Neutrophil Apoptosis Assays: A Comprehensive Guide for Assessing Inflammation Resolution in Research and Drug Development
This article provides a comprehensive guide for researchers and drug development professionals on the critical role of neutrophil apoptosis assays in evaluating inflammation resolution.
Neutrophil Apoptosis Assays: A Comprehensive Guide for Assessing Inflammation Resolution in Research and Drug Development
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on the critical role of neutrophil apoptosis assays in evaluating inflammation resolution. It explores the foundational biology connecting apoptotic death to inflammatory termination, details established and cutting-edge methodological approaches from flow cytometry to in vivo imaging, and addresses key troubleshooting considerations for data accuracy. Furthermore, it covers validation strategies across model systems and comparative analysis of assay outputs, synthesizing current knowledge to empower robust experimental design and highlight the translational potential of modulating neutrophil apoptosis as a therapeutic strategy for inflammatory diseases.
The Critical Link Between Neutrophil Apoptosis and Inflammation Resolution
Core Concepts and Key Molecular Regulators
Neutrophil apoptosis is a programmed cell death process that is essential for the timely resolution of inflammation. It ensures the safe removal of emigrated neutrophils from inflammatory sites, thereby limiting their capacity to cause collateral tissue damage and promoting the return to tissue homeostasis [1] [2]. The precise control of this death program provides a critical balance between effective host defense and the secure clearance of these potent effector cells.
The following table summarizes the key molecular regulators of neutrophil apoptosis discussed in this document.
Table 1: Key Molecular Regulators of Neutrophil Apoptosis
| Molecule/Pathway | Role in Neutrophil Apoptosis | Experimental/Therapeutic Relevance |
|---|---|---|
| Mcl-1 | Central anti-apoptotic regulator; short protein half-life closely correlates with survival kinetics [1]. | Key downstream target of survival and pro-apoptosis cues; determinant of neutrophil lifespan [1] [2]. |
| β2 Integrin Mac-1 (CD11b/CD18) | Bidirectional allosteric signaling receptor; generates contrasting survival or pro-apoptotic signals [1] [2]. | Ligation with ICAM-1, fibrinogen, or myeloperoxidase suppresses apoptosis. Phagocytosis of bacteria through Mac-1 induces apoptosis [1]. |
| ALX/FPR2 Receptor | G-protein-coupled receptor binding diverse ligands; signaling bias dictates pro-inflammatory or pro-resolving outcomes [2]. | Ligation with pro-resolving mediators (e.g., Lipoxin A4, Annexin A1) promotes neutrophil apoptosis and efferocytosis [2]. |
| Specialized Pro-Resolving Mediators (SPMs) | Endogenous lipid mediators (e.g., Lipoxins, Resolvins) that actively promote inflammation resolution [3]. | SPMs induce neutrophil apoptosis, inhibit neutrophil infiltration and degranulation, and promote macrophage efferocytosis [3]. |
| Caspase-8 | Executioner protease; phagocytosis-induced ROS generation activates caspase-8, overriding survival signals [2]. | Forms a complex with FLIP, which inhibits RIPK3-dependent necrosis and prevents degranulation [2]. |
Experimental Protocols for Neutrophil Apoptosis Research
Protocol: In Vitro Assessment of Neutrophil Apoptosis via Flow Cytometry
This protocol details a standard method for quantifying the rate of spontaneous and compound-induced neutrophil apoptosis in vitro using Annexin V/7-AAD staining and flow cytometric analysis, as applied in multiple studies [4] [5].
Key Research Reagent Solutions:
- Annexin V Binding Buffer: 10 mM HEPES, 140 mM NaCl, 2.5 mM CaClâ‚‚, pH 7.4.
- Fluorochrome-conjugated Annexin V: To label phosphatidylserine exposed on the outer leaflet of the apoptotic cell membrane.
- 7-Aminoactinomycin D (7-AAD) or Propidium Iodide (PI): Vital dyes to exclude late apoptotic/necrotic cells with compromised membrane integrity.
Methodology:
- Neutrophil Isolation: Isolate human neutrophils from peripheral blood of healthy donors using density gradient centrifugation (e.g., Percoll or Ficoll-Hypaque).
- Compound Treatment: Culture purified neutrophils (e.g., 1x10^6 cells/mL) in appropriate media and treat with the compound of interest (e.g., pro-resolving mediators, kinase inhibitors like roscovitine) or vehicle control. Incubate at 37°C, 5% CO₂ for a defined period (e.g., 6-20 hours).
- Cell Staining: a. Harvest cells by gentle centrifugation. b. Wash once with cold PBS. c. Resuspend cell pellet in 100 µL of Annexin V Binding Buffer. d. Add recommended volumes of fluorochrome-conjugated Annexin V and 7-AAD. e. Incubate for 15 minutes at room temperature in the dark. f. Add 400 µL of Annexin V Binding Buffer to each tube and mix gently.
- Flow Cytometric Analysis: Analyze samples using a flow cytometer within 1 hour. A minimum of 10,000 events per sample should be acquired. Apoptotic cells are identified as Annexin V-positive, 7-AAD-negative.
Protocol: Evaluating the Functional Impact of Apoptotic Neutrophils on Macrophage Efferocytosis
This protocol assesses a key functional consequence of neutrophil apoptosis: their clearance by macrophages (efferocytosis) and the subsequent induction of a pro-resolving macrophage phenotype [6] [7].
Key Research Reagent Solutions:
- Macrophage Culture Medium: RPMI 1640 or DMEM supplemented with 10% FBS and 1% Penicillin-Streptomycin.
- Fluorescent Cell Labeler: e.g., CFSE (5(6)-Carboxyfluorescein diacetate N-succinimidyl ester) or PKH67, to label neutrophil membranes.
- Differentiation Cytokines: M-CSF or GM-CSF to generate macrophages from human monocyte precursors.
Methodology:
- Generation of Macrophages: Differentiate human monocytes into macrophages by culturing in medium containing 50 ng/mL M-CSF for 5-7 days.
- Induction and Labeling of Apoptotic Neutrophils: a. Induce apoptosis in isolated neutrophils by culture overnight (spontaneous) or via treatment with a pro-apoptotic agent (e.g., UV irradiation). b. Confirm apoptosis rate (≥40-50%) via Annexin V/7-AAD staining. c. Label the neutrophil population with a fluorescent dye (e.g., 5 µM CFSE) for 15 minutes at 37°C. Quench the reaction with FBS and wash cells thoroughly.
- Co-culture and Efferocytosis: a. Seed macrophages in culture plates and allow to adhere. b. Add CFSE-labeled apoptotic neutrophils to macrophages at a defined ratio (e.g., 5:1 neutrophils to macrophages). c. Co-culture for 1-2 hours at 37°C. d. Remove non-phagocytosed neutrophils by vigorous washing with PBS.
- Analysis: a. Flow Cytometry: Detach macrophages and analyze the percentage of CFSE-positive macrophages to quantify efferocytosis. b. Microscopy: Fix cells and counterstain macrophage nuclei (e.g., DAPI). Count the number of ingested fluorescent neutrophils per macrophage under a fluorescence microscope. c. Macrophage Phenotyping: Post-efferocytosis, analyze macrophage culture supernatants for TGF-β and IL-10 (pro-resolving) vs. TNF-α and IL-6 (pro-inflammatory) cytokines by ELISA [7].
Advanced Experimental Models and Quantitative Data
Nanoparticle-Mediated Spatiotemporal Control of Neutrophil Apoptosis
Recent advances focus on inducing neutrophil apoptosis specifically at the site of injury. One approach utilizes poly(lactic-co-glycolic acid) (PLGA) nanoparticles loaded with roscovitine and catalase (RC NPs), which are internalized by circulating neutrophils [5].
Mechanism of Action: Upon migration to the infarcted heart, neutrophils are activated and generate high levels of reactive oxygen species (ROS), including Hâ‚‚Oâ‚‚. Intracellular catalase in the RC NPs converts Hâ‚‚Oâ‚‚ to oxygen, causing nanoparticle "detonation" and rapid release of roscovitine, thereby inducing apoptosis specifically in the activated neutrophil population at the injury site [5].
Table 2: Quantitative Profile of Roscovitine/Catalase-Loaded PLGA Nanoparticles (RC NPs)
| Parameter | Value/Measurement | Experimental Context |
|---|---|---|
| Hydrodynamic Diameter | 429.7 ± 72.8 nm | Optimized for neutrophil uptake [5] |
| Zeta Potential | -25.5 ± 4.9 mV | Optimized for neutrophil uptake [5] |
| Neutrophil Uptake | >90% of neutrophils | After 1 hour of incubation in vitro [5] |
| Roscovitine Release | >30% within 12-24 h | Faster release under H₂O₂ conditions (100-200 µM) [5] |
| Viability of NP-treated Neutrophils | >90% | 6 hours after treatment with RC NPs (20 µM roscovitine) in vitro [5] |
| Viability with Free Roscovitine | Significantly lower | 6 hours after treatment with free drug (20 µM) in vitro [5] |
Spatiotemporal Control of Neutrophil Apoptosis via RC NPs
Key Signaling Pathways Regulating Neutrophil Apoptosis
The fate of neutrophils is determined by the integration of signals from the inflammatory microenvironment through specific receptors and intracellular pathways [1] [2].
Key Regulatory Pathways in Neutrophil Apoptosis
Neutrophil apoptosis is a critical control point for the resolution of inflammation, and its dysregulation is a feature of many inflammatory diseases. The dynamic interplay between the anti-apoptotic protein Mcl-1 (Myeloid cell leukemia-1) and caspase activation forms a central regulatory axis determining neutrophil lifespan. This application note details experimental protocols for investigating these key molecular regulators, providing researchers with robust methods to advance inflammation resolution research and therapeutic development. Quantitative data and standardized methodologies presented herein enable precise interrogation of neutrophil apoptotic pathways for drug discovery applications.
Neutrophils are the most abundant leukocytes in circulation and form the first line of defense against invading pathogens. Under basal conditions, neutrophils undergo constitutive apoptosis within hours, but at inflammatory sites, their lifespan is extended by various survival signals [8] [1]. The timely apoptosis of neutrophils and their subsequent clearance by macrophages is essential for the resolution of inflammation without tissue damage [8] [2]. Failure of these processes leads to persistent tissue damage in conditions including acute respiratory distress syndrome (ARDS), sepsis, rheumatoid arthritis, and cystic fibrosis [1] [9].
The intrinsic apoptosis pathway in neutrophils is predominantly controlled by members of the Bcl-2 family, with Mcl-1 serving as the primary pro-survival regulator [1] [9]. Mcl-1 has an extremely short half-life (1-5 hours), making it ideally suited for dynamic control of neutrophil survival in response to rapidly changing inflammatory cues [9]. Downstream of mitochondrial commitment to apoptosis, caspase activation executes the final stages of cell death, though the relationship between Mcl-1 degradation and caspase activation in neutrophils has been historically complex [10].
Key Molecular Regulators
Mcl-1: The Master Regulator of Neutrophil Survival
Mcl-1 is a Bcl-2 homology (BH) domain-containing anti-apoptotic protein that is instrumental in controlling neutrophil survival. Unlike other anti-apoptotic Bcl-2 family members, Mcl-1 contains PEST domains (rich in proline, glutamic acid, serine, and threonine) that target it for rapid proteasomal degradation [1] [9]. Mcl-1 levels closely correlate with neutrophil survival kinetics, and its degradation is a critical early event in the apoptotic cascade [1] [10].
Caspases: Executioners of Neutrophil Apoptosis
Caspases are cysteine-aspartic proteases that serve as both initiators and executioners of apoptosis. In neutrophils, caspase activation leads to the characteristic morphological changes of apoptosis, including chromatin condensation, nuclear fragmentation, and presentation of "eat-me" signals such as phosphatidylserine [10] [11]. Effective caspase inhibition can almost completely abrogate neutrophil apoptosis, confirming the caspase dependence of this process [10].
Integrated Pathway Regulation
The relationship between Mcl-1 and caspases is bidirectional. While Mcl-1 degradation can initiate caspase activation, caspases can also cleave Mcl-1, creating a positive feedback loop that amplifies the apoptotic signal [10]. This regulatory network ensures rapid and irreversible commitment to cell death once the apoptotic threshold is reached.
Table 1: Quantitative Effects of Mcl-1 Manipulation on Neutrophil Apoptosis and Inflammation Resolution
| Experimental Condition | Effect on Neutrophil Apoptosis | Effect on Resolution Parameters | Key Molecular Changes |
|---|---|---|---|
| AT7519 (CDK inhibitor) | Concentration- and time-dependent induction; EC50: 61.1 nM at 6h [8] | Shortened resolution interval (Ri) from 19h to 7h in LPS model; Enhanced bacterial clearance [8] | Caspase-dependent Mcl-1 downregulation preceding caspase-3 activation [8] |
| Mcl-1 siRNA knockdown | Accelerated apoptosis in HL-60 neutrophil precursors [8] | Not measured | Caspase-independent Mcl-1 reduction; apoptosis blocked by Q-VD [8] |
| Q-VD.OPh (caspase inhibitor) | Profound inhibition of apoptosis; effective at concentrations as low as 100 nM [10] | Not measured | Early Mcl-1 decline still occurs; late Mcl-1 degradation is caspase-dependent [10] |
| zVAD.fmk (caspase inhibitor) | No significant inhibition below 100 μM [10] | Not measured | Ineffective at preventing Mcl-1 degradation [10] |
Table 2: Comparison of Caspase Inhibitors in Neutrophil Apoptosis Studies
| Inhibitor | Effective Concentration | Mechanism | Advantages | Limitations |
|---|---|---|---|---|
| Q-VD.OPh | 100 nM - 20 μM [10] | Irreversible pan-caspase inhibitor | High potency, low toxicity, highly cell permeable | Requires reconstitution in DMSO |
| zVAD.fmk | >100 μM required [10] | Irreversible pan-caspase inhibitor | Widely available, extensive literature | Low potency in neutrophils, potential toxicity at high concentrations |
Signaling Pathways
Experimental Protocols
Protocol 1: Assessing Mcl-1 Dynamics in Human Neutrophils
Purpose: To evaluate Mcl-1 protein expression changes during neutrophil apoptosis.
Materials:
- Highly purified human neutrophils (isolated via Percoll or OptiPrep gradient)
- RPMI 1640 culture medium with 10% FBS
- AT7519 (CDK inhibitor, stock solution in DMSO)
- Q-VD.OPh (caspase inhibitor, stock solution in DMSO)
- Lysis buffer (50 mM Tris, 50 mM NaF, 50 mM β-glycerophosphate, 10 mM Sodium Orthovanadate, 1% Triton-X100) with protease inhibitors
- SDS-PAGE and Western blot equipment
- Anti-Mcl-1 and anti-β-actin antibodies
- Enhanced chemiluminescence detection system
Procedure:
- Isolate human neutrophils from peripheral blood using a method that minimizes activation (see Protocol 3).
- Resuspend neutrophils at 5×10^6 cells/mL in complete RPMI 1640 medium.
- Treat cells with experimental compounds:
- AT7519 (0.1-10 μM) for Mcl-1 downregulation
- Q-VD.OPh (20 μM) to assess caspase-independent Mcl-1 changes
- Vehicle control (DMSO, equivalent concentration)
- Incubate at 37°C in 5% CO₂ for specified time points (0-20 hours).
- Collect cells by centrifugation at 300g for 2 minutes at 4°C.
- Lyse cell pellets in ice-cold lysis buffer for 30 minutes.
- Clarify lysates by centrifugation at 14,000g for 15 minutes at 4°C.
- Determine protein concentration and perform Western blot analysis with 30-50 μg protein per lane.
- Probe membranes with anti-Mcl-1 antibody (overnight at 4°C) followed by appropriate HRP-conjugated secondary antibody.
- Detect bands using enhanced chemiluminescence and quantify by densitometry normalized to β-actin.
Technical Notes:
- Mcl-1 has multiple isoforms; the predominant ~40 kDa band represents Mcl-1L (long form)
- Include both early (2-6h) and late (12-20h) time points to distinguish caspase-independent and dependent Mcl-1 degradation
- For phosphorylation studies, include phosphatase inhibitors in lysis buffer
Protocol 2: Quantifying Neutrophil Apoptosis via Annexin V/6-CFDA Staining
Purpose: To accurately distinguish viable, apoptotic, and necrotic neutrophil populations.
Materials:
- Purified human neutrophils
- Annexin V binding buffer (10 mM HEPES, 140 mM NaCl, 2.5 mM CaClâ‚‚, pH 7.5)
- Annexin V-Cy3 conjugate (APOAC kit, Sigma)
- 6-Carboxyfluorescein diacetate (6-CFDA)
- Parafilm-covered microscope slides
- Fluorescence microscope with fluorescein and rhodamine filter sets
Procedure (Improved Method):
- Suspend neutrophils at 1×10^6 cells/mL in culture medium.
- Treat with experimental compounds for desired time periods.
- Collect 1×10^6 cells by centrifugation at 200g for 5 minutes.
- Resuspend cell pellet in 100 μL of double staining solution (Annexin V-Cy3 and 6-CFDA in binding buffer).
- Incubate on ice for 15 minutes protected from light.
- Wash cells by adding 1 mL binding buffer and centrifuging at 200g for 5 minutes.
- Resuspend in 100 μL binding buffer and prepare wet mounts on Parafilm-covered slides.
- Visualize immediately using fluorescence microscopy:
- 6-CFDA (viable cells): fluorescein filter (excitation 450 nm, emission 490 nm)
- Annexin V-Cy3 (apoptotic cells): rhodamine filter (excitation 535 nm, emission 550 nm)
- Count at least 300 cells from randomly selected fields and classify as:
- Viable: Annexin V-Cy3â»/6-CFDAâº
- Apoptotic: Annexin V-Cy3âº/6-CFDAâº
- Necrotic: Annexin V-Cy3âº/6-CFDAâ»
Technical Notes:
- Staining cells in suspension minimizes activation artifacts from adhesion to charged surfaces
- Avoid fixation which can alter neutrophil morphology and staining
- Process samples immediately after staining for accurate quantification
- The percentage of apoptotic cells (Annexin V-Cy3âº/6-CFDAâº) provides the apoptotic index
Protocol 3: Optimal Neutrophil Isolation for Apoptosis Studies
Purpose: To isolate neutrophils with minimal activation for reliable apoptosis assays.
Materials:
- Fresh peripheral blood with appropriate anticoagulant (heparin or EDTA)
- HEPES-buffered RPMI 1640 medium
- One-step Fixation and RBC Lysis buffer
- CD15 and CD16 antibodies for neutrophil identification
- Flow cytometry equipment
Procedure (Whole Blood Pre-wash Fix/Lyse Method):
- Collect venous blood into heparin or EDTA tubes.
- Stain 100 μL whole blood with fluorescent antibodies (CD15, CD16) in pre-chilled tubes for 30 minutes at 4°C.
- Remove unbound antibodies by adding 2 mL cold PBS and centrifuging at 300g for 5 minutes at 4°C.
- Carefully aspirate supernatant and resuspend in One-step Fixation and RBC Lysis buffer.
- Incubate for 15 minutes at room temperature protected from light.
- Wash cells with PBS and resuspend in flow cytometry buffer.
- Analyze by flow cytometry, gating on CD15âºCD16⺠cells for neutrophil-specific analysis.
Technical Notes:
- Process samples within 3 hours of blood collection
- Maintain samples at 4°C throughout processing to minimize activation
- Remove unbound antibodies before fixation to reduce nonspecific binding
- This method minimizes neutrophil activation and degranulation compared to density gradient separation
Experimental Workflow
The Scientist's Toolkit
Table 3: Essential Research Reagents for Neutrophil Apoptosis Studies
| Reagent/Category | Specific Examples | Function/Application | Key Considerations |
|---|---|---|---|
| Mcl-1 Modulators | AT7519, R-roscovitine, Wogonin | Induce Mcl-1 downregulation and accelerate neutrophil apoptosis | AT7519 is ~100x more potent than R-roscovitine; use nM concentrations [8] |
| Caspase Inhibitors | Q-VD.OPh, zVAD.fmk | Define caspase dependence of apoptotic pathways | Q-VD.OPh significantly more effective in neutrophils (100 nM vs. >100 μM for zVAD) [10] |
| Apoptosis Detection | Annexin V-Cy3, 6-CFDA | Distinguish viable, apoptotic, and necrotic cells | Perform staining in suspension on Parafilm slides to avoid activation artifacts [11] |
| Neutrophil Isolation | One-step Fixation/RBC Lysis buffer, OptiPrep gradient | Obtain neutrophils with minimal activation | Methods with fewer manipulation steps reduce activation; avoid density gradients when possible [12] |
| Antibodies | Anti-Mcl-1, anti-cleaved caspase-3, CD16, CD15 | Molecular analysis and neutrophil identification | Remove unbound antibodies before fixation to reduce nonspecific binding [12] |
| Cell Culture | RPMI 1640 with 10% FBS, HEPES buffer | Maintain neutrophils during experiments | Include survival factors (GM-CSF) if studying delayed apoptosis; omit for constitutive apoptosis |
| Naproxen Sodium | Naproxen Sodium Salt | Bench Chemicals | |
| Micronomicin | Micronomicin, CAS:52093-21-7, MF:C20H41N5O7, MW:463.6 g/mol | Chemical Reagent | Bench Chemicals |
Data Interpretation Guidelines
- Mcl-1 Western Blots: Early Mcl-1 degradation (2-6 hours) that occurs despite caspase inhibition represents genuine regulatory events, while later degradation may be a consequence of caspase activation [10].
- Annexin V Staining: The Annexin Vâº/6-CFDA⺠population represents authentic apoptosis, while Annexin Vâº/6-CFDAâ» indicates secondary necrosis [11].
- Functional Correlations: Always correlate molecular changes with functional outcomes (phagocytosis, inflammation resolution) when possible [8].
- Physiological Relevance: Compare effects of pharmacological manipulations to physiological apoptosis inducers (e.g., phagocytosis of bacteria) [1].
Troubleshooting Common Issues
- High Background Apoptosis: Ensure rapid processing, maintain low temperatures during isolation, and use pre-wash fixation methods to minimize activation.
- Inconsistent Mcl-1 Results: Include protease and phosphatase inhibitors in lysis buffers, and process samples quickly after collection due to rapid Mcl-1 turnover.
- Poor Caspase Inhibition: Use Q-VD.OPh instead of zVAD.fmk for more effective caspase inhibition in neutrophils.
- Non-specific Antibody Binding: Remove unbound antibodies before fixation and consider heparin treatment to reduce ionic interactions with cationic neutrophil proteins [12].
The precise regulation of Mcl-1 dynamics and caspase activation represents a critical control point in neutrophil apoptosis and inflammation resolution. The protocols and methodologies detailed in this application note provide standardized approaches for investigating these key molecular regulators. By implementing these robust experimental systems, researchers can advance our understanding of neutrophilic inflammatory diseases and develop targeted therapeutic strategies that enhance inflammation resolution without compromising host defense.
The regulated process of neutrophil apoptosis is a critical checkpoint for the resolution of inflammation. In healthy immune responses, neutrophils undergo constitutive apoptosis within hours of their release into circulation, facilitating their silent clearance by macrophages and preventing the release of histotoxic contents. This process, known as efferocytosis, promotes an anti-inflammatory environment and tissue repair. However, dysregulation of this programmed cell death underlies the pathogenesis of numerous inflammatory conditions. In the context of Acute Respiratory Distress Syndrome (ARDS), sepsis, and autoimmunity, delayed neutrophil apoptosis creates a persistent inflammatory state that drives tissue injury and organ dysfunction. This application note examines the consequences of this dysregulation and provides established methodologies for investigating neutrophil apoptosis in inflammation resolution research.
Pathophysiological Consequences of Dysregulated Neutrophil Apoptosis
Acute Respiratory Distress Syndrome (ARDS)
In ARDS, a neutrophil-associated disease, delayed neutrophil apoptosis significantly contributes to persistent lung inflammation and tissue damage. Research demonstrates that neutrophils from ARDS patients exhibit extended lifespan due to delayed apoptosis, which enhances the formation of Neutrophil Extracellular Traps (NETs) [13]. These NETs, while initially protective against pathogens, cause collateral damage to lung tissue when produced in excess. The cyclin-dependent kinase inhibitor AT7519 has been shown to reverse delayed apoptosis in ARDS neutrophils, reducing NET formation and subsequent tissue damage [13]. This pathway represents a promising therapeutic target for breaking the cycle of inflammation in ARDS.
Table 1: Key Quantitative Findings in ARDS Pathogenesis
| Parameter | Experimental Finding | Significance | Citation |
|---|---|---|---|
| Neutrophil Apoptosis Rate | Significantly delayed in ARDS patients vs. healthy controls | Establishes prolonged neutrophil lifespan as a disease mechanism | [13] |
| NET Formation | Enhanced in ARDS neutrophils; correlates with apoptosis delay | Links delayed apoptosis to tissue-damaging NETosis | [13] |
| CDK Inhibition Effect | AT7519 reversed delayed apoptosis and reduced NETs | Identifies potential therapeutic pathway | [13] |
| cf-DNA Levels | Increased in ARDS plasma; inversely correlates with PaOâ‚‚/FiOâ‚‚ (r = -0.88) | Suggests NETs as biomarker and contributor to oxygenation deficit | [14] |
| Lung Injury Alleviation | NET inhibition (GSK484), depletion (anti-Ly6G), or degradation (DNase I) reduced injury scores and inflammation | Confirms pathogenic role of NETs and validates therapeutic strategies | [14] |
Sepsis and Sepsis-Induced ALI/ARDS
Sepsis represents a state of profound immune dysregulation where the synergistic interplay of inflammation and apoptosis creates a vicious cycle of tissue injury. In sepsis-induced ALI/ARDS, an overactivated inflammatory response exacerbates lung tissue damage and promotes excessive apoptosis of structural cells. Conversely, this rampant apoptosis further intensifies the inflammatory response [15]. Neutrophils in sepsis exhibit delayed apoptosis, leading to increased infiltration in lungs and heightened release of cytotoxic substances, including NETs [16]. These NETs, composed of nuclear DNA, histones, and granule proteins like myeloperoxidase (MPO) and neutrophil elastase (NE), directly damage the alveolar-capillary barrier, leading to pulmonary edema and dysfunction [14] [17]. Furthermore, NETs can trigger autophagic flux impairment in alveolar epithelial cells via METTL3-mediated methylation, unveiling a novel mechanism of sepsis-associated organ injury [14].
Autoimmunity
While the search results provided are less focused on autoimmunity, the mechanisms described have clear implications. Excessive NETosis contributes to the pathology of chronic inflammatory and autoimmune diseases by promoting inflammation and tissue damage [18]. The persistence of NET components, particularly citrullinated histones and DNA, can act as autoantigens in susceptible individuals, breaking immune tolerance and triggering autoimmune responses such as those seen in rheumatoid arthritis and systemic lupus erythematosus (SLE) [18]. The delayed clearance of apoptotic neutrophils may also lead to secondary necrosis and the release of intracellular contents, further amplifying the pool of potential autoantigens.
Experimental Protocols for Neutrophil Apoptosis Assays
Protocol: Assessment of Human Neutrophil Apoptosis via Flow Cytometry
This protocol is adapted from methodologies used in recent research to quantify the rate of neutrophil apoptosis in clinical samples [13].
Principle: This method uses Annexin V-FITC and Propidium Iodide (PI) staining to distinguish between viable (Annexin V-/PI-), early apoptotic (Annexin V+/PI-), and late apoptotic/necrotic (Annexin V+/PI+) cell populations by flow cytometry.
Materials:
- EasySep Direct Human Neutrophil Isolation Kit (STEMCELL Technologies) [13]
- Iscove’s modified Dulbecco’s medium with 10% FBS
- Annexin V-FITC/PI Apoptosis Detection Kit (e.g., KeyGEN) [13]
- Flow cytometer with 488 nm excitation laser
- Specific reagents for stimulation/inhibition (e.g., AT7519, GM-CSF, LPS) [13]
Procedure:
- Neutrophil Isolation: Isolate neutrophils from fresh human venous blood using the EasySep Direct Human Neutrophil Isolation Kit according to the manufacturer's instructions.
- Cell Culture: Resuspend isolated neutrophils at 1 × 10ⶠcells/mL in culture medium. Seed into a 6-well plate and culture with or without test compounds (e.g., pro-survival factors like GM-CSF/LPS or pro-apoptotic agents like AT7519) for the desired duration (e.g., 24 hours) at 37°C and 5% CO₂ [13].
- Cell Staining:
- Harvest neutrophils and wash once with cold DPBS.
- Resuspend the cell pellet in Annexin V binding buffer.
- Add Annexin V-FITC and PI to the cell suspension and incubate for 15 minutes at room temperature in the dark.
- Flow Cytometric Analysis: Analyze the stained cells within 1 hour using a flow cytometer. Collect a minimum of 10,000 events per sample. Use unstained and single-stained controls to set up compensation and gating.
- Data Analysis: Calculate the percentages of cells in each quadrant. The early apoptosis rate is represented by the Annexin V+/PI- population.
Protocol: In Vivo Assessment of NETosis Inhibition in Murine Sepsis-ALI Model
This protocol outlines the use of NETosis inhibitors to establish a causal link between NETs and pathology in a preclinical model [14].
Principle: Cecal Ligation and Puncture (CLP) is used to induce polymicrobial sepsis and subsequent ALI in mice. Pharmacological inhibition of NET formation or degradation of existing NETs is used to assess their functional role.
Materials:
- C57BL/6 mice (8-12 weeks old)
- GSK484 (PAD4 inhibitor) or DNase I [14]
- Sterile saline (vehicle control)
- Equipment for CLP surgery
- Supplies for sample collection (bronchoalveolar lavage, plasma)
Procedure:
- Model Induction: Perform the CLP procedure under anesthesia to induce sepsis-associated ALI [14].
- Therapeutic Intervention:
- For NET inhibition: Administer GSK484 (e.g., 5 mg/kg) or vehicle via intraperitoneal injection at designated time points post-CLP.
- For NET degradation: Administer DNase I (e.g., 10 mg/kg) intravenously or intraperitoneally [14].
- Sample Collection: At the experimental endpoint (e.g., 24 hours post-CLP), collect blood (for plasma cf-DNA analysis), perform bronchoalveolar lavage (BALF for cytokine measurement), and harvest lung tissue for histology.
- Downstream Analysis:
- Lung Injury Scoring: Score H&E-stained lung sections for hemorrhage, edema, alveolar septal thickening, and leukocyte infiltration [14].
- Pulmonary Edema: Calculate the lung wet/dry weight ratio.
- Systemic Inflammation: Quantify pro-inflammatory cytokines (TNF-α, IL-1β, IL-6) in plasma and BALF by ELISA.
- NET Quantification: Measure plasma cf-DNA levels using a fluorescent assay like PicoGreen [14].
Signaling Pathways and Workflows
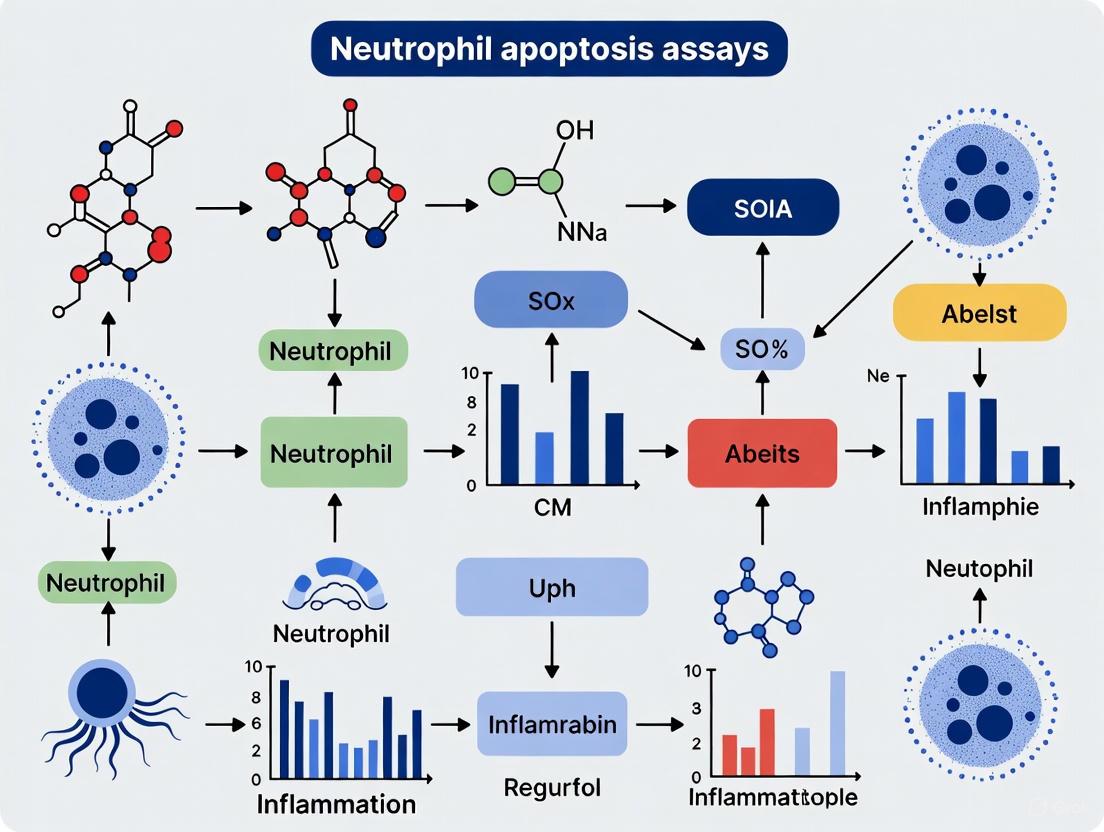
The diagram below illustrates the central role of dysregulated neutrophil apoptosis in driving pathology in ARDS, Sepsis, and Autoimmunity, and highlights key experimental intervention points.
Diagram Title: Neutrophil Apoptosis Dysregulation Core Pathway
The Scientist's Toolkit: Key Research Reagents
Table 2: Essential Reagents for Neutrophil Apoptosis and NETosis Research
| Reagent / Assay | Function / Target | Example Application |
|---|---|---|
| Annexin V / PI Apoptosis Kit | Flow cytometry-based detection of phosphatidylserine externalization (early apoptosis) and membrane integrity. | Quantifying rates of neutrophil apoptosis in patient samples or cultured cells [13]. |
| CDK Inhibitors (e.g., AT7519) | Promotes neutrophil apoptosis by activating GSK-3β and reducing levels of the anti-apoptotic protein Mcl-1 [13]. | Experimental therapeutic to reverse delayed apoptosis and reduce NET formation in ARDS models [13]. |
| PAD4 Inhibitors (e.g., GSK484) | Inhibits peptidylarginine deiminase 4, preventing histone citrullination and subsequent NET formation [14]. | Establishing the causal role of NETs in disease pathogenesis in vivo (e.g., murine CLP model) [14]. |
| DNase I | Degrades the DNA scaffold of existing Neutrophil Extracellular Traps. | Testing the effect of NET degradation on disease severity and inflammation [14]. |
| Anti-Ly6G Antibody | Depletes neutrophils in vivo in mouse models. | Determining the overall contribution of neutrophils to a specific disease pathology [14]. |
| PicoGreen / cf-DNA Assay | Fluorescent quantification of cell-free DNA in plasma or BALF. | Serving as a surrogate, quantifiable marker for NET burden and disease severity [14]. |
| Antibodies: Cit-H3, MPO, NE | Immunofluorescence detection of specific protein components of NETs. | Visualizing and confirming NET formation in tissue sections or cell cultures [13] [14]. |
| Miglustat | Miglustat Reagent|Glucosylceramide Synthase Inhibitor | High-purity Miglustat, a glucosylceramide synthase inhibitor for lysosomal storage disease research. For Research Use Only. Not for human use. |
| Minalrestat | Minalrestat, CAS:129688-50-2, MF:C19H11BrF2N2O4, MW:449.2 g/mol | Chemical Reagent |
Dysregulation of neutrophil apoptosis is a cornerstone of dysresolved inflammation in ARDS, sepsis, and autoimmunity. The consequent persistence of neutrophils and excessive NETosis creates a feed-forward loop of tissue damage and immune activation. The experimental protocols and tools outlined herein provide a foundation for researchers to dissect these mechanisms, validate novel therapeutic targets, and screen potential compounds designed to restore the physiological resolution of inflammation by promoting neutrophil apoptosis.
Integrin Signaling and Extracellular Cues in Fate Decision Making
Integrin receptors are fundamental mediators of cell-extracellular matrix (ECM) and cell-cell interactions, transducing crucial biochemical and mechanical signals that govern cell fate decisions, including survival, proliferation, and apoptosis [19]. In the context of neutrophil biology, these signals are paramount for regulating the inflammatory response. Neutrophils, the first responders to infection or injury, must be tightly controlled; their timely removal via apoptosis is essential for the resolution of inflammation and prevention of collateral tissue damage [20]. Dysregulation of neutrophil apoptosis is a hallmark of persistent inflammatory states. This Application Note delineates detailed protocols for investigating how integrin-mediated signaling and other extracellular cues influence the fate of human neutrophils, providing a critical toolkit for research aimed at resolving inflammation.
Background
Integrin Biology and Signaling Mechanisms
Integrins are heterodimeric transmembrane receptors composed of non-covalently associated α and β subunits. In humans, 18 α and 8 β subunits combine to form 24 distinct integrins [19]. They exist in a delicate equilibrium between inactive (bent) and active (extended) conformations, regulated by "inside-out" and "outside-in" signaling.
- Inside-Out Signaling: Intracellular signals, triggered by stimuli from other receptors, lead to talin and kindlin binding to the β-integrin cytoplasmic tail. This binding induces a conformational change in the integrin ectodomain, increasing its affinity for extracellular ligands [19].
- Outside-In Signaling: Ligand binding to the active integrin ectodomain induces clustering and further conformational changes, promoting the assembly of large multi-protein complexes called Integrin Adhesion Complexes (IACs). This initiates downstream signaling cascades [19] [21].
A key pathway in outside-in signaling involves the recruitment and activation of Focal Adhesion Kinase (FAK) and Src-family kinases. FAK autophosphorylation creates a binding site for Src, forming a fully active FAK-Src complex that phosphorylates downstream targets such as paxillin and PI3K. This cascade activates critical pro-survival pathways, including the ERK and AKT pathways [19] [21]. The diagram below illustrates the core integrin signaling pathway to survival and apoptosis.
Neutrophil Apoptosis in Inflammation Resolution
Neutrophils are short-lived cells, and their lifespan is dynamically regulated by signals from the microenvironment. Under homeostatic conditions, circulating neutrophils undergo spontaneous apoptosis within hours to days. At inflammatory sites, survival cues from cytokines, bacterial products, and the ECM can delay apoptosis to ensure effective pathogen clearance [20] [22]. Integrins, particularly β1 (e.g., VLA-3, -6) and β2 (e.g., αMβ2/Mac-1) families, are critical transducers of these extracellular survival signals. The eventual induction of apoptosis and subsequent clearance by macrophages is a crucial, non-phlogistic process that defines the resolution of inflammation [20]. Therefore, understanding and experimentally modulating integrin signaling provides a powerful means to control neutrophil lifespan and promote inflammation resolution.
Application Notes
Key Integrin Subtypes in Neutrophil Biology
Neutrophils express a repertoire of integrins that mediate adhesion, migration, and survival. The following table summarizes the key integrins relevant to neutrophil fate decisions.
Table 1: Key Integrin Subtypes in Neutrophil Biology
| Integrin | Major Ligands | Primary Functions in Neutrophils | Role in Fate Decision |
|---|---|---|---|
| αMβ2 (Mac-1, CR3) | iC3b, Fibrinogen, ICAM-1 | Phagocytosis, adhesion to endothelium, migration | Pro-survival: Strong outside-in signaling via FAK/PI3K-AKT upon ligand engagement [20]. |
| αLβ2 (LFA-1) | ICAM-1, ICAM-2 | Adhesion to endothelium, migration, immunological synapse | Pro-survival: Engagement can delay apoptosis, contributing to prolonged inflammatory response [19]. |
| α4β1 (VLA-4) | VCAM-1, Fibronectin | Adhesion to activated endothelium, migration | Pro-survival: Provides co-stimulatory signals that enhance neutrophil survival in tissues [19]. |
| α5β1 (VLA-5) | Fibronectin (RGD) | Adhesion to ECM | Pro-survival: Classical RGD-binding integrin; ligation activates potent anti-apoptotic signaling pathways [19] [21]. |
| α6β1 (VLA-6) | Laminin | Adhesion to basement membrane | Pro-survival: Engagement in tissues can transmit signals that delay constitutive apoptosis [19]. |
Quantitative Impact of Extracellular Cues on Neutrophil Apoptosis
The rate of neutrophil apoptosis is highly sensitive to the extracellular environment. The quantitative effects of various stimuli are summarized below.
Table 2: Impact of Extracellular Cues on Neutrophil Spontaneous Apoptosis
| Stimulus / Cue | Example | Approximate Effect on Apoptosis vs. Control | Primary Signaling Pathway(s) |
|---|---|---|---|
| Pro-Survival Inflammatory Mediators | LPS, GM-CSF, G-CSF | Delayed by 50-80% (at 18-24 hours) | JAK/STAT, NF-κB, PI3K/AKT [20] [22] |
| Integrin-Mediated Adhesion | Fibronectin (via α5β1), Fibrinogen (via αMβ2) | Delayed by 40-70% (at 18-24 hours) | FAK/Src, PI3K/AKT, ERK [20] [21] |
| Pro-Resolving Mediators | Lipoxin A4, Annexin A1 | Accelerated by 60-90% (at 6-12 hours) | cAMP/PKA, Caspase-8/3 activation [20] |
| Soluble Integrin Antagonists | RGD-mimetic peptides, Anti-β2 mAb | Accelerated by 20-50% (in adherent conditions) | Inhibition of FAK phosphorylation and downstream survival signals [19] [20] |
Protocols
Protocol 1: Assessing Integrin-Mediated Survival on Ligand-Coated Surfaces
This protocol evaluates the effect of specific integrin-ligand engagement on delaying neutrophil apoptosis.
Workflow Overview:
Materials:
- Research Reagent Solutions: See Section 5.1 for details.
Step-by-Step Procedure:
- Neutrophil Isolation: Isolate human neutrophils from fresh peripheral blood or buffy coats from healthy donors using density gradient centrifugation (e.g., Polymorphprep or Ficoll-Paque PLUS). Use dextran sedimentation and hypotonic lysis to remove residual erythrocytes. Resuspend cells in appropriate serum-free culture medium (e.g., RPMI-1640).
- Plate Coating: Coat sterile 24-well tissue culture plates by adding 300 µL of the desired ECM protein solution.
- Fibronectin: 10 µg/mL in PBS.
- Fibrinogen: 20 µg/mL in PBS.
- BSA (Control): 1% (w/v) in PBS.
- Incubate plates for 2 hours at 37°C or overnight at 4°C. Aspirate the coating solution and block non-specific binding sites with 1% heat-inactivated BSA in PBS for 1 hour at 37°C. Wash twice with PBS before cell seeding.
- Cell Seeding & Inhibition: Resuspend the isolated neutrophils in serum-free medium at 1 x 10^6 cells/mL. For inhibition studies, pre-incubate cells with function-blocking anti-integrin antibodies (e.g., 10 µg/mL anti-β2, clone IB4) or isotype control antibodies on ice for 30 minutes. Seed 500 µL of cell suspension per well. Include a suspension control (cells kept in polypropylene tubes) to assess apoptosis without adhesion.
- Incubation: Incubate the plates at 37°C in a 5% CO2 humidified incubator for the desired time (e.g., 6, 12, 18, 24 hours).
- Apoptosis Assessment (Annexin V/PI Staining):
- Gently harvest non-adherent and adherent cells (using gentle accutase or cell scraping) and combine them for analysis.
- Wash cells once with cold PBS and resuspend in 100 µL of 1X Annexin V Binding Buffer.
- Add 5 µL of Fluorescein isothiocyanate (FITC)-conjugated Annexin V and 5 µL of Propidium Iodide (PI) solution.
- Incubate for 15 minutes at room temperature in the dark.
- Add 400 µL of 1X Annexin V Binding Buffer and analyze by flow cytometry within 1 hour.
- Analysis: Calculate the percentage of apoptotic cells (Annexin V+/PI- for early apoptosis; Annexin V+/PI+ for late apoptosis/necrosis).
Protocol 2: Probing Downstream Signaling via FAK Phosphorylation
This protocol assesses the activation of key integrin downstream signaling pathways by detecting phosphorylation of FAK and ERK.
Workflow Overview:
Materials:
- Research Reagent Solutions: See Section 5.1 for details.
Step-by-Step Procedure:
- Cell Stimulation: Isolate and seed neutrophils on ligand-coated plates as described in Protocol 1, Steps 1-3. Use a higher cell density (e.g., 2-5 x 10^6 cells/well in a 6-well plate) for sufficient protein yield.
- Time Course: Allow cells to adhere and signal for short time points (e.g., 5, 15, 30, 60 minutes) in the 37°C incubator.
- Cell Lysis: At each time point, quickly place the plates on ice and aspirate the medium. Immediately lyse the cells directly in the well with 150-200 µL of cold RIPA Lysis Buffer containing 1X protease and phosphatase inhibitors. Scrape the wells thoroughly and transfer the lysate to a pre-chilled microcentrifuge tube.
- Protein Handling: Vortex lysates for 10-15 seconds and incubate on ice for 30 minutes. Centrifuge at 14,000 x g for 15 minutes at 4°C. Transfer the supernatant (cleared lysate) to a new tube.
- Protein Quantification & Western Blot: Determine protein concentration using a BCA Protein Assay Kit. Prepare samples with Laemmli buffer, denature at 95°C for 5 minutes, and separate 20-30 µg of total protein by SDS-PAGE (8-10% gel). Transfer to a PVDF membrane, block with 5% BSA in TBST for 1 hour, and probe with primary antibodies overnight at 4°C.
- Key Primary Antibodies: Anti-phospho-FAK (Tyr397), Anti-total FAK, Anti-phospho-p44/42 MAPK (ERK1/2, Thr202/Tyr204), Anti-total ERK1/2, Anti-β-Actin (loading control).
- Detection: Incubate with appropriate HRP-conjugated secondary antibodies for 1 hour at room temperature. Develop using enhanced chemiluminescence (ECL) substrate and visualize with a digital imager.
- Analysis: Perform densitometric analysis using software like ImageJ or Image Lab. Normalize the band intensity of p-FAK to total FAK and p-ERK to total ERK to determine fold-change in phosphorylation relative to the control condition (e.g., BSA-coated surface).
The Scientist's Toolkit
Research Reagent Solutions
The following table lists essential reagents for studying integrin signaling in neutrophil apoptosis.
Table 3: Essential Reagents for Integrin and Neutrophil Apoptosis Research
| Reagent / Material | Function / Application | Example(s) / Notes |
|---|---|---|
| Function-Blocking Anti-Integrin Antibodies | To specifically inhibit ligand binding and outside-in signaling from specific integrins. | Anti-human CD18 (β2 integrin) e.g., Clone IB4; blocks αLβ2, αMβ2. Anti-human CD49e (α5 integrin) e.g., Clone SAM-1; blocks α5β1 [19]. |
| Recombinant ECM Proteins | To provide specific ligands for integrin engagement in coating assays. | Fibronectin (ligand for α5β1, α4β1), Fibrinogen (ligand for αMβ2), Laminin (ligand for α6β1). Use purified, pathogen-free proteins [19]. |
| RGD-Mimetic Peptides | Competitive antagonists for a broad range of RGD-binding integrins (e.g., α5β1, αVβ3). | Cyclo(RGDfK); a potent and stable cyclic RGD peptide. Useful as a pan-inhibition control [19]. |
| Phospho-Specific Antibodies | Detection of key signaling molecule activation in Western blot. | Anti-phospho-FAK (Tyr397), Anti-phospho-ERK1/2 (Thr202/Tyr204), Anti-phospho-AKT (Ser473) [21]. |
| Annexin V Conjugates & Propidium Iodide (PI) | Detection of phosphatidylserine externalization (early apoptosis) and loss of membrane integrity (late apoptosis/necrosis). | FITC-Annexin V and PI are standard for flow cytometry. Use a calcium-containing binding buffer [20]. |
| Small Molecule Kinase Inhibitors | Pharmacological inhibition of downstream integrin signaling pathways. | PF-573228 (FAK Inhibitor), LY294002 (PI3K Inhibitor), U0126 (MEK1/2 Inhibitor). Use with appropriate vehicle controls [20] [21]. |
| Pro-Resolving Lipid Mediators | Positive controls for inducing apoptosis and promoting resolution. | Lipoxin A4, Resolvin D1. These endogenously produced mediators can redirect neutrophils to apoptosis [20]. |
| Minaprine | Minaprine for Research|High-Quality Chemical Reagent | Minaprine for Research Use Only (RUO). Explore this phenylpyridazine derivative's applications in neuroscience and inflammation research. Not for human consumption. |
| Minimycin | Minimycin, CAS:32388-21-9, MF:C9H11NO7, MW:245.19 g/mol | Chemical Reagent |
Efferocytosis, the process by which apoptotic cells are recognized and removed by phagocytes, is a critical biological mechanism for maintaining tissue homeostasis and ensuring the resolution of inflammation [23]. In the context of neutrophil biology, this process is particularly crucial. Neutrophils, as the most abundant leukocytes in human blood and key first responders at sites of inflammation, have a short lifespan and undergo apoptosis constitutively [1] [24]. The efficient clearance of apoptotic neutrophils by macrophages prevents secondary necrosis and the leakage of harmful intracellular substances, thereby promoting the resolution of inflammation and tissue repair [23] [7]. Dysregulation of this process has been implicated in various pathological conditions, including chronic inflammatory diseases, autoimmune disorders, and cancer [25]. This application note details the molecular mechanisms of the efferocytosis cascade and provides standardized protocols for studying neutrophil apoptosis and subsequent clearance within the broader context of inflammation resolution research.
Molecular Mechanisms of the Efferocytosis Cascade
Efferocytosis is a highly coordinated, multi-stage process that ensures the silent removal of apoptotic cells. The molecular cascade can be divided into distinct phases: the release of find-me signals, exposure of eat-me signals, recognition and engulfment by phagocytes, and subsequent immunomodulatory reprogramming of the efferocyte [25].
Table 1: Key Molecular Signals in the Efferocytosis Cascade
| Signal Type | Key Molecules | Source | Receptor on Phagocyte | Function |
|---|---|---|---|---|
| Find-Me Signals | ATP, UTP [25] | Apoptotic Cell | P2Y purinergic receptors [25] | Initial chemotaxis, enhance phagocyte motility |
| Lysophosphatidylcholine (LPC) [25] | Apoptotic Cell | G2A receptor [25] | Stimulates chemotactic migration | |
| Sphingosine-1-phosphate (S1P) [25] | Apoptotic Cell | S1PR1-5 [25] | Sustained recruitment, enhances efferocytic efficiency | |
| Fractalkine (CX3CL1) [25] | Apoptotic Cell | CX3CR1 [25] | Directs migration of immune cells | |
| Eat-Me Signals | Phosphatidylserine (PS) [7] [25] | Apoptotic Cell | Direct (e.g., TIM-4) or indirect (via MFG-E8, Gas6) [7] | Primary "eat-me" signal; triggers engulfment |
| Calreticulin [25] | Apoptotic Cell | CD91/LRP [25] | Complementary recognition signal | |
| Don't-Eat-Me Signals | CD47 [23] | Healthy Cell | SIRPα [23] | Prevents phagocytosis of viable cells |
| Soluble Bridging Molecules | Milk fat globule-EGF factor 8 (MFG-E8) [7] | Microenvironment | αVβ3 integrin [7] | Bridges PS to phagocyte receptor |
| Growth Arrest-Specific 6 (Gas6) [7] | Microenvironment | TAM receptors (Tyro3, Axl, MerTK) [23] | Bridges PS to phagocyte receptor |
The diagram below illustrates the core signaling pathway from initial apoptosis to macrophage reprogramming.
Find-Me and Eat-Me Signals
The process initiates with apoptotic cells releasing find-me signals such as nucleotides (ATP, UTP), lysophosphatidylcholine (LPC), and sphingosine-1-phosphate (S1P) [25]. These molecules establish a chemotactic gradient that recruits potential phagocytes, primarily macrophages, to the site of cell death. Upon arrival, phagocytes recognize eat-me signals on the apoptotic cell surface. The most well-characterized eat-me signal is phosphatidylserine (PS), a phospholipid normally restricted to the inner leaflet of the plasma membrane but exposed on the outer leaflet during apoptosis [7] [25]. PS is recognized either directly by receptors like TIM-4 on phagocytes or indirectly through soluble bridging proteins such as MFG-E8 and Gas6, which bind to integrins or TAM family receptors (Tyro3, Axl, MerTK), respectively [23] [7].
Engulfment and Phagocyte Reprogramming
Following recognition, the phagocyte engulfs the apoptotic cell through actin cytoskeleton rearrangement, forming a phagosome that matures by fusing with lysosomes to degrade the cargo [7]. This engulfment phase is followed by a critical functional reprogramming of the efferocytic macrophage. This reprogramming involves a shift from a pro-inflammatory (M1-like) phenotype to a pro-resolving (M2-like) phenotype, characterized by decreased production of pro-inflammatory cytokines (e.g., IL-1β, TNF) and increased secretion of anti-inflammatory and reparative mediators such as TGF-β, IL-10, and vascular endothelial growth factor (VEGF) [26] [7]. This switch is essential for the active resolution of inflammation and tissue repair.
Experimental Protocols
This section provides a detailed methodology for establishing an in vitro co-culture system to study the efferocytosis of apoptotic neutrophils by macrophages, a cornerstone assay in inflammation resolution research.
Protocol 1: Neutrophil Isolation and Apoptosis Induction
Objective: To isolate human neutrophils from peripheral blood and induce apoptosis in a controlled manner.
Materials:
- Research Reagent Solutions: Sodium Heparin tubes, Dextran Saline Solution (6% w/v), Ficoll-Paque PLUS, Hanks' Balanced Salt Solution (HBSS) without Ca²âº/Mg²âº, RPMI 1640 medium, Heat-inactivated Fetal Bovine Serum (FBS), Annexin V Binding Buffer.
- Key Equipment: Centrifuge, Class II biological safety cabinet, Hemocytometer, COâ‚‚ incubator.
Procedure:
- Neutrophil Isolation: Collect venous blood from healthy donors into sodium heparin tubes. Mix blood with an equal volume of dextran saline solution and allow red blood cells to sediment for 30-45 minutes at room temperature.
- Layer the leukocyte-rich supernatant over Ficoll-Paque and centrifuge at 400 × g for 25 minutes at 20°C.
- Aspirate the mononuclear cell layer and isolate the neutrophil pellet. Lyse any residual red blood cells with hypotonic saline. Wash neutrophils twice with HBSS without Ca²âº/Mg²âº.
- Viability and Purity Check: Resuspend cells in complete RPMI medium (RPMI 1640 + 10% FBS). Assess viability via Trypan Blue exclusion (should be >98%) and purity by morphological analysis on cytospin slides stained (should be >95%).
- Apoptosis Induction: Seed neutrophils at a density of 2 × 10ⶠcells/mL in complete RPMI medium.
- Induce apoptosis by incubating the cells in a humidified CO₂ incubator at 37°C for 18-20 hours. This spontaneous aging reliably induces apoptosis in 40-60% of neutrophils [1] [27].
- Apoptosis Quantification: After incubation, harvest neutrophils and stain with Annexin V-FITC and Propidium Iodide (PI) in Annexin V Binding Buffer for 15 minutes in the dark. Analyze by flow cytometry. Annexin V+/PI- cells are considered early apoptotic and are the primary targets for efferocytosis.
Protocol 2: Macrophage Differentiation and Efferocytosis Co-culture
Objective: To differentiate human monocyte-derived macrophages and establish a quantitative efferocytosis assay.
Materials:
- Research Reagent Solutions: Peripheral Blood Mononuclear Cells (PBMCs), Macrophage Colony-Stimulating Factor (M-CSF), Fluorescent dye (e.g., CellTracker Green CMFDA), Phosphate Buffered Saline (PBS), Paraformaldehyde (4% w/v).
- Key Equipment: Cell culture incubator, Flow cytometer or fluorescence microscope.
Procedure:
- Macrophage Differentiation: Isolate PBMCs from blood via density gradient centrifugation. Seed monocytes (e.g., by adherence or CD14+ selection) in tissue culture plates.
- Differentiate monocytes into macrophages by culturing for 5-7 days in complete RPMI 1640 medium supplemented with 50 ng/mL M-CSF, refreshing the medium every 2-3 days.
- Fluorescent Labeling of Apoptotic Neutrophils: After inducing apoptosis as in Protocol 1, label the neutrophil population with 5 µM CellTracker Green CMFDA in serum-free medium for 30 minutes at 37°C. Wash cells three times with PBS to remove excess dye.
- Efferocytosis Co-culture: Wash the differentiated macrophage monolayer with PBS. Add the labeled, apoptotic neutrophils to the macrophages at a ratio of 5:1 (neutrophils:macrophages).
- Allow efferocytosis to proceed for 60-90 minutes in a CO₂ incubator at 37°C.
- Termination and Staining: After co-culture, vigorously wash the monolayer with PBS to remove non-engulfed neutrophils. Fix the macrophages with 4% paraformaldehyde for 15 minutes.
- To distinguish between attached and truly internalized neutrophils, stain the macrophage outer membrane with an anti-CD45 antibody (or another macrophage surface marker) conjugated to a different fluorophore (e.g., APC) after fixation and permeabilization.
Quantification and Analysis
Flow Cytometry: Analyze the fixed macrophages by flow cytometry. Macrophages that are positive for both the neutrophil dye (Green) and the macrophage surface marker (APC) are scored as having performed efferocytosis. The percentage of double-positive macrophages quantifies the efferocytic index. Immunofluorescence Microscopy: Image fixed cells using a fluorescence microscope. The number of fluorescent inclusions (engulfed neutrophils) per 100 macrophages can be counted manually or using image analysis software.
The workflow for the complete co-culture assay is summarized below.
The Scientist's Toolkit
Table 2: Essential Research Reagent Solutions for Efferocytosis Studies
| Item | Function/Application | Example Reagents |
|---|---|---|
| Recombinant Human M-CSF | Differentiation of human monocytes into macrophages for efferocytosis assays. | Commercially available GMP-grade proteins. |
| Annexin V Conjugates | Flow cytometric or microscopic quantification of phosphatidylserine exposure during apoptosis. | Annexin V-FITC, Annexin V-APC. |
| Cell Tracker Dyes | Fluorescent labeling of apoptotic neutrophils for tracking and quantification in co-culture. | CellTracker Green CMFDA, CellTracker Red CMTPX. |
| TAM Kinase Inhibitors | Investigating the role of key efferocytosis receptors (Tyro3, Axl, MerTK) through pharmacological inhibition. | Small molecule inhibitors (e.g., UNC2025 for MerTK). |
| Pro-Resolving Mediators | Studying the enhancement of efferocytosis and inflammation resolution. | Resolvin E1, Lipoxin A4 [1] [26]. |
| Phagocytosis Inhibitors | Control experiments to confirm specific engulfment (e.g., cytochalasin D to disrupt actin polymerization). | Cytochalasin D, Latrunculin B. |
| Myramistin | Miramistin|CAS 15809-19-5|Antiseptic Research Agent | Miramistin for research: a broad-spectrum topical antiseptic. Study its applications in antimicrobial and biofilm research. For Research Use Only. |
| Mirincamycin Hydrochloride | Mirincamycin Hydrochloride | Mirincamycin hydrochloride is a lincosamide for malaria research. Shown to have causal prophylactic and radical cure activity. For Research Use Only. Not for human use. |
Core and Advanced Assay Methodologies for Apoptosis Quantification
The precise quantification of apoptosis, especially in complex inflammatory contexts, is fundamental to research on inflammation resolution. Among the various techniques available, flow cytometry-based assays, particularly the Annexin V/Propidium Iodide (PI) staining method, have emerged as a gold standard for identifying apoptotic cells. This application note details the core protocol for Annexin V/PI and its evolution into sophisticated multiparameter panels, providing researchers with a structured framework to accurately delineate early and late apoptotic stages in neutrophil studies. Adherence to the best practices outlined here is critical for generating reproducible, high-quality data that can reliably inform drug development efforts.
Apoptosis Assay Comparison
The following table systematically compares the major flow cytometry-based assays used for detecting regulated cell death, highlighting their specific applications and limitations.
Table 1: Comparison of Flow Cytometry-Based Apoptosis and Viability Assays
| Assay Type | Key Readout | Phase of Apoptosis Detected | Key Advantages | Key Limitations |
|---|---|---|---|---|
| Annexin V/PI | Phosphatidylserine (PS) exposure & membrane integrity [28] | Early (Annexin V+/PI-) & Late (Annexin V+/PI+) [28] | Simple, distinguishes early/late apoptosis and necrosis [28] | Calcium-dependent; cannot be used with EDTA [29] |
| Mitochondrial Potential (e.g., TMRM) | Loss of mitochondrial transmembrane potential (Δψm) [28] | Early | Sensitive marker for early apoptotic events [28] | Potential toxicity of probes; requires careful controls [28] |
| Caspase Activation (e.g., FLICA) | Activation of executioner caspases [28] | Early/Execution Phase | Directly probes key apoptotic machinery [28] | FLICA is an inhibitor; may interfere with pathway [28] |
| DNA Fragmentation (Sub-G1) | Loss of DNA content [28] | Late | Can be combined with cell cycle analysis [28] | Only detects late-stage apoptosis [28] |
| Fixable Viability Dyes (FVD) | Covalent labeling of compromised cells [29] | Viability (dead cells) | Compatible with intracellular staining; fixed samples [29] | Not a specific apoptosis marker; indicates general viability [29] [30] |
The Core Mechanism: Annexin V/Propidium Iodide Binding
The Annexin V/PI assay discriminates between healthy, early apoptotic, late apoptotic, and necrotic cells based on two fundamental changes in cell physiology: the translocation of phosphatidylserine (PS) from the inner to the outer leaflet of the plasma membrane, and the loss of plasma membrane integrity.
Diagram 1: Cellular states and corresponding Annexin V/PI staining patterns.
Detailed Experimental Protocols
Basic Annexin V/PI Staining Protocol
This protocol is adapted from standard methods [29] [31] and is suitable for the basic discrimination of apoptosis and necrosis in cell cultures.
Table 2: Reagents and Equipment for Annexin V/PI Staining
| Item | Function/Description | Example/Note |
|---|---|---|
| Annexin V Conjugate | Binds to exposed Phosphatidylserine (PS) | Fluorochrome-conjugated (e.g., FITC, APC); protect from light [29]. |
| Propidium Iodide (PI) | DNA intercalator; stains cells with permeable membranes | Viability dye; do not wash out after adding [29]. |
| 10X Binding Buffer | Provides optimal Ca²⺠and pH for Annexin V binding | Dilute to 1X with distilled water before use [29]. |
| Cell Wash Buffer | Removes media/serum without chelating Ca²⺠| 1X PBS, azide- and serum-free for some protocols [29]. |
| Flow Cytometer Tubes | Sample holding for acquisition | 12 x 75 mm round-bottom tubes recommended [29]. |
Procedure:
- Cell Preparation: Harvest and wash cells (e.g., neutrophils) once with 1X PBS and once with 1X Binding Buffer. Centrifuge at 400-600 x g for 5 minutes [29].
- Resuspension: Resuspend the cell pellet at a density of 1-5 x 10ⶠcells/mL in 1X Binding Buffer [29].
- Annexin V Staining: Add 5 µL of fluorochrome-conjugated Annexin V to 100 µL of cell suspension. Mix gently [29].
- Incubation: Incubate for 10-15 minutes at room temperature. Protect from light [29].
- Wash: Add 2 mL of 1X Binding Buffer and centrifuge (400-600 x g, 5 minutes). Discard the supernatant [29].
- PI Staining: Resuspend the cell pellet in 200 µL of 1X Binding Buffer. Add 5 µL of PI Staining Solution [29].
- Acquisition: Analyze by flow cytometry within 4 hours. Do not wash cells after PI addition [29].
Modified Annexin V/PI Protocol with RNase Treatment
Conventional Annexin V/PI protocols can yield false-positive PI signals (up to 40%) due to PI staining of cytoplasmic RNA, a problem particularly prevalent in large cells like macrophages and some neutrophils [32]. The following modification significantly improves accuracy.
Procedure Modifications (after Step 7 of the basic protocol):
- Fixation: After PI staining and incubation, add 500 µL of 1X Binding Buffer and 500 µL of 2% formaldehyde to the 200 µL sample, creating a 1% formaldehyde solution. Fix on ice for 10 minutes [32].
- Wash: Add 1 mL of 1X PBS, centrifuge at 425 x g for 8 minutes, and decant the supernatant. Repeat this wash step [32].
- RNase Treatment: Resuspend the fixed cell pellet by flicking the tube. Add 16 µL of a 1:100 diluted RNase A (final concentration 50 µg/mL). Incubate for 15 minutes at 37°C [32].
- Final Wash & Acquisition: Add 1 mL of 1X PBS, centrifuge (425 x g, 8 minutes), decant the supernatant, and resuspend in a suitable buffer for flow cytometry analysis [32].
Diagram 2: A comparison of the basic and modified Annexin V/PI staining workflows.
Designing Multiparameter Apoptosis Panels
Integrating Annexin V/PI into multiparameter panels allows for the contextual analysis of apoptosis within specific immune cell subsets, such as neutrophils, in a complex mixture.
Key Principles for Panel Design
- Know Your Cytometer: Understand the instrument's laser (e.g., 488nm, 633nm) and filter configuration. This dictates which fluorophores can be detected [33].
- Antigen Density Dictates Fluorophore Brightness: Pair bright fluorophores (e.g., PE, APC) with low-abundance antigens or rare cell populations. Use dimmer fluorophores (e.g., FITC, PerCP) for highly expressed antigens [34] [33].
- Minimize Spectral Overlap: Choose fluorophores with minimal emission spectrum overlap to reduce spillover and the need for compensation. Avoid problematic combinations like APC and PE-Cy5 [34] [33].
- Titrate Antibodies: For each antibody, perform a titration to find the "separating concentration" that provides the best signal-to-noise ratio, conserves antibody, and minimizes spillover spreading [34].
- Employ Critical Controls:
- Compensation Controls: Use single-stained controls for every fluorophore in the panel. The control must be at least as bright as the sample and use the same fluorophore-antibody conjugate [30].
- Fluorescence Minus One (FMO) Controls: Tubes containing all antibodies except one are essential for accurate gating, especially for dim markers and complex panels [34] [30].
- Viability Control: A viability dye (e.g., Fixable Viability Dye - FVD) is crucial to exclude dead cells, which bind antibodies non-specifically [29] [34]. Note: FVD eFluor 450 is not recommended with some Annexin V kits [29].
Exemplary 6-Color Panel for Neutrophil Apoptosis
Table 3: Example multiparameter panel for analyzing neutrophil apoptosis in mixed cultures
| Marker | Specificity / Purpose | Recommended Fluorophore | Allocation Rationale |
|---|---|---|---|
| Lineage (e.g., CD15) | Neutrophil identification | BV421 (or other violet laser-excited dye) | Bright dye for a key lineage marker; spectrally distinct. |
| Annexin V | PS exposure (Apoptosis) | FITC | Standard for apoptosis; well-characterized. |
| Active Caspase-3 | Caspase activation (Apoptosis) | PE | Very bright dye for an important intracellular target. |
| Propidium Iodide | Membrane integrity (Viability) | N/A (Detected in PI channel) | Standard viability counter-stain. |
| CD16 | Neutrophil maturation/activation | PE-Cy7 | Tandem dye; ensure proper compensation. |
| CD11b | Neutrophil activation | APC | Bright dye for an activation marker. |
| Viability Dye | Fixable viability marker | eF506 or eF780 (from FVD kits) | Distinguish live/dead cells prior to fixation. |
The Scientist's Toolkit: Essential Reagent Solutions
Table 4: Key reagents and resources for flow cytometry apoptosis analysis
| Tool / Reagent | Function | Example Products / Notes |
|---|---|---|
| Annexin V Apoptosis Kits | Provides optimized Annexin V conjugate, binding buffer, and viability dye. | Invitrogen Annexin V Apoptosis Detection Kits (available in FITC, PE, APC, etc.) [29]. |
| Fixable Viability Dyes (FVD) | Covalently labels dead cells prior to fixation/permeabilization. | Invitrogen FVD eFluor 506, eFluor 660, or eFluor 780 [29]. |
| Flow Cytometry Staining Buffer | Protein-supplemented buffer to reduce non-specific antibody binding. | Thermo Fisher Flow Cytometry Staining Buffer (Cat. No. 00-4222) [29]. |
| Intracellular Staining Kits | Permeabilization buffers for staining intracellular antigens (e.g., caspases). | Foxp3/Transcription Factor Staining Buffer Set or Intracellular Fixation & Permeabilization Buffer Set [29]. |
| Compensation Beads | Ultra-bright, uniform particles for setting compensation controls. | Used with antibodies to create consistent single-color controls [33]. |
| Panel Design Tools | Online software to visualize spectral overlap and design panels. | Invitrogen Flow Cytometry Panel Builder [29] [34]. |
| Mirodenafil | Mirodenafil | Mirodenafil is a potent, selective PDE5 inhibitor for research into erectile dysfunction, Alzheimer's, and stroke recovery. For Research Use Only. Not for human consumption. |
| Miroprofen | Miroprofen, CAS:55843-86-2, MF:C16H14N2O2, MW:266.29 g/mol | Chemical Reagent |
High-Throughput Screening (HTS) Assays for Compound Library Evaluation
High-throughput screening (HTS) of compound libraries represents a powerful approach in biomedical research for identifying novel therapeutic agents. Within inflammation resolution research, HTS assays targeting neutrophil apoptosis have emerged as a promising strategy for discovering compounds that can modulate the inflammatory response. Neutrophils, the most abundant leukocytes in human blood, have a short half-life of approximately 6-8 hours in circulation, and their programmed cell death (apoptosis) is a crucial anti-inflammatory mechanism that facilitates safe clearance by macrophages (efferocytosis) without releasing histotoxic contents [35] [36] [37]. The dysregulation of neutrophil apoptosis contributes to persistent inflammation in various diseases, making this process an attractive therapeutic target. This application note details a robust protocol for HTS of compound libraries using flow cytometric apoptosis assays of human neutrophils, enabling the identification of compounds that accelerate neutrophil apoptosis and potentially resolve inflammation [36] [38].
Key Applications and Context in Inflammation Resolution Research
The strategic focus on neutrophil apoptosis in HTS aligns with the broader thesis that targeting fundamental cellular resolution mechanisms offers superior therapeutic potential compared to simply inhibiting pro-inflammatory pathways. This protocol enables:
- Identification of Novel Modulators: Systematic screening of kinase inhibitor libraries and other compound classes to discover regulators of neutrophil apoptotic pathways [36] [38].
- Mechanistic Insights: Investigation of protein kinase signaling pathways that control neutrophil lifespan and death execution, including potential cross-talk with platelet-derived factors known to influence neutrophil apoptosis [35] [36].
- Therapeutic Development: Acceleration of drug discovery for neutrophil-driven inflammatory diseases including autoimmune conditions, where prolonged neutrophil survival perpetuates tissue damage [36] [37].
- Functional Validation: Assessment of compound efficacy in primary human cells, providing physiologically relevant data for lead optimization [36].
Table 1: Key Experimental Parameters for HTS Neutrophil Apoptosis Assays
| Parameter | Specification | Purpose/Rationale |
|---|---|---|
| Blood Volume | 40 ml per donor [38] | Obtain sufficient neutrophils for HTS |
| Neutrophil Yield | ~1 × 10ⶠcells/ml blood [36] [38] | Expected cell yield for screening |
| Neutrophil Purity | >95% [36] [38] | Ensure assay specificity |
| Compound Testing | Up to 88 compounds/experiment [36] | Maximize throughput, minimize variation |
| Key Apoptosis Markers | Annexin-V, TOPRO-3 [36] [38] | Detect phosphatidylserine exposure & membrane integrity |
| Culture Duration | 16-20 hours [36] [37] | Allow spontaneous & compound-induced apoptosis |
Experimental Protocol: HTS Apoptosis Assay for Human Neutrophils
Neutrophil Isolation from Peripheral Blood
This isolation method uses dextran sedimentation and discontinuous plasma/Percoll gradient centrifugation to achieve high purity neutrophils suitable for HTS [36] [38].
Materials & Reagents:
- Tri-sodium citrate (3.8% w/v) as anticoagulant [38]
- 6% Dextran T500 solution in saline [36] [38]
- Percoll and autologous platelet-poor plasma (PPP) for gradient preparation [36]
- RPMI 1640 media or Hank's Balanced Salt Solution [38]
- Equipment: Centrifuges, biological safety cabinet, water bath [36] [38]
Procedure:
- Blood Collection and Initial Processing:
Platelet-Poor Plasma (PPP) Preparation:
Neutrophil Isolation:
- Add 6 ml pre-warmed 6% dextran solution to the remaining blood cell layer and top up to 50 ml with saline [36] [38].
- Mix gently by inversion and allow red blood cells to sediment for 20-30 minutes at room temperature [36].
- Transfer the pale upper leukocyte layer to a clean tube and centrifuge at 224 × g for 6 minutes [36].
- Resuspend cell pellet in a small volume of saline or media [38].
Discontinuous Plasma/Percoll Gradient:
- Prepare the gradient lower phase by combining 1.02 ml 90% Percoll with 0.98 ml PPP [36].
- Layer the cell suspension over the gradient and centrifuge at appropriate speed to separate granulocytes from mononuclear cells [38].
- Collect the neutrophil-rich band, wash with buffer, and resuspend in appropriate culture medium [38].
High-Throughput Compound Screening and Apoptosis Assessment
Materials & Reagents:
- Kinase inhibitor library (e.g., Published Kinase Inhibitor Set - PKIS) [36]
- Culture media (e.g., RPMI 1640 with or without serum) [38]
- Annexin binding buffer (ABB) [36] [38]
- PE-conjugated Annexin-V (1:20 dilution) [36] [38]
- TOPRO-3 (1:7,500 dilution) [36] [38]
- Equipment: 96-well plates, COâ‚‚ incubator, flow cytometer with autosampler [36]
Procedure:
- Compound Treatment:
- Dispense neutrophils into 96-well plates at appropriate density (typically 1-5×10ⵠcells/well) [36].
- Add compounds from library using multichannel pipettes, including controls:
- Negative control: Vehicle (DMSO) only
- Positive control: Apoptosis inducer (if available) [36]
- Incubate plates for 4-16 hours in a humidified CO₂ incubator at 37°C [36].
Apoptosis Staining and Analysis:
- Prepare staining solution containing PE-conjugated Annexin-V and TOPRO-3 in Annexin binding buffer [36].
- Add staining solution to cells and incubate for 15-20 minutes at room temperature protected from light [36].
- Analyze plates using a high-throughput flow cytometer with autosampler capability [36].
- Assess a minimum of 5,000-10,000 events per well to determine apoptosis rates [36].
Data Analysis:
- Identify apoptotic populations: Annexin-Vâº/TOPRO-3â» (early apoptotic) and Annexin-Vâº/TOPRO-3⺠(late apoptotic/necrotic) [36].
- Calculate percentage apoptosis for each compound compared to vehicle controls [36].
- Use statistical analysis (e.g., Z'-factor) to validate assay quality and identify hit compounds [36].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Research Reagents for Neutrophil HTS Apoptosis Assays
| Reagent/Equipment | Function/Application | Specific Examples |
|---|---|---|
| Dextran T500 | Sedimentation of red blood cells during neutrophil isolation | 6% solution in saline [36] [38] |
| Percoll | Density gradient medium for neutrophil purification | 90% stock diluted with PPP [36] |
| Annexin-V Conjugates | Detection of phosphatidylserine exposure on apoptotic cells | PE-conjugated Annexin-V [36] [38] |
| Viability Probes | Discrimination of membrane integrity (live/dead cells) | TOPRO-3 [36] [38] |
| Kinase Inhibitor Libraries | Collection of compounds for screening apoptotic modulators | Published Kinase Inhibitor Set (PKIS) [36] |
| Flow Cytometer with Autosampler | High-throughput analysis of apoptosis in 96-well format | Attune Autosampler [36] |
| Odiparcil | Odiparcil, CAS:137215-12-4, MF:C15H16O6S, MW:324.4 g/mol | Chemical Reagent |
| Ofurace | Ofurace, CAS:58810-48-3, MF:C14H16ClNO3, MW:281.73 g/mol | Chemical Reagent |
Signaling Pathways and Experimental Workflow Visualization
Neutrophil HTS Workflow - This diagram illustrates the complete experimental pipeline from blood collection to hit identification for high-throughput screening of compounds affecting neutrophil apoptosis.
Apoptosis Regulation Network - This signaling pathway diagram shows key regulatory mechanisms of neutrophil apoptosis and how compound screening identifies modulators of this process.
Neutrophils are fundamental effector cells of the innate immune system, and their timely apoptosis is a critical control point for the resolution of inflammation. The core apoptotic machinery in neutrophils is governed by the synergistic relationship between caspase enzyme activation and the dissipation of mitochondrial membrane potential (ΔΨm). Caspase-3 and -7, executioner caspases, are pivotal downstream effectors that irreversibly commit the cell to apoptosis. Their activation is, in turn, often precipitated by an early loss of ΔΨm, a key indicator of mitochondrial permeability and the intrinsic apoptotic pathway. The accurate assessment of these two parameters provides researchers with a powerful toolkit for quantifying apoptotic progression in neutrophil biology, offering invaluable insights for inflammation resolution research and the development of novel therapeutic agents for inflammatory diseases.
Caspase Activity Measurement
Principle of the Caspase-Glo 3/7 Assay
The Caspase-Glo 3/7 Assay is a homogeneous, luminescent method designed for the direct measurement of caspase-3 and -7 activities. The assay is based on a proluminescent substrate containing the DEVD tetrapeptide sequence, which is specific for these executioner caspases. In the presence of active caspase-3/7, the substrate is cleaved, releasing aminoluciferin. This product serves as a substrate for luciferase, generating a stable "glow-type" luminescent signal. The single reagent is optimized to simultaneously lyse cells, provide the substrate, and supply the luciferase enzyme, making the procedure an simple "add-mix-measure" format ideal for high-throughput screening [39] [40].
Detailed Experimental Protocol
Reagent Preparation:
- Equilibrate the Caspase-Glo 3/7 Buffer and the lyophilized Caspase-Glo 3/7 Substrate to room temperature.
- Transfer the entire volume of the buffer into the amber bottle containing the substrate.
- Mix by swirling or inverting the bottle until the substrate is completely dissolved to form the Caspase-Glo 3/7 Reagent.
- The reconstituted reagent can be stored at 4°C for up to 3 days without significant loss of activity. Prolonged storage leads to reduced signal [39].
Cell Assay Procedure:
- Culture neutrophils or other cells of interest in a white-walled multiwell plate. For neutrophil apoptosis assays, typical seeding densities range from 1x10^5 to 5x10^5 cells per well in a 96-well format.
- Apply experimental treatments (e.g., pro-resolving mediators, inflammatory stimuli) for the desired duration.
- Remove the culture media from all wells.
- Add a volume of Caspase-Glo 3/7 Reagent equal to the volume of medium remaining in the well (typically a 1:1 ratio). For consistency, adding 100 µL of reagent directly to 100 µL of medium-containing cells is a common practice [39] [41].
- Seal the plate and mix contents gently using a plate shaker for 30 seconds.
- Incubate the plate at room temperature for 1 to 3 hours (optimize incubation time for specific cell type and basal activity).
- Measure the luminescence of each sample in a plate-reading luminometer following the manufacturer's instructions [39].
Data Normalization and Analysis: Luminescence output, which is proportional to caspase-3/7 activity, should be normalized to total protein concentration or cell number to account for variations in well-to-well seeding. Total protein concentration can be measured using assays like the Qubit Protein Assay Kit [39]. Data are typically presented as fold-change relative to an untreated control.
Table 1: Troubleshooting Guide for Caspase-Glo 3/7 Assay
| Issue | Potential Cause | Recommended Solution |
|---|---|---|
| Low Signal | Incomplete cell lysis | Ensure reagent is thoroughly mixed. Verify reagent composition is correct. |
| Short incubation time | Extend the incubation time (e.g., up to 3 hours). | |
| Inactive caspase-3/7 | Include a positive control (e.g., cells treated with a known apoptosis inducer). | |
| High Background | Contaminated reagents | Prepare fresh reagent using sterile techniques. |
| Too long incubation | Shorten the incubation time within the linear range of the assay. | |
| High Variability | Inconsistent pipetting | Use calibrated multichannel pipettes or an automated pipetting station. |
| Uneven cell seeding | Ensure a homogeneous cell suspension during seeding. |
Mitochondrial Membrane Potential (ΔΨm) Measurement
Principle of ΔΨm Assessment
The mitochondrial membrane potential (ΔΨm), typically -150 to -180 mV in healthy cells, is a key indicator of mitochondrial health and a critical early event in the intrinsic apoptosis pathway. A decrease in ΔΨm (depolarization) precedes caspase activation and DNA fragmentation. Several fluorescent probes are available to track these changes, each with distinct mechanisms and limitations. Common dyes like JC-1, TMRM, and MitoTracker Red FM are widely used but can suffer from issues like signal saturation, non-specific staining, and an inability to detect subtle changes in ΔΨm [42]. Novel probes like LDS 698 offer high sensitivity for tracking kinetic changes, while JC-10 allows for ratiometric measurement in microplate formats [42] [43].
Detailed Experimental Protocol: JC-10 Assay for Microplates
Reagent and Sample Preparation:
- Culture cells (e.g., A2058, HT144) in a 96-well plate and treat them with the compound of interest (e.g., I3A) for the desired period (e.g., 24 hours) [43].
- Reconstitute the JC-10 dye according to the manufacturer's instructions (e.g., Abcam JC-10 Mitochondrial Membrane Potential Assay Kit) to create the dye-loading solution.
Staining and Measurement:
- Add 50 µL of JC-10 dye-loading solution to each well.
- Incubate the plate in a CO₂ incubator at 37°C for 30 minutes.
- After incubation, add 50 µL of Assay Buffer B (provided in the kit) to each well.
- Immediately measure the fluorescence intensities using a microplate reader with appropriate filter sets:
- J-aggregates (healthy, high ΔΨm): Excitation 490 nm / Emission 590 nm.
- Monomeric form (depolarized, low ΔΨm): Excitation 490 nm / Emission 525 nm [43].
Data Analysis: The ratio of fluorescence at 590 nm (aggregates) to that at 525 nm (monomers) is calculated. A decrease in this ratio indicates a loss of ΔΨm (mitochondrial depolarization).
Protocol for LDS 698 Staining and Analysis
Staining Procedure:
- Plate cells on glass coverslips or in a multi-well plate.
- Load cells with 100-500 nM LDS 698 dye diluted in culture medium.
- Incubate for 30 minutes at 37°C in a CO₂ incubator.
- Replace the dye-containing medium with fresh pre-warmed medium or PBS.
- For co-staining, other organelle-specific trackers (e.g., MitoTracker Green) can be added during the final 15 minutes of the LDS 698 incubation period [42].
Detection and Analysis:
- Microscopy: Image cells using a fluorescence microscope with a filter set suitable for LDS 698 (Ex/Em: ~460/580-700 nm) [42].
- Flow Cytometry: Analyze 10,000 or more events per sample using a flow cytometer equipped with a blue laser (488 nm) and a detector for red fluorescence (e.g., PE-Texas Red channel) [42].
Table 2: Comparison of ΔΨm-Sensitive Fluorescent Probes
| Probe | Detection Method | Key Advantages | Key Limitations |
|---|---|---|---|
| JC-1 / JC-10 | Ratiometric (Em: 525 nm vs 590 nm) | Ratiometric measurement minimizes artifacts; suitable for microplate readers. | Can form non-specific aggregates; kinetic measurements are challenging [42]. |
| TMRM | Intensity-based | Reversible binding; can be used for kinetic studies. | Fluorescence intensity saturates at high concentrations/dye loading [42]. |
| MitoTracker Red FM | Intensity-based | Covalently binds to thiol groups, allowing fixed-cell analysis. | Not reversible; does not reflect subsequent changes in ΔΨm after fixation [42]. |
| LDS 698 | Intensity-based | High sensitivity to subtle changes; low background; good for kinetics. | Intensity-based, so requires careful loading and controls for cell number/dye uptake [42]. |
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for Apoptosis Assays
| Item | Function / Application | Example Product / Assay |
|---|---|---|
| Caspase-Glo 3/7 Assay | Homogeneous, luminescent measurement of caspase-3/7 activity in cell cultures. | Promega (G8090, G8091, etc.) [39] [40] |
| JC-10 Dye | Ratiometric fluorescent probe for measuring ΔΨm in microplate formats. | Abcam Mitochondrial Membrane Potential Assay Kit [43] |
| LDS 698 Dye | Highly sensitive fluorescent probe for tracking subtle and kinetic ΔΨm changes in live cells. | Exiton (Code 06980) [42] |
| MitoTracker Probes | Cell-permeant dyes that stain live-cell mitochondria; some are ΔΨm-dependent. | MitoTracker Red FM, MitoTracker Green (Invitrogen) [42] |
| Plate-Reading Luminometer | Instrument for detecting luminescent signals from multiwell plates. | GloMax-Multi Detection System [41] |
| Fluorescence Microplate Reader | Instrument for detecting fluorescence intensities and ratios in multiwell plates. | Standard microplate reader with 490 nm excitation and 525/590 nm emission [43] |
| Flow Cytometer | Instrument for analyzing fluorescence intensity of individual cells. | Flow cytometer with blue (488 nm) and red lasers [42] |
| Oglemilast | Oglemilast, CAS:778576-62-8, MF:C20H13Cl2F2N3O5S, MW:516.3 g/mol | Chemical Reagent |
| Okicenone | Okicenone, CAS:137018-54-3, MF:C15H14O4, MW:258.27 g/mol | Chemical Reagent |
Visualizing the Workflow and Signaling Pathways
Neutrophil Apoptosis Signaling Pathway
Diagram Title: Key Intrinsic Apoptosis Pathway in Neutrophils
Integrated Experimental Workflow
Diagram Title: Integrated Workflow for Apoptosis Assessment
Within the broader scope of investigating neutrophil apoptosis assays for inflammation resolution research, the accurate detection of morphological and biochemical markers of cell death is paramount. Neutrophils, as primary effector cells of the innate immune system, undergo constitutive apoptosis to facilitate the resolution of inflammation, and their timely clearance is critical for preventing chronic inflammatory states and tissue damage, such as in kidney diseases [3]. Among the various techniques available, the Terminal deoxynucleotidyl transferase dUTP nick end labeling (TUNEL) assay and DNA fragmentation analysis stand out as essential methods for identifying the hallmark DNA breakdown that occurs during the late stages of programmed cell death. This application note provides a detailed overview of the TUNEL assay principle, its integration within neutrophil apoptosis research, and structured protocols to guide scientists in applying these techniques effectively.
Principle of the TUNEL Assay
The TUNEL assay is a widely used technique for the in situ detection of DNA fragmentation, a key biochemical event in the late phase of apoptosis [44] [45]. During apoptosis, endogenous endonucleases are activated, cleaving genomic DNA into fragments and generating free 3'-hydroxyl (3'-OH) termini within the DNA strands. The TUNEL assay leverages the enzyme Terminal deoxynucleotidyl Transferase (TdT), which catalyzes the template-independent addition of deoxynucleotides to the 3'-OH ends of these fragmented DNA molecules [45]. The incorporated nucleotides are pre-labeled with tags such as fluorophores (e.g., fluorescein-dUTP), biotin-dUTP, or other modified nucleotides (e.g., BrdUTP, EdUTP), allowing subsequent detection via fluorescence microscopy, flow cytometry, or colorimetric methods [44] [46] [45].
A significant advancement in TUNEL technology is the development of click chemistry-based assays, such as the Click-iT TUNEL assays. These assays incorporate an alkyne-modified dUTP (EdUTP) into DNA breaks, which is later detected via a highly specific copper-catalyzed azide-alkyne cycloaddition reaction with a fluorescent or colorimetric azide tag [44]. This two-step method offers enhanced specificity and sensitivity, detecting a higher percentage of apoptotic cells compared to traditional one-step incorporation methods [44].
Figure 1: TUNEL Assay Workflow and Detection Principle. The assay detects DNA fragmentation resulting from apoptosis. Terminal deoxynucleotidyl transferase (TdT) enzyme incorporates labeled dUTP at 3'-OH ends of fragmented DNA, enabling detection through multiple platforms [44] [45].
Applications in Neutrophil Apoptosis Research
The TUNEL assay is particularly valuable in neutrophil research for quantifying spontaneous and induced apoptosis, a process critical for inflammation resolution. Delayed neutrophil apoptosis is a feature of chronic inflammatory states, including type 2 diabetes (T2DM), where peripheral blood neutrophils exhibit significantly reduced spontaneous apoptosis compared to those from healthy individuals (67.3% ± 3.9% vs. 85.3% ± 3.1% at 12 hours) [47]. This delay is associated with reduced caspase-3 and caspase-8 activity and is mediated through the advanced glycation endproducts (AGE) and RAGE ligand/receptor interaction [47]. Furthermore, specialized pro-resolving mediators (SPMs), endogenous lipid mediators that actively promote inflammation resolution, have been identified as key regulators of neutrophil apoptosis. SPMs facilitate the restoration of tissue homeostasis by inducing neutrophil programmed cell death and promoting macrophage-mediated efferocytosis, highlighting their therapeutic potential in neutrophil-mediated inflammatory kidney diseases [3].
Table 1: Key Research Findings on Neutrophil Apoptosis Using DNA Fragmentation Analysis
| Research Context | Key Finding | Assay Used | Quantitative Result | Biological Implication |
|---|---|---|---|---|
| Spontaneous Apoptosis in T2DM [47] | Delayed spontaneous PMN apoptosis in T2DM subjects. | Flow Cytometry (TUNEL) | Apoptosis at 12h: Healthy: 85.3% ± 3.1%; T2DM: 67.3% ± 3.9% | Suggests a mechanism for chronic inflammation in diabetes. |
| Caspase Inhibition [48] | Pan-caspase inhibitor Q-VD-OPh prevents apoptosis. | Flow Cytometry (TUNEL) | Markedly suppressed TUNEL positivity for ≥5 days. | Confirms caspase-dependence of constitutive neutrophil apoptosis. |
| Resolution Pharmacology [3] | SPMs promote neutrophil apoptosis and efferocytosis. | Not Specified (Review) | N/A | SPMs are novel therapeutic targets for resolving inflammation. |
Comparative Analysis of TUNEL Methodologies
Choosing the appropriate TUNEL methodology depends on the experimental requirements, including the sample type, desired readout, and need for multiplexing. The classic methods involve direct fluorescent labeling, indirect labeling with biotin or haptens, or modern click chemistry-based approaches.
Table 2: Comparison of Common TUNEL Assay Methodologies
| Methodology | Principle | Detection | Advantages | Disadvantages | Compatibility with Neutrophil Assays |
|---|---|---|---|---|---|
| Direct Fluorescence [45] | TdT incorporates dye-conjugated dUTP (e.g., FITC-dUTP). | Fluorescence (Microscopy, Flow Cytometry) | Fast, minimal steps. | Limited signal amplification. | Suitable for flow cytometric analysis of isolated neutrophils [47]. |
| Indirect (Biotin-dUTP) [46] [45] | TdT incorporates biotin-dUTP; detected with enzyme-streptavidin conjugates. | Colorimetric (e.g., DAB/HRP) or Fluorescence. | Signal amplification, stable colorimetric signal. | More steps; requires endogenous peroxidase/biotin blocking. | Ideal for histological analysis of neutrophils in tissue sections [49]. |
| Click-iT TUNEL [44] | TdT incorporates EdUTP; detected via click reaction with azide-dye. | Fluorescence or Colorimetric. | High specificity and sensitivity; flexible labeling. | Copper catalyst may affect some fluorescent proteins. | Click-iT Plus version is optimized for multiplexing with fluorescent proteins and phalloidin. |
| BrdU-based TUNEL [44] [45] | TdT incorporates BrdUTP; detected with anti-BrdU antibody. | Fluorescence or Colorimetric. | Bright signal, efficient incorporation. | Additional antibody incubation step. | Compatible with imaging and flow cytometry (APO-BrdU TUNEL assay) [44]. |
Detailed Experimental Protocols
Protocol 1: TUNEL Staining for Formalin-Fixed, Paraffin-Embedded (FFPE) Tissues
This protocol is adapted for FFPE tissue sections, such as those from studies investigating neutrophil infiltration in kidney or liver disease models [50] [49].
I. Sample Preparation and Deparaffinization
- Baking: Bake slides at 60°C for 20 minutes to melt the paraffin.
- Deparaffinization and Rehydration: Immerse slides in a series of solutions as follows [49] [46]:
- Xylenes: 3 changes, 5 minutes each.
- 100% Ethanol: 2 changes, 1 minute each.
- 95% Ethanol: 1 minute.
- 85% Ethanol: 1 minute.
- 70% Ethanol: 1 minute.
- Distilled Water: 3 minutes.
- Phosphate-Buffered Saline with 0.05% Tween (PBS-T): 5 minutes.
II. Antigen Retrieval and Permeabilization
- Proteinase K Digestion: Apply 1X Proteinase K solution (e.g., 20 µg/mL) to cover the tissue and incubate for 20 minutes at 37°C in a humidified chamber [49]. Note: Recent research indicates that Proteinase K can degrade protein antigenicity, and pressure cooker-based antigen retrieval is a compatible alternative for multiplexing with protein biomarkers [50].
- Washing: Rinse slides with PBS-T, 2 changes for 2 minutes each.
III. TUNEL Reaction
- Endogenous Peroxidase Blocking (for chromogenic HRP-DAB detection): Incubate slides with 2% hydrogen peroxide for 5 minutes at room temperature to quench endogenous peroxidases. Wash 2 x 5 minutes with PBS [46].
- Equilibration: Incubate slides with TdT Equilibration Buffer for 10 minutes at room temperature.
- Labeling Reaction: Prepare the TdT Reaction Cocktail (e.g., containing TdT reaction buffer, TdT enzyme, and biotin-dUTP or other modified nucleotides). Remove the equilibration buffer and apply the cocktail to the tissues. Incubate for 60 minutes at 37°C in a humidified chamber [46].
- Reaction Stop: Stop the reaction by immersing slides in 2X SSC buffer for 15 minutes.
- Washing: Wash slides 2 x 10 minutes in PBS with 3% BSA.
IV. Signal Detection and Visualization
- HRP-Conjugate Incubation: For biotin-dUTP based kits, apply HRP-streptavidin solution and incubate for 30 minutes at room temperature. Wash 2 x 5 minutes in PBS with 3% BSA [46].
- Chromogenic Development: Apply DAB staining solution and monitor color development (typically 1-10 minutes). Stop the reaction by rinsing with distilled water or PBS.
- Counterstaining and Mounting: Counterstain with hematoxylin for nuclear context, dehydrate, clear, and mount with a permanent mounting medium [49].
Figure 2: TUNEL Staining Workflow for FFPE Tissues. The protocol involves sample preparation, DNA end labeling, and detection. Including DNase-treated and no-TdT controls is essential for validation [49] [46].
Protocol 2: DNA Fragmentation Analysis by Agarose Gel Electrophoresis
This protocol provides a semi-quantitative, gel-based method to detect the characteristic "DNA ladder" pattern of internucleosomal cleavage in apoptotic cells [51].
- Cell Lysis: Pellet approximately 1-5 x 10^6 cells. Lyse the cell pellet in 0.5 mL of detergent buffer (10 mM Tris pH 7.4, 5 mM EDTA, 0.2% Triton X-100) by vortexing. Incubate on ice for 30 minutes [51].
- Separation of Fragmented DNA: Centrifuge the lysate at 27,000 x g for 30 minutes at 4°C. The supernatant contains the small, fragmented DNA, while the pellet contains intact chromatin and high-molecular-weight DNA.
- DNA Precipitation: Transfer the supernatant to a new tube. Add 0.5 mL of ice-cold 5 M NaCl and vortex. Add 600 µL of ethanol and 150 µL of 3 M sodium acetate (pH 5.2), mix, and incubate at -80°C for 1 hour. Centrifuge at 20,000 x g for 20 minutes to pellet the DNA. Carefully discard the supernatant [51].
- DNA Purification: Resuspend the DNA pellet in 400 µL of extraction buffer (10 mM Tris, 5 mM EDTA). Add DNase-free RNase (e.g., 2 µL of 10 mg/mL) and incubate for 5 hours at 37°C. Then add Proteinase K (e.g., 25 µL of 20 mg/mL) and incubate overnight at 65°C. Extract DNA with phenol/chloroform/isoamyl alcohol and precipitate with ethanol. Air-dry the final pellet [51].
- Gel Electrophoresis: Resuspend the DNA in Tris-acetate-EDTA (TAE) buffer with loading dye. Separate the DNA on a 2% agarose gel containing a DNA intercalating dye (e.g., ethidium bromide or a safer alternative). Visualize the DNA ladder pattern under UV light. A ladder of DNA fragments in multiples of ~180-200 base pairs indicates apoptosis, as opposed to the smeared pattern seen in necrosis [51].
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents and Kits for TUNEL and DNA Fragmentation Analysis
| Reagent / Kit | Function / Principle | Key Applications in Neutrophil Research | Example Product Types |
|---|---|---|---|
| Click-iT TUNEL Assays [44] | Utilizes EdUTP incorporation and click chemistry for detection with fluorescent or colorimetric azides. | High-sensitivity apoptosis detection in tissue sections and cultured cells; compatible with multiplexed imaging. | Click-iT Plus TUNEL Assay (for tissue), Click-iT TUNEL Alexa Fluor Imaging Assay (for cells). |
| APO-BrdU TUNEL Assay [44] | Incorporates BrdUTP, detected with an Alexa Fluor 488-labeled anti-BrdU antibody. Often includes PI for total DNA content. | Two-color analysis for flow cytometry, enabling correlation of apoptosis with cell cycle stage. | APO-BrdU TUNEL Assay Kit. |
| HRP-DAB TUNEL Kits [49] [45] | Biotin-dUTP incorporation detected with streptavidin-HRP and developed with DAB substrate for a brown precipitate. | Chromogenic detection of apoptotic neutrophils in FFPE tissue sections for brightfield microscopy. | Colorimetric IHC Detection Kits. |
| DNase I [49] [46] | Enzyme that introduces double-strand breaks in DNA, creating a positive control for TUNEL staining. | Validation of TUNEL assay performance on control tissue or cell slides. | Recombinant DNase I. |
| Proteinase K [49] [46] | Proteolytic enzyme used for antigen retrieval and permeabilization of FFPE tissue sections. | Unmasking DNA breaks in fixed tissues; optimization of digestion time is critical. | 20 µg/mL working solution. |
| Pan-Caspase Inhibitor (Q-VD-OPh) [48] | Irreversible, non-toxic caspase inhibitor used to confirm the caspase-dependent pathway of apoptosis. | Experimental control to suppress constitutive neutrophil apoptosis in functional assays. | Cell culture reagent, typically used at 10 µM. |
| OL-135 | OL-135|FAAH Inhibitor|For Research Use | Bench Chemicals | |
| Mixanpril | Mixanpril|Dual ACE/NEP Inhibitor|RUO | Mixanpril is a dual ACE and NEP inhibitor for cardiovascular research. This product is for Research Use Only (RUO) and not for human or veterinary diagnosis or therapy. | Bench Chemicals |
Integration with Spatial Proteomics and Concluding Remarks
A critical recent development is the harmonization of TUNEL with modern spatial proteomic methods like Multiplexed Iterative Labeling by Antibody Neodeposition (MILAN) and Cyclic Immunofluorescence (CycIF). A key finding is that the traditional use of Proteinase K for antigen retrieval in TUNEL consistently reduces or abrogates protein antigenicity, preventing robust multiplexing. Replacing Proteinase K with pressure cooker-based retrieval quantitatively preserves TUNEL signal without compromising protein antigenicity, enabling rich spatial contextualization of cell death within complex tissues [50]. This integration allows researchers to simultaneously map dozens of protein biomarkers alongside apoptotic cells on a single tissue section, dramatically enhancing the ability to delineate cell-type-specific death and its tissue microenvironment in inflammation resolution research.
In conclusion, the TUNEL assay and DNA fragmentation analysis remain cornerstone techniques for detecting apoptotic neutrophils. The choice of methodology, from traditional kits to advanced click-chemistry and multiplex-compatible protocols, should be guided by the specific research question. When applied with appropriate controls and optimized protocols, these powerful tools provide invaluable insights into the mechanisms of inflammation resolution and the role of neutrophil apoptosis in health and disease.
The resolution of inflammation is an active process essential for restoring tissue homeostasis, and the programmed cell death of neutrophil granulocytes represents a critical control point within this cascade [1]. Neutrophils are the first responders to infection or tissue injury, but their prolonged survival is linked to tissue damage and chronic inflammatory pathologies [2]. The pharmacological induction of neutrophil apoptosis has therefore emerged as a promising therapeutic strategy for promoting inflammation resolution [52]. Advancing this strategy requires robust and predictive in vivo models. The zebrafish (Danio rerio) tailfin injury model has established itself as a powerful system for the real-time study of neutrophilic inflammation and its resolution, providing direct insights into mammalian inflammatory processes, including those in the lung [53]. This application note details the protocols, quantitative outcomes, and molecular pathways uncovered through this model, positioning it as an indispensable tool for preclinical research into neutrophil apoptosis and the development of anti-inflammatory therapeutics.
Quantitative Data from the Zebrafish Tailfin Injury Model
The zebrafish tailfin injury model induces a sterile, neutrophilic inflammation that resolves spontaneously. Key quantitative data from this model are summarized in the tables below.
Table 1: Kinetics of Neutrophil Recruitment and Resolution in the Zebrafish Tailfin Injury Model
| Time Post-Injury | Neutrophil Number at Site | Key Biological Process |
|---|---|---|
| 4-6 hours | Peak (~40-50 cells) [52] | Maximum neutrophil recruitment |
| 24 hours | ~50% reduction from peak [52] | Active inflammation resolution |
| 24-48 hours | Return to near-baseline levels [52] | Completion of resolution |
Table 2: Pharmacological Modulation of Neutrophil Apoptosis and Resolution
| Pharmacological Agent | Effect on Neutrophil Apoptosis | Impact on Resolution (Neutrophil Numbers at 24h) |
|---|---|---|
| zVD.fmk (pan-caspase inhibitor) | Inhibits | No reduction (0.5 ± 8.1%) [52] |
| LPS (bacterial lipopolysaccharide) | Inhibits | Delayed resolution [52] |
| dbcAMP (stable cAMP analog) | Inhibits | Delayed resolution [52] |
| Roscovitine (CDK inhibitor) | Induces | Accelerated resolution [52] |
| Pyocyanin (bacterial toxin) | Induces | Accelerated resolution [52] |
Experimental Protocols
Protocol 1: Zebrafish Tailfin Injury and Inflammation Assay
This protocol is used to induce and quantify sterile inflammation in zebrafish larvae [52].
Materials:
- Transgenic zebrafish larvae (e.g., Tg(mpx:GFP) for neutrophil labeling) at 3-5 days post-fertilization (dpf)
- Tricaine methanesulfonate (MS-222) for anesthesia
- Sterile microdissection scalpel
- 96-well plates
- E3 embryo medium
- Fluorescence stereomicroscope
Procedure:
- Anesthetization: Immerse larvae in E3 medium containing 0.017% Tricaine [52].
- Tailfin Transection: Under microscopic guidance, perform a complete transection of the tailfin using a sterile microdissection scalpel [52].
- Recovery: Allow larvae to recover in fresh E3 medium at 28.5°C for a defined period (e.g., 4-6 hours to peak inflammation) [52].
- Assessment of Inflammation: Re-anesthetize larvae and image the injury site using a fluorescence stereomicroscope with a GFP filter set. Manually count the number of GFP-positive neutrophils at the wound site [52].
- Resolution Phase: For resolution studies, array larvae at 4 hours post-injury into 96-well plates and maintain at 28.5°C for up to 24-48 hours before final neutrophil counting [52].
Protocol 2: Pharmacological Modulation of Neutrophil Apoptosis
This protocol details how to test the effects of chemical compounds on inflammation resolution in the zebrafish model [52].
Materials:
- Test compounds (e.g., caspase inhibitors, pro-apoptotic agents)
- Dimethyl sulfoxide (DMSO) as a solvent
- 96-well plates
- E3 embryo medium
Procedure:
- Compound Preparation: Dissolve test compounds in DMSO to create stock solutions. Dilute stocks in E3 medium immediately before use, ensuring the final DMSO concentration does not exceed 1% (v/v). Include vehicle control groups (1% DMSO in E3) [52].
- Compound Administration: At a selected time post-injury (e.g., 4 hours), transfer larvae with a confirmed inflammatory response into the compound solutions within 96-well plates (typically 3-5 larvae per well) [52].
- Incubation and Scoring: Incubate plates at 28.5°C for a defined period (e.g., 20 hours). Re-anesthetize larvae and score neutrophil numbers at the inflammation site by fluorescence microscopy [52].
- Apoptosis Confirmation (Optional): For advanced analysis, fixed larvae can be co-stained using TUNEL assay (for apoptotic DNA fragmentation) and myeloperoxidase activity staining (TSA) to confirm neutrophil-specific apoptosis [52].
Signaling Pathways in Neutrophil Apoptosis
The intrinsic (mitochondrial) pathway is the central regulator of spontaneous neutrophil apoptosis. The balance between pro-survival and pro-apoptotic Bcl-2 family proteins determines neutrophil fate.
Diagram 1: Molecular regulation of neutrophil apoptosis and resolution. Key pathways identified in mammalian and zebrafish models show convergence on mitochondrial integrity. Pro-survival signals stabilize Mcl-1, while pro-apoptotic stimuli activate Bim/Noxa, triggering caspase-9-dependent apoptosis [54] [1] [55]. Macrophages then clear apoptotic cells [56].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Neutrophil Apoptosis and Resolution Research
| Reagent / Model | Function / Application | Key Experimental Insight |
|---|---|---|
| Tg(mpx:GFP) Zebrafish | In vivo, real-time visualization and quantification of neutrophils [52]. | Enables live imaging of neutrophil recruitment, apoptosis, and efferocytosis. |
| Caspase Inhibitors (e.g., zVD.fmk) | Pharmacological inhibition of neutrophil apoptosis [52]. | Delays inflammation resolution, confirming apoptosis as a key resolution mechanism. |
| Pro-apoptotic Compounds (e.g., Roscovitine) | Pharmacological induction of neutrophil apoptosis [52]. | Accelerates inflammation resolution, validating a therapeutic approach. |
| Hoxb8 Progenitor System | Generation of limitless, genetically tractable mouse neutrophils in vitro [54]. | Identified essential, synergistic pro-apoptotic role of Bim and Noxa proteins. |
| HAX1 Knockout Models | Study of severe congenital neutropenia gene in neutrophil maturation/survival [55]. | HAX1 inhibits mitochondrial apoptosis via BCL-2 family and TLR2-PU.1 signaling. |
| Macrophage ScRNAseq | High-resolution mapping of immune cell states during injury [56]. | Revealed sequential anti-inflammatory (Glucocorticoid→IL-10→IL-4) activation in macrophages. |
| ML-030 | ML-030, MF:C20H20N4O4S, MW:412.5 g/mol | Chemical Reagent |
| Omaciclovir | Omaciclovir, CAS:124265-89-0, MF:C10H15N5O3, MW:253.26 g/mol | Chemical Reagent |
Workflow: From In Vivo Screening to Mechanistic Validation
A combined approach using zebrafish and mammalian systems provides a powerful pipeline for drug discovery.
Diagram 2: Integrated drug discovery workflow. The pipeline begins with high-throughput screening in zebrafish, followed by mechanistic studies and validation in mammalian systems [52] [54] [57].
Optimizing Assay Precision and Navigating Common Technical Challenges
In inflammation resolution research, neutrophil apoptosis assays provide critical insights into the mechanisms governing the termination of immune responses. The validity of these assays is highly dependent on neutrophil viability and phenotypic stability, which are exceptionally vulnerable to pre-analytical variables. This Application Note details evidence-based protocols for blood collection and initial processing to minimize ex vivo neutrophil activation, thereby preserving the physiological relevance of apoptosis measurements for drug development and basic research.
The Impact of Pre-Analytical Variables on Neutrophil Phenotype
Anticoagulant Choice
The selection of anticoagulant is a primary consideration, as it constitutes the initial microenvironment for the blood sample. Research indicates that common anticoagulants exhibit minor differences in their impact on isolated polymorphonuclear neutrophils (PMNs).
- Heparin, EDTA, and Citrate: A comparative study found that these three major anticoagulants had no significant differential effects on PMN counts, respiratory burst activity, or the potential for activation following isolation. All three can be used to obtain blood samples suitable for PMN isolation [58].
Processing Temperature and Timelines
Temperature control during sample handling is critical for maintaining neutrophil function and stability.
- Storing Temperature: Isolated PMNs maintained at 37°C demonstrated a significantly higher respiratory burst activity compared to those stored at 4°C. Storing at 22°C also led to a significant decrease in PMN counts after three hours [58].
- Processing Delays: The time between blood draw and processing is a major driver of neutrophil activation. A strong positive correlation exists between the number of manipulation steps (and the time they take) and the levels of surface activation markers [12]. Furthermore, the respiratory burst activity of isolated PMNs is significantly reduced after 3- and 7-hour storing periods, even under optimal temperature conditions [58].
Table 1: Effects of Processing Time on Isolated Neutrophil Viability and Function
| Time Post-Isolation | Cell Count | Respiratory Burst Activity | Key Chemokine Changes |
|---|---|---|---|
| 1 Hour | Stable | No significant change | Relatively constant |
| 3 Hours | ~50% decrease | Significantly reduced | VEGF-A, IL-8, MIP-1β levels rise |
| 7 Hours | Stable at reduced level | Significantly reduced | VEGF-A, IL-8, MIP-1β remain elevated; IL-16 decreases |
Staining and Handling Techniques
The method of staining and the steps taken prior to red blood cell (RBC) lysis significantly influence the accuracy of neutrophil phenotyping.
- Antibody Removal Before Lysis: Staining whole blood at 4°C and removing unbound antibodies with a wash step prior to fixation and RBC lysis (as opposed to lysing in the presence of antibodies) minimizes nonspecific antibody binding. This is likely due to preventing cationic neutrophil proteins from interacting with antibody constructs during the lysis process [12].
- Minimizing Manipulation: Protocols with fewer manipulation steps (e.g., one-step fixation/RBC lysis of whole blood) result in significantly lower levels of neutrophil activation and degranulation, as measured by surface markers like CD11b and CD66b, compared to methods involving density gradient centrifugation [12].
Optimized Experimental Protocols
Protocol 1: Blood Collection for Neutrophil Apoptosis Studies
Objective: To collect peripheral blood with minimal ex vivo neutrophil activation. Reagents & Materials:
- Sterile blood collection system (21G butterfly needle or 18G venous catheter)
- Collection tubes containing heparin, EDTA, or sodium citrate
- Pre-chilled centrifuge
Procedure:
- Collect venous blood using a technique that minimizes shear stress, such as free flow into a sample vessel rather than aspiration with a syringe, as syringe use may lead to a more prominent decrease in respiratory burst over time [58].
- Gently invert collection tubes 8-10 times for immediate mixing with anticoagulant.
- Process whole blood within 3 hours of collection [12]. Keep samples at room temperature (22°C) prior to processing unless otherwise required by a specific protocol.
Protocol 2: Whole Blood Staining for Flow Cytometry
Objective: To accurately phenotype neutrophil surface markers with minimal activation-induced artifacts. Reagents & Materials:
- Fluorescently-labeled antibodies (e.g., anti-CD11b, CD66b, CD62L)
- One-step Fixation/RBC Lysis Buffer
- Flow cytometry staining buffer (DPBS with protein)
- Pre-chilled centrifuge
Procedure:
- Aliquot 100 µL of fresh whole blood into a FACS tube.
- Add predetermined titrated amounts of fluorochrome-conjugated antibodies.
- Incubate for 30 minutes at 4°C in the dark [12].
- Critical Step: Add 2-3 mL of cold staining buffer and centrifuge (e.g., 500 x g, 5 min, 4°C). Discard the supernatant to remove unbound antibodies [12].
- Add 1-2 mL of One-step Fixation/RBC Lysis Buffer. Vortex gently and incubate for 15 minutes at room temperature in the dark.
- Centrifuge, wash cells once with staining buffer, and resuspend in buffer for immediate acquisition on a flow cytometer.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Neutrophil Isolation and Phenotyping
| Reagent/Material | Function | Example & Notes |
|---|---|---|
| One-Step Fixation/RBC Lysis Buffer | Simultaneously fixes leukocytes and lyses red blood cells, minimizing processing steps and activation. | Commercial kits (e.g., BD Pharm Lyse). Use after removing unbound antibodies to reduce nonspecific binding [12]. |
| Heparin/EDTA/Citrate Tubes | Prevents blood coagulation during collection. | All three are suitable. Choice can be harmonized with other planned assays [58]. |
| Anti-human CD16 Antibody | Identifies mature neutrophils during flow cytometry gating. | Clone: 3G8. Used with CD15, CD11b, CD66b for precise identification [12]. |
| Anti-human CD11b Antibody | Marker of neutrophil degranulation; surface levels increase upon activation. | Clone: ICRF44. Key marker for assessing pre-analytical activation [12]. |
| Anti-human CD62L Antibody | Marker of neutrophil activation; surface levels decrease upon activation. | Clone: DREG-56. Shedding indicates pre-analytical activation [12]. |
Visualizing the Optimal Workflow
The following diagram outlines the standardized protocol to minimize neutrophil pre-activation, from blood draw to analysis.
The reliability of neutrophil apoptosis data in the context of inflammation resolution is fundamentally rooted in sample quality. By adhering to protocols that prioritize limited processing time, controlled temperatures, and minimalistic staining techniques—such as the critical wash step before RBC lysis—researchers can significantly reduce technical noise introduced by pre-analytical activation. These standardized methods ensure that observed phenotypes and functional readouts, such as the progression into apoptosis, truly reflect the in vivo state, thereby enhancing the translational value of research in drug development.
Standardizing Isolation Protocols to Preserve Native Neutrophil Phenotype
The study of neutrophil apoptosis is fundamental to inflammation resolution research, as the timely programmed cell death of neutrophils and their subsequent clearance by macrophages is a critical turning point between inflammatory progression and resolution [3]. However, investigating this process ex vivo presents a significant challenge due to the sensitive nature of neutrophil biology. Neutrophils are short-lived, terminally differentiated cells that are exquisitely sensitive to external cues, making them prone to activation during blood collection and isolation procedures [59]. This activation can profoundly alter their native phenotype and skew apoptosis assays, potentially leading to unreliable research data and difficulties in inter-study comparisons. The choice of isolation method directly impacts experimental outcomes, particularly for sensitive assays measuring apoptosis and other functional responses [59]. This application note provides detailed protocols and data-driven recommendations for standardizing neutrophil isolation to preserve native phenotypes, specifically within the context of neutrophil apoptosis research.
The Critical Impact of Isolation Method on Neutrophil Biology
The isolation process itself represents a significant source of experimental variability in neutrophil research. Neutrophils possess a diverse arsenal of pre-formed effector molecules stored in granules, which can be readily released upon activation [60]. Furthermore, they are equipped with various immune receptors, including Toll-like receptors (TLRs), Fc gamma receptors (FcγRs), and C-type lectin receptors (CLRs), which allow them to sense and respond to isolation-induced stress [61].
Recent comparative studies have systematically evaluated how different isolation methods affect key neutrophil parameters. The findings demonstrate that isolation techniques requiring red blood cell (RBC) lysis steps, particularly those involving hypertonic lysis buffers, consistently result in higher baseline activation of neutrophils [59]. This pre-activation not only alters surface marker expression but also diminishes neutrophil responsiveness to subtle physiological stimuli in subsequent functional assays. Such manipulations are particularly problematic for apoptosis studies, as the isolation method can inadvertently accelerate or delay spontaneous apoptosis, thereby obscuring true pharmacological or disease-relevant effects [62].
Comparative Analysis of Neutrophil Isolation Methods
Different isolation methods exert distinct effects on neutrophil yield, purity, and activation state. The table below summarizes the quantitative performance characteristics of five common isolation techniques, as determined by flow cytometric analysis.
Table 1: Performance Comparison of Neutrophil Isolation Methods
| Isolation Method | Relative Yield | Purity | Baseline Activation | Key Advantages | Key Limitations |
|---|---|---|---|---|---|
| Negative Immunomagnetic Selection (Miltenyi) | High | >95% | Low | Minimal manipulation; resembles untouched neutrophils in blood; high responsiveness to mild stimuli [59]. | Higher cost; requires specialized equipment. |
| Negative Immunomagnetic Selection (StemCell) | High | >95% | Low | Minimal manipulation; resembles untouched neutrophils in blood; high responsiveness to mild stimuli [59]. | Higher cost; requires specialized equipment. |
| Density Gradient (Histopaque/Percoll) | Moderate | >95% | Moderate | Good yield and purity; no RBC lysis required [59]. | Multiple centrifugation steps. |
| Density Gradient (Polymorphprep + RBC Lysis) | Moderate | >95% | High | Established, common protocol. | Hypertonic RBC lysis causes elevated activation; reduced responsiveness [59]. |
| Dextran Sedimentation/Ficoll + RBC Lysis | Moderate | >95% | High | Cost-effective. | Sedimentation time lengthy; RBC lysis causes elevated activation [59]. |
Impact on Apoptosis Assays
The choice of isolation method directly influences the outcomes of neutrophil apoptosis assays. Neutrophils isolated using methods that minimize activation (e.g., negative immunomagnetic selection) exhibit a normal progression through spontaneous apoptosis. In contrast, neutrophils subjected to isolation methods involving RBC lysis often show altered apoptotic kinetics, which can manifest as either accelerated death due to isolation stress or delayed apoptosis from unintended activation of pro-survival pathways [62]. This is critical because the objective of many studies is to identify compounds that can modulate the intrinsic apoptosis pathway. Using pre-activated neutrophils can mask a compound's true effect, leading to both false positives and false negatives during drug screening [62].
Recommended Standardized Protocols
Protocol 1: Negative Immunomagnetic Selection
This protocol is recommended for high-sensitivity applications like apoptosis studies due to its minimal activation of neutrophils [59].
Principle: Negative selection using antibody cocktails and magnetic beads to deplete non-neutrophil cells, leaving neutrophils untouched.
Materials:
- EasySep Direct Human Neutrophil Isolation Kit (Stemcell Technologies) or MACSxpress Neutrophil Isolation Kit (Miltenyi Biotec) [59].
- HBSS with Ca2+/Mg2+ supplemented with 2% Fetal Calf Serum (FCS) [59].
- Collection tubes coated with 2% FCS to prevent adhesion.
Procedure:
- Blood Collection: Collect peripheral blood into anti-coagulant tubes (e.g., tri-sodium citrate). Process samples within 2 hours of collection [62].
- Sample Preparation: Mix whole blood with the provided antibody cocktail and magnetic particles according to the manufacturer's instructions.
- Magnetic Separation: Place the tube into a magnetic field for the specified duration.
- Cell Harvesting: Carefully decant the supernatant containing the isolated neutrophils into a new tube. Avoid disturbing the bead-bound pellet.
- Washing: Centrifuge the neutrophil-containing supernatant and wash the cell pellet once with cold HBSS + 2% FCS.
- Resuspension: Gently resuspend the purified neutrophil pellet in an appropriate apoptosis assay buffer (e.g., RPMI 1640 with 10% FBS) [62].
- Quality Control: Determine cell count and viability using Trypan Blue exclusion. Assess purity via flow cytometry (CD16+/CD66b+ cells).
Protocol 2: Density Gradient Centrifugation without RBC Lysis
This method provides a good balance of performance and cost, avoiding the activating step of RBC lysis.
Principle: Uses a high-density medium like Histopaque-1119 to separate neutrophils from other blood components based on density, followed by a Percoll gradient to further refine the population [59].
Materials:
- Histopaque-1119 (Sigma-Aldrich)
- Percoll (GE Healthcare)
- HBSS with Ca2+/Mg2+ + 2% FCS
Procedure:
- Blood Collection: Collect blood as described in Protocol 1.
- Primary Gradient: Carefully layer 5 mL of anti-coagulated blood over 5 mL of Histopaque-1119. Centrifuge at 800× g for 20 minutes at 20°C with the brake disengaged.
- Collect Neutrophil-Rich Fraction: After centrifugation, collect the diffuse red phase above the erythrocyte pellet, which contains the granulocytes.
- Secondary Gradient (Percoll): Wash the collected cells and resuspend the pellet. Layer this suspension onto a pre-formed, discontinuous Percoll gradient (e.g., layers of 65%, 70%, 75%, 80%, and 85% Percoll). Centrifuge at 800× g for 20 minutes without brake.
- Harvest Neutrophils: Collect the neutrophils from the interface between the 75% and 65% Percoll layers.
- Washing and Resuspension: Wash the harvested neutrophils twice with cold HBSS + 2% FCS. Resuspend in assay buffer for downstream use.
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Key Research Reagent Solutions for Neutrophil Isolation and Apoptosis Assays
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Tri-sodium Citrate (3.8%) | Anti-coagulant | Preferred over heparin for functional assays as it minimally interferes with subsequent steps [62]. |
| Negative Selection Isolation Kits | Neutrophil purification | Miltenyi or StemCell kits enable isolation without neutrophil activation, ideal for apoptosis studies [59]. |
| HBSS with Ca2+/Mg2+ | Buffer for cell washing and resuspension | Maintains ion balance crucial for cell integrity. Supplement with 2% FCS to prevent adhesion [59]. |
| Percoll/Histopaque-1119 | Density gradient media | For density-based separation without the need for RBC lysis [59]. |
| Annexin V Binding Buffer | Essential component for apoptosis assay | Provides the appropriate calcium-containing environment for Annexin V binding to phosphatidylserine [62]. |
| PE-conjugated Annexin V & TOPRO-3 | Apoptosis detection dyes | Annexin V detects early apoptosis (PS externalization); TOPRO-3 detects late apoptosis/necrosis (membrane integrity) [62]. |
| Dimethyl Sulfoxide (DMSO) | Vehicle for compound libraries | Use at lowest possible concentration (<0.1%) to avoid non-specific effects on neutrophil viability [62]. |
Workflow for High-Throughput Apoptosis Screening
The following diagram and protocol outline a standardized workflow for screening compound libraries for their effect on neutrophil apoptosis, building upon the isolation methods described above.
Procedure for Apoptosis Screening:
- Neutrophil Plating: After isolation, resuspend neutrophils at a density of 1-2×10^6 cells/mL in pre-warmed RPMI 1640 supplemented with 10% FBS. Dispense 100 µL of cell suspension into each well of a 96-well plate.
- Compound Addition: Using a multi-channel pipette, add compounds from your library (e.g., kinase inhibitors) to the designated wells. Include controls: a vehicle control (e.g., DMSO) for spontaneous apoptosis, a pro-survival control (e.g., GM-CSF), and a pro-apoptotic control (e.g., pyocyanin) [62].
- Incubation: Incubate the plate at 37°C in a 5% CO2 incubator for the desired time period (typically 20 hours for spontaneous apoptosis).
- Staining: Prepare a staining cocktail in Annexin Binding Buffer containing PE-conjugated Annexin V (1:20 dilution) and TOPRO-3 (1:7,500 dilution). Add 100 µL of this cocktail directly to each well [62].
- Flow Cytometry: Acquire data using a high-throughput flow cytometer (e.g., Attune Autosampler) within 1 hour of staining. Analyze a minimum of 5,000 events per well.
- Data Analysis: Use flow cytometry analysis software (e.g., FlowJo) to quantify the percentage of cells in early apoptosis (Annexin V+/TOPRO-3-), late apoptosis (Annexin V+/TOPRO-3+), and necrosis (Annexin V-/TOPRO-3+). Data can then be processed and visualized using GraphPad Prism.
Standardizing neutrophil isolation protocols is not merely a technical detail but a fundamental prerequisite for generating reliable and reproducible data in inflammation resolution research. Evidence strongly indicates that negative immunomagnetic selection and density gradient methods avoiding RBC lysis best preserve the native neutrophil phenotype, leading to more accurate assessment of apoptosis. Adopting these standardized protocols and the accompanying high-throughput apoptosis assay will significantly enhance the quality of research, facilitate meaningful comparisons across studies, and accelerate the discovery of novel therapeutic agents that modulate neutrophil-driven inflammation.
Strategies for Donor Variability and Ensuring Experimental Reproducibility
Neutrophil apoptosis is a critical control point in the resolution of inflammation, making its accurate assessment vital for pharmaceutical development and basic research [1] [63]. The inherent biological characteristics of primary neutrophils—including their ex vivo instability, short lifespan, and pronounced donor-to-donor variability—present significant challenges for generating consistent, reproducible data [12] [64]. This application note details standardized protocols and strategic approaches to minimize technical artifacts and manage biological variability, thereby enhancing the reliability of neutrophil apoptosis assays within inflammation resolution research.
The execution of neutrophil apoptosis is governed by a complex network of intracellular pathways, with the balance of pro- and anti-apoptotic Bcl-2 family proteins being a key determinant. The anti-apoptotic protein Mcl-1, characterized by a very short half-life, is a central regulator of neutrophil survival and its levels closely correlate with apoptosis kinetics [1] [63]. Research indicates that neutrophil apoptosis can be influenced by multiple external factors, which can be broadly categorized as follows.
Biological and Pathophysiological Heterogeneity
Neutrophils demonstrate considerable heterogeneity in their basal apoptosis rates and responses to modulators. This variability stems from:
- Priming Status: Neutrophils from donors with slightly elevated proinflammatory cytokines in blood plasma can exhibit a primed phenotype (high CD11b, low CD62L), which responds differently to apoptotic stimuli compared to neutrophils from non-inflamed donors [64].
- Disease States: The inflammatory microenvironment in conditions like sepsis, ARDS, and rheumatoid arthritis provides potent survival signals, delaying neutrophil apoptosis [1] [63]. The plasma from septic patients, for instance, contains factors that can induce a distinct transcriptomic response in healthy reporter neutrophils [65].
Technical and Pre-analytical Factors
Technical handling is a major source of artifactual variability that can obscure true biological signals.
- Sample Processing: Neutrophils are readily activated by many common preparation methods, including density gradient centrifugation and RBC lysis protocols. The number of manipulation steps strongly correlates with the level of neutrophil activation and degranulation, measured by surface markers like CD11b, CD66b, and CD62L [12].
- Anticoagulant Choice, Time, and Temperature: The type of anticoagulant used for blood collection, delays in processing, and deviations from recommended staining and incubation temperatures can significantly alter neutrophil phenotype and viability [12].
Strategies for Managing Donor Variability
Donor Stratification and Pre-screening
To reduce variability arising from biological heterogeneity, researchers should characterize and stratify neutrophil donors based on key parameters.
- Plasma Profiling: Screen donor plasma for levels of proinflammatory cytokines (e.g., GM-CSF, IL-8) to identify individuals with a primed neutrophil status [64].
- Baseline Phenotyping: Prior to experiments, assess baseline surface expression of activation markers like CD11b and CD62L on freshly isolated neutrophils. This allows for the stratification of donors into cohorts with similar neutrophil activation states [12] [64].
Utilization of Alternative Cellular Models
For screening applications where donor variability is prohibitive, consider using standardized cell line models.
- Differentiated HL-60 Cells: The human myeloid HL-60 cell line can be differentiated into a neutrophil-like state. A combined treatment with all-trans retinoic acid (ATRA) and dimethyl sulfoxide (DMSO) for 5 days produces cells with typical neutrophil morphology, cell cycle arrest, increased CD11b, loss of CD71, and increased phagocytic capacity. These cells demonstrate a consistent, primed phenotype (high CD11b, low CD62L) and are suitable for evaluating the anti-apoptotic effects of agents like carbon nanoparticles or GM-CSF [64]. This model minimizes donor-to-donor variability and is ideal for initial hazard identification and screening.
Table 1: Comparison of Neutrophil Sources for Apoptosis Assays
| Source | Advantages | Disadvantages | Ideal Use Case |
|---|---|---|---|
| Primary Human Neutrophils | Physiologically most relevant, full functional capacity [12] | High donor variability, short ex vivo lifespan, complex isolation [12] [64] | Mechanistic studies, final validation of drug candidates |
| Differentiated HL-60 Cells [64] | Low variability, unlimited supply, culturable | May not fully recapitulate all primary neutrophil functions | High-throughput screening, initial hazard identification |
Standardized Protocols for Reproducible Neutrophil Characterization and Apoptosis Assays
Protocol: Minimizing Activation during Neutrophil Staining for Flow Cytometry
Accurate immunophenotyping is crucial for assessing apoptosis-related surface markers, but requires careful handling to prevent activation.
Key Principles:
- Minimize Manipulation: Reduce processing steps to prevent artifactual activation [12].
- Cold Temperature: Perform staining at 4°C to slow cellular metabolism and activation [12].
- Pre-wash Step: Remove unbound antibodies prior to fixation and RBC lysis to drastically reduce nonspecific antibody binding, which is particularly problematic due to cationic proteins in neutrophils [12].
Procedure:
- Blood Collection and Anticoagulant: Collect fresh venous blood into anticoagulant tubes (e.g., heparin or EDTA). Process samples within 3 hours of draw [12].
- Staining: Aliquot whole blood and incubate with fluorescently-conjugated antibodies (e.g., anti-CD11b, anti-CD66b, anti-CD62L) for 30 minutes at 4°C [12].
- Pre-wash: Centrifuge the stained blood sample and carefully aspirate the supernatant containing unbound antibodies.
- Fixation and RBC Lysis: Resuspend the cell pellet in a commercial One-step Fixation/RBC Lysis buffer. Incubate according to the manufacturer's instructions, then wash cells prior to flow cytometry analysis [12].
- Gating Strategy: Analyze neutrophils as SSC-Ahigh single cells expressing CD15 and CD16 (FcγRIII). Use negative gates for CD3, CD19, CCR3, and CD14 to exclude other leukocytes and neutrophil-leukocyte multiplets [12].
Protocol: Inducing and Quantifying Neutrophil Apoptosis
This protocol outlines methods to induce apoptosis via specific pathways and quantify the outcome.
Induction Methods:
- Pro-resolution Mediators: Compounds like lipoxin A4 and resolvin E1 promote apoptosis by overriding survival signals. They can attenuate Mac-1-mediated ERK/PI3K/NF-κB survival signaling, facilitate Mcl-1 degradation, and promote caspase-3 activation [1] [63].
- Cyclin-dependent kinase (CDK) Inhibitors: Drugs like roscovitine directly induce neutrophil apoptosis and have been used in clinical trials, showing therapeutic potential for enhancing inflammation resolution [5] [63].
- Phagocytosis-induced Cell Death (PICD): Phagocytosis of opsonized bacteria (e.g., E. coli) triggers NADPH oxidase-dependent ROS generation, leading to caspase-8 and caspase-3 activation and apoptosis [63].
Quantification of Apoptosis:
- Flow Cytometry: The gold-standard method. Use Annexin V-FITC to detect phosphatidylserine (PtdSer) externalization (early apoptosis) and propidium iodide (PI) to assess membrane integrity (late apoptosis/necrosis) [66] [5].
- Western Blotting: Monitor key apoptosis regulators, notably the degradation of Mcl-1 and the cleavage/activation of caspase-3 [1] [63].
- Functional Assays: Assess the downstream consequences of apoptosis, such as the phagocytosis of apoptotic neutrophils by macrophages (efferocytosis), which drives macrophage polarization toward an M2 pro-resolving phenotype [66] [5].
The following workflow integrates these strategies into a coherent framework for managing variability and conducting apoptosis assays.
The Scientist's Toolkit: Key Reagent Solutions
Table 2: Essential Research Reagents for Neutrophil Apoptosis Assays
| Reagent / Material | Function / Application | Key Considerations |
|---|---|---|
| Heparin/EDTA Tubes [12] | Anticoagulant for blood collection | Type of anticoagulant can influence neutrophil responses; must be consistent. |
| One-step Fixation/RBC Lysis Buffer [12] | Simultaneously fixes leukocytes and lyses red blood cells | Superior for preserving native neutrophil state compared to multi-step methods. |
| Anti-human CD11b, CD66b, CD62L Antibodies [12] | Flow cytometric analysis of neutrophil activation and degranulation | CD62L shedding and CD11b/CD66b upregulation are key activation indicators. |
| Annexin V / PI Apoptosis Kit [66] [5] | Standard flow cytometry assay to distinguish early/late apoptosis and necrosis | Essential for quantifying apoptosis rates in response to experimental treatments. |
| Pro-resolving Mediators (Lipoxin Aâ‚„, Resolvin Eâ‚) [1] [63] | Induce neutrophil apoptosis via specific receptor-mediated pathways (e.g., ALX/FPR2). | Key tools for testing resolution pharmacology; override Mac-1 survival signals. |
| Roscovitine [5] [63] | CDK inhibitor that directly induces neutrophil apoptosis. | Useful as a positive control for apoptosis induction; has known clinical safety data. |
| All-trans Retinoic Acid (ATRA) & DMSO [64] | Combined inducers for differentiating HL-60 cells into a primed, neutrophil-like state. | Provides a standardized, readily available cell model to reduce donor variability. |
Achieving reproducibility in neutrophil apoptosis assays demands a dual-focused strategy: the implementation of standardized, gentle protocols to minimize technical noise, and the strategic management of inherent biological variability through donor stratification or alternative models. The protocols and strategies detailed herein provide a robust framework for generating reliable, high-quality data that can accelerate the development of novel therapeutics designed to enhance the resolution of inflammation by targeting neutrophil apoptosis.
Troubleshooting False Positives/Negatives in Flow Cytometry and Fluorescent Staining
Inflammation resolution research relies heavily on accurate cellular phenotyping, with neutrophil apoptosis assays serving as a critical endpoint. Flow cytometry and fluorescent staining are indispensable tools for these investigations, yet their accuracy is frequently compromised by biological and technical artifacts leading to false positives and negatives. These inaccuracies can profoundly impact the interpretation of experimental outcomes, particularly when assessing delicate processes like macrophage efferocytosis of apoptotic neutrophils. Understanding the sources of interference is the first step toward developing robust, reproducible assays for screening therapeutic compounds. This application note provides a structured framework for identifying, troubleshooting, and mitigating common pitfalls in fluorescence-based neutrophil assays.
The fundamental principles of fluorescence detection are a common source of misunderstanding. Fluorescence occurs when a fluorophore absorbs light at a specific wavelength and emits it at a longer wavelength [67]. The difference between these wavelengths, known as the Stokes shift, is critical for separating the excitation signal from the emitted light that detectors capture [67]. In complex biological systems like those studying neutrophil apoptosis, this process is vulnerable to interference from multiple sources, including autofluorescence from media components or cells themselves, non-specific antibody binding, and the presence of therapeutic or endogenous compounds that quench fluorescence [68].
Biological and Chemical Interference
Multiple endogenous and exogenous factors can interfere with fluorescence detection. The table below summarizes the primary sources and their impact on assay data.
Table 1: Common Sources of Interference in Fluorescence-Based Assays
| Interference Category | Specific Source | Effect on Assay | Commonly Affected Parameters |
|---|---|---|---|
| Endogenous Autofluorescence | Riboflavins in media [68], NAD(P)H [68] | Elevated background, reduced signal-to-noise ratio | All channels, particularly UV/violet-excited |
| Cell granules (e.g., in neutrophils) | False positive signals | Multiple fluorescence channels | |
| Compound-Mediated Effects | Fluorescent test compounds [68] | Autofluorescence causing false positives | Specific channels depending on compound |
| Fluorescence quenching compounds [68] | Signal loss leading to false negatives | Specific channels depending on compound | |
| Sample & Reagent Issues | Non-specific antibody binding [69] | False positive cell population identification | Cell surface marker identification |
| Therapeutic monoclonal antibodies [69] | Blockade of target epitopes, false positive XM | Immunophenotyping, crossmatching | |
| Dead cells/debris [68] | Non-specific probe uptake, altered light scatter | Apoptosis assays, viability staining |
Technical and Instrumental Artifacts
Beyond biological factors, technical execution and instrument configuration are frequent culprits. Photobleaching, where fluorophores permanently lose their ability to fluoresce due to light-induced damage, can lead to false negatives, particularly during prolonged imaging or if laser powers are set incorrectly [67]. Spectral overlap occurs when the emission spectra of multiple fluorophores in a panel are too similar, causing signal "spillover" into adjacent detectors [70]. While spectral flow cytometry has advanced the ability to resolve complex panels by capturing full emission spectra, it requires meticulous validation and unmixing algorithms to avoid generating new types of analytical artifacts [70]. Furthermore, insufficient cell numbers due to cytotoxicity or loss of adherence can invalidate statistical analysis, while overly high cell concentrations can cause swarm effects and inaccurate volumetric measurements [68].
Systematic Troubleshooting Workflow
Adopting a systematic approach to troubleshooting is essential for identifying the root cause of aberrant data. The following diagram outlines a logical pathway for diagnosing common problems in neutrophil apoptosis assays.
Investigating False Positives
When facing unexpectedly high signal or cell populations where none are biologically expected, follow the left branch of the workflow. Begin by analyzing unstained controls and fluorescence-minus-one (FMO) controls to establish baseline autofluorescence and define positive/negative gates accurately. Proceed to assess cell viability using a dedicated viability dye, as dead cells and debris frequently exhibit non-specific antibody binding and accumulate fluorescent probes [68]. If using intracellular stains for apoptotic markers (e.g., active caspase-3), ensure fixation and permeabilization protocols are optimized to prevent non-specific staining. Finally, review compensation matrices; over-compensation can create false positive populations in the compensated channel.
Investigating False Negatives
For absent or diminished expected signal, follow the right branch of the workflow. First, confirm the activity of critical reagents such as fluorescently-labeled antibodies and detection dyes. Check expiration dates and ensure proper storage conditions. Next, verify instrument performance, including laser output and photomultiplier tube (PMT) voltages, using standard calibration beads [70]. Investigate the potential for fluorescence quenching by test compounds; this is a common yet overlooked issue in drug screening [68]. Finally, inspect for detector saturation, which can occur if the signal from a bright fluorophore is too strong, causing the detector to "max out" and clip the data, which can be misinterpreted as a negative result.
Recommended Protocols for Neutrophil Apoptosis Assays
Protocol 1: Basic Annexin V/Propidium Iodide Apoptosis Assay
This protocol provides a standard method for quantifying early and late apoptosis in neutrophil populations, a key metric in inflammation resolution studies.
- Key Reagents: Annexin V-FITC, Propidium Iodide (PI), Binding Buffer, Cell Wash Buffer.
- Procedure:
- Cell Preparation: Isolate neutrophils from human peripheral blood or inflammatory exudates using a standardized density gradient centrifugation method. Maintain cells in a suitable culture medium.
- Induction and Staining: Induce apoptosis as required (e.g., via serum starvation or drug treatment). Harvest ~1x10^6 cells per condition and wash twice in cold PBS.
- Staining: Resuspend cell pellet in 100 µL of Annexin V Binding Buffer. Add 5 µL of Annexin V-FITC and 5 µL of PI (or other viability dye). Incubate for 15 minutes at room temperature in the dark.
- Acquisition and Analysis: Add 400 µL of Binding Buffer to each tube and analyze by flow cytometry within 1 hour. Use unstained, single-stained, and FMO controls for proper gating and compensation.
- Troubleshooting Tips:
- High Background in Viability Channel: Titrate the PI concentration; excessive PI can stain early apoptotic cells.
- Low Annexin V Signal: Ensure calcium is present in the binding buffer, as Annexin V binding is Ca2+-dependent.
- Morphological Changes: Neutrophils may show altered light scatter properties during apoptosis; use a combination of SSC/FSC and viability dyes for accurate gating.
Protocol 2: Intracellular Staining for Apoptotic Markers
This protocol is for detecting intracellular targets like cleaved caspases or phosphorylated signaling proteins, which can provide mechanistic insights.
- Key Reagents: Fixation Buffer (e.g., 4% PFA), Permeabilization Buffer (e.g., Saponin-based), Primary and/or Fluorescently-Conjugated Antibodies, Flow Cytometry Staining Buffer.
- Procedure:
- Surface Staining (Optional): If immunophenotyping is required, stain surface markers first in suspension using standard protocols. Wash cells.
- Fixation and Permeabilization: Fix cells with IC Fixation Buffer for 20 minutes on ice. Wash twice, then permeabilize cells with Permeabilization Buffer for 10 minutes.
- Intracellular Staining: Centrifuge and resuspend cell pellet in Permeabilization Buffer containing the pre-titrated fluorescent antibody against the intracellular target (e.g., cleaved Caspase-3). Incubate for 30-60 minutes at room temperature in the dark.
- Acquisition and Analysis: Wash cells twice and resuspend in Flow Cytometry Staining Buffer. Acquire data on a flow cytometer. Use an isotype control and FMO control for the intracellular marker to set positive gates.
- Troubleshooting Tips:
- Poor Signal: Optimize antibody titration and permeabilization conditions (time, detergent concentration). Some antigens may require methanol-based permeabilization.
- High Background: Include a Fc receptor blocking step prior to surface or intracellular staining, especially for neutrophils. Ensure permeabilization buffer is thoroughly washed out.
The Scientist's Toolkit: Essential Reagents and Materials
Success in fluorescence-based assays depends on the selection and proper use of key reagents. The following table details critical solutions for research in this field.
Table 2: Research Reagent Solutions for Neutrophil Fluorescence Assays
| Reagent/Material | Function/Application | Key Considerations |
|---|---|---|
| Annexin V Conjugates | Detection of phosphatidylserine exposure on the outer leaflet of the plasma membrane, an early marker of apoptosis. | Requires calcium-containing buffer. Should be combined with a viability dye to distinguish early apoptosis from necrosis. |
| Caspase Activity Probes (e.g., FLICA) | Detection of active caspase enzymes within living cells, confirming engagement of the apoptotic pathway. | Cell-permeable and covalent binding; requires careful titration as it can be cytotoxic over long incubations. |
| Viability Dyes (e.g., Propidium Iodide, 7-AAD, DAPI) | Exclusion dyes to identify cells with compromised plasma membranes (necrotic/late apoptotic cells). | Impermeable to live and early apoptotic cells. Must be used on non-fixed cells. Spectral properties vary. |
| Fc Receptor Blocking Solution | Blocks non-specific binding of antibodies to Fc receptors on immune cells like neutrophils and macrophages. | Critical for reducing background in immunophenotyping. Use species-specific (e.g., human) for best results. |
| Compensation Beads | Ultra-bright, uniform particles used to calculate spectral spillover between channels on a flow cytometer. | Essential for multicolor panels. Should be used with the same antibodies and fluorochromes as the experimental samples. |
| Cell Viability Assay Kits (e.g., MTT, Resazurin) | Measure metabolic activity as a surrogate for cell viability and proliferation. | Can be used as an orthogonal method to confirm findings from flow cytometry and rule out general cytotoxicity. |
Mitigation Strategies and Best Practices
Experimental Design and Validation
Proactive experimental design is the most effective strategy for minimizing artifacts. Always include the following controls in every experiment: unstained cells to assess autofluorescence, single-stained controls for compensation, FMO controls for accurate gating, and biological controls (e.g., a known inducer of neutrophil apoptosis). For drug screening, include a vehicle control to isolate compound-specific effects. When working with therapeutic antibodies or patient sera, be aware that agents like Rituximab (anti-CD20) or Daratumumab (anti-CD38) can bind to target cells and cause false positive signals in flow-based crossmatch assays [69]. Mitigation strategies include using F(ab')2 fragments of secondary antibodies or pre-treating cells with pronase to cleave off surface-bound antibodies [71] [69].
Data Acquisition and Analysis
During acquisition, collect a sufficient number of events to ensure statistical power, especially for rare cell populations. Implement a doublet discrimination gate based on FSC-H vs FSC-A to exclude cell aggregates from analysis. For apoptosis assays, be mindful that neutrophils are fragile and can undergo secondary necrosis; therefore, rapid processing and immediate analysis are crucial. When analyzing data, use a sequential gating strategy to isolate the population of interest, and apply consistent gates across all samples and experiments. Finally, consider using autofluorescence as a identifying parameter for certain cell types; for instance, some studies suggest neutrophil autofluorescence can be distinguished from other leukocytes, though this can also be a source of interference if not properly controlled [68].
Critical Controls and Best Practices for High-Throughput Data Interpretation
Inflammation resolution is an active, highly programmed process, and the precise timing of neutrophil apoptosis is a critical turning point between inflammatory progression and resolution [3]. Research in this field increasingly relies on high-throughput data to decipher complex cellular interactions and signaling pathways. The movement of data engineering towards a "Data Product" approach, which emphasizes defined requirements, key performance indicators (KPIs), and continuous monitoring, provides a powerful framework for the rigorous interpretation of biological data [72]. This document outlines essential controls, best practices, and detailed protocols to ensure the accuracy, reliability, and reproducibility of high-throughput data within the specific context of neutrophil apoptosis assays.
Critical Controls for Data Integrity
Implementing robust controls is non-negotiable for generating trustworthy data. The principle of "garbage in, garbage out" remains fundamental; sophisticated analytical models cannot overcome the limitations of poor-quality underlying data [73]. The following controls should be integrated into every data pipeline.
Table 1: Critical Data Quality Controls for High-Throughput Assays
| Control Category | Description | Application in Neutrophil Apoptosis |
|---|---|---|
| Null Set Testing | Evaluates system handling of empty or null fields [74]. | Validate that missing values in flow cytometry data (e.g., from failed stains) do not cause downstream processing errors. |
| Completeness Testing | Verifies all expected data is present [74]. | Confirm that all required parameters (e.g., Annexin V, PI, caspase activity) are populated for every cell observation before analysis. |
| Boundary Value Testing | Examines system behavior at extreme input values [74]. | Check that image analysis software correctly handles maximum and minimum fluorescence intensities without saturation or loss of sensitivity. |
| Uniqueness Testing | Identifies duplicate records in datasets [74]. | Ensure that each data file from an automated microscope or plate reader is uniquely identified and ingested only once to prevent double-counting. |
| Referential Integrity | Validates relationships between database tables [74]. | Maintain integrity between experimental metadata (e.g., treatment conditions) and the resulting raw data files, preventing orphaned records. |
| Consistency Checks | Maintains uniformity across systems and formats [74]. | Standardize units for cytokine concentrations (e.g., pg/mL) and time measurements across all experiments and data exports. |
A proactive approach to Data Quality Management involves implementing automated checks at the point of data entry or collection to prevent incorrect data from ever entering the system [75]. Furthermore, establishing clear Data Governance roles, such as assigning data stewards within the research team, is crucial for maintaining data integrity, definitions, and access approvals on a day-to-day basis [76] [77].
Best Practices for Data Management
Building upon a foundation of rigorous controls, adopting modern data management practices transforms raw data into a strategic, reliable asset.
Establish a Data Governance Framework
A proactive, structured approach dictates how data assets are managed. This involves establishing clear policies, procedures, and accountability to ensure data is handled consistently and securely [75]. For research, this means defining protocols for data collection, transformation, storage, and sharing. A modern framework is built on three pillars: Automation (using tools for profiling and lineage), Embedded Collaboration (bringing governance into daily analysis tools), and Democratization (decentralizing decision-making to data stewards close to the science) [77].
Prioritize Data Quality Management
This is a continuous cycle of monitoring, measuring, and improving data integrity [75]. Key steps include:
- Implementing Automated Validation: Use tools to continuously monitor data streams and identify anomalies [75].
- Establishing Quality Metrics: Define measurable standards for data attributes like completeness and accuracy. For example, aim for 99.9% accuracy in cell count data from automated systems [75].
- Creating Feedback Loops: When errors are detected, trace them to their source and correct them, training personnel on standards accordingly [75].
Implement Intelligent Data Lifecycle Management
Data value changes over time. Intelligent Data Lifecycle Management (DLM) is a policy-based approach to managing information from creation to archival or deletion [75]. For high-throughput imaging data, this could mean storing raw, uncompressed files on high-performance storage immediately after acquisition, moving processed data to mid-tier storage for analysis, and archiving final datasets to a cost-effective long-term storage solution after project completion.
Adopt a "Data Product" Approach and Versioning
Treating data outputs as products means applying product management methodologies, including defined requirements, KPIs, and measurement processes [72]. This is enabled by data versioning, which creates branches of data for safe, isolated development and testing. It allows for full reproducibility, as scientists can always return to the exact data version used for a specific analysis [72]. This is implemented using data version control tools that provide capabilities like branching and time travel.
Experimental Protocols
Protocol: Assessing the Effect of Apoptotic Bodies (ApoBDs) on Neutrophil Apoptosis
This protocol is adapted from a study investigating ApoBDs derived from hypoxic bone marrow mesenchymal stem cells (BMSCs) [78].
Key Research Reagent Solutions:
- Alpha-Minimum Essential Medium (α-MEM): For culturing BMSCs, supplemented with 20% FBS, L-glutamine, and penicillin/streptomycin [78].
- RPMI 1640 Medium: For culturing isolated neutrophils, supplemented with 10% FBS and penicillin/streptomycin [78].
- Annexin V-FITC Apoptosis Detection Kit: To quantify apoptotic cells by flow cytometry via phosphatidylserine (PS) externalization [78].
- Lipopolysaccharide (LPS): Used to induce delayed neutrophil apoptosis, creating an inflammatory model [78].
- Neutrophil Isolation Kit: A magnetic bead-based kit (e.g., from Miltenyi Biotec) for obtaining high-purity neutrophils from bone marrow [78].
Methodology:
- BMSC Culture and ApoBD Generation:
- Harvest BMSCs from the bone marrow of mice (e.g., C57BL/6) and culture in α-MEM complete medium [78].
- Induce apoptosis by placing BMSCs in a sealed hypoxic chamber (e.g., AnaeroPack) for 48 hours [78].
- Collect the medium and sequentially centrifuge it (300×g for 10 min) and filter it through 5 μm and 1 μm membranes to remove cells and debris [78].
- Pellet ApoBDs by centrifuging the filtrate at 2000×g for 20 min. Characterize ApoBDs using transmission electron microscopy (TEM), dynamic light scattering (DLS) for size, and staining with Annexin V/Hoechst for confirmation [78].
Neutrophil Isolation and Treatment:
- Isolate neutrophils from mouse bone marrow using a commercial isolation kit to achieve high purity [78].
- Seed neutrophils in culture plates at a density of 1 × 10^6 cells per well.
- Pre-treat neutrophils with LPS (e.g., 10 ng/mL) for a defined period to delay apoptosis.
- Co-treat LPS-stimulated neutrophils with isolated ApoBDs (e.g., 2 μg/mL) for 18 hours. Include controls for basal apoptosis (untreated) and apoptosis delay (LPS only) [78].
Apoptosis Assay via Flow Cytometry:
- Harvest neutrophils and stain them using the Annexin V-FITC kit according to the manufacturer's instructions.
- Analyze samples using a flow cytometer. A minimum of 10,000 events per sample should be collected.
- Quantify the percentage of cells in early (Annexin V+/PI-) and late (Annexin V+/PI+) apoptosis.
Data Interpretation: ApoBDs from hypoxic BMSCs have been shown to reverse LPS-induced delayed apoptosis. This effect is attributed to the transfer of miR-125b-5p from ApoBDs to neutrophils, which inhibits the activation of the PI3K-AKT signaling pathway [78]. The following diagram illustrates this mechanism.
Protocol: Evaluating the Role of Specialized Pro-Resolving Mediators (SPMs)
This protocol outlines the assessment of SPMs, endogenous lipid mediators that actively promote inflammation resolution [3].
Key Research Reagent Solutions:
- SPM Analogs: Synthetic analogs of Lipoxins (e.g., LXA4), Resolvins (e.g., RvD1, RvE1), Protectins, or Maresins [3].
- Receptor Antagonists: For example, Boc-2, an antagonist for the LXA4 receptor, to confirm receptor-specific effects [3].
- Phospho-Specific Antibodies: For detecting phosphorylation status of signaling proteins like AKT, ERK, and p38 MAPK via western blot [3].
- ELISA Kits: For quantifying pro-inflammatory cytokines (TNF-α, IL-1β, IL-6) and anti-inflammatory cytokines (TGF-β, IL-10) in culture supernatants [7].
Methodology:
- Neutrophil Treatment with SPMs:
- Isolate and culture neutrophils as described in Protocol 4.1.
- Stimulate neutrophils with a pro-inflammatory agent like LPS (1-100 ng/mL) to delay apoptosis.
- Co-treat with a specific SPM analog (e.g., LXA4 at low nanomolar concentrations) for a defined period (e.g., 18 hours). Include controls with an SPM receptor antagonist to demonstrate specificity [3].
- Apoptosis and Functional Assays:
- Quantify apoptosis using Annexin V/PI flow cytometry as above.
- Collect cell lysates to analyze signaling pathways. Use western blotting with phospho-specific antibodies to assess the activity of pathways like PI3K/AKT and p38 MAPK, which are known targets of SPMs [3].
- Measure the secretion of inflammatory and resolving mediators in the culture supernatant using ELISA.
Data Interpretation: SPMs promote inflammation resolution by binding to specific G-protein coupled receptors (GPCRs), which transduce signals that lead to the induction of neutrophil apoptosis and inhibition of pro-inflammatory activation. The following diagram summarizes the key actions of SPMs on neutrophils.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for Neutrophil Apoptosis Assays
| Reagent / Material | Function / Application | Example |
|---|---|---|
| Magnetic Neutrophil Isolation Kit | Obtains high-purity neutrophil populations from bone marrow or blood, minimizing contamination from other cells that could affect assay results. | Kit from Miltenyi Biotec or similar [78]. |
| Annexin V-Based Apoptosis Kit | Flags early and late apoptotic cells by detecting phosphatidylserine (PS) externalization on the cell surface, a hallmark of apoptosis. | FITC Annexin V Apoptosis Detection Kit [78]. |
| Caspase Activity Assays | Measures the activation of executioner caspases (e.g., Caspase-3/7), providing a complementary metric of apoptosis commitment. | Fluorogenic substrate-based assays. |
| Lipopolysaccharide (LPS) | A toll-like receptor 4 (TLR4) agonist used to create an in vitro model of inflammatory stress and delayed neutrophil apoptosis. | From E. coli or other species [78]. |
| Specialized Pro-Resolving Mediator (SPM) Analogs | Synthetic analogs of endogenous resolution mediators (e.g., LXA4, RvD1) used to test their direct pro-apoptotic and anti-inflammatory effects. | Commercially available from Cayman Chemical and others [3]. |
| Phospho-Specific Flow Cytometry Antibodies | Allows multiplexed measurement of signaling pathway activity (e.g., p-AKT, p-ERK) at the single-cell level alongside apoptosis markers. | Antibodies from BD Biosciences, Cell Signaling Technology. |
| Cell Culture Inserts / Hypoxic Chambers | Creates a controlled low-oxygen environment to mimic the physiological hypoxic conditions of inflammatory sites and study its effects on cell death. | AnaeroPack system [78]. |
Translational Validation and Comparative Analysis of Assay Data
Neutrophil apoptosis is a precisely regulated process that serves as a critical control point for the resolution of inflammation. Research in this field relies heavily on in vitro models to elucidate molecular mechanisms, yet the physiological relevance of these findings must be validated through in vivo studies. This application note examines the key concordances and discrepancies between in vitro and in vivo findings in neutrophil apoptosis research, providing researchers with structured data, detailed protocols, and analytical frameworks to enhance translational relevance in drug development.
The transition from circulation to tissues fundamentally alters neutrophil biology. While in vitro studies using blood-derived neutrophils provide crucial insights into core apoptotic pathways, they may not fully capture the complex regulatory landscape within inflamed tissues. This document synthesizes evidence across experimental systems to bridge this gap, enabling more accurate interpretation of neutrophil apoptosis data in inflammation resolution research.
Comparative Analysis: Key Discrepancies Between Experimental Systems
Table 1: Major Discrepancies in Neutrophil Apoptosis Regulation Between In Vitro and In Vivo Environments
| Aspect | In Vitro Observations | In Vivo Observations | Experimental Evidence |
|---|---|---|---|
| Responsiveness to Anti-apoptotic Signals | Blood neutrophils consistently respond to anti-apoptotic stimuli (GM-CSF, LPS) with delayed apoptosis [79] | Tissue neutrophils show site-dependent responses; skin chamber neutrophils resist anti-apoptotic signals while synovial fluid neutrophils remain responsive [79] | Human skin chamber and synovial fluid models comparing response to identical stimuli [79] |
| Lifespan & Spontaneous Apoptosis | Rapid apoptosis within 24 hours under standard culture conditions [1] [54] | Potential for extended lifespan; gently isolated neutrophils show migratory activity up to 150 hours [80] | Live-cell imaging of minimally manipulated neutrophils [80] |
| Death Pathway Preference | Standard isolation (DGS) promotes NETosis within 8 hours [80] | Apoptosis predominates as physiological death pathway in minimally disturbed systems [80] | Comparison of DGS-isolated vs. gelafundin-isolated neutrophils [80] |
| Microenvironmental Integration | Response to individual, defined pro-survival or pro-apoptotic cues [1] | Integrated response to complex signal hierarchies from inflammatory microenvironment [1] | Analysis of transmigrated neutrophils in various inflammatory contexts [1] [79] |
| Molecular Regulation | Mcl-1 degradation central to apoptosis execution [54] | Tissue-specific factors (IL-1β) can override core molecular programs [79] | Autocrine IL-1β signaling in skin chamber neutrophils despite Mcl-1 regulation [79] |
Experimental Models and Methodologies
1In VitroModels for Neutrophil Apoptosis Studies
Protocol 1: Standard Isolation and Culture of Human Blood Neutrophils
- Principle: Density gradient separation enables isolation of highly pure neutrophil populations from peripheral blood for controlled in vitro experimentation.
- Reagents:
- Anticoagulated human peripheral blood
- Dextran solution (6% in saline)
- Ficoll-Paque density gradient medium
- Phosphate-buffered saline (PBS)
- RPMI-1640 culture medium with 10% FCS
- Procedure:
- Mix blood with equal volume of dextran solution and allow erythrocytes to sediment for 30 minutes at room temperature.
- Collect leukocyte-rich supernatant and layer onto Ficoll-Paque.
- Centrifuge at 400-500 × g for 30 minutes at 20°C without brake.
- Collect neutrophil pellet from above erythrocyte layer.
- Perform hypotonic lysis of residual erythrocytes using cold sterile water.
- Wash neutrophils twice in PBS and resuspend in RPMI-1640 with 10% FCS at 5×10^6 cells/mL.
- Culture at 37°C with 5% CO2 with or without experimental treatments.
- Technical Notes: Minimize g-force exposure during centrifugation as it can prime neutrophils and alter death pathways. For apoptosis assays, include Annexin V/7-AAD staining with flow cytometric analysis at 0, 6, 12, 20, and 24 hours [79] [80].
Protocol 2: Hoxb8 System for Genetic Manipulation of Neutrophil Apoptosis Pathways
- Principle: Conditionally immortalized progenitor cells enable genetic manipulation and subsequent differentiation into neutrophils, overcoming limitations of primary neutrophil transfection.
- Reagents:
- ER-Hoxb8 retroviral construct
- Bone marrow from genetically modified mice
- Stem cell factor (SCF)
- β-estradiol
- Differentiation medium (without β-estradiol)
- Procedure:
- Transduce bone marrow cells with ER-Hoxb8 retrovirus.
- Culture transduced cells in presence of SCF and β-estradiol to maintain progenitor state.
- For differentiation, wash cells and culture in medium containing SCF but without β-estradiol.
- Differentiate for 4 days to obtain mature neutrophils.
- Harvest neutrophils for apoptosis assays after SCF withdrawal [54].
- Applications: Ideal for studying specific gene functions in neutrophil apoptosis using knockout/knockdown approaches or transgene expression. Particularly valuable for assessing Bcl-2 family protein functions [54].
2In Vivoand Tissue-Relevant Models
Protocol 3: Human Skin Chamber Model for Studying Transmigrated Neutrophils
- Principle: This ex vivo model captures neutrophils that have undergone transendothelial migration, mimicking key aspects of tissue recruitment.
- Reagents:
- Sterile skin chambers
- Inflammatory stimulant (e.g., cytokine cocktail)
- Krebs-Ringer phosphate buffer with glucose and Ca2+
- Procedure:
- Apply sterile chambers to mildly abraded skin on healthy volunteers.
- Introduce inflammatory stimulus into chambers.
- After 12-24 hours, collect exudate fluid containing transmigrated neutrophils.
- Wash cells and resuspend in appropriate buffer for immediate analysis.
- Compare responses to blood neutrophils from same donor [79].
- Key Observations: Skin chamber neutrophils secrete high levels of IL-1β and resist further anti-apoptotic stimulation, highlighting how tissue migration alters apoptotic regulation [79].
Protocol 4: Analysis of Neutrophil Apoptosis in Murine Disease Models
- Principle: Animal models provide intact physiological context for studying neutrophil apoptosis in inflammation and resolution.
- Models:
- Procedure:
- Induce disease model according to established protocols.
- At appropriate timepoints, collect inflammatory exudates or tissues.
- Isolve neutrophils for apoptosis assessment via:
- Morphological analysis (May-Grünwald-Giemsa staining)
- Annexin V/PI flow cytometry
- Caspase-3/7 activity assays
- Calculate resolution indices (Tmax, T50, Resolution Interval) [81].
- Applications: Therapeutic testing of pro-resolving mediators (e.g., Angiotensin-(1-7), SPMs) [81] [3].
Molecular Regulation Across Systems
Core Apoptotic Machinery
The Bcl-2 protein family constitutes the fundamental regulatory network controlling neutrophil apoptosis, with both conserved and context-dependent functions across experimental systems.
Table 2: Molecular Regulators of Neutrophil Apoptosis Across Experimental Systems
| Molecule | Function | In Vitro Evidence | In Vivo Evidence |
|---|---|---|---|
| Mcl-1 | Short-lived anti-apoptotic protein; levels correlate with survival | Rapid degradation precedes spontaneous apoptosis; maintained by survival signals [1] [54] | Myeloid-specific knockout reduces neutrophil numbers by accelerating apoptosis [1] |
| Bim | Pro-apoptotic BH3-only protein | Deficiency provides partial protection from spontaneous apoptosis [54] | Loss increases neutrophil numbers in mice [54] |
| Noxa | Pro-apoptotic BH3-only protein | Cooperates with Bim; dual deficiency strongly protects [54] | Regulates termination of neutrophil function and inflammation [54] |
| IL-1β | Pro-inflammatory cytokine | Can delay apoptosis in blood neutrophils [79] | Autocrine signaling maintains survival in skin chamber neutrophils [79] |
| β2 Integrins | Adhesion receptors | Generate contrasting survival/apoptosis signals depending on ligands [1] | Integrate signals from inflammatory microenvironment; target for pro-resolving mediators [1] |
Molecular Regulation of Neutrophil Apoptosis Across Experimental Systems
Advanced Interventional Strategies
Nanoparticle-Mediated Neutrophil Apoptosis Induction
- Principle: Poly(lactic-co-glycolic acid) nanoparticles loaded with roscovitine and catalase (RC NPs) exploit the reactive oxygen species-rich environment of inflamed tissues to induce spatially-controlled neutrophil apoptosis [5].
- Mechanism:
- Intravenously injected RC NPs are taken up by circulating neutrophils migrating to infarcted heart
- Activated neutrophils at injury site generate H2O2
- Catalase converts H2O2 to oxygen, causing nanoparticle detonation
- Intracellular roscovitine release induces neutrophil apoptosis
- Apoptotic neutrophils promote macrophage efferocytosis and M2 polarization [5]
- Therapeutic Application: Single intravenous injection in MI rats induced neutrophil apoptosis at infarct site, promoted reparatory macrophage polarization, and preserved heart function [5].
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for Neutrophil Apoptosis Studies
| Category | Reagent/Solution | Function & Application | Key Considerations |
|---|---|---|---|
| Isolation | Dextran/Ficoll-Paque | Standard density gradient separation of blood neutrophils | Minimize g-force exposure; consider gelafundin for minimal manipulation [80] |
| Viability Assessment | Annexin V/7-AAD | Flow cytometric differentiation of apoptotic stages | Combine with morphological analysis for increased accuracy [79] |
| Molecular Tools | Hoxb8 progenitor system | Enables genetic manipulation of neutrophil apoptosis pathways | Essential for studying Bcl-2 family protein functions [54] |
| Pro-resolving Mediators | Lipoxin A4, Resolvin E1 | Induce neutrophil apoptosis and promote resolution | Target β2 integrin signaling; enhance efferocytosis [1] [3] |
| Therapeutic Nanoparticles | Roscovitine/Catalase-loaded PLGA NPs | Spatiotemporally controlled induction of neutrophil apoptosis | ROS-responsive release limits effects to inflamed tissues [5] |
| Cytokine Modulation | IL-1 Receptor Antagonist | Blocks IL-1β-mediated survival signaling | Particularly relevant for tissue neutrophil studies [79] |
Bridging in vitro and in vivo findings in neutrophil apoptosis research requires careful consideration of experimental context and limitations. While core molecular mechanisms involving Mcl-1, Bim, and Noxa remain consistent across systems, tissue-specific factors such as autocrine IL-1β signaling and β2 integrin engagement can profoundly alter apoptotic responses. Researchers should employ multiple complementary models—from minimally manipulated ex vivo systems to complex animal models—to fully understand neutrophil apoptosis regulation. The developing toolkit, including genetic manipulation systems and targeted nanotherapies, offers powerful approaches to translate mechanistic insights into therapeutic strategies for resolving inflammation in human disease.
The resolution of inflammation is a critical, active process for restoring tissue homeostasis, and the induction of neutrophil apoptosis is a key control point within this pathway [82]. Dysregulated neutrophil apoptosis is implicated in chronic inflammatory diseases, making pharmacological induction of this process a promising therapeutic strategy [83] [84]. Cyclin-dependent kinase 9 (CDK9) has emerged as a genetically and pharmacologically validated target for promoting inflammation resolution. CDK9 regulates transcription by forming the positive transcription elongation factor b (P-TEFb) complex with cyclin T, which phosphorylates RNA polymerase II to promote transcriptional elongation [85] [86]. This application note details experimental protocols for validating CDK9 inhibitors both in vitro and in vivo, framed within the context of neutrophil apoptosis assays for inflammation resolution research.
CDK9 Biology and Relevance to Inflammation
CDK9 exists as two primary isoforms (42 kDa and 55 kDa) that form the catalytic core of P-TEFb [85]. This complex is essential for the transcription of short-lived genes, including the neutrophil survival protein Mcl-1 and key inflammatory mediators [86]. Inhibition of CDK9 kinase activity rapidly depletes Mcl-1 levels, triggering apoptosis in inflammatory neutrophils and thereby promoting the resolution of inflammation [83] [86].
Table 1: Key Proteins in CDK9-Mediated Neutrophil Survival
| Protein | Function | Role in Neutrophil Apoptosis |
|---|---|---|
| CDK9 | Serine/threonine kinase component of P-TEFb | Regulates transcription of survival genes |
| Cyclin T | Regulatory subunit of P-TEFb | Essential for CDK9 activation |
| Mcl-1 | Anti-apoptotic Bcl-2 family member | Critical neutrophil survival factor |
| RNA Polymerase II | Transcriptional machinery | Phosphorylated by P-TEFb for elongation |
| Bim | Pro-apoptotic Bcl-2 family member | Promotes apoptosis when Mcl-1 is depleted |
Quantitative Evidence for CDK9 in Inflammation Resolution
Multiple studies have provided quantitative evidence supporting CDK9 inhibition as a strategy for promoting inflammation resolution through neutrophil apoptosis.
Table 2: Summary of Key Experimental Findings on CDK9 Inhibition
| Model System | Intervention | Key Quantitative Findings | Reference |
|---|---|---|---|
| Zebrafish tailfin injury | Pharmacological (AT7519, Flavopiridol) | Significant neutrophil reduction at 24h post-injury; AT7519 increased apoptotic neutrophils by 2.5-fold at 12hpi | [84] |
| Zebrafish tailfin injury | Genetic (CDK9 morpholino) | Reduced neutrophil numbers at wound site at 24hpi; increased apoptotic neutrophils at 8hpi | [84] |
| Zebrafish | CDK9 CRISPR/Cas9 knockout | Homozygous mutants: ~62% reduction in total neutrophils; significantly reduced wound recruitment at 24hpi (4±1 vs 11±2 cells in wild-type) | [84] |
| Primary human neutrophils | R-roscovitine, DRB | Significant time-dependent loss of RNAP II phosphorylation at Ser2 and Ser5; induction of apoptosis | [86] |
| RAW264.7 macrophages | iCDK9 inhibitor | Cytotoxicity IC~50~ = 0.09 ± 0.01 µM; suppression of NO, TNF-α, and IL-6 production at 0.06 µM | [87] |
Experimental Protocols
In Vivo Zebrafish Tailfin Injury Model
Principle: The zebrafish tailfin transection model enables real-time, in vivo quantification of neutrophil apoptosis and inflammation resolution in response to CDK9 modulation [84].
Materials:
- Tg(mpx:EGFP)~i114~ zebrafish (3 days post-fertilization)
- CDK9 inhibitors (AT7519, flavopiridol) dissolved in DMSO
- Morpholinos for CDK9 knockdown
- CRISPR/Cas9 system for CDK9 knockout
- Confocal microscopy system for live imaging
Procedure:
- Anesthetize 3 dpf zebrafish embryos in tricaine solution
- Transect the median tailfin using a sterile scalpel blade
- Treat embryos with CDK9 inhibitors (AT7519, flavopiridol) or vehicle control immediately post-injury
- For genetic approaches:
- Inject CDK9-specific morpholinos at 1-4 cell stage
- Generate heritable CDK9 knockouts using CRISPR/Cas9
- Perform serial imaging at 4, 8, 12, and 24 hours post-injury (hpi)
- Quantify neutrophil numbers within a standardized area (0.5 mm from tailfin tip)
- Assess apoptosis using TUNEL staining combined with neutrophil-specific labeling
- Track total neutrophil numbers throughout the embryo to assess systemic effects
Key Parameters:
- Neutrophil recruitment (peak at ~4 hpi)
- Resolution phase (4-24 hpi)
- Apoptotic neutrophils (TUNEL-positive)
- Macrophage recruitment (peaks at ~24 hpi)
In Vitro Neutrophil Apoptosis Assay
Principle: Primary human neutrophils treated with CDK9 inhibitors undergo apoptosis through transcriptional shutdown of survival genes, particularly Mcl-1 [86].
Materials:
- Primary human neutrophils isolated from healthy donors
- CDK9 inhibitors (R-roscovitine, DRB, iCDK9)
- LPS (E. coli O127:B8) for survival extension
- Annexin V/PI apoptosis detection kit
- Western blot reagents for Mcl-1, RNAP II phosphorylation
Procedure:
- Isolate human neutrophils from peripheral blood using density centrifugation
- Resuspend neutrophils in complete medium at 1×10^6^ cells/mL
- Pre-treat with LPS (100 ng/mL) for 1 hour to extend survival (optional)
- Add CDK9 inhibitors at optimized concentrations:
- R-roscovitine: 10-50 µM
- DRB: 10-30 µM
- iCDK9: 0.01-0.1 µM
- Incubate at 37°C for 2-24 hours
- Assess apoptosis by:
- Annexin V/PI staining and flow cytometry
- Morphological analysis of nuclear condensation
- Caspase-3 activation assays
- Analyze molecular mechanisms:
- Western blot for Mcl-1 degradation
- RNAP II phosphorylation status (Ser2, Ser5)
- Global transcriptional effects via microarray
CDK9 Degrader Evaluation in Inflammation Models
Principle: PROTAC-based CDK9 degraders offer enhanced efficacy over catalytic inhibitors by eliminating both enzymatic and scaffolding functions of CDK9 [88] [87].
Materials:
- CDK9-targeting PROTAC molecules (e.g., PO-8 series)
- LPS-stimulated RAW264.7 macrophage model
- Mouse model of acute lung injury (ALI)
- JAK-STAT signaling pathway reagents
Procedure:
- Treat LPS-stimulated RAW264.7 cells with iCDK9-based PROTAC molecules
- Assess cytotoxicity using MTT assay (24-48 hours)
- Measure inflammatory mediators:
- Nitric oxide production using Griess reagent
- TNF-α and IL-6 levels via ELISA
- Evaluate CDK9 degradation efficiency:
- Western blot for CDK9 protein levels
- Quantitative analysis of degradation kinetics
- Investigate mechanism of action:
- JAK2-STAT3 phosphorylation status
- RNAP II C-terminal domain phosphorylation
- Validate in vivo efficacy:
- Administer PROTACs in LPS-induced ALI mouse model
- Assess inflammatory cell infiltration in bronchoalveolar lavage fluid
- Measure cytokine levels in serum and lung tissue
Signaling Pathways and Experimental Workflows
Diagram 1: CDK9 Signaling in Neutrophil Apoptosis and Resolution Pathways. This diagram illustrates the core biological pathway of CDK9-mediated transcriptional regulation, intervention strategies for targeting CDK9, and the resulting physiological outcomes relevant to inflammation resolution.
Diagram 2: Experimental Workflows for CDK9 Inhibitor Validation. This diagram outlines the key methodological approaches for validating CDK9 inhibitors and degraders across in vivo, in vitro, and PROTAC development contexts.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for CDK9 Neutrophil Apoptosis Studies
| Reagent/Category | Specific Examples | Function/Application | Experimental Notes |
|---|---|---|---|
| CDK9 Inhibitors | R-roscovitine, DRB, AT7519, Flavopiridol, LDC000067, iCDK9 | Pharmacological inhibition of CDK9 kinase activity | Varying selectivity profiles; AT7519 and flavopiridol well-validated in zebrafish [84] |
| CDK9 Degraders | PO-8 series PROTACs | Targeted protein degradation via ubiquitin-proteasome system | Eliminates both enzymatic and scaffolding functions; enhanced efficacy over inhibition [87] |
| Genetic Tools | CDK9 morpholinos, CRISPR/Cas9 constructs | Genetic knockdown/knockout of CDK9 | Enables mechanistic validation; CDK9 knockout reduces neutrophil numbers by ~62% [84] |
| Model Organisms | Tg(mpx:EGFP) zebrafish | In vivo visualization of neutrophil dynamics | Enables real-time tracking of inflammation resolution [84] |
| Cell Systems | Primary human neutrophils, RAW264.7 macrophages | In vitro assessment of apoptosis and inflammation | Primary neutrophils essential for translational relevance [86] |
| Apoptosis Assays | TUNEL staining, Annexin V/PI, morphological analysis | Quantification of programmed cell death | Multi-method approach recommended for validation [84] [86] |
| Molecular Assays | Western blot (Mcl-1, p-RNAP II), ELISA (cytokines), microarray | Mechanistic studies of CDK9 inhibition | Monitor Mcl-1 depletion and RNAP II phosphorylation [86] |
Troubleshooting and Technical Considerations
Critical Parameters:
- Neutrophil Viability: Process primary human neutrophils within 2-3 hours of isolation for optimal viability [86]
- Inhibitor Specificity: Include appropriate controls to distinguish CDK9-specific effects from off-target activities
- Kinetic Considerations: CDK9 inhibition effects on transcription are rapid; time-course experiments are essential
Common Challenges and Solutions:
- Compensatory Mechanisms: CDK9 inhibition may trigger feedback loops; consider degradation as an alternative strategy [88]
- Cell-Type Specific Effects: CDK9 inhibition has distinct consequences in different immune cells; validate in relevant primary cells
- Translation to In Vivo: Consider pharmacokinetic properties when moving from cellular to animal models
CDK9 represents a genetically and pharmacologically validated target for promoting inflammation resolution through induction of neutrophil apoptosis. The integrated experimental approaches detailed in this application note—spanning in vivo zebrafish models, primary human neutrophil assays, and emerging PROTAC technologies—provide a robust framework for evaluating CDK9-targeting therapeutic strategies. These protocols enable comprehensive assessment of both efficacy and mechanism, supporting drug development efforts for inflammatory conditions characterized by dysregulated neutrophil survival.
Correlating Apoptotic Rates with Functional Resolution Biomarkers
The resolution of inflammation is an active, highly orchestrated process essential for restoring tissue homeostasis following injury or infection. Neutrophils, as the first responders of the innate immune system, play a pivotal role in both the initiation and resolution of inflammatory responses [2]. The apoptotic rate of neutrophils serves as a critical control point for inflammation resolution, governing the safe removal of these cells and subsequent promotion of healing processes [1]. This application note explores the quantitative relationship between neutrophil apoptotic rates and functional resolution biomarkers, providing detailed methodologies for researchers investigating inflammatory pathways and therapeutic development. The precise measurement of apoptosis, coupled with assessment of downstream resolution biomarkers, offers valuable insights into the inflammatory status and enables screening of potential pro-resolving therapeutic compounds [1] [2]. Within the broader context of neutrophil apoptosis assays in inflammation resolution research, establishing robust correlations between apoptotic indices and functional resolution parameters is fundamental for understanding disease mechanisms and developing targeted interventions.
Quantitative Data on Neutrophil Apoptosis and Resolution
Apoptotic Rates in Normal and Disease States
Table 1: Quantification of Neutrophil Apoptotic Rates in Homeostasis and Disease
| Condition | Apoptotic Rate (γ, /day) | Fold Change vs. Normal | Half-life of Apoptotic Cells | Influx to Efflux Ratio (V₀/GTR) | Reference |
|---|---|---|---|---|---|
| Normal Individuals | 0.28 ± 0.02 | 1.0x | 10.4 hours | 2.3 | [89] |
| Cyclical Neutropenia | ~3.64 | ~13x | 1.4 hours | N/D | [89] |
| Severe Congenital Neutropenia | ~3.64 | ~13x | ~0.6 hours | N/D | [89] |
| Myelokathexis | ~4.76 | ~17x | 0.4 hours | N/D | [89] |
Mathematical modeling of apoptosis in post-mitotic neutrophil precursors (CD15+ cells) reveals that approximately 55% of cells entering this compartment undergo apoptosis before release into circulation under normal conditions [89]. This significant apoptotic rate in the bone marrow highlights the importance of programmed cell death in maintaining neutrophil homeostasis even before cells enter the periphery. In pathological states such as congenital neutropenias, dramatically elevated apoptotic rates (13-17 times normal) contribute to neutrophil deficiency by drastically shortening cellular lifespan [89].
Functional Biomarkers of Resolution
Table 2: Key Functional Resolution Biomarkers and Their Sources
| Biomarker Category | Specific Molecule | Cellular Source | Functional Role in Resolution | Correlation with Apoptosis |
|---|---|---|---|---|
| Lipid Mediators | Lipoxin A4, Resolvins | Neutrophils, Platelets, Macrophages | Limit neutrophil trafficking, promote efferocytosis | Positive [1] [2] |
| Protein Mediators | Annexin A1 | Neutrophils, Epithelial cells | "Find-me" signal, inhibits neutrophil recruitment | Positive [2] [7] |
| Anti-inflammatory Cytokines | TGF-β, IL-10 | Efferocytosing Neutrophils, M2 Macrophages | Suppress pro-inflammatory cytokines, promote tissue repair | Positive [1] [7] |
| Growth Factors | HGF, FGF2, VEGF | Efferocytosing Neutrophils | Tissue regeneration, angiogenesis | Positive [7] |
| Surface "Eat-me" Signals | Phosphatidylserine (PS) | Apoptotic Neutrophils | Recognition and engulfment by phagocytes | Direct marker [7] |
| Pro-inflammatory Cytokines | TNF-α, IL-1β, IL-6 | Activated Neutrophils, M1 Macrophages | Propagate inflammatory response | Negative [7] |
The transition from inflammation to resolution is characterized by a shift in the lipid mediator profile from pro-inflammatory prostaglandins and leukotrienes to specialized pro-resolving mediators (SPMs) including lipoxins, resolvins, protectins, and maresins [2]. These mediators function as agonists of resolution by actively limiting further neutrophil infiltration and promoting the uptake of apoptotic neutrophils. The phagocytic clearance (efferocytosis) of apoptotic neutrophils by macrophages leads to the production of anti-inflammatory cytokines like TGF-β and IL-10, which further suppress inflammation and promote tissue repair [1] [7]. Recent evidence indicates that neutrophils themselves can perform efferocytosis, a process termed "neutrophil cannibalism," which is associated with the secretion of pro-resolving mediators including TGF-β, VEGF, and lipoxin A4 [7].
Experimental Protocols for Correlation Studies
Protocol 1: Quantification of Neutrophil Apoptotic Rate
Objective: To accurately measure the rate of apoptosis in neutrophil populations using flow cytometry.
Materials:
- Freshly isolated human neutrophils from peripheral blood
- Annexin V-FITC and Propidium Iodide (PI) from commercial apoptosis detection kit
- RPMI 1640 medium supplemented with 10% autologous serum
- Flow cytometer with appropriate filters for FITC and PI detection
- Cell culture incubator maintained at 37°C with 5% CO₂
Procedure:
- Isolate neutrophils from heparinized venous blood using density gradient centrifugation.
- Resuspend neutrophils at a density of 3-20 × 10ⴠcells/mL in RPMI 1640 with 10% autologous serum.
- Culture cells in a 5% CO₂ incubator at 37°C for 0-24 hours based on experimental requirements.
- At each timepoint, harvest cells and label with FITC-conjugated Annexin V and PI for 20 minutes at room temperature, protected from light.
- Wash cells twice with cold PBS and analyze immediately by flow cytometry, collecting a minimum of 10,000 events per sample.
- Analyze data using flow cytometry software to determine the percentage of cells in each quadrant:
- Annexin Vâ»/PIâ»: Viable, non-apoptotic cells
- Annexin Vâº/PIâ»: Early apoptotic cells
- Annexin Vâº/PIâº: Late apoptotic cells
- Annexin Vâ»/PIâº: Necrotic cells
Data Analysis: Calculate the apoptotic rate (γ) using mathematical modeling that incorporates the fraction of apoptotic cells (fâ‚), total post-mitotic population, and duration of the post-mitotic compartment [89]. The formula for the apoptotic rate is derived from the balance between cell influx, apoptosis, and efflux to circulation.
Protocol 2: Assessment of Functional Resolution Biomarkers
Objective: To measure the production of pro-resolving mediators following neutrophil apoptosis.
Materials:
- Cell culture supernatants from apoptosis assays
- ELISA kits for TGF-β, IL-10, Annexin A1, and Lipoxin A4
- Macrophage cell line (e.g., RAW 264.7) for efferocytosis assays
- Flow cytometer or confocal microscope for phagocytosis quantification
- Western blot equipment and antibodies for M1/M2 macrophage markers (iNOS, Arg1)
Procedure for Biomarker Measurement:
- Collect supernatant from neutrophil apoptosis cultures at various timepoints.
- Concentrate samples if necessary using centrifugal filter devices.
- Perform ELISA assays according to manufacturer protocols to quantify levels of TGF-β, IL-10, Annexin A1, and Lipoxin A4.
- Correlate mediator concentrations with the percentage of apoptotic neutrophils at corresponding timepoints.
Procedure for Efferocytosis Assay:
- Label apoptotic neutrophils with a fluorescent cell tracker dye (e.g., CFSE).
- Co-culture labeled apoptotic neutrophils with macrophages at a 5:1 ratio for 2 hours.
- Remove non-engulfed neutrophils by gentle washing.
- Analyze macrophages by flow cytometry or fluorescence microscopy to determine the percentage that has phagocytosed apoptotic cells.
- Alternatively, use flow cytometry to measure the expression of M2 macrophage markers (CD206, Arg1) following efferocytosis.
Data Analysis: Calculate correlation coefficients between apoptotic rates and resolution biomarker levels. Statistical significance can be determined using Pearson correlation analysis with p-values <0.05 considered significant.
Signaling Pathways Regulating Neutrophil Apoptosis and Resolution
The Mac-1 integrin (CD11b/CD18) serves as a bidirectional regulator of neutrophil apoptosis, generating contrasting signals depending on ligand engagement [1] [2]. When Mac-1 binds to certain ligands including fibrinogen or myeloperoxidase (MPO), it transduces survival signals that stabilize the anti-apoptotic protein Mcl-1, thereby extending neutrophil lifespan at inflammatory sites [1] [2]. Conversely, Mac-1-mediated phagocytosis of bacteria triggers a caspase-8-dependent apoptotic pathway that overrides these survival signals [2]. Specialized pro-resolving mediators like lipoxin A4 (LXA4) signal through the ALX/FPR2 receptor to promote neutrophil apoptosis by activating caspase pathways and accelerating Mcl-1 degradation [1] [2]. The central regulator of neutrophil survival is Mcl-1, which has a very short half-life and requires continuous expression to prevent apoptosis [1]. Following apoptosis, neutrophils expose phosphatidylserine (PS) on their surface, which serves as a key "eat-me" signal for efferocytosis by macrophages and other neutrophils [7]. This clearance process stimulates the production of functional resolution biomarkers including TGF-β, IL-10, and lipoxin A4, which actively promote tissue repair and restoration of homeostasis [7].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Neutrophil Apoptosis and Resolution Studies
| Reagent Category | Specific Product/Assay | Supplier Examples | Functional Application | Key Readouts |
|---|---|---|---|---|
| Apoptosis Detection | Annexin V/PI Apoptosis Detection Kit | R&D Systems, BioLegend | Differentiate early/late apoptosis vs. necrosis | % Annexin Vâº/PIâ» (early apoptotic) |
| Caspase Activity Assays | Caspase-8, Caspase-3 Activity Kits | Cell Signaling Technology, Abcam | Measure key executioner caspases in apoptosis | Caspase activity (fluorescence) |
| Flow Cytometry Antibodies | Anti-CD11b, Anti-CD66b, Anti-CD16 | BD Biosciences, BioLegend | Neutrophil identification and phenotyping | Surface marker expression |
| ELISA Kits | Human TGF-β, IL-10, Annexin A1 ELISA | R&D Systems, Thermo Fisher | Quantify resolution biomarkers in supernatant | Cytokine concentration (pg/mL) |
| Macrophage Polarization | Anti-iNOS, Anti-Arginase-1 Antibodies | Cell Signaling Technology, Abcam | Detect M1 vs. M2 macrophage phenotypes | Western blot, flow cytometry |
| Lipid Mediator Analysis | Lipoxin A4, Resolvin E1 EIA Kits | Cayman Chemical | Measure specialized pro-resolving mediators | SPM concentration (pg/mL) |
| Recombinant Proteins | Recombinant Annexin A1, GAS6 | R&D Systems, Sino Biological | Functional studies of resolution mechanisms | Efferocytosis efficiency |
| Signal Transduction Inhibitors Mcl-1, Caspase-8 inhibitors | Selleck Chemicals, Tocris | Pathway manipulation experiments | Apoptotic rate modulation |
The selection of appropriate research reagents is critical for accurate assessment of neutrophil apoptosis and resolution biomarkers. Annexin V/PI staining remains the gold standard for quantifying apoptotic rates, allowing discrimination between early apoptosis (Annexin Vâº/PIâ»), late apoptosis (Annexin Vâº/PIâº), and necrosis (Annexin Vâ»/PIâº) [89] [90]. For signaling studies, antibodies against key regulatory proteins such as Mcl-1, Bax, and Bak enable investigation of the Bcl-2 family balance that controls neutrophil lifespan [1] [90]. The assessment of functional resolution requires reliable detection methods for anti-inflammatory cytokines (TGF-β, IL-10) and specialized pro-resolving mediators (lipoxin A4, resolvins) that are produced following efferocytosis of apoptotic neutrophils [2] [7]. Furthermore, reagents for analyzing macrophage polarization (iNOS for M1, Arg1 for M2) provide insights into the downstream consequences of neutrophil clearance on the overall inflammatory microenvironment [7].
Comparative Analysis of Apoptosis-Inducing Agents and Their Mechanisms
Apoptosis, or programmed cell death, is a fundamental physiological process essential for maintaining tissue homeostasis by eliminating damaged or unwanted cells without inducing inflammation [91]. Within the context of inflammation resolution, neutrophil apoptosis is particularly critical. Neutrophils are the most abundant circulating leukocytes and key players in the innate immune response, rapidly recruited to sites of infection and injury [2] [92]. However, their powerful antimicrobial mechanisms can cause collateral tissue damage, making their timely removal through apoptosis vital for resolving inflammatory responses and preventing chronic inflammation [2] [7]. The molecular mechanisms of apoptosis are complex, involving intricate signaling pathways that can be targeted by specific inducing agents, making them valuable tools for both basic research and therapeutic development [91] [93]. This application note provides a comparative analysis of these agents and detailed protocols for their use in neutrophil apoptosis assays within inflammation resolution research.
Apoptosis Signaling Pathways: Molecular Mechanisms
Apoptosis proceeds primarily through two interconnected signaling pathways: the intrinsic (mitochondrial) pathway and the extrinsic (death receptor) pathway [91] [93]. Both converge on the activation of executioner caspases that mediate the characteristic biochemical and morphological changes associated with apoptotic cell death.
The Intrinsic Apoptotic Pathway
The intrinsic pathway is initiated internally in response to cellular stresses including DNA damage, reactive oxygen species, or lack of essential survival signals [93]. This pathway is tightly regulated by the B-cell lymphoma 2 (BCL-2) family of proteins, which balance the decision between cell survival and death [93]. Key events in this pathway include:
- BCL-2 Family Regulation: Anti-apoptotic members (BCL-2, BCL-XL, MCL-1) promote cell survival, while pro-apoptotic BH3-only proteins (BIM, PUMA, NOXA, BID) and effector proteins (BAX, BAK) promote cell death [93].
- Mitochondrial Outer Membrane Permeabilization (MOMP): Pro-apoptotic BAX and BAK oligomerize to form pores in the mitochondrial membrane, leading to the release of cytochrome c and other pro-apoptotic factors [91] [93].
- Apoptosome Formation: Cytochrome c forms a complex with apoptotic protease-activating factor 1 (APAF1) and procaspase-9, termed the apoptosome, where procaspase-9 is activated [93].
- Caspase Activation: Activated caspase-9 triggers a proteolytic cascade involving executioner caspases-3, -6, and -7, leading to the systematic dismantling of cellular components [91] [93].
The Extrinsic Apoptotic Pathway
The extrinsic pathway is initiated by the binding of death ligands to their cognate receptors at the plasma membrane [91] [93]. Key components include:
- Death Receptor Activation: Ligands such as tumor necrosis factor (TNF)-related apoptosis-inducing ligand (TRAIL) bind to TRAIL receptors (DR4/DR5), while Fas ligand binds to Fas (CD95) [93] [94].
- Death-Inducing Signaling Complex (DISC) Formation: Receptor ligation recruits the adaptor protein FADD and procaspase-8 to form the DISC [93].
- Caspase Activation Cascade: Within the DISC, procaspase-8 undergoes proximity-induced dimerization and activation [93]. Active caspase-8 can directly activate executioner caspases or cleave the BH3-protein BID to truncated tBID, which amplifies the death signal through the mitochondrial pathway [93].
The following diagram illustrates the key components and interactions within these core apoptotic pathways:
Comparative Analysis of Apoptosis-Inducing Agents
Apoptosis-inducing agents are valuable research tools for investigating death pathways and have significant therapeutic potential. The table below provides a comprehensive comparison of common inducers, their mechanisms, and research applications.
Table 1: Characterization of Common Apoptosis-Inducing Agents
| Agent | Primary Mechanism | Pathway Targeted | Key Molecular Targets | Research Applications |
|---|---|---|---|---|
| Staurosporine | Broad-spectrum protein kinase inhibitor [95] | Intrinsic [95] | Multiple protein kinases [95] | General apoptosis inducer; positive control studies [95] |
| ABD 5582 | Dimeric Smac mimetic; potent IAP inhibitor [95] | Both (via IAP inhibition) [95] | IAP proteins (XIAP, cIAP1) [95] [96] | Overcoming apoptosis resistance; cancer research [95] [96] |
| Camptothecin | Topoisomerase I inhibitor [95] | Intrinsic [95] | Topoisomerase I-DNA complex [95] | DNA damage-induced apoptosis studies [95] |
| Cisplatin | Platinum agent; induces DNA damage [95] | Intrinsic [95] | DNA (cross-links) [95] | Chemotherapy response; DNA damage signaling [95] |
| Doxorubicin | Antitumor antibiotic; inhibits DNA topoisomerase II [95] | Intrinsic [95] | DNA topoisomerase II [95] | Cancer research; cardiotoxicity studies [95] [97] |
| Etoposide | Topoisomerase II inhibitor [95] | Intrinsic [95] | Topoisomerase II [95] | Cell cycle-related apoptosis studies [95] |
| Nutlin-3 | MDM2 antagonist; inhibits MDM2-p53 interaction [95] | Intrinsic [95] | MDM2-p53 interaction [95] | p53 pathway studies; cancer therapeutics [95] [96] |
| Paclitaxel | Promotes assembly and inhibits disassembly of microtubules [95] | Intrinsic [95] | Microtubules [95] | Mitotic catastrophe studies; cancer research [95] |
| TRAIL | Death receptor agonist [98] [93] | Extrinsic [98] [93] | TRAIL receptors (DR4/DR5) [98] [93] | Cancer-specific apoptosis; therapeutic development [98] [93] |
| Necrostatin-1 | Induces caspase-dependent neutrophil apoptosis [92] | Intrinsic (neutrophils) [92] | Reduces Mcl-1, increases Bax [92] | Inflammation resolution studies; neutrophil apoptosis [92] |
| Venetoclax (ABT-199) | BH3 mimetic; BCL-2 inhibitor [98] [93] | Intrinsic [98] [93] | BCL-2 protein [98] [93] | Hematological malignancies; BCL-2 dependency studies [98] [93] |
| PRIMA-1MET | Restores mutant p53 activity [95] [98] | Intrinsic [95] [98] | Mutant p53 [95] [98] | p53 mutation cancer models; reactivation strategies [95] [98] |
The selection of appropriate apoptosis-inducing agents depends on the specific research context, particularly when studying neutrophil biology in inflammation resolution. The following diagram illustrates a decision framework for selecting agents based on research goals:
Experimental Protocols for Neutrophil Apoptosis Assays
Protocol 1: Assessment of Neutrophil Apoptosis Using Flow Cytometry
This protocol describes a standardized method for quantifying neutrophil apoptosis using Annexin V/propidium iodide (PI) staining and flow cytometry, suitable for screening apoptosis-inducing agents.
4.1.1 Materials and Reagents
- Isolated human neutrophils (from peripheral blood via density gradient centrifugation) [92]
- Apoptosis-inducing agents (e.g., Staurosporine, Necrostatin-1) [95] [92]
- RPMI 1640 medium supplemented with 10% fetal bovine serum [92]
- Annexin V-FITC conjugate [92]
- Propidium iodide (PI) staining solution [92]
- Phosphate-buffered saline (PBS), calcium and magnesium-free
- Flow cytometry tubes
- CO₂ incubator (37°C, 5% CO₂)
- Flow cytometer with FITC and PI detection capabilities
4.1.2 Procedure
- Neutrophil Isolation and Seeding: Isolate neutrophils from human peripheral blood through density gradient centrifugation. Seed neutrophils in 24-well plates at a density of 5×10ⶠcells/mL in RPMI 1640 medium with 10% FBS [92].
- Agent Treatment: Prepare stock solutions of apoptosis-inducing agents and dilute to appropriate working concentrations in culture medium. Treat neutrophils with varying concentrations of agents (e.g., Necrostatin-1 at 20μM, 50μM, and 100μM) [92]. Include untreated controls and vehicle controls if applicable.
- Incubation: Incubate cells for 3-20 hours at 37°C in a 5% CO₂ humidified incubator. Time points may vary based on the agent's mechanism and potency [92].
- Sample Harvesting and Staining:
- Harvest cells by gentle pipetting and transfer to flow cytometry tubes.
- Wash cells once with cold PBS.
- Resuspend cells in Annexin V binding buffer.
- Add Annexin V-FITC and PI according to manufacturer's instructions.
- Incubate for 15 minutes at room temperature in the dark.
- Flow Cytometric Analysis:
- Analyze samples within 1 hour using a flow cytometer.
- Collect a minimum of 10,000 events per sample.
- Use FITC channel for Annexin V detection and PI channel for propidium iodide.
- Data Analysis:
- Identify viable cells (Annexin Vâ»/PIâ»), early apoptotic cells (Annexin Vâº/PIâ»), late apoptotic cells (Annexin Vâº/PIâº), and necrotic cells (Annexin Vâ»/PIâº).
- Calculate the percentage of total apoptotic cells (early + late apoptotic populations) [92].
Protocol 2: Morphological Assessment of Neutrophil Apoptosis
This protocol utilizes nuclear staining to identify characteristic apoptotic morphology in neutrophils, providing complementary data to flow cytometric methods.
4.2.1 Materials and Reagents
- Isolated human neutrophils
- Apoptosis-inducing agents
- Cell culture medium
- Hoechst 33342 staining solution (or similar membrane-permeable DNA dye) [92]
- Glass slides and coverslips
- Fluorescence microscope with DAPI/blue filter set
- Cytospin centrifuge (optional)
4.2.2 Procedure
- Cell Treatment: Seed and treat neutrophils with apoptosis-inducing agents as described in Protocol 1, steps 1-3 [92].
- Nuclear Staining:
- Add Hoechst 33342 to cell culture at a final concentration of 1-5 μg/mL.
- Incubate for 15-20 minutes at 37°C.
- Sample Preparation:
- Option A: Direct observation - Place an aliquot of cell suspension on a glass slide and apply coverslip.
- Option B: Cytospin preparation - Centrifuge cells onto glass slides using a cytospin centrifuge, then apply mounting medium and coverslip.
- Microscopic Evaluation:
- Examine cells using a fluorescence microscope with appropriate filters.
- Identify apoptotic neutrophils by characteristic nuclear morphology: chromatin condensation, nuclear fragmentation, and formation of apoptotic bodies [92].
- Count a minimum of 200 cells per sample to determine the percentage of apoptotic cells.
- Documentation: Capture representative images for each treatment condition.
Protocol Optimization Notes
- Dose-Response Relationships: Perform initial dose-ranging experiments for each agent. Effective doses are dependent on cellular context and should be determined empirically [95].
- Time Course Considerations: If inducing apoptosis at a low dose or with a mild stimulus, longer treatment times may be necessary [95].
- Control Requirements: Include both positive (e.g., staurosporine-treated) and negative (vehicle-treated) controls in all experiments. Negative controls are essential for assessing baseline cell health and vehicle effects [95].
- Neutrophil Viability: Use freshly isolated neutrophils within 2-4 hours of isolation to maintain viability and prevent spontaneous apoptosis.
The following workflow diagram illustrates the integration of these protocols in a comprehensive neutrophil apoptosis assessment:
The Scientist's Toolkit: Essential Research Reagents
The following table compiles key reagents essential for conducting apoptosis research, particularly focused on neutrophil studies in inflammation resolution.
Table 2: Essential Research Reagents for Apoptosis Studies
| Category | Reagent | Specific Function | Research Applications |
|---|---|---|---|
| Apoptosis Inducers | Staurosporine | Broad-spectrum protein kinase inhibitor [95] | Positive control; general apoptosis induction [95] |
| Necrostatin-1 | Induces neutrophil apoptosis via Mcl-1 reduction and Bax enhancement [92] | Neutrophil-specific apoptosis; inflammation resolution studies [92] | |
| ABD 5582 (Smac mimetic) | Potent IAP inhibitor promoting caspase activation [95] | Overcoming apoptosis resistance; cancer research [95] [96] | |
| Caspase Inhibitors | Z-VAD-FMK | Irreversible pan-caspase inhibitor [95] | Caspase-dependency confirmation; blocking apoptotic execution [95] |
| Q-VD-OPH | Less toxic irreversible pan-caspase inhibitor; used in in-vivo studies [95] | In vivo apoptosis inhibition; caspase function studies [95] | |
| Z-DEVD-FMK | Irreversible inhibitor of caspase-3 [95] | Executioner caspase inhibition; mechanism studies [95] | |
| Detection Reagents | Annexin V conjugates | Binds phosphatidylserine externalized on apoptotic cells [92] | Flow cytometry; microscopy detection of early apoptosis [92] |
| Propidium Iodide (PI) | DNA intercalating dye impermeant to live cells [92] | Membrane integrity assessment; necrotic cell identification [92] | |
| Hoechst 33342 | Cell-permeable DNA stain for nuclear morphology [92] | Apoptotic nuclear changes; microscopy-based assays [92] | |
| Molecular Tools | Mcl-1 antibodies | Detects key anti-apoptotic protein regulating neutrophil lifespan [92] | Western blot; immunohistochemistry for survival signaling [92] |
| Bax/Bak antibodies | Detect pro-apoptotic BCL-2 family effectors [93] | Intrinsic pathway activation; mitochondrial studies [93] | |
| Cleaved caspase-3 antibodies | Detects activated executioner caspase [91] | Apoptosis confirmation; pathway activation studies [91] |
The strategic application of apoptosis-inducing agents provides powerful insights into the molecular regulation of programmed cell death, with particular relevance to inflammation resolution through neutrophil apoptosis. This comparative analysis demonstrates that agent selection should be guided by specific research goals, whether targeting intrinsic or extrinsic pathways, requiring broad or specific induction, or focusing on neutrophil-specific apoptosis. The experimental protocols outlined here provide standardized methodologies for assessing apoptotic responses, with flow cytometry offering quantitative analysis and morphological methods providing complementary structural insights. As research in this field advances, the continued refinement of these apoptotic agents and assessment techniques will enhance our understanding of inflammation resolution mechanisms and support the development of novel therapeutic strategies for inflammatory diseases.
Integrating Apoptosis Data with Other Resolution Parameters (e.g., Cytokine Profiles, Macrophage Phenotype)
In inflammation resolution research, neutrophil apoptosis is a critical, highly regulated event that must occur in a timely manner to prevent persistent inflammation and tissue damage. Accurately assaying this form of programmed cell death and correlating it with key resolution parameters provides a powerful systems biology approach to understanding inflammatory pathways. This application note provides detailed methodologies for the simultaneous quantification of neutrophil apoptosis alongside cytokine profiling and macrophage phenotyping, enabling researchers to build a comprehensive picture of the resolution process. The protocols are designed for integration, allowing for the efficient use of precious samples and the discovery of functional relationships between cell death fate and the immune microenvironment.
Theoretical Background and Key Apoptosis Markers
The Centrality of Apoptosis in Resolution
Apoptosis is a form of regulated cell death characterized by distinct morphological features: cell shrinkage, membrane blebbing, chromosome condensation, nuclear fragmentation, and the formation of apoptotic bodies that are swiftly phagocytosed by surrounding cells without provoking an inflammatory response [99] [100]. In the context of neutrophilic inflammation, the non-phlogistic nature of this process is fundamental. The swift and silent phagocytosis of apoptotic neutrophils by macrophages (a process known as efferocytosis) not only removes these potentially harmful cells but also actively instructs macrophages to adopt a pro-resolving, anti-inflammatory phenotype [100]. This transition is a cornerstone of inflammation resolution, making the simultaneous measurement of apoptosis and macrophage phenotype particularly insightful.
A Cascade of Biochemical Markers
The process of apoptosis is orchestrated by a cascade of biochemical events, which can be harnessed for its detection. The table below summarizes the primary markers and the corresponding detection methods, which can be leveraged in a multiplexed experimental design.
Table 1: Key Apoptosis Markers and Detection Methods
| Apoptosis Marker | Detection Method(s) | Key Characteristics |
|---|---|---|
| Phosphatidylserine (PS) Exposure | Flow cytometry with Annexin V staining [99] [101] [102] | Early-stage marker; requires viable cells; distinguishes apoptotic from necrotic cells. |
| Caspase Activation | Fluorometric substrate-based assays (e.g., for Caspase-3/7) [99] [103] | Commits cell to irreversible apoptosis; can be detected with live-cell analysis. |
| Mitochondrial Membrane Potential (ΔΨm) Loss | Flow cytometry/microscopy with JC-1 or similar probes [104] | Indicates intrinsic apoptosis pathway involvement. |
| DNA Fragmentation | TUNEL Assay [104] [99] | Late-stage marker; high sensitivity. |
| Chromatin Condensation | Microscopy analysis with DNA-binding dyes [99] | Morphological hallmark of terminal apoptosis. |
| Cell Membrane Permeability | Staining with propidium iodide (PI) or 7-AAD [105] [99] [101] | Distinguishes late apoptotic/necrotic cells (PI-positive) from early apoptotic cells (PI-negative). |
The following diagram illustrates the temporal relationship of these key apoptotic events and the points at which they can be measured in relation to macrophage efferocytosis and cytokine signaling, forming the basis for integrated assay design.
Diagram 1: Integrated apoptotic and resolution signaling.
Experimental Protocols for Integrated Assays
Multiplexed Apoptosis Assay via Flow Cytometry (Annexin V/PI)
This protocol is a workhorse for quantifying early and late apoptosis in neutrophil populations and can be easily paired with subsequent assays on supernatant or sorted cells [101] [102].
Materials & Reagents:
- Annexin V-FITC conjugate (e.g., from Annexin V FLUOS staining kit, Roche) [101]
- Propidium Iodide (PI) solution [101]
- 10X Binding Buffer (dilute to 1X with dHâ‚‚O for use) [102]
- PBS buffer (pH 7.4)
- Flow cytometer
Procedure:
- Cell Preparation: Seed and treat neutrophils (e.g., (1 \times 10^6) cells) in appropriate culture flasks. After incubation, collect both the supernatant (containing floating cells) and adherent cells (by gentle trypsinization), combining them for a complete representation [101].
- Washing: Wash the collected cells twice with cold 1X PBS by gentle centrifugation (670 × g, 5 min, RT) [101].
- Staining Cocktail: For each sample, prepare a 100 µL incubation reagent on ice, protected from light:
- 10 µL 10X Binding Buffer
- 10 µL Propidium Iodide solution
- 1 µL Annexin V-FITC
- 79 µL dH₂O [102]
- Staining: Gently resuspend each washed cell pellet in 100 µL of the staining cocktail.
- Incubation: Incubate in the dark for 15 minutes at room temperature [102].
- Dilution and Analysis: Add 400 µL of 1X Binding Buffer to each reaction tube. Analyze by flow cytometry within 1 hour [102].
Data Interpretation:
- Annexin V–/PI–: Viable, non-apoptotic cells.
- Annexin V+/PI–: Early apoptotic cells.
- Annexin V+/PI+: Late apoptotic or necrotic cells [101].
Live-Cell Kinetic Analysis of Apoptosis (Caspase-3/7 Activation)
This protocol enables real-time, non-invasive monitoring of apoptosis, ideal for kinetic studies and multiplexing with other live-cell dyes [103].
Materials & Reagents:
- Incucyte Caspase-3/7 Dye (Green or Red): Inert, non-fluorescent substrates that are cleaved by activated caspase-3/7 to release a DNA-binding fluorescent dye [103].
- Incucyte Live-Cell Analysis System (or similar live-cell imager) [103].
Procedure:
- Plating: Plate cells in a 96- or 384-well microplate.
- Treatment and Staining: Add your experimental treatments along with the Incucyte Caspase-3/7 Dye directly to the culture medium. No washing is required.
- Kinetic Reading: Place the plate in the Incucyte system for automated, time-lapse imaging inside the incubator. Data collection can run from 0 to over 10 days.
- Analysis: Use integrated software tools to automatically quantify the number of fluorescently labeled (apoptotic) cells in each well over time [103].
Correlative Analysis of Apoptosis and Macrophage Phenotype
This section outlines a strategy for connecting neutrophil apoptosis data with macrophage polarization states.
Workflow:
- Co-culture Setup: Establish a co-culture system of neutrophils and macrophages. Induce neutrophil apoptosis or use a resolution model.
- Apoptosis Measurement: At defined time points, use the flow cytometry (Protocol 3.1) or live-cell analysis (Protocol 3.2) protocol to quantify neutrophil apoptosis.
- Macrophage Phenotyping: Harvest macrophages from the same co-culture well.
- Surface Marker Analysis by Flow Cytometry: Stain for pro-inflammatory (e.g., CD86, MHC-II) and pro-resolving (e.g., CD206, CD163) surface markers.
- Intracellular Cytokine Staining: After stimulation with a protein transport inhibitor (e.g., Brefeldin A), fix and permeabilize macrophages. Stain for intracellular cytokines like TNF-α (pro-inflammatory) or IL-10 (pro-resolving) [99].
- Supernatant Collection: Collect culture supernatants from parallel wells at the same time points for cytokine profiling (see Protocol 3.4).
Cytokine Profiling from Culture Supernatants
The soluble factor milieu is a key parameter that bridges cellular events.
Procedure:
- Sample Collection: Centrifuge cell cultures at specified time points and carefully collect the supernatant.
- Clarification and Storage: Clarify the supernatant by a second centrifugation (e.g., 1000 × g, 10 min) to remove any remaining cells or debris. Aliquot and store at ≤ –80°C to prevent cytokine degradation.
- Multiplex Immunoassay: Use a multiplex bead-based immunoassay (e.g., Luminex) or a proximity ligation assay (e.g., Olink) according to the manufacturer's instructions to simultaneously quantify a panel of pro-inflammatory (e.g., TNF-α, IL-6, IL-1β, IL-8) and pro-resolving (e.g., TGF-β, IL-10) cytokines from a single, small volume of supernatant.
The following workflow diagram provides a visual guide for integrating these protocols into a single, cohesive experimental plan.
Diagram 2: Integrated experimental workflow.
Table 2: Key Research Reagent Solutions for Integrated Apoptosis and Resolution Studies
| Reagent / Assay | Function / Target | Example Application |
|---|---|---|
| Annexin V Conjugates (FITC, PE, Cy5) [99] | Binds exposed phosphatidylserine (PS) on apoptotic cell surfaces. | Flow cytometric distinction of early apoptotic cells. |
| Caspase-3/7 Fluorogenic Substrates (e.g., Incucyte Dyes) [103] | Cleaved by activated executioner caspases, releasing a fluorescent signal. | Real-time, kinetic measurement of irreversible apoptotic commitment in live cells. |
| Mitochondrial Probes (e.g., JC-1) [104] | Detects loss of mitochondrial membrane potential (ΔΨm). | Investigating the intrinsic (mitochondrial) apoptosis pathway. |
| TUNEL Assay Kits [104] [99] | Labels DNA strand breaks (nicks) via terminal deoxynucleotidyl transferase (TdT). | Highly sensitive detection of late-stage apoptotic cells with DNA fragmentation. |
| Propidium Iodide (PI) / 7-AAD [105] [99] | Membrane-impermeable DNA dyes that stain cells with compromised membrane integrity. | Discriminating late apoptotic and necrotic cells from early apoptotic cells. |
| Multiplex Cytokine Panels (e.g., Luminex) | Simultaneously quantifies multiple cytokines/chemokines from a small sample volume. | Profiling the inflammatory and resolving secretome. |
| Macrophage Phenotyping Antibodies (e.g., anti-CD86, anti-CD206) [99] | Labels surface markers indicative of macrophage polarization (M1 vs. M2). | Characterizing the functional state of macrophages in response to efferocytosis. |
Data Integration and Analysis Strategy
The power of these integrated protocols lies in the correlative analysis of the generated data. The objective is to move beyond independent datasets to a unified model of resolution.
- Temporal Correlation: Plot kinetic apoptosis data (from Protocol 3.2) alongside cytokine concentration data (from Protocol 3.4) on the same timeline. This can reveal, for instance, whether a spike in a specific pro-resolving cytokine (e.g., TGF-β) follows the peak of neutrophil apoptosis.
- Endpoint Correlation Analysis: At a key endpoint, compare the percentage of apoptotic neutrophils (from Protocol 3.1) with the percentage of pro-resolving macrophages (from Protocol 3.3, e.g., CD206+ cells) across different experimental conditions using scatter plots and statistical correlation tests (e.g., Pearson's r).
- Multivariate Analysis: For more complex datasets, employ multivariate analyses such as Principal Component Analysis (PCA). This can help visualize how different experimental treatments cluster based on their combined apoptosis, cytokine, and phenotype profiles, identifying the most influential variables driving resolution.
By adopting this multi-parametric approach, researchers can transition from observing isolated events to deciphering the functional interactions that define successful inflammation resolution, accelerating the identification of novel therapeutic targets for chronic inflammatory diseases.
Conclusion
The precise assessment of neutrophil apoptosis is indispensable for understanding and therapeutically manipulating the resolution of inflammation. This guide synthesizes key takeaways: that apoptosis is a non-phlogistic process crucial for safe neutrophil removal, that a multifaceted assay approach—from optimized in vitro flow cytometry to validated in vivo models—is required for robust data generation, and that pre-analytical variables profoundly impact results. Future directions should focus on developing even more standardized protocols, further exploring the genetic programs governing apoptotic delay in different inflammatory milieus, and translating these assay insights into clinical trials for CDK inhibitors and other novel pro-resolution therapeutics targeting neutrophil lifespan. The ultimate goal is to harness neutrophil apoptosis as a powerful lever to resolve inflammation and restore tissue homeostasis in chronic human diseases.
References
- 1. Modulation of Neutrophil Apoptosis and the Resolution of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3589696/]
- 2. Targeting Neutrophils for Promoting the Resolution of ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2022.866747/full]
- 3. Specialized pro-resolving mediators in neutrophil ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1589923/full]
- 4. Tumor cells that resist neutrophil anticancer cytotoxicity ... [https://www.nature.com/articles/s41423-025-01283-w]
- 5. Spatiotemporal control of neutrophil fate to tune ... [https://www.nature.com/articles/s41467-024-52812-6]
- 6. In situ neutrophil apoptosis and macrophage efferocytosis ... [https://www.sciencedirect.com/science/article/pii/S0168365924001822]
- 7. Clearance of apoptotic cells by neutrophils in inflammation ... [https://www.nature.com/articles/s41420-024-01809-7]
- 8. Downregulation of Mcl-1 has anti-inflammatory pro-resolution ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3940382/]
- 9. Regulation of Neutrophil Survival/Apoptosis by Mcl-1 - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3217587/]
- 10. Effective Caspase Inhibition Blocks Neutrophil Apoptosis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3017075/]
- 11. Improved apoptosis detection in ovine neutrophils by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2267505/]
- 12. Optimization of methods for the accurate characterization ... [https://www.nature.com/articles/s41598-022-07455-2]
- 13. Delayed neutrophil apoptosis may enhance NET formation in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9190136/]
- 14. Neutrophil extracellular traps-triggered impaired ... [https://www.nature.com/articles/s41420-022-01166-3]
- 15. Unraveling the synergy of inflammation and apoptosis in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12612658/]
- 16. endothelial cells and neutrophils in sepsis-induced acute ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1551138/full]
- 17. The role of neutrophil extracellular traps in acute lung injury [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2022.953195/full]
- 18. “The NET effectâ€: Neutrophil extracellular traps—a potential ... [https://ccforum.biomedcentral.com/articles/10.1186/s13054-025-05283-0]
- 19. Targeting integrin pathways: mechanisms and advances in ... [https://www.nature.com/articles/s41392-022-01259-6]
- 20. Role of Neutrophil Apoptosis in the Resolution of Inflammation [https://pmc.ncbi.nlm.nih.gov/articles/PMC5763753/]
- 21. Integrin Signaling in Cancer: Mechanotransduction, ... [https://www.sciencedirect.com/science/article/pii/S1535610819300418]
- 22. Neutrophils in cancer: from biology to therapy [https://www.nature.com/articles/s41423-024-01244-9]
- 23. Mapping the evolving trend of research on efferocytosis [https://pmc.ncbi.nlm.nih.gov/articles/PMC12376401/]
- 24. Molecular Mechanisms for Regulation of Neutrophil ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8245921/]
- 25. Efferocytosis: the art of cellular clearance and novel ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02484-7]
- 26. Resolution therapy: Harnessing efferocytic macrophages to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9651061/]
- 27. Molecular characterization of the surface of apoptotic ... [https://www.nature.com/articles/4400680]
- 28. Flow cytometry-based apoptosis detection - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3863590/]
- 29. Annexin V Staining Protocol for Flow Cytometry [https://www.thermofisher.com/us/en/home/references/protocols/cell-and-tissue-analysis/protocols/annexin-v-staining-flow-cytometry.html]
- 30. 5 Best Practices For Accurate Flow Cytometry Results [https://expertcytometry.com/best-practices-for-accurate-flow-cytometry-results/]
- 31. Annexin V Plus Propidium Iodide for Apoptosis - Flow Cytometry [https://flowcytometry.medicine.uiowa.edu/analysis-vs-cell-sorting-whats-difference/staining-protocols/annexin-v-plus-propidium-iodide]
- 32. Modified Annexin V/Propidium Iodide Apoptosis Assay For ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3169266/]
- 33. Designing a multicolor flow cytometry protocol [https://www.abcam.com/en-us/technical-resources/guides/flow-cytometry-guide/designing-a-multicolor-protocol]
- 34. Best Practices for Multiparametric Flow Cytometry [https://www.thermofisher.com/us/en/home/references/newsletters-and-journals/bioprobes-journal-of-cell-biology-applications/bioprobes-79/best-practices-multiparametric-flow-cytometry.html]
- 35. Platelets and Neutrophil Apoptosis: A New Frontier in ... [https://pubmed.ncbi.nlm.nih.gov/40951140/]
- 36. Isolation and High Throughput Flow Cytometric Apoptosis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7842575/]
- 37. Autologous apoptotic neutrophils inhibit inflammatory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7396436/]
- 38. Isolation and High Throughput Flow Cytometric Apoptosis ... [https://en.bio-protocol.org/en/bpdetail?id=3640&type=0]
- 39. Caspase 3/7 Activity [https://www.protocols.io/view/caspase-3-7-activity-d66n9hde.html]
- 40. Caspase-Glo® 3/7 Assay Protocol [https://www.promega.com/resources/protocols/technical-bulletins/101/caspase-glo-37-assay-protocol/]
- 41. Caspase Activity Assay [https://bio-protocol.org/exchange/minidetail?id=47642&type=30]
- 42. LDS 698: A highly sensitive probe for tracking ... [https://www.sciencedirect.com/science/article/abs/pii/S0006291X25011568]
- 43. Mitochondrial membrane potential (δψm) measurement [https://bio-protocol.org/exchange/minidetail?id=3339236&type=30]
- 44. TUNEL Assays | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/life-science/cell-analysis/cell-viability-and-regulation/apoptosis/tunel-assays.html]
- 45. TUNEL staining [https://www.abcam.com/en-us/technical-resources/guides/cell-health-guide/tunel-staining-or-tunel-assay]
- 46. TUNEL Apoptosis Assay (Chromogenic) [https://www.creative-bioarray.com/support/tunel-apoptosis-assay-chromogenic.htm]
- 47. Spontaneous PMN apoptosis in type 2 diabetes and the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6608059/]
- 48. Effects of the pan-caspase inhibitor Q-VD-OPh on human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11706505/]
- 49. TUNEL staining to detect apoptotic cells in formalin-fixed, ... [https://www.protocols.io/view/tunel-staining-to-detect-apoptotic-cells-in-formal-g82ybzyfx.html]
- 50. Harmonizing TUNEL with multiplexed iterative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12146639/]
- 51. Apoptosis DNA fragmentation analysis protocol [https://www.abcam.com/en-us/technical-resources/protocols/apoptosis-dna-fragmentation]
- 52. Pharmacological manipulation of inflammation resolution ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2812557/]
- 53. Modeling inflammation in the zebrafish: how a fish can help ... [https://pubmed.ncbi.nlm.nih.gov/18075830/]
- 54. Molecular analysis of neutrophil spontaneous apoptosis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3190116/]
- 55. HAX1 inhibits apoptosis and promotes maturation of neutrophils [https://biosignaling.biomedcentral.com/articles/10.1186/s12964-025-02353-2]
- 56. An anti-inflammatory activation sequence governs ... [https://www.nature.com/articles/s41467-022-33015-3]
- 57. Modeling Inflammation in Zebrafish for the Development of ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2020.620984/full]
- 58. Blood collection technique, anticoagulants and storing ... [https://www.nature.com/articles/s41598-020-71500-1]
- 59. methods determine human Isolation responses after... neutrophil [https://pmc.ncbi.nlm.nih.gov/articles/PMC10704165/]
- 60. Quantitative proteomics reveals tissue-specific, infection ... [https://www.nature.com/articles/s41598-024-56163-6]
- 61. Platelets and Neutrophil Apoptosis: A New Frontier in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12426582/]
- 62. and High Throughput Flow Cytometric Apoptosis Assay of... Isolation [https://bio-protocol.org/en/bpdetail?id=3640&type=0]
- 63. Targeting Neutrophil Apoptosis for Enhancing the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3972676/]
- 64. Differentiation of HL-60 cells into primed neutrophils for the ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0328717]
- 65. A transcriptomic reporter assay employing neutrophils to ... [https://translational-medicine.biomedcentral.com/articles/10.1186/1479-5876-12-65]
- 66. Apoptotic neutrophil-mediated inflammatory ... [https://www.sciencedirect.com/science/article/abs/pii/S1748013223001950]
- 67. An update on recent advances in fluorescent materials for ... [https://pubs.rsc.org/en/content/articlehtml/2025/ra/d5ra03102h]
- 68. Interference and Artifacts in High-content Screening - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK615088/]
- 69. Antibody Therapeutics as Interfering Agents in Flow ... [https://www.mdpi.com/2075-4426/13/6/1005]
- 70. Spectral Flow Cytometry: The Current State and Future of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12193525/]
- 71. Transition from CDCXM to flow cytometry in India [https://www.sciencedirect.com/science/article/abs/pii/S0966327425001091]
- 72. 15 Data Engineering Best Practices to Follow in 2025 [https://lakefs.io/blog/data-engineering-best-practices/]
- 73. Data Analytics Best Practices 2025 Guide for Businesses [https://kanerika.com/blogs/data-analytics-best-practices/]
- 74. Data Quality Testing: Key Techniques & Best Practices [2025] [https://atlan.com/data-quality-testing/]
- 75. 9 Best Practices for Data Management in 2025 [https://www.flowgenius.ai/post/9-best-practices-for-data-management-in-2025]
- 76. 10 Best Practices For Data Management in 2025 [https://numerous.ai/blog/best-practices-for-data-management]
- 77. Best Practices for Data Governance 2025: Modern Methods [https://www.ewsolutions.com/best-practives-for-data-governance/]
- 78. Apoptotic bodies derived from hypoxic bone marrow ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12530883/]
- 79. Regulation of Neutrophil Apoptosis Differs after in vivo ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6741625/]
- 80. Is the In Vitro Observed NETosis the Favored Physiological ... [https://www.mdpi.com/1422-0067/24/8/7368]
- 81. Angiotensin-(1-7) Promotes Resolution of Neutrophilic ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2017.01596/full]
- 82. Inflammation Resolution and the Induction of Granulocyte ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2019.00055/full]
- 83. Genetic and pharmacological inhibition of CDK9 drives ... [https://pubmed.ncbi.nlm.nih.gov/27833165/]
- 84. Genetic and pharmacological inhibition of CDK9 drives ... [https://www.nature.com/articles/srep36980]
- 85. CDK9 inhibitors for the treatment of solid tumors - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11580798/]
- 86. Cyclin-dependent kinases 7 and 9 specifically regulate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3504709/]
- 87. The CDK9-targeting degrader PO-8 alleviates LPS ... [https://www.sciencedirect.com/science/article/abs/pii/S0006295225006069]
- 88. Targeted degradation of CDK9 potently disrupts the MYC ... [https://pubmed.ncbi.nlm.nih.gov/40154489/]
- 89. The rate of apoptosis in post mitotic neutrophil precursors ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6734917/]
- 90. Apoptosis Assays [https://www.labome.com/method/Apoptosis-Assays.html]
- 91. Apoptosis: A Comprehensive Overview of Signaling Pathways ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11592877/]
- 92. Necrostatin-1 enhances the resolution of inflammation by ... [https://www.oncotarget.com/article/8346/text/]
- 93. Therapeutics Targeting the Core Apoptotic Machinery - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8198123/]
- 94. The multiple roles of Fas ligand in the pathogenesis ... [https://www.sciencedirect.com/science/article/pii/S1198743X14640659]
- 95. Apoptosis: Inducers and Inhibitors [https://www.novusbio.com/research-areas/apoptosis/inhibitors-activators-and-regulators?srsltid=AfmBOorhLRPLoxRrhlFkj6BtnI4L5dnCerD7D3Ekf-YXZoR9xDcSFu-d]
- 96. Reactivating apoptotic pathways in cancer: A review of ... [https://www.sciencedirect.com/science/article/abs/pii/S0014299925007198]
- 97. Comparison of Different Clinical Chemotherapeutical ... [https://www.mdpi.com/2073-4409/11/19/2942]
- 98. Therapeutic Targeting of Apoptosis, Autophagic Cell Death ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12293011/]
- 99. Apoptosis [https://www.abcam.com/en-us/technical-resources/guides/cell-health-guide/apoptosis]
- 100. Apoptosis [https://www.promega.com/resources/guides/cell-biology/apoptosis/]
- 101. Protocol for Apoptosis Assay by Flow Cytometry Using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4943750/]
- 102. Apoptosis Protocols - USF Health - University of South Florida [https://health.usf.edu/medicine/corefacilities/flowcytometry/methods-apoptosis]
- 103. Incucyte® Apoptosis Assays for Live-Cell Analysis [https://www.sartorius.com/en/applications/life-science-research/live-cell-assays/apoptosis]
- 104. Apoptosis Protocols | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/references/protocols/cell-and-tissue-analysis/apoptosis-protocol.html]
- 105. Apoptosis Assay Protocol | Technical Note 244 [https://www.denovix.com/tn-244-denovix-apoptosis-assay-protocol/]