The Dietary Inflammatory Index (DII) in Modern Research: A Comprehensive Guide to Assessment, Application, and Validation
This article provides a comprehensive resource for researchers and drug development professionals on the assessment of the Dietary Inflammatory Index (DII).
The Dietary Inflammatory Index (DII) in Modern Research: A Comprehensive Guide to Assessment, Application, and Validation
Abstract
This article provides a comprehensive resource for researchers and drug development professionals on the assessment of the Dietary Inflammatory Index (DII). It covers the foundational science linking diet to chronic inflammation and its role in disease pathogenesis, with examples from NAFLD, cancer, and metabolic syndrome. The guide details the DII's methodological framework, including calculation algorithms, data requirements, and application across study designs. It addresses common methodological challenges and optimization strategies, such as energy adjustment and cultural adaptation, as demonstrated by the new CHINA-DII. Finally, it explores validation techniques against inflammatory biomarkers like hs-CRP and comparative analysis with other dietary assessment tools, offering a holistic view for rigorous research application.
Understanding the Science: From Diet and Inflammation to the DII Framework
The Critical Link Between Chronic Inflammation and Disease Pathogenesis
Chronic inflammation is a sustained, low-grade immune response that plays a central role in the pathogenesis of numerous disorders, from metabolic and neurodegenerative conditions to cancer. Unlike acute inflammation, which resolves rapidly, chronic inflammation can persist for years and contributes to tissue damage, cellular dysfunction, and disease progression through complex molecular pathways [1]. The Dietary Inflammatory Index (DII) has emerged as a valuable research tool for quantifying the inflammatory potential of an individual's diet, enabling investigators to explore connections between dietary patterns, systemic inflammation, and disease risk [2] [3]. Understanding these connections is critical for developing targeted interventions across multiple disease states.
The molecular underpinnings of chronic inflammation involve a complex interplay of lipid mediators, cytokines, and immune cells. While acute inflammation is characterized by rapid resolution and restoration of homeostasis, chronic inflammation represents a maladaptive response that drives pathological changes across multiple organ systems [1]. This persistent inflammatory state creates a microenvironment conducive to disease progression through mechanisms that include oxidative stress, tissue remodeling, and cellular dysfunction.
Dietary Inflammatory Index: A Research Tool for Inflammation Assessment
DII Calculation Methodology and Protocol
The Dietary Inflammatory Index (DII) provides a standardized method for quantifying the inflammatory potential of an individual's diet based on scientific literature linking dietary components to inflammatory biomarkers. The development of DII originated from extensive review of approximately 2000 research articles examining relationships between 45 food parameters and six inflammatory biomarkers: IL-1β, IL-4, IL-6, IL-10, TNF-α, and CRP [2].
Protocol for DII Calculation:
- Dietary Data Collection: Administer a validated Food Frequency Questionnaire (FFQ) to assess habitual dietary intake. The FFQ should capture consumption frequency and portion sizes for a comprehensive list of food items [4].
- Food Parameter Selection: Identify available food parameters from the dietary data. While the original DII uses 45 parameters, researchers can calculate scores with a minimum of approximately 20 parameters from the desired list [2].
- Global Intake Comparison: Compare individual intake of each food parameter to a global reference database representing mean intakes from 11 populations worldwide [2] [4].
- Z-score Calculation: For each food parameter, calculate a Z-score using the formula: (individual mean intake - global mean intake) / global standard deviation [4].
- Percentile Conversion: Convert Z-scores to centered percentiles to achieve a symmetrical distribution bounded between -1 (maximally anti-inflammatory) and +1 (maximally pro-inflammatory) [5].
- Inflammatory Effect Scoring: Multiply each centered percentile value by the respective overall inflammatory effect score derived from literature to obtain food parameter-specific DII scores [5].
- Total DII Calculation: Sum all food parameter-specific DII scores to obtain an overall DII score for the individual [2] [5].
Table: Food Parameters for DII Calculation and Their Inflammatory Effects
| Pro-Inflammatory Parameters | Anti-Inflammatory Parameters | Neutral or Context-Dependent Parameters |
|---|---|---|
| Energy | Fiber | Alcohol |
| Carbohydrates | Vitamin D | Tea |
| Protein | Vitamin B6 | Caffeine |
| Total Fat | Riboflavin | |
| Saturated Fat | Folic Acid | |
| Cholesterol | Thiamin | |
| Trans Fat | Niacin | |
| Iron | Polyunsaturated Fatty Acids (PUFA) | |
| Vitamin B12 | Monounsaturated Fatty Acids (MUFA) | |
| Beta Carotene | ||
| Vitamin C | ||
| Vitamin A | ||
| Vitamin E | ||
| Zinc | ||
| Magnesium | ||
| Selenium |
Energy-Adjusted DII (E-DII) Protocol
For enhanced accuracy in research applications, the energy-adjusted DII (E-DII) is recommended to control for the effect of total energy intake. The E-DII is calculated per 1,000 calories of food consumed using the energy-standardized version of the world database [2] [4]. This adjustment is particularly important in studies where total caloric intake varies significantly between participants, as it isolates the inflammatory effect of dietary composition independent of quantity consumed.
DII Applications in Chronic Disease Research: Quantitative Evidence
Epidemiological studies across diverse populations have demonstrated significant associations between DII scores and chronic disease risk, providing evidence for the role of dietary patterns in disease pathogenesis through inflammatory pathways.
Table: DII Associations with Chronic Diseases from Recent Studies
| Disease Condition | Study Population | DII Association Measure | Key Findings |
|---|---|---|---|
| Cardiovascular Disease | 16,512 U.S. adults >60 years (NHANES 1999-2018) | OR = 1.05 per 1-unit DII increase [95% CI: 1.02, 1.09] | Highest DII quartile had 28% higher odds of CVD compared to lowest quartile [5] |
| Hypertension | 16,512 U.S. adults >60 years (NHANES 1999-2018) | OR = 1.03 per 1-unit DII increase [95% CI: 1.00, 1.06] | Significant positive association with DII scores [5] |
| Diabetes | 16,512 U.S. adults >60 years (NHANES 1999-2018) | OR = 1.17 for highest vs. lowest DII quartile | Strong association with pro-inflammatory dietary patterns [5] |
| ADHD | 500 Iranian children (200 cases, 300 controls) | OR = 1.133 per 1-unit E-DII increase [95% CI: 1.021, 1.258] | Significant association after adjusting for age, gender, BMI [4] |
| Multiple Chronic Conditions | 16,512 U.S. adults >60 years (NHANES 1999-2018) | β = 0.02 [95% CI: 0.01, 0.03], p = 0.003 | Each 1-unit DII increase associated with higher number of chronic diseases [5] |
Molecular Mechanisms Linking Pro-Inflammatory Diets to Disease
Pro-inflammatory diets contribute to disease pathogenesis through multiple interconnected biological mechanisms. In obesity, a TNF-α/stearate cooperative model drives IL-6 expression in 3T3-L1 adipocytes via an H3K9/18Ac-dependent mechanism, creating a pro-inflammatory adipose environment that exacerbates metabolic dysfunction [6]. Hypoxia in obese adipose tissue further amplifies inflammation and contributes to insulin resistance through complex metabolic dysregulation [6].
In neurodevelopmental conditions like ADHD, pro-inflammatory diets are hypothesized to disrupt neurodevelopment by impairing BDNF synthesis, altering neuronal migration via glial dysfunction, and modifying synaptic plasticity—mechanisms central to the disorder's cognitive and behavioral symptoms [4]. The association between higher E-DII scores and increased ADHD risk supports the involvement of inflammatory pathways in neurodevelopmental disorders.
Inflammatory Biomarkers in Disease Pathogenesis and Monitoring
Established and Emerging Inflammatory Biomarkers
Inflammatory biomarkers serve as measurable indicators of inflammatory processes and provide critical insights into disease mechanisms, progression, and therapeutic responses across various conditions.
Table: Key Inflammatory Biomarkers in Disease Pathogenesis
| Biomarker Category | Specific Biomarkers | Research and Clinical Applications |
|---|---|---|
| Cytokines | IL-1β, IL-6, TNF-α, IL-4, IL-10 | IL-6 and TNF-α drive acute neuroinflammation post-stroke; dynamic levels correlate with severity and prognosis [7] |
| Acute-Phase Proteins | CRP (including hs-CRP), Serum Amyloid A, Fibrinogen | CRP elevation assists in diagnosis, differential diagnosis of stroke subtypes, and prognostic evaluation [7] |
| Soluble Receptors | suPAR (soluble urokinase plasminogen activator receptor) | Promising serological predictor of mortality risk for emergency department patients [6] |
| Cellular Ratios | Neutrophil-to-Lymphocyte Ratio (NLR), Platelet-to-Lymphocyte Ratio (PLR), Systemic Immune-Inflammation Index (SII) | NLR and SII are powerful predictors of complications like stroke-associated pneumonia and poor functional outcomes [7] |
| Matrix Metalloproteinases | MMP-9 | Contributes to blood-brain barrier disruption in acute phase; facilitates tissue remodeling later [7] |
| Non-coding RNAs | miRNAs (miR-126, miR-155, miR-15a/16-1), lncRNAs | miRNAs regulate gene expression post-transcriptionally; identified as key modulators of immune cell differentiation [6] [7] |
| Novel Biomarkers | Galectin-3 (Gal-3) | Released by activated microglia; promotes inflammation via TLR-4/NF-κB pathway; elevated levels associated with poor 90-day outcomes [7] |
Biomarker Applications in Precision Medicine
Inflammatory biomarkers are increasingly guiding personalized treatment approaches across medical specialties. In ischemic stroke, specific inflammatory profiles help distinguish between stroke subtypes (e.g., atherosclerotic vs. cardioembolic), forming a basis for personalized treatment strategies [7]. Biomarkers also provide crucial insights for endovascular thrombectomy, with pre-operative SII and post-operative NLR predicting poor prognosis, while the fibrinogen-to-albumin ratio (FAR) indicates hemorrhagic transformation risk [7].
In dermatology, the assessment of cytokines and chemokines serves as a complementary diagnostic tool for inflammatory skin diseases, revealing distinct inflammatory signatures that guide targeted therapies for conditions like hidradenitis suppurativa and psoriasis [8]. The exploration of proteomic signatures in inflammatory skin diseases has further enriched understanding of disease pathogenesis and systemic inflammation [8].
Experimental Protocols for Inflammation Research
Protocol: Assessing DII and Hematological Inflammatory Markers in Depression
Background: This protocol examines relationships between dietary inflammatory potential and hematological inflammatory markers in depressed and healthy individuals, based on a cross-sectional analysis in the PERSIAN Organizational Cohort Study [9].
Materials and Reagents:
- Validated 118-item semi-quantitative Food Frequency Questionnaire (FFQ)
- Depression, Anxiety, and Stress Scale-21 (DASS-21) questionnaire
- Equipment for venipuncture and blood collection tubes
- Automated hematology analyzer for complete blood count (CBC)
- Lipid profile analysis reagents for HDL-C measurement
- Nutritionist IV software or equivalent for dietary analysis
Methodology:
- Participant Recruitment and Classification:
- Recruit participants aged 30-70 years through stratified sampling
- Administer DASS-21 questionnaire to classify participants as healthy (score 0-9) or depressed (score ≥10)
- Exclude participants with daily energy consumption <800 kcal or >4200 kcal
Dietary Assessment and DII Calculation:
- Conduct FFQ interviews with participants guided by trained nutritionists
- Collect data on consumption frequency and typical portion sizes over the past year
- Convert reported intakes to grams per day using household portion sizes
- Calculate DII scores using 37 dietary components (29 anti-inflammatory, 8 pro-inflammatory)
Blood Collection and Analysis:
- Collect blood samples after 10-12 hour fasting period
- Perform complete blood count (CBC) to assess RBC, WBC, hematocrit, platelet count, and RDW
- Conduct lipid profile analysis to measure HDL-C levels
- Calculate hematological inflammatory markers using formulas:
- Platelet-to-HDL ratio (PHR) = Platelet/HDL
- Monocyte-to-HDL ratio (MHR) = Monocyte/HDL
- Lymphocyte-to-HDL ratio (LHR) = Lymphocyte/HDL
- Additional ratios as required
Statistical Analysis:
- Express continuous data as mean ± standard deviation, categorical data as frequency (%)
- Use chi-square test for qualitative data, ANOVA for quantitative data
- Apply multinomial regression model with DII tertile as dependent variable
- Adjust for age, sex, smoking status, BMI, and physical activity
- Consider p-value <0.05 as statistically significant
Key Findings Application: In healthy individuals, a pro-inflammatory diet (tertile 3 vs. tertile 1) decreased monocyte counts by 25.1% (OR: 0.749) and LHR by 11% (OR: 0.89), while increasing MHR by 12.9% (OR: 1.129). No significant correlation was observed in depressed individuals, highlighting potential differences in inflammatory regulation between these groups [9].
Protocol: Cross-Sectional Analysis of DII and Chronic Diseases in Aging Populations
Background: This protocol outlines methods for investigating associations between DII and chronic diseases in older adults using NHANES data, applicable to large-scale epidemiological studies [5].
Materials:
- NHANES demographic, dietary, and health questionnaire data
- 24-hour dietary recall data
- Chronic disease ascertainment criteria (CVD, hypertension, diabetes, COPD, cancer)
- Statistical software capable of handling complex survey designs (e.g., R with "survey" package)
Methodology:
- Study Population Selection:
- Include adults aged >60 years from NHANES cycles
- Exclude participants with missing chronic disease data or parameters needed for DII calculation
DII Calculation from NHANES Data:
- Utilize dietary data from day one 24-hour dietary recall interviews
- Calculate DII using available food parameters (typically 28 in NHANES)
- Apply standard DII calculation protocol with global reference values
Chronic Disease Ascertainment:
- Cardiovascular disease: Self-reported history of coronary heart disease, congestive heart failure, heart attack, stroke, or angina
- Hypertension: Self-report, blood pressure >140/90mmHg, or use of anti-hypertensives
- Diabetes: Doctor diagnosis, HbA1c ≥6.5%, fasting glucose ≥7.0 mmol/L, or use of anti-diabetic medication
- COPD: Based on self-report, pre-bronchodilator FEV1/FVC ratio <0.7, or use of related drugs
- Cancer: Based on self-reported doctor diagnosis
Statistical Analysis:
- Categorize participants into DII quartiles
- Use logistic regression to estimate Odds Ratios (OR) and 95% confidence intervals for chronic diseases across DII quartiles
- Employ linear regression to assess association between DII score and number of chronic diseases
- Apply NHANES sampling weights and account for complex survey design
- Develop adjusted models:
- Model 1: Adjust for age and sex
- Model 2: Additionally adjust for smoking status, drinking status, BMI, ethnicity, poverty, marital status, education, annual family income, and citizenship
Research Reagent Solutions for Inflammation Studies
Table: Essential Research Reagents for Dietary Inflammation and Biomarker Studies
| Reagent Category | Specific Products/Assays | Research Applications |
|---|---|---|
| Dietary Assessment Tools | Validated Food Frequency Questionnaires (FFQ), 24-hour dietary recall protocols, Nutritionist IV software | Standardized assessment of dietary intake for DII calculation [4] [9] |
| Inflammatory Cytokine Assays | ELISA kits for IL-1β, IL-6, TNF-α, IL-4, IL-10; Multiplex bead-based arrays | Quantification of inflammatory mediators in serum, plasma, or other biological samples [2] [7] |
| Acute Phase Protein Tests | High-sensitivity CRP (hs-CRP) immunoassays, Fibrinogen test kits | Measurement of established inflammatory biomarkers for correlation with DII scores [6] [7] |
| Hematological Analysis | Complete Blood Count (CBC) with differential analyzers, Automated hematology systems | Determination of cellular inflammatory ratios (NLR, PLR, MHR, etc.) [9] |
| Molecular Biology Reagents | miRNA extraction kits, qPCR assays for specific miRNAs (miR-126, miR-155, miR-15a/16-1), Galectin-3 ELISA kits | Analysis of novel inflammatory biomarkers and their relationship to dietary patterns [6] [7] |
| Lipid Mediator Profiling | Mass spectrometry kits for specialized pro-resolving mediators (SPMs), ELISA for prostaglandins (PGE2) | Comprehensive analysis of lipid inflammatory mediators in research settings [1] |
Signaling Pathways in Diet-Induced Inflammation
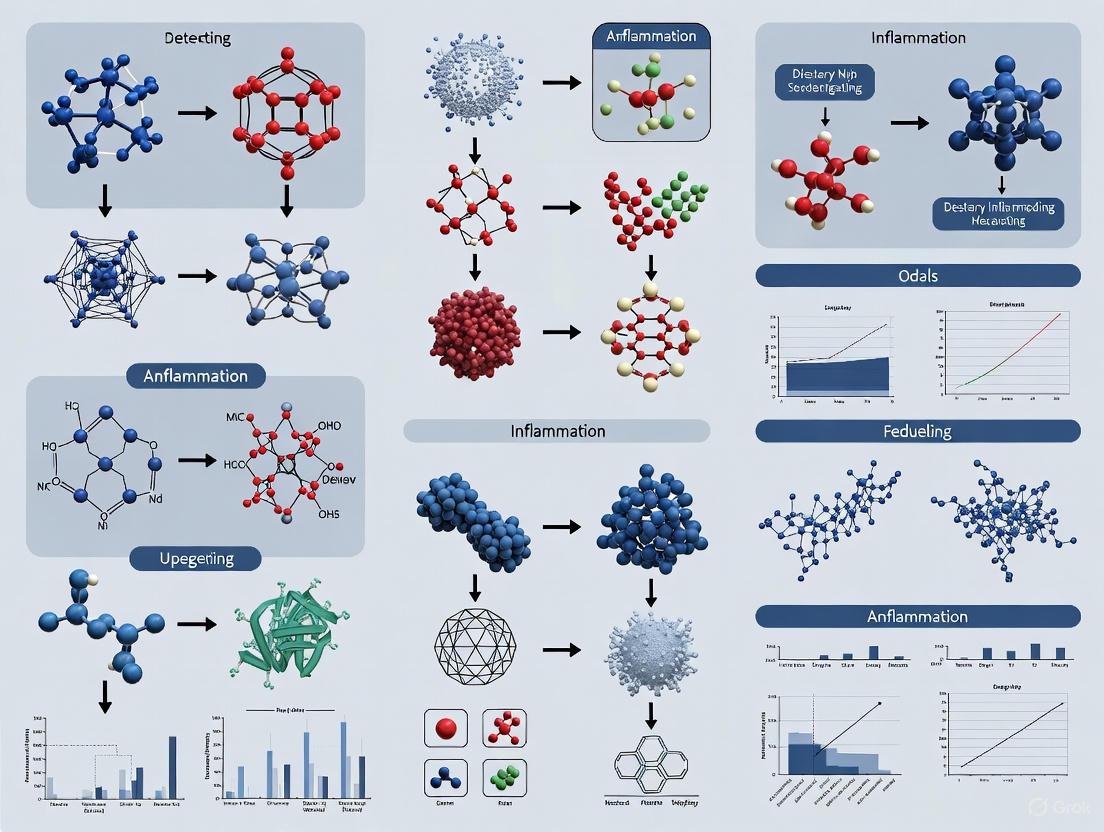
Diagram: Dietary Regulation of Inflammatory Pathways
This diagram illustrates the molecular mechanisms through which pro-inflammatory and anti-inflammatory diets modulate chronic inflammation and disease pathogenesis. Pro-inflammatory diets rich in processed fats and sugars initiate damage-associated molecular pattern (DAMP) release, triggering Toll-like receptor (TLR) activation and nuclear factor kappa-B (NF-κB) pathway signaling [7]. This cascade increases pro-inflammatory cytokine production (IL-1β, IL-6, TNF-α), promoting immune cell infiltration and tissue damage that drives chronic disease development [7] [1]. Conversely, anti-inflammatory diets stimulate production of specialized pro-resolving mediators (SPMs) and anti-inflammatory cytokines (IL-4, IL-10) that actively promote inflammation resolution and tissue homeostasis [1].
The critical link between chronic inflammation and disease pathogenesis underscores the importance of dietary patterns as modifiable risk factors across multiple disease states. The Dietary Inflammatory Index provides researchers with a validated, quantitative tool for assessing the inflammatory potential of diets in population studies and clinical trials. Evidence from recent studies demonstrates significant associations between higher DII scores and increased odds of cardiovascular disease, diabetes, hypertension, and neurodevelopmental disorders like ADHD [4] [5].
Future research directions should focus on validating DII associations in diverse populations, elucidating precise molecular mechanisms linking dietary components to inflammatory pathways, and developing targeted anti-inflammatory dietary interventions for specific disease states. The integration of novel inflammatory biomarkers, including non-coding RNAs and cellular ratios, with DII assessment will enhance our understanding of the diet-inflammation-disease axis and advance the development of personalized nutrition strategies for chronic disease prevention and management.
Chronic inflammation is a well-established contributor to the pathogenesis of numerous chronic diseases, including cancer, cardiovascular disease, and metabolic disorders [10]. The scientific understanding that dietary components significantly modulate inflammatory pathways created a pressing need for a standardized tool to quantify the overall inflammatory potential of an individual's diet. Prior to the development of the Dietary Inflammatory Index (DII), researchers relied on dietary pattern analyses or individual food components, which lacked a comprehensive, evidence-based foundation specifically targeting inflammation [11]. The DII was conceived to fill this methodological gap by providing a literature-derived, validated tool that could consistently evaluate the inflammatory potential of diets across diverse populations and research settings, thereby offering a quantitative means for assessing the role of diet in relation to health outcomes.
Historical Development and Methodological Evolution
The development of the DII represents a significant methodological advancement in nutritional epidemiology. The first version debuted in 2009, based on a systematic review of 927 peer-reviewed articles published through 2007 that linked dietary components to specific inflammatory biomarkers [11]. This foundational work established the principle of scoring dietary components according to their inflammatory effects.
Critical Enhancements in the Revised DII
Recognizing limitations in the original approach, developers created a substantially improved version. The revised DII, introduced in 2014, incorporated several critical methodological enhancements that increased its robustness and applicability [11]:
- Expanded Evidence Base: The literature review was updated through 2010, more than doubling the qualifying articles to 1,943, providing a more robust evidence foundation for scoring dietary parameters.
- Global Intake Reference: Instead of using raw consumption amounts, reported dietary intakes were linked to a composite global database constructed from 11 population-based surveys worldwide, enabling standardized z-score calculation relative to global norms.
- Inclusion of Flavonoids: Six categories of flavonoids (anthocyanidins, flavan-3-ols, flavonols, flavonones, isoflavones, and flavones) were added as important modulators of inflammation.
- Scoring Algorithm Refinement: The scoring system was inverted so that more anti-inflammatory scores are negative and more pro-inflammatory scores are positive, providing more intuitive interpretation.
Table 1: Evolution of Dietary Inflammatory Index (DII) Versions
| Feature | Original DII (2009) | Revised DII (2014) |
|---|---|---|
| Evidence Base | 927 articles (through 2007) | 1,943 articles (through 2010) |
| Dietary Parameters | Limited set of nutrients | 45 parameters, including flavonoids |
| Reference Database | Raw consumption amounts | Global composite database (11 populations) |
| Scoring Direction | Less intuitive | Negative (anti-inflammatory) to positive (pro-inflammatory) |
| Application | Limited research use | >200 studies and 12 meta-analyses to date |
DII Calculation: Standardized Methodology
Computational Protocol
The DII calculation follows a standardized protocol that can be adapted to various dietary assessment methods, including Food Frequency Questionnaires (FFQs), 24-hour recalls, and food records [10] [11]. The computational workflow involves these critical steps:
- Dietary Data Collection: Obtain complete dietary intake data using a validated assessment tool (e.g., 168-item FFQ).
- Parameter Alignment: Link individual food consumption data to the 45 DII food parameters, calculating daily intake amounts for each.
- Global Standard Comparison: For each parameter, calculate a z-score by comparing the individual's intake to the global mean and standard deviation:
z = (individual intake - global mean)/global standard deviation. - Percentile Conversion: Convert z-scores to percentiles to achieve a uniform distribution (value range: 0 to 1).
- Centering: Multiply each percentile by 2 and subtract 1 to center the values around zero (value range: -1 to +1).
- Inflammatory Scoring: Multiply each centered value by its respective inflammatory effect score (derived from literature review).
- DII Summation: Sum all values to obtain the total DII score for the individual.
Energy Adjustment Protocol
For studies where total energy intake may confound results, the Energy-Adjusted DII (E-DII) is recommended using the residual method:
- Regression Model: Regress each DII parameter on total energy intake using a linear regression model.
- Residual Calculation: Obtain the residuals from each regression, representing the variation in nutrient intake independent of total energy intake.
- Standardized Residuals: Add the expected nutrient value for mean energy intake to each residual to maintain meaningful scale.
- DII Calculation: Use these energy-adjusted values in the standard DII computation protocol.
Validation Studies: Establishing Predictive Utility
The validity of the DII has been established through numerous studies examining its relationship with inflammatory biomarkers and disease endpoints across diverse populations.
Inflammatory Biomarker Validation
A case-control study conducted in Iran demonstrated strong correlation between DII scores and specific inflammatory markers among gastric cancer patients and controls [10]. After adjusting for age, sex, BMI, education, smoking, alcohol, H. pylori infection, physical activity, aspirin/NSAID use, and total caloric intake, researchers found that for every one-unit increase in DII score, there was a statistically significant increase in hs-C-reactive protein (β=0.09), tumor necrosis factor-alpha (β=0.16), interleukin-6 (β=0.16), and IL-1b (β=0.10), with a corresponding decrease in the anti-inflammatory cytokine IL-10 (β=-0.11). This biomarker validation confirms that the DII accurately reflects the inflammatory status predicted by dietary composition.
Disease Endpoint Validation
The DII has demonstrated predictive validity for various disease outcomes:
- Gastric Cancer: In a fully adjusted model, subjects with DII scores > -1.77 had 3.39 times higher odds of gastric cancer (95% CI: 1.59-7.22) compared to those with lower DII scores [10].
- Chronic Obstructive Pulmonary Disease (COPD): Analysis of NHANES 2013-2018 data revealed that a one-unit increase in DII was associated with increased COPD risk (OR=1.05; 95% CI: 1.09-1.21; P=0.007). Those in the highest DII quartile had 1.34 times higher odds of COPD (95% CI: 1.01-1.77) compared to the lowest quartile [12].
- Menopausal Symptoms: Research in postmenopausal women showed both DII and food-based FDII were significantly associated with severity of sexual symptoms, with the lowest tertile of DII having substantially lower odds of severe symptoms (OR=0.252, P=0.002) compared to the highest tertile [13].
Table 2: DII Validation Across Health Outcomes
| Health Outcome | Study Design | Population | Key Finding | Adjustment Factors |
|---|---|---|---|---|
| Gastric Cancer | Case-control | 82 cases/95 controls (Iran) | OR=3.39 for high DII (95% CI: 1.59-7.22) | Age, sex, BMI, education, smoking, alcohol, H. pylori, physical activity, NSAIDs, calories |
| COPD | Cross-sectional | NHANES 2013-2018 (US) | OR=1.34 for highest vs. lowest DII quartile (95% CI: 1.01-1.77) | Age, sex, ethnicity, education, income, smoking, physical activity, comorbidities |
| Menopausal Symptoms | Cross-sectional | 149 postmenopausal women (Iran) | OR=0.252 for low DII sexual symptoms (P=0.002) | Age, BMI, physical activity, socioeconomic status |
| Inflammatory Biomarkers | Laboratory analysis | 177 participants (Iran) | Significant correlations with CRP, TNF-α, IL-6, IL-1β, IL-10 | Multiple covariate adjustment |
Research Applications and Adaptations
Food-Based DII (FDII) Development
Recognizing that people consume foods rather than isolated nutrients, researchers developed food-based adaptations. The Food-Based DII (FDII) uses specific food groups rather than nutrients to assess inflammatory potential [13]. The Iranian FDII version incorporates 28 food groups (13 anti-inflammatory and 15 pro-inflammatory), providing a more practical tool for dietary guidance while maintaining strong predictive validity for health outcomes like menopausal symptoms.
Implementation Workflow for Research Studies
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Materials for DII Studies
| Item Category | Specific Examples | Research Function | Protocol Notes |
|---|---|---|---|
| Dietary Assessment Tools | Validated FFQ (168-item), 24-hour recall protocols, Food records | Captures comprehensive dietary intake | Must include all 45 DII parameters; consider cultural adaptations |
| Laboratory Reagents | ELISA kits for CRP, TNF-α, IL-6, IL-1β, IL-10 | Biomarker validation of DII scores | Ensure proper sample collection after 10-12 hour fast [10] |
| Statistical Software | R, Python, SAS, Stata, SPSS | DII calculation and statistical analysis | Requires custom coding for DII algorithm; packages available |
| Reference Databases | Global composite database (means/SDs for 45 parameters) | Standardized z-score calculation | Provided by DII developers; essential for standardized scoring |
| Biomedical Literature | 1,943 qualifying articles on diet-inflammation links | Basis for inflammatory effect scores | Continuously updated evidence base |
| MG-262 | MG-262, CAS:179324-22-2, MF:C25H42BN3O6, MW:491.4 g/mol | Chemical Reagent | Bench Chemicals |
| Midostaurin (Standard) | Midostaurin|CAS 120685-11-2|Research Grade | Bench Chemicals |
The Dietary Inflammatory Index has evolved from a conceptual framework to a fully validated research tool with demonstrated utility across diverse populations and health outcomes. Its development represents a significant methodological advancement in nutritional epidemiology, providing an evidence-based approach to quantify the inflammatory potential of overall diet rather than focusing on isolated nutrients. The rigorous validation against inflammatory biomarkers and disease endpoints strengthens its credibility for research applications. Future development directions include continued refinement of scoring based on emerging evidence, creation of population-specific adaptations, and exploration of clinical applications for personalized nutrition interventions. As research continues, the DII provides a robust framework for investigating the critical relationship between diet, inflammation, and human health.
The Dietary Inflammatory Index (DII) is a literature-derived, quantitative tool designed to assess the inflammatory potential of an individual's diet. Unlike dietary indexes based on dietary recommendations or specific cuisines, the DII was developed through systematic evaluation of peer-reviewed literature linking dietary parameters to inflammatory biomarkers [11]. This evidence-based approach allows the DII to provide a universal assessment method applicable across diverse populations and study designs, addressing a critical gap in nutritional epidemiology by moving beyond narrow exposure variability inherent in other indexes [11]. The DII represents a paradigm shift in nutritional science, enabling researchers to quantify how specific dietary components collectively influence systemic inflammation, which serves as a fundamental mechanism underlying many chronic diseases.
Theoretical Foundation and Development
Historical Context and Evolution
Development of the DII began in 2004 in response to rapidly growing understanding of inflammation's role in health and diet's influence on inflammatory processes. The first version debuted in 2009, scoring 927 peer-reviewed articles published through 2007 that linked diet to inflammatory biomarkers [11]. This initial version, while pioneering, failed to gain significant traction in the biomedical community. The revised DII incorporated several critical enhancements based on lessons learned from the original, including: linking reported dietary intake to global norms rather than using raw consumption amounts; incorporating three additional years of literature (through 2010), which more than doubled the evidence base to 1,943 articles; adding flavonoids as important modulators of inflammation; and inverting the scoring algorithm so that anti-inflammatory scores are negative and proinflammatory scores are positive [11].
Inflammatory Biomarkers and Dietary Parameters
The DII development focused on six core inflammatory biomarkers: IL-1β, IL-4, IL-6, IL-10, TNF-α, and C-reactive protein (CRP) [11]. These biomarkers were selected based on their established roles in systemic inflammation and clinical relevance. The dietary parameters were not constrained in advance but emerged from systematic literature review, ultimately comprising 45 food parameters that encompass macronutrients, micronutrients, flavonoids, and other bioactive food components. This comprehensive approach ensures the DII captures the complex, multifaceted nature of diet-inflammation relationships.
Table 1: Core Inflammatory Biomarkers in DII Development
| Biomarker | Primary Role in Inflammation | Clinical Significance |
|---|---|---|
| IL-1β | Pro-inflammatory cytokine | Mediates acute phase response, involved in autoimmune diseases |
| IL-4 | Anti-inflammatory cytokine | Regulates immune response, suppresses pro-inflammatory cytokines |
| IL-6 | Pro-inflammatory cytokine | Induces acute phase proteins, including CRP |
| IL-10 | Anti-inflammatory cytokine | Potent anti-inflammatory, inhibits cytokine production |
| TNF-α | Pro-inflammatory cytokine | Central regulator of inflammatory response |
| CRP | Acute phase protein | Clinical marker of systemic inflammation |
Methodological Framework
Algorithm Development and Scoring System
The DII scoring algorithm transforms individual dietary intake data into a standardized inflammatory potential score through a multi-step process. First, individual intake of each food parameter is compared to a global reference database derived from 11 population-based surveys from around the world, including Australia, Bahrain, Denmark, India, Japan, Mexico, New Zealand, South Korea, Taiwan, the United Kingdom, and the United States [11]. This global composite provides means and standard deviations for each parameter, enabling calculation of z-scores that represent individual intake relative to global norms.
The algorithm proceeds through these computational steps:
- Z-score Calculation: Individual intake values are converted to z-scores relative to the global mean and standard deviation for each parameter
- Percentile Conversion: Z-scores are converted to percentiles (ranging from 0 to 1) to address right-skewing common in dietary data
- Centering: Percentiles are centered by multiplying by 2 and subtracting 1, creating a distribution with approximately equal negative and positive values
- Inflammatory Effect Score: Each centered value is multiplied by the respective food parameter's inflammatory effect score derived from literature review
- DII Summation: All parameter scores are summed to create the overall DII score
This sophisticated approach eliminates the arbitrariness of using raw consumption amounts and minimizes potential biases from skewed dietary intake distributions [11].
Global Reference Database
The global reference database forms the foundation for DII calculation, providing contextual framework for interpreting individual dietary intake. The composite dataset represents diverse dietary patterns across multiple continents and cultures, ensuring the DII's applicability across different populations and geographic regions. This global perspective is crucial for creating a universally relevant index that transcends specific dietary traditions or national guidelines.
Table 2: DII Food Parameters and Inflammatory Effects
| Parameter Category | Specific Components | General Inflammatory Effect |
|---|---|---|
| Macronutrients | Carbohydrates, protein, total fat, saturated fat, cholesterol | Varies by component (e.g., saturated fat pro-inflammatory) |
| Micronutrients | Vitamins A, B, C, D, E; iron, zinc, selenium, magnesium | Mostly anti-inflammatory |
| Flavonoids | Anthocyanidins, flavan-3-ols, flavonols, flavonones, isoflavones, flavones | Predominantly anti-inflammatory |
| Other Bioactives | Fiber, caffeine, garlic, ginger, onion, tea, turmeric | Mostly anti-inflammatory |
| Fatty Acids | Omega-3, omega-6, monounsaturated fatty acids | Varies (omega-3 anti-inflammatory, omega-6 pro-inflammatory) |
Practical Application and Protocols
Data Collection Requirements
Implementing the DII in research requires comprehensive dietary assessment capturing intake of all 45 parameters. Recommended methodologies include:
- Standardized Food Frequency Questionnaires (FFQ): Validated instruments that assess usual dietary intake over specified periods
- 24-Hour Dietary Recalls: Multiple recalls providing detailed intake data, preferably collected on non-consecutive days
- Dietary Records: Weighed or estimated food records maintained by participants for specified periods
Dietary assessment tools must be appropriately validated for the specific population under study and should capture intake of all DII parameters, including the recently added flavonoids [11]. The choice of assessment method depends on study objectives, population characteristics, and resource constraints.
Computational Protocol
The following workflow details the step-by-step procedure for calculating DII scores from raw dietary data:
Step-by-Step Protocol:
- Data Preparation: Compile individual intake data for all 45 food parameters, ensuring consistent units with the global reference database
- Z-score Computation: For each parameter, calculate z-score = (individual intake - global mean) / global standard deviation
- Percentile Transformation: Convert z-scores to percentiles using standard normal distribution
- Value Centering: Transform percentiles to centered scores: centered value = (percentile × 2) - 1
- Inflammatory Weighting: Multiply each centered value by the respective food parameter's inflammatory effect score from literature
- Score Aggregation: Sum all weighted parameter scores to obtain the overall DII score
- Validation Checks: Verify calculations and assess score distribution for outliers or errors
Energy Adjustment Protocol
Energy intake correlates with both dietary exposure and inflammatory outcomes, necessitating appropriate adjustment. The Energy-Adjusted DII (E-DII) is calculated using nutrient densities rather than absolute intakes:
- Calculate Nutrient Densities: Divide each nutrient intake by total energy intake (nutrient amount per 1000 kcal)
- Reference Database Standardization: Use energy-adjusted global norms for comparison
- Standard DII Computation: Apply standard DII algorithm to energy-adjusted values
This approach eliminates confounding by total energy intake and provides a more accurate assessment of dietary composition effects on inflammation [11].
Research Implementation Toolkit
Essential Research Reagents and Materials
Table 3: Research Reagent Solutions for DII Implementation
| Reagent/Material | Specification | Research Function |
|---|---|---|
| Validated FFQ | Population-specific, comprehensive | Captures usual intake of all DII parameters |
| Global Reference Database | Composite of 11 population surveys | Provides normative data for z-score calculation |
| Inflammatory Effect Scores | Literature-derived weights | Quantifies inflammatory impact of each food parameter |
| Statistical Software | R, SAS, SPSS, or Stata with custom macros | Performs DII algorithm calculations |
| Biomarker Assay Kits | High-sensitivity CRP, cytokine panels | Validates DII against inflammatory biomarkers |
| Mifentidine | Mifentidine|CAS 83184-43-4|H2-Receptor Antagonist | Mifentidine is a potent, long-acting H2-receptor antagonist for peptic ulcer disease research. For Research Use Only. Not for human use. |
| Miglitol | Miglitol|CAS 72432-03-2|Alpha-Glucosidase Inhibitor | Miglitol is an oral anti-diabetic agent for research. It acts as an alpha-glucosidase inhibitor to delay carbohydrate absorption. For Research Use Only. |
Quality Control Measures
Implement rigorous quality control procedures throughout DII assessment:
- Dietary Data Collection: Standardize interviewer training, use multiple-pass methods for recalls, implement real-time data checking
- Data Processing: Double-entry verification, range checks for implausible values, cross-check nutrient calculations
- DII Computation: Independent verification of algorithmic implementation, check score distributions against expected ranges
- Validation Studies: Conduct preliminary analyses correlating DII scores with inflammatory biomarkers in subset of population
Interpretation and Validation
Score Interpretation Guidelines
DII scores form a continuous scale where:
- Positive Values: Indicate pro-inflammatory dietary pattern
- Negative Values: Indicate anti-inflammatory dietary pattern
- Magnitude: Reflects strength of inflammatory potential, with higher absolute values indicating stronger effects
The DII does not have established categorical cut-points, as inflammatory potential exists on a continuum. Researchers may categorize scores into quantiles (quartiles, quintiles) based on population-specific distributions for analysis. Comparative interpretation should reference published DII values in similar populations, as absolute values may vary across study populations and dietary assessment methods.
Validation Studies and Evidence Base
The DII has been extensively validated against inflammatory biomarkers and health outcomes. Validation protocols include:
- Biomarker Validation: Correlating DII scores with circulating levels of CRP, IL-6, TNF-α, and other inflammatory markers
- Clinical Outcome Validation: Assessing DII's ability to predict incidence of inflammation-related chronic diseases
- Cross-population Consistency: Evaluating DII performance across diverse populations and geographic regions
To date, the DII has been used in over 200 studies and forms the basis for 12 meta-analyses, demonstrating robust associations with various health outcomes including cancers, cardiovascular diseases, depression, and maternal-child health outcomes [11]. This substantial evidence base supports the DII's validity as a measure of dietary inflammatory potential.
Advanced Methodological Considerations
Population-Specific Adaptations
While the DII was designed for universal application, researchers should consider population-specific factors:
- Cultural Dietary Patterns: Ensure dietary assessment instruments adequately capture culturally-specific foods
- Flavonoid Intake: Pay particular attention to assessment of flavonoid-rich foods relevant to specific cuisines
- Genetic Variants: Consider effect modification by genetic polymorphisms in inflammatory pathways
- Life Stage Considerations: Account for varying nutrient requirements across life stages (pregnancy, aging)
Integration with Other Methodologies
The DII can be enhanced through integration with complementary approaches:
- Omics Technologies: Combine with metabolomic profiling to identify biological pathways linking diet to inflammation
- Biomarker Measurement: Incorporate multiple inflammatory biomarkers to create multidimensional inflammation assessment
- Longitudinal Analysis: Apply DII in repeated measures designs to assess how changes in dietary patterns affect inflammatory trajectories
The DII's framework continues to evolve as new evidence emerges, ensuring it remains at the forefront of nutritional epidemiology and inflammatory research.
The Dietary Inflammatory Index (DII) is a quantitative tool designed to assess the inflammatory potential of an individual's diet. Developed by Shivappa and colleagues, the DII scoring algorithm is based on an extensive review of the scientific literature linking dietary components to six inflammatory biomarkers: IL-1β, IL-4, IL-6, IL-10, TNF-α, and CRP [14]. The index incorporates up to 45 food parameters, including specific nutrients, compounds, and food groups, each classified based on their pro- or anti-inflammatory properties [15] [3]. A higher DII score indicates a more pro-inflammatory diet, while a lower (more negative) score indicates a more anti-inflammatory diet [16]. The DII has been validated in various populations and serves as a powerful epidemiological tool for investigating the relationship between diet-induced inflammation and chronic disease risk, making it particularly valuable for researchers and drug development professionals studying disease mechanisms and preventive strategies.
The DII and Non-Alcoholic Fatty Liver Disease (NAFLD)
Epidemiological Evidence
Accumulating evidence from observational studies and meta-analyses demonstrates a significant association between higher DII scores (pro-inflammatory diets) and an increased risk of NAFLD, now also termed Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD).
Table 1: Summary of Key Studies on DII and NAFLD/MASLD
| Study Type | Population | Key Finding | Effect Size (OR/HR, 95% CI) | Citation |
|---|---|---|---|---|
| Cross-Sectional | 3,456 US adults (NHANES) | A one-SD increase in DII increased fatty liver risk. | OR: 1.21 (Not reported) | [15] |
| Cross-Sectional | 125 Iranian children (7-18 yrs) | Each unit increase in DII linked to higher odds of severe steatosis. | OR: 2.61 (1.28 - 5.32) | [16] |
| Meta-Analysis | 11 observational studies | Higher DII associated with increased NAFLD risk in cross-sectional studies. | Pooled OR: 1.56 (1.24 - 1.95) | [17] |
| Cohort | 2 UK Biobank studies | Higher DII associated with severe NAFLD risk. | HR: 0.21 (0.12 - 0.30)* | [17] |
| Cross-Sectional | 125 Iranian children (7-18 yrs) | Inflammatory diets (DII > +1) linked to more severe steatosis vs. anti-inflammatory. | OR: 4.11 (1.08 - 15.71) | [16] |
Note: The cohort study HR of 0.21 appears to be a reporting discrepancy; the original finding likely indicates increased risk.
Protocol: Assessing DII-NAFLD Association in an Observational Cohort
Objective: To investigate the association between dietary inflammatory potential, measured by the DII, and the incidence and severity of NAFLD/MASLD in an adult population.
Materials and Workflow:
Step-by-Step Procedure:
- Participant Recruitment: Enroll a representative sample (e.g., n > 3000). Apply exclusion criteria: pre-existing liver disease (viral hepatitis, autoimmune), significant alcohol consumption, use of steatogenic medications, and implausible energy intake reports [15].
- Dietary Assessment: Administer two non-consecutive 24-hour dietary recalls or a validated food frequency questionnaire (FFQ) to capture habitual intake [15]. The NHANES protocol uses the automated multiple-pass method for enhanced accuracy [15].
- DII Calculation:
- Obtain intake data for a minimum of 27-28 available food parameters from the dietary assessment [15] [18].
- Standardize each parameter's intake to a global mean and standard deviation from a representative reference database [15].
- Convert the Z-scores to centered percentiles.
- Multiply each centered percentile by its respective inflammatory effect score.
- Sum all values to obtain the overall DII score for each participant [15] [16].
- NAFLD/MASLD Ascertainment:
- Primary Method (for large cohorts): Use the Fatty Liver Index (FLI), a predictive model incorporating BMI, waist circumference, triglycerides, and GGT. An FLI ≥ 60 indicates fatty liver [15].
- Confirmatory/Clinical Methods: Utilize imaging techniques such as abdominal ultrasonography, Controlled Attenuation Parameter (CAP), or MRI for direct assessment of steatosis [17] [16]. Liver biopsy remains the gold standard for diagnosing steatohepatitis (MASH) but is less feasible in large studies.
- Covariate Assessment: Collect data on potential confounders via questionnaires, physical exams, and blood tests. Key covariates include age, sex, race, BMI, waist circumference, smoking status, physical activity level, and presence of type 2 diabetes [15] [18].
- Statistical Analysis: Employ multivariable-adjusted regression models (logistic for cross-sectional, Cox proportional hazards for cohort studies). Treat DII as both a continuous variable (per 1-unit increase) and in tertiles/quartiles. Adjust for all covariates from step 5. Use restricted cubic splines (RCS) to test for non-linear relationships [15] [18].
The DII in Cancer and Metabolic Diseases
Association with Hepatocellular Carcinoma (HCC)
Inflammation is a recognized driver of carcinogenesis. A French case-control study (CiRCE) investigating cirrhotic patients found that those with a pro-inflammatory diet had a significantly higher risk of developing HCC. After multi-variable adjustment, individuals in the highest DII tertile had a 2.33-fold increased risk (OR: 2.33, 95% CI: 1.16–4.67) of HCC compared to those in the lowest tertile [19]. Furthermore, the DII scores were positively correlated with circulating levels of inflammatory biomarkers (CRP, IL-6), supporting the biological plausibility of the mechanism [19].
Association with Metabolic Syndrome (MetS) and Mortality
The pro-inflammatory state induced by diet is a key contributor to metabolic dysregulation.
Table 2: DII Associations with Metabolic Syndrome and Mortality
| Health Outcome | Study Population | Key Finding | Effect Estimate (95% CI) | Citation |
|---|---|---|---|---|
| Metabolic Syndrome (MetS) | 8,180 US adults (NHANES) | Highest DII quartile vs. lowest increased MetS risk. | OR: 1.59 (1.25 - 2.03) | [20] |
| All-Cause Mortality | 13,751 US adults with MetS (NHANES) | Highest DII tertile vs. lowest increased all-cause mortality. | HR: 1.16 (1.01 - 1.34) | [18] |
| CVD Mortality | 13,751 US adults with MetS (NHANESES) | Highest DII tertile vs. lowest increased CVD mortality. | HR: 1.26 (0.95 - 1.68) | [18] |
| Phenome-Wide Association | 210,960 UK Biobank participants | Genetically predicted DII linked to obesity and hyperalimentation. | OR: 3.50 (3.08 - 3.93) | [14] |
Mechanistically, higher DII scores are significantly associated with adverse changes in individual MetS components, including increased waist circumference, BMI, triglycerides, and blood pressure, and decreased HDL-C levels [20].
Mechanistic Insights: Linking Pro-Inflammatory Diets to Disease
Diets with high DII scores (pro-inflammatory) are typically rich in refined carbohydrates, saturated fats, and processed meats, while being low in fiber, antioxidants, and omega-3 fatty acids. These dietary patterns activate key inflammatory pathways that drive disease pathogenesis.
The diagram illustrates the core mechanisms. The activation of pathways like NF-κB leads to the production of pro-inflammatory cytokines (e.g., IL-6, TNF-α). These cytokines, in turn, induce insulin resistance in the liver and adipose tissue, promoting lipolysis and de novo lipogenesis, which causes hepatic fat accumulation (steatosis) [17] [21]. Furthermore, these inflammatory mediators cause oxidative stress and activate hepatic stellate cells, driving the progression from simple steatosis to steatohepatitis (MASH), fibrosis, and ultimately cirrhosis and HCC [17] [16] [19]. A dysfunctional gut-liver axis, characterized by dysbiosis and increased intestinal permeability, allows bacterial products like LPS to enter the portal circulation and further fuel hepatic inflammation [15].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Resources for DII Research
| Item / Resource | Function / Application | Examples / Notes |
|---|---|---|
| Validated FFQ | Assesses habitual dietary intake to calculate DII. | 147-item FFQ [16]; 168-item FFQ [22]; NHANES 24-hour recall [15]. |
| Global Food Database | Provides reference mean and SD for standardizing DII parameters. | Global database from 11 populations for 45 food parameters [15]. |
| Inflammatory Biomarker Kits | Validates DII score against systemic inflammation. | ELISA kits for CRP, IL-6, TNF-α [22] [19]. |
| Liver Fat Assessment Tools | Determines NAFLD/MASLD status and severity. | FLI Formula [15]; Vibration-Controlled Transient Elastography (FibroScan for CAP and liver stiffness); MRI-PDFF (gold standard imaging). |
| Genetic Data & Tools | Enables Mendelian Randomization for causal inference. | GWAS summary data for DII-associated SNP (e.g., rs7910002) [14]. |
| Statistical Software | Performs complex survey data analysis and modeling. | R, SAS, or Stata with packages for survey analysis (e.g., survey in R) and multivariate regression. |
| Milacemide Hydrochloride | Milacemide Hydrochloride|High Purity|For Research | Milacemide hydrochloride is a glycine prodrug and MAO-B inhibitor for neurological research. For Research Use Only. Not for human or veterinary use. |
| COX-2-IN-36 | Selective COX-2 Inhibitor|COX-2-IN-36|RUO |
The Dietary Inflammatory Index provides a robust, evidence-based tool for quantifying the inflammatory potential of diet. Global evidence consistently demonstrates that higher DII scores are significantly associated with an increased risk of NAFLD/MASLD, hepatocellular carcinoma, metabolic syndrome, and related mortality. The mechanisms underpinning these associations involve the activation of central inflammatory pathways, leading to insulin resistance, hepatic steatosis, and fibrosis. For researchers and clinicians, the DII offers a valuable framework for developing targeted, anti-inflammatory dietary interventions and for stratifying patient risk in both clinical practice and drug development programs. Future research should focus on leveraging genetic instruments for causal inference and integrating multi-omics data to further elucidate the precise mechanisms linking diet, inflammation, and disease.
A Practical Guide to DII Calculation and Research Implementation
The Dietary Inflammatory Index (DII) is a literature-derived, population-based tool designed to quantify the inflammatory potential of an individual's diet [11]. As research continues to establish connections between diet-driven inflammation and chronic diseases, the need for standardized, robust methodologies for DII calculation becomes paramount for both academic research and drug development. The DII calculation is based on extensive research linking dietary parameters to inflammatory biomarkers, with the current version derived from an analysis of 1,943 peer-reviewed articles [11]. This protocol outlines the comprehensive data requirements and methodological considerations necessary for accurate DII assessment in research settings, providing a framework for reliable evaluation of dietary inflammation across diverse populations.
Core Data Requirements for DII Calculation
Essential Dietary Parameters
The DII calculation requires quantitative data on specific dietary parameters with established inflammatory effects. The current DII incorporates 45 food parameters, including nutrients and bioactive food components [11]. These parameters are categorized based on their documented effects on inflammatory biomarkers such as CRP, IL-1β, IL-4, IL-6, IL-10, and TNF-α [11] [23].
Table 1: Essential Dietary Parameters for DII Calculation
| Parameter Type | Specific Components | Inflammatory Effect |
|---|---|---|
| Macronutrients | Energy, carbohydrate, protein, total fat, saturated fat, trans fat | Pro-inflammatory [23] |
| Micronutrients | Iron, vitamin B12 | Pro-inflammatory [23] |
| Antioxidants | Vitamin A, C, E, β-carotene, selenium, magnesium, zinc | Anti-inflammatory [23] |
| Fatty Acids | Monounsaturated fatty acids (MUFAs), polyunsaturated fatty acids (PUFAs) | Anti-inflammatory [23] |
| Bioactive Compounds | Flavonoids (anthocyanidins, flavan-3-ols, flavonols, flavonones, isoflavones, flavones), caffeine, tea, pepper, onion | Anti-inflammatory [11] |
| Other Components | Alcohol, fiber, cholesterol | Varies by component [23] |
Dietary Assessment Methods
Accurate DII calculation depends on the quality of dietary intake data. Multiple assessment methods can be employed, each with distinct strengths and limitations:
- 24-Hour Dietary Recalls: This method involves detailed interviews conducted on 2 consecutive days to capture recent dietary intake [24]. The multiple-pass method enhances accuracy by systematically eliciting complete food recall.
- Food Frequency Questionnaires (FFQ): Semi-quantitative FFQs with 130-168 food items assess habitual intake over the previous year [23] [25]. This method is particularly valuable for capturing seasonal variations and long-term patterns.
- Supplemental Data Collection: Information on dietary supplement use must be collected separately through specialized questionnaires, as nutrient contributions from supplements are typically excluded from standard DII calculation [24].
DII Calculation Protocol
Standardization and Energy Adjustment
The DII calculation algorithm involves several critical steps to standardize dietary intake data relative to global reference values:
Global Reference Database: The DII algorithm utilizes a composite database of 11 population datasets from countries including the United States, Australia, Denmark, Japan, Mexico, and others to establish global means and standard deviations for each dietary parameter [11].
Z-score Calculation: For each dietary parameter, a z-score is computed using the formula:
Z-score = (individual mean intake - global mean intake) / global SD[25].Centering Procedure: To minimize the effect of right-skewing common in dietary data, these z-scores are converted to centered percentiles (values ranging from 0 to 1) [11].
Energy Adjustment: The energy density method is recommended, expressing dietary intake per 1,000 calories to account for variations in total energy intake [25].
Scoring Algorithm
The final DII score is derived through the following computational steps:
Inflammatory Effect Scores: Each centered percentile value is multiplied by the respective inflammatory effect score derived from the literature review [11]. These effect scores range from -1 (strongly anti-inflammatory) to +1 (strongly pro-inflammatory).
Score Aggregation: The resulting values for all food parameters are summed to generate the overall DII score [25].
Interpretation: Higher positive DII scores indicate a more pro-inflammatory diet, while lower negative scores represent a more anti-inflammatory diet [11].
Validation and Quality Control Protocols
Biomarker Correlation Analysis
To validate DII calculations, researchers should implement biomarker correlation protocols:
- Inflammatory Biomarkers: Measure high-sensitivity C-reactive protein (hs-CRP), IL-6, and TNF-α to assess correlation with calculated DII scores [23]. Studies have demonstrated significant positive correlations between DII scores and hs-CRP concentrations [23].
- Nutritional Biomarkers: Validate dietary intake data against objective nutritional biomarkers including:
Table 2: Research Reagent Solutions for DII Validation
| Reagent/Category | Specific Examples | Research Function |
|---|---|---|
| Inflammatory Biomarker Kits | High-sensitivity CRP, IL-6, TNF-α immunoassays | Quantify systemic inflammation levels for DII validation [23] |
| Nutritional Biomarker Assays | Plasma vitamin C, carotenoids, alkylresorcinols | Objectively verify dietary intake data accuracy [27] [26] |
| Dietary Assessment Platforms | Automated 24-hour recall systems, FFQ scanners | Standardize dietary data collection and processing [24] [25] |
| Reference Materials | NIST standard reference materials for biomarker assays | Ensure analytical accuracy and cross-laboratory comparability [26] |
| Data Processing Tools | DII calculation algorithms, nutrient database software | Convert dietary intake data to standardized DII scores [11] |
Data Quality Assessment
Implement rigorous quality control measures for dietary data:
- Energy Intake Screening: Identify outliers using the ratio of reported energy intake to basal metabolic rate (EI:BMR), excluding extreme values (e.g., top and bottom 0.5%) [23].
- Completeness Checks: Exclude dietary records with excessive missing items (e.g., FFQs with ≥10 missing answers) [23].
- Supplement Consideration: Document but typically exclude supplemental nutrients from DII calculation, as the index primarily reflects dietary inflammation [24].
Implementation Workflow
Applications in Research and Drug Development
The DII has demonstrated utility across diverse research contexts:
- Clinical Outcomes: Higher DII scores associate with increased all-cause and cardiovascular mortality in non-diabetic adults [24], elevated depression risk [28], and increased incidence of various cancers including lung and esophageal malignancies [29] [30].
- Neurodevelopmental Research: Recent case-control studies reveal significant associations between pro-inflammatory diets and attention deficit hyperactivity disorder (ADHD) in children [25].
- Chronic Disease Management: DII calculations inform nutritional interventions for multiple long-term conditions (MLTCs) where chronic inflammation is a pathological driver [23].
Methodological Considerations
Limitations and Mitigation Strategies
- Dietary Assessment Error: Self-reported dietary data inherently contains measurement error. Mitigation strategies include:
- Cultural Adaptations: When applying DII across diverse populations, researchers may need to exclude certain food parameters unavailable in local nutrient databases or irrelevant to regional dietary patterns [25].
- Temporal Factors: Dietary inflammation relationships may vary based on timing, including seasonal variations in food availability and diurnal rhythms in inflammatory biomarkers [26].
By adhering to these detailed protocols for data collection, calculation, and validation, researchers can ensure robust DII assessment that generates reliable, comparable evidence on diet-associated inflammation across diverse populations and research contexts.
Navigating the 45-Parameter DII vs. the Energy-Adjusted DII (E-DII)
The Dietary Inflammatory Index (DII) is a validated tool that quantifies the inflammatory potential of an individual's diet based on scientific literature linking dietary components to inflammatory biomarkers [3]. The standard DII assesses 45 food parameters, including nutrients, bioactive compounds, and spices, scoring their combined effect on six established inflammatory biomarkers: IL-1β, IL-4, IL-6, IL-10, TNF-α, and CRP [11] [14]. A higher DII score indicates a more pro-inflammatory diet, while a lower (more negative) score indicates a more anti-inflammatory diet [31].
The Energy-Adjusted DII (E-DII) was developed as a methodological refinement to account for the confounding effects of total energy intake [32] [33]. By standardizing food parameter intake per 1000 kilocalories, the E-DII improves comparability across individuals with varying energy requirements and enhances the accuracy of assessing diet-associated inflammation [34] [33]. This protocol provides a detailed guide for researchers on the application and differentiation of these two related tools.
Comparative Analysis: DII vs. E-DII
Table 1: Core Characteristics of the Standard DII and Energy-Adjusted DII
| Feature | Standard DII | Energy-Adjusted DII (E-DII) |
|---|---|---|
| Purpose | Quantifies overall inflammatory potential of diet [3] | Quantifies inflammatory potential per 1000 kcal, adjusting for total energy intake [32] [33] |
| Number of Parameters | 45 food parameters (e.g., nutrients, spices) [11] | Same 45 parameters, but intake is energy-adjusted [32] |
| Scoring Interpretation | More positive = more pro-inflammatory; More negative = more anti-inflammatory [11] | Same interpretation as DII [34] |
| Primary Advantage | Comprehensive assessment of overall dietary pattern [3] | Reduces confounding by total caloric intake, improves comparability [32] [33] |
| Calculation Basis | Compares individual's absolute nutrient intake to a global standard database [10] [11] | Compares individual's nutrient intake per 1000 kcal to a global standard database [32] [33] |
| Ideal Application | Assessing broad dietary patterns and general inflammatory potential [3] | Studies where energy intake is a key variable (e.g., obesity, metabolic diseases) [32] |
Table 2: Association with Health Outcomes in Recent Research
| Health Outcome | Standard DII Association | Energy-Adjusted DII Association | Study Details |
|---|---|---|---|
| Metabolic Syndrome (MetS) | - | 29% increased risk per unit increase in E-DII (OR=1.29; 95%CI: 1.22–1.36) [32] | Prospective cohort (n=2,252), 5-year follow-up [32] |
| Gastric Cancer | 3.4x higher odds with pro-inflammatory diet (OR=3.39; 95%CI: 1.59–7.22) [10] | - | Case-control study (82 cases/95 controls) [10] |
| Sleep Latency | - | 30% higher odds in highest E-DII quartile (OR=1.30; 95%CI: 1.11–1.51) [33] | Cross-sectional study (n=9,761) [33] |
| Diabetic Retinopathy | 51% increased risk with higher DII (HR=1.51; 95%CI: 1.15–1.99) [35] | - | Prospective cohort of 16,224 participants with diabetes [35] |
Calculation Protocols
Standard DII Calculation Methodology
The standard DII calculation involves a multi-step process to convert dietary intake data into a single inflammatory potential score [10] [11].
Step 1: Dietary Data Collection
- Collect dietary intake data using a validated Food Frequency Questionnaire (FFQ), 24-hour recall, or food records [10]. The DII has been validated across various dietary assessment instruments [11].
- For the standard DII, use absolute intake values of the 45 food parameters (e.g., grams, milligrams, micrograms).
Step 2: Z-score Calculation For each of the 45 parameters, calculate a Z-score relative to a global composite database:
Z = (individual's reported intake - global mean intake) / global standard deviation[11]- The global database was constructed from 11 population-based surveys from countries worldwide, providing a robust standard mean and deviation for each parameter [11].
Step 3: Convert to Centered Percentiles
- Convert Z-scores to centered percentiles to minimize the effect of right skewing:
Centered percentile = (2 * cumulative proportion value) - 1[11] - This creates a symmetrical distribution with values between -1 and +1.
Step 4: Apply Inflammatory Effect Scores
- Multiply each centered percentile by the respective food parameter's inflammatory effect score derived from systematic literature review [11] [14].
- The inflammatory effect scores are based on review of 1,943 qualifying articles published through 2010, with each parameter scored as pro-inflammatory (+1), anti-inflammatory (-1), or no effect (0) based on evidence [11].
Step 5: Summation
- Sum all food parameter-specific DII scores to obtain the overall DII score for the participant [33].
- Formula:
Overall DII score = Σ (centered percentile * inflammatory effect score)for all parameters
E-DII Calculation Methodology
The E-DII uses the same foundational calculation but with a crucial adjustment for energy intake [32] [33].
Step 1: Energy Adjustment of Parameters
- Convert all dietary parameters to intake per 1000 kilocalories before beginning the standard DII calculation process [32] [33].
- Example: If a participant consumes 80g of protein with a total energy intake of 2000 kcal, the energy-adjusted protein intake =
(80g / 2000 kcal) * 1000 = 40g per 1000 kcal.
Step 2-5: Identical to Standard DII
- Follow steps 2-5 of the standard DII protocol using the energy-adjusted intake values.
- This results in an E-DII score that represents the inflammatory potential per 1000 kcal of dietary intake.
Research Implementation Guide
Tool Selection Decision Pathway
Protocol for Validated DII Assessment in Cohort Studies
Study Design and Population
- Design: Prospective cohort studies are optimal for establishing temporal relationships between dietary inflammation and health outcomes [32] [14]. Case-control designs are also acceptable [10].
- Sample Size: Ensure adequate power based on outcome incidence. Large cohorts (n > 10,000) enable detection of subtle effects across multiple outcomes [14].
- Follow-up Duration: Minimum 5-year follow-up recommended for chronic disease outcomes [32] [35].
Dietary Assessment Protocol
- Primary Tool: Use validated 125-168 item Food Frequency Questionnaires (FFQ) to capture habitual intake [10] [32].
- Administration: Train interviewers to administer FFQs consistently. For cases (e.g., cancer patients), ensure reporting reflects pre-diagnosis diet [10].
- Supplementary Data: Collect additional food items not in standard FFQs but relevant to DII (e.g., ginger, saffron, garlic) through supplementary questions [10].
- Quality Control: Exclude participants with implausible energy intake (<800 or >5500 kcal/day) and those reporting major dietary changes during study period [10].
Data Processing and Calculation
- Nutrient Analysis: Use standardized nutrient analysis software (e.g., Nutritionist IV, Foodworks) to convert food intake to nutrient values [10] [34].
- Parameter Inclusion: Aim for maximum parameter coverage (25-31 of 45 possible parameters acceptable) [32] [33].
- Database Linkage: Link dietary data to the global representative database for Z-score calculation [11] [33].
Covariate Assessment and Adjustment
- Essential Covariates: Age, sex, body mass index, education, smoking status, alcohol consumption, physical activity, total caloric intake, and prevalent health conditions [10] [32].
- Disease-Specific Covariates: Include H. pylori status for gastric cancer [10]; medication use (aspirin/NSAIDs) for inflammatory conditions [10].
- Biomarker Validation: Where possible, validate DII scores against inflammatory biomarkers (hs-CRP, TNF-α, IL-6, IL-1β, IL-10) in subsets [10].
The Researcher's Toolkit
Table 3: Essential Reagents and Resources for DII Research
| Tool/Resource | Specifications | Application in DII Research |
|---|---|---|
| Validated FFQ | 125-168 food items, culturally adapted [10] [32] | Captures habitual intake of DII parameters; ensures comprehensive dietary assessment |
| Global Reference Database | Means and SDs for 45 parameters from 11 worldwide populations [11] | Provides standardized comparison for Z-score calculation; enables cross-population comparability |
| Nutrient Analysis Software | Foodworks, Nutritionist IV, or country-specific equivalents [10] [34] | Converts food intake data to nutrient values for DII parameters |
| Inflammatory Biomarker Kits | hs-CRP, TNF-α, IL-6, IL-1β, IL-10, IL-4 assays [10] | Validates DII scores against actual inflammatory markers; confirms biological plausibility |
| Statistical Software Packages | R, Stata, SAS with specialized nutritional epidemiology modules [32] [34] | Performs complex adjustments for nutritional data and calculates DII scores |
Applications in Clinical and Translational Research
Disease Association Studies
Recent large-scale studies demonstrate the utility of DII tools across diverse health outcomes:
Metabolic Diseases: E-DII shows strong associations with metabolic syndrome incidence, with particularly strong connections to waist circumference and triglyceride levels [32]. The association persists in both normal-weight and obese individuals, suggesting inflammatory dietary effects independent of BMI [32].
Cancer Research: In gastric cancer, DII scores demonstrated a dose-response relationship, with subjects in the highest DII category having 3.4 times higher odds of cancer compared to those in the lowest category [10]. Mechanistically, each unit increase in DII corresponded with significant increases in pro-inflammatory cytokines (hs-CRP, TNF-α, IL-6, IL-1β) and decrease in anti-inflammatory IL-10 [10].
Ophthalmologic Complications: For diabetic retinopathy, a J-shaped association emerged where risk significantly increased only when DII scores exceeded -2.5, suggesting a threshold effect [35]. Higher DII scores associated with thinning of the retinal pigment epithelium layer, indicating potential structural correlates [35].
Biomarker Validation Protocol
Objective: Validate computed DII scores against actual inflammatory biomarkers to confirm biological plausibility.
Sample Collection:
- Collect fasting venous blood samples (10mL) in sterile vacutainer tubes between 8:30-10:30 am after 10-12 hour fast [10].
- Exclude participants on corticosteroids, anti-inflammatory medications, or pain killers for at least 48 hours prior to collection [10].
- Process samples rapidly: centrifuge freshly drawn blood, separate serum, and store at -70°C until analysis [10].
Biomarker Analysis:
- Measure hs-CRP, TNF-α, IL-6, IL-1β, and IL-10 using standardized commercial ELISA kits [10].
- Follow manufacturer protocols precisely for each assay.
- Include appropriate controls and standards in each batch.
Statistical Validation:
- Use linear regression models to test associations between DII/E-DII scores and each inflammatory biomarker [10].
- Expect positive associations with pro-inflammatory markers (hs-CRP, TNF-α, IL-6, IL-1β) and inverse associations with anti-inflammatory IL-10 [10].
- Report beta coefficients and 95% confidence intervals for each unit increase in DII score [10].
The standard DII and E-DII provide complementary approaches for quantifying dietary inflammatory potential in research settings. The standard DII captures overall inflammatory patterns, while the E-DII offers refined assessment by accounting for energy intake, particularly valuable in studies of obesity, metabolic disorders, and across populations with varying energy requirements. Recent advances in DII application include large-scale phenome-wide association studies and Mendelian randomization approaches that strengthen causal inference [14]. By implementing the standardized protocols outlined in this document, researchers can robustly assess diet-induced inflammation and its health implications across diverse populations and disease contexts.
The Dietary Inflammatory Index (DII) represents a quantitative tool designed to assess the inflammatory potential of an individual's overall diet, providing researchers with a standardized method to evaluate diet-disease relationships through an inflammatory lens [3]. This empirically developed index scores diets on a continuum from maximally anti-inflammatory to maximally pro-inflammatory based on the effects of 45 food parameters on established inflammatory biomarkers including interleukin-1β (IL-1β), IL-4, IL-6, IL-10, tumor necrosis factor-α (TNF-α), and C-reactive protein (CRP) [36] [35]. The DII framework has enabled nutritional epidemiologists to systematically investigate connections between dietary patterns and various health outcomes across diverse observational study designs, thereby advancing our understanding of diet-induced inflammation as a modifiable risk factor in chronic disease pathogenesis.
The conceptual foundation of the DII stems from evidence that chronic low-grade inflammation serves as a significant underlying mechanism in the development of numerous non-communicable diseases [14]. Dietary components can either promote or suppress inflammatory pathways, with pro-inflammatory diets characterized by higher consumption of refined carbohydrates, saturated and trans fats, and processed meats, while anti-inflammatory diets typically emphasize fruits, vegetables, whole grains, nuts, olive oil, and fatty fish [17] [37]. By quantifying the overall inflammatory potential of diet rather than focusing on isolated nutrients or foods, the DII captures the complex, synergistic nature of dietary exposures, making it particularly valuable for studying multifactorial disease processes in free-living populations [3].
DII Calculation and Methodological Framework
Theoretical Foundation and Scoring Algorithm
The DII development process began with a systematic review of nearly 2,000 research articles published through 2010 that investigated relationships between dietary components and the six inflammatory biomarkers previously mentioned [3]. For each of the 45 food parameters considered, the literature was reviewed to assign an inflammatory effect score based on consistent findings regarding their directional effects on inflammatory markers: +1 for pro-inflammatory, -1 for anti-inflammatory, and 0 for no effects [36] [35]. To create a global comparison framework, the research team established a world representative database from 11 countries that provided a global mean and standard deviation for each food parameter, allowing for standardization of individual intakes relative to this global distribution [36].
The stepwise calculation of the DII proceeds as follows. First, for each food parameter, the individual's intake is converted to a z-score by subtracting the global mean and dividing by the global standard deviation. This z-score is then converted to a centered percentile score to minimize the effect of outliers. The centered percentile value for each food parameter is multiplied by its respective inflammatory effect score to obtain the food parameter-specific DII score. Finally, all food parameter-specific DII scores are summed to create the overall DII score for the individual [35]. In practice, researchers often use an energy-adjusted DII per 1000 kcal to account for variations in total energy intake, calculated by dividing the overall DII score by the individual's daily energy intake and multiplying by 1000 [35].
Practical Implementation Considerations
In operationalizing the DII within observational studies, researchers must make several methodological decisions that can affect the resulting scores. The number of food parameters available for calculation varies across studies depending on the dietary assessment method used, with most studies incorporating between 28 and 45 parameters [36] [35]. While the original DII was designed to incorporate all 45 parameters, practical applications in specific cohorts often utilize a subset due to limitations in dietary assessment tools. Validation studies have demonstrated that even DII scores based on fewer parameters maintain predictive validity for inflammatory biomarkers and health outcomes [36].
Dietary assessment methods commonly employed in DII research include 24-hour dietary recalls, food frequency questionnaires (FFQs), and dietary history interviews. Each method presents distinct advantages and limitations concerning the comprehensive capture of food parameters, with 24-hour recalls generally providing more detailed recent intake data while FFQs better capture habitual intake patterns over time [35] [37]. Researchers must carefully consider the dietary assessment method's validity and reliability within their specific population when interpreting DII-disease associations.
Figure 1: DII Calculation Workflow. This diagram illustrates the sequential steps in calculating the Dietary Inflammatory Index, from dietary assessment to final score generation.
Application Across Observational Study Designs
Cross-Sectional Studies
Cross-sectional studies represent the most frequent application of the DII in nutritional epidemiology, providing snapshot assessments of relationships between dietary inflammatory potential and health outcomes at a specific point in time. These studies efficiently generate hypotheses regarding diet-disease associations and are particularly valuable for examining the relationship between DII and prevalent disease states or continuous biomarkers of inflammation.
A recent investigation of gout patients (n=1,437) from the National Health and Nutrition Examination Survey (NHANES) 2007-2018 demonstrated the application of DII in a cross-sectional design [36] [38]. Researchers calculated DII using 28 food parameters from 24-hour dietary recalls and examined its association with cardiovascular disease (CVD) prevalence. After adjusting for multiple covariates including age, BMI, smoking status, and comorbidities, results revealed a significant positive association between DII and CVD risk, with participants in the highest DII quartile having a 118% increased odds (OR: 2.18, 95% CI: 1.52-3.13) of CVD compared to those in the lowest quartile [38]. The study employed restricted cubic splines to demonstrate a linear dose-response relationship and utilized machine learning algorithms to validate the robustness of findings.
Similarly, a cross-sectional study of 200 women with polycystic ovary syndrome (PCOS) applied DII to investigate associations with hormonal and metabolic profiles [39]. Dietary intake was assessed using a validated 168-item food frequency questionnaire, and DII scores were calculated based on available parameters. After adjusting for age, BMI, physical activity, and energy intake, higher DII scores were significantly associated with elevated fasting blood glucose (β=+13.34, P<0.001), high-sensitivity CRP (β=+1.18, P<0.001), and gonadotropin levels including luteinizing hormone (β=+3.97, P<0.001) [39]. These findings suggest that pro-inflammatory dietary patterns may exacerbate both metabolic and reproductive manifestations of PCOS.
Cohort Studies
Cohort studies employing the DII provide valuable evidence regarding the temporal relationship between dietary inflammatory potential and subsequent disease incidence. The prospective nature of these studies strengthens causal inference and allows for examination of DII-disease associations over extended follow-up periods.
The UK Biobank cohort has been instrumental in advancing understanding of DII and chronic disease risk. In a recent analysis of 189,561 participants followed for a median of 9.45 years, researchers examined the relationship between DII and lung cancer incidence [29]. DII was calculated from 24-hour dietary recall questionnaires, and Cox proportional hazards models were adjusted for age, sex, smoking status, BMI, physical activity, and other potential confounders. Results indicated that participants in the highest DII tertile had a 17% increased risk (HR: 1.17, 95% CI: 1.00-1.36) of developing lung cancer compared to those in the lowest tertile [29]. Notably, a significant non-linear association was observed, with lung cancer risk increasing sharply once DII exceeded a threshold of 0.07.
Another cohort study within the UK Biobank investigated the association between energy-adjusted DII and incident diabetic retinopathy among 16,224 participants with diabetes [35]. During follow-up, 1,257 cases (7.75%) of diabetic retinopathy were identified. After multivariable adjustment, higher DII scores were associated with increased retinopathy risk (HR: 1.51, 95% CI: 1.15-1.99), with a J-shaped relationship observed where risk significantly increased only when DII scores exceeded -2.5 [35]. This study additionally incorporated retinal imaging data to explore potential mechanisms, finding associations between higher DII scores and thinning of the retinal pigment epithelium layer, suggesting possible structural correlates of diet-induced inflammatory damage.
Case-Control Studies
While less common in recent DII literature, case-control studies offer an efficient design for examining associations between dietary inflammatory potential and diseases with low incidence or long latency periods. These studies compare DII scores between individuals with a specific condition (cases) and those without (controls), typically with careful matching or statistical adjustment for potential confounders.
The search results did not contain specific examples of case-control studies applying DII, which may reflect a trend toward prospective designs in nutritional epidemiology. However, earlier validation studies of the DII frequently employed case-control designs to establish initial evidence for associations with various cancers and other chronic conditions. In such designs, researchers typically assess dietary intake prior to disease diagnosis through interviewer-administered questionnaires or recalls, then calculate DII scores for both cases and controls to compare mean differences or assess odds ratios across DII categories.
Table 1: Key Characteristics of DII Applications Across Observational Study Designs
| Study Design | Temporal Direction | Primary Strength | Key Methodological Considerations | Example Application |
|---|---|---|---|---|
| Cross-Sectional | Exposure and outcome assessed simultaneously | Efficient for hypothesis generation and prevalence estimates | Cannot establish temporality; susceptible to reverse causation | DII and CVD prevalence in gout patients [36] |
| Cohort | Exposure precedes outcome | Establishes temporality; calculates incidence rates | Requires large sample size; lengthy follow-up; costly | DII and lung cancer risk in UK Biobank [29] |
| Case-Control | Outcome precedes exposure assessment | Efficient for rare diseases; multiple exposures | Susceptible to recall and selection bias | Limited recent examples in current literature |
Quantitative Evidence Synthesis
The expanding literature on DII and health outcomes has enabled meta-analyses that provide pooled effect estimates across multiple studies. A recent meta-analysis specifically examined the association between DII and non-alcoholic fatty liver disease (NAFLD), incorporating 11 observational studies (9 cross-sectional with 14 effect sizes and 2 cohort with 2 effect sizes) [17]. The analysis demonstrated that higher DII scores were significantly associated with increased NAFLD risk, with a pooled odds ratio of 1.56 (95% CI: 1.24-1.95; p<0.001) in cross-sectional studies and a hazard ratio of 0.21 (95% CI: 0.12-0.30; p<0.0001) in cohort studies [17]. Subgroup analyses revealed consistent associations across geographical regions, BMI categories, and age groups, supporting the robustness of the DII-NAFLD relationship.
A comprehensive phenome-wide association study further expanded understanding of DII health effects by examining associations with 845 health outcomes in 78,390 to 207,832 participants [14]. This hypothesis-free approach identified 133 outcomes significantly associated with DII after multiple comparison correction, with most pertaining to digestive, circulatory, and endocrine/metabolic systems [14]. Mendelian randomization analyses provided evidence for potential causal relationships between pro-inflammatory diets and several conditions, including abdominal hernia, cholelithiasis, and back pain. This systematic assessment underscores the wide-ranging health implications of dietary inflammatory potential across organ systems.
Table 2: Summary of Significant DII-Health Outcome Associations from Recent Observational Studies
| Health Outcome | Study Design | Population | Effect Measure | Effect Size (Highest vs. Lowest DII) | Citation |
|---|---|---|---|---|---|
| Non-alcoholic fatty liver disease | Meta-analysis | Multiple populations | Odds Ratio | 1.56 (95% CI: 1.24-1.95) | [17] |
| Cardiovascular disease in gout | Cross-sectional | 1,437 gout patients | Odds Ratio | 2.18 (95% CI: 1.52-3.13) | [38] |
| Lung cancer | Cohort | 189,561 UK Biobank participants | Hazard Ratio | 1.17 (95% CI: 1.00-1.36) | [29] |
| Diabetic retinopathy | Cohort | 16,224 with diabetes | Hazard Ratio | 1.51 (95% CI: 1.15-1.99) | [35] |
| Fasting blood glucose in PCOS | Cross-sectional | 200 women with PCOS | Regression Coefficient | β=+13.34, P<0.001 | [39] |
Detailed Experimental Protocols
DII Calculation Protocol for Observational Studies
Purpose: To standardize the calculation of Dietary Inflammatory Index scores in observational research studies using 24-hour dietary recall data.
Materials and Equipment:
- 24-hour dietary recall data (multiple recalls preferred)
- Food composition database or nutrient analysis software
- Global DII database (mean and standard deviation for 45 food parameters)
- Statistical software (R, SAS, Stata, or SPSS)
Procedure:
- Dietary Data Collection: Collect at least one 24-hour dietary recall per participant, with two non-consecutive recalls preferred to account for day-to-day variation. Interviewer-administered recalls using standardized protocols (e.g., USDA Automated Multiple-Pass Method) enhance data quality.
- Nutrient Intake Calculation: Process recall data through appropriate nutrient analysis software to estimate daily intake for each of the available DII parameters. The ideal scenario includes all 45 parameters, but practical applications typically incorporate 25-35 parameters.
- Energy Adjustment: Calculate energy-adjusted values for each nutrient using the nutrient density method (amount per 1000 kcal) or as a percentage of total energy intake for energy-yielding nutrients.
- Z-score Calculation: For each food parameter, compute a z-score using the formula: Z = (individual intake - global mean) / global standard deviation. Use the global means and standard deviations provided in the original DII development publications.
- Percentile Conversion: Convert Z-scores to centered percentiles using the formula: P = 2*(cumulative distribution function value) - 0.5, where the cumulative distribution function value is derived from the standard normal distribution.
- Inflammatory Effect Application: Multiply each centered percentile value by the corresponding food parameter-specific inflammatory effect score (ranging from -1 for anti-inflammatory to +1 for pro-inflammatory).
- Score Summation: Sum all food parameter-specific DII scores to obtain the overall DII score for each participant.
- Energy Adjustment of Final Score (Optional): For energy-adjusted DII, divide the overall DII score by the individual's daily energy intake and multiply by 1000.
Quality Control Considerations:
- Implement rigorous training and certification for dietary interviewers
- Establish standardized protocols for probing and quantification during recalls
- Conduct random duplicate recalls on a subset of participants to estimate within-person variation
- Apply stringent data cleaning procedures to identify and address implausible intake values
Statistical Analysis Protocol for DII-Outcome Associations
Purpose: To provide a standardized approach for analyzing relationships between DII scores and health outcomes across different observational study designs.
Materials and Equipment:
- Dataset containing DII scores, outcome data, and covariates
- Statistical software with advanced modeling capabilities
- Preferred software: R (with packages for regression modeling, spline functions, and effect modification)
Procedure for Cross-Sectional Analyses:
- Preliminary Analyses: Examine distributions of DII scores and outcome variables. Apply appropriate transformations for non-normal distributions.
- Model Specification: Employ multivariable logistic regression for binary outcomes or linear regression for continuous outcomes. Categorize DII scores into quartiles or tertiles to examine dose-response patterns, while also testing for linear trends.
- Confounder Adjustment: Include pre-specified potential confounders based on prior knowledge, including age, sex, BMI, smoking status, physical activity, total energy intake, and socioeconomic indicators.
- Non-Linearity Assessment: Use restricted cubic splines with 3-5 knots to flexibly model potential non-linear relationships between continuous DII scores and outcomes.
- Effect Modification Evaluation: Test for interactions between DII and key demographic variables (e.g., age, sex, BMI) by including cross-product terms in models.
Procedure for Cohort Analyses:
- Time-to-Event Framework: Utilize Cox proportional hazards regression for time-to-event data, with time scale defined as time from baseline assessment to event occurrence or censoring.
- Proportional Hazards Assumption: Verify the proportional hazards assumption using Schoenfeld residuals and time-dependent covariates.
- Multivariable Adjustment: Implement sequential model building, starting with minimal adjustment and progressively adding potential confounders and mediators to examine how associations change.
- Competing Risks Consideration: For outcomes with substantial competing mortality risks, consider complementary cumulative incidence function analyses or cause-specific hazards models.
Sensitivity Analyses:
- Exclude participants with extreme energy intake reports (<500 or >5000 kcal/day for women; <800 or >6000 kcal/day for men)
- Exclude early follow-up years to address potential reverse causality
- Conduct complete-case analyses versus analyses with multiple imputation for missing covariate data
- Recalculate DII using different numbers of food parameters to test robustness
Research Reagent Solutions
Table 3: Essential Methodological Components for DII Research
| Component | Specification | Research Function | Implementation Considerations |
|---|---|---|---|
| Dietary Assessment Tool | 24-hour recalls, FFQs, or dietary history | Captures individual food and nutrient intake | Multiple 24-hour recalls preferred for usual intake estimation; FFQs should be validated in target population |
| Food Composition Database | Country-specific nutrient databases | Converts food intake to nutrient values | Should include all 45 DII parameters when possible; consider compatibility with dietary assessment method |
| Global DII Reference Database | World representative means and standard deviations for 45 food parameters | Provides standardization reference for z-score calculation | Fixed reference allows comparison across studies; must use published values from original development |
| Inflammatory Effect Scores | Literature-derived scores (-1 to +1) for 45 parameters | Quantifies inflammatory potential of each food component | Fixed values based on systematic literature review; not study-specific |
| Statistical Analysis Software | R, SAS, Stata, or SPSS with appropriate packages | Performs DII calculation and association analyses | Should include capabilities for regression modeling, spline functions, and complex survey design |
Methodological Visualizations
Figure 2: DII Applications in Observational Research. This diagram illustrates the relationship between DII, study designs, analytical methods, and exemplar health outcomes with corresponding effect sizes.
The Dietary Inflammatory Index has emerged as a valuable tool in nutritional epidemiology, enabling systematic investigation of relationships between dietary patterns and health outcomes through the mechanistic pathway of inflammation. Its application across cross-sectional, cohort, and case-control studies has generated substantial evidence linking pro-inflammatory diets to increased risk of numerous chronic conditions, including non-alcoholic fatty liver disease, cardiovascular disease, diabetes-related complications, and various cancers [17] [29] [35]. The standardized calculation methodology facilitates comparison across populations and study designs, while ongoing refinements continue to enhance its utility in diverse research contexts.
Future directions for DII research include the development of population-specific adaptations, investigation of gene-DII interactions in disease risk, and application in randomized controlled trials of dietary interventions. As research in this field evolves, the DII promises to continue contributing valuable insights into the role of diet-induced inflammation in chronic disease etiology and prevention.
The Dietary Inflammatory Index (DII) is a quantitative tool that evaluates the inflammatory potential of an individual's diet. Developed through systematic review of scientific literature, the DII provides a standardized method for assessing how specific dietary components influence systemic inflammation [3]. This scoring system has become an essential instrument in nutritional epidemiology and chronic disease research, enabling researchers to investigate connections between diet, inflammation, and various health outcomes.
The DII's development was based on a comprehensive analysis of 1,943 articles published between 1950 and 2007, with the methodology updated in 2010 as research on diet and inflammation expanded [31]. The index quantitatively assesses the inflammatory potential of diets by examining their effects on six established inflammatory biomarkers: interleukin-1β (IL-1β), IL-4, IL-6, IL-10, tumor necrosis factor-α (TNF-α), and C-reactive protein (CRP) [3] [35]. A higher DII score indicates a more pro-inflammatory diet, while a lower score reflects anti-inflammatory potential [14].
DII Scoring Framework and Interpretation
Calculation Methodology
The DII calculation employs a sophisticated algorithm that evaluates up to 45 food parameters based on their documented effects on inflammatory biomarkers [14] [35]. The calculation involves several systematic steps:
Literature Review and Effect Assignment: Each food parameter receives an inflammatory effect score based on published research showing its impact on the six core inflammatory biomarkers. Parameters are classified as pro-inflammatory (+1), anti-inflammatory (-1), or neutral (0) [35].
Global Intake Comparison: Individual dietary intake data is compared to a global reference database representing standard mean intake and standard deviation for each parameter [35].
Z-score Calculation and Centering: For each food parameter, a Z-score is calculated by subtracting the "standard global mean" from the reported intake and dividing by its standard deviation. This Z-score is then converted to a percentile and centered to achieve a distribution between -1 and +1 [35].
Inflammatory Effect Integration: The centered percentile value is multiplied by the food parameter-specific inflammatory effect score to obtain the food parameter-specific DII score [35].
Overall DII Score Generation: All food parameter-specific DII scores are summed to create the overall DII score for an individual. For energy adjustment, this score is often divided by the individual's daily energy intake (in kilocalories) and multiplied by 1000 to derive the standard DII per 1000 kcal [35].
Table: DII Score Interpretation Framework
| DII Range | Inflammatory Classification | Dietary Pattern Characteristics | Associated Health Risks |
|---|---|---|---|
| < -2.5 | Highly Anti-inflammatory | Abundant in antioxidants, fiber, polyphenols; minimal processed foods | Lowest risk for inflammatory diseases |
| -2.5 to 0 | Moderately Anti-inflammatory | Balanced with more anti-inflammatory than pro-inflammatory components | Reduced risk for metabolic conditions |
| 0 | Neutral | Equal balance of pro- and anti-inflammatory components | Baseline inflammatory status |
| > 0 to +2.5 | Moderately Pro-inflammatory | More pro-inflammatory components with some anti-inflammatory elements | Moderately elevated disease risk |
| > +2.5 | Highly Pro-inflammatory | Dominated by pro-inflammatory elements; lacking anti-inflammatory components | Significantly elevated risk for multiple health conditions |
Research has revealed a J-shaped association between DII scores and health outcomes, where the relationship with disease risk becomes significant when the DII score exceeds -2.5 [35]. This threshold represents a critical inflection point where the inflammatory potential of diet begins to substantially impact health.
Food Parameters and Their Inflammatory Effects
The DII calculation incorporates numerous food parameters, each with documented effects on inflammatory pathways. The standard DII evaluates 45 parameters, though studies often utilize a subset based on data availability [40].
Table: Key DII Food Parameters and Their Inflammatory Effects
| Food Parameter | Inflammatory Effect Score | Pro-inflammatory Mechanisms | Anti-inflammatory Mechanisms |
|---|---|---|---|
| Trans fat | +1 | Increases TNF-α and IL-6; promotes endothelial dysfunction | - |
| Saturated fat | +1 | Activates TLR4 signaling; increases inflammatory cytokines | - |
| Carbohydrates | +1 | Promotes postprandial inflammation; advanced glycation end-products | - |
| Iron | +1 | Catalyzes free radical formation via Fenton reaction | - |
| Vitamin B12 | +1 | Potential role in promoting inflammatory pathways | - |
| Cholesterol | +1 | Contributes to foam cell formation; activates inflammasomes | - |
| Fiber | -1 | Fermented to SCFAs; regulates immune function; modulates gut microbiota | - |
| ω-3 fatty acids | -1 | Precursors to specialized pro-resolving mediators; reduce inflammatory eicosanoids | - |
| Vitamin C | -1 | Scavenges free radicals; reduces inflammatory cytokine production | - |
| Vitamin E | -1 | Inhibits NF-κB activation; decreases CRP and IL-6 | - |
| Magnesium | -1 | Regulates NLRP3 inflammasome; reduces TNF-α and IL-1β | - |
| Polyphenols | -1 | Modulates NF-κB, MAPK, and Nrf2 pathways; alters redox signaling | - |
| β-carotene | -1 | Quenches singlet oxygen; reduces oxidative stress | - |
Recent research has identified that specific dietary components contribute disproportionately to the inflammatory potential of diets. Weighted quantile sum regression analysis has revealed that fiber, alcohol, and energy intake are the primary contributors to inflammatory markers in the DII framework [40]. Conversely, adequacy components in healthy dietary patterns such as seafood and plant proteins, and whole grains contribute most to reduced inflammation [40].
Research Applications and Clinical Evidence
Association with Health Outcomes
Large-scale epidemiological studies have demonstrated significant associations between DII scores and numerous health conditions. A comprehensive population-based phenome-wide association study analyzing 845 health outcomes revealed that 133 outcomes were significantly associated with DII after multiple comparison correction [14]. Most of these health outcomes pertained to the digestive, circulatory, and endocrine/metabolic systems [14].
Mendelian randomization analyses, which help establish causal inference, have confirmed that genetically predicted higher DII levels increase the risk of specific conditions including abdominal hernia, cholelithiasis, and back pain [14]. The risk increase was substantial, with higher DII scores associated with a 2.34-fold higher risk of back pain, 2.38-fold higher risk of abdominal hernia, and 1.54-fold higher risk of cholelithiasis [14].
Table: DII Associations with Specific Health Conditions from Cohort Studies
| Health Condition | Hazard Ratio (HR) per DII Unit Increase | Confidence Interval | P-value | Study Population |
|---|---|---|---|---|
| Diabetic Retinopathy | 1.51 | 1.15-1.99 | 0.003 | UK Biobank (n=16,224) |
| Tobacco Use Disorder | 1.05 | 1.04-1.06 | 9.83×10^-13 | Population-based cohort (n=207,832) |
| Cholelithiasis and Cholecystitis | 1.05 | 1.03-1.06 | 8.25×10^-11 | Population-based cohort (n=207,832) |
| Cerebrovascular Disease | 1.04 | 1.03-1.05 | 3.36×10^-7 | Population-based cohort (n=207,832) |
| Overweight and Obesity | 3.50 (OR) | 3.08-3.93 | 5.84×10^-6 | MR-PheWAS analysis |
The association between DII and diabetic retinopathy demonstrates a clear J-shaped relationship, with risk significantly increasing only when DII scores exceed -2.5 [35]. This pattern highlights the importance of maintaining DII scores below this threshold for optimal health outcomes.
Relationship with Inflammatory Biomarkers
Validation studies have consistently demonstrated significant correlations between DII scores and established inflammatory markers. Research using NHANES data (2009-2018) with 19,110 participants showed that DII exhibits significant positive associations with white blood cell count, neutrophil count, neutrophil-to-lymphocyte ratio, and systemic immune-inflammation index [40].
The association between DII and inflammatory biomarkers follows a dose-response relationship, with progressively higher biomarker levels observed as DII scores increase. This relationship persists after adjustment for multiple potential confounders including age, gender, BMI, smoking status, and physical activity levels [40].
Diagram Title: DII-Mediated Inflammatory Pathways and Biomarker Relationships
Research Implementation Protocols
DII Assessment Methodology
Implementing DII assessment in research studies requires standardized protocols to ensure consistency and comparability across studies. The following workflow outlines the essential steps for proper DII calculation and application in research settings.
Diagram Title: DII Research Implementation Workflow
Dietary Assessment Methods
Different dietary assessment methods can be employed to collect data for DII calculation, each with specific advantages and limitations:
24-Hour Dietary Recall: The UK Biobank utilized this method through 70,000 recruiters, collecting data via email-based questionnaires at four different periods between February 2011 and April 2012 [35]. The questionnaire covered approximately 200 common foods and drinks across 11 categories including beverages, cereals, meat, fruits, and vegetables [35].
Food Frequency Questionnaires (FFQ): Semi-quantitative FFQs assess habitual dietary intake over extended periods (typically 3-12 months). While subject to measurement error, they provide practical means for assessing usual intake in large epidemiological studies.
Food Records/Diaries: Participants record all foods and beverages consumed for a specific period (typically 3-7 days). This method provides detailed information but requires high participant burden and may alter usual eating patterns.
Regardless of the method used, standardization is critical. Research protocols should specify:
- Number of assessment days (minimum 2-3 non-consecutive days recommended)
- Seasonality considerations
- Interviewer training protocols
- Standardized portion size estimation aids
- Quality control procedures
Laboratory Assessment Protocols
For studies validating DII scores against inflammatory biomarkers, standardized laboratory protocols are essential:
Blood Collection and Processing:
- Fasting blood samples (8-12 hour fast)
- Standardized collection tubes (EDTA for plasma, serum separator tubes)
- Processing within 2 hours of collection
- Storage at -80°C until analysis
Inflammatory Biomarker Assessment:
- CRP: High-sensitivity immunoassays (hs-CRP)
- Cytokines (IL-6, TNF-α, IL-1β): Multiplex bead-based assays or ELISA
- White Blood Cell Count: Automated hematology analyzers with differential
- Neutrophil-to-Lymphocyte Ratio: Calculated from complete blood count with differential
Quality control should include:
- Internal quality control samples
- External proficiency testing
- Blind duplicate analysis
- Standardized normalization procedures
Table: Essential Research Reagents for DII and Inflammation Studies
| Reagent/Resource | Specifications | Research Application | Example Sources/Protocols |
|---|---|---|---|
| Dietary Assessment Platform | Web-based 24-hour recall or FFQ system with nutrient database | Standardized dietary data collection | USDA Automated Multiple-Pass Method, Oxford WebQ |
| Inflammatory Biomarker Panels | Multiplex cytokine panels (IL-6, TNF-α, IL-1β, IL-10) | Quantifying inflammatory status | Milliplex MAP kits, Meso Scale Discovery assays |
| High-sensitivity CRP Assay | Sensitivity: <0.1 mg/L; Range: 0.1-20 mg/L | Cardiovascular inflammation assessment | Immunoturbidimetric methods, ELISA |
| DNA Collection and Genotyping Kits | Genome-wide SNP arrays with imputation | Mendelian randomization analyses | UK Biobank Axiom Array, Infinium Global Screening Array |
| DII Calculation Algorithm | R, Python, or SAS code for standardized DII computation | Consistent DII score calculation | "Dietaryindex" R package, Python 3.10 implementation |
| Statistical Analysis Software | R, SAS, STATA with specialized packages | Complex survey analysis, regression modeling | R "survey" package, SAS PROC SURVEYREG |
| Biomarker Biobanking Supplies | EDTA tubes, serum separator tubes, -80°C freezers | Sample integrity for longitudinal studies | Certified laboratory suppliers with temperature monitoring |
The Dietary Inflammatory Index provides researchers with a validated, quantitative tool for assessing the inflammatory potential of dietary patterns. Proper interpretation of DII scores—from highly anti-inflammatory to highly pro-inflammatory—requires understanding of the underlying calculation methodology, biomarker relationships, and clinical associations. The protocols and frameworks presented here offer researchers comprehensive guidance for implementing DII assessment in studies investigating diet-inflammation-disease pathways. As evidence continues to accumulate, the DII remains an essential tool for advancing our understanding of how diet influences inflammation and chronic disease risk across diverse populations.
Overcoming Challenges: Methodological Pitfalls and Adaptive Strategies for the DII
The Dietary Inflammatory Index (DII) has emerged as a valuable tool for quantifying the inflammatory potential of an individual's diet, with applications spanning various health outcomes including mental health, cognitive function, and chronic diseases [3]. However, the synthesis of evidence from multiple studies on the DII is consistently challenged by substantial heterogeneity, which refers to the variability in study findings beyond what would be expected by chance alone. This heterogeneity stems from differences in study populations, design methodologies, dietary assessment tools, and outcome measurements [41] [42]. Addressing this heterogeneity is methodologically crucial for deriving valid and reliable conclusions from meta-analyses, as unaccounted variability can lead to misleading summary estimates and inappropriate clinical or public health recommendations.
The importance of this challenge is reflected in recent high-quality meta-analyses, which have reported I² values ranging from 56% to 81.5%, indicating moderate to substantial heterogeneity [41] [43] [44]. Such heterogeneity necessitates sophisticated methodological approaches to identify its sources, quantify its impact, and provide refined estimates of the association between DII and health outcomes. This article provides comprehensive methodological guidance and practical protocols for addressing heterogeneity in DII research, with the goal of enhancing the rigor and validity of future synthetic research in this field.
Quantitative Evidence of Heterogeneity in DII Research
Table 1: Reported Heterogeneity in Recent DII Meta-Analyses
| Health Outcome | Number of Studies | Reported I² Value | Primary Sources of Heterogeneity Identified |
|---|---|---|---|
| Depression [41] [42] | 43 | 81.5% | Study design, geographic region, dietary assessment methods, depression measurement tools |
| Cognitive Impairment [43] | 9 | 56% | Study population, follow-up duration, cognitive assessment methods |
| Cancer Incidence [45] | 24 | Not specified | Cancer type, study design, population characteristics |
| Low Muscle Mass [46] | 1 (NHANES analysis) | Not applicable | BMI stratification, age, physical activity levels |
The consistent observation of high heterogeneity across DII meta-analyses underscores the complex nature of diet-inflammation-disease pathways. The I² value of 81.5% reported in the depression meta-analysis indicates that the vast majority of variability across studies stems from genuine differences in study methods or populations rather than sampling error alone [41] [42]. Similarly, the moderate heterogeneity (I² = 56%) in cognitive impairment research suggests meaningful methodological differences that must be addressed analytically [43]. These quantitative measures of heterogeneity highlight the necessity of implementing robust methodological approaches to ensure that summary estimates accurately reflect the underlying biological relationships.
Methodological Protocols for Addressing Heterogeneity
Pre-Analysis Protocol: Study Selection and Quality Assessment
A systematic approach to study selection and quality assessment forms the foundation for managing heterogeneity in DII research.
Table 2: Protocol for Quality Assessment in DII Meta-Analyses
| Assessment Domain | Tool/Method | Application to DII Research | Heterogeneity Management Function |
|---|---|---|---|
| Study Design Quality | Newcastle-Ottawa Scale (cohort), AHRQ checklist (cross-sectional) [42] | Evaluate selection, comparability, and outcome assessment | Identifies methodological variations that contribute to heterogeneity |
| Dietary Assessment Rigor | DII-specific quality criteria [3] | Assess validity of DII calculation method, number of food parameters | Controls for measurement heterogeneity in exposure assessment |
| Outcome Measurement | Outcome-specific validity metrics | Evaluate standardization of outcome measurements | Reduces heterogeneity from outcome classification differences |
Procedure:
- Define explicit inclusion criteria a priori in the study protocol, including specifications for study design, population characteristics, DII assessment method, and outcome measurement [42] [44].
- Implement dual independent reviewer system for study selection and quality assessment, with disagreements resolved through consensus or third-party adjudication [41] [47].
- Apply standardized quality assessment tools appropriate to study designs, with particular attention to DII-specific methodological quality including the number of food parameters used in DII calculation and validation of dietary assessment methods [42] [3].
- Document reasons for exclusion systematically to enable transparency and assessment of potential selection biases.
Statistical Protocol: Quantification and Analysis of Heterogeneity
The statistical quantification and modeling of heterogeneity is methodologically essential for valid evidence synthesis.
Procedure:
- Calculate heterogeneity statistics: Compute I², τ², and Cochran's Q statistic to quantify between-study variance [41] [44]. Interpret I² values as follows: 0-30% negligible; 30-50% low; 50-75% moderate; >75% substantial heterogeneity.
- Select appropriate meta-analytic model: Employ random-effects models when I² > 50% to account for between-study variability, as commonly required in DII research [42] [44].
- Conduct subgroup analyses: Pre-specify and conduct subgroup analyses for key variables identified as potential sources of heterogeneity:
- Perform meta-regression: When sufficient studies are available (typically >10), conduct meta-regression to quantitatively explore the association between study-level covariates and effect sizes [45].
- Test for subgroup differences: Statistically compare subgroup estimates using tests for interaction to identify significant moderators of the DII-outcome relationship.
Sensitivity Analysis and Reporting Protocol
Comprehensive sensitivity analyses test the robustness of findings and inform clinical and research implications.
Procedure:
- Conduct leave-one-out analysis: Iteratively remove each study and recalculate summary estimates to identify influential studies [44].
- Assess impact of study quality: Compare estimates including versus excluding studies with lower methodological quality ratings.
- Explore statistical approaches: Compare results using different effect measures (OR vs. RR) and transformation methods when appropriate.
- Evaluate publication bias: Use funnel plots, Egger's test, and other appropriate methods to assess potential publication bias, interpreting results cautiously in the context of substantial heterogeneity [42].
- Implement dose-response analysis: When feasible, use generalized least squares and restricted cubic splines to model nonlinear relationships, as demonstrated in recent DII depression research [41] [42].
Case Study Application: DII and Depression Risk
A recent comprehensive meta-analysis on DII and depression risk provides an exemplary case study of systematic heterogeneity assessment [41] [42]. The analysis included 43 studies and found an overall odds ratio of 1.53 (95% CI: 1.42 to 1.66) for depression risk comparing highest to lowest DII categories, but with substantial heterogeneity (I² = 81.5%).
The investigators implemented comprehensive subgroup analyses that revealed important patterns:
Table 3: Subgroup Analysis from DII-Depression Meta-Analysis
| Subgroup | Odds Ratio | 95% Confidence Interval | Heterogeneity within Subgroup |
|---|---|---|---|
| Overall Association | 1.53 | 1.42 - 1.66 | I² = 81.5% |
| By Study Design | |||
| Cohort studies | 1.31 | 1.19 - 1.45 | Reduced heterogeneity |
| Cross-sectional studies | 1.68 | 1.52 - 1.85 | Reduced heterogeneity |
| By Geographic Region | |||
| Asia | 1.71 | 1.52 - 1.92 | Reduced heterogeneity |
| Western countries | 1.41 | 1.28 - 1.55 | Reduced heterogeneity |
| By BMI Adjustment | |||
| Adjusted for BMI | 1.48 | 1.35 - 1.62 | Reduced heterogeneity |
| Not adjusted for BMI | 1.67 | 1.46 - 1.91 | Reduced heterogeneity |
The subgroup analyses demonstrated that study design, geographic region, and adjustment for BMI explained substantial portions of the observed heterogeneity. Additionally, the dose-response analysis revealed a non-linear relationship (p = 0.0019), with no significant association for DII scores below 0 (anti-inflammatory range) but progressively increasing risk for scores above 0 (pro-inflammatory range) [41] [42]. This nuanced finding exemplifies how sophisticated heterogeneity exploration can reveal clinically meaningful patterns that would be obscured in a simple summary estimate.
Table 4: Research Reagent Solutions for DII Heterogeneity Assessment
| Tool/Resource | Specific Application | Function in Addressing Heterogeneity |
|---|---|---|
| Statistical Software | ||
| STATA (version 18.0+) | Meta-analysis, generalized least squares, restricted cubic splines [41] [42] | Enables sophisticated modeling of nonlinear dose-response relationships and random-effects meta-analysis |
| R package "meta" | Comprehensive meta-analysis procedures [47] [44] | Provides robust statistical tools for heterogeneity quantification and subgroup analysis |
| Methodological Tools | ||
| Cochrane Risk-of-Bias Tool (ROB 2.0) | Randomized controlled trial quality assessment [47] | Standardizes quality evaluation of intervention studies |
| Newcastle-Ottawa Scale | Observational study quality assessment [42] | Provides consistent approach to evaluating methodological quality of cohort and case-control studies |
| DII Calculation Protocol | Standardized DII computation [3] [48] | Ensures consistent exposure assessment across studies |
| Reporting Guidelines | ||
| PRISMA Statement | Systematic review and meta-analysis reporting [41] [47] | Ensures transparent and complete reporting of methods and findings |
| MOOSE Guidelines | Meta-analysis of observational studies | Provides specific guidance for reporting observational study meta-analyses |
Addressing heterogeneity in DII research requires a systematic, multi-faceted approach throughout the meta-analytic process. Based on the evidence and methodologies presented in this article, we recommend the following best practices:
Embrace comprehensive subgroup analysis: Pre-specify and conduct thorough subgroup analyses based on study, population, and methodological characteristics. The consistent observation of differential effects across subgroups in DII research underscores the value of this approach [41] [46] [42].
Prioritize dose-response assessment: Move beyond categorical comparisons to model continuous relationships using sophisticated statistical approaches that can identify non-linear patterns, as demonstrated in recent DII research [41] [42].
Standardize DII assessment methodology: Promote consistent use of validated dietary assessment tools and DII calculation procedures to reduce measurement-related heterogeneity [3] [48].
Account for effect modifiers: Ensure appropriate adjustment for key potential effect modifiers, particularly BMI, which has been identified as a significant modifier in multiple DII studies [46] [48].
Implement transparent reporting: Fully document and report heterogeneity assessment and exploration methods to enable proper interpretation and contextualization of findings.
The systematic assessment and exploration of heterogeneity should not be viewed merely as a methodological requirement but as a scientific opportunity to understand nuanced patterns in the relationship between inflammatory potential of diet and health outcomes. By implementing these rigorous approaches, researchers can transform heterogeneity from a statistical challenge into a substantive opportunity for advancing our understanding of diet-disease relationships and developing targeted, personalized dietary recommendations.
The Dietary Inflammatory Index (DII) has emerged as a vital tool in nutritional epidemiology, quantifying the inflammatory potential of an individual's diet based on scientific literature linking dietary components to inflammatory biomarkers [3]. As research into diet-driven inflammation expands, the precision of DII calculation becomes paramount. A critical methodological challenge lies in accounting for variations in energy intake (total calories consumed) and distinguishing between absolute nutrient intake versus nutrient density. This application note details standardized protocols for addressing these variables, ensuring accurate, comparable DII scoring in research settings, which is essential for advancing our understanding of diet-disease relationships in chronic conditions.
Core Concepts: Energy Adjustment and Nutrient Density
The fundamental challenge in DII calculation is that reported intake of most nutrients correlates strongly with total energy intake. Without adjustment, individuals consuming more calories may artifactually appear to have more pro- or anti-inflammatory diets, confounding true associations between dietary patterns and health outcomes. Energy adjustment statistically removes the effect of total caloric intake, allowing comparison of dietary quality independent of quantity. Nutrient density expresses nutrient intake relative to energy intake (e.g., per 1,000 kcal), reflecting the concentration of nutrients in the diet.
The two primary methodological approaches are detailed in the table below.
Table 1: Energy Adjustment Methods for DII Calculation
| Method | Description | Calculation Steps | Key Advantages | Common Applications |
|---|---|---|---|---|
| Energy-Adjusted DII (E-DII) | Adjusts nutrient intakes for total energy before DII calculation [4] [49] [50]. | 1. Calculate nutrient density (intake per 1,000 kcal).2. Use density values in standard DII scoring [49]. | Isolates effect of food composition from total calories. | Large cohort studies (e.g., UK Biobank [49]), case-control studies [4]. |
| Residual Method | Uses statistical residuals from regression of nutrient intake on energy intake. | 1. Regress each nutrient on total energy.2. Use regression residuals for DII calculation. | Removes energy dependency statistically. | Studies requiring strong covariate control. |
Computational Protocol for Energy-Adjusted DII (E-DII)
This protocol provides a step-by-step guide for calculating the E-DII, the most widely used energy-adjustment method in contemporary research [4] [49] [50].
Materials and Reagents
Table 2: Research Reagent Solutions for DII Calculation
| Item | Specification/Function | Example Sources/Tools |
|---|---|---|
| Dietary Data | Quantitative intake data for foods/nutrients. | 24-hour recalls, Food Frequency Questionnaires (FFQs) [51] [4]. |
| Global Mean Intake Database | Reference values for standardizing nutrient intakes globally [52]. | Published literature from 11 countries [4]. |
| Inflammatory Effect Scores | Pre-defined weights for pro-/anti-inflammatory potential of 45 dietary components [3] [53]. | Shivappa et al. (2014) development paper. |
| Nutrition Analysis Software | Converts food intake to nutrient data. | NUTRITIONIST IV, Nutrition Data System for Research (NDSR), BesÄ°S [51]. |
| Statistical Software | For complex calculations and statistical modeling. | R, SAS, SPSS, Stata. |
Step-by-Step Procedure
Step 1: Data Collection and Preparation
- Collect dietary intake data using a validated dietary assessment tool (e.g., 24-hour recall or FFQ) [51] [4].
- Convert food items into nutrient intakes using appropriate nutritional analysis software. The DII can be computed from a variable number of dietary components; studies show reliable calculation with 26-30 parameters [52] [4] [53].
Step 2: Energy Adjustment of Nutrient Intakes
- For each individual and each nutrient, calculate the energy-adjusted intake using the density method:
Nutrient Density = (Absolute Nutrient Intake / Total Energy Intake in kcal) × 1,000 kcal [49]
Step 3: Standardization with Global Intake Data
- For each energy-adjusted nutrient intake, calculate a Z-score relative to a global reference database [52] [4] [49]:
Z-score = (Individual's Energy-Adjusted Intake - Global Mean Intake) / Global Standard Deviation
Step 4: Conversion to Percentiles and Inflammatory Scores
- Convert Z-scores to centered percentiles (to minimize skew) and multiply by the respective inflammatory effect score [52] [4]:
Centered Percentile = (Percentile Value × 2) - 1
Component DII Score = Centered Percentile × Inflammatory Effect Score
Step 5: Calculation of Overall E-DII Score
- Sum the individual DII scores for all dietary components to obtain the overall E-DII score for the participant [52].
Overall E-DII = Σ(Component DII Scores)
The following workflow diagram illustrates the E-DII calculation process, highlighting the critical branching decision point for energy adjustment.
Diagram 1: E-DII Calculation Workflow (71 characters)
Research Applications and Evidence
The E-DII method has been successfully applied in major research cohorts, demonstrating its utility in linking pro-inflammatory diets to various health outcomes while controlling for energy intake.
Table 3: Select Research Applications of Energy-Adjusted DII
| Study (Source) | Study Design & Population | Key Finding Related to E-DII |
|---|---|---|
| UK Biobank (2025) [49] | Prospective cohort (N=121,329) | Each 1-unit increase in E-DII was associated with a 3.3% increased risk of chronic liver disease (HR: 1.033, P<0.001). |
| Iranian Children (2025) [4] | Case-control (N=500) | Higher E-DII score was associated with increased odds of ADHD (OR: 1.133, 95% CI: 1.021–1.258) in adjusted models. |
| AAA Risk Study (2025) [50] | Prospective cohort (N=142,862) | Individuals with high E-DII scores had a 36% increased risk of abdominal aortic aneurysm (HR: 1.36, 95% CI: 1.09–1.71). |
Best Practices for Research Implementation
- Consistency in Component Selection: The number of dietary components used for DII calculation can vary (e.g., 26-30 components are common) [52] [4] [53]. Researchers must report which components were used and ensure consistency across all study analyses.
- Handling of Incomplete Data: The DII algorithm remains valid even when computed from fewer than the original 45 food parameters [52] [53]. Transparency in reporting missing components is critical for cross-study comparisons.
- Interpretation of Scores: Higher (more positive) DII/E-DII scores indicate a more pro-inflammatory diet, while lower (more negative) scores indicate a more anti-inflammatory diet [31] [53].
- Integration with Covariate Analysis: Energy adjustment does not eliminate the need for appropriate covariate control (e.g., age, BMI, physical activity) in multivariate models analyzing DII-health outcome relationships [4] [49].
The Dietary Inflammatory Index (DII) was established as a quantitative tool to evaluate the inflammatory potential of an individual's overall diet based on scientific literature linking dietary parameters to inflammatory biomarkers [54]. However, the original DII was developed primarily using Western dietary data, creating significant limitations when applied to populations with substantially different dietary patterns and food cultures. This methodological gap prompted the development of culturally adapted versions, notably the Chinese Dietary Inflammatory Index (CHINA-DII), designed specifically to reflect the inflammatory potential of diets within Chinese populations [55] [56].
Cultural adaptation of the DII addresses critical limitations in nutritional epidemiology by accounting for population-specific food combinations, cooking methods, and nutrient intake patterns that influence inflammatory pathways. The CHINA-DII represents a significant methodological advancement by incorporating dietary data relevant to Chinese adults, thereby providing a more accurate assessment of diet-induced inflammation in this population [56]. This protocol outlines the development, validation, and application procedures for population-specific DIIs, using CHINA-DII as a primary case study.
Development Protocol for Population-Specific DIIs
Database Establishment and Dietary Component Selection
The CHINA-DII development followed a rigorous systematic methodology to establish a representative dietary intake database for the target population [55] [56]:
Literature Search Strategy:
- Databases: Comprehensive search across five databases including China National Knowledge Infrastructure (CNKI), Wanfang Data, VIP Chinese Science and Technology Journal Database, PubMed, and Web of Science
- Timeframe: Literature published between January 2009 and December 2024
- Search Terms: Key terms included "dietary," "nutritional status," "nutrition," "intake," "consumption," "China," and "Chinese"
Inclusion and Exclusion Criteria:
- Participants: Chinese adults aged ≥18 years without conditions significantly affecting dietary intake (e.g., diabetes, pregnancy)
- Study Designs: Cross-sectional studies, cohort studies, case-control studies (using only control group data)
- Dietary Assessment Methods: 24-hour dietary recall, food diaries, weighed food method, and food frequency questionnaires (FFQ)
- Sample Size: Studies with ≥200 participants to ensure statistical reliability
- Data Requirements: Studies reporting dietary energy or nutrient intake data convertible to mean and standard deviation
Table 1: Dietary Components Incorporated in CHINA-DII Development
| Component Category | Specific Components Included | Number of Parameters |
|---|---|---|
| Macronutrients | Carbohydrates, protein, cholesterol, polyunsaturated fats (PUFAs), monounsaturated fats (MUFAs), saturated fat, total fat, dietary fiber | 8 |
| Vitamins | Vitamin A, B1 (thiamine), B2 (riboflavin), B6, B12, C, D, E, niacin, folic acid | 10 |
| Minerals | Iron, magnesium, zinc, selenium | 4 |
| Bioactive Compounds | Caffeine, β-carotene, alcohol | 3 |
| Fatty Acids | n-3 fatty acids, n-6 fatty acids | 2 |
Quality Assessment and Data Extraction: All identified literature underwent rigorous quality assessment using established tools. Researchers extracted mean and standard deviation values for each dietary component, creating a standardized database representing typical intake patterns across diverse Chinese subpopulations. The final CHINA-DII incorporated 27 dietary components derived from 33 eligible studies [56].
Calculation Method Adaptation
The CHINA-DII maintains the fundamental calculation structure of the original DII while adapting the reference values to Chinese dietary patterns [56]:
Standardization: Individual nutrient intakes are converted to z-scores by centering on Chinese population mean values and scaling by Chinese standard deviations
Percentile Conversion: z-scores are converted to percentiles and adjusted to a symmetrical -1 to +1 scale
Inflammatory Weight Application: Each value is multiplied by its respective inflammatory effect score derived from the global literature review of diet-inflammatory biomarker relationships
Summation: The overall CHINA-DII score represents the sum of all weighted values, with higher positive scores indicating pro-inflammatory diets and lower negative scores indicating anti-inflammatory diets
Validation Protocols for Population-Specific DIIs
Biomarker Validation Approach
The CHINA-DII validation protocol employed high-sensitivity C-reactive protein (hs-CRP) as an objective inflammatory biomarker to establish criterion validity [55] [56]:
Participant Recruitment:
- Sample: 256 newly diagnosed gastric cancer patients from Fujian Medical University Union Hospital (June 2023-November 2024)
- Inclusion Criteria: Adult Chinese patients with complete dietary and clinical data
- Exclusion Criteria: Conditions causing acute inflammation, corticosteroid use, infectious diseases
Biomarker Assessment:
- hs-CRP Measurement: Venous blood collection after confirmed 8-hour fast, analyzed in standardized laboratory settings
- Inflammatory Threshold: hs-CRP ≥3 mg/L defined as elevated inflammatory status
Statistical Validation Methods:
- Correlation Analysis: Spearman rank correlation between CHINA-DII scores and hs-CRP levels
- Logistic Regression: Multivariate models assessing association between CHINA-DII and elevated hs-CRP risk, adjusted for age, sex, BMI, and other confounders
Validation Results: The CHINA-DII demonstrated significant positive correlation with hs-CRP levels (r = 0.20, p ≤ 0.001). Participants with higher CHINA-DII scores had 1.90-fold increased odds of elevated hs-CRP (95% CI: 1.01-3.55), confirming the index's validity [55].
Disease Outcome Validation
The CHINA-DII was further validated through a case-control study examining gastric cancer risk [54] [57]:
Study Design:
- Participants: 336 newly diagnosed GC cases and 336 sex-matched healthy controls
- Dietary Assessment: Validated food frequency questionnaire (FFQ) covering 78 food items across 13 categories
- Statistical Analysis: Conditional logistic regression models assessing association between CHINA-DII and GC risk
Table 2: CHINA-DII Validation Against Gastric Cancer Outcomes
| Validation Parameter | Results | Statistical Significance |
|---|---|---|
| Overall CHINA-DII and GC Risk | OR = 1.45 (95% CI: 1.05-1.99) | p < 0.05 |
| Per 1-SD Increase in CHINA-DII | OR = 1.26 (95% CI: 1.07-1.48) | p < 0.05 |
| Subgroup: Age ≤55 years | OR = 2.44 (95% CI: 1.51-3.96) | p < 0.001 |
| Subgroup: Non-smokers | OR = 1.70 (95% CI: 1.14-2.54) | p < 0.05 |
| Subgroup: High stress | OR = 2.82 (95% CI: 1.67-4.75) | p < 0.001 |
Application Protocols for Research Settings
Dietary Assessment Methods
The CHINA-DII application requires standardized dietary data collection [54] [57]:
Food Frequency Questionnaire (FFQ) Administration:
- Structure: 78 food items across 13 categories (staple foods, vegetables, fruits, meats, seafood, etc.)
- Timeframe: Usual dietary intake over past 12 months
- Frequency Options: 9 response categories from "≥4 times/day" to "never"
- Portion Sizes: Standardized portions with visual aids for accuracy
Data Processing Protocol:
- Convert frequency responses to daily intake values
- Calculate nutrient composition using Chinese Food Composition Tables
- Compute individual dietary component scores
- Apply CHINA-DII algorithm to derive overall score
Statistical Analysis Guidelines
Primary Analysis Models:
- Continuous Analysis: Linear or logistic regression with CHINA-DII as continuous variable
- Categorical Analysis: Quartile or tertile analysis comparing extreme categories
- Adjustment Variables: Age, sex, energy intake, BMI, smoking, education, physical activity
Advanced Analytical Approaches:
- Stratified Analysis: Assessment of effect modification by demographic/lifestyle factors
- Mediation Analysis: Evaluation of DII as mediator between dietary patterns and health outcomes [58] [59]
- Dose-Response Analysis: Restricted cubic splines for nonlinear relationship assessment [60]
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Materials for CHINA-DII Implementation
| Research Tool | Specifications | Application Purpose |
|---|---|---|
| Validated FFQ | 78 food items, 13 categories, 9 frequency options, portion size images | Standardized dietary data collection in Chinese populations |
| Chinese Food Composition Table | Nutrient profiles for traditional Chinese foods and preparation methods | Accurate nutrient intake calculation |
| hs-CRP Assay Kits | High-sensitivity immunoassay, detection limit ≤0.1 mg/L | Objective inflammation biomarker validation |
| Dietary Analysis Software | Customizable database integrating Chinese dietary components | Efficient CHINA-DII score calculation |
| Biological Sample Collection | EDTA tubes, standardized phlebotomy protocols | Biomarker correlation studies |
Interpretation Guidelines and Clinical Relevance
Reference Ranges and Clinical Correlations
Based on validation studies, the average CHINA-DII score in Chinese populations is approximately -2.11 ± 0.62, reflecting the generally anti-inflammatory nature of traditional Chinese diets [54]. Each 1-standard-deviation increase in CHINA-DII score associates with a 26% increased gastric cancer risk (OR = 1.26, 95% CI: 1.07-1.48), providing quantitative risk assessment capabilities [54] [57].
Subgroup-Specific Considerations
Research indicates varying susceptibility to dietary inflammation across subpopulations:
- Younger adults (≤55 years) show stronger association between CHINA-DII and gastric cancer risk (OR = 2.44) [54]
- Non-smokers demonstrate greater dietary inflammation susceptibility than smokers [54]
- High-stress individuals exhibit significantly amplified DII-disease relationships [54]
The CHINA-DII development protocol provides a validated framework for creating population-specific dietary inflammation assessment tools. Its successful application demonstrates the critical importance of cultural adaptation in nutritional epidemiology. The comprehensive methodology spanning database development, biomarker validation, and disease outcome assessment establishes a rigorous standard for future population-specific DII development in diverse ethnic and cultural groups.
The provided protocols enable researchers to implement the CHINA-DII in studies examining diet-inflammatory disease relationships in Chinese populations, with potential adaptation for other cultural contexts. This methodological advancement addresses significant limitations in applying Western-developed dietary indices to non-Western populations, enhancing the accuracy and cultural relevance of nutritional epidemiology research worldwide.
The assessment of Dietary Inflammatory Index (DII) in observational research requires rigorous methodological evaluation to ensure result validity. Within nutritional epidemiology, the Risk Of Bias In Non-randomized Studies - of Interventions (ROBINS-I) tool and the Newcastle-Ottawa Scale (NOS) serve as critical instruments for evaluating study quality and potential biases. The DII, a quantitative measure of diet's inflammatory potential based on 45 food parameters, has been associated with diverse health outcomes including depression, COVID-19 severity, and cognitive decline in recent studies [14] [11] [42]. However, the observational nature of most DII research necessitates careful bias assessment to distinguish true biological effects from methodological artifacts. The ROBINS-I tool, recently updated to version 2 (ROBINS-I V2), provides a structured framework for assessing risk of bias across seven domains, while NOS offers a standardized approach for quality assessment of non-randomized studies in systematic reviews [61] [62]. This article provides detailed protocols for applying these tools specifically within DII research context.
The ROBINS-I Tool: Framework and Application to DII Research
ROBINS-I Version 2 Updates and Key Features
The ROBINS-I tool has recently been updated to Version 2 (November 2024), introducing several key enhancements over the 2016 version. A fundamental improvement is the addition of algorithms that map answers to signaling questions onto proposed risk-of-bias judgments for each domain [62]. The tool now differentiates between "strong" and "weak" responses to signaling questions, replacing the previous "(Probably) yes" or "(Probably) no" options [62]. This refinement allows for more nuanced risk assessment. Additionally, ROBINS-I V2 includes a new 'triage' section that provides quick mapping to 'Critical risk of bias' when appropriate and addresses specific biases such as those arising from immortal time through new questions in Domains 2 and 3 [62]. The tool now more clearly specifies whether a study is estimating a per-protocol effect (if analyses account for protocol deviations) or an intention-to-treat effect, with Domain 1 (confounding) split into two variants depending on the effect of interest [62].
ROBINS-I Assessment Protocol for DII Studies
The application of ROBINS-I to DII research requires careful consideration of the unique methodological challenges in nutritional epidemiology. The following protocol outlines a systematic approach:
Phase 1: Preliminary Setup
- Define the target trial: Specify the hypothetical randomized controlled trial that the observational study is attempting to emulate, including key elements like eligibility criteria, intervention (DII levels), comparator (reference DII category), outcomes, and follow-up [62].
- Specify the effect of interest: Determine whether the study aims to estimate the effect of assignment (intention-to-treat) or the effect of adherence (per-protocol), as this affects the assessment of Domain 1 (confounding) and Domain 4 (deviations from intended interventions) [62].
- Identify confounding domains: For DII studies, pre-specify likely important confounders such as age, sex, BMI, socioeconomic status, physical activity, smoking status, and total energy intake [14] [4].
Phase 2: Domain Evaluations Complete signaling questions for each of the seven bias domains, with particular attention to DII-specific considerations:
- Domain 1 (Confounding): Evaluate whether important confounders were appropriately measured and controlled for. In DII studies, special attention should be paid to total energy intake and physical activity, as these are strong potential confounders [14] [4].
- Domain 2 (Classification of Interventions): Assess whether DII assessment was biased. Consider the validity of dietary assessment tools (e.g., FFQs), timing of dietary assessment relative to outcome occurrence, and handling of immortal time bias [62].
- Domain 3 (Selection into the study): Evaluate whether selection of participants into the study based on DII levels or related factors introduced bias.
- Domain 4 (Missing data): The reconceived domain in V2 requires careful evaluation of the amount and nature of missing DII or outcome data and the appropriateness of handling methods [62].
- Domain 5 (Measurement of outcomes): Assess whether outcome assessment was blinded to DII status and used consistent methods across exposure groups.
- Domain 6 (Selection of reported result): Evaluate whether the analysis was pre-specified and whether selective reporting is evident [62].
Phase 3: Judgment and Synthesis
- Determine risk of bias: For each domain, judge risk as "Low," "Some concerns," "High," or "Critical" using the ROBINS-I V2 algorithms [62].
- Make overall judgment: Synthesize domain-level judgments into an overall risk of bias assessment, considering the worst domain judgment as starting point but evaluating if other domains elevate concern [62].
- Predict direction of bias: If risk of bias is not low, predict the likely direction of bias (e.g., toward or away from null) for each result.
ROBINS-I Signaling Pathway and Workflow
The following diagram illustrates the logical workflow for applying the ROBINS-I tool to DII studies:
ROBINS-I Assessment Workflow for DII Studies
Newcastle-Ottawa Scale (NOS): Framework and Protocol
NOS Structure and Scoring System
The Newcastle-Ottawa Scale is a specialized tool for assessing the quality of non-randomized studies in systematic reviews, using a "star system" to evaluate studies across three broad perspectives: selection of study groups, comparability of groups, and assessment of outcome or exposure [63] [42]. For cohort studies of DII and health outcomes, the NOS evaluates eight items with a maximum score of 9 stars, while case-control studies are evaluated across similar domains with appropriate modifications for study design differences. Studies are typically categorized as high quality (≥7 stars), moderate quality (4-6 stars), or low quality (≤3 stars) based on their total score [42]. The strength of NOS lies in its simplicity and widespread adoption in meta-analyses of observational studies, including recent DII research on depression, COVID-19, and cognitive outcomes [63] [42] [43].
NOS Assessment Protocol for DII Studies
Selection Domain (Maximum 4 stars)
- Representativeness of exposed cohort: Award one star if the DII study sample is truly representative of the average population (describe the sampling method and population framework).
- Selection of non-exposed cohort: Award one star if the non-exposed cohort (e.g., anti-inflammatory diet group) is drawn from the same community as the exposed cohort (pro-inflammatory diet group).
- Ascertainment of exposure: Award one star if DII is validated through secure record (e.g., dietary records) or structured interview where blind to case/control status.
- Demonstration that outcome of interest was not present at start: Award one star for prospective studies where participants were free of the health outcome at baseline.
Comparability Domain (Maximum 2 stars)
- Comparability of cohorts on basis of design or analysis: Award one star if the study controls for age and sex; award a second star if the study controls for other important confounders such as BMI, physical activity, smoking status, or total energy intake [14] [4].
Outcome Domain (Maximum 3 stars)
- Assessment of outcome: Award one star if outcome assessment is independent blind to DII status or based on secure records.
- Adequacy of follow-up length: Award one star if follow-up is sufficiently long for outcomes to occur (varies by outcome; e.g., ≥5 years for chronic diseases).
- Adequacy of follow-up completeness: Award one star if follow-up rate is ≥80% and no significant differences between completers and dropouts.
NOS Assessment Workflow
The following diagram illustrates the logical workflow for applying the NOS tool to DII studies:
NOS Assessment Workflow for DII Studies
Research Reagent Solutions for DII Studies
Table 1: Essential Methodological Components for DII Research Quality
| Research Component | Function in DII Research | Implementation Considerations |
|---|---|---|
| Validated FFQ | Assesses dietary intake of 45 food parameters for DII calculation | Must be validated in specific population; consider cultural dietary variations [11] [4] |
| Global Intake Database | Provides reference values for DII z-score calculation | Composite database from 11 countries provides global norms [11] |
| Energy Adjustment Method | Controls for confounding by total energy intake | Use energy density method (intake per 1000 calories) for E-DII calculation [4] |
| Inflammatory Biomarkers | Validates DII construct (e.g., CRP, IL-6, TNF-α) | Not required for DII calculation but important for validation [11] |
| Genetic Instruments | Enables Mendelian randomization to assess causality | e.g., SNP rs7910002 associated with DII in recent GWAS [14] |
| Covariate Assessment Tools | Measures potential confounders (age, sex, BMI, physical activity, smoking) | Standardized protocols essential for comparability across studies [14] [4] |
Comparative Analysis of Tool Applications in DII Research
Table 2: Application of ROBINS-I and NOS to Recent DII Studies
| Study Focus | ROBINS-I Assessment Considerations | NOS Quality Indicators | Key Findings |
|---|---|---|---|
| DII & Depression [42] | Domain 1: Control for physical activity, BMI; Domain 4: Missing data methods for dietary assessment | Comparability stars for controlling age, sex, BMI, physical activity | OR = 1.53 (95% CI: 1.42-1.66) for depression with higher DII; nonlinear relationship |
| DII & COVID-19 [63] | Domain 2: Timing of dietary assessment relative to pandemic; Domain 3: Selection bias in testing access | Outcome assessment: Independent diagnosis via medical records | OR = 1.57 (95% CI: 1.14-2.17) for infection; 1.31 increased risk per 1-point E-DII increase |
| DII & Cognitive Impairment [43] | Domain 1: Control for education, vascular risk factors; Domain 5: Blinding of cognitive assessment | Adequacy of follow-up length for dementia outcomes (≥5 years) | RR = 1.34 (95% CI: 1.15-1.55) for cognitive impairment with high DII |
| DII & ADHD [4] | Domain 2: Recall bias in FFQ administration by parents; Domain 1: Control for socioeconomic status | Ascertainment of exposure: Structured interview blind to case/control status | OR = 1.133 (95% CI: 1.021-1.258) for ADHD with higher E-DII in Iranian children |
| DII & Multiple Outcomes [14] | Domain 6: Selective reporting across 845 health outcomes; Domain 1: Control for multiple confounders | Representativeness: Large population-based cohort (UK Biobank) | 133 outcomes associated with DII; MR confirmed causality for abdominal hernia, cholelithiasis, back pain |
Advanced Methodological Protocols for DII Research
DII Calculation and Validation Protocol
The computation of DII scores requires meticulous attention to methodological details to ensure validity and comparability across studies:
Step 1: Dietary Data Collection
- Administer a validated food frequency questionnaire (FFQ) appropriate for the population being studied. The FFQ should capture intake of all available DII parameters (up to 45 food parameters) [11] [4].
- For pediatric populations (e.g., ADHD studies), parent-reported FFQs with visual aids for portion sizes may be necessary, though this introduces potential proxy-reporting bias [4].
Step 2: Energy Adjustment and Z-score Calculation
- Convert raw nutrient intakes to energy-adjusted values using the density method (intake per 1000 calories) to compute the Energy-adjusted DII (E-DII) [4].
- Calculate z-scores for each dietary parameter using the formula:
z-score = (individual mean intake - global mean intake) / global standard deviation[4]. The global means and SDs are derived from a composite database of 11 populations worldwide [11].
Step 3: DII Score Computation
- Convert z-scores to centered percentiles to address right-skewing:
percentile = (z-score cumulative proportion * 2) - 1[11] [4]. - Multiply each centered percentile by its respective overall inflammatory effect score from the literature [11].
- Sum the individual food parameter scores to obtain the overall DII score, where negative values indicate anti-inflammatory diets and positive values indicate pro-inflammatory diets [11].
Step 4: Validation and Sensitivity Analysis
- Where possible, validate DII scores against inflammatory biomarkers (e.g., CRP, IL-6) to confirm construct validity [11].
- Conduct sensitivity analyses using different subsets of DII parameters when complete data are unavailable, noting this as a limitation [4].
Mendelian Randomization Integration Protocol
Recent advances in DII research incorporate Mendelian randomization to address residual confounding:
Step 1: Genetic Instrument Identification
- Conduct genome-wide association studies (GWAS) to identify genetic variants associated with DII (e.g., SNP rs7910002) meeting genome-wide significance (P < 5×10â»â¸) [14].
- Calculate proportion of DII variance explained (e.g., 0.12% for rs7910002) and ensure F-statistic >10 to minimize weak instrument bias [14].
Step 2: MR Analysis Implementation
- Construct genetic risk scores for DII and assess associations with health outcomes in large biobanks (e.g., UK Biobank, FinnGen) [14].
- Apply two-sample MR methods (e.g., Wald ratio) to estimate causal effects of DII on health outcomes [14].
- Triangulate evidence from observational analyses and MR to identify convincing (Level I) versus suggestive associations [14].
The rigorous application of ROBINS-I and NOS tools is essential for evaluating methodological quality and risk of bias in DII research. The recent introduction of ROBINS-I Version 2 provides enhanced capacity to address specific biases in nutritional epidemiology, including immortal time and confounding [62]. When applied systematically alongside the standardized NOS assessment, these tools enable researchers to distinguish robust associations from methodological artifacts in the rapidly expanding field of diet-induced inflammation. The integration of Mendelian randomization approaches further strengthens causal inference in DII research [14]. As evidence accumulates linking pro-inflammatory diets to diverse health outcomes including mental health, neurodevelopmental disorders, and infection susceptibility [14] [4] [63], the consistent application of these quality assessment tools will be crucial for generating reliable evidence to inform public health recommendations and clinical practice.
Establishing Robustness: Biomarker Validation and Comparative Analysis of Dietary Indices
The Dietary Inflammatory Index (DII) is a quantitative tool developed to assess the inflammatory potential of an individual's overall diet [11]. It was designed to provide a standardized method for evaluating how diet modulates chronic inflammation, an underlying pathophysiological process in many chronic diseases [64] [3]. The validation of DII scores against established inflammatory biomarkers is crucial for establishing its utility in research and clinical practice, particularly for researchers and drug development professionals investigating nutrition-inflammation-disease pathways.
The DII is based on an extensive review of the scientific literature, initially encompassing 1,943 articles published between 1950 and 2010, which examined the effects of 45 dietary parameters on six inflammatory biomarkers: IL-1β, IL-4, IL-6, IL-10, TNF-α, and CRP [64] [11]. Each dietary parameter receives a score based on its effect on these biomarkers: +1 for pro-inflammatory effects (significantly increasing IL-1β, IL-6, TNF-α, or CRP, or decreasing IL-4 or IL-10), -1 for anti-inflammatory effects, and 0 for no significant effect [64]. The overall DII score for an individual represents the sum of the inflammatory potential of all dietary components consumed, with positive scores indicating pro-inflammatory diets and negative scores indicating anti-inflammatory diets [64] [11].
Table 1: Core Inflammatory Biomarkers Used in DII Validation
| Biomarker | Biological Role | Relationship with DII |
|---|---|---|
| hs-CRP | Acute-phase protein produced by the liver in response to inflammation | Consistently positively correlated with DII scores |
| IL-6 | Pro-inflammatory cytokine that stimulates immune response | Significantly associated with higher DII scores in multiple studies |
| TNF-α | Pro-inflammatory cytokine involved in systemic inflammation | Elevated in individuals with pro-inflammatory dietary patterns |
| IL-1β | Pro-inflammatory cytokine that promotes inflammation | Incorporated in DII development and validation |
| IL-4 | Anti-inflammatory cytokine that downregulates inflammation | Higher DII scores associated with reduced IL-4 |
| IL-10 | Anti-inflammatory cytokine that inhibits inflammatory responses | Higher DII scores associated with reduced IL-10 |
Quantitative Evidence: DII-Biomarker Correlations
Substantial evidence from observational studies and meta-analyses demonstrates consistent associations between DII scores and inflammatory biomarkers. A 2023 meta-analysis of 14 studies involving 59,941 individuals found that higher DII scores were significantly associated with increased odds of elevated CRP (E-CRP). The calculated pooled odds ratio (OR) of E-CRP in the highest DII category was 1.39 (95% CI: 1.06, 1.14) compared to the lowest DII category [65]. The same analysis showed that each unit increase in DII as a continuous variable generally elicited a 10% increase in the odds of E-CRP (OR 1.10, 95% CI 1.06, 1.14) [65].
Multiple cohort studies have validated the association between DII scores and inflammatory biomarkers across diverse populations. In a longitudinal analysis of 559 healthy participants, higher DII scores were associated with values of high-sensitivity (hs)-CRP greater than 3 mg/L [64]. A cross-sectional analysis with 2,524 healthy participants found the DII score was positively associated with IL-6 (>1.6 pg/mL) and homocysteine (>15 μmol/L) [64]. Among 2,567 postmenopausal women, the DII score was significantly associated with IL-6, TNF-α, and hs-CRP [64].
Table 2: Summary of Key DII-Biomarker Validation Studies
| Study Population | Sample Size | DII Assessment | Key Findings | Reference |
|---|---|---|---|---|
| Multiple Studies (Meta-analysis) | 59,941 individuals | Various methods | OR for elevated CRP = 1.39 (95% CI: 1.06-1.14) for highest vs. lowest DII | [65] |
| Healthy Participants | 559 | Not specified | Higher DII associated with hs-CRP >3 mg/L | [64] |
| Healthy Participants | 2,524 | Not specified | DII positively associated with IL-6 (>1.6 pg/mL) | [64] |
| Postmenopausal Women | 2,567 | Not specified | DII associated with IL-6, TNF-α, and hs-CRP | [64] |
| PREDIMED-Navarra Study | Not specified | Not specified | Greater DII associated with ~2x higher risk of telomere shortening | [64] |
The biological plausibility of these associations is supported by research showing that specific dietary components modulate inflammatory pathways. For instance, the Mediterranean diet - rich in fruits, extra-virgin olive oil, red wine, nuts, and polyphenols - demonstrates anti-inflammatory properties, while diets high in red meat and processed foods exhibit pro-inflammatory effects [64].
Experimental Protocols for DII Validation
Dietary Assessment and DII Calculation
Protocol Objective: To standardize the assessment of dietary intake and calculation of DII scores for correlation with inflammatory biomarkers.
Materials and Equipment:
- Validated Food Frequency Questionnaire (FFQ) or 24-hour dietary recall forms
- Nutrition analysis software (e.g., Nutritionist IV, NDS-R)
- Global database of mean intake values for 45 food parameters
- Standardized DII calculation algorithm
Procedure:
- Dietary Data Collection: Administer a validated FFQ or conduct 24-hour dietary recalls. The FFQ should capture frequency and portion size of food items consumed over a specified period (typically the past year) [66]. For 24-hour recalls, conduct multiple unannounced recalls (including both weekdays and weekend days) to account for day-to-day variation [67].
Nutrient Analysis: Process dietary data using nutrition analysis software to quantify intake of the DII parameters. Of the original 45 food parameters, typically 28-36 are used in practice depending on cultural dietary patterns and data availability [64] [66].
Z-score Calculation: For each food parameter, subtract the individual's intake from the global mean intake and divide by the global standard deviation to create a z-score:
The global means and standard deviations are derived from a composite database of 11 populations worldwide [11] [67].
Percentile Conversion: Convert z-scores to percentiles to achieve a symmetrical distribution centered on zero. This is done by doubling the percentile and subtracting 1 [64] [67].
Inflammatory Effect Scoring: Multiply each centered percentile by the respective food parameter's inflammatory effect score derived from the literature review [64] [11].
Total DII Calculation: Sum all food parameter-specific scores to obtain the overall DII score for each individual [64] [67].
Quality Control:
- Train dietitians in standardized dietary assessment techniques
- Use visual aids (e.g., food albums) to improve portion size estimation accuracy
- Implement data cleaning procedures to identify and address implausible intake values
- Conduct reliability assessments for dietary measures
DII Calculation Workflow: This diagram illustrates the standardized procedure for calculating Dietary Inflammatory Index scores from dietary intake data.
Biomarker Measurement Protocols
Protocol Objective: To standardize the collection, processing, and analysis of inflammatory biomarkers for correlation with DII scores.
Materials and Equipment:
- Phlebotomy supplies (needles, vacutainer tubes, serum separator tubes)
- Centrifuge capable of 1000-2000 × g
- -80°C freezer for sample storage
- ELISA kits for hs-CRP, IL-6, TNF-α, or other biomarkers of interest
- Microplate reader with appropriate filters
- Laboratory information management system (LIMS)
Blood Collection and Processing Procedure:
- Patient Preparation: Instruct participants to fast for 8-12 hours prior to blood collection. Record time of collection, recent illnesses, and medications.
Phlebotomy: Collect blood samples using appropriate venipuncture technique. Draw into serum separator tubes for cytokine analysis and EDTA tubes for complete blood count.
Sample Processing: Allow blood to clot at room temperature for 30 minutes. Centrifuge at 1000-2000 × g for 10-15 minutes. Aliquot serum into cryovials within 2 hours of collection.
Sample Storage: Store aliquots at -80°C until analysis. Avoid repeated freeze-thaw cycles.
hs-CRP Measurement via ELISA:
- Reagent Preparation: Bring all reagents and samples to room temperature. Prepare standards according to manufacturer's instructions.
Plate Setup: Add standards and samples to appropriate wells. Include blanks as specified.
Incubation: Incubate for specified time (typically 1-2 hours) at room temperature.
Washing: Wash plates 4-6 times with wash buffer.
Detection: Add detection antibody and incubate. Add substrate solution and incubate in dark.
Stop Reaction: Add stop solution and read absorbance at appropriate wavelength.
Calculation: Generate standard curve and calculate sample concentrations.
Quality Assurance:
- Include quality control samples with known concentrations in each assay run
- Determine intra-assay and inter-assay coefficients of variation
- Establish sample rejection criteria for hemolyzed, lipemic, or icteric samples
- Implement blind duplicate analysis for a subset of samples
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for DII Validation Studies
| Reagent/Equipment | Specifications | Research Application |
|---|---|---|
| Validated FFQ | Culture-specific, 100+ food items, tested for reproducibility | Standardized assessment of habitual dietary intake |
| 24-Hour Recall Forms | Structured interview protocol, multiple passes, portion size aids | Detailed assessment of recent dietary intake |
| Global DII Database | Means and SDs for 45 parameters from 11 populations worldwide | Reference for calculating Z-scores in DII algorithm |
| ELISA Kits (hs-CRP, IL-6, TNF-α) | High sensitivity, validated precision and accuracy | Quantification of inflammatory biomarkers in serum/plasma |
| Nutrition Analysis Software | Compatible with local food databases, calculates micro/macronutrients | Conversion of food intake to nutrient composition |
| Cryogenic Storage | -80°C freezers, barcoded cryovials, inventory system | Preservation of biological samples for batch analysis |
| LIMS | Sample tracking, chain of custody, QC data management | Maintenance of sample integrity and data accuracy |
Biological Pathways Linking Diet to Inflammation
The association between DII scores and inflammatory biomarkers reflects the complex interplay between dietary components and the immune system. Pro-inflammatory diets typically characterized by high intake of saturated fats, refined carbohydrates, and processed meats can activate multiple inflammatory pathways:
NF-κB Pathway Activation: Saturated fatty acids and advanced glycation end products (AGES) from processed foods can activate toll-like receptors (TLRs), leading to nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB) translocation to the nucleus. This promotes transcription of pro-inflammatory cytokines including TNF-α, IL-6, and CRP [64].
Inflammasome Activation: Certain dietary patterns may activate the NLRP3 inflammasome, resulting in increased production of IL-1β and IL-18 [3].
Anti-Inflammatory Mechanisms: Conversely, anti-inflammatory dietary components such as omega-3 fatty acids, polyphenols, and fiber from fruits, vegetables, and whole grains can inhibit NF-κB activation, promote production of anti-inflammatory cytokines like IL-10, and reduce expression of adhesion molecules [64] [11].
Diet-Inflammation Biological Pathways: This diagram illustrates the mechanistic pathways through which pro-inflammatory and anti-inflammatory dietary patterns influence systemic inflammation.
Methodological Considerations and Best Practices
DII Calculation Adaptations
Researchers have developed several adaptations of the original DII to address methodological considerations:
The energy-adjusted DII (E-DII) was developed to account for total energy intake, which can confound the relationship between diet and inflammation [11] [65]. In some studies, the E-DII has shown stronger associations with inflammatory biomarkers than the standard DII [65].
Cultural adaptations are often necessary, as the original 45 food parameters may not all be relevant in every population. For example, a study in Iran used 30 of the original 45 parameters due to cultural dietary patterns and limited food composition data [66]. Similarly, alcohol parameters are often excluded in studies of predominantly Muslim populations [66].
Biomarker Selection and Measurement
When validating DII scores against inflammatory biomarkers, researchers should consider:
Biomarker Specificity: CRP is a general marker of inflammation, while cytokines like IL-6 and TNF-α provide more specific information about immune activation. Including multiple biomarkers provides a more comprehensive assessment of inflammatory status [64] [65].
Temporal Relationships: Single measurements of inflammatory biomarkers may not reflect chronic inflammation. Where feasible, repeated measures of both diet and biomarkers provide more robust data on their relationship [67].
Measurement Methods: Studies using high-sensitivity CRP (hs-CRP) assays tend to find stronger associations with DII than those using standard CRP assays, as hs-CRP can detect lower levels of inflammation [65]. Similarly, studies using 24-hour dietary recalls may show different effect sizes compared to those using FFQs, possibly due to differences in dietary assessment accuracy [65].
The validation of DII scores against established inflammatory biomarkers provides a scientific foundation for using this tool in nutritional epidemiology, clinical research, and potentially clinical practice. The consistent associations observed between higher DII scores and elevated levels of hs-CRP, IL-6, and TNF-α across diverse populations support the utility of the DII as a valid measure of dietary inflammatory potential.
For researchers and drug development professionals, the DII offers a standardized approach to quantifying the inflammatory aspect of diet, which can be integrated into studies of disease etiology, prevention, and management. The protocols outlined in this document provide methodological guidance for conducting rigorous DII validation studies, with attention to dietary assessment, biomarker measurement, and data analysis considerations.
As research in this field evolves, further refinement of the DII and its adaptations will continue to enhance its validity and applicability across diverse populations and disease contexts.
Dietary pattern analysis has emerged as a critical methodology in nutritional epidemiology, moving beyond single-nutrient approaches to capture the complex interactions of foods and nutrients consumed in combination [68]. These methods broadly fall into two categories: a priori (hypothesis-driven) and a posteriori (exploratory) approaches [69] [70]. A priori methods, including the Dietary Inflammatory Index (DII), assess adherence to predefined dietary patterns based on existing nutritional knowledge or health evidence. In contrast, a posteriori methods use multivariate statistical techniques to derive dietary patterns specific to the study population [70] [68]. The DII represents a novel a priori approach that specifically quantifies the inflammatory potential of diet, filling a significant gap left by other indices that measure general diet quality or adherence to dietary guidelines without direct reference to inflammation [71] [11].
Theoretical Foundations and Index Construction
A Priori Dietary Indices: Conceptual Frameworks
A priori dietary indices are grounded in prior knowledge of diet-health relationships and are typically designed to measure adherence to dietary recommendations or specific dietary patterns associated with health outcomes [69] [70]. Unlike a posteriori methods, these approaches apply predetermined criteria to dietary intake data, allowing for comparison across studies and populations. The DII represents a specialized a priori approach that differs fundamentally from other indices as it is not based on dietary recommendations but rather on empirical evidence linking dietary components to inflammatory biomarkers [11].
Table 1: Key Characteristics of Major A Priori Dietary Indices
| Index Name | Theoretical Basis | Components | Scoring Approach | Primary Application |
|---|---|---|---|---|
| Dietary Inflammatory Index (DII) | Literature linking diet to inflammatory biomarkers [71] [11] | Up to 45 food parameters (nutrients, foods, compounds) [11] [72] | Continuous score (-pro-inflammatory to +anti-inflammatory) [11] | Quantifying inflammatory potential of diet |
| Healthy Eating Index (HEI) | USDA Dietary Guidelines [71] [70] | 13 components (9 adequacy, 3 moderation) [71] | 0-100 point scale [71] | Assessing adherence to federal dietary guidance |
| Alternative Healthy Eating Index (AHEI) | Dietary patterns associated with chronic disease risk [71] [70] | 9-11 components including specific foods and nutrients [71] | 0-10 per component, total 0-110 [71] | Predicting chronic disease risk |
| Mediterranean Diet Score (MDS) | Traditional Mediterranean dietary patterns [11] [68] | 7-9 components based on Mediterranean diet foods [68] | Various scoring systems, often 0-9 [68] | Assessing Mediterranean diet adherence |
A Posteriori Dietary Patterns: Data-Driven Approaches
A posteriori methods use statistical techniques to identify eating patterns within study populations without predefined nutritional hypotheses. These include:
- Factor Analysis and Principal Component Analysis (PCA): Identify intercorrelations between food groups to derive patterns that explain maximum variation in consumption [70] [68].
- Reduced Rank Regression (RRR): Derives patterns that explain variation in response variables (e.g., biomarkers) related to specific diseases [70] [68].
- Cluster Analysis: Classifies individuals into mutually exclusive groups with similar dietary intake [70] [68].
These methods are population-specific and may not be directly comparable across studies, representing a significant limitation compared to a priori approaches [70] [68].
The Dietary Inflammatory Index: A Specialized A Priori Tool
Development and Validation
The DII was developed through systematic review of peer-reviewed literature published through 2010 on the association between dietary components and six inflammatory biomarkers: IL-1β, IL-4, IL-6, IL-10, TNF-α, and CRP [71] [11] [72]. From 1,943 qualifying research articles, effect scores for 45 food parameters were derived, representing the inflammatory potential of each parameter [71] [11]. The DII calculation involves comparing actual intake of these parameters to a global reference database representing mean intakes from 11 populations worldwide [11]. This global standardization enables cross-population comparisons, addressing a significant limitation of other indices [11].
Calculation Methodology
The DII calculation protocol involves multiple steps to ensure standardized application across studies:
- Dietary Assessment: Collect dietary intake data using 24-hour recalls, food frequency questionnaires, or food records [11] [73].
- Parameter Alignment: Match available dietary data to the 45 DII food parameters (including nutrients, flavonoids, and spices) [11].
- Z-score Calculation: For each parameter, calculate a z-score by subtracting the global mean intake and dividing by the standard deviation using the world composite database [11].
- Percentile Conversion: Convert z-scores to percentiles to minimize the effect of right-skewing common in dietary data [11].
- Centering: Center percentiles by doubling and subtracting 1.0 to achieve a symmetric distribution centered on zero [11].
- Inflammatory Effect Scoring: Multiply centered scores by the respective food parameter's inflammatory effect score from the literature [11].
- Index Summation: Sum across all food parameters to obtain the overall DII score [11].
The DII can be energy-adjusted (E-DII) by calculating the score per 1000 kcal consumed, controlling for total energy intake [72] [74]. The theoretical range of DII scores is -8.87 (maximally anti-inflammatory) to +7.98 (maximally pro-inflammatory), with zero representing a neutral diet [72].
Figure 1: DII Calculation Workflow. The Dietary Inflammatory Index (DII) is derived through a multi-step process that compares individual dietary intake to global reference values and applies literature-derived inflammatory effect scores.
Comparative Analysis: DII versus Traditional Dietary Indices
Correlation with Established Indices
Research demonstrates significant correlations between the DII and other dietary quality indices, though these relationships are moderate, suggesting the DII captures unique aspects of dietary inflammatory potential. In the Energy Balance Study, linear regression analyses indicated that as DII increased (more pro-inflammatory), AHEI, HEI-2010, and DASH index scores decreased (more unhealthy, all p<0.01) [71]. Subsequent validation studies have reported correlation coefficients in the range of r = 0.52–0.65 between DII and traditional indices including HEI and DASH [72].
Table 2: Comparative Performance of Dietary Assessment Indices in Research Settings
| Index | Theoretical Foundation | Strengths | Limitations | Validation against Inflammatory Biomarkers |
|---|---|---|---|---|
| DII | Empirical evidence linking diet to inflammation [11] | Specifically measures inflammatory potential; applicable across populations [11] | Dependent on available dietary parameters; requires understanding of inflammatory biology [11] | Specifically validated against CRP, IL-6, TNF-α [11] [72] |
| HEI | USDA Dietary Guidelines [71] | Standardized scoring; tracks compliance with national guidelines [70] | Population-specific applicability issues; changes with guideline updates [68] | Moderate correlation with inflammatory markers via DII [71] [72] |
| AHEI | Foods and nutrients predictive of chronic disease [71] | Strong predictive validity for chronic diseases [70] | May not capture inflammatory potential specifically [71] | Associated with inflammation primarily through DII correlation [71] |
| DASH | Dietary pattern to reduce hypertension [71] | Clinical trial evidence for blood pressure reduction [70] | Originally designed for hypertension, not general inflammation [71] | Inverse association with DII; moderate correlation with inflammation [71] [72] |
| Mediterranean Diet Scores | Traditional Mediterranean dietary patterns [68] | Extensive evidence base for multiple health outcomes [68] | Multiple scoring systems; population-specific adaptations [68] | Anti-inflammatory effects demonstrated, but not specifically designed for inflammation [68] |
Predictive Validity for Health Outcomes
The DII has been validated against inflammatory biomarkers in multiple populations and has demonstrated associations with various health outcomes. A large study using NHANES data (2005-2018) found that 57% of American adults reported dietary intakes associated with inflammation based on E-DII scores [72]. Pro-inflammatory diets were more common among males, younger adults, non-Hispanic Black adults, and those with lower education or income, suggesting socioeconomic disparities in inflammatory dietary potential [72].
Studies examining the DII in specialized populations provide insights into its unique value. Research comparing vegetarians and omnivores found that while crude DII scores were similar between groups, energy-adjusted DII (E-DII) was significantly lower in vegetarians (2.43 ± 1.04 vs. 2.88 ± 0.95, P < 0.001), indicating greater anti-inflammatory potential after accounting for energy intake [74]. This highlights the importance of energy adjustment in DII calculation and interpretation.
Research Applications and Protocols
Protocol: Implementing DII in Observational Studies
Objective: To assess the inflammatory potential of diet using the DII in epidemiological research.
Materials:
- Dietary assessment tool (24-hour recall, FFQ, or food record)
- Nutrient analysis software
- DII calculation algorithm or software
- Global reference database for DII parameters
Procedure:
Dietary Data Collection:
- Administer validated dietary assessment tool appropriate for the research question and population [73].
- For 24-hour recalls, collect multiple recalls (ideally 2-3) on non-consecutive days to account for day-to-day variation [73].
- For FFQs, ensure the instrument captures foods relevant to the population and includes all DII parameters of interest [73].
Data Processing:
- Process dietary data using appropriate nutrient analysis software.
- Extract intake data for all available DII parameters (minimum of 15-20 recommended for valid DII calculation).
- For parameters not directly available, use appropriate conversion factors or estimation techniques.
DII Calculation:
- For each participant, calculate z-scores for each DII parameter using the global reference mean and standard deviation.
- Convert to percentiles, center, and multiply by respective inflammatory effect scores.
- Sum across all parameters to obtain the overall DII score.
- Consider calculating E-DII (DII per 1000 kcal) to control for energy intake.
Statistical Analysis:
- Analyze DII as continuous variable or categorize into quartiles/quintiles based on distribution.
- Use appropriate multivariate regression models adjusting for potential confounders (age, sex, BMI, physical activity, smoking status).
- For missing data, consider multiple imputation approaches rather than complete case analysis to reduce potential bias [72].
Interpretation: Higher (positive) DII scores indicate pro-inflammatory diets, while lower (negative) scores indicate anti-inflammatory diets. The theoretical range is -8.87 to +7.98, though observed ranges in populations are typically narrower.
Table 3: Essential Resources for Dietary Pattern Research
| Resource Category | Specific Examples | Application and Function |
|---|---|---|
| Dietary Assessment Tools | 24-hour recall protocols; Food Frequency Questionnaires; Food record forms [73] | Collect comprehensive dietary intake data from study participants |
| Nutrient Analysis Software | NDS-R; FoodWorks; NutriBase | Convert food intake data to nutrient values for DII parameter calculation |
| DII Calculation Resources | Global reference database; Inflammatory effect scores; DII calculation algorithms [11] | Standardized computation of DII scores across studies |
| Biomarker Assay Kits | CRP, IL-6, TNF-α ELISA kits; Multiplex immunoassays | Validate DII scores against inflammatory biomarkers |
| Statistical Software Packages | SAS, R, SPSS, Stata with specialized dietary analysis modules | Conduct complex statistical analyses of dietary pattern data |
Advanced Methodological Considerations
Energy Adjustment and Measurement Error
Energy adjustment is critical in DII application, as demonstrated in studies where energy-adjusted E-DII revealed associations masked by crude DII scores [74]. The E-DII calculates inflammatory potential per 1000 kcal, providing a measure of "dietary quality" independent of quantity [72] [74]. All self-reported dietary data are subject to measurement error, with systematic underreporting more common in specific subgroups (e.g., individuals with obesity) [73]. When possible, using recovery biomarkers (doubly labeled water for energy, urinary nitrogen for protein) can help correct for measurement error [73].
Handling Missing Data in Dietary Pattern Research
Missing data present a significant challenge in nutritional epidemiology. Complete case analysis, commonly used in DII studies, can introduce bias if data are not missing completely at random [72]. Multiple imputation methods are preferred when data are missing at random, as they preserve sample size and reduce potential bias [72]. Research comparing these approaches in DII studies found that multiple imputation and complete case analysis produced similar point estimates for socioeconomic differences in E-DII, with differences generally ≤20% [72].
Figure 2: Missing Data Decision Protocol. Appropriate statistical approaches for handling missing data in DII research depend on the missing data mechanism: Missing Completely at Random (MCAR), Missing at Random (MAR), or Missing Not at Random (MNAR).
The DII represents a specialized a priori approach that uniquely quantifies the inflammatory potential of diet, complementing traditional dietary indices that measure general diet quality or adherence to dietary guidelines. While correlated with indices such as HEI, AHEI, and DASH, the DII captures distinct aspects of diet related to inflammation and offers unique insights into diet-disease relationships mediated by inflammatory pathways.
For researchers implementing dietary pattern analyses, the following recommendations are provided:
- Method Selection: Choose dietary assessment methods aligned with research questions—DII for inflammation-focused studies; HEI/AHEI for guideline adherence; data-driven methods for exploratory population-specific patterns.
- Energy Adjustment: Always calculate and report E-DII alongside crude DII to control for energy intake effects.
- Missing Data: Employ multiple imputation methods rather than complete case analysis to handle missing data.
- Validation: Where feasible, validate DII scores against inflammatory biomarkers in study populations.
- Comparative Approaches: Consider applying both DII and traditional indices to comprehensively assess different dimensions of diet.
The DII has rapidly expanded our understanding of diet-inflammation relationships across diverse populations and health conditions. As research evolves, continued refinement and standardization of DII calculation and application will enhance its utility in developing targeted anti-inflammatory dietary interventions.
The Dietary Inflammatory Index (DII) was developed to quantify the inflammatory potential of an individual's overall diet based on scientific evidence linking dietary parameters to inflammatory biomarkers [75]. However, the original DII reference database was derived primarily from Western populations, limiting its direct applicability to Chinese dietary patterns characterized by distinct food compositions and nutrient intake profiles [56]. This case study details the development and validation of the China Dietary Inflammatory Index (CHINA-DII), a population-specific tool designed to assess dietary inflammatory potential in Chinese adults, with validation conducted in a cohort of gastric cancer patients using high-sensitivity C-reactive protein (hs-CRP) as the inflammatory biomarker [55].
Chronic low-grade inflammation represents a significant pathophysiological mechanism underlying numerous chronic diseases, including cancer, cardiovascular disease, and metabolic disorders [75]. Diet modulates inflammation through complex interactions between various food components and inflammatory pathways. The CHINA-DII was developed to provide a more accurate assessment tool for Chinese populations, enabling researchers and clinicians to better evaluate the relationship between dietary patterns, inflammation, and disease risk in this specific demographic [56].
Materials and Methods
Research Reagent Solutions and Essential Materials
Table 1: Key Research Reagents and Materials for CHINA-DII Validation
| Item | Function/Application | Specifications |
|---|---|---|
| Food Frequency Questionnaire (FFQ) | Assesses habitual dietary intake over the past year | 70+ food items; consumption frequency from "never" to "every day" [76] |
| High-Sensitivity C-Reactive Protein (hs-CRP) | Biomarker for systemic inflammation | Measured in mg/L; levels ≥3 mg/L indicate elevated inflammation [55] |
| Dietary Intake Database | Reference for calculating inflammatory scores | 27 dietary components from 33 studies (2009-2024) [55] |
| Statistical Software | Data analysis and validation | SAS, STATA, SPSS for trajectory modeling and regression analyses [76] |
CHINA-DII Development Protocol
Literature Search and Database Establishment
A systematic literature search was conducted across five databases: China National Knowledge Infrastructure (CNKI), Wanfang Data Knowledge Service Platform, VIP Chinese Science and Technology Journal Database, PubMed, and Web of Science [56]. The search timeframe spanned from January 1, 2009, to December 31, 2024, utilizing keywords including "dietary," "nutritional status," "nutrition," "intake," "consumption," "China," and "Chinese" [56].
Inclusion criteria encompassed: (1) Chinese adults aged ≥18 years; (2) cross-sectional studies, cohort studies, or case-control studies reporting dietary intake (with only control group data extracted from case-control studies); (3) validated dietary assessment methods including 24-hour dietary recall, food diaries, weighed food method, or FFQ; and (4) studies reporting dietary energy or nutrient intake data [56].
Exclusion criteria included: (1) non-Chinese adults or special populations (pregnant women, lactating women, individuals with diabetes); (2) review abstracts, conference proceedings, letters, or case reports; (3) sample size <200; (4) surveys conducted before 2009; (5) studies without extractable dietary intake data; (6) duplicate publications; (7) non-validated dietary assessment methods; and (8) low-quality studies [56].
Dietary Component Selection and Scoring
Following literature screening and quality assessment, 33 eligible studies were included to establish a dietary intake database encompassing 27 dietary components [55]. Each dietary parameter was assigned an inflammatory effect score based on a comprehensive review of literature assessing associations with six inflammatory biomarkers: IL-1β, IL-4, IL-6, IL-10, TNF-α, and CRP [56]. The scoring methodology followed the approach established by Shivappa et al., with scores ranging from -1 (strongest anti-inflammatory effect) to +1 (strongest pro-inflammatory effect) [56].
Validation Study Protocol
Participant Recruitment and Data Collection
The validation study recruited 256 newly diagnosed gastric cancer patients from Union Hospital of Fujian Medical University between June 2023 and November 2024 [55]. Demographic information, clinical data, and dietary data based on FFQ were collected from all participants [55]. The study protocol received ethical approval from the institutional review board, and all participants provided informed consent.
Dietary data collection utilized a validated Food Frequency Questionnaire (FFQ) assessing typical food and beverage consumption over the past year [76]. The FFQ covered approximately 70 items with consumption frequency reported on a nine-level scale ranging from "never" to "every day" [76]. Additional dietary behaviors including food preparation methods, fat intake, fiber intake, and vitamin/mineral consumption were also assessed [76].
hs-CRP Measurement and Analysis
Fasting blood samples were collected from all participants for hs-CRP measurement. Serum hs-CRP levels were quantified using standardized laboratory techniques, with values expressed in mg/L. Elevated inflammatory status was defined as hs-CRP ≥3 mg/L, consistent with established clinical thresholds [55].
Statistical Analysis
Spearman rank correlation analysis was employed to assess the relationship between CHINA-DII scores and hs-CRP levels [55]. Multivariate logistic regression analysis was conducted to evaluate the association between CHINA-DII scores and the risk of elevated hs-CRP (≥3 mg/L), with adjustment for potential confounding factors [55]. Odds ratios (ORs) with 95% confidence intervals (CIs) were calculated to quantify the magnitude of association [55].
Results and Data Analysis
Participant Characteristics and CHINA-DII Scores
Table 2: Baseline Characteristics and CHINA-DII Scores of Study Participants
| Parameter | Value |
|---|---|
| Participants | 256 newly diagnosed gastric cancer patients |
| Average CHINA-DII Score | -1.91 ± 0.35 |
| Mean hs-CRP Level | 3.68 ± 2.35 mg/L |
| Spearman Correlation (r) | 0.20 |
| P-value for Correlation | ≤0.001 |
Among the 256 gastric cancer patients, the average CHINA-DII score was -1.91 ± 0.35, indicating generally anti-inflammatory dietary patterns [55]. The mean hs-CRP level was 3.68 ± 2.35 mg/L, with a significant proportion of participants exhibiting elevated inflammatory status (hs-CRP ≥3 mg/L) [55].
Association Between CHINA-DII and hs-CRP
Table 3: Association Between CHINA-DII Scores and Risk of Elevated hs-CRP
| Comparison | Odds Ratio | 95% Confidence Interval |
|---|---|---|
| Higher vs. Lower CHINA-DII Scores | 1.90 | 1.01 - 3.55 |
| Per 1-SD Increase in CHINA-DII | 1.50 | 1.10 - 2.06 |
CHINA-DII scores demonstrated a statistically significant positive correlation with hs-CRP levels (Spearman r = 0.20, p ≤ 0.001) [55]. Multivariate logistic regression analysis, adjusted for potential confounders, revealed that individuals with higher CHINA-DII scores had a 1.90-fold increased risk of elevated hs-CRP (≥3 mg/L) compared to those with lower scores (OR = 1.90; 95% CI: 1.01-3.55) [55]. Furthermore, each 1-standard-deviation increase in CHINA-DII score was associated with a 1.50-times increased risk of elevated hs-CRP (OR = 1.50, 95% CI: 1.10-2.06) [55].
Discussion
The successful development and validation of the CHINA-DII represents a significant advancement in nutritional epidemiology research specific to Chinese populations. The positive association between CHINA-DII scores and hs-CRP levels demonstrates the tool's validity for assessing dietary inflammatory potential in Chinese adults [55]. These findings align with previous research investigating the original DII in diverse populations, where pro-inflammatory dietary patterns consistently associated with elevated inflammatory biomarkers [75].
The methodological approach employed in developing the CHINA-DII followed established protocols for creating population-specific dietary indices while incorporating Chinese dietary particularities [56]. The inclusion of 27 dietary components derived from 33 studies published between 2009 and 2024 ensured comprehensive coverage of contemporary Chinese dietary patterns [55]. The validation in a gastric cancer cohort is particularly relevant given the established relationship between chronic inflammation and cancer pathogenesis [55].
From a clinical and public health perspective, the CHINA-DII provides researchers and healthcare professionals with a validated tool to assess the inflammatory impact of dietary patterns in Chinese populations. This enables more targeted nutritional interventions for chronic disease prevention and management, particularly for inflammation-related conditions such as gastric cancer [55]. The ability to quantify dietary inflammatory potential facilitates personalized nutrition recommendations and public health strategies aimed at reducing diet-related inflammation in Chinese communities.
Future research directions should include validation of the CHINA-DII in broader Chinese population subgroups, investigation of its association with other inflammation-related health outcomes, and prospective studies examining its ability to predict disease risk. Additionally, translational research incorporating the CHINA-DII into clinical practice for nutritional assessment and intervention would maximize its public health impact.
The Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) framework is a systematic and transparent methodology for rating the certainty of evidence and strength of recommendations in health care research [77]. Originally developed for clinical interventions, GRADE is increasingly applied to evaluate evidence from nutritional epidemiology, including studies on the Dietary Inflammatory Index (DII) [78] [79]. The DII is a literature-derived tool that quantifies the inflammatory potential of an individual's diet based on its effects on specific inflammatory biomarkers such as IL-1β, IL-4, IL-6, IL-10, TNF-α, and CRP [11] [80].
Applying GRADE to DII research presents unique methodological considerations. Unlike pharmaceutical interventions, nutritional research often relies on evidence from observational studies, which GRADE initially classifies as low-certainty evidence due to potential confounding [78]. This starting point requires careful assessment of factors that may subsequently downgrade or upgrade the evidence, ensuring appropriate interpretation of DII-disease associations for researchers, clinicians, and policymakers.
Table 1: Key Concepts in GRADE Application to DII Research
| Concept | Description | Consideration for DII Research |
|---|---|---|
| Initial Quality of Evidence | Starting point for rating evidence | Observational studies begin as low quality; randomized trials as high quality |
| Risk of Bias | Systematic error in study design or execution | Assess blinding, attrition, selective reporting in DII studies |
| Imprecision | Uncertainty in effect estimates | Evaluate confidence interval width around DII effect sizes |
| Inconsistency | Unexplained variability in results | Examine heterogeneity across DII studies in different populations |
| Indirectness | Applicability to research question | Consider relevance of population, interventions, comparators, outcomes |
| Publication Bias | Selective publication of studies | Assess funnel plot asymmetry or other indicators for DII literature |
GRADE Methodology for DII Evidence Synthesis
Initial Assessment of DII Study Designs
The application of GRADE to DII research begins with classifying the study design of available evidence. For DII research, this typically involves observational studies (cohort, case-control, cross-sectional) that examine associations between dietary inflammatory potential and health outcomes [35] [81] [80]. Under GRADE, evidence from these observational studies starts as low certainty, while evidence from randomized controlled trials (RCTs) starts as high certainty [78].
The certainty of evidence can be rated down for several factors: risk of bias, imprecision, inconsistency, indirectness, and publication bias. Conversely, evidence from observational studies can be rated up for large magnitude of effects, dose-response relationships, or when all plausible confounding would reduce an apparent effect [78] [77]. For example, a recent DII study on diabetic retinopathy found a hazard ratio of 1.51 (95% CI: 1.15-1.99), demonstrating a potentially large effect that might warrant upgrading the evidence certainty [35].
Modifications for Nutritional Epidemiology
Standard GRADE approaches require modification for nutritional research like DII studies. Current GRADE criteria automatically classify observational evidence as low certainty due to lack of randomization, which may lead to excessive downgrading of nutritional evidence [78]. Alternative approaches such as NutriGrade have been developed specifically for nutritional studies, providing a more balanced evaluation framework [78].
The integration of ROBINS-I (Risk Of Bias In Non-randomized Studies - of Interventions) with GRADE may provide a more nuanced assessment of bias risk in DII observational studies by evaluating multiple bias domains rather than simply the lack of randomization [78]. This approach is particularly relevant for DII research, where long-term randomized trials are often infeasible.
Experimental Protocols for DII Research
DII Calculation and Validation Protocol
Objective: To standardize the calculation and validation of Dietary Inflammatory Index scores in research populations.
Materials and Reagents:
- Validated Food Frequency Questionnaire (FFQ)
- Nutrient analysis software (e.g., Nutritionist IV)
- Global dietary intake database for reference values
- Laboratory equipment for inflammatory biomarkers (hs-CRP, IL-6, TNF-α)
Table 2: Research Reagent Solutions for DII Studies
| Reagent/Resource | Function | Example Application |
|---|---|---|
| 168-item FFQ | Assess habitual dietary intake | Collect dietary data over preceding year [81] [80] |
| Global nutrient database | Provide reference intake values | Z-score calculation for 45 food parameters [11] [56] |
| Nutritionist IV software | Analyze nutrient composition | Convert food intake to nutrient values [81] [80] |
| High-sensitivity CRP assay | Validate inflammatory potential | Correlate DII scores with inflammatory biomarkers [37] [56] |
| Olink Proteomics panels | Multiplex inflammatory biomarker analysis | Measure IL-6, TNF-R1, TNF-R2 [37] |
Procedure:
- Dietary Assessment: Administer a validated FFQ (e.g., 168-item questionnaire) to assess habitual dietary intake over the preceding year [81] [80]. For pediatric populations, parents complete the FFQ with visual aids for portion size estimation [81].
- Nutrient Quantification: Process FFQ data using nutritional analysis software to quantify daily intake of DII parameters.
- Z-score Calculation: For each of the DII food parameters, calculate a z-score by comparing individual intake to global reference values: Z-score = (individual mean intake - global mean intake) / global standard deviation [35] [11].
- Percentile Conversion: Convert z-scores to centered percentiles to minimize right-skewing: Percentile = (2 × cumulative proportion) - 1 [11] [80].
- Inflammatory Effect Scoring: Multiply each food parameter's percentile by its literature-derived inflammatory effect score [11] [56].
- Total DII Calculation: Sum all food parameter-specific DII scores to obtain the overall DII score for each participant.
- Energy Adjustment: Adjust for total energy intake using the residual method or by dividing the DII score by energy intake (kcal) and multiplying by 1000 to obtain the energy-adjusted DII (E-DII) [35] [81].
- Validation: Correlate DII scores with inflammatory biomarkers (e.g., hs-CRP, IL-6) in a subset of participants to confirm predictive validity [37] [56].
Diagram 1: GRADE-DII Assessment Workflow (79 characters)
Retinal Imaging Protocol for DII and Diabetic Retinopathy
Objective: To quantify the association between DII scores and structural alterations in retinal layers using optical coherence tomography (OCT).
Materials:
- Spectral-domain OCT device (e.g., Topcon 3D OCT 1000 Mk2)
- Image analysis software with segmentation capabilities
- Quality control metrics for image acceptability
Procedure:
- Participant Preparation: Dilate pupils and position participants for macular volume scans.
- OCT Imaging: Acquire 512 horizontal A-scans and 128 B-scans in a 6×6-mm raster pattern centered on the fovea [35].
- Quality Control: Apply quality criteria including image quality score >45, good centration certainty, and adequate segmentation certainty. Exclude poorest 20% of images based on segmentation indicators [35].
- Retinal Layer Segmentation: Automatically segment retinal layers including internal limiting membrane (ILM), nerve fiber layer (NFL), ganglion cell layer (GCL), inner plexiform layer (IPL), inner nuclear layer (INL), external limiting membrane (ELM), photoreceptor inner and outer segment (ISOS), and retinal pigment epithelium (RPE) [35].
- Subfield Analysis: Divide retinal thickness measurements according to Early Treatment Diabetic Retinopathy Study subfields: central, inner inferior, inner nasal, inner superior, inner temporal, outer inferior, outer nasal, outer superior, and outer temporal regions [35].
- Statistical Analysis: Use linear regression models to explore associations between DII scores and retinal layer thickness, adjusting for relevant covariates.
Application of GRADE to Specific DII Studies
Case Study: DII and Diabetic Retinopathy
A 2025 prospective cohort study analyzed data from 16,224 UK Biobank participants with diabetes, including 1,257 who developed diabetic retinopathy (DR) during follow-up [35]. The study found higher DII scores associated with increased DR risk (HR=1.51, 95% CI: 1.15-1.99, p=0.003) and revealed a J-shaped association, with significant risk elevation only when DII scores exceeded -2.5 [35].
GRADE Assessment:
- Initial certainty: Low (observational cohort study)
- Risk of bias: Probably low (prospective design, large sample, adjusted models)
- Inconsistency: Undetected (single large study)
- Indirectness: Low (direct population, intervention, comparators, outcomes)
- Imprecision: Low (narrow confidence intervals, large sample)
- Publication bias: Unassessed (single study)
- Upgrading factors: Dose-response relationship (J-shaped curve), association with retinal layer thinning
- Final certainty: Moderate (likely upgraded for dose-response relationship)
Case Study: DII and ADHD in Children
A 2025 case-control study of 500 Iranian children (200 ADHD cases, 300 controls) found energy-adjusted DII directly associated with ADHD risk (OR=1.133, 95% CI: 1.021-1.258, p=0.019) after multivariate adjustment [81].
GRADE Assessment:
- Initial certainty: Low (observational case-control design)
- Risk of bias: Probably serious (case-control design susceptible to recall bias in FFQ)
- Inconsistency: Unknown (limited similar studies)
- Indirectness: Low (direct population and outcomes)
- Imprecision: Low (modest confidence intervals)
- Publication bias: Unassessed
- Upgrading factors: None identified
- Final certainty: Low (downgraded for risk of bias)
Table 3: GRADE Certainty Ratings for DII-Disease Associations
| Health Outcome | Study Design | Effect Estimate | Initial Certainty | Final Certainty | Key Factors Affecting Certainty |
|---|---|---|---|---|---|
| Diabetic Retinopathy [35] | Prospective cohort | HR=1.51 (1.15-1.99) | Low | Moderate | Dose-response, precise estimate, adjusted confounding |
| ADHD in Children [81] | Case-control | OR=1.13 (1.02-1.26) | Low | Low | Recall bias in FFQ, case-control design |
| Irritable Bowel Syndrome [80] | Case-control | OR=1.38 (1.20-1.56) | Low | Low | Case-control design, potential confounding |
| Chronic Inflammation [37] | Cross-sectional | β=-0.17 to -0.28 for biomarkers | Low | Moderate | Multiple biomarker validation, large sample |
Limitations and Alternative Approaches
Challenges in GRADE Application to DII Research
Applying GRADE to DII research faces several challenges. The framework's origin in clinical trials creates difficulties for nutritional observational evidence, which is automatically downgraded [78]. Dietary interventions involve complex substitutions rather than simple additions or removals, and their effects depend on replacement foods [78]. Additionally, dietary adherence and high dropout rates in nutritional studies present unique bias risks not fully captured by standard GRADE tools [78].
DII studies often rely on intermediate outcomes like inflammatory biomarkers rather than hard clinical endpoints. While Bradford Hill criteria consider biological plausibility, GRADE does not formally include this domain when evaluating certainty [78]. Furthermore, the dose-response relationships observable across population dietary intake distributions in observational studies provide valuable evidence that fixed-dose intervention trials cannot capture [78].
Alternative Evidence Grading Systems
Alternative evidence grading systems have been proposed to address limitations of standard GRADE for nutritional research:
NutriGrade: This scoring system does not automatically consider observational evidence as low certainty, instead using a quantitative score across 9 components [78]. Applied to the same body of evidence, NutriGrade and GRADE concurred for only 53% of outcomes in one analysis, highlighting significant methodological differences [78].
World Cancer Research Fund (WCRF) Approach: This system provides an alternative framework specifically designed for dietary and lifestyle evidence synthesis [78].
HEALM (Hierarchies of Evidence Applied to Lifestyle Medicine): This approach offers a modified hierarchy better suited to lifestyle interventions including diet [78].
Applying the GRADE framework to DII research requires careful consideration of nutritional epidemiology's unique characteristics. While standard GRADE provides a structured approach to evidence certainty assessment, modifications may be necessary to appropriately evaluate DII-disease associations. Future directions should include development of consensus methodology for grading nutritional evidence, validation of alternative tools like NutriGrade for DII research, and careful reporting of certainty ratings in DII studies to guide evidence-based recommendations.
Conclusion
The Dietary Inflammatory Index has solidified its role as a powerful, evidence-based tool for quantifying the inflammatory potential of diet in research. Its association with a spectrum of inflammation-driven chronic diseases, from NAFLD to gastric cancer, underscores its clinical relevance. Future directions should focus on enhancing the tool's precision through continued cultural adaptations, integration with multi-omics data, and the application of AI for analyzing complex dietary patterns. For the research and drug development community, mastering DII assessment is paramount for designing robust nutritional epidemiology studies, informing public health strategies for disease prevention, and developing novel, diet-based therapeutic interventions.
References
- 1. Distinct etiology of chronic inflammation – implications on ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1460302/full]
- 2. Dietary Inflammatory Index [https://bio-protocol.org/exchange/minidetail?id=5199187&type=30]
- 3. Scientific basis of dietary inflammatory index (DII) [https://www.sciencedirect.com/science/article/pii/S2667268525000415]
- 4. Associations between dietary inflammatory index (DII) scores ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12373831/]
- 5. Relationship between dietary inflammatory index and chronic ... [https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-025-22544-3]
- 6. New Molecular Mechanisms and Markers in Inflammatory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12249654/]
- 7. Inflammatory biomarkers offer new insights for precision ... [https://www.news-medical.net/news/20251120/Inflammatory-biomarkers-offer-new-insights-for-precision-medicine-in-ischemic-stroke.aspx]
- 8. Diagnostic and prognostic utility of inflammatory ... [https://pubmed.ncbi.nlm.nih.gov/41100394/?utm_source=FeedFetcher&utm_medium=rss&utm_campaign=pubmed-2&utm_content=1xONNp6hzwmdFthy7j4KmYq52h124kRo8imk_emfIXU05QZ9YY&fc=20210218095451&ff=20251025220928&v=2.18.0.post22+67771e2]
- 9. Dietary inflammatory index and its association ... - BMC Nutrition [https://bmcnutr.biomedcentral.com/articles/10.1186/s40795-025-01118-x]
- 10. Validation of a Dietary Inflammatory Index (DII) and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6103570/]
- 11. Perspective: The Dietary Inflammatory Index (DII) [https://pmc.ncbi.nlm.nih.gov/articles/PMC6416047/]
- 12. The Dietary Inflammatory Index (DII) and COPD [https://pmc.ncbi.nlm.nih.gov/articles/PMC12273714/]
- 13. Comparison of predictive effect of the dietary inflammatory ... [https://bmcwomenshealth.biomedcentral.com/articles/10.1186/s12905-023-02485-y]
- 14. The associations between diet-induced inflammation and ... [https://www.nature.com/articles/s41538-025-00583-9]
- 15. Dietary Inflammatory index and its association with fatty liver disease: a study in obese and non-obese populations | BMC Gastroenterology | Full Text [https://bmcgastroenterol.biomedcentral.com/articles/10.1186/s12876-024-03585-1]
- 16. Relationship between dietary inflammatory index and ... [https://www.nature.com/articles/s41598-025-89690-x]
- 17. Dietary inflammatory index and non-alcoholic fatty liver ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12231496/]
- 18. Frontiers | The relationship between dietary inflammatory index and all-cause and cardiovascular disease-related mortality in adults with metabolic syndrome: a cohort study of NHANES [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2024.1417840/full]
- 19. Association between the dietary inflammatory index and ... [https://www.sciencedirect.com/science/article/pii/S0261561424004187]
- 20. Association between dietary inflammatory index and metabolic syndrome: Analysis of the NHANES 2005–2016 - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9582939/]
- 21. The role of dietary inflammatory index in metabolic diseases: the associations, mechanisms, and treatments | European Journal of Clinical Nutrition [https://www.nature.com/articles/s41430-024-01525-6]
- 22. Cross-sectional study of the relationship between dietary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12623732/]
- 23. The Dietary Inflammatory Index and Its Associations with ... [https://www.mdpi.com/2076-3921/13/8/962]
- 24. Frontiers | Association of dietary and oxidative... inflammatory index [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1607162/full]
- 25. Associations between dietary ( inflammatory ) scores and... index DII [https://www.nature.com/articles/s41598-025-08919-x?error=cookies_not_supported&code=09abc15c-0e9e-4998-8190-414e7b442ee7]
- 26. Nutritional biomarkers [https://www.measurement-toolkit.org/diet/objective-methods/biomarkers]
- 27. Biomarkers of Nutrition and Health: New Tools for New ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6567133/]
- 28. Nonlinear dose–response relationship between dietary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12465630/]
- 29. A cohort study on the association of dietary inflammatory ... [https://www.nature.com/articles/s41598-025-15970-1]
- 30. Dietary inflammatory index and the risk of esophageal cancer [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-025-14199-5]
- 31. Understanding The Dietary Inflammatory Index and Its Uses [https://obesitymedicine.org/blog/foods-that-aid-in-stress-relief-and-lowering-inflammation/]
- 32. The association between energy-adjusted dietary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11330808/]
- 33. Association between energy-adjusted dietary inflammatory ... [https://jhpn.biomedcentral.com/articles/10.1186/s41043-025-00998-w]
- 34. sex-specific associations with quality of life, sleep, fatigue and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12476995/]
- 35. Association of standard dietary inflammatory index with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12538057/]
- 36. A cross-sectional exploration of the dietary inflammation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12488447/]
- 37. Development of empirical anti-inflammatory diet index: a cross ... [https://nutritionj.biomedcentral.com/articles/10.1186/s12937-025-01165-x]
- 38. A cross-sectional exploration of the dietary inflammation ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1591472/full]
- 39. Cross-sectional study of the relationship between dietary ... [https://www.nature.com/articles/s41598-025-24046-z]
- 40. Association of dietary quality and dietary inflammatory ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1596806/full]
- 41. Nonlinear dose-response relationship between dietary ... [https://pubmed.ncbi.nlm.nih.gov/41019538/]
- 42. Nonlinear dose–response relationship between dietary ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1645789/full]
- 43. Dietary inflammatory potential and the risk of cognitive ... [https://www.sciencedirect.com/science/article/pii/S1279770724005165]
- 44. Meta-analysis of the association between dietary ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2023.1104255/full]
- 45. Meta-analysis of the association between dietary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6056732/]
- 46. The dietary inflammatory index is positively associated with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11661051/]
- 47. Effects of Dietary Patterns on Biomarkers of Inflammation and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8803482/]
- 48. The association of dietary patterns with ... [https://www.nature.com/articles/s41598-021-86993-7]
- 49. Exploring the association between pro-inflammatory diets ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1537855/full]
- 50. Dietary inflammatory potential, genetic susceptibility, and ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1680225/full]
- 51. Evaluation of the Relationship Between Dietary Inflammatory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12358944/]
- 52. Calculation of the Dietary Inflammation Index [https://bio-protocol.org/exchange/minidetail?id=9878522&type=30]
- 53. Association between dietary inflammatory index and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11992876/]
- 54. Association between the Chinese Dietary Inflammatory ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1653575/full]
- 55. Development and Validation of the China Dietary ... [https://pubmed.ncbi.nlm.nih.gov/40431426/]
- 56. Development and Validation of the China Dietary ... [https://www.mdpi.com/2072-6643/17/10/1687]
- 57. Association between the Chinese Dietary Inflammatory Index ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12401693/]
- 58. the mediating role of dietary inflammatory index (DII) [https://pmc.ncbi.nlm.nih.gov/articles/PMC11786581/]
- 59. Dietary inflammatory index mediation lifestyle patterns and ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1578954/full]
- 60. Association of the dietary inflammation index with ... [https://www.nature.com/articles/s41598-025-02169-7]
- 61. ROBINS-I | Cochrane Bias [https://methods.cochrane.org/bias/risk-bias-non-randomized-studies-interventions]
- 62. Risk of bias tools - ROBINS-I V2 tool [https://www.riskofbias.info/welcome/robins-i-v2]
- 63. Association of dietary inflammatory index and the SARS-CoV ... [https://nutritionj.biomedcentral.com/articles/10.1186/s12937-024-00927-3]
- 64. The Role of Dietary Inflammatory Index in Cardiovascular Disease... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5000663/]
- 65. Dietary inflammatory index and elevated serum Câ€reactive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10563751/]
- 66. The relationship between dietary inflammatory indices and male... [https://bmcresnotes.biomedcentral.com/articles/10.1186/s13104-025-07554-z]
- 67. Associations between the Dietary Inflammatory Index and ... [https://www.mdpi.com/2072-6643/15/2/419]
- 68. What can we learn from dietary pattern analysis? - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10273249/]
- 69. Review of a priori dietary quality indices in relation to their ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6130981/]
- 70. A Systematic Review of the Methods Used to Assess and ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2022.892351/full]
- 71. Anti-inflammatory Dietary Inflammatory Index scores are ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4773655/]
- 72. Socio-demographic differences in the dietary inflammatory ... [https://www.cambridge.org/core/journals/public-health-nutrition/article/sociodemographic-differences-in-the-dietary-inflammatory-index-from-national-health-and-nutrition-examination-survey-20052018-a-comparison-of-multiple-imputation-versus-complete-case-analysis/7BEEA51160D7657B267F4C12A9AF1584]
- 73. Overview of Dietary Assessment Methods for Measuring ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8338737/]
- 74. Comparison of dietary inflammatory index and ... [https://www.nature.com/articles/s41598-024-69168-y]
- 75. The Dietary Inflammatory Index and Human Health [https://pmc.ncbi.nlm.nih.gov/articles/PMC8483957/]
- 76. A longitudinal study of dietary inflammatory index and ... [https://www.nature.com/articles/s41598-025-86431-y]
- 77. GRADE handbook [https://gradepro.org/handbook]
- 78. Grading nutrition evidence: where to go from here? - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8168365/]
- 79. a scoping review of nutrition and physical activity policies [https://implementationscience.biomedcentral.com/articles/10.1186/s13012-020-00984-2]
- 80. Association between dietary inflammatory index (DII) and risk ... [https://nutritionj.biomedcentral.com/articles/10.1186/s12937-021-00721-5]
- 81. Associations between dietary inflammatory index (DII) ... [https://www.nature.com/articles/s41598-025-08919-x]