The Oxidative-Inflammatory Axis in Chronic Disease: Mechanisms, Biomarkers, and Emerging Therapeutic Strategies
Chronic diseases, including cardiovascular, metabolic, and neurodegenerative disorders, share a common pathological denominator: a self-perpetuating cycle of oxidative stress and inflammation.
The Oxidative-Inflammatory Axis in Chronic Disease: Mechanisms, Biomarkers, and Emerging Therapeutic Strategies
Abstract
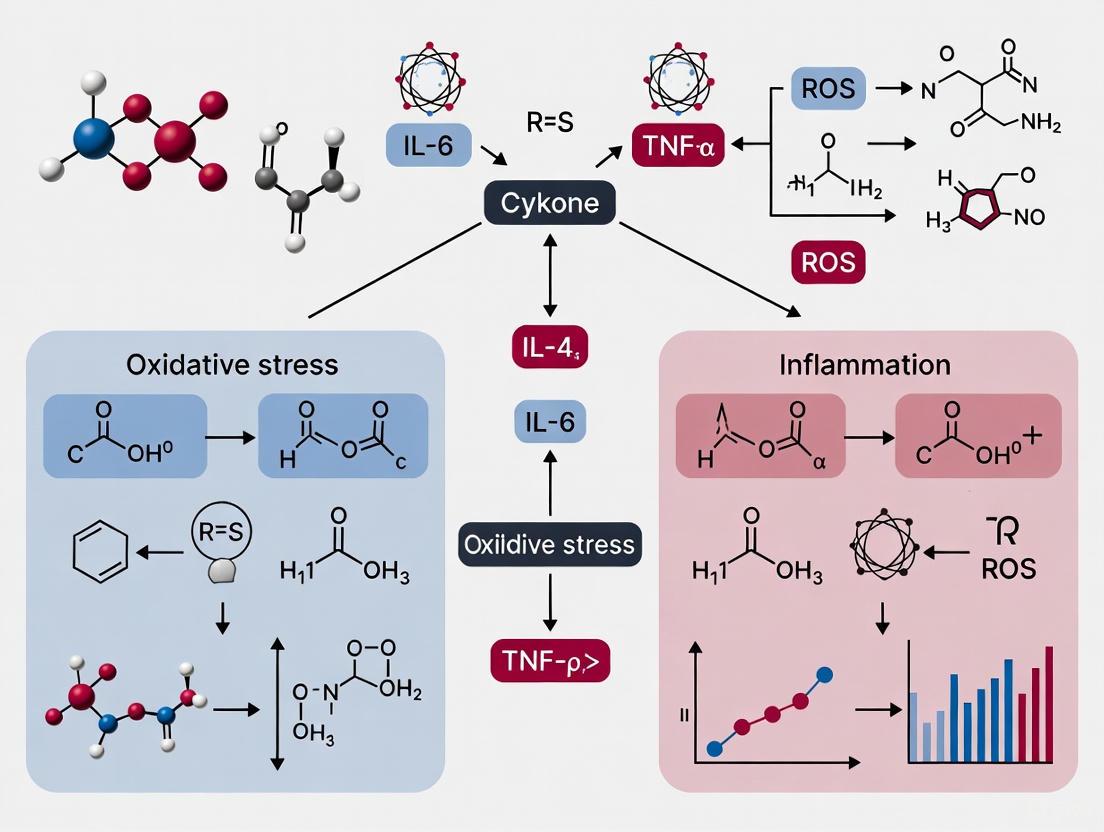
Chronic diseases, including cardiovascular, metabolic, and neurodegenerative disorders, share a common pathological denominator: a self-perpetuating cycle of oxidative stress and inflammation. This review provides a comprehensive analysis for researchers and drug development professionals, integrating foundational molecular mechanisms with translational applications. We explore the critical interplay between reactive oxygen species (ROS) and pro-inflammatory signaling pathways like NF-κB and Nrf2, which drives disease progression. The article critically assesses current methodologies for quantifying oxidative stress biomarkers and evaluates the paradoxical failure of conventional antioxidant trials. Furthermore, we detail innovative therapeutic strategies designed to overcome these limitations, such as mitochondria-targeted antioxidants, Nrf2 activators, and nanotechnology-based delivery systems. By synthesizing foundational knowledge, methodological applications, troubleshooting insights, and comparative validation data, this article aims to chart a course for developing effective, personalized redox medicine interventions.
Unraveling the Vicious Cycle: Core Molecular Mechanisms Linking ROS and Inflammatory Signaling
The interplay between reactive oxygen species (ROS) and chronic low-grade inflammation represents a core pathogenic axis in a wide spectrum of chronic diseases. This whitepaper delineates the key molecular players and mechanisms underpinning this relationship, focusing on the transition from acute, protective inflammatory responses to a state of persistent, pathological signaling. We detail the cellular sources of ROS, the redox-sensitive signaling pathways they activate, and the consequent perpetuation of a pro-inflammatory milieu. Furthermore, we provide a structured analysis of quantitative data, experimental protocols for key investigations, and visualizations of critical pathways. This resource is designed to equip researchers and drug development professionals with a consolidated, technical framework for advancing therapeutic strategies that target the ROS-inflammation nexus.
Inflammation is a fundamental defensive response conferred by the host against pathogenic insults and tissue injury [1]. While acute inflammation is a protective mechanism, its dysregulation leads to a state of chronic, low-grade inflammation that underpins numerous pathological conditions, including cardiovascular disorders, neurodegenerative diseases, metabolic syndromes, and autoimmune disorders [1] [2] [3]. Central to this dysregulation is the role of reactive oxygen species (ROS). Historically viewed merely as cytotoxic by-products of metabolism, ROS are now recognized as critical signaling molecules that regulate the progression of inflammatory disorders [1] [4].
The relationship between ROS and inflammation is synergistic and self-perpetuating. An enhanced generation of ROS at the site of inflammation contributes to endothelial dysfunction and tissue injury [1]. In turn, inflammatory mediators can stimulate the production of more ROS, creating a pathogenic feedback loop that sustains chronic inflammation even in the absence of an initial trigger [3]. This paper will define the key players in this process, from the specific ROS and their cellular sources to the signaling pathways they influence, within the broader context of oxidative stress and inflammation interplay in chronic disease research.
ROS are a class of partially reduced metabolites of oxygen with strong oxidizing capabilities. They function as double-edged swords: at low, physiological concentrations, they are indispensable signaling molecules, but at high, chronic concentrations, they oxidize cellular macromolecules, leading to damage and heightened inflammatory responses [1] [4].
Table 1: Key Reactive Oxygen and Nitrogen Species in Inflammation
| Reactive Species | Chemical Formula/Symbol | Primary Production Source | Reactivity and Role in Inflammation |
|---|---|---|---|
| Superoxide anion | O₂•⁻ | Mitochondrial ETC, NADPH oxidases (NOX), Xanthine Oxidase [1] [2] | Precursor to most other ROS; short half-life; can reduce and inactivate nitric oxide [1] |
| Hydrogen peroxide | H₂O₂ | Dismutation of O₂•⁻ by SOD, NOX4, DUOX [1] [2] | Membrane-permeable signaling molecule; can be converted to highly reactive OH• [3] |
| Hydroxyl radical | OH• | Fenton reaction (H₂O₂ + Fe²⁺) [1] [2] | Most potent oxidant; causes severe damage to lipids, proteins, and DNA [2] |
| Hypochlorous acid | HOCl | Myeloperoxidase (MPO) conversion of H₂O₂ [1] | Powerful microbial agent; can cause host tissue damage during inflammation [1] |
| Nitric oxide | NO• | Nitric oxide synthases (e.g., iNOS) [3] | Gasotransmitter; reacts with O₂•⁻ to form peroxynitrite [1] |
| Peroxynitrite | ONOO⁻ | Reaction between NO• and O₂•⁻ [2] [3] | Potent nitrating agent; induces nitrosative stress, damaging lipids, proteins, and DNA [2] |
The cellular generation of ROS is governed by multiple enzymatic and non-enzymatic sources. The major endogenous sources include:
- Mitochondrial Electron Transport Chain (ETC): During oxidative phosphorylation, an estimated 1–3% of electrons leak from complexes I and III, mediating the one-electron reduction of oxygen to O₂•⁻, which is then dismutated to H₂O₂ [2] [4].
- NADPH Oxidases (NOX): This family of enzymes, including NOX1–NOX5 and DUOX1/2, is dedicated to the regulated production of ROS. They catalyze the transfer of electrons from NADPH to molecular oxygen, generating O₂•⁻ or H₂O₂. NOX2, in particular, is critical for the "respiratory burst" in phagocytes for microbial killing [1] [3] [4].
- Endoplasmic Reticulum (ER): Oxidative protein folding in the ER involves enzymes like Ero1 and PDI, which can produce H₂O₂ as a by-product, particularly under conditions of ER stress [3].
- Xanthine Oxidase (XO): This enzyme catalyzes the oxidation of hypoxanthine to xanthine and then to uric acid, generating O₂•⁻ and H₂O₂ in the process [1] [4].
Signaling Pathways: The Mechanism of ROS-Mediated Inflammation
ROS propagate inflammation primarily by activating redox-sensitive signaling pathways. The following pathways are paramount in this process.
The NF-κB Pathway
The Nuclear Factor-kappa B (NF-κB) pathway is a master regulator of inflammation and is exquisitely sensitive to redox balance [3] [5].
Title: ROS activation of the NF-κB inflammatory signaling pathway.
Mechanism: In resting cells, NF-κB dimers (e.g., p50/p65) are sequestered in the cytoplasm by inhibitory proteins, IκBs. A wide array of pro-inflammatory stimuli (e.g., TNF-α, IL-1, LPS) and ROS itself can activate the IκB kinase (IKK) complex. ROS, particularly H₂O₂, can oxidize critical cysteine residues in IKK, leading to its activation [3] [5]. Activated IKK phosphorylates IκB, targeting it for ubiquitination and proteasomal degradation. This releases NF-κB, allowing it to translocate to the nucleus and induce the transcription of over 150 target genes, including those encoding pro-inflammatory cytokines (e.g., TNF-α, IL-1β, IL-6), adhesion molecules, and enzymes like cyclooxygenase-2 (COX-2) and inducible nitric oxide synthase (iNOS) [3] [5]. The induction of iNOS further increases NO• production, which can react with O₂•⁻ to form the damaging peroxynitrite (ONOO⁻), thereby amplifying oxidative stress and inflammation [1] [3].
The Nrf2/Keap1 Pathway
In opposition to NF-κB, the Nuclear factor erythroid 2-related factor 2 (Nrf2) pathway is a central regulator of cellular defense against oxidative stress and exerts anti-inflammatory effects [3] [5].
Title: Nrf2 activation by ROS leads to cytoprotective gene expression.
Mechanism: Under basal conditions, Nrf2 is bound to its cytosolic repressor, Keap1, which constantly targets Nrf2 for ubiquitination and proteasomal degradation, keeping its levels low. Oxidative stress or electrophiles modify critical cysteine residues on Keap1, leading to a conformational change that disrupts its ability to target Nrf2 for degradation. Consequently, Nrf2 stabilizes and translocates to the nucleus, where it heterodimerizes with small Maf proteins and binds to the Antioxidant Response Element (ARE) in the promoter regions of its target genes [3] [5]. This activates the transcription of a battery of cytoprotective genes, including those encoding heme oxygenase-1 (HO-1), NAD(P)H quinone dehydrogenase 1 (NQO1), and glutamate-cysteine ligase catalytic subunit (GCLC), a rate-limiting enzyme in glutathione synthesis. By enhancing the cellular antioxidant capacity, Nrf2 activation indirectly suppresses inflammation, notably by inhibiting NF-κB signaling and modulating macrophage polarization [3] [5].
Inflammasome Activation
ROS are key mediators in the activation of the NOD-like receptor family pyrin domain containing 3 (NLRP3) inflammasome, a multiprotein complex critical for the innate immune response [3].
Mechanism: Multiple DAMPs and PAMPs can prime the inflammasome by upregulating NLRP3 and pro-IL-1β expression via pathways like NF-κB. A second signal, which often involves ROS (particularly mitochondrial ROS), triggers inflammasome assembly. The assembled inflammasome activates caspase-1, which then cleaves pro-IL-1β and pro-IL-18 into their active, secreted forms. These potent pyrogenic cytokines drive inflammatory responses in conditions like gout, type 2 diabetes, and Alzheimer's disease [3].
Quantitative Data and Experimental Analysis
To facilitate research, key quantitative data on ROS and antioxidants are summarized below.
Table 2: Key Enzymatic Antioxidant Defenses and Their Roles
| Antioxidant Enzyme | Isoforms / Location | Reaction Catalyzed | Role in Inflammation |
|---|---|---|---|
| Superoxide Dismutase (SOD) | SOD1 (cytosol), SOD2 (mitochondria), SOD3 (extracellular) [2] [3] | 2 O₂•⁻ + 2H⁺ → H₂O₂ + O₂ [1] [2] | First line of defense; converts O₂•⁻ to the less reactive H₂O₂. Its dysregulation allows O₂•⁻ to accumulate and form ONOO⁻. |
| Catalase (CAT) | Primarily peroxisomes [2] | 2 H₂O₂ → 2 H₂O + O₂ [4] | Crucial for removing high concentrations of H₂O₂, preventing its conversion to the highly damaging OH• via Fenton chemistry. |
| Glutathione Peroxidase (GPx) | GPx1 (cytosol, mitochondria), GPx4 (membrane) [2] | H₂O₂ + 2 GSH → GSSG + 2 H₂O (or organic hydroperoxides) [4] | Plays a major role in H₂O₂ clearance at lower concentrations; maintains cellular redox balance via the GSH/GSSG ratio. |
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Research Reagents for Studying ROS and Inflammation
| Research Reagent / Material | Function / Application | Example Use in the Field |
|---|---|---|
| NOX Inhibitors (e.g., GKT136901, VAS2870) | Pharmacologically inhibit specific NADPH oxidase isoforms to dissect their contribution to ROS production and inflammatory signaling. | Used to demonstrate NOX4's role in endothelial cell inflammation and fibrosis models [1]. |
| Nrf2 Activators (e.g., sulforaphane, CDDO-Me) | Stabilize Nrf2 by modifying Keap1 cysteine residues, inducing ARE-driven gene expression for experimental or therapeutic purposes. | Preclinical studies use sulforaphane to boost antioxidant defenses and mitigate inflammation in models of metabolic syndrome [3] [5]. |
| ROS-Sensitive Fluorescent Probes (e.g., DCFH-DA, MitoSOX Red) | Detect and quantify general cellular ROS (DCFH-DA) or mitochondrial superoxide (MitoSOX) via flow cytometry or fluorescence microscopy. | Standard tools for confirming increased ROS generation in immune cells upon stimulation with TNF-α or LPS [1] [4]. |
| NF-κB Reporter Cell Lines | Engineered cells containing a luciferase gene under the control of an NF-κB response element; used to screen for pro- or anti-inflammatory compounds. | Used in high-throughput screens to identify novel compounds that inhibit ROS-induced NF-κB activation [3] [5]. |
| ELISA/Kits for Biomarkers | Quantify protein levels of oxidative damage markers (e.g., 3-nitrotyrosine, 4-HNE) or inflammatory cytokines (e.g., IL-1β, IL-6, TNF-α). | Essential for correlating oxidative stress with inflammatory burden in cell culture supernatants, plasma, or tissue homogenates [3] [4]. |
Key Experimental Protocols
To investigate the interplay between ROS and inflammation, robust and reliable experimental methodologies are required. Below are detailed protocols for two fundamental assays.
Protocol: Measuring Intracellular ROS using DCFH-DA
Principle: The cell-permeable dye 2',7'-Dichlorofluorescin diacetate (DCFH-DA) is deacetylated by cellular esterases to non-fluorescent DCFH, which is trapped inside the cell. Upon oxidation by intracellular ROS (primarily H₂O₂ and peroxidases), it is converted to highly fluorescent 2',7'-Dichlorofluorescein (DCF). Fluorescence intensity is proportional to ROS levels.
Materials:
- DCFH-DA reagent (prepare a 10-20 mM stock solution in DMSO)
- Phosphate Buffered Saline (PBS) or appropriate cell culture medium without serum
- Cells of interest (e.g., endothelial cells, macrophages) cultured in a 96-well black-walled plate
- Positive control (e.g., 100-500 µM tert-Butyl hydroperoxide, tBHP)
- Fluorescent microplate reader or flow cytometer
Method:
- Cell Preparation: Seed and culture cells to 70-80% confluency. Prior to treatment, wash the cells twice with pre-warmed, serum-free medium or PBS.
- Dye Loading: Incubate cells with 10-20 µM DCFH-DA in serum-free medium for 30-60 minutes at 37°C in the dark.
- Washing: Carefully remove the DCFH-DA solution and wash the cells twice with PBS to remove any extracellular dye.
- Treatment and Measurement:
- For kinetic studies: Add fresh medium with or without the test compounds/inflammatory stimuli (e.g., LPS, TNF-α) and immediately place the plate in a fluorescent microplate reader. Measure fluorescence (Ex/Em ~485/535 nm) at regular intervals (e.g., every 30 minutes for 2-4 hours).
- For endpoint analysis: Incubate cells with treatments for a desired period, then measure fluorescence.
- Data Analysis: Normalize fluorescence data to protein content (via BCA assay) or cell number. Express results as fold-change relative to the untreated control.
Protocol: Assessing NF-κB Activation via Electrophoretic Mobility Shift Assay (EMSA)
Principle: EMSA is used to detect protein-DNA interactions. It measures the binding of nuclear extract proteins, specifically NF-κB, to a radiolabeled or chemiluminescent DNA probe containing the κB consensus sequence. The protein-DNA complex has reduced mobility in a non-denaturing polyacrylamide gel.
Materials:
- Nuclear Extract Kit (e.g., NE-PER Kit)
- Double-stranded oligonucleotide containing the κB consensus sequence (5'-GGGACTTTCC-3')
- T4 Polynucleotide Kinase and [γ-³²P]ATP or biotin end-labeling kit
- Non-denaturing polyacrylamide gel electrophoresis system
- Buffers: Binding buffer, poly(dI•dC) as non-specific competitor
- Autoradiography film or chemiluminescence detection system
Method:
- Nuclear Extraction: Harvest control and treated cells (e.g., with ROS or TNF-α). Prepare nuclear extracts according to the commercial kit's instructions. Determine protein concentration.
- Probe Labeling: Label the κB oligonucleotide probe with [γ-³²P]ATP using T4 Polynucleotide Kinase, or with biotin. Purify the labeled probe.
- Binding Reaction: In a total volume of 20 µL, incubate 5-10 µg of nuclear extract with the labeled probe (50,000-100,000 cpm) in binding buffer containing poly(dI•dC) and other components for 20-30 minutes at room temperature.
- For specificity control (supershift): Pre-incubate the nuclear extract with an antibody against a specific NF-κB subunit (e.g., p65) for 15-30 minutes before adding the probe.
- For competition control: Include a 100-fold molar excess of unlabeled (cold) κB probe to demonstrate binding specificity.
- Gel Electrophoresis: Load the reactions onto a pre-run, non-denaturing 4-6% polyacrylamide gel in 0.5x TBE buffer. Run the gel at 100-150 V at 4°C until the dye front is near the bottom.
- Detection:
- For radioactive probes: Dry the gel and expose it to X-ray film at -80°C or use a phosphorimager.
- For biotinylated probes: Transfer the DNA-protein complexes to a positively charged nylon membrane, crosslink, and detect using a chemiluminescent nucleic acid detection module.
- Analysis: The presence of a shifted band indicates NF-κB binding. A supershifted band (higher molecular weight) confirms the identity of the subunit in the complex.
The transcription factor NF-κB serves as a critical molecular bridge connecting reactive oxygen species (ROS) signaling to inflammatory gene expression. This whitepaper examines the sophisticated mechanisms through which ROS activate NF-κB and how this pathway initiates and sustains inflammatory responses relevant to chronic diseases. We provide a comprehensive analysis of the bidirectional regulatory relationships, experimental methodologies for studying this pathway, and quantitative data on redox-sensitive molecular components. Understanding these mechanisms provides a rational basis for therapeutic interventions targeting oxidative stress-linked inflammatory conditions, including metabolic disorders, cardiovascular diseases, and neurodegenerative conditions.
Nuclear Factor-kappa B (NF-κB represents a family of inducible transcription factors that function as pivotal mediators of inflammatory responses, immune regulation, and cell survival [6]. Initially identified in 1986 as a nuclear factor binding to the kappa enhancer in B-cells, NF-κB is now recognized as a ubiquitously expressed stress response factor activated by diverse stimuli, including cytokines, pathogens, and oxidative stress [7]. The functional interplay between ROS and NF-κB establishes a fundamental signaling axis that drives pathological inflammation in chronic diseases. Under physiological conditions, this system maintains immune vigilance, but when dysregulated, it perpetuates a cycle of oxidative damage and inflammation that characterizes conditions such as atherosclerosis, metabolic syndrome, and neurodegenerative disorders [3].
The redox sensitivity of NF-κB positions it as a key sensor of cellular oxidative status, translating biochemical changes in ROS concentrations into transcriptional programs. This pathway exemplifies how oxidative stress extends beyond random macromolecular damage to encompass highly organized signaling processes that can be therapeutically targeted. The following sections delineate the molecular architecture of NF-κB signaling, its precise mechanisms of redox regulation, experimental approaches for its investigation, and its pathophysiological significance in human disease.
Molecular Architecture of the NF-κB Signaling System
NF-κB Protein Family
The NF-κB family comprises five structurally related members that form various homo- and heterodimers with distinct regulatory functions and DNA-binding specificities [7]:
- NF-κB1 (p105/p50): Processed from its p105 precursor to the mature p50 form, which lacks a transactivation domain
- NF-κB2 (p100/p52): Processed from p100 to p52, similarly lacking transactivation capability
- RelA (p65): Contains a transactivation domain and is the major transcriptional activator
- RelB: Partners with p52 in the non-canonical pathway
- c-Rel: Important in immune cell responses and inflammation
The most abundant and well-characterized NF-κB dimer is the p50/RelA heterodimer, which serves as the primary effector of the canonical pathway [8]. All family members share a conserved Rel homology domain (RHD responsible for DNA binding, dimerization, and interaction with inhibitory proteins [7].
Inhibitory IκB Proteins and IKK Complex
In unstimulated cells, NF-κB dimers are sequestered in the cytoplasm through interaction with inhibitory IκB proteins, which mask nuclear localization sequences and prevent DNA binding [8]. The IκB family includes:
- Typical IκBs (IκBα, IκBβ, IκBε): Mainly cytoplasmic, containing ankyrin repeats that mediate NF-κB binding
- Atypical IκBs (IκBζ, Bcl-3, IκBNS): Nuclear proteins that can either repress or activate specific NF-κB dimers
- Precursor proteins (p105 and p100): Function as IκB-like molecules through their C-terminal ankyrin repeat domains
The activation of NF-κB requires signal-induced phosphorylation of IκB proteins by the IκB kinase (IKK complex, which consists of two catalytic subunits (IKKα and IKKβ and a regulatory subunit (NEMO/IKKγ) [7]. Phosphorylation targets IκB for ubiquitination and proteasomal degradation, liberating NF-κB for nuclear translocation.
ROS-Mediated Activation of NF-κB Signaling
Canonical NF-κB Pathway Activation
The canonical NF-κB pathway responds to numerous stimuli including proinflammatory cytokines (TNF-α, IL-1, bacterial products (LPS, and ROS [6]. As shown in Figure 1, ROS influence multiple steps in this activation cascade:
Figure 1: ROS activation of the canonical NF-κB pathway
ROS influence multiple steps in NF-κB activation: (1) ROS can directly activate IKK through oxidative modification; (2) ROS inhibit phosphatases that normally suppress NF-κB signaling; (3) ROS promote the dissociation of NF-κB from IκB by enhancing IκB degradation; (4) In the nucleus, ROS can both inhibit and enhance DNA binding depending on concentration and cellular redox state.
Key Redox-Sensitive Molecular Targets in NF-κB Activation
Multiple components of the NF-κB signaling cascade demonstrate redox sensitivity through modification of critical cysteine residues:
Table 1: Redox-Sensitive Sites in the NF-κB Pathway
| Target Molecule | Redox Modification | Functional Consequence | Experimental Evidence |
|---|---|---|---|
| IKKβ | Oxidation of Cys-179 | Inhibition of kinase activity | H₂O₂ treatment inhibits TNF-α-induced IKK activity [8] |
| p50 subunit | Oxidation of Cys-62 | Decreased DNA binding capacity | Spatial regulation with oxidation in cytoplasm, reduction in nucleus [8] |
| NIK | Oxidation-induced activation | Enhanced IKKα phosphorylation | IL-1β treatment increases ROS-mediated NIK activation [8] |
| LC8 (dynein light chain) | Redox-dependent dissociation from IκBα | Allows IκBα phosphorylation | ROS oxidizes LC8, promoting NF-κB activation [8] |
| Ref-1 | Reduction of p50 | Enhanced DNA binding | Nuclear Ref-1 reduces Cys-62, restoring DNA binding [8] |
Biphasic and Context-Dependent ROS Effects
The relationship between ROS and NF-κB activation demonstrates complex biphasic characteristics. While moderate oxidative stress typically activates NF-κB, sustained or severe oxidative stress can inhibit NF-κB signaling through multiple mechanisms [8]:
- Early phase activation: Low to moderate ROS levels promote IKK activation and IκB degradation
- Sustained oxidative stress: Leads to proteasome inhibition, preventing IκB degradation and NF-κB activation
- Direct oxidative inhibition: High ROS levels oxidize critical cysteine residues in NF-κB subunits, impairing DNA binding
This biphasic relationship explains seemingly contradictory findings in the literature and underscores the importance of considering ROS concentration, timing, and cellular context when investigating this pathway.
NF-κB-Dependent Pro-Inflammatory Gene Expression
Upon activation and nuclear translocation, NF-κB dimers bind to specific κB enhancer elements in the promoters of target genes, initiating a pro-inflammatory transcriptional program. The specific gene repertoire induced depends on cell type, nature of the stimulus, and dimer composition.
Table 2: Major Categories of NF-κB Target Genes in Inflammation
| Gene Category | Specific Examples | Functional Role in Inflammation |
|---|---|---|
| Cytokines | TNF-α, IL-1β, IL-6, IL-12 | Amplify inflammatory signals; recruit immune cells |
| Chemokines | IL-8, MCP-1, MIP-1α | Direct leukocyte migration to sites of inflammation |
| Adhesion Molecules | ICAM-1, VCAM-1, E-selectin | Mediate leukocyte endothelial adhesion and transmigration |
| Enzymes | iNOS, COX-2 | Produce inflammatory mediators (NO, prostaglandins) |
| Regulatory Proteins | IκBα (feedback inhibition) | Terminate NF-κB signaling through negative feedback |
NF-κB activation in specific cell types generates distinct inflammatory outcomes:
- Macrophages: NF-κB drives polarization toward pro-inflammatory M1 phenotype with enhanced cytokine production [6]
- Endothelial cells: NF-κB increases adhesion molecule expression, enhancing leukocyte recruitment and vascular inflammation [9]
- Neutrophils: NF-κB extends lifespan and promotes formation of neutrophil extracellular traps (NETs) [9]
Interplay with Other Redox-Sensitive Pathways
Cross-Regulation with Nrf2 Antioxidant Pathway
The NF-κB pathway exhibits extensive cross-regulation with the Nrf2-Keap1 antioxidant system, creating a delicate balance between inflammatory and antioxidant responses:
Figure 2: NF-κB and Nrf2 pathway interactions
NF-κB and Nrf2 pathways interact through multiple mechanisms: (1) Competition for the transcriptional co-activator CBP, which can be limiting; (2) Nrf2 activation induces antioxidant genes that reduce ROS and indirectly suppress NF-κB; (3) NF-κB can modulate Nrf2 transcription and activity; (4) KEAP1, which normally targets Nrf2 for degradation, can also function as an IKKβ E3 ubiquitin ligase, linking the two pathways [8].
Feedback Loops and Oscillatory Dynamics
NF-κB signaling displays complex temporal dynamics characterized by oscillatory nucleocytoplasmic shuttling. Negative feedback regulators, particularly IκBα and the deubiquitinase A20, ensure transient responses to stimulation rather than sustained activation [8]. ROS can modulate these feedback loops by:
- Influencing the synthesis and degradation of IκB proteins
- Modifying the activity of deubiquitinating enzymes
- Affecting proteasome function, which is crucial for IκB degradation and NF-κB activation
These dynamic features allow fine-tuned inflammatory responses appropriate to the stimulus intensity and duration, with dysregulation leading to chronic inflammation.
Experimental Approaches for Studying ROS-NF-κB Interactions
Establishing ROS-Dependent NF-κB Activation
To demonstrate ROS-mediated NF-κB activation, researchers employ a combination of pharmacological and genetic approaches:
Protocol 1: Verification of ROS-Dependent NF-κB Activation
- Stimulation: Treat cells with ROS-generating agents (H₂O₂ 100-500 μM; menadione 10-50 μM; TNF-α 10-50 ng/mL as a positive control)
- ROS inhibition: Pre-treat with antioxidants (N-acetylcysteine 5-20 mM; catalase-PEG 100-500 U/mL; Tempol 1-5 mM) 30-60 minutes prior to stimulation
- NF-κB activation assessment:
- Electrophoretic Mobility Shift Assay (EMSA): Measure NF-κB DNA binding in nuclear extracts
- Immunofluorescence microscopy: Visualize p65 nuclear translocation
- Western blotting: Analyze IκBα degradation and p65 phosphorylation
- Luciferase reporter assay: Quantify NF-κB transcriptional activity
Specific Molecular Target Identification
To pinpoint specific redox-sensitive cysteine residues in NF-κB pathway components:
Protocol 2: Identification of Redox-Sensitive Cysteine Residues
- Site-directed mutagenesis: Replace candidate cysteine residues with serine or alanine
- Mass spectrometry: Identify oxidized cysteine residues in immunoprecipitated proteins
- Functional assays:
- Kinase activity assays: For IKK mutants after oxidative treatment
- DNA binding assays: For NF-κB subunit mutants using EMSA
- Gene reporter assays: Compare transcriptional activity of redox-insensitive mutants
Research Reagent Solutions
Table 3: Essential Research Tools for ROS-NF-κB Studies
| Reagent Category | Specific Examples | Application/Function |
|---|---|---|
| ROS Inducers | H₂O₂, menadione, tert-butyl hydroperoxide | Experimental generation of oxidative stress |
| ROS Scavengers | N-acetylcysteine (NAC), Tempol, catalase-PEG | Antioxidants to establish ROS dependence |
| IKK Inhibitors | IKK-16, BMS-345541, SC-514 | Pharmacological inhibition of IKK complex |
| NF-κB Reporters | NF-κB luciferase constructs, GFP-p65 fusion proteins | Monitoring NF-κB activation and localization |
| Antibodies | Phospho-IκBα, phospho-p65, total p65, IKKγ | Detection of pathway activation by Western blot, IF |
| Genetic Tools | siRNA against Nrf2, Nox isoforms, NF-κB subunits | Gene-specific manipulation of pathway components |
Pathophysiological Implications in Chronic Diseases
The ROS-NF-κB axis contributes significantly to the pathogenesis of numerous chronic inflammatory conditions:
Metabolic Diseases
In obesity and type 2 diabetes, elevated ROS production from nutrient overload activates NF-κB in adipocytes, hepatocytes, and immune cells, driving chronic low-grade inflammation that promotes insulin resistance [3]. This establishes a vicious cycle where metabolic dysfunction generates oxidative stress, which perpetuates inflammation through NF-κB, further worsening metabolic parameters.
Cardiovascular Diseases
Atherosclerosis represents a classic example of redox-sensitive NF-κB activation in vascular pathology. ROS generated within atherosclerotic plaques activate NF-κB in endothelial cells, smooth muscle cells, and macrophages, promoting expression of adhesion molecules, cytokines, and pro-coagulant factors [9]. NF-κB also contributes to the phenotypic switching of vascular smooth muscle cells from contractile to synthetic states, accelerating plaque progression.
Neurological Disorders
In ischemic stroke, reperfusion injury generates explosive ROS production through mitochondrial reverse electron transport, xanthine oxidase, and NADPH oxidases [10]. This oxidative burst activates NF-κB, amplifying inflammatory damage in vulnerable neuronal populations. Similar mechanisms operate in neurodegenerative diseases, where chronic oxidative stress and NF-κB activation drive neuroinflammation.
Pulmonary Diseases
Hyperoxic lung injury models demonstrate maturation-dependent NF-κB activation, with neonatal lungs showing preferential NF-κB activation upon hyperoxia exposure compared to adult lungs [8]. This differential response may contribute to developmental lung disorders such as bronchopulmonary dysplasia.
Therapeutic Implications and Future Directions
Targeting the ROS-NF-κB axis presents both opportunities and challenges for therapeutic development. Traditional antioxidant approaches have shown limited clinical success, likely due to non-specific actions and failure to address the nuanced role of ROS as signaling molecules [3]. More promising strategies include:
- Specific IKK inhibitors: Development of compounds that selectively target redox-sensitive IKK activation
- Nrf2 activators: Potentiation of endogenous antioxidant systems to indirectly modulate NF-κB
- Inhibitors of ROS-generating enzymes: Selective targeting of specific Nox isoforms
- Modulation of redox-sensitive phosphatases: Enhancing endogenous negative regulators of NF-κB signaling
Future research should focus on delineating cell-type-specific redox regulation of NF-κB, understanding temporal dynamics of pathway activation, and developing sophisticated delivery systems for tissue-specific targeting. The integration of systems biology approaches with single-cell technologies will further illuminate the complex interplay between oxidative stress and inflammation in human disease.
The activation of NF-κB by ROS constitutes a fundamental pro-inflammatory pathway with far-reaching implications for chronic disease pathogenesis. This whitepaper has detailed the molecular mechanisms, regulatory networks, experimental approaches, and pathophysiological significance of this critical signaling axis. The bidirectional nature of ROS-NF-κB interactions—with ROS both activating and being produced downstream of NF-κB—creates self-amplifying loops that sustain inflammatory responses in chronic diseases. Moving forward, sophisticated manipulation of this pathway, rather than blanket inhibition, holds promise for breaking the cycle of oxidative stress and inflammation in diverse pathological conditions.
The Nrf2-Keap1 signaling pathway is the principal cellular defense mechanism against oxidative and electrophilic stress [11] [12]. This system maintains cellular redox homeostasis by regulating the transcription of a broad network of antioxidant and cytoprotective genes [13] [14]. Under normal physiological conditions, the pathway ensures a finely-tuned, transient activation of Nrf2, preventing unnecessary antioxidant gene expression while maintaining readiness against oxidative insults [13]. However, dysregulation of this axis has been implicated in nearly all major human diseases, from neurodegenerative and cardiovascular diseases to diabetes and cancer, underscoring its critical role in the interplay between oxidative stress, inflammation, and chronic disease pathogenesis [11] [15].
The molecular players in this pathway are precisely structured for their roles. Nuclear factor erythroid 2-related factor 2 (NRF2) is a transcription factor belonging to the Cap'n'collar (CNC) basic leucine zipper (bZIP) family [14]. It is a modular protein composed of seven functional NRF2-ECH homology (Neh) domains [14]. The Neh2 domain contains DLG and ETGE motifs that facilitate binding to its negative regulator, KEAP1 [12] [14]. The Neh1 domain contains a CNC-bZIP DNA-binding motif that allows NRF2 to dimerize with small Maf proteins and bind to Antioxidant Response Elements (ARE) in DNA [12] [14]. The transactivation domains Neh3, Neh4, and Neh5 interact with coactivators, while Neh6 and Neh7 negatively regulate NRF2 through β-TrCP and RXRα interactions, respectively [14].
Kelch-like ECH-associated protein 1 (KEAP1) functions as the primary cellular sensor for oxidative and electrophilic stressors [12] [16]. This cysteine-rich, homodimeric protein contains five primary domains [16] [14]:
- BTB domain: Mediates KEAP1 homodimerization and binding to CUL3
- IVR domain: Rich in cysteine residues that function as stress sensors
- Kelch/DGR domain: Comprises six Kelch repeats that bind to the ETGE and DLG motifs of NRF2
- NTR and CTR domains: Flanking terminal regions
The following diagram illustrates the core regulatory mechanism of the Nrf2-Keap1 pathway under basal and stressed conditions:
Regulatory Mechanisms and Pathophysiological Roles
The Molecular Switch: From Basal Repression to Stress Activation
Under homeostatic conditions, KEAP1 forms part of a CUL3-RBX1 E3 ubiquitin ligase complex that tightly regulates NRF2 activity by targeting it for ubiquitination and proteasome-dependent degradation [12] [13]. The "hinge and latch" model explains this interaction: the KEAP1 homodimer binds NRF2 through two binding sites - a high-affinity ETGE motif (hinge) and a low-affinity DLG motif (latch) - creating a configuration that efficiently presents NRF2 for ubiquitination [12] [16].
During oxidative or electrophilic stress, specific cysteine residues in KEAP1 (notably Cys151 in the BTB domain and Cys273/Cys288 in the IVR domain) undergo modification [12] [16]. This induces conformational changes in KEAP1 that disrupt the "latch" interaction with the DLG motif while maintaining the "hinge" ETGE binding [16]. Consequently, NRF2 ubiquitination is impaired, leading to its stabilization and accumulation. Newly synthesized NRF2 escapes degradation, translocates to the nucleus, heterodimerizes with small Maf proteins, and binds to ARE/EpRE sequences in the promoter regions of target genes [12] [14].
The Double-Edged Sword: Protective versus Pathological Roles
The Nrf2-Keap1 axis exhibits a dual nature in human health and disease, functioning protectively in normal physiology but contributing to pathology when dysregulated.
Cytoprotective Roles: Under physiological conditions, transient NRF2 activation coordinates the expression of over 500 genes involved in cellular defense [15]. This includes antioxidants (SOD, catalase, GPx), glutathione synthesis and metabolism enzymes (GCLC, GCLM, GST), NADPH regeneration enzymes (G6PDH, 6PGD), and phase II detoxification enzymes (NQO1, HO-1) [12] [14] [15]. Through this extensive transcriptional program, NRF2 enhances cellular resilience against oxidative stress, reduces inflammation, and maintains redox homeostasis [11] [17].
Pathological Roles: Persistent NRF2 activation creates a environment conducive to tumorigenesis and therapy resistance [13] [16]. Cancer cells with constitutive NRF2 activation exhibit enhanced antioxidant capacity, metabolic reprogramming, chemoresistance, and immune evasion [18] [13] [14]. A 2025 study revealed that KEAP1 depletion or pharmacological inhibition diminishes PD-L1 expression across multiple cancer types, establishing the KEAP1/NRF2 axis as a novel mediator of this critical immune checkpoint protein [18]. This hyperactivation commonly results from somatic mutations in KEAP1, NRF2 (NFE2L2), or CUL3 genes, or from competitive inhibition of the KEAP1-NRF2 interaction by proteins like p62 [16] [19].
Table 1: NRF2 Target Genes and Their Protective Functions
| Gene Category | Representative Genes | Biological Function | Role in Disease Protection |
|---|---|---|---|
| Antioxidant Enzymes | SOD, CAT, GPx, HO-1 | Direct neutralization of ROS | Reduces oxidative damage in neurodegenerative and cardiovascular diseases [15] |
| Glutathione Metabolism | GCLC, GCLM, GST, GR | Glutathione synthesis and recycling | Maintains cellular redox buffer; critical for detoxification [14] [15] |
| NADPH Regeneration | G6PDH, 6PGD, TKT, TAL | Pentose phosphate pathway enzymes | Provides reducing equivalents for antioxidant systems [14] |
| Detoxification Enzymes | NQO1, HO-1 | Phase II conjugation and elimination | Chemoprotection against carcinogens and toxins [12] [15] |
| Proteostasis | p62/SQSTM1 | Selective autophagy adapter | Clearance of damaged proteins and organelles [16] [19] |
Table 2: Disease Associations with Nrf2-Keap1 Pathway Dysregulation
| Disease Category | Specific Conditions | NRF2 Status | Molecular Consequences |
|---|---|---|---|
| Neurodegenerative | Alzheimer's, Parkinson's, ALS | Reduced activity | Increased oxidative damage, protein aggregation, neuronal death [17] [19] |
| Metabolic | Type 2 diabetes, metabolic syndrome | Context-dependent | Insulin resistance, β-cell dysfunction, complications [14] |
| Cardiovascular | Atherosclerosis, hypertension, heart failure | Reduced activity | Endothelial dysfunction, vascular inflammation, remodeling [11] [15] |
| Cancer | Lung, liver, thyroid, others | Frequently hyperactive | Metabolic reprogramming, chemoresistance, immune evasion [18] [16] [14] |
| Respiratory | COPD, asthma, fibrosis | Reduced activity | Chronic inflammation, tissue remodeling, oxidative damage [20] |
Experimental Approaches and Research Methodologies
CRISPR Screening for Pathway Discovery
A 2025 study employed a powerful functional CRISPR gene knockout screening approach to identify druggable regulators of PD-L1 expression in the KEAP1/NRF2 axis [18]. The experimental workflow and key findings are summarized below:
Detailed Methodology:
Library Design: A custom-designed sgRNA library targeting approximately 1,400 "druggable" human genes (based on literature review and gene-drug interaction databases) with ~10,000 sgRNAs (7 sgRNAs/gene plus ~500 control sgRNAs) [18].
Cell Line Selection: Screening performed across 6 cancer lines - 3 ovarian (OVCAR4, CaOV3, SKOV3) and 3 pancreatic (MiaPaca2, ASPC1, KP4) - selected for robust PD-L1 induction in response to IFNγ [18].
Screening Execution: Cas9-expressing cells were lentivirally infected with the sgRNA library at low multiplicity of infection (MOI ≈ 0.25). After puromycin selection, cells were expanded to maintain ~500X coverage per sgRNA [18].
Sorting and Analysis: Following 15 days of expansion and 48 hours of IFNγ treatment, cells were fluorescence-activated cell sorted (FACS) into PD-L1-high (top 25%) and PD-L1-low (bottom 25%) populations. Genomic DNA was isolated, sgRNA sequences amplified by PCR, and barcodes counted through next-generation sequencing (NGS) [18].
Bioinformatic Analysis: Differential enrichment of sgRNA barcodes and gene-level enrichment analysis in PD-L1-low versus high cells was assessed by beta-binomial modeling using the CB2 tool [18].
In Vivo and In Vitro Validation Approaches
In Vitro Models:
- Cell Culture Systems: SH-SY5Y neuroblastoma cells for neuronal studies, cultured in MEM/DMEM-F12 medium with 10% FBS, penicillin (100 U/mL), and streptomycin (0.1 mg/mL) at 37°C with 5% CO₂ [19].
- Treatment Paradigms: Pb(C₂H₃O₂)₂ for lead exposure studies; N-acetylcysteine (antioxidant), Artemisitene (NRF2 activator), and Rapamycin (autophagy activator) for mechanistic interventions [19].
In Vivo Models:
- Animal Subjects: Four-week-old male Sprague-Dawley rats (98.31 ± 8.58 g) housed in specific pathogen-free conditions with 12-hour light-dark cycles [19].
- Exposure Protocol: Intraperitoneal injection of 2 mg/kg Pb(C₂H₃O₂)₂ once daily, 5 days/week for 12 weeks to induce sub-chronic lead exposure [19].
- Behavioral Assessment: Morris water maze test to evaluate learning and spatial memory performance, including swimming distance, escape latency, and platform crossings [19].
- Tissue Analysis: Hippocampal morphology examination via hematoxylin-eosin and Nissl staining; Pb concentration measurement using ICP-MS after microwave-assisted acid digestion [19].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Nrf2-Keap1 Pathway Investigation
| Reagent/Category | Specific Examples | Research Application | Mechanistic Insight |
|---|---|---|---|
| NRF2 Activators | Sulforaphane, Dimethyl fumarate, Bardoxolone, Artemisitene | Induce nuclear translocation of NRF2 | React with KEAP1 cysteine residues to disrupt NRF2 ubiquitination [12] [19] |
| KEAP1 Inhibitors | KI-696, K67 | Block KEAP1-NRF2 protein-protein interaction | Directly target Kelch domain to prevent NRF2 binding and degradation [13] |
| Genetic Tools | CRISPR/Cas9 KO, siRNA/shRNA, NRF2/KEAP1 expression vectors | Genetic manipulation of pathway components | Establish causal relationships in pathway regulation and function [18] |
| Antibodies | Anti-NRF2, Anti-KEAP1, Anti-HO-1, Anti-NQO1 | Western blot, IHC, immunofluorescence, ChIP | Detect protein expression, localization, and DNA binding [18] [19] |
| Reporters | ARE-luciferase constructs | Measure pathway activation | Quantify transcriptional activity in high-throughput screening [12] |
| Oxidative Stress Probes | DCFDA, MitoSOX, H2DCFDA | Measure ROS production | Assess functional consequences of pathway modulation [19] |
Therapeutic Implications and Future Directions
The Nrf2-Keap1 pathway represents a compelling therapeutic target for a broad spectrum of human diseases. Pharmacological activation of NRF2 holds promise for conditions characterized by oxidative stress, including neurodegenerative diseases, metabolic disorders, and inflammatory conditions [20] [17]. Preclinical studies demonstrate that NRF2 activators can provide neuroprotection, enhance mitochondrial function, and reduce inflammation [17] [19]. Conversely, NRF2 inhibitors are being explored for cancers with hyperactive NRF2 signaling, aiming to sensitize tumors to conventional therapies and overcome treatment resistance [13] [16].
Current research focuses on developing context-specific modulators that can precisely tune NRF2 activity without completely abrogating or constitutively activating the pathway. The integration of NRF2 modulators into precision medicine frameworks requires a deeper understanding of the heterogeneity of pathway activation across different disease states and genetic backgrounds [13]. Future studies must define biomarkers of NRF2 dependency, optimize therapeutic windows, and address long-term safety concerns associated with pharmacological NRF2 modulation [13]. As our knowledge of the complex regulatory networks surrounding the Nrf2-Keap1 axis continues to expand, so too will our ability to harness this fundamental pathway for therapeutic benefit across the spectrum of human disease.
The cellular response to stress is governed by sophisticated signaling networks, with the transcription factors Nuclear Factor-Kappa B (NF-κB) and Nuclear Factor Erythroid 2-Related Factor 2 (Nrf2) serving as master regulators of inflammation and oxidative stress responses, respectively. While NF-κB primarily controls the expression of pro-inflammatory cytokines and chemokines, Nrf2 regulates a battery of antioxidant and cytoprotective genes. Historically studied in isolation, emerging evidence reveals these pathways are intricately linked through bidirectional cross-talk, forming a critical regulatory circuit that determines cellular fate in stress conditions. This antagonistic relationship represents a fundamental biological paradigm where inflammatory and antioxidant responses are reciprocally controlled. Understanding the molecular intricacies of this cross-talk is essential for elucidating the pathophysiology of chronic diseases and developing targeted therapeutic interventions for conditions where oxidative stress and inflammation coexist.
Molecular Mechanisms of Nrf2 and NF-κB Signaling
The Nrf2 Antioxidant Response Pathway
Nrf2 is a basic-region leucine zipper (bZIP) transcription factor that serves as the master regulator of cellular antioxidant defense. Under homeostatic conditions, Nrf2 is continuously ubiquitinated and degraded by the proteasome through its association with the Kelch-like ECH-associated protein 1 (Keap1) repressor protein, which acts as a substrate adaptor for a Cullin 3 (Cul3)-based E3 ubiquitin ligase complex [21] [22]. Keap1 binds Nrf2 via a two-site mechanism ("hinge and latch" model) using DLG and ETGE motifs, maintaining Nrf2 at low basal levels with a short half-life of approximately 10-30 minutes [21].
Upon exposure to oxidative stress or electrophiles, specific cysteine sensors in Keap1 undergo modification, inducing conformational changes that disrupt its ability to target Nrf2 for degradation. Newly synthesized Nrf2 subsequently accumulates and translocates to the nucleus, where it forms heterodimers with small Maf proteins and binds to the Antioxidant Response Element (ARE) in the promoter regions of target genes [21] [23]. This activation cascade induces the expression of a extensive network of over 200 cytoprotective genes, including heme oxygenase-1 (HO-1), NAD(P)H quinone oxidoreductase 1 (NQO1), and glutamate-cysteine ligase catalytic (GCLC) and modulatory (GCLM) subunits, which collectively enhance cellular resilience to oxidative damage [21] [23].
Table 1: Primary Nrf2 Target Genes and Their Cytoprotective Functions
| Gene | Protein | Cellular Function |
|---|---|---|
| HMOX1 | Heme Oxygenase-1 (HO-1) | Heme catabolism, antioxidant, anti-inflammatory |
| NQO1 | NAD(P)H Quinone Oxidoreductase 1 | Quinone detoxification, antioxidant |
| GCLC | Glutamate-Cysteine Ligase Catalytic Subunit | Glutathione biosynthesis |
| GCLM | Glutamate-Cysteine Ligase Modulatory Subunit | Glutathione biosynthesis |
| FTH1 | Ferritin Heavy Chain | Iron sequestration |
| TXNRD1 | Thioredoxin Reductase 1 | Redox regulation |
| SRXN1 | Sulfiredoxin | Antioxidant enzyme |
Beyond the canonical Keap1-dependent regulation, Nrf2 is also controlled through Keap1-independent mechanisms. Glycogen synthase kinase-3 (GSK-3) can phosphorylate Nrf2, creating a recognition motif for β-transducin repeat-containing protein (β-TrCP), which serves as a substrate receptor for a Skp1-Cul1-Rbx1/Roc1 ubiquitin ligase complex, leading to Nrf2 ubiquitination and proteasomal degradation [21] [22]. Additionally, the autophagy adapter protein p62 can sequester Keap1 to autophagic degradation, resulting in Nrf2 activation, thereby creating a link between autophagy and the antioxidant response [21].
The NF-κB Inflammatory Signaling Pathway
NF-κB represents a family of inducible transcription factors that function as primary mediators of inflammatory and immune responses. The NF-κB family comprises five members: NF-κB1 (p50/p105), NF-κB2 (p52/p100), RelA (p65), RelB, and c-Rel, which form various homo- and heterodimers with distinct transcriptional activities [21] [7]. These proteins share a conserved Rel homology domain (RHD) responsible for DNA binding, dimerization, and nuclear localization. The most abundant and extensively studied dimer is the p65/p50 heterodimer, which exhibits strong transactivation potential [7].
NF-κB activation occurs through two principal signaling cascades: the canonical and non-canonical pathways. The canonical pathway is typically activated by pro-inflammatory stimuli such as tumor necrosis factor-α (TNF-α), interleukin-1 (IL-1), and pathogen-associated molecular patterns (PAMPs). In resting cells, NF-κB dimers are sequestered in the cytoplasm through interaction with inhibitory proteins of the IκB family, predominantly IκBα. Upon cellular stimulation, the IκB kinase (IKK) complex—composed of catalytic subunits IKKα and IKKβ and the regulatory subunit NEMO (IKKγ)—is activated and phosphorylates IκBα, leading to its K48-linked ubiquitination and subsequent proteasomal degradation [21] [7]. This process liberates the NF-κB dimer, allowing its translocation to the nucleus where it binds to κB consensus sequences in target gene promoters and initiates transcription of inflammatory mediators.
Table 2: Major NF-κB Target Genes and Their Pro-inflammatory Functions
| Gene | Protein | Cellular Function |
|---|---|---|
| TNF | Tumor Necrosis Factor-α | Pro-inflammatory cytokine |
| IL6 | Interleukin-6 | Pro-inflammatory cytokine |
| IL1B | Interleukin-1β | Pro-inflammatory cytokine |
| CXCL8 | Interleukin-8 | Neutrophil chemotaxis |
| ICAM1 | Intercellular Adhesion Molecule 1 | Leukocyte adhesion |
| VCAM1 | Vascular Cell Adhesion Molecule 1 | Leukocyte adhesion |
| COX2 | Cyclooxygenase-2 | Prostaglandin synthesis |
| iNOS | Inducible Nitric Oxide Synthase | Nitric oxide production |
The non-canonical pathway, activated by specific stimuli such as CD40 ligand, B cell-activating factor (BAFF), and lymphotoxin-β, depends on NF-κB-inducing kinase (NIK)-mediated phosphorylation of IKKα, which subsequently phosphorylates the p100 precursor protein, leading to its partial proteasomal processing to mature p52. The resulting p52/RelB dimer then translocates to the nucleus to regulate genes involved in lymphoid organ development and B-cell maturation [22].
Molecular Cross-Talk: Mechanisms of Antagonistic Regulation
Nrf2-Mediated Suppression of NF-κB Signaling
The activation of the Nrf2 pathway results in potent suppression of NF-κB signaling through multiple interconnected mechanisms that ultimately restrain inflammatory responses:
Antioxidant-Mediated Indirect Inhibition: Nrf2 activation elevates the expression of a comprehensive network of antioxidant and detoxification enzymes, including HO-1, NQO1, and glutathione peroxidase, which collectively diminish cellular reactive oxygen species (ROS) levels [23] [24]. Since ROS function as critical secondary messengers in NF-κB activation by promoting IKK activity and IκBα degradation, this redox modulation creates an unfavorable environment for NF-κB signaling. Specifically, the Nrf2 target gene HO-1 catalyzes the degradation of heme into biliverdin (subsequently converted to bilirubin), carbon monoxide, and free iron, all of which possess anti-inflammatory properties [23]. Bilirubin and biliverdin exhibit potent antioxidant activity, while carbon monoxide modulates inflammatory responses through mitochondrial and signaling effects.
Direct Interference with NF-κB Activation: Nrf2 activation can impair IKKβ phosphorylation and subsequent IκBα degradation, thereby preventing NF-κB nuclear translocation [23]. Studies using Nrf2-deficient macrophages demonstrate enhanced IKKβ activity and increased phosphorylation and degradation of IκBα following inflammatory stimulation compared to wild-type cells [23]. Additionally, Nrf2 target genes such as GCLM and GCLC, which are essential for glutathione synthesis, contribute to maintaining cellular redox homeostasis, further inhibiting NF-κB activation.
Competition for Transcriptional Coactivators: Both Nrf2 and NF-κB require the CREB-binding protein (CBP)/p300 complex as an essential transcriptional coactivator for efficient gene expression. These transcription factors compete for limited pools of CBP/p300 in the nucleus, establishing a molecular competition that can reciprocally regulate their transcriptional outputs [23]. Nrf2 interacts with CBP through its Neh4 and Neh5 domains, while NF-κB p65 subunit binds CBP when phosphorylated at Ser276. Overexpression of p65 can sequester CBP, limiting its availability for Nrf2 and thereby repressing ARE-mediated gene expression [23].
NF-κB-Mediated Repression of Nrf2 Signaling
The NF-κB pathway reciprocally inhibits Nrf2 signaling through several well-characterized mechanisms:
Cytokine-Mediated Suppression: NF-κB activation induces the expression of pro-inflammatory cytokines, including TNF-α, IL-1β, and IL-6, which can subsequently suppress Nrf2 signaling through various mechanisms. These cytokines can activate GSK-3β, which phosphorylates Nrf2, leading to its β-TrCP-mediated ubiquitination and proteasomal degradation via the Keap1-independent pathway [21] [23]. This mechanism represents an indirect but potent means of Nrf2 suppression during inflammatory responses.
Transcriptional Coactivator Competition: As mentioned previously, the competition for CBP/p300 represents a pivotal mechanism of mutual repression. During robust inflammatory responses, activated NF-κB p65 subunits can effectively sequester limiting quantities of CBP/p300, thereby depriving Nrf2 of this essential coactivator and blunting the antioxidant response [23]. This competitive interplay creates a molecular switch that prioritizes inflammatory gene expression over antioxidant responses during acute stress.
Nuclear Keap1-Mediated Repression: NF-κB activation can influence the subcellular localization of Keap1, potentially promoting its nuclear translocation where it can directly interfere with Nrf2 transcriptional activity [23]. While Keap1 is predominantly cytoplasmic, studies have demonstrated that p65 overexpression can increase nuclear Keap1 levels, potentially through interactions with the nuclear import protein karyopherin alpha 6 (KPNA6). Nuclear Keap1 may subsequently repress Nrf2-ARE signaling through mechanisms that remain incompletely characterized but likely involve disruption of Nrf2-DNA binding or facilitation of nuclear Nrf2 degradation [23].
The intricate antagonistic relationship between NF-κB and Nrf2 is visually summarized in Figure 1, which illustrates the key molecular mechanisms of their bidirectional cross-talk.
Figure 1: Molecular Cross-Talk Between NF-κB and Nrf2 Signaling Pathways. The diagram illustrates the antagonistic regulation between these pathways, including competition for transcriptional coactivators (CBP/p300), antioxidant-mediated suppression of NF-κB, and cytokine-mediated inhibition of Nrf2.
Experimental Approaches for Studying NF-κB/Nrf2 Cross-Talk
In Vitro Methodologies
Cell Culture Models: The investigation of NF-κB/Nrf2 cross-talk employs various cellular models, including immortalized cell lines (HEK293T, BV-2 microglial cells, THP-1 monocyte/macrophages) and primary cells (mouse embryonic fibroblasts - MEFs, primary peritoneal macrophages) [25] [26] [27]. THP-1 monocyte/macrophages are particularly valuable for inflammation studies and can be differentiated into macrophage-like cells using phorbol esters (e.g., PMA at 0.1 μM for 24 hours) [27]. Genetic manipulation through siRNA-mediated knockdown or CRISPR-Cas9 gene editing allows specific disruption of Nrf2, NF-κB components (p65, IKK subunits), or regulatory proteins (Keap1) to establish causal relationships in the cross-talk mechanisms [25] [26].
Stimulation and Inhibition Protocols: Inflammatory activation is typically induced using lipopolysaccharide (LPS) at concentrations ranging from 100-500 ng/mL for 6-24 hours [26] [27]. Oxidative stress can be triggered using compounds like tert-butyl hydroquinone (tBHQ) or sulforaphane (e.g., 14 μM for 6 hours), which modify Keap1 cysteine residues and activate Nrf2 [23] [26]. Specific pathway inhibitors include Bay 11-7082 (5-10 μM), which inhibits IκBα phosphorylation, and ML385, which directly blocks Nrf2 activity [27].
Luciferase Reporter Assays: Reporter constructs containing ARE or κB response elements upstream of a luciferase gene are transfected into cells to monitor pathway activity. For instance, the pHO1-15-LUC plasmid contains the HO-1 promoter with functional AREs, while κB-dependent reporters utilize multiple NF-κB binding sites [26]. Co-transfection with expression vectors for Nrf2, Keap1, p65, or dominant-negative mutants (e.g., ΔETGE-Nrf2, IκBS32A/S36A) enables mechanistic studies of pathway interactions [26].
Protein-Protein Interaction Studies: Co-immunoprecipitation (Co-IP) assays investigate physical interactions between Nrf2, Keap1, p65, and CBP/p300. Cells are lysed in appropriate buffers (e.g., RIPA buffer with protease and phosphatase inhibitors), and target proteins are immunoprecipitated using specific antibodies, followed by Western blotting to detect associated proteins [26]. GST pulldown assays using recombinant GST-tagged proteins (e.g., GST-PAK1 for RAC1 activation studies) further characterize direct molecular interactions [26].
In Vivo Models
Genetic Mouse Models: Tissue-specific knockout mice generated using Cre-loxP technology provide powerful tools for investigating cell-type-specific functions of NF-κB and Nrf2. For example, hepatocyte-specific Nrf2/p65 double knockout mice have revealed spontaneous liver inflammation and necrosis when both transcription factors are absent, along with complex interactions in hepatocyte proliferation control [25]. Nrf2 knockout mice generally exhibit heightened sensitivity to inflammatory stimuli and increased NF-κB activation in various injury models [23].
Disease Induction Models: Carbon tetrachloride (CCl4)-induced liver injury models demonstrate the functional consequences of NF-κB/Nrf2 cross-talk, with Nrf2 deficiency impairing hepatocyte proliferation under homeostatic conditions and after acute injury [25]. Lipopolysaccharide (LPS)-induced systemic inflammation models reveal exaggerated cytokine production and NF-κB activation in Nrf2-deficient animals [23]. Macrophage depletion studies using clodronate liposomes have established the non-cell-autonomous mechanisms through which Nrf2/p65 cross-talk controls hepatocyte proliferation via macrophage accumulation [25].
Table 3: Essential Research Reagents for Studying NF-κB/Nrf2 Cross-Talk
| Reagent Category | Specific Examples | Research Application |
|---|---|---|
| Cell Lines | THP-1 monocytes, BV-2 microglia, MEFs | In vitro modeling of immune and inflammatory responses |
| Activators | LPS (100-500 ng/mL), TNF-α (10-50 ng/mL) | NF-κB pathway induction |
| Activators | Sulforaphane (5-20 μM), tBHQ (10-50 μM) | Nrf2 pathway induction |
| Inhibitors | Bay 11-7082 (5-10 μM), SC-514 | IKK/NF-κB pathway inhibition |
| Inhibitors | ML385, Brusatol | Nrf2 pathway inhibition |
| Genetic Tools | siRNA against p65/Nrf2, CRISPR-Cas9 | Gene-specific knockdown/knockout |
| Reporter Plasmids | ARE-luciferase, κB-luciferase | Pathway activity measurement |
| Antibodies | Anti-p65, anti-Nrf2, anti-IκBα, anti-HO-1 | Protein detection by Western/IF/IHC |
Pathophysiological Implications and Therapeutic Opportunities
Role in Chronic Disease Pathogenesis
The dysregulation of NF-κB/Nrf2 cross-talk contributes significantly to the pathogenesis of numerous chronic conditions:
Neurodegenerative Disorders: In neurological conditions, Nrf2 deficiency exacerbates NF-κB activity, leading to augmented cytokine production that contributes to astrogliosis, neuronal death, and demyelination [23]. Nrf2 knockout mice display heightened sensitivity to neuroinflammation and neurodegeneration, while Nrf2 activators demonstrate protective effects in models of Parkinson's and Alzheimer's disease [23].
Cardiovascular Diseases: In coronary artery disease, oxidative stress and inflammation drive disease progression through reciprocal NF-κB activation and Nrf2 repression [24]. Increased endoplasmic reticulum stress and Nrf2 repression have been documented in peripheral blood mononuclear cells of patients with stable coronary artery disease, while Nrf2 activation protects against ischemia/reperfusion injury and delays progression to heart failure [24].
COVID-19 Pathogenesis: Severe COVID-19 is characterized by NF-κB-mediated cytokine storm coupled with suppression of the Nrf2 pathway, creating a deleterious imbalance that amplifies tissue damage [28]. Transcriptomic analyses of COVID-19 patients reveal upregulated NF-κB signaling genes alongside suppression of Nrf2 antioxidant response genes, potentially contributing to neurological complications observed in severe infections [28].
Metabolic and Inflammatory Conditions: The NF-κB/Nrf2 imbalance manifests in various inflammatory and autoimmune diseases, including rheumatoid arthritis, inflammatory bowel disease, and lupus nephritis, where exaggerated NF-κB signaling drives pathology while impaired Nrf2 activity fails to provide adequate counter-regulation [23].
Therapeutic Interventions Targeting NF-κB/Nrf2 Cross-Talk
Several therapeutic approaches aim to restore balance to the NF-κB/Nrf2 axis:
Nrf2 Activators: Sulforaphane, an isothiocyanate found in cruciferous vegetables, and synthetic triterpenoids like CDDO-Im potently activate Nrf2 by modifying Keap1 cysteine residues, resulting in enhanced antioxidant gene expression and concomitant NF-κB suppression [23]. These compounds demonstrate efficacy in preclinical models of inflammation, neurodegeneration, and metabolic disorders.
NF-κB Inhibitors: Proteasome inhibitors (e.g., bortezomib) prevent IκB degradation, thereby maintaining NF-κB in an inactive cytoplasmic complex [7]. IKK-specific inhibitors (e.g., SPC-839, BMS-345541) directly target the kinase complex responsible for NF-κB activation, while monoclonal antibodies against pro-inflammatory cytokines (e.g., anti-TNF-α) interrupt positive feedback loops that sustain NF-κB signaling [7].
Dual-Targeting Approaches: Fucoxanthin, a marine carotenoid, exemplifies natural products with dual activity, simultaneously inhibiting NF-κB nuclear translocation while activating the Nrf2/HO-1 pathway, thereby ameliorating both inflammatory and oxidative stress components in cellular models [27]. Similarly, the sirtuin SIRT6 has emerged as a regulatory node that activates Nrf2 through Keap1 inhibition while suppressing NF-κB signaling, producing coordinated antioxidant and anti-inflammatory effects [24].
Novel Therapeutic Strategies: Emerging approaches include non-coding RNA-based therapies that simultaneously modulate both pathways, CAR-T cell therapies engineered to target inflammatory disease components, and combination therapies that strategically engage both pathways to restore redox and inflammatory homeostasis [7].
Concluding Perspectives
The antagonistic cross-talk between NF-κB and Nrf2 represents a fundamental biological paradigm that integrates cellular responses to inflammatory and oxidative stresses. The molecular mechanisms underlying this reciprocal regulation—including competition for transcriptional coactivators, pathway-specific post-translational modifications, and redox-mediated feedback loops—create a sophisticated control system that determines cellular fate under stress conditions. Understanding these interactions provides critical insights into the pathogenesis of chronic diseases characterized by concurrent inflammation and oxidative damage. Future research should focus on elucidating tissue-specific variations in this cross-talk, temporal aspects of pathway interactions, and developing therapeutic strategies that effectively restore balance to this critical regulatory axis for treating complex chronic diseases.
Oxidative Stress as a Common Denominator in Age-Related Diseases and Cancer
Oxidative stress, characterized by an imbalance between reactive oxygen species (ROS) and antioxidant defenses, is a fundamental pathological mechanism underpinning both aging and carcinogenesis. This whitepaper synthesizes current evidence on the role of oxidative stress as a key mediator connecting physiological aging with age-related diseases and cancer. We detail the molecular pathways through which oxidative damage to lipids, proteins, and DNA drives cellular senescence, chronic inflammation, and malignant transformation. The document provides a comprehensive analysis of validated oxidative stress biomarkers, standardized methodologies for their quantification, and visualization of critical signaling pathways. Furthermore, we explore the therapeutic implications of targeting oxidative stress pathways, highlighting both challenges and opportunities for researchers and drug development professionals working at the intersection of redox biology and chronic disease.
The free radical theory of aging, first proposed by Denham Harman in 1956, posits that the cumulative damage inflicted by reactive oxygen species (ROS) throughout an organism's lifespan drives the functional declines characteristic of aging [29]. This theory has since evolved into the more nuanced oxidative stress theory of aging, which incorporates our modern understanding of redox signaling and antioxidant defense systems [30]. Oxidative stress results when the critical balance between pro-oxidant and antioxidant molecules shifts toward the former, leading to disruptive oxidation of cellular macromolecules and altered signal transduction [29].
Aging constitutes a progressive loss of tissue and organ function over time, with oxidative stress representing a core mechanism underlying age-associated functional declines [30]. The close relationship between oxidative stress, inflammation, and aging has led to the formulation of the "oxi-inflamm-aging" theory, which describes a vicious cycle wherein chronic oxidative stress particularly affects regulatory systems (nervous, endocrine, and immune), triggering inflammatory responses that further exacerbate oxidative damage [30]. This framework establishes oxidative stress as a common biological platform linking fundamental aging processes with multiple pathological conditions, including neurodegenerative diseases, cardiovascular disorders, metabolic diseases, and various cancers [31].
In the context of cancer, oxidative stress demonstrates a dual nature. While excessive ROS can cause irreversible damage to DNA, proteins, and lipids, promoting genomic instability and carcinogenesis, cancer cells also exploit ROS at moderate levels to drive proliferative signaling and survival pathways [32]. This paradoxical relationship establishes oxidative stress as a significant factor across the entire cancer continuum, from initiation and promotion to progression and metastasis.
Molecular Mechanisms and Pathophysiological Pathways
Reactive oxygen and nitrogen species (RONS) originate from both endogenous and exogenous sources. Endogenous production occurs primarily through:
- Mitochondrial electron transport: Electron leakage during oxidative phosphorylation generates superoxide anion (O₂•⁻), particularly at complexes I and III of the electron transport chain [29].
- NADPH oxidases (NOX): Membrane-associated enzymes that catalyze the production of superoxide anion by transferring electrons from NADPH to molecular oxygen [30].
- Other enzymatic systems: Xanthine oxidase, uncoupled endothelial nitric oxide synthase (eNOS), and reactions involving cytochrome P450 enzymes, lipoxygenase, and cyclooxygenase [32].
Exogenous RONS sources include ionizing radiation, environmental pollutants, tobacco smoke, certain pharmaceuticals (e.g., cyclosporine, tacrolimus), and industrial chemicals [30]. These exogenous stressors amplify the endogenous oxidative burden, accelerating cellular damage.
The superoxide anion undergoes dismutation by superoxide dismutase (SOD) to form hydrogen peroxide (H₂O₂), which is more stable and membrane-permeable. Through Fenton or Haber–Weiss reactions, H₂O₂ can be converted to the highly reactive hydroxyl radical (OH•), which reacts indiscriminately with cellular components [30]. Simultaneously, nitric oxide (NO) produced by nitric oxide synthase (NOS) isoforms can react with superoxide to form peroxynitrite (ONOO⁻), a potent nitrating agent that contributes to nitrosative stress [30].
Oxidative Damage to Cellular Macromolecules
RONS, whether endogenous or exogenous, cause oxidative modifications to all major cellular macromolecules, which can serve as biomarkers of oxidative stress [30].
Lipid Peroxidation
Poly-unsaturated fatty acids (PUFAs) in cell membranes are particularly vulnerable to oxidation by hydroxyl and peroxyl radicals [30]. This peroxidation generates reactive aldehydes including:
- Malondialdehyde (MDA)
- 4-Hydroxy-2-nonenal (4-HNE)
- Isoprostanes (F2-IsoPs)
These lipid peroxidation products can further damage proteins and DNA, and are implicated in various pathological processes including atherosclerosis and inflammation [30].
Protein Modification
Oxidative protein modifications include:
- Protein carbonyls (PC): Formed by Fenton reaction of oxidants with lysine, arginine, proline, and threonine residues, or via binding of aldehydic lipid oxidation products (Michael-addition reactions) [30].
- Nitrotyrosine (NT): Generated through reactions between reactive nitrogen species and tyrosine residues [33].
- Advanced Glycation End Products (AGEs): Result from non-enzymatic reactions between reducing sugars and amino groups of proteins, particularly enhanced under hyperglycemic conditions [33].
DNA Oxidation
Oxidative damage to DNA results in mutagenic lesions including:
- 8-oxo-7,8-dihydro-guanine (8-oxoGuo)
- 8-oxo-7,8-dihydro-2′-deoxyguanosine (8-oxodG)
- Various base modifications (2-hydroxy adenine, 8-oxoadenine, 5-hydroxycytosine)
8-oxoGuo represents a highly mutagenic lesion that can result in G-to-T transversion events, contributing to carcinogenesis [30].
Antioxidant Defense Systems
Biological systems employ sophisticated antioxidant defenses comprising both enzymatic and non-enzymatic components:
- Primary antioxidant enzymes: Superoxide dismutase (SOD) catalyzes the conversion of superoxide to hydrogen peroxide; catalase (CAT) decomposes hydrogen peroxide to water and oxygen; glutathione peroxidase (GSH-Px) reduces peroxides and hydroxyl radicals using reduced glutathione (GSH) as a substrate [30].
- Other antioxidant enzymes: Glutathione-S-transferase and glucose-6-phosphate dehydrogenase provide additional protective capacity [30].
- Non-enzymatic antioxidants: Include bilirubin, α-tocopherol (vitamin E), β-carotene, ascorbic acid (vitamin C), albumin, uric acid, glutathione, and phenolic compounds such as resveratrol [30] [32].
The delicate balance between ROS production and these antioxidant defenses determines the cellular redox state, with disruption of this equilibrium leading to oxidative stress and its pathological consequences.
Signaling Pathways Linking Oxidative Stress with Aging and Cancer
Oxidative Stress-Induced Cellular Senescence
Cellular senescence represents a state of irreversible growth arrest triggered by various stressors, including oxidative damage. Senescent cells acquire a distinctive secretory phenotype known as the senescence-associated secretory phenotype (SASP), characterized by secretion of pro-inflammatory cytokines, chemokines, growth factors, and proteases [30]. RONS induce cellular senescence through multiple interconnected mechanisms:
- mTOR pathway regulation: Oxidative stress modulates mammalian target of rapamycin complexes, influencing cellular growth and metabolism [30].
- FOXO protein inhibition: RONS inhibit FOXO transcription factors, which are involved in insulin/insulin-like growth factor-1-mediated protection from oxidative stress [30].
- Sirtuin activity reduction: Oxidative stress suppresses sirtuins, histone deacetylases that regulate stress response and longevity pathways, leading to increased ROS production and inflammation [30].
- Cell cycle regulation: RONS activate the p16INK4a/pRB and p53/p21 pathways, establishing and maintaining senescence-associated growth arrest [30].
The following diagram illustrates the key signaling pathways through which oxidative stress induces cellular senescence:
Oxidative Stress in Carcinogenesis
The role of oxidative stress in cancer is complex and context-dependent, contributing to both tumor initiation and progression through several mechanisms:
- Genomic instability: ROS-induced DNA damage creates mutations in oncogenes and tumor suppressor genes, initiating malignant transformation [32].
- Signal transduction activation: Moderate ROS levels activate growth-promoting signaling pathways including MAPK, PI3K/AKT, and NF-κB, driving cellular proliferation and survival [32].
- Hypoxia response: ROS stabilize hypoxia-inducible factor-1α (HIF-1α), promoting angiogenesis and metabolic adaptation in tumors [32].
- Epithelial-mesenchymal transition (EMT): Oxidative stress promotes EMT, enhancing invasive and metastatic potential [30].
Cancer cells typically exhibit elevated basal ROS levels compared to normal cells, creating a dependency on adaptive antioxidant responses. This vulnerability can be therapeutically exploited through ROS-inducing agents or inhibition of antioxidant systems in cancer cells.
The Oxidation-Inflammation Circuit in Chronic Disease
The interplay between oxidative stress and inflammation creates a self-amplifying cycle that drives the pathogenesis of numerous age-related conditions. This "oxi-inflamm-aging" circuit operates through several mechanisms:
- NF-κB activation: ROS activate the NF-κB pathway, a master regulator of inflammatory gene expression, leading to production of cytokines (TNF-α, IL-1β, IL-6) that further stimulate ROS production [30] [34].
- NLRP3 inflammasome activation: Oxidative stress triggers assembly of the NLRP3 inflammasome, resulting in caspase-1 activation and maturation of pro-inflammatory cytokines IL-1β and IL-18 [34].
- Immune cell infiltration: Inflammatory mediators recruit immune cells that produce additional ROS and RNS, perpetuating the cycle [35].
This oxidation-inflammation connection is particularly evident in diabetic vascular complications, where hyperglycemia-induced oxidative stress and chronic inflammation synergistically drive both microvascular and macrovascular pathology [34].
Quantitative Biomarker Analysis and Methodologies
Established Oxidative Stress Biomarkers
Reliable quantification of oxidative stress biomarkers is essential for both research and clinical applications. The table below summarizes key biomarkers, their analytical methods, and disease associations:
Table 1: Oxidative Stress Biomarkers and Detection Methodologies
| Biomarker Category | Specific Biomarker | Detection Methods | Clinical/Disease Associations |
|---|---|---|---|
| Lipid Peroxidation | Malondialdehyde (MDA) | TBARS assay, HPLC | Cardiovascular disease, cancer, aging [30] |
| 4-Hydroxy-2-nonenal (4-HNE) | Immunohistochemistry, GC-MS | Neurodegenerative diseases, atherosclerosis [30] | |
| F2-Isoprostanes | GC-MS, ELISA | Oxidative stress status in various diseases [30] | |
| Protein Oxidation | Protein Carbonyls (PC) | DNPH derivatization, Western blot, ELISA | Aging, neurodegenerative diseases, diabetes, HIV [30] [33] |
| Nitrotyrosine (NT) | Immunohistochemistry, ELISA | Inflammatory conditions, cardiovascular diseases [30] | |
| Advanced Glycation End Products (AGEs) | ELISA, HPLC, skin autofluorescence | Diabetes, renal failure, Alzheimer's disease [33] | |
| DNA Oxidation | 8-OHdG/8-oxodG | HPLC-EC, ELISA, LC-MS/MS | Cancer, aging, neurodegenerative disorders [30] [36] |
| Antioxidant Capacity | SOD, CAT, GPx activity | Spectrophotometric assays | Various chronic diseases, aging [30] |
| Glutathione (GSH/GSSG) | HPLC, enzymatic recycling assay | Oxidative stress status across pathologies [32] |
Methodological Protocols for Key Biomarkers
Protein Carbonyl Detection via ELISA
Principle: Protein carbonyl groups are derivatized with 2,4-dinitrophenylhydrazine (DNPH), forming stable dinitrophenylhydrazone adducts detected by anti-DNP antibodies.
Procedure:
- Sample Preparation: Isolate proteins from tissue homogenate or plasma via precipitation with 20% trichloroacetic acid (TCA)
- Derivatization: React protein pellet with 10mM DNPH in 2M HCl for 60 minutes at room temperature in the dark
- Washing: Remove excess DNPH by repeated TCA precipitation and washing with ethanol:ethyl acetate (1:1)
- Protein Resuspension: Dissolve final pellet in 6M guanidine hydrochloride
- ELISA Setup: Coat plates with derivatized proteins, incubate with anti-DNP primary antibody, followed by HRP-conjugated secondary antibody
- Quantification: Develop with TMB substrate, measure absorbance at 450nm, interpolate from standard curve [33]
Advantages: High throughput capability, requires small sample volumes (10-20μL plasma), compatible with standard laboratory equipment
8-Hydroxy-2'-Deoxyguanosine (8-OHdG) Quantification
Principle: 8-OHdG, a marker of oxidative DNA damage, can be detected in tissue, blood, or urine using chromatographic or immunoassay methods.
HPLC-ECD Protocol:
- DNA Extraction: Isolate DNA using phenol-chloroform extraction with chelating agents (e.g., deferoxamine) to prevent artifactual oxidation
- Enzymatic Digestion: Digest DNA to nucleosides using nuclease P1 (pH 5.5) and alkaline phosphatase (pH 7.4)
- Chromatographic Separation: Inject onto C18 reverse-phase column with isocratic elution (10% methanol in 50mM sodium phosphate buffer, pH 5.5)
- Detection: Quantify using electrochemical detector (oxidative mode: +600mV) with UV detection at 260nm for deoxyguanosine
- Calculation: Express results as 8-OHdG/10⁶ deoxyguanosine [32]
Clinical Utility: Elevated in various cancers including breast cancer, with levels potentially declining in advanced stages suggesting adaptive responses [32]
Experimental Workflow for Oxidative Stress Analysis
The following diagram illustrates a comprehensive experimental workflow for profiling oxidative stress status in biological systems, integrating multiple analytical approaches:
Therapeutic Implications and Research Applications
Targeting Oxidative Stress in Age-Related Diseases and Cancer
Therapeutic strategies targeting oxidative stress pathways include:
- Direct antioxidant administration: Supplementation with compounds such as vitamins C and E, N-acetylcysteine, and polyphenols to bolster endogenous defenses [30] [29].
- Indirect antioxidant approaches: Activation of transcription factors like Nrf2 that regulate multiple antioxidant gene networks [34].
- Senolytics: Compounds that selectively eliminate senescent cells, reducing SASP-mediated tissue damage [31].
- Metabolic modulators: Agents that improve mitochondrial function and reduce electron leakage, such as metformin and SGLT2 inhibitors [34].
- Combination with conventional therapies: Antioxidants as adjuvants to reduce side effects of chemotherapy or radiotherapy, though timing must be carefully considered to avoid interfering with ROS-mediated therapeutic mechanisms [32].
In cancer therapy, the pro-oxidant approach represents an alternative strategy that exploits the elevated basal ROS state of many cancer cells. By further increasing ROS production or inhibiting adaptive antioxidant responses, these therapies can push cancer cells beyond their redox capacity, triggering cell death [32].
Research Reagent Solutions
Table 2: Essential Research Reagents for Oxidative Stress Studies
| Reagent Category | Specific Examples | Research Application | Technical Notes |
|---|---|---|---|
| ROS Detection Probes | DCFH-DA, DHE, MitoSOX | Cellular ROS measurement by flow cytometry or microscopy | Validate specificity for particular ROS; consider compartmentalization (e.g., MitoSOX for mitochondrial superoxide) |
| Antioxidant Assay Kits | SOD, CAT, GPx activity assays | Quantifying antioxidant enzyme activities | Use appropriate controls; ensure linear range of assay; consider isoform-specific assays |
| Oxidative Damage Kits | Protein carbonyl ELISA, Lipid peroxidation (MDA) assays | Quantifying specific macromolecular damage | Include protein quantification normalization for protein carbonyls |
| DNA Damage Detection | 8-OHdG ELISA, Comet assay kits | Assessing oxidative DNA lesions | Use antioxidant during DNA extraction to prevent artifactual oxidation |
| Nrf2 Pathway Modulators | Sulforaphane, Bardoxolone methyl | Activating antioxidant response element | Confirm target engagement via gene expression of NQO1, HO-1 |
| ROS-Generating Systems | Menadione, Antimycin A, Tert-butyl hydroperoxide | Inducing controlled oxidative stress | Titrate concentration carefully; monitor cell viability concurrently |
| Specialized Assays | GSH/GSSG ratio kits, Fox assay for H₂O₂ | Assessing redox status and specific oxidants | Process samples rapidly for GSH/GSSG to prevent oxidation |
Oxidative stress serves as a critical biological nexus connecting fundamental aging processes with the pathogenesis of diverse age-related diseases and cancer. The molecular mechanisms through which reactive species mediate cellular damage, activate inflammatory pathways, and drive both senescence and carcinogenesis represent promising targets for therapeutic intervention. While significant progress has been made in characterizing oxidative stress biomarkers and understanding their pathophysiological roles, challenges remain in translating this knowledge into effective clinical therapies. Future research directions should focus on developing tissue-specific antioxidant delivery systems, precisely timing pro- and antioxidant approaches in cancer therapy, and identifying personalized oxidative stress profiles that can guide therapeutic decisions. The continued refinement of analytical methodologies and development of targeted interventions hold promise for breaking the connection between oxidative stress and chronic disease progression, potentially extending healthspan and improving outcomes for age-related conditions and cancer.
From Bench to Biomarker: Quantifying Oxidative Stress and Assessing Therapeutic Interventions
Oxidative stress, defined as a disturbance in the prooxidant-antioxidant balance in favor of the former, leads to disruption of redox signaling and molecular damage [37]. This biochemical phenomenon represents a common pathophysiological mechanism in numerous chronic diseases, including cardiovascular, neurodegenerative, and inflammatory disorders [38]. The interplay between oxidative stress and inflammation establishes a synergistic pathogenic loop that sust chronic disease progression, with reactive oxygen species (ROS) activating redox-sensitive transcription factors such as NF-κB, which subsequently upregulates pro-inflammatory cytokine expression [3]. This "excito-oxidative" damage is particularly detrimental in tissues with high oxygen consumption and unsaturated fatty acid content, such as the brain [39]. To quantitatively assess oxidative damage in research and clinical settings, several validated biomarkers have emerged that target the three major macromolecular targets of ROS: lipids, proteins, and DNA.
Lipid Peroxidation Biomarkers
Malondialdehyde (MDA)
Malondialdehyde (MDA) is a ketoaldehyde produced as an end product of polyunsaturated fatty acid peroxidation [40]. It represents one of the most widely used biomarkers of lipid peroxidation due to its ease of measurement via the thiobarbituric acid-reactive substances (TBARS) assay, which forms a red pigmentation measurable by spectrophotometry [40]. Elevated MDA levels are associated with smoking, atherosclerosis progression, and predict future cardiovascular events in patients with coronary artery disease [40]. However, this biomarker has significant limitations, including low specificity since TBARS measures various lipid peroxidation products beyond MDA, and the potential for artifactual generation during sample preparation and assay conditions [37] [40].
F2-Isoprostanes
F2-Isoprostanes (F2-IsoPs) are prostaglandin-like compounds formed through the non-enzymatic, free radical-mediated peroxidation of arachidonic acid [37]. Discovered by Morrow and Roberts in 1990, F2-IsoPs are considered superior biomarkers of lipid peroxidation due to their chemical stability, specificity for oxidative injury, and presence in detectable levels in all biological fluids and tissues [37] [40]. The isomer 8-iso-PGF2α is most frequently quantified in biological samples as it represents one of the most abundant stereoisomers, though it can be generated through both free-radical and cyclooxygenase-mediated pathways [37]. A systematic meta-analysis across 50 different health conditions revealed that cystic fibrosis, pulmonary arterial hypertension, chronic renal insufficiency, bronchiectasis, and Rett Syndrome demonstrated the highest levels of oxidative damage as measured by F2-IsoPs, surpassing traditionally associated conditions like cardiovascular disease [37]. Interestingly, cancer exhibited one of the lowest associations with elevated 8-iso-PGF2α levels [37].
Table 1: Comparative Analysis of Lipid Peroxidation Biomarkers
| Biomarker | Formation Pathway | Detection Methods | Advantages | Limitations |
|---|---|---|---|---|
| MDA | End product of PUFA peroxidation | TBARS assay, Spectrophotometry | Inexpensive, technically simple | Low specificity, artifactual generation, measures multiple products |
| F2-Isoprostanes | Free radical-mediated peroxidation of arachidonic acid | GC-MS, LC-MS/MS, ELISA | High specificity, chemical stability, sensitive | Complex formation/metabolism, multiple isomers require careful selection |
| 4-HNE | n-6 fatty acid oxidation | Immunohistochemistry, LC-MS/MS | High cytotoxicity, geographical distribution in tissues | Limited evidence in human newborns |
Methodologies for F2-Isoprostane Quantification
Sample Preparation Protocol:
- Collect biological samples (plasma, urine, tissues) under controlled conditions to prevent artifactual oxidation
- For plasma, add antioxidant agents (e.g., butylated hydroxytoluene) immediately upon collection
- For tissue samples, homogenize in chilled buffer containing antioxidants
- Extract lipids using Folch method (chloroform:methanol, 2:1 v/v)
- Hydrolyze phospholipid-esterified F2-IsoPs using base hydrolysis or enzymatic treatment with phospholipase A2
- Purify via solid-phase extraction (C18 and silica cartridges)
- Derivatize to pentafluorobenzyl esters or trimethylsilyl ethers for GC-MS analysis
Analytical Detection Methods:
- Gas Chromatography-Mass Spectrometry (GC-MS): Considered gold standard; provides structural information and high sensitivity with detection limits in picogram range
- Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS): Emerging preferred method; eliminates need for derivatization, higher throughput capacity
- Enzyme-Linked Immunosorbent Assay (ELISA): Commercial kits available; higher throughput but potentially lower specificity due to antibody cross-reactivity
Protein Oxidation Biomarker: Protein Carbonyls
Formation and Significance
Protein carbonylation represents one of the most prevalent and irreversible oxidative protein modifications, resulting from the direct metal-catalyzed oxidation of amino acid side chains (particularly proline, glutamic acid, lysine, and threonine) or secondary reactions with lipid peroxidation products [38]. This process generates ketone and aldehyde groups that compromise protein stability, enzymatic activity, and metabolic regulation [38]. In the context of inflammation, protein carbonylation in the immature brain manifests as a byproduct of reactive nitrogen species with profound implications for cellular injury and inflammation amplification [39]. Protein carbonylation has emerged as a reliable biomarker due to the relatively early formation and stability of carbonylated proteins, making them suitable for assessing cumulative oxidative damage [41].
Clinical Correlations and Therapeutic Targeting
Research demonstrates that serum protein carbonyl levels significantly associate with clinical parameters in chronic diseases. In end-stage renal disease patients undergoing hemodialysis, elevated protein carbonyl levels correlated with overhydration, nutritional status (albumin, prealbumin, transferrin), sarcopenia, and served as an independent predictor of all-cause mortality [41]. Multivariate analysis revealed that serum protein carbonyl levels (Hazard ratio 2.37), albumin (HR 0.17), prealbumin (HR 0.86), overhydration (HR 2.31), and sarcopenia (HR 2.72) were independent determinants of mortality [41]. Furthermore, protein carbonylation represents a potential therapeutic target, with studies demonstrating that administration of potent antioxidants like cannabidiol reduces cerebral damage, restores neurobehavioral performance, and preserves physiological myelination in models of neonatal brain injury through modulation of protein carbonylation [39].
Protein Carbonyl Detection Methodologies
Sample Preparation and Detection Protocol:
- Sample Collection: Collect serum or plasma using EDTA-containing tubes, process within 2 hours to prevent artifactual oxidation
- Protein Precipitation: Add 20% trichloroacetic acid (TCA) to precipitate proteins, incubate on ice for 15 minutes, centrifuge at 15,000×g for 10 minutes
- Derivatization with DNPH: Incubate protein pellet with 10mM 2,4-dinitrophenylhydrazine (DNPH) in 2M HCl for 1 hour with vortexing every 15 minutes
- Washing: Precipitate proteins with 20% TCA, wash pellet three times with ethanol:ethyl acetate (1:1) to remove free DNPH
- Solubilization: Dissolve protein pellet in 6M guanidine hydrochloride solution, incubate at 37°C for 15 minutes with vortexing
- Spectrophotometric Quantification: Measure absorbance at 370nm, calculate carbonyl content using molar extinction coefficient of 22,000 M⁻¹cm⁻¹
Alternative Methods:
- ELISA-based Detection: Commercial kits (e.g., Zenith Technologies) enable higher throughput with minimum detectability of 20 pmol/mg protein
- Immunoblotting: DNPH-derivatized proteins can be separated by electrophoresis, transferred to membranes, and detected with anti-DNP antibodies
- Redox Proteomics: Combination of 2D electrophoresis, anti-DNP immunodetection, and mass spectrometry identification of specific carbonylated proteins
DNA Oxidation Biomarker: 8-Hydroxy-2'-Deoxyguanosine (8-OHdG)
Mechanism and Biological Significance
8-Hydroxy-2'-deoxyguanosine (8-OHdG), also known as 8-oxo-7,8-dihydro-2'-deoxyguanosine (8-oxodG), represents the most frequently studied and abundant oxidative DNA lesion [42] [43]. This biomarker forms when hydroxyl radicals or singlet oxygen attack the C8 position of deoxyguanosine in DNA, creating a mutagenic lesion that can lead to G:C to T:A transversion mutations during DNA replication if not repaired [43]. The accumulation of 8-OHdG damage in DNA is associated with various pathologies, including neurodegeneration, cancer, aging, and inflammatory conditions [43]. In mammalian cells, 8-OHdG is primarily repaired by 8-oxoguanine DNA glycosylase-1 (OGG1), a key enzyme in the base excision repair pathway [43].
Clinical Applications and Evidence
8-OHdG has been established as a sensitive biomarker for evaluating oxidative DNA damage across diverse clinical contexts. A scoping review of medical radiation exposure found that 8-OHdG serves as a promising biomarker for detecting oxidative damage resulting from ionizing radiation, despite external influencing factors [42]. Studies demonstrate significantly elevated urinary 8-OHdG levels in children undergoing cardiac catheterization (increasing from 17.3 at baseline to 44.4 post-procedure), interventional physicians compared to controls (3.014±1.34 vs. 2.635±1.28), and radiation workers, with the highest levels in interventional radiology personnel (120.29±63.88) [42]. Additionally, chronic low-dose benzene exposure among gasoline station attendants resulted in significantly elevated urinary 8-OHdG levels that strongly correlated with both benzene exposure levels (r=0.377, p<0.001) and job seniority (r=0.312, p<0.01) [44]. Beyond chemical and radiation exposures, 8-OHdG has been investigated as a potential marker of age-related damage accumulation, with studies showing age-dependent increases in oxidized guanine lesions when comparing 21-30 year-old individuals to 81-90 year-old subjects [43].
Table 2: 8-OHdG Detection Methodologies Comparison
| Method | Principle | Sensitivity | Advantages | Limitations |
|---|---|---|---|---|
| LC-MS/MS | Liquid chromatography separation with tandem mass spectrometry | Femtomolar levels | High precision and sensitivity, absolute quantification | Requires DNA isolation, complex standard curve, expensive instrumentation |
| HPLC-ECD | High-performance liquid chromatography with electrochemical detection | ~1-5 fmol | High specificity for oxidized guanines, relatively sensitive | Requires DNA hydrolysis, potential for artifactual oxidation |
| ELISA | Enzyme-linked immunosorbent assay with anti-8-OHdG antibodies | Varies by kit | High throughput, commercially available, no DNA hydrolysis | Potential antibody cross-reactivity, semi-quantitative |
| Immunohistochemistry | Tissue staining with anti-8-OHdG antibodies | N/A | Spatial distribution in tissues, morphological context | Semi-quantitative, variable antibody specificity |
Protocol for 8-OHdG Quantification via ELISA
Sample Preparation:
- Urine Collection: Collect spot urine samples in containers with antioxidants (e.g., 0.1% butylated hydroxytoluene), store at -80°C until analysis
- DNA Extraction (for cellular 8-OHdG): Isolate DNA using phenol-chloroform extraction with chelating agents to prevent artifactual oxidation
- DNA Hydrolysis: Digest DNA to nucleosides using nuclease P1 (for dephosphorylation) and alkaline phosphatase
- Sample Dilution: Dilute urine or DNA hydrolysates in assay buffer to fit standard curve range
ELISA Procedure:
- Coating: Add anti-8-OHdG antibody to 96-well plates, incubate overnight at 4°C
- Blocking: Block nonspecific sites with 1% BSA in PBS for 2 hours at room temperature
- Standard Curve: Prepare 8-OHdG standards in concentration range of 0.1-100 ng/mL
- Sample Incubation: Add standards and samples to wells, incubate for 2 hours at 37°C
- Detection Antibody: Add horseradish peroxidase-conjugated detector antibody, incubate 1 hour at 37°C
- Substrate Reaction: Add TMB substrate, incubate 30 minutes in dark
- Stop Solution: Add stop solution (1M sulfuric acid)
- Measurement: Read absorbance at 450nm, calculate concentrations from standard curve
- Normalization: For urine samples, normalize 8-OHdG values to creatinine concentration
The Researcher's Toolkit: Essential Reagents and Materials
Table 3: Essential Research Reagents for Oxidative Damage Biomarker Analysis
| Reagent/Material | Application | Function/Purpose | Technical Notes |
|---|---|---|---|
| Butylated Hydroxytoluene (BHT) | Sample collection for all biomarkers | Antioxidant preservative | Prevents artifactual oxidation during sample processing; add to collection tubes (0.1-0.5%) |
| Thiobarbituric Acid (TBA) | MDA-TBARS assay | Reacts with MDA to form colored adduct | Specific for MDA measurement; measure absorbance at 532-535nm |
| DNPH (2,4-dinitrophenylhydrazine) | Protein carbonyl assay | Derivatization of carbonyl groups | Forms hydrazone derivatives measurable at 370nm; use fresh solution in 2M HCl |
| Anti-8-OHdG Antibody | 8-OHdG ELISA/IHC | Specific recognition of oxidized guanine | Validate specificity with competitive assays; check cross-reactivity with normal nucleosides |
| C18/Silica Solid-Phase Extraction Cartridges | F2-IsoP purification | Sample cleanup and concentration | Remove interfering substances before MS analysis; condition with methanol before use |
| Nuclease P1 & Alkaline Phosphatase | DNA hydrolysis for 8-OHdG | DNA digestion to nucleosides | Essential step for LC-MS/MS or ELISA of cellular 8-OHdG; include antioxidant in digestion buffer |
| Deuterated Internal Standards (d4-8-iso-PGF2α) | F2-IsoP quantification by MS | Internal standardization | Correct for recovery and matrix effects; essential for accurate quantification |
| Protein Carbonyl ELISA Kit | High-throughput protein carbonyl detection | Commercial assay system | Includes pre-coated plates, standards, detectors; check detection limit (~20 pmol/mg) |
The validated biomarkers of oxidative damage—MDA and F2-isoprostanes for lipid peroxidation, protein carbonyls for protein oxidation, and 8-OHdG for DNA oxidation—provide complementary insights into the molecular mechanisms linking oxidative stress with inflammation in chronic diseases. Each biomarker offers unique advantages and limitations, with selection depending on specific research questions, sample availability, and technical capabilities. The interplay between these biomarkers creates a comprehensive picture of oxidative damage across cellular components, reflecting the integrated nature of redox imbalance in disease pathogenesis. As research advances, simultaneous measurement of multiple biomarkers through validated protocols will enhance our understanding of the temporal sequence of oxidative events in chronic inflammatory diseases and facilitate development of targeted antioxidant therapies tailored to specific oxidative damage profiles.
Oxidative stress (OS) arises from an imbalance between reactive oxygen species (ROS) and the body's antioxidant defenses, leading to molecular damage and dysregulation of redox signaling pathways [45] [46]. This state is intricately linked with chronic inflammation, creating a self-perpetuating cycle that contributes to the pathogenesis of a wide range of conditions, including hypertension (HTN), diabetes mellitus (DM), neurodegenerative diseases, and cancer [45] [47] [46]. Under physiological conditions, redox homeostasis is maintained by endogenous antioxidant systems, such as the NRF2 pathway, which upregulates enzymes like superoxide dismutase (SOD), catalase, and glutathione peroxidase (GPx) [46]. However, chronic metabolic dysregulation, as seen in HTN and DM, exacerbates ROS production from sources like NADPH oxidases (NOXs) and dysfunctional mitochondria, overwhelming these defenses [45].
The ensuing oxidative damage to lipids, proteins, and DNA, coupled with aberrant redox signaling, promotes endothelial dysfunction, insulin resistance, and end-organ damage [45]. Consequently, the accurate measurement of OS and its downstream effects is paramount for understanding disease mechanisms and developing targeted therapies. This whitepaper provides an in-depth technical guide to three advanced analytical techniques—HPLC-MS/MS, EPR spectroscopy, and redox proteomics—that are indispensable for dissecting the complex interplay between oxidative stress and inflammation in chronic disease research.
High-Performance Liquid Chromatography-Tandem Mass Spectrometry (HPLC-MS/MS)
Core Principles and Technical Advantages
HPLC-MS/MS combines the superior separation power of high-performance liquid chromatography with the exquisite sensitivity and specificity of tandem mass spectrometry. This technique is particularly suited for the identification and quantification of specific, stable oxidative stress biomarkers in complex biological matrices such as plasma, urine, and tear fluid [48] [49] [50]. Its primary advantage lies in its ability to simultaneously measure multiple biomarkers across different molecular pathways, providing a comprehensive snapshot of the redox status in a single, high-throughput analysis [50].
Key Biomarkers and Analytical Methodologies
Table 1: Key Oxidative Stress Biomarkers Quantifiable by HPLC-MS/MS
| Biomarker Category | Specific Biomarker | Significance in Oxidative Stress & Disease | Representative Matrix |
|---|---|---|---|
| Lipid Peroxidation | F2-isoprostanes [45] [48] | Golden standard; stable end-products of arachidonic acid peroxidation; correlate with HTN/DM severity [45] [48]. | Plasma, Serum |
| DNA Oxidation | 8-Hydroxy-2'-deoxyguanosine (8-OHdG) [45] [49] | Reflects oxidative damage to guanine in DNA; surrogate marker for diabetic nephropathy [45]. | Urine, Amniotic Fluid |
| Protein Oxidation | 3-Nitrotyrosine (3-NO2-Tyr) [47] [49] | Indicates protein modification by reactive nitrogen species; implicated in neurodegeneration [47]. | Plasma, Tear Fluid, Tissues |
| o-Tyrosine, 3-Chlorotyrosine [49] | Specific markers of free radical damage and myeloperoxidase activity, respectively [47] [49]. | Amniotic Fluid | |
| Thiol Redox Status | Glutathione (GSH)/Glutathione Disulfide (GSSG) [50] | Primary endogenous antioxidant; GSH/GSSG ratio is a sensitive indicator of cellular redox balance [50]. | Tear Fluid, Serum, Tissues |
| Cysteine (Cys)/Cystine (CySS) [50] | Plasma redox couple; shifting to more oxidized state with aging and disease [47] [50]. | Plasma, Tear Fluid |
Detailed Experimental Protocol for Thiol Metabolite Analysis
The following protocol, adapted from a study analyzing thiols in human tear fluid, exemplifies a robust HPLC-MS/MS workflow [50].
Sample Collection and Preparation:
- Collect biological fluid (e.g., tear fluid using Schirmer test strips). Record the wetted length of the strip and interpolate the fluid volume using a pre-established calibration curve (e.g., volume = 0.88 × length (mm) + 1.77) [50].
- Place the strip in a molecular weight cut-off (MWCO) filter unit. Extract metabolites by adding a suitable solvent (e.g., 500 µL of 0.01% formic acid in water) and incubating at 4°C for 15 minutes.
- Centrifuge the filter unit at 13,000 × g for 30 minutes at 4°C. Repeat the extraction and combine the filtrates.
Chromatographic Separation:
- Column: Use a reversed-phase column (e.g., Phenomenex HydroRP, 4 µm, 250 × 2.0 mm).
- Mobile Phases: (A) 0.01% formic acid in water; (B) 0.01% formic acid in acetonitrile.
- Gradient: Initiate at 100% A for 1 min, ramp to 30% B by 4 min, then to 60% B by 5 min. Hold for 1 min before re-equilibrating to initial conditions. A flow rate of 0.3 mL/min and column temperature of 40°C are typical [50].
Mass Spectrometric Detection:
- Ion Source: Electrospray Ionization (ESI) in positive mode.
- Detection: Multiple Reaction Monitoring (MRM). Key MS/MS parameters for specific thiols are listed below.
- Data Analysis: Quantify analytes using internal standard calibration and normalized peak areas.
Table 2: Example MRM Transitions for Key Thiol Metabolites [50]
| Analyte | Q1 Mass (m/z) | Q3 Mass (m/z) | Retention Time (min) |
|---|---|---|---|
| Glutathione (GSH) | 308.1 | 76.1, 162.0 | ~2.1 |
| Cysteine (Cys) | 122.0 | 76.0, 59.0 | ~2.2 |
| Cystine (CySS) | 241.0 | 120.0, 74.0 | ~2.8 |
| Homocysteine | 136.0 | 90.0, 73.0 | ~2.2 |
| Methionine | 150.1 | 104.0, 56.0 | ~3.5 |
| Creatinine | 114.1 | 86.1, 44.1 | ~2.3 |
Electron Paramagnetic Resonance (EPR) Spectroscopy
Core Principles and Direct Detection Capabilities
Unlike HPLC-MS/MS, which measures stable end-products, Electron Paramagnetic Resonance (EPR) spectroscopy, also known as Electron Spin Resonance (ESR), is a powerful technique for the direct detection and quantification of paramagnetic species, most notably free radicals with unpaired electrons [51] [52] [53]. The fundamental principle involves applying a magnetic field to a sample, which causes the energy levels of unpaired electrons to split (Zeeman effect). Resonant absorption of microwave radiation occurs when the energy of the incident photons matches the energy separation, providing a characteristic spectrum for the radical species [51].
Key Methodologies and Applications in Disease Research
Spin Trapping: This is a critical methodology for investigating short-lived radical species (e.g., hydroxyl •OH, superoxide O2•−). Spin traps (e.g., DMPO, PBN) are diamagnetic compounds that react rapidly with transient radicals to form more stable, paramagnetic spin adducts, which can then be detected by EPR, allowing for both identification and quantification of the original radical [51]. This technique has been used to identify elevated superoxide in the glomeruli and tubules of diabetic rodents, correlating with albuminuria [45].
In Vivo EPR and Oximetry: EPR can be applied to live animals or tissues to measure real-time redox status and physiological parameters. EPR oximetry uses oxygen-sensitive paramagnetic probes to measure tissue oxygen concentration (pO2), a key variable in ischemia, tumors, and inflammation [51]. Multi-frequency EPR spectrometers (e.g., L-band at 1-2 GHz) are designed for use with aqueous samples and living systems [51].
Detailed Experimental Protocol for Spin Trapping
This protocol outlines the steps for detecting superoxide radicals in a biological sample [51].
Preparation of Spin Trap Solution: Dissolve an appropriate spin trap (e.g., DMPO) in a suitable buffer (e.g., phosphate-buffered saline) at a concentration of 50-100 mM. Purify the stock solution if necessary to remove contaminating radicals.
Sample Incubation:
- In a biological system (e.g., isolated mitochondria, activated neutrophils), initiate superoxide production (e.g., by adding a substrate or agonist).
- Immediately add the spin trap solution to the reaction mixture and mix thoroughly. The final concentration of the spin trap should be sufficient to compete with other reaction pathways.
EPR Measurement:
- Transfer the mixture to a quartz EPR flat cell suitable for aqueous solutions.
- Insert the cell into the cavity of the EPR spectrometer. Typical settings for X-band (∼9.5 GHz) spectroscopy might be: modulation frequency of 100 kHz, modulation amplitude of 1 G, microwave power of 20 mW, and a scan time of 60 seconds.
- Record the spectrum. The hyperfine splitting pattern of the resulting spin adduct (e.g., DMPO-OOH for superoxide) is characteristic and allows for radical identification.
Redox Proteomics
Core Principles and Biological Significance
Redox proteomics is a specialized branch of proteomics that focuses on the system-wide identification, characterization, and quantification of post-translational modifications (PTMs) induced by ROS and RNS on proteins [47]. This approach moves beyond measuring global oxidative damage to pinpointing specific functional consequences of oxidative stress, such as the alteration of enzymatic activity, protein-protein interactions, and signaling pathways [47] [46]. Cysteine (Cys) and methionine (Met) residues are primary targets due to the high reactivity of their sulfur-containing side chains.
Key Redox Modifications and Analytical Strategies
Table 3: Major Protein Oxidative Modifications Studied in Redox Proteomics
| Modification Type | Chemical Change | Biological Significance & Detection |
|---|---|---|
| Reversible Modifications | ||
| S-Sulfenylation (SOH) | Formation of sulfenic acid on Cys | Serves as a redox sensor and signaling intermediate; can be probed with dimedone-based reagents [47]. |
| S-Glutathionylation (SSG) | Mixed disulfide with glutathione (GSH) | Protects Cys from overoxidation; regulates protein function under oxidative stress [47] [46]. |
| S-Nitrosylation (SNO) | Addition of nitric oxide moiety to Cys | Key signaling mechanism mediated by reactive nitrogen species; detected by biotin-switch techniques [47]. |
| Irreversible Modifications | ||
| Carbonylation | Introduction of carbonyl groups (ketone/aldehyde) on Lys, Arg, Pro | Marker of severe oxidative damage; detected by derivatization with DNPH and immunoblotting/LC-MS [45] [47]. |
| Tyrosine Nitration | Addition of nitro group to Tyr ring (3-NO2-Tyr) | Disrupts protein structure/function; implicated in neurodegenerative diseases; detected by specific antibodies or LC-MS/MS [47] [49]. |
| Histidine & Lysine Adduction | Michael addition with lipid peroxidation products (e.g., 4-HNE) | Links lipid peroxidation to protein dysfunction; detected by LC-MS/MS [47]. |
Detailed Experimental Protocol for Redox Proteome Analysis
A common workflow involves enriching for redox-modified proteins or peptides before analysis by LC-MS/MS.
Sample Lysis and Protein Extraction:
- Lyse tissues or cells in a lysis buffer containing alkylating agents (e.g., iodoacetamide, N-ethylmaleimide) to rapidly block free thiols and "freeze" the native redox state, preventing artificial oxidation during preparation.
Enrichment of Redox-Modified Proteins/Peptides:
- For a specific modification like S-nitrosylation, the Biotin-Switch Technique (BST) is often used [47].
- Block: Block free thiols with methyl methanethiosulfonate (MMTS).
- Reduce: Selectively reduce S-nitrosylated thiols to free thiols using ascorbate.
- Label: Label the newly formed thiols with a biotin-conjugated thiol-reactive reagent (e.g., biotin-HPDP).
- Capture: Capture the biotinylated proteins on streptavidin beads, wash thoroughly, and elute for analysis.
Proteomic Analysis:
- Perform on-bead or in-solution digestion of the enriched proteins using trypsin.
- Analyze the resulting peptides using LC-MS/MS (typically on a high-resolution instrument).
- Use database search engines (e.g., MaxQuant, Proteome Discoverer) to identify proteins and sites of modification.
Research Reagent Solutions
Table 4: Essential Reagents and Materials for Featured Techniques
| Reagent/Material | Function/Application | Example in Context |
|---|---|---|
| Schirmer Test Strips | Non-invasive collection of tear fluid for biomarker analysis [50]. | Collection of human tear fluid for HPLC-MS/MS analysis of thiol metabolites [50]. |
| Spin Traps (DMPO, PBN) | Diamagnetic compounds that form stable adducts with short-lived radicals for EPR detection [51]. | Detection of superoxide (O2•−) radicals in a model of diabetic nephropathy [45] [51]. |
| Biotin-HPDP | Thiol-reactive biotinylation reagent used for labeling and enriching redox-modified proteins [47]. | Labeling of S-nitrosylated cysteine residues in the Biotin-Switch Technique for redox proteomics [47]. |
| Deuterated Internal Standards | Isotope-labeled analogs of analytes used for precise quantification in mass spectrometry [48] [50]. | Quantification of F2-isoprostanes and prostanoids in serum and tissue samples via UHPLC-MS/MS [48]. |
| Anti-DNP Antibodies | Antibodies specific for dinitrophenylhydrazone (DNP) derivatives of protein carbonyls [45]. | Detection of protein carbonylation, a marker of irreversible oxidative damage, via ELISA or immunoblotting [45] [47]. |
| Molecular Weight Cut-Off (MWCO) Filters | Ultrafiltration devices for removing high molecular weight matrix components and concentrating analytes [50]. | Sample preparation for tear fluid analysis; removes proteins and other large molecules prior to HPLC-MS/MS [50]. |
Integrated Workflow for Chronic Disease Research
The true power of these analytical techniques is realized when they are integrated to provide a multi-faceted view of oxidative stress and inflammation. For instance, in a study of hypertension and diabetes comorbidity [45]:
- EPR spectroscopy can directly quantify superoxide production in vascular tissue, identifying NOX and mitochondrial complexes as primary sources.
- HPLC-MS/MS can then be used to measure stable downstream biomarkers in plasma or urine, such as elevated F2-isoprostanes (lipid peroxidation) and 8-OHdG (DNA damage), which correlate with disease severity and end-organ complications.
- Redox proteomics can identify specific functional consequences, such as the nitration of key mitochondrial proteins or S-glutathionylation of signaling molecules, linking oxidative insult to metabolic and vascular dysfunction.
This integrated data provides a mechanistic framework for understanding disease progression and identifies specific targets for novel antioxidant therapies, such as mitochondria-targeted antioxidants (MitoQ) or Nrf2 activators, moving beyond the limitations of broad-spectrum antioxidants [45] [46].
Oxidative stress and chronic inflammation are deeply interconnected pathological processes that serve as critical drivers in the pathogenesis and progression of numerous chronic diseases [54] [55]. This destructive synergy creates a self-reinforcing cycle wherein reactive oxygen species (ROS) activate pro-inflammatory signaling pathways, while inflammatory mediators, in turn, stimulate further ROS production [55]. This vicious cycle establishes a persistent pathological microenvironment that contributes to conditions ranging from cancers, cardiovascular diseases, and neurodegenerative disorders to autoimmune conditions [54] [2] [56].
Within this context, targeting the redox-inflammatory axis has emerged as a promising therapeutic strategy. Research has focused on both natural products—including flavonoids and cordycepin—and synthetic compounds with antioxidant and anti-inflammatory properties [57] [55]. However, translating promising compounds into clinical applications requires rigorous preclinical evaluation using models that accurately recapitulate disease pathophysiology. This guide provides a comprehensive technical overview of current methodologies, experimental protocols, and key considerations for evaluating such compounds in preclinical models relevant to oxidative stress and inflammation.
Natural Products in Preclinical Research
Flavonoids: Multi-Target Polyphenolic Compounds
Flavonoids represent a large class of polyphenolic compounds abundantly found in fruits, vegetables, grains, and plant-derived beverages [54]. Six major flavonoid subgroups have demonstrated significant dietary relevance: anthocyanidins (e.g., pelargonidin, cyanidin), flavan-3-ols (e.g., epicatechin, epigallocatechin), flavonols (e.g., quercetin, kaempferol), flavones (e.g., luteolin, baicalein), flavanones (e.g., hesperetin, naringenin), and isoflavones (daidzein, genistein) [54] [56].
The therapeutic benefits of flavonoids are closely linked to their distinctive structural characteristics, particularly the number and position of hydroxyl groups and the presence of C2=C3 double bonds. These structural features enable flavonoids to chelate metal ions, terminate ROS (e.g., hydroxyl radicals formed by the Fenton reaction), and interact with specific biological targets to elicit therapeutic responses [54] [56]. Beyond their direct antioxidant activities, flavonoids modulate complex cellular processes by influencing the activity of ROS-scavenging enzymes, regulating the expression and activation of proinflammatory cytokines (e.g., IL-1β, IL-6, and TNF-α), inducing apoptosis and autophagy, and targeting key signaling pathways such as the nuclear factor erythroid 2-related factor 2 (Nrf2) and Bcl-2 family of proteins [54] [56].
Table 1: Preclinical Evidence for Selected Natural Products in Oxidative Stress and Inflammation Models
| Compound | Disease Model | Key Findings | Proposed Mechanisms | References |
|---|---|---|---|---|
| Cordycepin | Renal Ischemia-Reperfusion Injury (Mouse) | Alleviated histological damage, reduced inflammation, apoptosis, and ferroptosis | Suppressed p38/JNK signaling pathway; decreased IL-6, TNF-α, IL-1β | [58] |
| Cordycepin | Excessive Exercise-Induced Fatigue (Mouse) | Enhanced exercise endurance, reduced fatigue metabolites, improved learning/memory | Modulated Keap1/Nrf2/HO-1 pathway; enhanced BDNF levels | [59] |
| Cordyceps Sinensis Extract (CSE) | LPS-Induced Inflammation (Human THP-1 Macrophages) | Inhibited pro-inflammatory cytokines (IL-6, TNF-α, IL-8, IL-1β); reduced ROS | Upregulated Nrf2/HO-1 pathway; suppressed NF-κB translocation | [60] |
| Cordyceps Militaris Extract (CME) | LPS-Induced Colonic Damage (Piglet) | Attenuated intestinal morphology damage, improved gut microbiota | Enriched beneficial bacteria (e.g., Prevotella); modulated tryptophan metabolism | [61] |
| Quercetin (Flavonoid) | In Vitro LPS-Stimulated Human Lung Epithelial Cells | Downregulated NOX2-derived ROS, suppressed inflammatory signaling | Inhibited MAPK and NF-κB pathways | [55] |
Cordycepin and Cordyceps Extracts: Fungal-Derived Bioactives
Cordycepin (3'-deoxyadenosine), a primary bioactive nucleoside isolated from the fungus Cordyceps sinensis, has demonstrated significant therapeutic potential across diverse preclinical models [59] [58]. This compound exhibits a broad spectrum of biological activities, including anti-inflammatory, antioxidant, neuroprotective, and anti-fatigue effects [59] [61].
The mechanistic actions of cordycepin are pleiotropic, influencing multiple signaling pathways. Research indicates it can activate the AMPK signaling pathway, modulate the GSK-3β-Nrf2 pathway, and inhibit the PI3K/Akt/mTOR and p38/JNK pathways, depending on the disease context [58]. Similarly, extracts of Cordyceps sinensis (CSE) and Cordyceps militaris (CME) contain complex mixtures of bioactive components—including nucleosides, polysaccharides, sterols, proteins, and peptides—that contribute to their therapeutic effects through complementary mechanisms [60] [61].
Synthetic and Semi-Synthetic Antioxidants
While natural products offer diverse chemical scaffolds, synthetic and semi-synthetic antioxidants represent a complementary approach with potential advantages in terms of target specificity, pharmacokinetic properties, and controlled biosynthesis [57]. These compounds can be categorized into: (i) those primarily developed and synthesized as antioxidants, and (ii) compounds whose primary mechanism of action differs from their secondary antioxidant properties [57].
Promising synthetic agents include Ebselen (a glutathione peroxidase mimetic and NOX inhibitor), Edaravone (a free radical scavenger), MitoQ10 (a mitochondrial-targeted antioxidant), and N-acetylcysteine (a precursor to glutathione) [57]. Additionally, significant research efforts have focused on developing superoxide dismutase (SOD)/catalase mimetics, which are low-molecular compounds containing transition metals (e.g., manganese, iron, copper, or zinc) that mimic the activity of endogenous antioxidant enzymes [57].
A significant challenge in the field is that many synthetic antioxidants have failed to demonstrate clear therapeutic benefits in clinical trials, despite promising preclinical data. This translational gap may result from several factors, including insufficient dosage to elicit an antioxidant effect in vivo, poor oral bioavailability, a narrow therapeutic index, or toxicity that precludes clinical use [57]. Furthermore, the therapeutic benefits of some compounds may result from non-antioxidant mechanisms, highlighting the need for careful mechanistic studies.
Experimental Protocols for Preclinical Evaluation
In Vitro Model: Evaluating Anti-Inflammatory Effects in Macrophages
Objective: To assess the effects of test compounds on LPS-induced oxidative stress and inflammatory responses in THP-1 human macrophages [60].
Key Reagent Solutions:
- THP-1 Cells: Human monocytic cell line (can be differentiated into macrophages using PMA).
- LPS: Used to induce inflammatory activation (typically at 100-1000 ng/mL).
- Test Compound: e.g., Cordyceps sinensis extract (CSE) or pure compounds.
- DCFH-DA Fluorescent Probe: Cell-permeable dye to measure intracellular ROS.
- JC-1 Dye: Fluorescent probe for assessing mitochondrial membrane potential.
- ELISA Kits: For quantifying pro-inflammatory cytokines (TNF-α, IL-1β, IL-6, IL-8).
- Antibodies for Western Blot: For analyzing protein expression (e.g., Nrf2, HO-1, MMP9).
Methodology:
- Cell Culture and Differentiation: Maintain THP-1 monocytes in RPMI-1640 medium with 10% FBS. Differentiate into macrophages using 100 ng/mL PMA for 48 hours [60].
- Cell Viability Assessment (CCK-8 Assay): Seed differentiated THP-1 macrophages in 96-well plates. Treat with varying concentrations of test compound (e.g., CSE: 0.1-100 μg/mL) for 24 hours. Add CCK-8 reagent (10% v/v) and incubate for 2 hours. Measure absorbance at 450 nm to determine non-cytotoxic concentrations for subsequent experiments [60].
- Compound Treatment and LPS Challenge: Pre-treat cells with test compound for a predetermined time (e.g., 2-4 hours), then stimulate with LPS (e.g., 1 μg/mL) for an additional specified period (e.g., 6-24 hours) [60].
- ROS Measurement: Load cells with 10 μM DCFH-DA in serum-free medium for 30 minutes. After LPS challenge, measure fluorescence (Ex/Em: 488/525 nm) using a plate reader. Calculate percentage reduction in ROS compared to LPS-only controls [60].
- Mitochondrial Membrane Potential Assessment: Stain cells with 5 μg/mL JC-1 for 20 minutes. Measure red/green fluorescence ratio (Ex/Em: 488/590 nm vs 488/530 nm). A decreased ratio indicates mitochondrial depolarization [60].
- Cytokine Quantification: Collect cell culture supernatants. Quantify levels of TNF-α, IL-1β, IL-6, and IL-8 using commercial ELISA kits according to manufacturers' protocols [60].
- Protein Expression Analysis: Extract total proteins using RIPA buffer. Perform Western blotting to assess expression of targets such as Nrf2, HO-1, and MMP9 [60].
- Transcriptomic Analysis (Optional): For comprehensive mechanistic insights, extract total RNA for RNA sequencing. Identify differentially expressed genes and perform GO and KEGG pathway enrichment analyses [60].
In Vivo Model: Exercise-Induced Fatigue and Oxidative Stress
Objective: To evaluate the anti-fatigue and antioxidant effects of compounds (e.g., cordycepin) in a mouse model of forced excessive exercise [59].
Key Reagent Solutions:
- Experimental Animals: Male Kunming mice (6 weeks old).
- Forced Treadmill: Equipped with electric stimulus grid.
- Test Compound: e.g., Cordycepin (dissolved in saline for oral administration).
- Biochemical Assay Kits: For lactic acid (LA), blood urea nitrogen (BUN), lactate dehydrogenase (LDH), creatine kinase (CK), superoxide dismutase (SOD), malondialdehyde (MDA), liver glycogen (LG), muscle glycogen (MG).
- ELISA Kits: For neurotransmitters (acetylcholine, glutamate, 5-HTP, GABA) and BDNF.
- Specific Antibodies: For Western blot analysis of Keap1, Nrf2, HO-1.
Methodology:
- Animal Grouping and Drug Administration: Randomly allocate mice to groups (e.g., silent control, excessive exercise model, and exercise + various doses of test compound). Administer compound orally once daily for 22 days (e.g., cordycepin at 5, 10, and 25 mg/kg/day) [59].
- Forced Treadmill Exercise Protocol: Starting on day 16 of administration, subject mice to a 6-day incremental treadmill training protocol: 18 m/min for 2 hours (days 1-2), 25 m/min for 2 hours (days 3-4), and 30 m/min for 2 hours (days 5-6). Exhaustion criterion: inability to maintain running at 30 m/min despite electrical stimulation [59].
- Sample Collection: After the final exercise session, collect blood serum for biochemical analysis. Euthanize animals and rapidly dissect tissues (liver, skeletal muscle, brain) for glycogen measurement, biochemical assays, and molecular analyses [59].
- Biochemical Parameter Analysis: Measure serum levels of LA, BUN, LDH, CK, SOD activity, and MDA using commercial kits according to manufacturers' instructions [59].
- Glycogen Content Measurement: Analyze liver and muscle glycogen content using specific assay kits [59].
- Neurotransmitter and BDNF Analysis: Quantify levels of acetylcholine, glutamate, 5-HTP, GABA, and BDNF in brain tissues using ELISA [59].
- Protein Expression Analysis: Perform Western blot analysis on tissue homogenates to evaluate expression and activation of proteins in the Keap1/Nrf2/HO-1 pathway [59].
- Behavioral Assessment (Y-maze): To assess cognitive function, conduct Y-maze tests to evaluate spatial working memory and spontaneous alternation behavior [59].
Table 2: Key Biochemical Markers for Assessing Oxidative Stress and Inflammation in Preclinical Models
| Marker Category | Specific Marker | Biological Significance | Common Detection Methods |
|---|---|---|---|
| Oxidative Stress | Malondialdehyde (MDA) | End product of lipid peroxidation; indicates oxidative damage | TBARS assay kit |
| Superoxide Dismutase (SOD) | Key antioxidant enzyme; catalyzes superoxide dismutation | Colorimetric activity assay | |
| Reactive Oxygen Species (ROS) | Direct measure of oxidative burden | DCFH-DA fluorescence | |
| Inflammation | TNF-α, IL-6, IL-1β | Key pro-inflammatory cytokines | ELISA, RT-qPCR |
| NF-κB activation | Master regulator of inflammation | Western blot (nuclear fraction), EMSA | |
| Tissue Damage | Creatine Kinase (CK) | Indicator of muscle damage | Serum biochemical analysis |
| Lactate Dehydrogenase (LDH) | Marker of general tissue/cell damage | Serum biochemical analysis | |
| Metabolic Fatigue | Blood Urea Nitrogen (BUN) | Indicator of protein/amino acid metabolism during exercise | Serum biochemical analysis |
| Lactic Acid (LA) | Product of anaerobic metabolism | Serum biochemical analysis | |
| Transcriptional Regulation | Nrf2 Nuclear Translocation | Master regulator of antioxidant response | Western blot, immunofluorescence |
| HO-1 Expression | Nrf2-regulated cytoprotective enzyme | Western blot, RT-qPCR |
Signaling Pathways in Oxidative Stress and Inflammation
The therapeutic effects of natural products and synthetic compounds frequently involve modulation of key signaling pathways that bridge oxidative stress and inflammatory responses. The following diagrams illustrate the primary pathways targeted by these therapeutic interventions.
Nrf2 and NF-κB Pathway Interplay
The Nrf2/ARE and NF-κB pathways represent two critical, interconnected signaling axes that regulate cellular responses to oxidative stress and inflammation, respectively. Natural products like flavonoids and cordycepin often activate the Nrf2 pathway while inhibiting NF-κB signaling, thereby simultaneously enhancing antioxidant defenses and reducing inflammation [55].
Nrf2 Activation by Therapeutic Compounds
The Keap1-Nrf2-ARE pathway serves as a primary cellular defense mechanism against oxidative stress. Under basal conditions, Nrf2 is sequestered in the cytoplasm by its inhibitor Keap1 and targeted for proteasomal degradation. Compounds that modify specific cysteine residues on Keap1 or disrupt the Keap1-Nrf2 interaction promote Nrf2 stabilization and nuclear translocation, where it binds to Antioxidant Response Elements (ARE) and activates the transcription of cytoprotective genes [55].
The preclinical evaluation of natural products and synthetic compounds targeting oxidative stress and inflammation requires a multifaceted approach that integrates in vitro mechanistic studies with physiologically relevant in vivo models. The experimental protocols outlined in this guide provide a framework for generating robust, reproducible data on the efficacy and mechanisms of potential therapeutic agents.
Future directions in this field will likely focus on several key areas: (1) the development of more sophisticated disease models that better recapitulate the chronicity and complexity of human diseases; (2) advanced delivery systems such as nanoparticle-enabled delivery to improve bioavailability and tissue targeting; (3) the application of multi-omics approaches to comprehensively understand system-level responses to interventions; and (4) personalized medicine strategies that consider genetic and environmental factors influencing individual susceptibility to oxidative stress and inflammation [57] [55].
As research continues to elucidate the intricate connections between oxidative stress and inflammation, preclinical models will remain indispensable tools for validating therapeutic targets and accelerating the development of effective interventions for chronic diseases.
Oxidative stress and chronic inflammation are established as fundamental pathological processes in a wide range of chronic diseases, including cardiovascular disorders, neurodegeneration, diabetes, and cancer [62] [2]. These interconnected processes create a self-amplifying vicious cycle: reactive oxygen species (ROS) activate inflammatory signaling pathways, while inflammatory mediators stimulate further ROS production [55]. Within this pathological framework, the Mediterranean Diet (MD) has emerged as a promising non-pharmacological intervention capable of modulating these pathways. Characterized by high consumption of plant-based foods, monounsaturated fats from extra virgin olive oil (EVOO), and moderate fish intake, the MD represents a multi-component approach to combating oxidative stress and inflammation [63]. Recent evidence suggests that a significant portion of the MD's beneficial effects are mediated through its impact on the gut microbiome, positioning gut microbiota modulation as a crucial mechanism in the diet's ability to mitigate chronic disease pathways [63] [64]. This technical review examines the molecular mechanisms through which the MD influences the gut-microbiota-brain/liver axes and synthesizes current clinical and preclinical evidence supporting its role in managing oxidative stress and inflammation.
Molecular Mechanisms of Action
Bioactive Components and Signaling Pathways
The Mediterranean Diet exerts its effects through a diverse array of bioactive compounds that target key oxidative stress and inflammatory pathways. The table below summarizes the primary bioactive components and their molecular targets.
Table 1: Key Bioactive Components in the Mediterranean Diet and Their Molecular Actions
| Bioactive Component | Primary Dietary Sources | Molecular Targets | Biological Effects |
|---|---|---|---|
| Hydroxytyrosol | Extra virgin olive oil | NF-κB, ROS scavenging, antioxidant enzymes [63] | Reduces pro-inflammatory cytokines (IL-6, TNF-α), protects membrane lipids from oxidative damage [63] |
| Oleuropein | Extra virgin olive oil | NF-κB, NO production [63] | Inhibits NF-κB activation, stimulates NO production for vasodilation, activates antioxidant enzymes [63] |
| Omega-3 Fatty Acids | Fatty fish (salmon, mackerel, sardines) | PPARα/γ, inflammatory gene expression [63] | Improves insulin sensitivity, reduces LDL cholesterol, anti-inflammatory effects [63] |
| Polyphenols (Quercetin, Catechin) | Fruits, vegetables, red wine (moderate) | JNK kinase, Nrf2, MAPK, NF-κB [63] [55] | Reduces oxidative stress, improves endothelial function, inhibits lipid peroxidation [63] |
| Fiber | Whole grains, legumes, vegetables | SCFA production, gut barrier integrity [63] | Enhances gut barrier function, reduces systemic inflammation, improves metabolic homeostasis [63] |
The interplay between the NF-κB and Nrf2 signaling pathways represents a central mechanism in the MD's ability to reduce oxidative stress and inflammation. The NF-κB pathway serves as a primary regulator of inflammation, while the Nrf2 pathway coordinates antioxidant defense systems. As illustrated in the diagram below, bioactive compounds in the MD simultaneously inhibit NF-κB activation and promote Nrf2 translocation, creating a synergistic effect that breaks the cycle of oxidative stress and inflammation.
Gut Microbiome Modulation
The gut microbiome serves as a critical interface between dietary components and host physiology. The MD promotes a beneficial microbial ecosystem characterized by increased diversity and abundance of short-chain fatty acid (SCFA)-producing bacteria including Bifidobacterium, Faecalibacterium prausnitzii, and Roseburia [63]. These microbial changes mediate many systemic benefits through several interconnected mechanisms:
- SCFA Production: MD components, particularly dietary fiber, are fermented by gut microbes to produce SCFAs (acetate, propionate, butyrate) that enhance gut barrier integrity, reduce intestinal permeability, and exert systemic anti-inflammatory effects [63] [64].
- Pathogen Inhibition: Beneficial microbes stimulated by the MD competitively exclude pro-inflammatory pathobionts and reduce bacterial translocation [63].
- Immunomodulation: Microbial metabolites regulate immune cell function and differentiation, particularly through T-regulatory cell induction and suppression of pro-inflammatory cytokine production [64].
The gut-liver axis represents a particularly well-characterized pathway for MD-mediated protection. The following diagram illustrates the mechanistic relationship between MD consumption, gut microbiome modulation, and improved hepatic outcomes in metabolic dysfunction-associated steatotic liver disease (MASLD), as demonstrated in recent preclinical models [65].
Quantitative Clinical Evidence
Effects on Inflammatory Biomarkers
Recent meta-analyses of randomized controlled trials (RCTs) provide robust evidence for the anti-inflammatory effects of the Mediterranean Diet. The table below summarizes the impact of MD interventions on specific inflammatory biomarkers based on aggregated clinical data.
Table 2: Mediterranean Diet Effects on Inflammatory Biomarkers from Meta-Analyses
| Biomarker | Population | Number of RCTs/Participants | Effect Size | Statistical Significance | Source |
|---|---|---|---|---|---|
| hs-CRP | Adults with CVD risk | 33 RCTs / 3,476 participants | Significant reduction | p < 0.05 | [66] |
| IL-6 | Adults (< 60 years) | 33 RCTs / 3,476 participants | Significant reduction | p < 0.05 | [66] |
| IL-17 | General adult population | 33 RCTs / 3,476 participants | Significant reduction | p < 0.05 | [66] |
| CRP/hs-CRP | Adults with CVD risk | 15 RCTs / 2,477 participants | SMD: -0.96 (-1.49 to -0.44) | p < 0.05 | [67] |
| IL-6 | Adults with CVD risk | 15 RCTs / 2,477 participants | SMD: -1.85 (-3.69 to -0.01) | p < 0.05 | [67] |
| sICAM-1 | Adults with CVD risk | 15 RCTs / 2,477 participants | SMD: -2.37 (-4.34 to -0.40) | p < 0.05 | [67] |
| TNF-α | Healthy individuals | 65 studies | No significant reduction | p > 0.05 | [68] |
Subgroup analyses reveal that the anti-inflammatory effects of the MD are influenced by specific factors. The most pronounced reductions in IL-6 are observed in participants under 60 years of age, with intervention durations of less than 12 weeks, and in individuals with established cardiovascular disease [66]. This suggests that both population characteristics and intervention parameters significantly influence outcomes.
Impact on Oxidative Stress Markers
The effects of the MD on oxidative stress markers appear more nuanced compared to its anti-inflammatory benefits:
- MDA (Malondialdehyde): Weak association with reduction (ROM: 0.80; 95% CI: 0.57–1.13; p = 0.2092) [68]
- 8OHdG (8-hydroxydeoxyguanosine): Weak association with reduction (ROM: 0.81; 95% CI: 0.59–1.11; p = 0.1847) [68]
The relatively modest effects on classical oxidative stress biomarkers suggest that the MD's benefits may be mediated more through inflammatory pathway modulation and enhancement of endogenous antioxidant defenses rather than direct scavenging of ROS [68]. This highlights the importance of the Nrf2 pathway activation as a key mechanism, rather than merely direct antioxidant activity.
Experimental Models and Methodologies
Preclinical Model of MASLD
Recent research provides a detailed experimental approach for investigating MD mechanisms in metabolic dysfunction-associated steatotic liver disease (MASLD). The protocol below can be adapted for studying various disease models involving oxidative stress and inflammation [65].
Table 3: Experimental Protocol for MASLD Dietary Intervention Study
| Stage | Duration | Groups | Diet Composition | Key Assessments |
|---|---|---|---|---|
| Model Induction | 12 weeks | Control (n=13): Normal chow (NC)Model (n=31): High-fat diet (HFD) | NC: 20% protein, 10% fat, 70% carbsHFD: 20% protein, 60% fat, 20% carbs | Serum biochemistry, histopathology confirmation of MASLD |
| Dietary Intervention | 18 weeks | HF: Continued HFD (n=9)HF-NC: Switched to NC (n=9)HF-MD: Switched to MD (n=9) | MD: 15% protein, 35% fat, 50% carbohydrates | Weekly body weight and food intake |
| Terminal Analysis | Endpoint | All groups | - | Tissue collection, liver histopathology (H&E, Oil Red O), serum biomarkers, gut microbiota analysis |
Analytical Methods for Mechanistic Studies
Comprehensive assessment of MD effects requires multi-omics approaches and detailed biochemical analyses:
- Serum Biochemistry: Automated analyzers for liver enzymes (ALT, AST), lipid profiles (TC, TG, LDL-C, HDL-C), and metabolic parameters (glucose, bilirubin) [65]
- Inflammatory Mediators: ELISA-based quantification of hepatic IL-6 and TNF-α concentrations [65]
- Histopathological Assessment: H&E staining for cellular structure, Oil Red O for lipid accumulation [65]
- Gut Microbiota Analysis: Metagenomic sequencing of fecal DNA for microbial composition [65]
- Metabolomic Profiling: Targeted metabolomics for SCFAs and other microbial metabolites [65]
Integration of these datasets provides a systems-level understanding of how MD interventions alter host physiology through microbiome modulation.
Research Reagent Solutions
The table below outlines essential research tools for investigating the Mediterranean Diet's effects on oxidative stress, inflammation, and gut microbiome modulation.
Table 4: Essential Research Reagents for MD Mechanism Studies
| Reagent/Category | Specific Examples | Research Application | Key Functions |
|---|---|---|---|
| Oxidative Stress Biomarkers | MDA, 8OHdG, ROS assays | Quantifying oxidative damage | Assessment of lipid peroxidation, DNA oxidation, cellular ROS levels [68] |
| Inflammatory Cytokines | IL-6, TNF-α, IL-1β, IL-17 ELISA kits | Inflammation monitoring | Quantification of pro-inflammatory mediators in serum and tissues [66] [65] |
| Antioxidant Enzymes | SOD, Catalase, GPX activity assays | Endogenous defense evaluation | Measurement of cellular antioxidant capacity [2] [68] |
| Microbiota Analysis | 16S rRNA sequencing kits, metagenomic tools | Microbial composition profiling | Taxonomic classification, functional potential assessment [65] |
| SCFA Analysis | Acetate, propionate, butyrate standards | Microbial metabolite quantification | Targeted metabolomics for gut microbiome functional output [65] |
| Cell Signaling Assays | NF-κB, Nrf2 activation assays | Pathway activity measurement | Monitoring key transcriptional pathways in oxidative stress/inflammation [55] |
The Mediterranean Diet represents a multifaceted intervention that simultaneously targets oxidative stress and inflammation through direct molecular effects and gut microbiome modulation. The convergence of clinical evidence and preclinical mechanistic studies supports the role of MD as a powerful dietary strategy for preventing and managing chronic diseases. Future research should focus on personalized nutrition approaches that account for individual variations in microbiome composition, long-term intervention studies to establish durability of effects, and integration with other lifestyle interventions for maximal benefit. The development of MD-derived nutraceuticals and microbiome-targeted therapies represents a promising frontier for translating these findings into clinical applications, particularly for populations where dietary adherence presents challenges. As our understanding of the diet-gut-host axis deepens, targeted dietary interventions like the MD offer compelling strategies for addressing the root causes of chronic inflammation and oxidative stress in age-related diseases.
In the realm of chronic disease research, the bidirectional relationship between oxidative stress and inflammation has emerged as a critical pathological driver. This vicious cycle, where reactive oxygen species (ROS) activate immune cells to release pro-inflammatory cytokines which in turn stimulate further ROS production, sustains chronic tissue damage and accelerates disease progression [69]. Understanding this interplay is fundamental to modern clinical trial design, particularly in developing biomarkers that can accurately reflect underlying disease mechanisms.
The integration of biomarker endpoints into clinical trials represents a paradigm shift from traditional symptom-based assessment to targeted molecular evaluation. Biomarkers of oxidative stress and inflammation provide objective, quantifiable measures that can detect early pathological changes, stratify patient populations, and precisely monitor intervention efficacy. This technical guide examines current methodologies, biomarker classifications, and innovative approaches for correlating biomarker levels with clinical outcomes in chronic diseases characterized by oxidative stress and inflammation.
Key Biomarkers of Oxidative Stress and Inflammation
Established Biomarkers and Their Clinical Correlations
Table 1: Key Oxidative Stress Biomarkers and Measurement Techniques
| Biomarker | Molecular Significance | Measurement Techniques | Disease Correlations |
|---|---|---|---|
| Malondialdehyde (MDA) | Lipid peroxidation end-product | Thiobarbituric Acid-Reactive Substances (TBARS) assay | Hypertension severity, endothelial dysfunction [70] |
| 8-OHdG | DNA oxidation damage marker | HPLC-ECD, HPLC-MS/MS, ELISA | Diabetic nephropathy, neurodegenerative diseases [71] [70] |
| F2-isoprostanes | Stable lipid peroxidation product | Gas/Liquid chromatography-mass spectrometry | Cardiovascular risk, metabolic syndrome [70] |
| Protein Carbonyls | Protein oxidation marker | DNPH derivatization, immunoblotting, ELISA | Aging, neurodegenerative disorders [70] |
| Superoxide Dismutase (SOD) | Antioxidant enzyme activity | Spectrophotometric activity assays | β-cell failure, poor glycemic control [70] |
Table 2: Key Inflammatory Biomarkers and Their Pathological Significance
| Biomarker | Biological Role | Measurement Techniques | Disease Correlations |
|---|---|---|---|
| CRP/hs-CRP | Acute phase protein, systemic inflammation | Immunoassays (ELISA) | Cardiovascular risk, metabolic obesity phenotypes [71] [72] |
| IL-6 | Pro-inflammatory cytokine | Multiplex immunoassays, ELISA | Adipose tissue inflammation, insulin resistance [71] [72] |
| TNF-α | Pro-inflammatory cytokine | Multiplex immunoassays, ELISA | Synovial inflammation, cognitive decline in osteoarthritis [71] [72] |
| suPAR | Immune activation marker | Immunoassays | Mortality risk in emergency department patients [72] |
| IL-10 | Anti-inflammatory cytokine | Immunoassays, multiplex platforms | Frequently downregulated in heavy metal toxicity [71] |
Analytical Methodologies for Biomarker Quantification
Accurate biomarker measurement requires validated analytical approaches with appropriate sensitivity and specificity:
Chromatographic Methods: High-performance liquid chromatography (HPLC) coupled with electrochemical (ECD) or mass spectrometric detection (MS/MS) provides high sensitivity and specificity for biomarkers like 8-OHdG and F2-isoprostanes [70]. These methods offer precise quantification but require specialized equipment and technical expertise.
Immunoassays: Enzyme-linked immunosorbent assays (ELISAs) represent the most accessible platform for high-throughput biomarker analysis in clinical settings [71]. While offering practical advantages, potential antibody cross-reactivity requires careful validation against gold standard methods.
Advanced Detection Systems: Electron Paramagnetic Resonance (EPR) spectroscopy enables direct detection and quantification of ROS in biological tissues using spin trapping techniques [70]. This approach provides dynamic monitoring capabilities but remains primarily a research tool.
Omics Technologies: Redox proteomics and transcriptomics identify oxidative modifications and gene expression patterns, facilitating personalized therapeutic approaches through comprehensive molecular profiling [70].
Clinical Trial Designs for Biomarker Endpoint Validation
Biomarker-Informed Trial Designs
Table 3: Clinical Trial Designs for Biomarker Validation
| Design Type | Key Features | Advantages | Limitations | Example Applications |
|---|---|---|---|---|
| Enrichment Design | Enrollment restricted to biomarker-positive patients | Reduced sample size, increased probability of detecting treatment effect | Requires strong preliminary biomarker evidence | TOGA trial (HER2+ gastric cancer) [73] |
| Marker-by-Treatment Interaction Design | Randomizes all patients; stratified by biomarker status | Validates predictive utility of biomarker | Large sample size requirement | INTEREST trial (non-small cell lung cancer) [73] |
| Biomarker Strategy Design | Randomizes to biomarker-guided vs. standard strategy | Tests clinical utility of biomarker-based assignment | Does not identify best treatment for subgroups | SHIVA trial (molecularly targeted therapy) [73] |
| Sequential Testing Design | Primary analysis in overall population, then biomarker subgroup | Protects against false negatives in biomarker subgroup | May have low power for subgroup if prevalence is low | Adaptive signature designs [73] |
Methodological Framework for Biomarker Validation
The following workflow illustrates the comprehensive process for establishing biomarker-disease outcome correlations:
Biomarker Validation Workflow
Experimental Protocols for Key Biomarker Assays
Protocol: Quantification of 8-OHdG as a DNA Oxidation Biomarker
Principle: 8-hydroxy-2'-deoxyguanosine (8-OHdG) represents oxidative damage to guanine bases and serves as a sensitive marker of oxidative stress [70].
Sample Requirements:
- Urine: Collect 24-hour urine or first-morning void in preservative-free containers
- Tissue: Snap-freeze in liquid nitrogen and store at -80°C
- DNA extraction: Isolate DNA using phenol-chloroform method with chelating agents to prevent artificial oxidation
Procedure:
- DNA Hydrolysis: Digest DNA samples with nuclease P1 (pH 5.5) for 2 hours at 37°C, followed by alkaline phosphatase treatment (pH 7.5) for 1 hour at 37°C
- Sample Cleanup: Purify hydrolysates using solid-phase extraction cartridges (C18)
- HPLC Separation:
- Column: C18 reverse-phase column (4.6 × 250 mm, 5 μm particle size)
- Mobile phase: 50 mM sodium acetate (pH 5.2) with 5% methanol
- Flow rate: 1.0 mL/min
- Electrochemical Detection:
- Electrochemical detector with glassy carbon working electrode
- Applied potential: +0.4 to +0.6 V vs. reference electrode
- Quantification: Calculate 8-OHdG levels against authentic standard curve, normalize to creatinine (urine) or total DNA (tissue)
Quality Control:
- Include internal standard (8-OHdG-d3) to monitor recovery
- Process samples under reduced light to prevent photo-oxidation
- Analyze in batches with low, medium, and high concentration quality controls
Protocol: Multiplex Cytokine Profiling for Inflammatory Biomarkers
Principle: Simultaneous quantification of multiple inflammatory cytokines (IL-6, TNF-α, CRP) provides a comprehensive inflammatory profile [71] [72].
Sample Requirements:
- Serum/plasma: Collect in EDTA or heparin tubes, process within 2 hours, aliquot and store at -80°C
- Avoid repeated freeze-thaw cycles (maximum 2 cycles)
Procedure:
- Platform Selection: Magnetic bead-based multiplex immunoassay systems (e.g., Luminex)
- Assay Procedure:
- Add 50 μL of standards, controls, and samples to 96-well plate containing antibody-coupled magnetic beads
- Incubate for 2 hours at room temperature with shaking
- Wash twice with wash buffer
- Add biotinylated detection antibody mixture (25 μL/well)
- Incubate for 1 hour with shaking
- Wash twice, then add streptavidin-PE (50 μL/well)
- Incubate for 30 minutes with shaking
- Wash twice, resuspend beads in reading buffer
- Data Acquisition: Analyze using multiplex array reader with dual lasers
- Data Analysis: Calculate concentrations from 5-parameter logistic standard curve
Validation Parameters:
- Lower limit of quantification: Determine for each analyte
- Intra- and inter-assay precision: <15% CV
- Parallelism and spike recovery: 80-120%
- Reference range establishment in appropriate population
Emerging Technologies and Innovative Approaches
Machine Learning and Predictive Biomarker Discovery
Advanced computational approaches are revolutionizing biomarker discovery and validation. The MarkerPredict framework exemplifies this trend, integrating network motifs and protein disorder properties to classify potential predictive biomarkers with reported accuracy of 0.7-0.96 in leave-one-out cross-validation [74]. This approach utilizes:
- Random Forest and XGBoost algorithms for binary classification of biomarker potential
- Biomarker Probability Score (BPS) as a normalized summative rank across multiple models
- Network topological features and intrinsic disorder predictions to identify biomarker candidates
The successful application of these methods has identified 426 high-confidence predictive biomarkers for targeted cancer therapeutics, demonstrating the power of integrative computational-experimental approaches [74].
Digital Biomarkers and Continuous Monitoring
Digital biomarkers derived from wearables, smartphones, and connected devices enable continuous, real-world assessment of disease progression and treatment response [75]. Key applications include:
- Neurological Disorders: Continuous monitoring of motor function, speech patterns, and cognitive performance in neurodegenerative conditions
- Oncology: Integration of physiological data (heart rate variability, activity levels) with molecular biomarkers to create composite endpoints
- Metabolic Diseases: Continuous glucose monitoring coupled with activity tracking to assess metabolic control
These approaches facilitate high-resolution, longitudinal data collection that captures daily symptom fluctuations beyond traditional clinic-based assessments [75].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 4: Essential Research Reagents for Biomarker Studies
| Reagent Category | Specific Examples | Research Applications | Technical Considerations |
|---|---|---|---|
| Antibody Reagents | Phospho-specific antibodies, capture/detection antibody pairs | Immunoassays, Western blotting, immunohistochemistry | Validate species reactivity, check post-translational modification specificity |
| ELISA Kits | High-sensitivity cytokine kits, 8-OHdG ELISA, MDA ELISA | Quantitative biomarker measurement | Compare kit detection limits, validate against gold standard methods |
| PCR Assays | RT-qPCR primers/probes, miRNA assays, oxidative stress gene panels | Gene expression analysis of inflammatory and oxidative pathways | Verify amplification efficiency, include proper controls |
| Activity Assays | SOD activity assay, glutathione peroxidase assay, caspase assays | Functional assessment of antioxidant enzymes | Normalize to protein content, establish linear range |
| Metabolic Probes | DCFH-DA, MitoSOX, JC-1 dye | Cellular ROS measurement, mitochondrial function assessment | Optimize loading concentration, include appropriate controls |
| Protein Arrays | Cytokine array kits, phospho-kinase arrays, oxidative stress arrays | Multiplex protein profiling | Validate cross-reactivity, ensure linear dynamic range |
Implementation Framework and Regulatory Considerations
Pathway for Clinical Implementation of Biomarker Endpoints
The translation of biomarker-disease correlations into clinically validated endpoints requires systematic validation:
Clinical Translation Pathway
Regulatory and Standardization Considerations
Successful implementation of biomarker endpoints requires addressing key regulatory and methodological challenges:
- Analytical Validation: Establish precision, accuracy, sensitivity, specificity, and reproducibility using Clinical Laboratory Standards Institute (CLSI) guidelines
- Clinical Validation: Demonstrate association with clinical outcomes across diverse populations
- Standardization: Implement standardized operating procedures across multiple sites in multicenter trials
- Regulatory Qualification: Submit biomarker data to regulatory agencies for context-of-use qualification
- Data Transparency: Provide comprehensive documentation of analytical performance and clinical correlations
The recent ICH E6(R3) guideline emphasizes risk-based quality management and supports the integration of digital technologies, including digital biomarkers, in clinical trial design [75]. This regulatory evolution facilitates the adoption of innovative biomarker endpoints while maintaining rigorous standards for data integrity and patient safety.
The correlation of biomarker levels with disease progression and outcomes represents a cornerstone of precision medicine in chronic diseases driven by oxidative stress and inflammation. The integration of traditional biochemical biomarkers with emerging digital endpoints and computational prediction tools creates unprecedented opportunities for early intervention, patient stratification, and targeted therapeutic development. As biomarker science continues to evolve, the rigorous validation of these tools through appropriately designed clinical trials will be essential for translating mechanistic insights into measurable clinical benefits.
The future of biomarker-endpoint correlation lies in multidimensional assessment strategies that combine molecular profiling with continuous digital monitoring, enabling a more comprehensive understanding of disease progression and treatment response within the framework of oxidative stress and inflammatory pathways.
Overcoming the Antioxidant Paradox: Why Conventional Therapies Fail and How to Fix Them
Analyzing the Clinical Trial Failures of Non-Targeted Antioxidants (e.g., High-Dose Vitamin E)
The persistent failure of large-scale clinical trials on non-targeted, high-dose antioxidant supplements represents a critical paradox in modern therapeutics. Despite robust preclinical evidence linking oxidative stress to chronic disease pathogenesis, interventions like high-dose vitamin E have consistently failed to demonstrate efficacy and, in several instances, increased morbidity and mortality. This whitepaper analyzes the mechanistic underpinnings of these failures through the integrated lens of oxidative stress and inflammation interplay. We examine how the biological complexity of reactive oxygen species (ROS) signaling, the "antioxidant paradox," and critical shortcomings in experimental design have contributed to this translational gap. Furthermore, we propose a framework for future research centered on precision medicine approaches, including targeted antioxidant delivery and patient stratification using dynamic oxidative stress biomarkers.
The compelling hypothesis that supplemental antioxidants could mitigate chronic diseases by countering reactive oxygen species (ROS) has driven numerous clinical trials over recent decades. Oxidative stress, defined as an imbalance between ROS production and antioxidant defenses, is a well-established feature in the pathogenesis of cardiovascular, neurodegenerative, and neoplastic diseases [76] [77]. Epidemiological studies consistently observed correlations between high dietary antioxidant intake and reduced disease risk, creating strong rationale for intervention trials [78].
However, the transition from observational correlation to interventional causation has been largely unsuccessful. The case of high-dose vitamin E (α-tocopherol) is particularly illustrative: what was once a celebrated antioxidant became associated with enhanced risks of all-cause mortality, hemorrhagic stroke, and prostate cancer in several major trials [78]. This contradiction between mechanistic hypothesis and clinical outcome forms the core of the "antioxidant paradox" [78] [79].
The critical flaw in the non-targeted antioxidant approach lies in oversimplifying the sophisticated redox biology that underpins cellular homeostasis. ROS function not solely as damaging molecules but as crucial signaling mediators in physiological processes including immunity, cellular proliferation, and stress adaptation [2] [76]. This whitepaper deconstructs the molecular mechanisms, trial design limitations, and biological complexities that explain these clinical failures, while proposing refined strategies for future therapeutic development.
Clinical Evidence: Documented Failures of High-Dose Vitamin E
Major Trial Outcomes and Adverse Events
Table 1: Documented Adverse Outcomes from High-Dose Vitamin E Clinical Trials
| Trial/Study Reference | Population | Dosage | Primary Outcome | Adverse Effects |
|---|---|---|---|---|
| Selenium and Vitamin E Cancer Prevention Trial (SELECT) | Healthy men | 400 IU/day | No prostate cancer prevention | 17% increase in prostate cancer incidence [78] |
| Meta-Analysis (Miller et al.) | Various | ≥400 IU/day | All-cause mortality | Increased risk with dosages >150 IU/day, particularly with ≥400 IU/day [78] |
| HOPE-TOO | CV disease/diabetes | 400 IU/day | CV outcomes | Increased risk of heart failure hospitalization [78] |
| Multiple Trials | Patients on blood thinners | High-dose supplementation | - | Enhanced bleeding risk due to anticoagulant effects [78] |
The data from these large-scale interventions reveal a consistent pattern of null or harmful effects associated with high-dose vitamin E supplementation:
- Cancer Promotion: In the SELECT trial, vitamin E supplementation alone significantly increased prostate cancer risk rather than providing the anticipated protective effect [78]. Subsequent mechanistic studies revealed that vitamin E promoted cell proliferation and survival in premalignant prostate epithelial organoids, potentially facilitating tumorigenesis in early carcinogenesis stages [78].
- Mortality Concerns: A landmark meta-analysis established a dose-dependent relationship between vitamin E supplementation and all-cause mortality, with statistically significant risks emerging at doses exceeding 150 IU/day and becoming particularly pronounced at ≥400 IU/day [78].
- Cardiovascular Harm: Contrary to initial hypotheses predicting cardiovascular protection, high-dose vitamin E supplementation demonstrated associations with increased heart failure hospitalization in high-risk populations [78].
- Bleeding Complications: The anticoagulant properties of vitamin E, achieved through inhibition of vitamin K-dependent clotting factors, significantly amplified hemorrhage risk in patients concurrently administered blood-thinning medications like warfarin [78].
Underlying Mechanistic Flaws in the Antioxidant Hypothesis
Table 2: Mechanisms Underlying Clinical Failures of High-Dose Vitamin E
| Biological Mechanism | Pathophysiological Consequence | Clinical Manifestation |
|---|---|---|
| Pro-oxidant Shift | Generation of α-tocopheroxyl radicals; increased plasma oxidation by up to 27% [78] | Increased oxidative damage despite antioxidant intent |
| Interference with ROS Signaling | Disruption of physiological ROS roles in immune function and apoptosis [78] [76] | Impaired pathogen clearance and dysregulated cell proliferation |
| Anticoagulant Effect | Inhibition of protein kinase C and vitamin K-dependent carboxylase [78] | Increased bleeding risk, particularly hemorrhagic stroke |
| Metabolic Interference | Activation of cytochrome P450 enzymes; inhibition of glutathione S-transferases [78] | Altered drug metabolism and detoxification pathways |
| Disruption of Redox Balance | Over-compensation of endogenous antioxidant systems; paradoxical increase in oxidative stress [79] | Loss of physiological redox homeostasis |
Molecular Mechanisms: Unraveling the Biological Complexity
The Dual Nature of Reactive Oxygen Species in Cellular Signaling
The fundamental oversimplification in non-targeted antioxidant approaches lies in categorizing ROS as universally detrimental. In reality, ROS function as crucial signaling molecules at physiological concentrations, participating in essential cellular processes:
- Immune Function: Phagocytic neutrophils and macrophages intentionally generate ROS as a primary defense mechanism against invading pathogens [78] [76]. Excessive antioxidant activity can paradoxically impair this critical immune response.
- Cellular Homeostasis: Multiple gene transcription factors require intermittent oxidation for activation, including those regulating cell proliferation and differentiation [78]. The tumor suppressor p53 and retinoblastoma protein (Rb) both undergo ROS-mediated activation that halts cell cycle progression in response to stress [78].
- Apoptosis Regulation: While excessive oxidation inhibits apoptosis, physiological ROS levels stimulate this programmed cell death through caspase activation, representing a crucial mechanism for eliminating damaged cells [78].
The following diagram illustrates the paradoxical cellular responses to high-dose antioxidant supplementation:
The Inflammatory-Oxidative Nexus in Chronic Disease
The interplay between oxidative stress and inflammation creates a self-amplifying cycle that drives chronic disease progression. This nexus explains why simplistic antioxidant approaches have failed:
- NF-κB Activation: ROS directly activate the transcription factor NF-κB, a master regulator of inflammatory gene expression, leading to increased production of pro-inflammatory cytokines [2] [62].
- Inflammasome Activation: In conditions like myocardial ischemia-reperfusion injury, ROS bursts activate the NLRP3 inflammasome, triggering maturation and release of potent inflammatory mediators IL-1β and IL-18 [79].
- Cytokine-Induced ROS Production: Inflammatory cytokines themselves stimulate additional ROS generation through activation of enzymes like NADPH oxidase, creating a feed-forward cycle of inflammation and oxidation [2] [80].
The following diagram illustrates this vicious cycle and potential intervention points:
Methodological Approaches: Experimental Protocols & Techniques
Core Assessment Methodologies for Oxidative Stress
Research into oxidative stress and antioxidant efficacy employs standardized protocols for quantifying ROS production, oxidative damage, and antioxidant status:
Protocol 1: Lipid Peroxidation Measurement via Malondialdehyde (MDA) Assay
- Principle: Quantifies thiobarbituric acid reactive substances (TBARS) as a marker of lipid peroxidation [76].
- Procedure:
- Homogenize tissue samples or collect cell culture supernatants
- Add thiobarbituric acid reagent and incubate at 95°C for 60 minutes
- Cool samples and measure absorbance at 532 nm
- Calculate MDA concentrations using molar extinction coefficient of 1.56 × 10^5 M^-1cm^-1
- Applications: Evaluation of oxidative damage in cardiovascular tissues, neurodegenerative models, and hepatic toxicity studies [76].
Protocol 2: Glutathione Peroxidase (GPx) Activity Assay
- Principle: Measures enzyme activity through NADPH oxidation monitored at 340 nm [76].
- Procedure:
- Prepare tissue homogenates in cold buffer
- Add reaction mixture containing glutathione, glutathione reductase, and NADPH
- Initiate reaction with tert-butyl hydroperoxide
- Record decrease in absorbance at 340 nm for 3-5 minutes
- Calculate activity using NADPH extinction coefficient of 6.22 mM^-1cm^-1
- Applications: Assessment of endogenous antioxidant capacity in response to therapeutic interventions [76] [80].
Protocol 3: Protein Carbonyl Content Measurement
- Principle: Quantifies protein oxidation through derivatization with 2,4-dinitrophenylhydrazine (DNPH) [76].
- Procedure:
- Extract proteins and react with DNPH in 2M HCl
- Precipitate proteins with trichloroacetic acid
- Wash pellet with ethanol:ethyl acetate mixture
- Dissolve in guanidine hydrochloride
- Measure absorbance at 370 nm
- Applications: Evaluation of oxidative protein damage in neurodegenerative disease models and aging studies [76].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Oxidative Stress Investigation
| Reagent/Category | Specific Examples | Research Application | Technical Considerations |
|---|---|---|---|
| ROS Detection Probes | DCFH-DA, Dihydroethidium, MitoSOX | Cellular ROS measurement; mitochondrial superoxide detection | Probe specificity varies; requires validation with inhibitors [76] |
| Antioxidant Enzymes | Recombinant SOD, Catalase, GPx | Reference standards for activity assays; therapeutic candidates | Species-specific isoforms may show differential activity [80] |
| Lipid Peroxidation Assay Kits | TBARS, LOOH, 4-HNE detection kits | Standardized lipid peroxidation quantification | 4-HNE exhibits biological activity beyond being a marker [76] |
| Nrf2 Pathway Modulators | Sulforaphane, Bardoxolone methyl, KEAP1 inhibitors | Activation of endogenous antioxidant response | Potential off-target effects; dose-dependent efficacy [81] |
| Oxidized Biomarker ELISA Kits | 8-OHdG, nitrotyrosine, oxidized LDL kits | High-throughput assessment of oxidative damage | Sample collection conditions critically affect results [76] |
| Genetic Manipulation Tools | NOX knockout models, Nrf2 siRNA, antioxidant gene plasmids | Mechanistic studies of specific pathway components | Compensation by related genes may occur in knockout models [79] |
Path Forward: Precision Medicine Approaches in Redox Therapeutics
The repeated failures of non-targeted antioxidant trials necessitate a paradigm shift toward precision medicine strategies that account for individual variability in redox homeostasis:
Biomarker-Guided Patient Stratification
Future trials should incorporate comprehensive oxidative stress profiling to identify patient subsets most likely to benefit from antioxidant interventions:
- Dynamic Biomarkers: Measurement of F2-isoprostanes (lipid peroxidation), 8-hydroxy-2'-deoxyguanosine (DNA oxidation), and protein carbonyls (protein oxidation) for precise quantification of oxidative damage burden [76] [79].
- Inflammatory-Oxidative Signature: Multiplex assessment of both oxidative damage markers and inflammatory cytokines (IL-6, TNF-α, CRP) to identify patients with active oxidative-inflammatory cycles [2] [80].
- Genetic Profiling: Identification of polymorphisms in genes encoding NADPH oxidase subunits, NRF2, and antioxidant enzymes to predict therapeutic response [79] [82].
Targeted Delivery Systems and Novel Therapeutic Modalities
Emerging technologies offer promising approaches to overcome the limitations of systemic antioxidant administration:
- Mitochondria-Targeted Antioxidants: Compounds like MitoQ (ubiquinone conjugated to TPP+) and SkQ1 selectively accumulate in mitochondria, addressing the primary cellular source of ROS while minimizing disruption of physiological signaling [79].
- Nanoparticle-Based Delivery: Encapsulation of antioxidants in lipid nanoparticles or polymeric carriers enables tissue-specific delivery and enhanced bioavailability at target sites [79].
- NRF2 Activators: Pharmacological enhancement of endogenous antioxidant systems through KEAP1-NRF2 pathway activation provides a coordinated upregulation of multiple defense enzymes rather than single-agent supplementation [81].
- Combination Therapies: Strategic pairing of antioxidants with conventional therapeutics in specific pathological contexts, such as mitigating chemotherapy-induced oxidative damage while maintaining treatment efficacy [76].
Proposed Framework for Future Trial Design
The following diagram outlines a precision medicine approach for future antioxidant development:
The consistent failure of non-targeted, high-dose antioxidant trials represents not a repudiation of the oxidative stress hypothesis, but rather a demonstration of its profound biological complexity. The case of high-dose vitamin E exemplifies how therapeutic interventions that disrupt sophisticated redox signaling networks can produce unanticipated detrimental effects. The interplay between oxidative stress and inflammation creates particularly challenging therapeutic terrain, as these processes engage in self-amplifying cycles that resist simplistic intervention.
Future success in redox-based therapeutics requires abandoning the "one-size-fits-all" antioxidant paradigm in favor of precision medicine approaches that incorporate comprehensive patient stratification, targeted delivery systems, and biomarker-guided dosing. By respecting the dual nature of ROS as both damaging molecules and crucial signaling mediators, we can develop next-generation interventions that selectively inhibit pathological oxidative processes while preserving physiological redox signaling. This refined approach holds promise for finally realizing the long-unfulfilled potential of antioxidant therapeutics in chronic disease management.
Bioavailability and Delivery Challenges of Antioxidant Compounds
Antioxidant compounds demonstrate significant potential in mitigating oxidative stress and inflammation, key pathways in chronic diseases. However, their clinical translation is substantially hampered by inherent physicochemical properties leading to poor bioavailability. This whitepaper provides an in-depth technical analysis of the bioavailability challenges associated with natural and synthetic antioxidants and explores advanced delivery strategies designed to overcome these limitations. Within the context of chronic disease research, we examine how enhanced antioxidant delivery can modulate critical signaling pathways such as NF-κB and Nrf2 to disrupt the oxidative stress-inflammation cycle. The document summarizes quantitative bioavailability data in structured tables, details experimental methodologies for assessing antioxidant efficacy, and visualizes key biological pathways and formulation workflows. Aimed at researchers and drug development professionals, this review serves as a technical guide for advancing antioxidant-based therapeutic interventions.
Oxidative stress, resulting from an imbalance between reactive oxygen species (ROS) production and antioxidant defenses, is a major contributor to the pathogenesis of chronic diseases, including cardiovascular disorders, neurodegeneration, diabetes, and cancer [62] [2]. ROS, including superoxide (O₂•⁻), hydrogen peroxide (H₂O₂), and hydroxyl radicals (OH•), are generated from endogenous sources like mitochondrial metabolism and enzymatic reactions, as well as exogenous sources such as environmental toxins [2]. Crucially, oxidative stress and chronic inflammation are interconnected pathophysiological processes; ROS can activate pro-inflammatory signaling pathways like NF-κB, which in turn induces the expression of cytokines and enzymes that further amplify ROS production, creating a self-perpetuating cycle of cellular damage and disease progression [83] [2].
Therapeutic intervention using antioxidant compounds aims to break this cycle by neutralizing ROS and modulating inflammatory signaling. Antioxidants can be broadly categorized into natural bioactive compounds (e.g., polyphenols, carotenoids, flavonoids) and synthetic agents (e.g., edaravone, MitoQ, N-acetylcysteine) [2] [57]. Natural antioxidants, abundant in fruits and vegetables, often possess multiple favorable bioactivities, including antioxidant, anti-inflammatory, and antitumor properties [84]. However, the clinical application of both natural and synthetic antioxidants is severely limited by significant pharmacokinetic and physicochemical challenges, primarily their poor bioavailability [85] [84] [86]. This document examines these challenges in detail and outlines the advanced formulation strategies required to realize the full therapeutic potential of antioxidant compounds.
Core Bioavailability Challenges of Antioxidant Compounds
The term "bioavailability" refers to the proportion and rate at which an active compound enters systemic circulation and reaches its site of action. For most antioxidants, this parameter is critically low, often due to a confluence of factors.
Physicochemical and Biological Barriers
- Poor Aqueous Solubility: A vast number of potent antioxidant compounds, particularly flavonoids (e.g., quercetin) and polyphenols (e.g., curcumin), exhibit inherently low water solubility. This severely limits their dissolution in gastrointestinal fluids, a prerequisite for absorption [84] [86].
- Chemical Instability: Many antioxidants are chemically unstable and undergo rapid degradation or metabolism in the GI tract before absorption can occur. They are susceptible to the harsh acidic environment of the stomach, hydrolysis, and enzymatic degradation by oxidoreductases [85].
- Extensive Pre-systemic Metabolism: Following absorption, antioxidants are often subject to intensive first-pass metabolism in the liver and intestinal cells. This involves conjugation reactions (glucuronidation, sulfation, methylation) that can rapidly inactivate the compound and promote its biliary or renal excretion [84]. For some compounds like resveratrol, absorption is less than 10% [83].
- Low Permeability: While some antioxidants can passively diffuse across epithelial membranes, their molecular size and structure often result in low permeability. Furthermore, some flavonoids may be substrates for efflux transporters like P-glycoprotein, which actively pumps them back into the intestinal lumen, further reducing systemic absorption [84].
Clinical Implications of Low Bioavailability
The barriers described above directly translate to subtherapeutic concentrations at the target tissues, leading to ambiguous or failed clinical outcomes. For instance, despite strong preclinical evidence, the therapeutic benefits of many dietary antioxidants have not materialized in human trials, partly due to an insufficient dosage at the target site to elicit a meaningful antioxidant effect [57]. This bioavailability bottleneck underscores the critical need for advanced delivery systems that can protect antioxidants from degradation, enhance their solubility, and facilitate their targeted delivery.
Table 1: Quantitative Bioavailability Data of Selected Antioxidant Compounds
| Antioxidant Compound | Class | Reported Bioavailability | Major Challenges |
|---|---|---|---|
| Resveratrol | Polyphenol (Stilbene) | < 10% absorption [83] | Rapid metabolism, conjugation, low stability [86] |
| Curcumin | Polyphenol (Diarylheptanoid) | Very low [87] | Poor aqueous solubility, rapid metabolic conjugation [84] |
| Quercetin | Flavonoid (Flavonol) | Low [84] | Poor water solubility, extensive metabolism [84] [86] |
| Epigallocatechin gallate (EGCG) | Polyphenol (Flavon-3-ol) | Low (<1% in some studies) | Degradation in intestinal fluids, poor permeability [83] |
| Lycopene | Carotenoid | Variable, enhanced by fat | Low solubility, dependence on dietary fat for absorption [83] |
Advanced Delivery Systems to Enhance Bioavailability
To overcome the inherent limitations of antioxidants, a variety of advanced delivery systems have been developed. These platforms are designed to enhance the stability, solubility, and targeted delivery of bioactive compounds.
Lipid-Based Nanoparticles
Lipid nanoparticles are among the most clinically successful delivery platforms for hydrophobic compounds. They function by dissolving or encapsulating antioxidants, facilitating their transport and absorption.
- Nanoemulsions: These are heterogeneous mixtures of oil and water, stabilized by an emulsifier, with droplet sizes typically below 200 nm. They are classified as oil-in-water (O/W) or water-in-oil (W/O). O/W nanoemulsions are particularly effective for delivering lipophilic antioxidants (e.g., astaxanthin, curcumin) by solubilizing them in the inner oil phase, thereby altering absorption and enhancing biological accessibility [85]. Their composition (oil type, emulsifier, water-to-oil ratio) is critical for defining droplet size, stability, and release profile [85].
- Nanoliposomes: These are spherical vesicles composed of one or more phospholipid bilayers enclosing an aqueous core. This unique structure allows for the simultaneous encapsulation of hydrophilic compounds (e.g., certain polyphenols) within the aqueous interior and lipophilic compounds within the lipid bilayer, making them versatile carriers [88]. Surface modification with polymers like polyethylene glycol (PEG) can further extend their circulation time by reducing clearance by the reticuloendothelial system (RES) [88].
- Solid Lipid Nanoparticles (SLNs) and Nanostructured Lipid Carriers (NLCs): SLNs are composed of a solid lipid matrix at room and body temperature, offering controlled release profiles. NLCs are a second generation that blends solid and liquid lipids, creating a less ordered matrix that provides higher drug loading capacity and stability against drug expulsion during storage [86].
Polymer-Based and Other Delivery Systems
Polymer-based systems offer exceptional chemical flexibility for designing carriers with precise release characteristics.
- Polymeric Nanoparticles: Biodegradable polymers like PLGA (Poly(lactic-co-glycolic acid)) are widely used for their controlled release profiles and excellent biocompatibility [88]. Natural biopolymers such as chitosan are also employed, leveraging their mucoadhesive properties to enhance residence time and absorption at mucosal surfaces [88].
- Nanoencapsulation: This technique involves entrapping active ingredients within a protective shell or matrix. Biopolymers such as proteins (e.g., β-lactoglobulin) and polysaccharides (e.g., chitosan) are frequently used. Nanoencapsulation provides superior protection against degradation and enables controlled release mechanisms, significantly improving the stability and bioavailability of enclosed antioxidants [85].
- Cyclodextrin Complexes: Cyclodextrins are cyclic oligosaccharides with a hydrophilic exterior and a hydrophobic central cavity. They can form water-soluble inclusion complexes with poorly soluble antioxidants like flavonoids, effectively enhancing their solubility, chemical stability, and subsequent bioavailability [87].
- Micelles and Polymeric Micelles: These are self-assembled colloidal structures formed from amphiphilic block copolymers in an aqueous solution. The hydrophobic core serves as a reservoir for lipophilic antioxidants, while the hydrophilic shell stabilizes the structure. This makes them highly effective at increasing the apparent solubility of poorly water-soluble compounds [88].
Table 2: Advanced Delivery Systems for Antioxidants
| Delivery System | Key Components | Mechanism of Action | Target Antioxidant Type |
|---|---|---|---|
| Nanoemulsions | Oil, Water, Emulsifier (e.g., hydrophilic/hydrophobic surfactants) | Enhances solubility of lipophilics in oil droplets; alters absorption pathways [85] | Lipophilic (e.g., astaxanthin, curcumin) |
| Nanoliposomes | Phospholipids (e.g., phosphatidylcholine), Cholesterol | Encapsulates hydrophilic (in core) and lipophilic (in bilayer) compounds [88] | Both Hydrophilic & Lipophilic |
| Solid Lipid Nanoparticles (SLNs) | Solid lipids (e.g., tristearin), Surfactants | Dissolves compound in solid lipid matrix; controls release [86] | Lipophilic |
| Polymeric Nanoparticles (e.g., PLGA) | Biodegradable polymers (PLGA, Chitosan) | Protects compound in polymer matrix; enables sustained/controlled release [88] | Both Hydrophilic & Lipophilic |
| Cyclodextrin Complexes | Cyclodextrins (α-, β-, γ-) | Forms water-soluble inclusion complexes via host-guest interactions [87] | Poorly soluble molecules (e.g., flavonoids) |
Experimental Protocols for Assessing Bioavailability and Efficacy
Robust experimental methodologies are essential for evaluating the performance of novel antioxidant delivery systems. The following protocols outline key in vitro and in vivo assessments.
Protocol 1: In Vitro Bioaccessibility and Bioavailability Assessment using the INFOGEST Model
This standardized simulated gastrointestinal digestion model is used to predict the release of antioxidants from a food or delivery matrix during digestion.
- Oral Phase: Mix the antioxidant formulation with simulated salivary fluid (SSF) containing α-amylase and incubate for 2 minutes at pH 7.0.
- Gastric Phase: Adjust the pH to 3.0 and add simulated gastric fluid (SGF) containing pepsin. Incubate for 2 hours at 37°C under gentle agitation.
- Intestinal Phase: Adjust the pH to 7.0 and add simulated intestinal fluid (SIF) containing pancreatin and bile salts. Incubate for 2 hours at 37°C.
- Bioaccessible Fraction Collection: After intestinal digestion, centrifuge the sample at high speed (e.g., 10,000 × g, 60 min) to obtain the aqueous phase (micellar fraction). The concentration of the antioxidant in this fraction, analyzed by HPLC or LC-MS, represents the bioaccessible fraction—the portion available for intestinal absorption [87].
- Permeability Assessment: The bioaccessible fraction can be further tested using Caco-2 cell monolayers, a model of the human intestinal epithelium, to estimate permeability and predict absorption.
Protocol 2: In Vivo Assessment of Antioxidant Activity and Bioavailability
Animal studies are critical for understanding the pharmacokinetics and pharmacological effects of formulated antioxidants.
- Animal Dosing and Sample Collection:
- Use appropriate animal models (e.g., rats, mice). Divide into groups: control, pure antioxidant, and formulated antioxidant.
- Administer the compounds orally at an equivalent dose.
- Collect blood plasma samples at predetermined time points (e.g., 0.25, 0.5, 1, 2, 4, 8, 12, 24 h) via a catheter or serial sampling.
- Pharmacokinetic Analysis:
- Process plasma samples by protein precipitation, solid-phase extraction, or other suitable methods.
- Analyze antioxidant concentration using a validated analytical method (e.g., LC-MS/MS).
- Calculate key pharmacokinetic parameters: Cmax (maximum concentration), Tmax (time to reach Cmax), AUC0-t (area under the concentration-time curve), and half-life (t½). An increase in AUC and Cmax for the formulated group indicates enhanced bioavailability [85].
- Evaluation of Oxidative Stress Biomarkers:
- At sacrifice, collect relevant tissues (e.g., liver, brain, plasma).
- Quantify biomarkers of oxidative damage, such as:
- Lipid Peroxidation: Measure malondialdehyde (MDA) or 4-hydroxynonenal (4-HNE) levels via thiobarbituric acid reactive substances (TBARS) assay or LC-MS [83] [2].
- Protein Oxidation: Determine protein carbonyl content using a DNPH (2,4-dinitrophenylhydrazine) assay.
- Antioxidant Enzyme Activity: Assess the activity of endogenous enzymes like superoxide dismutase (SOD), catalase, and glutathione peroxidase (GPx) in tissue homogenates [2].
Visualization of Pathways and Workflows
Diagram 1: Nrf2-Keap1-ARE Signaling Pathway
This pathway is a central regulatory mechanism for the expression of antioxidant and cytoprotective genes. Many natural antioxidants activate this pathway.
Diagram 2: Workflow for Developing Nanoemulsion-Based Antioxidant Delivery
This flowchart outlines the key stages in the formulation and evaluation of a nanoemulsion for antioxidant delivery.
The Scientist's Toolkit: Key Research Reagents and Materials
Table 3: Essential Reagents for Antioxidant Delivery Research
| Reagent/Material | Function/Application | Example Uses |
|---|---|---|
| PLGA (Poly(lactic-co-glycolic acid)) | Biodegradable polymer for controlled-release nanoparticles. | Formulating nanoparticles for sustained antioxidant delivery [88]. |
| L-α-Phosphatidylcholine | Primary phospholipid for constructing liposomal bilayers. | Fabricating nanoliposomes for encapsulating hydrophilic/lipophilic antioxidants [88]. |
| PEGylated Lipids (e.g., DSPE-PEG) | Surface functionalization of lipid nanoparticles to impart "stealth" properties and prolong circulation. | PEGylation of liposomes to reduce RES clearance and enhance EPR effect [88]. |
| Cyclodextrins (α, β, γ) | Molecular carriers to form water-soluble inclusion complexes. | Enhancing aqueous solubility and stability of flavonoids and other poorly soluble actives [87]. |
| Caco-2 Cell Line | Human colon adenocarcinoma cell line; a model for intestinal permeability. | In vitro assessment of antioxidant absorption and transport [84]. |
| Simulated Gastrointestinal Fluids (SSF, SGF, SIF) | Standardized fluids for in vitro digestion simulation. | Assessing bioaccessibility of antioxidants using the INFOGEST protocol [87]. |
The interplay between oxidative stress and inflammation is a cornerstone of chronic disease pathology, positioning antioxidant compounds as promising therapeutic agents. However, their clinical potential remains largely untapped due to profound challenges with bioavailability and delivery. Overcoming these hurdles necessitates a shift from simple compound administration to sophisticated, engineered formulation strategies. Lipid-based nanoparticles, polymer-based carriers, and other advanced systems have demonstrated significant potential in enhancing the solubility, stability, and targeted delivery of antioxidants, thereby improving their pharmacokinetic profiles and therapeutic efficacy. Future progress in this field hinges on the continued integration of material science with biology, the validation of these advanced systems in robust clinical trials, and a refined understanding of the specific molecular contexts of antioxidant action. By bridging the gap between promising bioactivity and clinical delivery, researchers can unlock the full potential of antioxidants for the prevention and treatment of chronic diseases.
Oxidative stress, characterized by an imbalance between reactive oxygen species (ROS) production and cellular antioxidant defenses, is a key contributor to the pathogenesis of a wide spectrum of chronic diseases. When ROS levels exceed antioxidant capacity, they can cause significant molecular damage, disrupt redox signaling, and trigger pro-inflammatory pathways [89] [62]. This oxidative damage is particularly detrimental within mitochondria, the major cellular source of ROS, leading to a vicious cycle of mitochondrial dysfunction, amplified ROS production, and chronic low-grade inflammation [90] [89]. This interdependent relationship between oxidative stress and inflammation forms a core pathophysiological mechanism in conditions ranging from cardiovascular and neurodegenerative diseases to metabolic disorders [89] [62]. Traditional antioxidant therapies have largely yielded disappointing clinical results, often attributed to their inability to effectively reach the mitochondrial source of ROS and their failure to simultaneously address the intertwined inflammatory responses [89]. This review explores two innovative strategies to overcome these limitations: the development of the mitochondria-targeted antioxidant MitoQ and the application of advanced nanotechnology-based delivery platforms.
MitoQ: A Paradigm of Mitochondria-Targeted Antioxidant Therapy
Molecular Structure and Mechanism of Action
MitoQ (Mitoquinol Mesylate) is a first-in-class, mitochondrially-targeted antioxidant designed to overcome the delivery limitations of conventional antioxidants like Coenzyme Q10 [90] [91]. Its molecular structure consists of three key components:
- Antioxidant Head: A ubiquinone moiety, identical to that in CoQ10, which serves as the active antioxidant site for neutralizing free radicals [91].
- Short Carbon Chain: A 10-carbon chain that is shorter than that of native CoQ10, which enhances its absorption and bioavailability [91].
- Lipophilic Cation (TPP): A triphenylphosphonium (TPP) cation attached to the chain end, which confers a positive charge on the molecule [90] [91].
The mechanism is elegantly simple: the TPP cation is electrophoretically driven by the high negative membrane potential (typically -150 to -180 mV) across the inner mitochondrial membrane [90] [91]. This "electrophoretic accumulation" allows MitoQ to penetrate biological membranes easily and accumulate within the mitochondrial matrix at concentrations several hundred-fold higher than in the plasma [90]. Once inside, the antioxidant head integrates into the inner mitochondrial membrane, where it is continuously recycled between its active (mitoquinol) and oxidized (mitoquinone) forms by the electron transport chain, enabling a single molecule to neutralize multiple ROS [91].
Key Signaling Pathways and Mechanistic Insights
Research has elucidated that MitoQ's benefits extend beyond simple ROS scavenging to involve the modulation of key cytoprotective signaling pathways, most notably the Nrf2-ARE pathway [90] [92].
Diagram 1: MitoQ activates the Nrf2-ARE antioxidant pathway. MitoQ inhibits Keap1, allowing Nrf2 to translocate to the nucleus and upregulate protective genes like HO-1 and NQO1.
Under basal conditions, Nrf2 is sequestered in the cytoplasm by its inhibitor, Keap1, and targeted for proteasomal degradation. Oxidative stress, or MitoQ treatment, disrupts the Keap1-Nrf2 interaction, enabling Nrf2 stabilization and translocation into the nucleus [90]. There, it binds to the Antioxidant Response Element (ARE), initiating the transcription of a battery of cytoprotective genes, including heme oxygenase-1 (HO-1) and NAD(P)H quinone dehydrogenase 1 (NQO1) [90] [92]. This pathway is a crucial mechanism by which MitoQ reduces oxidative damage and apoptosis while improving cellular function in various disease models.
Efficacy Data from Preclinical and Clinical Studies
MitoQ has demonstrated significant protective effects across a range of experimental models and human conditions. The table below summarizes key quantitative findings from selected studies.
Table 1: Summary of Key Experimental Outcomes from MitoQ Studies
| Disease Model / Condition | Study Type | Dosage & Duration | Key Quantitative Outcomes | Primary Mechanism Implicated | Citation |
|---|---|---|---|---|---|
| Traumatic Brain Injury | In vivo (Mouse) | 4 mg/kg, i.p., 30 min post-TBI | ↓ Neuronal apoptosis, ↑ SOD/GPx activity, ↓ MDA content, ↑ Nrf2 nuclear translocation | Nrf2/ARE pathway activation, direct ROS scavenging | [90] |
| Vascular Aging | Clinical Trial (Older Adults) | 20 mg/day, oral, 6 weeks | ↑ Flow-mediated dilation by 42%, ↓ Aortic stiffness, ↓ Oxidized LDL by 13% | Reduction of mitochondrial ROS, improved NO bioavailability | [93] |
| Intestinal Ischemia/Reperfusion | In vivo (Mouse) & In vitro | 4 mg/kg (in vivo), 0.1-1.0 µM (in vitro) | Stabilized intestinal barrier, ↓ mtDNA damage (↓ 8-OHdG), ↑ TFAM stability | Nrf2/ARE activation, protection of mtDNA | [92] |
| Exercise Performance | Clinical Trial (Trained Cyclists) | 20 mg/day, oral, 4 weeks | ↑ Peak power by 4.4%, ↓ 8 km time trial by 10.8 seconds | Attenuation of exercise-induced oxidative DNA damage | [94] |
Advancing Delivery: Mitochondria-Targeted Nanomedicine Platforms
Rationale and Design Principles for Nanocarriers
While MitoQ represents a breakthrough in molecular design, its delivery can be further optimized, and its therapeutic scope expanded through nanotechnology. Mitochondria-targeted nanomedicine aims to overcome hierarchical biological barriers—including systemic circulation, tissue penetration, cellular uptake, and finally, subcellular localization—to achieve precise delivery of therapeutic cargo to mitochondria [95]. The design of these nanocarriers exploits specific mitochondrial characteristics:
- High Mitochondrial Membrane Potential (ΔΨm): Exploited by incorporating delocalized lipophilic cations (DLCs) like TPP, similar to MitoQ, to drive nanocarrier accumulation [95] [96].
- Mitochondrial Surface Markers: Utilizing specific targeting ligands (e.g., peptides, antibodies) that bind to proteins on the outer mitochondrial membrane, such as voltage-dependent anion channels (VDAC) or the translocator protein (TSPO) [95].
- Stimuli-Responsiveness: Designing nanocarriers that release their payload in response to the unique microenvironment of diseased cells or mitochondria, such as high ROS levels, low pH, or overexpressed enzymes [95] [96].
Classification and Applications of Nanocarriers
A diverse array of nanocarriers has been engineered for mitochondrial targeting, each with distinct advantages.
Table 2: Types of Mitochondria-Targeted Nanocarriers and Their Applications
| Nanocarrier Type | Key Composition & Targeting Strategy | Therapeutic Applications & Findings | Key Advantages | Citation |
|---|---|---|---|---|
| Lipid-based Nanoparticles | TPP-conjugated liposomes, DOTAP/DOPE cationic lipids. Use TPP for potential-driven uptake. | Delivery of anticancer drugs (e.g., Doxorubicin), pro-apoptotic peptides. Enhanced cytotoxicity in tumor models. | High biocompatibility, ability to encapsulate diverse cargo (hydrophilic/hydrophobic). | [95] [96] |
| Polymeric Nanoparticles | PLGA, chitosan, dendrimers. Surface-functionalized with TPP or mitochondrial targeting peptides (MTS). | Co-delivery of antioxidants and anti-inflammatory agents; "smart" NPs for triggered drug release in tumor microenvironments. | Tunable degradation rates, potential for high drug loading, versatile surface chemistry. | [95] |
| Inorganic Nanoparticles | Gold nanoparticles, quantum dots, carbon nanotubes. Often functionalized with TPP. | Primarily used for imaging and diagnostics; some therapeutic applications via photothermal therapy. | Unique optical/electronic properties, ease of functionalization. | [95] |
| Hybrid & Biomimetic Systems | Combinations of polymers/lipids; cell membrane-coated NPs. | Improved evasion of the immune system, enhanced tumor targeting via the EPR effect. | Superior ability to overcome multiple biological barriers. | [95] |
The following diagram illustrates the sequential journey of a mitochondria-targeted nanoparticle from administration to subcellular action.
Diagram 2: The multi-step journey of mitochondria-targeted nanoparticles involves overcoming several biological barriers to reach their subcellular target.
Experimental Protocols for Evaluating Mitochondrial-Targeted Therapies
This section provides detailed methodologies for key experiments used to validate the efficacy and mechanism of mitochondria-targeted compounds like MitoQ and nanocarriers.
In Vitro Assessment of Mitochondrial Function and Redox State
- Cell Culture and Treatment: Use relevant cell lines (e.g., primary neurons, endothelial cells, cancer cell lines). Pre-treat cells with MitoQ (typical range 0.1 - 1.0 µM) or nanoformulations for a set period (e.g., 6-24 h) prior to inducing oxidative stress (e.g., H₂O₂, hypoxia/reoxygenation) [92].
- Measurement of Mitochondrial ROS:
- Protocol: Load cells with fluorescent probes like MitoSOX Red (5 µM for 30 min at 37°C), which specifically targets mitochondria and becomes highly fluorescent upon oxidation by superoxide. Analyze fluorescence intensity via flow cytometry or fluorescence microscopy [96].
- Interpretation: A reduction in MitoSOX fluorescence in treated groups indicates successful mitigation of mitochondrial superoxide production.
- Assessment of Mitochondrial Membrane Potential (ΔΨm):
- Protocol: Use potentiometric dyes like JC-1 or TMRM. JC-1 forms red fluorescent aggregates in healthy, high-potential mitochondria and green fluorescent monomers in depolarized mitochondria. Incubate cells with JC-1 (2 µM for 30 min), wash, and measure the red/green fluorescence ratio [96].
- Interpretation: A higher red/green ratio indicates a maintained, healthy ΔΨm, which is often preserved by effective mitochondrial antioxidants.
- Analysis of Antioxidant Pathway Activation:
- Protocol: To investigate Nrf2 pathway activation, perform Western Blotting or immunofluorescence for Nrf2 nuclear translocation. Extract nuclear and cytosolic protein fractions from treated cells. Probe blots with anti-Nrf2 antibody. For immunofluorescence, fix and stain cells with anti-Nrf2 antibody and a nuclear marker (DAPI) [90] [92].
- Interpretation: Increased Nrf2 in the nuclear fraction or its co-localization with DAPI confirms pathway activation. Downstream targets like HO-1 and NQO1 can also be measured by Western Blot.
In Vivo Modeling and Efficacy Evaluation
- Animal Models:
- Traumatic Brain Injury (TBI): Utilize the Marmarou weight-drop model in mice. Anesthetize mice, make a scalp incision, and drop a defined weight (e.g., 200 g) from a specific height (e.g., 2.5 cm) onto the skull. Administer MitoQ (e.g., 4 mg/kg, i.p.) 30 minutes post-injury [90].
- Ischemia/Reperfusion (I/R): For intestinal I/R, anesthetize mice, perform a laparotomy, and occlude the superior mesenteric artery with a microvascular clamp for 30-45 minutes, followed by reperfusion for several hours. Administer MitoQ (e.g., 4 mg/kg, i.v.) shortly before ischemia [92].
- Functional and Endpoint Analyses:
- Neurobehavioral Scoring: In TBI models, assess neurological deficits at 1, 3, and 7 days post-injury using a 10-point Neurological Severity Score (NSS) that evaluates motor ability, balance, and alertness. Investigators should be blinded to the treatment groups [90].
- Vascular Function in Humans: In clinical trials, assess endothelial function via flow-mediated dilation (FMD) of the brachial artery. Use high-resolution ultrasonography to measure artery diameter before and after 5 minutes of forearm cuff occlusion. FMD is calculated as the percentage peak increase in diameter from baseline [93].
- Biomarker Quantification: Measure oxidative damage markers like malondialdehyde (MDA) in tissue homogenates using spectrophotometric kits. Assess apoptosis in tissue sections via TUNEL staining [90].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents for Mitochondrial Research and Targeted Therapy Development
| Reagent / Material | Function / Application | Specific Examples & Notes | Citation |
|---|---|---|---|
| MitoQ (Mitoquinol Mesylate) | Reference mitochondria-targeted antioxidant for in vitro and in vivo studies. | Available for research; used in clinical trials at 10-20 mg/day oral doses. A key positive control. | [90] [94] [93] |
| TPP (Triphenylphosphonium) Cation | Chemical moiety for conjugating to drugs or nanocarriers to facilitate mitochondrial targeting. | Synthetically conjugated to antioxidants, drugs, or nanoparticle surfaces. | [90] [95] [91] |
| Mitochondrial Dyes & Probes | Visualizing and quantifying mitochondrial health, ROS, and membrane potential. | MitoTracker (mass/viability), MitoSOX Red (mito-ROS), JC-1/TMRM (ΔΨm). Essential for validation. | [96] [92] |
| Nrf2 Pathway Modulators | Investigating the role of the Nrf2-ARE pathway in the mechanism of action. | Nrf2 siRNA to knock down gene expression; activators (e.g., sulforaphane) as positive controls. | [90] [92] |
| Nanocarrier Constituents | Building blocks for constructing mitochondrial-targeted delivery systems. | Cationic lipids (DOTAP, DOEPC), biodegradable polymers (PLGA, PLA), targeting ligands (peptides, dequalinium). | [95] [96] |
| Antibodies for Key Targets | Detecting expression and localization of proteins by Western Blot, IF, IHC. | Anti-Nrf2, Anti-HO-1, Anti-NQO1, Anti-TFAM, Anti-Cytochrome c, Anti-Bax. | [90] [92] |
The strategic targeting of mitochondria represents a frontier in the treatment of chronic diseases rooted in oxidative stress and inflammation. MitoQ has established a strong proof-of-concept, demonstrating that directed antioxidant delivery can yield significant functional improvements in both preclinical models and human trials by engaging cytoprotective mechanisms like the Nrf2 pathway. Concurrently, nanomedicine platforms offer a powerful and versatile toolbox to enhance the delivery and efficacy of a broader range of therapeutic agents, from established antioxidants to novel biologics. The convergence of these two fields—where nanocarriers are engineered to deliver MitoQ or similar agents with even greater precision and efficiency—holds particular promise. Future work must focus on refining the specificity of these nanotherapies, conducting long-term safety studies, and validating their efficacy in larger, more diverse clinical populations. By moving beyond non-targeted approaches and directly addressing the mitochondrial source of cellular dysfunction, these emerging solutions are poised to redefine therapeutic strategies for a host of intractable chronic diseases.
Within the framework of chronic disease pathogenesis, oxidative stress and chronic inflammation are established synergistic partners in a destructive cycle that promotes tissue damage and functional decline [2] [3]. This review pivots from the traditional antioxidant paradigm of direct reactive oxygen species (ROS) scavenging toward a sophisticated signaling-based approach: the targeted activation of endogenous defense systems. We focus on the transcription factor Nuclear factor erythroid 2-related factor 2 (NRF2), a master regulator of cellular resilience that coordinates the expression of over 300 genes involved in antioxidant defense, detoxification, inflammation resolution, and metabolic reprogramming [97] [98]. The molecular mechanics of the KEAP1-NRF2 pathway, the clinical and preclinical landscape of NRF2 inducers, and the dual roles of NRF2 in physiology and pathology are examined. This analysis provides researchers and drug development professionals with a rigorous technical guide to harnessing the cytoprotective power of NRF2 signaling, positioning it as a central therapeutic target for disrupting the oxidative-inflammatory axis in chronic diseases.
Oxidative stress results from an imbalance between the production of reactive oxygen species (ROS) and reactive nitrogen species (RNS) and the capacity of the cellular antioxidant apparatus to neutralize them [2]. This state disrupts cellular signaling, damages lipids, proteins, and DNA, and is a key pathogenic driver in a wide spectrum of conditions, including cardiovascular disorders, neurodegeneration, diabetes, and cancer [99] [3]. Critically, oxidative stress and chronic inflammation are locked in a self-perpetuating cycle. ROS activate redox-sensitive pro-inflammatory transcription factors such as Nuclear Factor-kappa B (NF-κB), leading to the upregulated expression of cytokines, chemokines, and adhesion molecules [3]. This inflammatory cascade, in turn, stimulates further ROS production from immune and non-immune cells, creating a feed-forward loop that sustains chronic tissue damage [2] [3].
The limitations of conventional antioxidant therapies, which often rely on direct stoichiometric scavenging of ROS, have prompted a paradigm shift. The new focus is on activating endogenous signaling pathways that orchestrate a coordinated, multi-faceted cytoprotective response. The NRF2 pathway represents the most prominent of these inducible defense systems, serving as a central node in the cellular adaptation to oxidative and electrophilic stress [100] [97].
The KEAP1-NRF2 Signaling Pathway: Molecular Mechanism
Architectural Domains of NRF2
NRF2 is a Cap 'n' Collar (CNC) basic leucine zipper (bZIP) transcription factor composed of seven highly conserved NRF2-ECH homology (Neh) domains [99] [98]. Each domain fulfills a distinct functional role:
- Neh2: This N-terminal domain contains the ETGE and DLG motifs critical for binding to its cytoplasmic repressor, KEAP1, thereby facilitating NRF2's constitutive ubiquitination and degradation [99] [98].
- Neh4 & Neh5: These domains act as primary transactivation domains, recruiting co-activators like CREB-binding protein (CBP) to initiate transcription [98].
- Neh6: Functions as a redox-insensitive degron, containing DSGIS and DSAPGS motifs that allow for KEAP1-independent degradation of NRF2 via the β-TrCP ubiquitin ligase adaptor [98].
- Neh7: Mediates repression of NRF2 transcriptional activity through interaction with the retinoid X receptor alpha (RXRα) [99].
- Neh1: Contains a bZIP domain that enables NRF2 to heterodimerize with small Maf (sMaf) proteins (MAFF, MAFG, MAFK) [99] [98].
- Neh3: The C-terminal domain contributes to transactivation and interacts with components of the transcriptional machinery [98].
The KEAP1 Repression and NRF2 Activation Cycle
Under homeostatic conditions, NRF2 is rapidly turned over with a half-life of approximately 20 minutes [98]. Its repressor, KEAP1, acts as a substrate adaptor for a Cullin 3 (CUL3)-based E3 ubiquitin ligase complex. KEAP1 homodimer binds NRF2 with high affinity via the "hinge-and-latch" model, using the ETGE (latch) and DLG (hinge) motifs, presenting NRF2 for ubiquitination and subsequent proteasomal degradation [100] [99].
Activation of the pathway is triggered by oxidative or electrophilic stress. Inducer molecules, often electrophiles, modify specific sensor cysteine residues (e.g., C151, C273, C288) within KEAP1 [99] [97]. This covalent modification induces a conformational change in KEAP1, disrupting its E3 ligase activity and the "hinge-and-latch" mechanism. Consequently, nascent NRF2 escapes ubiquitination, accumulates in the cytoplasm, and translocates to the nucleus [100] [97]. In the nucleus, NRF2 heterodimerizes with a sMaf protein and binds to the Antioxidant Response Element (ARE) or Electrophile Response Element (EpRE) in the promoter regions of its target genes, initiating their transcription [100] [98].
Diagram Title: The KEAP1-NRF2 Signaling Pathway and Activation Mechanism
Network of NRF2 Target Genes
NRF2 activation initiates a comprehensive transcriptional program that extends beyond classic antioxidant defense. Key target gene categories include [97] [98]:
- Antioxidant Proteins: NAD(P)H quinone oxidoreductase 1 (NQO1), heme oxygenase-1 (HMOX1), sulfiredoxin 1 (SRXN1), and thioredoxin reductase 1 (TXNRD1).
- Glutathione System: The catalytic (GCLC) and modifier (GCLM) subunits of glutamate-cysteine ligase, the rate-limiting enzyme in glutathione (GSH) synthesis, and glutathione S-transferases (GSTs).
- Detoxification Enzymes: UDP-glucuronosyltransferases (UGTs).
- Drug Transporters: Multidrug resistance-associated proteins (MRPs).
- Anti-inflammatory Mediators: NRF2 activation can indirectly suppress NF-κB signaling and inhibit the NLRP3 inflammasome [98] [3].
Landscape of Pharmacological NRF2 Inducers
A plethora of molecules, both natural and synthetic, have been identified as NRF2 inducers. They primarily function as electrophiles that modify the critical cysteine sensors on KEAP1. The table below summarizes the key characteristics of four lead compounds that have been extensively studied in clinical trials.
Table 1: Clinically Evaluated Pharmacological NRF2 Inducers
| Compound | Chemical Class | Primary Clinical Application | Mechanism of KEAP1 Interaction | Key Clinical Trial Biomarkers |
|---|---|---|---|---|
| Dimethyl Fumarate (DMF) [97] | Fumaric acid ester | Multiple Sclerosis, Psoriasis | Michael addition to C151 | Increased NQO1 activity in peripheral blood mononuclear cells (PBMCs); reduced MRI lesion activity |
| Bardoxolone Methyl (BARD-Me) [97] | Synthetic oleanane triterpenoid | Chronic Kidney Disease (e.g., in Alport syndrome, diabetic kidney disease) | Michael addition to C151 | Improved estimated glomerular filtration rate (eGFR); increased urinary GSH and plasma NQO1 levels |
| Sulforaphane (SFN) [97] | Isothiocyanate (from cruciferous vegetables) | Cancer Prevention, Autism Spectrum Disorder | Modification of KEAP1 cysteine residues | Increased levels of NRF2 target gene products (GSTs, NQO1) in tissues; enhanced carcinogen detoxification |
| Oltipraz [97] | Dithiolethione | Anti-schistosomal, Chemoprevention | Modification of KEAP1 cysteine residues | Induction of GST and NQO1; modulation of aflatoxin metabolism and DNA adduct formation |
The clinical development of these agents underscores the pharmacological relevance of the KEAP1-NRF2 axis. For instance, dimethyl fumarate (Tecfidera) is an FDA-approved therapy for multiple sclerosis, and its efficacy in animal models is abrogated in Nrf2-disrupted mice, confirming the pathway's central role in its mechanism of action [97].
Experimental Toolkit for NRF2 Research
Studying the NRF2 pathway requires a multifaceted approach to assess its activity, functional output, and biological consequences. The following table outlines essential reagents, models, and methodologies.
Table 2: Essential Research Tools for Investigating the NRF2 Pathway
| Category / Tool | Specific Example | Primary Function / Application in Research |
|---|---|---|
| Cell-Based Models | Primary macrophages [101], HepG2 hepatoma cells [100] | In vitro assessment of NRF2 activation, gene expression, and cytoprotection in relevant cell types. |
| Animal Models | Nrf2-knockout mice [100] [97], Keap1-knockout mice [100] | Definitive determination of NRF2-specific functions in vivo; study of systemic and tissue-specific responses. |
| Gene Expression Analysis | qPCR for NQO1, HMOX1, GCLC [97] | Standard method to quantify transcriptional activation of canonical NRF2 target genes. |
| Protein Analysis | Western Blot (NRF2, KEAP1, NQO1) [100], Chromatin Immunoprecipitation (ChIP) [100] | Measures protein accumulation, degradation, and direct binding of NRF2 to ARE sequences in promoters. |
| Functional Activity Assays | NQO1 enzymatic activity assay [97] | Assesses the functional consequence of NRF2 activation beyond mRNA/protein levels. |
| Pathway Reporter Assays | ARE-luciferase reporter gene construct [100] | High-throughput screening for NRF2 pathway activators or inhibitors. |
| Oxidative Stress Probes | DCFDA, MitoSOX | Measures intracellular ROS levels to evaluate the functional antioxidant capacity conferred by NRF2 activation. |
Detailed Experimental Protocol: Assessing NRF2 ActivationIn Vitro
A typical workflow for evaluating a compound's efficacy as an NRF2 inducer in a cell culture model is outlined below, synthesizing common methodologies from the literature [100] [97] [101].
Objective: To determine the potency and functional impact of a putative NRF2 inducer (e.g., sulforaphane) in HepG2 cells.
Materials:
- Cell Line: HepG2 (human hepatoma) or other relevant cell type.
- Test Compound: Sulforaphane (e.g., 1-20 µM), dissolved in DMSO. A vehicle control (DMSO) is essential.
- Antibodies: Anti-NRF2, Anti-KEAP1, Anti-NQO1, Anti-β-Actin (loading control).
- Reagents: qPCR primers for NFE2L2, NQO1, HMOX1, GCLC; TRIzol reagent; SYBR Green master mix.
- Equipment: Cell culture incubator, CO2 chamber, electrophoresis system, real-time PCR cycler, chemiluminescence imager.
Methodology:
- Cell Seeding and Treatment:
- Seed HepG2 cells in appropriate culture plates and allow to adhere for 24 hours.
- Treat cells with a range of sulforaphane concentrations (e.g., 1, 5, 10 µM) and vehicle control for a defined period (e.g., 6-24 hours).
Nuclear-Cytoplasmic Fractionation and Western Blotting:
- Harvest cells and perform subcellular fractionation to separate nuclear and cytoplasmic extracts.
- Resolve proteins by SDS-PAGE and transfer to a PVDF membrane.
- Probe membranes with anti-NRF2 antibody. A successful induction will show increased NRF2 protein levels in the nuclear fraction. KEAP1 levels can be monitored in the cytoplasmic fraction.
Gene Expression Analysis by qRT-PCR:
- Extract total RNA from treated cells using TRIzol.
- Synthesize cDNA and perform qPCR using primers specific for NRF2 target genes (NQO1, HMOX1, GCLC). Normalize data to a housekeeping gene (e.g., GAPDH). A significant, dose-dependent increase in target gene mRNA confirms transcriptional activation.
Functional Enzyme Activity Assay:
- Prepare cell lysates from treated and control cells.
- Perform an NQO1 catalytic activity assay, which typically measures the NADPH-dependent reduction of a substrate like menadione, monitored spectrophotometrically. Increased activity confirms functional upregulation of the NRF2 pathway.
Diagram Title: Experimental Workflow for Validating NRF2 Inducers
The Dual Role of NRF2 in Cancer: A Critical Consideration for Therapeutic Targeting
The role of NRF2 in cancer is complex and dualistic, presenting both a challenge and an opportunity for therapeutic development. This "dark side" of NRF2 must be carefully considered in drug development strategies [99] [101] [102].
Tumor Suppressor Role: In early carcinogenesis, NRF2's cytoprotective functions can prevent initial DNA damage and genomic instability caused by oxidative stress, thereby acting as a tumor suppressor [99].
Tumor Promoter Role: In established tumors, however, hyperactive NRF2 can be co-opted by cancer cells to promote survival, proliferation, and therapy resistance. Somatic mutations in KEAP1 or NFE2L2 genes, which constitutively activate NRF2, are frequently found in several cancers, including lung squamous cell carcinoma [99] [102]. This hyperactivation provides a selective advantage by:
- Enhancing chemoresistance and radiotherapeutic resistance by upregulating drug efflux pumps and detoxification enzymes [99].
- Supporting anabolic metabolism and proliferation to fuel tumor growth [99].
- Remodeling the tumor microenvironment. For instance, hemorrhage within tumors leads to heme release, which activates NRF2 in tumor-associated macrophages (TAMs). These NRF2-polarized TAMs adopt a pro-tumorigenic phenotype, driving cancer invasion, metastasis, and resistance to immunotherapy [101].
This duality necessitates a context-dependent therapeutic strategy: NRF2 activation is likely beneficial for disease prevention and in degenerative conditions, whereas NRF2 inhibition may be a valid strategy in certain advanced cancers with documented pathway hyperactivation.
The strategic activation of the KEAP1-NRF2 signaling pathway represents a powerful and mechanistically rational approach to counteracting the intertwined pathologies of oxidative stress and inflammation in chronic diseases. Moving beyond mere scavenging, NRF2 inducers amplify the body's own innate defense networks, offering a sustained, multi-gene protective response. The continued development of novel, potent, and selective NRF2 modulators, coupled with a refined understanding of the pathway's complex biology—including its cell-type-specific functions and its dual role in cancer—will be crucial for translating this knowledge into safe and effective therapeutics. Future research must focus on personalized medicine approaches, identifying patient subgroups most likely to benefit from NRF2-targeted interventions based on their genetic, metabolic, and disease context.
The intricate interplay between oxidative stress and inflammation constitutes a fundamental pathway in the pathogenesis of numerous chronic diseases. Personalized redox medicine emerges as a transformative approach, seeking to tailor therapeutic interventions based on an individual's unique genetic makeup and redox phenotype. This whitepaper provides an in-depth technical exploration of the core components of this paradigm, with a specific focus on the profiling of key genetic regulators like KEAP1 and NRF2. We detail the molecular mechanisms, present structured quantitative data on disease-associated polymorphisms, and outline advanced methodologies for phenotypic diagnosis. Furthermore, we discuss the integration of these insights into the development of targeted therapeutics, including NRF2 activators and inhibitors, thereby offering a roadmap for researchers and drug development professionals to advance this promising field.
Oxidative stress, characterized by an imbalance between reactive oxygen species (ROS) production and antioxidant defenses, is a ubiquitous player in chronic disease pathogenesis [2] [46]. The brain, with its high metabolic rate and lipid content, is particularly vulnerable, and oxidative damage is a documented contributor to neurodegenerative conditions like Alzheimer's and Parkinson's disease [103] [77]. Conversely, in cancer, oxidative stress can drive tumorigenesis and confer therapeutic resistance [104] [105].
This oxidative burden is deeply intertwined with chronic inflammation. ROS act as signaling molecules that activate key pro-inflammatory pathways, most notably the transcription factor NF-κB, which in turn promotes the expression of cytokines like IL-6 and TNF-α [2] [55]. This creates a self-perpetuating vicious cycle: inflammation generates more ROS, which further amplifies the inflammatory response [55]. The KEAP1-NRF2 system is a critical nodal point in regulating this axis. Under homeostasis, the KEAP1 protein targets NRF2 for proteasomal degradation, keeping its activity in check. Upon oxidative or electrophilic stress, this repression is lifted, allowing NRF2 to accumulate and orchestrate the expression of a battery of cytoprotective genes, including those involved in glutathione synthesis and ROS detoxification (e.g., NQO1, HO-1) [104] [46]. The centrality of this pathway makes its genetic and functional status a critical determinant of disease susceptibility and therapeutic response.
Molecular Mechanisms: The KEAP1-NRF2 Signaling Pathway
The KEAP1-NRF2 pathway is a sophisticated sensor for oxidative and electrophilic stress, and its precise regulation is paramount for cellular homeostasis. NRF2 (Nuclear factor erythroid 2-related factor 2) is a transcription factor containing six highly conserved Neh domains. The Neh2 domain at the N-terminus is responsible for its interaction with KEAP1 [106]. KEAP1 (Kelch-like ECH-associated protein 1) functions as a substrate adaptor for a Cullin 3 (Cul3)-based E3 ubiquitin ligase complex. A single KEAP1 homodimer binds to two distinct motifs within the Neh2 domain of NRF2: the high-affinity ETGE motif and the lower-affinity DLGex motif. This "hinge and latch" model facilitates the efficient ubiquitination and subsequent proteasomal degradation of NRF2, resulting in a very short half-life of less than 20 minutes under basal conditions [104].
The pathway is activated when specific reactive cysteine residues in KEAP1 are modified by ROS or electrophiles. This modification disrupts the ubiquitin ligase complex, allowing newly synthesized NRF2 to escape degradation, accumulate in the nucleus, form a heterodimer with a small Maf (sMaf) protein, and bind to the Antioxidant Response Element (ARE) in the promoter regions of its target genes [104] [106]. This leads to the coordinated upregulation of a network of over 200 genes involved in antioxidant defense, detoxification, drug transport, and inflammation resolution, enabling the cell to adapt and survive under stress [104].
The following diagram illustrates the core regulation and activation of the KEAP1-NRF2 pathway:
Genetic Profiling: KEAP1 and NRF2 Polymorphisms
Genetic variations in the KEAP1 and NFE2L2 (which encodes NRF2) genes can significantly alter the function of this critical pathway, influencing an individual's susceptibility to disease and response to treatment.
Key Polymorphisms and Their Functional Impact
Somatic and germline mutations in KEAP1 and NFE2L2 are found in various cancers, leading to constitutive activation of NRF2 and a phenotype known as "NRF2 addiction" [104] [106]. These mutations, often found in lung cancer, disrupt the KEAP1-NRF2 interaction, resulting in sustained NRF2 activity that promotes tumor survival, metabolic reprogramming, and resistance to therapy [104]. Beyond somatic mutations, specific single-nucleotide polymorphisms (SNPs) have been associated with disease risk across multiple populations.
Table 1: Disease-Associated Polymorphisms in KEAP1
| Gene/SNP | Amino Acid Change | Associated Disease Risk | Proposed Molecular Mechanism |
|---|---|---|---|
| KEAP1 (Various somatic) | Multiple (e.g., in Kelch/DGR domain) | Lung, Liver, Gallbladder Cancer [106] | Disrupted KEAP1-NRF2 binding, constitutive NRF2 activation [104] [106] |
| rs1048290 | Serine to Proline | Endometrial Cancer [106] | Altered protein function impacting cytoprotection [106] |
| rs11545829 | -- | Leukemia [106] | Modulated NRF2 pathway activity [106] |
| rs8113472 | -- | Rheumatoid Arthritis [106] | Inflammatory dysregulation via altered redox sensing [106] |
Table 2: Disease-Associated Polymorphisms in NRF2 (NFE2L2)
| Gene/SNP | Amino Acid Change | Associated Disease Risk | Proposed Molecular Mechanism |
|---|---|---|---|
| NFE2L2 (Somatic) | Multiple (in Neh2 domain) | Lung, Esophageal, Skin Cancers [106] | Impaired binding to KEAP1, leading to NRF2 stabilization [104] [106] |
| rs6721961 | -- | Oxidative Stress Injuries [106] | Altered transcriptional activity of NRF2 [106] |
| rs35652124 | -- | Neurodegenerative Diseases [106] | Compromised antioxidant defense in the brain [106] |
Genetic Associations Beyond Cancer: Evidence from Mendelian Randomization
Large-scale genetic studies have strengthened the causal link between redox regulatory drug targets and psychiatric disorders. A Mendelian randomization study identified that genetic variations in targets of redox-active compounds like vitamin C (OGFOD2) and melatonin (RORB) were significantly associated with the risk of schizophrenia (SCZ), while the vitamin E target (PRKCB) was linked to bipolar disorder (BD) risk [103]. This provides genetic evidence that redox imbalances are not merely correlative but play a causal role in a wide spectrum of chronic diseases, highlighting the potential for genetically-guided redox therapies.
Phenotype-Specific Diagnosis and Experimental Assessment
Beyond genetic profiling, functional assessment of the redox phenotype is crucial, as it represents the integrated output of genetic, epigenetic, and environmental influences.
Advanced FACS-Based Workflow for Redox and Mitochondrial Phenotyping
A novel fluorescence-activated cell sorting (FACS)-based protocol enables the simultaneous assessment of redox status and mitochondrial DNA (mtDNA) integrity in specific cell populations, such as hematopoietic stem cells or mesenchymal stromal cells [107]. This methodology provides a high-resolution, multi-parameter phenotypic profile at a single-cell level.
Detailed Experimental Protocol:
Cell Preparation and Staining:
- Viability Staining: Begin with a single-cell suspension. Use a fixable viability dye (e.g., eFluor 780) to exclude dead cells.
- Cell Barcoding (Optional): For multiple samples/treatments, use a proliferation dye like CellTrace Violet to barcode groups, reducing staining variability and reagent use [107].
- Surface Marker Staining: Stain with fluorochrome-conjugated antibodies against cell surface markers (e.g., CD34 for HSPCs, CD105 for MSCs) to identify the population of interest.
- Intracellular Staining for Redox and Mitochondria: Fix and permeabilize cells. Then stain intracellularly with:
- CellROX Green: A fixable, permeabilizable dye that measures general reactive oxygen species (ROS).
- Anti-Glutathione antibody: Measures the level of reduced glutathione (GSH), the primary cellular antioxidant.
- Anti-MTCO1 antibody: Targets a mtDNA-encoded protein (complex IV subunit). Its level reflects mtDNA integrity and translation.
- Anti-ATP5H antibody: Targets a nuclear DNA-encoded mitochondrial protein (ATP synthase subunit). Serves as a control for general mitochondrial protein content.
FACS Analysis and Data Calculation:
- Acquire data on a flow cytometer equipped with appropriate lasers and filters.
- Gate on live, phenotypically defined cells (e.g., Live/CD34+).
- Calculate key ratios:
- ROS:GSH Ratio: An index of oxidative burden.
- MTCO1:ATP5H Ratio (Median Fluorescence Intensity): An indicator of mtDNA genomic stability. A lower ratio suggests mtDNA damage [107].
Downstream Applications:
- Cells can be sorted based on any of the above parameters for further analysis, such as quantitative PCR (qPCR) to measure absolute mtDNA copy number per nucleus [107].
The following diagram outlines this comprehensive experimental workflow:
Diagnostic and Prognostic Redox Signatures
In non-small cell lung cancer (NSCLC), tumors with loss-of-function mutations in KEAP1 or STK11 exhibit a distinct redox signature characterized by the upregulation of oxidoreductase activity pathways. This signature is clinically relevant, as it is associated with a T-cell excluded tumor microenvironment, suppression of STING/MDA5-mediated interferon signaling, and resistance to immune checkpoint inhibitor therapy [108]. This underscores the value of redox phenotyping, whether via genetic sequencing or transcriptomic profiling, for predicting therapeutic outcomes and guiding treatment selection.
The Scientist's Toolkit: Key Research Reagent Solutions
The following table details essential reagents and tools for conducting research in personalized redox medicine, as derived from the cited experimental workflows.
Table 3: Key Research Reagents for Redox and Genetic Phenotyping
| Reagent / Tool | Function / Target | Experimental Application |
|---|---|---|
| Anti-ATP5H Antibody [107] | Binds to nuclear DNA-encoded subunit of ATP synthase | Mitochondrial content control in MTCO1:ATP5H ratio for mtDNA integrity [107] |
| Anti-MTCO1 Antibody [107] | Binds to mitochondrial DNA-encoded subunit of cytochrome c oxidase | Measurement of mtDNA-encoded protein levels; indicator of mtDNA health [107] |
| Anti-Glutathione Antibody [107] | Detects reduced form of glutathione (GSH) | Quantification of major cellular antioxidant capacity [107] |
| CellROX Green Reagent [107] | Fluorogenic sensor for reactive oxygen species (ROS) | Measurement of general oxidative stress in fixed/permeabilized cells [107] |
| CellTrace Violet [107] | Fluorescent cell membrane dye for barcoding | Staining multiple samples for pooled processing, reducing variability [107] |
| Fixable Viability Dye eFluor 780 [107] | Covalently labels non-viable cells | Exclusion of dead cells during flow cytometry analysis [107] |
| Pyocyanin [107] | Natural compound that generates H2O2 | Inducing acute or chronic oxidative stress in cell cultures [107] |
| Ethidium Bromide [107] | Intercalating agent that depletes mtDNA | Creating models of mtDNA depletion to validate assays [107] |
| GTEx eQTL Data [103] | Database of genetic variants affecting gene expression | Identifying instrumental variables for Mendelian randomization studies [103] |
Therapeutic Implications and Future Directions
The stratification of patients based on KEAP1/NRF2 genotype and redox phenotype creates opportunities for highly targeted therapeutic interventions.
For NRF2-Hyperactive Cancers: In tumors with constitutive NRF2 activation due to
KEAP1orNFE2L2mutations, NRF2 inhibitors are being explored to counteract the survival advantage and drug resistance conferred by this pathway [104]. Simultaneously, the redox-immunity connection suggests that combining these inhibitors with immunotherapy could overcome resistance inKEAP1-mutant lung cancers [108].For Diseases of Redox Insufficiency: In contrast, chronic diseases characterized by excessive oxidative stress and inflammation, such as neurodegenerative disorders, may benefit from NRF2 activators. Compounds like sulforaphane, curcumin, and synthetic derivatives designed to modify KEAP1 cysteines can boost the endogenous antioxidant response [2] [55]. The genetic findings linking vitamin C and E targets to psychiatric disorders further suggest that redox regulatory drugs (RRDs) like N-acetylcysteine (NAC) could be repurposed for patient subgroups with specific genetic backgrounds [103].
Future work must focus on validating these stratified approaches in clinical trials, developing more robust and standardized redox biomarkers, and creating advanced delivery systems (e.g., nanoparticles) for targeted redox modulators [55]. By deeply integrating genetic profiling with high-resolution phenotypic diagnosis, personalized redox medicine promises to transform the treatment of chronic diseases rooted in oxidative and inflammatory imbalance.
Comparative Efficacy and Future Directions: Validating Novel Targets and Integrated Treatment Modalities
The interplay between oxidative stress and chronic inflammation is a recognized cornerstone in the pathogenesis of a wide spectrum of diseases, including cardiovascular disorders, neurodegenerative diseases, diabetes, and cancer [2] [80]. This pathophysiological nexus creates a self-sustaining cycle where reactive oxygen species (ROS) activate pro-inflammatory signaling pathways, and conversely, inflammatory cells release additional ROS, exacerbating cellular damage and disease progression [80]. Targeting this vicious cycle presents a fundamental strategy for modern therapeutic intervention.
In the quest to develop effective treatments, the scientific community is actively exploring two parallel avenues: natural products/nutraceuticals and synthetic drug candidates. Natural products, derived from plants, fungi, and other biological sources, offer a diverse array of bioactive compounds, such as polyphenols, flavonoids, and terpenoids, which often exhibit multi-targeted antioxidant and anti-inflammatory effects [109] [110]. Conversely, synthetic compounds are engineered for high potency, specificity, and optimized pharmacokinetic properties [111]. This review provides a head-to-head comparison of these two approaches, evaluating their efficacy, mechanisms, advantages, and limitations within the context of oxidative stress and chronic inflammatory diseases, aiming to inform researchers and drug development professionals.
Molecular Mechanisms and Targets in Oxidative Stress and Inflammation
Key Pathways Linking Oxidative Stress and Inflammation
The interplay between oxidative stress and inflammation is mediated by several critical signaling pathways. Understanding these is prerequisite for evaluating the mechanisms of action of both natural and synthetic compounds.
- The NF-κB Pathway: A primary regulator of inflammation. Inactive NF-κB is sequestered in the cytoplasm by inhibitory proteins (IκB). In response to oxidative stress or inflammatory stimuli, the IκB kinase (IKK) complex is activated, leading to IκB phosphorylation and degradation. This releases NF-κB (typically a p50/p65 heterodimer), allowing it to translocate to the nucleus and induce the transcription of pro-inflammatory genes, including cytokines like TNF-α, IL-1β, and IL-6 [112]. Many natural products, such as curcumin, act by inhibiting IKK or preventing NF-κB nuclear translocation [2].
- The Nrf2/ARE Pathway: A central defender against oxidative stress. Under basal conditions, Nrf2 is bound to its repressor, Keap1, and targeted for degradation. Oxidative stress or electrophilic compounds disrupt this interaction, stabilizing Nrf2. Subsequently, Nrf2 translocates to the nucleus, binds to the Antioxidant Response Element (ARE), and upregulates the expression of a battery of cytoprotective and antioxidant enzymes, including heme oxygenase-1 (HO-1), NAD(P)H quinone dehydrogenase 1 (NQO1), and glutathione peroxidase [113] [2]. Activation of this pathway is a common mechanism for many natural products.
- The NLRP3 Inflammasome Pathway: A key component of the innate immune response. Cellular damage or ROS can activate the NLRP3 inflammasome, a multi-protein complex. Its assembly leads to the cleavage and activation of caspase-1, which in turn processes pro-IL-1β and pro-IL-18 into their active, secreted forms, driving inflammatory cell death (pyroptosis) [112]. This pathway represents a direct molecular link between ROS generation and inflammation.
The following diagram illustrates the core interplay between these pathways and their modulation by therapeutic agents:
Diagram Title: Core Inflammation-Oxidative Stress Pathways and Modulation
Comparative Mechanisms of Action
Natural products and synthetic candidates often engage with these pathways in distinctly different ways, which underpins their comparative therapeutic profiles.
Natural Products: Multi-Target and Synergistic Actions Natural products frequently exert their effects via multi-target mechanisms. For instance, the flavonoid baicalin (from Scutellaria baicalensis) and quercetin have been shown to simultaneously inhibit the NF-κB pathway and activate the Nrf2 pathway, thereby reducing pro-inflammatory cytokine production while enhancing cellular antioxidant defenses [112] [114]. Salidroside from Rhodiola rosea inhibits the release of the high-mobility group box 1 (HMGB1) protein, a late mediator of sepsis, by regulating the AMPK-SirT1 signaling pathway [113]. This polypharmacology is a hallmark of many natural compounds and plant extracts, allowing them to disrupt the inflammation-oxidation cycle at multiple nodes.
Synthetic Drugs: High Potency and Specificity Synthetic antioxidants are often designed for high specificity and potency towards a single target. Edaravone, a approved synthetic antioxidant for ischemic stroke and ALS, functions primarily as a potent radical scavenger, effectively neutralizing hydroxyl radicals and other ROS [111] [80]. Another strategy involves developing inhibitors for specific ROS-generating enzymes, such as NOX (NADPH oxidase) inhibitors like GKT137831, which directly block a major cellular source of superoxide anions [111]. This targeted approach aims to minimize off-target effects but may be less effective against complex, interconnected pathological networks.
Quantitative Efficacy and Safety Profile Comparison
Comparative Clinical and Preclinical Data
The following table synthesizes quantitative data from clinical and preclinical studies, highlighting the relative performance of natural and synthetic antioxidants on key biomarkers.
Table 1: Head-to-Head Comparison of Efficacy in Inflammatory Disease Models
| Compound / Intervention | Study Model | Reduction in ROS | Reduction in CRP | Reduction in TNF-α | Key Molecular Targets |
|---|---|---|---|---|---|
| Natural Antioxidant Blend (e.g., Polyphenols, Flavonoids) | Human RCT (Inflammatory Diseases, n=50) [115] | 53.5% reduction at 6 months | Significant reduction (p=0.02 at 6 months) | Significant reduction (p=0.02 at 6 months) | NF-κB, Nrf2, NLRP3 [2] [112] |
| Synthetic Antioxidants (e.g., BHT, BHA derivatives) | Human RCT (Inflammatory Diseases, n=50) [115] | 40% reduction at 6 months | Less reduction than natural group | Less reduction than natural group | Direct ROS scavenging, NOX inhibition [111] |
| Astaxanthin (Natural) | Preclinical (Mouse UV-induced Keratitis) [113] | Reduced corneal oxidative damage | N/A | Reduced inflammation | Reduced NF-κB positive cells |
| Edaravone (Synthetic) | Clinical (ALS, Ischemic Stroke) [111] [80] | Potent hydroxyl radical scavenger | N/A | N/A | Direct free radical scavenging |
| Berberine, Baicalin (Natural) | Preclinical (Rat Cerebral Ischemia) [113] | Reduced oxidative stress | N/A | Reduced inflammatory response | NF-κB, Nrf2, Autophagy |
CRP: C-reactive protein; TNF-α: Tumor Necrosis Factor-alpha; ROS: Reactive Oxygen Species; RCT: Randomized Controlled Trial; N/A: Data not available in the cited context.
Safety, Bioavailability, and Toxicity
Beyond efficacy, the practical application of therapeutics is governed by their safety and pharmacokinetic profiles.
Table 2: Comparison of Safety, Bioavailability, and Practical Considerations
| Parameter | Natural Products | Synthetic Drug Candidates |
|---|---|---|
| General Safety Profile | Generally favorable, low toxicity [116] | Variable; some show toxicity (e.g., troglitazone withdrawn) [111] |
| Common Limitations | Low oral bioavailability, short half-life, high metabolization [111] | Poor bioavailability for some, potential for off-target toxicity [111] |
| Bioavailability | Often very low (e.g., for many flavonoids) [111] | Generally better by design, but not a universal rule [111] |
| Blood-Brain Barrier (BBB) Penetration | Typically low or negligible [111] | Can be engineered for higher permeability (e.g., specific analogs) [111] |
| Tissue/Organelle Targeting | Low to negligible, with few exceptions (e.g., Ergothioneine) [111] | Better potential, often requiring advanced delivery systems (nanomaterials) [111] |
| Standardization & Quality Control | Major challenge due to complex composition and variability [109] | Straightforward; compounds are well-defined and reproducible [111] |
The data from [115] suggests that natural antioxidants may offer superior efficacy in reducing disease activity scores (DAS28) over a 6-month period. However, [111] critically notes that the therapeutic benefits of many antioxidants, both natural and synthetic, may not always arise from direct antioxidant mechanisms but from secondary effects like anti-inflammatory signaling or gene regulation.
Experimental Protocols for Comparative Analysis
To conduct rigorous head-to-head comparisons of natural and synthetic compounds, standardized experimental workflows are essential. The following protocols are representative of studies cited in this review.
In Vitro Assessment of Antioxidant and Anti-inflammatory Activity
Objective: To evaluate and compare the direct antioxidant capacity and anti-inflammatory effects of natural and synthetic compounds in cell cultures.
Methodology:
- Cell Culture: Use relevant cell lines such as murine macrophage RAW264.7 cells or human liver HepG2 cells. Maintain cells in appropriate media and conditions [113].
- Compound Treatment: Prepare a dose range of natural products (e.g., luteolin-6-C-neohesperidoside, TSG from Polygonum multiflorum) and synthetic candidates (e.g., edaravone, NOX inhibitors). Include a positive control (e.g., a known antioxidant like N-acetylcysteine) and a vehicle control.
- Induction of Oxidative Stress/Inflammation: Challenge cells with an inflammatory stimulus such as bacterial Lipopolysaccharide (LPS) or a pro-oxidant like hydrogen peroxide (H₂O₂).
- Outcome Measures:
- ROS Measurement: Quantify intracellular ROS levels using fluorescent probes like DCFH-DA and measure via flow cytometry or fluorescence microscopy [113].
- Inflammatory Markers: Analyze the production of nitric oxide (NO) using the Griess reagent. Measure levels of cytokines (TNF-α, IL-6) in the culture supernatant via Enzyme-Linked Immunosorbent Assay (ELISA).
- Protein Analysis: Use Western Blotting to assess the activation status of key pathways (e.g., phosphorylation of IκBα for NF-κB, nuclear translocation of Nrf2) [113] [112].
- Gene Expression: Perform Quantitative Polymerase Chain Reaction (qPCR) to measure mRNA levels of antioxidant genes (HO-1, NQO1) and pro-inflammatory genes (TNF-α, IL-1β) [113].
In Vivo Efficacy Study in a Disease Model
Objective: To compare the therapeutic efficacy and safety of natural versus synthetic compounds in a live animal model of inflammatory disease.
Methodology:
- Animal Model: Employ established models such as:
- Grouping and Dosing: Randomize animals into groups: disease model control, natural product treatment (at one or more doses), synthetic drug treatment (at an equivalent dose), and a healthy control. Administer compounds orally or via intraperitoneal injection for a predefined period (e.g., 6 months in a chronic study [115]).
- Data Collection and Analysis:
- Biochemical Analysis: At endpoint, collect blood and tissue samples (e.g., heart, liver, muscle). Measure plasma levels of ROS, CRP, TNF-α, and other relevant markers. Assess tissue levels of lipid peroxidation (e.g., malondialdehyde) and antioxidant enzymes (e.g., glutathione peroxidase) [113] [115].
- Functional and Clinical Assessment: Monitor disease-specific clinical scores (e.g., DAS28 for arthritis). Perform functional tests, such as the forced swimming test for fatigue assessment [113].
- Histopathological Examination: Analyze tissue sections (e.g., of heart, joint, or liver) after staining (e.g., H&E) to evaluate structural damage, inflammatory cell infiltration, and treatment-related protection or toxicity [113].
The workflow for a comprehensive in vivo study is summarized below:
Diagram Title: In Vivo Comparative Efficacy Workflow
The Scientist's Toolkit: Key Research Reagents and Models
This table details essential materials and models used in the experimental studies cited, providing a resource for designing comparable research.
Table 3: Key Research Reagent Solutions for Inflammation and Oxidative Stress Studies
| Reagent / Model Name | Type | Primary Function in Research | Example Context |
|---|---|---|---|
| RAW264.7 Cells | Cell Line | Murine macrophage line; model for studying inflammatory signaling and compound effects on LPS-induced responses. | Used to study the effect of TSG on LPS-induced inflammation [113]. |
| H9c2 Cardiomyocytes | Cell Line | Rat heart myoblast line; model for studying cardioprotection, hypoxia/reoxygenation (H/R) injury. | Used to test Hongjingtian extract on H/R-induced injury [113]. |
| Caecal Ligation and Puncture (CLP) | Animal Model | Gold-standard model for polymicrobial sepsis; used to study systemic inflammation and organ damage. | Used to investigate salidroside's effect on HMGB1 release [113]. |
| DCFH-DA Assay | Chemical Probe | Cell-permeable dye that becomes fluorescent upon oxidation; standard for measuring intracellular ROS. | Used to measure ROS levels in various cell-based studies [113]. |
| LPS (Lipopolysaccharide) | Biochemical Agent | Potent inflammatory stimulant derived from bacterial walls; used to induce robust NF-κB activation and cytokine production in vitro and in vivo. | Used to induce inflammation in RAW264.7 cells and study salidroside [113]. |
| ELISA Kits (TNF-α, IL-6, CRP) | Assay Kit | Immunoassay for precise quantification of specific protein biomarkers in serum, plasma, or culture supernatant. | Used in clinical and preclinical studies to measure inflammatory markers [115]. |
The head-to-head comparison between natural products and synthetic drug candidates reveals a landscape of complementary strengths and weaknesses. Natural products, with their multi-target, synergistic, and generally safe profiles, show great promise in modulating the complex networks of oxidative stress and inflammation, as evidenced by compelling clinical data [115]. However, their widespread adoption is hampered by challenges in standardization, bioavailability, and elucidating precise mechanisms of action. Synthetic candidates offer the advantages of specificity, potency, and reproducible quality, making them suitable for targeted interventions, though they may struggle with efficacy in complex diseases and can carry higher toxicity risks [111].
The future of treating chronic inflammatory diseases likely lies not in choosing one approach over the other, but in integrating their best qualities. Emerging strategies include:
- Semi-synthetic Derivatives: Modifying natural product scaffolds to improve their pharmacokinetic properties, potency, and selectivity [111].
- Advanced Delivery Systems: Employing nanotechnology, polymer complexation, and targeted delivery to enhance the bioavailability and tissue-specific delivery of both natural and synthetic compounds [111] [116].
- Personalized Medicine: Leveraging individual genetic and metabolic profiles to tailor interventions, potentially using nutraceuticals as a foundation for prevention and synthetic drugs for acute management [109].
- Novel Testing Paradigms: Moving beyond simple antioxidant assays to better define the molecular context of antioxidant action in vivo, including which biomolecules are protected and the specific radical species targeted [111].
In conclusion, a synergistic paradigm that harnesses the holistic, system-level effects of natural products and the targeted, potent action of synthetic chemistry holds the greatest potential for developing the next generation of therapies against oxidative stress and chronic inflammation.
Evaluating Multimodal and Combination Therapies for Synergistic Effects
In the landscape of chronic disease pathogenesis, the interplay between oxidative stress and inflammation forms a critical vicious cycle that perpetuates disease progression. Oxidative stress (OS), characterized by an imbalance between pro-oxidant reactive oxygen species (ROS) and antioxidant defenses, synergistically interacts with chronic inflammation, creating a self-amplifying loop that drives conditions such as cardiovascular disorders, neurodegeneration, diabetes, and cancer [3] [2]. This relationship is not merely sequential but bidirectional; oxidative stress activates inflammatory pathways, while inflammatory cells subsequently generate additional ROS, thus sustaining the pathological cascade [3]. Central to this interplay are redox-sensitive transcription factors including Nuclear Factor-kappa B (NF-κB), which promotes inflammation, and Nuclear Factor Erythroid 2-Related Factor 2 (Nrf2), which orchestrates antioxidant responses [3] [2]. The emergence of reductive stress (RS)—a pathological condition marked by excessive reducing equivalents—further complicates this dynamic, demonstrating that both extremes of the redox spectrum can disrupt immune function and contribute to disease pathogenesis [3].
Within this mechanistic framework, combination therapies and multimodal therapeutic approaches offer promising strategies for disrupting this cycle more effectively than single-target interventions. By simultaneously targeting multiple nodes in the oxidative stress-inflammation network, these approaches can produce synergistic effects that enhance efficacy while potentially reducing side effects and delaying resistance development [117] [118]. This technical guide examines current methodologies for evaluating such synergistic interactions, with particular emphasis on computational prediction models, experimental validation protocols, and biomarker assessment strategies that enable researchers to identify and optimize multimodal interventions targeting the oxidative stress-inflammation axis.
Computational Approaches for Synergy Prediction
Multi-Modal Data Integration Frameworks
Advanced computational approaches have revolutionized the prediction of synergistic drug combinations by integrating diverse data modalities that capture complementary aspects of drug action and disease biology. These frameworks typically incorporate: (1) drug structural information represented via molecular fingerprints, SMILES strings, or molecular graphs; (2) cell line characteristics including gene expression profiles, multi-omics data, and protein-protein interaction networks; and (3) biological network context such as drug-target interactions and disease-associated pathways [117] [118]. The MCDSP (Multi-modal Contrastive Drug Synergy Prediction) model exemplifies this approach by extracting both biomolecular features and entity embedding features from heterogeneous graphs, then employing contrastive learning to align these different modality features toward effective components for synergy prediction [117]. Similarly, MultiSyn integrates multi-omics data with biological networks and drug molecular features containing pharmacophore information, utilizing a semi-supervised attributed graph neural network to construct comprehensive cell line representations [118].
These multi-modal approaches address critical limitations of single-modality models by capturing the complex, higher-order relationships between drug properties, cellular contexts, and biological networks that underlie synergistic interactions. The Pisces framework further enhances predictive capability through data augmentation, creating multiple views for each drug pair based on different modalities and expanding the original data 64 times, which has demonstrated state-of-the-art results on both cell-line-based and xenograft-based drug synergy predictions [119]. This multi-modal paradigm is particularly relevant for targeting the oxidative stress-inflammation axis, as it enables modeling of compounds that might simultaneously modulate redox balance (e.g., through Nrf2 activation) and inflammatory pathways (e.g., through NF-κB inhibition).
Key Computational Methods and Architectures
Table 1: Computational Methods for Drug Synergy Prediction
| Method | Architecture | Data Modalities | Key Innovation |
|---|---|---|---|
| MCDSP [117] | Multi-modal contrastive learning | Molecular fingerprints, gene expression, heterogeneous graphs | Single modality guidance with contrastive learning for feature alignment |
| MultiSyn [118] | Graph neural network + transformer | Multi-omics, PPI networks, pharmacophore fragments | Integration of pharmacophore information with biological networks |
| Pisces [119] | Multi-modal data augmentation | Drug modalities, cell line features | Expands data 64x by creating multiple views for each drug pair |
| DeepSynergy [118] | Deep neural network | Molecular structure, genomic data | Early DL model integrating molecular and genomic data |
| DTSyn [118] | Transformer encoder | Chemical substructures, gene associations | Captures interactions among chemical substructures and gene associations |
Experimental Design and Validation Methodologies
In Vitro Synergy Screening Protocols
Robust experimental validation of predicted synergistic combinations requires standardized methodologies that quantitatively measure combination effects beyond additive expectations. The following protocol outlines a comprehensive approach for in vitro synergy screening, particularly relevant for combinations targeting oxidative stress and inflammation pathways:
Cell Line Selection and Culture Conditions:
- Select relevant cell lines representing disease models (e.g., cancer cell lines from CCLE for oncology, endothelial cells for cardiovascular inflammation) [117] [118].
- Culture cells according to standard conditions with appropriate media, supplements, and atmospheric conditions (typically 37°C, 5% CO₂).
- Ensure logarithmic growth phase at time of compound addition through proper seeding density and timing.
Compound Preparation and Treatment:
- Prepare individual compound stocks in appropriate vehicles (DMSO, ethanol, or aqueous solutions based on solubility).
- Design combination matrices using fixed-ratio or checkerboard designs spanning relevant concentration ranges (typically 0.1×IC₅₀ to 10×IC₅₀).
- Include appropriate controls: vehicle controls, positive controls (known synergistic combinations), and negative controls (single agents alone).
Viability Assessment and Synergy Quantification:
- Measure cell viability/response using validated assays (MTT, CellTiter-Glo, etc.) at appropriate endpoint (typically 72-144 hours post-treatment).
- Calculate combination indices (CI) using the Chou-Talalay method [118]:
- CI < 0.9 indicates synergy
- CI = 0.9-1.1 indicates additive effect
- CI > 1.1 indicates antagonism
- Alternatively, use Bliss independence or Loewe additivity models for synergy quantification.
- Perform dose-reduction analysis to determine potential for toxicity reduction.
Oxidative Stress and Inflammation-Specific Endpoints:
- For combinations targeting OS/inflammation axis, include additional endpoints:
- ROS measurement using fluorescent probes (DCFH-DA, MitoSOX)
- Antioxidant enzyme activities (SOD, catalase, GPx)
- Inflammatory cytokine profiling (IL-6, IL-1β, TNF-α) via ELISA or multiplex assays
- NF-κB and Nrf2 activation assays (reporter gene assays, nuclear translocation imaging)
Biomarker Validation in Complex Models
Advancing synergistic combinations beyond initial in vitro validation requires comprehensive biomarker assessment in more physiologically relevant models. Key biomarkers for evaluating therapies targeting oxidative stress and inflammation include:
Table 2: Biomarkers for Assessing Oxidative Stress and Inflammation Modulation
| Biomarker Category | Specific Markers | Detection Methods | Biological Significance |
|---|---|---|---|
| Lipid Peroxidation | MDA, F2-isoprostanes, 4-HNE | TBARS assay, GC-MS/MS, HPLC-MS/MS | Indicates oxidative damage to cellular membranes [120] [121] [70] |
| DNA Oxidation | 8-OHdG | HPLC-ECD, ELISA, HPLC-MS/MS | Reflects oxidative DNA damage [121] [70] |
| Protein Oxidation | Protein carbonyls | DNPH derivatization, immunoblotting | Measures oxidative protein modification [70] |
| Antioxidant Enzymes | SOD, catalase, GPx | Activity assays, Western blot | Endogenous antioxidant capacity [2] [70] |
| Inflammatory Cytokines | IL-6, IL-1β, TNF-α, IFN-γ | ELISA, multiplex immunoassays | Pro-inflammatory signaling status [121] [122] |
| Acute Phase Proteins | CRP, SAA | Immunoturbidimetry, ELISA | Systemic inflammation [121] |
| Redox-Sensitive Transcription Factors | NF-κB, Nrf2 | EMSA, nuclear fractionation, reporter assays | Activation status of key pathways [3] [121] |
Signaling Pathways in Oxidative Stress and Inflammation
Diagram 1: Oxidative Stress-Inflammation Signaling Network. This diagram illustrates the key molecular pathways connecting oxidative stress sources to inflammatory responses, highlighting potential intervention points for combination therapies.
Experimental Workflow for Synergy Evaluation
Diagram 2: Experimental Workflow for Synergy Evaluation. This workflow outlines the integrated computational-experimental approach for identifying and validating synergistic combinations targeting oxidative stress and inflammation.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Synergy Studies Targeting Oxidative Stress and Inflammation
| Reagent Category | Specific Examples | Application/Function | Technical Notes |
|---|---|---|---|
| ROS Detection Probes | DCFH-DA, MitoSOX Red, DHE | Detection of intracellular ROS, mitochondrial superoxide | Validate with positive controls (e.g., H₂O₂, antimycin A) [70] |
| Antioxidant Enzyme Assays | SOD, catalase, GPx activity kits | Quantification of endogenous antioxidant capacity | Normalize to protein content; consider isoform-specific assays [121] [70] |
| Lipid Peroxidation Assays | TBARS, F2-isoprostanes by GC/MS | Measurement of oxidative lipid damage | F2-isoprostanes considered gold standard [121] [70] |
| Protein Oxidation Assays | Protein carbonyl detection kits | Assessment of oxidative protein modifications | DNPH derivatization with spectrophotometric or immunodetection [70] |
| DNA Damage Detection | 8-OHdG ELISA, COMET assay | Quantification of oxidative DNA damage | HPLC-ECD/MS offers higher specificity than ELISA [121] [70] |
| Cytokine Profiling | Multiplex cytokine panels, ELISA | Comprehensive inflammation assessment | Include both pro-inflammatory and anti-inflammatory cytokines [121] |
| Pathway Reporters | NF-κB, Nrf2, ARE reporter cells | Monitoring pathway activation | Luciferase-based systems for high-throughput screening [3] [2] |
| Cell Viability Assays | MTT, CellTiter-Glo, Annexin V | Assessment of cytotoxicity and apoptosis | Use multiple methods for confirmation [118] |
The evaluation of multimodal and combination therapies for synergistic effects represents a paradigm shift in targeting complex pathological processes like the oxidative stress-inflammation axis in chronic diseases. The integrated computational-experimental framework outlined in this guide provides a systematic approach for identifying and validating synergistic combinations that simultaneously modulate multiple nodes in these interconnected pathways. As the field advances, several emerging trends promise to further enhance this approach: the development of more sophisticated multi-modal machine learning models that can better integrate diverse data types; the incorporation of patient-derived organoids and complex coculture systems for more physiologically relevant screening; and the implementation of standardized biomarker panels that can robustly assess both oxidative stress and inflammation modulation in clinical trials. By adopting these comprehensive evaluation strategies, researchers can more effectively develop combination therapies that disrupt the self-perpetuating cycle of oxidative stress and inflammation, ultimately leading to more effective treatments for chronic diseases characterized by these pathological processes.
The interplay between oxidative stress and inflammation constitutes a fundamental pathway in the pathogenesis of numerous chronic diseases. This whitepaper examines three emerging classes of therapeutic targets—sirtuins, immunometabolic modulators, and redox enzyme mimetics—that operate at this critical interface. We provide a comprehensive analysis of their molecular mechanisms, highlighting how sirtuins function as NAD+-dependent deacetylases that integrate metabolic and inflammatory signals, how immunometabolic reprogramming dictates immune cell function, and how novel biomimetic enzymes offer innovative approaches to redox regulation. Structured tables summarize key quantitative data, while detailed experimental protocols and visualization scripts support translational research applications. The collective evidence positions these targets as promising avenues for therapeutic intervention in conditions ranging from metabolic diseases to cancer and age-related pathologies.
Oxidative stress, characterized by an imbalance between reactive oxygen species (ROS) production and antioxidant defenses, synergistically interacts with inflammatory pathways to drive the progression of chronic diseases [2]. ROS, including superoxide anion (O₂•⁻), hydrogen peroxide (H₂O₂), and hydroxyl radicals (OH•), function as signaling molecules that activate pro-inflammatory cascades, while inflammatory cells themselves generate additional ROS, creating a self-perpetuating cycle of cellular damage [2] [123]. This vicious cycle contributes to pathological manifestations in cardiovascular disorders, neurodegeneration, diabetes, and cancer [2]. Within this framework, sirtuins have emerged as critical regulators of cellular homeostasis, acting as redox-sensitive enzymes that modulate both oxidative stress and inflammatory responses [124] [123]. Concurrently, the field of immunometabolism has revealed that metabolic reprogramming controls immune cell activation and differentiation, thereby influencing inflammatory outcomes [125] [126]. Most recently, advances in bioinspired catalysis have yielded novel redox enzyme mimetics that replicate the functional architecture of natural enzymes while offering enhanced stability and tunability [127]. This whitepaper explores the therapeutic targeting of these interconnected systems, providing researchers with mechanistic insights, experimental approaches, and clinical perspectives.
Sirtuins: Masters of Redox and Metabolic Integration
Sirtuins (SIRT1-7) constitute a family of NAD+-dependent deacetylases that have gained prominence for their roles in longevity, stress resistance, and metabolic homeostasis [124] [128]. These enzymes are localized to specific subcellular compartments: SIRT1, SIRT6, and SIRT7 reside primarily in the nucleus; SIRT2 is cytosolic; and SIRT3, SIRT4, and SIRT5 are mitochondrial [129] [128]. Their NAD+ dependence positions sirtuins as exquisite sensors of cellular energy status and redox balance, as the NAD+/NADH ratio reflects the metabolic state of the cell [123]. During caloric restriction, increased NAD+ availability activates sirtuins, enhancing stress resistance and maintaining metabolic homeostasis [124] [128]. Conversely, conditions of nutrient excess decrease NAD+ levels, contributing to metabolic dysfunction. Beyond their classical deacetylase activity, certain sirtuins (e.g., SIRT4 and SIRT5) also demonstrate ADP-ribosyltransferase and other deacylase activities, expanding their regulatory scope [124].
Table 1: Mammalian Sirtuins: Localization, Functions, and Redox Connections
| Sirtuin | Subcellular Localization | Primary Activities | Redox-Related Functions | Key Molecular Targets |
|---|---|---|---|---|
| SIRT1 | Nucleus | Deacetylase | FOXO activation, PGC-1α-mediated mitochondrial biogenesis, NF-κB inhibition | p53, FOXOs, PGC-1α, NF-κB |
| SIRT2 | Cytosol | Deacetylase | FOXO activation, regulation of oxidative stress pathways | FOXO3a |
| SIRT3 | Mitochondria | Deacetylase | SOD2 activation, IDH2 activation, fatty acid oxidation | SOD2, IDH2, AceCS2 |
| SIRT4 | Mitochondria | ADP-ribosyltransferase | Regulation of insulin secretion, glutamate metabolism | GDH |
| SIRT5 | Mitochondria | Demalonylase, Desuccinylase | Ammonia detoxification, fatty acid oxidation | CPS1 |
| SIRT6 | Nucleus | ADP-ribosyltransferase, Deacetylase | DNA repair, NF-κB inhibition, glucose metabolism | NF-κB, HIF-1α |
| SIRT7 | Nucleolus | Deacetylase | Regulation of rRNA synthesis, stress responses | p53 |
Molecular Mechanisms Linking Sirtuins to Antioxidant Defense
Sirtuins modulate cellular redox balance through multiple mechanisms, including direct regulation of antioxidant enzymes and control of transcription factors governing antioxidant gene expression. SIRT3, the primary mitochondrial deacetylase, directly deacetylates and activates manganese superoxide dismutase (SOD2), enhancing mitochondrial capacity to neutralize superoxide radicals [128]. SIRT3 also deacetylates and activates isocitrate dehydrogenase 2 (IDH2), promoting NADPH production that maintains reduced glutathione, a crucial cellular antioxidant [128]. In the nucleus, SIRT1 deacetylates and activates transcription factors belonging to the FOXO family, particularly FOXO3a, which induces expression of genes encoding SOD2, catalase, and other antioxidant proteins [124] [123]. Additionally, SIRT1 deacetylates and co-activates PGC-1α, a master regulator of mitochondrial biogenesis and antioxidant gene expression [128]. Through these coordinated actions across cellular compartments, sirtuins enhance the cell's ability to counteract oxidative stress.
Experimental Approaches for Sirtuin Research
Protocol: Assessing SIRT1 Activity in Cell Culture Models
- Cell Treatment: Seed appropriate cells (e.g., HEK293, HepG2) in 6-well plates. Treat with compounds of interest (e.g., resveratrol [1-50 μM], SRT1720 [0.1-5 μM], EX527 [1-10 μM]) for predetermined timepoints (typically 6-48 hours).
- Cell Lysis: Harvest cells in lysis buffer (50 mM Tris-HCl pH 8.0, 150 mM NaCl, 1 mM EDTA, 0.5% NP-40, 1 mM DTT) supplemented with protease inhibitors and 1 μM trichostatin A (class I/II HDAC inhibitor).
- Immunoprecipitation: Incubate cell lysates with SIRT1-specific antibody overnight at 4°C. Capture immune complexes with protein A/G beads.
- Activity Assay: Perform deacetylase activity measurement using fluorogenic substrates (e.g., Ac-p53 peptide) in reaction buffer (50 mM Tris-HCl pH 8.0, 4 mM MgCl₂, 0.5 mM DTT, 0.25 mM NAD+) for 30-60 minutes at 37°C.
- Quantification: Measure fluorescence (excitation 360 nm, emission 460 nm) and normalize to SIRT1 protein levels determined by western blotting.
Protocol: Evaluating Mitochondrial ROS in SIRT3-Knockout Cells
- Cell Preparation: Utilize wild-type and SIRT3-knockout MEFs or primary cells.
- Staining: Load cells with 5 μM MitoSOX Red in HBSS for 30 minutes at 37°C.
- Stimulation: Treat cells with oxidative stress inducers (e.g., 100-500 μM H₂O₂) if required.
- Analysis: Analyze by flow cytometry or fluorescence microscopy. For flow cytometry, use excitation/emission of 510/580 nm.
- Validation: Confirm mitochondrial specificity with mitochondrial uncouplers (e.g., FCCP) and correlate with SIRT3 status by western blotting.
Diagram Title: SIRT1-Mediated Antioxidant Pathway
Immunometabolic Modulators: Reprogramming Immune Responses
Metabolic Control of Immune Cell Function
Immunometabolism investigates the intricate connections between metabolic pathways and immune cell function [125] [126]. Immune cells undergo metabolic reprogramming upon activation, with different metabolic preferences distinguishing immune cell subsets and their functional states [125]. Pro-inflammatory macrophages (M1) primarily utilize aerobic glycolysis (the Warburg effect) for rapid energy generation, while anti-inflammatory macrophages (M2) rely more on oxidative phosphorylation and fatty acid oxidation [125]. Similarly, effector T cells engage glycolysis for proliferation and cytokine production, whereas regulatory T cells utilize lipid oxidation [125]. These metabolic pathways do not merely supply energy but also provide metabolites that serve as signaling molecules and epigenetic modifiers, influencing gene expression and cell fate decisions [130]. Key regulatory nodes in these metabolic pathways, including HIF-1α, mTOR, and AMPK, integrate environmental cues to direct immune responses, making them attractive therapeutic targets.
Table 2: Metabolic Pathways in Immune Cell Activation
| Immune Cell Type | Activation State | Preferred Metabolic Pathway | Key Metabolites | Functional Outcomes |
|---|---|---|---|---|
| Macrophage | M1 (Pro-inflammatory) | Aerobic glycolysis, PPP | Succinate, Citrate | IL-1β, TNF-α production, antimicrobial activity |
| Macrophage | M2 (Anti-inflammatory) | Oxidative phosphorylation, FAO | α-ketoglutarate, NAD+ | IL-10, tissue repair |
| Dendritic Cell | Activated | Aerobic glycolysis | Acetyl-CoA | Antigen presentation, cytokine production |
| T cell (Effector) | Activated | Aerobic glycolysis | Lactate | Proliferation, IFN-γ production |
| T cell (Regulatory) | Activated | Fatty acid oxidation | NAD+ | Immunosuppression, IL-10 production |
Sirtuins at the Immunometabolic Intersection
Sirtuins serve as critical bridges connecting metabolic sensing to immune regulation. SIRT1 deacetylates the p65 subunit of NF-κB, thereby inhibiting this master pro-inflammatory transcription factor and reducing expression of cytokines like TNF-α and IL-6 [130]. SIRT2 deacetylates and modulates the activity of glycolytic enzymes, potentially influencing the metabolic reprogramming of immune cells [130]. In macrophages, SIRT6 suppresses HIF-1α activity, reducing glycolysis and steering cells toward a more quiescent metabolic state [130]. These regulatory functions position sirtuins as promising targets for modulating immunometabolism in disease contexts, including autoimmune conditions, metabolic syndrome, and cancer.
Experimental Protocols for Immunometabolism Research
Protocol: Assessing Metabolic Reprogramming in Macrophages
- Cell Differentiation and Polarization: Differentiate THP-1 cells or primary human monocytes into macrophages with 100 ng/mL PMA for 48 hours. Polarize toward M1 phenotype with 100 ng/mL LPS + 20 ng/mL IFN-γ for 24 hours, or toward M2 phenotype with 20 ng/mL IL-4 for 24 hours.
- Metabolic Profiling:
- Glycolytic Rate: Measure extracellular acidification rate (ECAR) using Seahorse XF Analyzer. Perform Glycolysis Stress Test with sequential injection of glucose, oligomycin, and 2-DG.
- Mitochondrial Function: Measure oxygen consumption rate (OCR) using Seahorse XF Analyzer. Perform Mito Stress Test with sequential injection of oligomycin, FCCP, and rotenone/antimycin A.
- Metabolite Extraction: Use 80% methanol/water at -80°C for intracellular metabolite extraction.
- Metabolomic Analysis: Employ LC-MS/MS for targeted quantification of TCA cycle intermediates, amino acids, and nucleotides.
Protocol: Evaluating SIRT1 Role in T Cell Metabolism
- T Cell Isolation and Culture: Isolate naive CD4+ T cells from mouse spleen or human PBMCs using magnetic bead separation.
- Genetic/Pharmacological Manipulation: Treat cells with SIRT1 activators (resveratrol, SRT1720) or inhibitors (EX527), or use SIRT1-deficient cells.
- Activation and Differentiation: Activate cells with anti-CD3/CD28 beads and polarize toward Th1 (IL-12 + anti-IL-4), Th17 (TGF-β + IL-6), or Treg (TGF-β) phenotypes.
- Metabolic Assessment: Analyze glucose uptake (2-NBDG), mitochondrial mass (MitoTracker), and membrane potential (TMRE) by flow cytometry.
- Functional Assays: Measure cytokine production (ELISA/flow cytometry) and proliferation (CFSE dilution).
Diagram Title: Immunometabolic Circuit in Macrophage Polarization
Redox Enzyme Mimetics: Biomimetic Therapeutic Approaches
Design Principles for Enzyme Mimetics
Redox enzyme mimetics are synthetic catalysts designed to replicate the functional attributes of natural enzymes while overcoming limitations such as poor stability, high production costs, and limited tunability [127]. These materials typically incorporate redox-active metal centers that mimic the catalytic cores of natural metalloenzymes. Recent advances have focused on creating synergistic structures that incorporate both redox-active metals (functioning as electron transfer centers) and redox-inert metals (acting as Lewis acids to modulate substrate binding and transition state stabilization) [127]. This biomimetic approach was exemplified in the development of MₓV₂O₅·nH₂O nanostructures, where vanadium serves as the redox site and intercalated alkaline-earth metals (Mg²⁺, Ca²⁺, Sr²⁺) function as Lewis acids, mimicking the natural peroxidase architecture that contains both heme iron and calcium ions [127].
Table 3: Redox Enzyme Mimetics: Types and Applications
| Mimetic Type | Catalytic Metal | Natural Enzyme Counterpart | Therapeutic Applications | Key Advantages |
|---|---|---|---|---|
| MₓV₂O₅·nH₂O nanobelts | Vanadium (V) + Alkaline-earth metals (Mg²⁺, Ca²⁺, Sr²⁺) | Peroxidase (Fe³⁺/Ca²⁺) | Antibacterial wound dressings, ROS-scavenging | Tunable activity based on Lewis acidity, high stability |
| CeO₂ nanoparticles | Cerium (Ce³⁺/Ce⁴⁺) | Catalase/SOD | Radioprotection, neurodegenerative diseases | Self-regenerating antioxidant, multi-enzyme mimic |
| Metal-organic frameworks (MOFs) | Various transition metals | Multiple oxidoreductases | Drug delivery, diagnostic sensing | High surface area, modular design |
| Single-atom catalysts | Fe, Mn, Cu | Cytochrome P450, SOD | Targeted cancer therapy, inflammatory diseases | Maximum atom utilization, well-defined active sites |
Experimental Methodology for Mimetic Evaluation
Protocol: Synthesis and Characterization of MₓV₂O₅·nH₂O Nanobelts
- Synthesis:
- Dissolve V₂O₅ powder (1 g) in H₂O₂ (30 mL, 30%) with stirring for 30 minutes.
- Add alkaline-earth metal chloride (MgCl₂·6H₂O, CaCl₂, or SrCl₂·6H₂O) in molar ratio 1:2 (V:M).
- Transfer to Teflon-lined autoclave and heat at 180°C for 24-72 hours.
- Collect precipitate by centrifugation, wash with ethanol/water, and dry at 60°C.
- Structural Characterization:
- XRD: Confirm crystal structure and phase purity.
- SEM/TEM: Analyze morphology and dimensions.
- XPS: Determine oxidation states and oxygen vacancy concentration.
- Peroxidase Activity Assessment:
- Prepare reaction mixture containing mimetic (50 μg/mL), H₂O₂ (0.5-5 mM), and TMB (0.4 mM) in acetate buffer (pH 4.0).
- Monitor absorbance at 652 nm for 10 minutes.
- Calculate kinetic parameters (Kₘ, Vₘₐₓ) using Lineweaver-Burk plot.
Protocol: Antibacterial Efficacy Testing of Enzyme Mimetics
- Bacterial Culture: Grow Gram-positive (S. aureus) and Gram-negative (E. coli) bacteria to mid-log phase in LB broth.
- Treatment: Incubate bacteria (10⁶ CFU/mL) with mimetics (0-200 μg/mL) in presence of low H₂O₂ (50 μM) for 6 hours at 37°C.
- Viability Assessment:
- CFU Counting: Plate serial dilutions on LB agar and count colonies after 24 hours.
- ROS Detection: Stain with DCFH-DA (10 μM) and measure fluorescence.
- Morphological Analysis: Examine bacterial membrane integrity by SEM after fixation with glutaraldehyde.
Diagram Title: Biomimetic Enzyme Design Principle
Integrated Therapeutic Applications and Research Tools
Cross-Target Therapeutic Strategies
The interconnected nature of sirtuin signaling, immunometabolic pathways, and redox homeostasis suggests promising opportunities for combination therapies. Sirtuin activators may precondition tissues to better withstand oxidative stress, while redox enzyme mimetics could directly neutralize excess ROS in inflammatory environments [124] [127]. Simultaneously, immunometabolic modulators might redirect immune cell differentiation toward less inflammatory phenotypes in conditions like atherosclerosis, neurodegenerative diseases, and cancer [125] [130]. For example, in age-related diseases, SIRT1 activators could enhance stress resistance while enzyme mimetics compensate for declining endogenous antioxidant defenses. In cancer therapy, sirtuin inhibitors might sensitize tumor cells to chemotherapy while enzyme mimetics protect healthy tissues from off-target toxicity. The optimal therapeutic approach will likely involve context-specific combinations that consider disease stage, tissue microenvironment, and individual metabolic characteristics.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents for Target Validation
| Reagent Category | Specific Examples | Key Applications | Mechanistic Insights |
|---|---|---|---|
| SIRT Activators | Resveratrol, SRT1720, SRT2183, NAD+ precursors (NMN, NR) | Enhance sirtuin activity, mimic caloric restriction effects | FOXO activation, mitochondrial biogenesis, reduced inflammation |
| SIRT Inhibitors | Nicotinamide (NAM), EX527, sirtinol, AGK2 | Probe sirtuin functions, potential cancer therapeutics | Increased acetylation of targets, modulated stress responses |
| Metabolic Modulators | 2-DG (glycolysis inhibitor), Metformin (AMPK activator), Etomoxir (CPT1 inhibitor) | Redirect immunometabolic pathways, alter immune cell polarization | Shift between glycolysis and OXPHOS, altered cytokine production |
| Enzyme Mimetics | MₓV₂O₅·nH₂O nanobelts, CeO₂ nanoparticles, MOF-based catalysts | Scavenge or generate ROS, antibacterial applications | Biomimetic catalysis, modulation of redox signaling |
| Reporter Systems | ARE-luciferase, NF-κB-GFP, ROS-sensitive dyes (DCFH-DA, MitoSOX) | Real-time monitoring of pathway activation, high-throughput screening | Quantification of oxidative stress and inflammatory activation |
The therapeutic targeting of sirtuins, immunometabolic pathways, and redox enzymes represents a promising frontier in the management of chronic diseases driven by oxidative stress and inflammation. As master regulators of cellular homeostasis, sirtuins integrate metabolic and inflammatory signals, offering targets for interventions that could simultaneously address multiple pathological processes. The growing understanding of immunometabolism reveals that immune cell function can be modulated by targeting their metabolic preferences, opening possibilities for fine-tuning immune responses. Meanwhile, advances in nanotechnology and biomimetic catalysis have yielded novel enzyme mimetics with potent and tunable redox-regulating capacities. Future research directions should include the development of tissue-specific delivery systems for these therapeutics, personalized approaches based on individual metabolic and inflammatory profiles, and sophisticated combination strategies that simultaneously target multiple nodes in the oxidative stress-inflammation network. The integration of these approaches holds significant promise for breaking the cycle of oxidative damage and inflammation that drives progression of many chronic diseases.
Validation of Emerging Biomarkers for Early Diagnosis and Treatment Monitoring
The validation of emerging biomarkers represents a critical frontier in the battle against chronic diseases, many of which are fueled by the complex interplay between oxidative stress and inflammation. Oxidative stress, resulting from an imbalance between reactive oxygen species (ROS) production and antioxidant defenses, is a major factor in the pathogenesis of chronic conditions including cardiovascular disorders, neurodegeneration, diabetes, and cancer [2]. This redox imbalance establishes a synergistic relationship with inflammation, creating a pathogenic loop that sustains chronic disease progression [5]. Within this physiological context, biomarkers have evolved from simple diagnostic tools to essential instruments for early detection, prognostic assessment, and therapeutic monitoring.
The traditional approach of discussing oxidative stress and inflammatory pathways separately has limited translational impact, creating a pressing need for integrated analytical frameworks [2]. This technical guide addresses the entire biomarker validation pipeline, with particular emphasis on emerging biomarkers that can detect molecular signatures of oxidative stress and inflammation at the earliest stages of disease pathogenesis. By connecting molecular mechanisms with clinical evidence, we aim to provide researchers and drug development professionals with a comprehensive resource for developing robust, clinically applicable biomarkers that reflect the bidirectional nature of redox dysregulation in chronic diseases [5].
Biomarker Classes and Their Clinical Applications in Chronic Inflammatory Diseases
Biomarkers in the context of oxidative stress and inflammation can be categorized into multiple classes, each with distinct clinical applications and validation considerations. Table 1 summarizes the major biomarker categories, their molecular correlates, and primary clinical utilities, with special attention to their roles in diseases driven by oxidative stress and inflammation.
Table 1: Biomarker Classes for Early Diagnosis and Treatment Monitoring
| Biomarker Class | Key Examples | Molecular Correlates | Primary Clinical Utilities |
|---|---|---|---|
| Genetic Biomarkers | Circulating tumor DNA (ctDNA), SNP variants | Somatic mutations, genetic polymorphisms | Cancer detection, risk stratification, therapy selection [131] [132] |
| Transcriptomic Biomarkers | MicroRNAs (miR-122, miR-34a), non-coding RNAs | Gene expression signatures, regulatory RNA networks | Early disease detection, monitoring treatment response [131] [133] |
| Proteomic Biomarkers | Cytokines (IL-6), CRP, RCAS1, CT antigens | Inflammatory signaling, oxidative stress responses | Disease activity monitoring, therapeutic targeting [2] [131] |
| Metabolomic Biomarkers | Lipid peroxidation products, glutathione ratios | Redox balance, metabolic pathway activity | Assessment of oxidative stress, antioxidant capacity [2] [5] |
| Cellular Biomarkers | Circulating tumor cells (CTCs), immune cell subsets | Cellular heterogeneity, immune system activation | Liquid biopsy, immunotherapy monitoring [132] |
The clinical utility of these biomarkers is particularly evident in their ability to detect oxidative stress-related pathological processes before overt clinical symptoms emerge. For instance, redox imbalance disrupts cellular signaling, biomolecular functionality, and structural integrity, leading to significant functional alterations that can be captured through specific biomarker signatures [5]. Elevated ROS levels influence the activity of redox-sensitive transcription factors such as NF-κB, which drives the expression of adhesion molecules, cytokines, chemokines, and matrix metalloproteinases (MMPs) – many of which serve as measurable biomarkers of inflammatory progression [5].
Biomarker Validation Methodologies: From Discovery to Clinical Implementation
Analytical Validation: Establishing Robust Assay Performance
Analytical validation ensures that biomarker assays generate reliable, reproducible results that meet predefined performance standards. This process must address several key parameters, as outlined in Table 2, which summarizes the essential performance characteristics for biomarker assays used in detecting oxidative stress and inflammatory signatures.
Table 2: Essential Performance Characteristics for Biomarker Assays
| Performance Characteristic | Definition | Acceptance Criteria | Considerations for Oxidative Stress Biomarkers |
|---|---|---|---|
| Precision | Consistency of repeated measurements | CV < 20-30% depending on application [134] | High priority in biotech due to impact on data turnaround times and cost-efficiency [135] |
| Accuracy | Closeness to true value | Recovery 85-115% | Affected by rapid degradation of labile oxidative stress markers |
| Sensitivity | Lowest detectable concentration | Sufficient for biological range | Must detect physiological vs. pathological redox states [5] |
| Specificity | Ability to measure target exclusively | No cross-reactivity with analogs | Critical for distinguishing similar oxidative modifications |
| Dynamic Range | Concentration interval with validated performance | Cover expected physiological and pathological levels | Must accommodate fluctuating oxidative stress levels |
| Stability | Resistance to preanalytical variations | Defined freeze-thaw, storage conditions | Particularly important for redox equilibrium biomarkers |
The balance between assay precision and sensitivity often tilts toward precision in biomarker validation, as precision significantly impacts data turnaround times, cost-efficiency, and experimental repeats [135]. For clinical or commercial use assays, automation features help provide the rigor of documentation and traceability necessary for passing audits against regulatory standards (e.g., GLP, GMP, ISO) [135].
Experimental Protocols for Key Biomarker Assays
Circulating Tumor DNA (ctDNA) Analysis for Cancer Detection
Principle: ctDNA fragments released from tumor cells contain cancer-specific genetic alterations that can be detected in blood samples, providing a non-invasive method for cancer detection and monitoring [131] [132].
Workflow:
- Sample Collection: Collect whole blood in cell-stabilization tubes to prevent leukocyte lysis and contamination with genomic DNA.
- Plasma Separation: Centrifuge at 1600 × g for 10 minutes at 4°C, followed by a second centrifugation at 16,000 × g for 10 minutes to remove residual cells.
- DNA Extraction: Isolate cell-free DNA using silica membrane-based kits, with elution in low-EDTA TE buffer.
- Library Preparation: Use unique molecular identifiers (UMIs) to label original DNA molecules before amplification to distinguish true mutations from PCR errors.
- Sequencing Analysis: Perform next-generation sequencing with coverage of 10,000× or higher for sensitive mutation detection.
- Bioinformatic Processing: Apply UMI-aware pipelines to call variants with allele frequencies as low as 0.1%.
Key Considerations: Preanalytical variables significantly impact ctDNA quality; standardized protocols are essential. Challenges include low concentration and fragmentation of ctDNA, as well as clearance mechanisms [131].
Oxidative Stress Biomarker Panel Assessment
Principle: Multiplexed assessment of oxidative stress markers provides a comprehensive profile of redox status in chronic inflammatory diseases [2] [5].
Workflow:
- Sample Collection: Collect plasma, serum, or tissue samples with antioxidants (butylated hydroxytoluene) for lipid peroxidation markers.
- Biomarker Extraction: Deproteinize samples using acid precipitation or solid-phase extraction.
- Multiplex Analysis:
- Lipid Peroxidation Products: Measure MDA and 4-HNE using HPLC with fluorescence detection.
- Protein Carbonyls: Detect after derivatization with 2,4-dinitrophenylhydrazine using ELISA or Western blot.
- Antioxidant Enzymes: Assess SOD, catalase, and GPX activities using kinetic assays.
- Redox Status: Determine GSH/GSSG ratio using LC-MS/MS with stable isotope-labeled internal standards.
- Data Integration: Combine multiple parameters into a unified oxidative stress index.
Key Considerations: Rapid processing is critical due to the instability of many oxidative stress markers. Simultaneous measurement of multiple biomarkers provides a more reliable assessment than individual markers [2].
Clinical Validation: Establishing Disease Relevance
Clinical validation establishes the relationship between the biomarker and clinical endpoints of interest. This process must account for the intended use context—whether for early detection, prognosis, or treatment monitoring [134]. For biomarkers related to oxidative stress and inflammation, several specific considerations apply:
Within-Subject Correlation: When multiple observations are collected from the same subject, there is a distinct possibility of correlated results. Analyzing such data assuming independent observations will almost surely inflate the type I error rate and result in spurious findings of significance [136]. Mixed-effects linear models, which account for a dependent variance-covariance structure within subjects, should be employed to analyze biomarker data with repeated measures [136].
Multiplicity Concerns: Biomarker validation studies are sensitive to false positives because the list of potential markers is characteristically extensive. The probability of concluding that there is at least one statistically significant effect across a set of tests when in fact no effect exists increases with each additional test; therefore, it is necessary to control or limit the type I error rate [136]. Methods such as false discovery rate (FDR) control should be implemented when validating multiple biomarkers simultaneously.
Selection Bias: Retrospective biomarker studies may suffer from selection bias, the same as any retrospective observational study. Clinical validation cohorts should include samples with different subtypes and disease stages to ensure generalizability [134]. For oxidative stress biomarkers, it is particularly important to include controls matched for factors known to influence redox status, including age, comorbidities, and medications.
Technological Platforms for Biomarker Validation
The selection of appropriate technological platforms is crucial for successful biomarker validation. Table 3 provides a comparative overview of major platforms used for different biomarker classes, with particular emphasis on their applicability to oxidative stress and inflammation biomarkers.
Table 3: Technology Platforms for Biomarker Validation
| Platform Category | Example Platforms | Key Advantages | Limitations | Suitable Biomarker Classes |
|---|---|---|---|---|
| Genomics | Next-Generation Sequencing, RT-PCR, qPCR | High sensitivity, comprehensive mutation profiling | Expensive, complex data analysis for NGS | Genetic biomarkers, ctDNA [135] |
| Proteomics | ELISA, Meso Scale Discovery (MSD), Luminex | High specificity, quantitative, multiplex capabilities | Limited multiplexing for ELISA, expensive for MSD | Cytokines, inflammatory mediators [135] |
| Metabolomics | LC-MS/MS, GC-MS | Broad profiling capability, captures dynamic changes | Technical complexity, requires specialized expertise | Oxidative stress markers, metabolic signatures [2] |
| Cellular Analysis | Flow cytometry, single-cell RNA sequencing | Single-cell resolution, functional assessment | Expensive, complex data analysis | Immune cell subsets, CTCs [135] |
Generally, ELISA and qPCR platforms tend to be the most straightforward and widely used for biomarker validation due to their established protocols and relative cost-effectiveness [135]. However, for more complex biomarker profiles involving multiple analytes or requiring spatial resolution, platforms with multiplexing capabilities or spatial biology approaches are preferable.
Automation plays an increasingly important role in biomarker validation, improving consistency, reliability, and reproducibility of results while enabling higher throughput and standardization [135]. Automated systems can be scaled up or down depending on the volume of samples and assay requirements, which supports validation scenarios that may require testing under multiple conditions or with large patient cohorts.
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful biomarker validation requires carefully selected reagents and materials that ensure assay robustness and reproducibility. The following table details essential research reagent solutions for validating biomarkers in oxidative stress and inflammatory contexts.
Table 4: Essential Research Reagents for Biomarker Validation
| Reagent Category | Specific Examples | Primary Function | Technical Considerations |
|---|---|---|---|
| Sample Stabilization | Cell-free DNA BCT tubes, protease inhibitors, antioxidants | Preserve sample integrity during collection and storage | Critical for labile oxidative stress biomarkers [134] |
| Nucleic Acid Analysis | UMI adapters, targeted sequencing panels, digital PCR assays | Enable sensitive detection of genetic alterations | UMIs essential for distinguishing true mutations from artifacts [132] |
| Protein Detection | Phospho-specific antibodies, cytokine arrays, oxidation-sensitive probes | Detect post-translational modifications and inflammatory mediators | Validation of antibody specificity is crucial [134] |
| Separation Media | Immunoaffinity columns, HPLC columns, magnetic beads | Isolate specific analyte classes from complex mixtures | Reduce matrix effects in mass spectrometry analyses |
| Signal Amplification | Electrochemiluminescence reagents, enzyme substrates, fluorescent dyes | Enhance detection sensitivity | Balance between sensitivity and dynamic range [135] |
| Reference Materials | Synthetic biomarkers, pooled control sera, certified reference materials | Quality control and assay standardization | Essential for inter-laboratory reproducibility [134] |
Signaling Pathways in Oxidative Stress and Inflammation
Biomarkers frequently reflect alterations in key signaling pathways that connect oxidative stress with inflammatory responses. The NF-κB pathway represents a prime example of a redox-sensitive signaling cascade that can be monitored through specific biomarker signatures.
Diagram 1: NF-κB Activation by Oxidative Stress. This pathway illustrates how reactive oxygen and nitrogen species (ROS/RNS) activate IκB kinase (IKK), leading to phosphorylation and degradation of IκB proteins, nuclear translocation of NF-κB, and subsequent transcription of pro-inflammatory genes. Biomarkers targeting various points in this pathway provide insights into inflammatory status and oxidative stress levels.
The Nrf2-Keap1 pathway represents another critical system that can be monitored through biomarkers, serving as a protective mechanism against oxidative stress.
Diagram 2: Nrf2-Keap1 Antioxidant Pathway. This diagram shows the mechanism by which oxidative stress modifies cysteine residues on Keap1, leading to Nrf2 release, nuclear translocation, and activation of antioxidant gene expression. Biomarkers of Nrf2 pathway activity provide valuable indicators of cellular antioxidant capacity.
Biomarker Validation Workflow
The validation of emerging biomarkers follows a structured pathway from discovery to clinical implementation, with iterative refinement at each stage. The following workflow diagram outlines this multi-step process with specific considerations for biomarkers of oxidative stress and inflammation.
Diagram 3: Biomarker Validation Workflow. This flowchart illustrates the sequential phases of biomarker validation, highlighting key statistical and methodological considerations at each stage. The process requires addressing preanalytical standardization during analytical validation, and accounting for multiplicity and within-subject correlation during clinical validation.
The validation of emerging biomarkers for early diagnosis and treatment monitoring represents a paradigm shift in managing chronic diseases characterized by oxidative stress and inflammation. By employing rigorous analytical methodologies, accounting for statistical challenges, and leveraging advanced technological platforms, researchers can translate promising biomarker candidates into clinically useful tools. The integration of biomarker development with our growing understanding of redox biology and inflammatory signaling will ultimately enable more precise interventions for inflammation-related diseases, moving beyond descriptive summaries to functional assessment of disease mechanisms and therapeutic responses. As the field advances, the successful validation of biomarkers that capture the dynamic interplay between oxidative stress and inflammation will be essential for developing targeted therapies that restore redox homeostasis and modulate inflammatory responses in chronic diseases.
Gaps in Knowledge and Future Research Imperatives for Translational Success
The interplay between oxidative stress and inflammation represents a core pathogenic axis in numerous chronic diseases, including cardiovascular disorders, neurodegeneration, diabetes, and cancer [62] [2]. Despite decades of research demonstrating compelling mechanistic links in preclinical models, translational success has been remarkably limited. The fundamental hypothesis that therapeutic manipulation of this axis would yield clinical benefits has generated mostly disappointing results, with many antioxidant and anti-inflammatory therapies failing in late-stage clinical trials [137]. This whitepaper examines the critical gaps in knowledge impeding translational success and outlines essential future research imperatives required to bridge this chasm.
The oxidative stress-inflammation interface is characterized by self-amplifying feedback loops. Reactive oxygen species (ROS) activate redox-sensitive transcription factors such as nuclear factor kappa-B (NF-κB), leading to increased expression of pro-inflammatory cytokines, adhesion molecules, and enzymes like cyclooxygenase-2 (COX-2) [55]. Conversely, inflammatory mediators stimulate additional ROS production from immune and non-immune cells, creating a vicious cycle of tissue damage and chronic disease progression [2] [55]. This intricate crosstalk represents both a compelling therapeutic target and a source of profound translational complexity.
Critical Knowledge Gaps
Insufficient Understanding of Context-Dependent ROS Signaling
A fundamental gap lies in the continued treatment of ROS as universally detrimental, despite their dual role as damaging agents and essential signaling molecules [137] [55]. The context-dependent nature of ROS signaling—where the same molecule can exert protective or pathogenic effects depending on its source, concentration, spatial localization, and temporal dynamics—remains poorly characterized in human disease.
- Spatiotemporal Dynamics: Current biomarkers and therapeutic approaches largely fail to account for the compartmentalized nature of redox signaling. The biological effects of mitochondrial versus NADPH oxidase-derived ROS differ significantly, yet most measurement approaches provide only systemic, tissue-level assessments [137]. The diffusion distance of specific oxidants varies dramatically; for example, the diffusion distance of H₂O₂ decreases from approximately 1.5 mm to 1.5 μm in the presence of physiological levels of peroxiredoxin 2, highlighting the importance of subcellular microenvironments [138].
- Hormetic Responses: The biphasic dose-response relationship (hormesis) observed in redox signaling is not adequately incorporated into therapeutic design. Low-level ROS exposure can activate adaptive stress response pathways (e.g., NRF2), while higher levels cause damage [137]. Therapeutic strategies have typically aimed for maximal antioxidant effects without considering potential disruption of essential redox signaling.
Limitations in Biomarker Development and Validation
The field suffers from a critical shortage of clinically validated biomarkers that can accurately quantify oxidative stress and inflammation within specific tissues and cellular compartments in humans [139] [140].
- Static versus Dynamic Measurements: Most available biomarkers (e.g., lipid peroxidation products, protein carbonylation) provide static snapshots of cumulative damage rather than dynamic measures of flux through specific pathways [139]. This limitation hinders assessment of therapeutic target engagement and pathway modulation in clinical trials.
- Lack of Specificity and Sensitivity: Existing biomarkers often lack the specificity to distinguish between different ROS/RNS species and the sensitivity to detect early, pathogenic changes before irreversible tissue damage occurs [139] [140]. For neurodegenerative diseases, emerging biomarkers like neurofilament light chain (NfL) and glial fibrillary acidic protein (GFAP) show promise for early detection but require further validation [140].
Table 1: Limitations of Current Biomarker Approaches
| Biomarker Category | Representative Examples | Key Limitations | Clinical Implications |
|---|---|---|---|
| Lipid Peroxidation | MDA, 4-HNE, F2-isoprostanes | Lack pathway specificity; influenced by diet; measure damage rather than flux | Limited utility for target engagement in clinical trials |
| Protein Oxidation | Protein carbonylation, nitrotyrosine | Technically challenging to measure; poor stability in stored samples | Difficult to standardize across clinical sites |
| Antioxidant Capacity | Total antioxidant capacity, glutathione levels | Does not reflect compartmentalized redox status | Poor correlation with clinical outcomes |
| Inflammatory Mediators | CRP, IL-6, TNF-α | Not specific to oxidative stress-driven inflammation | Cannot identify oxidative stress-specific pathophysiology |
Inadequate Preclinical Models and Therapeutic Delivery
The translational failure of antioxidants highlights critical deficiencies in preclinical modeling and therapeutic delivery [138] [137].
- Disease Relevance: Many animal models do not adequately recapitulate the chronic, multi-factorial nature of human diseases driven by oxidative stress and inflammation. Studies often use acute challenges rather than modeling the slow progression of human conditions, potentially overlooking adaptive mechanisms [137].
- Bioavailability and Targeting: The poor bioavailability and lack of tissue specificity of many antioxidant compounds limit their efficacy [137] [55]. For instance, despite potent in vitro effects, natural polyphenols like curcumin and resveratrol often demonstrate limited clinical efficacy due to poor absorption, rapid metabolism, and inadequate tissue distribution [2] [55].
The Antioxidant Paradox and Clinical Trial Design
The "antioxidant paradox"—where compounds with potent antioxidant activity in vitro show limited or even harmful effects in vivo—remains incompletely understood [138] [137]. Several factors contribute to this paradox:
- Chemical versus Biological Antioxidants: A chemical that is a potent antioxidant in a defined system may be ineffective or even pro-oxidant in a biological context [138]. The nitrone compound PBN, for example, shows only modest antioxidant activity in lipid peroxidation assays but demonstrates powerful biological effects in disease models involving ROS [138].
- Inadequate Dosing and Timing: Clinical trials often extrapolate dosing from acute models to chronic diseases without rigorous pharmacokinetic-pharmacodynamic characterization in the target population [137]. The timing of intervention may also be critical, as many trials initiate treatment after established disease rather than targeting early pathogenic processes.
Future Research Imperatives
Develop Precision Targeting Strategies
Future research must prioritize the development of compartment- and pathway-specific interventions rather than systemic antioxidant approaches.
- Mitochondria-Targeted Antioxidants: Compounds like MitoQ represent a promising approach for targeting the primary cellular source of ROS [55]. Research should expand on this concept by developing tools to target other ROS-producing compartments and specific enzyme systems.
- NRF2 Activators: The transcription factor NRF2 orchestrates the expression of numerous antioxidant and cytoprotective genes. Developing specific NRF2 activators that avoid the pitfalls of previous compounds represents a promising avenue [62] [55]. The reciprocal regulation between NRF2 and NF-κB requires careful investigation for therapeutic manipulation [55].
- Advanced Delivery Systems: Nanoparticle-based delivery systems can enhance the bioavailability, tissue specificity, and intracellular distribution of antioxidants [55]. Future work should focus on designing systems that respond to the specific redox environment of diseased tissues.
Implement Multi-Omics and Systems Biology Approaches
Overcoming translational barriers requires a shift from reductionist to systems-level approaches that capture the complexity of redox-inflammatory networks.
- Redox Proteomics and Metabolomics: Advanced mass spectrometry techniques can map specific oxidative post-translational modifications on proteins and quantify redox-active metabolites, providing unprecedented insight into pathway activity [139].
- Single-Cell Analysis: Applying single-cell RNA sequencing and proteomics to clinical samples can reveal cell-type-specific oxidative and inflammatory responses currently masked in bulk tissue analyses [141].
- Computational Modeling: Developing quantitative models that simulate redox-inflammatory networks can help predict therapeutic responses, identify critical control points, and design combination therapies that account for pathway redundancies [55].
Advance Clinical Trial Design and Biomarker Implementation
Transformative changes in clinical trial methodology are essential for demonstrating efficacy in human populations.
- Precision Enrollment Strategies: Future trials should incorporate biomarkers to enroll patients with evidence of oxidative stress pathology rather than relying solely on clinical diagnoses [140] [137]. This approach would create more homogeneous populations likely to respond to targeted interventions.
- Biomarker-Driven Endpoints: Clinical trials must integrate mechanism-based biomarkers as secondary endpoints to demonstrate target engagement and pathway modulation, even if primary clinical endpoints are not met [137]. This strategy would provide critical proof-of-concept for future development.
- Combination Therapy Approaches: Given the network nature of oxidative stress and inflammation, monotherapies may be insufficient. Rational combination strategies should be explored, potentially targeting complementary pathways such as ROS production and inflammatory signaling simultaneously [62] [55].
Table 2: Essential Components of Next-Generation Clinical Trials
| Trial Component | Current Standard | Future Imperative | Implementation Challenge |
|---|---|---|---|
| Patient Selection | Based on clinical diagnosis alone | Biomarker-enriched populations (e.g., elevated oxidative stress markers) | Validation of predictive biomarkers |
| Dosing Strategy | Often based on maximum tolerated dose | Biomarker-informed dose selection to achieve target modulation | Understanding relationship between dose and pathway modulation |
| Trial Endpoints | Primarily clinical endpoints | Composite endpoints including target engagement biomarkers | Regulatory acceptance of biomarker endpoints |
| Therapeutic Approach | Mostly monotherapy | Rational combination therapies | Intellectual property and development complexity |
| Trial Duration | Often short-term in chronic diseases | Longer duration to detect disease modification | Cost and patient retention |
Focus on Early Intervention and Prevention
The most promising opportunity for impacting chronic diseases may lie in early intervention before irreversible tissue damage occurs [140].
- Biomarker Development for Early Detection: Research should prioritize discovering and validating biomarkers that can identify oxidative stress and inflammation at the earliest stages of disease pathogenesis [140]. For neurodegeneration, this includes further development of fluid biomarkers like NfL and GFAP [140].
- Personalized Prevention Strategies: Integrating redox and inflammatory biomarkers with genetic, epigenetic, and exposure data could enable personalized risk assessment and targeted preventive interventions [141].
Experimental Approaches and Methodologies
Protocol for Assessing Redox Signaling in Preclinical Models
Aim: To comprehensively evaluate the effects of experimental interventions on compartment-specific redox signaling and inflammatory responses.
Workflow:
- Intervention Administration: Administer test compound (e.g., NRF2 activator, mitochondria-targeted antioxidant) in established disease model.
- Tissue Collection and Subcellular Fractionation: Collect target tissues and separate into mitochondrial, cytoplasmic, nuclear, and membrane fractions.
- Redox Status Assessment:
- Measure glutathione redox couple (GSH/GSSG) in each fraction via HPLC.
- Quantify specific oxidative post-translational modifications (e.g., cysteine oxidations) via redox proteomics.
- Assess lipid peroxidation products (4-HNE, F2-isoprostanes) via LC-MS/MS.
- Inflammatory Pathway Analysis:
- Measure activation of NF-κB, MAPK, and JAK-STAT pathways via phosphoprotein analysis.
- Quantify cytokine production (IL-1β, IL-6, TNF-α) via multiplex immunoassays.
- Functional and Transcriptomic Assessment:
- Evaluate NRF2 activation and antioxidant gene expression via RNA sequencing.
- Assess functional outcomes (e.g., mitochondrial respiration, tissue histopathology).
Experimental Workflow for Redox Signaling Assessment
Protocol for Clinical Target Engagement Studies
Aim: To demonstrate that candidate therapeutics engage their intended molecular targets in human subjects and modulate relevant pathways.
Design: Randomized, placebo-controlled trial incorporating biomarker assessments.
Population: Patients with early evidence of target pathology (e.g., elevated oxidative stress biomarkers).
Intervention: Candidate therapeutic at multiple dose levels versus placebo.
Key Assessments:
- Primary Endpoint: Change from baseline in target-specific biomarker (e.g., NRF2 target gene expression for NRF2 activators).
- Secondary Endpoints:
- Changes in oxidative stress biomarkers specific to targeted pathway.
- Modulation of inflammatory mediators downstream of targeted pathway.
- Pharmacokinetic-pharmacodynamic relationships.
- Safety and tolerability.
Methodologies:
- Transcriptomic Analysis: RNA sequencing of peripheral blood mononuclear cells or target tissue biopsies to assess pathway modulation.
- Redox Metabolomics: Comprehensive profiling of redox-active metabolites and oxidation products.
- Molecular Imaging: When available, use of novel PET tracers to assess target engagement in specific tissues.
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Research Tools for Studying Redox-Inflammatory Interactions
| Research Tool Category | Specific Examples | Primary Research Application | Key Considerations |
|---|---|---|---|
| ROS Detection Probes | MitoSOX, H2DCFDA, Amplex Red | Detection of specific ROS in cellular and subcellular compartments | Varying specificity for different ROS; potential artifacts |
| NRF2 Pathway Modulators | Sulforaphane, Bardoxolone methyl, KEAP1 inhibitors | Activation of antioxidant response element pathway | Varying selectivity; potential off-target effects |
| Mitochondria-Targeted Antioxidants | MitoQ, SkQ1, MitoTEMPO | Specific targeting of mitochondrial ROS | Effects on mitochondrial function beyond antioxidant activity |
| NF-κB Pathway Inhibitors | BAY-11-7082, SC-514, IKK-16 | Inhibition of pro-inflammatory signaling | Specificity for different NF-κB activation pathways |
| Genetic Models | NRF2 knockout, NOX knockout mice, NRF2/KEAP1 mutant models | Investigation of specific pathway functions in disease contexts | Compensation during development; tissue-specific effects |
| Oxidized Lipid Standards | 4-HNE, 15-F2t-IsoP, 7-KC, oxLDL | Quantification of lipid peroxidation products | Stability during sample processing; analytical standardization |
Bridging the translational gap in oxidative stress and inflammation research requires a fundamental shift in approach. The historical focus on non-specific antioxidant therapies must give way to precision targeting of specific redox pathways and inflammatory processes within their biological context. Success will depend on developing more sophisticated biomarkers, implementing systems-level analyses, redesigning clinical trials, and focusing on early intervention strategies. By addressing these research imperatives, the field can overcome current limitations and realize the long-promised potential of targeting the oxidative stress-inflammation axis for therapeutic benefit in chronic diseases.
Conclusion
The intricate interdependence of oxidative stress and inflammation is no longer a peripheral observation but a central paradigm in understanding and treating chronic diseases. Moving forward, the field must transition from a one-size-fits-all antioxidant approach to sophisticated, biomarker-guided personalized medicine. Future success hinges on developing multimodal interventions that simultaneously disrupt the self-amplifying oxidative-inflammatory loop. This includes advancing targeted delivery systems, validating combination therapies that activate endogenous defense mechanisms like the Nrf2 pathway, and integrating multi-omics data for precise patient stratification. By embracing these strategies, biomedical research can translate the profound insights of redox biology into the next generation of effective clinical therapies for a wide spectrum of chronic conditions.
References
- 1. Reactive Oxygen Species in Inflammation and Tissue Injury [https://pmc.ncbi.nlm.nih.gov/articles/PMC3929010/]
- 2. Exploring the Interplay of Antioxidants, Inflammation, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12469104/]
- 3. Redox Imbalance in Inflammation: The Interplay of Oxidative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12189482/]
- 4. Reactive oxygen species (ROS) scavenging biomaterials ... [https://jhoonline.biomedcentral.com/articles/10.1186/s13045-023-01512-7]
- 5. Redox Imbalance in Inflammation: The Interplay of ... [https://www.mdpi.com/2076-3921/14/6/656]
- 6. NF-κB signaling in inflammation [https://www.nature.com/articles/sigtrans201723]
- 7. NF-κB in biology and targeted therapy - Nature [https://www.nature.com/articles/s41392-024-01757-9]
- 8. NF-κB in Oxidative Stress - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5978768/]
- 9. Cell Type-Specific Roles of NF-κB Linking Inflammation ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2019.00085/full]
- 10. Decoding the Redox Code of Ischemic Stroke ... [https://www.mdpi.com/1422-0067/26/22/10835]
- 11. The Anti-Inflammatory and Anti-Oxidant Mechanisms of the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6538222/]
- 12. The Molecular Mechanisms Regulating the KEAP1-NRF2 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7296212/]
- 13. The KEAP1-Cullin3-RBX1-Nrf2 Axis in Redox Homeostasis [https://pubmed.ncbi.nlm.nih.gov/41206404/]
- 14. The Role of NRF2/KEAP1 Signaling Pathway in Cancer ... [https://www.mdpi.com/1422-0067/22/9/4376]
- 15. Nrf2 and Oxidative Stress: A General Overview of ... [https://www.mdpi.com/2076-3921/11/12/2345]
- 16. Keap1-Nrf2 pathway: a key mechanism in the occurrence ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2024.1381467/full]
- 17. Nrf2/Keap1/ARE regulation by plant secondary metabolites [https://biosignaling.biomedcentral.com/articles/10.1186/s12964-024-01878-2]
- 18. Druggable genome CRISPR screening identifies the ... [https://www.nature.com/articles/s42003-025-08983-z]
- 19. The Role of P62/Nrf2/Keap1 Signaling Pathway in Lead ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12413483/]
- 20. The role of Keap1-Nrf2 signaling pathway in the treatment ... [https://www.sciencedirect.com/science/article/pii/S2405844024133579]
- 21. Dissecting the Crosstalk Between Nrf2 and NF-κB ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2021.809952/full]
- 22. Dissecting the Crosstalk Between Nrf2 and NF-κB Response ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8847224/]
- 23. Dissecting molecular cross-talk between Nrf2 and NF-κB ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4613495/]
- 24. The crosstalk between Nrf2 and NF-κB pathways in ... [https://www.sciencedirect.com/science/article/abs/pii/S0024320523006422]
- 25. An Nrf2-NF-κB Crosstalk Controls Hepatocyte Proliferation ... [https://www.sciencedirect.com/science/article/pii/S2352345X25000219]
- 26. Transcription Factors NRF2 and NF-κB Are Coordinated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4140883/]
- 27. The Regulation of the NF-κB p65 and Nrf2/HO-1 Signaling ... [https://www.mdpi.com/2304-8158/14/10/1746]
- 28. Divulging the Intricacies of Crosstalk Between NF-Kb and Nrf2 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7938034/]
- 29. A Comprehensive Overview of the Complex Role ... [https://www.frontiersin.org/journals/aging-neuroscience/articles/10.3389/fnagi.2022.827900/full]
- 30. Oxidative stress, aging, and diseases - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC5927356/]
- 31. Aging and aging-related diseases: from molecular ... [https://www.nature.com/articles/s41392-022-01251-0]
- 32. Targeting Oxidative Stress Biomarkers in Breast Cancer Development and the Potential Protective Effect of Phytochemicals [https://www.mdpi.com/2813-2998/4/2/23]
- 33. Clinical Relevance of Biomarkers of Oxidative Stress - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4657513/]
- 34. Oxidative–Inflammatory Crosstalk and Multi-Target Natural ... [https://www.mdpi.com/1467-3045/47/8/614]
- 35. Identification and validation of oxidative stress-related ... [https://www.dovepress.com/identification-and-validation-of-oxidative-stress-related-diagnostic-m-peer-reviewed-fulltext-article-JIR]
- 36. Association of DNA damage response signals and oxidative stress status with nivolumab efficacy in patients with Head and Neck Squamous Cell Carcinoma - PubMed [https://pubmed.ncbi.nlm.nih.gov/40410274/]
- 37. Classifying oxidative stress by F2-Isoprostane levels in human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5413206/]
- 38. Oxidative Stress Fundamentals [https://www.mdpi.com/2076-3417/15/18/10191]
- 39. Protein Carbonylation as a Biomarker of Oxidative Stress and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10603858/]
- 40. Biomarkers in ROS and Role of Isoprostanes in Oxidative ... [https://www.intechopen.com/chapters/52087]
- 41. Serum levels of protein carbonyl, a marker of oxidative stress ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7364609/]
- 42. 8-Hydroxy-2-Deoxyguanosine as Oxidative DNA Damage ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8236100/]
- 43. Detection of 8-OHdG as a diagnostic biomarker - Korkmaz [https://jlpm.amegroups.org/article/view/4605/html]
- 44. 8-Hydroxydeoxyguanosine as a biomarker of oxidative ... [https://www.sciencedirect.com/science/article/pii/S2214750017300306]
- 45. Linking oxidative biomarkers to stress progression and... disease [https://pmc.ncbi.nlm.nih.gov/articles/PMC12146192/]
- 46. Redox regulation: mechanisms, biology and therapeutic ... [https://www.nature.com/articles/s41392-024-02095-6]
- 47. Using Redox Proteomics to Gain New Insights into ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10812581/]
- 48. PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC5857282/]
- 49. A UPLC-MS/MS method for the determination of oxidative ... [https://www.sciencedirect.com/science/article/abs/pii/S0891584921011709]
- 50. Development of a HPLC-MS/MS Method for Assessment ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8384703/]
- 51. Electron paramagnetic resonance spectroscopy in radiation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3147108/]
- 52. Electron paramagnetic resonance (EPR) for investigating ... [https://www.sciencedirect.com/science/article/pii/S2773176623000081]
- 53. Principles of Electron Paramagnetic Resonance ... [https://link.springer.com/chapter/10.1007/978-1-4615-5081-5_2]
- 54. Flavonoids and their role in oxidative stress, inflammation, ... [https://www.sciencedirect.com/science/article/pii/S000927972500119X]
- 55. Therapeutic Strategies Targeting Oxidative Stress and ... [https://www.mdpi.com/2673-6411/5/4/35]
- 56. Flavonoids and their role in oxidative stress, inflammation, ... [https://pubmed.ncbi.nlm.nih.gov/40147618/]
- 57. Synthetic and semi-synthetic antioxidants in medicine and ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1599816/full]
- 58. Cordycepin alleviates renal ischemia-reperfusion injury by ... [https://www.sciencedirect.com/science/article/abs/pii/S1567576925002541]
- 59. Cordycepin combined with antioxidant effects improves ... [https://www.nature.com/articles/s41598-025-92790-3]
- 60. Cordyceps Sinensis Reduces Inflammation and Protects ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11930259/]
- 61. Cordyceps militaris extract and cordycepin ameliorate LPS- ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1530098/full]
- 62. Exploring the Interplay of Antioxidants, Inflammation, and ... [https://pubmed.ncbi.nlm.nih.gov/41002745/]
- 63. Gut Microbiota Modulation Through Mediterranean Diet Foods [https://pmc.ncbi.nlm.nih.gov/articles/PMC11944315/]
- 64. A Comprehensive Review of the Triangular Relationship ... [https://www.mdpi.com/1422-0067/26/18/8785]
- 65. Multi-omics integration reveals the impact of mediterranean ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1644014/full]
- 66. Mediterranean Diet Reduces Inflammation in Adults [https://pubmed.ncbi.nlm.nih.gov/41211687/]
- 67. The effects of the mediterranean diet supplemented with olive ... [https://nutritionandmetabolism.biomedcentral.com/articles/10.1186/s12986-025-00947-8]
- 68. Dietary Patterns, Oxidative Stress, and Early Inflammation [https://www.mdpi.com/2072-6643/17/3/548]
- 69. Editorial: The role of oxidative stress and systemic ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2023.1272525/full]
- 70. Linking oxidative stress biomarkers to disease progression ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1611842/full]
- 71. Inflammation and Oxidative Stress Biomarkers in Heavy ... [https://pubmed.ncbi.nlm.nih.gov/40813054/]
- 72. New Molecular Mechanisms and Markers in Inflammatory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12249654/]
- 73. Clinical trial designs incorporating predictive biomarkers [https://pmc.ncbi.nlm.nih.gov/articles/PMC4737867/]
- 74. MarkerPredict: predicting clinically relevant ... [https://www.nature.com/articles/s41540-025-00603-0]
- 75. Unlocking the Power of Digital Biomarkers in Clinical Trials [https://acrpnet.org/2025/08/19/unlocking-the-power-of-digital-biomarkers-in-clinical-trials]
- 76. Free radicals and their impact on health and antioxidant ... [https://www.nature.com/articles/s41420-024-02278-8]
- 77. Oxidative stress and inflammation in the pathogenesis of ... [https://www.sciencedirect.com/science/article/pii/S2211383524004040]
- 78. Vitamin E (α-Tocopherol): Emerging Clinical Role and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11891505/]
- 79. The unmet promise: a critical review of antioxidant ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1693441/full]
- 80. Potential use of antioxidants for the treatment of chronic ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2024.1378335/full]
- 81. Antioxidants, Volume 14, Issue 9 (September 2025) [https://www.mdpi.com/2076-3921/14/9]
- 82. Antioxidant effects of vitamin E and risk of cardiovascular ... [https://www.sciencedirect.com/science/article/pii/S0261561422001510]
- 83. Frontiers | Plant-based bioactives and oxidative stress in reproduction: anti-inflammatory and metabolic protection mechanisms [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1650347/full]
- 84. Opportunities and challenges in enhancing the bioavailability and bioactivity of dietary flavonoids: A novel delivery system perspective - PubMed [https://pubmed.ncbi.nlm.nih.gov/37566979/]
- 85. Nanotechnology-based Delivery Systems for Enhanced Bioavailability of Antioxidant Compounds in Fruits and Vegetables [https://www.foodandnutritionjournal.org/vol13nospl-issue-phytonutrients-2025/nanotechnology-based-delivery-systems-for-enhanced-bioavailability-of-antioxidant-compounds-in-fruits-and-vegetables/]
- 86. Methodologies for Improving Antioxidant Properties and ... [https://www.mdpi.com/2076-3921/14/11/1290]
- 87. Innovations in Drug Delivery Systems for Antioxidant ... [https://www.mdpi.com/journal/antioxidants/special_issues/YZ45B800L0]
- 88. Bridging the Gap: The Role of Advanced Formulation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12579833/]
- 89. Does the Interdependence between Oxidative Stress and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4736408/]
- 90. Mitochondrial-targeted antioxidant MitoQ provides ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6038061/]
- 91. How does MitoQ work – the mechanism of action [https://www.mitoq.com/blogs/journal/how-does-mitoq-work-the-mitoq-mechanism-of-action?srsltid=AfmBOorNDvqP-xDDQX2aSKeoWrnbfn-N72EsajoQkG1plGsnbO6IthBs]
- 92. The mitochondrially targeted antioxidant MitoQ protects ... [https://www.nature.com/articles/s41419-018-0436-x]
- 93. Chronic supplementation with a mitochondrial antioxidant ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5945293/]
- 94. mitoquinol mesylate research studies & clinical trials [https://www.mitoq.com/pages/research?srsltid=AfmBOooFnzqHX_zv6WlNhjV8EBPrE99UmOi77aOD89NUeAl-bJ5Ex9Ab]
- 95. Advancements in mitochondrial-targeted nanotherapeutics [https://pmc.ncbi.nlm.nih.gov/articles/PMC11524880/]
- 96. Unlocking the Mitochondria for Nanomedicine-based ... [https://www.sciencedirect.com/science/article/pii/S0169409X24000176]
- 97. Current Landscape of NRF2 Biomarkers in Clinical Trials - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7464243/]
- 98. NFE2L2 - Wikipedia [https://en.wikipedia.org/wiki/NFE2L2]
- 99. Frontiers | Nrf2 signaling pathway: current status and potential therapeutic targetable role in human cancers [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2023.1184079/full]
- 100. The Nrf2-Antioxidant Response Element Signaling Pathway and Its Activation by Oxidative Stress - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2679427/]
- 101. Hemorrhage-activated NRF2 in tumor-associated ... [https://www.jci.org/articles/view/174528]
- 102. A pan-cancer analysis shows immunoevasive ... [https://www.sciencedirect.com/science/article/pii/S2213231723000459]
- 103. The Association of Redox Regulatory Drug Target Genes with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11047424/]
- 104. The KEAP1–NRF2 System as a Molecular Target of Cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7795874/]
- 105. Redox platforms in cancer drug discovery and development [https://www.sciencedirect.com/science/article/abs/pii/S1367593110001559]
- 106. Association of single-nucleotide polymorphisms of the ... [https://www.sciencedirect.com/science/article/abs/pii/S1043661818307825]
- 107. A Novel FACS-Based Workflow for Simultaneous Assessment of... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9355044/]
- 108. Frontiers | Redox confers T cell-exclusion... phenotype [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1676797/abstract]
- 109. Natural products and nutraceuticals in the management of ... [https://pubmed.ncbi.nlm.nih.gov/40960578/]
- 110. Bioactive Natural and Synthetic Products in Human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11479150/]
- 111. Synthetic and semi-synthetic antioxidants in medicine and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12321848/]
- 112. Frontiers | Natural alleviate viral pneumonia by modulating... products [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1657829/full]
- 113. Targeting on Natural and Products ... Oxidative Stress Inflammation [https://pmc.ncbi.nlm.nih.gov/articles/PMC5818944/]
- 114. Editorial: Therapeutic potential of natural products in ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2024.1375788/full]
- 115. Comparative Study of Synthetic vs. Natural Antioxidants in ... [https://healthcare-bulletin.co.uk/article/comparative-study-of-synthetic-vs-natural-antioxidants-in-inflammatory-diseases-2536/]
- 116. Harnessing nutrients and natural products for sustainable ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1579266/full]
- 117. Multi-modal contrastive drug synergy prediction model guided ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12465304/]
- 118. Accurate prediction of synergistic drug combination using a ... [https://bmcbiol.biomedcentral.com/articles/10.1186/s12915-025-02302-y]
- 119. Pisces: A multi-modal data augmentation approach for ... [https://www.sciencedirect.com/science/article/pii/S2666979X2500148X]
- 120. Biomarkers of Oxidative Stress in Acute and Chronic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9495828/]
- 121. Common and Novel Markers for Measuring Inflammation and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8001241/]
- 122. Biomarkers of chronic inflammation in disease ... [https://www.nature.com/articles/ni.3828]
- 123. The Role of Sirtuins in Antioxidant and Redox Signaling [https://pmc.ncbi.nlm.nih.gov/articles/PMC5824489/]
- 124. The role of sirtuins in modulating redox stressors - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3253188/]
- 125. Metabolic regulation of the immune system in health and ... [https://www.nature.com/articles/s41392-024-01954-6]
- 126. Immunometabolism: Where Immunology and Metabolism Meet [https://pmc.ncbi.nlm.nih.gov/articles/PMC8787520/]
- 127. Biomimetic synergistic effect of redox site and Lewis acid for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11282276/]
- 128. The sirtuins, oxidative stress and aging: an emerging link [https://www.aging-us.com/article/100544/text]
- 129. Oxidative stress and inflammation regulation of sirtuins [https://pmc.ncbi.nlm.nih.gov/articles/PMC9437461/]
- 130. Metabolic mechanisms orchestrated by Sirtuin family to ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1448535/full]
- 131. Emerging biomarkers for early cancer detection and diagnosis [https://pmc.ncbi.nlm.nih.gov/articles/PMC12359849/]
- 132. Emerging biomarkers for non-invasive diagnosis and ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2024.1405267/full]
- 133. Emerging Biomarkers for Early Detection and Prognosis of ... [https://pubmed.ncbi.nlm.nih.gov/41114480/]
- 134. Biomarker Validation - an overview [https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/biomarker-validation]
- 135. Precision-Driven Biomarker Validation: A Biotech ... [https://www.criver.com/eureka/precision-driven-biomarker-validation-biotech-perspective-part-i]
- 136. Biomarker Validation: Common Data Analysis Concerns [https://pmc.ncbi.nlm.nih.gov/articles/PMC4122484/]
- 137. Targeting oxidative stress in disease: promise and ... [https://www.nature.com/articles/s41573-021-00233-1]
- 138. Translational Research Involving Oxidative Stress and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3156308/]
- 139. Biomarkers and Mechanisms of Oxidative Stress—Last 20 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8347360/]
- 140. The Interplay of Homeostasis, Inflammation, and Oxidative ... [https://www.frontiersin.org/journals/aging-neuroscience/articles/10.3389/fnagi.2025.1607669/full]
- 141. Chronic inflammation in the etiology of disease across ... [https://www.nature.com/articles/s41591-019-0675-0]