Neuroinflammation in Neurodegeneration: Mechanisms, Biomarkers, and Therapeutic Strategies
This article provides a comprehensive analysis of the pivotal role inflammatory responses play in the pathogenesis of neurodegenerative diseases, including Alzheimer's disease, Parkinson's disease, and Amyotrophic Lateral Sclerosis.
Neuroinflammation in Neurodegeneration: Mechanisms, Biomarkers, and Therapeutic Strategies
Abstract
This article provides a comprehensive analysis of the pivotal role inflammatory responses play in the pathogenesis of neurodegenerative diseases, including Alzheimer's disease, Parkinson's disease, and Amyotrophic Lateral Sclerosis. Aimed at researchers, scientists, and drug development professionals, the content explores foundational mechanisms of neuroinflammation, evaluates methodological approaches for identifying inflammatory biomarkers, discusses troubleshooting challenges in therapeutic development, and presents comparative validation of emerging treatment strategies. By synthesizing current research, this review aims to bridge molecular understanding with clinical application, highlighting the potential of immunomodulatory therapies to modify disease progression.
Core Mechanisms: Unraveling the Neuroinflammatory Cascade in Neurodegeneration
Neuroinflammation is a multifaceted and carefully regulated process within the central nervous system (CNS) that serves a dual function in both protecting neurons and contributing to neurodegenerative processes [1]. This process is primarily driven by activated microglia, astrocytes, and infiltrating immune cells that respond to neuronal damage, infections, or toxic exposures [1]. In recent years, research has increasingly recognized neuroinflammation not merely as a consequence of neurodegeneration but as a key underlying factor in the development and progression of multiple neurological conditions, including Alzheimer's disease (AD), Parkinson's disease (PD), multiple sclerosis (MS), and others [2]. The growing understanding of inflammatory pathways has revealed their central role in connecting various pathological mechanisms, making neuroinflammation a promising therapeutic target for potentially modifying the course of neurodegenerative diseases [3].
The significance of neuroinflammation in neurodegeneration is underscored by genetic studies that have identified several risk genes associated with the innate immune system specifically in microglia, the CNS's resident immune cells [2]. Furthermore, clinical observations indicate that individuals with severe systemic infections that activate the immune system have an increased risk of developing dementia, highlighting the causal linkage between inflammation and disease pathology [2]. This whitepaper provides a comprehensive technical overview of neuroinflammation as a common pathway in neurodegenerative diseases, examining key molecular mechanisms, research methodologies, and emerging therapeutic approaches relevant to researchers, scientists, and drug development professionals.
Key Molecular Pathways in Neuroinflammation
Core Signaling Pathways
Neuroinflammation in neurodegenerative diseases is mediated through several crucial molecular signaling pathways that coordinate the CNS immune response:
NF-κB Signaling: The nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB) pathway serves as a central regulator of neuroinflammatory responses. This pathway is activated in response to various stimuli, including cellular damage and protein aggregates, leading to the transcription of pro-inflammatory genes [1]. Activation of NF-κB in glial cells results in the production of cytokines such as TNF-α, IL-1β, and IL-6, which perpetuate inflammatory signaling and contribute to neuronal damage [1].
NLRP3 Inflammasome: The NLRP3 inflammasome is a multiprotein complex that plays a pivotal role in the innate immune response within the CNS. Upon activation by cellular damage or pathological protein aggregates such as amyloid-beta, the NLRP3 inflammasome catalyzes the cleavage of pro-caspase-1 to its active form, which subsequently processes pro-IL-1β and pro-IL-18 into their mature, active forms [1]. These cytokines drive potent inflammatory responses and have been implicated in the pathology of AD, PD, and other neurodegenerative conditions.
JAK/STAT Pathway: The Janus kinase/signal transducer and activator of transcription (JAK/STAT) signaling pathway is activated by various cytokines and growth factors. In neuroinflammation, sustained activation of this pathway contributes to chronic inflammatory states and glial activation [1]. The JAK/STAT pathway has been shown to regulate genes involved in immune cell differentiation and inflammatory responses, making it a significant contributor to the maintenance and amplification of inflammation in the CNS.
MAPK Pathway: Mitogen-activated protein kinase (MAPK) pathways, including p38, JNK, and ERK subfamilies, are activated in response to stress signals and inflammatory cytokines in the CNS [1]. These pathways regulate various cellular processes, including proliferation, differentiation, and apoptosis, but when chronically activated in neurodegenerative conditions, they contribute to sustained production of inflammatory mediators and neuronal dysfunction.
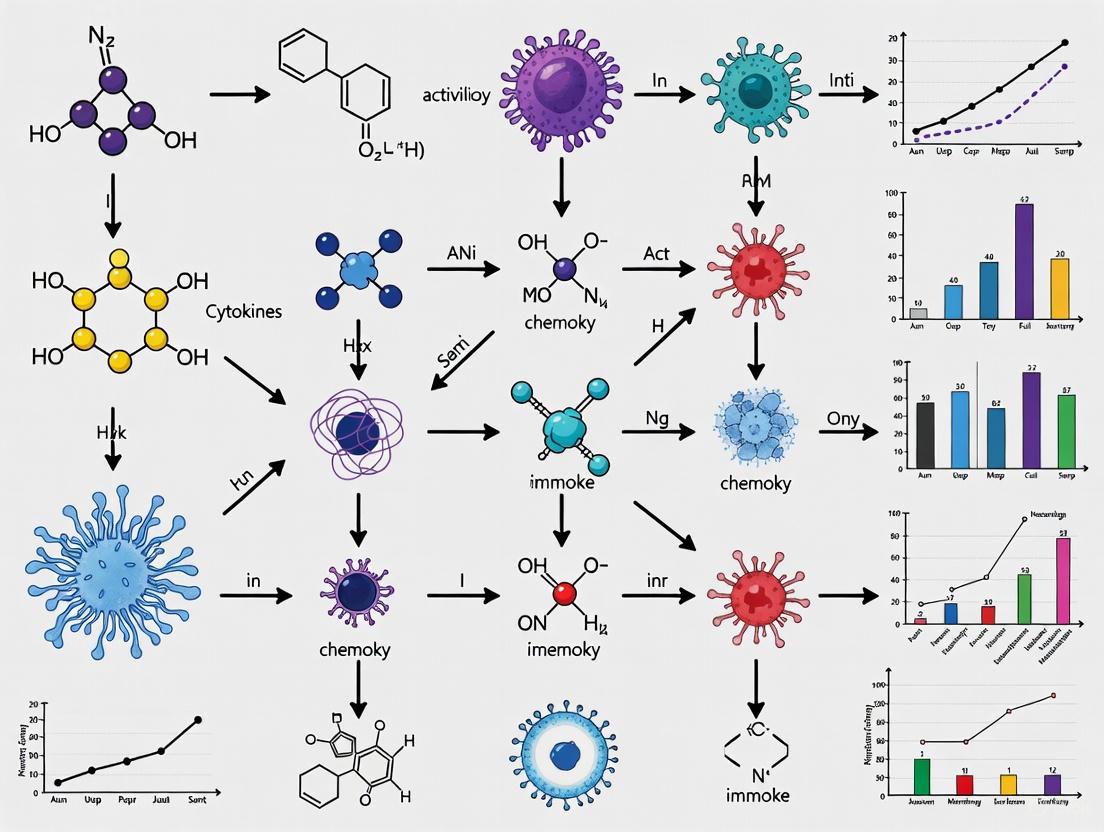
The interconnections and simplified workflow of these core neuroinflammatory pathways are visualized below:
Figure 1: Core Neuroinflammatory Signaling Pathways
Key Cellular Mediators and Inflammatory Components
The cellular landscape of neuroinflammation is characterized by the activation of CNS-resident glial cells and infiltration of peripheral immune cells:
Microglia: As the primary immune effector cells of the CNS, microglia exist in various activation states. In neurodegenerative conditions, microglia transition from a homeostatic surveillance state to an activated phenotype, releasing pro-inflammatory cytokines, chemokines, and reactive oxygen species [1]. Chronic microglial activation creates a self-perpetuating cycle of inflammation that drives neuronal damage.
Astrocytes: These star-shaped glial cells contribute to neuroinflammation through the release of inflammatory mediators and formation of glial scars. Activated astrocytes exhibit upregulated expression of pro-inflammatory genes and can present antigens to T-cells, amplifying the CNS immune response [4].
Infiltrating Immune Cells: Under conditions of blood-brain barrier (BBB) disruption, peripheral immune cells including T-lymphocytes, monocytes, and neutrophils infiltrate the CNS parenchyma [4]. These cells contribute to the inflammatory milieu and can recognize CNS antigens, potentially initiating autoimmune components in neurodegenerative diseases.
Table 1: Key Pro-inflammatory Mediators in Neuroinflammation
| Mediator | Primary Cellular Source | Main Functions | Role in Neurodegeneration |
|---|---|---|---|
| TNF-α | Microglia, Astrocytes | Pro-inflammatory signaling, cell death activation | Synaptic dysfunction, oligodendrocyte toxicity |
| IL-1β | Microglia (via NLRP3) | Fever, T-cell activation, chemokine production | Amyloid pathology, neuronal hyperexcitability |
| IL-6 | Microglia, Astrocytes | B-cell differentiation, acute phase response | Blood-brain barrier disruption, cognitive deficits |
| CCL2 | Microglia, Endothelial cells | Monocyte/macrophage recruitment | Leukocyte infiltration, chronic inflammation |
| CXCL10 | Astrocytes, Microglia | T-cell and NK cell recruitment | T-cell mediated neuronal damage |
Research Models and Methodologies
Experimental Models for Studying Neuroinflammation
Preclinical models are fundamental for understanding neuroinflammatory processes and developing therapeutic interventions. The selection of an appropriate model system depends on the specific research questions and the neurodegenerative disease being studied:
Experimental Autoimmune Encephalomyelitis (EAE): This is the most widely used animal model for studying multiple sclerosis and neuroinflammatory mechanisms [4]. EAE can be induced through active immunization with CNS antigens such as myelin oligodendrocyte glycoprotein (MOG), myelin basic protein (MBP), or proteolipid protein (PLP), typically administered with complete Freund's adjuvant (CFA) to enhance the immune response [4]. Alternatively, EAE can be induced through passive transfer of encephalitogenic T-cells into naïve recipient animals [4]. The EAE model reproduces key features of human MS, including immune cell infiltration, demyelination, and axonal damage, but has limitations in fully recapitulating the complexity of human disease.
Transgenic Models of Neurodegeneration: For Alzheimer's disease research, transgenic mouse models expressing mutant human genes associated with familial AD (e.g., APP, PSEN1, PSEN2) have been developed that exhibit both amyloid pathology and neuroinflammatory components [5]. Similarly, transgenic models exist for Parkinson's disease, amyotrophic lateral sclerosis, and other neurodegenerative conditions. These models allow researchers to study the specific interactions between disease-related protein aggregates and neuroinflammatory pathways.
Neuroinflammation Imaging Models: Animal models are essential for developing and validating imaging methods to detect neuroinflammation [5]. These include models that focus on specific aspects of inflammation, such as cell trafficking, expression of cell surface antigens, and associated changes in brain anatomy, physiology, and biochemistry. Such models enable the correlation of imaging findings with histological gold standards.
The general workflow for establishing and utilizing neuroinflammatory experimental models is summarized below:
Figure 2: Experimental Models Workflow
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Research Reagent Solutions for Neuroinflammation Studies
| Reagent/Category | Specific Examples | Function/Application | Technical Notes |
|---|---|---|---|
| Animal Models | C57BL/6 mice, SJL/J mice, APP/PS1 transgenic mice | Disease modeling, therapeutic testing | Strain selection critical for disease phenotype (e.g., SJL/J for relapsing-remitting EAE) |
| Induction Agents | MOG35-55 peptide, LPS, MPTP, CFA | Model establishment (EAE, systemic inflammation, Parkinson's) | Adjuvants like CFA essential for EAE; LPS doses vary by model (systemic vs direct CNS) |
| Cell Isolation Kits | Microglia isolation kits, Astrocyte separation kits | Primary cell culture, cell-specific analyses | Post-mortem timing critical for viability; purity confirmation via Iba1 (microglia) and GFAP (astrocytes) essential |
| Cytokine Assays | ELISA, Luminex, ELISA-spot, multiplex immunoassays | Quantifying inflammatory mediators | Multiplex platforms enable comprehensive cytokine profiling from limited samples |
| Imaging Tracers | [11C]PK11195, [18F]DPA-714, Gd-based contrast agents | PET/MRI visualization of neuroinflammation | TSPO tracers detect activated microglia; Gd enhancement indicates BBB disruption |
| Antibodies | Iba1, GFAP, CD68, CD11b, MHC-II | Immunohistochemistry, flow cytometry | Multiple markers needed to characterize microglial activation states (pro-/anti-inflammatory) |
| Nhs-mmaf | NHS-MMAF | NHS-MMAF reagent for antibody-drug conjugate (ADC) development. For Research Use Only. Not for human or veterinary diagnostic or therapeutic use. | Bench Chemicals |
| Apostatin-1 | Apostatin-1, MF:C19H27N3OS, MW:345.5 g/mol | Chemical Reagent | Bench Chemicals |
Neuroimaging and Visualization Approaches
Advanced neuroimaging techniques play a crucial role in visualizing and quantifying neuroinflammatory processes in both preclinical and clinical settings:
Magnetic Resonance Imaging (MRI): Conventional structural MRI can detect indirect signs of neuroinflammation, such as edema, blood-brain barrier disruption (using gadolinium contrast), and tissue atrophy [5]. Advanced MRI techniques including diffusion tensor imaging (DTI), magnetic resonance spectroscopy (MRS), and chemical exchange saturation transfer (CEST) provide additional information about tissue microstructure, metabolic changes, and protein aggregates associated with neuroinflammation [5].
Positron Emission Tomography (PET): PET imaging with radioligands that target translocator protein (TSPO), a marker of microglial activation, enables in vivo visualization and quantification of neuroinflammatory processes [5]. Second-generation TSPO tracers with improved specificity and binding characteristics are continuously being developed to enhance the sensitivity of detecting microglial activation in neurodegenerative diseases.
Programmatic Visualization Tools: The shift toward code-based neuroimaging visualization using tools such as MRIcron, R (with packages like ggseg), Python (with Nilearn), and MATLAB has significantly improved the reproducibility, flexibility, and scalability of neuroimaging research [6]. These tools allow researchers to create reproducible, publication-ready visualizations directly within programming environments, facilitating transparent reporting and efficient generation of multi-panel figures [6].
The integration of imaging data with molecular and histological findings is essential for validating the specificity and sensitivity of neuroimaging biomarkers for neuroinflammation. Animal models continue to play a critical role in this validation process, enabling direct correlation between imaging signals and tissue-level changes [5].
Clinical Translation and Therapeutic Development
Current Landscape of Neuroinflammation-Targeted Therapies
The recognition of neuroinflammation as a key driver of neurodegenerative diseases has spurred the development of therapeutic strategies targeting inflammatory pathways:
Alzheimer's Disease Drug Development: The 2025 Alzheimer's disease drug development pipeline includes 182 clinical trials testing 138 novel drugs, with a significant proportion targeting inflammatory mechanisms [7]. Biological disease-targeted therapies comprise 30% of the pipeline, while small molecule disease-targeted therapies account for 43% [7]. Repurposed agents, many with anti-inflammatory properties, represent approximately 33% of the pipeline agents, highlighting the interest in modulating neuroinflammation as a therapeutic approach [7].
Novel Anti-inflammatory Approaches: Emerging therapeutic strategies include monoclonal antibodies targeting specific cytokines or their receptors, small molecule inhibitors of inflammatory signaling pathways (e.g., JAK/STAT, NF-κB, NLRP3), and approaches aimed at promoting the transition of microglia from a pro-inflammatory to an anti-inflammatory, neuroprotective phenotype [2]. For example, the investigational compound INM-901 has demonstrated significant reduction in inflammatory biomarkers including IFN-γ, TNF-α, IL-1β, and neurofilament light chain (NfL) in preclinical studies [2].
Neuroprotection Strategies: Beyond purely anti-inflammatory approaches, there is growing interest in developing therapies that provide direct neuroprotection by safeguarding neurons from inflammatory-mediated damage [3]. This represents a paradigm shift from traditional symptom-management approaches to strategies that potentially modify disease progression by addressing the underlying inflammatory drivers of neurodegeneration.
Table 3: Selected Neuroinflammation-Targeted Therapies in Development
| Therapeutic Approach | Molecular Target | Development Stage | Key Findings/Mechanism |
|---|---|---|---|
| Anti-cytokine Therapies | IL-1β, TNF-α, IL-17A | Preclinical to Phase 2 | Reduced pro-inflammatory signaling; IL-17A inhibition associated with decreased amyloid plaques and tau pathology |
| NLRP3 Inflammasome Inhibitors | NLRP3 complex | Preclinical to Phase 1 | Reduced caspase-1 activation and IL-1β/IL-18 processing; improved outcomes in AD models |
| Microglial Modulators | TREM2, CSF1R | Phase 1-2 | Enhanced microglial phagocytosis of pathological proteins; promotion of neuroprotective phenotype |
| Repurposed Agents | GLP-1 receptors, S1P modulators | Phase 2-3 | GLP-1 agonists show neuroprotective and anti-inflammatory effects; potential reduction in amyloid plaques |
| Multi-target Approaches | Multiple inflammatory pathways | Preclinical to Phase 2 | INM-901 demonstrated reduction in multiple inflammatory biomarkers and trend toward normalization of gene expression |
Biomarkers and Clinical Trial Design
The development of sensitive and specific biomarkers is crucial for advancing neuroinflammation-targeted therapies:
Inflammatory Biomarkers: Fluid biomarkers such as cytokines, chemokines, and acute phase proteins in cerebrospinal fluid (CSF) and blood provide measurable indicators of neuroinflammatory processes [7]. Additionally, neurofilament light chain (NfL), a marker of axonal damage, is increasingly used as a downstream indicator of neuroinflammatory-mediated neuronal injury [3].
Imaging Biomarkers: PET imaging with TSPO tracers allows for direct visualization of microglial activation in clinical trials, providing a means to target engagement and pharmacodynamic effects of anti-inflammatory therapies [5]. Advanced MRI techniques offer additional biomarkers of tissue integrity, blood-brain barrier function, and metabolic changes associated with neuroinflammation.
Clinical Trial Considerations: Designing clinical trials for neuroinflammation-targeted therapies presents unique challenges, including patient selection, appropriate outcome measures, and trial duration [7]. There is a growing emphasis on patient-centric trial designs that incorporate patient-reported outcomes and consider factors such as convenience and long-term adherence, particularly for chronic conditions requiring sustained treatment [3].
The field is also exploring combination therapies that target multiple aspects of neurodegenerative diseases, including both protein aggregation and neuroinflammation, reflecting the multifactorial nature of these conditions [2].
Neurodegenerative diseases, including Alzheimer's disease (AD) and Parkinson's disease (PD), are characterized by a chronic inflammatory process within the central nervous system (CNS) that significantly contributes to disease pathogenesis and progression [8] [9]. This neuroinflammatory response is orchestrated by a complex interplay between resident CNS immune cells and infiltrating peripheral immune components, creating a self-perpetuating cycle of neuronal damage. Microglia, the principal innate immune cells of the brain, and astrocytes, crucial homeostatic supporters, undergo profound phenotypic changes in response to pathological protein aggregates such as amyloid-β and α-synuclein [8] [10]. Simultaneously, the integrity of the blood-brain barrier (BBB) is compromised, allowing peripheral immune cells and signaling molecules to infiltrate the CNS parenchyma and further shape the inflammatory milieu [11] [9]. Understanding the roles, states, and interactions of these cellular mediators is paramount for developing targeted therapeutic interventions aimed at modulating neuroinflammation in neurodegenerative diseases.
Core Cellular Mediators: Profiles and Functions
Microglia: The CNS Resident Macrophages
Origin and Homeostatic Functions: Microglia originate from yolk sac erythromyeloid progenitors (EMPs) that populate the brain during embryonic development, distinguishing them from other glial cells [8] [12]. In the healthy adult CNS, microglia are highly dynamic cells that continuously survey the parenchyma, extending and retracting their processes to monitor the microenvironment [13]. Their homeostatic functions include synaptic pruning to ensure proper neuronal circuitry, clearance of cellular debris and protein aggregates via phagocytosis, and trophic support for neurons through the release of factors like neurotropin-3 and insulin-like growth factor 1 (IGF1) [14] [13].
Activation States and Phenotypic Diversity: In response to pathological challenges such as protein aggregates or neuronal damage, microglia undergo activation, a process involving significant morphological, molecular, and functional remodeling [8]. The historical M1/M2 classification system—where M1 represents a pro-inflammatory, neurotoxic phenotype and M2 an anti-inflammatory, neuroprotective phenotype—fails to capture the full complexity of microglial responses in vivo [8] [12]. Advanced single-cell transcriptomic technologies have revealed a high degree of spatial and temporal heterogeneity, identifying context-specific activation states such as Disease-Associated Microglia (DAM) [8] [12]. DAM are characterized by a two-stage activation process: an initial Trem2-independent stage involving downregulation of homeostatic genes (e.g., Cx3cr1, P2ry12), followed by a Trem2-dependent stage featuring upregulation of genes involved in phagocytosis and lipid metabolism (e.g., ApoE, Lpl) [12]. This state is found clustered around pathological hallmarks like amyloid plaques in AD [8].
Table 1: Key Microglial Phenotypes in Neurodegeneration
| Phenotype | Key Markers | Primary Functions | Context |
|---|---|---|---|
| Homeostatic | CX3CR1, P2RY12, TREM119 [12] | Immune surveillance, synaptic pruning, trophic support [14] [13] | Healthy CNS |
| M1-like (Pro-inflammatory) | CD86, iNOS, IL-1β, TNF-α [12] | Release of pro-inflammatory cytokines, reactive oxygen species, neurotoxicity [12] [15] | Response to strong inflammatory signals (e.g., IFN-γ, TNF-α) [12] |
| M2-like (Anti-inflammatory) | ARG1, YM1/2, IL-10, TGF-β [12] | Phagocytosis of debris, release of anti-inflammatory and trophic factors, tissue repair [12] [15] | Response to IL-4, IL-13; resolution phase [12] |
| Disease-Associated (DAM) | ApoE, Lpl, Cst7, Trem2 (Stage 2) [12] | Phagocytosis of pathological protein aggregates, lipid metabolism [8] [12] | Neurodegenerative disease lesions (e.g., near Aβ plaques) [8] |
Astrocytes: Crucial Homeostatic Support and Inflammatory Contributors
Heterogeneity and Homeostatic Roles: Astrocytes are the most abundant glial cell type in the CNS and are fundamental for maintaining brain homeostasis [16]. Their functions include regulating ion and water balance, recycling neurotransmitters, forming and maintaining the blood-brain barrier, and modulating synaptic activity and synaptogenesis [16]. Similar to microglia, astrocytes exhibit significant morphological, molecular, and functional heterogeneity across different CNS regions and are now understood to comprise multiple subpopulations with specialized roles [10] [16].
Reactive Astrocytes in Neuroinflammation: Under pathological conditions, astrocytes transition into reactive states, a process commonly marked by the upregulation of Glial Fibrillary Acidic Protein (GFAP) [16]. Transcriptomic studies have identified distinct reactive sub-states, notably the neurotoxic A1 and the potentially neuroprotective A2 phenotypes [10] [16]. The induction of A1 astrocytes is driven by a cocktail of cytokines (IL-1α, TNF, C1q) released by activated microglia [10] [16]. These A1 astrocytes lose their normal homeostatic functions, such as promoting synapse formation and neuronal survival, and instead upregulate genes that drive complement activation and contribute to neuronal death [10] [16]. Reactive astrocytes contribute to neurodegeneration by producing pro-inflammatory cytokines, increasing the production of Aβ through elevated BACE1 and APP expression, and promoting tau pathology [14].
Table 2: Reactive Astrocyte Sub-States
| Sub-State | Inducing Signals | Characteristic Markers | Putative Functions |
|---|---|---|---|
| A1 (Neurotoxic) | Microglia-derived IL-1α, TNF, C1q [10] [16] | C3, H2-T23, FKBP5 [16] | Loss of homeostatic functions, complement activation, neuronal death [10] [16] |
| A2 (Neuroprotective) | Ischemia, IL-6, CNTF [10] [16] | S100a10, PTX3, Tm4sf1 [10] | Trophic factor production, tissue repair [10] |
Peripheral Immune Cells: Infiltration and CNS Reshaping
The chronic neuroinflammation in neurodegenerative diseases is often accompanied by a compromised BBB, facilitating the infiltration of peripheral immune cells that significantly contribute to the pathological process [11] [9].
- Monocytes and Macrophages: In response to peripheral inflammation or CNS damage, monocytes are recruited from the bloodstream and can differentiate into highly phagocytic macrophages within the brain parenchyma [14]. A distinct subset of human CD14+CD16+ monocytes has been identified with a heightened capacity to migrate across the BBB model in vitro [11]. Once in the CNS, these cells release pro-inflammatory cytokines and interact with resident glial cells, exacerbating neuroinflammation and neuronal hyperreactivity [11].
- Lymphocytes (T and B cells): The infiltration of peripheral T and B cells into the CNS not only contributes to neuronal demyelination but also participates in central immune surveillance, further shaping the local inflammatory environment [11].
- Systemic Communication via the Vagus Nerve: A critical body-brain circuit regulates peripheral inflammatory responses. The vagus nerve senses pro- and anti-inflammatory cytokines in the periphery and relays this information to the caudal nucleus of the solitary tract (cNST) in the brainstem [17]. In turn, this circuit modulates the peripheral immune response, demonstrating a sophisticated neural control of inflammation. Silencing this pathway leads to uncontrolled, runaway inflammation, while its activation suppresses the pro-inflammatory response [17].
Experimental Approaches and Methodologies
Key Experimental Protocols for Neuroimmune Research
1. Single-Cell RNA Sequencing (scRNA-seq) for Microglial and Astrocyte Heterogeneity:
- Purpose: To identify and characterize novel, disease-specific transcriptional states of microglia and astrocytes in human post-mortem tissue and animal models [8] [10].
- Workflow:
- Tissue Dissociation: Fresh or rapidly frozen CNS tissue from a specific region (e.g., hippocampus or substantia nigra) is dissociated into a single-cell suspension.
- Cell Capture and Barcoding: Single cells are captured in nanoliter droplets along with barcoded beads (e.g., using 10x Genomics platform). Each RNA transcript from a single cell is tagged with a unique cellular barcode.
- Library Preparation and Sequencing: cDNA libraries are constructed and sequenced using high-throughput next-generation sequencing.
- Bioinformatic Analysis: Sequences are demultiplexed using the cellular barcodes. Dimensionality reduction algorithms (e.g., PCA, UMAP) and graph-based clustering are applied to identify distinct cell populations and states (e.g., DAM, A1 astrocytes) based on their unique gene expression profiles [8] [12].
2. Chemogenetic Manipulation of Neuroimmune Circuits (e.g., Vagus Nerve-cNST Axis):
- Purpose: To establish causal links between specific neuronal populations and the regulation of peripheral immunity [17].
- Workflow:
- Targeting:
- Viral Vector Delivery: An adeno-associated virus (AAV) carrying a Cre-dependent Designer Receptor Exclusively Activated by Designer Drugs (DREADD) is stereotactically injected into the cNST of transgenic mice (e.g., TRAP or Vglut2-cre mice).
- Specificity: The Cre-recombinase is expressed only in neurons activated by a prior immune challenge (TRAP) or in glutamatergic neurons, ensuring targeted DREADD expression [17].
- Silencing or Activation:
- Inhibition: To silence the circuit, an inhibitory DREADD (iDREADD, e.g., hM4Di) is used. Administration of its designer ligand (Clozapine-N-Oxide, CNO) hyperpolarizes and silences the neurons.
- Activation: To activate the circuit, an excitatory DREADD (e.g., hM3Dq) is used. CNO administration depolarizes and activates the neurons [17].
- Immune Challenge and Readout: Mice are challenged with LPS. Peripheral blood is collected at multiple time points, and plasma cytokine levels (e.g., IL-1β, IL-6, IL-10) are quantified via ELISA to assess the effect of neuronal manipulation on the immune response [17].
- Targeting:
3. Assessing Microglial Phagocytic Capacity In Vitro:
- Purpose: To evaluate the functional impact of genetic mutations (e.g., TREM2 R47H) or therapeutic compounds on the ability of microglia to phagocytose substrates like Aβ [12].
- Workflow:
- Cell Culture: Immortalized microglial cell lines (e.g., BV-2) or primary microglia isolated from rodent brains are cultured.
- Treatment/Modification: Cells are pre-treated with a candidate drug or are genetically modified (e.g., CRISPR/Cas9, siRNA).
- Phagocytosis Assay: Fluorescently-labeled Aβ1-42 fibrils or latex beads are added to the culture medium.
- Quantification: After incubation and washing to remove non-internalized particles, cells are analyzed by flow cytometry or high-content imaging to quantify the fluorescence intensity per cell, which correlates with phagocytic uptake [12].
Visualization of Key Pathways and Relationships
The following diagrams illustrate the core interactions and experimental workflows described in this whitepaper.
Diagram 1: Body-Brain Immune Regulation Circuit. This diagram illustrates the neuroimmune axis where the vagus nerve senses peripheral inflammation and relays signals to the brainstem (cNST), which in turn sends out signals that suppress the peripheral inflammatory response [17].
Diagram 2: Cellular Crosstalk in Neuroinflammation. This diagram depicts the vicious cycle of cellular communication in neurodegenerative diseases, where activated microglia induce a neurotoxic astrocyte phenotype (A1), and infiltrating peripheral immune cells exacerbate the activation of both resident glial cells [10] [11] [9].
The Scientist's Toolkit: Essential Research Reagents and Models
Table 3: Key Reagents and Models for Neuroimmune Research
| Category / Reagent | Specific Example | Function/Application |
|---|---|---|
| Animal Models | 5xFAD AD model mice; LPS-induced neuroinflammation model; MPTP PD model | Provide in vivo systems to study disease progression, glial activation, and test therapeutics [12] [13]. |
| Cell Lines | BV-2 microglial cell line; Primary microglia/astrocyte cultures | Enable in vitro mechanistic studies on phagocytosis, cytokine release, and signaling pathways [8] [12]. |
| Key Antibodies | Iba1 (for microglia); GFAP (for astrocytes); P2RY12 (homeostatic microglia); C3 (A1 astrocytes) | Identify, label, and isolate specific cell types and phenotypes via IHC, flow cytometry [8] [14] [16]. |
| Cytokines & Inducers | Recombinant IL-1α, TNF, C1q (A1 astrocyte induction); LPS (TLR4 agonist, general inflammation) | Used to stimulate specific reactive states in glial cells in vitro and in vivo [10] [16]. |
| Genetic Tools | DREADDs (Chemogenetics); Cre-lox system (e.g., Cx3cr1-Cre, GFAP-Cre); TREM2 KO/R47H mutant mice | Allow precise manipulation and fate-mapping of specific cell populations in vivo [8] [17]. |
| Imaging Tracers | [11C]PK11195 (TSPO PET ligand); Fluorescent-Aβ/α-syn | Non-invasive imaging of glial activation in live animals/humans; tracing phagocytosis in vitro [8] [12]. |
| H-D-Phe-Pip-Arg-pNA dihydrochloride | H-D-Phe-Pip-Arg-pNA dihydrochloride, MF:C27H38Cl2N8O5, MW:625.5 g/mol | Chemical Reagent |
| Tubulin inhibitor 35 | Tubulin inhibitor 35, MF:C21H21N3O, MW:331.4 g/mol | Chemical Reagent |
Microglia, astrocytes, and peripheral immune cells function as an integrated unit in the neuroinflammatory landscape of neurodegenerative diseases. Their states and interactions are highly dynamic and context-dependent, moving far beyond simplistic binary classifications. The emergence of powerful single-cell technologies has been instrumental in decoding this complexity, revealing novel, disease-associated phenotypes like DAM and A1 astrocytes. Furthermore, the discovery of hardwired neuroimmune circuits, such as the vagus nerve-cNST axis, underscores the brain's active role in regulating peripheral and central immunity. Future therapeutic strategies must account for this complexity, aiming not to universally suppress glial activity but to precisely target maladaptive states or disrupt deleterious cellular crosstalk, thereby shifting the equilibrium from a toxic to a protective inflammatory environment.
Neurodegenerative diseases represent a significant and growing challenge to global health, characterized by progressive neuronal loss and impaired central nervous system function. Research over the past decade has increasingly highlighted the critical role of dysregulated immune responses and inflammatory signaling pathways in the pathogenesis of these disorders. While acute inflammation serves a protective function, chronic neuroinflammation drives pathological progression in conditions including Alzheimer's disease (AD), Parkinson's disease (PD), and amyotrophic lateral sclerosis (ALS). This technical review examines three key signaling pathways—the NLRP3 inflammasome, IL-17A cytokine signaling, and the 12/15-lipoxygenase (12/15-LOX) pathway—that collectively contribute to the inflammatory microenvironment in neurodegenerative diseases. Understanding the mechanisms, interactions, and therapeutic targeting potential of these pathways provides crucial insights for researchers and drug development professionals working to modify disease progression.
Pathway Fundamentals and Mechanisms
NLRP3 Inflammasome Pathway
The NLR family pyrin domain containing 3 (NLRP3) inflammasome is a multimeric protein complex that functions as a critical component of the innate immune system, detecting both pathogen-associated molecular patterns (PAMPs) and damage-associated molecular patterns (DAMPs) [18]. This pattern recognition receptor is expressed primarily in immune cells including dendritic cells and macrophages, but also in microglia, astrocytes, smooth muscle cells, endothelial cells, and cardiomyocytes [18]. The NLRP3 gene is located on chromosome 1q44 and encodes a protein containing a pyrin domain, a nucleotide-binding site (NBS) domain, and a leucine-rich repeat (LRR) motif [18].
Table 1: Core Components of the NLRP3 Inflammasome Complex
| Component | Symbol | Function | Expression |
|---|---|---|---|
| Sensor protein | NLRP3 | Pattern recognition receptor | Immune cells, microglia |
| Adaptor protein | ASC (Apoptosis-associated speck-like protein containing a CARD) | Bridges NLRP3 to caspase-1 | Ubiquitous |
| Effector protease | Caspase-1 | Cleaves pro-IL-1β and pro-IL-18 | Inflammasome-associated |
| Inflammatory cytokine | IL-1β | Pyrogen, neutrophil activation | Multiple cell types |
| Inflammatory cytokine | IL-18 | IFN-γ induction, Treg generation | Multiple cell types |
| Pore-forming protein | GSDMD (Gasdermin D) | Mediates pyroptosis | Inflammasome-associated |
The NLRP3 inflammasome activates through a canonical "two-hit" mechanism requiring both priming and activation steps [19]. The priming signal (often through Toll-like receptor activation) induces nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB)-mediated transcription of NLRP3, pro-IL-1β, and pro-IL-18 [19]. A subsequent activation signal triggers the assemblage of the NLRP3 inflammasome complex, leading to caspase-1 activation [18]. Active caspase-1 then cleaves pro-IL-1β and pro-IL-18 into their mature, biologically active forms and cleaves GSDMD, initiating pyroptotic cell death [20]. Activation triggers include extracellular ATP, crystalline uric acid, silica, cholesterol crystals, and reactive oxygen species (ROS) [18].
Diagram 1: NLRP3 Inflammasome Activation Pathway. The canonical two-signal mechanism leads to caspase-1 activation and inflammatory mediator release.
IL-17A Signaling Pathway
Interleukin-17A (IL-17A, commonly referred to as IL-17) is the founding member of the IL-17 cytokine family, which includes six structurally related cytokines (IL-17A through IL-17F) [21]. IL-17A was first identified in 1993 as cytotoxic T-lymphocyte-associated antigen 8 (CTLA-8) and is primarily produced by a distinct CD4+ T helper subset (Th17 cells), though it is also expressed by CD8+ T cells, γδ T cells, natural killer T cells, and innate lymphoid cells [22]. The human IL-17A monomer is a 155-amino acid glycoprotein that forms a 35 kDa homologous dimer through disulfide bonds [21].
Table 2: IL-17 Family Receptors and Ligands
| Receptor Subunit | Partner Subunit | Ligand Specificity | Primary Cell Types |
|---|---|---|---|
| IL-17RA | IL-17RC | IL-17A, IL-17F, IL-17A/F | Epithelial cells, mesenchymal cells |
| IL-17RA | IL-17RB | IL-17E (IL-25) | Hematopoietic cells |
| IL-17RA | IL-17RD | IL-17A (specific) | Various tissues |
| IL-17RB | - | IL-17B | Limited distribution |
| IL-17RE | - | IL-17C | Epithelial cells |
IL-17A signaling initiates when the cytokine binds to its receptor complex, typically composed of IL-17RA and IL-17RC subunits [21]. This binding triggers recruitment of the adaptor protein Act1 (also known as CIKS) through interactions with the SEFIR domains of IL-17R [21]. Act1 then recruits tumor necrosis factor receptor-associated factors (TRAFs), particularly TRAF6, leading to NF-κB activation and inflammatory gene expression [21]. The distal domain in the cytoplasmic tail of IL-17RA contains a C/EBP-β activation domain (CBAD) that associates with TRAF3 and the ubiquitin-editing enzyme A20, creating negative feedback regulation [21].
Diagram 2: IL-17A Signal Transduction Pathway. IL-17 binding initiates Act1-mediated signaling with built-in negative feedback mechanisms.
12/15-Lipoxygenase (12/15-LOX) Pathway
12/15-lipoxygenase (12/15-LOX), encoded by the ALOX15 gene in humans, is a non-heme iron-containing dioxygenase that catalyzes the stereospecific peroxidation of polyunsaturated fatty acids (PUFAs) [23]. The enzyme is constitutively expressed in reticulocytes, eosinophils, dendritic cells, alveolar macrophages, airway epithelial cells, vascular cells, resident peritoneal macrophages, pancreatic islets, and uterus [23]. In human peripheral blood monocytes, 12/15-LOX expression can be induced by IL-4 and IL-13 [23].
12/15-LOX metabolizes various PUFAs including linoleic acid, alpha-linolenic acid, gamma-linolenic acid, arachidonic acid, eicosapentaenoic acid, and docosahexaenoic acid [23]. When using arachidonic acid as substrate, human ALOX15 produces predominantly 15(S)-hydroperoxyeicosatetraenoic acid (15(S)-HPETE) and smaller amounts of 12(S)-HPETE, which are subsequently reduced to their corresponding hydroxy derivatives (15(S)-HETE and 12(S)-HETE) by cellular glutathione peroxidase [23]. These metabolites exhibit diverse biological activities, with 15(S)-HETE shown to bind and activate peroxisome proliferator-activated receptor γ (PPARγ) in macrophages [24].
Table 3: 12/15-LOX Enzymatic Products and Functions
| Enzyme | Primary Substrates | Main Products | Biological Activities |
|---|---|---|---|
| Human ALOX15 (12/15-LOX) | Arachidonic acid, Linoleic acid | 15(S)-HETE, 12(S)-HETE, 13(S)-HODE | PPARγ activation, inflammatory regulation |
| Human ALOX15B | Arachidonic acid, Linoleic acid | 15(S)-HETE, 13(S)-HODE | Exclusive 15-lipoxygenating activity |
| Murine Alox15 | Arachidonic acid, Linoleic acid | 12(S)-HETE, 15(S)-HETE | Primarily 12-lipoxygenating activity |
In contrast to ALOX15, ALOX15B (arachidonate 15-lipoxygenase type B) exhibits singular reaction specificity, exclusively producing 15(S)-HETE from arachidonic acid [24]. While ALOX15 expression in human monocyte-derived macrophages is strictly dependent on Th2 cytokines IL-4 and IL-13, ALOX15B is constitutively expressed [24]. ALOX15 plays a crucial role in generating specific phospholipid oxidation products needed for nonimmunogenic removal of apoptotic cells and synthesizing precursor lipids for specialized pro-resolving mediators (SPMs) that facilitate inflammation resolution [24].
Roles in Neurodegenerative Diseases
NLRP3 Inflammasome in Neurodegeneration
The NLRP3 inflammasome has been extensively implicated in the pathogenesis of multiple neurodegenerative diseases. In Alzheimer's disease, β-amyloid (Aβ) and tau act as DAMPs, activating the NLRP3 inflammasome in microglia [25]. This activation leads to release of IL-1β and IL-18, exacerbating neuroinflammation and accelerating neurodegeneration [25]. Peripheral immune cells and postmortem brain tissue from AD patients show elevated levels of IL-1β and IL-18, along with increased expression of NLRP3, ASC, and caspase-1 [25]. In APP/PS1 AD mouse models, crossing with NLRP3 or caspase-1 deficient models preserves memory and increases Aβ phagocytosis, indicating that NLRP3 inflammasome activation reduces Aβ clearance [25].
In Parkinson's disease, increased levels of ASC and NLRP3 have been detected in post-mortem tissue from PD patients [25]. The MPTP-induced mouse model of PD demonstrates that NLRP3 or caspase-1 knockout reduces dopaminergic neuron loss and improves motor function [25]. Additionally, caspase-1 can directly cleave α-synuclein, and blocking NLRP3 activation with the small molecule inhibitor MCC950 reduces α-synuclein aggregation, dopaminergic degeneration, neuroinflammation, and motor deficits in mouse models of PD [25].
For amyotrophic lateral sclerosis, elevated levels of NLRP3, ASC, IL-18, and caspase-1 have been detected in post-mortem tissue of ALS patients [25]. In SOD1G93A mouse models, astrocytes in the spinal cord are the main expressers of NLRP3 components, and caspase-1 inhibition delays disease onset, neurological deterioration, and mortality [25].
IL-17A in Neurodegenerative Pathology
While research on IL-17A in neurodegenerative diseases is less extensive than for the NLRP3 inflammasome, emerging evidence indicates significant roles in neuroinflammation. IL-17 is a highly versatile proinflammatory cytokine necessary for host immune defenses but also contributes to inflammatory disease pathogenesis [21]. The IL-17 signaling pathway has several similarities with the Toll-like receptor (TLR)/IL-1R signaling pathway, though Act1 functions differently in these pathways [21].
IL-17 can mediate protective innate immunity to pathogens or contribute to the pathogenesis of inflammatory diseases [22]. In the context of neurodegeneration, IL-17's ability to promote neutrophilic inflammation and its potent pro-osteoclastogenic effects may contribute to disease pathology [22]. The cytokine's involvement in both inflammation and protective antimicrobial immunity creates a "double-edged sword" scenario for diseases with complex etiologies like periodontitis, which has been linked to neurodegenerative conditions [22].
12/15-LOX in Neurological Disorders
12/15-LOX has been demonstrated to play important roles in oxidative and inflammatory responses in neurological disorders. A large number of studies have revealed the importance of 12/15-LOX in the pathogenesis of various human diseases, including cardiovascular, renal, neurological, and metabolic disorders [23]. In vitro studies have demonstrated the ability of 12/15-LOX metabolites to regulate expression of various genes and production of cytokines related to inflammation and resolution of inflammation [23].
The monohydroxy fatty acid products of the 12/15-LOX reaction exhibit biological activity and are thought to serve various physiological functions [24]. AA-derived 15- and 12-HETE exhibit both pro- and anti-inflammatory effects, with 15-HETE shown to bind and activate PPARγ in both human and murine macrophages [24]. In macrophages, ALOX15 functions to generate specific phospholipid oxidation products crucial for orchestrating the nonimmunogenic removal of apoptotic cells as well as synthesizing precursor lipids required for production of specialized pro-resolving mediators (SPMs) that facilitate inflammation resolution [24].
Experimental Methodologies
NLRP3 Inflammasome Assays
In vitro NLRP3 activation in macrophages: Isolate and culture bone marrow-derived macrophages (BMDMs) from wild-type and genetically modified mice. Prime cells with LPS (100 ng/mL, 3-4 hours) then stimulate with NLRP3 activators (ATP, nigericin, crystalline particulates) for specified durations [18] [19]. Measure caspase-1 activation via Western blot (detecting cleaved caspase-1 p10 subunit) or fluorescent caspase-1 activity assays. Quantify IL-1β and IL-18 release by ELISA [18].
ASC speck formation assay: Differentiate and prime THP-1 cells or primary human macrophages with PMA and LPS. Activate inflammasome with ATP or nigericin. Fix cells and immunostain for ASC. Visualize ASC speck formation (hallmark of inflammasome assembly) using confocal microscopy [19] [20].
LDH release assay for pyroptosis: Culture primed macrophages in 96-well plates. Following NLRP3 activation, collect culture supernatants and measure lactate dehydrogenase (LDH) release using colorimetric assay kits according to manufacturer protocols. Normalize values to total cellular LDH content (from lysed cells) to calculate percentage cell death [20].
IL-17 Signaling Analysis
IL-17 receptor binding assays: Culture epithelial cells or fibroblasts in 6-well plates until 80% confluent. Stimulate with recombinant IL-17A (10-100 ng/mL) for various time points. For receptor blocking experiments, pre-treat cells with IL-17RA/RC neutralizing antibodies (1-10 μg/mL) 1 hour prior to IL-17A stimulation [21] [22].
Act1 recruitment and TRAF6 ubiquitination: Transfect HEK293T cells with plasmids encoding IL-17RA, IL-17RC, Act1, and TRAF6. Immunoprecipitate Act1 or TRAF6 24-48 hours post-transfection and analyze ubiquitination by Western blot using anti-ubiquitin antibodies [21].
IL-17 target gene expression: Treat relevant cell types (keratinocytes, synovial fibroblasts, astrocytes) with IL-17A (50 ng/mL) for 6-24 hours. Isolate RNA and analyze expression of IL-17 target genes (CXCL1, CXCL5, CCL20, DEFB4) using quantitative RT-PCR [21] [22].
12/15-LOX Activity Measurement
Enzyme activity assay: Prepare cell lysates from IL-4/IL-13-stimulated macrophages or transfected cells expressing 12/15-LOX. Incubate lysates with arachidonic acid (50 μM) in assay buffer (pH 7.4) at 37°C for 10-30 minutes. Stop reaction with cold methanol and analyze 12(S)-HETE and 15(S)-HETE production using reverse-phase HPLC with UV detection at 235 nm or LC-MS/MS [23] [24].
SPM biosynthesis analysis: Differentiate human M2-like macrophages with IL-4/IL-13. Stimulate with calcium ionophore A23187 (10 μM) or opsonized zymosan in the presence of substrate PUFAs (EPA, DHA). Extract lipids using solid-phase extraction and analyze lipoxins, resolvins, protectins, and maresins using liquid chromatography-tandem mass spectrometry (LC-MS/MS) with multiple reaction monitoring [24].
Immunofluorescence staining for 12/15-LOX: Culture cells on chamber slides, fix with 4% paraformaldehyde, permeabilize with 0.1% Triton X-100, and block with 5% normal serum. Incubate with anti-ALOX15 primary antibody overnight at 4°C, followed by appropriate fluorescent secondary antibody. Counterstain with DAPI and visualize using fluorescence or confocal microscopy [23].
Research Reagent Solutions
Table 4: Essential Research Reagents for Pathway Investigation
| Reagent Category | Specific Examples | Research Applications | Key Functions |
|---|---|---|---|
| NLRP3 Inhibitors | MCC950 (CRID3), Glyburide, OLT1177 | Inhibit NLRP3 inflammasome assembly | Specific NLRP3 inhibition, IL-1β reduction |
| Caspase-1 Inhibitors | VX-740, VX-765, Z-YVAD-FMK | Block caspase-1 activity | Inhibit IL-1β/IL-18 maturation, pyroptosis |
| IL-17 Neutralizing Antibodies | Secukinumab, Ixekizumab | Block IL-17A signaling | Therapeutic antibodies for autoimmune diseases |
| IL-17 Receptor Antagonists | IL-17RA/RC blocking antibodies | Inhibit IL-17 receptor binding | Research tools for pathway dissection |
| 12/15-LOX Inhibitors | PD146176, Baicalein, ML355 | Suppress 12/15-LOX enzyme activity | Reduce HETE production, modulate inflammation |
| LOX Substrates | Arachidonic acid, Linoleic acid, DHA, EPA | 12/15-LOX activity assays | Enzyme substrates for metabolic studies |
| Cytokine Detection | IL-1β ELISA, IL-18 ELISA, IL-17 ELISA | Quantify cytokine production | Measure pathway activation and inhibition |
| Gene Expression Analysis | NLRP3, CASP1, IL1B, IL17A qPCR primers | Quantify pathway component expression | Assess transcriptional regulation |
The NLRP3 inflammasome, IL-17A signaling, and 12/15-LOX pathway represent three critical, interconnected mechanisms driving neuroinflammatory processes in neurodegenerative diseases. Each pathway contributes uniquely to disease pathogenesis: the NLRP3 inflammasome through its response to protein aggregates and subsequent production of IL-1β and IL-18; IL-17A through its promotion of neutrophilic inflammation and tissue responses; and 12/15-LOX through its generation of both pro-inflammatory and pro-resolving lipid mediators. The development of targeted therapeutics for these pathways shows considerable promise, with NLRP3 inhibitors like MCC950 demonstrating efficacy in preclinical models of AD and PD, IL-17A monoclonal antibodies (secukinumab, ixekizumab) already approved for autoimmune conditions, and 12/15-LOX modulators offering potential for fine-tuning inflammatory responses. Future research should focus on understanding the crosstalk between these pathways, identifying patient subgroups most likely to benefit from specific interventions, and developing strategies for combination therapies that simultaneously target multiple inflammatory mechanisms while preserving protective immune functions.
Neurodegenerative disorders, including Alzheimer's disease (AD), represent one of the most significant challenges in modern medicine, with pathological mechanisms centered on the interplay between protein aggregation and inflammatory processes [26]. The two prominent neuropathological hallmarks of AD are the extracellular neuritic plaques composed of aggregated β-amyloid (Aβ) and intracellular neurofibrillary tangles consisting of hyperphosphorylated tau protein [27]. Beyond these classic features, neuroinflammation has emerged as a third fundamental pathological hallmark, not merely as a secondary consequence but as a driving force in disease progression [28] [29].
The concept of a vicious cycle between protein aggregation and inflammatory amplification provides a crucial framework for understanding the progressive nature of neurodegenerative diseases. In this cycle, protein aggregates activate inflammatory pathways, which in turn promote further protein aggregation, creating a self-reinforcing feedback loop that drives disease progression [29] [27]. This interplay generates mechanisms that initially compensate for adverse effects and maintain brain homeostasis during the long prodromal phase of AD, but when these compensatory mechanisms fail, an irreversible transition to clinical disease occurs [29]. Mounting evidence indicates that tau pathology correlates more closely with cognitive dysfunction than amyloid pathology, and inflammation accompanies the entire pathological process, making understanding these interactions crucial for therapeutic development [27].
Molecular Mechanisms of Protein Aggregation
Amyloid-β Aggregation Pathways
Aβ peptides are 39-43 residue-long peptides produced through proteolytic cleavage of amyloid precursor protein (APP) by β- and γ-secretases [29]. The concentration-dependent aggregation of Aβ follows a complex nucleation-dependent polymerization mechanism that includes multiple steps: (1) primary nucleation, where Aβ monomers form oligomers; (2) conversion of oligomers into elongation-competent fibrillar particles; (3) elongation through monomer addition to growing fibril ends; and (4) secondary nucleation on the surface of existing fibrils, generating new oligomers [29]. This multi-step process can be represented by the following kinetic equation for Aβ monomer concentration:
$$\begin{array}{l}\dot{{a}{m}}={k}{+}-{k}{-}{a}{m}-{j}{1}{a}{m}^{n1}+{j}{-1}{a}{o}\-\frac{\,{nconv}}{\left(1+{nconv}\right)}{j}{2}{a}{m}^{{nconv}}{a}{o}-{j}{3}{a}{m}{a}{{fp}}-{j}{4}{a}{m}^{n2}{a}_{f}\end{array}$$
Where $\dot{{a}{m}}$ represents time-dependent changes in Aβ monomer concentration, ${k}{+}$ and ${k}{-}$ are generation and clearance rates, and ${j}{1}$ through ${j}_{4}$ represent rate constants for the various aggregation processes [29].
Tau Pathology and Propagation
Tau is a microtubule-associated protein predominantly found in neuronal axons, where it stabilizes microtubules and facilitates intracellular transport [27] [30]. In pathological conditions, tau undergoes various post-translational modifications, with hyperphosphorylation being the most extensively studied. The normal adult brain contains 2-3 mol of phosphate per mole of tau, but in the AD brain, tau becomes hyperphosphorylated with a two- to threefold increase in phosphate content [27]. This hyperphosphorylation destabilizes tau's interaction with microtubules and enhances its accumulation in the cytoplasm.
The propagation of tau pathology follows a "prion-like" seeding-nucleation mechanism [31]. In this process, pathological tau acts as a template that triggers the misfolding and aggregation of natively folded tau monomers into disease-associated forms [31]. This seeding activity enables tau pathology to spread throughout the brain along anatomically connected networks, explaining the stereotypical progression of tau pathology in AD [31]. Importantly, smaller, soluble tau oligomers—rather than large fibrillar inclusions—are now believed to play the most critical role in neurotoxicity and propagation [27].
Table 1: Key Proteins in Neurodegenerative Aggregation
| Protein | Normal Function | Pathological Form | Associated Diseases |
|---|---|---|---|
| Aβ | Derived from APP processing; precise physiological function unclear | Oligomers, fibrils, plaques | Alzheimer's disease, Cerebral amyloid angiopathy |
| Tau | Microtubule stabilization, intracellular transport | Hyperphosphorylated oligomers, neurofibrillary tangles | Alzheimer's disease, Frontotemporal dementia, PSP, CBD |
| TDP-43 | RNA metabolism, predominantly nuclear | Cytoplasmic aggregates | ALS, FTLD-TDP |
| SOD1 | Breakdown of superoxide radicals | Intraneuronal inclusions | Familial ALS |
Mechanisms of Inflammatory Amplification
Glial Cell Activation in Neuroinflammation
Neuroinflammation in neurodegenerative diseases is characterized by the activation of glial cells, particularly microglia and astrocytes [28]. These cells undergo phenotypic transformation into pro-inflammatory states: microglia transition to M1 (pro-inflammatory) states, while astrocytes become A1 (neurotoxic) astrocytes [28]. A1 astrocytes release numerous proinflammatory mediators and neurotoxins, contributing to neuronal damage [28]. The transition of astrocytes to the A1 state can be induced by a cocktail of cytokines, including TNF-α, IL-1α, and C1q [32]. Crucially, research demonstrates that Aβ can directly substitute for C1q in this cytokine cocktail, synergistically promoting pro-inflammatory activation of human astrocytes even at low, physiological concentrations (10 nM) [32].
Biomarkers of glial activation provide windows into neuroinflammatory processes. Glial fibrillary acidic protein (GFAP) elevates in both early- and late-onset AD patients, confirming astrocyte activation and degeneration as part of disease pathology [28]. Chitinase-3-like protein (CHI3L1/YKL-40), an A1 astrocytic protein, serves as a potential cerebrospinal fluid biomarker that increases with aging and early in AD [28]. Colony-Stimulating Factor 1 Receptor (CSF1R), expressed primarily in microglia, shows upregulation that parallels neuropathology in AD [28].
Cytokine Signaling and Inflammatory Mediators
Chronic neuroinflammation involves complex cytokine networks that drive disease progression. Key inflammatory mediators include IL-1β, IL-6, TNF-α, chemokines such as CCL2, reactive oxygen species, nitric oxide, matrix metalloproteinases, and vascular endothelial growth factor [28]. These molecules are released by activated glial cells and neurons, creating a neurotoxic environment that promotes neurodegeneration.
The transcription factor nuclear factor kappa-B (NF-κB) plays a central role in modulating gene expression and the release of inflammatory cytokines [33]. NF-κB activation induces transcription of genes encoding pro-inflammatory mediators, establishing sustained inflammatory responses. This pathway is highly conserved across species and represents a critical signaling node in neuroinflammation [33].
The Vicious Cycle: Coupled Aggregation-Inflammation Dynamics
Mathematical Modeling of Coupled Systems
The interplay between Aβ aggregation and inflammation can be represented through mathematical modeling that captures the essential feedback loops driving disease progression [29]. These models demonstrate that coupled Aβ aggregation-inflammation systems can exhibit enormously rich dynamics, ranging from overdamped kinetics to sustained oscillations [29]. The model incorporates inflammation-dependent modulation of Aβ generation and clearance rates following a Hill-type response function, representing the biological reality that inflammatory processes influence Aβ homeostasis.
In this framework, inflammation induced by Aβ aggregates (particularly oligomers and fibrils) modulates the rates of key processes in Aβ aggregation, including generation, clearance, nucleation, and elongation [29]. This coupling creates nonlinear system behavior that can transition from stable homeostasis to progressive pathology when parameters exceed critical thresholds. Prolonged sustained oscillations in such systems may lead to immune system exhaustion, representing a potential mechanism underlying the transition to progressive disease phases [29].
Diagram 1: Protein Aggregation-Inflammation Vicious Cycle. This diagram illustrates the self-reinforcing feedback loops between Aβ aggregation, tau pathology, and neuroinflammation that drive neurodegeneration.
Experimental Evidence for Cross-Amplification
Experimental studies provide compelling evidence for the vicious cycle between protein aggregation and inflammation. At nanomolar concentrations—physiologically relevant levels—Aβ acts synergistically with known cytokines to promote pro-inflammatory activation in primary human astrocytes [32]. This synergistic activation converts astrocytes to a reactive, A1-like state with a transcriptional signature similar to neurotoxic astrocytes known to accumulate with age and in AD [32].
The immune activation observed in response to Aβ shares similarities with classical innate immune responses. Aβ exhibits structural similarities with antimicrobial peptides like cathelicidin, which stimulates pro-inflammatory cytokine secretion in glial cells [32]. Additionally, Aβ can induce pores in cell membranes, a common characteristic of immune-activating antimicrobial peptides [32]. These findings suggest that immune activation may be a natural biological function of Aβ that contributes to coordinated pro-inflammatory responses in the CNS.
On the tau side, sustained and increased inflammatory responses in glial cells and neurons are pivotal cellular drivers that exacerbate tau pathology, which in turn worsens neuroinflammation [27]. Inflammatory cytokines can directly influence tau phosphorylation through various kinase pathways, including glycogen synthase kinase-3β (GSK3β), cyclin-dependent kinase-5 (CDK5), and p38 mitogen-associated protein kinase alpha (p38α MAPK) [27]. This intimate crosstalk creates a feed-forward loop that accelerates disease progression.
Experimental Models and Methodologies
Seed Amplification Assays for Tau Aggregation
Tau seed amplification assays (SAA) represent a breakthrough technology for detecting and amplifying small quantities of misfolded tau aggregates [31]. This method reproduces the prion-like seeding mechanism responsible for the spreading of tau pathology in a cell-free system. In SAA, tau seeds from biological samples template their conformation onto recombinant tau substrates through cycles of shaking and incubation, with amplification monitored in real-time using the amyloid-binding dye Thioflavin T (ThT) [31].
The Tau-SAA protocol involves several key steps:
- Expression and purification of tau isoforms: Recombinant human tau isoforms are expressed in E. coli and purified, with cysteine residues substituted for serine to prevent oligomerization through cysteine bridges [31].
- Sample preparation: Brain homogenates are diluted serially, with AD-derived seeds detectable even after 100-million-fold dilution [31].
- Amplification reaction: Samples are mixed with recombinant tau substrate and ThT in multiwell plates, then subjected to cyclic shaking and incubation [31].
- Fluorescence monitoring: Thioflavin T fluorescence is measured periodically to track amyloid formation [31].
- Data analysis: Aggregation kinetics are analyzed to determine seeding activity and potential inhibition by therapeutic compounds [31].
This assay demonstrates high sensitivity and specificity for AD brain tau seeds, distinguishing AD samples from controls with excellent accuracy [31]. Moreover, it serves as a valuable platform for screening tau aggregation inhibitors, with screening of 220 compounds revealing that approximately 57% of suspected aggregation inhibitors and ~3% of CNS-penetrant compounds inhibited over 75% of AD brain-templated tau aggregation [31].
Diagram 2: Tau Seed Amplification Assay Workflow. This diagram illustrates the key steps in detecting and amplifying pathological tau seeds using the SAA technology.
Model Systems for Studying Neuroinflammation
Various experimental models provide unique advantages for studying inflammatory responses in neurodegenerative diseases:
Rodent models: Mice and rats share approximately 85% of their genome with humans and exhibit significant physiological similarities, making them ideal for investigating complex diseases and inflammatory responses [33]. Their short reproductive cycles and lifespans enable longitudinal studies of disease progression. Importantly, rodents show conservation of innate and adaptive immune mechanisms, including similarities in epithelial barriers and the presence of T cells, B cells, and natural killer cells [33]. Key inflammatory pathways, including NF-κB activation and neutrophil chemotaxis regulation, involve the same receptor subtypes (P2Y2, A3, and A2a) as in humans [33].
Human iPSC-derived models: Induced pluripotent stem cell (iPSC)-derived neurons, astrocytes, microglia, endothelial cells, and pericytes provide human-specific platforms for disease modeling and drug discovery [28]. These cells can be used in various coculture systems, brain organoids, and neurovascular unit cultures that better recapitulate human disease pathophysiology [28]. iPSC models allow for the study of human-specific inflammatory responses and genetic influences on neuroinflammation.
Primary human glial cultures: Studies using primary human astrocytes have revealed important species-specific responses, such as the synergistic activation of astrocytes by Aβ in combination with cytokines [32]. These models provide critical translational insights that may not be apparent in animal models or immortalized cell lines.
Table 2: Experimental Models for Neuroinflammation Research
| Model System | Key Advantages | Limitations | Applications |
|---|---|---|---|
| Rodent Models | Genetic similarity to humans (~85%), well-characterized immune system, genetic manipulation possible | Limited translational predictability, genetic homogeneity of inbred strains | Studying complex disease pathophysiology, preclinical therapeutic testing |
| Human iPSC-Derived Cells | Human-specific responses, patient-specific genetic backgrounds, amenable to high-throughput screening | Immature phenotypes, limited representation of aging processes | Disease modeling, personalized medicine approaches, drug screening |
| Primary Human Glial Cultures | Species-specific responses, maintain relevant physiological characteristics | Limited availability, donor-to-donor variability, technical challenges | Mechanistic studies of human-specific inflammatory pathways |
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Table 3: Key Research Reagent Solutions for Protein Aggregation and Neuroinflammation Studies
| Reagent/Category | Specific Examples | Research Application | Technical Function |
|---|---|---|---|
| Recombinant Tau Proteins | Cysteine-free tau isoforms (0N3R, 1N3R, 0N4R, etc.) | Tau seed amplification assays, aggregation kinetics studies | Substrate for seeding experiments, enables study of isoform-specific effects |
| Amyloid-Binding Dyes | Thioflavin T (ThT) | Monitoring amyloid formation in real-time | Fluorescent reporter that increases quantum yield upon binding to β-sheet structures |
| Pro-Inflammatory Cytokines | TNF-α, IL-1α, C1q | Astrocyte activation studies, inflammation induction | Induce transition to neurotoxic A1 astrocyte phenotype |
| Cell Type-Specific Markers | GFAP (astrocytes), Iba1 (microglia), C3 (A1 astrocytes) | Identification and quantification of glial activation states | Immunodetection of activated glial populations in tissue and cell cultures |
| Kinase Inhibitors | GSK3β inhibitors, CDK5 inhibitors | Studying post-translational modifications of tau | Modulate phosphorylation pathways implicated in tau hyperphosphorylation |
| Cytokine Detection Assays | ELISA, multiplex immunoassays | Quantifying inflammatory mediators in biological samples | Sensitive detection and quantification of specific cytokines and chemokines |
| Sotuletinib dihydrochloride | Sotuletinib dihydrochloride, CAS:2222138-40-9, MF:C20H24Cl2N4O3S, MW:471.4 g/mol | Chemical Reagent | Bench Chemicals |
| (S)-Sunvozertinib | (S)-Sunvozertinib, MF:C29H35ClFN7O3, MW:584.1 g/mol | Chemical Reagent | Bench Chemicals |
Therapeutic Implications and Clinical Translation
Targeting the Aggregation-Inflammation Axis
The intricate interplay between protein aggregation and inflammation presents multiple therapeutic targets for interrupting the vicious cycle. Recent approaches include:
Immunotherapies: Monoclonal antibodies targeting Aβ, including aducanumab and lecanemab, have received FDA approval, though their clinical efficacy remains controversial [26] [27]. These antibodies promote clearance of amyloid plaques but demonstrate limited effects on tau pathology and neuroinflammation. Tau-directed immunotherapies are currently under investigation, with approaches targeting various tau epitopes and aggregation states [27].
Small molecule inhibitors: Diverse small molecules targeting various steps in the aggregation-inflammation axis are in development. These include selective inhibitors, dual-target inhibitors, allosteric modulators, covalent inhibitors, proteolysis-targeting chimeras (PROTACs), and protein-protein interaction modulators [26]. Tau aggregation inhibitors represent a particularly promising approach, with the Tau-SAA platform enabling high-throughput screening of compound libraries [31].
Multi-target strategies: Given the complexity of the aggregation-inflammation cycle, multi-target approaches may offer superior efficacy. These strategies might combine anti-aggregation compounds with anti-inflammatory agents to simultaneously target multiple nodes in the pathological network [27]. Precision medicine approaches that account for individual variations in both proteopathic and inflammatory pathways represent the future of therapeutic development for neurodegenerative diseases.
Biomarker Development for Clinical Trials
The development of biomarkers for both protein aggregation and neuroinflammation is crucial for patient stratification and therapeutic monitoring. Key biomarkers include:
Fluid biomarkers: Cerebrospinal fluid measures of Aβ42, phosphorylated tau, and total tau provide insights into amyloid and tau pathology [26] [27]. Neurofilament light chain (NfL) serves as a marker of neuronal axonal damage, while GFAP and CHI3L1/YKL-40 reflect astrocyte activation and neuroinflammation [28]. Recent advances enable measurement of many these biomarkers in blood, facilitating larger clinical trials and routine clinical monitoring.
Imaging biomarkers: Positron emission tomography (PET) ligands for amyloid and tau aggregates allow direct visualization of protein pathology in living brains [27]. Emerging PET tracers for neuroinflammation, such as those targeting CSF1R and P2Y12 receptors, enable quantification of microglial activation [28]. These imaging biomarkers provide spatial information about pathological burden and progression.
Seed amplification assays: SAAs for both Aβ and tau aggregates offer exceptional sensitivity for detecting pathological seeds years before symptom onset [31]. These assays have potential for early diagnosis, patient stratification, and monitoring treatment effects in clinical trials.
The vicious cycle between protein aggregation and inflammatory amplification represents a fundamental framework for understanding the progression of neurodegenerative diseases, particularly Alzheimer's disease. In this self-reinforcing feedback loop, protein aggregates activate inflammatory pathways, which in turn promote further aggregation through multiple mechanisms including enhanced production of pathogenic proteins, impaired clearance, and post-translational modifications that increase aggregation propensity.
Breaking this cycle requires integrated therapeutic approaches that simultaneously target both proteopathic and inflammatory components. Advances in experimental models, particularly human iPSC-derived systems and sensitive detection methods like seed amplification assays, provide powerful tools for dissecting the mechanisms driving this vicious cycle and for developing effective therapeutic interventions. The continued elucidation of the precise molecular mechanisms linking protein aggregation and neuroinflammation will undoubtedly yield new therapeutic targets and strategies for these devastating disorders.
Oxidative Stress and Mitochondrial Dysfunction as Inflammatory Consequences
Oxidative stress and mitochondrial dysfunction are interconnected pathological processes that amplify inflammatory responses, creating a self-perpetuating cycle central to neurodegenerative disease progression. This whitepaper delineates the molecular mechanisms linking mitochondrial impairment to reactive oxygen species (ROS) overproduction, damage-associated molecular pattern (DAMP) release, and chronic neuroinflammation. Within the context of neurodegenerative research, we present quantitative biomarkers, detailed experimental methodologies for detecting oxidative damage, and pathway visualization. Furthermore, we explore emerging therapeutic strategies that target these pathways, providing a technical foundation for researchers and drug development professionals working to disrupt this destructive cascade.
In the pathogenesis of neurodegenerative diseases, oxidative stress and mitochondrial dysfunction are not merely concurrent abnormalities but are fundamentally intertwined drivers of a chronic inflammatory state [34] [35]. The brain's high metabolic demand and oxygen consumption, coupled with its abundance of peroxidation-sensitive lipids and relatively weak antioxidant defenses, render it particularly vulnerable to these processes [34] [36]. Oxidative stress arises from an imbalance between the production of reactive oxygen species (ROS) and the cell's capacity to neutralize them, leading to damage of lipids, proteins, and DNA [36].
Mitochondria sit at the epicenter of this pathology, serving as both the primary source of ROS and a key target of oxidative damage [37] [38]. Dysfunctional mitochondria contribute to inflammation through multiple pathways, most notably via the release of mitochondrial DNA (mtDNA), which acts as a DAMP, triggering innate immune responses and sustaining a cycle of neuronal injury [35]. This triad of oxidative stress, mitochondrial dysfunction, and neuroinflammation establishes a vicious feed-forward cycle that accelerates neurodegeneration in conditions such as Alzheimer's disease (AD), Parkinson's disease (PD), and amyotrophic lateral sclerosis (ALS) [37] [35] [39]. Understanding these mechanistic links is paramount for developing targeted therapeutic interventions.
Molecular Mechanisms and Signaling Pathways
The Central Role of Mitochondrial Dysfunction
Mitochondrial integrity is crucial for neuronal survival. Dysfunction manifests through several interconnected mechanisms:
- Impaired Electron Transport Chain (ETC): Complex I and III of the ETC are major sites of ROS generation, primarily in the form of superoxide anion (O₂•â») [38]. Defects in these complexes, commonly observed in neurodegenerative diseases, lead to electron leakage and excessive ROS production [37] [39].
- Dysregulated Mitochondrial Dynamics: Neuronal mitochondria undergo constant fission and fusion. The fission protein Drp1 is recruited to the mitochondrial membrane by adapters like Mff and Fis1, facilitating division. Fusion is mediated by mitofusins (Mfn1/2) on the outer membrane and OPA1 on the inner membrane [38] [39]. An imbalance toward excessive fission fragments the mitochondrial network, segregating damaged organelles and priming them for degradation, a process often dysregulated in neurodegeneration [39].
- Failed Quality Control: Mitophagy, the selective autophagy of damaged mitochondria, is critical for quality control. The PINK1/Parkin pathway is a key regulator of this process. Impaired mitophagy leads to the accumulation of dysfunctional mitochondria, further exacerbating ROS production [39].
Oxidative Stress and Biomarker Generation
ROS overproduction damages all major classes of cellular macromolecules, generating measurable biomarkers detailed in Table 1 [40]. Lipid peroxidation of polyunsaturated fatty acids generates highly reactive aldehydes like malondialdehyde (MDA) and 4-hydroxynonenal (HNE), which can form protein adducts, impairing function [40]. Protein oxidation can result in carbonylation and tyrosine nitration, forming 3-nitrotyrosine [41] [40]. Nucleic acid oxidation, particularly of guanine to form 8-hydroxy-2'-deoxyguanosine (8-OHdG), is a marker for DNA/RNA damage [40].
The Inflammatory Nexus: mtDNA as a DAMP
The release of mitochondrial components into the cytosol or extracellular space is a pivotal link to inflammation. mtDNA, with its bacterial-like, hypomethylated CpG motifs, is a potent DAMP [35]. It can be released through several mechanisms, including permeability transition pore (mPTP) opening and mitochondrial-derived vesicles (MDVs) [35]. Once in the cytoplasm, mtDNA is sensed by pattern recognition receptors (PRRs) like TLR9 and the NLRP3 inflammasome, triggering the production of pro-inflammatory cytokines such as IL-1β and IL-6, and fostering a chronic neuroinflammatory environment mediated by activated microglia [35].
The following pathway diagram synthesizes these core mechanisms into a unified visual model.
Figure 1: Integrated Pathway of Mitochondrial Dysfunction, Oxidative Stress, and Neuroinflammation. This diagram illustrates the self-reinforcing cycle where primary insults induce mitochondrial dysfunction, leading to ROS production and mtDNA release. This triggers oxidative damage and DAMP-mediated neuroinflammation, ultimately driving neuronal death and disease progression in disorders like Alzheimer's (AD) and Parkinson's (PD). Abbreviations: ETC: Electron Transport Chain; mPTP: Mitochondrial Permeability Transition Pore; mtDNA: Mitochondrial DNA; DAMP: Damage-Associated Molecular Pattern; PRR: Pattern Recognition Receptor; ROS: Reactive Oxygen Species; MDA: Malondialdehyde; HNE: 4-Hydroxynonenal; 8-OHdG: 8-Hydroxy-2'-Deoxyguanosine.
Quantitative Biomarker Profiling
The detection and quantification of oxidative stress biomarkers in patient samples and model systems are essential for diagnostic and therapeutic monitoring. The following table summarizes key biomarkers and their detection methodologies.
Table 1: Key Oxidative Stress Biomarkers and Detection Methods in Neurodegenerative Disease Research
| Biomarker Class | Specific Marker | Biological Significance | Detection Methods | Representative Findings in Neurodegeneration |
|---|---|---|---|---|
| Lipid Peroxidation | Malondialdehyde (MDA), 4-Hydroxynonenal (HNE) | Reactive aldehydes formed from peroxidation of polyunsaturated fatty acids; form protein adducts disrupting function [40]. | Immunohistochemistry, ELISA, HPLC, mass spectrometry [40]. | Elevated in plasma and CSF of PD and AD patients; adducts detected in Lewy bodies in PD [40]. |
| Protein Oxidation | 3-Nitrotyrosine | Formed by peroxynitrite (ONOOâ»)-mediated nitration of tyrosine residues; marker of protein damage & RNS activity [41] [40]. | Immunohistochemistry, chromatography, specific antibodies [40]. | Increased levels in the brain, serum, and leukocytes of HD patients [40]. |
| Nucleic Acid Oxidation | 8-Hydroxy-2'-deoxyguanosine (8-OHdG)/8-oxodG | Oxidized derivative of deoxyguanosine; marker of oxidative damage to nuclear and mitochondrial DNA [40]. | Immunoassays, HPLC, LC-MS, specific antibodies [40]. | Elevated in the brain, CSF, and leukocytes of AD and HD patients; a sensitive biomarker for HD progression [40]. |
| Antioxidant Defense | Reduced Glutathione (GSH) | Major endogenous antioxidant; depletion indicates compromised antioxidant capacity [41]. | Colorimetric/fluorometric assays, HPLC. | Depletion observed in the substantia nigra of PD patients [41]. |
Mitochondrial function itself can be quantitatively assessed to provide a holistic view of cellular health. The following table outlines critical parameters for evaluating mitochondrial integrity and function in experimental models.
Table 2: Key Parameters for Assessing Mitochondrial Function in Experimental Models
| Parameter | Description & Method | Experimental Tools & Assays | Interpretation in Disease Models |
|---|---|---|---|
| ROS Production | Measure of superoxide and hydrogen peroxide generation by mitochondria. | MitoSOX Red (for mitochondrial O₂•â»), Hâ‚‚DCFDA (for cellular Hâ‚‚Oâ‚‚), fluorescent probes [41]. | Increased fluorescence indicates oxidative stress, a hallmark across AD, PD, and ALS models [41] [40]. |
| Mitochondrial Membrane Potential (ΔΨm) | Indicator of the proton gradient and energetic health of mitochondria. | JC-1 dye, TMRM, TMRE probes [39]. | Collapse of ΔΨm (shift in JC-1 emission) signifies mitochondrial dysfunction and early apoptosis. |
| Oxygen Consumption Rate (OCR) | Measure of mitochondrial respiration and ETC function. | Seahorse XF Analyzer, Clark-type oxygen electrode [37]. | Reduced OCR indicates impaired oxidative phosphorylation, commonly reported in AD and PD models [37] [39]. |
| ATP Production | Quantification of cellular ATP levels as a direct measure of energy output. | Luciferase-based assays (e.g., ATPlite). | Decreased ATP levels reflect bioenergetic failure, contributing to synaptic dysfunction [39]. |
| Calcium Buffering Capacity | Assessment of mitochondrial ability to sequester cytosolic calcium. | Fluorescent calcium indicators (e.g., Fura-2) in conjunction with mitochondrial toxins. | Impaired capacity leads to calcium dysregulation and excitotoxicity, implicated in AD and HD [35] [39]. |
Experimental Protocols
This section provides detailed methodologies for key techniques used to investigate oxidative stress and mitochondrial dysfunction in neurodegenerative disease research.
Protocol: Detecting Oxidative Stress Biomarkers via Immunohistochemistry
This protocol is adapted from methods used to detect markers like MDA, HNE, 3-nitrotyrosine, and 8-OHdG in formaldehyde-fixed, paraffin-embedded (FFPE) tissue sections from post-mortem human brain or animal models [40].
1. Sample Preparation and Sectioning:
- Fix tissue samples (e.g., brain cortex, substantia nigra) by immersion in 4% formaldehyde for 24-48 hours at 4°C.
- Dehydrate tissues through a graded ethanol series, clear with xylene, and embed in paraffin blocks.
- Section tissues at 5-8 µm thickness using a microtome and mount on charged glass slides. Dry slides overnight at 37°C.
2. Deparaffinization, Rehydration, and Antigen Retrieval:
- Deparaffinize sections by immersion in xylene (2 changes, 10 min each).
- Rehydrate through a graded ethanol series (100%, 95%, 70%) to distilled water.
- Perform antigen retrieval by incubating slides in pre-heated sodium citrate buffer (10 mM, pH 6.0) and heating in a microwave or pressure cooker for 10-15 minutes. Allow slides to cool to room temperature in the buffer.
3. Immunostaining:
- Quench endogenous peroxidase activity by incubating with 3% Hâ‚‚Oâ‚‚ in methanol for 10 minutes.
- Wash slides in PBS (pH 7.4) and block non-specific binding with 5% normal serum (from the species of the secondary antibody) in PBS for 1 hour at room temperature.
- Incubate with primary antibody (e.g., anti-MDA, anti-3-nitrotyrosine, anti-8-OHdG) diluted in blocking buffer overnight at 4°C in a humidified chamber.
- The next day, wash with PBS and incubate with a biotinylated secondary antibody (e.g., goat anti-rabbit IgG) for 1 hour at room temperature.
- Apply an avidin-biotin-peroxidase complex (ABC kit) according to the manufacturer's instructions for 30-60 minutes.
- Visualize the signal using a chromogen substrate such as 3,3'-diaminobenzidine (DAB). Counterstain with hematoxylin, dehydrate, clear, and mount with a permanent mounting medium.
4. Analysis:
- Analyze stained sections under a light microscope. Positive staining (brown precipitate) can be semi-quantified using image analysis software (e.g., ImageJ) by measuring the integrated optical density in specific brain regions of interest.
Protocol: Measuring Malondialdehyde (MDA) in Tissue Lysates and Body Fluids
This protocol describes a simple method for detecting MDA, a common lipid peroxidation product, useful for screening levels of oxidative stress in tissues like brain homogenates, plasma, or cerebrospinal fluid (CSF) [40].
1. Sample Preparation:
- Homogenize tissue samples in ice-cold PBS (e.g., 1:10 w/v) containing 0.5% butylated hydroxytoluene (BHT) to prevent further oxidation during processing. Centrifuge at 10,000 × g for 10 minutes at 4°C to collect the supernatant.
- For plasma or CSF, use the sample directly or after a 1:1 dilution with PBS.
2. Thiobarbituric Acid Reactive Substances (TBARS) Assay:
- Mix 100 µL of sample (supernatant, plasma, or CSF) with 200 µL of 8.1% SDS, 1.5 mL of 20% acetic acid (pH 3.5), and 1.5 mL of 0.8% thiobarbituric acid (TBA) solution.
- Heat the mixture at 95°C for 60 minutes in a heating block.
- Cool the tubes on ice for 10 minutes to stop the reaction.
- Add 1 mL of distilled water and 5 mL of a mixture of n-butanol and pyridine (15:1 v/v). Vortex vigorously for 30-60 seconds.
- Centrifuge at 1,500 × g for 10 minutes to separate the organic and aqueous phases.
3. Measurement and Quantification:
- Carefully transfer the upper (organic) phase, which contains the pink MDA-TBA adduct, to a cuvette.
- Measure the fluorescence of the adduct at an excitation wavelength of 532 nm and an emission wavelength of 553 nm.
- Quantify MDA concentration by comparison to a standard curve prepared using 1,1,3,3-tetramethoxypropane, which hydrolyzes to MDA.
The workflow for this multi-modal experimental approach is visualized below.
Figure 2: Multi-Modal Experimental Workflow for Assessing Oxidative Stress and Mitochondrial Dysfunction. This workflow outlines parallel paths for histopathological, biochemical, and functional analyses, enabling comprehensive and correlative data interpretation from tissue and biofluid samples. Abbreviations: IHC: Immunohistochemistry; TBA: Thiobarbituric Acid; OCR: Oxygen Consumption Rate; ECAR: Extracellular Acidification Rate.
The Scientist's Toolkit: Research Reagent Solutions
Successful investigation into these pathways relies on a suite of specific reagents and tools. The following table details essential materials and their applications.
Table 3: Essential Research Reagents for Investigating Oxidative Stress and Mitochondrial Dysfunction
| Reagent/Tool Category | Specific Examples | Function & Application |
|---|---|---|
| ROS Detection Probes | MitoSOX Red, Hâ‚‚DCFDA, Dihydroethidium (DHE) | Cell-permeable fluorescent dyes for detecting mitochondrial superoxide (MitoSOX), general cellular ROS (Hâ‚‚DCFDA), and superoxide (DHE) via flow cytometry, microscopy, or plate readers [41]. |
| Mitochondrial Function Probes | JC-1, Tetramethylrhodamine (TMRM/TMRE) | Cationic dyes that accumulate in active mitochondria; JC-1 measures ΔΨm via emission shift (greenred), while TMRM/TMRE indicate potential via fluorescence intensity [39]. |
| Antibodies for Oxidative Stress Biomarkers | Anti-3-Nitrotyrosine, Anti-MDA, Anti-HNE, Anti-8-OHdG | Specific antibodies for the immunohistochemical or western blot detection of oxidized proteins, lipids, and nucleic acids in tissues and cells [40]. |
| Mitochondrial Complex Inhibitors | Rotenone (Complex I), Antimycin A (Complex III), Oligomycin (ATP Synthase) | Pharmacological tools to induce experimental mitochondrial dysfunction and oxidative stress in in vitro and in vivo models [41]. |
| Inducers of Mitochondrial Biogenesis | PGC-1α agonists (e.g., Bezafibrate) | Activate the PGC-1α pathway to stimulate the generation of new mitochondria, potentially counteracting mitochondrial loss in disease models. |
| Modulators of Mitochondrial Dynamics | Mdivi-1 (Drp1 inhibitor) | Small molecule inhibitors that block mitochondrial fission by inhibiting Drp1, promoting a more fused network and used to probe the role of fission in disease [39]. |
| NAMPT inhibitor-linker 2 | NAMPT inhibitor-linker 2, MF:C34H33FN6O5, MW:624.7 g/mol | Chemical Reagent |
| BLI-489 hydrate | BLI-489 hydrate, MF:C13H12N3NaO5S, MW:345.31 g/mol | Chemical Reagent |
Therapeutic Implications and Future Directions
Targeting the nexus of oxidative stress, mitochondrial dysfunction, and inflammation presents a promising multi-faceted therapeutic strategy.
- Mitochondria-Targeted Antioxidants: Compounds like MitoQ, which consists of a ubiquinone antioxidant moiety attached to a triphenylphosphonium cation, accumulate within mitochondria driven by the membrane potential, directly scavenging ROS at its primary source [37] [36]. This approach overcomes the limitations of conventional antioxidants like vitamin E, which have shown poor efficacy in clinical trials, partly due to limited bioavailability and insufficient targeting to relevant subcellular compartments [41] [36].
- Modulators of Mitochondrial Quality Control: Enhancing the clearance of damaged mitochondria via mitophagy is a key therapeutic goal. Strategies include activating the PINK1/Parkin pathway or using compounds like Urolithin A to promote mitophagy [39]. Conversely, inhibiting excessive fission with Drp1 inhibitors (e.g., Mdivi-1) has shown protective effects in preclinical models of neurodegeneration [39].
- Anti-inflammatory Strategies Targeting DAMPs: Inhibiting the sensors of mtDNA, such as TLR9 or the NLRP3 inflammasome, could specifically dampen the neuroinflammatory response triggered by mitochondrial dysfunction without causing broad immunosuppression [35].
- Metabolic Modulators: Agents that boost mitochondrial biogenesis (e.g., via AMPK or PGC-1α activation) or support cellular energy metabolism (e.g., NAD⺠precursors) aim to correct the bioenergetic deficit that underpins neuronal vulnerability [39].
- Innovative Approaches: Artificial Mitochondrial Transfer: This emerging technique involves the direct transplantation of healthy isolated mitochondria into cells or tissues, offering a radical approach to replacing a damaged mitochondrial pool. While still in early stages, it holds significant potential for treating neurodegenerative diseases characterized by severe mitochondrial failure [39].
The path to clinical translation requires a deeper understanding of the temporal sequence of these pathological events and the development of biomarkers to identify patients most likely to benefit from these targeted interventions. Future research should focus on combination therapies that concurrently address multiple nodes of this destructive network.
Biomarkers and Detection: From Bench to Bedside Applications
The role of peripheral inflammation in central nervous system disorders represents a paradigm shift in neurodegenerative disease research. Traditionally viewed as isolated to the brain, conditions such as Alzheimer's disease (AD), autoimmune encephalitis (AE), and medication-overuse headache (MOH) are now recognized to involve significant systemic inflammatory components [42] [43] [44]. Blood-based inflammatory ratios—the neutrophil-to-lymphocyte ratio (NLR), monocyte-to-lymphocyte ratio (MLR), and platelet-to-lymphocyte ratio (PLR)—have emerged as accessible, cost-effective biomarkers that reflect the balance between innate and adaptive immune responses [43] [44]. These biomarkers offer practical advantages for both research and clinical applications, providing insights into disease mechanisms, progression, and treatment response across the neurodegenerative spectrum.
The NLR, PLR, and MLR serve as integrative measures of systemic inflammatory status, capturing the complex interplay between different immune cell populations. Neutrophils represent the innate immune system's first line of defense, releasing pro-inflammatory cytokines and reactive oxygen species that may contribute to neuroinflammation and blood-brain barrier disruption when chronically activated [43]. Lymphocytes regulate adaptive immunity, and their reduction may indicate immunosuppression or chronic inflammatory states. Monocytes participate in phagocytosis and can differentiate into tissue macrophages, while platelets release inflammatory mediators that modulate vascular function [44]. The ratios between these cell populations provide a more stable inflammatory measure than absolute cell counts, reducing inter-individual variability and offering superior prognostic value in various neurological conditions [43] [44] [45].
Biomarker Definitions and Physiological Significance
Calculation and Biological Basis
Peripheral inflammatory ratios are derived from routine complete blood count (CBC) data, making them widely accessible and cost-effective compared to specialized biomarker assays. The calculations are as follows:
Neutrophil-to-Lymphocyte Ratio (NLR): Calculated as absolute neutrophil count divided by absolute lymphocyte count. NLR reflects the balance between the innate (neutrophil-driven) and adaptive (lymphocyte-mediated) immune systems [43] [44]. Elevated NLR indicates a predominance of neutrophilic inflammation, which has been associated with oxidative stress and tissue damage through mechanisms such as neutrophil adhesion to endothelium and migration across the blood-brain barrier [43].
Platelet-to-Lymphocyte Ratio (PLR): Determined as absolute platelet count divided by absolute lymphocyte count. PLR represents interactions between coagulation pathways and immune responses, with platelets serving as sources of inflammatory mediators including cytokines, chemokines, and growth factors [44] [45].
Monocyte-to-Lymphocyte Ratio (MLR): Calculated as absolute monocyte count divided by absolute lymphocyte count. MLR reflects monocytic activation and migration potential, with monocytes capable of differentiating into brain macrophages that contribute to neuroinflammatory processes [44] [45].
Advanced Inflammatory Indices
Beyond the fundamental ratios, more comprehensive inflammatory indices integrate three or more cell populations to provide enhanced prognostic value:
Systemic Immune-Inflammation Index (SII): Calculated as (platelet count × neutrophil count)/lymphocyte count. SII simultaneously reflects inflammation (neutrophils), immunity (lymphocytes), and thrombosis (platelets) [42] [45].
Systemic Inflammation Response Index (SIRI): Determined as (monocyte count × neutrophil count)/lymphocyte count. SIRI has demonstrated utility in assessing neuroinflammatory conditions including medication-overuse headache [42].
Aggregate Index of Systemic Inflammation (AISI): Calculated as (platelet count × neutrophil count × monocyte count)/lymphocyte count. AISI incorporates four distinct cell lineages to provide a comprehensive assessment of systemic inflammatory status [42].
Table 1: Inflammatory Ratios and Indices in Neurodegenerative Research
| Biomarker | Calculation | Cellular Components | Research Applications |
|---|---|---|---|
| NLR | Neutrophils/Lymphocytes | Innate vs. adaptive immunity | AD severity, AE ICU admission prediction [44] [45] |
| PLR | Platelets/Lymphocytes | Thrombosis & inflammation | AD risk stratification [45] |
| MLR | Monocytes/Lymphocytes | Phagocytic activation | AD, AE severity assessment [44] [45] |
| SII | (Platelets × Neutrophils)/Lymphocytes | Comprehensive inflammation | MOH diagnosis and phenotyping [42] |
| SIRI | (Monocytes × Neutrophils)/Lymphocytes | Myeloid inflammation | Correlation with medication days in MOH [42] |
| AISI | (Platelets × Neutrophils × Monocytes)/Lymphocytes | Global inflammation | Superior MOH diagnostic accuracy [42] |
Signaling Pathways and Mechanistic Insights
The following diagram illustrates the proposed pathways through which peripheral inflammation mediates central nervous system pathology in neurodegenerative diseases, highlighting the roles of NLR, PLR, and MLR as accessible biomarkers reflecting these processes.
Diagram 1: Peripheral-Central Inflammation Axis. This pathway illustrates how elevated peripheral inflammatory ratios contribute to neuroinflammation and neurodegeneration through blood-brain barrier disruption and microglial activation.
Research Applications in Neurodegenerative Diseases
Alzheimer's Disease and Cognitive Impairment
In Alzheimer's disease, peripheral inflammatory ratios show significant correlations with disease risk and cognitive impairment severity. A 2025 study involving 225 AD patients and 2000 healthy controls demonstrated that NLR, PLR, and MLR were independent risk factors for AD, with increased ratios associated with greater cognitive decline as measured by the Mini-Mental State Examination (MMSE) [45]. The systemic immune-inflammation index (SII) and systemic inflammation response index (SIRI) also showed significant elevations in AD patients, suggesting broader inflammatory network dysfunction [45].
The association between peripheral inflammation and AD pathology may be mediated by several mechanisms. Neutrophils from AD patients exhibit heightened activation, producing elevated levels of reactive oxygen species and correlating with faster cognitive decline [43]. Lymphocyte reductions may reflect impaired adaptive immunity, with specific T-cell subsets showing infiltration into AD brain regions near amyloid-beta plaques [43]. These peripheral inflammatory changes correlate with both amyloid burden and tau pathology, suggesting potential utility as complementary biomarkers to established CSF and imaging markers [43] [45].
Autoimmune Encephalitis and Neuroinflammatory Conditions
In autoimmune encephalitis, inflammatory ratios demonstrate strong correlations with disease severity and clinical outcomes. A 2025 multicenter study of 176 AE patients found significantly elevated SII, NLR, MLR, and PLR compared to healthy controls, with these markers showing positive correlations with the Clinical Assessment Scale for Autoimmune Encephalitis (CASE) and modified Rankin Scale (mRS) scores [44]. Notably, NLR emerged as the strongest predictor of intensive care unit admission, with an optimal cutoff value of 3.906 (AUC=0.701), outperforming other ratios for identifying severe cases requiring critical care intervention [44].
Table 2: Inflammatory Ratio Cutoffs and Predictive Values Across Neurological Disorders
| Condition | Biomarker | Cutoff Value | Clinical Utility | AUC/Performance |
|---|---|---|---|---|
| Autoimmune Encephalitis [44] | NLR | 3.906 | Predicts ICU admission | AUC=0.701 |
| Autoimmune Encephalitis [44] | SII | - | Correlates with CASE score | r=0.243, p=0.001 |
| Autoimmune Encephalitis [44] | MLR | - | Correlates with CASE score | r=0.242, p=0.001 |
| Alzheimer's Disease [45] | NLR | - | Independent AD risk factor | p<0.05 |
| Alzheimer's Disease [45] | MLR | - | Independent AD risk factor | p<0.05 |
| Alzheimer's Disease [45] | PLR | - | Independent AD risk factor | p<0.05 |
| Medication-Overuse Headache [42] | AISI | - | Superior MOH diagnosis | Better than SII/SIRI |
Medication-Overuse Headache and Pain Disorders
In medication-overuse headache, peripheral inflammation indices provide insights into disease mechanisms and clinical phenotypes. A 2025 study comparing 128 MOH patients with 132 controls found significantly elevated aggregate index of systemic inflammation (AISI) in MOH patients compared to healthy controls, while both MOH and episodic migraine patients showed elevated systemic inflammation response index (SIRI) [42]. These indices correlated positively with headache frequency, duration, and days per month with acute medication use, suggesting that peripheral inflammation may contribute to the transformation from episodic to chronic headache patterns [42]. The AISI demonstrated superior diagnostic performance for MOH compared to SII and SIRI, highlighting the value of multi-parameter inflammatory indices in chronic pain conditions [42].
Standardized Experimental Protocols
Blood Collection and Processing Methodology
Standardized protocols for sample collection and processing are essential for reliable measurement of inflammatory ratios. The following workflow outlines the key procedural steps based on methodologies from recent studies:
Diagram 2: Experimental Workflow for Inflammatory Ratio Analysis. This standardized protocol ensures consistent measurement of peripheral inflammatory biomarkers from blood collection to statistical analysis.
Based on established methodologies from recent studies [42] [44] [45], the following protocol details ensure reproducible measurement of inflammatory ratios:
Participant Preparation: Participants should fast for 8-10 hours prior to blood collection to minimize dietary influences on immune cell counts. For headache and migraine studies, samples should be collected during headache-free periods (interictal phases), while for neurodegenerative studies, consistency in collection time helps control for diurnal variation [42].
Blood Collection: Collect 3-5ml venous blood into EDTA-containing vacuum tubes to prevent coagulation. Invert tubes gently 8-10 times immediately after collection to ensure proper anticoagulant mixing without causing cell activation or hemolysis [44].
Sample Processing: Process samples within 2 hours of collection to maintain cell integrity. For studies requiring biobanking, aliquot samples and store at -80°C, though fresh analysis is preferred for complete blood count parameters. Avoid freeze-thaw cycles for cellular analysis [42] [44].
Automated Hematological Analysis: Use standardized automated hematology analyzers (e.g., Beckman Coulter systems, XN-9100) following manufacturer protocols and daily calibration. These systems utilize electrical impedance and flow cytometry principles to differentiate leukocyte subsets, providing absolute counts for neutrophils, lymphocytes, monocytes, and platelets [42] [44].
Quality Control: Implement internal quality control measures using commercial control materials at low, normal, and high values. Participate in external quality assurance programs to maintain inter-laboratory consistency. Exclude samples with hemolysis, lipemia, or clot formation [44].
Data Analysis and Statistical Approaches
Robust statistical methodology is essential for validating the clinical utility of inflammatory ratios:
Ratio Calculation: Calculate NLR, PLR, and MLR from absolute cell counts rather than relative percentages to enhance accuracy and reproducibility. For advanced indices, apply the following formulas:
Statistical Analysis: Assess normality of distribution using Kolmogorov-Smirnov or Shapiro-Wilk tests. For non-normally distributed ratios, apply log-transformation before parametric tests or use non-parametric alternatives (Mann-Whitney U, Kruskal-Wallis) [44] [45]. Employ Spearman correlation to examine relationships between inflammatory ratios and clinical severity scales. Use receiver operating characteristic (ROC) curve analysis to determine optimal cut-off values for disease discrimination, selecting thresholds that maximize the Youden index (sensitivity + specificity - 1) [44].
Multivariate Adjustment: In regression models, adjust for potential confounders including age, sex, body mass index, smoking status, and comorbidities such as hypertension and diabetes that may influence systemic inflammation [45]. For neurodegenerative studies, adjust for educational attainment when using cognitive outcomes [45].
Table 3: Essential Research Materials for Inflammatory Ratio Studies
| Category | Specific Products/Platforms | Application Notes |
|---|---|---|
| Blood Collection | EDTA Vacutainer tubes (Becton Dickinson) | Preferred anticoagulant for cellular morphology |
| Hematology Analyzers | Beckman Coulter DxH series, Sysmex XN-series, Abbott Cell-Dyn | Provide differential leukocyte counts via impedance & flow cytometry |
| Quality Control | Bio-Rad Liquichek Hematology Controls, Streck Cell Control | Ensure analytical precision across measurement range |
| Data Analysis | IBM SPSS, R Project, GraphPad Prism | Statistical analysis & ROC curve generation |
| Ultra-sensitive Platforms | NULISA CNS Disease Panel, SIMOA HD-1 Analyzer | Complementary high-sensitivity inflammatory markers [46] [47] |
Integration with Established Biomarker Platforms
While peripheral inflammatory ratios offer accessibility and cost-effectiveness, they demonstrate enhanced utility when integrated with established neuroinflammatory and neurodegenerative biomarkers. Advanced proteomic platforms such as the NULISA CNS Disease Panel enable simultaneous measurement of brain-derived proteins including phosphorylated tau217, neurofilament light chain (NfL), and glial fibrillary acidic protein (GFAP) at attomolar sensitivity [46] [47]. Combining inflammatory ratios with these specific CNS markers provides a more comprehensive assessment of neuroimmune interactions.
In Alzheimer's disease, elevated NLR correlates with amyloid burden and cognitive decline, complementing the diagnostic information provided by plasma p-tau217 and GFAP [43] [47] [45]. Similarly, in autoimmune encephalitis, inflammatory ratios may reflect disease activity alongside more specific autoantibody titers [44]. This multi-modal biomarker approach facilitates deeper insights into the peripheral-central inflammation axis, potentially enhancing patient stratification and treatment monitoring in clinical trials targeting neuroimmune mechanisms [48] [49].
Peripheral inflammatory ratios (NLR, PLR, MLR) and advanced indices (SII, SIRI, AISI) represent accessible, cost-effective biomarkers with established utility across neurodegenerative and neuroinflammatory conditions. Their correlations with disease severity, progression, and critical outcomes underscore the significance of systemic inflammation in central nervous system disorders. Standardized measurement protocols and appropriate statistical approaches ensure reproducible implementation in both research and clinical settings.
Future research directions should prioritize longitudinal studies examining inflammatory ratio dynamics throughout disease progression, interventional trials assessing ratio modulation in response to anti-inflammatory therapies, and multi-omics approaches integrating inflammatory ratios with genomic, transcriptomic, and proteomic data. As therapeutic development increasingly targets neuroimmune mechanisms in neurodegeneration, peripheral inflammatory ratios offer practical biomarkers for patient stratification, treatment response monitoring, and personalized intervention strategies.
Transcriptomic Approaches to Identify Novel Inflammatory Signatures
The role of neuroinflammation in neurodegenerative diseases such as Alzheimer's disease (AD), Parkinson's disease (PD), and amyotrophic lateral sclerosis (ALS) has transitioned from being considered a secondary consequence to a primary driver of disease pathogenesis [50]. Transcriptomic technologies now provide unprecedented capability to decode the complex inflammatory signatures underlying these conditions at cellular and molecular levels. These approaches can identify novel biomarkers for early diagnosis, patient stratification, and therapeutic target discovery [51].
The central nervous system exhibits a specialized immune environment where microglia, astrocytes, and other resident cells mediate inflammatory processes. Traditionally, inflammation was viewed merely as a response to protein aggregates like amyloid-β in AD or α-synuclein in PD. However, emerging evidence indicates that inflammatory signaling may precede pathological protein aggregation and actively contribute to disease progression [50]. This paradigm shift underscores the critical need for precise inflammatory profiling through transcriptomic technologies.
Advanced transcriptomic methods now enable researchers to move beyond single-marker analysis toward comprehensive inflammatory signatures that capture the complexity of neuroimmune responses. These signatures reflect dynamic, multi-faceted biological processes that cannot be adequately characterized by measuring individual cytokines or immune mediators [52]. The integration of transcriptomics with other omics technologies and AI-driven analytics is accelerating the discovery of robust inflammatory signatures with diagnostic, prognostic, and therapeutic applications.
Major Transcriptomic Technologies and Methodologies
Core Transcriptomic Platforms
Table 1: Key Transcriptomic Technologies for Inflammatory Signature Discovery
| Technology | Resolution | Key Applications in Neuroinflammation | Advantages | Limitations |
|---|---|---|---|---|
| Bulk RNA Sequencing | Tissue-level | Identifying overall inflammatory pathway dysregulation [51] | Cost-effective for large cohorts; Established analysis pipelines | Cannot resolve cellular heterogeneity; May miss rare cell populations |
| Single-Cell RNA Sequencing (scRNA-seq) | Single-cell | Revealing cell-type specific inflammatory responses [53] [54] | Unbiased cell classification; Identifies novel cell states | High cost; Technical noise; Complex computational analysis |
| Single-Nucleus RNA Sequencing | Single-nucleus | Studying inflammatory responses in frozen tissues [55] | Applicable to archived tissues; Reduces dissociation artifacts | Nuclear transcriptome only; May miss cytoplasmic transcripts |
| Spatial Transcriptomics | Tissue location + Gene expression | Mapping inflammatory gradients in tissue architecture [51] | Preserves spatial context; Links location to function | Lower resolution than scRNA-seq; Higher cost |
Experimental Workflow for scRNA-seq in Neuroinflammation
The standard workflow for single-cell transcriptomic analysis of inflammatory signatures involves multiple critical stages:
1. Sample Preparation and Quality Control
- Tissue dissociation: Optimal enzymatic digestion to preserve cell viability while generating single-cell suspensions [54]
- Cell viability assessment: Typically >80% viability required using trypan blue or automated cell counters
- Mitochondrial RNA filtering: Exclusion of cells with >10% mitochondrial UMIs to remove low-quality cells [56]
2. Library Preparation and Sequencing
- Platform selection: 10X Genomics Chromium system commonly used for high-throughput applications
- Sequence depth: Typically 50,000-100,000 reads per cell recommended for inflammatory gene detection
- Sample multiplexing: Using cell hashing or genetic barcoding to process multiple samples simultaneously
3. Computational Analysis Pipeline
- Quality control: Filtering of low-quality cells and doublets using tools like DoubletFinder [56]
- Normalization and integration: SCTransform for normalization and Harmony or Seurat integration for batch correction
- Clustering and annotation: Graph-based clustering followed by cell type identification using canonical markers
- Differential expression: Identification of inflammatory genes using MAST or Wilcoxon rank-sum tests
Analytical Frameworks and Computational Approaches
Dimensionality Reduction and Visualization
The high-dimensional nature of transcriptomic data requires sophisticated dimensionality reduction techniques to visualize and interpret inflammatory signatures:
- Principal Component Analysis (PCA): Linear dimensionality reduction that identifies major axes of variation in inflammatory gene expression [57]
- t-Distributed Stochastic Neighbor Embedding (t-SNE): Non-linear method that preserves local structure, useful for identifying distinct inflammatory cell states [57]
- Uniform Manifold Approximation and Projection (UMAP): Non-linear technique that preserves both local and global structure, increasingly used for scRNA-seq visualization [55]
These methods transform high-dimensional gene expression data into two or three dimensions that can be visualized to assess sample similarity, identify outliers, and detect batch effects. For inflammatory studies, they often reveal segregation of disease states based on immune activation patterns [57].
Machine Learning for Signature Identification
Machine learning approaches are essential for identifying robust inflammatory signatures from complex transcriptomic data:
Supervised Learning methods build predictive models that classify disease states based on inflammatory gene expression patterns. Support Vector Machines (SVM) with linear kernels can achieve >90% accuracy in distinguishing neurodegenerative disease states using carefully selected gene pairs [55]. Random Forest algorithms provide feature importance metrics that identify the most informative inflammatory genes for classification [57].
Unsupervised Learning approaches discover novel inflammatory patterns without pre-defined labels. Clustering algorithms identify distinct inflammatory endotypes that may respond differently to therapies [57]. Non-negative Matrix Factorization (NMF) decomposes gene expression matrices into metagenes that represent co-regulated inflammatory programs [57].
Bivariate and Multivariate Analysis moves beyond single-gene assessments to capture synergistic relationships between inflammatory mediators. This approach has revealed that combinations of inflammatory genes (e.g., KCNIP1, CA10, CSPG5) can classify AD with high accuracy even when individual genes show minimal differential expression [55].
Pathway and Network Analysis
Functional interpretation of inflammatory signatures requires pathway analysis to place gene expression changes into biological context:
- Gene Set Enrichment Analysis (GSEA): Identifies coordinated upregulation or downregulation of predefined inflammatory pathways
- Weighted Gene Co-expression Network Analysis (WGCNA): Constructs networks of co-expressed genes and links modules to inflammatory traits
- Cell-Cell Communication Inference: Tools like CellChat predict how inflammatory signals are communicated between different CNS cell types [56]
These analyses help determine whether identified inflammatory signatures represent activation of specific immune pathways such as cytokine-cytokine receptor interactions, NF-κB signaling, or interferon responses [54].
Key Inflammatory Signatures in Neurodegenerative Diseases
Alzheimer's Disease Inflammatory Profiles
Transcriptomic studies have revealed complex inflammatory alterations in AD that vary by disease stage and brain region:
CNS Compartment Inflammatory Signatures
- Microglial Activation Signature: Upregulation of TREM2, APOE, and CX3CR1 in disease-associated microglia [51]
- Astrocytic inflammatory Signature: Increased expression of GFAP and complement genes in reactive astrocytes [52]
- Neuron-Specific inflammatory Response: Elevated expression of danger-associated molecular patterns (DAMPs) and HLA genes [50]
CSF Inflammatory Signatures Multi-analyte profiling of cerebrospinal fluid has identified distinct inflammatory signatures with different clinical correlations:
- Protective Inflammatory Signature: Characterized by elevated sTREM2, sTyro3, sAXL, and YKL-40 associated with better cognitive outcomes and slower atrophy rates [58]
- Detrimental Inflammatory Signature: Marked by increased CRP, IL-18, and complement factors linked to greater gray matter volume loss and worse memory performance [58]
The protective signature is thought to represent a compensatory glial response that promotes clearance of pathological proteins, while the detrimental signature reflects maladaptive chronic inflammation that accelerates neurodegeneration [58].
Parkinson's Disease and ALS Inflammatory Patterns
In PD, transcriptomic analyses have identified:
- Dopaminergic Neuron inflammatory Signature: Upregulation of MHC class I molecules and inflammatory mediators in vulnerable neurons [50]
- Microglial inflammatory Activation: Increased expression of IL-1β, TNF-α, and NLRP3 inflammasome components [51]
- Peripheral Immune Involvement: T-cell recruitment signatures and altered lymphocyte trafficking genes
In ALS, single-cell transcriptomics has revealed:
- Motor Neuron inflammatory Signature: Elevated expression of inflammatory response genes and stress pathways in vulnerable motor neurons [51]
- Glial inflammatory Contribution: Distinct inflammatory profiles in microglia and astrocytes that vary with disease progression [51]
- Endothelial inflammatory Activation: Vascular inflammatory changes that may compromise blood-brain barrier integrity
Cross-Disease Inflammatory Signatures
Comparative transcriptomic analyses have identified both shared and distinct inflammatory signatures across neurodegenerative conditions:
- Common Neurodegenerative inflammatory Signature: Upregulation of innate immune genes, complement components, and cytokine signaling across AD, PD, and ALS [59]
- Disease-Specific inflammatory Patterns: Unique inflammatory programs associated with specific protein pathologies (Aβ, tau, α-synuclein, TDP-43) [59]
- APOE ε4-Associated inflammatory Signature: Consistently observed inflammatory profile linked to APOE ε4 carriership across multiple neurodegenerative diseases [59]
Table 2: Experimentally-Defined Inflammatory Cell States in Neurodegeneration
| Cell Type | Inflammatory State | Key Marker Genes | Functional Role | Associated Disease |
|---|---|---|---|---|
| Disease-Associated Microglia | Neuroprotective | TREM2, APOE, LPL, SPP1 | Phagocytic clearance; Tissue repair [58] | Alzheimer's disease |
| Neuroinflammatory Microglia | Detrimental | IL1B, TNF, NLRP3, CCL2 | Chronic inflammation; Synapse loss [50] | Alzheimer's, Parkinson's |
| Reactive Astrocyte A1 | Detrimental | C3, SERPING3, H2-T23 | Complement activation; Neurotoxicity [50] | Alzheimer's, ALS |
| Reactive Astrocyte A2 | Protective | S100A10, PTX3, TM4SF1 | Tissue repair; Synapse support [50] | Alzheimer's, ALS |
| Inflammatory Endothelial Cells | Detrimental | SPP1, CCL2, ESAM [53] | Neutrophil recruitment; Barrier disruption | Vascular dementia |
Integration with Multi-Omics and Validation Approaches
Multi-Omics Integration Strategies
Transcriptomic inflammatory signatures gain biological context when integrated with other molecular data types:
Genomics-Transcriptomics Integration combines GWAS risk variants with expression quantitative trait loci (eQTLs) to identify functional mechanisms of neurodegenerative disease risk genes. This approach has revealed that many AD risk genes are highly expressed in microglia and show inflammatory regulation [51].
Proteomics-Transcriptomics Integration correlates transcriptomic inflammatory signatures with proteomic measurements to identify which inflammatory changes translate to protein level alterations. Large-scale proteomic studies have confirmed inflammatory pathway activation in neurodegenerative diseases and identified potential fluid biomarkers [59].
Epigenomics-Transcriptomics Integration links inflammatory gene expression changes to epigenetic modifications such as DNA methylation and chromatin accessibility, providing mechanistic insights into inflammatory gene regulation in neurodegeneration.
Experimental Validation of Transcriptomic Findings
Transcriptomic discoveries require rigorous validation through orthogonal methods:
Functional Validation Approaches
- Spatial Validation: RNAscope or immunohistochemistry to confirm localization of inflammatory signatures [56]
- Cell-Based Assays: Primary glial cultures or iPSC-derived models to test inflammatory pathway activation
- CRISPR Screens: Functional validation of identified inflammatory genes using CRISPR-based perturbation [51]
Analytical Validation Considerations
- Cross-Study Validation: Assessing inflammatory signature reproducibility across independent cohorts [55]
- Platform Consistency: Verifying signatures across different transcriptomic technologies (RNA-seq, microarrays) [55]
- Longitudinal Stability: Evaluating whether inflammatory signatures remain consistent across disease stages
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Transcriptomic Inflammation Studies
| Reagent Category | Specific Examples | Research Application | Considerations for Inflammation Studies |
|---|---|---|---|
| Single-Cell Isolation Kits | 10X Genomics Chromium Next GEM, Parse Biosciences Evercode | High-throughput single-cell partitioning for scRNA-seq [54] | Optimize for CNS tissue; Preserve RNA from fragile inflammatory cells |
| Library Preparation Kits | SMART-Seq v4, Nextera XT | cDNA amplification and sequencing library construction [54] | Maintain representation of inflammatory transcripts; Avoid 3' bias |
| Cell Surface Protein Detection | CITE-seq antibodies, TotalSeq barcoded antibodies | Simultaneous protein and RNA measurement at single-cell level | Include immune cell markers (CD45, CD11b, TREM2) for inflammatory characterization |
| Spatial Transcriptomics Platforms | 10X Visium, Nanostring GeoMx Digital Spatial Profiler | Gene expression analysis in tissue context [51] | Preserve tissue architecture for inflammatory gradient analysis |
| Bulk RNA-seq Library Kits | Illumina TruSeq Stranded mRNA, KAPA mRNA HyperPrep | Cost-effective transcriptional profiling of bulk tissue | Sufficient sequencing depth to detect low-abundance inflammatory mediators |
| qPCR Validation Assays | TaqMan Gene Expression Assays, SYBR Green reagents | Orthogonal validation of transcriptomic findings | Focus on key inflammatory signature genes; Use multiple reference genes |
| Bcl-2-IN-2 | Bcl-2-IN-2, MF:C48H57N7O7S, MW:876.1 g/mol | Chemical Reagent | Bench Chemicals |
| Chroman 1 dihydrochloride | Chroman 1 dihydrochloride, MF:C24H30Cl2N4O4, MW:509.4 g/mol | Chemical Reagent | Bench Chemicals |
Signaling Pathways in Neuroinflammatory Responses
Transcriptomic studies have consistently implicated specific inflammatory signaling pathways in neurodegenerative diseases:
Microglial Activation Pathways
- TREM2 Signaling: TREM2-DAP12 interactions activate SYK phosphorylation, leading to inflammatory gene expression and phagocytic activity [58]
- Complement Cascade: C1q, C3, and C4 upregulation promotes synaptic pruning and inflammatory activation [58]
- NF-κB Pathway: Central inflammatory signaling hub activated by diverse neurodegeneration-associated stimuli [50]
Cytokine and Chemokine Signaling
- Interleukin Signaling: IL-1β, IL-6, and IL-18 show altered expression patterns with disease-specific profiles [58]
- Chemokine Networks: CCL2, CCL3, CCL4, and CX3CL1 coordinate immune cell recruitment and microglial activation [54]
- JAK-STAT Pathway: Activation observed in specific T-cell populations and glial cells in neurodegenerative contexts [54]
Pattern Recognition Receptor Signaling
- Toll-like Receptor Pathways: TLR2, TLR4, and TLR7 activation by neurodegeneration-associated molecular patterns [50]
- Inflammasome Activation: NLRP3 inflammasome upregulation drives IL-1β and IL-18 processing in microglia [50]
Challenges, Limitations, and Future Directions
Technical and Analytical Challenges
Several significant challenges remain in the application of transcriptomic approaches to inflammatory signature discovery:
Technical Variability and Standardization
- Sample Processing Effects: Inflammatory genes are particularly sensitive to post-mortem intervals and tissue processing methods [52]
- Batch Effects: Technical artifacts can introduce spurious inflammatory signatures that require careful normalization [55]
- Platform Differences: Inconsistent results across transcriptomic platforms (microarray vs. RNA-seq) complicate meta-analyses [55]
Biological Complexity and Interpretation
- Cellular Heterogeneity: Inflammatory responses vary dramatically between cell subtypes and disease stages [52]
- Spatial Organization: Traditional single-cell methods lose critical information about inflammatory gradients and cellular neighborhoods [51]
- Temporal Dynamics: Cross-sectional studies cannot capture the evolution of inflammatory responses throughout disease progression [52]
Emerging Technologies and Future Applications
Several promising developments are poised to advance inflammatory signature research:
Spatial Multi-omics technologies that combine transcriptomic, proteomic, and epigenomic data within tissue architecture will provide unprecedented views of inflammatory processes in situ [51].
Longitudinal Sampling approaches using biofluids or novel in vivo monitoring techniques will enable tracking of inflammatory dynamics throughout disease progression.
Single-Cell Multi-omics methods that simultaneously measure transcriptome, epigenome, and surface proteins from the same cells will comprehensively characterize inflammatory cell states [51].
AI-Driven Discovery using explainable artificial intelligence approaches will identify complex, non-linear inflammatory signatures that escape conventional statistical methods [57] [55].
As these technologies mature and standardization improves, transcriptomic approaches will increasingly enable the identification of clinically relevant inflammatory signatures for diagnosis, prognosis, and treatment selection in neurodegenerative diseases. The integration of inflammatory signatures into the AT(I)N research framework represents a critical step toward precision medicine approaches for neurodegenerative disorders [52].
Imaging and Fluid Biomarkers for Neuroinflammatory Monitoring
Neuroinflammation, characterized by glial cell activation and blood-brain barrier (BBB) dysfunction, is a critical pathological process in aging and neurodegenerative diseases such as Alzheimer's disease (AD) and Parkinson's disease (PD). Advanced in vivo imaging modalities and fluid biomarkers now allow for the precise monitoring of these inflammatory events. This technical review details the methodologies and applications of key imaging techniques, including TSPO-PET and dynamic contrast-enhanced MRI, and fluid biomarkers from cerebrospinal fluid and blood. We provide standardized protocols, quantitative comparisons, and visual workflows to serve as a comprehensive resource for researchers and drug development professionals working to validate therapeutic targets and monitor treatment responses in the central nervous system.
Neuroinflammation involves a complex immune response within the central nervous system (CNS), typically triggered by injury, infection, or protein aggregates [60]. Under physiological conditions, the brain parenchyma is protected by the blood-brain barrier. However, in neurodegenerative diseases, this barrier can become dysfunctional, and the activation of glial cells (microglia and astrocytes) drives a chronic inflammatory state that contributes to neuronal damage and cognitive decline [61]. The growing recognition that neuroinflammation is a key feature of conditions like AD, PD, and multiple sclerosis (MS) has spurred the development of tools to quantify these processes in living patients. The integration of neuroinflammatory biomarkers into a broader framework, such as the ATN (Amyloid, Tau, Neurodegeneration) classification for AD, allows for a more granular, biological definition of disease that is crucial for the development of targeted immune therapies [62].
Imaging Biomarkers of Neuroinflammation
In-vivo imaging of neuroinflammation provides spatial and quantitative data on glial activation and BBB integrity. The primary modalities are positron emission tomography (PET) and magnetic resonance imaging (MRI), each offering distinct advantages.
Translocator Protein PET (TSPO-PET)
TSPO-PET is a molecular imaging technique that targets the 18-kDa translocator protein (TSPO), which is significantly upregulated in activated microglia.
Experimental Protocol:
- Tracer Administration: A radiolabeled TSPO ligand (e.g.,
[11C]PK11195,[11C]PBR28,[18F]GE-180) is administered intravenously. - Image Acquisition: Dynamic PET scanning is performed over 60-90 minutes post-injection.
- Input Function: Arterial blood sampling is often used to measure the plasma input function for accurate kinetic modeling.
- Image Reconstruction & Kinetic Modeling: Images are reconstructed, and time-activity curves are extracted from regions of interest. The simplified reference tissue model (SRTM) or Logan graphical analysis is applied to derive the non-displaceable binding potential (BP
ND), a measure of specific tracer binding. - Genotyping: Prior TSPO genotyping (for the rs6971 polymorphism) is essential, as it affects binding affinity and must be accounted for in quantitative analysis [61].
- Tracer Administration: A radiolabeled TSPO ligand (e.g.,
Key Findings: TSPO-PET studies have demonstrated increased glial activation in AD, particularly in regions like the temporal and parietal cortex, often correlating with cognitive decline. In MS, TSPO-PET signals are elevated in active lesions and normal-appearing white matter [61].
Magnetic Resonance Imaging (MRI) Protocols
MRI offers a non-invasive, radiation-free method for assessing structural and functional consequences of neuroinflammation, with a focus on BBB permeability.
Dynamic Contrast-Enhanced MRI (DCE-MRI):
- Purpose: Quantifies subtle BBB leakage.
- Protocol:
- Pre-contrast T1 Mapping: A baseline T1 relaxometry map is acquired.
- Contrast Agent Injection: A bolus of gadolinium-based contrast agent is administered.
- Dynamic Acquisition: A time-series of T1-weighted images is acquired over 10-15 minutes.
- Pharmacokinetic Modeling: The concentration-time curve in tissue and a vascular input function (from a major artery like the internal carotid) are fitted to a model, such as the Patlak model, to calculate the transfer constant
Ktrans(minâ»Â¹), which reflects BBB permeability [61] [60].
- Key Findings: DCE-MRI has revealed age-related BBB dysfunction in the hippocampus and gray matter, which is more pronounced in Mild Cognitive Impairment (MCI) and AD, independent of amyloid-β and tau pathology [60].
Additional MRI Techniques:
- Diffusion Tensor Imaging (DTI): Measures white matter microstructural integrity; changes in fractional anisotropy (FA) and mean diffusivity (MD) can indicate axonal damage and edema associated with inflammation.
- Magnetic Resonance Spectroscopy (MRS): Quantifies metabolic markers like myo-inositol (a putative glial marker) and choline, which can be elevated in neuroinflammatory states.
- Resting-State Functional MRI (rs-fMRI): Assesses functional connectivity between brain networks, which can be disrupted by inflammatory processes [60].
Table 1: Summary of Key Imaging Biomarkers for Neuroinflammation
| Biomarker / Technique | Measured Parameter | Biological Process | Key Findings in Aging/AD |
|---|---|---|---|
| TSPO-PET | Non-displaceable Binding Potential (BPND) |
Microglial Activation | Elevated in temporal/parietal cortex in AD; correlates with cognitive decline [61]. |
| DCE-MRI | Transfer Constant (Ktrans) |
BBB Permeability | Increased in hippocampus and gray matter in aging, MCI, and AD [60]. |
| DTI | Fractional Anisotropy (FA), Mean Diffusivity (MD) | White Matter Integrity | Reduced FA in aging and AD, indicating microstructural damage linked to inflammation [60]. |
| MRS | myo-Inositol (mIns), Choline (Cho) | Glial Activation, Membrane Turnover | Elevated mIns and Cho in AD brain regions [60]. |
The following workflow diagram illustrates the standard experimental pipeline for assessing neuroinflammation using multi-modal imaging.
Fluid Biomarkers of Neuroinflammation
Fluid biomarkers, derived from cerebrospinal fluid (CSF) and blood, offer a less invasive means to monitor neuroinflammatory pathways and have shown high diagnostic accuracy.
Core Cerebrospinal Fluid (CSF) Biomarkers
CSF is an optimal biofluid due to its proximity to the brain parenchyma.
- Sample Collection: Lumbar puncture at the L2–L3 or L3–L4 interspace to collect CSF [62].
- Analysis: Biomarker levels are typically measured using enzyme-linked immunosorbent assay (ELISA) or, increasingly, fully automated, high-throughput immunoassays [62].
Blood-Based Biomarkers
Recent advances have enabled the reliable measurement of brain-derived proteins in plasma, offering a more accessible and scalable option.
- Sample Collection: Standard venipuncture to collect plasma or serum.
- Analysis: Ultrasensitive single-molecule array (Simoa) technology is often used to detect low-abundance neurological biomarkers [63].
Table 2: Key Fluid Biomarkers for Neuroinflammatory Monitoring
| Biomarker | Biofluid | Biological Significance | Research Findings |
|---|---|---|---|
| sTREM2 (Soluble Triggering Receptor Expressed on Myeloid cells 2) | CSF | Microglial Activation & Function | Elevated in AD CSF; associated with reduced brain atrophy and slower cognitive decline, suggesting a potentially protective response [62]. |
| GFAP (Glial Fibrillary Acidic Protein) | CSF, Plasma | Astrocytic Activation (Astrogliosis) | Plasma GFAP is elevated in AD and predicts conversion from MCI to AD dementia; correlates with amyloid-PET positivity [63] [62]. |
| YKL-40 (CHI3L1) | CSF | Astrocytic & Microglial Activation, Innate Immunity | CSF YKL-40 levels are increased in AD and MCI and correlate with cortical thinning and disease progression [62]. |
| Neurofilament Light Chain (NfL) | CSF, Plasma | Axonal Damage & Neurodegeneration | A robust marker of neuronal injury; elevated in many neurological disorders; blood levels correlate strongly with CSF levels [63] [62]. |
The logical relationship between inflammatory triggers, biomarker release, and detection in biofluids is summarized in the following pathway diagram.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Neuroinflammation Biomarker Analysis
| Reagent / Material | Function / Application | Example Specifics |
|---|---|---|
| TSPO PET Tracers | Radioligands for in vivo quantification of microglial activation via PET. | [11C]PK11195, [18F]GE-180; requires TSPO genotyping for subject stratification [61]. |
| Gadolinium-Based Contrast Agents | T1-shortening agents for visualizing and quantifying BBB leakage in DCE-MRI. | Gadoterate meglumine; used to calculate the transfer constant Ktrans [61] [60]. |
| Anti-TREM2 Antibodies | Capture/detection antibodies for measuring soluble TREM2 (sTREM2) in CSF via ELISA. | Critical for investigating the role of TREM2 signaling in microglial function [62]. |
| Anti-GFAP Antibodies | Key reagents for immunoassays quantifying GFAP levels in CSF and plasma. | Used in ELISA and Simoa assays; plasma GFAP is a promising astrocyte-derived biomarker for AD [62]. |
| Ultrasensitive Immunoassay Kits | Platforms for quantifying low-abundance neurological biomarkers in blood. | Simoa (Quanterix) and ELLA (ProteinSimple) kits for NfL, GFAP, p-tau [63] [62]. |
| APOE ε4 Genotyping Assays | Genetic analysis to account for major risk factor in AD study design and data analysis. | PCR-based kits; essential for patient stratification as APOE ε4 status influences inflammation and BBB breakdown [60] [62]. |
| Tinlorafenib | Tinlorafenib|BRAF Kinase Inhibitor|For Research Use | Tinlorafenib is a potent, selective, and brain-penetrant BRAF V600E inhibitor for cancer research. For Research Use Only. Not for human use. |
| BR351 precursor | BR351 precursor, MF:C27H32N2O8S2, MW:576.7 g/mol | Chemical Reagent |
The convergence of advanced imaging and fluid biomarker technologies has fundamentally advanced our ability to monitor neuroinflammation in vivo. TSPO-PET and DCE-MRI provide spatial and quantitative insights into glial activation and BBB integrity, while CSF and plasma biomarkers like GFAP, sTREM2, and NfL offer accessible tools for screening and longitudinal tracking. Future progress hinges on methodological standardization, longitudinal multi-modal studies, and the validation of these biomarkers in the context of immune-targeted therapeutic trials. This integrated approach is paving the way for a new era of personalized medicine in neurodegenerative diseases, where neuroinflammatory profiles can guide targeted interventions in at-risk populations.
The investigation of inflammatory responses in neurodegenerative diseases such as Alzheimer's disease (AD) requires a sophisticated hierarchy of model systems, each offering distinct advantages and limitations. This whitepaper provides an in-depth technical guide to the progression from traditional animal models to advanced 3D co-culture platforms, with a specific focus on modeling neuroinflammation. We detail experimental protocols for inducing and quantifying inflammatory responses, summarize quantitative outcomes across different models, and visualize key signaling pathways disrupted in neurodegeneration. Furthermore, we present a structured toolkit of research reagents and materials essential for implementing these sophisticated model systems, equipping researchers with practical resources for studying inflammatory mechanisms in neurological diseases.
Model systems for studying neurodegenerative diseases have evolved significantly, driven by the need to better recapitulate the complex human pathophysiology of conditions like Alzheimer's disease (AD), Parkinson's disease (AD), and amyotrophic lateral sclerosis (ALS). Neuroinflammation has emerged as a critical driver of pathogenesis in these disorders, characterized by glial activation, release of pro-inflammatory cytokines, and subsequent neuronal damage [64]. This inflammatory cascade contributes to increased oxidative stress, synaptic dysfunction, and neuronal apoptosis, making it a prime target for therapeutic intervention.
The choice of model system profoundly influences the translational potential of research findings. Traditional two-dimensional (2D) cell cultures provide a simplified and controllable environment but suffer from disadvantages associated with the loss of tissue-specific architecture, mechanical and biochemical cues, and cell-to-cell and cell-to-matrix interactions [65]. Animal models offer an intact physiological system but present species-dependent sensitivity differences that can impede interpretation of preclinical outcomes [64]. Three-dimensional (3D) cell culture technologies have emerged as a powerful intermediate, better mimicking in vivo physiology by restoring morphological, functional, and microenvironmental features of human tissues [65]. Particularly promising are recent developments in microglia-containing organoid models that enable the study of dynamic neuroinflammatory states and their impact on AD progression [64].
Table: Evolution of Model Systems in Neurodegeneration Research
| Model System | Key Advantages | Major Limitations | Utility for Neuroinflammation Studies |
|---|---|---|---|
| 2D Cell Cultures | Easy to use, highly controllable, amenable to high-throughput screening | Lack tissue context, simplified cell interactions, poor predictor for certain drug responses | Useful for initial mechanistic studies on inflammatory signaling pathways |
| Animal Models | Intact physiological system, complex cellular interactions, behavioral assessment | Species differences, ethical concerns, high cost, time-consuming | Enable study of systemic inflammation and its impact on brain pathology |
| 3D Cultures (Spheroids/Organoids) | In vivo-like architecture and cellular interactions, human cell-derived, recapitulate protein aggregation | Can be variable, lack vasculature, may lack key cell types, challenging for high-throughput screening | Ideal for modeling neuroimmune interactions; patient-derived organoids develop AD hallmarks |
| Advanced Co-culture Platforms | Recapitulate tumor immune microenvironment, autologous settings, high-content imaging | Complex to establish, requires specialized expertise, can be costly | Enable study of patient-specific tumor-immune interactions; test immunotherapiums |
Experimental Protocols for Modeling Neuroinflammation
LPS-Induced Neuroinflammation in SH-SY5Y Cells
The lipopolysaccharide (LPS)-induced inflammation model offers a well-established approach for investigating AD-related neuroinflammation. LPS is a potent Toll-like receptor 4 (TLR4) signaling activator that reliably induces neuroinflammation through upregulation of pro-inflammatory cytokines [64].
Cell Culture and Treatment Protocol:
- Cell Line: SH-SY5Y human neuroblastoma cell line, utilized as a neuronal model to examine cellular responses to LPS-induced neuroinflammation.
- Culture Conditions: Maintain cells in Dulbecco's Modified Eagle Medium (DMEM) supplemented with 10% fetal bovine serum (FBS), 100 U/mL penicillin, and 100 µg/mL streptomycin at 37°C in a humidified atmosphere with 5% CO₂.
- Seeding Density: Plate cells at a density of 1 × 10ⶠcells/well in 6-well plates and allow to adhere overnight.
- Inflammation Induction: Treat SH-SY5Y cells with LPS at various concentrations (0.1, 0.5, 1, and 5 µg/mL) for different durations (6, 12, 24, and 48 hours). Control cells receive an equivalent volume of sterile phosphate-buffered saline (PBS).
Primary Cortical Neuron Isolation and Culture
To enhance the relevance of findings, primary cortical neurons can be isolated from newborn Sprague-Dawley rats (postnatal days 0-2) and cultured under sterile conditions.
Isolation and Culture Protocol:
- Animal Sourcing and Euthanasia: Source animals from a certified breeding facility. Perform euthanasia via rapid decapitation using sterile surgical scissors for neonatal pups (P0-2), following approved IACUC protocols.
- Tissue Processing: Enzymatically digest cortical tissues with 0.25% trypsin-EDTA at 2.5 mg/mL, supplemented with 0.1 mg/mL DNase I to prevent cell clumping. Perform digestion for 15 minutes at 37°C, followed by trituration.
- Plating and Maintenance: Plate cells on poly-D-lysine-coated dishes in Neurobasal medium supplemented with 2% B27, 0.5 mM L-glutamine, 100 U/mL penicillin, and 100 µg/mL streptomycin.
- Experimental Timeline: Use neurons for experiments after 7-10 days in vitro (DIV), when significant dendritic development is evident.
Establishment of 3D Co-culture Platforms
The TumorGraft3D co-culture platform represents a novel approach for modeling complex tissue environments, leveraging organoids from patient-derived xenograft models with matching immune cells.
Co-culture Establishment Protocol:
- Organoid Generation: Generate patient-derived xenograft organoids from surgical resections.
- Immune Cell Expansion: Expand tumor-infiltrating lymphocytes (TILs) using standard Rapid Expansion protocol.
- Co-culture Setup: Embed organoids with immune cells in autologous settings to maintain patient-specific characteristics.
- Analysis Methodologies: Employ 3D confocal analysis for deep evaluation of cancer-immune cellular interaction at the single-cell level. Develop a staining system allowing differentiation of cancer-immune cell spatial distribution and cellular death, complemented by proprietary pipelines for image analysis to evaluate tumor infiltration and drug cytotoxicity.
Quantitative Data Analysis in Model System Validation
Rigorous quantitative analysis is essential for validating model systems and interpreting experimental results. Statistical comparison between models helps determine the significance of observed differences and strengthens research conclusions.
Table: Quantitative Effects of LPS-Induced Neuroinflammation on SH-SY5Y Cells
| Parameter Measured | Control Conditions | LPS-Treated Conditions | Significance Level | Measurement Technique |
|---|---|---|---|---|
| Cell Viability | Normalized to 100% | Dramatically lowered | p < 0.001 | MTT assay, ATP-based assays |
| BDNF Levels | Baseline expression | Considerable decrease | p < 0.01 | ELISA, Western Blot |
| Pro-inflammatory Cytokines | ||||
| IL-6 | Low baseline | Considerable elevation | p < 0.001 | ELISA, Multiplex immunoassays |
| TNF-α | Low baseline | Considerable elevation | p < 0.001 | ELISA, Multiplex immunoassays |
| Inflammatory Mediators | ||||
| COX-2 | Low baseline | Elevated levels | p < 0.01 | Western Blot, Immunocytochemistry |
| iNOS | Low baseline | Elevated levels | p < 0.01 | Western Blot, Immunocytochemistry |
| Signaling Kinases | Baseline expression | Altered expression | p < 0.05 | Gene expression analysis, Western Blot |
Statistical Analysis Framework: For comparative analysis between experimental conditions, employ hypothesis testing with a significance level (α) typically set at 0.05. The t-test is appropriate for comparing means between two groups, with the formula:
[ t = \frac{\bar{X}1 - \bar{X}2}{sp \sqrt{\frac{1}{n1} + \frac{1}{n_2}}} ]
where (\bar{X}1) and (\bar{X}2) are sample means, (sp) is the pooled standard deviation, and (n1) and (n_2) are sample sizes. Prior to t-test analysis, perform an F-test to compare variances between datasets:
[ F = \frac{s1^2}{s2^2} \quad (\text{where } s1^2 \geq s2^2) ]
If the calculated t-statistic exceeds the critical value, or the p-value (P(T<=t) two-tail) is less than 0.05, the null hypothesis (no difference between groups) can be rejected, indicating a statistically significant difference [66].
Signaling Pathways in Neuroinflammation
LPS-induced neuroinflammation disrupts multiple critical signaling pathways in neuronal models. The following diagram illustrates key pathways affected in SH-SY5Y cells and primary neurons following LPS exposure, highlighting connections between inflammatory triggers and neuronal dysfunction.
LPS-Induced Neuroinflammatory Signaling Pathways
This graphical representation illustrates how LPS activation of TLR4 signaling triggers NFκB-mediated transcription of pro-inflammatory cytokines (IL-6, TNF-α), which subsequently suppress neuroprotective BDNF and alter key kinase pathways (PKA, AKT, MAPK), ultimately leading to reduced neuronal viability and synaptic dysfunction [64].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of advanced model systems requires specific reagents and materials optimized for 3D culture and inflammation research. The following table details essential components for establishing these platforms.
Table: Essential Research Reagents for Neuroinflammation Models
| Reagent/Material | Function/Application | Example Specifications | Key Considerations |
|---|---|---|---|
| SH-SY5Y Cell Line | Human neuroblastoma model for neuronal signaling and inflammatory responses | Purchased from cell repositories (e.g., Pasteur Institute) | Does not naturally express AD-specific pathology but responds to inflammatory stimuli |
| Lipopolysaccharide (LPS) | Potent TLR4 agonist to induce neuroinflammation | Various concentrations (0.1-5 µg/mL) for 6-48 hours | Species-dependent sensitivity differences; concentration and timing critical |
| Dulbecco's Modified Eagle Medium (DMEM) | Basal medium for cell culture | Supplemented with 10% FBS, penicillin/streptomycin | Standard for 2D culture; may require modification for 3D systems |
| Neurobasal Medium | Optimized for primary neuron culture and viability | Supplemented with B27, L-glutamine | Supports neuronal growth without excessive glial proliferation |
| Extracellular Matrix Substitutes | Support 3D culture structure and signaling | Matrigel, collagen, synthetic hydrogels | Lot-to-lot variability; complex composition influences cell behavior |
| Cytokine Analysis Kits | Quantify inflammatory mediators (IL-6, TNF-α) | ELISA, multiplex immunoassays | Sensitivity must match expected concentration ranges |
| 3D Confocal Imaging Reagents | Visualize spatial relationships in co-cultures | Live-cell dyes, immunofluorescence labels | Must penetrate 3D structure; photobleaching concerns |
| Cdk12-IN-4 | Cdk12-IN-4|CDK12 Inhibitor|For Research Use | Cdk12-IN-4 is a potent, selective CDK12 inhibitor for cancer research. It is for research use only and not for human or veterinary diagnostic or therapeutic use. | Bench Chemicals |
| Tubulin inhibitor 8 | Tubulin inhibitor 8, MF:C21H14N2O3, MW:342.3 g/mol | Chemical Reagent | Bench Chemicals |
The progression from traditional animal models to advanced 3D co-culture platforms represents a paradigm shift in how researchers model inflammatory responses in neurodegenerative diseases. Each model system offers distinct advantages: animal models provide physiological complexity, 3D cultures offer human-relevant architecture, and co-culture platforms enable the study of dynamic cell-cell interactions within a patient-specific context. The LPS-induced neuroinflammation model in SH-SY5Y cells serves as a valuable tool for deciphering molecular mechanisms underlying inflammatory responses, particularly the disruption of BDNF signaling and kinase pathways. However, researchers must carefully consider the limitations of each system when designing experiments and interpreting results. As the field advances, the integration of patient-derived cells, functional immune components, and sophisticated readout technologies in 3D co-culture platforms will enhance the translational relevance of preclinical findings, potentially accelerating the development of effective therapies for neurodegenerative diseases with inflammatory components.
Integrating Multi-Omics Data for Comprehensive Inflammatory Profiling
The complexity of inflammatory responses in neurodegenerative diseases necessitates moving beyond single-layer biological analyses. Multi-omics integration combines genomic, transcriptomic, proteomic, and metabolomic data to provide a systems-level understanding of neuroinflammation, revealing interconnected molecular networks that drive disease progression. In Alzheimer's disease (AD), integrating genome-wide association studies (GWAS), transcriptome-wide association studies (TWAS), and proteome-wide association studies (PWAS) has identified novel contributions to disease pathology that would remain hidden in single-omics approaches [67]. This unified framework enables researchers to dissect the intricate interplay between genetic predisposition, gene expression dysregulation, and protein-level alterations that collectively orchestrate neuroinflammatory processes.
The analytical power of multi-omics approaches is particularly valuable for decoding the heterogeneous nature of neuroinflammation in neurodegenerative conditions. Recent studies deploying these methods have revealed that inflammatory responses in AD involve highly specialized cellular states and signaling pathways that vary significantly between patients and disease stages [68]. By simultaneously visualizing multiple omics datasets on metabolic network diagrams, researchers can paint different molecular datasets onto distinct visual channels of biological pathway maps, creating integrated views of inflammatory mechanisms [69]. This capability transforms our ability to identify critical regulatory nodes within inflammatory networks that may serve as therapeutic targets for precision medicine approaches in neurodegeneration.
Key Inflammatory Pathways in Neurodegeneration Revealed by Multi-Omics
Central Inflammatory Signaling Networks
Multi-omics studies have systematically mapped core inflammatory pathways that drive neurodegeneration, with the JAK-STAT, PI3K-Akt, and MAPK signaling cascades emerging as central regulatory networks [70]. These pathways form interconnected circuits that coordinate neuroimmune responses across different CNS cell types. The JAK-STAT pathway has been identified as a key factor promoting neuroinflammation in AD, influenced by excessive activation of microglia and astrocytes [68]. Simultaneously, NF-κB signaling, a recognized inflammatory transcription factor, is activated in multiple cell types in the AD brain and induces transcription of TNF-α, IL-6 and other inflammatory mediators [68]. These pathways collectively construct a complex cytokine network that significantly impacts neuronal and vascular function.
Multi-omics integration has further revealed the critical role of the TREM2 signaling pathway in microglial metabolic reprogramming, plaque encapsulation, and inflammation regulation [68]. The NLRP3 inflammasome has been identified as another crucial component in AD-related pathology, where it induces interleukin-18 (IL-18) or interleukin-1β (IL-1β) to enhance disease progression [68]. These findings illustrate how multi-omics approaches can connect genetic risk factors with functional inflammatory outcomes, providing a more complete understanding of neuroinflammatory pathogenesis beyond what single-omics analyses can achieve.
Cellular Mediators of Neuroinflammation
Single-cell RNA sequencing (scRNA-seq) technologies have revolutionized our understanding of cellular heterogeneity in neuroinflammatory processes, enabling high-resolution profiling of diverse cell states within the CNS [68]. Disease-associated microglia (DAM) represent a transcriptionally distinct state first identified in the 5xFAD mouse model, showing Trem2 dependence and upregulation of Apoe, Lpl, Cst7, and Itgax genes [68]. Reactive astrocytes with altered A1/A2 subtype balance, infiltrating peripheral immune cells including CD8+ T cells, and endothelial cells with compromised blood-brain barrier function collectively contribute to the neuroinflammatory landscape in neurodegeneration [68].
Table 1: Key Inflammatory Cell Types in Neurodegeneration Identified via Multi-Omics
| Cell Type | Transcriptional Signatures | Functional Role in Inflammation | Identification Method |
|---|---|---|---|
| Disease-associated microglia (DAM) | TREM2-dependent, upregulated APOE, LPL, CST7, ITGAX | Phagocytic clearance, plaque encapsulation, inflammatory modulation | scRNA-seq of 5xFAD and human AD brain tissues [68] |
| Pro-inflammatory astrocytes | A1/A2 imbalance, complement component expression | Synaptic pruning, blood-brain barrier disruption, cytokine secretion | Integrated scRNA-seq and bulk transcriptomics [68] |
| Infiltrating CD8+ T cells | CXCL10/CXCR3 axis activation, interferon-γ signaling | Microglial activation, neuronal damage, adaptive immune response | scRNA-seq of human AD brain tissues [68] |
| Vascular endothelial cells | Altered junctional protein expression, adhesion molecules | Blood-brain barrier permeability, immune cell infiltration | Spatial transcriptomics and scRNA-seq integration [68] |
Methodological Framework for Multi-Omics Integration
Experimental Design and Data Generation
Robust multi-omics integration begins with systematic experimental design and rigorous data generation protocols. For inflammatory profiling in neurodegeneration, studies should incorporate data from multiple molecular layers, including genomic variants, transcriptomic profiles, proteomic measurements, and metabolomic readings. In a recent comprehensive analysis of Alzheimer's disease, researchers conducted genome-, transcriptome-, and proteome-wide association studies on 15,480 individuals from the Alzheimer's Disease Sequencing Project R4 (ADSP) to identify AD-associated inflammatory signals [67]. This approach ensures sufficient statistical power to detect meaningful associations across molecular domains while accounting for technical and biological variability.
Quality control procedures must be implemented at each omics level to ensure data reliability. For genomic data, this includes variant name standardization, removal of variants failing laboratory-based QC filters, exclusion of intentionally duplicated samples, and application of thresholds for minor allele count (MAC < 20), variant call rate (≥99%), and sample call rate (≥95%) [67]. For transcriptomic and proteomic data, similar rigorous quality metrics must be established, including normalization procedures, batch effect correction, and outlier detection. These standardized protocols ensure that subsequent integration approaches yield biologically meaningful insights rather than technical artifacts.
Data Integration and Analytical Approaches
Multi-omics data integration employs both sequential and simultaneous analytical approaches to extract meaningful biological insights. Sequential integration begins with univariate association analyses within each molecular layer, followed by integration through pathway enrichment or machine learning models. For inflammatory profiling, researchers first conduct GWAS to identify genetic variants associated with neuroinflammatory phenotypes, followed by TWAS to map expression quantitative trait loci (eQTLs) and PWAS to identify protein-level associations [67]. This sequential approach reveals how genetic variation influences inflammatory processes through regulatory effects on gene and protein expression.
Simultaneous integration approaches combine multiple omics datasets into unified analytical frameworks, often employing multivariate statistical models or machine learning algorithms. Random forest classifiers with transcriptomic and clinical covariate features have demonstrated superior performance in predicting neuroinflammatory risk, achieving area under the receiver operating characteristic (AUROC) of 0.703 and area under the precision-recall curve (AUPRC) of 0.622, significantly outperforming polygenic score models and baseline covariates [67]. These integrated models more accurately capture the complex, non-linear relationships between molecular features and inflammatory outcomes, providing enhanced predictive power for clinical applications.
Multi-Omics Analytical Workflow
Visualization and Interpretation of Multi-Omics Data
Pathway-Centric Visualization Approaches
Effective visualization is crucial for interpreting complex multi-omics data within inflammatory pathways. Tools like PathVisio enable simultaneous visualization of different omics data types on biological pathway diagrams by mapping distinct molecular measurements to specific visual attributes [71]. In this approach, transcriptomics data might be displayed by coloring reaction arrows, proteomics data as arrow thickness, and metabolomics data as metabolite node colors [69]. This multi-channel visualization allows researchers to identify coordinated changes across molecular layers within their biological context, revealing how genetic variants influence inflammatory responses through transcriptomic and proteomic alterations.
Interactive web-based metabolic charts that depict reactions, pathways, and metabolites provide powerful platforms for multi-omics visualization [69]. These tools employ automated graphical layout algorithms to generate pathway diagrams that can be painted with multiple omics datasets. Semantic zooming functionality provides increasing levels of detail as users zoom in, while animation capabilities enable visualization of time-course data to capture dynamic inflammatory processes. The ability to interactively adjust data value ranges to color and thickness mappings further enhances the interpretability of complex inflammatory networks across omics layers.
Data Preparation for Multi-Omics Visualization
Proper data formatting is essential for successful multi-omics visualization. Datasets should be combined into a single file with appropriate database identifiers and data type specifications [71]. The standard format includes columns for identifier, system code, quantitative values (e.g., log2 fold change), statistical measures (e.g., p-values), and data type (e.g., transcriptomics, proteomics) [71]. This structured approach ensures accurate mapping of diverse molecular measurements to their corresponding entities within biological pathways.
Table 2: Essential Research Reagent Solutions for Multi-Omics Inflammatory Profiling
| Reagent/Resource | Function | Application Example |
|---|---|---|
| ADSP R4 Dataset | Provides harmonized genomic, transcriptomic, and proteomic data from diverse population | Genome-wide association studies for inflammatory gene discovery [67] |
| GTEx Project v8 eQTL Models | Enables transcriptome-wide association studies through tissue-specific expression reference | Mapping genetic variants to inflammatory gene expression in CNS tissues [67] |
| PathVisio with PMMP Plugins | Biological pathway analysis and multi-omics data visualization | Painting transcriptomic and proteomic data onto neuroinflammatory pathways [71] |
| scRNA-seq Platforms (10x Genomics) | Single-cell resolution transcriptomic profiling | Identification of novel inflammatory cell states in neurodegeneration [68] |
| PrediXcan Software | Imputation of transcriptome-wide gene expression from genetic data | TWAS for inflammatory gene prioritization [67] |
| MASHR Models | Multivariate adaptive shrinkage for eQTL effect size estimation | Improved precision in mapping genetic regulation of inflammatory genes [67] |
Signaling Pathways in Neuroinflammation
Key Inflammatory Cascades in Neurodegeneration
Multi-omics studies have systematically identified several interconnected signaling cascades that drive neuroinflammation in conditions like Alzheimer's disease. The JAK-STAT pathway emerges as a central regulator, influenced by excessive activation of microglia and astrocytes in response to inflammatory stimuli [68]. Simultaneously, the NF-κB pathway functions as a master inflammatory transcription factor that becomes activated across multiple CNS cell types, driving the expression of pro-inflammatory cytokines including TNF-α and IL-6 [68]. These pathways form a coordinated signaling network that amplifies and sustains neuroinflammatory responses throughout disease progression.
The TREM2 signaling pathway plays a critical role in microglial responses to neurodegenerative pathology, regulating metabolic reprogramming, plaque encapsulation, and inflammation modulation [68]. Complementing this pathway, the NLRP3 inflammasome has been identified as a crucial mediator of AD-related pathology, facilitating the maturation and secretion of pro-inflammatory cytokines IL-18 and IL-1β [68]. Multi-omics integration reveals how genetic risk variants in these pathways (e.g., TREM2 R47H mutation) alter cellular responses to amyloid deposition and tau pathology, creating self-reinforcing inflammatory cycles that accelerate disease progression.
Neuroinflammatory Signaling Network
Cross-Talk Between Inflammatory and Cellular Metabolic Pathways
Multi-omics approaches have revealed extensive interactions between inflammatory signaling and cellular metabolic pathways in neurodegenerative conditions. Pathway enrichment analyses of integrated GWAS, TWAS, and PWAS data consistently identify cholesterol metabolism and immune signaling pathways as co-regulated processes in Alzheimer's disease [67]. These integrated analyses demonstrate how inflammatory activation reprograms cellular metabolism to support the energetic and biosynthetic demands of immune responses, while simultaneously revealing how metabolic disturbances can trigger or amplify neuroinflammation.
The application of semantic technologies, including ontologies and knowledge graphs, further enhances our ability to map these complex interactions across molecular scales [72]. These computational approaches facilitate the integration of diverse data types by establishing standardized frameworks for representing biological knowledge, enabling more sophisticated queries across multi-omics datasets. By representing inflammatory pathways as interconnected networks rather than linear cascades, these methods capture the multidimensional nature of neuroinflammation and its metabolic relationships, providing a more comprehensive foundation for identifying therapeutic intervention points.
Validation and Functional Characterization
Experimental Validation of Multi-Omics Discoveries
Candidate discoveries from multi-omics analyses require rigorous experimental validation to establish their functional roles in inflammatory processes. For identified inflammatory miRNAs, this involves combining candidate molecules (e.g., miR-339-3p, miR-28-3p, miR-423-3p, miR-144-5p) and assessing their effects on neuronal and inflammatory markers [70]. Functional validation demonstrates that miRNA combinations can significantly reduce AD marker expression while promoting neuronal progenitor cell marker expression, though effects on mature neuronal markers (MAP2, NeuN) may be limited without appropriate neuronal environmental cues [70]. This approach confirms the therapeutic potential of multi-omics-derived targets while highlighting the importance of cellular context in functional outcomes.
Cell-based assays using primary microglial cultures, astrocyte cultures, and neuronal models provide essential platforms for validating the functional consequences of multi-omics discoveries. For inflammatory pathway components identified through integrated analyses, manipulation through genetic approaches (CRISPR, RNAi) or pharmacological inhibitors in these cellular systems can establish causal relationships between molecular targets and inflammatory phenotypes [70]. These validation experiments bridge the gap between computational predictions and biological mechanisms, transforming correlative associations from multi-omics studies into validated regulatory components of neuroinflammatory processes.
Translational Applications for Targeted Therapeutics
The ultimate goal of multi-omics inflammatory profiling is to identify novel therapeutic opportunities for neurodegenerative diseases. Integrative analyses have revealed treatment frameworks that combine immunomodulation with neuroregeneration strategies, addressing both the inflammatory drivers and neuronal consequences of neurodegeneration [70]. This dual approach recognizes that successful interventions must not only suppress maladaptive neuroinflammation but also support neuronal integrity and function in the inflammatory environment.
Multi-omics data further enables patient stratification based on molecular subtypes, facilitating precision medicine approaches that match therapeutic strategies to individual inflammatory profiles [68]. AI-driven analytics integrated with multi-omics platforms enhance the identification of patient-specific molecular signatures that predict treatment responsiveness, potentially explaining the variable outcomes observed in clinical trials of anti-inflammatory therapies for neurodegenerative conditions [68]. This personalized approach to targeting neuroinflammation represents a paradigm shift from one-size-fits-all interventions to tailored strategies based on comprehensive molecular profiling.
Therapeutic Challenges: Navigating Roadblocks in Anti-Inflammatory Drug Development
Blood-Brain Barrier Penetration and Targeted CNS Delivery
The blood-brain barrier (BBB) represents one of the most significant challenges in developing therapeutics for central nervous system (CNS) disorders, particularly neurodegenerative diseases. This highly selective cellular interface strictly regulates molecular exchange between the bloodstream and brain parenchyma, protecting the CNS from toxins and pathogens while maintaining homeostasis [73]. However, the BBB's remarkable protective function also prevents more than 98% of small-molecule drugs and nearly 100% of large-molecule therapeutics from reaching the brain [74] [73]. This limitation severely compromises treatment efficacy for neurodegenerative diseases such as Alzheimer's disease (AD), Parkinson's disease (PD), and amyotrophic lateral sclerosis (ALS) [75] [74].
The growing recognition of neuroinflammation as a fundamental component in neurodegenerative disease pathogenesis further underscores the critical need for effective BBB-penetrating therapeutics [50]. Chronic neuroinflammation, characterized by activated microglia and astrocytes along with elevated cytokine levels, contributes significantly to neuronal damage and disease progression [76] [50]. This technical guide comprehensively addresses current strategies, methodologies, and experimental approaches for overcoming the BBB challenge, with particular emphasis on their application within neuroinflammatory contexts of neurodegenerative disease research.
Blood-Brain Barrier Structure and Function in Health and Disease
Physiological Composition of the BBB
The BBB functions as a multicellular vascular unit composed primarily of brain microvascular endothelial cells (BMECs), pericytes, astrocytes, and the basement membrane [74] [73]. BMECs form the core physical barrier through tight junctions (TJs) comprising proteins such as claudins, occludin, and zonula occludens (ZO) proteins, which create continuous cellular connections that eliminate fenestrations and significantly reduce paracellular permeability [77] [73]. These specialized endothelial cells exhibit markedly reduced pinocytotic activity compared to peripheral endothelial cells and contain increased mitochondrial content to support energy-dependent regulatory functions [78] [73].
Pericytes embedded within the basement membrane play crucial roles in BBB development, maintenance, and regulation through the secretion of signaling factors including vascular endothelial growth factor (VEGF) and transforming growth factor-beta (TGF-β) [77] [73]. Astrocytic end-feet processes extensively envelop the brain vasculature, releasing soluble factors that promote and maintain the barrier phenotype of endothelial cells [77] [74]. Together, these components form the neurovascular unit, which dynamically regulates CNS homeostasis.
Molecular Transport Mechanisms Across the BBB
The BBB facilitates controlled molecular exchange through several specialized transport mechanisms:
- Paracellular diffusion: Restricted to small hydrophilic molecules under 400 Da due to tight junction integrity [73].
- Transcellular passive diffusion: Allows passage of small lipophilic molecules (typically <500 Da) with favorable physicochemical properties [74] [73].
- Carrier-mediated transcytosis (CMT): Utilizes specific transporters (e.g., GLUT1 for glucose, LAT1 for large neutral amino acids) for essential nutrients [74].
- Receptor-mediated transcytosis (RMT): Enables selective uptake of macromolecules via specific receptors (e.g., transferrin receptor, insulin receptor) [74] [73].
- Adsorptive-mediated transcytosis (AMT): Involves electrostatic interactions between cationic molecules and anionic membrane microdomains [74].
- Cell-mediated transcytosis: Allows transport of certain immune cells that can carry therapeutic cargo [74].
Active efflux transporters, particularly P-glycoprotein (P-gp) and multidrug resistance-associated proteins (MRPs), significantly limit brain penetration of many therapeutic compounds by actively extruding substrates back into the bloodstream [74] [73].
BBB Dysfunction in Neurodegenerative Diseases
In neurodegenerative conditions, the BBB undergoes significant pathological changes that alter its structure and function. Neuroinflammation drives activation of brain endothelial cells, disruption of tight junctions, and increased BBB permeability [78] [74]. Proinflammatory cytokines such as TNF-α and IL-1β contribute to TJ protein downregulation and enhanced leukocyte adhesion and infiltration [78] [50]. The BBB's role as a signaling interface becomes compromised, potentially allowing increased passage of neurotoxic substances from the periphery while reducing efficient clearance of CNS metabolites [78].
Damage-associated molecular patterns (DAMPs) released during neurodegeneration, including HMGB1, S100 proteins, and ATP, activate pattern recognition receptors (PRRs) such as Toll-like receptors (TLRs) on CNS resident cells, perpetuating neuroinflammatory cycles [76] [50]. This inflammatory environment further damages BBB integrity, creating a vicious cycle of neurodegeneration and barrier dysfunction.
Computational Approaches for Predicting BBB Permeability
In Silico Screening and Machine Learning Models
Recent advances in computational-aided drug development (CADD) have enabled high-throughput screening of BBB-permeable compounds through machine learning and deep learning approaches [75]. These in silico techniques utilize physicochemical properties and structure-activity relationships to predict BBB permeability and CNS activity during early drug discovery phases [75]. Key molecular descriptors considered include molecular weight, lipophilicity (LogP), polar surface area (PSA), hydrogen bonding capacity, and charge characteristics [74] [79].
Pharmacophore-based virtual screening tools such as Pharmit, ChemMine, and Swiss Similarity employ Tanimoto similarity scoring to identify structurally similar molecules to known CNS-active compounds from databases including PubChem, DrugBank, and ChEMBL [75]. These approaches allow researchers to rapidly screen large chemical libraries before committing to resource-intensive experimental work.
Solubility-Diffusion Model for Passive Permeability Prediction
The solubility-diffusion model (SDM) provides a valuable framework for predicting intrinsic passive BBB permeability (Pâ‚€,BBB) based on a molecule's physicochemical properties [79]. This approach models passive membrane permeation as a process of partitioning into and diffusion through lipid membranes, which can be predicted using hexadecane/water partition coefficients estimated by computational methods such as COSMOtherm and Linear Solvation Energy Relationship (LSER) approaches [79].
Table 1: Key Parameters for Predicting Passive BBB Permeability
| Parameter | Ideal Range for BBB Permeability | Experimental Correlation |
|---|---|---|
| Molecular Weight | <500 Da | Direct correlation with Caco-2/MDCK permeability [79] |
| Lipophilicity (LogP) | 2-5 | SDM predictions show RMSE = 1.32-1.93 for small molecules [79] |
| Polar Surface Area | <60-70 Ų | Critical for passive transcellular diffusion [74] |
| Hydrogen Bond Count | <6 | Limited H-bond donors/acceptors enhance permeability [74] |
| Charge | Neutral or positive at physiological pH | Cationic compounds may utilize AMT [74] |
Studies demonstrate that Pâ‚€,BBB values show strong correlation with Caco-2 and MDCK permeability measurements (RMSE = 0.86; N = 34), validating these cell-based assays as reliable predictors of passive BBB penetration [79]. Notably, research has found no clear evidence for an absolute molecular size cutoff for BBB permeability when using the appropriate SDM framework [79].
Experimental Models for Assessing BBB Permeability
In Vitro BBB Models
In vitro BBB models offer controlled, reproducible systems for evaluating drug permeability while reducing animal use. These range from simple monocultures of brain endothelial cells to more complex multicellular systems incorporating pericytes and astrocytes [77] [80].
Transwell Model Protocol:
- Culture primary brain endothelial cells, pericytes, and astrocytes on opposite sides of porous membrane inserts (0.4-3.0 μm pore size) [77] [80]
- Monitor transendothelial electrical resistance (TEER) using volt-ohm meter with chopstick electrodes
- Validate barrier integrity with permeability tracers (e.g., sodium fluorescein, Evans blue-labeled albumin)
- Apply test compounds to donor compartment and measure appearance in receiver compartment over time
- Calculate permeability coefficient: Papp = (dQ/dt) / (A × C₀), where dQ/dt is transport rate, A is membrane area, and C₀ is initial donor concentration [77]
Microfluidic Model Protocol (from Nature Protocols) [80]:
- Fabricate microfluidic devices with adjacent channels separated by porous membrane
- Seed brain endothelial cells in vascular channel and astrocytes/pericytes in brain parenchymal channel
- Perfuse channels with appropriate medium at physiological shear stress (1-10 dyn/cm²)
- Allow 5-7 days for barrier maturation with continuous perfusion
- Measure permeability using fluorescent tracers and computational image analysis
- Extract RNA/protein for expression analysis of TJ proteins and transporters
These advanced microfluidic models replicate physiological shear stress conditions and demonstrate permeability values within the range expected in vivo, providing more clinically relevant data than traditional static models [80].
In Vivo and Imaging Approaches
In vivo methods remain essential for validating BBB permeability under physiological conditions. Quantitative imaging techniques provide non-invasive assessment of BBB integrity in real-time.
Quantitative Ultrashort Time-to-Echo Contrast Enhanced (QUTE-CE) MRI Protocol [81]:
- Acquire baseline 3D-UTE MRI images prior to contrast administration
- Administer intravenous bolus of ferumoxytol (6 mg/ml Fe) tailored to individual subject weight
- Acquire 7 consecutive post-contrast scans with parameters: TE = 13 μs, TR = 4 ms, flip angle = 20°
- Process images with motion correction and spatial alignment algorithms
- Register images to 3D brain atlas with 118 segmented anatomical regions
- Calculate BBB permeability biomarker as slope of cerebral blood volume (CBV) vs. time curve
- Perform statistical analysis with repeated measures ANOVA and linear regression
This methodology has demonstrated sensitivity to detect BBB permeability changes following mild head impacts in prefrontal cortex, basal ganglia, hippocampus, amygdala, and brainstem regions [81]. The technique offers advantages over traditional dynamic contrast-enhanced MRI with gadolinium-based agents, which carry FDA black-box warnings for brain retention [81].
Strategic Approaches for CNS Drug Delivery
Formulation Strategies
Advanced drug delivery systems have emerged as promising solutions for enhancing brain exposure to therapeutic compounds:
Nanoparticle Systems:
- Liposomes: Spherical phospholipid bilayers that encapsulate hydrophilic and hydrophobic drugs, enabling surface modification with targeting ligands [74]
- Polymer nanoparticles: Biodegradable polymeric matrices (e.g., PLGA, chitosan) that provide controlled release and functionalization capabilities [76] [74]
- Inorganic nanoparticles: Metal/metal oxide particles, silica nanoparticles, and quantum dots with tailored surface chemistry [73]
- Biomass-derived materials: Exosomes, cell membranes, and other biological vesicles with innate targeting properties [73]
These nanocarriers improve CNS delivery through multiple mechanisms, including enhanced permeability at sites of BBB disruption, receptor-mediated transcytosis following surface functionalization, and protection from efflux transporters [76] [74] [73].
Classification of Targeting Strategies:
- Passive targeting: Relies on inherent physicochemical properties of nanocarriers and the enhanced permeability and retention (EPR) effect at sites of BBB disruption [74]
- Active targeting: Utilizes surface-bound ligands (antibodies, peptides, aptamers) that engage specific receptors on BBB endothelial cells to initiate RMT [74] [73]
Permeability Enhancement Technologies
Stimuli-Responsive Systems: Stimuli-responsive nanoparticles release their payload or undergo structural changes in response to specific triggers:
- Internal stimuli: pH, enzyme concentration, redox status [73]
- External stimuli: focused ultrasound, magnetic fields, light [73]
Focused ultrasound combined with microbubbles represents a particularly promising approach for localized, reversible BBB disruption. This technique uses acoustic energy to induce temporary opening of tight junctions, enabling enhanced drug delivery to targeted brain regions [76] [73].
Intranasal Administration: The intranasal route bypasses the BBB completely by delivering therapeutics directly to the CNS via the olfactory and trigeminal neural pathways [73]. This method offers non-invasive access to the brain while minimizing systemic exposure and associated side effects.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Research Reagents for BBB and Neuroinflammation Studies
| Reagent/Material | Function/Application | Example Use Cases |
|---|---|---|
| Primary Brain Microvascular Endothelial Cells | Core component of in vitro BBB models | Establishing monoculture and coculture BBB systems [77] [80] |
| Astrocytes and Pericytes | Essential supporting cells for neurovascular unit | Creating physiologically relevant multicellular BBB models [77] [80] |
| Transwell Inserts | Permeable supports for barrier formation | Measuring transendothelial electrical resistance and compound flux [77] [80] |
| TEER Measurement System | Quantitative assessment of barrier integrity | Validating BBB model quality and monitoring barrier disruption [77] |
| Claudin-5, Occludin, ZO-1 Antibodies | Tight junction protein detection | Immunofluorescence and Western blot analysis of BBB integrity [77] [73] |
| P-gp/ABCB1 Substrates (e.g., Rhodamine 123) | Efflux transporter activity assessment | Characterizing functional transporter expression in BBB models [74] [73] |
| Ferumoxytol | MRI contrast agent for permeability studies | Non-invasive BBB permeability measurement using QUTE-CE MRI [81] |
| Fluorescent Dextrans | Permeability tracers of varying sizes | Evaluating paracellular permeability in BBB models [80] [81] |
| Microfluidic Platforms | Physiologically relevant flow models | Creating more authentic BBB models with shear stress [80] |
| Cytokine Panels (TNF-α, IL-1β, IL-6) | Neuroinflammation assessment | Quantifying inflammatory responses in BBB models [76] [50] |
Signaling Pathways in Neuroinflammation and BBB Dysfunction
The relationship between neuroinflammation and BBB dysfunction involves multiple interconnected signaling pathways. The following diagram illustrates key neuroinflammatory signaling pathways that impact BBB integrity in neurodegenerative diseases:
Key Neuroinflammatory Signaling Pathways Impacting BBB Integrity
This diagram illustrates the vicious cycle of neuroinflammation and BBB dysfunction in neurodegenerative diseases. DAMPs/PAMPs initiate the cascade through PRR engagement, leading to NF-κβ activation and pro-inflammatory cytokine production [76] [50]. These inflammatory mediators disrupt tight junctions, enhance leukocyte infiltration, and activate glial cells, which further amplifies cytokine production [78] [50]. The resulting BBB dysfunction contributes to neuronal damage, which releases additional DAMPs, perpetuating the neuroinflammatory cycle [78] [50].
Integrated Experimental Workflow for CNS Drug Development
The following diagram presents a comprehensive workflow for screening and evaluating BBB-permeable neurotherapeutics:
Integrated CNS Drug Development Workflow
This integrated workflow begins with computational approaches to screen large compound libraries, followed by progressive experimental validation [75]. Promising candidates advance through increasingly complex models, from in vitro systems to in vivo validation, with continuous refinement based on performance data [75] [80]. This systematic approach increases the likelihood of successful CNS drug development while efficiently allocating resources.
Effective BBB penetration remains a critical hurdle in developing therapeutics for neurodegenerative diseases, particularly given the central role of neuroinflammation in their pathogenesis. A multifaceted approach combining computational prediction, advanced in vitro modeling, and innovative delivery technologies offers the most promising path forward. The integration of physiologically relevant human BBB models with targeted nanocarrier systems represents a particularly exciting avenue for future research. As our understanding of BBB biology in neurodegenerative diseases continues to evolve, so too will our ability to design effective CNS therapeutics that can modulate neuroinflammatory processes and ultimately alter disease progression.
Balancing Neuroprotective and Detrimental Immune Modulation
Neuroinflammation is a ubiquitous hallmark across the spectrum of neurological disorders, from chronic neurodegenerative diseases like Alzheimer's disease (AD) and Parkinson's disease (PD) to acute central nervous system (CNS) injuries [82] [50]. This dynamic immune response within the CNS is primarily controlled by microglia, the brain's resident macrophages, which comprise approximately 5-10% of all glial cells [82]. Under physiological conditions, microglia maintain CNS homeostasis through continuous environmental surveillance, performing essential functions including synaptic pruning, clearance of cellular debris, and trophic support to neurons [82] [83]. However, when confronted with pathogenic stimuli such as protein aggregates, infections, or tissue damage, microglia undergo rapid activation and functional phenotypic changes [82].
The persistence and chronicity of neuroinflammation determines its ultimate impact on neuronal health. Unlike self-limiting acute inflammation that resolves once threats are eliminated, chronic neuroinflammation represents a maladaptive immune state that drives progressive neuronal dysfunction and degeneration [50] [83]. This sustained inflammatory environment arises from complex interactions between CNS-resident cells and infiltrating peripheral immune cells, creating a feedback loop that perpetuates tissue damage [83]. Understanding how to balance the neuroprotective and detrimental aspects of this immune modulation represents a critical frontier in developing effective therapies for neurodegenerative diseases.
Microglial Polarization: Metabolic Regulation of Functional Phenotypes
The Metabolic Basis of Microglial Activation States
Microglia exhibit remarkable phenotypic plasticity, dynamically shifting between different functional states in response to environmental cues [82]. The traditional binary classification of microglial activation has evolved to recognize a continuum of functional states, with two broadly defined poles:
Pro-inflammatory (M1-like) Phenotype: Characterized by release of neurotoxic mediators including reactive oxygen species (ROS), nitric oxide, and pro-inflammatory cytokines such as TNF-α [82]. This state demonstrates reliance on aerobic glycolysis for rapid ATP generation, even in oxygen-rich environments [82]. The glycolytic burst supports immediate effector functions but can lead to accumulation of metabolic intermediates like succinate that further amplify inflammatory responses through pathways including the NLRP3 inflammasome [82].
Anti-inflammatory/Resolving (M2-like) Phenotype: Associated with production of anti-inflammatory cytokines, enhanced phagocytic capacity, and tissue repair functions [82]. This state preferentially utilizes oxidative phosphorylation (OXPHOS) and fatty acid oxidation (FAO) to support energy-intensive processes like pathogen clearance and damage resolution [82]. Recent single-cell and spatial transcriptomics reveal more nuanced microglial states within this continuum, including Disease-Associated Microglia (DAM) in AD and Lipid-Droplet-Accumulating Microglia (LDAM) in aging, both driven by underlying metabolic reprogramming [82].
Table 1: Characteristics of Microglial Phenotypic States
| Feature | Pro-inflammatory (M1-like) | Anti-inflammatory/Resolving (M2-like) |
|---|---|---|
| Primary Metabolic Pathway | Aerobic glycolysis | OXPHOS/Fatty acid oxidation |
| Key Metabolic Regulators | HIF-1α, mTOR | AMPK, PGC-1α |
| Characteristic Outputs | TNF-α, IL-1β, ROS, nitric oxide | IL-10, TGF-β, growth factors |
| Primary Functions | Pathogen defense, neurotoxicity | Phagocytosis, tissue repair, inflammation resolution |
| Role in Disease | Drives neuronal damage | Promotes resolution and repair |
Metabolic Sensors as Phenotypic Switches
The transition between microglial phenotypes is intrinsically regulated by key metabolic sensors that interpret the cellular energy status and environmental cues:
AMPK (AMP-activated protein kinase): Functions as a master regulator of cellular energy homeostasis. Activated under conditions of energy depletion (high AMP:ATP ratio), AMPK promotes catabolic pathways including FAO and OXPHOS, steering microglia toward anti-inflammatory, resolving phenotypes [82]. AMPK activation enhances mitochondrial biogenesis and phagocytic capacity, supporting the metabolic demands of tissue repair.
mTOR (mechanistic target of rapamycin): Integrates signals from growth factors, nutrients, and cellular energy status to promote anabolic processes. mTOR activation drives glycolytic metabolism and supports pro-inflammatory microglial polarization [82]. The reciprocal regulation between AMPK and mTOR creates a metabolic switch that determines microglial functional orientation.
HIF-1α (Hypoxia-inducible factor 1-alpha): Stabilized under hypoxic conditions but also activated by inflammatory stimuli in normoxia. HIF-1α acts as a master regulator of glycolytic gene expression, reinforcing the glycol metabolic program of pro-inflammatory microglia [82]. HIF-1α signaling promotes the production of various inflammatory mediators, creating a feed-forward loop that sustains inflammatory responses.
The interplay between these metabolic sensors creates a sophisticated regulatory network that coordinates microglial functional states with metabolic programming, positioning metabolic reprogramming as a determining factor in microglial phenotype and function [82].
Neuroinflammatory Signaling Pathways in Neurodegeneration
Key Inflammatory Pathways in Alzheimer's Disease
In Alzheimer's disease, the pathological hallmarks of amyloid-β (Aβ) plaques and neurofibrillary tangles (composed of hyperphosphorylated tau) engage in a complex interplay with neuroinflammatory processes [50]. Aβ aggregates act as damage-associated molecular patterns (DAMPs), binding to pattern recognition receptors including Toll-like receptors (TLRs), receptor for advanced glycation end products (RAGE), and NOD-like receptors (NLRs) on microglia [50]. This receptor engagement triggers downstream signaling cascades including NF-κB and MAPK pathways, driving production of pro-inflammatory cytokines and creating a chronic inflammatory milieu [50].
The relationship between protein pathology and neuroinflammation demonstrates bidirectional reinforcement. Initially, activated microglia attempt to clear Aβ deposits through phagocytosis, but chronic activation leads to impaired clearance capacity and sustained release of neurotoxic mediators [50]. Microglial activation provides a critical link between Aβ pathology and tau hyperphosphorylation, with inflammatory signaling promoting the formation of neurofibrillary tangles [50]. Additionally, neurons burdened with soluble oligomeric Aβ exhibit early inflammatory profiles, suggesting neuroinflammation may precede insoluble plaque formation in disease pathogenesis [50].
Diagram 1: Neuroinflammatory Signaling in Alzheimer's Disease
Inflammatory Mechanisms in Parkinson's Disease
Parkinson's disease pathology is characterized by the accumulation of α-synuclein aggregates forming Lewy bodies and progressive loss of dopaminergic neurons in the substantia nigra [50]. Similar to Aβ in AD, α-synuclein aggregates function as DAMPs, activating microglial pattern recognition receptors and initiating neuroinflammatory responses [50]. The vulnerability of dopaminergic neurons to inflammatory-mediated damage is particularly relevant to PD pathogenesis, with evidence suggesting that neuroinflammatory processes may begin decades before clinical motor symptoms emerge [50].
The sustained microglial activation in PD creates a self-reinforcing cycle where inflammatory mediators promote further α-synuclein aggregation and spread, while aggregated α-synuclein perpetuates microglial activation [50]. This cyclic relationship between protein pathology and neuroinflammation shares mechanistic similarities with AD while exhibiting disease-specific features related to the unique vulnerability of dopaminergic signaling pathways.
Experimental Methodologies for Studying Neuroimmune Balance
Assessing Microglial Phenotypic and Metabolic States
Comprehensive evaluation of microglial function requires integrated methodological approaches spanning molecular, metabolic, and functional analyses:
Metabolic Profiling: Direct assessment of microglial metabolic preferences can be performed through extracellular flux analysis to measure glycolytic rates and oxygen consumption rates (OCR). This approach enables real-time monitoring of the shift between glycolytic and OXPHOS metabolism in response to polarizing stimuli [82]. Complementary techniques include stable isotope tracing to track nutrient utilization through specific metabolic pathways.
Transcriptomic and Proteomic Analysis: Single-cell RNA sequencing enables resolution of microglial heterogeneity and identification of distinct activation states in pathological conditions [82]. Proteomic profiling through mass spectrometry-based approaches quantifies expression of inflammatory mediators, surface receptors, and metabolic enzymes, providing multi-dimensional characterization of microglial phenotypes.
Functional Assays: Phagocytic capacity can be quantified using pH-sensitive fluorescent beads or assay kits measuring uptake of labeled substrates [82]. Production of reactive oxygen species is measurable using fluorescent probes like DCFDA or MitoSOX for mitochondrial-specific ROS. Cytokine secretion profiles are typically determined by ELISA or multiplex bead-based arrays for comprehensive inflammatory mediator quantification.
Imaging Approaches: Live-cell imaging of microglial morphology and dynamic responses provides insights into functional states, while immunofluorescence of brain sections allows spatial assessment of microglial activation in relation to pathological hallmarks [82]. Advanced techniques including PET imaging with TSPO ligands enable non-invasive monitoring of microglial activation in vivo, though challenges remain in distinguishing protective versus detrimental activation states [82].
Table 2: Key Methodologies for Assessing Neuroimmune Balance
| Method Category | Specific Techniques | Primary Applications | Key Output Parameters |
|---|---|---|---|
| Metabolic Assessment | Extracellular flux analysis, Stable isotope tracing, Metabolic inhibitor studies | Determination of glycolytic vs OXPHOS preference, Metabolic flexibility | OCR, ECAR, ATP production rates, Nutrient oxidation |
| Molecular Profiling | scRNA-seq, Nanostring, Western blot, ELISA, Multiplex immunoassays | Phenotype characterization, Inflammatory mediator quantification | Gene expression clusters, Protein phosphorylation, Cytokine concentrations |
| Functional Assays | Phagocytosis assays, ROS detection, Morphological analysis, Chemotaxis assays | Effector function measurement, Activation state assessment | Phagocytic index, ROS fluorescence, Process length/branching, Migration distance |
| In Vivo Imaging | TSPO-PET, MRS, Multiphoton microscopy, Immunofluorescence | Spatial localization, Temporal dynamics, Non-invasive monitoring | Standardized uptake value, Metabolite concentrations, Cell motility, Marker co-localization |
In Vitro and In Vivo Modeling Approaches
Modeling neuroimmune interactions requires consideration of species-specific differences, particularly between rodent and human microglia [82]. Human microglia exhibit unique gene expression patterns, including exclusive disease-associated microglia signatures that don't precisely mirror murine phenotypic categories [82]. This represents a significant challenge for translational extrapolation of metabolic pathways and therapeutic responses.
In vitro systems range from primary microglial cultures to human induced pluripotent stem cell (iPSC)-derived microglia, with the latter offering improved human relevance while lacking the complexity of intact CNS environment [82]. Organoid models incorporating microglia provide more physiologically relevant context for studying cell-cell interactions in a three-dimensional architecture.
In vivo approaches utilize transgenic models of neurodegenerative diseases with careful consideration of species differences in microglial biology [82]. CX3CR1-GFP reporter mice enable visualization and isolation of microglia based on GFP expression, while parabiosis models and bone marrow chimeras help distinguish resident microglia from infiltrating peripheral macrophages.
Therapeutic Modulation of Neuroimmune Responses
Metabolic Reprogramming Strategies
Targeting microglial metabolism represents a promising therapeutic approach for shifting the balance from detrimental to protective neuroimmune responses:
AMPK Activators: Metformin, a widely prescribed antidiabetic medication, activates AMPK signaling and promotes microgl polarization toward an anti-inflammatory phenotype [82]. Preclinical studies demonstrate that metformin reduces neuroinflammation and enhances phagocytic clearance of protein aggregates in models of AD and PD [82].
mTOR Inhibitors: Rapamycin (sirolimus) and its analogs inhibit mTOR signaling, reducing glycolytic drive in pro-inflammatory microglia [82]. mTOR inhibition promotes autophagic clearance of protein aggregates and shifts microglial metabolism toward OXPHOS, supporting resolution functions [82].
Ketogenic Interventions: Ketone bodies (β-hydroxybutyrate, acetoacetate) and ketogenic diets provide alternative energy substrates that bypass glycolytic metabolism [82]. These interventions reduce HIF-1α stabilization and promote mitochondrial oxidative metabolism, favoring anti-inflammatory microglial phenotypes [82]. Clinical studies report benefits of ketogenic diets on cognitive outcomes in AD and motor symptoms in PD.
Gut-Brain Axis Modulation: Emerging evidence indicates that gut microbiota significantly influence microglial maturation and function [82]. Probiotic supplementation and dietary fiber interventions modulate systemic inflammation and microbial metabolite production, indirectly shaping neuroimmune responses through the gut-brain axis [82].
Table 3: Therapeutic Approaches for Immune Modulation in Neurodegeneration
| Therapeutic Strategy | Representative Agents | Molecular Targets | Effects on Microglial Phenotype |
|---|---|---|---|
| AMPK Activation | Metformin, AICAR, A-769662 | AMPK, LKB1 | Enhanced OXPHOS/FAO, Anti-inflammatory polarization, Improved phagocytosis |
| mTOR Inhibition | Rapamycin, Everolimus, Temsirolimus | mTORC1, PI3K/Akt | Reduced glycolysis, Enhanced autophagy, Attenuated pro-inflammatory signaling |
| Ketone-Based Metabolism | Ketogenic diet, β-hydroxybutyrate, Exogenous ketones | HDAC inhibition, GPCR signaling | Reduced HIF-1α stability, Enhanced mitochondrial function, Anti-inflammatory effects |
| PPAR-γ Activation | Pioglitazone, Rosiglitazone | PPAR-γ transcription factor | Enhanced FAO, Mitochondrial biogenesis, Resolution of inflammation |
| NLRP3 Inflammasome Inhibition | MCC950, CY-09, β-hydroxybutyrate | NLRP3 oligomerization | Reduced IL-1β/IL-18 processing, Attenuated pyroptosis, Limited inflammation propagation |
Targeting Specific Inflammatory Pathways
Beyond metabolic reprogramming, more targeted approaches address specific inflammatory signaling pathways implicated in neurodegeneration:
NF-κB Pathway Inhibition: Multiple strategies have been developed to inhibit this central inflammatory pathway, including IKKβ inhibitors and proteasome inhibitors that prevent NF-κB subunit degradation [50]. Challenges remain in achieving CNS penetration and avoiding immunosuppressive effects.
NLRP3 Inflammasome Inhibition: Small molecule inhibitors including MCC950 specifically target NLRP3 oligomerization and activation, reducing maturation of IL-1β and IL-18 [82]. The NLRP3 inflammasome is particularly relevant in AD, where Aβ and tau pathologies both contribute to its activation.
Cytokine-Targeted Therapies: Monoclonal antibodies against specific cytokines including TNF-α and IL-1β have shown efficacy in animal models but face challenges with blood-brain barrier penetration [50]. Intrathecal delivery approaches are being explored to overcome this limitation.
Specialized Pro-Resolving Mediators (SPMs): Rather than broadly suppressing inflammation, SPMs including resolvins, protectins, and maresins actively promote resolution of inflammation without compromising host defense [50]. These lipid mediators enhance phagocytic clearance of cellular debris and protein aggregates while restoring tissue homeostasis.
Diagram 2: Therapeutic Modulation of Neuroimmune Balance
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Neuroimmune Studies
| Reagent Category | Specific Examples | Research Applications | Functional Role |
|---|---|---|---|
| Polarizing Agents | LPS, IFN-γ, IL-4, IL-13, IL-10, TGF-β | Microglial polarization in vitro and in vivo | Induce specific activation states; LPS/IFN-γ for M1-like, IL-4/IL-13 for M2-like |
| Metabolic Modulators | 2-DG, Oligomycin A, Metformin, Rapamycin, BHB | Metabolic pathway manipulation | Inhibit specific metabolic pathways; 2-DG (glycolysis), Oligomycin (OXPHOS) |
| Cytokine Detection | ELISA kits, Multiplex bead arrays, ELISpot kits | Quantification of inflammatory mediators | Measure secreted or intracellular cytokines; Multiplex enables high-parameter analysis |
| Metabolic Probes | 2-NBDG, MitoTracker, TMRM, JC-1, Seahorse kits | Metabolic flux assessment | Visualize and quantify nutrient uptake, mitochondrial membrane potential, and function |
| Phenotypic Markers | IBA1, CD11b, CD45, TMEM119, P2RY12 | Microglial identification and characterization | Distinguish microglia from macrophages; Identify activation states |
| Pathology Detection | Thioflavin S, Amylo-Glo, AT8, pS129 α-synuclein | Protein aggregate visualization | Identify and quantify protein aggregates; AT8 for phosphorylated tau |
| In Vivo Tracers | TSPO-PET ligands ([11C]PK11195, [18F]GE180) | Non-invasive microglial activation monitoring | Quantify neuroinflammation in live animals and humans |
Balancing neuroprotective and detrimental immune modulation requires sophisticated understanding of microglial biology, particularly the metabolic reprogramming that underlies functional phenotypic states [82]. The interplay between key metabolic sensors including AMPK, mTOR, and HIF-1α creates a regulatory network that determines microglial contributions to neurodegenerative processes [82]. Future therapeutic development must account for the dynamic nature of neuroimmune responses and the continuum of microglial activation states, moving beyond simplistic M1/M2 dichotomies [82] [83].
Promising research directions include developing temporally-regulated interventions that account for the evolving nature of neuroimmune responses across disease stages, and creating dual-target approaches that simultaneously address protein pathology and maladaptive inflammation [82] [50]. The integration of human iPSC-derived microglial models and single-cell multi-omics technologies will enhance translational relevance and resolve cellular heterogeneity in human neurodegenerative diseases [82]. Ultimately, successful therapeutic strategies will likely require personalized approaches based on individual neuroimmune signatures and stage-specific pathological drivers.
Neurodegenerative diseases, including Alzheimer's disease (AD) and Parkinson's disease (PD), represent a growing global health burden. Their pathophysiological mechanisms are complex, involving selective neuronal vulnerability, dysregulated lipid metabolism, mitochondrial dysfunction, and crucially, neuroinflammation [84]. Chronic neuroinflammation, characterized by the sustained activation of glial cells and release of pro-inflammatory cytokines, is now recognized as a key driver of disease progression rather than merely a consequence [85]. This understanding has shifted therapeutic strategies toward targeting inflammatory pathways, creating opportunities to repurpose existing anti-inflammatory and metabolic drugs. The repurposing approach offers significant advantages for neurodegenerative drug development, including established safety profiles, reduced development timelines, and lower costs, which is particularly valuable given the urgent need for effective therapies [86]. This technical review examines the repurposing potential of NSAIDs, statins, and antidiabetic drugs, with a specific focus on their mechanisms for mitigating neuroinflammatory processes in neurodegenerative diseases.
Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
Molecular Mechanisms and Nano-Formulations
NSAIDs primarily exert their effects through the inhibition of cyclooxygenase (COX) enzymes, which are key players in the inflammatory cascade. COX inhibition reduces the synthesis of prostaglandins, lipid compounds that mediate inflammation, pain, and fever [87]. In the context of neurodegeneration, chronic activation of the COX pathway, particularly COX-2, contributes to neuroinflammation and neuronal damage. Beyond this canonical pathway, some NSAIDs, such as Ketoprofen, have demonstrated additional anticancer properties, including the induction of apoptosis and inhibition of proliferation in melanoma cells, suggesting broader mechanistic actions [88].
A significant challenge in using conventional NSAIDs for chronic neuroinflammation is their poor bioavailability and limited penetration of the blood-brain barrier. To address this, innovative nano-formulations have been developed. Oil-in-water nanoemulsions utilizing surfactants like Capryol 90, Lauroglycol 90, or Plurol Diisostearique, with Tween 80 as a hydrophilic surfactant and Transcutol as a cosurfactant, have shown promising results [88]. These formulations achieve high drug loading, small droplet sizes (139.1–170.5 nm), and improved stability, thereby enhancing drug delivery to target tissues.
Table 1: Key Characteristics of Optimized Ketoprofen-Loaded Nanoemulsions
| Parameter | Result | Significance |
|---|---|---|
| Droplet Size | 139.1–170.5 nm | Enhances tissue penetration and bioavailability |
| Polydispersity Index (PDI) | 0.240–0.292 | Indicates reasonably homogeneous droplet distribution |
| Zeta Potential | -6.38 to -9.40 mV | Suggests neutral surface charge and good stability |
| pH | ~4.0 | Ensures skin compatibility for topical administration |
| Drug Release | Biphasic (burst followed by sustained) | Provides immediate and prolonged therapeutic effect |
Experimental Protocol for In Vitro Cytotoxicity Assessment
Objective: To evaluate the cytotoxicity and anti-proliferative efficacy of ketoprofen-loaded nanoemulsions on B16.F10 murine melanoma cells [88].
- Cell Culture: Maintain B16.F10 murine melanoma cells in Dulbecco's Modified Eagle Medium (DMEM), supplemented with 10% fetal bovine serum (FBS) and 1% penicillin-streptomycin, at 37°C in a 5% CO₂ atmosphere.
- Treatment Preparation: Prepare serial dilutions of the following in culture medium: (a) optimized ketoprofen-loaded nanoemulsions, (b) blank nanoemulsions (vehicle control), and (c) free ketoprofen solution (conventional control).
- Cell Seeding and Treatment: Seed cells in 96-well plates at a density of 5 x 10³ cells per well and allow to adhere for 24 hours. Subsequently, treat the cells with the prepared formulations across a range of concentrations.
- Viability Assay: After a 72-hour incubation period, assess cell viability using the MTT (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide) assay. Add MTT reagent to each well and incubate for 4 hours to allow formazan crystal formation. Dissolve the crystals in dimethyl sulfoxide (DMSO) and measure the absorbance at 570 nm using a microplate reader.
- Data Analysis: Calculate the percentage of cell viability relative to untreated control cells. Determine the half-maximal inhibitory concentration (ICâ‚…â‚€) values using non-linear regression analysis.
Key Findings: Optimized ketoprofen-loaded nanoemulsions significantly reduced B16.F10 cell viability and demonstrated an enhanced cytotoxic effect compared to the free drug, underscoring the efficacy of the nano-delivery system [88].
Diagram 1: NSAID Mechanism and Nano-Formulation Enhancement. This diagram illustrates the primary inflammatory pathway targeted by NSAIDs, highlighting the crucial role of nano-formulations in enhancing drug delivery to the central nervous system.
Statins
Pleiotropic Anti-Inflammatory Mechanisms and Clinical Evidence
Statins, known primarily as HMG-CoA reductase inhibitors for cholesterol management, exhibit significant pleiotropic anti-inflammatory effects [89] [90]. Their mechanism extends beyond lipid lowering to include modulation of critical inflammatory pathways:
- Inhibition of the NF-κB Pathway: This is a primary mechanism, reducing the transcription of pro-inflammatory genes [90].
- Reduction of Pro-inflammatory Cytokines: Statins significantly lower levels of IL-6, TNF-α, and CRP, as confirmed by meta-analyses of randomized controlled trials (RCTs) [91].
- Modulation of the NLRP3 Inflammasome: This complex is a key component of the innate immune response, and its inhibition reduces the production of IL-1β and IL-18 [90].
- Inhibition of Protein Prenylation: By blocking the mevalonate pathway, statins prevent the prenylation of small GTPases (e.g., Ras, Rho), which are involved in intracellular signaling and inflammation [91] [90].
A recent systematic review and meta-analysis evaluating statins as immune-modulatory agents in adults with chronic diseases found that statin therapy significantly reduced key inflammatory markers. The results, detailed in Table 2, show that the efficacy can vary by specific statin type and treatment duration [91].
Table 2: Statin Efficacy in Reducing Inflammatory Markers and Lipids (Meta-Analysis Data) [91]
| Statin Type | Effect on IL-6 (MD, ng/dL) | Effect on TNF-α (MD, ng/dL) | Effect on CRP (MD, mg/L) | Effect on LDL-C (MD, mg/dL) | Key Findings |
|---|---|---|---|---|---|
| Atorvastatin | -0.24 [-0.36 to -0.13] | -0.74 [-1.08 to -0.40] | -1.58 [-2.22 to -0.94] | - | Most significant reduction in IL-6 and TNF-α, especially with treatment >4 months. |
| Fluvastatin | - | - | Greatest impact on CRP reduction. | - | - |
| Rosuvastatin | - | - | - | Greatest impact on LDL-C reduction. | Demonstrated hs-CRP reduction in the JUPITER trial. |
MD: Mean Difference.
Hungarian regulatory data from 2008–2025 revealed five approved off-label statin uses, including three dermatologic and two pediatric metabolic conditions, highlighting the clinical translation of repurposing efforts. However, approval requires thorough documentation and post-treatment reporting to ensure patient safety [89].
Experimental Protocol for Assessing Anti-Inflammatory Effects
Objective: To evaluate the impact of different statins and treatment durations on systemic inflammatory biomarkers in patients with chronic diseases via systematic review and meta-analysis [91].
- Search Strategy: Conduct a systematic literature search in databases (PubMed, Web of Science, Scopus, Cochrane) for RCTs published between 1999 and 2023.
- Eligibility Criteria: Include RCTs that report pre- and post-treatment levels of inflammatory markers (IL-6, TNF-α, CRP) and lipid profiles in adults with chronic diseases receiving statin therapy.
- Study Selection and Data Extraction: Two independent reviewers should screen records, extract data (including study design, patient characteristics, statin type and dose, treatment duration, and outcome measures), and assess risk of bias using the Cochrane tool.
- Statistical Analysis: Perform a meta-analysis using random effects models and the inverse variance method. Calculate the mean difference (MD) and 95% confidence intervals (CI) for continuous outcomes. Assess heterogeneity using the I² statistic. Conduct subgroup analyses based on statin type, treatment duration (>4 months vs. ≤4 months), and patient comorbidities.
Diagram 2: Statins' Anti-inflammatory Signaling Pathways. This diagram visualizes the key molecular mechanisms through which statins exert their pleiotropic anti-inflammatory effects, ultimately leading to potential neuroprotection.
Antidiabetic Drugs
Repurposing for Neuroinflammation and Shared Pathways
The repurposing of antidiabetic drugs for neurodegenerative conditions is supported by strong pathophysiological links between metabolic dysregulation and neuroinflammation. Diabetes and neurodegenerative diseases share common features, including insulin resistance, chronic inflammation, and mitochondrial dysfunction [85] [92]. Key mechanisms and drug candidates include:
- GLP-1 Receptor Agonists (e.g., Liraglutide, Semaglutide): These drugs improve glycaemic control and have demonstrated direct anti-inflammatory effects. Liraglutide has been shown to reduce neuroinflammatory markers in obese patients, independent of weight loss [93] [85]. Semaglutide is currently being assessed in clinical trials for early AD [86].
- SGLT2 Inhibitors (e.g., Empagliflozin): Beyond their metabolic benefits, SGLT2 inhibitors like empagliflozin offer neuroprotection and support neurovascular remodelling, which is crucial for maintaining cognitive function [85].
- Metformin: This first-line T2D drug inhibits mitochondrial complex I and activates AMPK, disrupting cellular energy production and inhibiting the mTOR pathway. These actions are relevant for curbing cancer cell proliferation and may also confer neuroprotective benefits [92].
- Sulphonylureas (e.g., Gliburide): Gliburide effectively inhibits the NLRP3 inflammasome, a key driver of neuroinflammation, suggesting its potential for treating neuroinflammatory disorders [85].
The shared pathway between diabetes and neuroinflammation often involves the NLRP3 inflammasome and subsequent production of IL-1β. Chronic hyperactivation of the hypothalamic-pituitary-adrenal (HPA) axis and innate immunity are implicated in both neurological disorders and diabetes, providing a common therapeutic target [85].
Experimental Protocol for Evaluating Neuroprotection
Objective: To investigate the effect of a GLP-1 receptor agonist (e.g., Liraglutide) on neuroinflammatory markers in an obese rodent model [85].
- Animal Model and Grouping: Use a diet-induced obesity (DIO) rodent model (e.g., C57BL/6J mice). Randomly assign animals to three groups: (a) control group on standard diet, (b) DIO group receiving vehicle treatment, and (c) DIO group receiving liraglutide treatment.
- Drug Administration: Administer liraglutide or vehicle via daily subcutaneous injection for a predetermined period (e.g., 8-12 weeks). Monitor body weight and glycaemic control (e.g., fasting glucose, glucose tolerance test) throughout the study.
- Tissue Collection and Processing: At the endpoint, euthanize the animals and perfuse transcardially with ice-cold phosphate-buffered saline (PBS). Dissect out brain regions of interest (e.g., hippocampus, cortex). Homogenize tissue samples for protein and RNA extraction.
- Analysis of Neuroinflammatory Markers:
- Immunohistochemistry (IHC): Stain brain sections for microglial (Iba1) and astrocytic (GFAP) markers to assess activation. Quantify staining intensity and cell morphology.
- Enzyme-Linked Immunosorbent Assay (ELISA): Measure levels of pro-inflammatory cytokines (e.g., TNF-α, IL-1β, IL-6) in brain homogenates.
- Western Blotting: Analyze protein expression of key pathway components, such as components of the NLRP3 inflammasome or phosphorylated signaling proteins.
- Cognitive and Behavioral Testing: Conduct behavioral assays (e.g., Morris water maze, Y-maze) prior to tissue collection to assess cognitive function and correlate with molecular findings.
Table 3: Molecular Targets of Repurposed Antidiabetic Drugs in Neuroinflammation
| Drug Class | Example Agents | Primary Molecular Target | Key Anti-neuroinflammatory Mechanism |
|---|---|---|---|
| GLP-1 RAs | Liraglutide, Semaglutide | GLP-1 Receptor | Reduces neuroinflammatory markers; improves metabolic parameters. |
| SGLT2i | Empagliflozin | SGLT2 Co-transporter | Promotes neurovascular remodelling; inhibits inflammation. |
| Biguanides | Metformin | Mitochondrial Complex I/AMPK | Activates AMPK; inhibits mTOR; disrupts energy metabolism. |
| Sulphonylureas | Gliburide | NLRP3 Inflammasome | Directly inhibits NLRP3 activation and IL-1β production. |
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents and Materials for Drug Repurposing Studies
| Research Reagent / Material | Function / Application |
|---|---|
| B16.F10 Murine Melanoma Cell Line | In vitro model for assessing cytotoxicity of repurposed drugs (e.g., ketoprofen) and nano-formulations [88]. |
| Capryol 90, Lauroglycol 90, Plurol Diisostearique | Hydrophobic surfactants used in the development of oil-in-water nanoemulsions for improved drug delivery [88]. |
| Tween 80 | Hydrophilic surfactant used in nanoemulsion formulation to stabilize droplet formation [88]. |
| Transcutol | Cosurfactant/Cosolvent used in nanoemulsions to enhance drug solubility and permeation [88]. |
| Enzyme-Linked Immunosorbent Assay (ELISA) Kits | Essential for quantifying levels of inflammatory biomarkers (e.g., IL-6, TNF-α, CRP) in cell culture supernatants, blood serum, or tissue homogenates [91]. |
| Antibodies for Iba1 and GFAP | Critical for immunohistochemical detection and quantification of activated microglia and astrocytes, respectively, in brain tissue sections [85]. |
| Diet-Induced Obesity (DIO) Rodent Models | Preclinical in vivo models for studying the interplay between metabolism, neuroinflammation, and the efficacy of repurposed antidiabetic drugs [85]. |
| Protein Misfolding Cyclic Amplification (PMCA) | Technology used for cross-species screening of anti-prion compounds and studying protein aggregation in neurodegenerative diseases [84]. |
Resolution pharmacology represents a paradigm shift in therapeutic approaches to chronic inflammatory conditions, moving beyond traditional anti-inflammatory strategies to actively promote the natural resolution processes of inflammation. This whitepaper examines the core principles, molecular mechanisms, and therapeutic applications of resolution pharmacology within the context of neurodegenerative disease research. We detail the specialized pro-resolving mediators (SPMs), their receptors, and signaling pathways that orchestrate inflammation resolution, with particular emphasis on their disruption in neurodegenerative pathologies. Comprehensive experimental methodologies for investigating resolution pathways are provided, along with visualization of key signaling networks and reagent solutions for research applications. The emerging evidence supports resolution pharmacology as a promising framework for developing disease-modifying treatments for Alzheimer's disease, Parkinson's disease, and other neurodegenerative conditions characterized by chronic neuroinflammation.
Resolution pharmacology is an innovative therapeutic concept first formally coined in 2015 that focuses on harnessing the biology of inflammation resolution to produce novel therapeutics [94]. Unlike conventional anti-inflammatory approaches that primarily block pro-inflammatory pathways, resolution pharmacology aims to actively stimulate endogenous resolution mechanisms to promote the natural termination of inflammatory responses while encouraging tissue repair and healing [94] [95]. This approach recognizes that the resolution of inflammation is not a passive process but an actively regulated program controlled by specific molecular mediators and cellular processes [96].
Within neurodegenerative disease research, resolution pharmacology offers particular promise given the central role of chronic, non-resolving neuroinflammation in conditions such as Alzheimer's disease (AD), Parkinson's disease (PD), and amyotrophic lateral sclerosis (ALS) [96] [50]. The failure of resolution mechanisms leads to persistent immune activation that drives neuronal damage and disease progression [50]. The core premise of resolution pharmacology is that pro-resolving drugs will work most effectively in the presence of florid inflammatory status, which would augment the expression of resolution targets [94]. These drugs are designed to be patient-centric in their pharmacology, promoting natural processes of healing and repair rather than broadly suppressing immune function [94].
Molecular Mechanisms of Inflammation Resolution
Specialized Pro-Resolving Mediators (SPMs)
The resolution of inflammation is actively mediated by a family of bioactive lipid molecules known as specialized pro-resolving mediators (SPMs), which include resolvins, protectins, maresins, and lipoxins [96]. These mediators are enzymatically derived from essential polyunsaturated fatty acids (PUFAs), particularly eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) [96]. SPMs function in a coordinated manner to control the termination of inflammatory responses without being immunosuppressive.
Table 1: Major Classes of Specialized Pro-Resolving Mediators
| SPM Class | Precursor | Key Members | Primary Biological Functions |
|---|---|---|---|
| E-series Resolvins | Eicosapentaenoic Acid (EPA) | RvE1, RvE2 | Inhibit neutrophil infiltration, promote macrophage phagocytosis, reduce pro-inflammatory cytokines [96] |
| D-series Resolvins | Docosahexaenoic Acid (DHA) | RvD1, RvD2, RvD3, RvD5 | Enhance macrophage phagocytosis of cellular debris and protein aggregates, modulate microglial function, reduce neuroinflammation [96] |
| Protectins | Docosahexaenoic Acid (DHA) | PD1 (also known as NPD1) | Protect neural cells from oxidative stress, reduce transmigration of neutrophils, promote tissue repair [96] |
| Maresins | Docosahexaenoic Acid (DHA) | MaR1, MaR2 | Stimulate tissue regeneration, enhance phagocytic clearance, promote nerve regeneration [96] |
| Lipoxins | Arachidonic Acid | LXA4, LXB4 | Limit neutrophil recruitment, stimulate non-phlogistic phagocytosis of apoptotic cells, resolve inflammation in peripheral and neural tissues [96] |
SPM Receptors and Signaling Pathways
SPMs exert their pro-resolving effects through specific G-protein-coupled receptors (GPCRs) that activate intracellular signaling pathways to promote resolution programs [96]. The known receptors for SPMs include ALX/FPR2 (lipoxin and formyl peptide receptor 2), DRV1/GPR32, DRV2/GPR18, and chemokine-like receptor 1 (CMKLR1, also known as ChemR23 or ERV1) [96].
The signaling mechanisms of SPMs involve multiple coordinated actions: (1) inhibition of neutrophil infiltration and transmigration; (2) enhancement of macrophage phagocytosis of apoptotic cells, debris, and protein aggregates; (3) reduction in pro-inflammatory cytokine production; and (4) promotion of tissue repair and regeneration [96]. For example, RvE1 binding to ERV1/ChemR23 activates downstream pathways that inhibit NF-κB signaling in inflammatory cells, thereby promoting neutrophil apoptosis and macrophage-mediated phagocytosis [96]. Similarly, RvD1 and RvD2 signal through ALX/FPR2 and DRV2/GPR18 respectively, modulating microglial function and reducing neuroinflammation in neurodegenerative models [96].
Figure 1: SPM Signaling Pathway - This diagram illustrates the sequential signaling cascade from SPM binding to GPCR receptors through intracellular signaling to cellular responses and ultimate resolution outcomes.
Resolution Pathways in Neurodegenerative Diseases
Dysregulation of Resolution in Neurodegeneration
In neurodegenerative diseases, chronic non-resolving neuroinflammation is a hallmark feature that contributes significantly to disease progression [96] [50]. The failure of resolution mechanisms leads to persistent activation of microglia and astrocytes, creating a self-perpetuating cycle of inflammation and neuronal damage [97] [50]. Key resolution pathways become impaired in neurodegenerative conditions, with documented reductions in SPM production and signaling observed in Alzheimer's disease, Parkinson's disease, and ALS [96].
In Alzheimer's disease, for example, diminished production of RvD1 has been reported in human patients, correlating with increased neuroinflammation and cognitive decline [96]. The persistent inflammatory environment in AD is characterized by sustained microglial activation, cytokine release, and inflammasome activation that accelerates disease progression [98]. Similar disruptions in resolution pathways have been documented in Parkinson's disease, where RvD2 has been shown to prevent activation of the TLR4/NF-κB pathway, suggesting a protective role that may be compromised in PD pathology [96].
Genetic Regulators of Resolution
Genetic studies have identified several key regulators of microglial function that impact resolution pathways in neurodegenerative diseases. Notable among these is triggering receptor expressed on myeloid cells 2 (TREM2), a membrane receptor exclusively expressed on microglia that plays a critical role in clearing toxic protein aggregates, including amyloid-beta (Aβ), TDP-43, and alpha-synuclein [49]. Variants in TREM2 have been identified as risk factors for AD, PD, frontotemporal dementia (FTD), and ALS [49].
Other genetic regulators include CD33/Siglec-3, which suppresses microglial uptake of Aβ when elevated, and progranulin (PGRN), mutations in which are associated with impaired lysosomal function and enhanced neuroinflammation [49]. These genetic factors influence the capacity of CNS immune cells to engage resolution pathways and clear pathological protein aggregates, thereby modulating disease progression and severity.
Table 2: Key Genetic Regulators of Resolution in Neurodegeneration
| Genetic Regulator | Expression | Function in Resolution | Association with Neurodegeneration |
|---|---|---|---|
| TREM2 | Microglia | Enhances phagocytosis of protein aggregates, promotes microglial survival, modulates lipid metabolism [49] | R47H variant increases AD risk 2-4 fold; associated with PD, FTD, and ALS [49] |
| CD33/Siglec-3 | Microglia | Suppresses microglial uptake of Aβ when elevated; knockout enhances anti-inflammatory responses [49] | Elevated expression in AD suppresses Aβ clearance [49] |
| Progranulin (PGRN) | Microglia, neurons | Regulates lysosomal function, neuroinflammation, and neuronal survival [49] | Mutations cause FTD and neuronal ceroid lipofuscinosis [49] |
| APOE | Astrocytes, microglia | Modulates lipid transport, amyloid aggregation, and neuroinflammatory responses [97] | ε4 allele is primary genetic risk factor for sporadic AD [97] |
| LILRB4 | Microglia | Immunoreceptor tyrosine-based inhibition motif (ITIM)-containing receptor that regulates phagocytosis [49] | Emerging target in AD; modulates microglial function [49] |
Experimental Models and Methodologies
In Vitro Assessment of Pro-Resolving Activity
Primary Microglial Phagocytosis Assay: Isolate primary microglia from postnatal day 1-3 mouse pups following established protocols [49]. Culture cells in DMEM/F12 medium supplemented with 10% FBS, 1% penicillin-streptomycin, and 5 ng/mL GM-CSF at 37°C with 5% CO₂. For phagocytosis assessment, seed cells in 24-well plates at a density of 1×10ⵠcells/well and treat with SPMs (e.g., RvD1, RvD2, MaR1) at concentrations ranging from 1-100 nM for 24 hours. Add pHrodo-labeled Aβ42 fibrils (1 µg/mL) or fluorescent latex beads (0.5 µm diameter) for 4 hours. Quantify phagocytosis using flow cytometry or high-content imaging analysis. Include controls with cytochalasin D (5 µM) to inhibit actin polymerization and confirm phagocytosis-specific uptake [49] [96].
Microglial Phenotyping via Cytokine Profiling: Treat human microglial cell lines (e.g., HMC3) or primary microglia with SPMs in the presence of inflammatory stimuli (e.g., LPS at 100 ng/mL or Aβ oligomers at 500 nM). After 24 hours, collect culture supernatants and analyze pro-inflammatory (TNF-α, IL-1β, IL-6) and anti-inflammatory (IL-10, TGF-β) cytokine profiles using multiplex ELISA. Simultaneously, extract RNA for transcriptomic analysis of polarization markers (iNOS, Arg1, Ym1) via qRT-PCR [49] [96].
In Vivo Models of Neuroinflammation Resolution
Transgenic Mouse Models: Utilize APP/PS1 mice for Alzheimer's disease studies or α-synuclein overexpression models for Parkinson's disease research. Administer SPMs via intracerebroventricular injection (dose: 100-500 ng in 2 µL vehicle) or intraperitoneal injection (dose: 1-5 µg in 100 µL vehicle) three times per week for 1-3 months. Behavioral assessments should include Morris water maze for spatial memory (AD models) or open field and rotarod tests for motor function (PD models) [96].
Tissue Collection and Analysis: Following behavioral testing, perfuse animals transcardially with cold PBS followed by 4% PFA. Collect brains for immunohistochemical analysis of amyloid burden (6E10 antibody), microglial activation (Iba1, CD68), and astrocytosis (GFAP). Quantify plaque burden and microglial coverage using image analysis software. Alternatively, prepare fresh brain tissue for flow cytometric analysis of immune cell populations or for biochemical assessment of cytokine levels and protein aggregates [49] [96].
Assessment of Resolution Indices: Measure key resolution indices including: (1) maximum neutrophil infiltration, (2) resolution interval (time from maximum neutrophil infiltration to 50% reduction), (3) phagocytic index (percentage of microglia with engulfed material), and (4) cytokine balance (ratio of pro-resolving to pro-inflammatory mediators) [96].
Figure 2: Experimental Workflow for Assessing Resolution - This diagram outlines the integrated experimental approach from in vitro and in vivo models through behavioral and tissue analysis to resolution metrics.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Resolution Pharmacology Studies
| Reagent Category | Specific Examples | Research Application | Key Functions |
|---|---|---|---|
| Specialized Pro-Resolving Mediators | RvD1, RvD2, RvE1, MaR1, LXA4 (Cayman Chemical) | In vitro and in vivo resolution assays | Activate specific GPCRs to stimulate resolution pathways; enhance phagocytosis; reduce neutrophil infiltration [96] |
| TREM2 Modulators | AL002 (Alector), VHB937 (Novartis), VG-3927 (Vigil Neurosciences) | Microglial function studies | Agonist antibodies and small molecules that enhance TREM2 signaling; promote microglial phagocytosis and survival [49] |
| CD33 Inhibitors | AL003 (Alector) | Alzheimer disease models | CD33-blocking antibody that enhances microglial uptake of Aβ; reduces plaque burden [49] |
| Nanobodies (sdAbs) | Anti-Aβ fibril single-domain antibodies | Targeted drug delivery to plaques | Small size enables good tissue penetration; targets regions of neuroinflammation; can be conjugated to anti-inflammatory payloads [97] |
| Flow Cytometry Antibodies | Anti-CD11b, Anti-CD45, Anti-TMEM119, Anti-P2Y12 | Microglial characterization and sorting | Identify and isolate specific microglial subpopulations; distinguish CNS-resident microglia from peripheral macrophages [49] |
| Cytokine Analysis Kits | Multiplex ELISA for TNF-α, IL-1β, IL-6, IL-10, TGF-β | Inflammation and resolution monitoring | Quantify pro-inflammatory and anti-inflammatory mediators; assess cytokine balance shifts during resolution [49] [96] |
Therapeutic Applications and Clinical Translation
Current Clinical Development
Several resolution-targeting therapeutic approaches are currently in clinical development for neurodegenerative diseases. TREM2-targeting agents represent one of the most advanced classes, with multiple candidates in clinical trials:
AL002 (Alector): A TREM2-activating monoclonal antibody currently in Phase 2 clinical studies (NCT04592874 and NCT05744401) for Alzheimer's disease. In Phase 1 trials (INVOKE-1, NCT03635047), AL002 infusion resulted in a dose-dependent reduction in soluble TREM2 (sTREM2) in CSF, accompanied by increases in biomarkers of TREM2 signaling and microglial recruitment [49].
VHB937 (Novartis): A TREM2-activating monoclonal antibody that increases TREM2 surface expression and activates downstream signaling, enhancing microglial phagocytosis and chemotaxis. A Phase 2 trial (NCT06643481) is currently underway to evaluate efficacy and safety in early-stage ALS [49].
VG-3927 (Vigil Neurosciences): A brain-penetrant small-molecule TREM2 agonist that in preclinical models reduced Aβ pathology and induced a disease-associated microglia (DAM)-like phenotype. A Phase 1 trial (NCT06343636) demonstrated tolerability and dose-dependent reduction of CSF sTREM2 [49].
Novel Delivery Strategies
Advanced delivery approaches are being developed to enhance targeted engagement of resolution pathways in the CNS. Nanobody-mediated delivery represents a promising strategy that combines single-domain antibodies (sdAbs) against Aβ fibrils with anti-inflammatory drugs [97]. These sdAbs feature small size, good tissue penetration, and lack of Fc-mediated immune reactions, making them ideal for targeted delivery to regions of neuroinflammation associated with plaques in AD patients [97]. This approach aims to control the function of activated microglia and astrocytes while avoiding unnecessary immunosuppression.
Biomarkers for Clinical Monitoring
The development of biomarkers to monitor resolution engagement is crucial for clinical translation. Promising biomarkers include:
sTREM2: Soluble TREM2 in CSF is considered a biomarker of microglial activation, with elevated levels observed in AD, particularly during early symptomatic stages [49].
SPM Profiles: Liquid chromatography-tandem mass spectrometry (LC-MS/MS) methods can quantify SPM levels in CSF and plasma, providing direct measures of resolution engagement [96].
Cytokine Ratios: The balance between pro-inflammatory cytokines (IL-1β, TNF-α, IL-6) and pro-resolving mediators (IL-10, TGF-β) can indicate resolution status [99] [96].
Resolution pharmacology represents a transformative approach to treating neurodegenerative diseases by actively engaging natural resolution mechanisms rather than simply suppressing inflammation. The growing understanding of SPMs, their receptors, and signaling pathways has revealed multiple therapeutic targets for promoting the resolution of chronic neuroinflammation in conditions like Alzheimer's disease and Parkinson's disease.
Future developments in this field will likely focus on several key areas: (1) optimization of brain-targeted delivery systems for resolution mediators; (2) personalized approaches based on individual resolution capacity and genetic background; (3) combination therapies that simultaneously target protein aggregates and enhance resolution pathways; and (4) advanced biomarker development to monitor resolution engagement in clinical trials.
The continued elucidation of resolution mechanisms in neurodegeneration, coupled with innovative therapeutic strategies, holds significant promise for developing disease-modifying treatments that can break the cycle of chronic neuroinflammation and promote neural repair and recovery.
Timing and Patient Stratification for Optimal Therapeutic Efficacy
The pursuit of effective treatments for neurodegenerative diseases (NDDs) has been hampered by high failure rates in clinical trials, often attributed to patient heterogeneity and intervention at inappropriate disease stages. The recognition that inflammatory responses and non-cell-autonomous mechanisms are core drivers of disease progression has fundamentally reshaped therapeutic development [49]. Microglial dysfunction, chronic neuroinflammation, and impaired phagocytosis create a destructive feedback loop that accelerates neurodegeneration across conditions including Alzheimer's disease (AD), amyotrophic lateral sclerosis (ALS), Parkinson's disease (PD), and frontotemporal dementia (FTD) [49]. Within this pathophysiological context, the dual principles of optimal timing and precision stratification have emerged as critical determinants of therapeutic success. This technical guide synthesizes current evidence and methodologies for aligning intervention timing with disease biology and implementing biomarker-driven patient stratification to enhance clinical trial outcomes and therapeutic efficacy for researchers, scientists, and drug development professionals.
Table 1: Key Challenges in Neurodegenerative Disease Therapeutics Addressed by Timing and Stratification
| Challenge | Impact on Drug Development | Strategic Solution |
|---|---|---|
| Clinical & Biological Heterogeneity | Variable treatment responses; failed primary endpoints | Biomarker-driven patient stratification; precision medicine approaches |
| Extended Preclinical/Prodromal Period | Late intervention on established pathology | Early detection biomarkers; preclinical/secondary prevention trials |
| Complex Co-pathologies | Misdiagnosis; confounding treatment effects | Multi-modal biomarker panels; disease-specific signatures |
| Variable Progression Rates | Insensitive outcome measures; noisy trial data | Prognostic biomarkers; enrichment for progressive populations |
The Evolving Therapeutic Landscape and Imperative for Precision Approaches
The neurodegenerative therapeutic pipeline has expanded significantly, with 138 drugs currently being assessed in 182 clinical trials in 2025 [7]. Biological and small-molecule disease-targeted therapies (DTTs) dominate the pipeline, comprising 30% and 43% respectively, while repurposed agents represent 33% of investigated treatments [7]. This diversification coincides with the landmark approval of anti-amyloid immunotherapies (lecanemab, donanemab) for early-stage AD, which demonstrated that targeting core pathologies can slow cognitive decline when applied at the appropriate disease stage [100]. These advances underscore a fundamental shift in the treatment paradigm: the transition from symptomatic management to disease modification necessitates earlier intervention and more precise patient selection.
Concurrently, the growing understanding of inflammatory pathways in neurodegeneration has revealed microglial targets as promising therapeutic avenues. Genes including TREM2, CD33, and PGRN regulate microglial phagocytosis, neuroinflammation, and metabolic functions, positioning them strategically for intervention [49]. The success of therapies targeting these pathways depends critically on resolving the timing of their dysregulation and identifying patient subgroups most likely to respond. This evolving landscape demands sophisticated stratification tools that extend beyond conventional diagnostic categories to capture the underlying molecular heterogeneity of neurodegenerative processes.
Temporal Considerations: The Therapeutic Window of Opportunity
Disease Continuum and Intervention Timepoints
Neurodegenerative diseases span a continuum from preclinical/asymptomatic phases to severe dementia, with pathophysiological processes beginning years before clinical manifestation [100]. The therapeutic window of opportunity is now understood to be early in this continuum, when interventions can potentially alter disease trajectory before irreversible neuronal loss occurs. Research on anti-amyloid immunotherapies demonstrates that efficacy is most pronounced in early AD stages (mild cognitive impairment [MCI] and mild dementia), with significantly reduced benefits as disease advances [100]. This temporal dynamic reflects the biology of escalating pathological burden, where amyloid deposition, tau propagation, and neuroinflammatory processes eventually reach a threshold beyond which targeted interventions have limited clinical impact.
Table 2: Intervention Timing Relative to Disease Stage and Pathology
| Disease Stage | Dominant Pathology | Therapeutic Goals | Established/Investigational Therapies |
|---|---|---|---|
| Preclinical | Amyloid accumulation; early tau seeding | Primary prevention; delay clinical onset | Anti-amyloid vaccines; BACE inhibitors (under investigation) |
| Prodromal/MCI | Amyloid + early tau spread; initial neuroinflammation | Secondary prevention; slow progression | Lecanemab; Donanemab; BIIB080 (anti-tau) |
| Mild Dementia | Significant tau pathology; substantial neuroinflammation | Disease modification; symptomatic + functional stabilization | Cholinesterase inhibitors + disease-modifying therapies |
| Moderate-Severe Dementia | Widespread neurodegeneration; chronic inflammation | Symptomatic management; functional support | Memantine; combination therapies; neuropsychiatric symptom treatments |
Inflammatory Trajectories and Temporal Dynamics
The neuroinflammatory component of neurodegenerative diseases exhibits its own temporal dynamics that must be considered for optimal intervention. Microglial phenotypes evolve throughout disease progression, with early protective functions transitioning to maladaptive states that drive pathology [49]. Biomarkers such as soluble TREM2 (sTREM2) in cerebrospinal fluid (CSF) show elevation particularly during early symptomatic stages, suggesting a period of heightened microglial activation that may represent a critical window for immunomodulatory therapies [49]. Postmortem and longitudinal biomarker studies further indicate that inflammatory processes may accelerate as disease progresses, creating self-sustaining cycles of neuronal damage. Therapies targeting these inflammatory mechanisms must therefore be timed to specific phases of the neuroinflammatory cascade, with some approaches potentially beneficial early (e.g., TREM2 activation to enhance clearance) while others may be more appropriate later (e.g., suppression of specific cytokine signaling).
Patient Stratification: From One-Size-Fits-All to Precision Medicine
Stratification Biomarkers: Technologies and Applications
Modern patient stratification employs multi-modal biomarker approaches to resolve disease heterogeneity into mechanistically coherent subgroups. These biomarkers facilitate precision enrollment in clinical trials and enable targeted therapeutic deployment in clinical practice.
Imaging Biomarkers
Structural and molecular neuroimaging provides critical information for patient stratification. Amyloid PET enables confirmation of Alzheimer's pathology in early clinical stages and was essential for patient selection in anti-amyloid immunotherapy trials [100]. Tau PET tracks the spatial distribution and burden of neurofibrillary tangles, which correlate more closely with symptom severity and disease stage than amyloid pathology [100]. Structural MRI measures, particularly medial temporal lobe atrophy, serve as indicators of neurodegenerative burden and disease progression [101]. Advanced imaging techniques that combine multiple modalities can identify network-level dysfunction patterns that predict disease trajectory and treatment response.
Fluid Biomarkers
Cerebrospinal fluid and blood-based biomarkers offer minimally invasive tools for molecular stratification. The fully automated ultra-sensitive Simoa technology exemplifies recent advances, enabling precise quantification of Alzheimer's-related pathology (phospho-tau205, phospho-tau212), neuroaxonal injury (neurofilament light chain [NfL]), astrocytic activation (GFAP), and synaptic dysfunction (PSD-95) [102]. Plasma biomarkers such as p-tau217 have demonstrated high accuracy in detecting amyloid pathology, with algorithmic approaches like LucentAD Complete achieving ≥90% accuracy in amyloid risk stratification [102]. For inflammatory stratification, biomarkers including sTREM2 (microglial activation), MCP-1, and YKL-40 provide windows into neuroinflammatory processes relevant to therapeutic targeting [49].
Genetic Stratification
Monogenic and risk-modifying genes enable stratification by molecular subtype and disease mechanism. In Alzheimer's disease, APOE ε4 status not only influences disease risk but also predicts treatment response and side effect profile, with ε4 carriers showing higher rates of amyloid-related imaging abnormalities (ARIA) with anti-amyloid immunotherapies [49]. Variants in microglial genes including TREM2, CD33, and ABI3 identify patients with specific immune-related dysfunction potentially amenable to targeted interventions [49]. Beyond Alzheimer's, genetic stratification guides therapy in ALS (e.g., SOD1 mutations for tofersen) and frontotemporal dementia (e.g., C9orf72, GRN mutations), supporting mechanism-specific trial designs.
Artificial Intelligence and Prognostic Modeling
Artificial intelligence (AI) approaches are transforming patient stratification by integrating multimodal data to predict individual disease trajectories. The Predictive Prognostic Model (PPM) exemplifies this capability, using baseline data (β-amyloid, APOE4, medial temporal lobe gray matter density) to stratify patients into slow versus rapid progression categories with 91.1% accuracy [101]. When applied retrospectively to the failed AMARANTH trial of lanabecestat, AI-guided stratification revealed that slow progressors showed 46% slowing of cognitive decline with active treatment—a significant effect masked in the unstratified analysis [101]. This demonstrates how AI-driven prognosis can enrich clinical trials with patients most likely to demonstrate treatment benefits within conventional trial timelines, potentially reducing required sample sizes and enhancing statistical power.
Experimental Protocols for Stratification Biomarker Validation
Protocol 1: AI-Guided Patient Stratification Using Predictive Prognostic Modeling
Objective: To develop and validate a machine learning model for stratifying patients by likely progression rate to enrich clinical trials.
Materials:
- Multimodal baseline data (amyloid PET, structural MRI, genetic data)
- Longitudinal clinical outcomes (CDR-SB, ADAS-Cog, or disease-specific scales)
- Computational infrastructure for machine learning
Methodology:
- Data Preprocessing: Harmonize multimodal data across sites; quality control for imaging and genetic data; handle missing values.
- Feature Selection: Identify strongest predictors of progression (e.g., amyloid burden, medial temporal lobe volume, APOE status, specific genetic variants).
- Model Training: Implement Generalized Metric Learning Vector Quantization (GMLVQ) or similar algorithm on training cohort (e.g., ADNI) to discriminate stable from declining patients.
- Model Validation: Test trained model on independent cohort (e.g., clinical trial data) using predefined performance metrics (accuracy, AUC, sensitivity, specificity).
- Prognostic Index Calculation: Compute individual prognostic scores based on distance from model prototypes in the learned metric space.
- Stratification Thresholds: Establish thresholds for progression categories (e.g., slow, intermediate, rapid) based on prognostic index distribution and clinical outcomes.
Validation: Apply to historical clinical trial data to determine if stratification reveals treatment effects masked in unstratified analyses [101].
Protocol 2: Multi-Analyte Biomarker Panel Development for Inflammatory Stratification
Objective: To develop a fluid biomarker panel for stratifying patients by neuroinflammatory profile.
Materials:
- Plasma or CSF samples from well-characterized cohorts
- Ultra-sensitive immunoassay technology (e.g., Simoa, Olink)
- Validated assays for inflammatory markers (sTREM2, MCP-1, YKL-40, GFAP)
Methodology:
- Sample Collection: Standardize collection, processing, and storage protocols across sites to minimize pre-analytical variability.
- Assay Development: Optimize multiplex or single-plex assays for target analytes; establish precision, sensitivity, and dynamic range.
- Discovery Phase: Measure biomarkers in discovery cohort; identify patterns associated with clinical phenotypes, progression rates, or pathological subtypes.
- Validation Phase: Confirm findings in independent validation cohort; establish reference ranges and pathological thresholds.
- Algorithm Development: Combine biomarkers into diagnostic or prognostic algorithms using multivariate methods; validate against clinical outcomes.
- Clinical Translation: Develop clinical grade tests; establish standardization across laboratories.
Applications: Stratification for trials of immunomodulatory therapies; tracking target engagement of inflammatory interventions [102] [49].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Key Research Reagent Solutions for Timing and Stratification Studies
| Technology/Reagent | Primary Application | Key Features | Representative Examples |
|---|---|---|---|
| Ultra-Sensitive Immunoassay Platforms | Quantifying low-abundance biomarkers in biofluids | Single-molecule detection; multiplex capability | Quanterix Simoa [102] |
| Multi-Omics Platforms | Comprehensive molecular profiling | High-dimensional data; pathway analysis | SomaScan; Olink; Mass Spectrometry [59] |
| Automated Biomarker Assays | High-throughput sample analysis | Standardization; reduced variability | Simoa fully automated p-tau205, p-tau212 [102] |
| Algorithmic Diagnostic Tests | Integrated biomarker interpretation | Multivariate classification; risk stratification | LucentAD Complete (p-tau217 + algorithm) [102] |
| Multi-modal Data Integration Platforms | AI-driven patient stratification | Combines imaging, fluid, genetic biomarkers | Predictive Prognostic Model (PPM) [101] |
Clinical Trial Applications and Outcomes
Successful Stratification in Neurodegenerative Trials
The practical application of timing and stratification strategies is demonstrating significant impacts on clinical trial outcomes. The anti-amyloid immunotherapies lecanemab and donanemab established that biomarker-confirmed early AD populations show statistically significant slowing of decline, leading to their regulatory approval [100]. Similarly, the ALS Summit trial of Neuronata-R revealed that while the overall trial missed its primary endpoint, pre-specified subgroup analysis demonstrated significant benefits in patients with slower disease progression, with improved functional ratings (ALSFRS-R: 31.2 vs. 26.4) and respiratory function (SVC: 62.2% vs. 50.6%) [103]. This success was paralleled by biomarker evidence of neuroprotection, with sustained reductions in neurofilament light chain (NfL) and MCP-1 confirming the biological effect of treatment [103].
The reanalysis of the AMARANTH trial using AI-guided stratification provides perhaps the most compelling evidence for precision approaches. The original trial of lanabecestat, a BACE1 inhibitor, was terminated for futility despite target engagement (amyloid reduction). When restratified using the PPM algorithm, patients classified as slow progressors showed 46% slowing of cognitive decline (CDR-SB) with active treatment compared to placebo [101]. This dramatic reversal of the trial conclusion highlights how conventional enrollment criteria may obscure efficacy in biologically distinct subgroups, and demonstrates the power of AI-driven stratification to reveal treatment effects.
Inflammatory Targeting and Stratification Strategies
Trials targeting neuroinflammatory mechanisms increasingly incorporate microglia-specific biomarkers for patient selection and target engagement assessment. Phase 2 trials of TREM2-targeting therapies (AL002, VG-3927) employ CSF sTREM2 measurements to confirm mechanism of action and guide dosing [49]. These studies strategically enroll patients in early disease stages when microglial activation is most dynamic and potentially modifiable. The evolving understanding of microglial heterogeneity (DAM, MGnD, LDAM subtypes) further enables refinement of stratification approaches to match specific therapeutic mechanisms with appropriate inflammatory phenotypes [49].
Implementation Framework and Future Directions
Integrated Strategy for Timing and Stratification
Successful implementation of timing and stratification strategies requires systematic approaches across the drug development continuum:
Preclinical Discovery: Identify mechanistically relevant biomarkers alongside therapeutic targets; establish relationship between target modulation and biomarker response.
Phase 1 Trials: Incorporate target engagement biomarkers; establish pharmacokinetic-pharmacodynamic relationships; explore preliminary stratification hypotheses.
Phase 2 Trials: Implement prospective stratification strategies; validate biomarker thresholds; identify enriched populations for Phase 3.
Phase 3 Trials: Confirm stratification value in large populations; demonstrate treatment benefits in predefined subgroups; validate biomarker utility for clinical practice.
Clinical Practice: Translate validated stratification approaches to guide treatment decisions; monitor response and safety.
Emerging Technologies and Future Perspectives
The future of timing and stratification in neurodegenerative therapeutics will be shaped by several technological advances. Single-cell multi-omics is unraveling microglial heterogeneity, promising increasingly refined stratification based on specific activation states [49]. Large-scale consortia like the Global Neurodegeneration Proteomics Consortium (GNPC) are assembling massive proteomic datasets (approximately 250 million protein measurements from >35,000 samples) to identify novel biomarker signatures across diseases [59]. Blood-brain barrier penetrating technologies, including advanced delivery systems and receptor-mediated transcytosis platforms, may expand the therapeutic window for previously undruggable targets [104]. Finally, adaptive trial designs (basket, umbrella, platform trials) efficiently evaluate multiple targeted therapies simultaneously, accelerating the development of personalized approaches [104].
The convergence of these technologies with deepened understanding of neuroinflammatory mechanisms promises a new era of precision medicine for neurodegenerative diseases. By aligning intervention timing with pathogenic processes and matching therapeutic mechanisms with appropriately stratified patients, the field is poised to significantly improve outcomes for these devastating conditions.
Comparative Efficacy: Validating Therapeutic Targets Across Disease Models
Direct Comparison of Inflammatory Biomarker Performance Across Disorders
Inflammatory responses represent a core pathological mechanism bridging diverse neurological and psychiatric conditions. The identification and validation of inflammatory biomarkers are crucial for improving early diagnosis, disease monitoring, prognostication, and development of targeted therapies across the spectrum of brain disorders. This whitepaper provides a technical comparison of inflammatory biomarker performance across neurodegenerative diseases, psychiatric disorders, and acute neurological insults, synthesizing recent evidence to guide researchers and drug development professionals in biomarker selection and interpretation.
Inflammatory Biomarker Alterations Across Neurological and Psychiatric Disorders
Table 1: Inflammatory Biomarker Profiles in Neurodegenerative Proteinopathies [105] [106]
| Biomarker | Biofluid | Lewy Body Diseases (LBD) | Multiple System Atrophy (MSA) | 4-Repeat Tauopathies (4RT) | Control Subjects |
|---|---|---|---|---|---|
| Transferrin | CSF | ↓ Significantly lower | ↓ Significantly lower | Not significantly different | Reference level |
| C3 Complement | CSF | ↓ Significantly lower | ↓ Significantly lower | Not significantly different | Reference level |
| Orosomucoid | CSF | ↓ Significantly lower | ↓ Significantly lower | Not significantly different | Reference level |
| C4 Complement | CSF | Not significantly different | ↓ Significantly lower | Not significantly different | Reference level |
| Orosomucoid | Serum | ↓ Significantly lower | Not significantly different | Not significantly different | Reference level |
| β2 Microglobulin | Serum | ↓ Significantly lower | Not significantly different | Not significantly different | Reference level |
| C3 Complement | Serum | Not significantly different | Not significantly different | ↑ Higher than synucleinopathies | Reference level |
Table 2: Established Neuroinflammatory Fluid Biomarkers in Alzheimer's Disease Continuum [107]
| Biomarker | Primary Cellular Source | Preclinical/Prodromal AD | AD Dementia | Longitudinal Association |
|---|---|---|---|---|
| CSF sTREM2 | Microglia | ↑ Elevated | ↑ Elevated (early symptomatic) | Associated with disease progression |
| Plasma GFAP | Astrocytes | ↑ Elevated (with Aβ pathology) | ↑ Elevated | Predictive of cognitive decline |
| CSF YKL-40 | Astrocytes, macrophages | Variable | ↑ Elevated | Limited longitudinal data |
Table 3: Inflammatory Biomarker Alterations in Psychiatric Disorders [108] [109]
| Disorder | Consistently Elevated Biomarkers | Inconsistently Altered/Underpowered Findings | State vs. Trait Characteristics |
|---|---|---|---|
| Major Depressive Disorder (MDD) | IL-6, CRP, TNF-α | Multiple cytokines in underpowered studies | Both state and trait components observed |
| Schizophrenia (SCZ) | IL-6, CRP | Inconsistent findings across treatment states | More reproducible in first-episode vs. controls |
| Bipolar Disorder (BD) | IL-4, IL-6, CRP | Variable findings across mood states | Distinct inflammatory profiles in manic vs. depressive states |
| Autism Spectrum Disorder (ASD) | IL-6, TNF-α | Multiple cytokines with limited evidence | Trait-associated alterations |
| Post-Traumatic Stress Disorder (PTSD) | IL-6, CRP | Limited number of well-powered studies | State-dependent fluctuations observed |
Experimental Methodologies for Biomarker Assessment
The case-control study investigating neurodegenerative proteinopathies employed standardized protocols for biomarker measurement. CSF and blood serum samples were collected from 83 Lewy body disease (LBD) patients, 24 multiple system atrophy (MSA) patients, 31 4-repeat tauopathy (4RT) patients, and 83 control subjects. Six immune-related proteins were quantified: C3 complement, C4 complement, haptoglobin, transferrin, orosomucoid, and β2 microglobulin (β2M). Samples were processed using enzyme-linked immunosorbent assay (ELISA) and multiplex immunoassay platforms following manufacturer protocols. Statistical analyses were performed using ANCOVA with adjustments for age and sex, with post-hoc tests for between-group comparisons. The CSF/serum quotient (Q) for each biomarker was calculated to assess blood-brain barrier function and central production.
The identification of inflammatory response-related long non-coding RNAs (lncRNAs) in acute ischemic stroke involved a comprehensive multi-omics workflow. Researchers analyzed gene expression datasets from the GEO database, identifying differentially expressed genes (DEGs), miRNAs (DEMIs), and lncRNAs (DELs) using the "limma" R package. Inflammation-related DEGs were identified through intersection with the GeneCards database. A competing endogenous RNA (ceRNA) network was constructed using lncBase, TargetScan, and miRDB databases to establish lncRNA-miRNA-mRNA interactions. Protein-protein interaction networks were analyzed using STRING database and Cytoscape, with hub genes identified via CytoHubba. Diagnostic performance was validated using receiver operating characteristic curves with the "pROC" R package.
The Parkinson's disease study integrated bioinformatics and machine learning to identify inflammatory biomarkers. Differential expression analysis of inflammatory response genes was performed on substantia nigra datasets from GEO. Protein-protein interaction networks were constructed and enrichment analysis conducted. Three machine learning algorithms were applied: LASSO regression, Support Vector Machine-Recursive Feature Elimination (SVM-RFE), and Random Forest. Feature importance was ranked across algorithms, and intersection of top features identified robust biomarker candidates. Validation included drug sensitivity analysis, mRNA-miRNA network construction, and single-cell transcriptome analysis to verify cell-type-specific expression.
Visualizing Biomarker Discovery Workflows
Neuroinflammatory Biomarker Analysis Pipeline
Cross-Disorder Biomarker Performance Assessment
Research Reagent Solutions for Inflammatory Biomarker Studies
Table 4: Essential Research Reagents and Platforms for Inflammatory Biomarker Discovery
| Reagent/Platform | Specific Function | Application Examples |
|---|---|---|
| Multiplex Immunoassay Panels | Simultaneous quantification of multiple inflammatory proteins (cytokines, complement factors, acute-phase proteins) | Measurement of IL-6, TNF-α, CRP in psychiatric disorders [108] |
| SomaScan/Olink Platforms | High-throughput proteomic analysis of thousands of proteins in biofluids | Large-scale proteomic profiling in neurodegenerative diseases [59] |
| ELISA Kits | Quantitative measurement of specific inflammatory markers | C3 complement, transferrin in neurodegenerative proteinopathies [105] [106] |
| Single-Cell RNA Sequencing | Cell-type-specific transcriptomic profiling of inflammatory responses | Identification of microglial subtypes in neurodegenerative diseases [49] |
| LncRNA/miRNA PCR Arrays | Profiling of non-coding RNAs involved in inflammatory regulation | MALAT1, GAS5, SNHG8 in acute ischemic stroke [110] |
| Machine Learning Algorithms (LASSO, SVM-RFE, Random Forest) | Feature selection and biomarker prioritization from high-dimensional data | Identification of IL18R1, NMUR1, RELA in Parkinson's disease [111] |
Discussion and Future Directions
The direct comparison of inflammatory biomarkers across neurological and psychiatric disorders reveals both shared and distinct pathophysiological mechanisms. Core inflammatory mediators including IL-6, CRP, and complement proteins demonstrate transdiagnostic alterations, while specific biomarkers like CSF sTREM2 in Alzheimer's disease and IL-4 in bipolar disorder show disorder-specific patterns. The emerging evidence supports a dimensional approach to neuroinflammation across traditional diagnostic boundaries.
Future research directions should prioritize standardized biomarker measurement protocols across disorders, longitudinal studies to establish temporal dynamics of inflammatory responses, and integration of multi-omic data to elucidate causal pathways. The Global Neurodegeneration Proteomics Consortium represents a promising model for large-scale collaborative biomarker discovery, having established one of the world's largest harmonized proteomic datasets encompassing over 35,000 biofluid samples across Alzheimer's disease, Parkinson's disease, frontotemporal dementia, and amyotrophic lateral sclerosis [59]. Such efforts will accelerate the development of inflammation-targeted therapies and companion diagnostics for personalized treatment approaches across the spectrum of brain disorders.
Interleukin-17A (IL-17A) has emerged as a critical pro-inflammatory cytokine with far-reaching implications across autoimmune, inflammatory, and neurodegenerative conditions. As the hallmark effector of T helper 17 (Th17) cells, IL-17A functions as a central coordinator of innate and adaptive immune responses, inducing the expression of chemokines, cytokines, and antimicrobial peptides that recruit neutrophils and other immune cells to sites of inflammation [112] [113]. Under physiological conditions, the IL-17A pathway provides essential defense against extracellular pathogens, particularly at mucosal barriers; however, dysregulated IL-17A signaling drives pathological inflammation in numerous disease states [113] [114]. The discovery that IL-17A is produced not only by Th17 cells but also by γδ T cells, innate lymphoid cells, and even central nervous system (CNS)-resident cells has expanded understanding of its multifaceted roles in both peripheral and neuroinflammatory diseases [112] [114].
The development of targeted biologic therapies against IL-17A has revolutionized treatment for certain autoimmune conditions while creating opportunities for therapeutic exploration in neurodegenerative diseases. This review synthesizes current preclinical and clinical evidence regarding IL-17A pathway inhibition, with particular emphasis on its relevance to inflammatory mechanisms in neurodegenerative disease research.
Molecular Mechanisms of IL-17A Signaling
IL-17A Production and Receptor Activation
The differentiation of naive CD4+ T cells into IL-17A-producing Th17 cells requires specific cytokine signals, primarily transforming growth factor-beta (TGF-β) together with interleukin-6 (IL-6) or interleukin-21 (IL-21) [112] [113]. This combination activates the JAK2/STAT3 pathway, leading to nuclear translocation of STAT3 and subsequent upregulation of the master transcription factors retinoic acid receptor-related orphan receptor gamma t (RORγt) and RORα [112] [113]. Interleukin-23 (IL-23) then sustains Th17 differentiation and promotes robust IL-17A production [112]. The resulting IL-17A signals through a receptor complex consisting of IL-17RA and IL-17RC subunits, which are widely expressed on epithelial cells, fibroblasts, and various immune cells [112] [113].
Downstream Signaling Cascades
Upon IL-17A binding, the IL-17RA/RC complex recruits the E3 ubiquitin ligase Act1 via the intracellular SEFIR domain, which subsequently engages TNF receptor-associated factor 6 (TRAF6) [112]. This interaction triggers activation of nuclear factor-kappa B (NF-κB) and mitogen-activated protein kinase (MAPK)/activator protein 1 (AP-1) signaling pathways, ultimately driving the expression of pro-inflammatory mediators [112]. These include chemokines (CXCL1, CXCL2, CXCL8) that recruit neutrophils, cytokines (G-CSF, IL-6) that amplify innate inflammation, and antimicrobial peptides that enhance host defense [113] [114].
Figure 1: IL-17A Signaling Pathway. IL-17A binding to its receptor complex (IL-17RA/RC) recruits Act1 and TRAF6, activating NF-κB and MAPK/AP-1 pathways that drive expression of inflammatory mediators.
Preclinical Evidence for IL-17A Inhibition
Animal Models of Neurodegenerative and Inflammatory Conditions
Preclinical studies across diverse disease models have demonstrated the therapeutic potential of IL-17A pathway inhibition. In investigations of anesthetic-induced neurotoxicity, genetic deletion of IL-17A or its pharmacological inhibition ameliorated sevoflurane-induced cognitive impairment in neonatal mice, with treated animals showing improved learning and memory function in behavioral tests [115]. IL-17A deficiency reduced neuroinflammation, as evidenced by downregulation of IL-1β, IL-6, and NADPH oxidase isoforms NOX2 and NOX4 in hippocampal tissues [115]. Mechanistically, IL-17A deletion promoted extracellular signal-regulated protein kinase (ERK) signaling pathway activation and cAMP response element-binding (CREB) protein nucleation in neurons, suggesting enhanced neurodevelopmental processes [115].
In immune checkpoint inhibitor-induced psoriasiform dermatitis models, combined anti-PD-1 and anti-CTLA-4 treatment synergistically amplified imiquimod-induced skin inflammation by upregulating IL-17A expression [116]. IL-17A monoclonal antibody (mAb) administration significantly ameliorated dermatitis severity, reflected by reduced ear thickness and Psoriasis Area and Severity Index (PASI) scores, alongside attenuation of epidermal hyperplasia on histology [116]. Transcriptomic analysis revealed that IL-17A blockade reversed pro-inflammatory gene expression patterns and suppressed IL-17, TNF, and Th17 signaling pathways [116].
Key Experimental Protocols in Preclinical Research
Imiquimod-Induced Dermatitis Model: Researchers established a low-dose imiquimod (IMQ)-induced dermatitis model in mice to evaluate ICI-exacerbated psoriasiform skin inflammation [116]. Mice received topical IMQ application daily for 7 days, combined with intraperitoneal injections of anti-PD-1 and/or anti-CTLA-4 monoclonal antibodies. For therapeutic intervention, anti-IL-17A mAb was administered at multiple time points (days -1, 3, and 5). Disease severity was assessed through serial measurements of ear thickness, PASI scoring, and histopathological evaluation of skin sections. Molecular analyses included RT-qPCR of inflammatory cytokines (IL-17A, IL-6, IL-22, IL-23) and RNA sequencing of skin samples [116].
Sevoflurane-Induced Cognitive Impairment Model: To investigate anesthetic-induced neurotoxicity, neonatal mice (postnatal day 6) were exposed to 3% sevoflurane for 2 hours daily over three consecutive days [115]. IL-17A knockout mice and wild-type controls were used to assess the specific role of IL-17A. For pharmacological inhibition studies, anti-IL-17A neutralizing antibody was administered intraperitoneally. Behavioral tests including Morris water maze and fear conditioning were conducted during adulthood to assess long-term cognitive function. Hippocampal tissues were analyzed for inflammatory markers, oxidative stress parameters, and neurodevelopmental proteins via Western blot, RT-PCR, and immunohistochemistry [115].
Table 1: Key Preclinical Findings of IL-17A Pathway Inhibition
| Disease Model | Intervention | Key Outcomes | Reference |
|---|---|---|---|
| Sevoflurane-induced cognitive impairment (neonatal mice) | IL-17A genetic deletion or anti-IL-17A mAb | Improved learning and memory; reduced neuroinflammation (IL-1β, IL-6, NOX2/4); enhanced ERK/CREB signaling | [115] |
| ICI-induced psoriasiform dermatitis (mice) | Anti-IL-17A mAb (secukinumab) | Decreased ear thickness and PASI scores; attenuated epidermal hyperplasia; downregulated IL-17/Th17 signaling | [116] |
| Experimental autoimmune encephalomyelitis (mice) | IL-17A neutralization or genetic deficiency | Ameliorated disease severity; reduced CNS inflammation and demyelination | [114] |
Clinical Evidence for IL-17A-Targeted Therapies
Neurological and Autoimmune Applications
Clinical studies have begun to validate the therapeutic potential of IL-17A inhibition across multiple conditions. In a retrospective study of patients with acetylcholine receptor antibody-positive myasthenia gravis (MG), secukinumab treatment (150 mg weekly for 4 weeks, then 150 mg every 4 weeks for 24 weeks) resulted in significant clinical improvements [117]. By week 24, patients demonstrated 60.7% reduction in Quantitative MG (QMG) scores, 58.3% improvement in MG-specific quality of life (MG-QOL15), and 64.1% enhancement in activities of daily living (MG-ADL) scores [117]. These clinical benefits correlated with immunomodulatory effects, including reduced autoantibody titers, suppression of pathogenic Th17/T follicular helper cells, and downregulation of the IL-17A/IL-6 pathway [117].
In oncology settings, IL-17A blockade successfully managed immune-related cutaneous adverse events (ircAEs) induced by checkpoint inhibitor therapy [116]. Five cancer patients who developed grade 2-3 psoriasiform rashes during ICI treatment achieved rapid symptom control with secukinumab, enabling uninterrupted antitumor therapy. Notably, hepatic tumor regression was observed in one patient with hepatocellular carcinoma, suggesting IL-17A inhibition does not compromise antitumor efficacy [116].
For psoriatic arthritis, the nanobody sonelokimab—which targets both IL-17A and IL-17F with high affinity—demonstrated robust efficacy in a phase 2 trial [118]. At week 12, significantly more patients achieved ACR50 response with sonelokimab (46.3-46.5%) versus placebo (20.0%), with comparable benefits observed across secondary endpoints including ACR20 and PASI90 responses [118]. The nanobody's smaller molecular size (~40 kDa) may enhance tissue penetration to difficult-to-reach inflammatory sites [118].
Clinical Trial Methodologies
Myasthenia Gravis Study Design: This retrospective study enrolled 29 AChR-Ab+ generalized MG patients (MGFA class IIa-IVb) who received secukinumab according to a standardized regimen [117]. Stable doses of conventional therapies (pyridostigmine, corticosteroids, immunosuppressive agents) were permitted throughout the study. Longitudinal assessments included clinical scoring (QMG, MG-QOL15, MG-ADL), serum AChR-Ab titers, flow cytometry analysis of Th17/Tfh cell frequencies, and cytokine profiling at baseline, 4, 12, and 24 weeks [117].
Immune Checkpoint Inhibitor Toxicity Management: Cancer patients who developed moderate-to-severe psoriasiform rashes during ICI therapy received secukinumab (150 mg/week) alongside conventional treatments such as oral prednisone [116]. Dermatological response was assessed using the Dermal Toxicity Assessment Scale (DTAS), with documentation of symptom evolution, time to resolution, and ICI treatment continuity. Tumor response was monitored radiologically and through serial tumor markers [116].
Table 2: Clinical Evidence for IL-17A-Targeted Therapies
| Condition | Therapeutic Agent | Study Design | Key Efficacy Outcomes | Reference |
|---|---|---|---|---|
| Myasthenia Gravis | Secukinumab (anti-IL-17A mAb) | Retrospective, 29 patients, 24 weeks | 60.7% reduction in QMG score; 64.1% improvement in MG-ADL; reduced AChR-Ab titers | [117] |
| ICI-induced psoriasiform rash | Secukinumab (anti-IL-17A mAb) | Case series, 5 patients | Rapid symptom control within 24h; complete rash resolution by 3 weeks; maintained antitumor response | [116] |
| Psoriatic Arthritis | Sonelokimab (anti-IL-17A/F nanobody) | Phase 2 RCT, 207 patients, 12 weeks | ACR50: 46.3-46.5% vs 20.0% placebo; PASI90: 59.3-76.9% vs 15.4% placebo | [118] |
Experimental Visualization: Workflow for Evaluating IL-17A Inhibition
Figure 2: Integrated Workflow for Evaluating IL-17A Inhibition. Comprehensive experimental approach spanning preclinical and clinical research methodologies for investigating IL-17A pathway modulation.
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Research Reagents for IL-17A Pathway Investigation
| Reagent/Category | Specific Examples | Research Application | Key Functions |
|---|---|---|---|
| Animal Models | IL-17A knockout mice; Imiquimod-induced dermatitis; Sevoflurane neurotoxicity | Disease modeling; Mechanistic studies | Enable investigation of IL-17A functions in specific pathological contexts |
| Therapeutic Antibodies | Secukinumab (anti-IL-17A); Ixekizumab (anti-IL-17A); Sonelokimab (anti-IL-17A/F) | Preclinical and clinical intervention | Neutralize IL-17A signaling; some agents target both IL-17A and IL-17F |
| Detection Assays | IL-17A ELISA; Flow cytometry (Th17 cells); Phospho-STAT3 staining | Biomarker quantification; Immune monitoring | Measure IL-17A pathway activity and cellular responses |
| Molecular Tools | RORγt antagonists; STAT3 inhibitors; siRNA for IL-17RA | Pathway modulation; Target validation | Specifically inhibit components of IL-17A signaling cascade |
| Analysis Methods | RNA sequencing; Cytokine profiling; Histopathological scoring | Comprehensive phenotyping | Characterize transcriptomic, inflammatory, and tissue responses |
The accumulating preclinical and clinical evidence solidifies IL-17A as a compelling therapeutic target across multiple disease domains, particularly within neuroinflammatory contexts. The consistent findings that IL-17A blockade ameliorates pathological processes without compromising host defense or antitumor immunity underscore its strategic value in therapeutic development [116] [117] [115]. The dual benefit observed in oncology settings—where IL-17A inhibition managed immune-related adverse events while potentially enhancing antitumor responses—suggests complex immunomodulatory mechanisms that warrant further investigation [116].
Future research directions should prioritize elucidating tissue-specific aspects of IL-17A signaling, particularly within the central nervous system where IL-17A may directly influence neuronal function and blood-brain barrier integrity [112] [115]. The development of novel therapeutic modalities such as nanobodies with enhanced tissue penetration and dual-specificity agents targeting both IL-17A and IL-17F represents promising avenues for optimizing therapeutic efficacy [118]. Additionally, prospective clinical trials with longer follow-up durations are needed to establish the long-term safety profile of IL-17A-targeted therapies, especially in vulnerable populations such as cancer patients and those with chronic neurodegenerative conditions [116] [117].
As precision medicine approaches advance, identifying biomarkers that predict treatment response will be crucial for optimizing patient selection. The integration of IL-17A pathway modulation into combination therapies may yield synergistic benefits, particularly for complex neurodegenerative diseases where neuroinflammation intersects with multiple pathological processes. Continued investigation into the intricate biology of IL-17A will undoubtedly expand therapeutic opportunities and deepen understanding of inflammatory mechanisms in human disease.
12/15-Lipoxygenase Inhibition in Stroke and Neurodegeneration Models
Inhibition of the 12/15-lipoxygenase (12/15-LOX) pathway represents an emerging therapeutic strategy for cerebrovascular and neurodegenerative diseases. This whitepaper synthesizes current evidence demonstrating that 12/15-LOX inhibition significantly mitigates neuroinflammation, reduces infarct volume, improves functional outcomes, and attenuates key neurodegenerative pathologies across multiple disease models. The enzyme has been implicated in the pathogenesis of ischemic stroke, vascular dementia, Alzheimer's disease, and subarachnoid hemorrhage through mechanisms involving lipid peroxidation, inflammasome activation, blood-brain barrier disruption, and neuroinflammatory signaling. This technical analysis comprehensively examines the molecular mechanisms, preclinical evidence, experimental methodologies, and therapeutic potential of 12/15-LOX inhibition, providing researchers with essential protocols and resources for advancing investigation in this promising field.
12/15-lipoxygenase is a non-heme iron-containing dioxygenase that catalyzes the oxidation of arachidonic acid and other polyunsaturated fatty acids, generating bioactive lipid mediators including 12-hydroxyeicosatetraenoic acid (12-HETE) and 15-HETE [119]. The enzyme is highly expressed in brain regions vulnerable to ischemic and degenerative damage, including the cerebellum, basal ganglia, hippocampus, neurons, and specific glial populations [119]. Under pathological conditions, 12/15-LOX activation triggers a cascade of detrimental events: it directly oxidizes lipid membranes containing polyunsaturated fatty acids without preceding phospholipase action, leading to organelle damage [120]; generates pro-inflammatory mediators that perpetuate neuroinflammation [121]; and contributes to blood-brain barrier disruption, edema formation, and neuronal cell death [121].
The pivotal role of 12/15-LOX in neurodegenerative processes is substantiated by its elevated expression in the frontal and temporal lobes and cerebrospinal fluid of Alzheimer's disease patients [119], and its upregulation following cerebral ischemia [120]. 12/15-LOX and its metabolites directly activate p38 mitogen-activated protein kinase (p38 MAPK) and cytosolic phospholipase A2 (cPLA2), creating a feed-forward loop that amplifies neuroinflammatory signaling [119]. Within the broader context of inflammatory responses in neurodegenerative disease research, 12/15-LOX represents a convergent pathway linking oxidative stress, neuroinflammation, and cellular damage across multiple neurological conditions.
Molecular Mechanisms and Signaling Pathways
Core Pathway Architecture
The 12/15-LOX pathway functions as a critical amplifier of neuroinflammatory signaling through multiple interconnected mechanisms. As illustrated below, the pathway integrates with key inflammatory processes including inflammasome activation, cytokine signaling, and neurodegenerative protein aggregation.
Figure 1: 12/15-LOX Neuroinflammatory Signaling Pathway. This diagram illustrates the core signaling mechanisms through which 12/15-LOX activation amplifies neuroinflammatory processes. The pathway demonstrates how 12/15-LOX initiates a feed-forward cycle of inflammation through cPLA2-mediated arachidonic acid release and generates oxidized lipids that activate inflammasome complexes, ultimately driving neurodegenerative pathology.
Key Pathophysiological Mechanisms
The diagram above captures several critical pathophysiological mechanisms through which 12/15-LOX contributes to neurodegeneration:
Lipid Peroxidation and Membrane Damage: 12/15-LOX directly oxidizes lipid membranes containing polyunsaturated fatty acids without requiring preceding phospholipase action, leading to direct attack on organelles including mitochondria [120]. This underlies the cytotoxic activity of 12/15-LOX, which is upregulated in neurons and endothelial cells after stroke [121].
Inflammasome Activation: Oxidized lipids generated by 12/15-LOX activate NLRP1 and NLRP3 inflammasomes [121]. Inhibition of 12/15-LOX with ML351 significantly reduces NLRP1 and NLRP3 immunoreactivity following cerebral ischemia, with NLRP3 showing more pronounced expression [121].
Blood-Brain Barrier Disruption: 12/15-LOX activation contributes to edema formation through direct effects on vascular integrity [120]. The enzyme is upregulated in endothelial cells after stroke, where it promotes barrier dysfunction [121].
Protein Aggregation Pathology: 12/15-LOX inhibition reduces both Aβ1-42 deposition and Tau hyperphosphorylation in models of vascular dementia [119]. The enzyme's metabolites have been detected in elevated levels in the brains of Alzheimer's disease patients [119].
Quantitative Evidence from Preclinical Studies
Efficacy Outcomes Across Disease Models
Table 1: Therapeutic Efficacy of 12/15-LOX Inhibition in Preclinical Neurological Disease Models
| Disease Model | Inhibitor | Key Efficacy Parameters | Proposed Mechanisms | Citation |
|---|---|---|---|---|
| Ischemic Stroke (MCAo mouse) | ML351 (50 mg/kg) | ↓ Infarct volume 40-60%↓ Neurological deficit scores↓ Lipid peroxidation (MDA) | Suppressed NLRP3 inflammasome↓ IL-1β, IL-6, TNF-α↑ IL-10, TGF-β | [121] |
| Vascular Dementia (rUCCAO mouse) | Brozopine (BZP) | Improved cognitive functionRestored fine motor skills↓ Aβ1-42 & p-Tau | Inhibited 12/15-LOX/cPLA2/p38 MAPK↓ TNF-α, IL-1β | [119] |
| Subarachnoid Hemorrhage (Mouse model) | ML351 (25 mg/kg) | ↓ Microvessel constriction↓ Microthrombi formationImproved cerebral perfusion | ↓ 12-S-HETEReduced platelet activation | [122] |
| Global Cerebral Ischemia | LOXBlock-1 | ↓ Infarct size when given 4h post-ischemiaReduced tPA-associated bleeding | Reduced lipid peroxidationBlood-brain barrier protection | [120] |
Neuroinflammatory Modulation
Table 2: Effects of 12/15-LOX Inhibition on Neuroinflammatory Parameters
| Inflammatory Parameter | Effect of Inhibition | Temporal Window | Significance |
|---|---|---|---|
| Pro-inflammatory Cytokines | ↓ IL-1β, IL-6, TNF-α | Significant at 6h and/or 24h | Suppresses acute neuroinflammation |
| Anti-inflammatory Cytokines | ↑ IL-10, TGF-β | Increased at 24h-72h | Promotes resolution phase |
| Inflammasome Signaling | ↓ NLRP1 & NLRP3 activation | All timepoints (6h-72h) | Reduces innate immune activation |
| Lipid Peroxidation | ↓ MDA levels | Sustained reduction (6h-72h) | Attenuates oxidative membrane damage |
| Caspase-1 Activation | ↓ Cleaved caspase-1 | Co-localized with NLRP3 reduction | Limits pyroptotic cell death |
Experimental Protocols and Methodologies
In Vivo Disease Models
Focal Cerebral Ischemia Model (Middle Cerebral Artery Occlusion)
The transient middle cerebral artery occlusion (MCAo) model represents the gold standard for preclinical stroke research:
Surgical Procedure:
- Anesthetize mice (8-12 weeks) using 4% isoflurane for induction, maintained at 1-2% during surgery.
- Maintain body temperature at 37±0.2°C using a homeothermic blanket with rectal probe.
- Monitor oxygen saturation and heart rate throughout the procedure using pulse oximetry.
- Expose the common, external, and internal carotid arteries through a midline cervical incision.
- Insert a silicone-coated monofilament (6-0 or 7-0) into the external carotid artery and advance to the origin of the middle cerebral artery.
- Confirm occlusion by measuring regional cerebral blood flow (rCBF) using laser Doppler flowmetry; successful occlusion is defined as rCBF reduction to <30% of baseline.
- Maintain occlusion for 60 minutes, then withdraw the filament to allow reperfusion.
- Administer the 12/15-LOX inhibitor (e.g., ML351 at 50 mg/kg) or vehicle intraperitoneally at recanalization [121].
Outcome Measures:
- Infarct volume quantification at 24h or 72h post-reperfusion using TTC staining or Nissl staining.
- Neurological deficit scoring using a standardized scale (0 = no deficit, 1 = forelimb flexion, 2 = decreased resistance to lateral push, 3 = unidirectional circling, 4 = longitudinal spinning, 5 = no movement).
- Lipid peroxidation assessment via malondialdehyde (MDA) assay.
- Inflammasome activation analysis through immunohistochemistry for NLRP1 and NLRP3 [121].
Vascular Dementia Model (Unilateral Carotid Artery Occlusion)
The right unilateral common carotid artery occlusion (rUCCAO) model produces chronic cerebral hypoperfusion:
Surgical Procedure:
- Anesthetize C57BL/6 mice (6-8 weeks) using isoflurane (4% induction, 2% maintenance).
- Make a midline cervical incision and carefully isolate the right common carotid artery from the vagus nerve.
- Double-ligate the artery both proximally and distally to the heart using 6-0 surgical sutures.
- Close the incision and allow recovery in a controlled environment.
- For sham operations, expose and isolate the artery without ligation.
- Administer the 12/15-LOX inhibitor (e.g., Brozopine) or vehicle for 28 days post-surgery [119].
Outcome Measures:
- Cognitive assessment using Morris water maze or novel object recognition tests.
- Motor function evaluation through beam walking or rotarod performance.
- Biochemical analysis of brain tissue for Aβ1-42 deposition, tau phosphorylation, and inflammatory markers.
- Western blot analysis of 12/15-LOX, cPLA2, p-p38 MAPK, and cytokine expression [119].
In Vitro Assessment Methods
HT22 Cell Neuroprotection Assay
The HT22 mouse hippocampal cell line provides a standardized model for assessing 12/15-LOX-dependent oxidative stress:
Procedure:
- Maintain HT22 cells in high-glucose Dulbecco's Modified Eagle Medium (DMEM) supplemented with 10% fetal bovine serum at 37°C in 5% CO₂.
- Plate cells in 96-well plates at a density of 10,000 cells/well and allow to adhere overnight.
- Pre-treat cells with 12/15-LOX inhibitors at varying concentrations for 2-6 hours before insult.
- Induce oxidative stress using 1-5mM Hâ‚‚Oâ‚‚ for 12-24 hours or transfect cells to overexpress 12/15-LOX.
- Assess cell viability using MTT assay, calcein-AM staining, or LDH release.
- Quantify lipid peroxidation products using C11-BODIPYâµâ¸Â¹/âµâ¹Â¹ fluorescence or MDA assay.
- Analyze 12/15-LOX metabolic products (12-HETE, 15-HETE) via ELISA or LC-MS [119] [120].
Research Reagent Solutions
Table 3: Essential Research Reagents for 12/15-LOX Investigation
| Reagent Category | Specific Examples | Research Application | Key Features |
|---|---|---|---|
| 12/15-LOX Inhibitors | ML351, Brozopine (BZP), Baicalein, LOXBlock-1 | In vivo and in vitro target validation | ML351: Potent and selective (IC₅₀ ~0.2-0.5 µM)BZP: In clinical development for strokeBaicalein: Natural product inhibitor |
| Antibodies | Anti-12/15-LOX (Santa Cruz, sc-365194)Anti-15-LOX (Santa Cruz, sc-133085)Anti-NLRP3Anti-p-p38 MAPK | Target protein detection and localization | Western blot, immunohistochemistry, and immunofluorescence applications |
| ELISA Kits | 12-HETE ELISA (Abcam, ab133034)15-HETE ELISAp-Tau217 ELISAAβ1-42 ELISA | Metabolic and biomarker quantification | Sensitive detection in biological fluids and tissue homogenates |
| Cell Lines | HT22 (mouse hippocampal)12/15-LOX-overexpressed HT22 | In vitro mechanism studies | Well-established model for oxidative stress and neuroprotection assays |
| Animal Models | 12/15-LOX-/- micerUCCAO modelMCAo model | In vivo pathophysiological studies | Genetic validation of pharmacological effects |
Therapeutic Implications and Clinical Translation
The therapeutic targeting of 12/15-LOX represents a promising strategy for multiple neurodegenerative conditions. Brozopine (BZP), a novel 12/15-LOX inhibitor developed in China, has demonstrated significant neuroprotective efficacy while successfully progressing through preclinical, phase I, and phase II clinical trials for ischemic stroke, and is currently undergoing phase III evaluation [119]. This clinical advancement underscores the translational potential of this mechanism.
The optimal therapeutic window for 12/15-LOX inhibition appears relatively wide, with efficacy demonstrated even when treatment is initiated 4 hours after ischemia onset in experimental models [120]. This is clinically significant given the typical delays in hospital presentation following stroke. Additionally, 12/15-LOX inhibitors have shown potential to reduce tPA-associated bleeding complications, suggesting possible combination therapy approaches [120].
Beyond acute cerebrovascular applications, 12/15-LOX inhibition demonstrates promise for chronic neurodegenerative conditions. The pathway's involvement in Aβ and tau pathology [119], along with its role in sustaining chronic neuroinflammation through microglial and astrocyte activation [123], positions it as a compelling target for Alzheimer's disease, vascular dementia, and potentially other proteinopathies.
12/15-LOX inhibition represents a mechanistically grounded therapeutic approach with demonstrated efficacy across multiple preclinical models of stroke and neurodegeneration. The consistent findings of reduced infarct volume, improved functional outcomes, attenuated neuroinflammation, and suppressed protein aggregation pathology highlight the potential of targeting this pathway. Future research directions should include optimization of brain-penetrant inhibitors, exploration of combination therapies with neuroprotective or thrombolytic agents, extension to additional neurodegenerative conditions, and identification of biomarkers for patient stratification. The ongoing clinical development of 12/15-LOX inhibitors offers promising prospects for addressing the significant unmet needs in cerebrovascular and neurodegenerative diseases.
Microglial dysfunction is a core driver of pathogenesis in neurodegenerative diseases, creating a compelling rationale for therapeutic targeting. This whitepaper provides a comparative analysis of current strategies for modulating microglial activity, from receptor-targeted biologics to small molecule interventions and cellular repopulation. We synthesize data from recent preclinical and clinical studies, highlighting the mechanistic pathways, developmental status, and key challenges for each approach. The analysis is framed within the context of inflammatory responses in neurodegenerative disease research, emphasizing how precise modulation of microglial function can interrupt the chronic neuroinflammatory cascade. For researchers and drug development professionals, this review offers both a strategic overview of the therapeutic landscape and detailed methodological insights for advancing microglial-focused investigations.
Within the central nervous system (CNS), microglia serve as the primary resident immune cells, constantly surveying the microenvironment and responding to homeostatic disturbances [8] [124]. In neurodegenerative diseases, including Alzheimer's disease (AD), Parkinson's disease (PD), and amyotrophic lateral sclerosis (ALS), microglial activation transitions from a protective to a chronic, dysregulated state that amplifies neuroinflammation and accelerates neuronal damage [125] [83]. Genome-wide association studies have solidified the link between microglial genes and neurodegenerative disease risk, highlighting pathways that now represent promising therapeutic targets [49] [124].
The simplistic M1/M2 polarization paradigm has been superseded by a more nuanced understanding of microglial states, revealed through single-cell technologies that identify diverse, disease-associated profiles such as disease-associated microglia (DAM) and lipid-droplet-accumulating microglia (LDAM) [49] [8]. This heterogeneity underscores the complexity of therapeutic modulation—the goal is not merely to suppress microglial activity but to reprogram these cells toward protective, homeostatic functions. This whitepaper analyzes the leading therapeutic strategies designed to achieve this rebalancing, providing a comparative framework for researchers developing interventions against neuroinflammatory pathogenesis.
Comparative Analysis of Therapeutic Strategies
Therapeutic approaches for microglial modulation target specific receptors, signaling pathways, and cellular processes to restore immune homeostasis. The following analysis and tables provide a structured comparison of these strategies.
Table 1: Receptor-Targeted Therapeutic Approaches
| Therapeutic Target | Class of Modulator | Mechanism of Action | Key Findings/Outcomes | Development Status |
|---|---|---|---|---|
| TREM2 | Agonist mAb (AL002/VHB937) | Activates TREM2 signaling, enhances phagocytosis, promotes microglial survival [49] | Reduced Aβ plaque burden, improved cognition in AD models; dose-dependent reduction of CSF sTREM2 in Phase 1 [49] | Phase 2 trials for AD and early-stage ALS (NCT04592874, NCT06643481) [49] |
| TREM2 | Small Molecule Agonist (VG-3927) | Brain-penetrant TREM2 agonist, induces DAM-like phenotype [49] | Reduced Aβ pathology in preclinical models [49] | Phase 1 trial (NCT06343636), data expected 2025 [49] |
| CD33/Siglec-3 | Blocking Antibody (AL003) | Suppresses CD33 activity to enhance Aβ uptake [49] | CD33 knockout enhances anti-inflammatory response, reduces Aβ plaques, improves cognition [49] | Ongoing clinical trials (NCT identifier not specified in sources) [49] |
| c-Cbl | E3 Ubiquitin Ligase Modulator | Regulates transition from M1 to M2 phenotype via PI3K/Akt pathway [126] | c-Cbl deletion exacerbates pro-inflammatory response and dopaminergic neuron loss in PD models [126] | Preclinical research stage [126] |
Table 2: Targeting Signaling Pathways and Novel Cell Death Mechanisms
| Therapeutic Focus | Specific Target/Pathway | Mechanism of Action | Key Findings/Outcomes | Development Status |
|---|---|---|---|---|
| Microglial Polarization | PI3K/Akt Signaling | c-Cbl modulates phenotype shift; inhibition promotes M1 state [126] | c-Cbl knockout shifts microglia to neurotoxic M1 state, accelerating PD pathology [126] | Preclinical research stage [126] |
| Novel Cell Death Pathways | Ferroptosis, Cuproptosis | Inhibition of microglial inflammatory cell death [125] | Attenuates neuroinflammation and neurodegeneration [125] | Early preclinical investigation [125] |
| Microglial Repopulation | CSF1R Inhibition | Temporary microglial depletion allows repopulation with homeostatic cells [127] | Repopulated microglia exhibit restored homeostasis and function [127] | Preclinical stage; challenges in clinical translation [127] |
Experimental Protocols for Key Methodologies
Assessing Microglial Phagocytosis In Vitro
Purpose: To quantify the phagocytic capacity of different microglial models in response to therapeutic modulators, such as TREM2 agonists [49] [128].
Primary Workflow:
- Cell Culture: Plate primary human microglia, iPSC-derived microglia, or immortalized cell lines (e.g., HMC3) in appropriate culture vessels. Maintain cells in serum-supplemented or defined media [128].
- Therapeutic Pre-treatment: Incubate cells with the modulator (e.g., TREM2 agonist antibody or small molecule) and an appropriate vehicle control for a predetermined time (e.g., 24 hours) [49].
- Phagocytosis Assay: Add pHrodo-labeled substrates (e.g., Aβ1-42 fibrils, E. coli bioparticles, or synaptosomes) to the culture medium. pHrodo fluorescence intensifies in the acidic phagolysosomal environment, allowing quantitative measurement [128].
- Quantification and Analysis:
- Flow Cytometry: Harvest cells and analyze the fluorescence intensity of the cell population to determine the percentage of phagocytic cells and the mean uptake per cell.
- High-Content Imaging: Fix cells after the assay and stain with a microglial marker (e.g., Iba1). Use automated microscopy to count the number of fluorescently labeled particles per cell.
Key Considerations: Primary human microglia and iPSC-derived microglia demonstrate significantly higher baseline phagocytic capacity compared to immortalized cell lines like HMC3 [128]. The choice of substrate (Aβ, myelin debris, etc.) should be relevant to the disease context being studied.
Evaluating Microglial Phenotype Polarization
Purpose: To determine the effect of a modulator on the polarization state of microglia, typically assessed by shifts in M1 (pro-inflammatory) and M2 (anti-inflammatory) marker expression [126].
Primary Workflow:
- Cell Stimulation and Treatment:
- Induce a pro-inflammatory state using lipopolysaccharide (LPS, e.g., 100 ng/mL) or IFN-γ.
- Co-treat cells with the experimental modulator (e.g., a c-Cbl mimetic or PI3K/Akt pathway activator) [126].
- For M2 polarization, use stimuli such as IL-4 or IL-13.
- RNA Extraction and qRT-PCR: Isolate total RNA and synthesize cDNA. Perform quantitative PCR using primers for M1 markers (e.g., IL1B, TNF, NOS2) and M2 markers (e.g., ARG1, CD206, IL10) [126].
- Protein Analysis:
- Immunofluorescence/Cytochemistry: Fix and stain cells for M1 (e.g., iNOS) and M2 (e.g., CD206) markers. Quantify fluorescence intensity or positive cell count [126].
- ELISA: Measure the secretion of pro-inflammatory (TNF-α, IL-6, IL-1β) and anti-inflammatory (IL-10, TGF-β) cytokines in the conditioned media [126].
- Functional Assays: Correlate phenotypic changes with functional readouts, such as nitric oxide production (an M1-associated function) or phagocytic capacity.
Key Considerations: The M1/M2 classification is an oversimplification of microglial states in vivo. Where possible, supplement these analyses with single-cell RNA sequencing to uncover more complex, disease-relevant transcriptional signatures [8].
Signaling Pathways in Microglial Modulation
The efficacy of microglial modulators depends on their engagement with specific intracellular signaling cascades. The following diagrams, generated using DOT language, visualize two key pathways targeted by current therapeutic strategies.
TREM2 Signaling Pathway
c-Cbl Modulation of Microglial Phenotype
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Models for Microglial Research
| Reagent / Model | Specification/Example | Primary Function in Research |
|---|---|---|
| Primary Human Microglia | Isolated from biopsy/autopsy tissue [128] | Gold standard for human microglial biology; high phagocytic capacity and relevant antigenicity [128] |
| iPSC-Derived Microglia | Differentiated from induced pluripotent stem cells (>40 day protocol) [128] | Recapitulates human microglial expression profile; suitable for patient-specific disease modeling [128] |
| Immortalized Cell Lines (HMC3) | SV40-immortalized human microglial clone [128] | Accessible, homogenous resource for high-throughput screening; may differ phenotypically from primary cells [128] |
| Primary Mouse Microglia | Isolated from neonatal or adult mouse brain [128] | Readily available model for in vivo and in vitro studies; notable species-specific differences in secretome (e.g., nitric oxide production) [128] |
| TREM2 Agonist Antibodies | AL002c, VHB937 [49] | Tool compounds for validating TREM2-targeted therapies and studying TREM2-dependent phagocytosis and signaling [49] |
| CSF1R Inhibitors | PLX3397, PLX5622 [127] | Pharmacological agents for microglial depletion studies, enabling investigation of microglial repopulation dynamics [127] |
| Polarization Inducers | LPS/IFN-γ (M1), IL-4/IL-13 (M2) [126] | Standard stimuli to drive microglial polarization toward pro-inflammatory or anti-inflammatory states in vitro [126] |
| Iba1 Antibody | Ionized calcium-binding adapter molecule 1 [8] | Gold-standard immunohistochemical marker for identifying microglia in tissue sections [8] |
The strategic modulation of microglia represents a frontier in developing disease-modifying therapies for neurodegenerative diseases. As this analysis demonstrates, the therapeutic landscape is diverse, encompassing biologic, small-molecule, and cellular replacement strategies aimed at recalibrating the neuroimmune environment. The translation of these approaches from preclinical models to the clinic hinges on a deepening understanding of microglial heterogeneity and the complex signaling networks that dictate their function. For researchers, the continued refinement of experimental models, coupled with the application of single-cell omics and multimodal data integration, will be critical for aligning specific microglial states with therapeutic outcomes. The progress in targeting key regulators like TREM2 and emerging pathways such as microglial-specific cell death underscores the potential of immune-focused strategies to alter the trajectory of neurodegenerative diseases.
Lessons from Failed Trials and Promising New Directions
Neurodegenerative diseases represent one of the most significant public health challenges of our time, with more than 57 million people affected globally—a figure projected to double every 20 years [59]. While these conditions exhibit diverse clinical presentations and underlying pathologies, chronic inflammation has emerged as a critical biological pathway connecting Alzheimer's disease (AD), Parkinson's disease (PD), frontotemporal dementia (FTD), and amyotrophic lateral sclerosis (ALS). The intricate interplay between neuroinflammation and disease progression has become a focal point for therapeutic development, yet targeting this complex biological process has proven exceptionally challenging.
The failure of multiple high-profile clinical trials targeting inflammatory mechanisms in neurodegenerative diseases has revealed fundamental gaps in our understanding of disease pathophysiology and trial methodology. Simultaneously, emerging technologies and novel approaches are providing unprecedented insights into inflammatory pathways, offering hope for more targeted interventions. This whitepaper analyzes key lessons from recent trial failures, examines promising new directions in inflammatory targeting, and provides technical guidance for researchers navigating this complex landscape. Understanding both the pitfalls and prospects of targeting neuroinflammation is essential for advancing effective treatments for these devastating conditions.
Analysis of Recent Clinical Trial Failures
The high failure rate of clinical trials in neurodegenerative diseases underscores the complexity of targeting inflammatory pathways and the methodological challenges in trial design and execution.
GLP-1 Agonists in Alzheimer's Disease
The recent failure of Novo Nordisk's semaglutide in two Phase III Alzheimer's trials (EVOKE and EVOKE+) represents a significant setback for the theory that GLP-1 receptor agonists could combat neurodegeneration through anti-inflammatory mechanisms [129] [130]. These studies, which enrolled 3,808 adults with mild cognitive impairment or mild dementia due to Alzheimer's disease, demonstrated no significant benefit over placebo in reducing disease progression after two years of follow-up [130].
Table 1: GLP-1 Agonist Trial Failure Analysis
| Trial Component | Details | Implications |
|---|---|---|
| Mechanistic Rationale | Proposed reduction of brain inflammation, improved insulin signaling, discouragement of harmful protein buildup [130] | Theory not validated in human trials despite supportive preclinical data |
| Trial Design | Two large Phase III trials (EVOKE/EVOKE+) with 2-year follow-up [130] | Rigorous design eliminates methodological concerns about failure |
| Biomarker Results | Improvement in some Alzheimer's biomarkers without clinical benefit [129] [130] | Suggests dissociation between biomarker changes and clinically meaningful outcomes |
| Therapeutic Context | Building on prior liraglutide mid-stage failure with similar results [130] | Indicates class-specific limitation rather than compound-specific issue |
Despite strong mechanistic rationale based on GLP-1 drugs' profound benefits on metabolism and their ability to reduce inflammation in peripheral tissues, the results highlight the distinct challenges of targeting neuroinflammation specifically within the central nervous system. The dissociation between positive biomarker changes and lack of clinical benefit suggests that the inflammatory components targeted by semaglutide may not be drivers of clinical progression in established Alzheimer's disease, or that treatment may need to begin much earlier in the disease course [130].
The "Regression to the Truth" Phenomenon in Clinical Development
The concept of "regression to the truth" provides a critical framework for understanding why promising Phase II results often fail to translate into Phase III successes. This statistical phenomenon describes the tendency for extreme results—either positive or negative—observed in an initial trial to move closer to the true effect when replicated in larger, more rigorous studies [131]. In neurodegenerative drug development, this manifests when positive Phase II trial results may simply reflect statistical anomaly rather than true efficacy.
Analysis of clinical development success rates across therapeutic areas reveals that only approximately 30% of Phase III trials yield positive results after a successful Phase II trial [131]. In idiopathic pulmonary fibrosis (IPF), which shares pathophysiological similarities with neurodegenerative conditions including inflammatory components, three pivotal trials of novel therapies (zinpentraxin alfa, ziritaxestat, and pamrevlumab) demonstrated this pattern dramatically:
Table 2: "Regression to Truth" Case Studies in IPF Drug Development
| Therapeutic Candidate | Mechanism | Phase II Results | Phase III Results | Analysis of Discrepancy |
|---|---|---|---|---|
| Zinpentraxin Alfa | Recombinant human pentraxin-2 protein [131] | Positive (FVC, 6MWD) [131] | Negative (terminated early for futility) [131] | Post-hoc analysis revealed Phase II results driven by outliers in placebo group [131] |
| Ziritaxestat | Autotaxin inhibitor targeting LPA pathway [131] | Positive signal for forced vital capacity (FVC) [131] | Negative (terminated early for safety concerns) [131] | Narrow therapeutic window and safety concerns not apparent in smaller trial [131] |
| Pamrevlumab | Monoclonal CTGF antibody [131] | Positive (FVC) [131] | Negative [131] | Inadequate Phase II sample size provided unreliable efficacy estimates [131] |
These cases highlight fundamental methodological flaws that contribute to false positive Phase II results, including inadequate sample sizes, overreliance on surrogate endpoints, and failure to account for background therapies [131]. For neurodegenerative disease researchers, these examples underscore the importance of robust Phase II trial designs with sufficient sample sizes to generate reliable efficacy estimates before progressing to pivotal trials.
Novel Therapeutic Directions Targeting Inflammation
Despite recent setbacks, several innovative approaches to targeting neuroinflammation show significant promise, leveraging novel mechanisms and advanced therapeutic modalities.
Targeting the NLRP3 Inflammasome Pathway
The NLRP3 inflammasome, a multiprotein complex that plays a central role in triggering inflammation in response to infection or tissue damage, has emerged as a promising target for neurodegenerative diseases [132]. When dysregulated, NLRP3 activation contributes to chronic inflammation and cellular damage in conditions including Alzheimer's, Parkinson's, and rare genetic disorders.
Researchers at UC Irvine have made a critical breakthrough by identifying drugs that can bind directly to a unique part of NLRP3 called the pyrin domain [132]. This approach differs from previous strategies by targeting an earlier stage in the inflammatory cascade and avoiding domains associated with off-target effects. The methodology involves designing molecules that resemble damaged pieces of DNA—specifically oxidized guanine—to block NLRP3 at the pyrin domain, preventing the initiation of the inflammatory chain reaction [132].
NLRP3 Inflammasome Inhibition Pathway
The UC Irvine team is currently using cryo-electron microscopy to visualize exactly how these drug molecules bind to the NLRP3 pyrin domain, representing a crucial step in optimizing compound efficacy and specificity before advancing to clinical trials [132]. This structural biology approach enables rational drug design rather than reliance on phenotypic screening.
Multi-Targeted Approaches and Platform Trials
Recognition of the complex, multifactorial nature of neurodegenerative diseases has spurred development of therapeutic candidates with novel mechanisms that simultaneously target multiple pathways. The investigational drug CT1812 represents one such approach, with NIH-funded research demonstrating its ability to prevent neurotoxicity by displacing toxic protein aggregates at synapses [133]. Significantly, the molecule can displace two different types of protein aggregates—beta-amyloid and alpha-synuclein—each known to contribute to multiple types of dementia and to trigger neuroinflammatory responses [133].
Methodologically, researchers are addressing disease complexity through innovative trial designs such as the PSP Platform Trial for progressive supranuclear palsy, a rare tauopathy [133]. This platform trial improves research efficiency by testing multiple different treatments under a single protocol, allowing for shared control groups and infrastructure. The trial will test at least three different therapies for PSP, with researchers committed to sharing data widely with the research community to further accelerate clinical development [133]. This approach is particularly valuable for evaluating therapies targeting inflammatory pathways in rare neurodegenerative conditions where patient populations are limited.
Emerging Research Tools and Methodologies
Advanced research technologies and collaborative frameworks are transforming our ability to identify and validate inflammatory targets in neurodegenerative diseases.
Large-Scale Proteomics for Biomarker and Target Discovery
The Global Neurodegeneration Proteomics Consortium (GNPC) has established one of the world's largest harmonized proteomic datasets, representing a transformative resource for inflammatory target discovery [59]. The consortium includes approximately 250 million unique protein measurements from multiple platforms across more than 35,000 biofluid samples (plasma, serum, and cerebrospinal fluid) contributed by 23 partners [59].
The GNPC methodology involves:
- Standardized Sample Processing: Consistent protocols across collection sites to minimize technical variability
- Multi-Platform Proteomic Profiling: Utilization of SomaScan, Olink, and mass spectrometry platforms to capture a sizable portion of the circulating proteome
- Data Harmonization: Computational integration of datasets across platforms and cohorts to enable combined analysis
- Cross-Disease Comparison: Simultaneous analysis of Alzheimer's disease, Parkinson's disease, frontotemporal dementia, and ALS to identify shared and distinct inflammatory signatures
This approach has already yielded significant insights, including the identification of a robust plasma proteomic signature of APOE ε4 carriership that is reproducible across multiple neurodegenerative conditions, as well as distinct patterns of organ aging across these diseases [59]. The dataset will be available to the wider research community via the Alzheimer's Disease Data Initiative's AD Workbench, representing a powerful resource for investigating neuroinflammatory pathways [59].
Table 3: Essential Research Reagent Solutions for Neuroinflammation Studies
| Research Tool Category | Specific Examples | Research Applications | Technical Considerations |
|---|---|---|---|
| Proteomic Profiling Platforms | SomaScan, Olink, Mass Spectrometry [59] | Biomarker discovery, target validation, pathway analysis | Platform selection affects proteome coverage, sensitivity, and dynamic range |
| Structural Biology Tools | Cryo-electron microscopy [132] | Target-ligand interaction mapping, rational drug design | Requires specialized expertise and infrastructure |
| Animal Models | Transgenic models expressing human mutant proteins [133] | In vivo efficacy and safety testing | Limited recapitulation of human disease pathology and inflammatory responses |
| Biomaterial Resources | Plasma, serum, cerebrospinal fluid banks [59] | Biomarker verification, disease monitoring | Standardized collection and storage protocols critical for data quality |
Advanced Clinical Trial Methodologies
Future success in targeting neuroinflammation will require implementation of more sophisticated clinical trial designs and analytical approaches:
- Adaptive Trial Designs: Protocols that allow modification based on interim data without compromising trial integrity
- Bayesian Statistical Methods: Approaches that incorporate prior knowledge and continuously update probability estimates as data accumulates [131]
- Composite Endpoints: Carefully constructed endpoints that capture multidimensional treatment effects relevant to inflammatory pathways
- Precision Enrollment Strategies: Patient selection based on inflammatory biomarker profiles rather than clinical symptoms alone
These methodologies address key limitations of conventional trial designs, particularly their inability to account for the heterogeneity of neuroinflammatory responses across patient populations and disease stages.
The repeated failure of promising neuroinflammatory targets in late-stage clinical development represents both a significant challenge and a learning opportunity for the field. The lessons from these failures point to several critical priorities for future research:
First, the disconnect between biomarker effects and clinical outcomes in trials such as semaglutide for Alzheimer's disease highlights the need for better understanding of the causal relationship between specific inflammatory pathways and clinical manifestations of neurodegeneration. Simply demonstrating target engagement or modification of inflammatory markers is insufficient without establishing a direct link to clinically meaningful benefits.
Second, the "regression to the truth" phenomenon underscores the importance of adequate Phase II trial sizing and design before advancing to pivotal studies. Investment in larger, more rigorously controlled Phase II trials may prevent costly Phase III failures and more accurately identify genuinely effective therapies.
Third, novel target discovery approaches, including large-scale proteomics and structural biology, are revealing previously unappreciated inflammatory pathways such as the NLRP3 pyrin domain that may offer more specific intervention points with better therapeutic windows.
Finally, innovative trial designs including platform trials and adaptive methodologies present opportunities to more efficiently evaluate multiple therapeutic approaches while accounting for the substantial heterogeneity in neuroinflammatory responses across patient populations.
As the field continues to evolve, successful targeting of neuroinflammation in neurodegenerative diseases will require integration of robust basic science exploring inflammatory mechanisms, sophisticated biomarker development to identify responsive patient populations, and innovative clinical trial methodologies that can efficiently demonstrate clinical benefits. While the challenges are substantial, the growing understanding of inflammatory pathways and their role in neurodegeneration continues to offer promising avenues for developing effective treatments for these devastating conditions.
Conclusion
The evidence unequivocally establishes neuroinflammation as a fundamental driver of neurodegenerative pathogenesis, not merely a secondary consequence. Successful therapeutic intervention requires moving beyond broad immunosuppression toward precisely targeted modulation that preserves protective immune functions while inhibiting chronic damaging inflammation. Future research must prioritize developing sensitive inflammatory biomarkers for early detection, personalizing immunomodulatory approaches based on individual inflammatory profiles, and exploring combination therapies that simultaneously target multiple aspects of the neuroinflammatory cascade. The convergence of resolution pharmacology, targeted biologic therapies, and multi-omics profiling represents the most promising path toward effective disease-modifying treatments for neurodegenerative disorders.
References
- 1. A mechanistic insight of neuro-inflammation signaling ... [https://pubmed.ncbi.nlm.nih.gov/41266692/]
- 2. Neuroinflammation a Key Underlying Factor in Alzheimer's ... [https://www.fiercebiotech.com/sponsored/neuroinflammation-key-underlying-factor-alzheimers-disease-risk]
- 3. Evolving Neurology And Neuroinflammation Therapies ... [https://www.clinicalleader.com/doc/evolving-neurology-and-neuroinflammation-therapies-and-trials-in-0001]
- 4. Experimental Models of Neuroimmunological Disorders [https://pmc.ncbi.nlm.nih.gov/articles/PMC7235321/]
- 5. The use of animal models of neuroinflammation for ... [https://www.sciencedirect.com/science/article/abs/pii/B9780323917711000113]
- 6. A Practical Guide for Generating Reproducible and ... [https://apertureneuro.org/article/85104-a-practical-guide-for-generating-reproducible-and-programmatic-neuroimaging-visualizations]
- 7. Alzheimer's disease drug development pipeline: 2025 - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12131090/]
- 8. Microglia in neurodegenerative diseases: mechanism and ... [https://www.nature.com/articles/s41392-023-01588-0]
- 9. Neuroimmune crosstalk in chronic neuroinflammation [https://www.frontiersin.org/journals/cellular-neuroscience/articles/10.3389/fncel.2025.1575022/abstract]
- 10. Functional roles of reactive astrocytes in ... - Nature [https://www.nature.com/articles/s41582-023-00822-1]
- 11. The Modulation of Neuroimmune Responses in Peripheral ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12258403/]
- 12. Roles of Microglia in Neurodegenerative Diseases - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10867232/]
- 13. New insight on microglia activation in neurodegenerative ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2023.1308345/full]
- 14. The roles of microglia and astrocytes in neuroinflammation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12092354/]
- 15. Review Dual role of microglia in neuroinflammation and ... [https://www.sciencedirect.com/science/article/pii/S096999612500350X]
- 16. The Role of Astrocytes in CNS Inflammation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8284746/]
- 17. A body–brain circuit that regulates body inflammatory ... [https://www.nature.com/articles/s41586-024-07469-y]
- 18. NLRP3: Role in ischemia/reperfusion injuries - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC9552576/]
- 19. NLRP3 inflammasome in neurodegenerative disease - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10614656/]
- 20. Neurodegenerative Disease and the NLRP3 Inflammasome [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2021.643254/full]
- 21. The IL-17 family in diseases: from bench to bedside [https://www.nature.com/articles/s41392-023-01620-3]
- 22. Basic biology and role of interleukin-17 in immunity and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4530463/]
- 23. Emerging role of 12/15-Lipoxygenase (ALOX15) in human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6338518/]
- 24. Regulation and Functions of 15-Lipoxygenases in Human ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2019.00719/full]
- 25. NLRP3 Inflammasome and Neurodegenerative Diseases [https://biospective.com/resources/nlrp3-inflammasome-neurodegenerative-diseases]
- 26. Recent advances in Alzheimer's disease: mechanisms ... [https://www.nature.com/articles/s41392-024-01911-3]
- 27. Tau and neuroinflammation in Alzheimer's disease [https://jneuroinflammation.biomedcentral.com/articles/10.1186/s12974-023-02853-3]
- 28. Recent Research Trends in Neuroinflammatory and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10969521/]
- 29. Bifurcations in coupled amyloid-β aggregation- ... [https://www.nature.com/articles/s41540-024-00408-7]
- 30. Proteomics Approaches for Biomarker and Drug Target ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6579929/]
- 31. Design and application of a Tau seed amplification assay for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12482674/]
- 32. Amyloid beta acts synergistically as a pro-inflammatory cytokine [https://pmc.ncbi.nlm.nih.gov/articles/PMC8502211/]
- 33. Experimental Models and Their Applicability in Inflammation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12250041/]
- 34. Oxidative stress and inflammation in the pathogenesis of neurological disorders: Mechanisms and implications - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11873663/]
- 35. Mitochondrial Dysfunction, Oxidative Stress, and Neuroinflammation: Intertwined Roads to Neurodegeneration - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7466131/]
- 36. Oxidative Stress and Mitochondrial Dysfunction in Alzheimer’s Disease: Insights into Pathophysiology and Treatment [https://www.mdpi.com/3042-4518/2/2/17]
- 37. Mitochondrial Dysfunction in Neurodegenerative Diseases [https://pubmed.ncbi.nlm.nih.gov/39996748/]
- 38. Mitochondria in oxidative stress, inflammation and aging [https://pmc.ncbi.nlm.nih.gov/articles/PMC12159213/]
- 39. Mitochondrial dysfunction in neurodegenerative disorders [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-023-04493-w]
- 40. Detecting Oxidative Stress Biomarkers in ... [https://www.mdpi.com/2409-9279/3/4/66]
- 41. Oxidative Stress in Neurodegenerative Diseases [https://pmc.ncbi.nlm.nih.gov/articles/PMC3236428/]
- 42. Association Between Peripheral Inflammation Biomarkers and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12638438/]
- 43. Neutrophil-to-Lymphocyte Ratio in the Alzheimer's Disease ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12154037/]
- 44. The clinical value of the neutrophil-to-lymphocyte ratio ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2025.1498007/full]
- 45. Association of red blood cell count, hemoglobin ... [https://www.nature.com/articles/s41598-025-02468-z]
- 46. Brain to Blood: Biomarkers Transforming Alzheimer's ... [https://alamarbio.com/brain-blood-biomarkers-neurodegeneration/]
- 47. Biomarker discovery in Alzheimer's and neurodegenerative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12096316/]
- 48. The Critical Role of Biomarkers for Drug Development ... [https://www.sciencedirect.com/science/article/pii/S2274580724001614]
- 49. Biomarkers and therapeutic strategies targeting microglia in ... [https://molecularneurodegeneration.biomedcentral.com/articles/10.1186/s13024-025-00867-4]
- 50. Role of neuroinflammation in neurodegeneration ... [https://www.nature.com/articles/s41392-023-01486-5]
- 51. Genomic and Transcriptomic Approaches Advance the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11855287/]
- 52. Analysis and interpretation of inflammatory fluid markers in ... [https://jneuroinflammation.biomedcentral.com/articles/10.1186/s12974-025-03432-4]
- 53. Single-cell transcriptomics reveals predominantly ... [https://pubmed.ncbi.nlm.nih.gov/40969743/]
- 54. Single-cell RNA sequencing reveals the pro-inflammatory ... [https://www.nature.com/articles/s41467-024-53104-9]
- 55. Cross study transcriptomic investigation of Alzheimer's ... [https://www.nature.com/articles/s41598-025-01017-y]
- 56. Single-cell transcriptomics reveals predominantly ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1629226/full]
- 57. The benefits and pitfalls of machine learning for biomarker ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10558383/]
- 58. Different inflammatory signatures based on CSF biomarkers ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11176056/]
- 59. The Global Neurodegeneration Proteomics Consortium [https://www.nature.com/articles/s41591-025-03834-0]
- 60. Imaging markers of neuroinflammation in aging and ... [https://www.sciencedirect.com/science/article/abs/pii/S0149763425002714]
- 61. Imaging brain inflammation and blood brain barrier ... - PubMed [https://pubmed.ncbi.nlm.nih.gov/41257741/]
- 62. Current perspectives on Alzheimer's disease fluid biomarkers ... [https://jlpm.amegroups.org/article/view/9119/html]
- 63. Fluid-based biomarkers for neurodegenerative diseases [https://pubmed.ncbi.nlm.nih.gov/40122396/]
- 64. LPS-Induced Neuroinflammation Disrupts Brain-Derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12602814/]
- 65. Three-Dimensional Cell Cultures in Drug Discovery and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5448717/]
- 66. A Quick Comparison of Experimental Results [https://www.chemedx.org/blog/quick-comparison-experimental-results]
- 67. Integrative multiâ€omics approaches identify molecular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12614089/]
- 68. Decoding neuroinflammation in Alzheimer's disease [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1616899/full]
- 69. Visual analysis of multi-omics data [https://pubmed.ncbi.nlm.nih.gov/39318761/]
- 70. Multi-omics integration reveals key miRNAs, immune ... [https://www.sciencedirect.com/science/article/pii/S0141813025084314]
- 71. Tutorial: Multi-omics data visualization with PathVisio [https://pathvisio.org/tutorials/multi-omics-tutorial.html]
- 72. A systematic mapping study of semantic technologies in ... [https://www.sciencedirect.com/science/article/pii/S1532046425000383]
- 73. The blood–brain barrier: Structure, regulation and drug ... [https://www.nature.com/articles/s41392-023-01481-w]
- 74. Strategies for delivering drugs across the blood-brain ... [https://www.frontiersin.org/journals/drug-delivery/articles/10.3389/fddev.2025.1644633/full]
- 75. Neurotherapeutics across blood–brain barrier: screening of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12511116/]
- 76. Neuroinflammation Treatment via Targeted Delivery of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7555434/]
- 77. Experimental Models to Study the Functions of the Blood ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10215847/]
- 78. The Blood Brain Barrier in Neurodegenerative Disease [https://pmc.ncbi.nlm.nih.gov/articles/PMC2761151/]
- 79. Blood-brain barrier permeability revisited: Predicting ... [https://www.sciencedirect.com/science/article/pii/S0928098725003513]
- 80. Engineered human blood–brain barrier microfluidic model ... [https://www.nature.com/articles/s41596-021-00635-w]
- 81. Quantitative Imaging of Blood-Brain Barrier Permeability ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8515019/]
- 82. “Rewiring brain immunity: targeting microglial metabolism for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12647335/]
- 83. Neuroimmune crosstalk in chronic neuroinflammation [https://www.frontiersin.org/journals/cellular-neuroscience/articles/10.3389/fncel.2025.1575022/full]
- 84. Natural Products, Drug Repurposing, and Biomolecular Targets [https://pmc.ncbi.nlm.nih.gov/articles/PMC12467000/]
- 85. Repurposing the hypoglycaemic agents for neuroinflammation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12325842/]
- 86. Drug repurposing for Alzheimer's disease and other ... [https://www.nature.com/articles/s41467-025-56690-4]
- 87. Potential role of NSAIDs loaded nano-formulations to treat ... [https://pubmed.ncbi.nlm.nih.gov/39953360/]
- 88. Anti-inflammatory drug repurposing in skin diseases [https://www.sciencedirect.com/science/article/pii/S0014299925007460]
- 89. A Critical Appraisal of Off-Label Use and Repurposing of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12347899/]
- 90. Molecular and Immunomodulatory Mechanisms of Statins ... [https://www.mdpi.com/1422-0067/26/17/8429]
- 91. Impact of statins as immune-modulatory agents on ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0323749]
- 92. The Dual Role of Metformin: Repurposing an Antidiabetic ... [https://www.mdpi.com/2076-3417/15/21/11576]
- 93. Repurposing metabolic drugs as anti-inflammatory agents [https://www.sciencedirect.com/science/article/pii/S1043276025001493]
- 94. Resolution Pharmacology: state-of-the-art and therapeutic ... [https://www.sciencedirect.com/science/article/pii/S0031699725075052]
- 95. Innovative therapeutic approaches based on the biology of ... [https://www.frontiersin.org/research-topics/7350/resolution-pharmacology--innovative-therapeutic-approaches-based-on-the-biology-of-resolution-to-control-chronic-diseases-of-western-societies/magazine]
- 96. Resolution of Inflammation in Neurodegenerative Diseases [https://pmc.ncbi.nlm.nih.gov/articles/PMC7132591/]
- 97. Beyond amyloid: nanobody-mediated neuroinflammatory ... [https://translationalneurodegeneration.biomedcentral.com/articles/10.1186/s40035-025-00513-5]
- 98. Effect of neuroinflammation on the progression ... [https://www.sciencedirect.com/science/article/pii/S2667242125000715]
- 99. Cytokines and immune biomarkers in neurodegeneration and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12290485/]
- 100. A 2025 update on treatment strategies for the Alzheimer's ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12637128/]
- 101. AI-guided patient stratification improves outcomes and ... [https://www.nature.com/articles/s41467-025-61355-3]
- 102. Advancing Neurodegenerative Disease Research with ... [https://www.quanterix.com/blog-advancing-neurodegenerative-disease-research-with-simoa-technology-at-ad-pd-2025/]
- 103. Neuronata-R® Phase 3 Results Confirm Subgroup Benefit ... [https://www.biospace.com/press-releases/neuronata-r-phase-3-results-confirm-subgroup-benefit-at-pactals-2025-strengthening-biomarker-driven-pathway]
- 104. Neurodegenerative diseases - Improving clinical trial ... [https://neurotorium.org/next-steps-for-improving-clinical-trial-outcomes-neurodegenerative-disease/]
- 105. Comparison of inflammatory biomarker levels in ... [https://pubmed.ncbi.nlm.nih.gov/40029428/]
- 106. Comparison of inflammatory biomarker levels in ... [https://www.springermedicine.com/biomarkers/idiopathic-parkinson-disease/comparison-of-inflammatory-biomarker-levels-in-neurodegenerative/50704460]
- 107. Neuroinflammatory fluid biomarkers in patients with ... [https://www.nature.com/articles/s41380-025-02939-9]
- 108. Inflammation-related biomarkers in major psychiatric disorders [https://pmc.ncbi.nlm.nih.gov/articles/PMC6751188/]
- 109. Systemic Inflammatory Biomarkers in DSM-5–Defined ... [https://www.sciencedirect.com/science/article/pii/S2667174322000118]
- 110. Identification and validation of the inflammatory response ... [https://www.nature.com/articles/s41598-025-98101-0]
- 111. Identification of biomarkers associated with inflammatory ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0320257]
- 112. The Role of IL-17A in Mediating Inflammatory Responses and ... [https://pmc.ncbi.nlm.nih.gov/articles/pmid/40141149/]
- 113. The critical role of Th17 cells and IL-17A in autoimmune ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1656422/full]
- 114. The role of Th17 cells/IL-17A in AD, PD, ALS and the strategic ... [https://jneuroinflammation.biomedcentral.com/articles/10.1186/s12974-022-02446-6]
- 115. IL-17A is a key regulator of neuroinflammation and ... [https://www.sciencedirect.com/science/article/abs/pii/S0891584924010736]
- 116. IL-17A blockade alleviates immune checkpoint inhibitor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12624807/]
- 117. Exploring the therapeutic potential of IL-17A inhibition in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12606481/]
- 118. Sonelokimab, an IL-17A/IL-17F-inhibiting nanobody for ... [https://www.nature.com/articles/s41591-025-03971-6]
- 119. Inhibition of 12/15-LOX hyperactivation mitigates cognitive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12372482/]
- 120. The potential of 12/15-lipoxygenase inhibitors in stroke ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4280907/]
- 121. 12/15-lipoxygenase inhibition attenuates ... [https://www.frontiersin.org/journals/cellular-neuroscience/articles/10.3389/fncel.2023.1277268/full]
- 122. 12/15-Lipooxygenase Inhibition Reduces Microvessel ... [https://link.springer.com/article/10.1007/s12975-024-01295-0]
- 123. The Role of Inflammation in Neurodegenerative Diseases [https://pmc.ncbi.nlm.nih.gov/articles/PMC12154089/]
- 124. Pathogenesis and therapeutic applications of microglia ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1508023/full]
- 125. Potential targets of microglia in the treatment of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12407519/]
- 126. The E3 ligase c-Cbl modulates microglial phenotypes and ... [https://www.nature.com/articles/s41420-025-02482-0]
- 127. Exploring microglial replacement: From disease models to ... [https://www.sciencedirect.com/science/article/pii/S0889159125002223]
- 128. In vitro models of microglia: a comparative study [https://www.nature.com/articles/s41598-025-99867-z]
- 129. Novo's GLP-1 Fails to Slow Alzheimer's, Sending Shares ... [https://www.biospace.com/drug-development/novos-glp-1-fails-to-slow-alzheimers-sending-shares-down-10]
- 130. Novo Nordisk's GLP-1 misses goal in closely watched ... [https://www.biopharmadive.com/news/novo-glp1-alzheimers-trials-evoke/806256/]
- 131. “Regression to the truthâ€: lessons learned from negative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12004256/]
- 132. UC Irvine Researchers Explore Promising New Pathway for ... [https://www.bio.uci.edu/uc-irvine-researchers-explore-promising-new-pathway-for-treating-inflammatory-diseases/]
- 133. 2025 NIH Alzheimer's Disease and Related Dementias ... [https://www.nia.nih.gov/about/2025-nih-dementia-research-progress-report]