Oxidative Stress Biomarkers in Chronic Disease: A Comparative Guide for Research and Drug Development
This article provides a comprehensive analysis of oxidative stress biomarkers across major chronic diseases, including cardiovascular disease, diabetes, chronic kidney disease, and neurodegenerative disorders.
Oxidative Stress Biomarkers in Chronic Disease: A Comparative Guide for Research and Drug Development
Abstract
This article provides a comprehensive analysis of oxidative stress biomarkers across major chronic diseases, including cardiovascular disease, diabetes, chronic kidney disease, and neurodegenerative disorders. Tailored for researchers and drug development professionals, it explores the pathophysiological roles of these biomarkers, compares their clinical validity and disease-specific expressions, and evaluates advanced methodological approaches for their measurement. The content further addresses key challenges in biomarker validation and interpretation, offering insights into integrated assessment strategies and future directions for leveraging oxidative stress markers in diagnostics, prognostics, and therapeutic development.
Understanding Oxidative Stress: Core Biomarkers and Their Pathophysiological Roles in Chronic Diseases
{Introduction}
Oxidative stress is defined as a physiological state where the production of reactive oxygen species (ROS) overwhelms the body's antioxidant defense capacities [1] [2] [3]. This imbalance leads to oxidative damage of vital cellular structures—lipids, proteins, and DNA—and is a recognized contributor to a wide spectrum of chronic diseases [1] [4] [3]. For researchers and drug development professionals, the accurate assessment of oxidative stress through specific, measurable biomarkers is crucial for understanding disease pathogenesis, monitoring activity, and evaluating novel therapeutic interventions. This guide provides a comparative overview of key oxidative stress markers and the experimental protocols used to measure them in chronic disease research.
{Comparative Biomarker Profiles Across Chronic Diseases}
The following tables summarize the alterations in key oxidative stress biomarkers as observed in recent clinical studies across different pathological conditions. This comparative analysis highlights both common and disease-specific oxidative signatures.
Table 1: Markers of Oxidative Damage and Antioxidant Capacity in Chronic Diseases
| Biomarker | Long COVID [5] | Inflammatory Bowel Disease (IBD) [6] | Hypertension & Diabetes [4] | Medication Overuse Headache (MOH) [7] |
|---|---|---|---|---|
| Lipid Peroxidation (MDA) | - | ↑ in active vs. inactive IBD and HC | ↑ (Predicts endothelial dysfunction) | - |
| DNA Damage (8-OHdG) | - | - | ↑ (Surrogate for diabetic nephropathy) | - |
| Antioxidant Enzymes (SOD, GPx) | - | ↓ in active IBD vs. HC | ↓ (Associated with β-cell failure) | - |
| Total Antioxidant Capacity (BAP/TAC) | BAP ↓ with age/BMI; Inverse correlation with CRP/ferritin | TAC ↓ in active CD vs. inactive CD | - | - |
| Composite Ratios (MHR, NHR, LHR) | - | - | - | ↑ in MOH vs. Healthy Controls |
Table 2: Clinically Accessible Composite Markers of Inflammation and Oxidative Stress These ratios, derived from routine blood tests, serve as proxies for systemic oxidative stress and inflammation [7].
| Marker | Formula | Association with Disease |
|---|---|---|
| Monocyte to HDL Ratio (MHR) | Monocyte count (/µL) / HDL-C (mg/dL) | Independently associated with Medication Overuse Headache (OR = 2.32) [7] |
| Neutrophil to HDL Ratio (NHR) | Neutrophil count (/µL) / HDL-C (mg/dL) | Independently associated with Medication Overuse Headache (OR = 2.09) [7] |
| Lymphocyte to HDL Ratio (LHR) | Lymphocyte count (/µL) / HDL-C (mg/dL) | Independently associated with Medication Overuse Headache (OR = 2.56) [7] |
| Oxidative Stress Index (OSI) | (d-ROMs / BAP) × C | OSI > 1.92 identifies brain fog in Long COVID [5] |
{Experimental Protocols for Key Oxidative Stress Assays}
Standardized methodologies are essential for generating reliable and comparable data on oxidative stress. Below are detailed protocols for several cornerstone techniques in the field.
1. Diacron-Reactive Oxygen Metabolites (d-ROMs) Test
- Principle: This assay measures hydroperoxides (ROOH) in the serum, which react via a Fenton-like reaction to generate radicals that oxidize an alkyl-substituted aromatic amine substrate, producing a pink chromogen [5].
- Detailed Protocol:
- Sample Preparation: Collect venous blood and allow it to clot. Centrifuge at 3000 rpm for 10 minutes to obtain clear serum.
- Reagent Preparation: Reconstitute the provided chromogen substrate (N,N-diethyl-p-phenylenediamine) in the appropriate buffer according to the manufacturer's instructions (Diacron International) [5].
- Reaction: Mix 10 µL of serum sample with 1 mL of the reconstituted reagent in a cuvette.
- Incubation: Incubate the mixture at 37°C for exactly 1 minute.
- Measurement: Measure the absorbance of the solution photometrically at 505 nm using a spectrophotometer (e.g., on an AU480 automated analyzer) [5].
- Calculation: The d-ROMs concentration is directly proportional to the absorbance and is expressed in Carratelli Units (CARR U), where 1 CARR U corresponds to 0.08 mg of Hâ‚‚Oâ‚‚/dL [5].
2. Biological Antioxidant Potential (BAP) Test
- Principle: The BAP test quantifies the collective ability of serum antioxidants to reduce ferric ions (Fe³âº) to ferrous ions (Fe²âº). The ferrous ions then react with a thiocyanate derivative to produce a colored complex, the decolorization of which is inversely proportional to the serum's antioxidant power [5].
- Detailed Protocol:
- Sample Preparation: Use the same serum sample as for the d-ROMs test.
- Reagent Preparation: Prepare a colored solution containing ferric chloride and a thiocyanate derivative.
- Reaction: Add 10 µL of serum to 1 mL of the colored reagent and mix thoroughly.
- Incubation: Incubate at 37°C for 5-10 minutes.
- Measurement: Measure the absorbance at 505 nm. A higher final absorbance indicates a lower reduction of Fe³⺠and thus a lower antioxidant potential.
- Calculation: The BAP value is calculated based on the decrease in absorbance relative to a blank and is expressed in µmol/L [5].
3. Measurement of Lipid Peroxidation via Malondialdehyde (MDA)
- Principle: MDA, a secondary product of lipid peroxidation, reacts with thiobarbituric acid (TBA) to form a pink fluorescent adduct, the Thiobarbituric Acid Reactive Substances (TBARS) [4] [8].
- Detailed Protocol:
- Sample Preparation: Homogenize tissue or dilute plasma/serum in a phosphate-buffered saline (PBS).
- Reaction: Add TBA reagent and acetic acid to the sample in a test tube.
- Heating: Heat the mixture at 95°C for 60 minutes.
- Cooling & Extraction: Cool the tubes on ice and add n-butanol. Vortex and centrifuge to separate the organic (pink) layer.
- Measurement: Measure the fluorescence of the organic layer (Excitation: 515-535 nm, Emission: 553-555 nm) or its absorbance at 532-535 nm.
- Calculation: Quantify MDA concentration using a standard curve prepared from 1,1,3,3-tetramethoxypropane [8].
4. Quantification of DNA Damage via 8-Hydroxy-2'-Deoxyguanosine (8-OHdG)
- Principle: 8-OHdG is a major product of oxidative DNA damage. After DNA extraction and enzymatic hydrolysis, it can be measured with high sensitivity using High-Performance Liquid Chromatography with electrochemical detection (HPLC-ECD) or mass spectrometry (HPLC-MS/MS) [4] [8].
- Detailed Protocol (HPLC-ECD):
- DNA Isolation: Isolate DNA from whole blood or tissue samples using a commercial kit with precautions to avoid artifactual oxidation (e.g., using chelating agents).
- Enzymatic Digestion: Digest the purified DNA (e.g., 50-100 µg) to deoxynucleosides using a mixture of nuclease P1, phosphodiesterase I, and alkaline phosphatase.
- Chromatography: Inject the digest into an HPLC system equipped with a C18 reverse-phase column.
- Detection: Use an electrochemical detector for specific detection of 8-OHdG and a UV detector for simultaneous detection of unmodified deoxyguanosine (dG).
- Calculation: The level of oxidative damage is expressed as the ratio of 8-OHdG per 10ⵠor 10ⶠdG [4] [8].
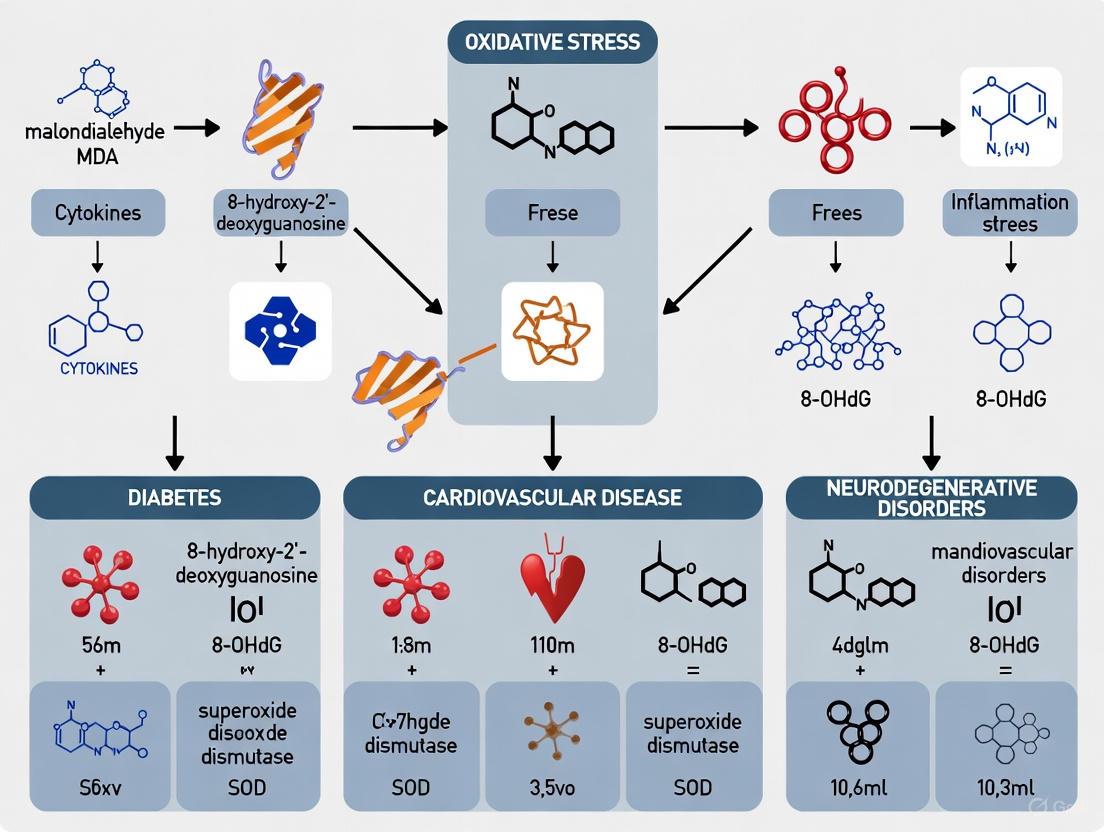
{Visualizing the Oxidative Stress Pathway and Experimental Workflow}
The following diagrams illustrate the core concepts of oxidative stress and a generalized experimental workflow for its assessment.
Diagram 1: The Oxidative Stress Equilibrium. This diagram illustrates the balance between ROS production and antioxidant defenses. An imbalance favoring ROS leads to oxidative stress and cellular damage [1] [2] [3].
Diagram 2: Oxidative Stress Assessment Workflow. A generalized flowchart for evaluating oxidative stress status through multiple complementary assays on biological samples [5] [4] [8].
{The Scientist's Toolkit: Key Research Reagent Solutions}
A successful oxidative stress study relies on specific reagents and tools. The following table details essential items for setting up core experiments.
Table 3: Essential Research Reagents for Oxidative Stress Analysis
| Research Reagent / Kit | Function / Application | Experimental Example |
|---|---|---|
| d-ROMs & BAP Test Kits (Diacron International) | Integrated system for measuring serum hydroperoxide levels (oxidant load) and total antioxidant capacity on automated clinical chemistry analyzers. | Used to establish oxidative stress index (OSI) cut-off values for identifying brain fog in Long COVID patients [5]. |
| Thiobarbituric Acid (TBA) | Key reagent for the TBARS assay; reacts with malondialdehyde (MDA) to form a quantifiable pink chromogen, measuring lipid peroxidation. | Employed in clinical trials to demonstrate that almond supplementation (>60 g/day) significantly reduces plasma MDA levels [9]. |
| 8-OHdG ELISA Kits | Immunoassay-based kits for high-throughput quantification of 8-hydroxy-2'-deoxyguanosine in urine or serum, a marker of oxidative DNA damage. | Used to show that almond consumption significantly reduces urinary 8-OHdG excretion [9]. |
| Superoxide Dismutase (SOD) Activity Assay Kits | Colorimetric or fluorometric kits to measure the activity of SOD, a key enzymatic antioxidant that catalyzes the dismutation of superoxide radical. | Meta-analyses show reduced SOD activity in active inflammatory bowel disease compared to healthy controls [6]. |
| F2-Isoprostane Standards (for GC-MS/LC-MS) | Authentic chemical standards of F2-isoprostanes, gold-standard biomarkers for in vivo lipid peroxidation, used for accurate quantification via mass spectrometry. | Considered a validated biomarker correlating with disease progression in hypertension and diabetes research [4] [8]. |
{Conclusion}
The comparative data and methodologies outlined herein underscore that while oxidative stress is a common thread in chronic diseases, its specific biomarker profile can vary significantly. The choice of biomarkers—from gold-standard specific molecules like F2-isoprostanes to accessible composite ratios like MHR—must be aligned with the research question and clinical context. A multi-parametric approach, integrating measures of oxidant load, antioxidant capacity, and resultant biomolecular damage, provides the most comprehensive assessment. For drug development, these biomarkers offer valuable endpoints for evaluating the efficacy of novel antioxidant or redox-modulating therapies, paving the way for more targeted and effective interventions in conditions driven by oxidative stress.
Oxidative stress, characterized by an imbalance between reactive oxygen species (ROS) and the body's antioxidant defenses, is a common pathophysiological mechanism in numerous chronic diseases [4] [10]. This imbalance leads to molecular damage through oxidation of crucial biomolecules: lipids, proteins, and DNA [11]. The resulting oxidative modifications serve as valuable biomarkers, providing measurable indicators of oxidative stress intensity, cellular damage, and disease progression [10]. These biomarkers have gained significant importance in research and clinical settings for diagnosing disease severity, monitoring progression, and evaluating therapeutic efficacy across diverse conditions including cardiovascular diseases, neurodegenerative disorders, diabetes, and cancer [4] [12] [13]. The reliable detection of these oxidized molecules offers a window into the oxidative microenvironment within tissues and cells, enabling researchers and clinicians to assess the oxidative burden in patients and model systems [14] [11].
This guide provides a comprehensive comparison of the three major biomarker classes—lipid peroxidation products, protein modifications, and DNA oxidation markers—focusing on their mechanisms, measurement methodologies, disease associations, and research applications. We present experimental data and technical protocols to facilitate informed biomarker selection for chronic disease research and drug development.
Lipid Peroxidation Products
Formation Mechanisms and Key Biomarkers
Lipid peroxidation is a chain reaction wherein ROS attack polyunsaturated fatty acids (PUFAs) in cell membranes and lipoproteins [14] [11]. This process proceeds through three distinct mechanisms: free radical-mediated oxidation, free radical-independent non-enzymatic oxidation, and enzymatic oxidation [14]. The primary products of lipid peroxidation are lipid hydroperoxides, which are unstable and undergo further reactions to form a variety of secondary products with diverse biological activities [14].
Key biomarkers include:
- Isoprostanes (IsoPs): Prostaglandin-like compounds formed in situ from arachidonic acid via non-enzymatic, free radical-catalyzed peroxidation. F2-isoprostanes are considered a "gold standard" for assessing oxidative stress in vivo [14] [4]. They are esterified in phospholipids and released into circulation by phospholipases.
- Neuroprostanes (NPs): Similar to IsoPs but derived from docosahexaenoic acid (DHA), which is highly enriched in neuronal membranes. They are particularly relevant for neurodegenerative diseases [14] [12].
- Hydroxyoctadecadienoic acids (HODEs): Oxidation products of linoleic acid, the most abundant PUFA in vivo. The ratio of cis,trans-HODE to trans,trans-HODE can indicate the efficacy of radical-scavenging antioxidants [14].
- Malondialdehyde (MDA): A reactive dialdehyde end-product of lipid peroxidation, commonly measured via the thiobarbituric acid-reactive substances (TBARS) assay [4] [13].
- 4-Hydroxynonenal (4-HNE): A highly reactive aldehyde that forms protein adducts, impacting signal transduction and cell function [12] [11].
- Oxysterols: Cholesterol oxidation products such as 7-ketocholesterol and 7-hydroxycholesterol, formed by enzymatic and non-enzymatic mechanisms [14].
Experimental Detection and Analysis
Accurate measurement of lipid peroxidation biomarkers requires sophisticated analytical techniques due to their low concentrations, instability, and complex isomeric profiles.
Standard Protocols:
- Sample Preparation: Biological samples (plasma, tissues, urine) are typically processed with reduction (e.g., sodium borohydride or triphenylphosphine) to convert hydroperoxides to stable hydroxides, followed by saponification to hydrolyze esterified lipids [14].
- Extraction: Liquid-liquid extraction with organic solvents (e.g., chloroform/methanol) is commonly used to isolate lipids from biological matrices.
- Analysis:
- Gas Chromatography-Mass Spectrometry (GC-MS): Considered the reference method for F2-isoprostanes and HODEs due to high sensitivity and specificity [14] [15].
- Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS): Increasingly used for simultaneous quantification of multiple lipid peroxidation products (e.g., isoprostanoids, HODEs, oxysterols) without derivatization [14] [15].
- Enzyme-Linked Immunosorbent Assay (ELISA): Available for F2-isoprostanes and 4-HNE, offering high-throughput capability though potentially lower specificity than MS methods [14].
Disease Associations and Research Applications
Lipid peroxidation biomarkers show significant elevations across multiple chronic diseases, reflecting their role in pathogenesis.
Table 1: Lipid Peroxidation Biomarkers in Chronic Diseases
| Biomarker | Cardiovascular Diseases | Neurodegenerative Diseases | Diabetes/Metabolic Disorders |
|---|---|---|---|
| F2-IsoPs | Significantly elevated in heart failure (ROM=2.83 vs controls) [13]; Associated with endothelial dysfunction in hypertension [4] | Increased in Alzheimer's disease (AD) plasma and CSF; Correlates with β-amyloid pathology in MCI [12] [15] | Elevated in diabetic patients; Correlates with glycemic control and complications [4] |
| MDA | Elevated in heart failure (ROM=1.87) [13]; Predicts endothelial dysfunction in hypertension [4] | Increased in AD brain and MCI patients [12] | Higher in diabetic patients with complications; Associated with insulin resistance [4] |
| HODEs | Proposed for evaluating antioxidant therapy efficacy in atherosclerosis [14] | Altered profiles in AD and MCI [14] | Used to assess oxidative burden in metabolic syndrome [14] |
| 4-HNE | Protein adducts formed in atherosclerotic plaques; Contributes to endothelial dysfunction [11] [10] | Increased protein adducts in AD brain; Linked to synaptic dysfunction [12] | Adducts formed in pancreatic β-cells under hyperglycemia [4] |
| Oxysterols | Accumulate in atherosclerotic plaques; Promote foam cell formation [14] [10] | Elevated in AD brain; Contribute to neuronal toxicity [14] | Associated with hypercholesterolemia in diabetes [14] |
Protein Oxidation Modifications
Formation Mechanisms and Key Biomarkers
Proteins are major targets for oxidative damage due to their abundance and rapid reaction rates with oxidants [16]. Oxidative protein modifications can occur directly by ROS or indirectly through reaction with lipid peroxidation products (e.g., 4-HNE, acrolein) or carbohydrate derivatives (advanced glycation end products) [12] [16].
Key biomarkers include:
- Protein Carbonyls: Formed by direct oxidation of amino acid side chains (Lys, Arg, Pro, Thr), peptide backbone cleavage, or binding of lipid peroxidation products [12] [16]. They represent a stable, broad marker of protein oxidation.
- 3-Nitrotyrosine (3-NT): Generated by tyrosine nitration mediated by peroxynitrite (ONOOâ»), a reaction product of nitric oxide and superoxide [12] [10]. It indicates nitrosative stress and altered protein signaling.
- Protein-Bound 4-HNE and Acrolein: Michael adducts formed with cysteine, lysine, or histidine residues, leading to protein dysfunction and aggregation [12].
- Advanced Oxidation Protein Products (AOPP): Dityrosine-containing cross-linked protein products formed mainly by myeloperoxidase activity [10].
- Methionine Sulfoxide: Oxidation of methionine residues to methionine sulfoxide, which can be reversed by methionine sulfoxide reductases [16].
Experimental Detection and Analysis
Protein oxidation biomarkers require specific detection methods due to their diverse chemical nature and occurrence in complex biological matrices.
Standard Protocols:
- Protein Carbonyl Detection:
- Derivatization with 2,4-Dinitrophenylhydrazine (DNPH): Sample proteins are reacted with DNPH to form hydrazone products, which can be detected spectrophotometrically (absorbance at 370-375 nm) or immunochemically using anti-DNP antibodies (Western blot or ELISA) [4] [12].
- Redox Proteomics: Protein separation by 2D-gel electrophoresis followed by Western blotting with anti-DNP antibodies or direct detection using LC-MS/MS [12] [16].
- 3-Nitrotyrosine Detection:
- 4-HNE-Adduct Detection:
Disease Associations and Research Applications
Oxidative protein modifications contribute to disease pathogenesis by impairing enzyme function, disrupting cellular signaling, and promoting protein aggregation.
Table 2: Protein Oxidation Biomarkers in Chronic Diseases
| Biomarker | Cardiovascular Diseases | Neurodegenerative Diseases | Diabetes/Metabolic Disorders |
|---|---|---|---|
| Protein Carbonyls | Elevated in atherosclerosis and heart failure; Correlates with disease severity [10] | Significantly increased in AD brain and MCI; Redox proteomics identifies specific oxidized proteins [12] | Higher in diabetic patients; Associated with hyperglycemia and complications [4] |
| 3-Nitrotyrosine | Increased in atherosclerotic plaques; Associated with endothelial dysfunction [10] | Elevated in AD brain; Detected in neurofibrillary tangles and amyloid plaques [12] | Elevated in diabetic vasculature; Contributes to insulin resistance [4] [10] |
| 4-HNE-Adducts | Detected in oxidized LDL and atherosclerotic lesions; Promotes endothelial apoptosis [10] | Increased in AD brain; Modifies key enzymes involved in energy metabolism [12] | Forms adducts in pancreatic islets; Impairs insulin secretion [4] |
| AOPP | Accumulates in plasma of CVD patients; Promotes inflammation [10] | Elevated in AD and Parkinson's disease; Correlates with cognitive decline [12] | Higher in diabetic nephropathy; Serves as renal damage marker [4] |
DNA Oxidation Markers
Formation Mechanisms and Key Biomarkers
Nuclear and mitochondrial DNA are vulnerable to oxidative damage, leading to mutations, impaired transcription, and genomic instability [11]. The hydroxyl radical (HO•) is particularly reactive with DNA, causing various base modifications and strand breaks [13] [11].
Key biomarkers include:
- 8-Hydroxy-2'-Deoxyguanosine (8-OHdG): The most extensively studied DNA oxidation product, formed by HO• attack at the C8 position of deoxyguanosine [4] [13]. It is a predominant form of ROS-induced DNA damage.
- 8-Hydroxyguanosine (8-OHG): The RNA equivalent of 8-OHdG, indicating oxidative damage to RNA [10].
- Purine 5',8-Cyclo-2'-Deoxynucleosides (cPu): Intrastrand cross-linked lesions (cdA and cdG) formed exclusively by HO• attack, repaired only by nucleotide excision repair (NER) [11].
- 8-Oxo-7,8-Dihydro-2'-Deoxyadenosine (8-oxo-dA): An oxidation product of adenine that pairs with cytosine, leading to G→T transversion mutations [11].
- Strand Breaks and Abasic Sites: Result from direct radical attack on the sugar-phosphate backbone or as intermediates of DNA repair [13].
Experimental Detection and Analysis
Accurate measurement of oxidized DNA bases requires sensitive techniques to avoid artifactual oxidation during sample preparation.
Standard Protocols:
- Sample Preparation: DNA extraction using chaotropic methods (e.g., sodium iodide) with antioxidant chelators (e.g., deferoxamine) to prevent spurious oxidation [13].
- Enzymatic Digestion: Isolated DNA is digested to nucleosides using nuclease P1 and alkaline phosphatase for LC-MS analysis.
- Analysis:
- LC-MS/MS: The most specific and reliable method for simultaneous quantification of multiple DNA lesions (8-OHdG, 8-oxo-dA, cPu) without derivatization [4] [11].
- HPLC with Electrochemical Detection (HPLC-ECD): Highly sensitive for 8-OHdG detection, though with lower specificity than MS methods [4].
- Gas Chromatography-MS (GC-MS): Requires derivatization but provides comprehensive profiling of various modified bases [12].
- ELISA: Commercial kits available for 8-OHdG, enabling high-throughput analysis but with potential cross-reactivity issues [4] [13].
- Comet Assay (Single Cell Gel Electrophoresis): Detects overall DNA damage, including strand breaks and alkali-labile sites, at single-cell level [13].
Disease Associations and Research Applications
DNA oxidation biomarkers reflect cumulative oxidative damage to the genome and are associated with disease risk, progression, and aging.
Table 3: DNA Oxidation Biomarkers in Chronic Diseases
| Biomarker | Cardiovascular Diseases | Neurodegenerative Diseases | Diabetes/Metabolic Disorders |
|---|---|---|---|
| 8-OHdG | Significantly elevated in heart failure (ROM=2.24 vs controls) [13]; Associated with atherosclerosis progression [10] | Increased in AD brain, CSF, and plasma; Correlates with cognitive decline [12] | Elevated in diabetic patients; Predictive for nephropathy development [4] |
| 8-OHG | RNA oxidation in vascular cells; Contributes to endothelial dysfunction [10] | Widespread RNA oxidation in AD brain; Impairs protein synthesis [12] | Increased in pancreatic β-cells under hyperglycemia [4] |
| cPu Lesions | Accumulate in atherosclerotic plaques due to inefficient repair [11] | Detected in AD brain; Persistent due to poor repair in neurons [11] | Potential marker for cumulative oxidative damage in diabetes [11] |
| Telomere Attrition | Shorter telomeres in heart failure (ROM=0.66) and atherosclerosis [13] [10] | Associated with accelerated aging in neurodegenerative diseases [10] | Accelerated shortening in diabetes; Links oxidative stress to cellular aging [4] |
Comparative Analysis Across Biomarker Classes
Technical Comparison and Research Considerations
Each biomarker class offers distinct advantages and limitations for research applications, influencing their selection for specific study designs.
Table 4: Technical Comparison of Oxidative Stress Biomarker Classes
| Parameter | Lipid Peroxidation Products | Protein Modifications | DNA Oxidation Markers |
|---|---|---|---|
| Stability | Variable: Some products (MDA) are reactive; Others (IsoPs) are stable [14] | Generally stable: Protein carbonyls and 3-NT are relatively long-lived [16] | Relatively stable with careful sample processing to prevent artifactual oxidation [11] |
| Sensitivity | High for MS-based methods (low nM-pM range) [14] [15] | Moderate to high: Immunoassays less sensitive than MS methods [16] | Very high: MS methods can detect 1-10 lesions/10⸠nucleotides [11] |
| Specificity | Varies: IsoPs specific to free radical damage; HODEs can distinguish oxidation mechanisms [14] | Moderate: Protein carbonyls are general markers; 3-NT more specific to peroxynitrite [12] | High: 8-OHdG specific to oxidative damage; cPu exclusive to HO• attack [11] |
| Sample Types | Plasma, urine, tissues, CSF [14] [15] | Plasma, tissues, cells, CSF [12] [16] | Blood cells, urine, tissues, isolated DNA [13] [11] |
| Key Advantages - Gold standards exist (F2-IsoPs); - Multiple pathways yield diverse markers; - Can assess antioxidant efficacy [14] | - Direct link to functional impairment; - Redox proteomics identifies specific targets; - Stable cumulative markers [12] [16] | - Direct genotoxic damage assessment; - Strong association with mutation risk; - Urinary 8-OHdG non-invasive [13] [11] | |
| Major Challenges - Complex sample preparation; - Artificial oxidation during processing; - Multiple isomers require separation [14] | - Low abundance in circulation; - Requires specific antibodies; - Site-specific analysis technically demanding [16] | - High risk of artifactual oxidation; - Requires rigorous sample handling; - Low abundance necessitates sensitive detection [11] |
Integrated Oxidative Stress Assessment
Combining multiple biomarker classes provides a comprehensive assessment of oxidative stress status in chronic diseases. The simultaneous measurement of lipid, protein, and DNA oxidation products reveals different aspects of oxidative damage dynamics and compensatory mechanisms [10]. For instance, in Alzheimer's disease research, elevated F2-isoprostanes (lipid), protein carbonyls (protein), and 8-OHdG (DNA) in the same patients provide compelling evidence for widespread oxidative damage [12]. Similarly, in heart failure, concurrent increases in MDA, protein carbonyls, and 8-OHdG highlight the multi-faceted nature of oxidative stress in disease progression [13] [10].
Signaling Pathways and Molecular Interactions
Oxidative stress biomarkers are not merely passive indicators of damage but active participants in cellular signaling pathways that influence disease progression.
Oxidative Stress Biomarkers in Signaling Pathways: This diagram illustrates how reactive oxygen species (ROS) generate different classes of oxidative biomarkers, which in turn participate in and amplify cellular stress pathways through complex feedback mechanisms that influence disease progression [10].
The Scientist's Toolkit: Research Reagent Solutions
Successful measurement of oxidative stress biomarkers requires specific reagents and methodologies optimized for each biomarker class.
Table 5: Essential Research Reagents and Methodologies
| Reagent/Methodology | Application | Key Considerations |
|---|---|---|
| Mass Spectrometry Systems (LC-MS/MS, GC-MS) | Gold-standard quantification of IsoPs, HODEs, 8-OHdG, protein carbonyls [14] [11] [15] | High specificity and sensitivity; Requires technical expertise; Enables multiplexing of different biomarkers |
| Anti-DNP Antibodies | Detection of protein carbonyls after DNPH derivatization (ELISA, Western blot) [12] | Broad specificity for carbonylated proteins; Quality varies between vendors; Requires proper controls |
| Anti-3-Nitrotyrosine Antibodies | Specific detection of protein nitration (IHC, Western blot, ELISA) [12] | Specificity confirmation essential; May require epitope retrieval for tissue samples |
| Anti-8-OHdG Antibodies | Immunoassays for DNA oxidation (ELISA, IHC) [13] | Potential cross-reactivity with normal nucleosides; Requires careful DNA isolation |
| DNA Digestion Enzymes (Nuclease P1, Alkaline Phosphatase) | Sample preparation for MS-based DNA oxidation analysis [11] | Enzyme purity critical to prevent artifactual oxidation; Include antioxidant in buffers |
| Reducing Agents (NaBHâ‚„, Triphenylphosphine) | Stabilization of lipid hydroperoxides to alcohols before analysis [14] | Fresh preparation essential; Control reduction efficiency |
| Solid-Phase Extraction Cartridges | Sample clean-up and concentration before analysis [15] | Improve sensitivity and remove interfering compounds; Select appropriate phase chemistry |
| Stable Isotope-Labeled Internal Standards (dâ‚„-8-iso-PGF₂α, ¹âµNâ‚…-8-OHdG) | MS quantification for improved accuracy [14] [15] | Correct for recovery losses and matrix effects; Essential for precise quantification |
| Calphostin C | Calphostin C, CAS:121263-19-2, MF:C44H38O14, MW:790.8 g/mol | Chemical Reagent |
| Pbox-15 | Pbox-15, CAS:354759-10-7, MF:C28H19NO3, MW:417.5 g/mol | Chemical Reagent |
The comparative analysis of lipid peroxidation products, protein modifications, and DNA oxidation markers reveals distinct yet complementary perspectives on oxidative stress in chronic diseases. Lipid peroxidation biomarkers, particularly F2-isoprostanes, offer sensitive indicators of early oxidative damage and are established gold standards in cardiovascular and neurodegenerative research [14] [15]. Protein oxidation markers provide direct links to functional impairment of enzymes and cellular structures, with redox proteomics enabling identification of specifically modified proteins in conditions like Alzheimer's disease [12] [16]. DNA oxidation markers, especially 8-OHdG, represent genotoxic consequences of oxidative stress with strong implications for genomic instability and cellular aging across multiple chronic conditions [13] [11].
The selection of appropriate biomarkers should be guided by research objectives, with multi-class biomarker approaches providing the most comprehensive assessment of oxidative stress status. As methodologies advance, particularly in mass spectrometry-based techniques, simultaneous quantification of multiple biomarkers across classes is becoming increasingly feasible, offering powerful tools for understanding oxidative mechanisms in disease pathogenesis and evaluating novel antioxidant therapies [14] [11] [15].
The accurate diagnosis, prognosis, and management of complex chronic diseases rely heavily on the identification and interpretation of biomarkers. While conditions such as cardiovascular disease, metabolic syndrome, and chronic kidney disease often coexist and share common pathophysiological pathways, each disorder exhibits a unique molecular signature. Understanding these disease-specific biomarker profiles is critical for researchers and drug development professionals aiming to develop targeted therapies and precision medicine approaches. This guide provides a structured comparison of characteristic biomarker patterns across these disease domains, supported by experimental data and methodological protocols, with a particular focus on their relationship to oxidative stress pathways.
Comparative Biomarker Profiles Across Disease Domains
The tables below synthesize key biomarker patterns across cardiovascular, metabolic, and renal conditions, highlighting their clinical relevance and disease-specific associations.
Table 1: Core Pathophysiological Processes and Representative Biomarkers by Disease Domain
| Disease Domain | Core Pathophysiological Processes | Representative Biomarkers |
|---|---|---|
| Cardiovascular | Chronic inflammation, endothelial dysfunction, fibrosis, mitochondrial dysfunction, oxidative stress | suPAR, Galectin-3, GDF-15, MDA, 8-OHdG, F2-isoprostanes [17] [4] |
| Metabolic (MetS) | Insulin resistance, dyslipidemia, central obesity, chronic inflammation, oxidative stress | Leptin, Adiponectin, IL-6, TNF-α, Oxidized LDL, Uric acid, LysoPC a C18:2 [18] [19] |
| Renal (CKD) | Glomerular & tubular injury, fibrosis, inflammation, oxidative stress | KIM-1, NGAL, Cystatin C, suPAR, TGF-β1, IL-6, TNF-α [20] [21] [22] |
Table 2: Characteristic Biomarker Patterns and Functional Roles in Specific Diseases
| Biomarker | Cardiovascular Conditions | Metabolic Conditions | Renal Conditions |
|---|---|---|---|
| suPAR | Predicts atherosclerosis & coronary artery calcification; marker of systemic inflammation [17] | Associated with metabolic disorders & insulin resistance [17] | Strongly associated with CKD progression & glomerular dysfunction [17] [21] |
| Galectin-3 | Key regulator of cardiac fibrosis & remodeling; prognostic in heart failure [17] | Linked to hepatic fibrosis in MASLD [17] | Associated with kidney disease progression & fibrosis [17] |
| GDF-15 | Implicated in mitochondrial dysfunction & cardiovascular aging [17] | Elevated in metabolic stress & insulin resistance [17] | Not a primary renal biomarker |
| KIM-1 | Not a primary cardiovascular biomarker | Not a primary metabolic biomarker | Urinary marker of tubular injury; predicts CKD progression [20] [21] |
| NGAL | Not a primary cardiovascular biomarker | Not a primary metabolic biomarker | Marker of acute & chronic kidney damage; predicts CKD progression [20] [21] |
| LysoPC a C18:2 | Not a primary cardiovascular biomarker | Negatively associated with MetS & all 5 components; potential protective role [19] | Not a primary renal biomarker |
| Amino Acids (e.g., BCAA, Phe) | Not a primary cardiovascular biomarker | Positively associated with MetS; indicates impaired catabolism [19] | May be altered in uremic milieu |
| MDA / 8-OHdG | Elevated; indicates lipid peroxidation & DNA damage in hypertension [4] | Elevated; indicates systemic oxidative stress [18] | Elevated; indicates oxidative kidney injury [20] |
Experimental Protocols for Biomarker Analysis
Protocol for Oxidative Stress Biomarker Measurement
The following protocol is adapted from clinical studies evaluating oxidative stress in chronic disease populations, including long COVID and metabolic syndrome [5] [4].
- Sample Collection: Collect blood samples (e.g., 5 mL) and process to obtain serum or plasma. For urinary DNA damage markers, collect mid-stream urine. Store aliquots at -80°C until analysis.
- Measurement of Oxidative Stress (d-ROMs Test):
- Principle: Measures hydroperoxides which react via the Fenton reaction to generate radicals that oxidize an amine substrate, creating a colored complex [5].
- Procedure: Add serum to a buffered reagent containing the chromogen. Incubate and measure absorbance photometrically at 505 nm. Results are expressed in Carratelli Units (CARR U) [5].
- Measurement of Antioxidant Capacity (BAP Test):
- Calculation of Oxidative Stress Index (OSI): OSI = C × (d-ROMs / BAP), where C is a standardization coefficient [5].
- Advanced Oxidative Damage Assays:
- Lipid Peroxidation: Malondialdehyde (MDA) can be measured via the Thiobarbituric Acid-Reactive Substances (TBARS) assay. F2-isoprostanes, more stable end-products, are quantified using gas or liquid chromatography-mass spectrometry (HPLC/MS-MS) for high specificity [4].
- DNA Oxidation: 8-hydroxy-2'-deoxyguanosine (8-OHdG) is quantified using HPLC with electrochemical or mass spectrometry detection (HPLC-ECD or HPLC-MS/MS) or via ELISA kits [4].
Protocol for Multiplexed Kidney Biomarker Analysis
This protocol details the simultaneous measurement of a 21-protein panel in plasma and urine, as used in studies characterizing AKI and CKD/ESKD [22].
- Sample Preparation:
- Plasma: Collect blood via phlebotomy into appropriate tubes. Centrifuge to isolate plasma, aliquot, and freeze at -80°C. Avoid freeze-thaw cycles.
- Urine: Collect mid-stream urine or from an indwelling catheter. Centrifuge to remove debris, aliquot the supernatant, and freeze at -80°C.
- Multiplex Immunoassay Procedure:
- Bead Addition: Add 50 μL of the mixed capture beads to each well of a 96-well plate.
- Washing: Wash the plate using a magnetic plate washer.
- Sample & Standard Incubation: Add 25 μL of Universal Assay Buffer to each well, followed by 25 μL of sample (undiluted plasma/urine or pre-diluted, as optimized) or standard. Incubate for 60 minutes at room temperature with shaking.
- Detection Antibody Incubation: After washing, add 25 μL/well of biotinylated detection antibody mix. Incubate for 30 minutes with shaking.
- Streptavidin-PE Incubation: After washing, add 50 μL/well of Streptavidin-PE solution. Incubate for 30 minutes with shaking.
- Reading: After a final wash, add Reading Buffer and analyze the plate on a compatible Luminex system (e.g., Bio-Plex 200) [22].
- Data Analysis: Use instrument software to calculate concentrations from standard curves. Apply statistical and machine learning models to identify diagnostic profiles.
Integrated Pathophysiological Pathways
The following diagram illustrates the interconnected pathways and biomarkers shared across cardiovascular, metabolic, and renal systems, highlighting oxidative stress as a central mechanism.
Diagram: Interconnected Pathways in Chronic Disease. This diagram shows how oxidative stress acts as a central driver of key pathophysiological processes (center), which in turn promote tissue damage in cardiovascular, metabolic, and renal systems (bottom). Characteristic biomarkers for each process are shown (right).
The Scientist's Toolkit: Key Research Reagents & Materials
Table 3: Essential Research Reagents for Biomarker Profiling
| Reagent / Material | Function / Application | Example Biomarkers |
|---|---|---|
| AbsoluteIDQ p150/p180 Kit | Targeted metabolomics for simultaneous quantification of amino acids, acylcarnitines, lipids, etc. | LysoPC a C18:2, Branched-chain amino acids, Glycine [19] |
| Human ProcartaPlex Kidney Panels | Multiplex immunoassays for simultaneous protein biomarker quantification in plasma/urine. | KIM-1, NGAL, Cystatin C, TFF3, β2-microglobulin [22] |
| d-ROMs & BAP Test Kits | Photometric assays for determining oxidative stress and antioxidant capacity. | Hydroperoxides, Biological Antioxidant Potential [5] |
| Luminex xMAP Instrumentation | Platform for fluorescent bead-based multiplex immunoassays. | suPAR, Galectin-3, Cytokines [22] |
| HPLC-ECD / HPLC-MS/MS | High-sensitivity quantification of specific oxidative damage molecules. | 8-OHdG, F2-isoprostanes [4] |
| Troponin I Immunoassay | Gold-standard immunoassay for myocardial injury. | Troponin I (not covered in detail, but critical for CVD) [23] |
| Pci 29732 | Pci 29732, CAS:330786-25-9, MF:C22H21N5O, MW:371.4 g/mol | Chemical Reagent |
| Quarfloxin | Quarfloxin, CAS:865311-47-3, MF:C35H33FN6O3, MW:604.7 g/mol | Chemical Reagent |
In the cellular world, two transcription factors, Nuclear Factor-Kappa B (NF-κB) and Nuclear Factor Erythroid 2-Related Factor 2 (Nrf2), serve as central regulators of the body's response to inflammation and oxidative stress. These systems are not isolated; they engage in extensive crosstalk, forming a coordinated defense network [24] [25]. Dysregulation of the delicate balance between NF-κB-driven inflammation and Nrf2-mediated antioxidant response is a hallmark of numerous chronic diseases, including cardiovascular diseases, neurodegenerative disorders, and cancer [24] [26] [25]. This guide provides a comparative analysis of these two pivotal signaling pathways, offering experimental data and methodologies relevant for researchers and drug development professionals working in the field of oxidative stress.
Comparative Analysis of Nrf2 and NF-κB Pathways
The following tables provide a structured comparison of the core structural components, regulatory mechanisms, and functional roles of the Nrf2 and NF-κB pathways.
Table 1: Core Structural Components and Regulatory Mechanisms
| Feature | Transcription Factor Nrf2 | Transcription Factor NF-κB |
|---|---|---|
| Protein Family | Cap'n'Collar (CNC) subfamily of basic leucine zipper (bZIP) transcription factors [24] [27] | NF-κB/Rel family [28] |
| Key Domains | Seven Nrf2-ECH homology (Neh) domains (Neh1-Neh7). Neh1 contains CNC-bZIP region; Neh2 contains DLG/ETGE motifs for Keap1 binding [24] [27] | Rel Homology Domain (RHD) for dimerization, DNA binding, and nuclear localization [24] [28] |
| Primary Inhibitor | Kelch-like ECH-associated protein 1 (Keap1) in the cytoplasm [24] [29] [27] | Inhibitor of κB (IκB), most commonly IκBα [24] [28] |
| Regulatory Mechanism (Basal State) | Keap1 promotes ubiquitination and proteasomal degradation of Nrf2, keeping it at low levels [24] [27] | IκB binds to and sequesters NF-κB in the cytoplasm, preventing its nuclear translocation [24] [28] |
| Activation Trigger | Oxidative stress, electrophiles [24] | Pro-inflammatory cytokines, pathogen-associated molecular patterns (PAMPs), damage-associated molecular patterns (DAMPs) [25] |
| Activation Mechanism | Stress modifies Keap1 cysteine residues, disrupting Nrf2 ubiquitination. Nrf2 stabilizes, translocates to nucleus, forms heterodimer with sMaf, and binds ARE [24] [28] | Activators trigger IκB Kinase (IKK). IKK phosphorylates IκB, leading to its ubiquitination and degradation. NF-κB dimer translocates to nucleus [24] [28] |
| Key Downstream Targets | Antioxidant genes: HO-1, NQO1, GCL, GSTs [24] [30] | Pro-inflammatory genes: TNF-α, IL-6, IL-1β, CRP [25] |
Table 2: Functional Roles in Health and Disease
| Aspect | Nrf2 Pathway | NF-κB Pathway |
|---|---|---|
| Primary Function | Master regulator of antioxidant and cytoprotective responses; maintains redox homeostasis [24] [29] | Master regulator of innate and adaptive immune and inflammatory responses [24] [25] |
| Role in Disease Pathogenesis | Deficiency/Low Activity: Linked to increased susceptibility to oxidative damage, inflammation, and diseases like Alzheimer's and CAD [30] [25]Hyperactivation: Associated with cancer progression and chemoresistance [27] | Overactivation: Drives chronic inflammation, contributing to atherosclerosis, rheumatoid arthritis, and cancer [24] [25] |
| Therapeutic Goal | Activation is desirable for cytoprotection in neurodegenerative and cardiovascular diseases [27] [25] | Inhibition is often the goal to curb chronic inflammation in autoimmune and cardiovascular diseases [25] |
| Key Experimental Biomarkers | - mRNA/protein levels of Nrf2, Keap1 [27]- ARE-reporter gene activity [29]- Target gene expression: HO-1, NQO1 [24] [29] | - mRNA/protein levels of NF-κB subunits (p65, p50) [25]- NF-κB DNA-binding activity (EMSA) [25]- Cytokine levels: TNF-α, IL-6, IL-1β [25] |
The Critical Crosstalk Between Nrf2 and NF-κB
The Nrf2 and NF-κB pathways do not operate in isolation but engage in a complex, bidirectional crosstalk that is crucial for integrating the cellular response to stress [24] [25] [28]. This interplay represents a key regulatory node in disease pathogenesis and a potential therapeutic target.
- Nrf2 Antagonizes NF-κB Signaling: Nrf2 activation can suppress NF-κB signaling through multiple mechanisms. By enhancing the expression of antioxidant enzymes like HO-1 and scavenging reactive oxygen species (ROS), Nrf2 reduces the oxidative stress that acts as a potent activator of NF-κB [25] [28]. Furthermore, HO-1 and its metabolic products can directly inhibit NF-κB activation [28]. Some evidence also suggests Nrf2 can compete with NF-κB for the transcriptional coactivator CBP, thereby limiting NF-κB-driven gene expression [28].
- NF-κB Inhibits Nrf2 Activity: The influence is mutual. NF-κB can suppress the Nrf2 pathway, potentially by recruiting histone deacetylases to the antioxidant response element (ARE), leading to transcriptional repression [24]. This creates a vicious cycle where inflammation begets more oxidative stress and impaired antioxidant defense.
- SIRT6 as a Regulatory Node: Recent research highlights SIRT6, a NAD+-dependent deacetylase, as a key regulator of this crosstalk. SIRT6 can activate the Nrf2/HO-1 pathway while simultaneously suppressing NF-κB signaling and its downstream inflammatory cytokines, thereby attenuating both oxidative stress and inflammation in conditions like coronary artery disease [25].
Experimental Protocols for Pathway Analysis
Assessing Nrf2 Signaling Activity
Objective: To evaluate the activation status of the Nrf2 pathway in cell culture models treated with a compound of interest (e.g., sulforaphane).
Methodology:
- Cell Lysis and Fractionation: Lyse treated cells and perform cytoplasmic and nuclear fractionation using commercially available kits.
- Western Blot Analysis:
- Targets: Probe for Nrf2 in both nuclear and cytoplasmic fractions. An increase in the nuclear-to-cytoplasmic Nrf2 ratio indicates activation [29].
- Key Downstream Proteins: Probe for classic Nrf2 target proteins like HO-1 and NQO1 in whole cell lysates [24].
- Loading Controls: Use Lamin B1 for nuclear fractions and α-Tubulin for cytoplasmic fractions.
- Quantitative RT-PCR (qRT-PCR):
- Measure mRNA expression levels of Nrf2 target genes (e.g., HMOX1, NQO1, GCLC) to confirm transcriptional activation [24].
- Reporter Gene Assay:
- Transfert cells with a plasmid containing the ARE promoter linked to a luciferase reporter gene. Treat with the test compound and measure luciferase activity as a direct readout of Nrf2-mediated transcription [29].
Evaluating NF-κB Signaling Activity
Objective: To determine the effect of a pro-inflammatory stimulus (e.g., TNF-α) on NF-κB pathway activation.
Methodology:
- Immunofluorescence (IF):
- Seed cells on coverslips, treat with stimulus, and fix. Stain with an antibody against the p65 subunit of NF-κB and a fluorescent secondary antibody. Use DAPI to stain nuclei.
- Analysis: Visualize using fluorescence microscopy. In unstimulated cells, p65 is cytoplasmic. Upon activation, p65 translocates to the nucleus, visible as DAPI co-localization [24].
- Electrophoretic Mobility Shift Assay (EMSA):
- Isolate nuclear extracts from treated cells. Incubate with a labeled DNA probe containing the NF-κB consensus binding sequence.
- Analysis: Run on a native gel. A shift in the probe's mobility indicates NF-κB binding to the DNA, confirming activation [25].
- ELISA for Cytokines:
- Collect cell culture supernatant after treatment.
- Use specific ELISA kits to quantify the secretion of NF-κB-dependent pro-inflammatory cytokines, such as TNF-α, IL-6, and IL-1β [25].
Measuring Oxidative Stress Biomarkers
Objective: To quantify oxidative stress levels in patient plasma or cell culture supernatant.
Methodology:
- Malondialdehyde (MDA) Assay:
- Superoxide Dismutase (SOD) Activity Assay:
- Principle: SOD is a key antioxidant enzyme that catalyzes the dismutation of superoxide radicals.
- Protocol: Use a commercial SOD activity kit, typically based on the ability of SOD to inhibit the oxidation of a tetrazolium salt by superoxide anion generated by a xanthine/xanthine oxidase system [31].
Signaling Pathway Visualizations
Nrf2 Signaling and Regulation
Nrf2 Pathway Regulation
NF-κB Signaling Pathway
NF-κB Pathway Activation
Nrf2/NF-κB Crosstalk
Nrf2/NF-κB Crosstalk
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for Studying Nrf2 and NF-κB Pathways
| Reagent / Assay | Function / Application | Specific Example Targets |
|---|---|---|
| Antibodies for Western Blot/IF | Detect protein expression, localization, and post-translational modifications. | Nrf2, Keap1, HO-1, NQO1, NF-κB p65, Phospho-IκBα, IκBα [24] [25] |
| Cytokine ELISA Kits | Quantify secreted inflammatory mediators in cell supernatant or serum. | TNF-α, IL-6, IL-1β [25] |
| ARE Reporter Plasmid | Measure Nrf2 transcriptional activity in a high-throughput manner. | Firefly luciferase gene under control of ARE promoter [29] |
| Nuclear Extraction Kit | Isolate nuclear and cytoplasmic fractions to study transcription factor translocation. | Analysis of Nrf2 and NF-κB nuclear import [29] |
| Commercial Activity Assay Kits | Quantify oxidative stress markers and antioxidant enzyme activity. | MDA (Lipid Peroxidation), SOD Activity, GSH/GSSG Ratio [31] |
| Pathway Agonists & Antagonists | Experimentally manipulate pathway activity for functional studies. | Nrf2 Agonists: Sulforaphane [29]IKK/NF-κB Inhibitors: BAY 11-7082 |
| Quinacainol | Quinacainol, CAS:86073-85-0, MF:C21H30N2O, MW:326.5 g/mol | Chemical Reagent |
| Quinagolide hydrochloride | Quinagolide hydrochloride, CAS:94424-50-7, MF:C20H34ClN3O3S, MW:432.0 g/mol | Chemical Reagent |
NF-κB and Nrf2 represent two pivotal, interconnected transcriptional pathways that coordinate the cellular response to inflammation and oxidative stress. Their antagonistic crosstalk is a critical determinant of cellular fate in chronic disease. A deep understanding of their distinct mechanisms, regulatory nodes like SIRT6, and the experimental tools to study them is essential for advancing therapeutic strategies. Future research will continue to elucidate the complexity of this interaction, paving the way for novel interventions that can precisely modulate this balance to treat cancer, neurodegenerative, cardiovascular, and metabolic diseases.
The Inflammation-Oxidative Stress Nexus represents a fundamental, self-amplifying biological circuit in which reactive oxygen species (ROS) and inflammatory mediators engage in reciprocal regulation, driving the pathogenesis of numerous chronic diseases. This intricate crosstalk creates a vicious cycle where ROS activate pro-inflammatory signaling pathways, and the resulting inflammatory response, in turn, stimulates further ROS production [33]. This nexus is not merely sequential but synergistic, establishing pathogenic loops that sustain chronic inflammation in conditions ranging from cardiovascular and neurodegenerative disorders to cancer and metabolic diseases [34] [35]. Understanding the molecular architecture of this interplay—specifically the cytokine networks and their interaction with reactive species—provides critical insights for therapeutic intervention in chronic disease pathology.
The balance between oxidative and reductive forces (redox balance) is crucial for maintaining physiological homeostasis. However, emerging evidence suggests that deviations to either extreme—oxidative stress (OS) or the less-appreciated reductive stress (RS)—can disrupt immune function and contribute to disease progression [34]. This review examines the molecular machinery of this nexus, compares oxidative stress markers across disease contexts, details experimental approaches for its study, and explores therapeutic implications for drug development.
Molecular Mechanisms: Signaling Pathways and Transcription Factors
Reactive Oxygen Species as Pro-Inflammatory Signaling Molecules
Reactive oxygen species, including superoxide anion (O₂•â»), hydrogen peroxide (Hâ‚‚Oâ‚‚), and hydroxyl radicals (•OH), function as crucial second messengers in cellular signaling while also serving as damaging agents in excess [33] [36]. These molecules originate from multiple cellular sources:
- Mitochondria: The electron transport chain, particularly complexes I and III, constitutes the primary endogenous source of ROS, where electron leakage to oxygen generates superoxide anions [34] [37].
- NADPH Oxidases (NOX): Enzyme systems dedicated to ROS production, with NOX2 playing a central role in the oxidative burst essential for microbial killing in phagocytes [34] [38].
- Endoplasmic Reticulum: Oxidative protein folding during ER stress generates Hâ‚‚Oâ‚‚ release through enzymes like Ero1 and protein disulfide isomerase [34].
The dual nature of ROS—as signaling mediators and damaging agents—depends on their concentration, spatial localization, and temporal dynamics [36]. At physiological levels, ROS facilitate normal cellular proliferation and differentiation, but when produced excessively, they trigger oxidative damage and activate inflammatory pathways [38].
Key Redox-Sensitive Transcription Factors
Table 1: Major Redox-Sensitive Transcription Factors in the Inflammation-Oxidative Stress Nexus
| Transcription Factor | Activation Trigger | Key Target Genes | Biological Outcome |
|---|---|---|---|
| NF-κB | ROS-mediated IκB phosphorylation | TNF-α, IL-6, IL-1β, COX-2, iNOS | Pro-inflammatory cytokine production, inflammasome activation |
| Nrf2 | Oxidative modification of Keap1 cysteine residues | HO-1, NQO1, GCLC, GST | Antioxidant response element (ARE) activation, cytoprotection |
| HIF-1α | ROS inhibition of PHD enzymes | VEGF, glycolytic enzymes | Angiogenesis, metabolic adaptation, inflammation |
| AP-1 | ROS activation of MAPK pathways | MMPs, cyclin D1, pro-inflammatory cytokines | Proliferation, tissue remodeling, inflammation |
| NLRP3 | ROS-induced TXNIP dissociation from Trx1 | IL-1β, IL-18 | Inflammasome assembly, inflammatory cell death (pyroptosis) |
The NF-κB pathway represents the most well-characterized redox-sensitive inflammatory pathway [34] [33]. ROS activate IκB kinase (IKK), leading to phosphorylation and degradation of IκB, which frees NF-κB dimers (p65/p50) to translocate to the nucleus and promote transcription of pro-inflammatory genes encoding cytokines, adhesion molecules, and enzymes like COX-2 and iNOS [34] [33]. This pathway establishes a feed-forward loop where NF-κB target genes, particularly those encoding cytokines like TNF-α and IL-1β, further stimulate ROS production from immune cells.
The Nrf2-Keap1 pathway functions as a critical protective axis against oxidative stress [34] [33]. Under basal conditions, Nrf2 is bound to Keap1 and targeted for ubiquitination and degradation. OS modifies critical cysteine residues on Keap1, leading to Nrf2 stabilization and nuclear translocation, where it binds to antioxidant response elements (AREs) and induces transcription of cytoprotective genes including heme oxygenase-1 (HO-1), NAD(P)H quinone dehydrogenase 1 (NQO1), and glutamate-cysteine ligase catalytic subunit (GCLC) [34]. Nrf2 activation not only mitigates oxidative damage but also exerts anti-inflammatory effects by suppressing NF-κB-driven transcription [34] [33].
A pivotal mechanism in the oxidative-inflammatory network is the reciprocal regulation between NF-κB and Nrf2 pathways [33]. These transcription factors compete for limited co-activators, such as CREB-binding protein (CBP), and exert mutually antagonistic effects. NF-κB activation suppresses Nrf2-mediated transcription by sequestering CBP, thereby limiting the antioxidant response. Conversely, Nrf2 activation reduces oxidative burden and inhibits NF-κB signaling through suppression of IKK activity [33].
Figure 1: Core Signaling Circuitry of the Inflammation-Oxidative Stress Nexus. ROS activate both pro-inflammatory NF-κB and antioxidant Nrf2 pathways. NF-κB induces cytokine production that further stimulates ROS generation, creating an amplification loop, while Nrf2 induces antioxidants that neutralize ROS. The pathways exhibit reciprocal inhibition, competing for transcriptional co-activators.
Comparative Analysis of Oxidative Stress Markers Across Chronic Diseases
The assessment of oxidative stress in clinical and research settings relies on measuring specific molecular biomarkers that reflect oxidative damage to cellular components. The table below summarizes key oxidative stress biomarkers and their alterations across major chronic disease categories.
Table 2: Oxidative Stress Biomarkers Across Chronic Diseases: Comparison and Clinical Utility
| Biomarker | Molecular Nature | Analytical Methods | Disease Contexts & Alterations | Research & Clinical Utility |
|---|---|---|---|---|
| Malondialdehyde (MDA) | Lipid peroxidation product | TBARS assay, HPLC, LC-ESI-MS/MS | ↑ CVD, CKD, CCHS, NASH, neurodegenerative diseases | Gold standard lipid peroxidation marker; urinary MDA useful for risk stratification in CCHS [39] |
| 8-Hydroxy-2'-Deoxyguanosine (8-OHdG) | Oxidized DNA nucleoside | ELISA, HPLC-ECD, GC/MS | ↑ Cancer, neurodegenerative disorders, CVD | Sensitive marker of oxidative DNA damage; correlates with disease progression [36] |
| F2-Isoprostanes | Prostaglandin-like compounds from lipid peroxidation | GC/MS, LC-MS/MS | ↑ Diabetes, obesity, neurodegenerative diseases | Robust marker of lipid peroxidation; not artifactual; elevated in AD, diabetes [36] [26] |
| 4-Hydroxy-2-Nonenal (HNE) | Reactive aldehyde from lipid peroxidation | Immunohistochemistry, LC-MS/MS | ↑ AD, PD, metabolic diseases, cancer | Highly reactive; modifies proteins, DNA; implicated in neurodegeneration, carcinogenesis [26] |
| Protein Carbonyls | Oxidatively modified proteins | DNPH assay, Western blot | ↑ Pulmonary fibrosis, aging, neurodegenerative diseases | Marker of protein oxidation; L. minor extract reduces levels in bleomycin-induced fibrosis [39] |
| Cys34 Albumin Oxidation | Oxidized thiol on plasma albumin | Mass spectrometry | ↑ Duchenne muscular dystrophy (mdx mice) | Blood biomarker reflecting muscle protein thiol oxidation; superior to protein carbonylation in DMD [39] |
| 8-iso-PGF2α | Isoprostane from lipid peroxidation | GC/MS, immunoassays | ↑ Diabetes, atherosclerosis, renal disease | Reliable in vivo oxidant stress marker; elevated in diabetic complications [32] |
The comparative analysis of these biomarkers across diseases reveals both common and pathology-specific patterns of oxidative damage. For instance, lipid peroxidation products (MDA, HNE, F2-isoprostanes) show consistent elevation across cardiovascular, metabolic, and neurodegenerative conditions, suggesting shared mechanisms of oxidative membrane damage [39] [26]. In contrast, Cys34 albumin oxidation appears particularly valuable for monitoring dystrophic pathology in Duchenne muscular dystrophy, indicating its potential as a disease-specific biomarker [39].
The context-dependent utility of these markers is exemplified by urinary MDA monitoring in Congenital Central Hypoventilation Syndrome (CCHS), where it serves as a key biomarker of oxidation for patient risk stratification [39]. Similarly, plasma Cys34 albumin thiol oxidation more closely reflects changes in protein thiol oxidation in dystrophic muscle than the more commonly used protein carbonylation, highlighting the importance of selecting appropriate biomarkers for specific pathological contexts [39].
Experimental Approaches: Methodologies for Assessing the Nexus
Standard Protocols for Oxidative Stress Biomarker Assessment
Lipid Peroxidation Measurement via MDA Quantification The thiobarbituric acid reactive substances (TBARS) assay represents a widely used method for assessing lipid peroxidation through malondialdehyde (MDA) detection [39] [36]. The protocol involves:
- Sample Preparation: Homogenize tissue or biofluid in PBS containing butylated hydroxytoluene (0.01%) to prevent artificial lipid peroxidation during processing.
- Reaction Mixture: Combine 100μL sample with 200μL of 8.1% SDS, 1.5mL of 20% acetic acid (pH 3.5), and 1.5mL of 0.8% thiobarbituric acid.
- Incubation: Heat mixture at 95°C for 60 minutes, then cool on ice.
- Extraction & Measurement: Centrifuge at 3,000g for 15 minutes, measure supernatant absorbance at 532nm. Quantify MDA using molar extinction coefficient of 1.56×10âµ Mâ»Â¹cmâ»Â¹.
- Advanced Validation: For improved specificity, employ LC-ESI-MS/MS with DNPH derivatization, particularly in complex matrices like exhaled breath condensate [39].
Protein Carbonyl Content Determination Protein carbonyls serve as reliable markers of protein oxidation. The standard DNPH-based protocol includes:
- Derivatization: React protein samples (1mg/mL) with 10mM 2,4-dinitrophenylhydrazine (DNPH) in 2M HCl for 60 minutes in darkness.
- Protein Precipitation: Add 20% trichloroacetic acid, incubate on ice for 15 minutes, then centrifuge at 11,000g for 10 minutes.
- Washing: Wash pellet three times with ethanol:ethyl acetate (1:1) to remove free DNPH.
- Solubilization & Measurement: Dissolve final pellet in 6M guanidine hydrochloride, measure absorbance at 370nm. Calculate carbonyl content using molar absorptivity of 22,000 Mâ»Â¹cmâ»Â¹.
Comprehensive Lipidomic Profiling for Lipid Peroxidation Products Advanced mass spectrometry approaches provide detailed assessment of oxidative lipid damage:
- Lipid Extraction: Use modified Bligh-Dyer method with chloroform:methanol (2:1 v/v) containing internal standards.
- LC-MS Analysis: Employ reverse-phase C18 column with gradient elution (water/acetonitrile:isopropanol). Perform nanoESI-MS or LC/MS for intact lipid and lipid hydroperoxide detection [39].
- Data Processing: Use specialized software (e.g., LipidSearch, XCMS) for peak alignment, identification, and quantification. Key peroxidized lipids include triglyceride hydroperoxides (TGOOH) and phosphatidylcholine hydroperoxides (PCOOH), identified as diagnostic biomarkers in chronic kidney disease and NASH models [39].
Research Reagent Solutions for Investigating the Nexus
Table 3: Essential Research Reagents for Studying Oxidative Stress and Inflammation
| Reagent/Category | Specific Examples | Research Application | Mechanistic Insight |
|---|---|---|---|
| ROS Detection Probes | DCFH, DHE, BODIPY variants | Cellular ROS measurement, flow cytometry, microscopy | Specificity for different ROS species (Hâ‚‚Oâ‚‚ vs O₂•â»); compartment-targeted probes available [36] |
| Antioxidant Compounds | NAC, quercetin, curcuminoids | Experimental antioxidant interventions | NAC boosts glutathione; quercetin downregulates NOX2-derived ROS, suppresses MAPK/NF-κB [33] [36] |
| Enzyme Inhibitors | NOX inhibitors (apocynin), NF-κB inhibitors | Pathway-specific inhibition | Apocynin blocks NOX assembly; NF-κB inhibitors prevent nuclear translocation [34] |
| Cytokine Assays | ELISA, Luminex, ELISA-based cytokine panels | Inflammatory mediator quantification | Multiplex panels enable parallel measurement of TNF-α, IL-6, IL-1β, IL-18 in biological samples [34] [38] |
| Nrf2 Activators | Sulforaphane, bardoxolone methyl | Enhancement of antioxidant response | Induce Nrf2 dissociation from Keap1, promote ARE-driven gene expression (HO-1, NQO1) [34] [33] |
| Animal Models of Disease | mdx mice (DMD), BLM-induced pulmonary fibrosis, NASH models | Pathophysiological context testing | mdx mice show elevated Cys34 albumin oxidation; bleomycin model demonstrates oxidative protein damage [39] |
Figure 2: Comprehensive Experimental Workflow for Assessing the Inflammation-Oxidative Stress Nexus. The integrated approach combines measurement of reactive species, oxidative damage biomarkers, and inflammatory mediators from biological samples, enabling comprehensive profiling of the redox-inflammatory axis.
Therapeutic Implications and Future Directions
Targeting the inflammation-oxidative stress nexus presents both challenges and opportunities for therapeutic development. Conventional antioxidant approaches have demonstrated limited clinical efficacy, likely due to non-specific actions, poor bioavailability, and failure to address the bidirectional nature of redox dysregulation [34] [33]. This has prompted development of more sophisticated strategies:
Mitochondria-Targeted Antioxidants These compounds (e.g., MitoQ, SkQ1) concentrate in mitochondria, the primary ROS source, offering superior efficacy compared to untargeted antioxidants. In animal models, they improve coronary angiogenesis and cardiac function in mitochondrial infarction [26] [37].
Nrf2 Activators Pharmacological activation of the Nrf2 pathway provides a systems-level approach to enhancing antioxidant capacity. Compounds like bardoxolone methyl induce a coordinated antioxidant response, showing promise in diabetic kidney disease and other oxidative stress-related conditions [33].
Advanced Delivery Systems Nanoparticle-enabled delivery of antioxidants addresses bioavailability limitations. Single-atom nanozymes with catalase-like and SOD-like activity (e.g., Mn-based catalysts) attenuate neuroinflammation and promote blood-brain barrier reconstruction in traumatic brain injury models [26].
Dual-Target Approaches Simultaneous targeting of oxidative and inflammatory pathways may offer synergistic benefits. For instance, nano-formulated curcumin (80mg/day) in multiple sclerosis patients significantly reduced both IL-6 and oxidative markers, indicating dual antioxidant and anti-inflammatory activity [33].
The emerging recognition of reductive stress as a potential pathological state suggests that therapeutic strategies must aim to restore redox homeostasis rather than simply suppress oxidation [34]. Future research directions should include disease-specific redox profiling, development of compartment-specific redox biomarkers, and personalized interventions based on individual redox signatures.
The inflammation-oxidative stress nexus represents a fundamental pathological circuit in chronic diseases, with cytokine networks and reactive species engaging in sophisticated cross-talk. Comprehensive understanding of this interplay, facilitated by the experimental approaches and biomarkers detailed here, provides a roadmap for developing targeted therapeutic strategies that disrupt this vicious cycle and restore physiological redox balance.
Analytical Approaches: Techniques for Measuring Oxidative Stress Biomarkers in Research and Clinical Settings
Biomarker quantification is a cornerstone of modern clinical and preclinical research, providing critical data for diagnosing diseases, monitoring treatment efficacy, and understanding pathological mechanisms. Among the plethora of analytical techniques available, Liquid Chromatography-Mass Spectrometry (LC-MS), Gas Chromatography-Mass Spectrometry (GC-MS), and Enzyme-Linked Immunosorbent Assay (ELISA) have emerged as three cornerstone methodologies. Each technique offers distinct advantages and limitations, making their selection crucial for research validity, particularly in complex fields like oxidative stress marker analysis in chronic diseases. This guide provides a objective, data-driven comparison of these gold standard methods, equipping researchers and drug development professionals with the information needed to select the optimal technology for their specific biomarker quantification needs.
Understanding the fundamental working principles of each technology is essential for appreciating their comparative strengths and applications in biomarker analysis.
Liquid Chromatography-Mass Spectrometry (LC-MS) combines the physical separation capabilities of liquid chromatography with the mass analysis capabilities of mass spectrometry. In LC-MS, the sample is dissolved in a liquid mobile phase and separated through a column packed with a stationary phase. The separated analytes are then ionized, most commonly via electrospray ionization (ESI), and the resulting ions are separated based on their mass-to-charge ratio (m/z) and detected [40]. This technique is exceptionally versatile for analyzing a wide range of biomolecules, from small molecules to proteins, without the need for derivatization.
Gas Chromatography-Mass Spectrometry (GC-MS) similarly couples the separation power of gas chromatography with mass spectrometry. However, it requires that analytes be volatile and thermally stable. The sample is vaporized and carried by an inert gas through a column, where separation occurs. The separated components are then ionized, typically by electron impact (EI) or chemical ionization (CI), before mass analysis [41] [40]. For non-volatile compounds, this often necessitates a derivatization step to increase volatility and thermal stability, adding complexity to sample preparation.
Enzyme-Linked Immunosorbent Assay (ELISA) is an immunoassay that detects antigen-antibody interactions. It utilizes an enzyme-linked conjugate and a chromogenic substrate that generates a measurable color change. The core principle involves immobilizing an antigen or antibody on a solid phase (typically a 96-well microplate), followed by a series of binding and washing steps. The intensity of the color produced is proportional to the amount of analyte present and is measured spectrophotometrically [42]. Common formats include direct, indirect, and sandwich ELISA, with the latter offering high specificity through the use of two antibodies that "sandwich" the target antigen.
Comparative Performance Analysis
The selection of an analytical platform hinges on its performance characteristics. The table below provides a structured comparison of LC-MS, GC-MS, and ELISA across key parameters, with a focus on implications for oxidative stress biomarker research.
Table 1: Performance Comparison of LC-MS, GC-MS, and ELISA for Biomarker Quantification
| Performance Parameter | LC-MS/MS | GC-MS | ELISA |
|---|---|---|---|
| Sensitivity | High (e.g., LOD for cotinine: 0.1 ng/mL) [43] | High (comparable to LC-MS/MS for targeted analytes) [41] | Variable; can be very high (e.g., picomolar range for competitive ELISA); often lower than MS [43] [44] |
| Specificity | Very High (based on mass and fragmentation pattern) | Very High (based on mass and fragmentation pattern) | High, but subject to antibody cross-reactivity [45] [44] |
| Throughput | Moderate to High | Moderate (longer run times and sample prep) [41] | Very High (amenable to full 96-well plates) [42] |
| Sample Preparation | Moderate (e.g., protein precipitation, SPE) [41] | Complex (often requires derivatization) [41] | Simple (often minimal processing required) [42] |
| Analyte Scope | Very Broad (small molecules, lipids, proteins) [40] | Limited to volatile/derivatizable compounds (e.g., steroids, fatty acids) [40] | Broad (proteins, hormones, peptides, antibodies) [42] |
| Multiplexing Capability | Limited in targeted mode, broader in untargeted | Limited | Available with multiplex immunoassay platforms [46] |
| Cost & Accessibility | High capital cost, requires specialized expertise | High capital cost, requires specialized expertise | Low to moderate cost, widely accessible [43] |
Key Implications for Oxidative Stress Research
- Analyte Scope and Specificity: Oxidative stress encompasses diverse biomarkers, including lipid peroxidation products (e.g., MDA, isoprostanes), DNA adducts (e.g., 8-OHdG), and modified proteins. LC-MS is exceptionally suited for quantifying a wide panel of these metabolites with high specificity, minimizing ambiguity. GC-MS is a robust tool for specific volatile compounds, while ELISA kits are available for many markers but can suffer from cross-reactivity with structurally similar molecules [47] [32].
- Sensitivity for Low-Abundance Markers: Many oxidative stress markers circulate at low concentrations. The high sensitivity of LC-MS/MS and GC-MS makes them ideal for detecting these low levels, as demonstrated in studies measuring trace-level environmental exposures [43]. While ELISA sensitivity can be improved via signal amplification, it may not reliably detect very low-level markers in all biological matrices [44].
- Quantification and Standardization: MS-based methods provide absolute quantification using internal standards, which is critical for longitudinal studies and inter-laboratory comparisons. ELISA provides relative quantification against a standard curve, and results can vary significantly between different commercial kits, even for the same analyte, due to differences in antibody specificity [45].
Experimental Protocols and Data Concordance
Empirical comparisons highlight how methodological choice can directly influence research outcomes.
Case Study: Quantifying Cotinine in Saliva
A 2020 study directly compared LC-MS/MS and ELISA for quantifying salivary cotinine, a biomarker for tobacco smoke exposure in children [43].
- Protocol: Saliva samples from 218 children were analyzed in parallel using both LC-MS/MS (with isotope dilution) and a commercial ELISA kit. The limit of quantitation (LOQ) was 0.1 ng/mL for LC-MS/MS and 0.15 ng/mL for ELISA.
- Results: While the intraclass correlation was high (0.884), the geometric mean cotinine concentration measured by LC-MS/MS (4.1 ng/mL) was significantly lower than that from ELISA (5.7 ng/mL). This consistent overestimation by ELISA is attributed to antibody cross-reactivity with other nicotine metabolites like 3'-hydroxycotinine and its glucuronide [43]. Crucially, significant associations between cotinine levels and child sex/race were only detectable using the more sensitive and specific LC-MS/MS data, demonstrating its superior power for revealing subtle exposure-disease relationships.
Case Study: Measuring Vitamin D-Binding Protein (DBP)
A critical comparison of a monoclonal ELISA, a polyclonal ELISA, and LC-MS/MS for measuring DBP revealed profound platform-specific biases [45].
- Protocol: Serum DBP was measured in 125 participants using all three assays. Participants were genotyped for common DBP isoforms (Gc1f, Gc1s, Gc2).
- Results: The monoclonal ELISA (R&D Systems) showed a strong genotype-dependent bias, yielding disproportionately lower concentrations for the Gc1f isoform (common in Black individuals), thereby creating a spurious racial disparity. In contrast, LC-MS/MS and the polyclonal ELISA showed no significant race-based differences [45]. This highlights that immunoassay performance can be critically dependent on the specific antibodies used and the genetic variability of the target protein, a bias that MS methods largely avoid.
Table 2: Summary of Key Comparative Studies Highlighting Platform Concordance and Discordance
| Study Focus | Key Finding | Implication for Researchers |
|---|---|---|
| Cotinine Analysis [43] | ELISA overestimated concentrations vs. LC-MS/MS due to cross-reactivity; LC-MS/MS revealed significant associations with demographics that ELISA missed. | For low-level exposure studies or when metabolite specificity is critical, LC-MS/MS is strongly preferred. |
| DBP Analysis [45] | Monoclonal ELISA, but not polyclonal ELISA or LC-MS/MS, introduced significant genotype-dependent bias in quantification. | Antibody-based assays require rigorous validation against genetic variants; MS provides a more reliable absolute quantitation. |
| Benzodiazepine Analysis [41] | LC-MS/MS and GC-MS showed comparable accuracy and precision, but LC-MS/MS required minimal sample prep and no derivatization. | LC-MS/MS offers a more efficient workflow for high-throughput analysis of labile compounds without sacrificing data quality. |
| Multiplex Protein Detection [46] | In skin tape strips, the MSD platform showed higher detectability of low-abundance proteins than Olink or NULISA platforms. | For complex matrices with low protein yield, platform sensitivity is a primary consideration for successful biomarker detection. |
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful biomarker quantification relies on a suite of specialized reagents and materials. The following table details key solutions for setting up these analyses.
Table 3: Essential Research Reagent Solutions for Biomarker Quantification
| Item | Function | Application Notes |
|---|---|---|
| Deuterated Internal Standards | Corrects for sample matrix effects and variability in sample preparation and ionization. | Critical for LC-MS/GC-MS. Isotope-labeled versions of the analyte (e.g., cotinine-d4) are added to the sample before processing [43] [41]. |
| Solid-Phase Extraction (SPE) Columns | Purifies and pre-concentrates analytes from complex biological matrices (e.g., urine, plasma). | Used in sample prep for both LC-MS and GC-MS to reduce ion suppression and improve sensitivity [41]. |
| Derivatization Reagents | Increases volatility and thermal stability of non-volatile analytes for GC-MS analysis. | Required for many biomarkers (e.g., steroids, organic acids) prior to GC-MS. Example: MTBSTFA [41]. |
| High-Affinity Capture & Detection Antibodies | Binds specifically to the target analyte in a "sandwich" format for high-sensitivity detection. | The core of a sensitive and specific Sandwich ELISA. Monoclonal antibodies offer high specificity [42] [44]. |
| Enzyme-Labeled Conjugates & Chromogenic Substrates | Generates a measurable signal (colorimetric, chemiluminescent) proportional to the analyte amount. | HRP/TMB and AP/pNPP are common enzyme/substrate pairs. Signal amplification systems can boost sensitivity [42] [44]. |
| Multiplex Immunoassay Panels | Allows simultaneous quantification of dozens of protein biomarkers from a single small-volume sample. | Platforms like Meso Scale Discovery (MSD) and Olink offer pre-configured panels for pathways like inflammation [46]. |
| Quinalizarin | Quinalizarin|CAS 81-61-8|CK2 Inhibitor | |
| N-Formylfortimicin A | N-Formylfortimicin A, CAS:74228-81-2, MF:C18H35N5O7, MW:433.5 g/mol | Chemical Reagent |
Experimental Workflow and Pathway Diagrams
The following diagrams illustrate the generalized workflows for ELISA and MS-based quantification, highlighting the key decision points and steps.
Diagram 1: Sandwich ELISA Workflow. Critical wash steps (red) remove unbound material to ensure specificity [42].
Diagram 2: LC-MS/GC-MS Biomarker Quantification Workflow. The addition of an internal standard early in the process is critical for accurate quantification [43] [41].
The choice between LC-MS, GC-MS, and ELISA is not a matter of identifying a single "best" technology, but rather of selecting the most fit-for-purpose tool based on the specific research question, analyte properties, and operational constraints.
- Choose LC-MS/MS when: Your priority is maximum specificity and sensitivity for a wide range of biomarkers, particularly for small molecules and lipids in oxidative stress research. It is essential for absolute quantification, detecting low-level exposures, and when metabolite cross-reactivity is a concern [43] [41] [32].
- Choose GC-MS when: Analyzing volatile compounds or those easily made volatile (e.g., specific fatty acids, steroids). It remains a robust and highly respected technology for targeted analysis where its resolution is advantageous, though its requirement for derivatization can be a limitation [41] [40].
- Choose ELISA when: The project requires high-throughput analysis of many samples, cost is a primary constraint, or specialized expertise for MS is unavailable. It is ideal for measuring specific proteins or hormones where highly specific antibodies are available and absolute quantification is less critical than relative changes. Multiplex ELISA platforms can be powerful for exploratory protein biomarker studies [42] [46].
For a research field as nuanced as oxidative stress in chronic diseases, a tiered approach is often most effective. Multiplexed immunoassays can serve as excellent tools for initial biomarker discovery and screening, while LC-MS/MS provides the definitive, quantitative validation for key candidates, ensuring that findings are built on a foundation of robust and reliable data.
The study of complex chronic diseases demands a holistic approach to unravel their intricate molecular mechanisms. The integration of high-throughput omics technologies with advanced screening methods has revolutionized our capacity to systematically investigate pathological states, particularly in the context of oxidative stress. High-throughput omics enables comprehensive, large-scale analysis of diverse biomolecular data across multiple levels, including genomics, transcriptomics, proteomics, and metabolomics [48]. These technologies generate extensive datasets that, when combined with sophisticated bioinformatics pipelines, provide unprecedented insights into the complexity of living systems. Within this technological framework, oxidative stress has emerged as a crucial pathological mechanism, representing a loss of physiological balance between pro-oxidant factors and antioxidant defenses that leads to excessive production of reactive oxygen species (ROS) and reactive nitrogen species (RNS), which are toxic to cells [39]. This comparative guide examines the performance and applications of cutting-edge platforms and methodologies that are advancing oxidative stress biomarker research across chronic diseases.
Technology Platform Comparison: Omics and High-Throughput Screening Systems
High-Throughput Omics Technologies
Table 1: Comparative Analysis of High-Throughput Omics Platforms
| Omics Type | Key Technologies | Primary Outputs | Applications in Oxidative Stress Research | Practical Considerations |
|---|---|---|---|---|
| Genomics | Next-generation sequencing (NGS), third-generation sequencing (TGS) | Genome sequences, genetic variants | Identification of genetic predispositions to oxidative damage | Use integrated databases (e.g., Ensembl) for annotation [48] |
| Transcriptomics | RNA sequencing (RNA-Seq), microarray | Gene expression profiles, splicing variants | Analysis of gene expression changes under oxidative stress | Combine with single-cell RNA-seq for detailed insights [48] |
| Proteomics | Mass spectrometry, protein databases | Protein identification, quantification | Understanding protein oxidation, antioxidant defense systems | Employ bioinformatics tools (e.g., MaxQuant) for data processing [48] |
| Metabolomics | NMR spectroscopy, mass spectrometry | Metabolite profiles, metabolic pathways | Identification of metabolic changes induced by oxidative stress | Use MetaboAnalyst for comprehensive analysis [48] |
| Lipidomics | Mass spectrometry, chromatography | Lipid profiles, lipid interactions | Investigation of lipid peroxidation products | Utilize LipidSearch for detailed lipid analysis [48] |
The field of omics technology continues to evolve with sequencing and mass spectrometry serving as fundamental experimental tools. Sequencing-based approaches are primarily utilized for studies on genome, transcriptome, and their epitomes and interactomes involving DNA/RNA, while MS-based techniques are employed to interrogate proteome, metabolome, and interactomes that do not involve DNA/RNA [49]. Next-generation sequencing technologies have dramatically improved the speed and scalability of genomic analyses, though they suffer from short read lengths that can limit accuracy and their ability to capture structural variants [49]. Third-generation sequencing, represented by PacBio SMRT and Oxford Nanopore Technologies, addresses these limitations through single molecular real-time sequencing that allows for long-read sequencing with reduced alignment and mapping errors [49].
For proteomic and metabolomic investigations, mass spectrometry-based platforms provide powerful tools for identifying and quantifying proteins and metabolites altered under oxidative stress conditions. The integration of multi-omics data is essential to unravel the complexity of cellular processes and disease mechanisms, facilitated by sophisticated bioinformatics tools and statistical methods for managing the large datasets generated by these technologies [48].
High-Throughput Screening Systems
Table 2: Comparison of High-Throughput Screening Platforms and Applications
| Screening Type | Throughput Capacity | Detection Methods | Key Applications | Limitations |
|---|---|---|---|---|
| Conventional HTS | Up to 100,000 compounds/day | Fluorescence, luminescence, enzymatic assays | Primary compound screening, toxicity assessment | Cost, technical complexity, false positives [50] |
| Ultra-HTS (uHTS) | >300,000 compounds/day | Miniaturized fluorescence, microfluidic sensors | Large library screening, multiple analyte monitoring | Significant complexity and cost [50] |
| Biochemical HTS | Variable (depends on format) | Fluorescence, MS, NMR, differential scanning fluorimetry | Enzyme-targeted screening, protein-ligand interactions | May not capture cellular context [50] |
| Cell-based HTS | Variable (depends on format) | Viability assays, reporter systems, imaging | Functional screening, toxicity assessment, complex phenotypes | Higher variability, more complex data interpretation [50] |
| High-content Screening | Moderate | Automated imaging, multiparameter analysis | Subcellular localization, multiplexed phenotypic assays | Data storage and analysis challenges [50] |
High-throughput screening encompasses automated, miniaturized assays and supporting data analysis to rapidly identify novel compounds or biological targets [50]. HTS systems rely on several key components including automated liquid-handling robots capable of low-volume dispensing of nanoliter aliquots of sample, thereby minimizing assay setup times while providing accurate and reproducible liquid dispensing [50]. These systems typically operate in 96-, 384-, and 1536-well formats, with ultra-HTS pushing into even higher densities through advances in microfluidics and high-density microwell plates with typical volumes of 1-2 µL [50].
A significant challenge in HTS is the generation of false positive data, which can arise from various sources including assay interference from chemical reactivity, metal impurities, assay technology limitations, measurement uncertainty, autofluorescence, and colloidal aggregation [50]. This has led to the development of multiple in silico approaches for false positive detection, generally based on expert rule-based approaches or machine learning models trained on historical HTS data [50].
Oxidative Stress Biomarkers: Analytical Platforms and Methodologies
Key Biomarkers and Detection Platforms
Table 3: Oxidative Stress Biomarkers and Analytical Approaches
| Biomarker Category | Specific Biomarkers | Detection Methods | Technology Platforms | Chronic Disease Applications |
|---|---|---|---|---|
| Lipid peroxidation products | Malondialdehyde (MDA), Lipid hydroperoxides (TGOOH, PCOOH) | HPLC-MS/MS, nanoESI-MS, LC-ESI-MS/MS | Agilent, Thermo Fisher MS systems | CKD, NASH, cardiovascular diseases [39] [51] |
| Protein oxidation | Protein carbonylation, Protein peroxidation, Cys34 albumin thiol oxidation | Immunoblotting, mass spectrometry | Proteomic platforms | Duchenne muscular dystrophy, pulmonary fibrosis [39] |
| DNA/RNA damage | 8-OHdG, DNA strand breaks | ELISA, comet assay, chromatography | Microplate readers, capillary electrophoresis | Cancer, neurodegenerative diseases [39] |
| Antioxidant enzymes | SOD, catalase, glutathione peroxidase | Enzymatic activity assays, immunoassays | Spectrophotometers, microplate readers | Diabetes, cardiovascular diseases [31] |
| Metabolic signatures | Ketone bodies, amino acid profiles | 1H-NMR spectroscopy, LC-MS | NMR spectrometers, MS systems | Takotsubo syndrome, metabolic disorders [39] |
Oxidative stress constitutes a crucial mechanism in the onset and progression of various chronic inflammatory diseases, including cardiovascular diseases, neurodegenerative diseases, infection diseases, diabetes, and cancer [39]. The identification and validation of oxidative stress biomarkers has become a fundamental phase for developing personalized therapies and achieving individualized decisions in the complex management of both acute and chronic diseases [39].
Advanced detection platforms have enabled increasingly precise measurement of oxidative stress markers in different biological materials. For example, nanoelectrospray ionization-mass spectrometry (nanoESI-MS) based lipidomic profiling has revealed the key role of oxidative stress and lipid dysregulation in renal lipid droplet alteration at the molecular level in chronic kidney disease, identifying specific lipid hydroperoxides as diagnostic biomarkers [39]. Similarly, HPLC-MS/MS methods have been developed for quantitative determination of oxidative biomarkers in urine, with malondialdehyde emerging as a particularly relevant biomarker for assessing systemic oxidative status [51].
Experimental Protocols for Key Oxidative Stress Assays
Lipid Peroxidation Assay via Mass Spectrometry
Purpose: To identify and quantify lipid peroxidation products in biological samples. Sample Preparation:
- Extract lipids from tissue homogenates or cell lysates using chloroform-methanol mixture (2:1 v/v)
- Aspirate lipid droplets directly from cells using nanotips followed by in-tip microextraction [51]
- Derivatize if necessary for enhanced detection sensitivity
Instrumentation: Nanoelectrospray mass spectrometry system (e.g., Thermo Fisher Orbitrap platforms) Analysis Parameters:
- Ionization mode: Electrospray ionization in positive or negative mode depending on analyte
- Mass resolution: >60,000 for accurate mass measurements
- Data acquisition: Full scan mode followed by data-dependent MS/MS for structural confirmation
Data Processing:
- Use specialized software (e.g., LipidSearch, XCMS) for peak detection and alignment
- Perform statistical analysis to identify significantly altered lipid species
- Validate identified biomarkers using authentic standards when available [51]
High-Throughput Screening for Antioxidant Compounds
Purpose: To rapidly identify compounds with antioxidant activity from large chemical libraries. Assay Principle: Cellular or biochemical assays measuring reduction in oxidative stress markers or protection against oxidative damage.
Workflow:
- Plate Preparation: Dispense test compounds into 384-well plates using automated liquid handling systems
- Cell Treatment: Seed appropriate cell lines (e.g., HepG2 for hepatotoxicity models) and treat with compounds
- Oxidative Stress Induction: Apply oxidative stress inducer (e.g., Hâ‚‚Oâ‚‚, tert-butyl hydroperoxide)
- Viability Assessment: Measure cell viability using resazurin reduction or ATP content assays
- Oxidative Stress Measurement: Quantify reactive oxygen species using fluorescent probes (e.g., DCFH-DA, DHE)
- Data Analysis: Calculate protection percentage and determine ICâ‚…â‚€ values for active compounds
Quality Control:
- Include reference antioxidants (e.g., N-acetylcysteine, Trolox) as positive controls
- Implement Z'-factor calculations to validate assay performance (>0.5 acceptable)
- Use replicate wells to assess reproducibility [50]
Diagram 1: High-Throughput Screening Workflow for Antioxidant Discovery. This diagram illustrates the multi-stage process from initial assay development through lead optimization in antioxidant compound screening.
Integrated Data Analysis and Bioinformatics Approaches
The integration of multi-omics data represents a critical challenge and opportunity in oxidative stress research. Sophisticated bioinformatics pipelines are required to handle the complexity and volume of data generated by high-throughput technologies, integrating various software tools and databases to pre-process, analyze, and interpret data [48]. Two fundamental approaches govern omics data integration: similarity-based methods that identify common patterns, correlations, and pathways across different omics datasets, and difference-based methods that focus on detecting unique features and variations between different omics levels [48].
Similarity-based integration methods include correlation analysis that evaluates relationships between different omics levels to identify co-expressed genes or proteins, clustering algorithms such as hierarchical clustering and k-means clustering that group similar data points from different omics datasets, and network-based approaches like Similarity Network Fusion (SNF) that construct similarity networks for each omics type and then integrate them into a single network [48]. Difference-based methods include differential expression analysis that compares expression levels between different states, variance decomposition that separates total variance into components attributable to different omics levels, and feature selection methods such as LASSO and Random Forests that select the most relevant features from each omics dataset [48].
Popular integration algorithms include Multi-Omics Factor Analysis (MOFA), an unsupervised approach that uses Bayesian factor analysis to identify latent factors responsible for variation in multiple omics datasets, and Canonical Correlation Analysis (CCA), which identifies linear relationships between two or more omics datasets to facilitate discovery of correlated traits and common pathways [48]. Platforms such as OmicsNet and NetworkAnalyst provide critical tools for managing and analyzing multi-omics data, offering capabilities for visual analysis of biological networks by integrating genomics, transcriptomics, proteomics, and metabolomics data [48].
Diagram 2: Multi-Omics Integration for Oxidative Stress Research. This diagram shows how different molecular layers respond to oxidative stress and contribute to biomarker discovery and therapeutic target identification.
Research Reagent Solutions for Oxidative Stress Studies
Table 4: Essential Research Reagents and Platforms for Oxidative Stress Studies
| Reagent Category | Specific Products/Platforms | Manufacturer/Provider | Primary Applications | Key Features |
|---|---|---|---|---|
| Multi-mode Microplate Readers | Synergy HTX Multimode Reader, CLARIOstar Plus | Agilent Technologies, BMG LABTECH | HTS assays, absorbance, fluorescence, luminescence | Dual optics, temperature control, reagent injectors [52] |
| Automated Liquid Handling | Freedom EVO series, Microlab Prep | Tecan, Hamilton | Compound library preparation, assay automation | Dual liquid handling arms, nanoliter dispensing [52] |
| Cell Counting & Viability | NucleoCounter NC-200, Via2-Cassette | ChemoMetec | Cell-based assays, toxicity assessment | Image cytometry, specialized assays for difficult cells [52] |
| Specialized Assay Kits | Caspase-Glo 3/7, Proteasome-Glo, Kinase Glo | Promega Corp. | Apoptosis, proteasome activity, kinase screening | Homogeneous formats, HTS compatibility [52] |
| DNA Synthesis & Libraries | Clonal Genes, Oligo Pools, Combinatorial Libraries | Twist Bioscience | Functional genomics, synthetic biology | High-quality DNA synthesis, massive parallelism [52] |
| Microplates for Immunology | immunoGrade, hydroGrade, lipoGrade BRANDplates | BRANDTECH Scientific | ELISA, RIA, FIA assays | Specially treated surfaces, various well formats [52] |
The selection of appropriate reagents and platforms is critical for successful implementation of omics and high-throughput screening approaches in oxidative stress research. Automated systems such as the Agilent BioTek Synergy HTX Multimode Reader provide versatile detection capabilities for various assay formats including UV-Vis absorbance, fluorescence, luminescence, and AlphaScreen/AlphaLISA workflows, making them suitable for diverse oxidative stress applications [52]. Similarly, automated liquid handling platforms like Tecan's Freedom EVO series with dual liquid handling arms offer unrivalled processing speed and flexibility for compound library preparation and assay automation [52].
For cell-based screening approaches, precise cell counting and viability assessment are essential, with systems like the NucleoCounter NC-200 providing high precision automated cell counting utilizing state-of-the-art image cytometry [52]. Specialized assay kits such as the Caspase-Glo 3/7 Assay System enable highly sensitive caspase activity measurements relevant to apoptosis studies in oxidative stress research [52].
The integration of high-throughput omics approaches with advanced screening technologies has created powerful platforms for elucidating the role of oxidative stress in chronic diseases. These complementary methodologies enable researchers to move from descriptive biomarker identification to functional characterization of oxidative stress mechanisms and interventions. Genomics and transcriptomics platforms provide insights into genetic susceptibilities and transcriptional responses to oxidative stress, while proteomic and metabolomic technologies directly quantify the molecular consequences of oxidative damage. High-throughput screening systems enable rapid identification of therapeutic compounds that modulate oxidative stress pathways.
The continuing evolution of these technologies, particularly through advances in single-cell analysis, spatial omics, and artificial intelligence-driven data integration, promises to further enhance our understanding of oxidative stress in chronic diseases. As these platforms become more accessible and sophisticated, they will increasingly support the development of personalized therapeutic approaches targeting oxidative stress mechanisms across diverse patient populations. The convergence of omics and screening technologies represents a powerful paradigm for addressing the complexity of oxidative stress in chronic disease research and therapeutic development.
The accurate measurement of oxidative stress is fundamental to understanding the pathogenesis of a wide array of chronic diseases, including cardiovascular, metabolic, and neurodegenerative disorders [53] [54]. The selection of an appropriate biological sample matrix is a critical first step in the design of robust and clinically relevant studies. Blood, urine, tissue, and exhaled breath condensate (EBC) each offer distinct advantages and limitations for the quantification of oxidative stress biomarkers, influencing analytical sensitivity, disease specificity, and practical feasibility [55] [56]. This guide provides an objective, data-driven comparison of these four sample types, focusing on their application in chronic disease research. It synthesizes current experimental data, details standardized protocols, and offers practical tools to assist researchers and drug development professionals in selecting the optimal sample matrix for their specific investigative needs.
Comparative Analysis of Sample Types
The choice of sample matrix directly impacts the biological interpretation of oxidative stress levels. The table below provides a systematic comparison of blood, urine, tissue, and EBC across key parameters relevant to chronic disease research.
Table 1: Comparative Analysis of Sample Types for Oxidative Stress Biomarker Research
| Parameter | Blood (Serum/Plasma) | Urine | Tissue (Biopsy) | Exhaled Breath Condensate (EBC) |
|---|---|---|---|---|
| Invasiveness | Invasive (venipuncture) [55] | Non-invasive [55] | Highly invasive [53] | Non-invasive [57] [56] |
| Primary Biomarker Examples | MDA, SOD, GPx, 8-iso-PGF2α [53] [9] | 8-iso-PGF2α, 8-OHdG, CysLTR1 [57] [53] [58] | Tissue-specific lipid peroxides, protein carbonylation [53] | 8-iso-PGF2α, 8-OHdG, various metabolites (SESI-HRMS) [57] [56] |
| Key Advantages | Reflects systemic status; rich in both enzymatic and non-enzymatic biomarkers [53] [59] | Easily collected for long-term monitoring; integrates systemic oxidative load over time [53] [55] | Provides direct, tissue-specific assessment of oxidative damage and localized pathology [53] | Lung-specific; allows real-time, dynamic monitoring of airway oxidative stress and inflammation [57] [56] |
| Major Limitations | Subject to diurnal variation and acute stress; requires trained personnel for collection [55] | Requires normalization (e.g., to creatinine); biomarker levels can be influenced by renal function [55] | Limited accessibility; not suitable for longitudinal studies or healthy controls; ethical constraints [53] | Low concentration of biomarkers; requires highly sensitive analytical platforms; sample dilution is a concern [57] [56] |
| Typical Normalization Methods | Volume, protein content | Creatinine, specific gravity [57] [55] | Total protein, tissue weight | No universal standard; some methods use dilutional markers or conductivity [56] |
| Suitability for Longitudinal Monitoring | Moderate | High [55] | Low | High [57] |
| Analytical Platform Examples | ELISA, HPLC-MS/MS, spectrophotometric enzyme assays [53] [9] | ELISA, LC-MS/MS, GC-MS [57] [58] [9] | Immunohistochemistry, HPLC-MS/MS, redox proteomics [53] | SESI-HRMS, LC-MS/MS, Immunoassay [57] [56] |
Detailed Experimental Protocols
To ensure reproducibility and reliability, standardized protocols for sample collection, processing, and analysis are paramount. The following section details established methodologies for key experiments cited in comparative studies.
Protocol 1: Urinary 8-iso-PGF2α and 8-OHdG Analysis via ELISA and LC-MS/MS
The quantification of specific oxidative stress biomarkers in urine, such as 8-iso-prostaglandin F2α (8-iso-PGF2α) and 8-hydroxy-2'-deoxyguanosine (8-OHdG), is a cornerstone of non-invasive assessment [57] [53]. The protocol below outlines the parallel use of ELISA for high-throughput screening and LC-MS/MS for confirmatory, high-specificity analysis.
Sample Collection & Storage: Collect first-morning void urine into sterile containers [58]. Centrifuge at 3,000 × g for 10 minutes to remove particulate matter. Aliquot the supernatant and store immediately at -80°C until analysis to prevent analyte degradation [57].
Creatinine Normalization: Assess urinary creatinine concentration using a commercial ELISA or spectrophotometric kit per manufacturer's instructions (e.g., Invitrogen) [57]. All biomarker concentrations are normalized to creatinine (e.g., pg/mg creatinine) to account for variations in urine dilution [57] [55].
ELISA Protocol:
- Procedure: Use commercial ELISA kits (e.g., Cell Biolabs for 8-iso-PGF2α) following the manufacturer's protocol [57]. This typically involves adding samples and standards to antibody-coated wells, incubating, washing, adding a detection antibody, and finally adding a substrate for color development.
- Data Analysis: Measure absorbance using a microplate reader. Generate a standard curve from known concentrations and interpolate sample concentrations. Subtract the mean blank value from all measurements [57].
LC-MS/MS Protocol for High-Specificity Quantification:
- Sample Preparation: Thaw urine samples on ice. For 8-OHdG analysis, a validated protocol involves filtering urine samples using molecular mass cut-off filters (e.g., 3,000 Da) and solid-phase extraction (e.g., Oasis HLB Extraction Cartridges) [58].
- Stable-Isotope Dilution: Add known quantities of stable isotope-labeled internal standards (e.g., 8-OH-dG-15N5) to each sample prior to extraction to correct for losses during preparation and ionization variability during mass spectrometry [58].
- Instrumental Analysis: Analyze samples using a liquid chromatography-tandem mass spectrometry (LC-MS/MS) system. Chromatographic separation is achieved with a C18 column. Mass spectrometry is performed using Multiple Reaction Monitoring (MRM) mode for high sensitivity and specificity [58].
- Quantification: Calculate the ratio of the analyte peak area to the internal standard peak area. Use a calibration curve constructed from pure standards to determine the absolute concentration in the sample [58].
Protocol 2: Real-Time Breath Analysis via SESI-HRMS
Real-time breath analysis using Secondary Electrospray Ionization High-Resolution Mass Spectrometry (SESI-HRMS) represents a cutting-edge, non-invasive method for capturing a broad spectrum of volatile and non-volatile metabolites related to oxidative stress and airway inflammation [57].
Breath Sampling:
- Participant Preparation: Subjects should fast and refrain from using toothpaste, chewing gum, or cosmetics for at least one hour prior to measurement to minimize confounding signals [57].
- Standardized Collection: Use a commercially available exhalation interface (e.g., Exhalion) that simultaneously measures CO2, flow rate, exhaled volume, and pressure drop. Participants perform six prolonged exhalations into a mouthpiece fitted with a bacterial filter [57].
SESI-HRMS Analysis:
- Platform Configuration: Couple a SUPER SESI ion source to a high-resolution mass spectrometer (e.g., Q Exactive Plus). Use a non-coated silica capillary emitter with 0.1% formic acid in water for electrospray formation [57].
- Instrument Parameters: Set the ion chamber temperature to 90°C and the sampling line temperature to 130°C to minimize analyte adsorption. Acquire mass spectra in full-scan mode over a range of m/z 100–400 with a high resolution (e.g., 140,000) [57].
- Data Acquisition: Define the exhalation time window based on CO2 concentrations exceeding 2.5%. Average the mass spectra from the corresponding exhalation scans to generate a representative breath profile for each subject [57].
Data Preprocessing & Statistical Analysis:
- Convert raw files and perform peak alignment and mass calibration. Generate a feature list by binning centroid peaks.
- Replace zero-intensity values using regression on order statistics (ROS).
- Correlate breath features with established urinary or systemic biomarkers (e.g., urinary 8-iso-PGF2α) using Spearman's correlation. Control for multiple testing using the Benjamini-Hochberg method to manage the false discovery rate (FDR) [57].
The following workflow diagram illustrates the key steps of this protocol.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful execution of oxidative stress biomarker studies requires specific reagents and instruments. The table below details essential solutions and their functions for the featured experiments.
Table 2: Key Research Reagent Solutions for Oxidative Stress Biomarker Analysis
| Reagent/Instrument | Function/Application | Sample Type |
|---|---|---|
| Oasis HLB Extraction Cartridges | Solid-phase extraction for purifying and concentrating analytes (e.g., 8-OHdG) from complex urine matrices prior to LC-MS/MS [58]. | Urine |
| Stable Isotope-Labeled Internal Standards (e.g., 8-OH-dG-15N5) | Used in stable-isotope dilution mass spectrometry to correct for matrix effects and analyte loss during sample preparation, ensuring quantitative accuracy [58]. | Urine, Blood |
| Commercial ELISA Kits (e.g., for 8-iso-PGF2α, cotinine) | High-throughput, immunologically-based quantification of specific biomarkers. Ideal for large cohort studies [57] [9]. | Urine, Blood, EBC |
| SUPER SESI Ion Source | A specialized ionization source that allows for real-time, soft ionization of breath volatiles and semi-volatiles when coupled to a high-resolution mass spectrometer [57]. | Exhaled Breath |
| Exhalion Exhalation Interface | Standardized breath collection device that provides parallel, real-time measurement of CO2, flow, and volume, enabling the identification of the alveolar portion of the breath [57]. | Exhaled Breath |
| Formic Acid in Water (0.1%) | Electrospray solvent used in SESI-HRMS to generate charged droplets for the ionization of breath analytes [57]. | Exhaled Breath |
| Antibody-coated Microplates | Core component of ELISA kits; surface is coated with capture antibodies specific to the target biomarker (e.g., 8-iso-PGF2α) [57]. | Urine, Blood |
| LC-MS/MS with C18 Column | Gold-standard platform for high-specificity separation (chromatography) and sensitive detection (mass spectrometry) of a wide range of oxidative stress biomarkers [53] [58]. | Urine, Blood, Tissue, EBC |
| Quinaprilat | Quinaprilat, CAS:82768-85-2, MF:C23H26N2O5, MW:410.5 g/mol | Chemical Reagent |
| Nicainoprol | Nicainoprol, CAS:76252-06-7, MF:C21H27N3O3, MW:369.5 g/mol | Chemical Reagent |
The comparative analysis of blood, urine, tissue, and EBC reveals that no single sample matrix is universally superior for oxidative stress research. The optimal choice is dictated by the specific research question, the biological compartment of interest, and practical constraints. Urine remains the gold standard for non-invasive, longitudinal assessment of systemic oxidative load, with 8-iso-PGF2α and 8-OHdG being highly validated biomarkers [57] [53]. EBC offers unparalleled potential for lung-specific, real-time monitoring, though it demands advanced analytical instrumentation like SESI-HRMS [57]. Blood provides a comprehensive snapshot of systemic redox status, while tissue biopsies deliver definitive, localized data at the expense of invasiveness [53]. Future research directions should focus on standardizing EBC collection and analysis, validating multi-matrix biomarker panels, and integrating data from these diverse sources through systems biology approaches to build a holistic understanding of oxidative stress in chronic diseases.
Oxidative stress, characterized by an imbalance between the production of reactive oxygen species (ROS) and the body's antioxidant defenses, is a central pathological component across numerous chronic diseases, including cardiovascular disorders, diabetes, neurodegenerative conditions, and metabolic syndrome [60] [61]. For researchers and drug development professionals, accurately assessing the components of this balance is paramount for understanding disease mechanisms, identifying prognostic biomarkers, and evaluating therapeutic efficacy. Functional assays provide critical tools for this purpose, primarily falling into two categories: those that evaluate the Total Antioxidant Capacity (TAC) of a biological system, and those that measure the susceptibility of lipoproteins to oxidation.
TAC assays offer a composite measure of the combined antioxidant capacity of all soluble compounds in a biological sample, providing an integrated parameter rather than focusing on individual components [62]. Meanwhile, the evaluation of lipoprotein oxidation susceptibility, particularly for pro-atherogenic particles like Low-Density Lipoprotein (LDL), is crucial because oxidized LDL (ox-LDL) is not merely a biomarker but an active pathogenic mediator. Ox-LDL contributes to endothelial dysfunction, foam cell formation, and plaque instability in atherosclerosis, and has also been implicated in the pathophysiology of diabetes, chronic kidney disease, and neurodegenerative disorders [63] [61]. This guide objectively compares the performance, applications, and limitations of key functional assays used to evaluate these parameters within chronic disease research.
Comparative Analysis of Total Antioxidant Capacity (TAC) Assays
Total Antioxidant Capacity represents the cumulative capacity of all antioxidants in a sample to neutralize free radicals. This global assessment is vital because measuring individual antioxidants is labor-intensive and may not reflect synergistic interactions [62]. No single assay can fully capture the complex antioxidant profile of a biological sample, as different methods operate on distinct chemical principles and may be sensitive to different classes of antioxidants [64]. The most common spectrophotometric TAC assays can be classified based on their underlying reaction mechanisms: Hydrogen Atom Transfer (HAT) and Single Electron Transfer (SET) methods [62].
HAT-based methods measure the ability of an antioxidant to quench free radicals by hydrogen donation. These reactions are pH-independent and typically rapid. In contrast, SET-based methods detect an antioxidant's ability to transfer a single electron to reduce a compound, including metals, carbonyls, and radicals. These assays are pH-dependent and generally slower than HAT-based methods [62]. The table below provides a structured comparison of the most widely used TAC assays, detailing their mechanisms, primary applications, and key advantages and limitations.
Table 1: Comparison of Major Total Antioxidant Capacity (TAC) Assays
| Assay Name | Reaction Mechanism | Key Readout | Primary Applications | Advantages | Limitations |
|---|---|---|---|---|---|
| ORAC (Oxygen Radical Absorbance Capacity) | HAT-based | Fluorescence decay over time | Food science, plant polyphenol analysis, nutraceutical development [62] | Biologically relevant radical source; measures inhibition period | Longer assay time; less suited for automated analysis [62] |
| TEAC/ABTS (Trolox Equivalent Antioxidant Capacity) | SET-based | Absorbance decay of pre-formed ABTS•+ radical | Clinical studies, rapid sample screening, automated high-throughput analysis [62] | Operational simplicity; measures both hydrophilic/lipophilic antioxidants [62] | Non-physiological radical source; may overestimate certain antioxidants [64] |
| FRAP (Ferric Reducing Antioxidant Power) | SET-based | Absorbance increase from Fe3+ to Fe2+ reduction | Serum/plasma analysis in metabolic and cardiovascular disease research [62] [64] | Simple, fast, and inexpensive; does not require specialized equipment [62] | Non-physiological conditions (low pH); ignores antioxidants that do not reduce iron [62] |
| CUPRAC (Cupric Reducing Antioxidant Capacity) | SET-based | Absorbance increase from Cu2+ to Cu1+ reduction | Plant extracts, food analysis, physiological fluids [64] | Operates at physiological pH; high sensitivity to thiol-type antioxidants [64] | Less established in clinical settings compared to FRAP or TEAC |
A critical consideration for researchers is that TAC values obtained from different assays are often poorly correlated because each method measures a different aspect of the antioxidant response and is sensitive to different compounds [62] [64]. For instance, in human serum, the TEAC assay primarily measures albumin and uric acid, while the FRAP assay is highly sensitive to uric acid and ascorbic acid [62]. Therefore, a panel of integrated assays is highly recommended for a comprehensive assessment of a sample's antioxidant status, rather than reliance on a single method [62].
Evaluating Lipoprotein Oxidation Susceptibility
The oxidation of lipoproteins, particularly Low-Density Lipoprotein (LDL), is a key event in the pathogenesis of atherosclerosis and is also implicated in other chronic conditions [61]. Unlike TAC assays that measure defensive capabilities, assays for lipoprotein oxidation susceptibility evaluate a offensive process—the propensity of lipids to undergo peroxidation. Oxidized LDL (ox-LDL) is a complex particle containing various oxidation products, and its formation is a multi-stage process involving the oxidation of polyunsaturated fatty acids (PUFAs) within the lipoprotein particle [65].
The pathological significance of ox-LDL is well-established. It is more readily taken up by macrophages via scavenger receptors, leading to foam cell formation—the hallmark of early atherosclerotic lesions [61]. Beyond cardiovascular disease, elevated ox-LDL levels have been documented in type 2 diabetes mellitus (T2DM), pulmonary tuberculosis, and their comorbidities, suggesting its role as a cross-disease risk factor [63]. Furthermore, oxidized Lipoprotein(a) [ox-Lp(a)] has been shown to exhibit enhanced atherogenic potential by more effectively impairing fibrinolysis compared to its native form, highlighting the broader relevance of oxidized lipoproteins in thrombotic risk [66].
Table 2: Key Markers for Assessing Lipoprotein Oxidation
| Oxidation Marker | Type | What It Measures | Significance in Disease & Research |
|---|---|---|---|
| Conjugated Dienes (CD) | Primary Product | Early-stage hydroperoxides from PUFA oxidation | Research tool for tracking initial oxidation kinetics in isolated lipoproteins [65] |
| Lag Phase of LDL Oxidation | Kinetic Parameter | Resistance time of isolated LDL to copper-induced oxidation ex vivo | Measures intrinsic susceptibility of LDL to oxidation; shorter lag time indicates higher risk [67] |
| Oxidized LDL (ox-LDL) | Direct Measurement | Circulating levels of in vivo oxidized LDL via ELISA | Clinical biomarker; independent risk factor for CVD; elevated in diabetes, CKD [63] [61] [67] |
| Malondialdehyde (MDA) | Secondary Product | End-product of lipid peroxidation | General marker of oxidative stress; used in TBARDs assay; correlates with disease severity [65] |
| Lipoprotein(a) [Lp(a)] Oxidation | Functional Assay | Impairment of fibrinolysis by oxidized Lp(a) via chromogenic substrate assay | Research tool to study thrombotic mechanisms and enhanced atherogenicity of ox-Lp(a) [66] |
The susceptibility of lipoproteins to oxidation can be modulated. For example, a meta-analysis of clinical trials concluded that vitamin E supplementation significantly reduces ox-LDL levels and increases the lag time of LDL oxidation, confirming its protective role [67]. Furthermore, rational formulation of composite antioxidants that combine radical scavengers like ethoxyquin (EQ) and butylated hydroxytoluene (BHT) with metal chelators like citric acid (CA) has been shown to provide superior, synergistic protection against lipid peroxidation in complex systems like animal feed, outperforming single-component systems [65].
Experimental Protocols for Key Assays
TEAC/ABTS Assay Protocol
This protocol is adapted for a 96-well microplate reader and is based on established methodologies [65] [62].
- ABTS•+ Radical Cation Generation: Incubate 7 mM ABTS stock solution with 2.45 mM potassium persulfate (final concentration) in the dark at room temperature for 12-16 hours before the assay. This results in the formation of the stable blue-green ABTS•+ radical.
- Working Solution Preparation: Dilute the pre-formed ABTS•+ solution with phosphate-buffered saline (PBS, pH 7.4) or another suitable buffer until an absorbance of 0.70 (±0.02) at 734 nm is achieved.
- Sample and Standard Preparation: Prepare serial dilutions of both the sample (e.g., serum, plant extract) and the Trolox standard (a water-soluble vitamin E analog) in the same buffer.
- Reaction: Pipette 10-20 µL of sample/standard and 180-190 µL of the ABTS•+ working solution into each well. Mix thoroughly.
- Measurement: Incubate the plate at 30°C or room temperature for a fixed time (e.g., 6-10 minutes). Measure the absorbance at 734 nm exactly at the end of the incubation period.
- Calculation: Calculate the percentage inhibition of absorbance for each sample and standard. Construct a Trolox standard curve (Percentage Inhibition vs. Trolox concentration). Express the TAC of the sample as Trolox Equivalents (TE), e.g., mmol TE/L for fluids or µmol TE/g for solids.
2Ex VivoLDL Oxidation Lag Time Assay
This protocol measures the kinetic resistance of isolated LDL to copper-induced oxidation [67].
- LDL Isolation: Isolate LDL from fresh human or animal plasma via sequential ultracentrifugation in the density range of 1.019-1.063 g/mL. Dialyze the isolated LDL extensively against a cold, oxygen-free buffer (e.g., PBS, pH 7.4, containing 100 µM EDTA) to remove salts and exogenous antioxidants. Remove EDTA via further dialysis before the assay, as it chelates copper.
- Reaction Setup: Dilute the LDL to a standardized protein concentration (e.g., 50-100 µg/mL) in PBS without EDTA. Add copper sulfate (CuSO₄) to a final concentration of 5-10 µM to initiate oxidation. Distribute the solution into multiple wells of a temperature-controlled microplate reader.
- Kinetic Measurement: Continuously monitor the formation of conjugated dienes by measuring absorbance at 234 nm over time at 37°C.
- Data Analysis: Plot absorbance at 234 nm versus time. The resulting curve has three characteristic phases: a lag phase (minimal absorbance increase), a propagation phase (rapid, linear increase), and a plateau phase. The lag time is defined as the intercept of the tangents to the lag and propagation phases, as shown in the workflow diagram. A shorter lag time indicates higher susceptibility of the LDL to oxidation.
Chromogenic Substrate Assay for ox-Lp(a) Impairment of Fibrinolysis
This assay evaluates the functional consequence of Lp(a) oxidation on the fibrinolytic system [66].
- Preparation of ox-Lp(a): Chemically oxidize isolated Lp(a) using a system containing glucose oxidase, myeloperoxidase (MPO), and sodium nitrite (NaNO₂). Incubate for 30 minutes at 37°C and stop the reaction with butylated hydroxytoluene (BHT).
- Fibrin Clot Formation: In a PEG-2000 coated 96-well plate, add human fibrinogen to a final concentration of 200 µg/mL in HEPES buffer (pH 7.4). Add thrombin alpha-IIa (50 nM) to initiate clot formation and incubate for 20 minutes at 37°C. Stop the thrombin activity by adding hirudin.
- Fibrinolysis Reaction: To the formed fibrin clot, add glu-plasminogen (200-5000 nM), tissue plasminogen activator (tPA, 1 nM), and the chromogenic substrate for plasmin, S-2302 (2 mM). Include either native Lp(a) or oxidized Lp(a) at low and high concentrations in separate wells.
- Kinetic Monitoring: Immediately monitor the increase in absorbance at 405 nm, which corresponds to plasmin generation from plasminogen, at 30-second intervals.
- Interpretation: Compare the initial rates (Vmax) of plasmin formation and the total plasmin generated over time. Oxidized Lp(a) will typically show a significant inhibitory effect, evidenced by an earlier plateau and reduced overall plasmin levels, indicating impaired fibrinolysis.
Visualizing Assay Workflows and Pathophysiological Context
TAC Assay Selection and Workflow
The following diagram outlines the logical decision-making process for selecting an appropriate TAC assay based on research objectives and the general workflow for a typical SET-based assay like TEAC.
Diagram 1: Decision workflow for TAC assay selection and the general TEAC protocol.
Pathogenesis of Oxidized Lipoproteins in Chronic Disease
This diagram illustrates the central role of lipoprotein oxidation in the pathogenesis of multiple chronic diseases, connecting the molecular event of oxidation to clinical outcomes.
Diagram 2: The pathogenic role of oxidized LDL in chronic diseases.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagent Solutions for Functional Antioxidant and Lipoprotein Assays
| Reagent / Kit | Function in Assay | Key Characteristics & Research Considerations |
|---|---|---|
| ABTS (2,2'-Azinobis-(3-ethylbenzothiazoline-6-sulfonic acid)) | Precursor for generating the stable ABTS•+ radical cation in TEAC assay. | Water-soluble; requires pre-incubation with oxidant (e.g., persulfate, H₂O₂/enzyme); stability of working solution must be validated [62]. |
| Trolox (6-Hydroxy-2,5,7,8-tetramethylchroman-2-carboxylic acid) | Water-soluble vitamin E analog used as a primary standard. | Allows expression of results as Trolox Equivalents (TE), enabling comparison across different samples and studies [62] [64]. |
| TPTZ (2,4,6-Tripyridyl-s-triazine) | Chromogenic agent that complexes with Fe²⺠in the FRAP assay. | The Fe²âº-TPTZ complex is blue and measured at 593 nm; the assay is performed at low pH (3.6) to maintain iron solubility [62] [60]. |
| Neocuproine (2,9-Dimethyl-1,10-phenanthroline) | Chromogenic agent for CUPRAC assay, complexes with Cuâº. | The Cuâº-neocuproine complex is orange-yellow (450 nm); key advantage is operation at physiological pH [64]. |
| Human ox-LDL ELISA Kits | Quantify circulating levels of in vivo oxidized LDL in serum/plasma. | Uses specific monoclonal antibodies against oxidized apoB-100 epitopes; crucial for clinical correlation studies [63] [61]. |
| AAPH (2,2'-Azobis(2-amidinopropane) dihydrochloride) | Water-soluble azo compound that generates peroxyl radicals at a constant rate upon thermal decomposition. | Used as a physiological radical source in the ORAC assay [62]. |
| Copper Sulfate (CuSO₄) | Pro-oxidant used to induce LDL oxidation ex vivo in the lag time assay. | Standard concentration is 5-10 µM; requires EDTA-free buffer conditions to be effective [67]. |
| Chromogenic Substrate S-2302 | Synthetic plasmin substrate (H-D-Pro-Phe-Arg-pNA) used in fibrinolysis assays. | Cleavage by plasmin releases p-nitroaniline, measured at 405 nm; used to study ox-Lp(a) effects [66]. |
| Nicanartine | Nicanartine | Antioxidant Research Compound | Nicanartine is a synthetic antioxidant and cholesterol-lowering agent for research into atherosclerosis and diabetic retinopathy. For Research Use Only. |
| Niddamycin | Niddamycin, CAS:20283-69-6, MF:C40H65NO14, MW:783.9 g/mol | Chemical Reagent |
Non-invasive assessment tools, particularly questionnaires and composite indices, are fundamental to large-scale population studies in chronic disease research. Their ability to efficiently collect standardized data across diverse populations makes them indispensable for epidemiological research, risk stratification, and public health surveillance. Within the specific context of oxidative stress markers comparison across chronic diseases, these tools enable researchers to investigate relationships between oxidative balance, lifestyle factors, and disease prevalence without resorting to complex biochemical measurements in all study participants. The emergence of digital technologies is further transforming this field, enhancing the scalability, speed, and cost-effectiveness of data collection while introducing new considerations regarding data equivalence and mode effects [68]. This guide provides a comparative analysis of these tools, focusing on their application in chronic disease research, with specific emphasis on methodologies for validating their performance in population-based studies.
Comparison of Major Non-Invasive Assessment Tools
The following tables summarize key non-invasive tools used in population studies, highlighting their characteristics, applications, and performance metrics.
Table 1: Comparison of General Composite Indices for Nutritional and Health Security Assessment
| Tool Name | Primary Construct Measured | Components/Scoring | Validation & Performance Data | Key Chronic Disease Applications |
|---|---|---|---|---|
| Oxidative Balance Score (OBS) [69] | Balance of pro- and anti-oxidant exposures | 16 dietary nutrients & 4 lifestyle factors; higher scores indicate antioxidant balance [69] | Inverse association with CIAD (Q4 vs Q1 OR: 0.71, 95% CI 0.64-0.81); Linear dose-response relationship [69] | Chronic inflammatory airway diseases (Asthma, COPD, Chronic Bronchitis) [69] |
| Global Health Security Index (GHSI) [70] | Country-level preparedness for infectious disease outbreaks | 6 domains: Prevention, Detection, Response, Health System, Norms, Risk Environment [70] | Not addressed in this article | Not applicable; macro-level health security |
| Nutritional Risk Index (NRI) [71] | Nutritional status in cirrhosis | Albumin and weight change | Sensitivity: 83.3%; NPV: 90.7%; AUC: 0.800 for predicting mortality/complications [71] | Liver cirrhosis |
| Subjective Global Assessment (SGA) [71] | Nutritional status | History and physical exam | Highest accuracy (AUC: 0.794) for predicting mortality/complications in cirrhosis [71] | Liver cirrhosis |
Table 2: Digital Delivery Modes for Questionnaires and Their Impact on Data Quality
| Delivery Mode | Key Characteristics | Impact on Data Quality (vs. Alternatives) | Reported Advantages & Limitations |
|---|---|---|---|
| Smartphone/Tablet Apps [68] | Apps running on consumer smart devices; high scalability | Data Equivalence: No significant differences in mean scores vs. other modes [68]. Data Completeness: Better than paper and SMS in uncontrolled settings [68]. Time: Findings on completion speed are contradictory [68]. | Maximizes scalability and speed; reduces cost; improves adherence to sampling protocols vs. paper [68]. |
| Web-Based Technologies [72] | Online platforms, telehealth services | Not inferior to traditional care; improves medication adherence, symptom management, and reduces rehospitalization [72]. | Enables personalized healthcare programs; effective for monitoring and feedback [72]. |
| Digitized Pen-and-Paper Questionnaires [73] | Direct digital translation of existing paper forms | Screening accuracy varies widely (Sensitivity: 0.32-1.00; Specificity: 0.37-1.00; AUC: 0.57-0.98) [73]. | High risk of bias in studies; field is in early stages with high-quality evidence lacking [73]. |
Experimental Protocols for Tool Validation
A critical component of employing non-invasive tools is understanding and validating their performance characteristics. Below are detailed methodologies for key validation experiments cited in this field.
Protocol for Validating the Oxidative Balance Score (OBS)
The association between OBS and chronic inflammatory airway diseases (CIAD) was validated using a large-scale population-based approach [69].
- Study Population & Design: Data were gathered from the National Health and Nutrition Examination Survey (NHANES) 2013–2018 cycles. The cross-sectional study included 12,458 adults aged 20 and older, with 2,495 participants identified as having CIAD (asthma, chronic bronchitis, or COPD) based on self-report.
- OBS Calculation: The OBS was calculated using 20 components (16 dietary nutrients from 24-hour recall interviews without supplements, and 4 lifestyle factors). Dietary fiber, carotene, riboflavin, niacin, total folate, vitamin B6, vitamin B12, vitamin C, vitamin E, calcium, magnesium, zinc, copper, selenium were categorized as antioxidants. Iron and total fat were classified as pro-oxidants. For lifestyle, physical activity was an antioxidant, while alcohol consumption, BMI, and serum cotinine were pro-oxidants. Each component was scored 0, 1, or 2 based on sex-specific percentiles, and all scores were summed.
- Statistical Analysis: Multiple logistic regression models were used to examine the association between OBS quartiles and the prevalence of CIAD, adjusting for confounders including age, sex, race, education, and family income. Dose-response relationships were analyzed using restricted cubic spline (RCS) regression. For mortality outcomes, Kaplan-Meier survival analysis and multiple COX regressions were conducted.
- Key Outcome Measures: The primary outcomes were odds ratios (ORs) for the prevalence of CIAD across OBS quartiles. Secondary outcomes included hazard ratios (HRs) for all-cause and respiratory disease mortality among CIAD patients.
Protocol for Assessing Nutritional Tool Performance in Cirrhosis
The diagnostic performance of various nutritional screening and assessment tools for predicting outcomes in cirrhotic patients was evaluated as follows [71].
- Study Population: 94 patients with cirrhosis were enrolled and followed for 1 year.
- Tools Compared: Nutritional screening was performed using the Royal Free Hospital-Nutritional Prioritizing Tool (RFH-NPT), Liver Disease Undernutrition Screening Tool (LDUST), Malnutrition Universal Screening Tool (MUST), Prognostic Nutritional Index (PNI-O), Nutritional Risk Index (NRI), and others. Nutritional assessment was performed using BMI, triceps skinfold (TSF), midarm circumference (MAC), midarm muscle circumference (MAMC), six-minute walk test (6MWT), Subjective Global Assessment (SGA), and Royal Free Hospital Subjective Global Assessment (RFH-SGA).
- Outcome Measure: The composite outcome was a combination of mortality and complications of cirrhosis over the 1-year follow-up period.
- Statistical Analysis: The sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and accuracy (reflected by the Area Under the Curve, AUC) of each tool in predicting the composite outcome were calculated and compared.
Protocol for Evaluating Digital Mental Health Assessment Tools
The validity of digital mental health assessment tools was systematically reviewed using the following methodology [73].
- Search Strategy & Study Selection: A systematic search was conducted in MEDLINE, Embase, Cochrane Library, and other databases for articles published between 2005 and 2021. Studies were included if they evaluated the accuracy of a question-and-answer-based digital mental health tool against a gold standard reference test (e.g., assessment by a psychiatrist or structured diagnostic interview).
- Data Extraction & Analysis: Two independent reviewers extracted data on study characteristics, the digital tool used, the mental health condition assessed, and outcomes of accuracy including sensitivity, specificity, and the area under the receiver operating characteristic curve (AUC). The revised tool for the Quality Assessment of Diagnostic Accuracy Studies (QUADAS-2) was used to assess the risk of bias and applicability of the included studies.
Visualizing Workflows and Compositions
Oxidative Balance Score (OBS) Framework and Validation
Oxidative Balance Score Framework and Validation Workflow
Composite Index Development and Validation Logic
Composite Index Development and Validation Logic
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents and Materials for Non-Invasive Assessment Research
| Item | Function/Application in Research | Example from Literature |
|---|---|---|
| NHANES Dataset | Provides comprehensive, population-level data on health, nutrition, and examination metrics for calculating composite scores and validating associations. | Used to calculate OBS and investigate its association with chronic inflammatory airway diseases and mortality [69]. |
| Structured Clinical Interview (e.g., SCID) | Serves as a gold standard reference for validating the diagnostic accuracy of digital mental health screening tools. | Used as a comparator for digital assessments of conditions like major depressive disorder and generalized anxiety disorder [73]. |
| Liver Biopsy Specimen | The histological gold standard for staging liver fibrosis, against which non-invasive tools like elastography and MV-flow are validated. | Used as the reference standard for validating microvascular flow imaging and elastography in chronic liver disease patients [74]. |
| Ultrasound with Elastography & MV-Flow | Non-invasive devices for measuring liver stiffness and microvascular architecture to assess fibrosis. | RS85 ultrasound (Samsung Medison) and FibroScan (Echosens) were used to measure liver stiffness and microvascular changes correlated with biopsy-proven fibrosis [74]. |
| Standardized Nutritional Assessment Tool (e.g., SGA, RFH-SGA) | Provides a clinician-evaluated benchmark of nutritional status for validating simpler nutritional screening tools. | Used as a comparator for tools like NRI, MUST, and CONUT in predicting mortality and complications in cirrhotic patients [71]. |
| Rabeprazole | Rabeprazole Sodium|Proton Pump Inhibitor for Research | Research-grade Rabeprazole, a potent proton pump inhibitor. Explore its applications in gastric acid studies. For Research Use Only. Not for human use. |
Overcoming Challenges: Validation, Standardization, and Interpretation of Oxidative Stress Data
Oxidative stress is a common pathway in the pathogenesis of numerous chronic diseases, yet the translation of its biomarkers from research to clinical application is fraught with analytical challenges. For researchers and drug development professionals, a critical understanding of the limitations in specificity, sensitivity, and reproducibility is essential for advancing diagnostic and therapeutic strategies. This guide provides a comparative analysis of these limitations, supported by experimental data and detailed methodologies.
The Core Challenge: A Plethora of Markers Lacking Standardization
The fundamental hurdle in oxidative stress biomarker research is the vast diversity of markers and the frequent lack of correlation between them, compounded by the use of non-specific methods and sophisticated techniques that are impractical for routine clinical use [75]. A biomarker, as defined by the World Health Organization, is any substance, structure, or process that can be measured in the body and can influence or predict disease incidence or outcome [75]. To be clinically useful, a biomarker must demonstrate specificity for a certain disease, have prognostic value, and/or correlate with disease activity [75] [76].
The table below summarizes the primary analytical challenges faced by key categories of oxidative stress biomarkers.
Table 1: Core Analytical Limitations of Major Oxidative Stress Biomarker Categories
| Biomarker Category | Specificity Concerns | Sensitivity & Dynamic Range | Reproducibility Challenges |
|---|---|---|---|
| Lipid Peroxidation (e.g., MDA, F2-isoprostanes) [4] [9] | MDA measured via TBARS assay is notoriously non-specific [4]. F2-isoprostanes are more specific but require advanced technology. | F2-isoprostanes are stable and sensitive markers of in vivo oxidation, suitable for detecting systemic oxidative stress [4]. | High heterogeneity (I² >90%) reported in MDA measurements across studies, often due to variability in assay design and population [9]. |
| Protein Oxidation (e.g., Protein Carbonyls, AGEs) [75] | Protein carbonyls can arise from multiple oxidative mechanisms, making it difficult to pinpoint the exact source of damage [75]. | Carbonyl concentration is generally higher than other biomarkers, facilitating detection, but may lack sensitivity for early disease stages [75]. | Commercial ELISA kits provide ease of use but many do not specify the antibody used, hindering inter-laboratory comparison [75]. |
| DNA Damage (8-OHdG) [4] | A specific marker of oxidative DNA damage, elevated in aging, cancer, and diabetes [4]. | Highly sensitive detection is achievable with HPLC-MS/MS. ELISA kits offer high throughput but risk cross-reactivity [4]. | Requires careful validation of ELISA kits to avoid antibody cross-reactivity, which can compromise reproducibility [4]. |
| Antioxidant Capacity (BAP, TAC) [5] [77] | Reflects the combined action of all antioxidants, providing a global status but no insight into specific antioxidant deficiencies [77]. | Can indicate depleted defenses or a temporary adaptive response to stress. Lower levels suggest diminished capacity [77]. | As a functional assay, results can be influenced by pre-analytical conditions and the specific methodology employed. |
| Global Oxidative Stress (d-ROMs, OSI) [5] | d-ROMs measure hydroperoxides, intermediate ROS, providing a general oxidative load rather than a disease-specific signal [5] [77]. | Useful for assessing the overall "oxidative burden." Cut-off values (e.g., OSI >1.92 for brain fog in Long COVID) are being defined for clinical use [5]. | The test's reliability depends on standardized sample collection and analysis protocols, which are not yet universal [5]. |
Experimental Protocols for Key Biomarker Assays
A clear understanding of common experimental methodologies is key to interpreting data and identifying sources of variability.
Measurement of Protein Carbonyls
Protein carbonyls are formed through oxidative cleavage of protein backbones or by binding of aldehydic lipid oxidation products [75].
- Protocol: The most common detection method involves derivatization of the carbonyl group with 2,4-dinitrophenylhydrazine (DNPH), which forms a carbonyl-2,4-dinitrophenylhydrazone adduct [75].
- Detection: This adduct can be detected and quantified using:
Measurement of d-ROMs and BAP
The simultaneous measurement of diacron-reactive oxygen metabolites (d-ROMs) and biological antioxidant potential (BAP) provides a snapshot of oxidative stress and antioxidant capacity [5].
- d-ROMs Test: This test measures serum hydroperoxides. Under acidic conditions, iron is released from proteins and converts hydroperoxides to alkoxyl and peroxyl radicals. These radicals then oxidize an amine substrate (N,N-diethyl-p-phenylenediamine) to generate a pink chromogen, which is measured photometrically at 505 nm. Results are expressed in Carratelli Units (CARR U) [5] [77].
- BAP Test: This test assesses the ferric-reducing ability of the serum. The sample is added to a colored solution containing ferric chloride and a thiocyanate derivative. Antioxidants in the serum reduce the ferric ions to ferrous ions, causing decolorization. The extent of this change, measured at 505 nm, is proportional to the serum's antioxidant capacity and is expressed in μmol/L [5].
- Oxidative Stress Index (OSI): The OSI is calculated from the d-ROMs and BAP values using the formula: OSI = C × (d-ROMs/BAP), where C is a standardization coefficient [5].
Quantification of 8-Hydroxy-2'-Deoxyguanosine (8-OHdG)
As a marker of oxidative DNA damage, 8-OHdG is a guanine base modification caused by ROS [4].
- High-Performance Liquid Chromatography (HPLC): This is the gold-standard method.
- Separation: DNA is extracted from samples (e.g., blood cells, tissue) and enzymatically digested to deoxynucleosites.
- Detection: The digest is separated by HPLC and 8-OHdG is specifically detected using either electrochemical detection (HPLC-ECD) or tandem mass spectrometry (HPLC-MS/MS). These methods offer high sensitivity and specificity [4].
- Enzyme-Linked Immunosorbent Assay (ELISA):
- Protocol: Competitive or sandwich ELISA formats use antibodies specific for 8-OHdG. This is a cost-effective, high-throughput alternative to HPLC.
- Limitation: Potential for antibody cross-reactivity with other guanine derivatives necessitates careful validation [4].
Diagram 1: Generalized Workflow for Oxidative Stress Biomarker Analysis. This flowchart outlines the parallel assessment of oxidative damage and antioxidant defense, culminating in integrated data analysis.
Research Reagent Solutions and Essential Materials
Selecting the appropriate reagents and tools is fundamental for generating reliable and reproducible data in oxidative stress research.
Table 2: Essential Research Reagent Solutions for Oxidative Stress Analysis
| Reagent / Kit | Function / Application | Key Considerations |
|---|---|---|
| d-ROMs & BAP Kits (Diacron International) | Simultaneous measurement of oxidative metabolites (hydroperoxides) and total antioxidant capacity in serum on automated analyzers [5]. | Enables calculation of the Oxidative Stress Index (OSI). Standardized for clinical settings but requires specific instrumentation. |
| OxyBlot Kit | Sensitive immunodetection of protein carbonyls after derivatization with DNPH. Used for Western blot analysis [75]. | Provides specificity for protein oxidation. Semi-quantitative and useful for identifying specific carbonylated proteins. |
| 8-OHdG ELISA Kits | High-throughput quantification of oxidative DNA damage in urine, serum, or tissue extracts [4]. | Cost-effective but requires rigorous validation to ensure antibody specificity and avoid cross-reactivity. |
| Thiobarbituric Acid Reactive Substances (TBARS) Assay Kit | Colorimetric measurement of malondialdehyde (MDA) as a marker of lipid peroxidation [4]. | Well-established but known for non-specificity; measures other TBA-reactive compounds besides MDA. |
| Antibodies for AGEs (e.g., anti-CML) | Immunohistochemistry, immunoblot, and ELISA for detecting Advanced Glycation End-products [75]. | Polyclonal antibodies may have undefined specificity. Structural heterogeneity of AGEs complicates comprehensive detection. |
| Spectrofluorometric Reader | Non-invasive measurement of AGEs in skin based on autofluorescence properties [75]. | Must be standardized for body region, surrounding light, and skin conditions (e.g., tattoos). |
Signaling Pathways and Redox Biology in Disease
Oxidative stress is not merely a bystander but an active participant in disease pathogenesis through the disruption of key signaling pathways.
Diagram 2: Key Signaling Pathways Disrupted by Oxidative Stress. This diagram illustrates how an oxidative imbalance triggers pro-inflammatory responses, impairs antioxidant defenses, and causes endothelial dysfunction, collectively driving chronic disease progression [4] [78] [76].
Comparative Performance Data Across Chronic Diseases
The clinical utility of a biomarker is ultimately determined by its performance in specific disease contexts. The following table consolidates findings from recent clinical studies.
Table 3: Biomarker Performance Across Chronic Disease Contexts
| Disease Context | Key Biomarkers & Findings | Implications for Specificity/Sensitivity |
|---|---|---|
| Long COVID [5] | OSI: Positively correlated with inflammatory markers (CRP, fibrinogen). Optimal cut-off of 1.92 for identifying brain fog, especially in females. d-ROMs: Higher in females (579.8 vs 462.2 CARR U) and correlated with cortisol. | OSI shows prognostic potential for specific neurological symptoms. Highlights significant gender-dependent variations in oxidative stress. |
| Cardiovascular Disease (CVD) [76] | Oxidized LDL (ox-LDL): Key mediator, uptake via LOX-1 receptor drives foam cell formation. ROS: Inactivate nitric oxide (NO), forming peroxynitrite and causing endothelial dysfunction. | ox-LDL is a specific trigger for atherosclerosis. Markers of endothelial dysfunction are sensitive indicators of early CVD risk. |
| Hypertension & Diabetes [4] | MDA: Predicts endothelial dysfunction in hypertension. 8-OHdG: A surrogate marker for diabetic nephropathy. SOD/GPx: Diminished activity associated with β-cell failure and poor glycemic control. | MDA and 8-OHdG are sensitive to disease progression and complications. Antioxidant enzymes may have prognostic value for metabolic deterioration. |
| Almond Supplementation (Meta-analysis) [9] | Intervention: >60 g/day significantly reduced MDA (-0.46 WMD) and 8-OHdG (-5.83 WMD), while increasing SOD (2.02 WMD). Heterogeneity: I² = 92–96%. | Demonstrates the sensitivity of these biomarkers to dietary intervention. Extreme heterogeneity underscores reproducibility challenges across studies. |
Addressing the analytical limitations of oxidative stress biomarkers requires a multi-faceted approach. The future lies in developing and validating more specific markers (e.g., F2-isoprostanes over MDA), standardizing protocols across laboratories, and embracing technological advancements. These include high-throughput screening (HTS) systems, label-free live-cell imaging assays, and omics approaches (redox proteomics, transcriptomics) that provide a more comprehensive and personalized view of redox biology [79] [4]. For researchers in drug development, a rigorous, critical, and standardized approach to biomarker selection and validation is paramount for translating oxidative stress research into effective clinical therapies.
In the study of chronic diseases, oxidative stress markers have emerged as crucial indicators of pathophysiological processes. However, the accuracy and reproducibility of these measurements are critically dependent on the handling of biological samples before they ever reach the analyzer. Preanalytical variables—encompassing sample collection, processing, storage conditions, and freeze-thaw cycles—represent a significant source of variability that can compromise data integrity and translational potential [80] [81]. Research indicates that preanalytical factors account for the majority (55-77%) of laboratory errors in biomedical research, making their standardization particularly vital for oxidative stress biomarkers, which are often inherently labile [80] [82].
This guide provides a systematic comparison of how these preanalytical variables affect biomarker stability, with a specific focus on their implications for chronic disease research involving oxidative stress markers. We synthesize experimental data on diverse analytes—from traditional enzymes like paraoxonase-1 (PON-1) to novel microRNAs and protein biomarkers—to equip researchers with evidence-based protocols for maintaining sample integrity from collection to analysis.
Comparative Stability of Biomarkers Under Various Preanalytical Conditions
Effects of Storage Temperature on Biomarker Stability
The temperature at which samples are stored prior to analysis significantly impacts biomarker integrity, with different classes of biomarkers demonstrating varying stability profiles.
Table 1: Impact of Storage Temperature on Biomarker Stability
| Biomarker Category | Specific Analyte | Room Temperature (20-25°C) | Refrigerated (4°C) | Frozen (-20°C) | Ultra-Low (-80°C or below) | Primary Matrix | Citation |
|---|---|---|---|---|---|---|---|
| Oxidative Stress Enzyme | PON-1 Activity | Significant decrease after 48h (diagnostically irrelevant) | Significant decrease after 48h (diagnostically irrelevant) | Stable for short-term; significant fluctuations after 1 month | Not tested | Serum | [80] |
| Antioxidant Capacity | FRAP | Not stable >24h | Not stable >48h | Moderate stability for 1 month | Stable for 6 months | Serum | [83] |
| Protein Oxidation | AOPP | Not stable >24h | Not stable >48h | Moderate stability for 1 month | Stable for 6 months | Serum | [83] |
| Circulating microRNAs | miR-103a-3p, miR-191-5p, others | Stable up to 48h | Not tested | Stable with fluctuations | Stable for up to 17 years | Plasma | [84] |
| Myokine | Myostatin | Stable at RT | Not tested | Stable (≥4 freeze-thaw cycles) | Not tested | Serum | [82] |
| Immune Cell Markers | T cell subsets (CD56, CD57) | Not stable - require fresh analysis | Not stable - require fresh analysis | Notable alterations after long-term storage | Markers unstable after long-term storage | PBMCs | [85] |
The data reveal important patterns for chronic disease research. Oxidative stress enzymes like PON-1 show reasonable short-term stability but degrade with prolonged storage even at -20°C, suggesting that analysis should be conducted within weeks if samples are maintained at standard freezer temperatures [80]. For antioxidant capacity assays like FRAP and protein oxidation markers like AOPP, -80°C storage is clearly superior for studies extending beyond one month [83]. Conversely, circulating microRNAs demonstrate remarkable stability, maintaining integrity for up to 17 years at ultra-low temperatures, making them exceptionally suitable for retrospective chronic disease studies [84].
Effects of Freeze-Thaw Cycles on Biomarker Integrity
Repeated freezing and thawing of samples introduces mechanical and thermal stress that can degrade biomarkers. The sensitivity to these cycles varies considerably across biomarker types.
Table 2: Impact of Freeze-Thaw Cycles on Biomarker Integrity
| Biomarker Category | Specific Analyte | 1 Cycle | 2 Cycles | 3 Cycles | 4+ Cycles | Primary Matrix | Citation |
|---|---|---|---|---|---|---|---|
| Oxidative Stress Enzyme | PON-1 Activity | Affected (p<0.01) | Affected (p<0.01) | Affected (p<0.01) | Diagnostically significant (p<0.01) | Serum | [80] |
| Circulating microRNAs | miR-30c-5p | Minimal effect | Minimal effect | Minimal effect | Significant effect | Plasma | [84] |
| Circulating microRNAs | miR-103a-3p, miR-191-5p, others (most) | Minimal effect | Minimal effect | Minimal effect | Minimal effect | Plasma | [84] |
| Myokine | Myostatin | Minimal effect | Minimal effect | Minimal effect | Minimal effect | Serum | [82] |
| Optical Properties | Serum Autofluorescence | <1% variability | Not tested | Not tested | Not tested | Serum | [86] |
| SERS Signatures | Serum SERS Profile | 15% variability | Not tested | Not tested | Not tested | Serum | [86] |
Freeze-thaw stability shows striking biomarker-specific patterns. PON-1 activity is particularly sensitive to freeze-thaw cycles, showing statistically significant effects even after a single cycle and diagnostically relevant changes after four cycles [80]. This has profound implications for oxidative stress research, as repeated thawing would substantially compromise data quality. In contrast, most circulating microRNAs and myostatin demonstrate remarkable resilience to multiple freeze-thaw cycles, maintaining stability even after four cycles [84] [82]. For optical spectroscopy techniques, regular Raman spectroscopy shows minimal freeze-thaw effects (<1% variability), while surface-enhanced Raman spectroscopy (SERS) is more substantially influenced (15% variability) [86].
Experimental Protocols for Assessing Preanalytical Variables
Protocol for Evaluating Storage Temperature Effects
The following methodology, adapted from multiple studies, provides a standardized approach for determining optimal storage conditions for novel biomarkers [80] [83]:
Sample Preparation:
- Collect blood samples using standardized venipuncture techniques into appropriate collection tubes (e.g., serum clot activator tubes for serum, EDTA tubes for plasma).
- Allow complete clot formation (30 minutes at room temperature for serum samples).
- Centrifuge at 2,000-4,000 × g for 10-15 minutes at 4°C.
- Aliquot supernatant into sterile cryovials to avoid repeated freeze-thaw cycles of primary samples.
Storage Conditions and Timing:
- Analyze aliquots immediately after processing (T0) to establish baseline values.
- Store aliquots under the following conditions and analyze at specified timepoints:
- Room temperature (20-25°C): 24h, 48h, 120h
- Refrigerated (4°C): 24h, 48h, 120h
- Frozen (-20°C): 24h, 48h, 1 week, 1 month, 3 months
- Ultra-low (-80°C): 1 month, 2 months, 3 months, 6 months
- Before analysis, ensure frozen samples are properly thawed (typically on ice or at 4°C) and mixed gently.
Analysis and Interpretation:
- Measure biomarker levels using validated assays (e.g., spectrophotometric assays for enzymatic activities, ELISA for specific proteins, PCR for microRNAs).
- Compare results at each timepoint/temperature condition to baseline (T0) values using appropriate statistical tests (e.g., repeated measures ANOVA, paired t-tests).
- Apply desirable bias criteria to determine clinically or scientifically relevant changes beyond statistical significance [83].
Protocol for Assessing Freeze-Thaw Stability
This protocol evaluates the effect of repeated freezing and thawing on biomarker integrity [80] [84]:
Sample Processing:
- Process blood samples as described in section 3.1 to obtain serum or plasma.
- Aliquot into multiple cryovials to enable single-use for each freeze-thaw cycle assessment.
- Flash-freeze aliquots in a -80°C freezer or using liquid nitrogen before transfer to long-term storage at -80°C.
Freeze-Thaw Cycling:
- Cycle 1: Thaw one set of aliquots on ice or at 4°C, then analyze immediately.
- Subsequent Cycles: For remaining aliquots, after analysis, re-freeze samples at -80°C using standardized freezing conditions (e.g., controlled-rate freezer or Mr. Frosty device).
- Repeat the process for up to 4 cycles, analyzing a fresh set of aliquots at each cycle.
- Ensure consistent thawing conditions (temperature, duration) across all cycles.
Quality Control Measures:
- Include pool samples with known biomarker concentrations as controls.
- Monitor sample integrity indicators (e.g., hemoglobin for hemolysis, visual inspection for precipitates).
- Analyze all samples from the same subject in the same assay batch to minimize inter-assay variability.
Data Analysis:
- Express results as percentage of baseline (pre-freeze) values.
- Use statistical process control methods to determine acceptable limits of variation.
- Establish a freeze-thaw stability threshold based on analytical performance specifications or biological variation.
Research Reagent Solutions for Preanalytical Studies
Table 3: Essential Research Reagents and Equipment for Preanalytical Stability Studies
| Reagent/Equipment Category | Specific Examples | Function/Application | Considerations for Oxidative Stress Biomarkers |
|---|---|---|---|
| Blood Collection Tubes | Serum clot activator tubes (e.g., Greiner Bio-One), EDTA plasma tubes | Determines sample matrix | Heparin can interfere with PCR assays; serum vs. plasma yields different biomarker profiles |
| Cryogenic Storage Vials | Cryo.s cryovials (Greiner Bio-One), Eppendorf vials | Sample aliquoting and storage | Material composition affects sample adhesion; internal thread design prevents leakage |
| Cryoprotectants | Dimethyl sulfoxide (DMSO), Fetal Bovine Serum (FBS) | Cell viability preservation for PBMCs | DMSO concentration critical for cell integrity; not typically needed for serum/plasma biomarkers |
| Protein Stability Reagents | Protease inhibitor cocktails, phosphatase inhibitors | Prevent protein degradation | Essential for phosphoprotein analysis; may interfere with some enzymatic assays |
| Nucleic Acid Protectants | RNase inhibitors, DNA stabilizers | Preserve RNA/DNA integrity | Critical for microRNA studies; some can interfere with downstream PCR applications |
| Automated Analyzers | Cobas Integra 400 plus (Roche), Konelab 20i | High-throughput biomarker analysis | Standardized platforms enable cross-study comparisons; require method validation |
| Multiplex Assay Systems | ProcartaPlex Immunoassays (Thermo Fisher), Luminex xMAP | Simultaneous measurement of multiple biomarkers | Efficient for biomarker panels; potential cross-reactivity needs assessment |
| Specialized Spectroscopy | Raman spectroscopy, SERS, autofluorescence spectroscopy | Label-free biomarker detection | Minimal sample preparation; highly sensitive to preanalytical variations |
Implications for Chronic Disease Research on Oxidative Stress
The stability profiles of oxidative stress biomarkers have profound implications for research into chronic diseases such as cardiovascular disorders, diabetes, neurodegenerative conditions, and cancer.
Longitudinal and Retrospective Studies: The exceptional stability of circulating microRNAs at -80°C for up to 17 years makes them invaluable for long-term chronic disease studies and biobank-based research [84]. However, researchers must exercise caution with enzymatic oxidative stress markers like PON-1, which show significant fluctuations after just one month at -20°C, potentially confounding long-term storage studies [80].
Multi-Site Collaborations: The variable effects of freeze-thaw cycles across different biomarker classes necessitate standardized sample handling protocols in consortium research. While myokines and most microRNAs withstand multiple freeze-thaw cycles, PON-1 activity shows statistically significant alterations even after the first cycle, requiring strict limits on thawing protocols for certain analyte classes [80] [84] [82].
Novel Spectroscopy Approaches: For techniques like Raman spectroscopy and SERS, freeze-thaw cycles introduce measurable variability (15% for SERS), though disease-specific signatures still remain detectable [86]. This suggests that while preanalytical controls are essential, disease biomarkers can still be identified despite some sample processing variability.
The systematic comparison of preanalytical variables presented in this guide underscores the critical importance of standardized sample handling protocols in oxidative stress research. Key findings indicate that storage temperature and freeze-thaw cycles affect biomarker classes differently, necessitating analyte-specific handling procedures. Circulating microRNAs demonstrate exceptional stability under long-term storage conditions, making them particularly suitable for retrospective chronic disease studies, while traditional enzymatic biomarkers like PON-1 require more stringent controls and faster processing timelines.
For researchers investigating oxidative stress in chronic diseases, we recommend: (1) establishing biomarker-specific standard operating procedures based on stability data; (2) implementing centralized biobanking with consistent storage at -80°C for long-term preservation; and (3) rigorously limiting freeze-thaw cycles, particularly for labile biomarkers. Future methodological studies should focus on expanding stability data for emerging oxidative stress biomarkers and developing improved stabilization technologies to further enhance reproducible measurement in chronic disease research.
Oxidative stress, characterized by an imbalance between the production of reactive oxygen species (ROS) and the body's antioxidant defenses, is a common pathophysiological mechanism in a wide spectrum of chronic diseases [59] [87]. While individual biomarkers of oxidative damage provide valuable snapshots, they often fail to capture the systemic and multifaceted nature of redox dysregulation. This limitation has driven the development of composite scoring systems that integrate multiple biomarkers and lifestyle factors into unified indices [88] [89]. These integrated indices aim to provide a more holistic assessment of an individual's oxidative stress status, offering enhanced predictive value for disease risk stratification, progression monitoring, and therapeutic intervention evaluation in chronic diseases. This guide compares the performance, methodological frameworks, and applications of leading oxidative stress indices, providing researchers and drug development professionals with a structured analysis of available tools.
Comparative Analysis of Major Oxidative Stress Indices
The table below summarizes the components, scoring methodologies, and key performance metrics of three prominent approaches to oxidative stress assessment.
Table 1: Comparison of Integrated Oxidative Stress Indices
| Index Name | Core Components & Biomarkers | Scoring Methodology | Validation & Predictive Performance |
|---|---|---|---|
| Oxidative Balance Score (OBS) [88] | 16 Dietary Factors: Fiber, carotenoids, vitamins B/C/E, folate, calcium, magnesium, zinc, etc.4 Lifestyle Factors: Physical activity, alcohol intake, serum cotinine, BMI. | Sex-specific tertiles assigned scores 0-2. Antioxidants score 2 for highest intake; pro-oxidants score 2 for lowest exposure. Total score range: 0-40. | In overweight adults (n=28,377), higher OBS inversely associated with CKD risk (OR per unit: 0.975, 95% CI: 0.969–0.981). In machine learning models, achieved an AUC of 0.833 for CKD prediction [88]. |
| Traditional Biomarker Panels [53] [89] | Damage Markers: F2-isoprostanes (lipid peroxidation), 8-OHdG (DNA oxidation), protein carbonyls (protein oxidation).Antioxidant Enzymes: SOD, catalase, GPx activity. | Individual biomarkers measured via specialized assays (e.g., GC/MS for F2-isoprostanes, HPLC-ECD for 8-OHdG, DNPH assay for carbonyls). Often interpreted as a profile rather than a single score. | Strong correlations with disease progression in hypertension and diabetes. Specific predictive values depend on the disease context and biomarker combination [53]. |
| Clinical Oxidative Stress Panel (OxyCheck) [90] | 10-Point Panel: Zinc, Copper, Cu/Zn ratio, Selenium, Uric acid, hs-CRP, oxidized LDL, GPx, Glutathione reductase, Thiols. | Biomarker levels are input into a Support Vector Machine (SVM) model to classify patients into severity grades (e.g., asymptomatic, mild, severe). | In a COVID-19 cohort (n=28), the SVM model predicted clinical severity with 93% accuracy. Low Zn, low thiols, and high Cu/Zn ratio were key severity predictors [90]. |
Detailed Experimental Protocols for Index Development and Validation
Protocol for Oxidative Balance Score (OBS) Calculation and Validation
The OBS is developed through a multi-step process that integrates nutritional and lifestyle data.
- 1. Data Collection: Dietary intake is assessed using two 24-hour dietary recalls, and the average intake of nutrients is calculated [88]. Lifestyle factors like physical activity are determined using standardized MET scores, while smoking exposure is quantified via serum cotinine levels [88].
- 2. Scoring Assignment: Each of the 20 OBS components is categorized into sex-specific tertiles. For antioxidant components (e.g., dietary fiber, vitamins, physical activity), scores are assigned as 0 (lowest tertile), 1 (middle tertile), and 2 (highest tertile). For pro-oxidant components (e.g., total fat, iron, serum cotinine, BMI), the scoring is reversed: 2 for the lowest tertile and 0 for the highest [88].
- 3. Statistical Analysis: The association between the total OBS and disease outcomes (e.g., CKD) is evaluated using survey-weighted logistic regression models with multivariable adjustment for confounders like age, sex, and comorbidities [88].
- 4. Machine Learning Validation: Model performance can be enhanced by training algorithms like GLMBoost on the data and validating using techniques such as five-fold cross-validation. Model interpretability is achieved using SHapley Additive exPlanations (SHAP) analysis to identify the most influential predictors [88].
Protocol for Targeted Biomarker Assays (e.g., OxyCheck Panel)
Focused biomarker panels prioritize measurable analytes in biological fluids with clinical applicability.
- 1. Sample Collection and Pre-processing: Collect venous blood and separate plasma or serum. For certain biomarkers like thiols, pre-analytical stability is critical, and samples should be processed promptly [90].
- 2. Analytical Techniques:
- Trace Elements (Zn, Cu, Se): Typically measured using inductively coupled plasma mass spectrometry (ICP-MS) [90].
- Enzymatic Antioxidants (GPx, Glutathione Reductase): Activity is determined using kinetic assays that monitor the oxidation of NADPH at 340 nm [53].
- Oxidized LDL and hs-CRP: Quantified using commercial enzyme-linked immunosorbent assay (ELISA) kits [90].
- Thiols (Markers of redox status): Measured using colorimetric assays (e.g., Ellman's reagent) or HPLC [90].
- 3. Data Integration and Modeling: The measured levels of all biomarkers are compiled. A support vector machine (SVM) model is trained on this data, using the clinical severity grade of patients as the outcome variable. The model learns to classify new patients based on their biomarker profile [90].
Visualization of Signaling Pathways and Workflows
Key Signaling Pathways in Oxidative Stress
The following diagram illustrates the core cellular pathways involved in oxidative stress generation and the body's primary antioxidant defense response, which these composite indices aim to capture.
Cellular Oxidative Stress Pathways
Composite Index Development Workflow
This diagram outlines the general workflow for developing and validating a composite oxidative stress index, integrating elements from the OBS and OxyCheck methodologies.
Index Development Workflow
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key reagents, assays, and materials essential for researching and measuring components of integrated oxidative stress indices.
Table 2: Essential Research Reagents and Assays for Oxidative Stress Indices
| Item Name / Category | Function / Application | Representative Examples / Specifics |
|---|---|---|
| Dietary Assessment Tools | To quantify intake of pro- and antioxidant nutrients for scores like OBS. | Automated Self-Administered 24-hour Recall (ASA24), Food Frequency Questionnaires (FFQs), USDA Food and Nutrient Database [88]. |
| Biomarker Assay Kits | To measure specific oxidative damage markers and antioxidant levels in biofluids. | ELISA Kits: For 8-OHdG, MDA, Oxidized LDL, Protein Carbonyls, hs-CRP.Activity Assay Kits: For SOD, Catalase, Glutathione Peroxidase (GPx) [53] [90]. |
| Chromatography-Mass Spectrometry | Gold-standard quantification for specific oxidative stress biomarkers. | Gas Chromatography-Mass Spectrometry (GC-MS): For F2-isoprostanes.Liquid Chromatography-MS (LC-MS): For 8-OHdG, metabolomics profiling [53]. |
| Spectrophotometry / Plate Readers | To measure the absorbance in colorimetric and kinetic enzyme activity assays. | UV-Vis Microplate Readers for high-throughput analysis of assays for thiols, total antioxidant capacity, and enzyme activities like GPx [53] [90]. |
| Clinical Chemistry Analyzers | To measure routine clinical biomarkers that contribute to composite scores. | Automated analyzers for measuring trace elements (Zn, Cu, Se), uric acid, and standard lipid profiles [90]. |
| Machine Learning & Statistical Software | To develop predictive models, calculate scores, and perform SHAP analysis for interpretability. | R, Python (with scikit-learn, SHAP libraries), SAS, SPSS for logistic regression, SVM modeling, and cross-validation [88] [90]. |
Oxidative stress, characterized by an imbalance between reactive oxygen species (ROS) production and antioxidant defenses, represents a fundamental pathophysiological mechanism across numerous chronic diseases [78] [87]. The accurate measurement of oxidative stress biomarkers provides critical insights into disease mechanisms, progression, and therapeutic responses. However, the interpretation of these biomarkers is complicated by numerous confounding factors and medication influences that can significantly alter their levels and clinical significance [4] [91]. This complex interplay necessitates sophisticated contextual interpretation frameworks for researchers and drug development professionals working with these biomarkers across different disease states.
The clinical and research landscape of oxidative stress biomarkers has evolved substantially, with biomarkers now categorized by their specific molecular targets: lipid peroxidation products (MDA, F2-isoprostanes), protein oxidation markers (carbonyl groups), DNA damage indicators (8-OHdG), and antioxidant enzymes (SOD, GPx, catalase) [4] [9]. Each category offers distinct insights into oxidative damage pathways, yet each is susceptible to different confounding influences. This review systematically examines these confounding factors across major chronic disease domains, presents standardized methodological approaches for biomarker assessment, and provides visual frameworks for interpreting results within appropriate context.
Comparative Analysis of Oxidative Stress Biomarkers Across Chronic Diseases
Biomarker Profiles in Cardiovascular and Metabolic Diseases
In cardiovascular and metabolic diseases, specific oxidative stress biomarkers demonstrate consistent patterns across hypertension (HTN) and diabetes mellitus (DM). Research has established that malondialdehyde (MDA), 8-hydroxy-2'-deoxyguanosine (8-OHdG), and F2-isoprostanes show significant elevations in these conditions and correlate with disease progression and end-organ complications [4]. The NADPH oxidase (NOX) family and mitochondrial dysfunction serve as primary ROS sources in HTN, contributing to endothelial impairment and vascular remodeling, while DM features hyperglycemia-induced ROS production through AGE-RAGE signaling, PKC activation, and the polyol pathway [4].
Table 1: Oxidative Stress Biomarkers in Cardiovascular and Metabolic Disorders
| Biomarker | Hypertension | Diabetes Mellitus | Primary Confounding Factors |
|---|---|---|---|
| Malondialdehyde (MDA) | Predicts endothelial dysfunction; correlates with BP severity | Associated with insulin resistance and β-cell dysfunction | Lifestyle factors (diet, smoking); renal function; antioxidant supplementation |
| 8-OHdG | Moderate elevation; marker of oxidative DNA damage | Strong correlation with nephropathy progression; diabetic complications | Age; renal clearance; smoking status; metabolic rate |
| F2-isoprostanes | Gold standard for lipid peroxidation; correlates with vascular dysfunction | Elevated in uncontrolled DM; indicates lipid peroxidation rate | Sample processing (ex vivo oxidation); NSAIDs; lipid-lowering agents |
| Superoxide Dismutase (SOD) | Reduced activity in resistant HTN | Diminished in β-cell failure | Antioxidant supplementation; inflammatory status; genetic polymorphisms |
| Glutathione Peroxidase (GPx) | Variable changes based on HTN duration and therapy | Decreased activity correlating with glycemic control | Selenium status; renal function; metal chelators |
Clinical evidence confirms that plasma MDA strongly predicts endothelial dysfunction in HTN, while urinary 8-OHdG serves as a reliable surrogate for diabetic nephropathy progression [4]. Conversely, diminished antioxidant capacity (particularly reduced SOD and GPx activities) associates with β-cell failure and poor glycemic control in DM [4]. These biomarkers are particularly vulnerable to confounding by renal function, concurrent inflammation, and lifestyle factors including diet and physical activity patterns.
Biomarker Patterns in Neurological and Inflammatory Conditions
Neurological and inflammatory disorders demonstrate distinct oxidative stress profiles that require careful interpretation. In medication overuse headache (MOH), patients exhibit significantly elevated composite ratios including monocyte to HDL ratio (MHR), lymphocyte to HDL ratio (LHR), and neutrophil to HDL ratio (NHR) compared to healthy controls [7]. These peripheral markers reflect the low-grade systemic inflammatory and oxidative state characteristic of MOH pathogenesis, with odds ratios of 2.32, 2.56, and 2.09, respectively, for independent association with MOH [7].
Table 2: Oxidative Stress Biomarkers in Neurological and Inflammatory Disorders
| Biomarker | Medication Overuse Headache | Inflammatory Bowel Disease | Primary Medication Interferences |
|---|---|---|---|
| MHR/LHR/NHR | Significantly elevated; independent risk markers | Not typically used in IBD assessment | Statins; NSAIDs; immunomodulators |
| Malondialdehyde (MDA) | Limited data | Significantly elevated in active disease; differentiates active vs inactive CD | Aminosalicylates; corticosteroids; biologics |
| Paraoxonase 1 (PON1) | Not reported | Reduced in active UC and CD; indicates antioxidant deficit | Statins; NSAIDs; antioxidant supplements |
| Albumin | Not a primary marker | Decreased in active disease; indicates protein oxidation/consumption | Immunosuppressants; biologics; nutritional status |
| Free Thiols | Investigated in limited studies | Reduced in active UC; indicates redox status | Antioxidant supplements; anti-inflammatory drugs |
In inflammatory bowel disease (IBD), meta-analyses reveal significant alterations in oxidative stress profiles, with active disease showing increased malondialdehyde (MDA) alongside reduced paraoxonase 1 (PON1), catalase, albumin, transferrin, and total antioxidant capacity compared to inactive disease [6]. These biomarkers demonstrate particular value in differentiating between active and inactive states, with MDA, PON1, catalase, albumin, transferrin, and total antioxidant capacity serving as reliable indicators for Crohn's disease flares, while PON1, glutathione peroxidase, catalase, albumin, transferrin, and free thiols indicate ulcerative colitis exacerbations [6]. Importantly, even during disease inactivity, oxidative stress biomarkers remain dysregulated compared to healthy controls, suggesting persistent redox imbalance [6].
Chronic Obstructive Pulmonary Disease Biomarkers
In chronic obstructive pulmonary disease (COPD), integrated bioinformatics approaches have identified five core oxidative stress-associated genes: HSPA1A, GCLM, IL-1β, ICAM1, and GCLC [92]. These biomarkers form the foundation of a diagnostic model with exceptional discriminatory power (AUC of 0.981) and reflect the intricate connection between oxidative stress and immune responses in COPD pathogenesis [92]. The identification of these genetic markers highlights the potential for targeted biomarker approaches in specific disease contexts while introducing confounding factors related to genetic polymorphisms and expression regulation.
Methodological Considerations for Biomarker Assessment
Standardized Analytical Protocols
The accurate measurement of oxidative stress biomarkers requires rigorous methodological standardization to minimize technical variability and pre-analytical confounding:
Lipid Peroxidation Assessment: Malondialdehyde (MDA) is most accurately quantified via the Thiobarbituric Acid-Reactive Substances (TBARS) assay with HPLC detection, while F2-isoprostanes represent the gold standard and require gas or liquid chromatography-mass spectrometry (HPLC/MS-MS) for optimal specificity [4]. Sample processing must minimize ex vivo oxidation through the addition of antioxidants (butylated hydroxytoluene) and maintenance of anaerobic conditions during storage.
Protein Oxidation Measurement: Protein carbonyl groups serve as reliable biomarkers of protein oxidation, typically detected through derivatization with 2,4-dinitrophenylhydrazine (DNPH) followed by spectrophotometric quantification at 370-375 nm [4]. Alternative approaches include immunoblotting with anti-DNP antibodies and ELISA-based methods for higher throughput applications.
DNA Damage Quantification: 8-hydroxy-2'-deoxyguanosine (8-OHdG) measurement as a DNA oxidation biomarker optimally employs high-performance liquid chromatography (HPLC) coupled with electrochemical or mass spectrometry detection (HPLC-ECD or HPLC-MS/MS) [4]. While ELISA kits offer cost-effective high-throughput alternatives, they require careful validation to address potential antibody cross-reactivity issues.
Advanced Direct Detection Methods: Electron Paramagnetic Resonance (EPR) Spectroscopy enables direct detection and quantification of ROS in biological tissues through spin trapping techniques [4]. This method has identified elevated superoxide anion (O₂•â») in glomeruli and tubules of diabetic rodents correlating with albuminuria, and quantifies vascular ROS (e.g., peroxynitrite) in resistant hypertension models using NOX-specific probes [4].
Integrated Workflow for Oxidative Stress Biomarker Analysis
The following workflow diagram illustrates a standardized approach for oxidative stress biomarker analysis that incorporates confounding factor assessment:
Major Confounding Factors in Oxidative Stress Biomarker Interpretation
Medication Influences on Biomarker Levels
Medications significantly impact oxidative stress biomarker levels through both therapeutic and off-target effects, creating substantial interpretation challenges:
Antihypertensive and Metabolic Medications: Angiotensin-converting enzyme inhibitors and angiotensin receptor blockers demonstrate direct antioxidant properties by reducing NADPH oxidase activity, potentially lowering MDA and F2-isoprostane levels independently of blood pressure effects [4]. Statins similarly exhibit pleiotropic antioxidant effects beyond lipid lowering, while metformin reduces mitochondrial ROS production in diabetes, confounding the relationship between biomarker levels and underlying disease activity [4].
Analgesics and Anti-inflammatory Drugs: In medication overuse headache, the primary medications of interest (NSAIDs, triptans, combination products) directly influence oxidative stress pathways, creating a complex feedback loop where treatment contributes to the pathological mechanism [7]. Studies indicate that treatment with onabotulinumtoxinA or targeted antibodies against calcitonin gene-related peptide over six-month periods improves plasma levels of oxidative stress biomarkers, further demonstrating the medication confounding effect [7].
IBD Therapeutics: Aminosalicylates, corticosteroids, and biologics used in IBD management directly modulate oxidative stress pathways, potentially normalizing biomarker levels independently of underlying inflammatory activity [6]. This creates particular challenges for differentiating treatment effects from genuine disease remission in clinical trials and practice.
Lifestyle and Environmental Confounders
Lifestyle factors introduce substantial variability in oxidative stress biomarker measurements, requiring careful documentation and statistical adjustment:
Dietary Influences: Intervention studies demonstrate that almond supplementation (>60 g/day) significantly reduces MDA (WMD = -0.46, p = 0.002), 8-OHdG (WMD = -5.83, p < 0.001), and uric acid (WMD = -0.64, p = 0.009) while increasing SOD activity (WMD = 2.02, p = 0.008) [9]. The Mediterranean and DASH diets similarly reduce lipid peroxidation products and enhance antioxidant enzymes, potentially masking underlying disease-related oxidative stress [4].
Smoking and Environmental Exposures: Cigarette smoke introduces both superoxide (O₂•â») and nitric oxide (NO•), directly elevating free radical levels and confounding disease-specific biomarker measurements [78]. Ozone exposure triggers lipid oxidation and promotes neutrophil infiltration, while heavy metals (iron, copper, cadmium, mercury) catalyze lipid peroxidation and interact with proteins and DNA [78].
Biological and Demographic Variables
Intrinsic factors significantly influence oxidative stress biomarker baselines and must be incorporated into interpretive frameworks:
Renal Function Impact: The kidneys play a crucial role in clearing oxidized molecules and maintaining redox balance, with renal dysfunction leading to accumulated MDA, protein carbonyls, and advanced oxidation protein products independent of primary disease processes [91]. Studies confirm inverse correlations between eGFR and oxidative stress markers even in early-stage kidney impairment [91].
Age and Sex Considerations: Aging associates with progressive decline in antioxidant capacity and increased ROS production, while sex differences influence both baseline oxidative stress levels and responses to interventions [89]. These variables necessitate age- and sex-matched control groups in clinical studies and appropriate reference ranges for clinical interpretation.
Molecular Pathways of Oxidative Stress and Therapeutic Targets
The NRF2-Keap1 and NF-κB pathways represent central regulatory mechanisms in oxidative stress response and inflammation, serving as both biomarkers and therapeutic targets:
Research Reagent Solutions for Oxidative Stress Studies
Table 3: Essential Research Reagents for Oxidative Stress Biomarker Analysis
| Reagent Category | Specific Examples | Research Application | Technical Considerations |
|---|---|---|---|
| Lipid Peroxidation Assays | Thiobarbituric Acid Reactive Substances (TBARS) assay; F2-isoprostanes ELISA kits; Lipid hydroperoxide probes | Quantification of oxidative damage to cellular membranes and lipoproteins | Sample matrix effects; standardization against HPLC-MS; antioxidant preservation during processing |
| Protein Oxidation Detection | OxyBlot Protein Oxidation Detection Kit; Anti-nitrotyrosine antibodies; Protein carbonyl ELISA kits | Detection of protein carbonylation, nitration, and chlorination | Specificity validation; reduction of artifactual oxidation; normalization to total protein |
| DNA Damage Assessment | 8-OHdG ELISA kits; Comet assay reagents; Anti-8-OHdG antibodies | Measurement of oxidative DNA damage and repair capacity | Cross-reactivity concerns; nuclear extraction efficiency; cell viability considerations |
| Antioxidant Capacity Assays | Total Antioxidant Capacity (TAC) kits; CUPRAC; FRAP; ORAC assays | Global assessment of antioxidant defense systems | Standardization across methods; biological relevance interpretation; substrate specificity |
| ROS Detection Probes | DCFH-DA; Dihydroethidium; MitoSOX Red; Amplex Red | Cellular ROS production measurement; mitochondrial superoxide detection | Probe specificity; cellular uptake variability; calibration with positive controls |
| Enzyme Activity Assays | Superoxide dismutase activity kits; Glutathione peroxidase assays; Catalase activity tests | Functional assessment of antioxidant enzymes | Tissue/cell lysate preparation; cofactor requirements; interference from other enzymes |
| NRF2 Pathway Tools | NRF2 activation ELISA; ARE-luciferase reporter constructs; NRF2 siRNA | Investigation of antioxidant response pathway modulation | Cell type-specific responses; kinetic considerations; pathway crosstalk |
The accurate interpretation of oxidative stress biomarkers across chronic diseases requires sophisticated frameworks that systematically account for confounding factors and medication influences. The evidence reviewed demonstrates that consistent patterns emerge across disease states, with specific biomarkers showing particular susceptibility to different types of confounding. Future research directions should prioritize the development of integrated assessment panels that combine multiple biomarker classes with comprehensive confounding factor documentation, enabling more accurate disease-specific interpretations. Additionally, technological advances in targeted antioxidant therapies and personalized redox medicine approaches hold promise for more specific interventions with reduced confounding effects. As the field progresses, standardized methodological protocols and contextual interpretation frameworks will be essential for advancing our understanding of oxidative stress mechanisms across the spectrum of chronic diseases and translating this knowledge into improved clinical outcomes.
The translation of basic scientific discoveries into clinical practice represents a critical pathway for improving patient outcomes, particularly in the field of oxidative stress research. Despite revolutionary advances in biomedicine, significant barriers continue to impede the effective implementation of research findings into routine clinical care. This review examines the multifaceted challenges in translational research, with a specific focus on oxidative stress biomarkers across chronic diseases. We analyze the "valley of death" between preclinical discovery and clinical application, highlighting methodological, regulatory, and cultural obstacles. Through a systematic comparison of oxidative stress biomarkers and their experimental validation, we provide frameworks for enhancing translational efficiency. The integration of innovative technologies, streamlined regulatory processes, and multidisciplinary collaboration emerges as essential for bridging the current translational gap and delivering oxidative stress-based diagnostics and therapeutics to patients.
Translational research describes the critical continuum wherein basic science discoveries are utilized to prevent or treat human disease, embodying an iterative "bench to bedside and back to bench" approach [93]. This process has been formally conceptualized in phases: T1 (basic science to clinical science), T2 (clinical science to clinical practice), and T3 (clinical practice to widespread health improvements) [93]. Despite significant investments in biomedical research, the translation of findings into therapeutic advances has been far slower than anticipated, with a concerning gap between scientific discovery and clinical application known as the "valley of death" [94].
In oxidative stress research, this translational gap is particularly pronounced. While oxidative stress constitutes a crucial mechanism in the onset and progression of various chronic inflammatory diseases, including cardiovascular diseases, neurodegenerative diseases, diabetes, and cancer [39] [95], the implementation of this knowledge into clinical practice remains limited. The growing understanding of redox dynamics and biological disease mechanisms has led to the development of specific, sensitive instruments for measuring oxidative stress in different biological materials [39]. Many of these biomarkers have been proposed as effective tools for monitoring different diseases and evaluating treatment effectiveness [39] [51], yet their routine clinical adoption faces substantial barriers.
This review examines the challenges in translating oxidative stress research into clinical practice, with particular emphasis on biomarker validation, methodological standardization, and regulatory hurdles. By comparing oxidative stress markers across chronic diseases and providing detailed experimental frameworks, we aim to identify strategic opportunities for enhancing translational efficiency in this critical field of biomedical research.
The Translational "Valley of Death": Systemic Barriers
Cultural and Disciplinary Divides
The translational pathway is frequently impeded by fundamental cultural differences between basic scientists and clinicians. These divisions stem from lack of communication, differences in education and training, and divergent goals and reward mechanisms [93]. Basic scientists often prioritize mechanistic insights and publication in high-impact journals, while clinicians focus on patient outcomes and practical applications. This cultural schism is exacerbated by current academic promotion systems that heavily weight individual research output such as high-impact publications, grants, and invited lectures, rather than valuing contributions to team-based translational projects [93].
Regulatory Complexity
The translational process is increasingly encumbered by complex regulatory requirements encompassing ethics approval for human research, tissue banking and material transfer regulations, intellectual property rights, toxicology and manufacturing regulations, FDA approvals, study sponsorship and insurance, as well as trial and data monitoring [93]. These regulatory hurdles are becoming even more complex with expanding work in fields like cell and gene therapies. Streamlining initiatives such as the Integrated Research Application System (IRAS) in the UK and the establishment of the National Center for Advancing Translational Sciences (NCATS) in the USA represent important steps toward reducing this regulatory burden [93].
Resource Limitations and Infrastructural Deficits
Translational research faces significant resource constraints, including lack of trained interdisciplinary staff to support investigations throughout the research cycle, limited protected research time for clinicians, and insufficient access to shared resources [93]. The shortage of investigators with translational expertise is compounded by poorly defined research-based career paths and inadequate mentoring programs. This resource limitation extends to oxidative stress research, where sophisticated analytical equipment and specialized technical expertise are often required for biomarker validation [39].
Preclinical Model Limitations
A critical barrier in translational research, particularly relevant to oxidative stress studies, is the limited predictive utility of animal models for human disease [94]. Despite their usefulness for understanding disease pathobiology and drug mechanisms, targets and therapies developed in animal models frequently fail in human studies. This problem is exemplified in oxidative stress research, where animal models may not fully recapitulate the complex redox dynamics of human chronic diseases [95] [96]. The traditional method of identifying pathways in vitro, followed by generating experimental animal models of human disease in vivo, has proven insufficient for reliable translation to human applications [94].
Table 1: Key Barriers in Translational Oxidative Stress Research
| Barrier Category | Specific Challenges | Impact on Translation |
|---|---|---|
| Cultural & Educational | Divergent reward systems between basic and clinical researchers; Limited cross-disciplinary training | Reduces collaborative efficiency; impedes knowledge exchange |
| Methodological | Limited predictivity of animal models; Lack of standardized biomarker assays | High attrition rates in clinical development; Irreproducible findings |
| Regulatory | Complex approval pathways; Evolving requirements for biomarkers | Increased time and cost; Delayed implementation |
| Resource & Infrastructure | Limited funding for validation studies; Lack of shared core facilities | Incomplete biomarker validation; Restricted access to specialized technologies |
| Workforce Development | Shortage of translational researchers; Inadequate mentoring programs | Reduced pipeline of skilled investigators; Limited knowledge transfer |
Oxidative Stress Biomarkers: Comparative Analysis Across Chronic Diseases
Biomarker Classification and Measurement Approaches
Oxidative stress biomarkers can be broadly categorized by the type of molecular damage they detect: lipid peroxidation products, protein modifications, DNA/RNA oxidation markers, and alterations in antioxidant defense systems [39] [51]. The measurement of these biomarkers employs diverse methodological approaches, each with specific advantages and limitations for clinical translation.
Lipid peroxidation represents a major consequence of oxidative stress, generating various bioactive species that can serve as biomarkers. Malondialdehyde (MDA) is frequently measured using thiobarbituric acid-reactive substances (TBARS) assays or more specific chromatographic methods [39] [97]. Lipid hydroperoxides (LOOH), including specific types such as triglyceride hydroperoxide (TGOOH) and phosphatidylcholine hydroperoxide (PCOOH), have been identified as sensitive markers in conditions like chronic kidney disease and non-alcoholic steatohepatitis [39]. These can be detected using techniques such as liquid chromatography-mass spectrometry (LC-MS), providing molecular specificity [39].
Protein oxidation markers include advanced oxidation protein products (AOPP), protein carbonyls, and specific modifications like cysteine thiol oxidation [39] [97]. In Duchenne muscular dystrophy research, plasma Cys34 albumin thiol oxidation has been identified as a useful blood biomarker of oxidative stress that more closely reflects changes in dystrophic muscle than the commonly used protein carbonylation [39].
Nucleic acid oxidation is frequently assessed through markers like 8-hydroxy-2'-deoxyguanosine (8-OHdG) for DNA oxidation and 5-hydroxymethyl-2'-deoxyuridine (HMdU) [32]. These markers can be measured using techniques such as enzyme-linked immunosorbent assay (ELISA), gas chromatography/mass spectrometry (GC/MS), or liquid chromatography with electrochemical detection [32].
Table 2: Oxidative Stress Biomarkers Across Chronic Diseases
| Disease Category | Specific Conditions | Key Biomarkers | Detection Methods | Clinical Utility |
|---|---|---|---|---|
| Cardiovascular Diseases | Atherosclerosis, Hypertension, IRI | MDA, AOPP, NO metabolites, LOOH | LC-MS, HPLC, ELISA | Risk stratification; Treatment monitoring |
| Neurodegenerative Diseases | Alzheimer's Disease, HIE | 8-OHdG, Protein carbonylation, MDA | 1H-NMR, HPLC-MS/MS | Early diagnosis; Disease progression |
| Renal Diseases | Chronic Kidney Disease | TGOOH, PCOOH, MDA | NanoESI-MS, LC-MS | Diagnostic biomarkers; Disease monitoring |
| Metabolic Diseases | NASH, Diabetes, Obesity | MDA, LOOH, AOPP, AGE products | LC/MS, Colorimetric assays | Assessment of oxidative damage extent |
| Genetic Disorders | CCHS, DMD | Urinary MDA, Cys34 albumin oxidation | HPLC-MS/MS, Immunoassays | Patient stratification; Therapy evaluation |
Disease-Specific Biomarker Profiles
Different disease states exhibit characteristic patterns of oxidative stress biomarkers, reflecting their distinct pathophysiological mechanisms. In cardiovascular diseases, endothelial dysfunction is characterized by reduced nitric oxide (NO) production and increased oxidative stress, with key contributors including superoxide (O₂•â») and hydrogen peroxide (Hâ‚‚Oâ‚‚) [98] [96]. These reactive species can be measured directly or through their reaction products, providing insights into vascular oxidative stress status.
Neurodegenerative conditions such as Alzheimer's disease demonstrate distinctive cerebrovascular alterations associated with oxidative stress [96] [99]. The brain's high metabolic demand and rich lipid content make it particularly vulnerable to oxidative damage, with markers like 8-OHdG, protein carbonyls, and lipid peroxidation products elevated in patients [96]. Recent research has highlighted the role of oxidative stress in blood-brain barrier dysfunction through redistribution of tight junction proteins like claudin-5 and occludin [96].
Metabolic diseases including non-alcoholic steatohepatitis (NASH) and diabetes exhibit pronounced lipid dysregulation and peroxidation [39] [97]. Comprehensive lipidomic analyses covering both intact lipids and lipid hydroperoxides in tissues using liquid chromatography-mass spectrometry have revealed the crucial role of oxidative stress in lipid dysregulation at the molecular level [39]. In obesity, studies have shown a shift in total antioxidant status toward oxidation, with increased lipid and protein oxidation, glycation, and nitration [97].
Methodological Considerations in Biomarker Assessment
The accurate measurement of oxidative stress biomarkers requires careful methodological consideration. Pre-analytical factors including sample collection, processing, and storage can significantly impact biomarker stability [32] [51]. For example, markers like malondialdehyde can be affected by sample hemolysis or prolonged storage, while protein carbonyls require specific processing to prevent artificial oxidation.
Analytical considerations include the specificity and sensitivity of detection methods. While colorimetric assays like TBARS for MDA detection offer practicality for high-throughput analysis, they may lack specificity compared to chromatographic methods [32]. Advanced techniques such as nanoelectrospray ionization-mass spectrometry (nanoESI-MS) provide detailed lipidomic profiling but require specialized equipment and expertise [39].
The selection of appropriate biological matrices is another critical consideration. Oxidative stress biomarkers can be measured in blood (plasma, serum), urine, exhaled breath condensate, or specific tissues [39] [51]. Urinary biomarkers offer non-invasive collection advantages, while blood biomarkers may provide more immediate information about systemic oxidative status. Recent research has demonstrated the utility of dried blood spots (DBS) for measuring markers like MDA and C-reactive protein, facilitating sample collection and storage in large epidemiological studies [39].
Experimental Approaches and Research Reagents
Standardized Methodologies for Oxidative Stress Assessment
Reliable measurement of oxidative stress biomarkers requires standardized experimental protocols with appropriate controls and quality assurance measures. For lipid peroxidation assessment, the thiobarbituric acid-reactive substances (TBARS) assay represents a widely used method, though it requires careful optimization to improve specificity [32]. More advanced approaches utilize liquid chromatography with mass spectrometric detection to identify specific lipid hydroperoxide species [39].
Protein oxidation analysis often involves detection of protein carbonyl groups through derivatization with 2,4-dinitrophenylhydrazine (DNPH) followed by spectrophotometric, HPLC, or immunoassay detection [32] [97]. Advanced proteomic approaches enable identification of specific oxidized proteins and modification sites, providing deeper insights into oxidative damage mechanisms.
DNA oxidation measurement typically focuses on 8-OHdG detection using techniques such as ELISA, GC/MS, or LC with electrochemical detection [32]. Each method offers different balances of sensitivity, specificity, and throughput, with LC-ECD generally providing the most specific quantification.
Antioxidant status assessment employs various approaches including total antioxidant capacity assays like the oxygen radical absorbance capacity (ORAC) assay, ferric reducing antioxidant power (FRAP) assay, and total peroxyl radical-trapping antioxidant parameter (TRAP) assay [32]. Additionally, specific antioxidant enzymes including superoxide dismutase (SOD), glutathione peroxidase (GPx), and catalase can be measured using activity-based assays [97].
Research Reagent Solutions
Table 3: Essential Research Reagents for Oxidative Stress Analysis
| Reagent Category | Specific Examples | Application & Function | Technical Considerations |
|---|---|---|---|
| Detection Assays | TBARS Assay Kit, Protein Carbonyl ELISA, 8-OHdG ELISA | Quantification of specific oxidative damage markers | Standardize against reference materials; validate cross-reactivity |
| Antibody-Based Reagents | Anti-DNP, Anti-Nitrotyrosine, Anti-HNE | Detection of specific protein modifications | Optimize dilution and blocking conditions; confirm specificity |
| Chromatography Standards | 8-iso-PGF2α, MDA, 8-OHdG authentic standards | Quantification by LC-MS/GC-MS | Use stable isotope-labeled internal standards for precise quantification |
| Fluorescent Probes | DCFH-DA, DHE, MitoSOX | Cellular ROS detection by flow cytometry/fluorescence | Optimize concentration and loading time; validate specificity |
| Enzyme Activity Assays | SOD, GPx, Catalase activity kits | Antioxidant enzyme function assessment | Control for sample hemolysis; normalize to protein content |
| Redox Sensors | roGFP, HyPer | Dynamic redox monitoring in live cells | Calibrate for pH sensitivity; confirm compartment-specific expression |
Visualizing Oxidative Stress Pathways and Workflows
Oxidative Stress Signaling in Endothelial Dysfunction
Figure 1: Oxidative Stress Pathways in Endothelial Dysfunction
Biomarker Validation Workflow
Figure 2: Biomarker Validation and Implementation Workflow
Strategies for Overcoming Translational Barriers
Fostering Multidisciplinary Collaboration
Successful translation of oxidative stress research requires integrated multidisciplinary teams spanning basic science, clinical research, bioinformatics, and regulatory affairs [93]. The establishment of academic centers specifically focused on translational research, such as the Clinical and Translational Science Awards (CTSA) consortium in the United States, provides infrastructure to support these collaborative efforts [93]. These centers facilitate the formation of interdisciplinary research teams with complementary expertise, enhancing the potential for successful translation.
Mentorship represents another critical component for developing the next generation of translational researchers. Programs such as the Academy of Medical Sciences mentoring scheme in the UK offer one-to-one mentoring for early career clinician-scientists by leading scientists in their fields [93]. Effective mentorship helps bridge cultural and methodological divides between basic and clinical researchers, facilitating knowledge transfer and skill development.
Enhancing Preclinical Predictivity
Improving the predictivity of preclinical models is essential for enhancing translational success in oxidative stress research. This includes utilizing more complex disease models that better recapitulate human pathophysiology, such as humanized animal models, three-dimensional tissue cultures, and organs-on-chips [94]. Incorporating multiple species in preclinical testing can also improve the predictivity of findings for human applications.
Rigorous experimental design in preclinical studies is equally important. This includes appropriate sample size calculations, randomization, blinding, and comprehensive reporting following guidelines such as ARRIVE [94]. Additionally, incorporating pharmacokinetic and pharmacodynamic assessments in preclinical studies provides valuable data for designing human trials.
Streamlining Regulatory Processes
Regulatory agencies have implemented various initiatives to streamline the approval process for new diagnostics and therapeutics. The FDA's Biomarkers, EndpointS, and other Tools (BEST) resource provides a common terminology for biomarker classification, facilitating regulatory review [93]. Similarly, the Integrated Research Application System (IRAS) in the UK captures information required for multiple review bodies through a single online system, reducing administrative burden [93].
Engaging regulatory agencies early in the development process through mechanisms like the FDA's Pre-Submission Program can identify potential issues before significant resources are invested. These early interactions provide valuable guidance on validation requirements and study designs likely to support regulatory approval.
Leveraging Technological Innovations
Advanced technologies offer significant opportunities for enhancing translational efficiency in oxidative stress research. High-throughput omics technologies (genomics, proteomics, metabolomics, lipidomics) enable comprehensive molecular profiling, facilitating biomarker discovery and validation [39] [99]. These approaches can identify biomarker signatures with improved diagnostic and prognostic performance compared to single biomarkers.
Microsampling techniques such as dried blood spots enable simplified sample collection, storage, and transport, facilitating larger and more diverse clinical studies [39]. When combined with sensitive analytical methods like LC-MS/MS, these approaches support the validation of oxidative stress biomarkers in real-world settings.
Biosensor technologies represent another promising approach for oxidative stress biomarker monitoring. These devices can provide continuous, real-time measurement of oxidative stress parameters, enabling dynamic assessment of disease states and treatment responses [98].
The translation of oxidative stress research into clinical practice faces significant barriers, but strategic approaches can enhance translational efficiency. The integration of multidisciplinary teams, improved preclinical models, streamlined regulatory processes, and technological innovations represents promising pathways for bridging the current translational gap. As oxidative stress continues to be recognized as a fundamental mechanism in diverse chronic diseases, overcoming these translational barriers becomes increasingly imperative for improving patient care.
Future directions in translational oxidative stress research will likely include the development of standardized biomarker panels validated across multiple diseases, the implementation of point-of-care testing devices for oxidative stress parameters, and the integration of oxidative stress biomarkers into clinical decision-support systems. Additionally, the growing understanding of redox signaling complexity suggests that future therapeutic approaches may need to target specific oxidative modifications rather than globally reducing oxidative stress.
The continuing challenges of translational research in oxidative stress reflect broader issues in biomedical research translation. By addressing the systemic, methodological, and regulatory barriers identified in this review, and by applying the detailed experimental frameworks provided, researchers can enhance the clinical impact of their work, ultimately bridging the gap between bench discoveries and bedside applications to improve patient outcomes in diverse chronic diseases.
Biomarker Performance Assessment: Comparative Utility Across Disease States and Clinical Applications
The pursuit of precision medicine has elevated the importance of biomarkers in clinical diagnostics and therapeutic development. Biomarkers, which are measurable indicators of biological states or conditions, are crucial for early detection, accurate diagnosis, and monitoring disease progression. Their clinical utility is predominantly determined by two key statistical measures: sensitivity, the ability to correctly identify those with the disease (true positive rate), and specificity, the ability to correctly identify those without the disease (true negative rate). In chronic diseases, particularly those mediated by oxidative stress, the accurate quantification of these diagnostic parameters enables researchers and clinicians to stratify patient populations, monitor therapeutic efficacy, and develop targeted interventions. This guide provides a comparative analysis of key biomarkers across neurological, metabolic, and cardiovascular diseases, focusing on their sensitivity and specificity profiles in different pathological contexts.
Comparative Diagnostic Accuracy of Biomarkers Across Disease States
Table 1: Sensitivity and Specificity Profiles of Key Biomarkers in Neurological, Metabolic, and Cardiac Diseases
| Disease Category | Biomarker | Sensitivity (%) | Specificity (%) | Biological Material | Clinical/Research Context |
|---|---|---|---|---|---|
| Alzheimer's Disease | CSF Aβ42 & tau/p-tau | 78-100 | 47-81 [100] | Cerebrospinal Fluid (CSF) | Differentiating AD from normal controls [100] |
| CSF p-tau181 | 77 | 87 [100] | CSF | AD diagnosis, positive predictive value of 90% [100] | |
| Parkinson's Disease | CSF α-synuclein SAA | 87.7-91 | 95-96.3 [101] | CSF | Differentiating PD from healthy/non-neurodegenerative controls [101] |
| Plasma NDEV-derived α-syn | ~90 (AUC) | ~90 (AUC) [101] | Blood Plasma | Identifying individuals at high risk of prodromal PD [101] | |
| Cardiac MIBG Scintigraphy | 85-92 | 85-94 [102] | Heart (imaging) | Differentiating PD from atypical parkinsonism [102] | |
| Prediabetes/Diabetes | HbA1c (vs. FPG/OGTT) | 58.9 | 96 [103] | Blood | Diagnosing diabetes [103] |
| HbA1c for prediabetes | 35.4 | 83.4 [103] | Blood | Identifying prediabetes [103] | |
| Fructosamine (FA) | 82 | 94 [103] | Blood | Diagnosing diabetes (FPG >7 mmol/L or HbA1c≥6.5%) [103] | |
| Glycated Albumin (GA) | 83 | 83 [103] | Blood | Diagnosing diabetes [103] | |
| 1,5-Anhydroglucitol (1,5-AG) | 96 | 88 [103] | Blood | Diagnosing diabetes (HbA1c >6% cutoff) [103] | |
| Acute Myocardial Infarction (AMI) | Cardiac Troponin | ~100 (hs-TnT) | Limited (hs-TnT) [104] | Blood | First-line test for AMI diagnosis [104] [105] |
| Heart-type Fatty Acid-Binding Protein (H-FABP) | 86.96 (4-12h post-AMI) | Less than Troponin & CK-MB [104] | Blood | Detecting AMI 4-12 hours after symptom onset [104] |
The data reveals significant variation in biomarker performance across different conditions. In neurological diseases, cerebrospinal fluid (CSF) biomarkers generally show high sensitivity and specificity, but their invasive collection method limits widespread use. CSF α-synuclein seeding amplification assays (SAA) for Parkinson's disease demonstrate particularly high diagnostic accuracy, reflecting their ability to detect the underlying prion-like seeding activity of misfolded proteins [101]. Blood-based biomarkers, while more accessible, often show more variable performance, as seen with HbA1c, which has high specificity but moderate sensitivity for diagnosing diabetes and prediabetes [103]. For acute conditions like myocardial infarction, cardiac troponin is the gold standard due to its nearly perfect sensitivity, especially with high-sensitivity assays, though its specificity can be lower [104].
Detailed Experimental Protocols for Key Biomarker Assays
Cerebrospinal Fluid (CSF) Biomarker Analysis for Neurodegenerative Diseases
The detection of specific proteins in CSF is a cornerstone for diagnosing Alzheimer's disease (AD) and Parkinson's disease (PD). The protocol for CSF analysis typically involves lumbar puncture to collect CSF, followed by centrifugation to remove cells and debris, and immediate freezing at -80°C until analysis [100] [101].
Alzheimer's Disease Biomarkers (Aβ42, t-tau, p-tau): The most widely used method is enzyme-linked immunosorbent assay (ELISA). In this protocol, CSF samples are added to microplate wells coated with capture antibodies specific to the target protein (e.g., Aβ42 or tau). After incubation and washing, a detection antibody is added, followed by an enzyme-linked secondary antibody and a colorimetric substrate. The concentration of the biomarker is proportional to the color intensity measured by a spectrophotometer [100]. The ratio of Aβ42 to tau is often calculated to improve diagnostic accuracy for AD [100].
Parkinson's Disease Biomarkers (α-synuclein SAA): The α-synuclein seeding amplification assay (SAA) is a more recent and powerful technique. This method detects the prion-like seeding activity of misfolded α-synuclein. In this protocol, CSF samples are mixed with recombinant α-synuclein substrate and a fluorescent dye (e.g., thioflavin T) that binds to amyloid fibrils. The mixture is subjected to cycles of shaking and incubation in a plate reader. If pathological α-synuclein "seeds" are present in the CSF, they template the aggregation of the recombinant substrate, leading to a increase in fluorescence that is monitored in real-time. The time to fluorescence positivity is a key readout, with shorter times indicating a higher seed concentration [101].
Oxidative Stress Biomarker Profiling
The evaluation of oxidative stress is critical in chronic diseases like diabetes, hypertension, and neurodegenerative disorders. The following are standard protocols for key oxidative stress biomarkers [39] [4]:
Lipid Peroxidation (Malondialdehyde - MDA): The Thiobarbituric Acid-Reactive Substances (TBARS) assay is a common method. Briefly, the biological sample (e.g., serum, plasma, or urine) is heated with thiobarbituric acid (TBA) under acidic conditions. MDA, a secondary product of lipid peroxidation, reacts with TBA to form a pink chromogen, which is measured spectrophotometrically at 532-535 nm. For higher specificity, liquid chromatography-mass spectrometry (LC-MS/MS) is employed. In this method, MDA is often derivatized with 2,4-dinitrophenylhydrazine (DNPH) before analysis to improve sensitivity and separation [39] [4].
DNA Oxidation (8-hydroxy-2'-deoxyguanosine - 8-OHdG): The gold standard for 8-OHdG quantification is high-performance liquid chromatography with electrochemical detection (HPLC-ECD). DNA is first extracted from blood or tissue samples and enzymatically hydrolyzed to deoxynucleosides. The hydrolysate is then injected into an HPLC system. 8-OHdG is separated from other nucleosides on a reverse-phase column and detected with high sensitivity using an electrochemical detector. Alternatively, commercial ELISA kits provide a higher-throughput, though sometimes less specific, alternative [4].
Protein Carbonyl Content: This marker of protein oxidation is commonly measured by derivatization with 2,4-dinitrophenylhydrazine (DNPH). Proteins from the sample are precipitated and reacted with DNPH, which binds to carbonyl groups. The derivatized proteins are then dissolved, and the carbonyl content is quantified by measuring the absorbance at 370-375 nm. This can be followed by western blotting with anti-DNP antibodies to visualize specific oxidized proteins [4].
Oxidative Stress Biomarker Pathway
Cardiac Biomarker Testing for Acute Myocardial Infarction
The diagnosis of AMI relies heavily on the measurement of cardiac troponins (cTnI or cTnT) using high-sensitivity immunoassays. The experimental protocol involves collecting a blood sample (serum or heparinized plasma is preferred). The sample is then analyzed on an automated clinical analyzer. The assay principle is typically a "sandwich" immunoassay. The sample is added to a reaction vessel containing magnetic beads or a solid surface coated with a capture antibody specific to cardiac troponin. After washing, a second detection antibody, linked to an indicator molecule (e.g., an enzyme, chemiluminescent compound, or electrochemiluminescent tag), is added. The signal generated by the indicator is measured and is directly proportional to the concentration of cardiac troponin in the sample. Current guidelines define AMI by troponin levels exceeding the 99th percentile of a healthy reference population [104] [105].
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Research Reagents for Biomarker Analysis
| Reagent/Assay Kit | Primary Function | Application Examples |
|---|---|---|
| ELISA Kits | Quantify specific proteins (e.g., tau, α-synuclein) using antibody-based colorimetric detection. | Measuring CSF Aβ42, t-tau, and p-tau in Alzheimer's research [100]. |
| Seeding Amplification Assay (SAA) Kits | Detect misfolded protein aggregates via fluorescence-based amplification. | Identifying pathological α-synuclein in Parkinson's disease CSF [101]. |
| HPLC-ECD/Tandem MS | Separate and quantify small molecules with high sensitivity and specificity. | Measuring 8-OHdG (DNA oxidation) and F2-isoprostanes (lipid peroxidation) [4]. |
| DNPH (2,4-Dinitrophenylhydrazine) | Derivatize carbonyl groups for spectrophotometric or immunoblot detection. | Quantifying protein carbonyl content as a marker of protein oxidation [4]. |
| TBA (Thiobarbituric Acid) | React with malondialdehyde (MDA) to form a measurable chromophore. | Assessing lipid peroxidation through the TBARS assay [39] [4]. |
| High-Sensitivity Troponin Immunoassays | Detect very low concentrations of cardiac troponins I and T. | Gold-standard diagnosis and risk stratification of acute myocardial infarction [104]. |
| Antibodies (anti-DNP, anti-pS129 α-syn) | Specific recognition of target epitopes for blotting or immunoassays. | Detecting protein carbonyls (anti-DNP) or pathological α-synuclein (anti-pS129) [4] [101]. |
Biomarker Detection Workflow
The diagnostic accuracy of biomarkers is highly context-dependent, influenced by the disease mechanism, the biological matrix, and the analytical technique employed. This comparison highlights that while single biomarkers with high sensitivity and specificity exist—such as cardiac troponin for AMI and CSF α-synuclein SAA for PD—many complex chronic diseases require a multi-marker approach. The integration of novel biomarkers, particularly those reflecting underlying oxidative stress pathways, holds significant promise for improving early detection, patient stratification, and the evaluation of novel therapeutics in conditions like Alzheimer's, Parkinson's, diabetes, and cardiovascular diseases. The continued standardization of experimental protocols and the development of more accessible, high-performance assays will be crucial for translating these biomarkers from research tools into clinical practice.
Within the landscape of chronic disease research, oxidative stress has emerged as a critical pathological mechanism and a promising source of prognostic biomarkers. The prognostic value of these markers—their ability to correlate with and potentially predict disease progression, complications, and therapeutic outcomes—is of paramount importance for developing targeted interventions. This review provides a comparative analysis of oxidative stress markers across a spectrum of chronic conditions, including neurodegenerative, cardiovascular, and metabolic diseases. By synthesizing recent clinical evidence and standardizing experimental data, we aim to equip researchers and drug development professionals with a clear framework for evaluating the translational potential of these biomarkers in prognosis and therapy.
Comparative Prognostic Utility of Oxidative Stress Biomarkers Across Chronic Diseases
The clinical utility of oxidative stress biomarkers is largely determined by their correlation with specific disease stages and outcomes. The table below provides a structured comparison of key biomarkers and their validated prognostic significance across different disease domains.
Table 1: Prognostic Value of Key Oxidative Stress Biomarkers Across Chronic Diseases
| Disease Area | Key Biomarkers | Correlation with Disease Progression | Association with Complications | Link to Treatment Outcomes |
|---|---|---|---|---|
| Neurodegenerative Diseases | CSF Malondialdehyde (MDA), Serum Reactive Oxygen Species (ROS), 8-OHdG [106] [107] [108] | Elevated CSF MDA and serum ROS differentiate MCI patients with abnormal amyloid (MCI A+) from healthy controls and MCI A- patients [106]. Mitochondrial DNA damage and lipid peroxidation are central to PD pathogenesis [107]. | In MCI, CSF MDA levels were significantly higher in males, and serum MDA was higher in older patients within the MCI A+ group, suggesting demographic influences on complication risk [106]. | Treatment with onabotulinumtoxinA or anti-CGRP therapies in headache disorders improved plasma oxidative stress biomarkers over six months [7]. |
| Cardiovascular Diseases (CVD) | 8-iso-PGF2α, Oxidized LDL (oxLDL), Myeloperoxidase (MPO), MHR, NHR, LHR [7] [76] [109] | MHR, NHR, and LHR were independently associated with Medication Overuse Headache (MOH) [7]. oxLDL is a key instigator of atherogenesis, and 8-iso-PGF2α predicts endothelial dysfunction [76] [109]. | Levels of adhesion molecules (sVCAM-1, sICAM-1), PAI-1, and ROS are elevated in young individuals with central adiposity, an early CVD risk factor [110]. | Mitochondria-targeted antioxidants (e.g., MitoQ) show promise in improving vascular function in resistant hypertension [4] [109]. |
| Metabolic Diseases (Diabetes) | Malondialdehyde (MDA), 8-OHdG, F2-isoprostanes, SOD, GPx, TNF-α [111] [4] | Urinary 8-OHdG is a surrogate for diabetic nephropathy, and plasma MDA predicts endothelial dysfunction [4]. TNF-α levels rise with diabetes duration [111]. | High SOD and GPx activity suggests chronic oxidative stress, while increased BMI is linked to lower enzyme levels [111]. IL-6 levels are higher in patients not using metformin [111]. | Antioxidant therapies have shown inconsistent outcomes; targeted approaches like Nrf2 activators are under investigation [4]. |
Methodological Framework for Biomarker Analysis
Standardized and detailed experimental protocols are crucial for ensuring the reproducibility and accurate interpretation of data on oxidative stress biomarkers.
Blood-Based Biomarker Ratios in Headache Disorders
- Study Design: A cross-sectional study compared patients with Medication Overuse Headache (MOH), episodic migraine (EM), and healthy controls (HC) matched for age and sex [7].
- Participants: 109 MOH patients, 68 EM patients, and 86 HC were recruited from a tertiary headache clinic [7].
- Blood Collection and Analysis: Following an 8-10 hour fast, blood samples were drawn. A complete blood count was performed to determine monocyte, neutrophil, and lymphocyte counts. A biochemical profile was used to measure High-Density Lipoprotein Cholesterol (HDL-C) levels [7].
- Calculation of Ratios: The Monocyte to HDL Ratio (MHR), Neutrophil to HDL Ratio (NHR), and Lymphocyte to HDL Ratio (LHR) were calculated from the absolute cell counts and HDL-C concentration [7].
- Statistical Analysis: Univariate and multivariate logistic regression analyses were employed to identify if MHR, NHR, and LHR were independent factors associated with MOH, expressed as Odds Ratios (OR) with 95% Confidence Intervals (CI) [7].
Oxidative Stress Profiling in Mild Cognitive Impairment (MCI)
- Cohort Classification: 114 adults were divided into three groups: 38 MCI patients with a normal CSF Aβ42/Aβ40 ratio (A-), 38 MCI patients with an abnormal ratio (A+), and 38 healthy controls with a normal ratio [106].
- Biomarker Measurement:
- Established CSF Biomarkers: Aβ40, Aβ42, phosphorylated tau (p-tau), and total tau (t-tau) were analyzed using an automated immunochemical method [106].
- Oxidative Stress Markers: Total ROS levels in serum were measured by fluorometry. Malondialdehyde (MDA) levels in serum and cerebrospinal fluid (CSF) were determined by a competitive inhibition enzyme immunoassay [106].
- Data Analysis: Statistical differences in oxidative stress markers between groups were analyzed, with further stratification based on sex and age [106].
Analytical Workflows and Pathological Mechanisms
The diagrams below illustrate the core experimental workflow for biomarker analysis and the central role of oxidative stress in disease pathogenesis.
Biomarker Analysis Workflow
Oxidative Stress in Disease Pathogenesis
The Researcher's Toolkit: Essential Reagents and Assays
The reliable measurement of oxidative stress requires a suite of validated research reagents and analytical platforms. The following table details key solutions essential for work in this field.
Table 2: Key Research Reagent Solutions for Oxidative Stress Analysis
| Reagent / Assay Kit | Specific Target | Research Function | Example Methodology |
|---|---|---|---|
| Thiobarbituric Acid-Reactive Substances (TBARS) Assay | Malondialdehyde (MDA) | Quantifies lipid peroxidation, a key marker of oxidative damage to cell membranes [4]. | Spectrophotometric measurement of pink chromogen formed by MDA-TBA reaction [4]. |
| Competitive Inhibition Enzyme Immunoassay | Malondialdehyde (MDA) | Provides a high-throughput, antibody-based method for quantifying MDA in serum and CSF [106]. | Microplate-based immunoassay using anti-MDA antibodies for detection in biological fluids [106]. |
| Gas/Liquid Chromatography-Mass Spectrometry (GC/LC-MS) | F2-isoprostanes | The gold-standard method for specific and accurate quantification of stable lipid peroxidation end-products [4]. | Sample extraction, chromatographic separation, and highly specific detection and quantification via mass spectrometry [4]. |
| ELISA Kits (e.g., Quantikine) | 8-OHdG, Cytokines (IL-6, etc.), Adhesion Molecules (sICAM-1) | Enables sensitive, high-throughput quantification of DNA damage, inflammatory markers, and endothelial activation [106] [110]. | Microplate-based immunoassay using specific capture and detection antibodies for colorimetric or fluorometric readout [106] [110]. |
| DNPH Assay / Anti-DNP Antibodies | Protein Carbonyls | Measures protein oxidation, a marker of irreversible oxidative damage, via spectrophotometry or immunoblotting/ELISA [4]. | Derivatization of carbonyl groups with 2,4-dinitrophenylhydrazine (DNPH) followed by detection [4]. |
| Fluorometric Assays (e.g., DCFH-DA) | Intracellular Reactive Oxygen Species (ROS) | Provides a dynamic measure of overall intracellular ROS production in live cells or fresh tissue samples [4]. | Cell-permeable DCFH-DA is deacetylated and then oxidized by ROS to fluorescent DCF, measured fluorometrically [4]. |
| Enzyme Activity Kits (e.g., Randox) | Superoxide Dismutase (SOD), Glutathione Peroxidase (GPx), Glutathione Reductase (GR) | Measures the activity of key enzymatic antioxidant defenses, indicating the body's capacity to counteract ROS [111] [110]. | Kinetic assays based on the enzyme's ability to catalyze a specific redox reaction, monitored spectrophotometrically [111] [110]. |
Implications for Prognosis and Targeted Therapy
The prognostic application of oxidative stress biomarkers is evolving beyond simple correlation toward guiding personalized treatment strategies.
Biomarker-Guided Personalization
The differential expression of biomarkers based on patient demographics and clinical status underscores their potential for personalizing prognosis and care. For instance, in Mild Cognitive Impairment (MCI), CSF MDA levels are significantly higher in males within the MCI A+ group, and serum MDA is markedly higher in older MCI A+ patients [106]. Similarly, in diabetes, IL-6 levels are higher in patients not using metformin, and TNF-α levels rise with disease duration, potentially serving as a biomarker for progression and complications [111]. These findings highlight the need for demographic-specific biomarker reference ranges and their utility in stratifying patients for more aggressive monitoring or tailored therapeutic interventions.
Emerging Therapeutic and Diagnostic Strategies
Research is actively translating the understanding of oxidative stress into novel therapeutic and diagnostic approaches.
- Targeted Antioxidant Therapies: Moving beyond broad-spectrum antioxidants like vitamin E, new strategies include mitochondria-targeted antioxidants (MitoQ) to enhance vascular function in resistant hypertension, Nrf2 activators to restore redox balance in early diabetes, and specific inhibitors of NADPH oxidase (NOX) isoforms [107] [4] [109].
- Advanced Delivery Systems: Nanotechnology is being explored to deliver antioxidants directly to affected sites, such as pancreatic islets or atherosclerotic plaques, improving efficacy and reducing off-target effects [4].
- Integrated 'Omics' for Diagnostics: The integration of redox proteomics and transcriptomics helps identify oxidative modifications and gene expression patterns, paving the way for personalized therapy and more precise biomarker panels [4] [109].
The comprehensive comparison of oxidative stress biomarkers across chronic diseases confirms their significant and growing prognostic value. From simple blood cell ratios like MHR and LHR in headache disorders to sophisticated measures like F2-isoprostanes and 8-OHdG in diabetes and CVD, these biomarkers provide a critical window into disease activity, severity, and risk of complications. The future of this field lies in the standardization of assays, the validation of biomarker panels in large, diverse cohorts, and the integration of this data with other 'omics' technologies. This integrated approach will enable the transition from reactive measurement to proactive, personalized redox medicine, ultimately improving clinical outcomes across the spectrum of chronic disease.
Oxidative stress, defined as a disruption of the prooxidant-antioxidant balance in favor of the former, is a key pathophysiological mechanism in a wide spectrum of chronic diseases, including cardiovascular disease, diabetes, neurodegenerative disorders, and cancer [47] [112]. The reliable assessment of oxidative stress in clinical and research settings depends on accurate biomarkers that reflect molecular damage to key biological macromolecules. Among the most extensively studied biomarkers are products of lipid peroxidation and protein oxidation. Malondialdehyde (MDA) and F2-isoprostanes (F2-IsoPs) represent the most validated markers of lipid peroxidation, while protein carbonyls and advanced glycation end products (AGEs) serve as principal indicators of protein damage [113] [114]. This guide provides a comparative analysis of these biomarker classes, evaluating their analytical methodologies, biological significance, and applicability in chronic disease research and drug development.
Biomarker Profiles: Analytical and Biological Characteristics
Table 1: Comparative Profile of Major Lipid Peroxidation and Protein Oxidation Biomarkers
| Characteristic | Malondialdehyde (MDA) | F2-Isoprostanes (F2-IsoPs) | Protein Carbonyls | Advanced Glycation End Products (AGEs) |
|---|---|---|---|---|
| Biomarker Class | Lipid Peroxidation | Lipid Peroxidation | Protein Oxidation | Protein Oxidation (Glycoxidation) |
| Precursor Molecule | Polyunsaturated Fatty Acids (PUFAs) | Arachidonic Acid | Amino Acid Side Chains (Lys, Arg, etc.) | Reducing Sugars + Amino Groups |
| Formation Mechanism | Fragmentation of lipid hydroperoxides [112] | Non-enzymatic, free radical peroxidation of arachidonic acid [112] [115] | Direct oxidation or adduction by lipid peroxidation products [116] [114] | Non-enzymatic Maillard reaction, often potentiated by oxidative stress [114] |
| Primary Sample Matrices | Plasma, serum, urine [113] | Plasma, urine, tissue [112] [115] | Plasma, tissue, cell lysates [116] [117] | Plasma, skin (via autofluorescence) [114] |
| Key Analytical Methods | TBARS assay, HPLC, GC-MS [113] [112] | GC-MS, LC-MS/MS, ELISA [112] [115] | DNPH derivatization + spectrophotometry/immunoblotting [53] [114] | ELISA, HPLC, LC-MS/MS, skin autofluorescence [114] |
| Key Advantages | Widely used, cost-effective assays | Gold standard for lipid peroxidation; specific and stable [118] [115] | Early formation, relative stability [116] [117] | Reflect both glycaemic and oxidative stress; multiple detection methods |
Table 2: Clinical and Research Utility in Chronic Diseases
| Utility Aspect | MDA | F2-IsoPs | Protein Carbonyls | AGEs |
|---|---|---|---|---|
| Association with Disease Severity | Elevated in atherosclerosis, diabetes [112] | Strongly elevated in cystic fibrosis, pulmonary hypertension, renal disease [115] | Increased in cellular aging, neurodegenerative diseases [116] [117] | Accumulate in diabetes, renal failure, aging [114] |
| Sensitivity to Interventions | Reduced by almond supplementation [9] | Responsive to antioxidant regimes [115] | Can monitor efficacy of interventions [116] | Skin AGEs modifiable by diet and therapy [114] |
| Limitations & Challenges | Lack of specificity in TBARS assay; reactivity [113] [115] | Complex formation and metabolism; multiple isomers [115] | Can derive from multiple pathways [114] | Formation influenced by multiple factors beyond oxidation [114] |
| Ideal Use Case | Initial, high-throughput screening | Definitive quantification of lipid peroxidation in clinical trials [115] | General biomarker of protein oxidative damage [117] | Tracking long-term metabolic and oxidative stress |
Experimental Protocols for Biomarker Assessment
Quantification of Lipid Peroxidation Markers
A. Malondialdehyde (MDA) via TBARS Assay The Thiobarbituric Acid-Reactive Substances (TBARS) assay is a commonly used method for estimating MDA levels. In this protocol, biological samples (e.g., plasma or tissue homogenate) are mixed with thiobarbituric acid (TBA) under acidic conditions and heated. The reaction between MDA and TBA generates a pink chromophore that can be measured spectrophotometrically at 532–535 nm [113] [112]. While widely used due to its low cost and simplicity, the TBARS assay lacks absolute specificity for MDA, as other aldehydes and sample components can react with TBA. For greater accuracy, HPLC or GC-MS methods with specific MDA detection are recommended [113].
B. F2-Isoprostanes via Gas Chromatography-Mass Spectrometry (GC-MS) The gold-standard protocol for F2-IsoPs involves solid-phase extraction followed by derivatization and analysis by GC-MS. The specific isomer 8-iso-PGF2α is frequently quantified. Steps include: 1) addition of an internal standard (e.g., deuterated 8-iso-PGF2α), 2) alkaline hydrolysis to release esterified F2-IsoPs from lipids, 3) solid-phase extraction for purification, 4) derivatization to pentafluorobenzyl esters and trimethylsilyl ethers, and 5) analysis using negative chemical ionization GC-MS [112] [115]. This method provides high sensitivity and specificity, distinguishing F2-IsoPs from enzymatically derived prostaglandins.
Quantification of Protein Oxidation Markers
A. Protein Carbonyls via DNPH Derivatization The most common protocol for measuring protein carbonyls involves derivatization with 2,4-dinitrophenylhydrazine (DNPH). The procedure is as follows: 1) Protein samples are precipitated with trichloroacetic acid (TCA). 2) The pellet is reacted with DNPH, which covalently binds to carbonyl groups, forming a dinitrophenylhydrazone product. 3) Unreacted DNPH is removed by washing. 4) The derivatized protein is re-dissolved, and the absorbance is measured spectrophotometrically at ~370 nm. The carbonyl content is calculated using a molar absorption coefficient [53] [114]. For proteomic identification, DNPH-derivatized proteins can be separated by 2D-gel electrophoresis, transferred to membranes for immunodetection with anti-DNP antibodies, and identified by mass spectrometry [116] [117].
B. Advanced Glycation End Products (AGEs) via ELISA and LC-MS Multiple protocols exist for AGE measurement. A common high-throughput approach is the enzyme-linked immunosorbent assay (ELISA) using specific antibodies against common AGE structures like carboxymethyllysine (CML) [114]. For specific and quantitative analysis, liquid chromatography coupled with tandem mass spectrometry (LC-MS/MS) is employed. This protocol typically involves protein hydrolysis, followed by LC separation and targeted MS analysis using multiple reaction monitoring (MRM) for specific AGEs, providing high specificity and sensitivity [114].
Biomarker Formation Pathways and Experimental Workflow
Formation Pathways of Lipid and Protein Oxidation Biomarkers
The following diagram illustrates the key formation pathways for the biomarkers discussed, highlighting their common trigger in oxidative stress.
Generalized Experimental Workflow for Biomarker Analysis
This workflow outlines the standard procedural steps for quantifying these biomarkers, from sample collection to data analysis.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Biomarker Analysis
| Reagent / Material | Primary Function | Application Examples |
|---|---|---|
| Thiobarbituric Acid (TBA) | Reacts with MDA to form a measurable chromophore. | Quantification of MDA in the TBARS assay [113]. |
| 2,4-Dinitrophenylhydrazine (DNPH) | Derivatizing agent for protein carbonyl groups. | Spectrophotometric or immunochemical detection of protein carbonyls [53] [114]. |
| Deuterated Internal Standards (e.g., d₄-8-iso-PGF₂α) | Allows for precise quantification via mass spectrometry. | GC-MS or LC-MS/MS analysis of F2-IsoPs for high accuracy [115]. |
| Anti-DNP Antibody | Binds specifically to DNPH-derivatized protein carbonyls. | Western blotting or ELISA for detecting carbonylated proteins [116] [117]. |
| Solid-Phase Extraction (SPE) Cartridges | Purify and concentrate analytes from complex biological fluids. | Isolation of F2-IsoPs from plasma or urine prior to GC-MS analysis [112] [115]. |
| Specific AGE Antibodies (e.g., anti-CML) | Immunodetection of specific AGE structures. | ELISA or immunohistochemistry for AGE quantification in tissues or fluids [114]. |
The selection between lipid peroxidation markers (MDA, F2-IsoPs) and protein oxidation markers (Carbonyls, AGEs) should be guided by the specific research question, required specificity, and available analytical resources. MDA offers a cost-effective entry point, while F2-IsoPs provide an unequivocal gold standard for lipid peroxidation in rigorous clinical trials [115]. Protein carbonyls serve as a robust general marker of protein damage, and AGEs provide a unique window into the interplay between glycaemic and oxidative stress. The future of oxidative stress biomarker research lies in the move towards personalized redox medicine. This includes the use of multi-marker panels, the application of advanced omics technologies (redox proteomics) for discovering novel modifications [116] [53], and the development of point-of-care tests to integrate these biomarkers into clinical practice for improved diagnosis and targeted therapy monitoring in chronic diseases.
Oxidative stress, characterized by an imbalance between reactive oxygen species (ROS) and antioxidant defenses, serves as a critical pathophysiological link in chronic diseases such as cardiovascular disease, diabetes, and chronic kidney disease [53] [87]. The resulting oxidative damage to lipids, proteins, and DNA not only accelerates disease progression but also generates measurable biomarkers that provide insights into disease severity and prognosis [54]. This comparative guide evaluates disease-specific clinical tools for risk prediction and monitoring, framing their utility within the context of oxidative stress mechanisms. We systematically analyze performance metrics of cardiovascular risk scores in diabetic populations, oxidative stress biomarkers in diabetes monitoring, and renal function prediction models, providing researchers with structured experimental data and methodologies for translational research applications.
Cardiovascular Risk Prediction in Diabetes: A Comparative Analysis
Performance Comparison of Cardiovascular Risk Prediction Models
Accurate cardiovascular disease (CVD) risk stratification in individuals with type 2 diabetes is essential for targeting preventive therapies. A large-scale validation study compared 22 risk prediction models—13 derived from general populations and 9 developed specifically for diabetes—in a cohort of 168,871 UK-based individuals with type 2 diabetes without pre-existing CVD [119]. Discrimination was assessed using Harrell's C statistic, where values below 0.70 indicate inadequate discrimination, 0.70-0.80 acceptable discrimination, and 0.80-0.90 excellent discrimination [119].
Table 1: Performance of Selected Cardiovascular Risk Prediction Scores in Type 2 Diabetes
| Risk Prediction Model | Derivation Population | Number of Predictors | C Statistic for CVD (95% CI) | C Statistic for CVD+ (95% CI) | Calibration Slope (95% CI) |
|---|---|---|---|---|---|
| SCORE CVD | General population | 6 | 0.67 (0.67, 0.67) | 0.69 (0.69, 0.70) | 0.74 (0.72, 0.76) |
| QRISK3 | General population | 19 | 0.66 (0.66, 0.67) | 0.68 (0.68, 0.69) | 0.63 (0.61, 0.65) |
| UKPDS (CHD) | Type 2 diabetes | 12 | 0.64 (0.64, 0.65) | 0.66 (0.65, 0.66) | 0.38 (0.37, 0.39) |
| Framingham (CHD) | General population | 8 | 0.62 (0.62, 0.63) | 0.64 (0.64, 0.65) | 0.45 (0.43, 0.47) |
The Systemic Coronary Risk Evaluation (SCORE) CVD rule, derived from the general population, demonstrated superior performance for predicting both standard CVD (coronary heart disease and stroke) and an expanded CVD+ definition (which includes heart failure and atrial fibrillation) [119]. Notably, diabetes-specific models like the UK Prospective Diabetes Study (UKPDS) risk scores performed significantly worse than SCORE CVD (p<0.001), challenging the assumption that disease-specific models inherently outperform general population models in diabetic cohorts [119].
Experimental Protocol for Cardiovascular Risk Model Validation
The methodology for validating cardiovascular risk prediction models in diabetic populations involves several critical stages, as implemented in the CALIBER study [119]:
Study Population Definition: Researchers identified 168,871 individuals with type 2 diabetes from linked English electronic health records (primary care, hospital episodes, and death registrations). Participants were aged ≥18 years without pre-existing CVD+ diagnoses prior to or within 30 days after type 2 diabetes diagnosis [119].
Cohort Phenotyping: Type 2 diabetes cases were identified using validated CALIBER phenotyping algorithms harmonizing data from general practitioner records and Hospital Episodes Statistics. The algorithm has demonstrated high accuracy in UK primary care data where diagnosis coding is rigorously maintained for reimbursement purposes [119].
Variable Extraction: Participant characteristics including demographics, smoking status, clinical measurements (HbA1c, blood pressure, lipid profiles), and biomarkers were extracted from electronic health records. Missing data were addressed using multiple imputation techniques [119].
Outcome Ascertainment: Participants were followed from initial diabetes diagnosis until first cardiovascular event, death, or 10-year follow-up. CVD events included fatal/non-fatal myocardial infarction, sudden cardiac death, ischemic heart disease, fatal/non-fatal stroke, or peripheral artery disease. The expanded CVD+ definition additionally included heart failure and/or atrial fibrillation [119].
Statistical Validation: Model performance was assessed using discrimination (Harrell's C statistic) and calibration (calibration-in-the-large and calibration slope). A recalibration process was performed in a 10% training sample before evaluating performance in the remaining 90% test sample [119].
Diabetes Monitoring: Oxidative Stress Biomarkers and Clinical Correlations
Key Oxidative Stress Biomarkers in Diabetes Pathogenesis
In diabetes, chronic hyperglycemia drives excessive ROS production through multiple pathways including AGE-RAGE signaling, protein kinase C activation, and the polyol pathway [53]. This oxidative overload contributes to both insulin resistance and beta-cell dysfunction, making oxidative stress biomarkers valuable indicators of disease severity and progression [87].
Table 2: Clinically Validated Oxidative Stress Biomarkers in Diabetes Monitoring
| Biomarker | Biomolecular Target | Significance in Diabetes | Detection Methods | Reference Ranges |
|---|---|---|---|---|
| Malondialdehyde (MDA) | Lipids | Marker of lipid peroxidation; correlates with endothelial dysfunction in hypertension and diabetes | Thiobarbituric Acid-Reactive Substances (TBARS) assay; HPLC/MS-MS | Varies by method; significant reductions observed with interventions |
| 8-OHdG (8-hydroxy-2'-deoxyguanosine) | DNA | Surrogate for diabetic nephropathy; reflects oxidative DNA damage | HPLC-ECD; HPLC-MS/MS; ELISA | Elevated in diabetic complications; decreases with antioxidant interventions |
| F2-isoprostanes | Lipids | Stable end-products of arachidonic acid oxidation; correlate with disease progression | Gas or liquid chromatography-mass-mass spectrometry | Strong correlation with disease progression |
| Superoxide Dismutase (SOD) | Enzymatic antioxidant | Diminished activity associated with β-cell failure and poor glycemic control | Spectrophotometric activity assays | Reduced in diabetes; increases with almond supplementation (>60g/day) |
| Glutathione Peroxidase (GPx) | Enzymatic antioxidant | Reduced activity in insulin resistance; contributes to oxidative burden | Spectrophotometric activity assays | Variable response to interventions |
Interventional Evidence: Almond Supplementation and Oxidative Stress Reduction
A recent meta-analysis of randomized controlled trials demonstrates that dietary interventions can significantly modulate oxidative stress in chronic diseases. Almond supplementation at doses exceeding 60g/day significantly reduced multiple oxidative stress biomarkers [9]:
- Malondialdehyde (MDA): Weighted mean difference (WMD) = -0.46, p = 0.002
- 8-OHdG: WMD = -5.83, p < 0.001
- Uric acid: WMD = -0.64, p = 0.009
- Superoxide dismutase (SOD): WMD = 2.02, p = 0.008
These findings support the potential of targeted nutritional interventions as adjunct strategies for reducing oxidative stress in diabetic populations [9].
Experimental Protocol for Oxidative Stress Biomarker Assessment
Standardized methodologies for quantifying oxidative stress biomarkers ensure reproducibility across research settings:
Sample Collection and Preparation: Collect blood (serum/plasma) and urine samples following standardized protocols. For lipid peroxidation markers, add antioxidant preservatives (e.g., butylated hydroxytoluene) to prevent ex vivo oxidation [53] [9].
Malondialdehyde (MDA) Quantification:
- Utilize the Thiobarbituric Acid-Reactive Substances (TBARS) assay
- React samples with thiobarbituric acid under acidic conditions
- Measure pink chromogen formation at 532-535nm
- Alternatively, employ high-performance liquid chromatography with mass spectrometry (HPLC/MS-MS) for improved specificity [53]
8-OHdG Measurement:
- Extract DNA from blood samples using commercial kits
- Digest DNA to nucleosides using nuclease P1 and alkaline phosphatase
- Quantify 8-OHdG using HPLC with electrochemical detection (HPLC-ECD) or HPLC-MS/MS
- For high-throughput analysis, use ELISA kits with validation against chromatographic methods [53]
Antioxidant Enzyme Activity Assays:
- Superoxide Dismutase (SOD): Measure inhibition of cytochrome C reduction at 550nm
- Glutathione Peroxidase (GPx): Monitor NADPH oxidation at 340nm using hydrogen peroxide as substrate
- Catalase (CAT): Follow hydrogen peroxide decomposition at 240nm [120]
Quality Control: Include internal standards, assay controls, and replicate measurements. For EPR spectroscopy, use spin traps like DMPO for direct ROS detection in biological tissues [53].
Renal Function Assessment: Predictive Models for Chronic Kidney Disease
Performance of CKD Risk Prediction Models in Healthy and Diabetic Populations
Chronic kidney disease (CKD) prediction models enable early identification of high-risk individuals for targeted interventions. A systematic review identified 36 models for healthy populations and 12 models specifically for type 2 diabetes populations, with performance varying significantly across development cohorts [121].
Table 3: Chronic Kidney Disease Risk Prediction Models: Performance Characteristics
| Model Type | Number of Models | C Statistic Range | AUC Range | Models with Good Discriminatory Performance | Key Predictors |
|---|---|---|---|---|---|
| Healthy populations | 36 | 0.65 - 0.91 | 0.63 - 0.91 | 13 | Age, hypertension, diabetes status, baseline kidney function |
| Type 2 diabetes populations | 12 | 0.56 - 0.81 | 0.71 - 0.83 | 4 | Diabetes duration, HbA1c, albuminuria, eGFR |
The review highlighted substantial heterogeneity in model variables and validation methodologies, precluding meta-analysis. For diabetic populations, models incorporating diabetes-specific parameters (duration, glycemic control, albuminuria) demonstrated superior performance compared to general population models [121].
Experimental Protocol for CKD Risk Model Development and Validation
Data Source and Study Design: Utilize prospective cohort studies with extended follow-up (≥5 years). For diabetes-specific models, the Hong Kong Diabetes Registry and UKPDS cohort represent validated data sources [122] [121].
Predictor Variable Selection: Include demographic factors (age, sex), clinical parameters (blood pressure, BMI), diabetes-specific variables (duration, HbA1c), and baseline renal function (eGFR, albuminuria) [121].
Outcome Definition: Define CKD as estimated glomerular filtration rate (eGFR) <60 mL/min/1.73m², albuminuria (urine albumin-to-creatinine ratio ≥30 mg/g), or both, persisting for >3 months [121].
Statistical Analysis:
- Employ Cox proportional hazards regression for model development
- Assess discrimination using Harrell's C statistic or area under the ROC curve (AUC)
- Evaluate calibration using Hosmer-Lemeshow test and calibration plots
- Perform internal validation via bootstrapping and external validation in independent cohorts [121]
Methodological Quality Assessment: Use the QUADAS-2 tool to evaluate risk of bias across four domains: patient selection, index test, reference standard, and flow/timing [121].
Integrated Signaling Pathways: Oxidative Stress in Chronic Disease
Oxidative Stress Signaling in Cardiorenal-Metabolic Disease
Oxidative Stress in Chronic Disease Pathogenesis
Antioxidant Defense Mechanisms and Therapeutic Targeting
Cellular Antioxidant Defense System
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Essential Research Reagents for Oxidative Stress and Chronic Disease Studies
| Research Reagent | Application | Specific Function | Example Methodologies |
|---|---|---|---|
| Thiobarbituric Acid | Lipid peroxidation assay | Reacts with MDA to form fluorescent pink adduct | TBARS assay for malondialdehyde quantification |
| DCFH-DA (2',7'-Dichlorodihydrofluorescein diacetate) | Intracellular ROS detection | Cell-permeable dye oxidized to fluorescent DCF by ROS | Flow cytometry, fluorescence microscopy |
| DMPO (5,5-Dimethyl-1-pyrroline N-oxide) | ROS detection via EPR spectroscopy | Spin trap that forms stable adducts with free radicals | Electron paramagnetic resonance spectroscopy |
| Anti-DNP Antibody | Protein carbonylation detection | Recognizes dinitrophenylhydrazone derivatives of carbonyl groups | ELISA, western blot for protein carbonyls |
| SOD Activity Assay Kit | Antioxidant enzyme assessment | Measures inhibition of superoxide-mediated reduction | Spectrophotometric cytochrome C reduction assay |
| 8-OHdG ELISA Kit | Oxidative DNA damage quantification | Monoclonal antibody specific for 8-hydroxy-2'-deoxyguanosine | Enzyme-linked immunosorbent assay |
| HPLC-MS/MS System | Biomarker separation and quantification | High-resolution separation and detection of oxidized biomolecules | Quantification of F2-isoprostanes, 8-OHdG, MDA |
This comparative analysis demonstrates that disease-specific clinical tools exhibit varying performance across different clinical contexts. In cardiovascular risk prediction, general population models like SCORE CVD may outperform diabetes-specific tools in contemporary diabetic cohorts, highlighting the importance of regular model validation and recalibration [119]. For diabetes monitoring, oxidative stress biomarkers provide mechanistic insights into disease progression and response to interventions, with specific biomarkers like 8-OHdG and MDA showing consistent associations with complications [53] [9]. In renal function assessment, diabetes-specific CKD prediction models incorporating parameters such as disease duration and glycemic control demonstrate superior performance compared to general population models [121].
The integration of oxidative stress biomarkers with traditional clinical prediction tools offers a promising approach for enhancing risk stratification and monitoring in chronic diseases. Future research directions should focus on validating multi-marker panels, developing standardized assay protocols, and exploring targeted interventions that address underlying oxidative stress mechanisms across the spectrum of cardiorenal-metabolic diseases.
Oxidative stress (OS), characterized by an imbalance between reactive oxygen species (ROS) and the body's antioxidant defenses, is a fundamental pathogenetic mechanism in a wide spectrum of chronic diseases [87]. In clinical research and drug development, the accurate measurement of OS is paramount for diagnosing disease activity, monitoring progression, and evaluating the efficacy of novel therapeutics. A plethora of biomarkers has been developed to quantify oxidative damage to lipids, proteins, and DNA, as well as to assess antioxidant capacity [75] [4]. However, the translation of these biomarkers from research settings to routine clinical practice and as endpoints in clinical trials is highly dependent on their level of clinical validation. This guide provides a comparative analysis of key oxidative stress biomarkers, evaluating their evidence levels, methodological protocols, and readiness for integration into patient management and interventional studies.
Comparative Evidence Levels for Oxidative Stress Biomarkers
The clinical validity of a biomarker is gauged by its specificity for a disease, its prognostic value, and its correlation with disease activity, which then allows for the assessment of treatment efficacy [75]. The hierarchy of evidence, which ranks research methodologies from systematic reviews (Level I) to expert opinion (Level V), provides a framework for this evaluation [123] [124] [125]. The following section and table present a structured comparison of established and emerging OS biomarkers across different chronic conditions, summarizing their evidence levels and key clinical correlations.
Table 1: Evidence Levels and Clinical Correlations of Oxidative Stress Biomarkers in Chronic Diseases
| Biomarker | Type of Measure | Chronic Disease Context | Reported Clinical Correlation | Evidence Level |
|---|---|---|---|---|
| MDA (Malondialdehyde) | Lipid peroxidation | Hypertension, Diabetes [4] | Predicts endothelial dysfunction and correlates with disease severity [4]. | Level II-III (Cohort & Case-Control Studies) |
| F2-Isoprostanes | Lipid peroxidation | Hypertension, Diabetes [4] | Strong correlation with disease progression and end-organ complications; considered a gold standard [4]. | Level II-III (Cohort & Case-Control Studies) |
| 8-OHdG (8-hydroxy-2'-deoxyguanosine) | DNA oxidation | Diabetes, Neurodegenerative Diseases, Cancer [4] | Surrogate marker for diabetic nephropathy; correlates with aging and cancer [4]. | Level II-III (Cohort & Case-Control Studies) |
| Protein Carbonyls | Protein oxidation | Neurodegenerative Diseases, Diabetes, Renal Failure [75] | Elevated in numerous conditions; stable and measurable post-reperfusion injury [75]. | Level II-III (Cohort & Case-Control Studies) |
| MHR (Monocyte to HDL Ratio) | Composite inflammatory/OS marker | Medication Overuse Headache (MOH) [7] | Independently associated with MOH; distinct inflammatory profile vs. controls [7]. | Level III (Case-Control Study) |
| LHR (Lymphocyte to HDL Ratio) | Composite inflammatory/OS marker | Medication Overuse Headache (MOH) [7] | Elevated in MOH patients compared to healthy controls [7]. | Level III (Case-Control Study) |
| NHR (Neutrophil to HDL Ratio) | Composite inflammatory/OS marker | Medication Overuse Headache (MOH) [7] | Elevated in MOH patients compared to healthy controls [7]. | Level III (Case-Control Study) |
Detailed Experimental Protocols for Key Biomarkers
Standardized, high-throughput methodologies are a prerequisite for the clinical adoption of any biomarker. The following section details the experimental protocols for some of the most clinically relevant oxidative stress markers, as derived from current literature.
Protein Carbonyls (Protein Oxidation)
Protein carbonyls are formed through oxidative cleavage of protein backbones or by binding of aldehydic lipid oxidation products, resulting in concentrations that are commonly higher than other biomarkers and thus easier to detect [75]. The most widely used detection method involves derivatization with 2,4-dinitrophenylhydrazine (DNPH).
- Sample Preparation: Plasma or serum samples are obtained from fasting participants. Proteins are isolated and purified to remove interfering substances.
- Derivatization: The protein sample is reacted with DNPH, which binds specifically to carbonyl groups, forming a hydrazone product.
- Quantification:
- Spectrophotometry: The carbonyl-DNPH adduct is measured by its absorbance at 370-375 nm, with the absorbance being proportional to the carbonyl content [75] [4].
- ELISA: Commercial ELISA kits using anti-DNP antibodies provide a higher-throughput alternative, are more convenient for larger sample sizes, and require significantly less sample volume [75]. Results from ELISA correlate well with the colorimetric assay.
F2-Isoprostanes (Lipid Peroxidation)
F2-isoprostanes are stable end-products of arachidonic acid oxidation and are considered a gold-standard biomarker for lipid peroxidation due to their specificity and stability [4].
- Sample Collection: Urine or plasma samples can be used. Urinary F2-isoprostanes are often preferred as they provide a non-invasive, integrated measure of systemic oxidative stress.
- Extraction and Purification: Solid-phase extraction (SPE) is typically employed to isolate F2-isoprostanes from the biological matrix.
- Quantification:
- Gas Chromatography-Mass Spectrometry (GC-MS) or Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS): These mass spectrometry-based methods are considered the reference standards due to their high sensitivity and specificity [4]. They allow for precise identification and quantification of specific F2-isoprostane isomers.
8-OHdG (DNA Oxidation)
8-hydroxy-2'-deoxyguanosine is a well-established biomarker of oxidative DNA damage, reflecting guanine base damage caused by ROS [4].
- Sample Source: Measured in urine, plasma, or isolated cellular DNA.
- DNA Extraction and Digestion: If using cellular DNA, it must be extracted and enzymatically digested to deoxynucleosides.
- Quantification:
- High-Performance Liquid Chromatography with Electrochemical Detection (HPLC-ECD) or Tandem Mass Spectrometry (HPLC-MS/MS): These chromatographic methods offer high sensitivity and specificity and are considered highly reliable [4].
- ELISA: Commercial ELISA kits provide a cost-effective and high-throughput alternative for large-scale studies. However, potential antibody cross-reactivity requires careful validation of the assay [4].
Oxidative Stress Pathways and Biomarker Origins
The biomarkers discussed originate from specific molecular pathways activated by reactive oxygen and nitrogen species. The following diagram illustrates the core mechanisms of oxidative stress and the biomolecular sources of key biomarkers.
The Researcher's Toolkit: Essential Reagents and Kits
The reliable measurement of oxidative stress biomarkers depends on specific research reagents and commercial kits. The table below details essential materials required for the experimental protocols cited in this guide.
Table 2: Essential Research Reagents and Kits for Oxidative Stress Biomarker Analysis
| Reagent / Kit | Biomarker Application | Function / Principle |
|---|---|---|
| DNPH (2,4-Dinitrophenylhydrazine) | Protein Carbonyls | Derivatizing agent that reacts with protein carbonyl groups to form a measurable hydrazone adduct [75]. |
| Anti-DNP Antibody | Protein Carbonyls | Antibody used in ELISA and immunoblotting to detect and quantify DNPH-derivatized protein carbonyls [75]. |
| Commercial Protein Carbonyl ELISA Kit | Protein Carbonyls | High-throughput kit providing pre-coated plates, standards, and antibodies for quantifying protein carbonyls in serum/plasma [75]. |
| SPE (Solid-Phase Extraction) Columns | F2-Isoprostanes | Used for the purification and concentration of F2-isoprostanes from urine or plasma prior to mass spectrometry analysis [4]. |
| 8-OHdG ELISA Kit | 8-OHdG | Immunoassay kit for the quantitative detection of 8-OHdG in urine, serum, or tissue homogenates, enabling high-throughput screening [4]. |
| TBARS Assay Kit | MDA (Malondialdehyde) | Colorimetric kit that measures thiobarbituric acid reactive substances (TBARS), a common but non-specific method for estimating lipid peroxidation [4]. |
| Spectrofluorometer | General / Multiple | Instrument used to measure the fluorescence of certain biomarkers or probes (e.g., AGE autofluorescence, DCFH-DA for intracellular ROS) [75] [4]. |
| HPLC-ECD / HPLC-MS/MS System | 8-OHdG, F2-Isoprostanes | High-performance liquid chromatography systems coupled with electrochemical (ECD) or tandem mass spectrometry (MS/MS) detectors for highly specific and sensitive biomarker quantification [4]. |
Conclusion
Oxidative stress biomarkers represent powerful tools for understanding disease mechanisms and developing targeted therapies, yet their effective application requires careful consideration of disease-specific patterns, methodological rigor, and integrated assessment approaches. The comparative analysis reveals that while certain markers like F2-isoprostanes and protein carbonyls show broad utility across multiple conditions, others demonstrate particular value in specific disease contexts. Future directions should focus on standardizing analytical methods, validating composite biomarker panels, and establishing clear clinical reference ranges. For drug development, these biomarkers offer promising endpoints for assessing therapeutic efficacy against oxidative damage, particularly as novel antioxidant strategies emerge. The continued refinement of oxidative stress biomarker applications will enhance both personalized medicine approaches and the development of targeted interventions for chronic inflammatory and metabolic diseases.
References
- 1. Oxidative Stress and Antioxidant Defense - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC3488923/]
- 2. Oxidative Stress - PMC - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC4300202/]
- 3. Oxidative Stress and Antioxidant Strategies: Relationships ... [https://www.mdpi.com/2073-4409/13/22/1871]
- 4. Linking oxidative stress biomarkers to disease progression ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1611842/full]
- 5. Clinical Evaluation of Oxidative Stress Markers in Patients with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12466392/]
- 6. Oxidative stress-related biomarkers as promising indicators of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11490685/]
- 7. Systemic Inflammation and Oxidative Stress Markers in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12537848/]
- 8. Oxidative Stress Biomarkers - an overview [https://www.sciencedirect.com/topics/veterinary-science-and-veterinary-medicine/oxidative-stress-biomarkers]
- 9. The impact of almond supplementation on oxidative stress ... [https://www.nature.com/articles/s41598-025-14701-w]
- 10. Redox-related biomarkers in human cardiovascular ... disease [https://pmc.ncbi.nlm.nih.gov/articles/PMC8113038/]
- 11. Biomarkers of Oxidative and Radical Stress [https://www.mdpi.com/2218-273X/14/2/194]
- 12. Oxidatively modified proteins in Alzheimer's disease (AD ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2818870/]
- 13. and Oxidative Damage Stress in... | Preprints.org DNA Biomarkers [https://www.preprints.org/manuscript/202510.0095]
- 14. Lipid peroxidation biomarkers for evaluating oxidative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3541426/]
- 15. Plasma lipid peroxidation biomarkers for early and non- ... [https://www.sciencedirect.com/science/article/abs/pii/S0891584918311596]
- 16. Protein oxidation - Formation mechanisms, detection and ... [https://www.sciencedirect.com/science/article/pii/S2213231721000495]
- 17. Pathophysiology and emerging biomarkers of ... [https://www.frontiersin.org/journals/cardiovascular-medicine/articles/10.3389/fcvm.2025.1661563/full]
- 18. Systematic Review of Metabolic Syndrome Biomarkers [https://pmc.ncbi.nlm.nih.gov/articles/PMC4716817/]
- 19. Identification of candidate metabolite biomarkers for metabolic ... [https://cardiab.biomedcentral.com/articles/10.1186/s12933-023-01862-z]
- 20. A Comprehensive Review of Biomarkers for Chronic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11512660/]
- 21. Emerging Biomarkers and Advanced Diagnostics in Chronic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12110191/]
- 22. A novel multiplex biomarker panel for profiling human ... [https://www.nature.com/articles/s41598-023-47418-9]
- 23. Biomarkers in Cardiovascular Disease - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC5253084/]
- 24. Dissecting the Crosstalk Between Nrf2 and NF-κB Response ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8847224/]
- 25. The crosstalk between Nrf2 and NF-κB pathways in ... [https://www.sciencedirect.com/science/article/abs/pii/S0024320523006422]
- 26. Oxidative Stress in Health and Disease - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC10669448/]
- 27. Targeting epigenetic and post-translational modifications of ... [https://www.nature.com/articles/s41420-025-02491-z]
- 28. The Nrf2/NF-κB signalling pathway and upstream factors of ... [https://www.sciencedirect.com/science/article/abs/pii/S0031942222003454]
- 29. Activation of Nrf2-antioxidant signaling attenuates NF-κB- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2610259/]
- 30. Oxidative stress response and NRF2 signaling pathway in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12099462/]
- 31. A Systematic Review and Network Meta-Analysis [https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2021.700055/full]
- 32. Antioxidant Nutrients and Chronic Disease: Use of ... [https://www.sciencedirect.com/science/article/pii/S0022316622157081]
- 33. Therapeutic Strategies Targeting Oxidative Stress and ... [https://www.mdpi.com/2673-6411/5/4/35]
- 34. Redox Imbalance in Inflammation: The Interplay of Oxidative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12189482/]
- 35. Oxidative Stress and Inflammation: From Mechanisms to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9031318/]
- 36. A guide to reactive oxygen species in tumour hypoxia [https://pmc.ncbi.nlm.nih.gov/articles/PMC12591319/]
- 37. Mitochondria in oxidative stress, inflammation and aging [https://www.nature.com/articles/s41392-025-02253-4]
- 38. The significance of reactive oxygen species in ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1540075/full]
- 39. Biomarkers of Oxidative Stress in Acute and Chronic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9495828/]
- 40. The Difference Between GC/MS and LC/MS Systems [https://conquerscientific.com/the-difference-between-gc-ms-and-lc-ms-systems/]
- 41. Comparison of LC–MS-MS and GC–MS Analysis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4885916/]
- 42. An overview of ELISA: a review and update on best laboratory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11808753/]
- 43. Comparison of Liquid Chromatography Mass Spectrometry ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7068296/]
- 44. Why are Sensitivity and Specificity Important Parameters ... [https://www.enzo.com/note/why-are-sensitivity-and-specificity-important-parameters-for-an-elisa/]
- 45. Comparison of Two ELISA Methods and Mass ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4945118/]
- 46. Comparison of three multiplex immunoassays for ... [https://www.nature.com/articles/s41598-025-23579-7]
- 47. Measurement and Clinical Significance of Biomarkers of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5494111/]
- 48. The Power of High-Throughput Omics Integration - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11417901/]
- 49. Advances and Trends in Omics Technology Development [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2022.911861/full]
- 50. High-Throughput Screening - Drug Discovery [https://www.technologynetworks.com/drug-discovery/articles/high-throughput-screening-principles-applications-and-advancements-405121]
- 51. Biomarkers of Oxidative Stress in Acute and Chronic ... [https://www.mdpi.com/journal/antioxidants/special_issues/biomarker_oxidative_disease]
- 52. High-Throughput Screening Products & Reviews [https://www.selectscience.net/products?techniques=high-throughput-screening]
- 53. Linking oxidative stress biomarkers to disease progression ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12146192/]
- 54. Oxidative Stress Fundamentals [https://www.mdpi.com/2076-3417/15/18/10191]
- 55. Urinary Biomarkers and Point-of-Care Urinalysis Devices ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10135468/]
- 56. Evaluation of lung oxidative stress and inflammatory state ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12539092/]
- 57. Urinary marker of oxidative stress in children correlates ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1511119/full]
- 58. Investigation of Oxidative DNA Damage Levels in Urine ... [https://www.mdpi.com/2305-6304/13/11/990]
- 59. Free radicals and their impact on health and antioxidant ... [https://www.nature.com/articles/s41420-024-02278-8]
- 60. How to assess antioxidant activity? Advances, limitations, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12572074/]
- 61. The various pathological roles of oxidized LDL in diseases [https://www.sciencedirect.com/science/article/abs/pii/S2451847625000661]
- 62. Spectrophotometric assays for total antioxidant capacity (TAC ... [https://bmcvetres.biomedcentral.com/articles/10.1186/s12917-016-0792-7]
- 63. Study on the correlation between oxidized low- density ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12065307/]
- 64. Comparison of Various Assays of Antioxidant Activity/ ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12346529/]
- 65. A Comparative Study on Oxidative Stability of Lipids ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12382763/]
- 66. Investigation of the Influence of Lipoprotein(a) ... [https://www.e-jla.org/DOIx.php?id=10.12997/jla.2025.14.2.229]
- 67. A systematic review and meta-analysis of clinical trials [https://www.sciencedirect.com/science/article/abs/pii/S0014299925002456]
- 68. Comparison of selfâ€administered survey questionnaire ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8152947/]
- 69. Oxidative balance score and its association with chronic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11796618/]
- 70. Research on the Compilation of a Composite Index ... [https://www.mdpi.com/2071-1050/15/19/14574?]
- 71. Comparison of nutritional screening and assessment tools ... [https://www.sciencedirect.com/science/article/pii/S2667268524000081]
- 72. Mobile health technology: a novel tool in chronic disease ... [https://www.sciencedirect.com/science/article/pii/S2667102621000346]
- 73. The Current State and Validity of Digital Assessment Tools for ... [https://mental.jmir.org/2022/3/e32824]
- 74. Diagnostic performance of microvascular flow imaging for ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0322102]
- 75. Clinical Relevance of Biomarkers of Oxidative Stress - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4657513/]
- 76. Oxidative Stress and Its Biomarkers in Cardiovascular Diseases [https://arteryresearch.biomedcentral.com/articles/10.1007/s44200-024-00062-8]
- 77. Making Sense of Oxidative Stress Markers: A Guide [https://www.jinfiniti.com/oxidative-stress-markers/?srsltid=AfmBOorviBsvkoo9eahzSUa2CqZ5LcEFopNL73pxDkwEiC2lwsGUk284]
- 78. Exploring the Interplay of Antioxidants, Inflammation, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12469104/]
- 79. Oxidative Stress Assay Market Size & Share Analysis [https://www.mordorintelligence.com/industry-reports/oxidative-stress-assay-market]
- 80. affecting the measurement of serum... Preanalytical variables [https://pmc.ncbi.nlm.nih.gov/articles/PMC7758704/]
- 81. Common and Novel Markers for Measuring Inflammation and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8001241/]
- 82. Measuring myokines with cardiovascular functions: pre - analytical ... [https://atm.amegroups.org/article/view/15688/html]
- 83. The Influence of Serum Sample Storage Conditions on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7168228/]
- 84. Impact of long-term storage and freeze-thawing on eight ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0227648]
- 85. Impact of Long-Term Cryopreservation on Blood Immune ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2020.582330/full]
- 86. The freeze – thaw effect on blood serum autofluorescence... cycle [https://pubs.rsc.org/en/content/articlelanding/2025/an/d4an01215a]
- 87. Oxidative stress and free radicals in disease pathogenesis [https://link.springer.com/article/10.1007/s44337-025-00303-y]
- 88. Frontiers | Oxidative balance score predicts chronic kidney disease ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1641496/full]
- 89. Exploring Biomarkers of Oxidative Stress in Health and ... [https://www.mdpi.com/journal/antioxidants/special_issues/6I161U0DR1]
- 90. JMIR Formative Research - Oxidative Markers and Prediction... Stress [https://formative.jmir.org/2025/1/e66509]
- 91. Association Between Oxidative–Inflammation Biomarkers ... [https://www.mdpi.com/2076-3921/14/8/975]
- 92. Identification of Oxidative Stress-Associated Biomarkers in ... [https://pubmed.ncbi.nlm.nih.gov/40161396/]
- 93. The Continuing Challenges of Translational Research [https://pmc.ncbi.nlm.nih.gov/articles/PMC3459259/]
- 94. Lost in translation: the valley of death across preclinical and ... [https://transmedcomms.biomedcentral.com/articles/10.1186/s41231-019-0050-7]
- 95. Nature Inspired Protective Agents Against Oxidative Stress [https://pmc.ncbi.nlm.nih.gov/articles/PMC8874147/]
- 96. Oxidative Stress: A Major Player in Cerebrovascular ... [https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2018.00806/full]
- 97. Effects of age and gender on the redox homeostasis ... [https://www.sciencedirect.com/science/article/pii/S0891584921004688]
- 98. Endothelial Dysfunction: Redox Imbalance, NLRP3 ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11939635/]
- 99. The Implication of Oxidative Stress on Human Aging and ... [https://www.mdpi.com/journal/antioxidants/special_issues/K07M310U4P]
- 100. Biomarkers in Alzheimer's Disease - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC3139171/]
- 101. Biomarkers and neuroimaging markers in Parkinson's disease [https://pmc.ncbi.nlm.nih.gov/articles/PMC12487944/]
- 102. Neuroimaging and fluid biomarkers in Parkinson's disease ... [https://www.nature.com/articles/s41467-024-49949-9]
- 103. Novel biomarkers for prediabetes, diabetes, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5565252/]
- 104. Cardiac Biomarkers - StatPearls - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK545216/]
- 105. Cardiac Biomarkers (Blood) [https://www.urmc.rochester.edu/encyclopedia/content?contenttypeid=167&contentid=cardiac_biomarkers]
- 106. Oxidative Stress Biomarkers as Preclinical Markers of Mild ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12113603/]
- 107. Mitochondrial dysfunction and oxidative stress in ... [https://pubmed.ncbi.nlm.nih.gov/40813952/]
- 108. Oxidative stress and inflammation in the pathogenesis of ... [https://www.sciencedirect.com/science/article/pii/S2211383524004040]
- 109. Redox imbalance and oxidative stress in cardiovascular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12550685/]
- 110. Profiling endothelial function, oxidative stress and ... [https://www.nature.com/articles/s41440-025-02392-9]
- 111. Oxidative stress markers and inflammation in type 1 and 2 ... [https://www.nature.com/articles/s41598-025-05818-z]
- 112. Measurement and Clinical Significance of Lipid Peroxidation as a Biomarker of Oxidative Stress: Oxidative Stress in Diabetes, Atherosclerosis, and Chronic Inflammation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6466575/]
- 113. Assessment of lipid peroxidation by measuring malondialdehyde (MDA) and relatives in biological samples: Analytical and biological challenges - PubMed [https://pubmed.ncbi.nlm.nih.gov/27789233/]
- 114. Protein oxidation - Formation mechanisms, detection and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8113053/]
- 115. Classifying oxidative stress by F2-Isoprostane levels in human disease: The re-imagining of a biomarker - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5413206/]
- 116. Proteomic quantification and identification of carbonylated ... [https://pubmed.ncbi.nlm.nih.gov/23689083/]
- 117. Proteomic quantification and identification of carbonylated ... [https://www.sciencedirect.com/science/article/abs/pii/S1874391913002492]
- 118. Isoprostanes and Neuroprostanes as Biomarkers of Oxidative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4020162/]
- 119. Cardiovascular risk prediction in type 2 diabetes [https://pmc.ncbi.nlm.nih.gov/articles/PMC8894164/]
- 120. The Complexity of Oxidative Stress in Human Age-Related ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12299016/]
- 121. Risk Prediction Score for Chronic Kidney Disease in ... [https://www.cdc.gov/pcd/issues/2023/22_0380.htm]
- 122. Comparison of four cardiovascular risk prediction functions ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4188120/]
- 123. Evidence Based Practice for Nursing Tutorial: Levels of ... [https://library-cuanschutz.libguides.com/Evidence/Levels]
- 124. Levels of Evidence - Evidence-Based Medicine [https://guides.library.stonybrook.edu/evidence-based-medicine/levels_of_evidence]
- 125. Understanding the Levels of Evidence in Medical Research [https://pmc.ncbi.nlm.nih.gov/articles/PMC12064251/]