflammatory responses and assessing the efficacy of therapeutic interventions [50] [51]. By simulating a localized intra-abdominal infection, this model provides critical insights into the complex dynamics of innate immunity, including the sequential influx of immune cells and the production of inflammatory mediators [4] [51]. Its reliability and reproducibility make it an indispensable tool for preclinical testing of novel compounds, from conventional antibiotics to cutting-edge biologic agents and targeted degraders. This protocol details the application of the mouse peritonitis model for evaluating three distinct therapeutic classes, providing a standardized framework for researchers in drug development.
Model Selection and Experimental Setup
Choosing an Induction Method
The choice of peritonitis induction method depends on the research focus. The two primary models offer distinct advantages:
- Cecal Ligation and Puncture (CLP): This surgically-induced polymicrobial model closely mimics human fecal peritonitis and sepsis, triggering a robust local and systemic inflammatory response [50] [4]. It is ideal for studying sepsis pathophysiology and testing interventions aimed at modulating systemic inflammation. The procedure involves exteriorizing the cecum, ligating it below the ileocecal valve, and puncturing it with a needle to allow fecal content leakage into the peritoneal cavity [4].
- Thioglycollate Broth Injection: This sterile, chemical-induced model elic a sterile inflammatory response characterized by a predictable and synchronized influx of immune cells, primarily neutrophils and macrophages [51]. It is particularly suitable for studying innate immune cell recruitment, macrophage polarization, and the resolution of inflammation without the confounding variables of live bacterial replication.
Key Readouts and Parameters
Quantifiable endpoints for therapeutic evaluation include:
- Cell Counts and Phenotyping: Analysis of peritoneal lavage fluid for total and differential leukocyte counts (neutrophils, monocytes, macrophages) using flow cytometry. Surface markers (e.g., CD11a, CD18) can provide further insight into cell activation states [50].
- Cytokine/Chemokine Levels: Measurement of pro-inflammatory mediators (e.g., IL-1β, IL-6, TNF-α) in peritoneal lavage fluid, plasma, or bronchoalveolar lavage fluid via ELISA [52] [4].
- Bacterial Load: In CLP models, quantitative culture of peritoneal fluid or blood assesses antibiotic efficacy.
- Histopathology: Examination of affected tissues, such as the lungs, for inflammation and injury [4].
- Molecular Analyses: Western blot, RT-qPCR, and ChIP assays to investigate drug effects on specific signaling pathways and epigenetic modifications [4].
Protocols for Therapeutic Testing
Protocol 1: Testing Intraperitoneal Antibiotic Regimens
This protocol is adapted from clinical studies on Automated Peritoneal Dialysis (APD)-associated peritonitis and is suitable for evaluating antibiotic efficacy and delivery methods in a pre-clinical setting [53] [54].
Objective: To compare the efficacy of continuous versus intermittent dosing of intraperitoneal antibiotics in resolving peritonitis and preventing systemic complications.
Materials:
- Mice with CLP-induced peritonitis.
- Antibiotics (e.g., Ceftazidime, Vancomycin).
- Saline for reconstitution and dilution.
- Equipment for intraperitoneal injection.
Method:
- Induction: Establish peritonitis using the CLP model [4].
- Randomization: Randomize animals into treatment and control groups.
- Dosing Regimens:
- Intermittent Dosing: Administer antibiotics via a single, concentrated bolus injection into the peritoneal cavity.
- Continuous Dosing: Administer the same total daily antibiotic dose, but divided and delivered via multiple injections or continuous infusion to maintain a steady state.
- Control Group: Receive a vehicle control.
- Monitoring: Monitor animals for signs of distress and disease progression.
- Endpoint Analysis: At 24-48 hours post-treatment, collect peritoneal lavage for bacterial culture, leukocyte count, and cytokine analysis (e.g., IL-1β, IL-6, TNF-α) [50].
Data Interpretation: Successful treatment is indicated by a significant reduction in bacterial load, normalization of leukocyte counts, and decreased pro-inflammatory cytokine levels in the treatment group compared to controls. Studies have shown that intermittent dosing can yield better primary response (91% vs 69%) and complete cure rates (93% vs 74%) than continuous regimens in some contexts [54].
Protocol 2: Evaluating Biologics and Molecular Glue Degraders
This protocol focuses on testing targeted therapies, such as the NEK7-directed molecular glue degrader MRT-8102, which modulates specific inflammatory pathways [52].
Objective: To assess the efficacy of a novel molecular glue degrader in inhibiting the NLRP3 inflammasome and reducing inflammatory cytokine production in vivo.
Materials:
- Mice with thioglycollate-induced peritonitis.
- Investigational drug (e.g., MRT-8102).
- Vehicle control.
- ELISA kits for IL-1β, IL-6, TNF-α.
Method:
- Induction: Inflame the peritoneal cavity by injecting 3% thioglycollate broth intraperitoneally [51].
- Pre-treatment: Administer the investigational drug (e.g., MRT-8102) or vehicle control orally or via intraperitoneal injection prior to or concurrent with thioglycollate challenge.
- Lavage and Sampling: At predetermined time points (e.g., 6-24 hours), euthanize animals and perform peritoneal lavage.
- Analysis:
- Cytokine Measurement: Analyze lavage fluid for IL-1β, IL-1α, IL-6, and TNF-α levels via ELISA [52].
- Cell Analysis: Count total and differential leukocytes in the lavage fluid.
- Mechanistic Studies: In separate experiments, isolate peritoneal macrophages for Western blot analysis to confirm target degradation (e.g., NEK7) and suppression of downstream effectors like caspase-1 [52].
Data Interpretation: A potent inhibitor will cause a significant, dose-dependent reduction in key inflammatory cytokines (IL-1β, IL-6) and leukocyte infiltration in the lavage fluid compared to the vehicle control. For example, MRT-8102 demonstrated near-complete suppression of IL-1β and caspase-1 in pre-clinical models [52].
Protocol 3: Investigating Epigenetic Modulators
This protocol uses the CLP model to investigate drugs that target epigenetic regulators of inflammation, such as the IKZF1 inhibitor lenalidomide [4].
Objective: To determine the effect of IKZF1 inhibition on macrophage-mediated inflammation and associated lung injury in acute peritonitis.
Materials:
- Mice with CLP-induced peritonitis.
- Lenalidomide.
- Vehicle control.
- Reagents for ELISA, Western blot, and histology (H&E staining).
Method:
- Induction and Treatment: Induce peritonitis via CLP. Administer lenalidomide or vehicle control therapeutically (post-CLP).
- Sample Collection: At 24 hours post-CLP, collect peritoneal lavage fluid and plasma for cytokine analysis. Harvest lung tissues.
- Analysis:
- Inflammatory Response: Measure TNF-α, IL-6, and IL-1β in lavage and plasma by ELISA.
- End-Organ Damage: Inflate and fix lungs with 4% PFA. Process for H&E staining to assess inflammatory cell infiltration and tissue injury [4].
- Mechanistic Validation: Isolate peritoneal macrophages for analysis of IKZF1 and SDHB expression (via RT-qPCR/Western blot) and assessment of mitochondrial function (ROS, ATP levels) [4].
Data Interpretation: Effective IKZF1 inhibition with lenalidomide should attenuate the inflammatory response (reduced cytokines) and mitigate remote lung injury. Mechanistically, this should correlate with restored mitochondrial function and SDHB expression in macrophages [4].
Data Analysis and Therapeutic Efficacy
Table 1: Efficacy Outcomes of Different Therapeutic Classes in Mouse Peritonitis Models
| Therapeutic Class | Example Compound | Key Efficacy Readouts | Observed Outcome | Citation |
|---|---|---|---|---|
| Antibiotics (IP) | Ceftazidime & Vancomycin | Peritonitis resolution rate, Time to resolution | 90.6% resolution (APD bags); 81.3% (manual exchange) | [53] |
| Molecular Glue Degrader | MRT-8102 (NEK7-targeting) | Inhibition of IL-1β, IL-6, TNF-α in peritoneal lavage | Potent inhibition of multiple cytokines; superior to NLRP3 inhibitor selnoflast in vitro | [52] |
| Epigenetic Modulator | Lenalidomide (IKZF1 inhibitor) | Cytokine levels (TNF-α, IL-6, IL-1β); Lung injury score | Attenuated inflammatory response and mitigated lung injury | [4] |
Signaling Pathways for Novel Therapeutic Targets
The mouse peritonitis model is powerful for probing novel signaling pathways. Key pathways currently under investigation include:
- The NLRP3/NEK7 Inflammasome Axis: Activation of the NLRP3 inflammasome, a critical process in inflammation, depends on the kinase NEK7. Molecular glue degraders like MRT-8102 target NEK7 for degradation, thereby inhibiting NLRP3 inflammasome assembly and subsequent release of IL-1β and IL-18 [52].
- The IKZF1/HDAC3-SDHB-Succinate Axis: The transcription factor IKZF1 is upregulated in macrophages during peritonitis. It recruits HDAC3 to the promoter of the SDHB gene, epigenetically repressing its expression. This leads to mitochondrial dysfunction, accumulation of succinate, and amplified pro-inflammatory signaling. Inhibiting IKZF1 with lenalidomide can reverse this effect [4].
The diagram below illustrates the IKZF1 signaling pathway identified as a key driver of inflammation in the CLP peritonitis model.
The Scientist's Toolkit
Table 2: Essential Research Reagent Solutions for Mouse Peritonitis Studies
| Reagent / Material | Function / Application | Example Use in Protocol |
|---|---|---|
| Thioglycollate Broth | Elicits sterile inflammation and synchronized immune cell recruitment. | Inducing neutrophil and macrophage influx for studying cell recruitment and polarization [51]. |
| Ceftazidime & Vancomycin | Broad-spectrum antibiotic combination for treating polymicrobial infections. | Testing efficacy and optimal dosing regimens (intermittent vs. continuous) in CLP models [53]. |
| Lenalidomide | IKZF1 inhibitor and immunomodulatory drug. | Investigating the role of IKZF1 in epigenetic regulation of macrophage inflammation [4]. |
| MRT-8102 | First-in-class NEK7-directed molecular glue degrader. | Targeting the NLRP3 inflammasome upstream to inhibit multiple inflammatory cytokines [52]. |
| ELISA Kits (IL-1β, IL-6, TNF-α) | Quantification of protein levels of specific cytokines in biological fluids. | Measuring inflammatory response in peritoneal lavage, plasma, or BALF as a key efficacy readout [52] [4]. |
| Flow Cytometry Antibodies (e.g., CD11b, F4/80, Ly6G) | Identification and quantification of specific immune cell populations. | Differentiating and counting neutrophils, monocytes, and macrophages in peritoneal lavage [51]. |
| CLP Surgical Kit | Standardized tools for performing cecal ligation and puncture. | Creating a polymicrobial, clinicaly relevant model of sepsis and peritonitis [50] [4]. |
Addressing Variability and Enhancing Reproducibility in Sepsis Modeling
Mouse models of peritonitis are indispensable tools for investigating the pathophysiology of inflammatory responses and evaluating potential therapeutic interventions. Within these models, two critical experimental parameters—the dose of the inflammatory slurry and the timing of antibiotic administration—profoundly influence the resulting pathophysiology, survival outcomes, and translational relevance. This Application Note synthesizes current research to provide detailed protocols and data analysis focused on these factors, specifically within the context of meconium-induced chemical peritonitis and bacterial peritonitis. The goal is to equip researchers with standardized methodologies that enhance reproducibility and the accurate interpretation of model outcomes, thereby supporting robust preclinical drug development.
The dosage of the inflammatory agent and the timing of antibiotic intervention are primary determinants of disease severity and mortality in peritonitis models. The data below summarize key quantitative findings from recent studies.
Table 1: Summary of Slurry Dose and Antibiotic Timing Effects in Mouse Peritonitis Models
| Model Type | Inducing Agent & Dose | Animal Subjects | Key Outcome Measures | Effect of Antibiotic Timing |
|---|---|---|---|---|
| Meconium Peritonitis [55] | Human Meconium Slurry (MS); LD40 established at 200 µL per 4-day-old pup | 4-day-old neonatal mouse pups | Dose-dependent mortality: 100-300 µL range; Hematological/ hepatorenal abnormalities; Increased inflammatory gene expression | Antibiotics (Imipenem) ineffective when given at induction; Heat inactivation of MS digestive enzymes improved survival |
| LPS-Induced Peritonitis [5] | LPS; 10 mg/kg intraperitoneally | Male C57BL/6 mice (6-8 weeks) | 290 Differentially Expressed Genes (DEGs) in blood: 242 up, 48 down; Activation of NOD-like & Toll-like receptor pathways | Not a focus of this particular study |
| Thioglycollate-Induced Peritonitis [22] | Thioglycollate; 4% (w/v) in 1 ml sterile saline | 8-10 week-old male BABL/c mice | Induction of sterile inflammation for immune cell recruitment and analysis | Not a focus of this particular study |
Detailed Experimental Protocols
Protocol 1: Neonatal Mouse Model of Meconium-Induced Chemical Peritonitis
This protocol details the induction of meconium peritonitis, which is a non-infectious chemical peritonitis caused by fetal intestinal perforation [55].
Stock Human Meconium Slurry (MS) Preparation
- Meconium Collection: Aseptically collect fresh meconium from healthy term human newborns via rectal stimulation after obtaining parental consent.
- Slurry Preparation: Weigh the meconium and add phosphate-buffered saline (PBS) to achieve a concentration of 500 mg/mL (1.0 mL of PBS per 500 mg of meconium).
- Homogenization: Vigorously stir the mixture. Aspirate the MS through a 23-gauge needle into a syringe to ensure homogenization.
- Storage and Quality Control: Aliquot the MS into 1-2 mL cryovials and store at -80°C. Before use, thaw an aliquot and plate 50 µL onto brain/heart infusion (BHI) agar to confirm sterility after 24 hours of incubation at 37°C. Use only sterile stocks.
Meconium Peritonitis Induction
- Animals: Use 4-day-old mouse pups, which are immunologically comparable to human preterm infants.
- Administration: Administer the MS dose (e.g., the established LD40 of 200 µL) via intraperitoneal injection.
- Monitoring: Monitor pups daily for health and survival for up to 7 days. Record body weights of survivors daily starting 24 hours post-induction.
Intervention with Antibiotics and Heat Inactivation
- Antibiotic Treatment: To test antibiotic efficacy, administer 100 mg/kg of imipenem and cilastatin sodium (or a vehicle control) subcutaneously immediately before the intraperitoneal administration of the MS dose. Monitor survival for 7 days [55].
- Heat Inactivation: To test the role of digestive enzymes in MS, heat-shock an aliquot of MS at 70°C or 100°C for 15 minutes before intraperitoneal administration. Compare survival rates against pups administered non-treated MS.
The following workflow diagram illustrates the key stages of this protocol:
Protocol 2: LPS-Induced Peritonitis for Transcriptomic Analysis
This protocol is used to study the systemic transcriptomic response to localized inflammation [5].
- Animals: Use 6-8 week-old male C57BL/6 mice.
- Peritonitis Induction: Administer a single intraperitoneal injection of LPS at a dose of 10 mg/kg.
- Sample Collection: At the designated endpoint (e.g., 24 hours post-injection), collect blood via cardiac puncture or other appropriate method under anesthesia.
- Transcriptomic Analysis: Extract RNA from blood samples for bulk RNA sequencing. Subsequent bioinformatics analysis can include identification of differentially expressed genes (DEGs), pathway enrichment analysis (e.g., KEGG, GO), and protein-protein interaction network analysis to identify hub genes.
Signaling Pathways and Molecular Mechanisms
The inflammatory response in peritonitis involves complex, interacting signaling pathways. LPS-induced models primarily activate pathogen recognition receptors, while meconium peritonitis triggers a distinct sterile inflammatory cascade.
Diagram 1: Core Inflammatory Signaling in Peritonitis
Key pathways activated in LPS-induced peritonitis include the Toll-like receptor (TLR) and NOD-like receptor signaling pathways, leading to a systemic inflammatory state characterized by the upregulation of hundreds of genes in the blood [5]. In contrast, the pathology of meconium peritonitis is driven mainly by digestive enzymes, and its systemic responses are distinct from classical sepsis, explaining the ineffectiveness of antibiotics and the efficacy of enzymatic inactivation [55].
The Scientist's Toolkit: Essential Research Reagents
Selecting the appropriate inducing agents and reagents is fundamental to successfully modeling different aspects of peritonitis.
Table 2: Key Research Reagent Solutions for Mouse Peritonitis Models
| Reagent / Material | Function in the Model | Key Considerations |
|---|---|---|
| Human Meconium Slurry [55] | Induces chemical peritonitis; models fetal intestinal perforation. | Sterility is critical; test before use. Pathogenic agent is primarily heat-labile digestive enzymes. |
| Lipopolysaccharide (LPS) [5] | Induces robust systemic inflammation via TLR4 activation; models Gram-negative bacterial infection. | Dose determines severity; 10 mg/kg i.p. induces strong transcriptomic changes. |
| Thioglycollate [22] | Induces sterile inflammation; used to recruit immune cells (e.g., macrophages) to the peritoneal cavity. | Concentration is key; 4% (w/v) is commonly used for eliciting peritoneal macrophages. |
| Imipenem/Cilastatin [55] | Broad-spectrum antibiotic used to test efficacy against bacterial components or co-infections. | Ineffective against meconium-induced chemical peritonitis when administered at model induction. |
| Fluoroquinolones (e.g., Moxifloxacin) [56] | Antibiotics with good intracellular penetration; used to study efficacy against intracellular pathogens (e.g., S. aureus). | Efficacy is influenced by pharmacokinetic/pharmacodynamic (PK/PD) parameters like Cmax/MIC ratio. |
In murine models of peritonitis, the implementation of robust supportive care, specifically fluid resuscitation and analgesia, is critical not only for animal welfare but also for the scientific validity and reproducibility of research outcomes. Unrelieved pain and dehydration can induce significant physiological stress, confounding immune and inflammatory readouts central to studying peritonitis pathophysiology [57] [58]. This protocol provides detailed methodologies for administering fluid therapy and analgesia, framed within the context of a fecal-induced peritonitis model, to ensure high standards of experimental rigor and translational relevance.
Fluid therapy is essential for maintaining tissue perfusion and correcting hypovolemia in septic mice. The following protocol, adapted from multi-laboratory sepsis studies, outlines a standardized approach for subcutaneous fluid resuscitation [59] [60].
Materials and Reagent Solutions
- Crystalloid Solution: Ringer's Lactate (Preferred) or 0.9% Saline [60].
- Syringes: 1 mL insulin syringes with 25-30 gauge needles.
- Heating Apparatus: Heating blankets or controlled thermal pads.
Step-by-Step Experimental Protocol
- Timing of Administration: Fluids are typically administered at the same time as antibiotic and analgesic treatment, approximately 4 hours post-induction of peritonitis, to minimize handling stress [60].
- Dosage and Route: Administer Ringer's Lactate subcutaneously at a volume of 0.3 mL per mouse [60]. Common injection sites include the loose skin over the scapulae or the flank.
- Supportive Care: Place heating blankets under half of the home cage to allow mice to self-regulate their body temperature and mitigate heat loss associated with fluid administration and disease [60].
- Monitoring: Monitor for local reactions at the infusion site, such as thrombosis or phlebitis. Systemic over-resuscitation, though less common with subcutaneous administration, can manifest as edema [61].
Table 1: Composition of Common Crystalloid Solutions for Fluid Resuscitation
| Solution | pH | Osmolarity (mOsm/L) | Sodium (mmol/L) | Chloride (mmol/L) | Other Key Electrolytes | Primary Indication |
|---|---|---|---|---|---|---|
| Ringer's Lactate | 6.5 | 280 | 131 | 112 | K⁺: 5; Ca²⁺: 3.7; Lactate: 28 | Resuscitation in sepsis, dehydration [61] [60] |
| 0.9% Saline | 6.0 | 308 | 154 | 154 | None | Fluid resuscitation (less ideal than balanced solutions) [61] |
| Dextrose 5% | 3.5–6.5 | 278 | 0 | 0 | Glucose: 252 | Source of free water post-resuscitation [61] |
Analgesia Protocol
Effective pain management is mandatory for ethical and scientific reasons. Pre-emptive analgesia is required unless specifically justified in an approved animal protocol [58].
Materials and Reagent Solutions
- Analgesics: Buprenorphine (opioid), Carprofen (NSAID), or Meloxicam (NSAID) [58].
- Syringes: 1 mL insulin syringes with 25-30 gauge needles.
- Assessment Tools: Mouse Grimace Scale (MGS) scoring sheet, nesting material for behavioral monitoring.
Step-by-Step Experimental Protocol
- Pre-emptive Analgesia: Administer the first dose of analgesic prior to or immediately following the initiation of peritonitis. This practice controls pain before it becomes established [58].
- Drug Selection and Dosage: The choice of analgesic should be tailored to the model. Evidence from leukemia xenograft models suggests tramadol may be superior to metamizole for hematological malignancies, but standard options are listed below [57].
- Buprenorphine: Administer 0.05 – 0.1 mg/kg SC every 4-8 hours. For sustained effect, extended-release formulations (Buprenorphine-SR, 0.5-1.0 mg/kg SC) provide coverage for 48-72 hours, reducing handling stress [58].
- Carprofen: Administer 5 mg/kg SC every 24 hours. This NSAID is effective for inflammatory pain and does not affect cardiomyocyte contractility, making it suitable for cardiovascular research [62] [58].
- Meloxicam: Administer 2-5 mg/kg SC or PO every 24 hours [58].
- Pain Assessment: Monitor mice at least daily using a combination of clinical and behavioral parameters. Key indicators include:
- Treatment Duration: Continue analgesic coverage for at least 48-72 hours post-procedure or until all signs of pain have resolved.
Table 2: Analgesics for Use in Murine Peritonitis Models
| Drug (Class) | Recommended Dose & Route | Frequency | Key Considerations |
|---|---|---|---|
| Buprenorphine (Opioid) | 0.05–0.1 mg/kg, SC or IP | 4-8 hours | Pre-emptive use may reduce anesthetic requirements; respiratory depressant effects [58]. |
| Buprenorphine-SR (Opioid) | 0.5–1.0 mg/kg, SC | 48-72 hours | Gold standard for prolonged relief; minimizes handling [58]. |
| Carprofen (NSAID) | 5 mg/kg, SC | 24 hours | No impact on cardiomyocyte contractility; suitable for inflammatory pain [62] [58]. |
| Meloxicam (NSAID) | 2-5 mg/kg, SC or PO | 24 hours | Effective for inflammatory pain [58]. |
| Tramadol | 1 mg/mL in drinking water | On-demand | Shown more effective than metamizole in ALL xenograft models [57]. |
Integrated Supportive Care Workflow
The following diagram illustrates the integration of fluid resuscitation and analgesia into a typical experimental timeline for a murine peritonitis study.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagent Solutions for Supportive Care in Murine Peritonitis
| Item | Function/Description | Example Use Case |
|---|---|---|
| Ringer's Lactate | Balanced crystalloid solution for hydration and electrolyte balance. | Subcutaneous fluid resuscitation in septic mice [61] [60]. |
| Buprenorphine-SR | Sustained-release opioid analgesic. | Provides 48-72 hours of continuous analgesia post-procedure, reducing animal handling [58]. |
| Carprofen | Non-steroidal anti-inflammatory drug (NSAID). | Management of inflammatory pain without affecting cardiomyocyte contractility [62] [58]. |
| Nesting Material | Enrichment to assess natural behavior. | Reduction in nesting activity is a sensitive indicator of pain and distress [57]. |
| Mouse Grimace Scale (MGS) | Standardized scoring system for pain assessment. | Objective evaluation of pain through facial expression changes [57] [58]. |
| Heating Blanket/Pad | External heat source to prevent hypothermia. | Placed under half the home cage to support thermoregulation during critical illness [60]. |
Within preclinical research on inflammatory responses, the Murine Sepsis Score (MSS) has been established as a robust, non-invasive clinical assessment tool for monitoring disease progression and severity in mouse models of peritonitis. Sepsis, a life-threatening condition triggered by a dysregulated host response to infection, is frequently studied using abdominal sepsis models such as fecal-induced peritonitis (FIP) and cecal ligation and puncture (CLP) [63] [33]. The MSS provides researchers and drug development professionals with a standardized, ethically acceptable method to quantify clinical illness, predict mortality, and define humane endpoints, thereby reducing the need to use death as an experimental endpoint and improving the translational value of preclinical studies [63] [64].
The Murine Sepsis Score: Components and Scoring System
The MSS is a composite scoring system that evaluates seven independent clinical variables based on the observable physical appearance and behavior of mice [63] [33]. Each variable is assigned a score from 0 (healthy/normal) to 4 (most severely impaired), and the final MSS is the average of these seven component scores [33].
Table 1: Detailed Scoring Criteria for the Murine Sepsis Score (MSS)
| Score | 0 | 1 | 2 | 3 | 4 |
|---|---|---|---|---|---|
| Appearance | Smooth coat | Patches of piloerected hair | Majority of back piloerected | Puffy appearance, piloerection may or may not be present | Emaciated appearance, piloerection may or may not be present |
| Level of Consciousness | Active | Active but avoids standing upright | Noticeably slowed activity, still ambulant | Impaired activity, only moves when provoked with tremor | Severely impaired, remains stationary when provoked |
| Activity | Normal activity (eating, drinking, climbing) | Slightly suppressed activity, moving around cage bottom | Suppressed activity, stationary with occasional investigation | No activity | No activity, experiences tremors (hind legs) |
| Response to Stimulus | Immediate response to auditory or touch stimulus | Slow/no response to auditory; strong escape response to touch | No auditory response; moderate touch response (moves a few steps) | No auditory response; mild touch response (no locomotion) | No auditory/touch response, cannot right itself |
| Eyes | Open | Not fully open, possibly with secretions | At least half closed, possibly with secretions | Half closed or more, possibly with secretions | Closed or milky |
| Respiration Rate | Normal, rapid mouse respiration | Slightly decreased (rate not quantifiable by eye) | Moderately reduced (rate at upper range of eye quantification) | Severely reduced (easily countable, ~0.5s between breaths) | Extremely reduced (>1s between breaths) |
| Respiration Quality | Normal | Brief periods of laboured breathing | Laboured, no gasping | Laboured with intermittent gasps | Gasping |
Validation and Performance of the MSS
The MSS has been extensively validated in multiple independent studies, demonstrating high reliability and predictive power for sepsis severity and mortality.
Table 2: Validation and Performance Characteristics of the MSS
| Validation Metric | Reported Performance | Context and Significance |
|---|---|---|
| Predictive Power for Mortality | MSS ≥ 3 had 100% specificity for predicting death within 24 hours [63] [33]. | Allows for early humane intervention and accurate prognosis. |
| Inter-rater Reliability | Intra-class coefficient = 0.96 [63]. | Excellent consistency between different observers. |
| Internal Consistency | Cronbach alpha coefficient = 0.92 [63]. | High degree of correlation between the seven score components. |
| Comparison to Body Temperature | AUC = 0.95 for modified MSS vs. 0.88 for body temperature in predicting death [64]. | MSS is a highly robust standalone predictor. |
| Early Diagnosis (A-MSS) | 87.5% sensitivity, 100% specificity at 4 hours post-induction (A-MSS ≥ 3.5) [65]. | Adapted MSS (A-MSS) includes glucose, temperature, and weight for earlier detection. |
Experimental Protocol for MSS Application in Mouse Peritonitis
Model Induction
Two primary models are used for inducing abdominal sepsis:
- Fecal-Induced Peritonitis (FIP): Prepare a fecal slurry from cecal contents of donor mice or rats, homogenized and filtered in sterile saline [33] [29]. Administer via intraperitoneal (IP) injection at a defined concentration (e.g., 90 mg/mL for a polymicrobial sepsis with high mortality) [33].
- Cecal Ligation and Puncture (CLP): Under anesthesia, perform a laparotomy, exteriorize the cecum, ligate a portion, and puncture with a needle (e.g., 18-22 gauge) to extrude a small amount of feces [4] [64].
MSS Monitoring Workflow
The following diagram illustrates the standard workflow for MSS monitoring in a peritonitis study:
Key Procedural Notes
- Monitoring Schedule: In acute studies, monitor mice every 2-4 hours for the first 12 hours, and then hourly thereafter [33] [64].
- Humane Endpoints: Common criteria for euthanasia include an MSS greater than 21 (on the 0-28 scale), or any single component score reaching 4 [33].
- Environmental Support: Provide supportive care such as subcutaneous fluids (e.g., Ringer's lactate) and analgesia (e.g., buprenorphine). External heat sources should be available to allow mice to self-regulate body temperature [64] [29].
Integration with Physiological and Molecular Data
The clinical assessment provided by the MSS is powerfully complemented by physiological measurements and molecular analyses. Research shows that the MSS correlates strongly with the progression of key pathophysiological events in sepsis.
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for Peritonitis and MSS Studies
| Reagent/Material | Function/Application | Example Specifications |
|---|---|---|
| Fecal Slurry | Induction of polymicrobial sepsis in FIP model. | Prepared from cecal contents (mouse or rat) in sterile saline or phosphate buffer, typically at 90-100 mg/mL concentration [33] [29]. |
| Anesthetic | Surgical anesthesia for CLP model or IP injections. | Isoflurane (inhalant) or Ketamine/Xylazine (injectable) cocktail [4] [64]. |
| Analgesic | Post-procedure pain relief, adhering to animal welfare. | Buprenorphine (0.05-0.1 mg/kg, subcutaneously), administered every 8-12 hours [64] [29]. |
| Fluid Resuscitation | Supportive therapy to counteract hypovolemia. | Sterile Ringer's Lactate or 0.9% Saline, administered subcutaneously (e.g., 1 mL) [64] [66]. |
| Antibiotics | Mimics clinical practice; can be timed to modulate severity. | Piperacillin-tazobactam or imipenem administered intraperitoneally [29]. |
| IKZF1 Inhibitor | Investigational tool to probe macrophage-mediated inflammation. | Lenalidomide (Len), used to attenuate inflammatory responses [4] [27]. |
| ELISA Kits | Quantification of systemic inflammatory cytokines. | Commercial kits for mouse IL-6, IL-1β, TNF-α (e.g., BioLegend LEGEND MAX) [4]. |
The Murine Sepsis Score is an indispensable, validated tool for objectively monitoring disease severity in mouse models of peritonitis. Its high reliability, predictive power for mortality, and strong correlation with underlying pathophysiological changes make it a cornerstone for ethical and scientifically robust preclinical research. When integrated with physiological measurements and molecular analyses, the MSS provides a comprehensive framework for evaluating novel therapeutic strategies and advancing our understanding of the host response to sepsis.
Navigating Inter-Laboratory Variability in Multi-Center Studies
Inter-laboratory variability represents a significant challenge in preclinical research, particularly in studies utilizing mouse peritonitis models for evaluating inflammatory responses. Despite rigorous standardization efforts, fundamental differences in experimental outcomes persist across research facilities, threatening the translational validity of scientific findings and impeding drug development progress. This application note examines the sources and impacts of this variability within the context of multi-center studies, providing evidence-based protocols and strategic frameworks to enhance methodological harmonization and experimental reproducibility.
Recent investigations by the National Preclinical Sepsis Platform (NPSP) have quantified substantial disparities in outcomes between research sites. In a meticulously standardized fecal-induced peritonitis (FIP) model, the same protocol yielded 60% mortality at one site versus 88% mortality at another – a statistically significant difference (p < 0.05) despite identical fecal slurry doses (0.75 mg/g) and implementation procedures [60] [29]. This phenomenon underscores the complex interplay of environmental, technical, and biological factors that collectively contribute to inter-laboratory variability, necessitating comprehensive strategies that extend beyond protocol standardization alone.
Quantitative Evidence of Inter-Laboratory Disparities
The NPSP multi-laboratory study systematically documented variability across multiple parameters, providing compelling evidence of the reproducibility challenge in preclinical sepsis research.
Table 1: Inter-Laboratory Variability in Murine Fecal-Induced Peritonitis Models [60] [29]
| Experimental Parameter | Site 1 Results | Site 2 Results | Statistical Significance |
|---|---|---|---|
| Mortality (0.75 mg/g dose) | 60% | 88% | p < 0.05 |
| Body Temperature Patterns | Moderate hypothermia | Severe hypothermia | Marked differences observed |
| Murine Sepsis Score Utility | Poor association with mortality progression | Poor association with mortality progression | Consistent limitation across sites |
| Early Antibiotic Efficacy | 100% survival with 4h administration | 100% survival with 4h administration | Consistent benefit across sites |
| Fecal Slurry Dose Response | Increased severity with escalating doses (0.5-2.5 mg/g) | Increased severity with escalating doses (0.5-2.5 mg/g) | Consistent response across sites |
The consistency in certain responses (e.g., dose-dependent severity increases, antibiotic efficacy) demonstrates that core biological mechanisms remain intact across sites, while the marked differences in mortality and physiological parameters highlight the substantial impact of site-specific factors [60] [29]. Additional research has revealed that even subtle differences in housing conditions, animal supplier sub-strains, or technician technique can significantly alter inflammatory responses and experimental outcomes in mouse peritonitis models [67].
Standardized Experimental Protocols
Fecal-Induced Peritonitis (FIP) Model Protocol
The FIP model minimizes surgical variability and operator dependence, making it particularly suitable for multi-laboratory studies [60] [29].
Table 2: Key Research Reagent Solutions for Fecal-Induced Peritonitis Models [60] [29]
| Reagent/Material | Specifications | Function in Protocol |
|---|---|---|
| Fecal Slurry | Prepared from Sprague Dawley rat cecal contents; 100 mg/mL concentration in 5% dextrose with 10% glycerol | Induces polymicrobial peritoneal infection; standardized aliquots stored at -80°C |
| Animal Strain | C57BL/6 mice (Helicobacter hepaticus-free); 8-10 weeks old; 20-30 g weight | Provides consistent genetic background for inflammation studies |
| Anesthetic | Isoflurane | Ensures humane, consistent anesthesia for intraperitoneal injection |
| Antibiotic Regimen | Piperacillin-tazobactam or imipenem in 100 μL Ringer's lactate | Mimics clinical sepsis management; timing critically affects outcomes |
| Supportive Care | Subcutaneous Ringer's lactate and buprenorphine analgesia | Maintains animal welfare and complies with MQTiPSS recommendations |
| Vehicle Control | 5% dextrose solution with 10% glycerol | Serves as negative control for fecal slurry injection |
Protocol Workflow:
Critical Procedural Steps:
Fecal Slurry Preparation: Create standardized batches from donor rat cecal contents homogenized in 50 mM phosphate buffer (6 mL/g). Filter through 100 μM cell strainer, centrifuge at 3000 × g for 25 minutes at 4°C, and resuspend in 5% dextrose with 10% glycerol to 100 mg/mL concentration. Aliquot and store at -80°C to minimize batch-to-batch variability [60] [29].
Animal Injection: Administer fecal slurry via intraperitoneal injection in the lower abdominal quadrant using a 25-gauge needle under isoflurane anesthesia. Maintain consistent injection technique across all operators and sites [60].
Supportive Care Administration: Provide subcutaneous Ringer's lactate (fluid resuscitation) and buprenorphine (analgesia) to all animals following MQTiPSS recommendations. Implement external heat support via heating blankets placed beneath half of each cage to allow behavioral thermoregulation [60] [29].
Antibiotic Timing: Administer antibiotics (piperacillin-tazobactam or imipenem) according to experimental design. Early administration (within 4 hours of inoculation) demonstrates significant survival benefit compared to late administration (after 12 hours) [60].
Monitoring and Endpoints: Assess animals for 72 hours using modified Murine Sepsis Score (MSS), though note its documented limitation in predicting mortality progression. Collect terminal samples for bacterial load quantification in blood and peritoneal fluid [60] [29].
Alternative Peritonitis Model: Thioglycollate-Induced Inflammation
For studies focusing specifically on innate immune cell recruitment without the complexity of live infection, thioglycollate-induced peritonitis offers a complementary approach.
Protocol Workflow:
Key Steps:
- Prepare 4% (w/v) thioglycollate in sterile saline [22].
- Administer 1 mL intraperitoneally to 8-10 week old male BABL/c mice [22].
- Introduce experimental treatments 4 hours post-induction.
- Collect peritoneal cells via lavage with 5 mL HBSS at 24 hours post-induction.
- Perform differential cell counts using hematology analyzers or flow cytometry [22].
Understanding the factors contributing to variability is essential for developing effective mitigation strategies.
Key Variability Sources:
Environmental Conditions: Documented differences in ambient temperature ranges (20-22°C vs 21-24°C) between facilities correlate with variations in mortality outcomes, potentially through effects on thermoregulation and metabolic stress [60] [29].
Technical Execution: Subtle variations in fecal slurry preparation, injection technique, and monitoring consistency introduce operator-dependent variability despite standardized protocols [60].
Biological Factors: Emerging evidence indicates significant sex-associated differences in peritoneal immune responses, with scRNA-seq analyses revealing sexually dimorphic gene expression in omental stromal cells that correlates with macrophage polarization states [67]. These biological differences may interact with experimental conditions to produce site-specific outcomes.
Mitigation Strategies for Multi-Center Studies
Comprehensive Standardization Framework
Effective multi-center studies require a systematic approach to standardization that addresses both procedural and environmental variables:
Centralized Reagent Production: Prepare master batches of critical reagents (e.g., fecal slurry) at a central facility and distribute aliquots to all participating sites to minimize batch-to-batch variability [60] [29].
Cross-Site Training: Implement hands-on training workshops for all technical staff to ensure consistent procedural execution, particularly for technically sensitive steps like intraperitoneal injections and clinical scoring.
Environmental Monitoring and Control: Standardize and continuously monitor housing conditions (temperature, humidity, light cycles) across facilities with defined acceptable ranges narrower than typical animal facility standards.
Predefined Analytical Plans: Establish rigorous statistical plans prior to study initiation, including predefined sample sizes, primary endpoints, and covariate adjustment strategies for known sources of variability (e.g., animal sex, batch effects) [60] [68].
Blinded Outcome Assessment: Implement blinding procedures for outcome assessments, particularly for subjective measures like clinical scoring systems, to minimize observer bias across sites.
Data Harmonization and Reporting Standards
Adopt standardized data collection and reporting frameworks aligned with ARRIVE 2.0 guidelines and MQTiPSS recommendations to enhance transparency and reproducibility [60] [29]. Include detailed methodological descriptions that would enable exact protocol replication, including specific housing conditions, technician training procedures, and quality control measures.
Inter-laboratory variability presents a formidable but addressable challenge in multi-center peritonitis studies. The documented disparities in experimental outcomes across research sites stem from complex interactions between environmental conditions, technical execution, and biological factors. Through implementation of robust standardization frameworks, centralized reagent production, cross-site training initiatives, and rigorous environmental monitoring, researchers can significantly enhance the reproducibility and translational impact of mouse peritonitis models. The strategies outlined in this application note provide a practical roadmap for navigating variability challenges, ultimately strengthening the scientific validity of multi-center preclinical studies in inflammatory response research and drug development.
Incorporating Aged Animals to Improve Clinical Translatability
The use of preclinical models has been the backbone of translational research for more than a century, with mice serving as critical models in the preliminary stages of drug testing for determining efficacy and ruling out potential human-relevant toxicities [69]. Historically, most preclinical pharmacological studies have utilized young, relatively healthy, inbred male models in highly controlled environments, with limited testing beyond six months to avoid geriatric issues [69]. However, in the field of inflammation and peritonitis research, this approach creates a significant translational gap, as the human patient population most susceptible to severe peritonitis outcomes is typically aged, with complex comorbidities and polypharmacy [69] [70].
The growing focus on using more appropriate preclinical models is particularly relevant for testing therapeutics commonly used in older populations [69]. This application note provides detailed methodologies and protocols for incorporating aged animals into mouse models of peritonitis, specifically framed within research evaluating inflammatory responses. By optimizing preclinical models of ageing, researchers can significantly improve the translation of findings into clinical trials, ultimately enhancing the development of effective therapeutic strategies for peritonitis in aging human populations.
Establishing Aged Mouse Models of Peritonitis: Methodological Approaches
Animal Model Considerations and Selection Criteria
Age and Sex Representation:
- Optimal Age Selection: Vendors like the Jackson Laboratory now offer several mouse strains aged up to 80 weeks, removing a significant barrier to aged animal research [69]. For peritonitis studies, consider using mice at 18-24 months to represent an aged population.
- Sex Inclusion: The use of both sexes is critical for generalizability. Despite well-established differences in ageing trajectories and pharmacology, females remain under-represented in biomedical research [69]. Include both sexes in experimental designs with appropriate statistical power.
Genetic Diversity:
- A key criticism of the inbred C57BL/6 mouse, one of the most widely used strains in mammalian biomedical research, is the lack of genetic heterogeneity that accurately reflects human populations [69].
- Genetically heterogeneous mouse lines such as the UM-HET3, diversity outbred, or collaborative cross have been developed to address this issue and are increasingly utilized in ageing research [69].
Health Status Assessment:
- Implement frailty assessment tools to measure clinically relevant outcomes in preclinical studies. These tools allow the use of frailty as a primary outcome in testing therapeutics and geroprotectors in preclinical models [69].
- Conduct comprehensive healthspan assessments using standardized approaches for studying healthspan in rodents, including proposed toolbox of validated measures [69].
Experimentally-Induced Peritonitis Models in Aged Mice
Several well-established methods for inducing peritonitis in mice can be adapted for aged animal research. The selection of a specific model should align with the research objectives and clinical context being modeled.
Cecal Ligation and Puncture (CLP) Model: The CLP model is widely considered the gold standard for modeling polymicrobial sepsis secondary to peritonitis and is particularly relevant for aged animal studies due to its clinical relevance [4].
Procedure:
- Anesthetize aged mice via isoflurane inhalation.
- Exteriorize the cecum through a midline abdominal incision.
- Ligate the cecum below the ileocecal valve.
- Puncture once with a 22-gauge needle to extrude a small amount of feces.
- Replace the cecum into the abdominal cavity and close the abdominal wall in layers.
- Administer 0.3 mL of saline subcutaneously for fluid resuscitation immediately after surgery [4].
Lipopolysaccharide (LPS)-Induced Peritonitis Model: LPS-induced peritonitis provides a controlled model for studying inflammatory responses to gram-negative bacterial components [5].
Procedure:
- Administer LPS (10 mg/kg) intraperitoneally to aged mice.
- Collect blood samples and peritoneal lavage fluid at appropriate timepoints for analysis.
- Monitor inflammatory responses through cytokine measurements and cellular infiltration [5].
Chemical Irritant Models: Thioglycollate-induced peritonitis is valuable for studying sterile inflammatory responses and macrophage recruitment [22] [4].
Procedure:
- Inject 3-4% (w/v) thioglycollate broth intraperitoneally in 1 mL volume.
- After 3-4 days, collect peritoneal macrophages by lavage for ex vivo studies [22] [4].
Clinical Biomarker Assessment in Aged Peritonitis Models
The table below outlines key inflammatory and bacterial biomarkers relevant for monitoring peritonitis progression and therapeutic response in aged mouse models:
Table 1: Key Biomarkers for Assessing Peritonitis in Aged Mouse Models
| Biomarker | Biological Function | Measurement Technique | Significance in Aged Peritonitis |
|---|---|---|---|
| IL-6 | Pro-inflammatory cytokine | ELISA, multiplex immunoassay | Correlates with organ failure scores; massively elevated in meconium peritonitis [70] [9] |
| TNF-α | Pro-inflammatory cytokine | ELISA, multiplex immunoassay | Key mediator in systemic inflammatory response; elevated in stercoraceous peritonitis [70] |
| PCT (Procalcitonin) | Prohormone of calcitonin | ELISA, immunoassay | Guides antibiotic discontinuation in intra-abdominal sepsis [70] |
| HMGB1 | Nuclear protein released during cell damage | ELISA, Western blot | Late mediator in sepsis; marker of disease severity [70] |
| CRP | Acute phase protein | Immunoassay, ELISA | General marker of inflammation; elevated in purulent and pancreatitis-associated peritonitis [70] |
| NLR | Neutrophil-to-Lymphocyte Ratio | Complete blood count (CBC) | Hematological indicator of systemic inflammation [70] |
| NGAL | Neutrophil gelatinase-associated lipocalin | ELISA, immunoassay | Identifies infection in peritoneal dialysis patients [70] |
Quantitative Assessment of Age-Related Differences in Peritonitis Responses
The integration of aged animals into peritonitis research necessitates careful consideration of the quantitative differences in inflammatory responses, metabolic profiles, and therapeutic outcomes compared to young animals. The table below summarizes key parameters that demonstrate differential responses in aged versus young mice in peritonitis models:
Table 2: Comparative Responses in Young vs. Aged Mice in Peritonitis Models
| Parameter | Young Mice (2-4 months) | Aged Mice (18-24 months) | Clinical Relevance |
|---|---|---|---|
| Inflammatory Cytokine Production | Moderate IL-6, TNF-α response | Exaggerated and prolonged pro-inflammatory cytokine release [69] | Mimics cytokine storms in elderly patients |
| Immune Cell Recruitment | Robust neutrophil influx, coordinated macrophage activation | Dysregulated leukocyte infiltration, impaired macrophage phagocytosis [69] | Reflects immunosenescence in aging humans |
| Metabolic Alterations | Transient mitochondrial dysfunction | Persistent ROS production, succinate accumulation, ATP deficiency [4] | Represents age-related metabolic inflexibility |
| Mortality Rates | Model-dependent (e.g., LD40 in meconium peritonitis) [9] | Significantly elevated in comparable insult models [69] | Correlates with higher sepsis mortality in elderly |
| Organ Dysfunction | Limited to primary affected systems | Multi-organ failure, particularly lung injury and renal impairment [4] | Models clinical complexity in aged patients |
| Frailty Progression | Rapid recovery post-resolution | Persistent functional decline, increased frailty index [69] | Captures clinical geriatric syndrome outcomes |
| Therapeutic Response | Standard drug efficacy | Altered pharmacokinetics/pharmacodynamics, requires dose adjustment [69] | Informs dosing in elderly patients with polypharmacy |
Advanced Technical Approaches for Aged Peritonitis Research
Transcriptomic and Molecular Analyses
Advanced omics technologies provide powerful tools for understanding the molecular mechanisms underlying age-specific responses to peritonitis.
Bulk RNA Sequencing:
- Application: Characterize gene expression profiles in blood and peritoneal tissues during peritonitis [5].
- Protocol: Collect blood samples from control and peritonitis-aged mice; perform RNA extraction and sequencing; identify differentially expressed genes (DEGs) through bioinformatics analysis [5].
- Aged-Specific Considerations: Focus on pathways related to immunosenescence, inflammaging, and mitochondrial dysfunction.
Single-Cell RNA Sequencing:
- Application: Resolve cellular heterogeneity in peritoneal immune responses [5].
- Protocol: Isolate peritoneal cells from aged mice; perform single-cell encapsulation and library preparation; analyze cell-type specific transcriptional changes.
- Integration: Cross-reference findings with human sepsis patient data to validate clinical relevance [5].
Molecular Dynamics Simulations:
- Application: Explore structural characteristics of key proteins identified through transcriptomic analyses [5].
- Protocol: Identify hub proteins from DEG analyses; perform 300 ns molecular dynamics simulations; analyze structural parameters (Rg, RMSF, RMSD, hydrogen bonding) [5].
Metabolic and Epigenetic Profiling
Recent research has highlighted the crucial role of metabolic and epigenetic regulation in inflammatory responses, particularly in aged models.
Mitochondrial Function Assessment:
- Evaluate reactive oxygen species (ROS) production, ATP levels, and succinate accumulation in macrophages from aged mice [4].
- Mechanistic studies should include chromatin immunoprecipitation (ChIP), co-immunoprecipitation (Co-IP), and HDAC activity assays [4].
Epigenetic Modulation:
- Investigate IKZF1/HDAC3-SDHB-succinate axis in macrophage hyperactivation [4].
- Analyze SDHB expression and acetylation status under LPS stimulation, with acetate supplementation to modulate histone H3K9 acetylation [4].
Visualization of Experimental Workflows and Signaling Pathways
Aged Mouse Peritonitis Study Workflow
IKZF1-Mediated Inflammatory Signaling in Aged Macrophages
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for Aged Mouse Peritonitis Studies
| Reagent/Material | Specification | Application | Aged Model Considerations |
|---|---|---|---|
| Aged Mice | C57BL/6 (18-24 months) or genetically diverse strains (UM-HET3) | Model organism | Source from vendors providing aged animals; ensure health monitoring [69] |
| Lipopolysaccharide (LPS) | Escherichia coli, 10 mg/kg dosing | Induce sterile inflammation | Age-adjusted dosing may be required due to altered metabolism [5] |
| Thioglycollate Broth | 3-4% (w/v) in sterile saline | Macrophage recruitment and elicitation | Monitor enhanced inflammatory response in aged animals [22] [4] |
| Lenalidomide | IKZF1 inhibitor, 100 mg/kg | Target inflammatory transcription factors | Test in context of polypharmacy models [4] [69] |
| ELISA Kits | IL-6, TNF-α, IL-1β, PCT | Cytokine and biomarker quantification | Include age-specific reference ranges [4] [70] |
| RNA Sequencing Kits | Bulk and single-cell RNA preparation | Transcriptomic profiling | Focus on immunosenescence and inflammaging pathways [5] |
| Frailty Assessment Tools | Clinical frailty index for mice | Healthspan and functional assessment | Critical for determining baseline health status [69] |
| HDAC Activity Assay Kits | Colorimetric/fluorometric detection | Epigenetic regulation studies | Target for mitigating age-enhanced inflammation [4] |
The incorporation of aged animals into mouse models of peritonitis represents a critical advancement in improving the clinical translatability of inflammatory response research. By implementing the protocols, assessment tools, and methodological considerations outlined in this application note, researchers can significantly enhance the predictive value of their preclinical studies. The optimal preclinical ageing studies of therapeutics for peritonitis should be completed in old, genetically diverse models of both sexes, with careful attention to frailty assessment, polypharmacy considerations, and clinically relevant outcome measures [69]. This approach will facilitate the development of more effective therapeutic strategies for the aging population most vulnerable to the severe consequences of peritonitis and sepsis.
Ensuring Model Fidelity and Translational Potential for Drug Development
In preclinical research on inflammatory responses, the mouse peritonitis model serves as a critical experimental system for investigating sepsis pathophysiology and therapeutic interventions. A cornerstone of this research involves validating biomarkers that accurately reflect disease severity, a process that requires correlating quantifiable molecular measurements with clinically relevant disease scores. This application note details standardized protocols for establishing these critical correlations between clinical scores, cytokine levels, and bacterial loads in murine peritonitis models, enabling robust biomarker validation for drug development. The systematic approach outlined here provides a framework for researchers to generate reproducible, clinically translatable data on inflammatory responses, enhancing the predictive value of preclinical studies in sepsis and peritonitis research.
Experimental Models of Mouse Peritonitis
Several well-established mouse peritonitis models are available for sepsis and inflammatory response research, each with distinct characteristics and applications. The choice of model significantly influences the inflammatory profile and clinical progression, thereby impacting biomarker validation strategies.
Table 1: Comparison of Mouse Peritonitis Models for Biomarker Research
| Model Type | Induction Method | Key Characteristics | Best Applications |
|---|---|---|---|
| Cecal Ligation and Puncture (CLP) | Ligation and puncture of cecum with needle [71] | Polymicrobial infection, reproducible hyperinflammation, multi-organ failure [71] | ACLF, sepsis with multi-organ failure, systemic inflammation |
| Fecal-Induced Peritonitis (FIP) | Intraperitoneal injection of standardized fecal slurry [66] | Tunable severity, compatible with antibiotics/fluids, age-dependent responses [66] | Age-specific sepsis responses, therapeutic intervention studies |
| LPS-Induced Peritonitis | Intraperitoneal LPS injection (e.g., 10 mg/kg) [5] | Sterile inflammation, controlled inflammatory cascade, rapid onset | Transcriptomic studies of innate immunity, sterile inflammation mechanisms |
| Meconium Slurry-Induced | Intraperitoneal human meconium administration [9] | Chemical peritonitis, sterile inflammation, neonatal model | Neonatal peritonitis, digestive enzyme-mediated inflammation |
Quantitative Biomarker Profiles in Peritonitis
Comprehensive biomarker validation requires establishing baseline profiles across different peritonitis models. The following data represent aggregate quantitative measurements from published studies to serve as reference points for correlation analyses.
Table 2: Biomarker Measurements in Murine Peritonitis Models
| Parameter | CLP Model [71] | FIP Model (Aged Mice) [66] | LPS Model [5] | Measurement Method |
|---|---|---|---|---|
| Inflammatory Cytokines | ||||
| IL-6 | Significantly elevated | Markedly elevated in non-survivors | Not specified | ELISA, Multiplex immunoassay [71] [66] |
| TNF-α | Upregulated in kidney tissue | Not specified | Not specified | RT-qPCR, ELISA [71] |
| MCP-1/CCL2 | Not specified | Elevated in non-survivors | Not specified | Multiplex immunoassay [66] |
| Organ Function Markers | ||||
| Serum Creatinine | Increased [71] | Not specified | Not specified | Dri-Chem analyzer [71] |
| Blood Urea Nitrogen (BUN) | Elevated [71] | Not specified | Not specified | Dri-Chem analyzer [71] |
| AST | Significantly elevated [71] | Not specified | Not specified | Dri-Chem analyzer [71] |
| Bacterial Load | Widespread tissue colonization [71] | Impaired clearance in aged non-survivors [66] | Not applicable | CFU counting [71] [66] |
| Clinical Scores | Neurological behavior test scores worsened [71] | Modified Murine Sepsis Score [66] | Not specified | Standardized scoring systems [71] [66] |
Detailed Experimental Protocols
Protocol 1: Cecal Ligation and Puncture (CLP) with Biomarker Sampling
This protocol describes the established CLP procedure for inducing polymicrobial peritonitis with simultaneous clinical scoring and biomarker collection [71].
Materials:
- Male C57BL/6J mice (6 weeks old, 20-25g)
- Carbon tetrachloride (CCl4) for pre-existing cirrhosis induction (optional)
- Isoflurane/oxygen anesthesia system
- 3-0 silk suture
- 30-gauge needle for cecal puncture
- Buprenorphine (0.3 mg/kg) for analgesia
Procedure:
- Pre-conditioning (optional): For ACLF studies, induce cirrhosis by i.p. injections of CCl4 (1 µL/g body weight) in olive oil twice weekly for 12 weeks until ascites development [71].
- Anesthesia and Preparation: Anesthetize mice with inhaled isoflurane/oxygen. Administer buprenorphine (0.3 mg/kg) subcutaneously for analgesia.
- CLP Surgery: Perform laparotomy to isolate the cecum. Ligate approximately 2/3 of the cecum with 3-0 silk suture. Puncture the ligated cecum once with a 30-gauge needle.
- Post-operative Care: Return extruded stool to abdominal cavity and suture abdominal wall and skin. Administer buprenorphine every 12 hours until endpoint.
- Clinical Scoring: Assess modified murine sepsis score (MSS) components including posture, respiration quality, responsiveness, activity, and appearance at 4h, 8h, and 12h post-procedure [66].
- Sample Collection: At designated endpoints (typically 24h), collect blood via cardiac puncture for serum separation. Perform peritoneal lavage with 1mL warm HBSS for bacterial and inflammatory cell quantification. Harvest organs for histology and gene expression analysis.
Protocol 2: Correlation of Clinical Scores with Biomarker Measurements
This protocol standardizes the process for establishing correlations between clinical assessments and molecular biomarkers.
Clinical Scoring System: Utilize the Modified Murine Sepsis Score (MSS) with the following components, each scored 0 (healthy) to 3 (severely affected) [66]:
- Posture: Normal stance (0) to hunched position (3)
- Respiration: Normal (0) to labored breathing (3)
- Responsiveness: Alert (0) to non-responsive to stimulation (3)
- Activity: Normal movement (0) to immobile (3)
- Appearance: Normal fur (0) to piloerection (3)
Biomarker Sampling Timeline:
- Baseline: Collect blood and clinical scores immediately pre-procedure
- Early Phase (4-8h): Assess clinical scores and collect samples from subgroup
- Peak Inflammation (12-24h): Comprehensive sampling including serum, peritoneal fluid, and tissues
- Resolution Phase (48-72h): Long-term studies with therapeutic interventions
Sample Processing Methods:
- Serum Cytokines: Use multiplex immunoassays (Meso Scale Discovery) or ELISA for IL-6, IL-10, MCP-1, TNF-α, and others [72] [66]
- Bacterial Quantification: Plate serial dilutions of peritoneal lavage fluid on blood agar plates, incubate aerobically/anaerobically at 37°C for 24h, and count CFUs [73]
- Organ Function Markers: Analyze serum creatinine, BUN, AST, and ALT using clinical chemistry analyzers [71]
- Gene Expression: Extract RNA from tissues, synthesize cDNA, and perform RT-qPCR for inflammatory markers (Kim-1, Il-6, Tnf) [71]
Regulatory and Validation Considerations
Biomarker validation for regulatory submission requires careful consideration of context of use (COU) and fit-for-purpose validation strategies [74] [75].
Biomarker Categories and Definitions:
- Monitoring Biomarkers: Measured serially to assess disease status changes (e.g., cytokine levels during sepsis progression)
- Response Biomarkers: Change in response to therapeutic intervention
- Safety Biomarkers: Indicate potential organ injury during treatment (e.g., serum creatinine for kidney function) [74]
Fit-for-Purpose Validation: The level of analytical validation should be tailored to the specific COU [74] [75]:
- For early drug discovery: Focus on precision and relative accuracy
- For regulatory decision-making: Require comprehensive validation including sensitivity, specificity, reproducibility, and reference ranges
- For biomarkers supporting efficacy claims: Demonstrate clinical validity through consistent correlation with clinical outcomes
Advanced Analytical Technologies: While ELISA has been the traditional gold standard, advanced platforms offer enhanced performance:
- Multiplex Immunoassays (MSD): Provide superior sensitivity (up to 100x greater than ELISA) and broader dynamic range with cost savings for multiple analytes [72]
- LC-MS/MS: Enables detection of low-abundance biomarkers and analysis of hundreds to thousands of proteins in single runs [72]
Visualization of Experimental Workflows and Signaling Pathways
Experimental Workflow and Signaling Pathways in Peritonitis Biomarker Research
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful execution of peritonitis biomarker studies requires carefully selected reagents and materials. The following table details essential solutions and their applications.
Table 3: Research Reagent Solutions for Peritonitis Biomarker Studies
| Reagent/Material | Function/Application | Specifications/Alternatives |
|---|---|---|
| Fecal Slurry Preparation | Standardized septic peritonitis induction [66] | Rat fecal slurry (0.75 mg/g) in 5% dextrose with 10% glycerol |
| CXC Chemokines | Enhance neutrophil recruitment to infection site [73] | CXCL1 (50 ng) + CXCL2 (500 ng) in saline, administered i.p. |
| Multiplex Immunoassay Kits | Simultaneous quantification of multiple cytokines [72] | MSD U-PLEX platform for IL-6, IL-10, MCP-1, TNF-α, etc. |
| Analytical Standards | Calibration and quality control for biomarker assays [75] | Recombinant cytokines with certificate of analysis |
| Peritoneal Lavage Solution | Recovery of peritoneal cells and bacteria [73] | Warm HBSS without calcium/magnesium |
| Culture Media | Bacterial quantification from peritoneal fluid [73] | 5% sheep blood agar plates for aerobic/anaerobic culture |
| Antibiotic Therapy | Mimic clinical sepsis management [66] | Imipenem (25 mg/kg) every 12 hours for 5 days post-CLP |
| Analgesia | Humane pain management post-procedure [71] | Buprenorphine (0.3 mg/kg) every 12 hours |
The systematic correlation of clinical scores with cytokine profiles and bacterial loads provides a robust framework for biomarker validation in mouse peritonitis models. By implementing standardized protocols, utilizing advanced analytical platforms, and adhering to fit-for-purpose validation principles, researchers can generate clinically relevant data that enhances the predictive value of preclinical sepsis research. The integrated approach outlined in this application note facilitates the development of qualified biomarkers that can accelerate therapeutic discovery and improve the translation of findings from bench to bedside.
Comparative Analysis of Model Strengths and Limitations
Peritonitis, the inflammation of the peritoneal membrane, represents a life-threatening condition frequently encountered in clinical settings, often leading to sepsis and multi-organ failure. Research into its complex pathophysiology and the development of novel therapeutics relies heavily on robust, reproducible animal models that accurately mimic the human condition. The mouse peritonitis model has emerged as a cornerstone in inflammatory response research, offering a vital platform for investigating immune mechanisms, host-pathogen interactions, and potential therapeutic interventions. This application note provides a comprehensive comparative analysis of the primary murine peritonitis models, detailing their specific strengths, limitations, and optimal applications to guide researchers in selecting the most appropriate system for their investigative goals. The content is framed within the context of a broader thesis on utilizing mouse peritonitis models for evaluating inflammatory responses, providing detailed protocols and data presentation suitable for researchers, scientists, and drug development professionals.
The most prevalent murine peritonitis models can be broadly categorized into three groups: polymicrobial sepsis models, monomicrobial infection models, and chemical induction models. Each system offers distinct advantages and is characterized by specific experimental parameters and outcomes.
Table 1: Comparative Overview of Major Mouse Peritonitis Models
| Model Type | Induction Method | Key Features | Inflammatory Response | Typical Mortality Rates | Primary Applications |
|---|---|---|---|---|---|
| Polymicrobial (CLP) | Surgical ligation and puncture of the cecum [71] [76] [77] | Reproduces polymicrobial sepsis; progressive, hyperdynamic then hypodynamic hemodynamics [77] | High levels of IL-6, TNFα, G-CSF, MCP-1; multi-organ damage [71] [77] | Standard-grade: 40% (7-day); High-grade: 71% (7-day) [77] | Gold standard for sepsis pathophysiology and antibiotic studies [76] [77] |
| Monomicrobial (E. coli) | Intraperitoneal injection of defined bacterial strain (e.g., E. coli ER2272, tdTomato-marked) [44] [25] | Controlled, reproducible bacterial load; modifiable with virulence enhancers [25] | Phagocyte recruitment (LPMs, SPMs); cytokine release (IL-6, TNFα) [44] | Strain and dose-dependent; ~100% with 10^7 CFU + mucin in BALB/c [25] | Leukocyte recruitment studies, phagocytosis, pathogen-specific immunity [44] |
| Chemical (LPS Endotoxemia) | Intraperitoneal injection of bacterial lipopolysaccharide (LPS) [45] [78] | Sterile inflammation; highly reproducible and tunable via dosage [45] [78] | Rapid cytokine storm (TNFα, IL-6, IL-1β); febrile response [45] | Typically low with sublethal doses; tunable with dose [45] | Acute inflammatory signaling, cytokine kinetics, fever response [45] |
| Chemical (Zymosan) | Intraperitoneal injection of zymosan (yeast cell wall particles) [78] | Sterile, granulomatous inflammation; sustained response [78] | Biphasic inflammation; neutrophil then monocyte infiltration [78] | Low in acute phase [78] | Chronic granulomatous inflammation, leukocyte migration studies [78] |
Table 2: Technical and Practical Considerations for Model Selection
| Characteristic | Cecal Ligation and Puncture (CLP) | Monomicrobial Injection | LPS Endotoxemia |
|---|---|---|---|
| Pathophysiological Relevance | High (mimics human sepsis) [77] | Moderate (dependent on pathogen) [25] | Low (sterile, non-infectious) [45] |
| Technical Difficulty | High (surgical procedure required) [71] [77] | Low (simple injection) [25] | Low (simple injection) [78] |
| Reproducibility | Moderate (variability with surgeon skill, ligation length, needle gauge) [71] [77] | High (precise CFU control) [44] [25] | Very High (precise LPS dose) [45] |
| Time Course of Inflammation | Prolonged (days), multi-phasic [77] | Acute (hours to days) [44] | Rapid, transient (peaks at 2-6 hours) [45] |
| Associated Organ Failure | Yes (renal, hepatic, cardiac) [71] [77] | Possible (dose and strain-dependent) [25] | Rare (with sublethal doses) [45] |
| Suitable for Drug Screening | Late-stage therapeutic validation [76] | Mid to high-throughput screening [79] | High-throughput screening [78] |
Detailed Experimental Protocols
High-Grade Cecal Ligation and Puncture (CLP)
The CLP procedure is the gold standard for modeling polymicrobial sepsis and is performed under aseptic conditions [77].
Materials:
- Anesthetized male C57BL/6J mice (8-10 weeks old)
- Isoflurane/oxygen anesthesia system
- Buprenorphine (0.3 mg/kg) for analgesia
- Sterile surgical instruments (forceps, scissors, needle holder)
- 3-0 silk suture
- 30-gauge needle
- Heating pad for postoperative recovery
Procedure:
- Anesthetize the mouse using inhaled isoflurane/oxygen and administer buprenorphine subcutaneously for preoperative analgesia.
- Secure the mouse in a supine position and shave the abdominal area. Disinfect the surgical site with alternating scrubs of povidone-iodine and 70% alcohol.
- Perform a 1-1.5 cm midline laparotomy to expose the abdominal cavity and carefully exteriorize the cecum.
- Ligate approximately two-thirds of the cecum distal to the ileocecal valve using 3-0 silk suture, ensuring not to occlude the intestinal lumen.
- Puncture the ligated cecum once with a 30-gauge needle through-and-through. Gently compress the cecum to extrude a small amount of fecal material (~1 mm) into the peritoneal cavity to confirm patency.
- Return the cecum to the abdominal cavity and close the abdominal wall and skin in two layers with simple interrupted sutures using 3-0 silk.
- Administer warmed, sterile saline (1 mL) subcutaneously for fluid resuscitation and place the animal on a heating pad until fully recovered from anesthesia.
- Administer buprenorphine (0.3 mg/kg) every 12 hours post-operatively for analgesia until the endpoint [71] [77].
Monitoring: Monitor animals every 4-8 hours for the first 48 hours and at least twice daily thereafter. Assess body weight, clinical disease index (CDI), and behavior. Euthanize mice exhibiting severe moribund state according to institutional guidelines [77].
Monomicrobial Peritonitis with E. coli
This protocol utilizes a clinical isolate of E. coli to induce a controlled bacterial peritonitis, ideal for studying pathogen-specific immune responses [44] [25].
Materials:
- E. coli ER2272 strain harboring pUC19-tdTomato construct (or other suitable strain)
- LB broth for culture
- Phosphate-buffered saline (PBS)
- Hog gastric mucin (Sigma-Aldrich)
- BALB/c or ICR mice (6-week-old, female)
- Spectrophotometer
Procedure:
- Inoculate E. coli into LB broth and culture overnight at 37°C with shaking to stationary phase.
- Centrifuge the bacterial culture, wash twice with PBS, and resuspend in PBS.
- Measure the absorbance at 600 nm and adjust the bacterial concentration to 1 × 10^8 CFU/mL using PBS, confirmed by serial dilution and plating.
- Prepare a 6% (w/v) solution of hog gastric mucin in PBS by stirring and mild heating until fully dissolved. Sterilize by autoclaving.
- Immediately before injection, mix equal volumes of the bacterial suspension (1 × 10^8 CFU/mL) and 6% hog gastric mucin to achieve a final inoculum of 1 × 10^7 CFU in 0.2 mL with 3% mucin.
- Inject the 0.2 mL inoculum intraperitoneally into isoflurane-anesthetized mice.
- Monitor survival every 12 hours and sacrifice surviving mice at 24 hours for sample collection, or as required by the experimental design [25].
Note: The use of hog gastric mucin is critical for enhancing bacterial virulence and establishing a robust infection with clinical isolates, as it impairs initial bacterial clearance by phagocytes [25].
Signaling Pathways and Experimental Workflows
The following diagrams visualize the core inflammatory signaling pathway in peritonitis and the generalized experimental workflow for model establishment and analysis.
Figure 1: Inflammatory Signaling Pathway in Murine Peritonitis. This diagram illustrates the core signaling cascade triggered by various insults (LPS, bacteria, tissue damage) in mouse peritonitis models, leading to both pro-inflammatory and compensatory anti-inflammatory responses, ultimately resulting in physiological changes and potential mortality [45] [71] [77].
Figure 2: Experimental Workflow for Murine Peritonitis Models. This flowchart outlines the generalized sequence of steps for establishing, monitoring, and analyzing data from mouse peritonitis studies, from model selection through to final data interpretation [44] [71] [25].
The Scientist's Toolkit: Key Research Reagent Solutions
The following table catalogues essential reagents and materials frequently employed in murine peritonitis research, as identified from the current literature.
Table 3: Essential Research Reagents for Murine Peritonitis Studies
| Reagent / Material | Function / Application | Example Usage in Context |
|---|---|---|
| Lipopolysaccharide (LPS) | Potent inflammogen; induces sterile, acute inflammation via TLR4 signaling [45] [78] | Modeling acute endotoxemia; studying early cytokine kinetics (TNFα, IL-6) and febrile responses [45]. |
| Hog Gastric Mucin | Virulence-enhancing agent; impedes phagocytic clearance of bacteria [25] | Co-injection with clinical bacterial isolates (e.g., carbapenem-resistant E. coli) to establish robust infection in monomicrobial models [25]. |
| Retinoic Acid (RA) | Immunomodulator; regulates macrophage function and population dynamics [44] | Studying enhancement of macrophage phagocytic capacity and modulation of LPM/SPM distribution during E. coli peritonitis [44]. |
| mPEG-PLGA Nanoparticles | Biocompatible, biodegradable drug delivery vehicle for controlled release [79] | Co-delivery of antibiotics with differing pharmacokinetics (e.g., colistin and niclosamide) to overcome resistant bacterial infections [79]. |
| Recombinant CXCR4/IL-10 MSCs | Cell-based therapy; potential enhanced homing (CXCR4) and anti-inflammatory (IL-10) activity [76] | Investigating advanced therapeutic strategies for modulating severe inflammation and promoting tissue repair in polymicrobial sepsis (CLP model) [76]. |
| Antibodies for Flow Cytometry (e.g., anti-CD11b, F4/80, MHC-II) | Identification and quantification of specific immune cell populations by surface marker expression [44] | Distinguishing between large peritoneal macrophages (LPMs: CD11b+, F4/80HIGH, MHC-IILOW) and small peritoneal macrophages (SPMs: CD11b+, F4/80LOW, MHC-IIHIGH) in lavage fluid [44]. |
The selection of an appropriate murine peritonitis model is paramount to the scientific validity and translational potential of research findings. The Cecal Ligation and Puncture model remains the most clinically relevant for studying polymicrobial sepsis due to its incorporation of a viable infectious focus and progressive pathophysiology mirroring human disease. In contrast, monomicrobial injection models offer superior reproducibility and are ideal for dissecting pathogen-specific immunity, while LPS-induced endotoxemia provides a highly controlled system for acute inflammatory signaling studies. Researchers must carefully weigh the strengths and limitations of each model—including pathophysiological relevance, technical complexity, and reproducibility—against their specific research objectives. The continued refinement of these models, coupled with advanced monitoring techniques and novel therapeutic agents, will undoubtedly enhance our understanding of peritoneal inflammation and foster the development of more effective treatments for this critical condition.
Histopathological and Functional Assessment of Organ Injury
Within the scope of a broader thesis on mouse peritonitis models for evaluating inflammatory responses, the precise assessment of organ injury is a critical pillar of research. This document provides detailed application notes and protocols for the histopathological and functional evaluation of organ damage in a neonatal mouse model of meconium peritonitis [9]. The provided methodologies are designed to offer researchers a standardized framework for quantifying inflammatory responses and multi-organ dysfunction, facilitating robust and reproducible data for therapeutic development.
Key Quantitative Findings in a Neonatal Mouse Meconium Peritonitis Model
Intraperitoneal administration of human meconium slurry (MS) to neonatal mice induces significant systemic inflammation and organ-specific pathology. The following tables summarize core quantitative data from this model, establishing key parameters for injury assessment.
Table 1: Survival and Model Characterization Data [9]
| Parameter | Findings | Experimental Details |
|---|---|---|
| Established Lethal Dose (LD40) | 200 µL/body weight | Dose was determined in 4-day-old mouse pups. |
| Mortality Rate | Dose-dependent | Monitored for up to 7 days post-MS administration. |
| Pathogenic Agent | Primarily digestive enzymes | Survival improved with heat inactivation of MS; antibiotic treatment was ineffective. |
| Systemic Response | Distinct from bacterial sepsis | Confirmed via comparison with a non-surgical neonatal sepsis model. |
Table 2: Hematological, Biochemical, and Inflammatory Marker Profiles [9]
| Assessment Category | Specific Parameter | Observation |
|---|---|---|
| Hematology | Complete Blood Count (CBC) | Substantial hematological abnormalities observed. |
| Serum Biochemistry | Liver and Kidney Function Markers | Significant hepatorenal abnormalities confirmed. |
| Inflammatory Gene Expression | Innate and Adaptive Immune Response Genes | Marked increase in pro-inflammatory gene expression (e.g., IL-6) in liver tissue. |
Experimental Protocols
This section outlines detailed, sequential protocols for inducing peritonitis and assessing subsequent organ injury.
Objective: To generate a sterile chemical peritonitis in neonatal mice via intraperitoneal injection of human meconium slurry. Materials:
- Animals: 4-day-old mouse pups (immunologically equivalent to human preterm infants).
- Human Meconium Slurry (MS): Prepared aseptically from fresh meconium from healthy term infants, suspended in PBS (500 mg/mL), and stored at -80°C. Sterility must be confirmed before use.
- Equipment: Sterile syringes, 23-gauge needles, cryovials, and a warming pad.
Procedure:
- MS Preparation: Thaw an aliquot of stock MS at room temperature. Vortex thoroughly to ensure a homogenous suspension.
- Animal Preparation: Label pups for identification. Keep them on a warming pad throughout the procedure to maintain body temperature.
- Administration: Administer the established LD40 dose of 200 µL MS intraperitoneally to each pup.
- Post-Procedural Care: Return pups to their mothers. Monitor health and survival daily for 7 days. Record body weight daily, beginning 24 hours post-injection.
Objective: To evaluate hematological and serum biochemical changes as indicators of systemic inflammation and organ dysfunction. Materials: Lithium heparin capillary blood collection tubes, veterinary hematology analyzer, automated biochemical analyzer.
Procedure:
- Blood Collection: At 24 hours post-MS induction, sacrifice pups via decapitation under room air. Immediately collect 30–80 µL of blood from the trunk into lithium heparin capillary tubes.
- Sample Pooling: Pool blood from 2-3 pups to obtain sufficient volume for analysis.
- Hematology: Perform a Complete Blood Count (CBC) with differential using a veterinary hematology analyzer.
- Serum Biochemistry: Submit plasma for analysis of liver (e.g., AST, ALT, bilirubin) and kidney (e.g., creatinine, BUN) function markers.
Objective: To quantify the expression of key immunomodulatory genes in the liver. Materials: RNA extraction kit (e.g., RNAeasy Mini Kit), cDNA synthesis kit (e.g., RT2 First Strand Kit), Mouse Innate & Adaptive Immune Responses PCR Array, real-time PCR system.
Procedure:
- Tissue Collection: At 6 hours post-MS induction, sacrifice pups. Immediately harvest the liver, snap-freeze pieces (approx. 5x5x1 mm) in liquid nitrogen, and store at -80°C.
- RNA Extraction: Extract total RNA from liver tissue according to the standard protocol of the RNA extraction kit.
- cDNA Synthesis: Synthesize cDNA from the extracted RNA using the cDNA synthesis kit.
- Real-Time PCR: Perform real-time PCR on the prepared cDNA using the pre-configured PCR array plate and SYBR Green master mix.
- Data Analysis: Calculate fold changes in gene expression using the ΔΔCt method, comparing the MS group to vehicle-treated controls.
Visualizing the Experimental Workflow and Inflammatory Pathway
The following diagrams, generated using Graphviz DOT language, illustrate the core experimental workflow and the key inflammatory signaling pathway implicated in meconium peritonitis.
Experimental Workflow for Organ Injury Assessment
Key Inflammatory Pathway in Meconium Peritonitis
The Scientist's Toolkit: Essential Research Reagents
The following table details key reagents and materials required to execute the described meconium peritonitis model and organ injury assessments.
Table 3: Research Reagent Solutions for Mouse Peritonitis Studies
| Reagent / Material | Function / Application | Example / Note |
|---|---|---|
| Human Meconium Slurry | Induces sterile chemical peritonitis. | Prepared from healthy term infants; sterile stock is critical [9]. |
| Phosphate-Buffered Saline (PBS) | Diluent for preparing meconium slurry. | Standard, sterile, without calcium or magnesium. |
| RNAeasy Mini Kit | Total RNA extraction from tissue samples (e.g., liver). | Ensures high-quality RNA for downstream gene expression analysis [9]. |
| PCR Array (Mouse Innate & Adaptive Immune Response) | Profiles expression of 84 immune-related genes. | Provides a focused, quantitative view of the inflammatory response [9]. |
| Lithium Heparin Capillary Tubes | Collection of small-volume blood samples from neonatal mice. | Prevents coagulation for hematological and biochemical analysis [9]. |
| LysM-EGFP Mice | Enables in vivo tracking of circulating myeloid cells (neutrophils) during peritonitis. | Useful for monitoring immune cell dynamics via intravital flow cytometry [17]. |
| Sparstolonin B (SsnB) | Natural compound with dual antibacterial/anti-inflammatory activity. | Example therapeutic for validating the model; inhibits TLR-2/4 signaling and MRSA [80]. |
| Anti-CD64 / Anti-Ly6G Antibodies | Flow cytometry staining to identify and characterize neutrophils. | Used for ex vivo validation of immune cell populations [17]. |
Sepsis, a life-threatening organ dysfunction caused by a dysregulated host response to infection, remains a leading cause of mortality worldwide. Murine models of peritonitis, particularly lipopolysaccharide (LPS)-induced peritonitis, are extensively used to investigate the pathophysiology of sepsis and evaluate potential therapeutic interventions. However, a significant translational gap exists between findings from animal models and clinical applications in human patients. This application note outlines standardized protocols and analytical frameworks for integrating murine transcriptomic data with human sepsis profiles, enabling researchers to validate findings from mouse models in clinically relevant contexts and identify therapeutic targets with enhanced translational potential.
The systemic inflammatory response in sepsis involves complex molecular mechanisms that can be effectively modeled using LPS-induced peritonitis in mice. Intraperitoneal administration of LPS triggers a robust immune activation characterized by significant transcriptomic alterations in both local peritoneal tissues and systemic circulation [5] [35]. By employing cross-species validation approaches, particularly through single-cell RNA sequencing data from human sepsis patients, researchers can now determine which molecular pathways identified in mouse models are conserved in human sepsis, thereby increasing the predictive value of preclinical findings.
Quantitative Data Synthesis from Murine Transcriptomic Studies
Comprehensive transcriptomic profiling of murine peritonitis models has revealed consistent patterns of differential gene expression and pathway activation across multiple studies. The table below summarizes key quantitative findings from recent investigations:
Table 1: Transcriptomic Alterations in Murine Peritonitis Models
| Experimental Model | Tissue Analyzed | Differentially Expressed Genes (DEGs) | Key Upregulated Pathways | Key Downregulated Pathways | Identified Hub Genes/Proteins |
|---|---|---|---|---|---|
| LPS-induced peritonitis (10 mg/kg, i.p.) [5] | Blood | 290 DEGs (242 up, 48 down) | NOD-like receptor signaling, Toll-like receptor signaling, Apoptosis, Phagocytosis | Th1/Th2 cell differentiation, T cell receptor signaling | LDLR, FNBP1L, SNX18, FAM20C, INPP5F, PACSIN1, ZAP70, SYNJ2 |
| LPS-induced peritonitis (10 mg/kg, i.p.) [35] | Peritoneum | 4201 DEGs (1759 up, 2442 down) | Inflammatory response, TLR4 signaling | Various cellular developmental processes | Validated through TAK 242 (TLR4 inhibitor) response |
| E. coli-induced intra-abdominal sepsis [81] | Peritoneal cells | 5244 DEGs across time points | Early: Antigen presentation, cellular development; Late: Cell death pathways | Variable by temporal stage | PLAGL2, EBF1, TCF7, KLF10, SBNO2 |
Integration of these datasets reveals conserved inflammatory pathways across different murine sepsis models, with TLR4 signaling representing a central node in the inflammatory response. The identification of hub genes across studies provides high-value targets for further validation in human systems.
Experimental Protocols
Protocol 1: Murine LPS-Induced Peritonitis Model and Blood Transcriptomic Analysis
Materials and Reagents
- Male C57BL/6 mice (6-8 weeks old)
- Lipopolysaccharide (LPS) from E. coli (serotype O111:B4)
- Phosphate-buffered saline (PBS)
- RNA stabilization solution (RNAlater or equivalent)
- RNA extraction kit (e.g., RNeasy Mini Kit)
- Equipment for bulk RNA sequencing
Experimental Procedure
- Animal Preparation: Acclimate mice for at least 7 days under standard housing conditions (12-h light/dark cycle, 20-22°C, ad libitum access to food and water).
- LPS Administration: Prepare LPS solution at 1 mg/mL in sterile PBS. Administer LPS intraperitoneally at 10 mg/kg body weight using sterile technique [5].
- Control Group: Administer equivalent volume of sterile PBS to control animals.
- Blood Collection: At designated time points (typically 6-24 hours post-LPS administration), euthanize animals and collect blood via cardiac puncture.
- RNA Stabilization: Mix blood samples immediately with RNA stabilization solution according to manufacturer's instructions.
- RNA Extraction: Isolate total RNA using commercial kits following manufacturer's protocols. Assess RNA quality using Agilent Bioanalyzer or similar (RIN > 8.0 recommended).
- Library Preparation and Sequencing: Prepare RNA sequencing libraries using TruSeq Stranded mRNA or similar kit. Sequence on Illumina platform to achieve minimum of 30 million reads per sample.
- Bioinformatic Analysis:
- Quality control of raw reads (FastQC)
- Alignment to reference genome (STAR aligner)
- Quantification of gene expression (featureCounts)
- Identification of DEGs (DESeq2, edgeR)
- Functional enrichment analysis (clusterProfiler)
Note: All animal procedures must be approved by appropriate Institutional Animal Care and Use Committee and follow relevant guidelines.
Protocol 2: Cross-Species Validation Using Human Single-Cell RNA Sequencing Data
Materials and Reagents
- Publicly available single-cell RNA sequencing datasets from human sepsis patients (e.g., from GEO database)
- Computational resources for single-cell analysis (R/Python environment)
- Single-cell analysis packages (Seurat, Scanpy)
Computational Procedure
Data Acquisition:
- Identify and download relevant single-cell RNA sequencing datasets of human sepsis patients. Key search terms: "sepsis scRNA-seq," "peritonitis single-cell," "human sepsis PBMC" [5].
- Include datasets with appropriate controls (healthy individuals) and clinical metadata.
Data Preprocessing:
- Quality control filtering (remove cells with high mitochondrial content, low feature counts)
- Normalization and scaling using standard methods (SCTransform for Seurat)
- Integration of multiple datasets using harmony or similar integration methods
Cell Type Identification:
- Cluster cells using graph-based clustering methods
- Annotate cell types using canonical marker genes
- Pay particular attention to immune cell populations (monocytes, T cells, B cells)
Cross-Species Gene Expression Validation:
- Project murine hub genes to human orthologs using biomaRt or similar tools
- Calculate module scores for hub gene sets in human single-cell data
- Compare expression patterns across cell types and between sepsis patients and controls
- Validate cell-type specific expression patterns (e.g., ZAP70 in T cells, LDLR in monocytes) [5]
Clinical Correlation Analysis:
- Correlate hub gene module scores with clinical parameters (SOFA score, APACHE-II)
- Assess ability of gene signatures to distinguish sepsis subtypes and predict outcomes
Signaling Pathways and Experimental Workflows
Cross-Species Transcriptomic Integration Workflow
The following diagram illustrates the comprehensive workflow for generating and validating murine transcriptomic findings in human sepsis contexts:
Molecular Pathways in LPS-Induced Peritonitis
The diagram below details key signaling pathways activated in LPS-induced peritonitis and their cross-species relevance:
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Reagents for Murine-Human Sepsis Transcriptomic Studies
| Reagent/Material | Specifications | Application | Key Considerations |
|---|---|---|---|
| Lipopolysaccharide (LPS) | E. coli serotype O111:B4; 10 mg/kg in PBS | Induction of sterile peritonitis in mice | Dose optimization required for specific mouse strains; sterile preparation critical [5] [35] |
| TAK-242 (Resatorvid) | TLR4-specific inhibitor; 3 mg/kg | Validation of TLR4-dependent mechanisms in murine models | Pre-treatment (30 min before LPS) demonstrates TLR4-specific effects [35] |
| RNA Stabilization Reagents | RNAlater or similar commercial formulations | Preservation of RNA integrity in blood and tissues | Immediate mixing with blood samples essential for quality transcriptomics [5] |
| Bulk RNA Sequencing Kits | Illumina TruSeq Stranded mRNA Kit | Transcriptome profiling from murine samples | Input RNA quality critical (RIN >8.0); minimum 30M reads/sample recommended [5] |
| Single-Cell RNA Sequencing Platforms | 10X Genomics Chromium System | Human patient profiling for cross-species validation | Requires fresh cells; cell viability >90% essential for quality data [5] |
| Bioinformatic Tools | DESeq2, Seurat, clusterProfiler | Differential expression and pathway analysis | Consistent parameter settings across analyses enables cross-study comparisons |
Discussion and Implementation Notes
The integration of murine transcriptomic data with human sepsis profiles represents a powerful approach for bridging the translational gap in sepsis research. The protocols outlined herein provide a standardized framework for generating mechanistically relevant data in mouse models and validating their clinical significance using human single-cell sequencing data.
Key considerations for successful implementation include:
Temporal Dynamics: Transcriptomic changes in both murine models and human sepsis are highly time-dependent. Researchers should carefully consider timing of sample collection in relation to disease progression. In murine models, early time points (6-24 hours) typically capture peak inflammatory responses [5] [81].
Compartment-Specific Responses: Significant differences exist between local (peritoneal) and systemic (blood) transcriptomic profiles in response to intra-abdominal infection [35] [81]. The choice of tissue for analysis should align with research questions, with blood transcriptomics offering greater clinical translatability.
Model Selection: Different murine sepsis models (LPS, CLP, fecal slurry) produce distinct transcriptomic signatures [82] [66]. LPS-induced peritonitis provides a standardized, highly reproducible model for studying specific inflammatory pathways, while polymicrobial models may better reflect clinical heterogeneity.
Age Considerations: Aging significantly impacts host response to sepsis [66]. Most murine studies utilize young animals (6-8 weeks), while sepsis predominantly affects older humans. Incorporating aged mice into study designs enhances translational relevance.
The cross-species validation approach described here has demonstrated clinical utility, with hub genes identified in murine models showing conserved expression patterns in human sepsis patients and correlation with disease severity scores such as SOFA and APACHE-II [5] [83]. This framework not only validates preclinical findings but also identifies promising therapeutic targets with enhanced potential for clinical translation.
For comprehensive research design, researchers should consult original citations and consider multi-center validation approaches to enhance reproducibility and clinical relevance of findings.
Mouse models of peritonitis are indispensable tools in sepsis and inflammatory response research, bridging the gap between basic scientific discovery and clinical application. These experimental systems provide a controlled environment for elucidating the complex mechanisms driving systemic inflammation and for evaluating novel therapeutic strategies. This application note presents three case studies demonstrating successful preclinical research using mouse peritonitis models, highlighting detailed methodologies, key findings with clinical relevance, and experimental protocols. By integrating quantitative data analysis, pathway visualization, and reagent specifications, we provide a comprehensive resource for researchers aiming to design robust translational studies in inflammatory disease research.
Case Study 1: Transcriptomic Profiling and Hub Gene Identification in LPS-Induced Peritonitis
Experimental Protocol
Objective: To characterize the systemic transcriptomic changes and identify key hub genes in a lipopolysaccharide (LPS)-induced murine peritonitis model.
Materials:
- Animals: Male C57BL/6 mice (6-8 weeks old)
- Inducing Agent: LPS from Escherichia coli (10 mg/kg)
- Sample: Blood collected 6 hours post-injection (n=6 per group)
- Controls: Phosphate-buffered saline (PBS)-injected mice
Methodology:
- Model Induction: Administer LPS (10 mg/kg) via intraperitoneal (i.p.) injection.
- Sample Collection: Collect blood samples 6 hours post-injection in PAXgene Blood RNA Tubes.
- RNA Sequencing: Perform bulk RNA sequencing on Illumina platform.
- Bioinformatic Analysis:
- Identify differentially expressed genes (DEGs) with threshold of |log2FC| > 1 and adjusted p-value < 0.05.
- Conduct functional enrichment analysis using Gene Ontology (GO) and Kyoto Encyclopedia of Genes and Genomes (KEGG).
- Construct protein-protein interaction (PPI) network using STRING database.
- Identify hub genes via cytoHubba plugin in Cytoscape.
- Validation: Integrate four independent public single-cell RNA-sequencing datasets from human sepsis patients.
Results and Data Analysis
The transcriptomic analysis revealed significant alterations in the blood of mice with LPS-induced peritonitis. The key quantitative findings are summarized in the table below:
Table 1: Transcriptomic Profile of LPS-Induced Peritonitis
| Analysis Parameter | Result | Clinical Relevance |
|---|---|---|
| Differentially Expressed Genes | 290 total (242 upregulated, 48 downregulated) | Conserved expression patterns in human sepsis patients |
| Activated Pathways | NOD-like receptor, Toll-like receptor, Apoptosis, Phagocytosis | Associated with human systemic inflammatory response |
| Inhibited Pathways | Th1/Th2 cell differentiation, T cell receptor signaling | Reflects immunosuppression phase in human sepsis |
| Identified Hub Proteins | LDLR, FNBP1L, SNX18, FAM20C, INPP5F, PACSIN1, ZAP70, SYNJ2 | Potential diagnostic biomarkers/therapeutic targets |
| Clinical Validation | Module score significantly distinguished sepsis patients from controls (p < 0.05) | Strong clinical relevance for patient stratification |
The eight identified hub proteins demonstrated structural stability in molecular dynamics simulations, maintaining conformation over 300 ns. Crucially, cross-species validation confirmed that these hub genes showed cell-type-specific expression patterns in human sepsis patients, with ZAP70 downregulation in T cells and LDLR upregulation in monocytes, highlighting their potential clinical relevance.
Signaling Pathway Diagram
The following diagram illustrates the key signaling pathways activated in LPS-induced peritonitis, highlighting the interconnected inflammatory response:
Case Study 2: Therapeutic Efficacy of Vioprolide A in Inflammatory Pain
Experimental Protocol
Objective: To evaluate the antinociceptive effects of the mRNA translation inhibitor vioprolide A in murine models of inflammatory pain, including zymosan-induced peritonitis.
Materials:
- Animals: C57BL/6N mice (8-12 weeks old, both sexes)
- Peritonitis Induction: Zymosan A suspension (2 mg/mL in PBS, i.p. injection)
- Therapeutic: Vioprolide A (0.3 mg/kg, subcutaneous administration)
- Controls: Vehicle (1% DMSO in 0.9% NaCl)
Methodology:
- Pretreatment: Administer vioprolide A (0.3 mg/kg) or vehicle subcutaneously 16 hours prior to peritonitis induction.
- Model Induction: Induce peritonitis via i.p. injection of zymosan A (0.5 mL of 2 mg/mL suspension).
- Pain Assessment: Evaluate visceral inflammatory hypersensitivity at 5 hours post-zymosan using automated dynamic weight bearing (DWB) device.
- Data Analysis: Calculate frontpaw to hindpaw ratio; reduced ratio indicates visceral pain.
- Pharmacokinetics: Measure plasma and brain levels of vioprolide A in separate cohort.
Results and Data Analysis
Vioprolide A demonstrated significant antinociceptive effects in the zymosan-induced peritonitis model. The quantitative outcomes are summarized below:
Table 2: Therapeutic Efficacy of Vioprolide A in Murine Pain Models
| Parameter | Vioprolide A Group | Vehicle Control Group | Significance |
|---|---|---|---|
| Visceral Inflammatory Hypersensitivity | Significantly alleviated | Persistent hypersensitivity | p < 0.05 |
| Somatic Inflammatory Hypersensitivity | Attenuated in dose-dependent manner | Persistent hypersensitivity | p < 0.05 at 1-3 mg/kg |
| Established Hypersensitivities | No effect | No improvement | Not significant |
| Brain Penetrance | Not detected | Not applicable | Short plasma half-life |
| NOP14 Expression | Expressed in sensory neurons | Expressed in sensory neurons | Target engagement confirmed |
The study demonstrated that vioprolide A pretreatment significantly alleviated visceral inflammatory hypersensitivity during zymosan-induced peritonitis. However, treatment after hypersensitivity establishment showed no effect, indicating the importance of intervention timing. Pharmacokinetic analysis revealed limited brain penetration, suggesting a peripheral mechanism of action.
Case Study 3: Mesenchymal Stromal Cell Therapy in Polymicrobial Sepsis
Experimental Protocol
Objective: To investigate the therapeutic potential of human adipose-derived mesenchymal stromal cells (hASCs) in a murine model of polymicrobial sepsis induced by cecal ligation and puncture (CLP).
Materials:
- Animals: C57BL/6 mice
- Sepsis Model: Cecal ligation and puncture (CLP) surgery
- Therapeutic: Wild-type hASCs and modified hASCs (transiently expressing CXCR4 and IL-10)
- Cell Dose: 1×10^6 cells per animal, administered via peritoneal injection
- Controls: Sham-operated mice and CLP mice without cell therapy
Methodology:
- Sepsis Induction:
- Anesthetize mice with isoflurane.
- Perform midline laparotomy to expose the cecum.
- Ligate approximately 50-75% of the cecum with 3-0 silk suture.
- Puncture the ligated cecum once with a 21-gauge needle.
- Express small amount of fecal material through the puncture.
- Return cecum to abdomen and close incision.
- Cell Therapy: Administer 1×10^6 hASCs (wild-type or modified) in 100 μL saline via peritoneal injection post-surgery.
- Supportive Care: Provide fluid resuscitation and analgesia to all mice.
- Monitoring: Assess weight loss, behavior, and mortality daily for 11 days.
- Endpoint Analyses: Collect peritoneal fluid and blood for cytokine measurement and microbiological analysis at days 5 and 11.
Results and Data Analysis
hASC therapy demonstrated significant benefits in the polymicrobial sepsis model, with key findings summarized below:
Table 3: Therapeutic Outcomes of hASC Therapy in Murine Sepsis
| Outcome Measure | Control Group | Wild-type hASCs | Modified hASCs |
|---|---|---|---|
| 24-Hour Mortality | 8% | 8% | 8% |
| Overall Mortality | 3/group | 2/group | 1/group |
| Weight Loss | Progressive decrease | Max 10% loss with recovery | Similar recovery pattern |
| Behavioral Score | Severe impairment | Mild difficulty for 2-3 days | Mild difficulty for 2-3 days |
| Blood Culture | Positive for pathogens | No growth | No growth |
| Anti-inflammatory Cytokines | No significant change | Increased IL-4 | Increased IL-10 |
| Pro-inflammatory Cytokines | Elevated IL-1β, IL-12, IFN-γ, TNF-α | Decreased IL-12 | Decreased IL-12 |
Both wild-type and modified hASCs effectively mitigated sepsis severity, with no significant differences between cell types. Treated animals showed improved weight recovery, behavioral scores, and bacterial clearance compared to controls. Cytokine profiling demonstrated that hASC therapy modulated the inflammatory response, enhancing anti-inflammatory cytokines while reducing specific pro-inflammatory mediators.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Mouse Peritonitis Models
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Peritonitis Inducing Agents | LPS (E. coli), Zymosan A, Cecal slurry, Live bacteria | Initiate controlled inflammatory response of varying severity |
| Surgical Sepsis Models | Cecal ligation and puncture (CLP) equipment | Reproduce polymicrobial sepsis with tissue necrosis |
| Therapeutic Compounds | Vioprolide A, Monoclonal antibodies, Mesenchymal stromal cells | Evaluate novel treatment efficacy and mechanisms |
| Analgesics & Anesthetics | Buprenorphine, Isoflurane | Ensure humane animal treatment per ethical guidelines |
| Supportive Care Reagents | Ringer's lactate, Antibiotics (imipenem, piperacillin-tazobactam) | Mimic clinical standard of care and improve model validity |
| Sample Collection | PAXgene Blood RNA Tubes, EDTA tubes, Peritoneal lavage kit | Preserve molecular and cellular integrity for analysis |
| Analysis Kits | ELISA cytokine kits, RNA sequencing kits, Bacterial culture media | Quantify inflammatory markers and pathogen load |
Experimental Workflow Diagram
The following diagram outlines a generalized workflow for therapeutic evaluation in mouse peritonitis models:
Mouse peritonitis models continue to provide valuable platforms for evaluating novel therapeutics and understanding inflammatory pathogenesis. The case studies presented herein demonstrate how carefully designed preclinical studies using these models can generate clinically relevant findings, from identifying novel biomarker candidates to evaluating promising therapeutic interventions. By adhering to standardized protocols, incorporating relevant supportive care, and implementing robust endpoint analyses, researchers can enhance the translational potential of their findings, ultimately contributing to improved treatments for sepsis and inflammatory disorders.
Conclusion
Mouse peritonitis models remain an indispensable component of inflammatory disease and sepsis research. A deep understanding of their foundational pathophysiology, coupled with meticulous methodological execution and robust validation, is paramount for generating reliable and translatable data. Future directions must prioritize the widespread adoption of standardized protocols, such as those developed by multi-laboratory consortia, and the integration of clinically relevant factors like aging and supportive care. By systematically addressing current challenges in reproducibility and validation, these refined models will significantly accelerate the development of novel anti-inflammatory and anti-sepsis therapies, ultimately bridging the persistent gap between promising preclinical results and successful clinical application.
References
- 1. Peritonitis - Symptoms and causes [https://www.mayoclinic.org/diseases-conditions/peritonitis/symptoms-causes/syc-20376247]
- 2. Peritonitis: What it is, Symptoms, Causes & Treatment [https://my.clevelandclinic.org/health/diseases/17831-peritonitis]
- 3. IKZF1 exacerbates the inflammatory response by ... [https://pubmed.ncbi.nlm.nih.gov/41019036/]
- 4. IKZF1 exacerbates the inflammatory response by ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1600903/full]
- 5. Insights into transcriptomic changes in blood of a mouse ... [https://www.sciencedirect.com/science/article/abs/pii/S0041008X25003990]
- 6. Peritoneal Lavage With Low GDP Neutral pH PD Solution ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12411685/]
- 7. Experimental peritonitis [https://bio-protocol.org/exchange/minidetail?id=9627005&type=30]
- 8. A Focus on Inflammatory and Bacterial Biomarkers in ... [https://www.mdpi.com/2073-4409/14/21/1653]
- 9. A neonatal mouse model of meconium peritonitis ... [https://www.nature.com/articles/s41390-024-03470-3]
- 10. The NLRP3 Inflammasome: An Overview of Mechanisms of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6651423/]
- 11. An update on the regulatory mechanisms of NLRP3 ... [https://www.nature.com/articles/s41423-021-00670-3]
- 12. The NLRP3 Inflammasome Pathway: A Review of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9226403/]
- 13. The mechanism of NLRP3 inflammasome activation and its ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2022.1109938/full]
- 14. Cell type-specific roles of NLRP3, inflammasome ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2023.1214289/full]
- 15. Mechanisms underlying the involvement of peritoneal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11693514/]
- 16. Mechanisms of Peritoneal Fibrosis: Focus on Immune Cells ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2021.607204/full]
- 17. Monitoring Circulating Myeloid Cells in Peritonitis with an ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11351726/]
- 18. A neonatal mouse model of meconium peritonitis generated using... [https://www.nature.com/articles/s41390-024-03470-3?error=cookies_not_supported]
- 19. The mouse peritonitis model: present and future use [https://pubmed.ncbi.nlm.nih.gov/8335524/]
- 20. The Mouse Peritonitis/Sepsis Model [https://www.sciencedirect.com/science/article/abs/pii/B9780127753904501536]
- 21. Peritonitis Models [https://www.creative-bioarray.com/services/peritonitis-models.htm]
- 22. Mouse model of peritonitis [https://bio-protocol.org/exchange/minidetail?id=7940095&type=30]
- 23. Mild peritonitis mice model assay [https://bio-protocol.org/exchange/minidetail?id=2126907&type=30]
- 24. Mouse Peritonitis Sepsis Model of MRSA Infection [https://noblelifesci.com/mouse-peritonitis-sepsis-model/]
- 25. Establishment of Experimental Murine Peritonitis Model ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5382051/]
- 26. Establishment of Experimental Murine Peritonitis Model ... [https://icjournal.org/DOIx.php?id=10.3947/ic.2017.49.1.57]
- 27. IKZF1 exacerbates the inflammatory response by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12463629/]
- 28. Identification of sex- and inflammation-associated ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1670112/full]
- 29. Development and characterization of a fecal-induced ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10352196/]
- 30. Current Protocols in Immunology: Cecal Ligation and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3058382/]
- 31. Cecal Ligation Puncture Procedure - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC3339843/]
- 32. Impact of age on the host response to sepsis in a murine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10923763/]
- 33. A robust scoring system to evaluate sepsis severity in an ... [https://bmcresnotes.biomedcentral.com/articles/10.1186/1756-0500-7-233]
- 34. 2.16. LPS-Induced Peritonitis In Vivo Model [https://bio-protocol.org/exchange/minidetail?id=7331291&type=30]
- 35. Transcriptomics Changes in the Peritoneum of Mice with ... [https://www.mdpi.com/1422-0067/22/23/13008]
- 36. Forsythoside A Modulates Zymosan-Induced Peritonitis in ... [https://www.mdpi.com/1420-3049/23/3/593]
- 37. Zymosan Induced Peritonitis [https://www.inotiv.com/solutions/zymosan-induced-peritonitis]
- 38. Zymosan-Induced Peritonitis - an overview [https://www.sciencedirect.com/topics/medicine-and-dentistry/zymosan-induced-peritonitis]
- 39. Peritonitis-induced peritoneal injury models for research in ... [https://rrtjournal.biomedcentral.com/articles/10.1186/s41100-017-0100-4]
- 40. Apoptosis inhibitor of macrophage ameliorates fungus ... [https://www.nature.com/articles/s41598-017-06824-6]
- 41. The mRNA Translation Inhibitor Vioprolide A Prevents ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12345401/]
- 42. 🐈🌟FIP Treatment Update - New guidance ... [https://www.facebook.com/kittencoalition/posts/fip-treatment-update-new-guidance-from-international-cat-care-july-2025-shows-th/1108010811513404/]
- 43. Spectrum of care approach to animal shelter management ... [https://www.frontiersin.org/journals/veterinary-science/articles/10.3389/fvets.2025.1570267/full]
- 44. Retinoic acid modulates peritoneal macrophage function ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1545720/full]
- 45. Mathematical model of the inflammatory response to acute ... [https://www.nature.com/articles/s41540-024-00473-y]
- 46. FIP Treatment Protocols [https://www.fipvetguide.com/protocols]
- 47. An improved mouse model of sepsis based on intraperitoneal injections of the enriched culture of cecum slurry - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0024320524001735]
- 48. An improved mouse model of sepsis based on intraperitoneal injections of the enriched culture of cecum slurry - PubMed [https://pubmed.ncbi.nlm.nih.gov/38527668/]
- 49. Whole-mount immunofluorescence imaging and isolation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9898286/]
- 50. Analysis of local and systemic inflammatory induced by... responses [https://pubmed.ncbi.nlm.nih.gov/11759107/]
- 51. Identifying important parameters in the inflammatory process with... [https://journals.plos.org/ploscompbiol/article?id=10.1371/journal.pcbi.1007172]
- 52. Release Details [https://ir.monterosatx.com/news-releases/news-release-details/monte-rosa-therapeutics-presents-preclinical-data-aha-scientific]
- 53. Simplifying Antibiotic Management of Peritonitis in APD [https://pmc.ncbi.nlm.nih.gov/articles/PMC12383089/]
- 54. Outcome of Peritonitis in Automated Peritoneal Dialysis [https://www.sciencedirect.com/science/article/pii/S259005952500189X]
- 55. A neonatal mouse model of meconium peritonitis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12119350/]
- 56. A hollow fiber infection model to study intracellular and ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11930174/]
- 57. Improving pain management for murine orthotopic xenograft ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12575361/]
- 58. Guidelines on Anesthesia and Analgesia in Mice - Research A-Z [https://az.research.umich.edu/animalcare/guidelines/guidelines-anesthesia-and-analgesia-mice/]
- 59. Assessing the effects of fluids and antibiotics in an acute ... [https://f1000research.com/articles/14-472]
- 60. Development and characterization of a fecal-induced ... [https://icm-experimental.springeropen.com/articles/10.1186/s40635-023-00533-3]
- 61. Intravenous fluid therapy: essential components and key ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12321458/]
- 62. Systemic administration of analgesic buprenorphine, but ... [https://www.sciencedirect.com/science/article/pii/S2772976125002016]
- 63. A robust scoring system to evaluate sepsis severity in an ... [https://pubmed.ncbi.nlm.nih.gov/24725742/]
- 64. Body temperature and mouse scoring systems as ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6063809/]
- 65. Improving the Research in Experimental Sepsis Mouse Model [https://pmc.ncbi.nlm.nih.gov/articles/PMC8814713/]
- 66. Impact of age on the host response to sepsis in a murine ... [https://icm-experimental.springeropen.com/articles/10.1186/s40635-024-00609-8]
- 67. Identification of sex- and inflammation-associated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12589825/]
- 68. The obesity paradox in murine sepsis models: a systematic ... [https://www.ait-journal.com/The-obesity-paradox-in-murine-sepsis-models-a-systematic-review-and-meta-analysis,207612,0,2.html]
- 69. Optimizing preclinical models of ageing for translation to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11671336/]
- 70. A Focus on Inflammatory and Bacterial Biomarkers in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12609305/]
- 71. An optimized peritonitis-induced ACLF model that ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12180834/]
- 72. Beyond ELISA: the future of biomarker validation [https://www.drugtargetreview.com/article/154316/beyond-elisa-the-future-of-biomarker-validation/]
- 73. Early Enhanced Local Neutrophil Recruitment in Peritonitis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5540308/]
- 74. Use of Biomarkers in Drug Development for Regulatory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12489174/]
- 75. Why is Biomarker Assay Validation Different from that of ... [https://link.springer.com/article/10.1208/s12248-025-01135-5]
- 76. Study of the Effect of Wild-Type and Transiently Expressing ... [https://www.mdpi.com/1422-0067/25/1/520]
- 77. Precision Profiling of Disease Progression in Murine ... [https://www.mdpi.com/1422-0067/26/20/9954]
- 78. Models in vivo and in vitro for the study of acute and ... [https://www.sciencedirect.com/science/article/abs/pii/S1567576924008129]
- 79. Amphiphilic mPEG-PLGA copolymer nanoparticles co- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12037906/]
- 80. Sparstolonin B attenuates MRSA-induced wound and ... [https://www.nature.com/articles/s41598-025-90710-z]
- 81. Transcriptomic analysis of peritoneal cells in a mouse model ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3621573/]
- 82. Transcriptional responses in different mouse models of ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1556392/full]
- 83. Increased peritoneal B1-like cells during acute phase of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11231613/]