The Tug of War Within Us
How Opposite T Cell Personalities Control Our Health
Introduction: The Peacekeepers of Our Immune System
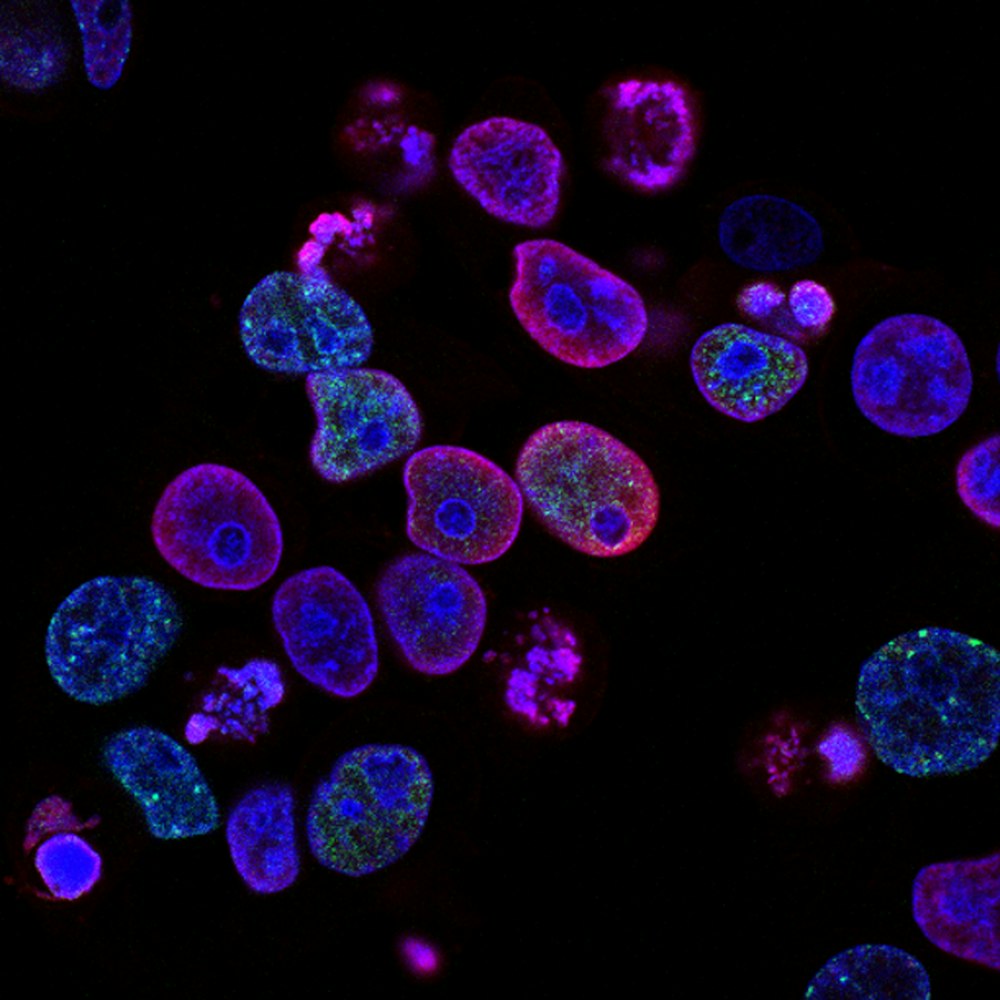
Imagine an intricate battlefield within your body where constant skirmishes determine your health—defenses against pathogens, repairs to damaged tissues, and unfortunately, sometimes friendly fire against your own cells. This is the reality of your immune system, a remarkably sophisticated network that requires not just soldiers but also dedicated peacekeepers to maintain order. Among these peacekeepers are regulatory T cells (Tregs), which specialize in suppressing excessive immune responses that could otherwise lead to autoimmune diseases like diabetes, multiple sclerosis, and rheumatoid arthritis.

For years, scientists viewed Tregs as a uniform population of suppressors. But groundbreaking research has revealed an unexpected diversity within these cells, with distinct subtypes that possess almost opposite functions. The discovery that the receptors TIGIT and CD226 mark these divergent Treg populations has revolutionized our understanding of immune regulation 1 4 . This article will explore how scientists uncovered these different Treg personalities and what this means for the future of treating diseases ranging from autoimmunity to cancer.
Tregs, Immune Balance, and the CD226/TIGIT Pathway
The Masters of Immune Control
Regulatory T cells, typically identified by their expression of the transcription factor FoxP3, serve as critical guardians of immune tolerance 5 . Without these cells, our immune systems would turn against our own tissues, a devastating consequence visible in both mice and humans lacking functional FoxP3. These specialized controllers employ multiple strategies to maintain peace, including:
- Releasing suppressive cytokines like IL-10 and TGF-β
- Disrupting cellular communication through molecules like CTLA-4
- Depleting essential nutrients from the environment through enzymes like CD39
Until recently, Tregs were considered a relatively uniform population, but advanced profiling techniques have revealed remarkable heterogeneity within these peacekeepers 4 . Scientists discovered that Tregs can be divided into different subsets based on their origin, activation status, and—most importantly—their expression of various surface receptors that dictate their function and stability.
Treg Functions
The Yin and Yang of Immune Regulation: CD226 and TIGIT
The CD226/TIGIT pathway represents a fascinating immune checkpoint system where competing receptors battle for influence over immune responses 6 . These two receptors engage in a molecular tug of war, competing for the same ligand (CD155) found on antigen-presenting cells and various tissue cells 4 .
CD226: The Accelerator
CD226 acts as an accelerator for immune responses. When engaged, it enhances T cell activation, promotes inflammatory cytokine production, and drives robust immune attacks . Not surprisingly, genetic variations in CD226 have been linked to increased susceptibility to various autoimmune conditions 4 .
TIGIT: The Brake
In contrast, TIGIT serves as a brake on immunity. This inhibitory receptor, containing an immunoreceptor tyrosine-based inhibitory motif (ITIM) in its cytoplasmic tail, dampens T cell activation and reinforces immune tolerance 8 . The balance between these opposing forces—the accelerator (CD226) and the brake (TIGIT)—helps maintain precise control over immune responses.
A Closer Look at the Key Experiment: Uncovering Treg Personalities
Methodical Investigation of Treg Subsets
To better understand the functional significance of CD226 and TIGIT expression on Tregs, researchers designed a comprehensive study to isolate and characterize these distinct subpopulations 1 4 . Their systematic approach involved:
Donor Selection & Cell Isolation
Collecting peripheral blood from healthy donors and isolating immune cells through density gradient centrifugation.
Cell Sorting & Separation
Using fluorescence-activated cell sorting (FACS) to precisely separate CD4+CD25+CD127lo/- Tregs into four distinct populations based on their expression patterns of CD226 and TIGIT.
In Vitro Expansion & Functional Assessment
Expanding these isolated subsets in culture under identical conditions to compare their proliferation rates, lineage stability, suppressive capability, and cytokine production profiles.
Epigenetic Analysis
Examining the Treg-specific demethylated region (TSDR) in the FOXP3 gene to assess the stability of Treg identity in each subset.
Revelatory Findings: Opposite Ends of the Regulatory Spectrum
The experimental results revealed striking functional differences between TIGIT-positive and CD226-positive Treg subsets that extended far beyond surface marker expression:
Functional Characteristics of Treg Subsets
| Treg Subset | Suppressive Capacity | Lineage Stability |
|---|---|---|
| TIGIT+CD226- | High | High (stable FoxP3) |
| TIGIT+CD226+ | Moderate-high | Moderate |
| TIGIT-CD226+ | Low | Low (FoxP3 loss) |
| TIGIT-CD226- | Low-moderate | Moderate |
Cytokine Production After Stimulation
| Treg Subset | IFN-γ | IL-10 | TNF-α |
|---|---|---|---|
| TIGIT+CD226- | Low | Moderate | Low |
| TIGIT+CD226+ | Moderate | High | Moderate |
| TIGIT-CD226+ | High | High | High |
| TIGIT-CD226- | Low | Low | Low |
Stable Tregs: TIGIT+
Perhaps most significantly, researchers discovered that TIGIT+ Tregs demonstrated remarkable lineage stability, maintaining high FoxP3 expression and strong suppressive function even after extensive expansion 1 4 . Epigenetic analysis confirmed that these cells showed complete demethylation of the FOXP3 TSDR, characteristic of thymically-derived Tregs with stable regulatory programming.
Plastic Tregs: CD226+
In contrast, CD226+ Tregs exhibited concerning plasticity, with many cells losing FoxP3 expression during expansion and gaining the ability to produce proinflammatory cytokines like IFN-γ—a hallmark of conventional effector T cells 4 . This functional divergence between TIGIT-positive and CD226-positive Tregs represents a critical dimension of immune regulation with far-reaching implications for human health and disease.
The Scientist's Toolkit: Research Reagent Solutions
Studying these intricate Treg subsets requires a sophisticated arsenal of research tools that enable precise identification, isolation, and functional characterization.
Surface Marker Antibodies
Anti-CD4, CD25, CD127, TIGIT, CD226
Identification & IsolationIntracellular Staining
Anti-FoxP3, Helios, IFN-γ, TNF-α
Lineage StabilityEpigenetic Analysis
TSDR methylation analysis
Lineage AssessmentBeyond the Lab: Therapeutic Implications and Future Directions
The Balance Gone Wrong: CD226/TIGIT in Human Disease
The discovery of functionally divergent Treg subsets has opened new avenues for understanding and treating human diseases. Research has revealed that the delicate balance between CD226 and TIGIT expression becomes disrupted in various pathological conditions:
Autoimmune Diseases
In autoimmune diseases like primary Sjögren's syndrome and dermatomyositis, scientists have observed abnormal increases in CD226+ T cells alongside expanded populations of TIGIT+CD226+ CD4 T cells with enhanced effector functions 6 9 . These dysregulated T cell populations correlate with disease activity and may contribute to the loss of self-tolerance that characterizes autoimmunity.
Cancer Environments
Conversely, in cancer environments, TIGIT expression often dominates on both Tregs and exhausted effector T cells, creating a powerfully immunosuppressive milieu that prevents effective antitumor immunity 7 8 . This discovery has positioned TIGIT as a promising target for cancer immunotherapy, particularly in combination with existing PD-1/PD-L1 blockade approaches.
Harnessing the Knowledge: Emerging Therapeutic Strategies
The growing understanding of CD226/TIGIT biology has inspired several innovative therapeutic approaches currently under investigation:
TIGIT Blockade in Cancer
Antibodies targeting TIGIT (such as tiragolumab) are being evaluated in clinical trials for non-small cell lung cancer and other malignancies 7 . These agents aim to release the brakes on antitumor immunity.
TIGIT Agonism in Autoimmunity
In autoimmune contexts, researchers are exploring TIGIT-activating approaches to enhance the stability and function of Tregs 3 . TIGIT agonism can boost Treg suppressive capacity and reinforce immune tolerance.
Cellular Engineering
The discovery that TIGIT+ Tregs represent a highly stable population has inspired efforts to engineer these cells for adoptive transfer therapies 5 , developing powerful treatments for autoimmune diseases.
Conclusion: A New Paradigm in Immune Regulation
The discovery of divergent Treg phenotypes marked by TIGIT and CD226 has fundamentally transformed our understanding of immune regulation. No longer can we view the peacekeepers of our immune system as a uniform population—instead, we recognize a spectrum of cellular personalities with opposing functions and therapeutic implications.
This more nuanced understanding helps explain why previous broad approaches to immune modulation often yielded inconsistent results and offers hope for more precisely targeted interventions. As research continues to unravel the complexities of the CD226/TIGIT axis, we move closer to a future where we can deliberately tip the balance toward health—whether by reinforcing immune tolerance in autoimmune disease or unleashing controlled immune attacks against cancer.
The journey from basic discovery to therapeutic application exemplifies how investigating fundamental biological questions can ultimately transform human health. The tug of war between CD226 and TIGIT within our bodies represents not just a regulatory mechanism for immunity, but a promising frontier for the medicine of tomorrow.