Optimizing Inflammatory Marker Stability: A Comprehensive Guide to Storage Conditions for Reliable Research and Diagnostics
This article provides a definitive guide for researchers and drug development professionals on optimizing storage conditions to ensure the stability of inflammatory markers.
Optimizing Inflammatory Marker Stability: A Comprehensive Guide to Storage Conditions for Reliable Research and Diagnostics
Abstract
This article provides a definitive guide for researchers and drug development professionals on optimizing storage conditions to ensure the stability of inflammatory markers. Covering foundational principles, methodological applications, troubleshooting, and validation strategies, it synthesizes current evidence on the temporal stability of key biomarkers like CRP, IL-6, and TNF-α, the critical impact of temperature on various sample matrices (including plasma, VAMS devices, and urine), and practical frameworks for implementing Good Storage Practices. The content addresses common pitfalls such as pre-analytical variability and inter-assay differences, offering evidence-based protocols for enhancing data integrity, reproducibility, and long-term biobanking success in both research and clinical settings.
Understanding Inflammatory Marker Stability: Core Concepts and Critical Challenges
Troubleshooting Guides
Guide 1: Addressing Biomarker Instability in Long-Term Storage
Problem: Researchers observe a steady decline in measured biomarker concentrations in samples stored for extended periods in biobanks, raising concerns about data reliability for longitudinal studies.
Solution: Implement storage duration tracking and statistical correction methods.
- Step 1: Identify susceptible biomarkers. Evidence indicates TNF-α demonstrates significant sensitivity to long-term storage, showing a linear decrease over time, while IL-6 remains stable for over a decade at -80°C [1].
- Step 2: Record precise storage duration. For each sample, meticulously document the date of collection and storage time until analysis.
- Step 3: Apply statistical controls. Incorporate storage length as a covariate in statistical models to account for degradation-related bias [1].
- Step 4: Establish quality controls. Implement regular stability testing by re-assaying a subset of samples to monitor degradation rates specific to your storage conditions.
Guide 2: Managing Pre-Analytical Variability in Saliva Biospecimens
Problem: High variability and potential contamination in salivary biomarker measurements compromise reproducibility.
Solution: Standardize collection protocols and account for patient-specific confounders.
- Step 1: Control pre-collection factors. Instruct participants to avoid eating, drinking, toothbrushing, or using mouthwash for at least one hour before sample collection [2].
- Step 2: Use passive drool method. Collect unstimulated whole saliva into sterile tubes, as collection methods significantly impact analyte concentrations [2].
- Step 3: Characterize sample properties. Record flow rate, pH, and visually assess for blood contamination using a standardized scale [2].
- Step 4: Quantify confounders. Measure cotinine (nicotine exposure) and transferrin (blood contamination) levels to control for these variables in analysis [2].
Guide 3: Ensuring Accurate Urinary Biomarker Measurements
Problem: Urinary biomarkers show unexpected variability linked to storage conditions and pH levels.
Solution: Optimize storage parameters based on biomarker-specific stability profiles.
- Step 1: Select appropriate storage temperature. Avoid storing unstable biomarkers like U-NAG at -20°C and U-RBP for extended periods at -80°C [3].
- Step 2: Monitor urinary pH. For most biomarkers, maintain pH between 5.0-7.5, noting that U-NAG and U-RBP are particularly pH-sensitive [3].
- Step 3: Limit storage duration. For unstable biomarkers like U-IgG, avoid long-term storage even at -80°C and prioritize rapid analysis [3].
- Step 4: Validate stability. Conduct pilot studies to establish stability timelines for your specific biomarkers under local storage conditions.
Frequently Asked Questions (FAQs)
FAQ 1: What is the recommended storage temperature for preserving inflammatory cytokines in plasma samples?
For long-term storage of plasma cytokines, -80°C is recommended. IL-6 demonstrates excellent stability at this temperature for over 11 years. TNF-α is more sensitive, showing degradation after approximately 6 years [1]. For short-term storage (up to one week), -20°C or 4°C may be acceptable for some biomarkers, though stability should be validated [4].
FAQ 2: How reliable are single measurements of inflammatory biomarkers for predicting clinical outcomes?
Single measurements have value but serial assessments provide superior predictive capability. Research shows that temporal changes in CRP are more strongly associated with heart failure and cardiovascular disease risk than single measurements [5]. Similarly, sustained high levels of IL-6 correlate with 2.3-fold higher mortality risk compared to sustained low levels [5].
FAQ 3: What minimum sample size is recommended for biomarker reliability studies?
Sample size requirements for reliability studies far exceed those for hypothesis testing. While no universal minimum exists, studies with inadequate samples often produce misleading reliability estimates. The objective should determine sample size: classification problems require larger populations than simple group comparisons [6].
FAQ 4: Which exclusion criteria are essential for immune profiling studies in neurological diseases?
For core studies, exclude participants with: inflammatory/autoimmune diseases, acute/chronic infections (CRP >10 mg/L), active malignancies, recent major surgery/trauma (<6 weeks), and immunosuppressant use [7]. Well-controlled diabetes may not require exclusion, but steroids (within 3 months) and recent vaccinations (within 4 weeks) should be excluded [7].
FAQ 5: What statistical measures should accompany reports of diagnostic biomarker accuracy?
Beyond sensitivity and specificity, reports should include: positive/negative likelihood ratios, positive/negative predictive values, false discovery rates, and area under the ROC curve—all with confidence intervals [6]. For reliability studies, use appropriate intraclass correlation coefficient (ICC) versions rather than simple linear correlation [6].
Quantitative Biomarker Stability Data
Table 1: Long-Term Stability of Plasma Inflammatory Biomarkers at -80°C
| Biomarker | Sample Size | Storage Duration | Stability Outcome | Correlation with Storage Time |
|---|---|---|---|---|
| IL-6 | n=1,206 | Up to 11.6 years | Stable | Not significant [1] |
| TNF-α | n=1,223 | Up to 6 years | Stable | r = -0.217; p<0.001 [1] |
| TNF-α | n=50 | >6 years | Linear decrease | r = 0.59 (test-retest) [1] |
Table 2: Stability of Urinary Biomarkers Under Different Storage Conditions
| Biomarker | 25°C for 8 hours | 4°C for 7 days | -20°C for 12 weeks | -80°C for 12 months | Optimal pH Range |
|---|---|---|---|---|---|
| U-Albumin | Stable | Stable | Stable | Stable | 5.0-6.0 [3] |
| U-α1MG | Stable | Stable | Stable | Stable | 5.0-7.5 [3] |
| U-CysC | Stable | Stable | Stable | Stable | 5.0-7.5 [3] |
| U-NAG | Stable | Unstable after 4 days | Unstable | Not tested | Unstable [3] |
| U-IgG | Stable | Stable | Unstable after 8 weeks | Unstable after 1 month | 5.0-6.0 [3] |
| U-RBP | Stable | Stable | Significant upward trend | Unstable after 5 months | Unstable [3] |
Table 3: Serum Analyte Stability Across Storage Temperatures (Percentage Change from Baseline)
| Analyte | 24h at 4°C | 24h at -20°C | 24h at 25°C | 72h at 4°C | 72h at -20°C | 72h at 25°C |
|---|---|---|---|---|---|---|
| Urea | 0% | 0% | -3.3% | 0% | 0% | -6.7% [4] |
| Creatinine | 0% | 0% | -8.3% | 0% | 0% | -16.7% [4] |
| AST | -2.0% | -0.8% | -20% | -4.0% | -1.6% | -40% [4] |
| ALT | -0.7% | 0% | -16.7% | -3.3% | -1.7% | -40% [4] |
| Total Protein | 0% | 0% | -2.9% | -1.4% | 0% | -7.1% [4] |
| Albumin | 0% | 0% | -5.0% | -2.5% | 0% | -12.5% [4] |
Experimental Protocols
Protocol 1: Saliva Collection and Processing for Biomarker Analysis
Basic Protocol 1: Saliva Collection by Passive Drool Method
- Preparation: Instruct participants to avoid eating, drinking, smoking, or oral hygiene activities for at least one hour before collection. Perform water rinse immediately prior to collection [2].
- Collection: Have participants passively drool through a sterile straw into a pre-chilled cryovial. Collect 2-5 mL of unstimulated whole saliva.
- Initial Processing: Centrifuge samples at 1,500-2,000 × g for 15 minutes at 4°C to separate supernatant from cellular debris.
- Aliquoting: Transfer clear supernatant to fresh cryovials in small aliquots to avoid repeated freeze-thaw cycles.
- Storage: Store at -80°C for long-term preservation. Record collection time, date, and participant characteristics [2].
Basic Protocol 2: Saliva Characterization
- pH Measurement: Use pH indicator strips or micro pH electrode to record salivary pH.
- Flow Rate Calculation: Determine flow rate (mL/min) by dividing volume collected by collection time.
- Visual Assessment: Examine samples for discoloration using a standardized scale to detect blood contamination [2].
Protocol 2: Stability Validation for Novel Biomarkers
- Sample Pooling: Create a large pool of biological matrix (plasma, serum, urine) containing the biomarker of interest.
- Baseline Measurement: Aliquot and analyze immediately after collection to establish baseline values.
- Storage Conditions: Aliquot samples and store under various conditions: room temperature (25°C), refrigeration (4°C), freezing (-20°C), and ultra-low freezing (-80°C).
- Time Points: Analyze aliquots at predetermined intervals: 0, 24h, 72h, 1 week, 1 month, 3 months, 6 months, and annually.
- Stability Assessment: Compare measured concentrations to baseline using predetermined acceptance criteria (typically ±15% change) [1] [3] [4].
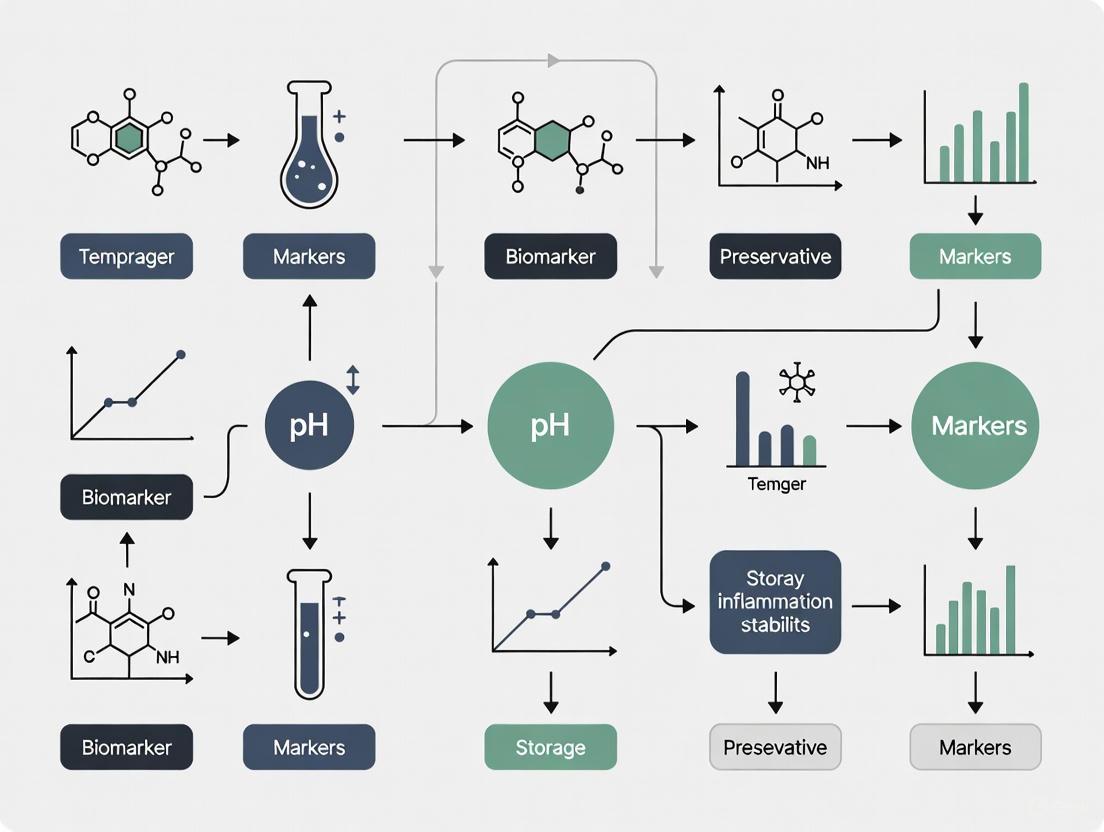
Research Workflow Visualization
Biomarker Stability Validation Workflow
Factors Influencing Biomarker Stability
Research Reagent Solutions
Table 4: Essential Materials for Biomarker Stability Research
| Item | Function | Application Notes |
|---|---|---|
| EDTA Vacutainers | Plasma collection with anticoagulant | Preferred for cytokine studies [1] |
| Sterile Saliva Collection Tubes | Non-invasive biospecimen collection | Use passive drool method for consistency [2] |
| Cryogenic Vials | Long-term sample storage at -80°C | Use O-ring seals to prevent evaporation [1] |
| pH Indicator Strips | Sample quality assessment | Critical for urine and saliva characterization [2] [3] |
| Portable Centrifuge | Immediate sample processing | Pre-cool to 4°C for temperature control [2] |
| Cotinine ELISA Kit | Quantify nicotine exposure | Essential confounder for salivary biomarkers [2] |
| Transferrin Assay | Detect blood contamination | Important for oral health assessment [2] |
| High-Sensitivity Cytokine Kits | Low-abundance analyte measurement | Required for inflammatory markers like IL-6 [1] [8] |
Troubleshooting Guides & FAQs
Frequently Asked Questions
Q1: Which inflammatory biomarkers remain most stable during long-term frozen storage?
Biomarkers show vastly different degradation profiles during frozen storage. C-reactive Protein (CRP) demonstrates exceptional stability, showing no significant decrease after five years of storage at -80°C [9]. In contrast, under the same conditions, TRAIL levels decrease by approximately 30% and IP-10 decreases by about 17% over the same period [9]. For lyophilized secretome samples containing cytokines like BDNF, bNGF, and VEGF-A, storage at -80°C preserves over 70% of components for up to 30 months, while storage at -20°C or higher temperatures leads to significant degradation [10].
Q2: What is the impact of using different blood collection tubes on cytokine measurements?
The choice of blood collection tube significantly influences cytokine quantification results. Studies show that cytokine levels are generally higher in plasma than in serum from healthy individuals [11]. For the most reliable results with cytokine panels, serum samples collected in tubes containing a separation gel, centrifuged within 4 hours of collection, and stored at -20°C for up to 24 hours provide optimal stability for most cytokines [11].
Q3: Can non-invasive sampling methods reliably measure inflammatory markers like CRP?
Yes, emerging research shows strong correlations between non-invasive samples and traditional blood measurements. Saliva and urine CRP levels show strong correlation with serum CRP (saliva: r=0.709, p<0.001; urine: r=0.886, p<0.001) [12]. A multimodal approach using both urine and saliva CRP can predict serum CRP levels with 76.1% accuracy [12]. Additionally, patients significantly prefer these non-invasive methods over blood draws [12].
Q4: How does immediate sample processing affect cytokine stability in mucosal samples?
For cervical mucous samples, refrigeration immediately after collection provides better conservation for certain cytokines compared to immediate snap-freezing. Specifically, TNF-α, IFN-γ, and IL-1β show significantly higher levels in refrigerated samples versus snap-frozen pairs when processed within 8 hours of collection [13]. For other cytokines including IL-2, IL-4, IL-6, IL-8, IL-10, IL-12, and GM-CSF, no significant differences were observed between refrigeration and snap-freezing [13].
Troubleshooting Common Scenarios
Scenario: Inconsistent cytokine measurements across multiple study sites
| Problem | Possible Cause | Solution |
|---|---|---|
| Variable cytokine readings | Different sample processing protocols | Implement standardized SOPs: use consistent tube types, processing timelines (<4h), and immediate refrigeration for specific cytokines [11] [13]. |
| Degradation of specific biomarkers | Inappropriate long-term storage temperature | Store biomarkers at -80°C; for lyophilized samples, use trehalose supplementation to enhance stability at higher temperatures [9] [10]. |
| Unreliable CRP measurements in remote settings | Dependency on venipuncture | Implement dried blood spot (DBS) sampling: fingerstick blood on filter paper, dried 24h, then mailed to lab [14]. |
Quantitative Stability Data
Biomarker Stability Under Different Storage Conditions
Table 1: Long-term stability of serum biomarkers at -80°C [9]
| Biomarker | 5-Year Stability | Degradation Pattern |
|---|---|---|
| CRP | No significant decrease | Highly stable |
| IP-10 | ~17% decrease | Moderately stable |
| TRAIL | ~30% decrease | Less stable |
Table 2: Stability of lyophilized MSC-secretome components [10]
| Storage Temperature | Storage Duration | Affected Components | Preservation Level |
|---|---|---|---|
| -80°C | 30 months | All evaluated components | >70% preserved |
| -20°C | 30 months | BDNF, bNGF, VEGF-A | Significant decrease |
| 4°C & Room Temp | 30 months | BDNF, bNGF, VEGF-A, IL-6, sVCAM-1 | Major decrease |
Table 3: Correlation between non-invasive and serum CRP measurements [12]
| Sample Type | Correlation with Serum CRP | Statistical Significance |
|---|---|---|
| Urine | r=0.886 | p<0.001 |
| Saliva | r=0.709 | p<0.001 |
| Multimodal (Urine+Saliva) | 76.1% predictive accuracy | - |
Experimental Protocols
Protocol 1: Dried Blood Spot (DBS) Sampling for CRP Analysis
Purpose: To enable remote, at-home blood sampling for CRP measurement with stability comparable to venous plasma [14].
Materials:
- Sterile lancets (BD Microtainer contact-activated lancet, 2.0 mm depth)
- Whatman CF12 grade filter paper (ISO9001 certified)
- Isopropyl alcohol wipes
- Gel pack (42°C, for finger warming if needed)
- Ziplock bags with desiccant
Procedure:
- Finger Preparation: Clean puncture site with isopropyl alcohol wipe and allow to dry. Apply warm gel pack for maximal 3 minutes if blood flow is insufficient.
- Puncture: Use lancet on fingertip. Wipe away first blood drop with clean gauze.
- Spotting: Gently squeeze finger to form blood drops. Apply drops to filter paper, completely filling pre-printed circles.
- Drying: Leave filter paper cards at room temperature for at least 24 hours.
- Storage & Transport: Place dried cards in ziplock bags with desiccant. Ship at ambient temperature.
- Laboratory Analysis:
- Punch 3×8 mm discs from DBS cards into Eppendorf tubes
- Add 150 µL PBS (pH 7.4)
- Incubate 15 min at room temperature on orbital shaker (600 rpm)
- Centrifuge at 21,130×g for 3 minutes
- Transfer supernatant to analyzer cups
- Measure CRP on automated chemistry analyzer (e.g., Atellica CH Analyzer)
Validation Parameters:
- Excellent correlation with venous plasma: R²=0.986 [14]
- Correct classification of high CVD risk: Sensitivity 1.00, Specificity 0.96 [14]
- Stable for 31 days at ambient temperature [14]
Protocol 2: Multimodal Non-Invasive Biomarker Assessment
Purpose: To simultaneously collect and compare inflammatory biomarkers from multiple non-invasive sources against serum reference [12].
Materials:
- Serum separator tubes (venipuncture control)
- Midstream urine collection cups
- Saliva collection swabs (Salimetrics SalivaBio Oral Swab)
- Sweat patches (PharmChek Sweat Patch)
- Core body temperature sensor (greenTEG CaleraResearch CORE)
- Exhaled breath analyzer (Bosch Vivatmo me device)
- Stool sample collection kit
- Portable freezer (-20°C for temporary storage)
Procedure:
- Participant Preparation: 2-hour fasting (except water); avoid chewing gum, tooth brushing, mouthwash, or smoking.
- Sample Collection Order:
- Venous blood draw (reference standard)
- Midstream urine collection with dipstick test for UTI screening
- Saliva collection: place swab under tongue for 3 minutes
- Apply two sweat patches to arms or abdomen
- Attach core body temperature sensor to upper body
- Perform exhaled breath measurement
- Provide instructions for stool sampling
- 48-Hour Follow-up: Collect sweat patches, temperature sensor, and stool sample.
- Storage: Centrifuge blood samples within 30 minutes; store all samples at -80°C until analysis.
- Patient Preference Assessment: Participants rank sampling methods from 1 (most preferred) to 7 (least preferred).
Key Findings:
- Urine and saliva CRP significantly elevated in inflammation group vs controls [12]
- Patients strongly favor non-invasive methods over blood tests [12]
- Multimodal approach (urine + saliva) outperforms single-modality predictions [12]
Visualization Diagrams
Biomarker Stability Decision Pathway
Sample Processing Workflow Comparison
Research Reagent Solutions
Essential Materials for Inflammatory Marker Stability Research
Table 4: Key research reagents and materials for stability studies
| Reagent/Material | Function/Application | Specification Considerations |
|---|---|---|
| Filter Paper Cards | Dried blood spot sampling [14] | Whatman CF12 grade, ISO9001 certified |
| Trehalose Supplement | Lyophilization stabilizer [10] | Prevents degradation during freeze-drying and storage |
| Serum Separator Tubes | Blood collection for cytokine analysis [11] | Tubes containing separation gel |
| Saliva Collection Swabs | Non-invasive saliva sampling [12] | Salimetrics SalivaBio Oral Swabs |
| Sweat Patches | Non-invasive sweat collection [12] | PharmChek Sweat Patch |
| PBS Buffer (pH 7.4) | DBS extraction [14] | Standard phosphate-buffered saline |
| Automated Chemistry Analyzer | High-throughput biomarker quantification [14] | e.g., Atellica CH Analyzer |
| Luminex/Bio-Plex System | Multiplex cytokine measurement [13] | Multi-analyte profiling platform |
Troubleshooting Guides and FAQs
Frequently Asked Questions
Q1: What is the maximum time I can store plasma samples for inflammatory markers at 4°C before analysis? A: For a range of inflammatory (IL-6), hemostasis (D-dimer, PAI-1), endothelial dysfunction (E-selectin, sICAM-1, sVCAM-1), and oxidative stress (nitrite) biomarkers, plasma samples processed within 1 hour of collection can be transported and stored at 4°C for up to 24 hours with minimal effect on precision (differences ≤7% compared to -80°C control) [15].
Q2: My research involves dried blood spots (DBS). Which metabolite classes are most unstable at room temperature? A: Lipid metabolites, particularly phosphatidylcholines (PCs) and triglycerides (TAGs), are the most unstable in DBS samples stored at room temperature, showing significant time-dependent degradation [16]. For longer-term stability, storage at -20°C or -80°C is recommended [17].
Q3: I have historic serum samples stored at -20°C, not -80°C. Are they still usable for metabolomic studies? A: It depends on the analytes. A 2022 study found that 120 out of 193 metabolites and proteins were unaffected by long-term storage at -20°C compared to -80°C [18]. However, 15 analytes were clearly susceptible. The glutamate/glutamine ratio greater than 0.20 was identified as a specific biomarker indicative of sub-optimal storage at -20°C [18].
Q4: Are there inflammatory markers stable enough for repeated, non-invasive collection in urine? A: Yes, a feasibility study identified a panel of markers detectable and stable in urine, including CRP, Fractalkine, G-CSF, GM-CSF, IFN-α2, IFNγ, IL-1RA, IL-7, IP10, MCP-1, MIP-1β, and VEGF. These were stable at room temperature for 24-48 hours, making them suitable for ecological momentary assessments in biobehavioral research [19].
Troubleshooting Common Scenarios
Problem: Inconsistent biomarker readings after shipping samples from satellite collection sites. Solution: Implement a cold chain using gel packs (4°C) for transport. Research shows this is a feasible and effective alternative to dry ice for a 24-hour transport window for many inflammatory and coagulation biomarkers, with minimal impact on precision [15].
Problem: Degradation of a specific biomarker, Pentraxin 3 (Ptx3), in serum samples. Solution: Ensure immediate freezing at -80°C for long-term storage (stable for 48 months) or -20°C for mid-term storage (stable for 8 months). Avoid any exposure to warmer temperatures, as Ptx3 degrades rapidly at +37°C [20].
Problem: Choosing between dried blood microsamplers (DBM) and plasma for field collection. Solution: DBM samples show superior stability at 4°C compared to plasma, particularly for lipid classes. For studies where immediate ultra-low freezing is not possible, DBM offers a more robust collection matrix [17].
Table 1: Plasma Biomarker Stability After 24-Hour Transport at Different Temperatures
Data presented as percent difference from control (-80°C). Adapted from [15].
| Biomarker Category | Specific Biomarker | Dry Ice (-79°C) | Cold Gel Packs (4°C) | Room Temperature (21°C) |
|---|---|---|---|---|
| Inflammation | IL-6 | ≤ 7% | ≤ 7% | > 7% |
| Inflammation | hs-CRP | ≤ 7% | ≤ 7% | > 7% |
| Hemostasis | D-dimer | ≤ 7% | ≤ 7% | > 7% |
| Hemostasis | PAI-1 | ≤ 7% | ≤ 7% | Up to 12% |
| Endothelial Dysfunction | E-selectin | ≤ 7% | ≤ 7% | > 7% |
| Endothelial Dysfunction | sVCAM-1 | ≤ 7% | ≤ 7% | Up to 12% |
Table 2: Stability of Metabolite Classes in Dried Blood Spots (DBS) at Different Temperatures
Based on data from [16]. "Stable" denotes <15% change in relative standard deviation (RSD) over 21 days.
| Metabolite Subclass | 4°C | 25°C | 40°C |
|---|---|---|---|
| Amino Acids | Stable | Stable | Unstable after 14 days |
| Phosphatidylcholines (PCs) | Unstable | Unstable | Unstable |
| Triglycerides (TAGs) | Unstable | Unstable | Unstable |
| Lysophosphatidylcholines (LysoPCs) | Stable | Unstable after 7 days | Unstable after 7 days |
| Carbohydrates | Stable | Unstable after 14 days | Unstable after 14 days |
| Sphingomyelins (SMs) | Stable | Stable | Stable |
| Fatty Acids | Stable | Stable | Stable |
Table 3: Long-Term Serum Storage: Analytes Affected by -20°C vs. -80°C
Summary of key findings from [18] after a median of 4.2 years of storage.
| Category | Representative Analytes Unaffected by -20°C | Representative Analytes Susceptible to -20°C |
|---|---|---|
| Proteins | Apo A-I, Apo B, Complement 3, C-Peptide | Fetuin A, Cystatin C, RANTES |
| Metabolites | Lactate, Pyruvate, Citrate, Glycerol | Glutamate/Glutamine ratio, Kynurenine, Acetylcarnitine |
Detailed Experimental Protocols
Protocol 1: Evaluating Transport Temperature on Plasma Biomarkers
This method is adapted from the study that investigated the stability of inflammatory, hemostasis, endothelial function, and oxidative stress biomarkers [15].
1. Sample Collection:
- Collect blood into appropriate vacutainers (e.g., lithium heparin, sodium citrate, K2EDTA).
- Critical Step: Centrifuge all specimens at 1,300-2,000 x g for 10 minutes at 18-25°C within 1 hour of collection.
- Aliquot the plasma into cryovials.
2. Simulation of Transport Conditions:
- Control: Place one set of aliquots directly into a -80°C freezer.
- Test Conditions: Package other sets of aliquots in insulated shippers for 24 hours under:
- Dry Ice: Approximately -79°C
- Cold Gel Packs: Maintains ~4°C
- Room Temperature: ~21°C
- After 24 hours, measure the temperature inside the shippers, then transfer all test boxes to -80°C for batch analysis.
3. Biomarker Analysis:
- Analyze biomarkers using standardized, validated assays (e.g., multiplex immunoassays for IL-6, PAI-1; colorimetric kits for nitrite; clinical analyzers for hs-CRP and D-dimer).
4. Data Analysis:
- Calculate the mean and median concentrations for each biomarker across all conditions.
- Determine stability by calculating the percent change for each transport temperature compared to the -80°C control. A difference of ≤5% is generally considered a small, acceptable change.
Protocol 2: Assessing Metabolite Stability in Dried Blood Spots (DBS)
This protocol is based on an untargeted metabolomics study of DBS stability [16].
1. Sample Preparation:
- Spot a consistent volume of whole blood (e.g., 50 μL) onto Guthrie cards (Whatman 903 protein saver cards).
- Dry the spots for 3 hours at room temperature in a dark, low-humidity environment.
- Store individual spots in light-resistant, desiccant-containing bags.
2. Experimental Storage Conditions:
- Store replicate DBS cards at:
- 4°C (Refrigeration)
- 25°C (Room Temperature)
- 40°C (Elevated Temperature, simulating harsh conditions)
- Include a control (T0) analyzed immediately.
3. Time-Course Analysis:
- Remove samples from each storage condition at predetermined time points (e.g., 3, 7, 14, and 21 days).
4. Metabolite Extraction and Profiling:
- Punch a fixed diameter (e.g., 5-mm) from each DBS.
- Extract metabolites using a methanol/acetonitrile/water solution with sonication and agitation.
- Perform untargeted metabolic profiling using platforms like UHPLC-MS and GC-MS in both positive and negative ionization modes.
5. Stability Assessment:
- Process raw data and perform peak alignment and identification.
- Use Principal Component Analysis (PCA) to visualize overall effects of storage temperature and time.
- A metabolite is typically classified as "stable" if the Relative Standard Deviation (RSD) of its intensity is below 15-20% over the storage period compared to the T0 control.
Visual Workflows
Diagram 1: Plasma Transport Stability Experiment
Diagram 2: DBS Storage Stability Metabolomics Workflow
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 4: Key Materials for Storage Stability Experiments
| Item | Function & Application | Example from Literature |
|---|---|---|
| Lithium Heparin / K2EDTA / Sodium Citrate Vacutainers | Anticoagulant blood collection tubes for plasma preparation. The choice of anticoagulant is critical for specific biomarker assays. | Used for collecting plasma for IL-6, hs-CRP, D-dimer, and other biomarkers [15]. |
| Volumetric Absorptive Microsamplers (VAMs) | Collects a precise volume (e.g., 10 µL) of whole blood directly from a capillary prick, overcoming hematocrit bias seen in traditional DBS. | Mitra microsamplers were used in a comparative stability study with DBS and plasma [17]. |
| Guthrie Cards (Protein Saver Cards) | Filter paper cards for traditional DBS collection. Inexpensive and well-established, but subject to hematocrit effects. | Whatman 903 cards were used to study metabolite stability at different temperatures [16]. |
| Multiplex Immunoassay Kits | Allows simultaneous measurement of multiple protein biomarkers (e.g., cytokines, adhesion molecules) from a single small-volume sample. | Used with Bio-Plex 200 instrument to measure IL-6, PAI-1, E-selectin, sICAM-1, and sVCAM-1 [15]. |
| Cryovials & Specimen Boxes | For secure, organized, long-term storage of plasma and serum aliquots at ultra-low temperatures. | 0.5 mL cryovials in 100-cell specimen boxes were used for transport simulation [15]. |
| Desiccant & Humidity Indicator Cards | Protects dried samples (DBS, DBM) from moisture-induced degradation during storage. | DBS and DBM were stored in light-resistant bags with desiccant [17]. |
The reliability of any research data, particularly in studies focusing on inflammatory marker stability, is heavily dependent on the integrity of biological samples before they are ever analyzed. This phase, known as the pre-analytical phase, is the most vulnerable to errors in the total testing process. It is estimated that pre-analytical errors contribute to 60-75% of all laboratory errors, compromising data quality and potentially leading to erroneous conclusions [21] [22]. For researchers and drug development professionals, controlling these variables is not merely a matter of protocol but a fundamental requirement for generating valid, reproducible scientific data. This guide provides troubleshooting and best practices to identify, manage, and mitigate these critical pre-analytical variables.
Troubleshooting Common Pre-Analytical Issues
Here are some frequently encountered problems related to pre-analytical variables and their solutions.
FAQ 1: A large percentage of my samples are hemolyzed. What could be causing this and how can I prevent it?
Hemolysis, the rupture of red blood cells, is a leading cause of sample rejection and can significantly alter analytical results [21].
- Causes & Solutions:
- Cause: Improper phlebotomy technique, such as using a needle that is too small or forcing blood from a syringe into a collection tube.
- Solution: Ensure trained personnel perform blood collection using appropriate needle gauges and avoid turbulent transfer.
- Cause: Prolonged tourniquet application or excessive fist clenching.
- Solution: Apply a tourniquet for less than one minute and advise patients to avoid repeated fist clenching [23].
- Cause: Handling errors post-collection, such as vigorous shaking of tubes or improper freezing/thawing.
- Solution: Gently invert tubes according to the manufacturer's instructions. Avoid multiple freeze-thaw cycles; instead, aliquot samples before storage.
FAQ 2: My sample results show inexplicable variations in analyte levels (e.g., potassium). What patient or collection factors should I investigate?
Several factors during collection can lead to physiologically implausible results.
- Investigation Checklist:
- Patient Posture: A change from lying to standing can cause a ~9% elevation in serum concentrations of proteins or protein-bound constituents due to a shift in blood volume [22].
- Sample Timing: For analytes with circadian rhythms (e.g., cortisol, iron), ensure collection times are standardized and documented [22].
- Collection Tube Order: Cross-contamination from tube additives can occur if the order of draw is not followed. Collect serum tubes before plasma tubes with anticoagulants like EDTA or citrate.
- Tube Fill Volume: Under-filling anticoagulant tubes (e.g., citrate for coagulation studies) alters the blood-to-additive ratio, leading to artificially prolonged clotting times [24].
FAQ 3: How long can my samples be stored at room temperature before processing without significant biomarker degradation?
Stability is analyte-specific, but delays in processing are a major source of pre-analytical variation.
- General Guidance: The stability of biomarkers at room temperature is finite. Delays of over 4 hours between collection and processing can affect the results of many routine tests [24]. For specialized research, stability must be empirically determined.
- Case Example: A 2025 study on bile samples for cholangiocarcinoma research found that proteins and circulating tumor DNA (ctDNA) remained stable for up to 7 hours at room temperature (20-25°C) without significant degradation [25]. This highlights the need for stability studies specific to your sample matrix and analytes of interest.
- Best Practice: Define and adhere to a maximum allowed processing window in your study protocol. When possible, process samples immediately and freeze aliquots at the appropriate temperature.
FAQ 4: In a multi-center trial, how can I ensure consistent sample handling across different sites?
Decentralization introduces significant variability in sample collection, handling, and transport.
- Strategies for Harmonization:
- Standardized Kits & SOPs: Provide all sites with identical sample collection kits and meticulously detailed Standard Operating Procedures (SOPs) [26].
- Comprehensive Training: Conduct mandatory training for all site personnel involved in the sample handling chain, from phlebotomy to shipping.
- Stabilization Technology: Utilize blood collection tubes with stabilizers that allow for room-temperature storage and transport, mitigating the effects of processing delays and temperature fluctuations during transit [27].
- Centralized Laboratory: Using a single, central laboratory for all sample analysis reduces inter-laboratory variability and ensures consistent handling [26].
Quantitative Data on Pre-analytical Errors
The table below summarizes the distribution and frequency of common pre-analytical errors.
Table 1: Frequency and Impact of Common Pre-analytical Errors
| Error Category | Specific Error Type | Estimated Frequency | Primary Impact on Research Data |
|---|---|---|---|
| Sample Quality | Hemolysis | 40-70% of poor quality samples [21] | False elevation of intracellular analytes (K+, LDH, AST); spectral interference [23] [21] |
| Insufficient Sample Volume | 10-20% [21] | Inability to perform all tests; potential sample rejection | |
| Clotted Sample | 5-10% [21] | Invalid results for hematology and coagulation tests | |
| Wrong Collection Tube | 5-15% [21] | Analyte degradation or additive interference | |
| Test Request & Identification | Inappropriate Test Request | 11-70% (varies by test) [21] | Wasted resources, irrelevant data |
| Patient/Sample Misidentification | Significant contributor to phlebotomy errors [21] | Catastrophic data integrity failure; incorrect results |
Experimental Protocols for Investigating Pre-analytical Variables
To optimize storage conditions for inflammatory markers, you must first establish how they are affected by pre-analytical conditions. The following protocols provide a framework for this investigation.
Protocol 1: Evaluating Temporal Stability at Room Temperature
This protocol assesses the integrity of your target biomarkers under different pre-processing storage times.
- Objective: To determine the maximum allowable time between sample collection and processing at room temperature for specific inflammatory markers.
- Materials:
- Blood collection tubes (e.g., Serum Separator Tubes, EDTA plasma tubes)
- Centrifuge
- Aliquot tubes
- -80°C freezer
- Relevant assay kits (e.g., ELISA for cytokines like IL-6, TNF-α)
- Methodology:
- Collect blood from consented donors under standardized conditions.
- For each donor, aliquot the whole blood into multiple tubes immediately after draw.
- Process one set of tubes immediately (Time 0 control) by centrifuging at recommended speed and time (e.g., 16,000 × g for 10 min at 4°C) [25]. Immediately freeze the resulting plasma/serum at -80°C.
- Leave the remaining whole blood tubes at room temperature (20-25°C).
- Process and freeze additional sets of tubes at pre-defined time points (e.g., 1, 3, 5, and 7 hours post-collection) [25].
- Analyze all frozen aliquots in the same batch using your validated assay. Compare the analyte concentrations at each time point against the Time 0 control.
- Data Analysis: Use repeated measures ANOVA or similar statistical tests to determine if analyte degradation over time is significant. A p-value of < 0.05 is typically considered significant [25].
Protocol 2: Assessing the Impact of Centrifugation Variations
This protocol evaluates how deviations in processing conditions affect sample quality.
- Objective: To investigate the effect of centrifugation speed and duration on biomarker stability and sample quality (e.g., platelet removal).
- Materials:
- Blood collection tubes
- Centrifuges (different models if testing multi-site variability)
- Aliquot tubes
- -80°C freezer
- Methodology:
- Collect blood and pool it to create a homogeneous sample.
- Distribute the blood into multiple identical tubes.
- Centrifuge groups of tubes under different conditions (e.g., Protocol A: 2,000 × g for 10 min; Protocol B: 1,500 × g for 15 min; Protocol C: 3,000 × g for 5 min).
- Carefully aliquot the plasma/serum from each tube, ensuring not to disturb the buffy coat or cells.
- Analyze the aliquots for your target biomarkers and also for sample quality indicators (e.g., platelet count in plasma to assess residual platelet contamination).
- Data Analysis: Compare analyte levels and sample quality indices across the different centrifugation protocols to identify the most reproducible and effective method.
Workflow and Relationship Diagrams
The following diagrams visualize the pre-analytical workflow and a strategy for error detection.
Diagram 1: Pre-analytical Phase Workflow
Diagram 2: Strategy for Detecting Pre-analytical Errors
The Scientist's Toolkit: Key Research Reagent Solutions
Selecting the right materials is crucial for standardizing the pre-analytical phase and ensuring sample integrity.
Table 2: Essential Materials for Pre-analytical Control in Research
| Item | Function & Importance |
|---|---|
| Stabilizing Blood Collection Tubes (e.g., for cfDNA, cfRNA) | Preserves specific biomarkers at room temperature, allowing for longer transport times and batch processing. Crucial for multi-center trials and liquid biopsy research [28] [27]. |
| Serum Separator Tubes (SST) | Contains a gel that forms a barrier between serum and clot during centrifugation, simplifying serum harvesting and improving sample quality. |
| EDTA Plasma Tubes | Prevents coagulation by chelating calcium. The preferred sample type for many molecular and proteomic assays. |
| Citrated Tubes (e.g., 3.2% Sodium Citrate) | Used for coagulation studies. The strict 1:9 anticoagulant-to-blood ratio is critical; under-filling prolongs clotting times [24]. |
| PaxGene RNA Tubes | Stabilizes intracellular RNA profiles immediately upon collection, minimizing gene expression changes that can occur during processing delays. |
| Validated Assay Kits | Provides reliable and reproducible methods for quantifying inflammatory markers (e.g., IL-1β, IL-6, TNF-α). Using validated kits ensures data comparability [29]. |
Clinical and Research Implications of Unstable Marker Measurements
Troubleshooting Guide: Common Scenarios & Solutions
Scenario 1: Inconsistent Biomarker Results After Room Temperature Storage
- Problem: Measured protein concentrations or ctDNA mutation levels vary significantly between samples processed at different times.
- Investigation: Check if room temperature storage duration exceeds stability limits. Bile-derived proteins and ctDNA can remain stable for at least 7 hours at room temperature (20-25°C) without significant degradation [25].
- Solution: Establish a standard operating procedure (SOP) to process all samples within the stable time window. For bile samples, complete centrifugation and aliquoting within 7 hours of collection [25].
Scenario 2: Degradation of Low-Abundance Proteins in Cell Lysates
- Problem: Faint or absent bands on a western blot for a low-abundance target protein, such as a GPCR.
- Investigation: Review sample preparation steps. Proteolytic or phosphatase activity during lysis can degrade targets.
- Solution: Always perform lysis on ice using a denaturing buffer (e.g., RIPA buffer) and include a fresh, complete cocktail of protease and phosphatase inhibitors (see Table 1) [30]. For very low-abundance proteins, consider prior enrichment via immunoprecipitation or WGA beads [30].
Scenario 3: Unstable Drug Concentrations in Blood Samples During Transport
- Problem: Measurements of Direct Oral Anticoagulant (DOAC) levels are unreliable when samples are shipped from satellite clinics.
- Investigation: Confirm sample type and storage conditions against validated stability data.
- Solution: For DOACs (rivaroxaban, dabigatran, edoxaban), whole blood samples can be stored in a refrigerator (+2–8 °C) for up to 7 days without significant concentration deviation (<±20%) [31]. Centrifuged citrated plasma can be stored refrigerated or frozen at -20°C for the same duration [31].
Scenario 4: Choosing Between ELISA and Western Blot for Protein Analysis
- Problem: Uncertainty about which technique provides reliable data for a new inflammatory marker.
- Investigation: Define the research goal: initial quantification and screening vs. confirmation and size characterization.
- Solution:
Frequently Asked Questions (FAQs)
Q1: How long can I store bile samples at room temperature before protein and ctDNA degrade? A1: Proteins (like E-Cadherin and N-Cadherin) and ctDNA (e.g., mutant KRAS) in bile samples demonstrate no significant degradation when stored at room temperature (20-25°C) for up to 7 hours [25].
Q2: What are the recommended storage conditions for transporting blood samples for DOAC testing? A2: For DOACs (rivaroxaban, dabigatran, edoxaban), you have several stable options for up to 7 days [31]:
- Citrated whole blood in a refrigerator (+2–8 °C)
- Citrated plasma in a refrigerator (+2–8 °C)
- Citrated plasma frozen (-20 °C)
Q3: My western blot results are inconsistent. What are the critical steps in sample preparation? A3: For consistent western blots, ensure [30]:
- Lysis on Ice: Always keep samples cold during lysis to inhibit enzymatic activity.
- Use Inhibitors: Always add fresh protease and phosphatase inhibitors to your lysis buffer.
- Proper Buffer: Choose a lysis buffer (e.g., RIPA, NP-40) appropriate for your protein's subcellular location.
- Accurate Concentration: Precisely determine protein concentration after lysis using a compatible assay (e.g., BCA, Bradford).
Q4: When should I use a dot plot instead of a bar graph for my data? A4: Replace bar graphs with dot plots (or box plots/violin plots) when you need to show the underlying data distribution. This is crucial for [33]:
- Studies with small sample sizes.
- When responses are highly variable or heterogeneous.
- When you want readers to be able to critically evaluate the data distribution and variability.
Stability Data for Research Materials
The following table summarizes stability data for various sample types, crucial for planning experiments and shipments.
Table 1: Documented Stability of Biomarkers and Analytes
| Sample Matrix | Analyte | Stable Storage Condition | Maximum Documented Stability | Key Findings |
|---|---|---|---|---|
| Bile [25] | Proteins (E-Cadherin, N-Cadherin) | Room Temp (20-25°C) | 7 hours | No significant degradation in concentration or enzyme activity (P > 0.05). |
| Bile [25] | ctDNA (mutant KRAS) | Room Temp (20-25°C) | 7 hours | Mutant allele levels remained stable without significant changes (P > 0.05). |
| Citrated Whole Blood [31] | DOACs (Rivaroxaban, Dabigatran, Edoxaban) | Refrigerated (+2–8 °C) | 7 days | Median deviation from baseline <5.5%. Suitable for transport. |
| Citrated Plasma [31] | DOACs (Rivaroxaban, Dabigatran, Edoxaban) | Refrigerated (+2–8 °C) or Frozen (-20 °C) | 7 days | Median deviation from baseline <1% for most conditions. |
Detailed Experimental Protocols
Protocol 1: Bile Sample Processing for Liquid Biopsy
This protocol is optimized for the stability of proteins and ctDNA in cholangiocarcinoma research, based on the method described by Scientific Reports [25].
- Sample Collection: Collect bile via percutaneous transhepatic biliary drainage (PTBD). A minimum of 10 mL is recommended.
- Room Temperature Storage: Process aliquots at defined intervals (e.g., 1, 3, 5, 7 hours). Keep samples at approximately 25°C during this period.
- Centrifugation: Centrifuge samples at 16,000 × g for 10 minutes at 4°C to separate supernatant from pellet.
- Pellet Washing: Resuspend the pellet in a two-fold volume of chilled phosphate-buffered saline (PBS). Re-centrifuge at 16,000 × g for 5 minutes at 4°C. Discard the supernatant.
- Storage: Store the resulting bile supernatant and the air-dried pellet at -80°C for further analysis of ctDNA and proteins, respectively.
Protocol 2: Western Blot Sample Preparation from Cell Lysates
A detailed protocol for preparing stable and high-quality protein samples [30].
- Lysis Buffer Preparation: Prepare a denaturing lysis buffer (e.g., RIPA buffer). Add protease and phosphatase inhibitors immediately before use (See Table 2 for common inhibitors).
- Cell Lysis: Place culture dish on ice. Aspirate media and wash cells with cold PBS. Add cold lysis buffer (e.g., 100-200 µL for a 35 mm dish). Scrape cells and transfer the suspension to a pre-chilled microcentrifuge tube.
- Clarification: Incubate on ice for 10-30 minutes. Centrifuge at ≥12,000 × g for 15 minutes at 4°C to remove insoluble debris.
- Protein Quantification: Transfer the clear supernatant to a new tube. Determine protein concentration using a colorimetric assay (e.g., Bradford or BCA assay), ensuring compatibility with your lysis buffer components.
- Sample Preparation for SDS-PAGE: Mix protein lysate with an equal volume of 2X Laemmli sample buffer. For reduced samples, add fresh β-mercaptoethanol or DTT. Heat samples at 95°C for 5 minutes.
- Storage: If not used immediately, store protein samples at -80°C. Avoid repeated freeze-thaw cycles.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for Biomarker Stability and Detection
| Reagent | Function | Example & Notes |
|---|---|---|
| Protease Inhibitor Cocktail | Inhibits a broad range of proteolytic enzymes (serine, cysteine, metalloproteases) to prevent protein degradation [30]. | Commercially available tablets or solutions. Examples: PMSF (serine proteases), Aprotinin, Leupeptin. |
| Phosphatase Inhibitor Cocktail | Prevents dephosphorylation of proteins, preserving post-translational modification states [30]. | Examples: Sodium orthovanadate (tyrosine phosphatases), β-glycerophosphate (serine/threonine phosphatases). |
| NucleoSpin cfDNA XS Kit | Extraction of circulating tumor DNA (ctDNA) from biofluids like bile or plasma [25]. | Optimized for small-volume, low-concentration samples. |
| ddPCR KRAS Screening Multiplex Kit | Ultra-sensitive detection and absolute quantification of mutant KRAS alleles in ctDNA [25]. | Used with a droplet digital PCR system (e.g., Bio-Rad QX200). |
| ELISA Kits (E-Cadherin, N-Cadherin) | Quantification of specific protein concentrations or activity in complex biological samples [25]. | High-throughput and quantitative. |
| Phospholipon 90G | A phospholipid used in the formulation of nanocarriers like ethosomes to enhance drug delivery and stability [34]. | Key component for creating stable lipid vesicles for topical application. |
Experimental Workflow & Decision Pathways
Sample Processing Workflow for Bile Liquid Biopsy
Method Selection for Protein Analysis
Implementing Optimal Storage Protocols: From Biobanking to Point-of-Care Testing
FAQ: Sample Storage and Stability
What is the recommended storage temperature for common biological samples prior to assay?
For long-term storage, most biological samples should be aliquoted and stored at -20°C or below to preserve biomarker integrity [35]. The table below summarizes standard pre-assay storage conditions for various sample types.
| Sample Type | Short-term Storage (before processing) | Long-term Storage (after processing) | Key Considerations |
|---|---|---|---|
| Serum | Allow to clot for 30 mins at room temperature [35]. | ≤ -20°C [35] | Centrifuge at 1000 x g for 15 mins after clotting [35]. |
| Plasma | Centrifuge within 30 mins of collection [35]. | ≤ -20°C [35] | Use EDTA, heparin, or citrate as an anticoagulant [35]. |
| Cell Culture Supernates | Centrifuge at 500 x g for 5 mins to remove particulates [35]. | ≤ -20°C [35] | Assay immediately or aliquot for storage [35]. |
| Peripheral Blood Mononuclear Cells (PBMCs) | Room Temperature (before processing) [36] | Cryopreservation at -80°C or in liquid nitrogen [36] | Refrigeration at 4°C before processing markedly reduces cell yield [36]. |
How does long-term storage at -80°C affect specific inflammatory biomarkers?
Long-term storage at -80°C can differentially affect protein biomarkers. The stability of TRAIL, IP-10, and CRP was evaluated over five years, with results shown in the table below [9].
| Biomarker | Full Name | Stability at -80°C over 5 Years |
|---|---|---|
| TRAIL | TNF-related apoptosis-inducing ligand | Decreased by ~30% [9] |
| IP-10 | Interferon γ-induced protein 10 | Decreased by ~17% [9] |
| CRP | C-reactive protein | No significant decrease [9] |
What are the consequences of incorrect sample storage temperatures?
Incorrect storage can compromise experimental results, data integrity, and sample viability.
- Storage Too Warm: Accelerates decomposition and bacterial growth in biological tissues, leading to odor, tissue changes, and potential degradation of forensic or toxicological evidence [37]. In blood samples stored at room temperature, it can lead to co-purification of low-density neutrophils with PBMCs and reduced expression of certain cell surface receptors like chemokine receptors [36].
- Storage Too Cold: Freezing tissues causes ice crystals that rupture cell membranes; once thawed, damaged cells decompose much faster, complicating subsequent embalming or analysis [37]. Refrigerating whole blood at 4°C before PBMC processing has a marked negative effect on cell yield compared to room temperature storage [36].
Experimental Protocols for Sample Handling
Protocol 1: Processing Serum and Plasma Samples
This protocol is adapted from standard ELISA sample preparation guidelines [35].
Materials:
- Serum separator tube (SST) for serum or EDTA/heparin/citrate tube for plasma
- Centrifuge
- Pipettes and aliquoting tubes
- Freezer (-20°C or lower)
Workflow:
- Collection: Draw blood into the appropriate vacutainer tube.
- For Serum: Allow the sample to clot for 30 minutes at room temperature [35].
- Centrifugation: Centrifuge the sample at 1000 x g for 15 minutes [35].
- Aliquot Removal: Carefully remove the supernatant (serum or plasma) without disturbing the pellet or intermediate layers.
- Storage: Aliquot the supernatant into fresh tubes to avoid repeated freeze-thaw cycles and store at ≤ -20°C [35].
Protocol 2: Processing Whole Blood for PBMC Isolation
This protocol highlights the critical temperature consideration before density gradient centrifugation [36].
Materials:
- Whole blood collected in sodium heparin tubes
- Ficoll-Paque PLUS density gradient medium
- Centrifuge
- PBS
Workflow:
- Collection: Draw blood into sodium heparin vacutainers.
- Pre-Processing Storage: Store samples at Room Temperature (approx. 20°C) before processing. Do not refrigerate, as storage at 4°C significantly reduces PBMC yield [36].
- Density Gradient Separation: Within the desired timeframe (e.g., 6 or 24 hours), mix blood with an equal volume of PBS. Underlay with Ficoll-Paque and centrifuge at 500 x g for 30 minutes with the brake off [36].
- PBMC Isolation: Isolate PBMCs from the plasma-Ficoll interface.
- Wash and Cryopreserve: Wash cells with PBS supplemented with FBS. Cryopreserve PBMCs in freezing medium (e.g., containing 10% DMSO) at -80°C or in liquid nitrogen [36].
Sample Processing and Storage Workflow
Troubleshooting Common Scenarios
Problem: Poor cell yield after PBMC isolation from shipped blood samples.
- Possible Cause: Exposure to low temperatures (e.g., 15°C) during shipping, even for as little as 2 hours, can compromise PBMC recovery [36].
- Solution: Ensure blood samples are shipped at stable room temperature and processed as soon as possible. Validate shipping conditions with temperature logs.
Problem: Inconsistent or weak signal in downstream immunoassays like ELISA.
- Possible Cause: Incorrect storage of assay components or repeated freeze-thaw cycles of samples [35] [38].
- Solution:
Problem: Decreased levels of specific biomarkers detected in long-term biobank samples.
- Possible Cause: Some proteins, like TRAIL, degrade over time even at -80°C [9].
- Solution: When designing studies using biobanked samples, account for biomarker-specific degradation dynamics. Test sample stability for your specific biomarkers of interest under your storage conditions [9].
The Scientist's Toolkit
| Reagent / Material | Function | Example Use Case |
|---|---|---|
| EDTA/Heparin Tubes | Anticoagulant for plasma collection [35]. | Prevents blood clotting for plasma preparation. |
| Serum Separator Tubes (SST) | Facilitates serum separation after clotting [35]. | Used for clean serum sample collection. |
| Ficoll-Paque PLUS | Density gradient medium for isolating mononuclear cells [36]. | Separation of PBMCs from whole blood. |
| DMSO (Dimethyl Sulfoxide) | Cryoprotectant for freezing cells [36]. | Prevents ice crystal formation during cryopreservation of PBMCs. |
| Brilliant Stain Buffer | Reduces non-specific background in flow cytometry [39]. | Used when staining cells with polymer dye-conjugated antibodies. |
| Fc Receptor Binding Inhibitor | Blocks non-specific antibody binding via Fc receptors [39]. | Improves specificity of flow cytometry staining on human cells. |
| LIVE/DEAD Fixable Stain | Distinguishes live cells from dead cells [39]. | Viability staining for flow cytometry analysis. |
Troubleshooting Guides and FAQs
Frequently Asked Questions
Q1: What is the single most significant source of error in laboratory testing, and how can it be managed? The pre-analytical phase, encompassing everything from test ordering to sample processing, is the most significant source of error, accounting for 60-70% of all laboratory errors [21]. Many of these errors occur outside the laboratory proper. Management requires a multi-pronged approach, including the implementation of Standard Operating Procedures (SOPs), comprehensive education and training for all personnel involved in sample collection and handling, and the adoption of automation where possible to reduce manual errors [40] [21] [41].
Q2: For inflammatory marker research, which matrix is more suitable: serum or plasma? The choice depends on the specific analyte and research goals. Serum and plasma metabolomes are discernibly different [40]. Serum preparation involves a clotting process at room temperature, which can lead to the release of metabolites from platelets and other cells [40]. For cytokine stability research, studies on volumetric absorptive microsampling (VAMS) devices indicate that plasma might offer more consistent results, especially given that cytokine concentrations from finger-prick samples (often used with novel matrices) are much more variable than those from venous blood [42].
Q3: How critical is sample storage temperature for the stability of inflammatory markers like cytokines? Extremely critical. For cytokines stored in novel matrices like VAMS devices, room temperature—often the standard for dried blood spots—performed the poorest [42]. Storage at 4°C or colder is necessary for stability; at -20°C, 25 out of 31 cytokines were quantifiably stable for 3 months [42]. Similarly, for extracellular vesicle (EV) bioactivity, storage at -20°C or -80°C preserved function for 4-6 weeks [43].
Q4: What is the most common cause of a hemolyzed sample, and how can it be prevented? Most hemolysis identified in the laboratory (over 98%) is due to in vitro rupture of cells during or after collection, not a biological condition in the patient [44]. Prevention strategies include [44] [45]:
- Minimizing tourniquet time.
- Using an appropriately sized needle.
- Ensuring disinfectant alcohol has dried before venipuncture.
- Avoiding forceful transfer of blood from a syringe to a tube.
- Gently inverting tubes to mix, never shaking them.
Q5: Why is the order of draw during blood collection important? The correct order of draw prevents cross-contamination between sample tubes. For instance, if a tube containing the anticoagulant K3EDTA is used before a serum tube, trace amounts of EDTA can contaminate the serum sample. This leads to spuriously low calcium, magnesium, and zinc concentrations, falsely elevated potassium, and reduced alkaline phosphatase activity [44]. Adhering to a standardized order of draw is a simple but critical quality control step.
Troubleshooting Common Pre-analytical Problems
The following table outlines common issues, their potential impacts on your research data, and recommended corrective actions.
| Problem | Potential Impact on Research Data | Possible Root Cause | Corrective Action |
|---|---|---|---|
| Hemolyzed Sample [21] [44] | False elevation of intracellular analytes (K+, phosphate, LDH, AST); spectral interference. | Difficult venipuncture, forced syringe transfer, shaking tubes. | Adopt proper phlebotomy technique; gentle tube inversion. |
| Incorrect Sample Matrix [40] | Non-representative metabolite concentrations; inaccurate biomarker levels. | Use of serum when plasma is specified, or vice versa. | Validate and specify matrix in SOP; understand metabolite differences between serum/plasma. |
| Prolonged Clotting Time [40] | Altered metabolite profile (e.g., elevated lyso-phosphatidylcholines, serotonin). | Clotting time not standardized or overly long. | Standardize and strictly adhere to a defined clotting time (e.g., 30-60 min) for serum. |
| Improper Storage Temperature [42] [43] | Loss of analyte stability and bioactivity; degraded cytokines or EV function. | Samples left at room temperature for too long; inconsistent storage. | Validate stability for your analyte; store at 4°C or colder per established protocols. |
| Inadequate Sample Mixing [45] | Clotting in anticoagulated tubes; inhomogeneous sample. | Failure to properly invert tubes after collection. | Follow manufacturer's instructions for inversions; ensure lyophilized heparin is fully dissolved. |
| Air Exposure (for blood gases) [45] | Altered pO2 and, to a lesser extent, pH and pCO2. | Air bubbles in syringe; syringe not capped. | Expel bubbles immediately after draw; cap syringe; analyze promptly. |
Experimental Protocols & Stability Data
Stability of Inflammatory Markers in Novel Matrices
Research on the stability of cytokines in volumetric absorptive microsampling (VAMS) devices reveals that storage temperature is a critical determinant of analyte stability [42]. The following table summarizes quantitative findings for cytokine stability under different storage conditions over a 5-month period.
Table: Cytokine Stability in VAMS Devices Over 5 Months [42]
| Storage Temperature | Number of Stable Cytokines (Out of 21) | Key Findings |
|---|---|---|
| Room Temperature | 8 | Poorest performance; significant losses in 13/21 analytes. |
| 4°C | 17 | Good stability for the majority of analytes. |
| -20°C | Data extrapolated to 3 months: 25/31 stable | Optimal for longer-term storage; preserves most cytokine functionality. |
Detailed Methodology for Cytokine Stability in VAMS [42]:
- Sample Collection: Venous blood is collected from participants and spiked with recombinant cytokines.
- VAMS Sampling: Blood is collected into 30 µL volumetric absorptive microsampling (VAMS) devices.
- Storage Conditions: Prepared VAMS devices are stored at room temperature, 4°C, and -20°C for up to 5 months. Matching liquid extracts from VAMS are stored at -80°C as a comparator.
- Analysis: At predefined timepoints, samples are extracted from the VAMS devices and analyzed using a multiplex immunoassay (e.g., Luminex) for the quantification of up to 31 cytokines.
Stability of Extracellular Vesicle (EV) Bioactivity
For research involving extracellular vesicles, maintaining bioactivity is often the priority. The table below summarizes how storage conditions affect MSC-EV function.
Table: Stability of MSC Extracellular Vesicle (EV) Bioactivity [43]
| Storage Condition | Duration of retained Bioactivity | Key Findings |
|---|---|---|
| Room Temperature (Lyophilized) | Up to 6 weeks | Retained pro-vascularization and anti-inflammatory effects. |
| -20°C | Up to 4-6 weeks | Preserved bioactivity and functionality of loaded RNA cargo. |
| -80°C | Up to 4-6 weeks | Preserved bioactivity and functionality of loaded RNA cargo. |
Detailed Methodology for EV Storage and Bioactivity Testing [43]:
- EV Isolation: Mesenchymal stem/stromal cells (MSCs) are cultured in EV-depleted media. Conditioned medium is collected and EVs are isolated via differential ultracentrifugation with a final step of 100,000 × g. Pelleted EVs are resuspended in PBS and sterile-filtered.
- Storage Conditions: Isolated EVs are aliquoted and stored at RT, 4°C, -20°C, and -80°C. Separate aliquots are lyophilized and stored at RT.
- In Vitro Bioactivity Assay (Pro-vascularization): Human umbilical vein endothelial cells (HUVECs) are grown to a confluent monolayer. A scratch is made to create a "gap." Serum-starved HUVECs are treated with stored EVs, and gap closure is measured over 11 hours compared to controls.
- In Vivo Validation: The regenerative bioactivity of EVs (e.g., those loaded with lncRNA HOTAIR) can be tested in an animal model, such as a db/db mouse wound healing model.
Experimental Workflow and Decision Pathways
Pre-analytical Workflow for Blood Metabolomics
The following diagram outlines a standardized workflow for processing blood samples for metabolomics and inflammatory marker research, highlighting critical decision points to ensure sample integrity.
Troubleshooting Logic for Laboratory Equipment
Adopt a systematic "funnel" approach to efficiently diagnose and resolve instrument issues, moving from broad categories to a specific root cause [46].
The Scientist's Toolkit: Essential Research Reagents & Materials
| Item | Function in Pre-analytical Protocol |
|---|---|
| K3EDTA Tubes | Tripotassium ethylenediaminetetraacetic acid tubes are the preferred anticoagulant for plasma metabolomics and lipidomics studies, preventing coagulation by chelating calcium [47]. |
| Serum Tubes with Clot Activator | Used for serum preparation; the clot activator accelerates the clotting process. Requires standardized room-temperature incubation [40]. |
| Volumetric Absorptive Microsampling (VAMS) Devices | Novel matrix collection tool that accurately collects a fixed volume of blood (e.g., 30 µL) from a finger-prick, minimizing volume-based hematocrit effects [42]. |
| Lyophilized Heparin Syringes | Electrolyte-balanced, lyophilized heparin in commercial blood gas syringes prevents clotting without the sample dilution associated with liquid heparin, crucial for accurate pCO2 measurement [45]. |
| Cryogenic Vials | Specially designed vials for the secure long-term storage of aliquoted samples at ultra-low temperatures (-80°C) [40] [43]. |
| Liquid Chromatography-Mass Spectrometry (LC-MS) | A core analytical platform for reliably measuring a wide array of metabolites and lipids in clinical research samples [47]. |
| Nanoparticle Tracking Analysis (NTA) | Instrumentation (e.g., Nanosight) used for the quantification and size distribution of isolated extracellular vesicles prior to functional assays [43]. |
Volumetric Absorptive Microsampling (VAMS) is a novel technique for collecting small, precise volumes of biological fluids, such as blood, onto a porous, hydrophilic tip for dried sample analysis [48] [49]. This method is gaining traction in biomedical research and drug development for its ability to enable remote, minimally invasive sampling while maintaining sample integrity [50] [51]. A critical application of VAMS is the stabilization and quantification of cytokines—key protein markers of inflammation—which are notoriously unstable in both liquid and dried blood formats [52] [53]. This guide provides technical support for researchers aiming to optimize VAMS protocols specifically for cytokine stability research, framed within the broader context of optimizing storage conditions for inflammatory markers.
Troubleshooting Guides and FAQs
Frequently Asked Questions (FAQs)
FAQ 1: What is the primary advantage of using VAMS over traditional Dried Blood Spots (DBS) for cytokine analysis? VAMS devices actively absorb a fixed volume of blood (e.g., 10, 20, or 30 µL), which is largely independent of the blood's hematocrit (HCT) level [48] [54] [49]. Traditional DBS are applied to filter paper, where spot size and analyte distribution are highly influenced by HCT, leading to potential inaccuracies in quantification [53] [54]. Since VAMS uses the entire tip for analysis, it also negates issues related to spot inhomogeneity that can occur with DBS sub-punching [54] [49].
FAQ 2: Can cytokine levels from a finger-prick VAMS sample correlate with venous blood measurements? Yes, studies show that capillary whole blood microsamples collected via VAMS from a finger-stick can yield data that correlates with values from traditional venous blood collection [50]. However, it is important to note that cytokine concentrations from finger-prick samples can be more variable than those from venous blood [52]. Rigorous method validation, including correlation studies with venous blood, is essential for your specific assay [50].
FAQ 3: Why is room temperature storage not recommended for VAMS samples intended for cytokine analysis? While room temperature storage is often considered a standard for dried samples, it performs the poorest for cytokine stability. One study found significant losses in 13 out of 21 cytokines after 5 months of storage at room temperature [52]. Storage at 4 °C or colder is necessary for the majority of cytokines to remain quantifiably stable over extended periods [52] [53].
FAQ 4: How long does it typically take to implement a validated VAMS method for cytokine analysis? A full process from education to validation can take approximately 6 to 8 months [50]. This timeline includes phases for education and familiarization with the technology (1-2 weeks), method evaluation including extraction and linearity studies (4-6 weeks), and finally, a complete method validation including stability testing and pilot studies (6-8 months) [50].
Troubleshooting Common Experimental Issues
Problem: Inconsistent or low recovery of cytokines during extraction.
- Potential Cause: The extraction solvent or buffer conditions are not optimized for your target cytokines. Inefficient recovery, as was noted for fractalkine in one study, can be caused by the extraction process itself [52].
- Solution: Systematically optimize the extraction protocol. Key parameters to test include:
- Extraction Buffer: Compare different commercial protein extraction buffers (e.g., M-PER with salts) or tailor-made buffers [55]. The addition of protease inhibitors is crucial to prevent protein degradation during elution [55].
- Extraction Time and Agitation: Implement orbital shaking overnight at room temperature to maximize protein elution efficiency [55].
- Centrifugation: Use sufficient force (e.g., 12,000×g for 6 minutes) to ensure the entire eluate is collected [55].
Problem: High inter-sample variability in cytokine quantification.
- Potential Cause 1: Inconsistent sample collection technique, such as plunging the tip too deeply into the blood or not discarding the first blood drop, can lead to overfilling or contamination [49] [56].
- Solution: Standardize the finger-prick protocol. Clean the fingertip, discard the first blood drop, and hold the VAMS device at a 45° angle, dipping only the tip's leading surface into a subsequent droplet [49] [56].
- Potential Cause 2: Inadequate drying of the VAMS tips before storage can promote analyte degradation [54].
- Solution: Ensure tips are dried for a minimum of 2 hours at room temperature in a controlled environment, preferably with desiccant, before sealing for storage [54].
Problem: Analyte instability despite using VAMS.
- Potential Cause: Suboptimal storage temperature for the specific cytokines of interest. The optimal storage temperature can differ for each analyte [52] [53].
- Solution: Prior to committing to long-term studies, conduct a pilot stability test for your target cytokines across different temperatures (e.g., -20°C, 4°C, and room temperature) over a relevant timeframe. Store samples at -20°C or lower for the highest level of stability for most cytokines [52].
Data Presentation: Cytokine Stability in VAMS
The following table summarizes key quantitative data on cytokine stability in VAMS devices under different storage temperatures, based on a pivotal study that tracked stability for up to 5 months [52].
Table 1: Stability of Cytokines in VAMS Devices Under Different Storage Temperatures
| Storage Temperature | Storage Duration | Number of Stable Cytokines (Out of Total Tested) | Key Findings and Notes |
|---|---|---|---|
| Room Temperature | 5 months | 8 out of 21 | Poorest performance. Significant losses observed for 13 analytes. |
| +4 °C | 5 months | 17 out of 21 | Good performance for the majority of analytes. |
| -20 °C | 3 months | 25 out of 31 | Optimal short-to-mid-term storage condition. |
| Liquid Extracts at -80°C | 5 months | Used as a reference | Serves as a baseline for comparing dried sample stability. |
Experimental Protocols
Detailed Protocol: Assessing Cytokine Stability in VAMS
This protocol is adapted from stability research on cytokines in human blood collected using VAMS [52].
1. Sample Collection and Preparation:
- Collect venous blood from participants using standard venipuncture into anticoagulant tubes (e.g., K2EDTA). Alternatively, for a remote setting, use a finger-prick with a lancet.
- For method development, spike whole blood with recombinant cytokines at physiologically relevant concentrations.
- Use a 30 µL VAMS device (Mitra device). Hold the device at a 45° angle and touch the tip to the blood until it is fully saturated, indicated by a color change. Avoid plunging the entire tip into the blood.
- Repeat to prepare multiple VAMS devices per donor or condition.
2. Drying and Storage:
- Place the saturated VAMS devices in their dedicated cartridges or racks to dry for at least 2 hours at room temperature [54].
- Once dried, assign samples to different storage conditions for longitudinal stability testing. Key conditions to test include:
- Room temperature (e.g., ~20-25°C) +4 °C (standard refrigerator) -20 °C (standard freezer) -80 °C (for maximum stability, as a control)
- Include matching liquid extracts stored at -80°C as a reference for 100% recovery.
3. Sample Extraction:
- At each predetermined timepoint (e.g., 1 week, 1 month, 3 months, 5 months), remove samples from storage and allow them to equilibrate to room temperature.
- Place the entire VAMS tip into a microcentrifuge tube.
- Add an appropriate volume of extraction buffer. A recommended starting point is 300-350 µL of a commercial mammalian protein extraction reagent (e.g., M-PER) supplemented with protease inhibitors [52] [55].
- Securely cap the tubes and place them on an orbital shaker for overnight extraction (~16 hours) at room temperature [55].
- Centrifuge the tubes at 12,000 × g for 6-10 minutes to pellet any particulates [55].
- Carefully collect the supernatant (the extract) for immediate analysis or temporary storage at -80°C.
4. Cytokine Quantification:
- Analyze the extracts using a sensitive multiplex immunoassay, such as Luminex xMAP technology, capable of quantifying up to 31 cytokines simultaneously [52].
- Generate a standard curve using recombinant cytokine standards in the same extraction buffer to account for any matrix effects.
- Quantify cytokine concentrations in the samples and compare them to the baseline (T=0) concentrations and the liquid extract controls to determine percent recovery and stability.
Workflow Visualization
The following diagram illustrates the core experimental workflow for a VAMS cytokine stability study.
Figure 1: VAMS Cytokine Stability Study Workflow
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Key Reagents and Materials for VAMS-based Cytokine Research
| Item | Function/Description | Example/Note |
|---|---|---|
| VAMS Device | Collects a fixed volumetric sample of blood. | Mitra devices (10, 20, or 30 µL tips). 30 µL is common for proteomic studies [52] [48]. |
| Protease Inhibitor Cocktail | Prevents proteolytic degradation of cytokines during extraction and storage. | Add to extraction buffer to maintain protein integrity [55]. |
| Protein Extraction Buffer | Elutes proteins from the dried VAMS tip. | Commercial buffers like M-PER (Mammalian Protein Extraction Reagent), often requiring optimization with salts [52] [55]. |
| Recombinant Cytokines | Used for spiking experiments, standard curve generation, and assay controls. | Essential for method validation and quantifying recovery [52]. |
| Multiplex Immunoassay Kit | Quantifies multiple cytokines simultaneously from a small sample volume. | Luminex xMAP technology is widely used for this application [52] [55]. |
| Desiccant Packs | Controls humidity during sample storage and transport. | Prevents moisture-related degradation; store samples with desiccant in low-gas-permeable bags [55]. |
| Low-Protein Binding Plates/Tubes | Minimizes analyte loss due to adhesion to plastic surfaces. | Used during the extraction and assay steps to improve recovery [55]. |
Good Storage Practice (GSP) and Good Distribution Practice (GDP) Frameworks
Troubleshooting Guides and FAQs
How can I prevent the degradation of inflammatory markers in stored serum samples?
Problem: Measured concentrations of cytokines (e.g., TRAIL, IP-10) in serum samples decrease over time, potentially compromising research data.
Solution:
- Immediate Freezing: Process and freeze serum samples at -80°C or lower as soon as possible after blood collection. [9]
- Avoid Room Temperature Storage: Do not store samples at room temperature for extended periods. Volumetric absorptive microsampling (VAMS) devices stored at room temperature showed significant losses in most cytokines after 5 months. [42]
- Monitor Storage Duration: Be aware that degradation rates are biomarker-specific. For example, after five years at -80°C, TRAIL levels can decrease by ~30%, while CRP remains stable. [9]
Our temperature monitoring data shows an excursion during transport. What steps should we take?
Problem: A temperature logger indicates that a shipment of research samples exceeded the required temperature range.
Solution:
- Document the Excursion: Record all details of the deviation, including the magnitude, duration, and external conditions. [57] [58]
- Investigate the Root Cause: Perform a thorough investigation. Was the packaging validated? Was the pre-qualified shipping lane used? [57]
- Implement CAPA: Establish and document corrective and preventive actions (CAPA) to prevent recurrence. This is a key requirement inspectors will check. [57] [58]
- Assess Sample Impact: Evaluate whether the stability of the inflammatory markers in the shipment has been compromised based on known stability data for the specific biomarkers. [9]
How should I qualify a new storage unit or warehouse for my research materials?
Problem: A new freezer or storage room needs to be commissioned for storing temperature-sensitive reagents and samples.
Solution:
- Perform Temperature Mapping: Before use, conduct a mapping study under representative conditions (empty, full, seasonal extremes). Place data loggers at identified potential hot and cold spots to understand temperature variation. [57]
- Justify Sensor Placement: Provide a clear, risk-based rationale for the number and placement of monitoring sensors. [57]
- Define Requalification Triggers: Establish a protocol for re-mapping, which should be triggered by events like layout changes, HVAC modifications, or after a major temperature excursion. [57]
Stability of Common Inflammatory Markers
The table below summarizes stability data for selected inflammatory markers to inform your storage protocols.
Table 1: Stability Data for Selected Inflammatory Markers
| Biomarker | Full Name | Storage Condition | Storage Duration | Observed Change | Key Consideration |
|---|---|---|---|---|---|
| TRAIL [9] | TNF-related apoptosis-inducing ligand | -80°C | 5 years | ↓ ~30% | Highly sensitive to long-term storage; avoid repeated freeze-thaw cycles. |
| IP-10 [9] | Interferon γ-induced protein 10 | -80°C | 5 years | ↓ ~17% | Moderately stable for long-term storage. |
| CRP [9] | C-reactive protein | -80°C | 5 years | No significant decrease | Highly stable; suitable for retrospective studies using biobanks. |
| General Cytokines [42] | e.g., IL-1β, IL-6, TNF-α | 4°C (in VAMS devices) | 5 months | 17 of 21 analytes stable | 4°C is significantly better than room temperature for medium-term storage. |
| General Cytokines [42] | e.g., IL-1β, IL-6, TNF-α | Room Temp (in VAMS devices) | 5 months | 13 of 21 analytes showed significant losses | Least preferable storage condition. |
Experimental Workflow for Sample Stability Validation
Use the following workflow to design experiments for validating the stability of your inflammatory markers under specific storage conditions.
Research Reagent Solutions and Essential Materials
Table 2: Essential Materials for Inflammatory Marker Stability Research
| Item | Function/Application | Key Consideration |
|---|---|---|
| Volumetric Absorptive Microsampling (VAMS) Devices [42] | Standardized blood microsampling; minimizes volume variation. | Allows for stability testing of small sample volumes under different storage temperatures. [42] |
| Temperature Data Loggers | Continuous monitoring of storage units and shipments. | Must be calibrated and traceable to international standards (e.g., ISO 17025). [57] |
| Luminex Multiplex Assays [42] | Simultaneous quantification of multiple cytokines from a single sample. | Efficient for analyzing many analytes across multiple timepoints in a stability study. [42] |
| Pharmaceutical-Grade Freezers (-80°C) | Long-term storage of serum and plasma samples for biobanking. | Preferred for preserving integrity of most biomarkers; ensure continuous temperature monitoring. [9] [59] |
| Validated Sample Packaging | Maintaining temperature during transport of samples between sites. | Use qualified, validated containers for shipments to prevent stability-compromising excursions. [57] [59] |
Regulatory and Quality Framework
The following diagram outlines the core interconnected components of a GDP/GSP quality system that ensures data integrity in a research setting.
Leveraging Electronic Lab Notebooks (ELNs) for Tracking Storage Conditions and Metadata
FAQs: ELNs for Storage Condition Tracking
Q1: How can an ELN help ensure the integrity of my inflammatory marker samples? An ELN ensures sample integrity through centralized, structured data capture. You can record storage conditions (e.g., freezer temperature, freeze-thaw cycles) directly in the sample's digital record in real-time. The ELN automatically tracks changes and maintains a complete audit trail, documenting who recorded the data and when, which is crucial for proving sample integrity and data provenance [60] [61].
Q2: What specific metadata should I track for inflammatory markers like CRP or IL-6? For inflammatory markers, essential metadata includes storage temperature, tube type (e.g., cryovial), freeze-thaw count, and storage location (e.g., freezer ID, shelf, box) [62]. Critically, you should also record the time interval between sample measurements, as stability varies significantly over time. The ELN can standardize this metadata entry, ensuring all required fields are completed for FAIR (Findable, Accessible, Interoperable, and Reusable) data principles [60] [61].
Q3: My ELN doesn't have a template for tracking freezer temperatures. What should I do? Many modern ELNs are configurable, allowing you to create custom data entry forms or templates without needing developer support [63] [64]. Design a template with fields for date/time, temperature, equipment ID, and the researcher's name. If your ELN is not flexible, avoid over-customizing a rigid platform, as this can lead to fragile systems and high maintenance costs; instead, consider a more configurable solution [63].
Q4: How do I link a specific storage location in the freezer with a sample record in the ELN? Best practice involves using the ELN's sample management features to record the precise storage path—including freezer ID, shelf, rack, and box coordinates—within the sample's digital record [65] [62]. Some systems allow you to pre-define these locations in the inventory. It is not recommended to simply paste a file path link to a dataset, as these can change; instead, document the full location details directly in the ELN record [62].
Q5: We use multiple freezers. How can the ELN help manage stability across different storage units? An ELN with integrated inventory management provides a central dashboard showing all storage units and their contents. You can assign samples to specific freezers and use the ELN's search and filtering functions to quickly locate all samples stored under a particular condition (e.g., all samples in a -80°C freezer versus a -20°C freezer) [65]. This provides a complete overview for monitoring stability across your entire storage infrastructure [66].
Troubleshooting Guides
Problem: Inconsistent Metadata is Compromising Data Reproducibility
- Symptoms: Difficulty tracing sample history, conflicting storage records between team members, inability to replicate previous experiments.
- Solution:
- Standardize with Templates: Create and enforce the use of standardized ELN templates for specific sample types (e.g., "Plasma Sample - Cytokine Analysis") [60] [66].
- Define Required Fields: Configure templates to make critical metadata fields (like storage temperature and freeze-thaw count) mandatory [60].
- Train the Team: Conduct training to ensure all lab personnel understand the protocols and consistently use the same terminology [63] [67].
- Prevention: Involve all end-users in the template design process to ensure the workflow is practical and adopted. Use the ELN's access control to designate who can edit core metadata fields, preventing unauthorized changes [62] [67].
Problem: Unable to Track Sample Lineage and Provenance
- Symptoms: Uncertainty about a sample's origin (e.g., parent sample), previous manipulations, or complete storage history.
- Solution:
- Leverage Inventory Links: Use the ELN's inventory function to create a master record for each original sample. Link all aliquots and derivatives back to this master record [65].
- Record Every Action: Document every activity (e.g., "aliquoted from Sample X," "moved to Freezer Y") as a step in the ELN protocol, creating a chronological timeline [61].
- Utilize Audit Trails: Rely on the ELN's automatic audit trail to verify the complete history of changes to the sample record [60] [64].
- Prevention: Implement a lab policy that requires creating sample records in the ELN before the physical sample is generated. This builds provenance into the process from the very start [67].
Problem: Integration Failure Between ELN and Temperature Monitoring Hardware
- Symptoms: Manual data entry from standalone temperature loggers is prone to errors and delays; data silos.
- Solution:
- Check for Native Integrations: Verify if your ELN vendor offers pre-built integrations with common lab monitoring hardware [63].
- Explore API Options: For specialized instruments, investigate if your ELN supports API (Application Programming Interface) connections to automate data flow [64].
- Implement a Unified Platform: Consider a platform that combines ELN with LIMS (Laboratory Information Management System) functionalities, as they often have stronger instrument integration capabilities for a cohesive data environment [63] [65].
- Prevention: Before purchasing new storage equipment or an ELN, evaluate integration capabilities as a key selection criterion to avoid fragmentation [63] [68].
Experimental Protocol: Monitoring Inflammatory Marker Stability
Objective: To systematically assess the stability of inflammatory markers (e.g., CRP, IL-6, TNF-α) under different storage conditions using an ELN for data integrity.
Background: The stability of inflammatory biomarkers is time-dependent. The following quantitative data should guide the design of stability assessment experiments [69]:
Table 1: Temporal Stability of Key Inflammatory Markers
| Inflammatory Marker | Stability <6 Months (r) | Stability 6 Months - 3 Years (r) | Stability >3 Years (r) |
|---|---|---|---|
| C-Reactive Protein (CRP) | Strong (0.80-0.61) | Moderate (0.60-0.51) | Low (0.39-0.30) |
| Interleukin-6 (IL-6) | Strong (0.80-0.61) | Moderate (0.60-0.51) | Low (0.39-0.30) |
| Tumor Necrosis Factor-α (TNF-α) | Strong (0.80-0.61) | Moderate (0.60-0.51) | Low (0.39-0.30) |
| Fibrinogen (Fg) | Variable | Variable | Moderate (0.53) |
Source: Meta-analysis data on stability estimates (correlation coefficients) across different time intervals [69].
Methodology
ELN Setup (Pre-Experiment):
Sample Storage and Condition Tracking:
- Divide Samples: Aliquot samples into groups for different storage conditions (e.g., -80°C, -20°C, 4°C).
- Record Metadata: For each aliquot in the ELN, log the following metadata [62] [61]:
Sample ID(linked to inventory)Storage TemperatureStorage Location(e.g., Freezer ID, box coordinates)Date/Time of StorageResearcher
- Monitor Conditions: Use integrated temperature probes and record data directly into the ELN, or manually log temperatures at set intervals as defined in the protocol.
Periodic Analysis and Data Recording:
- Based on the stability data in Table 1, establish a measurement schedule (e.g., baseline, 1 month, 6 months, 1 year, 3+ years).
- For each time point, retrieve the relevant samples, record the freeze-thaw cycle count in the ELN, and perform the assay.
- Upload the raw data files (e.g., instrument outputs) directly to the corresponding ELN experiment entry and link them to the sample records [61].
Data Analysis and Documentation:
- Use the ELN's note-taking features to document observations and initial conclusions.
- Export data for statistical analysis. The correlation coefficients (r) from your analysis can be compared against the reference data in Table 1 to validate your storage conditions.
- Store the final analysis results and reports in the ELN, ensuring a complete chain of custody from raw data to final result [60] [61].
Workflow and Data Relationships
The following diagram illustrates the integrated workflow for tracking samples and metadata in an ELN, from initial setup to final analysis, ensuring data provenance.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Inflammatory Marker Stability Research
| Item | Function in Experiment |
|---|---|
| Validated Immunoassay Kits (e.g., ELISA) | To quantitatively measure the concentration of specific inflammatory markers (CRP, IL-6, TNF-α) in samples at each stability time point. |
| Low-Protein Binding Tubes | To prevent the adhesion of proteins (like cytokines) to tube walls, which could artificially lower measured concentrations and skew stability data. |
| Controlled-Temperature Freezers (-80°C, -20°C) | To provide stable, documented long-term storage environments for testing the impact of different temperatures on biomarker integrity. |
| Programmable Temperature Loggers | To continuously monitor and document the storage temperature of freezers, providing critical metadata to correlate with analyte stability. |
| LIMS/ELN with Sample Tracking | To manage sample inventory, record all storage condition metadata, link raw data files, and maintain a full audit trail for reproducibility and compliance [65] [66]. |
| Liquid Handling Robots | To automate the aliquoting of samples, ensuring consistency and minimizing pre-analytical variability that could affect stability results. |
| Barcode/Label Printer | To generate unique, scannable identifiers for every sample aliquot, ensuring unambiguous tracking and linking to the ELN record throughout its lifecycle [67]. |
Solving Stability Problems: Addressing Pre-analytical Variability and Recovery Issues
Frequently Asked Questions
1. Why is my fractalkine recovery from VAMS samples low, even when other cytokines perform well? Specific research has identified that fractalkine can suffer from inefficient recovery during the extraction process from VAMS devices, a problem not observed with all cytokines [42]. This suggests the issue is not with storage but is specific to how fractalkine is liberated from the VAMS tip and prepared for analysis.
2. What are the best storage conditions for VAMS samples containing cytokines like fractalkine? While the extraction process is critical for fractalkine, overall sample integrity depends on proper storage. For cytokine stability in VAMS devices, storage at 4 °C or colder is recommended. One study found that room temperature storage, which is often a standard for dried samples, resulted in the poorest performance, with significant losses in over half of the cytokines analyzed over five months [42].
3. My method has low recovery. Can I just use a correction factor for my final results? It is generally not recommended to use a recovery correction factor (e.g., dividing your result by 0.4 for a 40% recovery) as it can mask underlying issues with the method's performance. Best practice is to investigate and optimize the extraction or sample preparation to resolve the root cause of low recovery [70].
Troubleshooting Guide: Low Fractalkine Recovery in VAMS
Problem: Inefficient Extraction from VAMS Matrix
The primary identified cause for poor fractalkine recovery is its inefficient release from the VAMS tip during the extraction process [42]. A suboptimal protocol can lead to the analyte being trapped or degraded.
Solution: Optimize Your Extraction Protocol Implement a robust, homogenization-intensive extraction method. The protocol below, adapted from a validated approach for challenging analytes, has been shown to enhance recovery and reduce variability [71].
Detailed Experimental Protocol: Optimized VAMS Extraction
- Step 1: Sample Preparation. Open the VAMS cartridge using the manufacturer's tool. Using a pipette tip, gently push the VAMS tip into a reinforced 2 mL extraction tube containing three stainless steel balls.
- Step 2: Solvent Addition. Add 100 µL of a desorption solvent (e.g., 40% methanol containing appropriate internal standards) to the tube.
- Step 3: Sonication. Sonicate the sample tubes at 30°C for 10 minutes. This helps desorb the analyte from the polymer.
- Step 4: Precipitation and Homogenization. Add 200 µL of an extraction solvent (e.g., methanol: 0.2 M ZnSO4, 80:20, v/v). Then, homogenize the mixture at 6800 rpm for 5 minutes with intermittent pauses (e.g., 20-second pauses). This bead-based impact step is crucial for mechanically breaking apart the matrix and achieving high, reproducible recovery.
- Step 5: Final Processing. Mix the tubes on a Bioshaker at 1800 rpm for 5 minutes, followed by centrifugation at 16,000 RCF for 5 minutes at 4°C. Transfer the supernatant for analysis [71].
Problem: Suboptimal Storage Conditions
Although the main issue with fractalkine is extraction, improper storage can compound problems and affect other biomarkers in your study.
Solution: Implement Cold Storage Immediately After Drying Do not store your VAMS samples at room temperature for extended periods. The evidence indicates that for longitudinal stability of cytokines in VAMS:
- For storage up to 3 months, -20 °C is optimal.
- For storage up to 5 months, 4 °C is effective for most cytokines [42].
The following table summarizes the quantitative stability data for cytokines stored under different conditions, highlighting the superiority of cold storage [42].
Stability of Cytokines in VAMS Devices Under Different Storage Temperatures
| Storage Duration | Storage Temperature | Number of Stable Cytokines (out of total tested) | Key Performance Note |
|---|---|---|---|
| 3 Months | -20 °C | 25 / 31 | Optimal short-to-mid term storage condition |
| 4 °C | Information missing | Performance good, but inferior to -20°C | |
| Room Temperature | Information missing | Significant analyte losses observed | |
| 5 Months | 4 °C | 17 / 21 | Recommended for mid-term storage |
| Room Temperature | 8 / 21 | Poorest performance; significant losses in 13/21 analytes |
Problem: Matrix Effects and Interference
Matrix effects can suppress or enhance the analyte signal during LC-MS/MS analysis, leading to inaccurate quantification and low apparent recovery.
Solution: Investigate and Mitigate Matrix Effects
- Change the Solvent Composition: Modify the solvent used for extraction. This can include adding a very small amount of a weak base (like ammonia) or an acid to the extraction solvent to improve efficiency and reduce side reactions [70].
- Improve Chromatographic Separation: If a large interfering peak is seen near the fractalkine peak, modify the LC method (e.g., gradient, column type) to achieve better separation and reduce interference [70].
- Consider Alternative Ionization: In cases of severe matrix suppression in ESI+, switching to an APCI (Atmospheric Pressure Chemical Ionization) source can sometimes reduce these effects [70].
The Scientist's Toolkit: Essential Research Reagents & Materials
The following table lists key materials and their functions for successfully working with VAMS and analyzing fractalkine.
Essential Materials for VAMS-based Fractalkine Research
| Item | Function in the Workflow |
|---|---|
| Volumetric Absorptive Microsampling (VAMS) Devices | Collects a fixed volume (e.g., 10-30 µL) of whole blood or plasma, minimizing hematocrit effects compared to DBS [72] [56]. |
| Reinforced Extraction Tubes | Withstands the mechanical stress of high-speed homogenization with stainless steel balls [71]. |
| Stainless Steel Homogenization Balls | Provides mechanical bead-based impact to disrupt the VAMS matrix and enhance analyte recovery [71]. |
| Sonication Water Bath | Aids in the desorption of the analyte from the VAMS tip using ultrasonic energy [71] [73]. |
| LC-MS/MS System | Provides the high sensitivity and selectivity required for quantifying low levels of fractalkine in small sample volumes [72] [73]. |
| C18 or C8 LC Column | Stationary phase for chromatographic separation of fractalkine from matrix components before mass spectrometric detection [73]. |
Mitigating Inter-assay and Inter-laboratory Variability in Biomarker Measurement
Technical Support Center: Troubleshooting Guides
ELISA Troubleshooting Guide
Problem: Weak or No Signal
| Possible Cause | Solution |
|---|---|
| Reagents not at room temperature | Allow all reagents to sit on bench for 15–20 minutes before starting assay [74]. |
| Incorrect storage of components | Double-check storage conditions on kit label; most kits need 2–8°C storage [74]. |
| Expired reagents | Confirm expiration dates on all reagents; do not use expired reagents [74]. |
| Insufficient detector antibody | Follow manufacturer-recommended antibody dilutions precisely [74]. |
| Capture antibody didn't bind to plate | Ensure you are using an ELISA plate (not tissue culture plate) and correct coating protocol [74]. |
Problem: High Background Signal
| Possible Cause | Solution |
|---|---|
| Insufficient washing | Increase duration of soak steps; add 30 seconds each time you let wash buffer soak [74]. |
| Plate sealers not used or reused | Use fresh plate sealers each time the plate is opened to prevent well contamination [74]. |
| Substrate exposed to light | Ensure substrate is not exposed to light; store in dark place and limit light exposure during assay [74]. |
| Longer incubation times | Follow recommended incubation times precisely [74]. |
Problem: Poor Replicate Data
| Possible Cause | Solution |
|---|---|
| Insufficient washing | Ensure complete drainage after each wash step; invert plate on absorbent tissue and tap forcefully [74]. |
| Inconsistent incubation temperature | Maintain consistent incubation temperature; be aware of environmental fluctuations [74]. |
| Incorrect pipetting technique | Check pipetting technique and double-check dilution calculations [74]. |
Sample Storage & Stability Troubleshooting
Problem: Inconsistent Cytokine Measurements in Dried Blood Samples
| Possible Cause | Solution |
|---|---|
| Room temperature storage | Avoid RT storage; significant losses occur in 13/21 analytes at 5 months [42]. |
| Inefficient analyte recovery | Optimize extraction protocols; fractalkine showed poor recovery due to extraction issues [42]. |
| Sample type variability | Use venous blood instead of finger-prick samples when possible;后者 show much higher variability [42]. |
Recommended Storage Conditions for Cytokines in VAMS Devices
| Storage Temperature | Performance | Recommended For |
|---|---|---|
| Room Temperature | Poorest performance | Not recommended for long-term storage |
| 4°C | 17/21 cytokines stable at 5 months | Short to medium-term storage |
| -20°C | 25/31 cytokines stable at 3 months | Long-term storage recommended |
Frequently Asked Questions (FAQs)
Pre-Analytical Phase
Q: What are the most critical pre-analytical factors affecting biomarker stability? A: Pre-analytical errors account for up to 75% of testing errors. Critical factors include: collection tube type and components, sample-to-anticoagulant ratio, time between venepuncture and centrifugation, centrifugation speed/temperature, processing time before analysis, and storage duration/temperature. Automated procedures can reduce error rates [75].
Q: How does sample type affect inflammatory biomarker measurements? A: Significant differences exist between sample types. Venous blood provides more consistent results than finger-prick samples, which show much higher variability. Different biofluids (serum, urine, sweat, saliva) may show varying correlations with gold-standard serum measurements [42] [76].
Analytical Validation
Q: What is the difference between analytical and clinical validation? A: Analytical Validation establishes the technical performance of the detection method (sensitivity, specificity, accuracy, precision). Clinical Validation evaluates the biomarker's usefulness as a decision-making tool for its intended Context of Use. Analytical validation must precede clinical validation [77].
Q: What performance specifications should we use for biomarker assays? A: Use the biological variation (BV) framework with three performance levels. For example, with HbA1c (CVI=1.2%, CVG=5.4%): Optimum (CVa<0.3%, TEa<1.2%), Desirable (CVa<0.6%, TEa<2.4%), and Minimum (CVa<0.9%, TEa<3.6%). Clinical guidelines may specify additional requirements like CV<1.5% [78].
Methodologies & Protocols
Q: What experimental design is needed for validating storage stability? A: The NOVA study protocol provides a robust framework: include both test and control groups (e.g., patients with systemic inflammation vs controls), collect multiple biofluids simultaneously (serum, urine, sweat, saliva, exhaled breath, stool), measure core biomarkers (CRP, IL-1β, IL-6, IL-8, IL-10, TNF-α) across all samples, and store at different temperatures for longitudinal analysis [76].
Experimental Workflow for Storage Stability Validation
Q: How do we implement quality control for long-term biomarker studies? A: Implement a comprehensive QC system including: Internal Quality Control (IQC) to monitor ongoing validity against specified criteria, and External Quality Assessment (EQA) to compare performance across laboratories. Analyze both intra-laboratory variation (within-lab precision) and inter-laboratory variation (between-lab consistency) using statistical methods like robust algorithms per ISO 13528 guidelines [78].
Quality Control Implementation Framework
Data Analysis & Interpretation
Q: How do we analyze inter-laboratory variation data? A: Use established statistical methods: calculate robust averages and standard deviations per ISO 13528, determine coefficient of variation (CV) for both intra-lab and inter-lab comparisons, evaluate against biological variation criteria (optimum, desirable, minimum), and analyze manufacturer-specific bias by comparing group robust averages against overall targets [78].
Q: What constitutes acceptable performance for inflammatory biomarker assays? A: Performance requirements depend on context of use. For diagnostic applications, aim for optimum biological variation standards (CVa<0.3%). For research use, desirable (CVa<0.6%) or minimum (CVa<0.9%) standards may suffice. Always consider clinical needs - for HbA1c, clinical guidelines require CV<1.5% for intra-laboratory variation and <2.5% for inter-laboratory variation [78].
Research Reagent Solutions & Essential Materials
Key Materials for Inflammatory Biomarker Stability Research
| Reagent/Material | Function & Application | Technical Considerations |
|---|---|---|
| Volumetric Absorptive Microsampling (VAMS) Devices | Standardized blood collection; precise 30 µL volume [42] | Optimal storage: 4°C or -20°C; avoid room temperature |
| Multiplex Immunoassay Panels (Luminex) | Simultaneous quantification of up to 31 cytokines [42] | Validate against single-analyte assays; check cross-reactivity |
| High-Sensitivity CRP (hs-CRP) Assays | Detect low-grade inflammation in psychiatric disorders [79] | Differentiates pentameric vs monomeric CRP isoforms |
| ELISA Kits for Cytokine Profiling | Quantify IL-1β, IL-6, IL-8, IL-10, TNF-α [76] | Ensure proper storage (2-8°C); bring to RT before use |
| Quality Control Materials (Bio-Rad) | Liquid control samples based on human whole blood [78] | Verify homogeneity and stability per ISO 13528:2022 |
| CLSI Evaluation Protocols (EP05, EP15) | Standards for assay precision validation [75] | EP05 for extensive validation; EP15 for verification |
Experimental Protocols for Key Experiments
Protocol: Stability Testing of Inflammatory Biomarkers in VAMS Devices
Objective: Evaluate the stability of cytokines in volumetric absorptive microsampling (VAMS) devices under different storage conditions for up to 5 months [42].
Materials:
- VAMS devices (30 µL capacity)
- Venous blood from healthy participants (n=4)
- Recombinant cytokines for spiking
- Storage conditions: Room temperature, 4°C, -20°C
- Analysis platform: Luminex for 31 cytokines
Procedure:
- Collect venous blood from participants
- Spike with recombinant cytokines to known concentrations
- Collect into 30 µL VAMS devices using standardized technique
- Store devices at three temperatures (RT, 4°C, -20°C)
- Prepare matching liquid extracts stored at -80°C as controls
- Analyze cytokines at multiple timepoints over 5 months
- Include remote clinical study validation over 8 months
Quality Control:
- Monitor extraction efficiency (fractalkine showed poor recovery)
- Use venous blood rather than finger-prick samples due to lower variability
- Include both healthy and patient populations in validation studies
Protocol: Inter-laboratory Variation Assessment
Objective: Evaluate intra-laboratory and inter-laboratory variations using EQA and IQC data [78].
Materials:
- EQA samples (5 liquid control samples based on human whole blood)
- IQC materials (two QC levels)
- Multiple participating laboratories (n=326)
- Standardized reporting platform
Procedure:
- Distribute EQA samples to all participating laboratories annually
- Collect results electronically via standardized platform
- Analyze data using robust algorithm per ISO 13528:2022
- Calculate acceptance rates per sample, per year, and per manufacturer
- Collect monthly IQC data voluntarily from participating labs
- Calculate intra-laboratory CV from IQC data
- Calculate inter-laboratory CV from EQA data
Performance Specifications:
- Biological variation criteria: Optimum (CVa=0.3%, TEa=1.2%), Desirable (CVa=0.6%, TEa=2.4%), Minimum (CVa=0.9%, TEa=3.6%)
- Clinical guidelines: Intra-laboratory CV <1.5%, Inter-laboratory CV <2.5%
Statistical Analysis:
- Use non-parametric statistics for non-normal distributions
- Shapiro-Wilk test for normality
- Mann-Whitney U test or Kruskal-Wallis test for differences
- Dunn's multiple comparisons test for post-hoc analysis
Protocol: Multi-Biofluid Inflammatory Biomarker Correlation
Objective: Evaluate relationship between serum inflammatory biomarkers and non-invasively measured biomarkers in urine, sweat, saliva, exhaled breath, and stool [76].
Study Design: Single-center, cross-sectional study with 20 participants (10 patients with systemic inflammation, 10 controls)
Primary Endpoint: C-reactive protein (CRP) levels Secondary Endpoints: IL-1β, IL-6, IL-8, IL-10, TNF-α levels Tertiary Endpoints: Fractional exhaled nitric oxide, calprotectin, core body temperature
Sample Collection:
- Collect serum (gold standard), urine, sweat, saliva, exhaled breath, and stool samples simultaneously
- Measure core body temperature using sensor
- Process all samples within specified timeframes
- Store aliquots at appropriate temperatures
Analytical Methods:
- CRP and cytokine levels: ELISA and electrochemiluminescence immunoassay
- Statistical analysis: Shapiro-Wilk test for normality, t-test or Wilcoxon rank sum test for group comparisons
- Correlation analysis: Pearson and Spearman coefficients
- Predictive modeling: All-subset regression analysis for optimal biomarker combinations
Context of Use Framework for Biomarker Development
Urine presents an ideal, non-invasive source of biomarkers for monitoring inflammatory conditions and various diseases [80]. Unlike blood, whose composition is tightly regulated, urine is not subjected to homeostatic mechanisms and can range widely in pH, osmolality, and solute concentration, even within the same individual over hours or days [81]. This inherent variability, combined with the instability of many analytes after collection, poses significant challenges for researchers seeking to implement reliable urine-based assays. Proper collection, storage, and handling are crucial to maintaining sample integrity and ensuring accurate analytical results [82]. This technical guide addresses the key considerations for optimizing urine sample stability, with a specific focus on applications in inflammatory marker research, to support robust and reproducible experimental outcomes.
Fundamental Concepts of Urine Stability
Key Factors Affecting Urine Analyte Integrity
Multiple factors can compromise the integrity of urine samples between collection and analysis. Understanding these variables is the first step in designing a robust storage protocol.
- Time and Temperature: Urine is an unstable fluid that begins changing composition immediately after elimination [82]. Bacterial growth is a primary concern at room temperature, which can metabolize glucose, alter pH, and degrade target analytes [82]. Generally, the cooler the storage temperature, the longer the stability of most analytes.
- pH and Osmolality: The highly variable pH of urine can directly affect the stability of proteins and nucleic acids. Furthermore, enzymatic activity and chemical degradation rates are often pH-dependent.
- Bacterial Contamination: Introduced during collection or present in the urinary tract, bacteria can consume analytes, produce interfering substances, and release nucleases that degrade nucleic acids [82] [83].
- Physical Processes: Repeated freeze-thaw cycles can denature proteins and fragment nucleic acids. Exposure to light can decompose light-sensitive compounds like bilirubin and urobilinogen [82].
Stability of Different Analyte Classes
Not all biomarkers degrade at the same rate. The table below summarizes general stability findings for different classes of molecules relevant to inflammatory and disease research, based on the provided literature.
Table 1: Stability of Urinary Analytes Under Different Storage Conditions
| Analyte Class | Example Biomarkers | Room Temperature | Refrigerated (4°C) | Frozen (-20°C or -80°C) | Key Evidence |
|---|---|---|---|---|---|
| Inflammatory Proteins | CRP, VEGF, IL-1RA, IP-10 | Limited stability; significant changes in MMP-9, APOE, ANG reported within 24h [83]. | Stable for up to 1 week for multiple proteins in multiplex immunoassays [83]. | Stable for at least 1 month at -20°C [83]. | Study on 10-plex bladder cancer immunoassay (Oncuria) [83]. |
| Extracellular Vesicle (EV) RNAs | mRNA, miRNA (e.g., RNY4) | EV RNAs show remarkable stability; stable for up to 6 months at RT in preservative [81]. | Suitable for short-term storage. | Long-term preservation at -80°C is standard [81]. | Evaluation of urine storage at RT and -80°C for 6 months [81]. |
| Cell-Free DNA (cfDNA) | Tumor DNA, Fetal DNA | Highly unstable without preservatives; rapid degradation by nucleases [84]. | Requires stabilization; cold chain alone may not prevent degradation. | Long-term storage after stabilization. | Research indicates need for novel stabilization solutions [84]. |
| General Urinalysis Parameters | Cells, Casts, Crystals | Unstable; should be analyzed within 1-2 hours of collection [82]. | Can be refrigerated for up to 24 hours [82] [85]. | Not recommended for microscopic examination. | Standard clinical guideline [82]. |
Frequently Asked Questions (FAQs)
Q1: What is the maximum time a urine sample can be stored at 4°C before processing for protein biomarker analysis? For a broad range of protein biomarkers, refrigeration at 4°C provides excellent short-term stability. One study evaluating a 10-protein multiplex immunoassay (Oncuria) found that urine samples stored at 4°C showed little-to-no change in the measured concentrations of any of the 10 analytes for up to one week [83]. For standard urinalysis, refrigeration for up to 24 hours is acceptable [82] [85].
Q2: Can I use the first morning void instead of 24-hour urine collection to reduce participant burden in longitudinal studies? This decision requires careful consideration. While first morning void urine is more concentrated and often preferred for detecting trace analytes [82], it may not accurately reflect the total daily excretion of all biomarkers. A study specifically designed to test this found that correlations between inflammatory marker levels in overnight portions and 24-hour urine samples "varied widely between individuals" [86]. The authors concluded that 24-hour urine cannot be reliably replaced by an overnight portion for all research applications. The choice should be piloted for your specific biomarkers of interest.
Q3: How can I stabilize cell-free DNA (cfDNA) in urine for transport without immediate freezer access? Urinary cfDNA is particularly susceptible to degradation by nucleases at room temperature [84]. Commercial liquid preservation reagents (e.g., Streck Urine Preserve) are designed to mitigate cell lysis and inhibit nuclease activity, stabilizing nucleic acids for up to seven days at temperatures between 6-37°C [84]. This provides a practical alternative to immediate freezing or resource-intensive cold chain logistics.
Q4: What is the best method to normalize urinary biomarker levels to account for variations in urine concentration? This remains a methodological challenge. While creatinine normalization is most common, it has limitations, as its variations are not solely due to urine concentration and it can mask disease-related changes [81]. Alternative strategies showing promise include:
- Total urine protein or albumin: These showed excellent correlation with extracellular vesicle (EV) content in one study [81].
- Time-normalization (24-h collection): Considered gold standard but is burdensome [81].
- Endogenous EV RNA normalizers: Research suggests specific RNAs, such as RNY4 and a small miRNA panel, can effectively reflect inter-sample EV variation and serve as post-analytical normalizers [81]. The optimal method may depend on your specific analyte and research question.
Troubleshooting Guide
Table 2: Common Urine Sample Problems and Solutions
| Problem | Potential Consequences | Recommended Solutions | Root Cause |
|---|---|---|---|
| Degradation of Protein Biomarkers | Altered concentration measurements, loss of signal, inaccurate data. | Process immediately or refrigerate at 4°C. For stability beyond 24h, freeze at -20°C or -80°C. Test analyte-specific stability [83]. | Enzymatic degradation, bacterial growth, or protein denaturation at elevated temperatures. |
| Low Yield of Urinary cfDNA | Inability to perform downstream genetic analyses (qPCR, ddPCR). | Use a commercial urine preservative at collection to inhibit nucleases [84]. Avoid freeze-thaw cycles. | Degradation by nucleases present in urine, which is exacerbated by delayed processing or storage at RT. |
| High Variability in Biomarker Levels | Inability to distinguish biological from pre-analytical variation. | Standardize collection time (e.g., first morning void). Implement a consistent normalization strategy (see FAQ #4) [81]. | Natural diurnal variation and differences in urine concentration due to hydration status. |
| Bacterial Contamination | Altered pH, consumption of glucose, generation of false-positive/false-negative results [82]. | Use clean-catch collection methods. Refrigerate samples promptly. Consider adding antibiotics (e.g., Trimethoprim) for certain assays, though efficacy may vary [83]. | Improper collection technique or proliferation of bacteria during prolonged storage at RT. |
| Inconsistent EV Recovery | Biased omics data, poor reproducibility. | Standardize the EV isolation protocol (e.g., UC, precipitation). Correlate EV counts with normalization factors like total protein [81]. | Inefficient or variable isolation methods and inherent fluctuations in EV secretion into urine. |
Detailed Experimental Protocols
Protocol: Intensive Longitudinal Urine Collection for Inflammatory Marker Stability Assessment
This protocol is adapted from a study that successfully measured inflammatory markers in daily urine collections over 63 days [86].
Objective: To assess the long-term stability and intra-individual variability of inflammatory markers in urine stored under conditions simulating a longitudinal study.
Materials:
- Sterile screw-cap containers for 24-hour urine collection.
- Portable coolers or refrigerators for participants.
- Aliquot tubes (e.g., 2 mL cryovials).
- -80°C freezer for long-term storage.
- Multiplex immunoassay kits (e.g., for CRP, Fractalkine, IL-1RA, IFN-α, IFN-γ, IP-10, MIP-1β, VEGF).
Method:
- Participant Instruction: Train participants in the clean-catch midstream technique and the proper procedure for 24-hour urine collection. Emphasize the importance of keeping the collection container cool throughout the day.
- Sample Collection: Participants collect all urine produced over a full 24-hour period for 63 consecutive days. The total volume is measured and recorded.
- Sample Processing: Upon return, mix the 24-hour urine sample thoroughly. Aliquot into cryovials. Centrifuge aliquots intended for analysis at 1000–2000 × g for 10 minutes to remove cells and debris, if required by the downstream assay.
- Storage: Store all aliquots at -80°C immediately after processing to preserve analyte integrity until batch analysis.
- Analysis: Thaw samples on ice and analyze using a multiplex bead-based immunoassay or ELISA. Correlate biomarker levels with potential normalization factors (e.g., creatinine, total urine volume).
Visual Workflow:
Protocol: Evaluating Temperature and Preservative Effects on Urinary Proteins
This protocol is based on a study that systematically tested storage parameters for a multiplex protein assay [83].
Objective: To determine the optimal storage conditions (temperature, time, preservatives) for a specific panel of urinary protein biomarkers.
Materials:
- Fresh, pooled urine from healthy donors.
- Sterile conical tubes.
- Commercial urine preservatives (e.g., Protease Inhibitor Cocktail, Norgen Biotek Urine Preservation Tubes).
- Antibiotics (e.g., Trimethoprim).
- Refrigerated centrifuge.
- Freezers (-20°C, -80°C).
Method:
- Urine Pooling: Collect urine from multiple healthy donors, centrifuge at 1000 × g for 5-10 minutes to remove sediment, and pool to minimize individual variability.
- Preservative Addition: Aliquot the pooled urine into several tubes:
- Control: No additive.
- Preservative A: e.g., cOmplete Protease Inhibitor Cocktail.
- Preservative B: e.g., Norgen Biotek Urine Collection and Preservation Tube.
- Antibiotic: e.g., Trimethoprim (20 μL/mL).
- Time-Temperature Incubation: For each group, store aliquots at:
- Room Temperature (e.g., 20°C): for 0.5, 1, 2, 4, 8, and 24 hours.
- Refrigerated (4°C): for 24h, 48h, and 1 week.
- Frozen (-20°C): for 1 week and 1 month.
- Termination: After each time point, transfer the corresponding aliquots to a -80°C freezer to halt all degradation processes until batch analysis.
- Analysis: Thaw all samples simultaneously and analyze using your target protein assay (e.g., the Oncuria multiplex immunoassay or ELISA). Compare analyte concentrations in test conditions to the control sample frozen immediately at -80°C.
Visual Workflow:
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for Urine Stabilization
| Reagent/Material | Function | Application Example | Evidence/Outcome |
|---|---|---|---|
| Streck Urine Preserve | A liquid reagent that stabilizes nucleic acids by inhibiting nucleases and preventing cell lysis. | Stabilization of urinary cell-free DNA (cfDNA) for transport and storage. | Stabilizes cfDNA for up to 7 days at 6-37°C, enabling room-temperature transport [84]. |
| cOmplete Protease Inhibitor Cocktail | A broad-spectrum solution that inhibits a wide range of serine, cysteine, and metalloproteases. | Added to urine samples to prevent proteolytic degradation of protein biomarkers. | Tested in multiplex protein assays; showed variable efficacy in stabilizing a specific 10-plex panel at RT [83]. |
| Norgen Biotek Urine Collection & Preservation Tubes | Commercial tubes containing proprietary preservatives for maintaining the integrity of urine components. | Designed for room-temperature storage of urine for DNA, RNA, and protein analysis. | Evaluation showed it could not fully prevent analyte level alterations for a specific protein panel at RT [83]. |
| Trimethoprim | An antibiotic that suppresses bacterial overgrowth in urine samples. | Used to prevent changes in analyte levels caused by bacterial metabolism. | Added to urine to assess its effect on protein biomarker stability; efficacy was context-dependent [83]. |
| Sterile Urine Collection Containers (Screw-cap) | Provides a clean, leak-proof container for sample collection, minimizing external contamination. | Essential for all urine collection procedures, especially clean-catch and 24-hour protocols. | Fundamental for reducing pre-analytical variability and contamination [86] [82]. |
This technical support center provides troubleshooting guides and FAQs for researchers and scientists working on the stability of inflammatory markers. The content is framed within the broader thesis of optimizing storage conditions to ensure reliable and accurate research outcomes.
Frequently Asked Questions (FAQs)
Q1: Why is validating shipment and storage conditions critical for inflammatory marker research? The concentration of sensitive blood proteins, such as cytokines, is known to vary with storage conditions, even in liquid samples stored at -80°C for extended periods [52]. Validating these conditions through Mean Kinetic Temperature (MKT) and excursion studies ensures that the integrity of your samples is maintained from collection through analysis, preventing analyte degradation that could compromise your data [42].
Q2: What is the key difference between a systematic and an intuitive troubleshooting approach? A systematic approach follows a structured process from problem identification to solution implementation and is best for complex or unfamiliar issues [87]. An intuitive approach relies on the experience and pattern recognition of seasoned troubleshooters for rapid diagnosis [87]. For validating storage conditions, a systematic approach is recommended to ensure all variables are documented and controlled.
Q3: Our cytokine levels from finger-prick blood samples are highly variable. What could be the cause? Research has shown that cytokine concentrations from finger-prick samples are inherently much more variable than those from venous blood draws [52] [42]. This variability is a characteristic of the sample collection method itself. For more consistent results in longitudinal studies, consider using venous blood collection.
Q4: What should we do if our samples experience a temperature excursion during shipment? First, consult your pre-defined crisis management plan [88]. Then, assess the impact by reviewing the data from the temperature logger and comparing the duration and magnitude of the excursion against stability data for your specific analytes. The troubleshooting guide below provides further detailed steps.
Troubleshooting Guide
Use the following table to diagnose and address common problems in stability studies.
| Error / Issue | Potential Cause | Solution |
|---|---|---|
| Significant loss of cytokine analytes | Samples stored at room temperature, which performs poorest for many cytokines [52]. | Store samples at 4°C or colder immediately after collection. For long-term storage, -20°C is optimal for most cytokines [42]. |
| High variability in analyte recovery from VAMS devices | Inefficient recovery during the extraction process for specific analytes [52]. | Optimize and validate the extraction protocol for each specific cytokine of interest before committing to longitudinal study collection [52]. |
| Unexpected supply chain disruption (e.g., shipping delay) | External factors like extreme weather, logistical failures, or customs holds [89]. | Collaborate with suppliers on contingency plans and invest in technology for real-time tracking of shipments [88]. |
| Poor performance from a key supplier | Inadequate due diligence and a lack of regular performance monitoring [88]. | Conduct thorough due diligence before selection and monitor suppliers regularly through audits and performance reviews [88]. |
Experimental Protocol: Validating Cytokine Stability in Dried Blood Samples
The following methodology is adapted from a peer-reviewed study on the stability of inflammation markers in human blood collected using Volumetric Absorptive Microsampling (VAMS) devices [52] [42].
Objective
To determine the stability of up to 31 cytokines when stored on VAMS devices under various laboratory storage temperatures for up to 5 months.
Materials (Research Reagent Solutions)
| Item | Function |
|---|---|
| Volumetric Absorptive Microsampling (VAMS) devices | To collect accurate and precise volumetric (30 µL) samples of whole blood, minimizing hematocrit effects [52]. |
| Luminex assay platform | A multiplex immunoassay technology used for the simultaneous quantification of multiple cytokines in the sample extracts [52]. |
| Recombinant cytokines | Used to "spike" blood samples from healthy participants to ensure a measurable and known baseline of analytes [52]. |
Step-by-Step Methodology
- Sample Collection: Collect venous blood from participants (e.g., 4 healthy donors). Spike the blood with a cocktail of recombinant cytokines.
- Sample Preparation: Use the VAMS devices to absorb 30 µL of the spiked blood according to the manufacturer's instructions.
- Storage: Store the prepared VAMS devices at different temperatures (Room Temperature, 4°C, and -20°C). Simultaneously, prepare matching VAMS liquid extracts and store them at -80°C to serve as a baseline control.
- Longitudinal Testing: At predetermined timepoints (e.g., 1, 3, and 5 months), extract the cytokines from the VAMS devices.
- Analysis: Quantify the cytokine concentrations in all extracts using the Luminex assay.
- Data Analysis: Compare the cytokine levels from the different storage temperatures against the -80°C control at each timepoint to determine stability and significant losses.
The table below summarizes key findings from the stability study, illustrating the number of stable cytokines over time under different storage conditions [42].
| Storage Temperature | 3-Month Stability (out of 31 analytes) | 5-Month Stability (out of 21 analytes) |
|---|---|---|
| -20°C | 25 stable | Data not specified in source |
| 4°C | Data not specified in source | 17 stable |
| Room Temperature | Data not specified in source | Significant losses in 13 |
Experimental Workflow and Decision Pathways
Cytokine Stability Study Workflow
Temperature Excursion Response
Implementing FEFO and Advanced Inventory Control for Sample Management
Troubleshooting Guides
Issue 1: Inaccurate Expiry Tracking Leading to Sample Degradation
Problem: Samples are being compromised because the system fails to correctly identify and prioritize items with the earliest expiration dates.
Solution:
- Implement Automated Capture: Use barcode scanning or RFID at receiving to record expiration dates and lot numbers, eliminating manual typing errors [90].
- Standardize Date Formats: Adopt a single, unambiguous date format (YYYY-MM-DD) across all labels and system records to prevent misreads [90].
- Configure System Alerts: Utilize your Warehouse Management System (WMS) to generate automated alerts for samples approaching their expiration date, allowing for proactive measures like prioritized use or discounts [91] [90].
Issue 2: Inconsistent Sample Integrity During Storage
Problem: Variable storage conditions are causing unpredictable degradation of inflammatory markers, compromising research data.
Solution:
- Validate Storage Temperatures: Establish and monitor specific storage temperatures based on analyte stability profiles. Research indicates that for many cytokines, storage at 4°C or colder is significantly more effective than room temperature [42].
- Define Sample Lifecycle States: Implement a sample management system with clear lifecycle states (e.g., "Registered," "Tested," "Archived") to ensure consistent handling and tracking from collection to disposal [92].
Issue 3: System Suggests Blocked or Invalid Samples
Problem: The FEFO logic in your inventory system incorrectly suggests samples from blocked lots or storage locations for use.
Solution:
- Verify System Configuration: Ensure that bins and lots flagged as "blocked" are properly excluded from available inventory calculations. This may require a software update or configuration change to enforce movement restrictions [93].
- Establish a Quarantine Area: Create a clearly marked physical area and corresponding system status for damaged, recalled, or questionable samples to prevent their accidental use [90].
Frequently Asked Questions (FAQs)
What is the fundamental difference between FEFO and FIFO?
FEFO (First Expired, First Out) prioritizes items with the earliest expiration date, which is critical for perishable goods or samples with limited stability [91] [94]. FIFO (First In, First Out) moves the oldest stock first, regardless of its expiration date, and is better suited for non-perishable goods [91].
Why is FEFO particularly important in pharmaceutical and biomedical research?
FEFO helps ensure regulatory compliance (e.g., EU GDP Guidelines), reduces financial losses from wasted samples, and, most importantly, guarantees that products or samples reaching end-users have sufficient quality and remaining shelf life, which is paramount for research integrity and patient safety [94].
How does sample storage temperature impact the stability of inflammatory markers?
Stability varies significantly by analyte and temperature. The table below summarizes key experimental findings on the stability of specific biomarkers, illustrating the need for validated storage conditions.
Table: Stability of Biomarkers Under Different Storage Conditions
| Biomarker | Storage Temperature | Storage Duration | Result | Citation |
|---|---|---|---|---|
| Cytokines (31 analytes) | Room Temperature | 5 months | Significant losses in 13 out of 21 analyzable cytokines [42]. | |
| Cytokines (31 analytes) | 4°C | 5 months | 17 out of 21 analyzable cytokines remained stable [42]. | |
| Cytokines (31 analytes) | -20°C | 3 months | 25 out of 31 cytokines were quantifiably stable [42]. | |
| TRAIL | -80°C | 5 years | Levels decreased by approximately 30% [9]. | |
| IP-10 | -80°C | 5 years | Levels decreased by 17% [9]. | |
| CRP | -80°C | 5 years | No significant decrease [9]. |
What are the key steps to implementing a FEFO system in a research lab?
- Reliable Data Capture: Mandate the recording of expiration dates and lot numbers for all new samples [90].
- Standardized Labeling: Use clear, consistent labels with a standardized date format on all containers [90].
- Storage Design: Organize storage units so that samples with the nearest expiration dates are the most accessible [91] [90].
- Staff Training: Train personnel on FEFO procedures and the importance of sample stability for research outcomes [91] [90].
- Regular Audits: Perform periodic cycle counts to verify expiration dates and system accuracy [90].
Experimental Protocols for Stability Validation
Protocol: Evaluating Long-Term Stability of Serum Biomarkers at -80°C
Methodology:
- Sample Collection: Collect venous blood from participants following IRB-approved protocols and obtain written consent [9].
- Sample Processing: Separate serum from blood cells. Aliquot serum into suitable cryovials.
- Storage: Store aliquots at -80°C for the duration of the study (e.g., up to 5 years).
- Analysis: At predetermined time points, thaw samples and analyze biomarker concentrations (e.g., TRAIL, IP-10, CRP) using a validated immunoassay platform like Luminex [9].
- Data Comparison: Compare concentrations at each time point to baseline measurements (time zero) to determine degradation rates.
Protocol: Comparing Analyte Stability Across Storage Temperatures
Methodology:
- Sample Preparation: Collect blood and spike with recombinant analytes of interest (e.g., cytokines). Use devices like volumetric absorptive microsampling (VAMS) to ensure consistent sample volumes [42].
- Storage Conditions: Divide each sample and store replicates at different temperatures: Room Temperature, 4°C, and -20°C [42].
- Time-Course Analysis: Extract and analyze samples at multiple time points (e.g., 1, 3, 5 months) for analyte quantification [42].
- Statistical Comparison: Perform statistical analysis to identify significant losses in analyte concentration under each condition compared to baseline or optimal storage.
Workflow and System Diagrams
Sample Management FEFO Workflow
Sample Stability Validation Protocol
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Materials for Sample Inventory Management and Stability Research
| Item / Solution | Function / Application |
|---|---|
| Volumetric Absorptive Microsampling (VAMS) Devices | Ensures accurate and consistent blood sample volumes for reliable stability comparisons across different storage conditions [42]. |
| Cryogenic Vials & Labels | For long-term storage of serum and other biological samples at ultra-low temperatures (-80°C). Barcode-compatible labels are essential for tracking [9]. |
| Barcode/RFID Scanner | Enables accurate, non-manual capture of sample IDs, lot numbers, and expiration dates, forming the foundation of a reliable FEFO system [95] [90]. |
| Warehouse Management System (WMS) | A software platform that automates expiration tracking, generates picking lists based on FEFO, and sends alerts for short-dated samples [91] [90]. |
| Multiplex Immunoassay Platform (e.g., Luminex) | Allows simultaneous quantification of multiple inflammatory markers (e.g., cytokines, TRAIL, IP-10) from a single sample aliquot, crucial for stability studies [42] [9]. |
| Temperature-Monitored Storage | Freezers (-20°C, -80°C) and refrigerators (4°C) with continuous data logging to ensure and document compliance with validated storage conditions [42] [9]. |
| Standardized Labeling System | Printer and labels (e.g., ZPL format) to create consistent, machine-readable sample labels containing ID, type, lot, and expiry information [92]. |
Validating Storage Efficacy and Comparing Marker Performance Across Conditions
A Stability Validation Master Plan (VMP) is a strategic, high-level document that outlines the comprehensive framework for all validation activities your facility must undertake to demonstrate that storage conditions and processes consistently maintain product stability and quality [96]. In the context of research on inflammatory markers (e.g., CRP, TNF-α, IL-6, IL-1β), a well-designed VMP provides the documented evidence that your storage equipment and monitoring processes are fit for their intended use, ensuring the integrity of your sensitive biological samples over time [97] [98].
The plan specifies which elements require validation, details the schedules and standards to be applied, and assigns responsibilities [96]. For a stability study program, this typically involves qualifying stability chambers and freezers, validating the storage conditions, and establishing reliable testing intervals [98]. Regulatory authorities closely examine the VMP as it demonstrates a systematic, risk-based approach to guaranteeing data reliability and product safety [96].
The Qualification Lifecycle: From Design to Performance
The qualification process for equipment and systems is a structured, multi-stage lifecycle. It ensures that every aspect, from initial selection to ongoing performance, is controlled and documented.
Stage 1: Design Qualification (DQ)
Design Qualification (DQ) is the foundational stage where you define and document the specific user requirements that your stability storage equipment must meet to support your research [99].
- Purpose: To ensure the proposed design of the equipment or facility is suitable for its intended use before it is procured or built.
- Key Activities: Assessing capabilities against research needs, such as temperature range, uniformity, size, capacity, and power requirements. It also involves evaluating construction materials to ensure they present no hazard to the biological samples (e.g., preventing leaching of substances from plastic liners) and verifying manufacturer quality and support [99].
- Output: A formal document justifying the equipment selection based on its ability to meet all defined user requirements for inflammatory marker stability research.
Stage 2: Installation Qualification (IQ)
Installation Qualification (IQ) verifies that the equipment has been delivered, installed, and configured correctly according to the manufacturer's specifications and your design requirements [100] [101] [99].
- Purpose: To provide documented evidence that the installation is correct and complete.
- Key Activities [101] [99]:
- Cross-checking received equipment and parts against purchase orders and packing lists.
- Checking for any transport damage.
- Verifying proper installation in the correct location and environment.
- Ensuring connections to utilities (power, data) and other systems are correct.
- Recording initial calibration data and validation dates for any critical instruments.
- Organizing and archiving all supplied manuals, certificates, and documentation.
- Output: An IQ report confirming successful installation.
Stage 3: Operational Qualification (OQ)
Operational Qualification (OQ) follows a successful IQ and involves testing the equipment to ensure it operates consistently within established tolerances and predefined operational limits [100] [99].
- Purpose: To verify that the installed equipment functions according to its specifications across its intended operating ranges.
- Key Activities [101] [99]:
- Testing all operational functions, displays, and signals.
- Verifying the equipment's ability to maintain the specified temperature (and humidity, if applicable) uniformly throughout the chamber.
- Challenging the system under "worst-case" conditions, such as testing recovery after door openings or power interruptions.
- Verifying that alarm systems function correctly when operational limits are breached.
- Output: An OQ report documenting that the equipment operates as required under all expected conditions.
Stage 4: Performance Qualification (PQ)
Performance Qualification (PQ) is the final stage, demonstrating that the equipment and process can perform consistently and reproducibly under normal operating conditions to produce the desired result [100] [101] [99].
- Purpose: To document evidence that the system (e.g., a stability chamber) consistently maintains the required environment for preserving sample integrity over time.
- Key Activities: PQ is conducted under real-world conditions using the actual storage protocols, trained personnel, and monitoring procedures [101]. For a stability chamber, this involves:
- Loading the chamber with a representative load (e.g., simulated samples).
- Running the chamber for an extended period under normal storage conditions (e.g., 5°C ±3°C, 25°C ±2°C/60%RH ±5%RH) as defined in your stability protocol [98].
- Continuously monitoring and documenting conditions to prove consistent control and uniformity.
- Output: A PQ report that proves the process is stable, reliable, and capable of consistently meeting the specified acceptance criteria for long-term storage.
The logical relationship and workflow of these four stages are outlined in the diagram below.
The Scientist's Toolkit: Essential Research Reagent Solutions
When conducting stability studies for inflammatory markers, specific reagents and materials are critical. The following table details key solutions and their functions.
Table 1: Key Research Reagents for Inflammatory Marker Stability Studies
| Research Reagent / Material | Function in Stability Studies |
|---|---|
| Critical Inflammatory Markers (e.g., CRP, IL-6, TNF-α, IL-1β) [97] | The primary analytes whose stability is under investigation. Serves as the direct measure of storage condition efficacy. |
| Appropriate Biological Matrices (e.g., Blood Serum/Plasma) [97] | The medium in which the inflammatory markers are suspended. Matrix interactions can significantly impact analyte stability. |
| Stability-Indicating Assays (e.g., ELISA, CLIA) [98] | Validated analytical methods capable of detecting and quantifying changes in the quality attributes of the inflammatory markers over time. |
| Forced Degradation Materials (e.g., buffers for extreme pH, oxidants) [98] | Used in stress testing to deliberately degrade samples and validate that the analytical method can detect changes (i.e., is "stability-indicating"). |
| Calibrators and Controls | Essential for ensuring the accuracy and precision of the analytical methods used throughout the long-term stability study. |
Troubleshooting Common Stability Study Issues
FAQ: How to Respond to a Stability Chamber Alarm?
Q: What immediate actions should a researcher take upon a stability chamber alarm indicating a temperature excursion?
A:
- Document the Event: Immediately record the date, time, alarm type, and current chamber display readings.
- Assess the Samples: Determine if the samples being stored are critical (e.g., for an ongoing PPQ study) and assess their tolerance to the excursion.
- Check Chamber: Visibly inspect the chamber door to ensure it is closed and check for any obvious malfunctions.
- Follow SOP: Adhere to your site's specific Standard Operating Procedure for equipment alarm response and escalation, which should include notifying responsible personnel (e.g., Quality Assurance, Stability Manager) [98].
- Investigate Root Cause: Initiate a formal investigation to determine the cause, which could range from a power outage to equipment failure [98].
FAQ: How to Handle a Stability Failure?
Q: During a scheduled stability timepoint testing, a sample fails to meet its predefined quality attributes (e.g., significant change in cytokine concentration). What is the process for investigation?
A:
- Classify the Failure: Determine if it is an OOS (Out-of-Specification) result, where a single result falls outside acceptance criteria, or an OOT (Out-of-Trend) result, where a result is within specification but shows an unexpected shift from the established stability profile [98].
- Initiate a Laboratory Investigation: Before blaming the product or process, conduct a thorough investigation of the analytical process to rule out laboratory error. This includes checking instrument calibration, sample handling, and analyst technique.
- Expand the Investigation: If no lab error is found, the investigation widens. A key strategy is to systematically examine potential root causes [102]:
- Raw Materials: Were there any changes or inconsistencies in the materials used to prepare the samples? This is a common culprit, as even minor changes in a supplier's process (e.g., mining location for a base material) can introduce impurities or deficiencies that impact stability [102].
- Facility & Equipment: Have there been any unqualified changes to the storage facility or equipment?
- Process: Was the sample preparation process followed exactly?
- Implement Corrective Actions: Based on the root cause, implement fixes. This could involve changing a supplier, adding a control step (e.g., supplementing a identified deficiency [102]), or revising procedures.
- Document Everything: The entire investigation, conclusions, and corrective actions must be thoroughly documented.
Case Study: Troubleshooting a Failed Process Performance Qualification (PPQ)
A biopharmaceutical company experienced a failed PPQ campaign for a biological product, where cell health and quality attributes deteriorated unexpectedly during runs [102]. The troubleshooting process provides a valuable model for stability study issues.
The Investigation [102]: The team systematically ruled out potential causes:
- Cell Bank: Quickly ruled out through lab-scale tests.
- Facility/Equipment: Changes from stainless steel to single-use equipment were reviewed but showed no obvious link to the failure.
- Raw Materials: Identified as the most likely source. The team conducted extensive testing of raw material lots and worked with vendors to discover that a supplier had changed the physical mining location for a base material (a carbonate). This change altered the impurity profile, leading to a critical manganese deficiency that impacted the cell culture process [102].
The Solution: The team developed a control strategy to add a manganese supplement to the process, which was validated through lab, pilot, and manufacturing-scale runs before successfully repeating the PPQ [102].
Experimental Protocols for Key Stability Activities
Protocol for Stability Chamber Performance Qualification (PQ)
Objective: To demonstrate that the stability chamber consistently maintains the specified temperature (and humidity, if applicable) throughout its entire volume under normal loaded conditions over a defined period.
Materials:
- Qualified stability chamber
- Multiple calibrated and traceable temperature sensors (e.g., thermocouples, data loggers). The number should be sufficient to map the entire storage volume.
- A representative load (e.g., containers of water or placebo solution to simulate product mass).
Methodology:
- Sensor Placement: Place temperature sensors at predefined locations within the chamber, including corners, center, and near the air inlet and outlet to cover potential cold/warm spots.
- Chamber Loading: Place the representative load inside the chamber, ensuring it does not obstruct airflow but simulates the maximum expected storage density.
- Study Execution: Set the chamber to the desired storage condition (e.g., 5°C ±3°C). Start data logging and run the study for a minimum of 24 hours, though longer periods (e.g., 7-30 days) are common to capture performance over time.
- Data Collection: Continuously record the temperature from all sensors at frequent intervals (e.g., every 5-10 minutes).
Evaluation:
- Compile all data and compare against acceptance criteria.
- Acceptance Criteria Example:
- All sensor readings must remain within the specified range (e.g., 2°C to 8°C for a 5°C chamber).
- The temperature uniformity (difference between highest and lowest reading) should be within a specified limit (e.g., ±2°C).
- No individual sensor may show a persistent drift or excursion beyond limits.
Protocol for Stability Study Sampling and Testing Intervals
Objective: To establish a schedule for withdrawing samples from stability storage and testing them to build a stability profile for an inflammatory marker.
Materials:
- Samples placed in the qualified stability chamber.
- Validated, stability-indicating analytical methods (e.g., ELISA for cytokine quantification).
- Necessary reagents and lab equipment for testing.
Methodology [98]:
- Initial Time Point (T=0): Test samples immediately after preparation and before storage to establish the baseline quality attributes.
- Defined Intervals: Withdraw samples from stability storage at predefined time points and test them. The ICH guidelines provide a standard framework for intervals:
- Long-term Testing: Typically at 0, 3, 6, 9, 12, 18, and 24 months during the first year, and annually thereafter [98].
- Accelerated Testing: At 0, 1, 2, 3, and 6 months.
- Testing Parameters: For inflammatory markers, this typically includes:
- Potency/Concentration: Using a validated bioassay or immunoassay.
- Purity/Impurities: Assessing degradation products or aggregation.
- Physical Properties: Such as color, clarity, and pH of the solution.
Evaluation:
- Plot the quantitative data (e.g., concentration, purity) against time.
- Perform statistical analysis (e.g., regression analysis, confidence limits) to determine the rate of degradation and establish a preliminary shelf-life or re-test period.
Troubleshooting Guides
Guide: Addressing Degraded Analyte Signals
Problem: Unexpectedly low measurements for IL-6 or CRP in samples stored long-term at -80°C.
Investigation & Solution:
- Step 1: Review Pre-Freeze Handling: Verify records of the time between sample collection, processing, and freezing. For serum intended for cytokine analysis, a maximum storage of 3 days at 4°C before freezing is recommended to maintain the stability of most analytes [103].
- Step 2: Check Freeze-Thaw History: Audit the sample's freeze-thaw cycle log. Repeated freeze-thaw cycles can degrade cytokines. For long-term studies, align single-use aliquots during initial processing [104].
- Step 3: Validate with Controls: If possible, compare results with freshly collected and processed samples from a similar donor cohort to distinguish between true biological variation and storage-related degradation.
Guide: Managing Biofluid Samples for EV Research
Problem: Inconsistent results when analyzing extracellular vesicles (EVs) isolated from archived biofluids for inflammatory research.
Investigation & Solution:
- Step 1: Assess Biofluid Storage: Note that biofluids like plasma stored before EV isolation can affect the yield, content, and function of EVs [105].
- Step 2: Optimize EV Storage: Isolated EVs resuspended in PBS are unstable at 4°C. For long-term storage, maintain isolated EVs at -80°C or lower to preserve their number, surface markers, and size characteristics [105].
- Step 3: Minimize Handling: Avoid repeated freeze-thaw cycles of both the original biofluid and the isolated EV samples, as this is known to cause EV degradation [105].
Frequently Asked Questions (FAQs)
Q1: What is the documented stability of IL-6 in serum/plasma stored at -80°C? The thermal stability of IL-6 is reasonably good. Current evidence indicates that IL-6 is stable for at least 30 days when serum is stored at 4°C prior to freezing [103]. While a definitive maximum storage duration at -80°C is not explicitly established for periods over 4 years, one study successfully measured IL-6 in serum that had been collected and stored at -80°C, demonstrating its functional stability for research purposes over at least the study's timeframe [106]. The source of the cytokine (endogenous vs. recombinant) also affects measured stability, with endogenous cytokines generally being more stable [104].
Q2: Is the multimeric structure of CRP stable in long-term archived samples? Evidence suggests that the multimeric structure of human CRP is very stable. One study found no difference in the multimeric structures (pentameric, monomeric, etc.) of human CRP between samples stored at -80°C for twenty-four hours and those stored for three months [107]. This indicates that archived samples stored at -80°C in large longitudinal studies are suitable for investigating CRP multimeric forms, although studies specifically confirming stability beyond 4 years are not available [107].
Q3: Does the type of blood collection tube (serum vs. plasma) affect the long-term stability of these biomarkers? Yes, the sample matrix can influence stability. For cytokine analysis, protein levels have been found to be generally more stable in unseparated serum compared to plasma for most analytes [103]. Furthermore, blood collection tubes with additives (e.g., EDTA, heparin) can yield different cytokine levels compared to serum tubes without additives, partly due to processes like immunothrombosis [104].
Q4: What are the critical steps in the sample processing protocol to ensure biomarker stability for long-term research? The pre-analytical phase is critical. Key steps include:
- Rapid Processing: Minimize the time between blood draw and serum separation.
- Short-Term Storage: If immediate freezing is not possible, store unseparated serum at 4°C for a maximum of 3 days before freezing [103].
- Aliquoting: Aliquot samples to avoid repeated freeze-thaw cycles.
- Stable Freezing: Use a -80°C freezer for long-term storage and ensure it is monitored with continuous temperature logging.
Table 1: Documented Stability of CRP and IL-6 under Various Storage Conditions
| Analyte | Sample Type | Storage Condition | Documented Stable Duration | Key Findings | Source |
|---|---|---|---|---|---|
| IL-6 | Human Serum | 4°C prior to freezing | Up to 30 days | No significant signal degradation for most of 12 analyzed proteins, including IL-6. | [103] |
| IL-6 | Human Serum | -80°C (long-term) | Not explicitly stated for >4y | Successfully measured in samples stored at -80°C, confirming stability for research purposes. | [106] |
| CRP (Multimeric Structure) | Transgenic Rat Serum/Plasma | -80°C | 3 months (tested) | No difference in multimeric structures between 24-hour and 3-month storage. | [107] |
| General Cytokines | Human Serum | 4°C prior to freezing | Recommended max 3 days | To ensure stability for biobanked samples intended for cytokine analysis. | [103] |
Table 2: Comparative Stability of Other Relevant Biomarkers
| Analyte / Biological | Sample Type | Storage Condition | Stability Observation | Source |
|---|---|---|---|---|
| CCL19 | Human Serum/Plasma | 4°C prior to freezing | Significant signal degradation after 4 days. | [103] |
| Human Primary Cells (Fibroblasts) | Cells in Cryomedium | Liquid Nitrogen Vapor Phase | Optimal cell attachment after 0-6 months storage; viability above 80% at 3 months. | [108] |
| Extracellular Vesicles (EVs) | Isolated EVs in PBS | 4°C | Unstable; decrease in number and surface marker expression. | [105] |
| Extracellular Vesicles (EVs) | Isolated EVs in PBS | -80°C or lower | Recommended for long-term storage to ensure stability. | [105] |
Detailed Experimental Protocols
Protocol: Assessing CRP Multimeric Stability in Archived Samples
This protocol is adapted from a study investigating the stability of human CRP multimeric forms [107].
1. Sample Collection and Storage:
- Collect serum or plasma samples. Heparin plasma can be used.
- Split samples into multiple aliquots to avoid repeated freeze-thaw cycles.
- Store aliquots at various temperatures (e.g., 4°C, -20°C, -80°C) for different durations.
2. Protein Extraction and Quantification (for tissue samples):
- Homogenize frozen tissues in a protein extraction reagent with a protease inhibitor cocktail.
- Centrifuge the homogenate and collect the supernatant.
- Determine protein concentration using a standard assay like the BCA assay.
3. Non-Denaturing Western Blot Analysis:
- Gel Electrophoresis: Load 20 µg of total protein onto a 4-12% non-denaturing polyacrylamide gel. Heating samples is not recommended as it can disrupt multimeric structures.
- Transfer: Transfer proteins from the gel to a PVDF membrane.
- Blocking and Incubation: Block the membrane with 5% milk. Incubate with a primary anti-human CRP antibody overnight.
- Detection: Incubate with an HRP-conjugated secondary antibody. Develop the signal using a chemiluminescent substrate and expose to X-ray film.
- Analysis: Compare the banding patterns (representing pentamers, trimers, monomers, etc.) between samples stored under different conditions.
Protocol: Measuring IL-6 in Long-Term Stored Serum
This protocol summarizes the methodology used in a study of community-acquired pneumonia patients where IL-6 was measured in stored samples [106].
1. Sample Acquisition and Ethical Considerations:
- Obtain samples under a study protocol approved by an ethics committee (e.g., in accordance with the Declaration of Helsinki).
- Collect and process blood samples, then store the resulting serum at -80°C until analysis.
2. IL-6 Measurement by Electrochemiluminescence Immunoassay:
- Use a validated commercial immunoassay (e.g., Elecsys IL-6 test on a Cobas 8000 e602 analyzer).
- Follow manufacturer instructions. Briefly, the assay uses a biotinylated monoclonal IL-6-specific antibody and a monoclonal IL-6-specific antibody labeled with a ruthenium complex.
- The reaction mixture is incubated, and streptavidin-coated microparticles are added. The complex is measured via electrochemiluminescence.
- For values below the detection limit, assign a value at the lower limit of quantification (e.g., 1.5 pg/mL) for statistical purposes.
3. Data Analysis:
- Perform statistical analysis to correlate IL-6 levels with clinical outcomes, adjusting for covariates like age and sex to validate the biological relevance of the measurements from stored samples [106].
Signaling Pathways and Experimental Workflows
Experimental Workflow for Biomarker Stability Studies
Research Reagent Solutions
Table 3: Essential Materials for Stability Experiments
| Item | Function / Application | Example / Note |
|---|---|---|
| Cryogenic Vials | Long-term storage of serum, plasma, and cell samples at -80°C. | Ensure they are leak-proof and certified for low-temperature use. |
| Elecsys IL-6 Immunoassay | Quantitative measurement of IL-6 in serum samples. | Used on Cobas 8000 e602 analyzer [106]. |
| Anti-human CRP Antibody | Detection of CRP and its multimeric forms in Western Blot. | Critical for identifying different structural isoforms [107]. |
| Non-denaturing Polyacrylamide Gel (4-12%) | Separation of native CRP multimers without disrupting structure. | Key for assessing multimeric stability [107]. |
| Protease Inhibitor Cocktail | Prevents protein degradation in samples during processing and storage. | Added to tissue protein extraction reagents [107]. |
| CoolCell or Mr. Frosty | Provides a controlled freezing rate of ~-1°C/minute for cells. | Optimizes cell viability during cryopreservation [108]. |
| Cryoprotectant (DMSO) | Membrane-permeating agent that protects cells from freezing damage. | Commonly used at 10% concentration in cryomedium [108]. |
FAQs: Addressing Common Stability and Pre-Analytical Challenges
Q1: What are the most critical pre-analytical factors affecting cytokine stability in serum and plasma? Cytokine stability is highly dependent on sample handling immediately after collection. For serum, use a red-top separator tube (SST) and allow the sample to clot for 30 minutes at room temperature before centrifugation. Centrifuge at 1000g for 15 minutes, after which the serum should be aliquoted and immediately stored at -80°C [109]. For plasma, collect blood using EDTA, heparin, or citrate as an anticoagulant. It is critical to centrifuge the tube within 30 minutes of collection at 1000g for 15 minutes. The harvested plasma must then be aliquoted and stored at -80°C [109]. Delays in processing or multiple freeze-thaw cycles can significantly degrade cytokine integrity.
Q2: How stable are complete blood count (CBC)-derived inflammatory ratios, and what are the key considerations for their analysis? CBC-derived ratios, such as the Neutrophil-to-Lymphocyte Ratio (NLR) and Systemic Inflammation Response Index (SIRI), are derived from cellular counts and are generally stable when analyzed from fresh blood samples [110]. The key to their reliability is the consistency of the analytical method. All CBC measurements used to calculate these ratios should be performed on a single, standardized hematology analyzer to prevent inter-instrument variability from affecting the results. For example, the foundational study on type 2 diabetes patients used a Sysmex XN-9000 analyzer for all measurements [110]. While the cellular components are more stable than many soluble proteins, prolonged storage of whole blood before analysis can lead to cell lysis or activation, altering the counts.
Q3: For multi-marker studies, what is the recommended approach to sample collection when measuring both proteins and cellular components? For studies integrating multiple analyte types, a multi-tube collection strategy is essential. To profile both cytokines and CBC-derived ratios, collect:
- One tube with anticoagulant (e.g., EDTA) for plasma and CBC analysis: Process this tube within 30 minutes for plasma isolation and run the CBC analysis from a fresh aliquot [109].
- One serum separator tube (SST) for serum-based protein biomarkers: Process according to the standard serum protocol [109]. This approach ensures that the stability requirements for each type of biomarker are met without compromise.
Q4: What are the best practices for long-term storage of samples intended for novel biomarker research? The universal standard for long-term storage of all sample types—including serum, plasma, cell culture supernatants, urine, and cerebrospinal fluid (CSF)—is -80°C [109]. To preserve stability and prevent freeze-thaw degradation, aliquoting is mandatory. Samples should be portioned into single-use volumes to avoid repeated freezing and thawing of the same stock. All sample tubes must be clearly labeled, and storage should be organized in a dedicated, monitored -80°C freezer to maintain sample integrity over many years [109].
Q5: How can study design minimize confounding factors in inflammatory marker research? To identify disease-specific immune signatures, it is crucial to exclude participants with conditions that cause systemic inflammation. Core study cohorts should exclude individuals with [111]:
- Primary inflammatory or autoimmune disorders.
- Active cancer or a history of hematological malignancy.
- Acute infection (CRP >10 mg/L can be a useful screening cutoff) or chronic infection (e.g., HIV, hepatitis).
- Recent major surgery or trauma (within 6 weeks).
- Use of immunosuppressant or anti-inflammatory medications (other than low-dose aspirin).
Experimental Protocols for Stability and Profiling Research
Protocol for Serum and Plasma Processing from Whole Blood
This protocol is fundamental for ensuring the stability of cytokines and other soluble markers [109].
- Materials: Red-top serum separator tubes (SSTs), EDTA/heparin plasma tubes, sterile pipettes, cryovials, centrifuge, -80°C freezer.
- Procedure:
- Collection: Draw venous blood into the appropriate vacutainer tubes.
- Clotting (Serum only): For SSTs, leave the tube at room temperature for 30 minutes to allow a complete clot to form.
- Centrifugation: Centrifuge both serum and plasma tubes at 1000g for 15 minutes at room temperature.
- Aliquoting: Carefully remove the supernatant (serum or plasma) without disturbing the buffy coat or pellet. Transfer into pre-labeled cryovials.
- Storage: Immediately place the aliquots in a -80°C freezer. Record the storage location.
Protocol for Luminex Multiplex Assay for Protein Biomarkers
This method allows for the simultaneous quantification of multiple cytokines or novel protein markers from a single sample, maximizing data yield from precious biobanked samples [112].
- Materials: Luminex 200 system or comparable analyzer, bead-based multiplex immunoassay kits, pre-wet buffer, wash buffer, biotinylated detection antibodies, streptavidin-phycoerythrin, sheath fluid, 96-well filter plates.
- Procedure:
- Prewetting: Add 100 µL of wash buffer to each well of a filter plate and incubate for 10 minutes.
- Reagent Loading: Remove wash buffer. Add 25 µL of standard, control, or sample to designated wells, followed by 25 µL of assay buffer.
- Bead Incubation: Add 25 µL of antibody-conjugated beads to each well. Seal the plate and incubate overnight at 4°C on a plate shaker.
- Wash and Detection: Wash wells twice. Add 25 µL of biotinylated detection antibody and incubate for 1 hour. Wash, then add 25 µL of streptavidin-phycoerythrin and incubate for 30 minutes.
- Signal Reading: Wash twice, add 100 µL of sheath fluid to resuspend beads, and read the plate on the Luminex analyzer.
- Analysis: Use software (e.g., SoftMax Pro) with a five-parameter logistic regression curve to calculate biomarker concentrations [112].
Data Presentation: Stability and Performance of Different Marker Classes
Table 1: Stability and Pre-Analytical Considerations for Multi-Marker Panels
| Marker Class | Specific Examples | Key Stability Considerations | Optimal Sample Type | Relative Cost & Accessibility |
|---|---|---|---|---|
| Cytokines | IL-6, GDF-15, suPAR [112] | Highly sensitive to freeze-thaw; requires rapid processing and strict -80°C storage [109]. | Plasma (EDTA) or Serum [109] | High (requires specialized immunoassays) [112] |
| CBC-Derived Ratios | NLR, SIRI, SII, nMLR [110] [113] | Stable from fresh whole blood; sensitive to delays in CBC analysis causing cell degradation. | Whole Blood (EDTA) [110] | Very Low (uses routine lab data) [110] [113] |
| Novel Protein Markers | CLEC3B, AOC3, SEPP1 [114] | Stability profile often unknown; should be treated like cytokines (aliquot, store at -80°C) until validated. | Plasma or Serum [114] | Variable (often high for discovery) |
| Traditional Tumor Markers | CA19-9, CEA, CA-125 [115] [116] | Generally stable with standard serum processing protocols. | Serum [115] | Moderate |
Table 2: Diagnostic Performance of Multi-Marker Panels vs. Single Markers
| Panel Description | Clinical Context | Performance (AUC) | Key Insight |
|---|---|---|---|
| Machine Learning Panel (CA19-9, GDF-15, suPAR) [112] | Pancreatic Ductal Adenocarcinoma Diagnosis | AUC 0.992 (All stages) AUC 0.976 (Early stage) [112] | Significantly outperforms CA19-9 alone (AUC 0.952 all stages, 0.868 early stage) [112]. |
| CBC-Derived Ratios (NLR, SIRI) [110] | Predicting All-Cause Mortality in Type 2 Diabetes | Hazard Ratio (HR) up to 2.49 for highest vs. lowest quartile [110] | Provides independent prognostic value and superior risk stratification over traditional factors [110]. |
| Novel Protein Panel (AOC3, CAT, CLEC3B, etc.) [114] | Early-Stage Lung Cancer Screening | Decision Tree Model: AUC 0.868 [114] | Combining novel and traditional markers (CEA, CYFRA21-1) improves screening accuracy [114]. |
| Multi-Biomarker Panel (SCC-Ag, CA125, IL-6, CRP, NLR) [116] | Predicting CRT Response in Cervical Cancer | Correlated with poorer response and survival [116] | A multi-parameter panel captures more biological complexity than any single marker [116]. |
Signaling Pathways and Experimental Workflows
Diagram 1: Inflammatory Signaling in Disease Pathogenesis
Diagram 2: Multi-Marker Discovery & Validation Workflow
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Reagents and Materials for Multi-Marker Studies
| Reagent / Material | Function / Application | Example Use Case |
|---|---|---|
| EDTA / Heparin Blood Collection Tubes | Anticoagulant for plasma and CBC analysis; preserves cell morphology [109]. | Baseline blood collection for CBC-derived ratio calculation (NLR, PLR) [110] [116]. |
| Serum Separator Tubes (SSTs) | Promotes clot formation and provides a barrier for clean serum separation [109]. | Collection of serum for cytokine, CRP, and traditional tumor marker analysis (e.g., CA19-9, CA-125) [112] [116]. |
| Luminex Bead-Based Multiplex Kits | Enables simultaneous quantification of dozens of analytes (e.g., cytokines, novel proteins) from a single small-volume sample [112]. | Profiling a 47-protein panel for pancreatic cancer biomarker discovery [112]. |
| Protease Inhibitor Cocktails | Added to homogenization buffers to prevent protein degradation during tissue or cell extraction [109]. | Preparation of tissue lysates for Western blot or mass spectrometry analysis of novel protein markers [114]. |
| Recombinant Proteins & Antibodies | Serve as standards for assay calibration and as capture/detection reagents in immunoassays like ELISA [114]. | Validating the expression of candidate markers (e.g., CLEC3B, AOC3) in human plasma via ELISA [114]. |
Troubleshooting Guide: Frequently Asked Questions
FAQ 1: How does long-term storage at -80°C affect the stability of key protein biomarkers used in cardiovascular risk prediction?
Several protein biomarkers crucial for cardiovascular risk assessment show significant degradation over time, even when stored at -80°C. The stability profile varies significantly by analyte.
- Evidence: A 2025 study investigating serum sample stability found that after five years of storage at -80°C, TRAIL levels decreased by approximately 30%, and IP-10 levels decreased by 17%. In contrast, CRP levels did not show a significant decrease under the same conditions [9].
- Recommendation: For research employing biobanks with long-term storage, it is critical to account for the differential stability of each biomarker in your panel. The age of samples and their storage history should be considered as potential confounding variables in longitudinal analyses.
FAQ 2: What is the optimal short-term storage temperature for inflammatory markers in blood collected via volumetric absorptive microsampling (VAMS)?
For VAMS devices, refrigeration or freezing is vastly superior to room temperature storage for preserving cytokine integrity.
- Evidence: Research from 2023 tested the stability of up to 31 cytokines in VAMS devices. Storage at room temperature performed the poorest, with significant losses observed in 13 out of 21 analytes over five months. In contrast, storage at 4°C or -20°C was beneficial for the majority of analytes. Specifically, 17 out of 21 cytokines remained quantifiably stable after 5 months at 4°C, and 25 out of 31 were stable at -20°C for 3 months [52].
- Recommendation: Avoid standard room temperature storage for VAMS if your analytes of interest include cytokines. For short-term studies (up to 5 months), refrigeration at 4°C is effective. For longer-term stability, store at -20°C.
FAQ 3: How do storage conditions impact common biochemical serum analytes, and what are the clinical implications for risk prediction models?
Pre-analytical storage conditions critically influence the measured values of standard biochemical analytes, which can directly affect the accuracy of clinical risk scores.
- Evidence: A 2025 comparative analysis demonstrated that storage temperature and duration significantly affect common serum analytes. Enzymatic markers like AST and ALT are particularly sensitive, showing a 40% decrease in activity after 72 hours at 25°C. Even metabolites like urea and creatinine showed declines at room temperature, while electrolytes were affected by factors like evaporation [4].
- Recommendation: To ensure the integrity of data used in risk prediction models like the American Heart Association's Life's Essential 8 score [117], strict standardization of pre-analytical protocols is essential. Freezing is best for long-term preservation, while refrigeration is suitable for short-term storage.
FAQ 4: Can improving biomarker stability and incorporating novel markers directly impact clinical cardiovascular outcomes?
Yes. Enhancing the accuracy of risk prediction through stable biomarker measurement and the inclusion of novel markers like epigenetic scores and polygenic risk scores can significantly improve patient identification and management, thereby preventing adverse clinical outcomes.
- Evidence:
- Epigenetic Biomarkers: A recent study discovered over 100 novel epigenetic biomarkers related to cardiovascular health. Individuals with favorable methylation profiles had up to a 32% lower risk of incident CVD, 40% lower cardiovascular mortality, and 45% lower all-cause mortality [117].
- Polygenic Risk Scores (PRS): Research presented at AHA 2025 showed that adding PRS to the PREVENT risk calculator improved risk detection. For individuals near the statin treatment threshold, those with a high PRS were almost twice as likely to develop atherosclerotic cardiovascular disease. Widespread use could identify over 3 million additional high-risk individuals in the U.S. and prevent an estimated 100,000 cardiovascular events over a decade [118].
Table 1: Long-Term Stability of Protein Biomarkers at -80°C
| Biomarker | 5-Year Storage at -80°C | Notes |
|---|---|---|
| TRAIL | ~30% decrease | High sensitivity to long-term storage [9] |
| IP-10 | ~17% decrease | Moderate sensitivity to long-term storage [9] |
| CRP | No significant decrease | High stability over time [9] |
Table 2: Stability of Serum Analytes Across Different Storage Temperatures (72 Hours)
| Analyte | 72 Hours at 4°C | 72 Hours at -20°C | 72 Hours at 25°C |
|---|---|---|---|
| Urea | Stable (0% change) | Stable (0% change) | -6.7% change [4] |
| Creatinine | Stable (0% change) | Stable (0% change) | -16.7% change [4] |
| AST | -4% change | -1.6% change | -40% change [4] |
| ALT | -3.3% change | -1.7% change | -40% change [4] |
| Total Protein | -1.4% change | Stable (0% change) | -7.1% change [4] |
| Sodium | Stable (0% change) | Stable (0% change) | -3.6% change [4] |
Table 3: Cytokine Stability in VAMS Devices After 5 Months
| Storage Temperature | Performance | Stable Analytes |
|---|---|---|
| Room Temperature | Poorest performance | 8/21 analytes stable |
| 4°C (Refrigeration) | Good performance | 17/21 analytes stable |
| -20°C (Frozen) | Good performance | Data supports stability [52] |
Experimental Protocols
Objective: To determine the stability of cytokines for up to 5 months when stored on volumetric absorptive microsampling (VAMS) devices under typical laboratory storage temperatures.
Materials:
- Blood Source: Venous blood collected from participants.
- Sample Collection: Volumetric Absorptive Microsampling (VAMS) devices (30 µL volume).
- Key Reagents: Recombinant cytokines for spiking experiments.
- Analytical Instrument: Luminex platform for multiplex cytokine quantification (up to 31 analytes).
Workflow:
- Sample Preparation: Blood collected from healthy participants was spiked with recombinant cytokines.
- Loading: The spiked blood was collected into 30 µL VAMS devices.
- Storage: The prepared VAMS devices were stored under three different conditions: Room Temperature, 4°C, and -20°C. Matching liquid extracts from VAMS were stored at -80°C as a reference.
- Longitudinal Testing: Samples were analyzed at multiple timepoints over a period of up to 5 months (8 months for a remote clinical study).
- Analysis: At each timepoint, samples were extracted from the VAMS devices and analyzed via Luminex to quantify cytokine concentrations.
Objective: To evaluate the effect of different storage temperatures and durations on the stability of selected biochemical serum analytes.
Materials:
- Sample Collection: Serum samples from 100 healthy adults, collected in plain vacutainers.
- Analytes Measured: Urea, Creatinine, AST, ALT, Total Protein, Albumin, Sodium, Potassium.
- Analytical Instrument: Random Access Chemistry Analyzer.
- Key Methods:
- Urea: Urease GLDH method
- Creatinine: Enzymatic method
- AST/ALT: IFCC method (without PLP)
- Total Protein: Biuret method
- Albumin: Bromocresol green dye binding method
- Sodium/Potassium: Ion-selective electrodes
Workflow:
- Baseline Measurement: All analyte values were established immediately after collection and serum separation.
- Storage Conditions: Aliquots of each sample were stored at -20°C, 4°C, and 25°C.
- Time-Point Analysis: Stored samples were re-assessed at 24 hours, 48 hours, 72 hours, and 1 week.
- Statistical Analysis: Stability was determined using paired t-tests and ANOVA to compare values against baseline across the different storage conditions.
Workflow Diagrams
Biomarker Stability Assessment
Stability Impact on Clinical Utility
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials for Biomarker Stability Research
| Item | Function/Benefit |
|---|---|
| Volumetric Absorptive Microsampling (VAMS) Devices | Enables standardized, low-volume (e.g., 30 µL) blood collection from participants. Minimizes pre-analytical variation and is suitable for remote collection studies [52]. |
| Luminex Multiplex Assay Panels | Allows for high-throughput, simultaneous quantification of multiple cytokines or proteins (e.g., 31-plex) from a single sample extract, conserving precious sample material [52]. |
| Stable Isotope-Labeled Internal Standards | Used in mass spectrometry-based workflows to correct for losses during sample preparation and analysis, improving quantification accuracy despite storage-related degradation. |
| Controlled Temperature Storage Systems | Reliable -80°C, -20°C, and 4°C environments are non-negotiable for conducting rigorous stability studies and for the long-term preservation of valuable biobank samples [52] [4] [9]. |
| Tris-Based Buffer Systems | Superior to PBS for stabilizing mRNA in lipid nanoparticles (LNPs); thought to capture degradation impurities. Evidence suggests similar benefits may extend to protein stability in liquid formulations [119]. |
Platform Selection Guide & Quantitative Performance Comparison
FAQ: What are the key performance differences between ELISA, Multiplex, and Immunonephelometry platforms for inflammatory marker analysis?
The choice of immunoassay platform significantly impacts data quality, efficiency, and applicability for inflammatory marker stability research. The table below summarizes the core technical characteristics of each platform.
Table 1: Technical Performance Comparison of Major Immunoassay Platforms
| Feature | Traditional ELISA | Multiplex Immunoassays | Immunonephelometry |
|---|---|---|---|
| Detection Capacity | Single analyte per assay [120] [121] | Multiple analytes simultaneously (up to 80+ in a single well) [122] [123] | Single analyte per run, high-throughput capable |
| Sample Volume Required | Higher volume for multiple analytes (separate assay per analyte) [121] | Low volume (e.g., 1–50 µL per panel) [120] [122] [123] | Typically requires moderate sample volume |
| Sensitivity | High sensitivity for individual analytes [121] | Variable; can be very high (e.g., fg/mL for Simoa), but may be lower for some low-abundance analytes in standard multiplex [124] [121] [123] | Generally high for abundant serum proteins |
| Dynamic Range | Narrow relative to other technologies [120] | Broad dynamic range (up to nearly 5 orders of magnitude) [120] [124] [122] | Good for quantifying proteins within a specific concentration range |
| Multiplexing Capability | Not available | High (Bead-based: up to 80 proteins; Planar: up to 10+; PEA: 5,000+) [125] [122] [123] | Not available |
| Throughput | Moderate | High throughput, especially for multi-analyte profiles [122] | Very high for single-analyte testing |
| Cost-Effectiveness | Cost-effective for 1-2 analytes [121] | Cost-effective for multi-analyte studies [120] [122] | Cost-effective for high-volume single-analyte testing |
| Primary Best Use Case | Focused, precise quantification of a single or few analytes [121] | Comprehensive biomarker profiling, limited sample volume, pathway analysis [120] [122] | Rapid quantification of specific, abundant serum proteins (e.g., CRP, immunoglobulins) |
Detailed Methodologies & Experimental Protocols
FAQ: Can you provide a generalized protocol for a multiplex bead-based immunoassay?
The following protocol is adapted for analyzing inflammatory markers in serum or plasma samples using a bead-based platform like Luminex xMAP technology [120] [122] [126].
Protocol: Multiplex Bead-Based Immunoassay for Inflammatory Cytokines
Principle: Color-coded magnetic beads, each coated with a capture antibody for a specific cytokine, are mixed with the sample. After a series of washes, a biotinylated detection antibody is added, followed by a streptavidin-phycoerythrin reporter. A flow-based analyzer identifies the bead (and thus the analyte) and quantifies the signal [122].
Key Research Reagent Solutions:
- Bead Set: Magnetic beads spectrally coded and pre-coated with analyte-specific capture antibodies (e.g., ProcartaPlex panels) [122].
- Assay Buffer: To dilute samples and standards and to block non-specific binding.
- Analyte Standards: A serial dilution of known analyte concentrations for generating a standard curve.
- Detection Antibodies: A cocktail of biotinylated, analyte-specific detection antibodies.
- Streptavidin-Reporter: Streptavidin conjugated to R-Phycoerythrin (SAPE) or a similar fluorophore [122] [126].
- Wash Buffer: To remove unbound proteins between steps.
Step-by-Step Workflow:
- Bead Preparation: Resuspend the bead mix by vortexing and sonicating. Add the required number of beads to each well of a 96-well microtiter plate [122].
- Wash: Wash the beads twice using a magnetic plate washer or a hand-held magnet.
- Standard & Sample Addition: Add the standard curve points, quality controls, and diluted test samples to the appropriate wells. Seal the plate and incubate with shaking for the recommended time (e.g., 2 hours).
- Wash: Wash the plate 2 times to remove unbound protein.
- Detection Antibody Incubation: Add the biotinylated detection antibody cocktail to each well. Seal the plate and incubate with shaking (e.g., 1 hour).
- Wash: Wash the plate 2 times.
- Reporter Incubation: Add Streptavidin-PE to each well. Seal the plate and incubate with shaking (e.g., 30 minutes).
- Wash: Perform a final wash step.
- Resuspension & Reading: Resuspend the beads in reading buffer and analyze on the appropriate analyzer (e.g., Luminex FLEXMAP 3D or MAGPIX). The instrument identifies each bead by its color code and quantifies the PE fluorescence associated with it [122].
- Data Analysis: Use software to generate a 5-parameter logistic (5-PL) standard curve and interpolate sample concentrations.
Diagram 1: Multiplex Bead-Based Assay Workflow
Troubleshooting Common Experimental Issues
FAQ: Our multiplex data shows poor concordance with previous ELISA results. What could be the cause?
This is a common challenge. The discrepancies can arise from several factors inherent to the technologies [127].
- Matrix Effects & Assay Format: Multiplex assays are more sensitive to the complex mix of proteins and potential inhibitors in serum or plasma than ELISA. In ELISA, the capture antibody and complexes are immobilized to the plate well, whereas in bead-based multiplex, all reactions occur in a solution phase with freely mobile components, making them more vulnerable to interference from other serum components [120].
- Cross-Reactivity: In a multiplex format, there is a higher potential for non-specific interactions or cross-reactivity between the multiple different antibodies and antigens present in the same reaction solution [120] [125].
- Proportional Bias: Studies have shown that multiplex assays can produce results that are proportionally biased (consistently higher or lower) compared to singleplex ELISAs, even when comparing kits from the same manufacturer. Merging such data can bias epidemiologic associations [127].
- Antibody Pair Differences: Even when measuring the same analyte, different platforms use different antibody clones that may recognize different epitopes. A protein's conformation when bound to a plate (ELISA) versus a bead (multiplex) can also affect antibody binding and the final measurement [123].
Troubleshooting Guide:
- Action: Do not directly merge data from different platforms. Always validate the new multiplex assay against your existing ELISA for a subset of samples to understand the correlation and any systematic bias [127].
- Action: Ensure you are using the same sample type (e.g., serum vs. plasma) across comparisons, as results can differ significantly between them [120].
- Action: Check the manufacturer's data for known cross-reactivities within the multiplex panel. If a specific analyte is problematic, consider confirming its levels with a validated singleplex ELISA [121].
FAQ: We are getting high background signals in our multiplex assay. How can we reduce this?
High background can obscure true signals and reduce assay sensitivity.
- Cause: Inadequate washing, leading to residual unbound detection antibody or reporter.
- Cause: Non-specific binding of antibodies or sample proteins to the beads or plate.
- Cause: Degraded or old reagents.
Troubleshooting Guide:
- Action: Optimize the washing procedure. Ensure the wash buffer is fresh and the correct pH. If using a manual magnet, ensure complete bead capture and careful aspiration. Increase the number of washes if necessary.
- Action: Include a protein-based blocking agent in the assay buffer (e.g., BSA, commercial immunoassay blockers) to minimize non-specific binding.
- Action: Titrate the detection antibody and reporter concentrations. Using excessively high concentrations can saturate the system and increase background.
- Action: Check reagent expiration dates and avoid repeated freeze-thaw cycles for antibodies and samples.
Platform-Specific Advantages and Limitations
FAQ: Despite its age, why is ELISA still considered a gold standard in many applications?
ELISA remains the first choice for many applications due to its proven track record, simplicity, and reliability [121].
- High Sensitivity and Specificity: The use of highly selective antibodies for a single analyte ensures accurate results with minimal cross-reactivity [121].
- Simplicity and Accessibility: Protocols are straightforward and easy to standardize. The required equipment (microplate readers) is standard in most laboratories, and data analysis is generally simple [121].
- Well-Established and Reproducible: Decades of use have resulted in a vast body of literature and thoroughly validated protocols. ELISA is trusted for its high reproducibility and accuracy in both research and clinical settings [121].
- Cost-Effectiveness: For projects requiring the measurement of only one or a few analytes, ELISA is far more economical than multiplex assays in terms of reagent and equipment costs [120] [121].
FAQ: What are the key technological variations within multiplex immunoassays?
"Multiplex" encompasses several distinct technologies, each with unique strengths. The choice depends on the project's needs for plex level, sensitivity, and sample volume.
Table 2: Comparison of Multiplex Immunoassay Technologies
| Technology | Principle | Example Platforms | Key Advantages | Typical Plex Level |
|---|---|---|---|---|
| Bead-Based (Suspension) | Fluorescently-coded beads analyzed by flow cytometry [120] [122] | Luminex xMAP, ProcartaPlex [122] | Flexible plex, high throughput, good dynamic range [122] | Medium-High (up to 80) [122] |
| Planar Electrochemiluminescence | Capture antibodies spotted on electrode surface; detection via electrochemiluminescence [120] | Mesoscale Discovery (MSD) [125] [127] | Very high sensitivity, wide dynamic range, low background [120] [123] | Low-Medium (up to ~10) [120] |
| Proximity Extension Assay (PEA) | Uses antibody pairs with DNA tags; quantification via qPCR/NGS [123] | Olink [123] | High specificity, very low sample volume, high plex [123] | Very High (up to 5000+) [123] |
Diagram 2: Immunoassay Platform Selection Guide
Conclusion
Optimizing storage conditions for inflammatory markers is not merely a technical detail but a fundamental requirement for generating reliable, reproducible data in both research and clinical diagnostics. The evidence clearly demonstrates that a one-size-fits-all approach is insufficient; instead, marker-specific, validated protocols are essential. Success hinges on integrating foundational knowledge of biomarker stability with rigorous methodological application, proactive troubleshooting, and comprehensive validation. Future directions must focus on standardizing pre-analytical protocols across laboratories, developing novel stabilization technologies for point-of-care applications, and establishing universal stability criteria for emerging biomarkers. By adopting these evidence-based practices, researchers and drug development professionals can significantly enhance data quality, strengthen clinical correlations, and accelerate the translation of inflammatory biomarkers into meaningful diagnostic and therapeutic applications.
References
- 1. Long-term storage stability of plasma TNF-α and IL-6 ... [https://www.sciencedirect.com/science/article/pii/S1043466625001802]
- 2. Methodological Considerations in Saliva‐Based Biomarker ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12560811/]
- 3. Impact of Storage Conditions on the Stability of Urinary ... [https://pubmed.ncbi.nlm.nih.gov/40387750/]
- 4. Effect of Storage Temperature (-20°C, 4°C, 25°C) and ... [https://healthcare-bulletin.co.uk/article/effect-of-storage-temperature-20-c-4-c-25-c-and-duration-24h-1week-on-biochemical-serum-analyte-stability-in-healthy-adult-samples-a-comparative-analysis-4086/]
- 5. Temporal change in inflammatory biomarkers and risk of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8497383/]
- 6. Biomarkers in Clinical Practice: Challenges & Opportunities [https://esmed.org/biomarkers-in-clinical-practice-challenges-opportunities/]
- 7. “Recommendations for clinical study protocols for immune ... [https://www.nature.com/articles/s41531-025-01146-1]
- 8. The Relationship Between Systemic Inflammatory Index ... [https://www.mdpi.com/2227-9059/13/8/2029]
- 9. Impact of Serum Sample Storage on the Stability of TRAIL, ... [https://www.medrxiv.org/content/10.1101/2025.01.22.25320787v1]
- 10. Storage conditions affect the composition of the lyophilized ... [https://www.nature.com/articles/s41598-024-60787-z]
- 11. Optimal conditions for sampling of blood cytokine tests ... [https://pubmed.ncbi.nlm.nih.gov/39931752/]
- 12. Multimodal Noninvasive Assessment of C-Reactive Protein ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12379750/]
- 13. Effect of storage temperatures on the stability of cytokines ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1945112/]
- 14. Analysis of C-reactive protein from finger stick dried blood ... [https://www.nature.com/articles/s41598-023-27522-6]
- 15. EFFECTS OF TRANSPORT TEMPERATURE ON THE STABILITY OF INFLAMMATORY, HEMOSTASIS, ENDOTHELIAL FUNCTION, AND OXIDATIVE STRESS PLASMA BIOMARKER CONCENTRATIONS - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5432385/]
- 16. Evaluation of metabolite stability in dried blood spot stored ... [https://www.nature.com/articles/s41598-024-82041-2]
- 17. Effects of Storage Temperature and Time on Metabolite ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10842436/]
- 18. Effect of serum sample storage temperature on ... [https://www.nature.com/articles/s41598-022-08429-0]
- 19. Identification of inflammatory markers suitable for non-invasive, repeated measurement studies in biobehavioral research: A feasibility study | PLOS One [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0221993]
- 20. Time- and Temperature-Dependent Pentraxin 3 Stability in ... [https://pubmed.ncbi.nlm.nih.gov/40576635/]
- 21. Preanalytical Errors in Clinical Laboratory Testing at a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10981510/]
- 22. Pre-Analytical Variation | myadlm.org [https://myadlm.org/cln/articles/2016/july/preanalytical-variation-the-leading-cause-of-error-in-laboratory-medicine]
- 23. Preanalytical Variables and Their Influence on the Quality ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6238383/]
- 24. Pre-Analytical Variables [https://www.practical-haemostasis.com/Quality%20Assurance/pre_analytical_variables.html]
- 25. Optimization of bile preparation for liquid biopsy in ... [https://www.nature.com/articles/s41598-025-96170-9]
- 26. Reducing Pre- and Post-Analytical Errors - Versiti Clinical Trials [https://versiticlinicaltrials.org/resources/insights/reducing-pre-and-post-analytical-errors]
- 27. Five common pre-analytical variables - Streck [https://www.streck.com/blog/five-common-pre-analytical-variables/]
- 28. Why Pre-Analytical Variables Can Make or Break Your Assay [https://mtgroupbio.com/the-hidden-challenge-in-assay-development-why-pre-analytical-variables-can-make-or-break-your-assay/]
- 29. Development, Optimization, and Stability Study of a ... [https://www.mdpi.com/2310-2861/11/1/64]
- 30. Western Blot: The Complete Guide [https://www.antibodies.com/applications/western-blotting]
- 31. Stability of Direct Oral Anticoagulants Concentrations in Blood ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10384965/]
- 32. ELISA vs Western Blot: When to Use Each Immunoassay ... [https://www.thermofisher.com/blog/life-in-the-lab/western-blot-or-elisa/]
- 33. Reveal, Don't Conceal: Transforming Data Visualization to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8947810/]
- 34. Development and optimization of a novel nanocarrier ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12321823/]
- 35. ELISA Sample Preparation & Collection Guide [https://www.rndsystems.com/resources/protocols/elisa-sample-preparation-collection-guide]
- 36. Effects of storage time and temperature on highly ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7921292/]
- 37. The Complete Guide to the Temperature of Morgue Coolers [https://mymortuarycooler.com/blogs/news/the-complete-guide-to-the-temperature-of-morgue-coolers?srsltid=AfmBOooWLQ26AU8-fFUfyJ0yJtHUQ9V4mxQtSlqw4Kn0UmPNMcRbaeFr]
- 38. ELISA Troubleshooting Guide | Thermo Fisher Scientific - ID [https://www.thermofisher.com/id/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/overview-elisa/elisa-troubleshooting-guide.html]
- 39. Staining Cell Surface Targets for Flow Cytometry [https://www.thermofisher.com/us/en/home/references/protocols/cell-and-tissue-analysis/protocols/staining-cell-surface-targets-flow-cytometry.html]
- 40. An Overview of Pre-Analytical Factors Impacting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11433674/]
- 41. Common Laboratory Problems and Solutions That Drive ... [https://blog.creliohealth.com/common-laboratory-problems-and-solutions-that-drive-efficiency/]
- 42. Stability of inflammation markers in human blood collected ... [https://www.sciencedirect.com/science/article/pii/S1043466623002338]
- 43. The Impact of Storage Condition and Duration on Function ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10079553/]
- 44. Preparation for blood tests: what can go wrong before the ... [https://australianprescriber.tg.org.au/articles/preparation-for-blood-tests-what-can-go-wrong-before-the-sample-reaches-the-lab.html]
- 45. Useful tips to avoid preanalytical errors in blood gas testing [https://acutecaretesting.org/en/articles/useful-tips-to-avoid-preanalytical-errors-in-blood-gas-testing-ph-pco2-and-po2]
- 46. Teaching Your Lab Staff to Successfully Troubleshoot [https://www.labmanager.com/teaching-your-lab-staff-to-successfully-troubleshoot-32784]
- 47. Pre-analytical sample handling standardization for reliable ... [https://www.sciencedirect.com/science/article/pii/S2667145X23000093]
- 48. Volumetric Absorptive Microsampling in Therapeutic Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9821248/]
- 49. Tutorial: Volumetric absorptive microsampling (VAMS) [https://www.sciencedirect.com/science/article/abs/pii/S0003267018310626]
- 50. Top 5 Microsampling Questions [https://www.neoteryx.com/microsampling-blog/top-5-microsampling-questions]
- 51. Automated Mitra with VAMS Technology - ILT [https://www.iltusa.com/automated-mitra-with-vams-technology/]
- 52. Stability of inflammation markers in human blood collected ... [https://pubmed.ncbi.nlm.nih.gov/37690424/]
- 53. Dried Spot Paradigm: Problems and Prospects in Proteomics [https://pmc.ncbi.nlm.nih.gov/articles/PMC12027537/]
- 54. Volumetric absorptive microsampling: Current advances ... [https://www.sciencedirect.com/science/article/abs/pii/S0731708517311615]
- 55. Optimization, validation and initial clinical implications of a ... [https://www.nature.com/articles/s41598-022-09633-8]
- 56. Volumetric Absorptive Microsampling in Toxicology [https://www.mdpi.com/2305-6304/13/1/25]
- 57. Good Distribution Practice (GDP) | Requirements and ... [https://eupry.com/gdp/]
- 58. A Guide to Good Distribution Practice (GDP) [https://safetyculture.com/topics/good-distribution-practice-gdp]
- 59. Best Practices in Storage and Distribution of Medical ... [https://www.sekologistics.com/en/resource-hub/knowledge-hub/best-practices-in-storage-and-distribution-of-medical-products/]
- 60. How ELNs Help You Comply with the NIH 2025 Data Policy [https://www.lablynx.com/resources/articles/nih-data-compliance-eln/]
- 61. Structure-based knowledge acquisition from electronic lab ... [https://jbiomedsem.biomedcentral.com/articles/10.1186/s13326-021-00257-x]
- 62. Electronic Laboratory Notebooks (ELNs) Guidelines [https://ari.hms.harvard.edu/electronic-laboratory-notebooks-elns-guidelines]
- 63. Avoiding Common ELN Pitfalls in High-Throughput Labs [https://www.labmanager.com/avoiding-common-eln-pitfalls-in-high-throughput-labs-34161]
- 64. Choosing an Electronic Lab Notebook in 2025 - Blogs [https://www.logilabeln.com/blog/the-eln-selection-process-decoded-choosing-an-electronic-lab-notebook-in-2025/]
- 65. A comprehensive guide to Laboratory Information ... [https://www.scispot.com/blog/a-comprehensive-guide-to-laboratory-information-management-systems-lims]
- 66. Electronic Lab Notebook (ELN) Best Practices For Life ... [https://genemod.net/blog/electronic-lab-notebook-eln-best-practices-for-life-sciences-researchers]
- 67. Ten simple rules for managing laboratory information - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10703290/]
- 68. Navigating ELN Finder: A Comprehensive Guide [https://labhorizons.co.uk/2025/03/navigating-eln-finder-a-comprehensive-guide/]
- 69. A systematic review and meta-analysis of the stability ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9729419/]
- 70. Low recovery factor & Validation Issue [https://nitrosamines.usp.org/t/low-recovery-factor-validation-issue/13549]
- 71. Extraction of VAMS samples for LC-MS/MS analysis [https://bio-protocol.org/exchange/minidetail?id=17953722&type=30]
- 72. Analytical and Clinical Validation of Assays for Volumetric ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10459922/]
- 73. Blood and Plasma Volumetric Absorptive Microsampling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7179185/]
- 74. ELISA Troubleshooting Guide [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/overview-elisa/elisa-troubleshooting-guide.html]
- 75. Exploring technical aspects of biomarker assays - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK513094/]
- 76. Noninvasive, Multimodal Inflammatory Biomarker ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11576606/]
- 77. Biomarker Program FAQs [https://www.ninds.nih.gov/current-research/focus-tools-topics/biomarkers-research/biomarker-program-faqs]
- 78. Intra‐Laboratory and Inter‐Laboratory Variations Analysis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12019688/]
- 79. Analytical Biomarkers for Inflammation Status Monitoring of ... [https://www.mdpi.com/1424-8247/18/8/1213]
- 80. Urine biomarkers can outperform serum ... [https://www.sciencedirect.com/science/article/pii/S2590280623000086]
- 81. Urine stabilization and normalization strategies favor ... [https://www.nature.com/articles/s41598-022-22577-3]
- 82. Urinalysis - StatPearls - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK557685/]
- 83. Effects of Different Voided Urine Sample Storage Time, ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11763964/]
- 84. Improving Urine Nucleic Acid Target Stability | The Scientist [https://www.the-scientist.com/improving-urine-nucleic-acid-target-stability-72702]
- 85. Proper Storage and Handling of Urine Samples in Urgent ... [https://www.needle.tube/product-articles-3/proper-storage-and-handling-of-urine-samples-in-urgent-care-clinics-guidelines-and-best-practices-a-comprehensive-overview-2]
- 86. Identification of inflammatory markers suitable for non- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6759186/]
- 87. How to Create a Troubleshooting Guide for Your Business [https://www.proprofskb.com/blog/troubleshooting-guides/]
- 88. Supply Chain Safety: 5 Critical Strategies [https://veriforce.com/blog/supply-chain-safety-5-critical-strategies]
- 89. The Ultimate Guide to Supply Chain Safety [https://safetyculture.com/topics/supply-chain-management/supply-chain-safety]
- 90. Common FEFO Mistakes and Best Practices [https://racklify.com/encyclopedia/common-fefo-mistakes-and-best-practices/]
- 91. An Ecommerce Guide to First Expired, First Out (FEFO) ... [https://www.shipbob.com/blog/fefo/]
- 92. Enable and configure sample management (preview) [https://learn.microsoft.com/en-us/dynamics365/supply-chain/inventory/quality-sample-management-admin]
- 93. FEFO picking considers item that uses a blocked lot ... [https://support.microsoft.com/en-us/topic/fefo-picking-considers-item-that-uses-a-blocked-lot-number-from-a-blocked-bin-incorrectly-when-you-create-a-warehouse-pick-for-the-item-in-microsoft-dynamics-nav-2009-bf56f5a9-74bc-94a1-b8e9-b1b516d5b2dd]
- 94. FIFO, FEFO, LIFO: What is the meaning? [https://www.gmp-compliance.org/gmp-news/fifo-fefo-lifo-what-is-the-meaning]
- 95. Inventory Control Defined: Best Practices, Systems, & ... [https://www.netsuite.com/portal/resource/articles/inventory-management/what-are-inventory-management-controls.shtml]
- 96. Validation master plan (VMP) – when and how to create one? [https://www.gmpsop.com/validation-master-plan-vmp-when-and-how-to-create/]
- 97. Reliability of blood inflammatory markers at constant real-life ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12517492/]
- 98. Stability Study Program - GMP Validation Master Plan (VMP) [https://www.gmp7.com/stability-study-program-plan-gmp-vmp-validation-master-plan]
- 99. The Four Stages of Equipment Qualification [https://www.patheon.com/us/en/insights-resources/blog/the-four-stages-of-equipment-qualification.html]
- 100. A Basic Guide to IQ, OQ, PQ in FDA-Regulated Industries [https://www.thefdagroup.com/blog/a-basic-guide-to-iq-oq-pq-in-fda-regulated-industries]
- 101. What is IQ, OQ, PQ? [Quick Guide to Process Validation] [https://www.greenlight.guru/blog/iq-oq-pq-process-validation]
- 102. Troubleshooting A Failed Process Performance Qualification [https://www.outsourcedpharma.com/doc/troubleshooting-a-failed-process-performance-qualification-lessons-learned-0001]
- 103. Effect of storage duration on cytokine stability in human ... [https://pubmed.ncbi.nlm.nih.gov/29909979/]
- 104. Review article Thermal stability of cytokines: A review [https://www.sciencedirect.com/science/article/abs/pii/S1043466619302583]
- 105. Impact of Storage Conditions on EV Integrity/Surface ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9146501/]
- 106. Persistent systemic interleukin-6 elevation after community-acquired pneumonia is associated with one-year mortality | Respiratory Research | Full Text [https://respiratory-research.biomedcentral.com/articles/10.1186/s12931-025-03402-7]
- 107. Multimeric Stability of Human C-reactive Protein in Archived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3597618/]
- 108. Optimisation of cryopreservation conditions, including storage ... [https://bmcmolcellbiol.biomedcentral.com/articles/10.1186/s12860-024-00516-6]
- 109. Sample Collection & Storage [https://cytokinelab.umn.edu/sample-collection-storage]
- 110. The Prognostic Value of Complete Blood Count-Derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12535702/]
- 111. “Recommendations for clinical study protocols for immune and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12537938/]
- 112. Development of a serum protein biomarker panel for the ... [https://www.nature.com/articles/s41598-025-19631-1]
- 113. Complete Blood Count-Derived Inflammatory Markers and ... [https://www.mdpi.com/2076-3271/13/4/274]
- 114. Screening and identification of novel protein markers ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1567673/full]
- 115. The Future of Tumor Markers: Advancing Early Malignancy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12294060/]
- 116. Prognostic value and early response stratification of a multi ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12611648/]
- 117. Novel Biomarkers May Help Improve Cardiovascular Disease ... [https://news.feinberg.northwestern.edu/2025/09/10/novel-biomarkers-may-help-improve-cardiovascular-disease-risk-prediction/]
- 118. AHA 2025: New study from Genomics shows polygenic risk ... [https://www.genomics.com/newsroom/aha-2025-new-study-from-genomics-shows-polygenic-risk-scores-improve-the-accuracy-of-cardiovascular-disease-risk-prediction]
- 119. Examining the Impact of Storage Conditions on the Stability ... [https://www.mdpi.com/1999-4923/17/9/1194]
- 120. ELISA AND MULTIPLEX TECHNOLOGIES FOR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2562869/]
- 121. ELISA vs. Multiplex Immunoassays: Why ELISA Remains ... [https://www.cusabio.com/c-21191.html?srsltid=AfmBOop9UN0YQ9FfBG4jfUCMOEgBDeB5EcB7j6ac8dpDpoV400qm80Uv]
- 122. Guide to Multiplex Immunoassays: Multiplex ELISA and More [https://www.thermofisher.com/blog/life-in-the-lab/guide-to-multiplex-immunoassays-multiplex-elisa-and-more/]
- 123. Olink Cytokine Panel vs Other Cytokine Detection Methods [https://olinkpanel.creative-proteomics.com/knowledge/olink-cytokine-panel-vs-other-methods.html]
- 124. Multiplex Assays vs ELISA in Complex Disease States [https://www.quanterix.com/what-you-need-to-know-about-multiplex-assays-vs-elisa-when-assessing-complex-disease-states/]
- 125. ELISA in the multiplex era: Potentials and pitfalls - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6680274/]
- 126. Highly Sensitive and Specific Multiplex Antibody Assays To ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8111153/]
- 127. A multiplex immunoassay gives different results than ... [https://www.sciencedirect.com/science/article/abs/pii/S0009912012001725]